Abstract
Background:
Post-traumatic stress disorder (PTSD) acts as a complex mental illness in which individuals are prone to long-lasting mental disorders after suffering traumatic events. PTSD is usually accompanied by some comorbidities, such as depressive disorder and sleep disorder, which seriously threaten patients’ life and health. Evidences showed that acupuncture could remarkably relieve the symptoms of PTSD patients. The review aims at assessing the safety and effectiveness exhibited by acupuncture for treating PTSD patients.
Methods and analysis:
The literature identified by searching 8 English electronic databases and 5 Chinese electronic databases from their inception to April 20, 2020 will be incorporated into the study. Two researchers will independently take charge of the research selection, the data extraction, as well as the assessment on research quality. The primary outcomes will be total PTSD symptoms, measured by different instruments including interviews and self-report measures. Data analysis will be performed via the RevMan 5 software, and Grading of Recommendations Assessment, Development, and Evaluation will help to assess the evidence level. A heterogeneity x2 test, the Higgins’ I2 test as well as visually inspecting the forest plot will help to investigate the heterogeneity of data. A sensitivity analysis and subgroup analyses will assist in investigating the sources of heterogeneity.
Ethics and dissemination:
The review neither assesses the individual information of patients nor impacts their rights, so it is not necessary for it to be approved by ethical institution. The article will be published in a peer-reviewed journal and present at relevant conferences.
OSF registration number:
Keywords: acupuncture, protocol, post-traumatic stress disorder, systematic review
1. Introduction
Post-traumatic stress disorder (PTSD) acts as a complex mental illness in which individuals are prone to long-lasting mental disorders after suffering traumatic events. Its core symptoms are classified into 4 clusters:
-
(1)
persistent event re-experiencing, for example, flashbacks and nightmares;
-
(2)
persistent avoidance regarding trauma-related stimuli and memories;
-
(3)
negative mood and cognitive changes, for example, a pervasive sense of imminent threat, uncontrollable thoughts and mood swings; and
-
(4)
obvious reactivity and arousal changes, for example, panic attacks, hypervigilance, depression, and insomnia.[1–3]
What's more, PTSD is usually accompanied by many comorbidities, such as depressive disorder, anxiety disorder, and sleep disorder, which seriously threaten patients’ life and health.[4] A study[5] showed that the overall prevalence of PTSD was about 11%. PTSD annual prevalence was found to be 1.1% in transnational samples from 27 countries.[6] In the United States, the incidence of PTSD is up to 3.5%, much higher than that of other mental disorders. According to a survey, many veterans were diagnosed with PTSD, and their prevalence was as high as 23%.[7] At present, first-line therapies[8] for PTSD include:
-
(1)
Psychotherapy. The most common psychotherapy for PTSD treatment is cognitive-behavioral therapy, including trauma focused exposure therapy, cognitive restructuring therapy, and stress inoculation therapy, and so on;
-
(2)
Pharmacotherapy. Only 2 kinds of medicines, namely, paroxetine and sertraline, are approved by FDA for treating PTSD.[9]
In addition, venlafaxine and nefazodone have also been recommended for PTSD.[10] They are antidepressants in the class of selective serotonin reuptake inhibitors (SSRIs). Despite the good tolerance of SSRIs treatment, the anxiety symptoms, jitteriness, restlessness, headache or insomnia increase in the first few days or weeks following treatment and there are other side-effects including nausea, anorexia fatigue, dizziness, and weight gain, which may affect the compliance of patients.[11] Currently, commonly used SSRIs class antidepressants and venlafaxine are not recommended as first-line drugs.[12] Acupuncture, as a classic traditional Chinese medicine therapy, has played a full advantage in mental diseases such as depression, anxiety, and insomnia. Acupuncture is accepted by the majority of patients. Evidences showed that acupuncture could remarkably relieve the symptoms of PTSD patients.[9,13,14] The study aims at assessing the treatment effectiveness and safety of acupuncture for PTSD patients.
2. Methods
2.1. Study registration
This systematic review protocol has been registered on Open Science Framework platform and the registration number is https://osf.io/dc3js.
The written document of the systematic review protocol followed the statement guidelines of preferred reporting items for systematic reviews and meta-analyses protocols.[15]
2.2. Inclusion and exclusion criteria regarding study selection
Inclusion criteria: All randomized controlled trials (RCTs) of using acupuncture to treat PTSD. The review will be presented only in Chinese and English. Exclusion criteria: Non-RCTs, quasi-RCTs, animal studies, case series, and reviews.
