Abstract
Purpose:
Research on urban/rural disparities in alcohol, drug use, and mental health (ADM) conditions is inconsistent. This study describes ADM condition prevalence and access to care across diverse geographies in a predominantly rural state.
Methods:
Multimodal cross-sectional survey in South Dakota from November 2013 to October 2014, with oversampling in rural areas and American Indian reservations. Measures assessed demographic characteristics, ADM condition prevalence using clinical screenings and participant self-report, perceived need for treatment, health service usage, and barriers to obtaining care. We tested for differences among urban, rural, isolated, and reservation geographic areas, controlling for participant age and gender.
Findings:
We analyzed 7,675 surveys (48% response rate). Generally, ADM condition prevalence rates were not significantly different across geographies. However, respondents in isolated and reservation areas were significantly less likely to have access to primary care. Knowledge of treatment options was significantly lower in isolated regions and individuals in reservation areas had significantly lower odds of reporting receipt of all needed care. Across the sample there was substantial discordance between ADM clinical screenings and participant self-reported need; 98.1% of respondents who screened positive for alcohol or drug misuse and 63.8% of respondents who screened positive for a mental health condition did not perceive a need for care.
Conclusion:
In a predominantly rural state, geographic disparities in ADM conditions are related to differences in access as opposed to prevalence, particularly for individuals in isolated and reservation areas. Educational interventions about ADM condition characteristics may be as important as improving access to care.
Keywords: health disparities, health services research, mental health, rural health, substance use
Rural populations in the United States experience significant health disparities, routinely ranking poorly on mortality, morbidity, and quality of care measures.1–5 Urban-rural differences have been documented for a variety of health indicators, including obesity,6,7 suicide,7 heart disease,6 general chronic disease,7 cancer mortality,8 cancer diagnosis and treatment,9 diabetes,6,10 renal disease,11 and injury and trauma.12 In one study, death rates in rural counties were 40% higher than rates in counties on the fringe of urban centers.13 However, the evidence for rural-urban disparities in the prevalence and treatment of alcohol, drug use, and mental health (ADM) conditions—and for variation across different kinds of rural areas—is less clear.
Annually, one-fourth of adults (26%) meet diagnostic criteria for a mental health disorder and almost half (46%) will develop one in their lifetime.14 Lifetime and 12-month prevalence rates for alcohol use disorders are 30.3% and 8.5%, respectively,15 and they are 10.3% and 2.0% for drug use disorders.16 Although use of ADM services in the United States has increased in recent decades, the majority of individuals with a mental health condition do not receive any treatment,17 and only one-third of those in treatment receive minimally adequate care.18 Treatment gaps for patients with a DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th edition) substance use disorder may be even greater; national studies indicate that the 12-month treatment rates were 6.1% for drug abuse16 and 3.1% for alcohol abuse.16 There is strong evidence that prevalence of ADM conditions varies with sociodemographic characteristics such as age, sex, race/ethnicity, and household income.15,16,19–21 Although urban versus rural residence is commonly cited as a risk factor for the development of ADM conditions, the evidence regarding the directionality of such associations is inconsistent or nonexistant.15,16,22–24
Detailed data on geographic variation in ADM condition prevalence and treatment patterns have the potential to play a critical role in how we prioritize and implement interventions to improve health care delivery. Current health care transformation efforts, through implementation of Patient Centered Medical Home (PCMH) Principles, the Affordable Care Act (ACA), and the Mental Health Parity and Addiction Equity Act (MHPAEA), are poised to dramatically change the landscape of ADM service provision.25–29 PCMH Principles emphasize the importance of providing patient-centered, coordinated, whole person care with attention to ADM conditions.29–31 The ACA expands coverage and requires mental health and addiction services to be part of the “essential health benefits” for plans offered under the ACA. The MHPAEA requires plans that offer ADM services to provide benefits at the same level as those provided for medical-surgical services. Together, the PCMH, ACA, and MHPAEA create the potential for millions of Americans to obtain access to a comprehensive set of ADM benefits. This impact may be amplified for rural populations based on patterns of Medicaid coverage expansion32–34 and rural health care provision.35,36
Data on ADM conditions can be used to inform policies, resource allocation, and intervention selection. This data may be particularly important in rural settings given research demonstrating that rural populations are generally disadvantaged compared to their urban counterparts in the central tenants of access to care: availability, accessibility, affordability, and acceptability.37–43 However, comparative studies on the prevalence and treatment of ADM conditions in rural settings are often limited by small sample sizes that may hinder or complicate systematic inferences. Research further suggests that rural adults may be less likely to be diagnosed or treated for ADM conditions.37,44–46 There may also be variation in these conditions by region (eg, opioid use in Appalachian states, methamphetamines in Western and Midwestern states)47–50 and/or across different kinds of rural areas—which can include remote or isolated regions that are especially far from urban centers51,52 and American Indian reservations.
Therefore, we conducted a statewide health needs survey in South Dakota and oversampled rural, isolated, and reservation communities to assess disparities in ADM condition prevalence, perceived need, and access to care across diverse types of rural areas. The data support an extensive assessment of ADM conditions and treatment across an expanded set of urban/rural geographic categories, with a focus on a predominantly rural state.
Methods
We conducted a cross-sectional statewide health needs assessment from November 2013 to October 2014, using a combination of mail, telephone, and in-person surveys administered to a geographically representative random sample of noninstitutionalized adults across the state of South Dakota. South Dakota, a predominantly rural state, has a total population of 853,175 according to 2014 US Census estimates;53 14.8% of the population is over 65 years of age and 10.5% report American Indian race/ethnicity.54
Our study team engaged regional and tribal service providers in the design and content of survey questions. To facilitate data collection within the American Indian population, team members gained formal approvals from 7 of the 9 tribes in South Dakota prior to data collection; data were not collected in counties that fall within the boundaries of the 2 nonparticipating tribes. We also hired and trained local community members as research assistants to support in-person data collection within reservation communities. Finally, study findings were shared in regional meetings across South Dakota and with the leadership of each participating tribe. This study was approved by the Institutional Review Board at Oregon Health & Science University; the National Institute of Mental Health under the authority of the United States Department of Health and Human Services issued a Certificate of Confidentiality to protect the privacy of research participants.
Eligibility Criteria
Minimal participation eligibility criteria were: (1) age 18 years or older; (2) a primary owner/occupant of the household; and (3) presence of ZIP code/sample strata in study data.
