Abstract
Trismus is a frequent complication of healed Noma infection and is caused by soft tissue and muscle contraction. Free-flap surgery is recommended to replace the missing oral mucosa and soft tissue. However, significant complications can occur if this surgery is performed in places like Africa, where conditions are usually less than optimal. In 2007, the authors started to treat patients with trismus in Niamey, Niger by distracting the soft tissue and muscle constriction between the jaws with a bone distractor continuously for 1 month with the aim of achieving a mouth opening of 3 cm. The distraction was limited to 1 mm/d. performed under local anesthesia with some sedation. Minor complications such as infection in the pin holes were easily managed. In 2009, 2 patients with trismus after Noma with a follow-up of 2 years were reported. Till date, the authors have successfully performed trismus release in more than 69 patients in Niamey and Guinea Bissau. The present study analyses the results of distraction therapy in 40 patients with follow-ups until 60 months. At the end of distraction, the mean interincisal distance was 2.7 ± 0.5 cm. Mouth opening 6 months after distraction had not reverted. However, 3 to 5 years after treatment, some signs of relapse were detected, with an average mouth opening of 1.5 ± 1.9 cm. Physiotherapy was unfortunately not feasible. The presented results strongly support the efficacy of distraction therapy to correct trismus in Noma patients.
Keywords: Distraction, Noma, trismus
Noma is a type of facial tissue gangrene that destroys the oral mucous membranes, the soft cheek tissue, and the maxilla and mandible. This disease is caused mainly by malnutrition and systemic illness such as measles, scarlet fever, and tuberculosis that negatively affect general health. Noma is endemic mainly in the sub-Saharan region; the estimated frequency in some communities may vary from 1 to 7 patients per 1000. Noma most often begins as an atypical periodontal infection in children aged between 2 and 16 years.1 The gums and buccal mucosa become inflamed and develop necrotizing ulcers. If the infection spreads to the skin and bone of the cheek, it destroys the orofacial tissues and other neighboring structures. Loss of extensive facial tissue, general sepsis, and even death may occur.1,2
Healing in the cheek is followed by fibrous tissue development; additionally, a reflex muscle spasm of the closing muscles of the jaw (temporalis, masseter, and pterygoideus medialis) often follows the early inflammatory state. Trismus, lockjaw, or extraarticular ankylosis is a frequent consequence of a healed Noma infection and causes restricted mouth opening (MO). In the pterygoid and masseter muscles, ossification, and dystrophic calcification may occur combined with osseous overgrowth; in some patients, this can result in bony ankyloses, a true bony fusion between the mandible and the maxilla.3 Very rarely, articular ankylosis of the temporomandibular joints occurs. In 30% to 43% of Noma patients, trismus or extraarticular bony ankylosis of the mandible, maxilla, and zygoma has been found, in this order of frequency; such ankylosis is mostly unilateral.3
Trismus causes numerous complications. Eating is extremely difficult and only possible if the food is in smaller-sized morsels. Small food particles may enter the mouth through existing tiny interdental gaps. Younger Noma patients are usually already malnourished, underweight, anemic, and have growth difficulties; additional feeding problems compound the issue. Speech defects prevent social contacts and personal development. Surgical correction of restricted MO in Noma patients mostly needs replacement of missing mucosal lining and scar tissue with local or distant skin flaps.2–4 This surgical procedure can be difficult to perform in Africa. Especially, the free flap procedure is associated with numerous risks if performed in the 3rd world.
In 2009, we published a paper on the possibility of distracting the scar formation between the jaws without surgical release to correct trismus.5 This was achieved with a bone distractor, originally prepared for distraction osteogenesis of the mandible. The question was whether the scar tissue can be distracted by 1 mm/d until an acceptable MO is achieved. In this study, we described use of the distraction procedure in 2 patients with post-Noma trismus and demonstrated successful MO with a follow-up period of 2 years. These encouraging results caused us to proceed with this concept in patients with fibrotic constricting trismus in Africa.