2.3. Types of participants
Participants refer to patients clinically diagnosed with PTSD. No restrictions exist regarding gender, nationality, educational background, job, and ethnicity. Participants will include, but not be limited to, combat veterans, war refugees, earthquake survivors, male and female prison inmates, socially disadvantaged persons, police officers, firefighters, as well as nurses and doctors under stress.
2.4. Types of interventions
2.4.1. Experimental interventions
The experimental group will consist of patients receiving manual acupuncture, body acupuncture, electroacupuncture and other types of acupuncture treatment, as well as those receiving treatment combined with acupuncture.
2.4.2. Control interventions
The control group will consist of patients receiving control interventions like sham acupuncture, placebo acupuncture, western medicine, routine care, herbs, conventional therapy or no treatment (waiting list control).
2.5. Types of outcome measures
2.5.1. Primary outcomes
The primary outcomes will be total PTSD symptoms, measured by different instruments including interviews and self-report measures. Interviews will include, but not be limited to, Clinician-Administered PTSD Scale for DSM-5,[16] PTSD Symptom Scale Interview (PSS-I and PSS-I-5),[17] Structured Interview for PTSD,[18] Structured Clinical Interview: PTSD Module,[19] and Short PTSD Rating Interview.[20] Self-Report Instruments will include, but not be limited to, Davidson Trauma Scale,[21] Impact of Event Scale-Revised,[22] Modified PTSD Symptom Scale,[23] PTSD Checklist for DSM-5,[24] and PTSD Symptom Scale Self-Report Version.[25]
2.5.2. Secondary outcomes
If there are no interviews or self-report measures in the study, the descriptions of PTSD symptoms will be categorized as secondary outcomes.
3. Search methods for study identification
3.1. Electronic searches