Sampling
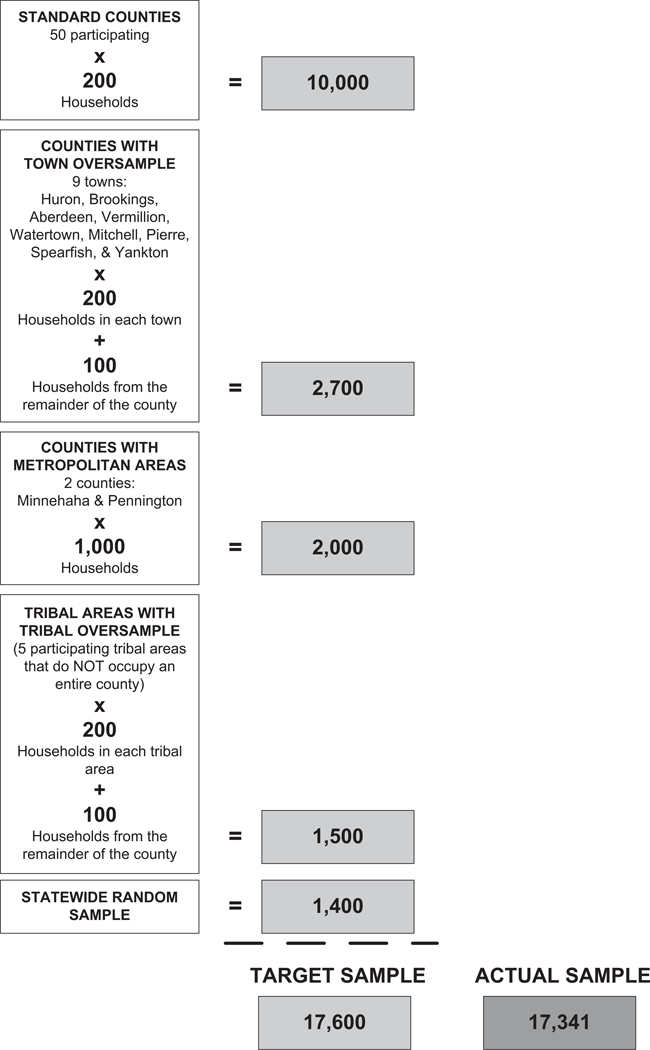
We used address-based sampling to produce county-level and statewide estimates while ensuring sufficient representation within rural and American Indian reservation subpopulations. Each of South Dakota’s 66 counties was considered the primary sampling unit. We set minimum sampling targets around several populations of interest, including the state’s 2 metropolitan areas (minimum sample size of 1,000 each), regional population centers with at least 10,000 residents (minimum sample size of 200 each), and American Indian reservations (minimum sampling size of 200 each).
As displayed in Figure 1 and summarized below we identified the sample in 3 steps: (1) standard counties; (2) counties with oversamples (ie, some reservation/tribal areas, urban centers); and (3) statewide random sample. First, for standard counties (ie, those without an embedded oversample) we started with a list of all valid, noninstitutional USPS residential mailing addresses and pulled 200 randomly sampled households. Second, for counties with an embedded oversample (reservation/tribal areas), we split the “host” county into 2 mutually exclusive sampling units based on a review of regional ZIP codes: 1 for the town/tribal area itself, and 1 for all households in the county outside of the town/tribal area/ We sampled up to the goal of 200 households in the town/tribal area cell and then sampled at least 100 additional households from outside the town/tribal area. This created an effective minimum sample size of 300 in counties where the targeted town/tribal oversamples reside while ensuring that we achieved our targets in both the county and town/tribal sampling units. In addition, for the state’s 2 metropolitan statistical areas (ie, Minnehaha and Pennington counties), which are key access points for specialty care in the state, we included an additional random sample of 1,000 households. Our third step, after filling these county and regional minimums, was to fill the rest of our sampling quota with a simple random sample of households across the state. This approach yielded a representative, stratified random sample of 17,341 South Dakota households. This sampling frame included 2,874 households in reservation towns/tribal areas (16% of the total sample compared with 9% of the actual state population) and over 9,000 households located outside of towns with 10,000 or more residents.
Figure 1.
Three-Step Case Selection Approach: Standard Counties, Counties With Oversamples (ie, Reservation Town/Tribal Area, Urban Areas),Statewide Random Sample.
Data Collection
We used a multimode fielding protocol including mail, telephone, and in-person data collection to maximize response rates and facilitate data collection in hard-to-reach populations. A prescreening postcard was sent to inform respondents that the survey was coming and test for valid addresses. A multiwave mailing protocol followed, with 2 survey attempts that provided both prepaid mail and web-based response options. Automated reminder calls were used to prompt participation. Nonresponders to the mail survey were advanced into a telephone completion arm, with multiple calls to each household occurring over a several-week period.
Nonresponders in reservation areas were advanced to a special “face-to-face” completion arm based on an expectation that these communities might be less responsive to mail and phone surveys. This approach was designed to be compatible with the mail surveys; local research assistants approached residents at their homes, invited them to fill out a paper survey in private, and instructed them to return the completed survey to the research assistant in a sealed envelope.
Respondents were paid a modest cash stipend for their time; a $5 bill was included in the original mailed survey and those completing the survey in person received $20 in cash. We removed 1,340 invalid addresses from our initial sample of 17,341, resulting in a final sample of 16,001 households.
Measures
Our survey consisted of 79 questions that collected data on participant demographics, prevalence of physical and ADM conditions, perceived need, access, and barriers to care. We used previously validated questions and response scales when available. The survey instrument was refined using stakeholder feedback and cognitive testing with 7 participants with demographic characteristics similar to the sampling target. The full survey instrument is available in Appendix 1 (online only).
Demographics
We asked standard questions to determine participants’ self-reported age in years, gender, educational attainment (less than high school, high school diploma or GED, vocational training or 2-year degree, 4-year college degree, advanced or graduate degree), living arrangement (alone, with other relatives including children, with spouse or partner, with parents, with friends or roommates), health insurance coverage (no insurance, private coverage through employer, private coverage through myself, Medicare, Medicaid, Military health care, Indian Health Service, other), and employment status (employed by someone else, self-employed, not currently employed, retired).
Geographic Area
We categorized household locations into 4 mutually exclusive geographic clusters: urban, rural, isolated, and reservation. We used the ZIP code version of the Rural-Urban Commuting Areas (RUCAs) taxonomy to cluster respondents into 3 classifications based on population density, urbanization, and daily commuting patterns: urban (50,000 or more), rural (2,500–49,999), and isolated areas (<2,5 0 0).51,52 We combined small (2,500–9,999) and large (10,000–49,999) micropolitan areas into one “rural” category because our initial analysis showed response similarities and a limited number of responses from small micropolitan areas. We created a fourth distinct “reservation” category for ZIP codes fully or partially overlapping with American Indian tribal land. Additional details on this classification scheme appear in Figure 2.
