Highlights
-
•
Report of measles inclusion body encephalitis in child with leukemia.
-
•
It is necessary to determine antibodies to measles virus in the cerebrospinal fluid.
-
•
We found intrathecal synthesis of IgG antibodies to measles virus.
-
•
The disease had a dramatic course and ended in death.
Keywords: Measles, Leukemia, Measles inclusion body encephalitis, Infection, Children
Abstract
The measles epidemic was observed in Ukraine during 20172019. According to WHO, in Ukraine there was registered the highest number of measles cases in Europe during that period [8].
Measles is characterized by an acute course with fever, maculopapular rash, cough, conjunctivitis and can lead to central nervous system complications (encephalitis, encephalomyelitis) and bronchopulmonary system complications (laryngotracheobronchitis, bronchiolitis, pneumonia).
In immunocompetent patients, viremia ends after the end of clinical signs, in contrast to immunosuppressed individuals, who could develop viremia from one month up to a year.
We have described a case of measles inclusion body encephalitis (MIBE) or subacute measles encephalitis (SME) in an unvaccinated child with an acute lymphoblastic leukemia (ALL). The diagnosis was confirmed by the synthesis of IgG antibodies to the measles virus in the cerebrospinal fluid and by the MRI results. The disease had a dramatic course and ended in death.
Introduction
Measles is an acute infectious disease that is accompanied by maculopapular rash, fever, cough, coryza, conjunctivitis and Koplik’s spots which may appear two to three days after symptoms begin. The incubation period can last from 7 to 21 days [1].
Measles is one of the most common causes of morbidity and mortality among children globally, despite the availability and accessibility of safe and effective vaccine.
Generalized immunosuppression, which accompanies disease and can last for several weeks after apparent recovery, often leads to various complications [2].
The most common complication of the central nervous system is encephalitis. The measles virus causes 4 types of encephalitis, namely: acute measles encephalitis, acute disseminated encephalomyelitis, subacute sclerosis panencephalitis and measles inclusion body encephalitis [3].
Patients with a defect in cell-mediated immunity (due to immunosuppressive therapy or cancer) can have severe course of measles and atypical clinical presentation of the disease. Exanthem may be absent, evanescent, or severe and desquamative. Purpura has also been described. A high level of suspicion should be present when an immunocompromised host presents with pneumonia or encephalitis, particularly after measles exposure and despite history of previous immunization. (https://www.uptodate.com/contents/measles-clinical-manifestations-diagnosis-treatment-and-prevention) [9].
One of the severe complications in immunocompromised patients is measles inclusion body encephalitis (MIBE).
MIBE, also referred to as subacute measles encephalitis, acute encephalitis of the delayed type, and immunosuppressive measles encephalitis, is associated with immunodeficiency and typically develops within months of measles virus infection [4]. These patients usually present with seizures, often epilepsy partialis continua and an altered mental status.
Case report
A 5-year-old patient was admitted to the intensive care unit of Western Ukrainian Specialized Children's Medical Center on the 2nd of August 2018, with complaints about one-time vomiting, tonic-clonic seizures with loss of consciousness. All the symptoms developed at home. Simultaneously impaired consciousness, visual hallucinations, visual impairment, dysarthria and bilateral blepharoptosis developed. Patient’s condition was severe, RR-20/min, HR-81/min, SpO2−98%.Nervous system examination revealed general hypotonia, pupils D = S, photoreaction is depressed, tendon reflexes D = S, Achilles reflexes were depressed, meningeal symptoms were negative.
CBC (03.08.18): RBC-416 × 1012/l, HGB-125 g/dl, Plt-193 × 109 /l, WBC-166 × 109/l, neutrophils-95 %, lymphocytes-2%, monocytes-3%, ESR-32 mm/h.
Serologic tests for infections
IgG, IgM Borrelia burgdorferi – negative.
Ig G Toxoplasma gondii – positive (215 IU/mL), IgM – negative.
CSF investigation: PCR HV types 1,2,6, CMV – negative.
Ophthalmologist’s examination: macular edema of both eyes.
These symptoms developed in the background of complete remission of acute lymphoblastic leukemia, which had been established on 03/04/18. Child received a chemotherapy according to the ALL IC-BFM 2009 program.
Myelogram (3.04.18): lymphoblasts-76 %, normocytes-7%, Lym-11 %, GRN-6%.