Electronic searches will focus on databases of Nature, Science Online, PubMed, the Cochrane Library, MEDLINE, WorldSciNet, EMbase, Allied and Alternative Medicine, the Wanfang Databse, China Biology Medicine Disc, China National Knowledge Infrastructure, the Chongqing VIP, and Chinese Science and Technology Periodical Database, with the temporal from the inception of database to April 20, 2020.
3.2. Other search resources
Manually retrieving and reviewing a reference list of those potential and qualified studies together with relevant system reviews will help to confirm the location of other RCTs. Researchers will contact the author of trial for getting the latest clinical data for the convenience of ongoing RCTs.
3.3. Search strategy
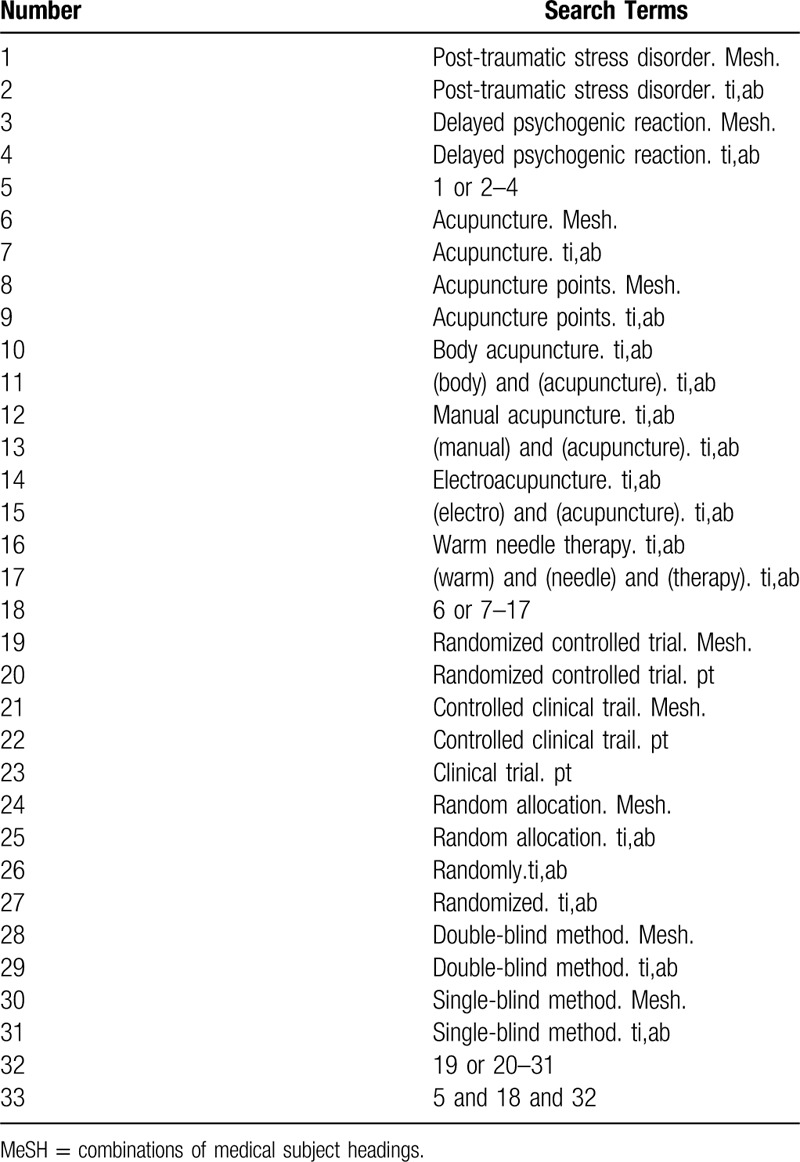
Search terms will include 2 parts: PTSD (“post-traumatic stress disorder,” and “delayed psychogenic reaction”) and acupuncture (“acupuncture,” “acupuncture points,” “body acupuncture,” “manual acupuncture,” “electroacupuncture,” and “warm needle therapy”). Terms of “zhenjiu,” “zhenci,” “dianzhen,” “wenzhen,” “chuangshanghouyingjizhangai,” “chuangshanghouyalixinlizhangaizheng,” “yanchixingxinyinxingfanying,” “chuangshanghouyalifanying,” and “suijiduizhao” will be adopted from the Chinese databases. By multiple searches and proper modifications, the final search strategy of each database will be determined. Table 1 lists the search strategy specific to the PubMed database.
Table 1.
Search strategy for the PubMed database.
4. Data collection and analysis
4.1. Study selection
After the independent information extraction from literature included in the study, 2 researchers will input the extracted information into a unified statistical table of data. Ineligible studies as well as duplicate records will be first eliminated, followed by a review on the full text of eligible studies for confirming their compliance to the abovementioned inclusion criteria. If the 2 researchers cannot come to an agreement, the final judgement will be made by a third researcher. A research flowchart will be drawn to show the whole process of study selection (Fig. 1).
Figure 1.
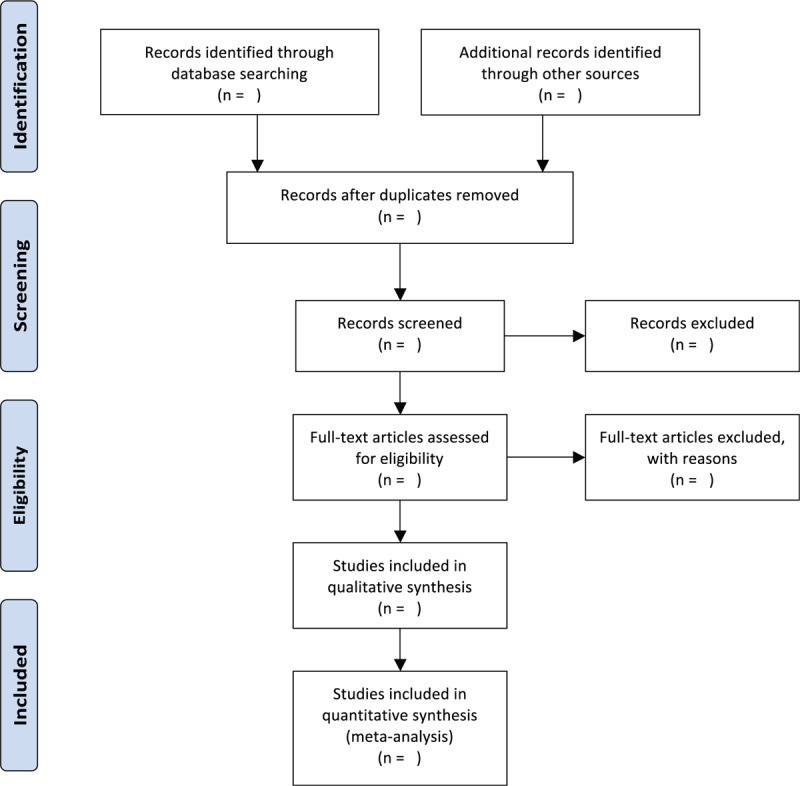
Flowchart of study selection.