Figure 2.
Detailed Description of Geographic Clustering Procedure for South Dakota Health Survey.
We clustered responses in 4 distinct geographic clusters to analyze differences: urban, rural, isolated, and reservation areas. We used a 3-category rural/urban classification based on the ZIP code version of the Rural-Urban Commuting Areas (RUCAs) taxonomy to capture variation in the type of rurality based on population size and commuting patterns.51,52 Small (2,500–9,999) and large (10,000–49,999) micropolitan areas were combined into one “rural” category due to response similarities and limited number of small micropolitan areas. Isolated regions were kept distinct. A fourth “reservation” category was created for ZIP codes fully or partially overlapping with AI tribal land. The RUCA codes for these 4 designations follow:
Urban: Metropolitan cores and commuting patterns to areas with populations of 50,000 or more [RUCA: 1.0, 1.1, 2.0, 2.1, 3.0, 4.1, 5.1, 7.1, 8.1, 10.1]
Rural: Micropolitan areas and commuting patterns to or within population centers of 2,500–49,000 and not overlapping with AI tribal land. Includes both small and large micropolitan area RUCA codes. [RUCA: 4.0, 4.2, 5.0, 5.2, 6.0, 6.1 7.0, 7.2, 7.3, 7.4, 8.0, 8.2, 8.3, 8.4, 9.0, 9.1, 9.2]
Isolated: Commuting flow to areas without population centers of 2,500 or more, no commuting flow to urban areas, and no overlap with AI tribal land. [RUCA: 10.0, 10.2, 10.3, 10.4, 10.5, 10.6]
Reservation: ZIP code fully or partially overlapping with tribal land of an AI tribe. Includes ZIP codes that would otherwise be categorized as rural or isolated.
Prevalence of ADM Conditions
We assessed prevalence of depression with the 2-question version of the Patient Health Questionnaire (PHQ-2),55,56 anxiety with the 2-item General Anxiety Disorder scale (GAD-2),55,57 and post-traumatic stress disorder (PTSD) with the Primary Care PTSD Screen (PC-PTSD).58 Alcohol misuse was assessed with the 3-item Alcohol Use Disorders Identification Test (AUDIT-C). Positive AUDIT-C screens were defined as scores of 4 or more for males and 3 or more for females.59–61 Because a relatively large percentage (>30%) of the population typically screens positive using this scale, we also tested for less sensitive and more specific cutoffs for both genders using AUDIT-C scores greater than 6 or 9. In addition, heavy drinking was defined as drinking over weekly recommended limits or an average of 8 or more drinks per week for women or 15 or more drinks per week for men. Binge drinking was defined as drinking 5 or more drinks on any one occasion in the past year. Measures from the National Survey on Drug Use and Health (NSDUH) were used to assess use of marijuana, methamphetamines, and nonmedical prescription painkillers.62 In addition to these screenings, respondents were asked to self-report whether they had ever been told by a health professional that they had depression, anxiety, PTSD, bipolar disorder, addiction issues, or other mental health conditions.63
Perceived Need and Access to Medical and ADM Services
We used questions modeled from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) to assess perceived need for and access to general medical care, prescription medications, mental health services, and alcohol or drug treatment.64 All respondents were asked these initial questions. For example, perceived need for medical care was assessed with the following yes/no survey question: “Was there a time in the last 12 months when you needed medical care?” Primary care access and health care coverage measures were based on the Behavioral Risk Factor Surveillance System questionnaire (BRFSS).63 We also assessed self-reported emergency department or inpatient hospitalization for mental health or substance use problems in the last 12 months using questions modeled after examples from CAHPS and the National Health and Nutrition Examination Survey (NHANES).65,66 Only participants who reported a need for medical, mental, and/or alcohol and drug treatment were asked to responded to a series of follow-up questions regarding the level of care received in the last 12 months using 4 response options: “I got all the [type of] care needed,” “I got some but not all needed [type of] care,” I got no [type of] care at all,” and “I don’t know.”
Barriers to Care
Respondents who indicated they went without needed care were asked to identify the main reasons by selecting from a list of common barriers from the published literature including variables assessing the 4 dimensions of access identified by Penchansky and Thomas: availability (eg, didn’t know where to go, couldn’t get an appointment), accessibility (eg, I didn’t have transportation), affordability (eg, no health insurance, insurance wouldn’t cover), and acceptability (eg, could handle it without treatment, was worried about what people would think).43 The list of barriers was developed through an initial review of the literature and refined in a series of studies by members of our team over the last 10 years.67,68
Specific questions assessed knowledge of treatment locations and distance to care for ADM conditions. Questions probing perceived stigma associated with receiving treatment for mental illness, drug use, and alcohol use were based on the Perceived Discrimination Devaluation Scale and the Stigma Concerns about Mental Health Care questionnaire.69 To assess perceived discrimination respondents were asked: “How much do you agree or disagree with the following statements? I think most people around here would think badly of someone who ... has been treated for [a mental illness, drug abuse, alcohol abuse].” Perceived stigma was assessed using the following yes/no question: “Would you avoid getting help for any of the following because you are afraid of what others might think?” with prompts for mental illness, drug abuse, and alcohol abuse.
Data Analysis
We used SAS version 9.2.2.2 (SAS Institute Inc., Cary, North Carolina) for all statistical analyses, using survey specific functions in SAS to correct for finite survey population and correlations among survey strata. Responses were weighted to account for oversampling and to accurately represent the state’s true population distribution. First, we weighted each response by the inverse of the probability of selection of the address and a nonresponse adjustment for each sampling unit. We then applied a post-stratification weight adjustment to account for age group differences between our respondents and 2010 census data, because our respondents tended to be older than the actual South Dakota population, potentially impacting prevalence estimates in the absence of these adjustments.