Our earlier published manuscript5 on distracting the soft-tissue scar in the cheek in patients with Noma infection was based on the concept of soft-tissue adaptation following bone distraction.6 Several studies concerning soft-tissue behavior after maxillary or mandibular distraction demonstrated soft-tissue changes in the upper face, lower face, nasal soft tissue, and lower and upper lip regions.7 Other studies8 have reported augmentation or lengthening of hard- and soft-tissue elements after distraction osteogenesis. It has been shown through computed tomography scans that mandibular distraction not only lengthens the affected skeleton but also expands the associated soft-tissue envelope.9
Muscle inactivity due to long-standing soft-tissue ankylosis leads to shortening of the temporalis, masseter, and medial pterygoid muscles, not only on the infected but also on the opposite side.
Animal experiments on lower extremity skeletal distraction have demonstrated an adaptation of the attached muscles by an increase in type I collagen cross-linking, myoblast proliferation, and fusion.9–11
The obvious plasticity of soft tissue seen during bone distraction encouraged us to extend the MO-limiting scar tissue and muscles by performing slow distraction (1 mm/d). Usually this tissue, located in the cheek and molar region, needs to be extended only by 1.5 to 2 cm to achieve an interincisal distance of 3 cm (Fig. 1A).
FIGURE 1.
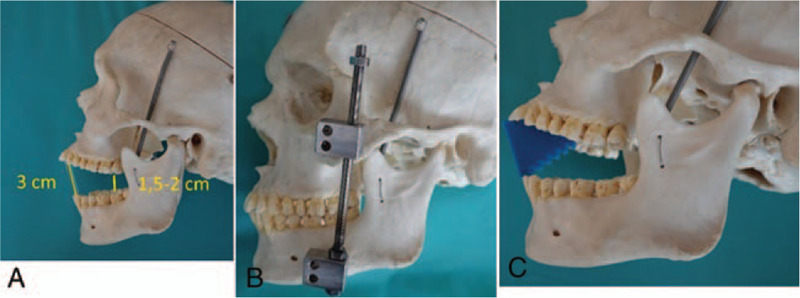
(A) Cadaver skull measurements demonstrating that an interincisal distance of 3 cm means that the distance between the molars, where the soft-tissue constriction is usually located, is only between 1.5 and 2 cm. This is the amount of scar distraction needed to achieve an acceptable mouth opening of 3 cm. (B) A skull with the distractor positioned in the zygoma bone, 1 cm caudal of the lateral eye canthus and in the mandibular bone, lateral to the mental foramen. (C) Medical grade silicon block with the widest dimension of 3 cm to be used as a spacer between the incisors at night. Position demonstrated on a skull.
An MO of 3 cm is an acceptable result in trismus patients after Noma.18,19
We decided to treat such trismus patients only by distracting the scar tissue and the constricted chewing muscles by 1 mm daily for 30 days. According to our experience, an acceptable MO of 3 cm is usually obtained after 30 days of distraction. To prevent relapse, the distractor was left attached to the bone for another 30 days.
METHODS
Since our 1st publication in 2009,5 we have treated 69 Noma patients with trismus in Niamey and Guinea Bissau, Africa. This study was undertaken between November 2006 and December 2017.
A cheap and simple 1-dimensional distractor was fixed between the zygoma and mandible (Fig. 1B).
Patients with trismus due to a healed Noma infection and those who had undergone reconstructive surgery for facial soft-tissue defects were accepted for distraction therapy. Noma patients with bony ankyloses of the jaw or patients with Pierre Robin syndrome were excluded.
We treated a total of 61 patients in Niamey, Niger and 8 patients in Guinea Bissau.
In most patients, written records were unavailable in Niamey, Niger. To exclude patients with bony ankyloses, since radiographs were unavailable, we asked the patients to open the mouth and move the jaw as much as possible to diagnose bony ankylosis. Only patients with some movement between the jaws, mostly <1 to 2 mm and often in a horizontal direction, were included. Patients with no movement at all were identified as having bony ankylosis between the maxilla and the mandible and were excluded. The general health situation was checked clinically by checking the blood pressure and temperature; examining the heart and lungs; and blood analysis for malaria, hepatitis B and C, human immunodeficiency virus, C-reactive protein, and red and white blood cell count.