4.2. Data extraction and management
Information of the title, the reference ID, the first author, year of publication, age of patient, intervention type, control intervention type, intervention group's sample size, intervention time, randomization, measure of outcome, allocation concealment method, blinding method, primary outcomes, follow-up duration, fund source and type, as well as a list of the standards for Reporting Interventions in controlled trials of acupuncture will be extracted from each study. Researchers will contact the author of study in the case of insufficient reported data. If negotiation cannot help to come to an agreement of the extraction of data, the final judgement will come to a third researcher.
4.3. Assessment of risk of bias in included studies
Two researchers will adopt the Cochrane collaboration risk-of-bias assessment for assessing the quality of literature included in the review independently, together with completing the standards for Reporting Interventions in controlled trials of acupuncture checklist.[26] Assessments include selective reporting, random sequence generation, allocation concealment, incomplete outcome data, blinding as well as other possible biases. Related standards proposed in the Cochrane Intervention System Assessment Manual will be considered to classify risk of bias into 3 levels, low risk, high risk, and unclear risk. Discussion will be performed to resolve the discrepancy and a third research will take charge of making the final judgement if the 2 researchers cannot come into an agreement via discussion.
4.4. Treatment effect measures
Odds ratios and MS and standardized mean difference will assist in measuring the treatment effects specific to dichotomous outcomes and continuous outcomes, respectively. All these outcomes report 95% confidence interval (CI).
4.5. Missing data management
The reason for the loss of data missed in the period of data screening and extraction will be identified in the review. Corresponding author will be contacted for obtaining missing data. With missing data unable to be obtained, available data will be analyzed only and the reason and effect of such exclusion will be explained.
4.6. Heterogeneity assessment
Meta-analysis will be carried out with the help of a random- or fixed-effects model. Cochrane Handbook for Systematic Reviews of Interventions describes that either visually inspecting forest plot, a heterogeneity x2 test, or the Higgins’ I2 statistic can help to assess the heterogeneity.[27,28] The data will be pooled by a fixed-effects model with P-value over .10 and the I2 value less than 50%, and by a random-effects model in other cases. When a set of studies exhibit an obvious heterogeneity, factors leading to the heterogeneity will be discussed, like the characteristics of patients and the variation degree in interventions. The heterogeneity will be evaluated via the subgroup analysis or the sensitivity group if applicable.
4.7. Reporting bias assessment
The biases of reporting will be assessed by virtue of a funnel plot if there are more than 10 trails in the meta-analysis. The asymmetry exhibited by the funnel plot will be evaluated via the Egger and Begg tests, and P-value < .05 means the publication bias is significant.
4.8. Data synthesis
Data analysis will rely on the RevMan 5 software (V. 5.3; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). The heterogeneity degree will help to confirm the model type, a random-effects model or a fixed-effects model. The 2 categorical variables will adopt the index of risk ratio or odds ratio and 95% CI. Continuous variables will adopt the index of WMD or standardized mean difference and 95% CI. Meta-analysis will not be conducted if no assessment, like subgroup analysis, is able to explain the existing meaningful heterogeneity. The subgroup analysis shall carefully consider each subgroup in certain case.
4.9. Subgroup analysis
Subgroup analyses will consider the heterogeneity exhibited by the acupuncture type (such as manual acupuncture, body acupuncture, or electroacupuncture), the control type (placebo or sham acupuncture, no acupuncture, medical treatment or conventional therapy), the acupoint and the clinical difference.
4.10. Sensitivity analysis
For testing if review conclusions are robust, primary outcomes will receive a sensitivity analysis based on the criteria involving the size of sample, the quality of heterogeneity, and the statistic model (a random-effects model or a fixed-effects model).
4.11. Evidence quality grading
The evidence quality of obtained results will be assessed via the Grading of Recommendations Assessment, Development, and Evaluation method.[29] The assessment contains risk of bias exhibited by studies, heterogeneity, evidence directness, estimate effect precision, and risk of bias of publication. We will divide evidence into 4 categories considering the level, namely high, moderate, low, and very low risk.
4.12. Ethics and dissemination
The results of system review will be published in journals reviewed by peers, disseminated at related conference or publications reviewed by peers. The review neither assess individual information of patients nor affect their rights, so it does not need to be approved by ethical institution.