The primary outcomes for this analysis focused on the findings from common clinical ADM screens (eg, depression, anxiety, PTSD, alcohol misuse, drug use), self-reported diagnosis of medical and ADM conditions, perceived need for ADM treatment, access to primary care and ADM treatment services, and reported barriers to care. To test for differences by geography, we used weighted logistic regression with strata clustered errors and a finite population correction to calculate adjusted odds ratios and 95% confidence intervals for each outcome after controlling for age and sex. In accordance with the Institute of Medicine’s definition of disparities (ie, a difference not justified by differences in health status or preferences),70,71 we did not include indicators of socioeconomic status (eg, race/ethnicity, education, income) in our analyses. While these indicators are likely to be correlated with both rurality and ADM conditions, the IOM definition includes these factors as components of the disparity, and not as factors that should be conditioned on or adjusted for in estimating the extent of the disparity. Sensitivity analyses that included race/ethnicity, income, employment status, and education were qualitatively similar to our main analyses, which restrict statistical adjustment to variables recommended by the IOM.
Results
We obtained a 48% response rate (n = 7,675); 86% of the returned surveys were completed by mail, 4% by phone, 4% online, and 6% in-person. After adjusting for the sampling weights, respondents represented urban (44.4%), large/small rural (33.3%), isolated (17.6%), and reservation (4.7%) areas, proportions comparable to South Dakota’s overall population distribution. As summarized in Table 1, compared to census data on the overall South Dakota population, respondents tended to be female (57% vs. 50% statewide) and white (89% vs. 83% statewide). Respondents were also less likely to have been unemployed (9.6% vs. 15.3%) or to have not completed high school (3.9% vs. 13.4%). American Indian respondents made up 9.3% of the total sample and completed 64.4% of the surveys from reservation areas.
Table 1.
South Dakota Health Survey (SDHS) Respondent Characteristics (n = 7,675)
| Characteristic | Unweighted SDHS | Weighted SDHS | SD Populationa | US Populationa |
|---|---|---|---|---|
| Age | ||||
| 18–34 | 7.6% | 30.3% | 30.8% | 30.6% |
| 35–64 | 56.0% | 50.6% | 49.6% | 50.9% |
| 65 and older | 36.5% | 19.1% | 19.6% | 18.5% |
| Gender | ||||
| Male | 47.7% | 42.6% | 49.8% | 48.6% |
| Female | 52.3% | 57.4% | 50.2% | 51.4% |
| Race/ethnicity | ||||
| Hispanic or Latino | 1.1% | 1.0% | 3.2% | 17.1% |
| Non-Hispanic White | 91.2% | 88.7% | 83.4% | 62.4% |
| Non-Hispanic Black | 0.1% | 0.2% | 1.5% | 12.3% |
| American Indian (AI) | 6.8% | 9.3% | 10.5% | 1.7% |
| Other | 0.9% | 0.8% | 2.5% | 11.6% |
| Residential status | ||||
| Live alone | 24.3% | 21.6% | 29.2% | 27.7% |
| Live with spouse | 64.1% | 64.0% | 50.3% | 48.0% |
| Other | 11.6% | 14.4% | 14.2% | 17.9% |
| Employment status | ||||
| Not employed | 6.6% | 9.6% | 15.3% | 25.3% |
| Employed part time | 18.4% | 18.9% | 19.4% | 17.9% |
| Employed full time | 46.3% | 54.1% | 65.3% | 56.8% |
| Retired | 28.7% | 17.4% | N/A | N/A |
| Rural/urban statusb | ||||
| Urban (50,000+) | 17.5% | 44.4% | 39.1% | 80.8% |
| Large Rural (10,000–49,999) | 19.5% | 26.3% | 25.2% | 9.7% |
| Small Rural (2,500–9,999) | 6.4% | 7.0% | 9.0% | 5.4% |
| Isolated (<2,500) | 41.7% | 17.6% | 26.6% | 4.1% |
| Reservation (AI tribal lands) | 14.9% | 4.7% | N/A | N/A |
| Education | ||||
| Less than high school | 6.2% | 3.9% | 13.4% | 8.4% |
| High school diploma or GED | 40.6% | 33.1% | 31.3% | 27.8% |
| Vocational or 2-yr. degree | 23.9% | 23.9% | 11.4% | 8.1% |
| 4-Year college degree | 19.6% | 25.4% | 18.9% | 18.4% |
| Advanced or graduate degree | 9.7% | 13.8% | 7.6% | 11.2% |
From United States Census Bureau. 2013 American Community Survey.54
Rural/urban status determined using the University of Washington Rural Urban Community Area (RUCA) codes. Reservation areas were identified based on ZIP codes fully or partially overlapping with American Indian tribal land. We combined small (2,500–9,999) and large (10,000–49,999) micropolitan areas into one “rural” category due to response similarities and limited number of participants in small micropolitan areas.
Prevalence of ADM Conditions
Table 2 displays prevalence for ADM conditions across the 4 rural-urban classifications. We display the prevalence as identified by validated screening mechanisms (eg, PHQ-2) as well as self-reported diagnosis measures. There were no significant differences between individuals in urban and rural, isolated, and reservation areas in terms of the prevalence rates for mental health conditions based on clinical screenings. Based on self-reported diagnoses, respondents in rural areas had significantly lower odds of reporting PTSD, bipolar disorder, and other mental health conditions. Respondents in isolated areas had lower self-reported diagnoses of anxiety (OR 0.61, 95% CI: 0.440.84) when compared to their urban counterparts.
Table 2.