Distraction was performed in a local hospital belonging to the German Hilfsaktion Noma foundation. The patients were placed in the supine position. Using local anesthesia and mild sedation, a step incision was taken on the skin above the body of the zygomatic bone, 1 cm below the lateral eyelid canthus. Through the skin incision, a pin with a cutting thread was drilled into the body of the zygoma bone. A hand-driven drill was used to bolt up the pin until it was stably attached to the bone. A 2nd pin was drilled into the mandible lateral to the mental foramen to achieve the proper direction of distraction; this was found to be the ideal location to ensure the correct vector for distraction.
The day after surgery, we started by distracting 1 mm on each side; we continued distracting by 1 mm daily for 30 days. Usually, an interincisal distance of 3 cm was achieved 30 days after beginning the procedure. The distraction procedure was painless if the distraction was limited to 1 mm/d.
The patients were observed in the hospital during distraction; if a pin became unstable or infected, we replaced it with another pin placed close by. No other complications occurred in this period. The patients could eat and drink normally during this process.
To keep the MO result as stable as possible, we decided to retain the distractors in place for another month; they were removed 2 months after beginning distraction.
To reduce the relapse of trismus, patients were asked to perform physiotherapy with a spacer between the incisors at night for at least a year after therapy, but they were not supplied with a spacer and this was not controlled by the hospital authorities.
To evaluate the long-term outcome of his new treatment in Africa, we tried to control the MO of our patients. Since most patients lived at long distances, the follow-ups were insufficient. Local hospital staff was not available as needed to control the results of therapy in every patient.
RESULTS
We could follow-up consistently with 40 patients who were treated in Niamey.
Figure 2 shows an 8-year-old boy with a typical early result of distraction therapy.
FIGURE 2.

An 8-year-old patient with trismus following Noma infection before treatment (A), with the distractor in place 3 weeks after beginning of distraction (B), and 6 months after treatment (C).
In some patients, the follow-ups continued for up to 5 years postoperatively. The remaining 21 patients could not be followed due to inconsistent availability of local staff and lack of patient compliance. The distraction worked in every patient, with a mean interincisional distance of 2.7 cm at the end of 30 days’ therapy.
The target distance of 3 cm was not reached in every patient due to lack of follow-up by patients or unavailability of local staff. Some patients lost their motivation to continue the distraction. The controlled mean MO in 22 patients at 6 months was 3 ± 1.6 cm.
After 6 months, the MO was found to continually reduce; this was considered a sign of trismus relapse. The long-time measurements in 22 patients 3 to 5 years posttreatment resulted in a mean distance of 1.5 cm MO and a standard deviation of 1.9 cm.
The demographic data of the patients demonstrating the individual results of distraction in 40 patients, in 23 patients up to 60 months, is provided in Supplemental Digital Content, Table 1.
Statistical Analysis
The average distance at the end of the distraction was 2.7 ± 0.5 cm, which differs significantly from a preoperative value of 0 (t = 32.2, df = 39, P < 0.001). All (100%) patients had an MO of over 1, 1 cm, and 3 to 5 years afterwards, 5% had an MO of >1 cm. The values of measurements of the years 1 to 5, marked in red in the Table 2 are not statistically significant due to the fragmentary members of values (Supplemental Digital Content, Table 2).
Figure 3 shows box plots of MO distribution after distraction and all follow-ups.
FIGURE 3.