5. Discussion
PTSD acts as a complex psychological disease due to patients’ being exposed to traumatic events. It is mainly characterized by persistent even re-experiencing; persistent avoidance of trauma-related stimuli and memories; negative mood and cognition changes; and obvious reactivity and arousal changes. In more than 50% of cases, patients with PTSD are usually accompanied by other comorbidities, such as anxiety and substance-use disorders.[30] The persistent condition can interfere patients with relationships, ability to hold a job, the quality of life, and overall health. What's worse, a study shows that PTSD is associated with internal disease, serious disability, and premature death.[31] Based on the above situation, early identifying symptoms together with the prevention and intervention programs will assist in reducing the occurrence of PTSD and other mental diseases.[8] Therapies for PTSD include psychological, pharmacologic, and other alternative interventions.[3] Psychotherapy and pharmacotherapy are the conventional methods for treating PTSD patients, the latter includes anxiolytic drugs and antidepressants. However, as revealed by research, the response to abovementioned therapies, and their side effects are significantly different.[4] Hence, it is necessary to develop better therapies for PTSD treatment.
Traditional Chinese medicine is used to treat disease itself rather than only symptoms. Acupuncture, accepted by the majority of patients,[32] offers a new option to help patients solve mental issues caused by traumatic events. There are growing clinical and experimental evidences for promoting acupuncture to be applied for different mental health disorders. A study, to evaluate if electroacupuncture is safe and efficient, includes 138 patients who had PTSD caused by earthquake. The results show that electroacupuncture is significantly effective compared with previous treatment, in addition, the electroacupuncture group exhibits a stronger efficacy relative to the paroxetine group.[33] Moiraghi et al suggest that acupuncture may serve as a helpful intervention tool for public health, which could quicken the psychologic health recovery speed in disaster-stricken areas.[2] According to the research, acupuncture can affect the autonomic nervous system, and the prefrontal as well as limbic brain structures, making it able to relieve the symptoms of PTSD.[34]
The review holds the purpose of providing extra relevant knowledge regarding the available option and clinical application to clinicians. Meanwhile, the resulting evidence of this review may contribute to essential information that can help health policy makers, practitioners, acupuncturists, and patients.
Author contributions
Conceptualization: Ning Ding, Linzhi Li, Kai Song.
Data curation: Ning Ding, Linzhi Li, Kai Song.
Formal analysis: Kai Song, Ailing Huang.
Funding acquisition: Ning Ding, Rensong Yue.
Methodology: Ailing Huang.
Project administration: Ning Ding, Linzhi Li, Kai Song.
Writing – original draft: Ning Ding, Linzhi Li.
Writing – review & editing: Hong Zhang.
All authors read the article and approved it for publication.
Footnotes
How to cite this article: Ding N, Li L, Song K, Huang A, Zhang H. Efficacy and safety of acupuncture in treating post-traumatic stress disorder: a protocol for systematic review and meta-analysis. Medicine. 2020;99:26(e20700).
Abbreviations: CI = confidence interval, MD = mean difference, PTSD = post-traumatic stress disorder, RCTs = randomized controlled trials, SSRIs = selective serotonin reuptake inhibitors.
ND and LL contributed equally to this study.
This work was supported by the National Natural Science Foundation of China (no. 81873384).
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Farooqui M, Quadri SA, Suriya SS, et al. Posttraumatic stress disorder: a serious post-earthquake complication. Trends Psychiatry Psychother 2017;39:135–43. [DOI] [PubMed] [Google Scholar]
- [2].Carlo M, Paola P, Antonio P. An observational study on acupuncture for earthquake-related post-traumatic stress disorder: the experience of the lombard association of medical acupuncturists/acupuncture in the world, in Amatrice, Central Italy. Med Acupunct 2019;31:116–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N Engl J Med 2017;376:2459–69. [DOI] [PubMed] [Google Scholar]
- [4].Matthew J, Bruce C, Matthew F. Pharmacotherapy for posttraumatic stress disorder: review with clinical applications. J Rehabil Res Dev 2012;49:703–5. [DOI] [PubMed] [Google Scholar]
- [5].Katherine P, Josie MS, Aimée G, et al. Prevalence of PTSD and common mental disorders amongst ambulance personnel: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol 2018;53:897–909. [DOI] [PubMed] [Google Scholar]