The immunophenotype of blast cells:
| CD45−55% | CD33-(-) | CD2-(-) | CD10-(100 %) |
|---|---|---|---|
| CD34−84% | CD65-(-) | CD3-(-) | CD19-(100 %) |
| CD38−99% | CD13-(-) | CD4-(-) | CD20-(93 %) |
| Anti-MPO (-) | CD47-(-) | CD7-(-) | CD22-(98 %) |
| AntiTdT 86 | CD15-(-) | CD8-(-) | cCD79f-(100 %) |
Myelogram (7.05.18): blasts-3%, normocytes-12 %, Lym-61 %, GRN-22 %, MRD-negative.
The beginning of the chemotherapy took place on 04.04.18. On day 33 of the Protocol I remission stage was achieved.
In June 2018, she suffered measles (IgM antibodies to the measles virus were positive). The course of the disease was mild and ended up in recovery. During the hospitalization child received symptomatic and antibiotic therapy and was discharged home under the supervision of a hematologist. A month after measles, the protocol Mm was started (in order to prevent neuroleukemia) – methotrexate intravenously - at a dose of 2 g/m2 and methotrexate intrathecally 12 mg. A month after receiving the protocol the above-listed symptoms appeared.
Despite the treatment, the child's condition deteriorated progressively, neurologic deficit with the formation of right hemiparesis increased and complete blindness developed, consciousness-coma I. There was a weakening of swallowing and cough reflexes, tonic-clonic seizures on the right side. In the background of the bilateral pneumonia and respiratory distress the child developed seizure status with apnea.
It was decided to put the patient on a mechanical ventilation and then perform intraoperative tracheostomy.
Computed tomography of the chest: Atelectasis of the right upper lobe and subsegmental atelectasis on the left (S1/2,S7).
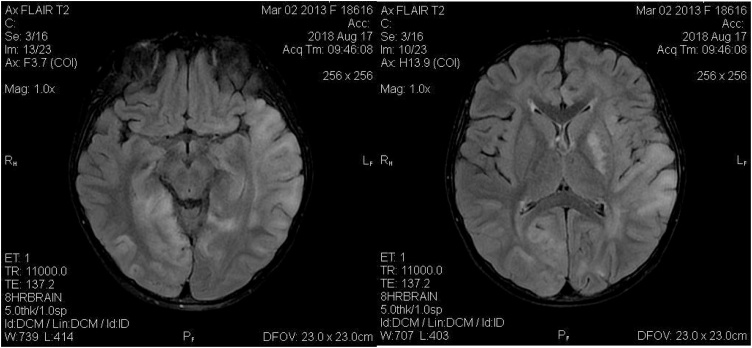
On MRI there was spread of diffuse multifocal lesions of the parenchyma of both cerebral hemispheres, formation of encephalomalacia sites in the parenchyma of both cerebral hemispheres, reduced volume of the cerebral hemispheres and cerebellum, MRI signs of inflammatory changes in the brain (Fig. 1).
Fig. 1.
MRI from 17.08.2018 shows diffuse multifocal lesions of the parenchyma of both cerebral hemispheres, progressive encephalopathy.
Such changes are typical for measles inclusion body encephalitis, in order to confirm which it is necessary to determine IgG, IgM antibodies to measles virus in the cerebrospinal fluid. In the child’s blood IgG and IgM antibodies to the measles virus were detected (IgM, IgG = 2.7, positive result>1.1).
MRI studies of the patient were sent to foreign colleagues and they shared our opinion on the diagnosis.
In Ukraine, the determination of antibodies to measles virus in cerebrospinal fluid cannot be performed, so this study was carried out in the laboratory of Germany (Dr. Rodger's laboratory). The study included a quantitative determination of IgG antibodies in serum and cerebrospinal fluid.
There was found intrathecal synthesis of IgG antibodies to measles virus.The resultsthat we received confirmed measles etiology and made it possible to establish the final diagnosis.
In the period of October 2018 - January 2019 the patient’s condition remained stably severe, coma I-III.
Atrophic changes in the brain increased (due to MRI results) and there was constant clonic twitching of eyebrows and the right hand. There was no photoreaction of the pupils.
During the hospitalization patient received therapy with corticosteroids, anticonvulsants (valproic acid, levetiracetam, benzobarbital), antibacterial and antifungal therapy(voriconazole, fluconazole, echinocandins) and symptomatic therapy. In spite of intensive and multicomponent treatment, the child's condition quickly deteriorated and remained severe due to neurological deficits.