Adjusted Odds Ratios and Prevalence of Alcohol, Drug Use, and Mental Health Conditions by Geographic Category (Urban = Reference, 95% CI), Controlling for Age and Gender
| Prevalence by Geographic Category |
Adjusted Odds Ratios (Urban = Reference) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Total Sample (N = 7675) | Urban (N = 1346) | Rural (N = 1989) | Isolated (N = 3198) | Reservation (N = 1142) | Rural AOR (95% CI) | Isolated AOR (95% CI) | Reservation AOR (95% CI) | |
| Mental health screening | ||||||||
| Depression (PHQ-2) | 5.55% | 6.30% | 4.30% | 5.50% | 8.20% | 0.67 (0.42–1.07) | 0.86 (0.55–1.34) | 1.36 (0.83–2.21) |
| Anxiety (GAD-2) | 7.51% | 7.80% | 7.70% | 5.60% | 10.30% | 0.99 (0.61–1.60) | 0.76 (0.47–1.23) | 1.31 (0.82–2.10) |
| Posttraumatic stress disorder (PC-PTSD) | 5.98% | 6.40% | 4.80% | 5.90% | 10.30% | 0.74 (0.45–1.22) | 0.99 (0.56–1.74) | 1.62 (0.98–2.68) |
| Alcohol abuse screening | ||||||||
| AUDIT-C positive | 42.39% | 42.80% | 45.50% | 35.80% | 40.60% | 1.13 (0.89–1.42) | 0.80 (0.65–0.98)* | 0.91 (0.68–1.20) |
| AUDIT-C breakpoints | ||||||||
| AUDIT 6+ | 11.49% | 11.40% | 11.60% | 9.80% | 17.60% | 1.06 (0.71–1.57) | 0.90 (0.63–1.28) | 1.82(1.07–3.08)* |
| AUDIT 9+ | 2.46% | 1.40% | 3.60% | 2.80% | 2.80% | 2.84 (1.50–5.39)* | 2.13 (1.17–3.89)* | 2.28 (1.20–4.33)* |
| Heavy drinkinga | 3.92% | 3.40% | 5.00% | 3.00% | 4.10% | 1.51 (0.84–2.71) | 0.94 (0.57–1.57) | 1.21 (0.63–2.33) |
| Binge drinkingb | 39.10% | 38.60% | 41.60% | 34.90% | 41.60% | 1.17 (0.90–1.53) | 0.96 (0.77–1.20) | 1.19 (0.87–1.62) |
| Drug use screening | ||||||||
| Any drug use | 8.33% | 9.50% | 6.20% | 6.40% | 21.40% | 0.65 (0.36–1.17) | 0.75 (0.43–1.31) | 2.78 (1.70–4.52) |
| Marijuana | 6.73% | 8.00% | 4.50% | 5.00% | 18.70% | 0.54 (0.28–1.04) | 0.72 (0.39–1.33) | 2.81 (1.66–4.74) |
| Methamphatamine | 0.37% | 0.20% | 0.30% | 0.60% | 1.70% | 1.22 (0.31–4.71) | 2.69 (0.40–18.13) | 7.33 (1.89–28.41) |
| Prescription pain killers | 1.34% | 1.20% | 1.30% | 1.40% | 2.80% | 1.21 (0.36–4.13) | 1.33 (0.42–4.24) | 2.69 (0.92–7.89) |
| Self-reported medical diagnosis | ||||||||
| Depression | 17.04% | 18.80% | 16.00% | 15.00% | 15.70% | 0.80 (0.58–1.11) | 0.77 (0.56–1.06) | 0.77 (0.54–1.10) |
| Anxiety | 17.62% | 19.60% | 17.80% | 12.40% | 16.90% | 0.86 (0.58–1.28) | 0.61 (0.44–0.84)* | 0.78 (0.54–1.13) |
| PTSD | 3.40% | 4.30% | 1.90% | 3.30% | 6.40% | 0.43 (0.24–0.77)* | 0.81 (0.38–1.73) | 1.50 (0.80–2.83) |
| Bipolar disorder | 1.69% | 2.30% | 0.40% | 2.10% | 3.50% | 0.18 (0.07–0.47)* | 1.08 (0.39–2.98) | 1.48 (0.55–3.98) |
| Another MH condition | 2.52% | 3.10% | 1.30% | 3.10% | 3.30% | 0.40 (0.23–0.71)* | 1.03 (0.44–2.41) | 1.02 (0.49–2.13) |
| Addiction issues | 2.61% | 2.30% | 2.80% | 2.70% | 3.30% | 1.20 (0.59–2.44) | 1.27 (0.52–3.09) | 1.43 (0.64–3.20) |
Indicates significant difference (P < .05) as compared to urban respondents.
Heavy drinking is defined as drinking over weekly recommended limits or an average of 8 or more drinks per week for women or 15 or more drinks per week for men.
Binge drinking is defined as drinking 5 or more drinks on any one occasion in the past year.
Relative to mental health conditions, rural-urban differences in substance use patterns were slightly more common. In analyses of the AUDIT-C screen for alcohol abuse, only respondents in isolated areas had significantly lower odds of screening positive than respondents in urban areas (OR 0.80, 95% CI: 0.65–0.98). However, analyses that used a higher threshold of 9 or more on the AUDIT-C to indicate alcohol abuse found significantly higher odds for all 3 rural categories when compared to urban respondents: rural OR 2.84, 95% CI: 1.50–5.39; isolated OR 2.13, 95% CI: 1.17–3.89; reservation OR 2.28, 95% CI: 1.20–4.33. Compared to urban respondents, respondents from reservation areas also had significantly higher odds of marijuana (OR 2.81, 95% CI: 1.66–4.74) and methamphetamine use (reservation OR 7.33, 95% CI: 1.89–28.41), although the absolute level of methamphetamine use was only 1.7% in reservation areas.
Perceived Need and Health Service Use
Table 3 displays perceived need for health care in the last year. Statewide, 75.1% of respondents perceived a need for medical care within the past year, 9.7% perceived a need for mental health care, and 1.6% perceived a need for substance use treatment. Although prevalence of ADM conditions was similar across geographies, respondents in rural or isolated areas were significantly less likely to report needing care. For example, respondents in isolated areas were significantly less likely to report needing medical (OR 0.64, 95% CI: 0.51–0.80) or substance use treatment (OR 0.41, 95% CI: 0.18–0.92), and respondents in rural areas were less likely to report perceived need for mental health care (OR 0.65, 95% CI: 0.43–0.99).
Table 3.