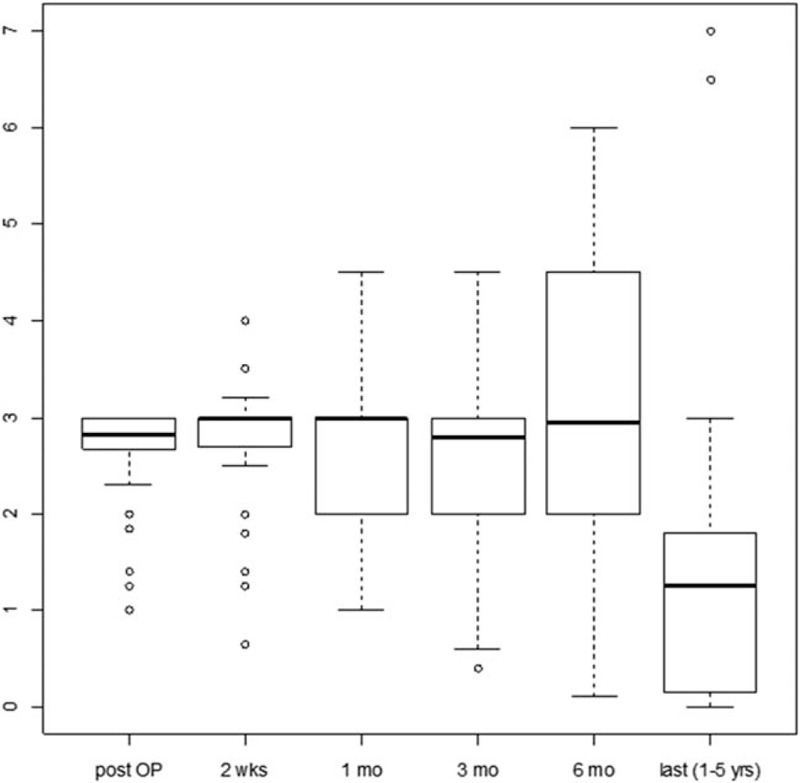
Box plots of mouth opening distribution at postoperative and follow-up, showing the distribution of mouth opening during all measurements. The bold lines indicate the median mouth opening and the rectangles indicate the Q1-Q3 interval.
DISCUSSION
To the best of our knowledge, there are few long-term follow-up studies concerning surgical release of trismus in Noma patients.
In 2016, Baumann12 published a review study on surgery for extra-articular trismus. The studies including all reasons of trismus, not only Noma, showed a mean postoperative gain of approximately 2 cm in MO; with an average MO of 1.9 cm during follow-ups of 6 months to 2 years. Patients with Noma were a special category in this survey because of the limited resources for treatment due to poverty. It was found that patient compliance had a significant impact on the long-term result.
Dammer13 published the results of trismus correction with temporalis muscle flaps in 14 patients with a follow-up period of 2 years. The MO postoperatively was 1.5 to 3.4 cm, with a reduction of 50% after 2 years.
Oluwasanmi et al2 reported the results of distraction in 30 patients, but without long-term follow-up. Among the 30 patients, 8 had full MO, among whom 3 had satisfactory results. Surgery failed in 7 patients although postoperative physiotherapy was mandatory. Multiple operations during admission to the hospital were usually necessary.
Adams-Ray et al14 stated that an MO >3 cm was a good result, while that >2 cm was acceptable. However, they performed surgery using a flap for the inner and outer lining; in 9 of 10 patients, an MO of >2 cm was seen. However, they did not provide any follow-ups.
Giessler et al15 reported 2 patients with trismus due to a Noma infection. The facial defect and trismus was reconstructed with free flaps. After 6 months, an MO of 2 to 2.5 cm was obtained.
Giessler et al published another study in 2005,16 an overview of 31 patients, all treated with free flap surgery. Three flaps failed completely and 1 partly; 4 patients showed minor wound infection.
Bisseling et al17 published a study performed in Africa that had a long-term follow-up. The mean MO in this group was 1.03 cm after a mean follow-up of 43 months. A better MO was observed in patients who continued physiotherapy after discharge.
Pittet18 published postoperative results of 32 patients treated in Switzerland, with a mean MO of 2.5 and 2 cm after 6 months. However, 20 months after surgery, the MO was only 1.8 cm.
Rüegg et al19 published their results on the surgical management of extra-articular ankyloses in Noma patients, operated in Geneva, Switzerland. Over 20 years, various approaches were followed under optimal surgical and postoperative conditions. Their series includes 121 patients operated between 1990 and 2015. Surgical procedures included bone-bridge excision and soft-tissue reconstruction with local, pedicled, and large free flaps, sometimes combined with bilateral coronoidectomy. Bilateral coronoidectomy combined with free flap transfer was the only procedure with a significantly improved immediate postoperative MO of 2.6 ± 1.0 cm. Over the 3-year follow-up, an MO of 2.1 ± 1.2 cm was maintained. Physiotherapy was the most important factor to prevent recurrence, which remained problematic in the management of Noma sequelae. They stated that if physiotherapy and long-term follow-up cannot be offered, patients should not be operated.