In January 2019, due to the absence of changes or any improvement in the child's condition the child was dismissed home with the respiratory support on a portable mechanical ventilation and stayed at a home hospice.
On 25th of September 2019, child had a relapse of acute lymphoblastic leukemia, which was revealed by a regular complete blood count.
CBC: RBC-381 × 1012/l, HGB-12 g/dl, Plt-44 × 109/l, WBC-6,6 × 109/l, blasts-11 %, bands-29 %, metamyelocytes-3%, segmented neutrophils-10 %, lymphocytes-45 %, monocytes-2%.
The child's parents refused chemotherapy and in October 17, 2019 the child died.
Discussion
Encephalitis is the most frequent neurological complication of measles virus infection. Measles inclusion body encephalitis is one of the four types of measles-induced encephalitis and most commonly occurs in immunocompromised patients. The disease begins in 5 weeks-6 months (up to 1 year) after an acute course of measles with disorders in mental status and seizures, without fever [5]. Treatment is mainly symptomatic, supportive. Mortality according to many sources is> 75 % [6]
We conducted a differential diagnosis between PRES (posterior reversible encephalopathy syndrome) and progressive multifocal encephalopathy (PML).
PRES is a rare central nervous system (CNS) complication in patients with childhood hematologic-oncologic disease and shows various neurological symptoms between patients, ranging from numbness of extremities to generalized seizures. PRES represents with MRI findings of subcortical/cortical hyperintensity in T2-weighted sequences, more often observed in parietal-occipital lobes, accompanied by clinical neurologic alterations [7].
However, the child's condition progressively deteriorated and after repeated MRI we found negative dynamics and spread of diffuse multifocal lesions of the parenchyma of both cerebral hemispheres. Therefore, PRES syndrome was left out and progressive multifocal leukoencephalopathy was considered as one of the possible variants of the disease.
In order to confirm or exclude PML diagnosis, PCR analysis for the JC poliomavirus was performed and the result was negative.
The progressive deterioration of MRI results, transferred measles, antibodies synthesis against measles virus in the cerebrospinal fluid and a background disease allowed us to confirm the MIBE.
Children with acute lymphoblastic or myeloid leukemia, children undergoing immunosuppressive therapy after organ or bone marrow transplantation are at high risk for severe complications of measles, so alertness to this disease should be high.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Carol J. Baker, M.D. Faap, Red Book Atlas of Pediatric Infectious Diseases, 3rd edition. p.372-373.
- 2.Honda T., Yoneda M., Sato H., Kai C. Pathogenesis of encephalitis caused by persistent measles virus infection. Encephalitis. 2013:251–262. doi: 10.5772/54434. [DOI] [Google Scholar]
- 3.Katrak S.M., Mahadevan A., Taly Arun B., Sinha S., Shankar S.K. A 16-year old male with cortical blindness and focal motor seizures. Ann Indian Acad Neurol. 2010;13:225–232. doi: 10.4103/0972-2327.70887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bitnun A., Shannon P., Durward A., Rota P.A., Bellini W.J., Graham C. Measles inclusion-body encephalitis caused by the vaccine strain of measles virus. Clin Infect Dis. 1999;29(4):855–861. doi: 10.1086/520449. 15 August. [DOI] [PubMed] [Google Scholar]
- 5.Perry R.T., Halsey N.A. The clinical significance of measles: a review. J Infect Dis. 2004;189(SUPPL. 1):S4–S16. doi: 10.1086/377712. [DOI] [PubMed] [Google Scholar]
- 6.Fisher D.L., Defres S., Solomon T. Measles-induced encephalitis. QJM. 2015;108(3):177–182. doi: 10.1093/qjmed/hcu113. March. [DOI] [PubMed] [Google Scholar]
- 7.Arzanian M.T., Shamsian B.Sh, Karimzadeh P., Kajiyazdi M., Malek F., Hammoud M. Posterior reversible encephalopathy syndrome in pediatric hematologic-oncologic disease: literature review and case presentation. Iran J Child Neurol. 2014;8(2):1–10. Spring. [PMC free article] [PubMed] [Google Scholar]
- 8.Measles – European Region. Disease outbreak news - update 6 May 2019. https://www.who.int/csr/don/06-may-2019-measles-euro/en/.
- 9.2019. Measles: clinical. manifestations, diagnosis, treatment, and prevention-update Dec 05.https://www.uptodate.com/contents/measles-clinical-manifestations-diagnosis-treatment-and-prevention [Google Scholar]