Perceived Need for Medical, Alcohol, Drug Use, and Mental Health Treatment and Receipt of Care by Geographic Category (Urban = Reference, 95% Cl), Controlling for Age and Gender
| Total Sample (N = 7675) | Distribution by Geographic Category |
Adjusted Odds Ratios (Urban = Reference) |
||||||
|---|---|---|---|---|---|---|---|---|
| Urban (N = 1346) | Rural (N = 1989) | Isolated (N = 3198) | Reservation (N = 1142) | Rural AOR (95% Cl) | Isolated AOR (95% Cl) | Reservation AOR (95% Cl) | ||
| Perceived treatment need | ||||||||
| Medical | 75.11% | 77.10% | 76.30% | 68.60% | 72.50% | 0.91 (0.70–1.18) | 0.64 (0.51–0.80)* | 0.76 (0.56–1.04) |
| Mental Health | 9.73% | 11.50% | 8.00% | 8.40% | 10.20% | 0.65 (0.43–0.99)* | 0.74 (0.50–1.09) | 0.83 (0.54–1.28) |
| Substance Use | 1.57% | 1.80% | 1.50% | 0.70% | 3.00% | 0.85 (0.32–2.26) | 0.41 (0.18–0.92)* | 1.71 (0.65–4.47) |
| Have PCP | 77.42% | 78.60% | 81.60% | 74.20% | 48.30% | 1.22 (0.88–1.70) | 0.67 (0.52–0.87)* | 0.23 (0.17–0.31)* |
| Knowledge of treatment options | ||||||||
| Mental Health | 61.96% | 65.00% | 61.40% | 55.40% | 61.60% | 0.86 (0.68–1.10) | 0.67 (0.55–0.82)* | 0.87 (0.66–1.16) |
| Substance Use | 51.93% | 53.70% | 53.80% | 43.70% | 52.90% | 1.02 (0.80–1.29) | 0.67 (0.55–0.81)* | 0.99 (0.75–1.31) |
| Received all needed carea | ||||||||
| Medical | 86.99% | 87.80% | 88.80% | 86.70% | 65.80% | 1.13 (0.75–1.69) | 0.85 (0.57–1.28) | 0.27 (0.18–0.39)* |
| Mental health | 64.18% | 68.00% | 62.60% | 62.30% | 39.10% | 0.84 (0.35–2.03) | 0.77 (0.29–2.03) | 0.32 (0.13–0.80)* |
| Substance use | 54.39% | 56.70% | 64.10% | 32.70% | 37.50% | 3.03 (0.79–11.62) | 0.50 (0.08–3.20) | 0.86 (0.11–6.83) |
| Hospital utilization for ADM conditions (1 or more visit In past year) | ||||||||
| ED, mental health | 11.20% | 11.80% | 9.40% | 10.50% | 21.00% | 0.76(0.52–1.11) | 0.90 (0.63–1.29) | 2.04 (1.40–2.97)* |
| Inpatient, mental health | 5.69% | 5.80% | 4.80% | 5.70% | 10.80% | 0.76 (0.48–1.20) | 0.89 (0.60–1.33) | 1.99 (0.99–4.02) |
| ED, substance use | 0.74% | 1.20% | 0.20% | 0.10% | 2.50% | 0.21 (0.05–0.95)* | 0.11 (0.03–0.46)* | 2.19 (0.65–7.40) |
| Inpatient, substance use | 0.44% | 0.50% | 0.40% | 0.10% | 1.20% | 0.91 (0.17–4.74) | 0.19 (0.04–0.90)* | 2.51 (0.56–11.31) |
Indicates significant difference (P < .05) as compared to urban respondents.
Responses provided for those answering “yes” to perceived need.
We found significant disparities across the 4 rural/urban geographies when assessing receipt of care for those who perceived a need. Compared to urban respondents, respondents in reservation areas were significantly less likely to receive all needed medical (OR 0.27, 95% CI: 0.18–0.39) or mental health care (OR 0.32, 95% CI: 0.13–0.80). Respondents in isolated and reservation areas were less likely to have a primary care provider (isolated OR 0.67, 95% CI: 0.52–0.87; reservation OR 0.23, 95% CI: 0.17–0.31). Residents in isolated areas were also less likely to know where to go for mental health care (OR 0.67, 95% CI: 0.55–0.82) and substance use treatment (OR 0.67, 95% CI: 0.55–0.81).
Despite low perceived need for ADM condition treatment, emergency department (ED) and inpatient admissions were high across the study population (Table 3). Statewide, 11.2% of respondents reported 1 or more visits to the ED and 5.7% reported 1 or more inpatient visits for a mental health problem over the past year. Respondents in reservation areas were twice as likely to report 1 or more visits to the ED for mental health as compared to those from urban areas (OR 2.04, 95% CI: 1.40–2.97). In contrast, respondents in rural and isolated areas had significantly lower odds of reporting 1 or more visit in the past year to the ED for substance use.
Barriers to Care
Table 4 displays barriers to care and perceived stigma for ADM treatment. Although prevalence of ADM conditions was generally similar across geographies, respondents in rural and isolated areas had significantly higher odds of going without needed mental health care due to reasons associated with cost (rural OR 2.52, 95% CI: 1.06–6.00; isolated OR 2.65, 95% CI: 1.03–6.84). Respondents in reservation areas were significantly more likely than urban participants to report problems with the availability of mental health treatment or logistical issues in obtaining care (availability OR 14.9, 95% CI: 2.94–75.62; logistics OR 3.51, 95% CI: 1.08–11.39).
Table 4.
Barriers to Care and Perceived Stigma for Alcohol, Drug Use, and Mental Health Treatment by Geographic Category (Urban = Reference, 95% Cl), Controlling for Age and Gender
| Total Sample (N = 7675) | Geographic Category |
Adjusted Odds Ratios (Urban = Reference) |
||||||
|---|---|---|---|---|---|---|---|---|
| Urban (N = 1346) | Rural (N = 1989) | Isolated (N = 3198) | Reservation (N = 1142) | Rural AOR (95% Cl) | Isolated AOR (95% Cl) | Reservation AOR (95% Cl) | ||
| Main reasons for going without mental health treatmenta | ||||||||
| Cost | 19.00% | 13.50% | 25.20% | 24.50% | 25.80% | 2.52 (1.06–6.00)* | 2.65 (1.03–6.84)* | 2.22 (0.91–5.44) |
| Personal choice | 12.42% | 10.30% | 16.00% | 8.60% | 25.30% | 1.72 (0.74–3.99) | 0.82 (0.36–1.88) | 2.87 (1.00–8.27) |
| Availability | 11.18% | 9.90% | 11.40% | 8.70% | 29.10% | 1.19 (0.32–4.48) | 0.91 (0.25–3.32) | 3.51 (1.08–11.39)* |
| Stigma/fear | 7.01% | 5.00% | 10.30% | 4.50% | 16.70% | 2.32 (0.65–8.24) | 0.85 (0.28–2.65) | 3.79 (0.99–14.45) |
| Logistical reasons | 3.81% | 1.80% | 2.10% | 7.40% | 21.20% | 1.24 (0.26–6.03) | 4.92 (0.87–27.92) | 14.92 (2.94–75.62)* |
| Other reasons | 4.98% | 4.40% | 7.20% | 2.50% | 6.30% | 1.72 (0.39–7.53) | 0.47 (0.13–1.77) | 1.28 (0.33–5.01) |
| Distance to treatment | ||||||||
| Over 20 miles to mental Health care | 55.54% | 41.70% | 56.30% | 85.20% | 68.10% | 1.87 (1.46–2.39)* | 8.40 (6.49–10.86)* | 3.39 (2.38–4.84)* |
| Over 20 miles to Substance use care | 62.45% | 52.80% | 59.60% | 91.00% | 67.80% | 1.39(1.08–1.80)* | 10.87 (8.23–14.34)* | 2.10(1.55–2.84)* |
| Would avoid treatment because of what others would think | ||||||||
| Mental illness | 9.41% | 10.00% | 7.80% | 10.90% | 9.30% | 0.75 (0.50–1.14) | 1.22 (0.83–1.79) | 0.86 (0.54–1.37) |
| Alcohol abuse | 6.54% | 6.20% | 6.40% | 7.30% | 7.50% | 1.05 (0.64–1.74) | 1.27 (0.82–1.98) | 1.20 (0.69–2.09) |
| Drug abuse | 7.00% | 7.00% | 6.40% | 7.80% | 8.00% | 0.91 (0.56–1.48) | 1.21 (0.77–1.90) | 1.14(0.66–1.98) |
| Think badly of others in treatmentb | ||||||||
| Mental illness | 38.42% | 38.80% | 36.70% | 39.10% | 44.60% | 1.00 (0.77–1.30) | 1.10 (0.88–1.37) | 1.13 (0.81–1.57) |
| Alcohol abuse | 41.89% | 43.00% | 41.00% | 40.80% | 41.90% | 1.05 (0.80–1.40) | 1.01 (0.81–1.27) | 0.89 (0.63–1.25) |
| Drug abuse | 49.53% | 50.50% | 47.90% | 50.70% | 47.90% | 1.02 (0.77–1.33) | 1.07 (0.86–1.35) | 0.80 (0.57–1.14) |
Indicates significant difference (P < .05) as compared to urban respondents.