An MO of 2 to 3 cm is an enormous gain for patients with post-Noma trismus. Local flaps are in most patients not available in the right dimension and free flap transfer is possible, but is connected with possible flap loss or other complications. As there are thousands of trismus patients in the Sahel Zone in Africa,1 trismus release with free flap surgery in every patient is not realistic.
In contrast to the aftereffects of severe surgical interventions, slow distraction transforms and extends the contracted soft tissue and mouth closing muscles.5–11 The effort, risks, and complications related to distraction therapy are minimal compared to those of other surgical procedures. Our results support the efficacy of distraction therapy. The treatment was successful in every patient. However, we do not know why an MO of 3 cm was not achieved in every patient at the end of the distraction; this is a limitation of our study. We believe it could have been due to patient noncompliance or lack of availability or follow-ups by local staff.
Follow-up measurements were also missing in several patients because the patients lived too far away and did not report for follow-ups. We also believe that patients with successful treatment are less likely to report for a follow-up.
Montandon,2 Pittet,18 Huang,20 Dijkastra,21 and Kamstra22 have all emphasized the importance of regular physiotherapy for at least 1 year after the MO procedures; they mentioned that patient compliance with physiotherapy had a significant impact on the results. Physiotherapy includes therapeutic exercise modalities including the dynamic bite opener TheraBite (Atos; Medical GmbH, D-53840 Troisdorf, Deutschland), active range of motion exercises, rubber plugs, and other stretching techniques.
In our study in Africa, we could perform the treatment, but we could not guarantee postoperative physiotherapy due to lack of local medical staff and reduced patient compliance.
Since 2017, as we noted the high tendency of relapse, we provided our patients with a silicon rubber plug as a physiotherapy method. This elastic silicon plug between the incisors prevents the tendency of trismus relapse during night (Fig. 1C).
The present results strongly support the efficacy of distraction therapy. We therefore conclude that distraction therapy allows for an appreciable improvement in the MO in patients with pure soft-tissue trismus due to a healed Noma infection. All follow-up measures differed on average significantly from 0 and changes from 1 measurement to the next were not significant. Posttreatment physiotherapy is mandatory to improve the long-standing results of MO.
The surgery performed in Africa was financially supported by the German HILFSAKTIONNOMA and the Austrian NOMAHILFE; both nonprofit fund-raising organizations.
Supplementary Material
Footnotes
This study was carried out in cooperation with the German Hilfsaktion Noma Foundation.
The authors report no conflicts of interest.