- [6].Karam EG, Friedman MJ, Hill ED, et al. Cumulative traumas and risk thresholds: 12-month PTSD in the World Mental Health (WMH) surveys. Depress Anxiety 2014;31:130–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jane M, Kristina J, Shayna B, et al. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychol Addict Behav 2016;30:743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kim YD, Heo I, Shin BC, et al. Acupuncture for posttraumatic stress disorder: a systematic review of randomized controlled trials and prospective clinical trials. Evid Based Complement Alternat Med 2013;2013:e615857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wynn GH. Complementary and alternative medicine approaches in the treatment of PTSD. Curr Psychiatry Rep 2015;17:62. [DOI] [PubMed] [Google Scholar]
- [10].Lee DJ, Schnitzlein CW, Wolf JP, et al. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety 2016;33:792–806. [DOI] [PubMed] [Google Scholar]
- [11].Bandelow B, Zohar J, Hollander E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders – first revision. World J Biol Psychiatry 2009;9:248–312. [DOI] [PubMed] [Google Scholar]
- [12].National Collaborating Centre for Mental Health (NCCMH). Post-traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. England: The Royal College of Psychiatrists; 2005. [Google Scholar]
- [13].Yang QF, Ding JC, Qi ZZ, et al. Comparative research on intervention in anxiety behavior of PTSD-like rats by electro-acupuncture and repetitive transcranial magnetic stimulation and serum corticosterone. J Nanjing Univ Tradit Chin Med 2012;28:357–9. [Google Scholar]
- [14].Hickey AH. Adding a Face and the Story to the Data: Acupuncture for PTSD in the Military. Cambridge: Springer International Publishing; 2015. [Google Scholar]
- [15].Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Weathers FW, Bovin MJ, Lee DJ, et al. The clinician-administered PTSD scale for DSM-5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychol Assess 2018;30:383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Foa EB, Riggs DS, Dancu CV, et al. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress 1993;6:459–73. [Google Scholar]
- [18].Davidson JR, Malik MA, Travers J. Structured interview for PTSD (SIP): psychometric validation for DSM-IV criteria. Depress Anxiety 1997;5:127–9. [DOI] [PubMed] [Google Scholar]
- [19].First MB, Spitzer RL, Miriam G, et al. User's Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders: SCID-I: Clinical Version. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- [20].Connor KM, Davidson JR. SPRINT: a brief global assessment of post-traumatic stress disorder. Int Clin Psychopharmacol 2001;16:279–84. [DOI] [PubMed] [Google Scholar]
- [21].Davidson JR, Book SW, Colket JT, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med 1997;27:153–60. [DOI] [PubMed] [Google Scholar]
- [22].Mark C, Richard B, Salvina F. Psychometric properties of the impact of event scale - revised. Behav Res Ther 2003;41:1489–96. [DOI] [PubMed] [Google Scholar]
- [23].Falsetti SA, Resnick HS, Resick PA. The modified PTSD symptom scale: a brief self-report measure of posttraumatic stress disorder. Behav Ther 1993;16:161–2. [Google Scholar]
- [24].Blevins CA, Weathers FW, Davis MT, et al. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 2015;28:489–98. [DOI] [PubMed] [Google Scholar]
- [25].Edna BF, Laurie C, Lisa J, et al. The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Eur J Psychol Assess 1997;9:445–51. [Google Scholar]
- [26].Cochrane, Julian PT. Assessing Risk of Bias in Included Studies. Cochrane Book Series. 2008. [Google Scholar]
- [27].Cochrane: The Cochrane Statistical Methods Group, Deeks JJ, Higgins JP, Altman DG. Analysing Data and Undertaking Meta-Analyses. 2008. [Google Scholar]
- [28].Higgins JT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [29].Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pietrzak RH, Goldstein RB, Southwick SM, et al. Prevalence and axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord 2011;25:456–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Schlenger WE, Corry NH, Williams CS, et al. A prospective study of mortality and trauma-related risk factors among a nationally representative sample of vietnam veterans. Am J Epidemiol 2015;182:980–90. [DOI] [PubMed] [Google Scholar]
- [32].King HC, Spence DL, Hickey AH, et al. Auricular acupuncture for sleep disturbance in veterans with post-traumatic stress disorder: a feasibility study. Mil Med 2015;180:582–90. [DOI] [PubMed] [Google Scholar]
- [33].Wang Y, Hu Y, Wang W, et al. Clinical studies on treatment of earthquake-caused posttraumatic stress disorder using electroacupuncture. Evid Based Complement Alternat Med 2012;2012:e431279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Helané W, Angela S, Rachel N, et al. Complementary and alternative medicine for posttraumatic stress disorder symptoms: a systematic review. J Evid Based Complementary Altern Med 2014;19:161–75. [DOI] [PMC free article] [PubMed] [Google Scholar]