Responses provided for those answering “yes” to perceived need.
Respondents reporting “agree” or “somewhat agree.”
In addition to low self-reported need for mental health or substance use treatment (Table 3), we observed substantial discordance between positive screening results and self-reported need for ADM treatment across the state. Almost all respondents (98.1%) who screened positive for substance use did not perceive a need for care (95% CI: 96.75–98.99) and 63.8% of respondents who screened positive for a mental health condition did not perceive a need for care (95% CI: 56.02–71.49).
Discussion
This study suggests that relatively similar prevalence rates for ADM conditions exist across urban, small/large rural, isolated, and reservation geographic regions in South Dakota. Our findings add to a growing body of literature exploring rural/urban disparities in ADM condition prevalence. However, findings from epidemiologic research and community-based studies are inconsistent, suggesting that prevalence of ADM conditions may not vary between rural and urban areas.22,23,48 Some of this uncertainty may be driven by different ways of analyzing rural/urban differences—through bivariate comparisons versus more nuanced geographic levels—and in how ADM conditions are measured. For example, a 2010 meta-analysis of 20 “higher quality” population surveys in developed countries found that the pooled urban prevalence rate for various mental health conditions (eg, any psychiatric disorder, mood disorders, or anxiety disorders) was higher than that in rural areas, but no significant differences were detected for substance use.22 In contrast, a 2014 analysis of the National Survey of Drug Use and Health explored 4 geographic levels and found that the prevalence of mental health disorders was not higher in the most urban compared to the most rural areas.23 Moreover, studies indicate that ADM conditions may vary regionally,47–50,72 a factor that may eliminate significant differences in analyses of national data.
Although prevalence rates for ADM conditions were similar in our study, we observed significant differences in access to care across the 4 rural/urban geographies. For example, respondents from rural areas had lower rates of self-reported mental health diagnoses and had access to primary care and knowledge of ADM treatment options comparable to respondents from urban areas. In contrast, respondents in isolated communities were significantly less likely to have a primary care provider or to express knowledge of ADM treatment options. Respondents in reservation communities were also less likely to have a primary care provider and more frequently reported not receiving all needed medical and mental health care in the past year. Additionally, across the sample we observed significant discordance between the results of ADM clinical screenings and participant perceived need for treatment.
Our findings emphasize the barriers that rural populations face in obtaining ADM treatment due to challenges with availability, accessibility, affordability, and acceptability of care, and they resonate with prior research findings.37–43 Although ADM prevalence rates may be similar across urban and rural areas, individuals in isolated and reservation areas had significant gaps in access to primary care and their knowledge of ADM treatment options. In light of Anderson and Aday’s behavioral model of health services usage, our findings suggest that individuals living in isolated and reservation communities may experience different enabling resources and predisposing factors for ADM treatment.73,74 Because perceived need for treatment is often viewed as an essential “first step” in seeking care75–77 and prior research studies suggest that rural residents are less likely to perceive a need for treatment or to actively seek care,37,42,78 these findings emphasize that expanding coverage or increasing the number of available treatment facilities may be a necessary but insufficient step in improving ADM care.
This study suggests several avenues to improve access to care for ADM treatment across diverse rural geographic areas. Addressing barriers associated with cost of care, such as through Medicaid expansion, may offer one mechanism. However, various states, including South Dakota, chose not to adopt Medicaid expansion as part of ACA implementation,79 and insurance coverage does not automatically result in improvements in population health. Models that integrate ADM treatment at the primary care level, such as through implementing PCMH principles, may be a second mechanism for improving care, particularly in rural and reservation areas.80,81 Integrating medical and ADM services in one setting may confront multiple barriers to ADM treatment with a single intervention, regardless of geographic setting. However, rural, isolated, and reservation areas may experience additional barriers to implementing these models given the shortages of mental health and addiction specialists in rural settings.82 A third option may be to improve telehealth for ADM services, which may overcome barriers related to logistics, travel distance, and provider shortages.83–85
However, interventions that enhance access to care without adequate attention to the factors that shape perceptions of ADM treatment need may be ineffective. Our team conducted a qualitative follow-up study of survey participants to explore the discordance we detected between positive clinical screens and an individual’s perceived need for care. We conducted key informant interviews with 33 rural and American Indian respondents who recommended that in addition to improving access to and quality of ADM treatment, community-level interventions were needed to (a) educate the population about the conditions and opportunities for recovery; (b) reduce the stigma associated with pursing care; and (c) create social structures that facilitate prevention and early detection.86 Community-level education and outreach interventions have the potential to complement large-scale national changes such as implementation of the ACA and MHPAEA which are designed to improve access to care for individuals with ADM disorders.
Limitations
Our study has a few important limitations. First, we relied on self-report data, which are subject to recall bias and may result in under reporting of ADM condition prevalence. Second, using multiple fielding procedures we obtained a 48% response rate. Population survey response rates are typically between 40% and 80% and are generally considered acceptable within this range.87–89 However, our survey sample differed slightly from the overall population in South Dakota, with respondents more likely to be older and female. Individuals with significant ADM conditions may have been unwilling or unable to respond to the survey; using an address-based sampling method also precluded the engagement of homeless populations who may be at higher risk for these conditions.90,91 Third, our cross-sectional data captured a moment-in-time snapshot, limiting our ability to detect temporal relationships. Mental health and substance use are not static constructs and our study does not follow the longer-term consequences of ADM conditions and poor access to services.