REFERENCES
- 1.Enwonwu CO, Falkler WA, Jr, Idigbe EO, Savage KO. Noma (cancrum oris): questions and answers. Oral Dis 1999; 5:144–149. [DOI] [PubMed] [Google Scholar]
- 2.Rüegg EM, Baratti-Mayer D, Jaquinet A, et al. The surgical management of extra-articular ankylosis in Noma patients. Int J Oral Maxillofac Surg 2018; 47:1527–1533. [DOI] [PubMed] [Google Scholar]
- 3.Oluwasanmi JO, Lagundoye SB, Akinyemi OO. Ankylosis of the mandible from cancrum oris. Plast Reconstr Surg 1976; 57:342–350. [DOI] [PubMed] [Google Scholar]
- 4.Montandon D, Lehmann C, Chami N. The surgical treatment of noma. Plast Reconstr Surg 1991; 87:76–86. [DOI] [PubMed] [Google Scholar]
- 5.Holle J. Lockjaw treatment after noma in the third world. J Craniofac Surg 2009; 20:1910–1912. [DOI] [PubMed] [Google Scholar]
- 6.Ilizarov GA. The tension-stress on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res 1989; 238:249–281. [PubMed] [Google Scholar]
- 7.Dindaroglu F, Duran GS, Görgülü S. Effects of rapid maxillary expansion on facial soft tissues: deviation analysis on three-dimensional images. J Orofac Orthop 2016; 77:242–250. [DOI] [PubMed] [Google Scholar]
- 8.Altug-Atac AT, Grayson BH, McCarthy JG. Comparison of skeletal and soft-tissue changes following unilateral mandibular distraction osteogenesis. Plast Reconstr Surg 2008; 121:1751–1759. [DOI] [PubMed] [Google Scholar]
- 9.Mackool RJ, Hopper RA, Grayson BH, et al. Volumetric change of the medial pterygoid following distraction osteogenesis of the mandible: an example of the associated soft-tissue changes. Plast Reconstr Surg 2003; 111:1804–1807. [DOI] [PubMed] [Google Scholar]
- 10.De Deyne PG, Meyer R, Paley D, Herzenberg JE. The adaptation of perimuscular connective tissue during distraction osteogenesis. Clin Orthop Relat Res 2000; 379:259–269. [DOI] [PubMed] [Google Scholar]
- 11.Day CS, Moreland MS, Floyd SS, Jr, Huard J. Limb lengthening promotes muscle growth. J Orthop Res 1997; 15:227–235. [DOI] [PubMed] [Google Scholar]
- 12.Fisher E, Staffenberg DA, McCarthy JG, et al. Histopathologic and biochemical changes in the muscles affected by distraction osteogenesis of the mandible. Plast Reconstr Surg 1997; 99:366–371. [DOI] [PubMed] [Google Scholar]
- 13.Baumann MA, Dijkstra U, Reintsema H, et al. Surgery for extra-articular trismus: a systematic review. Br J Oral Maxillofac Surg 2016; 54:253–259. [DOI] [PubMed] [Google Scholar]
- 14.Dammer R, Dünzl B, Kühnel T. Therapy of bony and fibrous contractures and buccal defects after noma using the temporalis muscle flap [in German]. Mund Kiefer Gesichtschir 2005; 9:225–232. [DOI] [PubMed] [Google Scholar]
- 15.Adams-Ray WE, James JH. Cancrum oris: functional and cosmetic reconstruction in patients with ankylosis of the jaws. Br J Plast Surg 1992; 45:193–198. [DOI] [PubMed] [Google Scholar]
- 16.Giessler GA, Schmidt AB, Deubel U, Cornelius CP. Free flap transfer for closure and interposition-arthroplasty in noma defects of the lateral face associated with bony ankylosis. J Craniofac Surg 2004; 15:766–772. [DOI] [PubMed] [Google Scholar]
- 17.Giessler GA, Fieger A, Cornelius CP, Schmidt AB. Microsurgical reconstruction of noma-related facial defects with folded free flaps: an overview of 31 cases. Ann Plast Surg 2005; 55:132–138. [DOI] [PubMed] [Google Scholar]
- 18.Bisseling P, Bruhn J, Erdsach T, et al. Long-term results of trismus release in noma patients. Int J Oral Maxillofacial Surg 2010; 39:873–877. [DOI] [PubMed] [Google Scholar]
- 19.Pittet B, Jaquinet A, Montandon D. Clinical experience in the treatment of noma sequelae. J Craniofac Surg 2001; 12:273–283. [DOI] [PubMed] [Google Scholar]
- 20.Huang IY, Wu CF, Shen YS, et al. Importance of patient's cooperation in surgical treatment for oral submucous fibrosis. J Oral Maxillofac Surg 2008; 66:699–703. [DOI] [PubMed] [Google Scholar]
- 21.Dijkastra PU, Sterken MW, Pater R, et al. Exercise therapy for trismus in head and neck cancer. Oral Oncol 2007; 48:389–394. [DOI] [PubMed] [Google Scholar]
- 22.Kamstra JI, van Leeuwen M, Roodenburg JLN, et al. Exercise therapy for trismus secondary to head and neck cancer: a systemic review. Head Neck 2017; 39:2352–2362. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