Conclusion
The South Dakota Health Survey represents the largest survey of its kind conducted within a state with a predominantly rural population; extensive oversampling and outreach provided sufficient granularity to assess differences in ADM conditions across urban, rural, isolated, and reservation areas. Our results suggest relatively similar prevalence rates for ADM conditions across the 4 geographic areas. However, we found significant geographic differences in access to care as well as discordance between findings on ADM clinical screenings and a participant’s perceived need across the full sample. Detailed data on ADM conditions offer critical insights for improving health service delivery, particularly in rural areas where this information is often not available. Although current health transformation efforts such as the PCMH, ACA, and MHPAEA have the potential to rapidly transform access and coverage for ADM conditions, these policy changes may be inadequate to improve ADM outcomes if we do not concurrently implement interventions to raise awareness of treatment need. Our study provides a careful assessment of ADM needs in South Dakota, highlighting the need for improved access to care in rural, isolated and reservation areas as well as locally relevant, targeted education around ADM conditions and treatment.
Supplementary Material
Acknowledgments:
Two consultants provided helpful feedback on study design and progress (Spero Manson, PhD, and Rodger Kessler, PhD). Regional assistance with data collection was provided by Stacey Tieszen, Andrea Denke, Tim Jurgens, and Lutheran Social Services of South Dakota. We appreciate the effort of the regional research assistants who helped administer face-to-face surveys: Julie Babbe, Nicholas Brokenleg, Randy Dobberpuhl, Tina Eberhardt, Gail Hubbeling, Melissa LaPointe, Martina Moves Camp, Jennilee Rooks, Petra Reyna, and Marcie Sprague.
Funding: This study was supported by a grant from The Leona M. and Harry B. Helmsley Charitable Trust (Grant #2014PG-RHC003). Dr. Davis’s time is partially supported by an Agency for Healthcare Research & Quality-Funded Patient Centered Outcomes Research (PCOR) K12 award (Award Number 1 K12 HS022981 01).
Footnotes
Disclosures: The authors report no conflicts of interest. This study was approved by the Oregon Health & Science University Institutional Review Board (#9606). Respondents were advised that the survey was voluntary and they could stop at any time.
Five of the 7 participating reservation towns/tribal areas required targeted oversampling because the tribal lands/reservation only made up part of the county. Two reservations did not require oversampling because their geographic areas covered 1 or more counties in their entirety.
Supporting Information
Additional supporting information may be found in the online version of this article at the publisher’s web site.
Appendix 1. Study Instrument, The South Dakota Health Survey (SDHS).
References
- 1.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torio CM, Andrews RM. Geographic Variation in Potentially Preventable Hospitalizations for Acute and Chronic Conditions, 2005–2011: Statistical Brief# 178. 2006. Available at: http://europepmc.org/abstract/med/25411684 Accessed February 20, 2015. [PubMed]
- 3.Joynt KE, Orav EJ, Jha AK. Mortality rates for medicare beneficiaries admitted to critical access and non-critical access hospitals, 2002–2010. JAMA. 2013;309(13):1379–1387. doi: 10.1001/jama.2013.2366. [DOI] [PubMed] [Google Scholar]
- 4.Gamm L, Hutchison L, Bellamy G, Dabney BJ. Rural healthy people 2010: identifying rural health priorities and models for practice. J Rural Health. 2002;18(1):9–14. [DOI] [PubMed] [Google Scholar]
- 5.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004;94(10):1682–1686. doi: 10.2105/AJPH.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connor A, Wellenius G. Rural–urban disparities in the prevalence of diabetes and coronary heart disease. Public Health. 2012;126(10):813–820. doi: 10.1016/j.puhe.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 7.Eberhardt M, Ingram D, Makuc D. Urban and Rural Health Chartbook. Hyattsville, Maryland: National Center for Health Statistics; 2001. Accessed March 9, 2015. [Google Scholar]
- 8.Singh GK, Williams SD, Siahpush M, Mulhollen A. Socioeconomic, rural-urban, and racial inequalities in US Cancer Mortality: Part I—All cancers and lung cancer and Part II—Colorectal, prostate, breast, and cervical cancers. J Cancer Epidemiol. 2011;2011:1–27. doi: 10.1155/2011/107497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sariego J. Patterns of breast cancer presentation in the US: does geography matter? Am Surg. 2009;75:545–549. [DOI] [PubMed] [Google Scholar]
- 10.Krishna S, Gillespie KN, McBride TM. Diabetes burden and access to preventive care in the rural United States. J Rural Health. 2010;26(1):3–11. doi: 10.1111/j.1748-0361.2009.00259.x. [DOI] [PubMed] [Google Scholar]
- 11.Joyce Fan Z, Lackland DT, Lipsitz SR, et al. Geographical patterns of end-stage renal disease incidence and risk factors in rural and urban areas of South Carolina. Health Place. 2007;13(1):179–187. doi: 10.1016/j.healthplace.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Grossman D, Kim A, MacDonald S, Klein O, Copass M, Maier R. Urban-rural differences in prehospital care of major trauma. J Trauma Inj Infect Crit Care. 1997;42:723–729. [DOI] [PubMed] [Google Scholar]
- 13.Meit M, Knudson A, Gilbert T, et al. The 2014 Update of the Rural-Urban Chartbook Rural Health Reform Policy Res Cent. 2014. Available at: http://ruralhealth.und.edu/projects/health-reform-policy-research-center/pdf/2014-rural-urban-chartbook-update.pdf Accessed February 20, 2015. [Google Scholar]
- 14.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health. 2008;29(1): x115–129. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- 15.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 16.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64(5):566. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. NEngl J Med. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the united states: results from the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 19.Kessler RC, Chiu W, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUH_resultsPDFWHTML2013/Web/NSDUHresults2013.pdf Accessed March 9, 2015. [Google Scholar]
- 21.Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Arch Gen Psychiatry. 2005;62(1):99–108. [DOI] [PubMed] [Google Scholar]
- 22.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand. 2010;121(2):84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 23.Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? J Psychiatr Res. 2014;56:50–55. doi: 10.1016/j.jpsychires.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Weaver A, Himle JA, Taylor RJ, Matusko NN, Abelson JM. Urban vs rural residence and the prevalence of depression and mood disorder among African American women and non-Hispanic White Women. JAMA Psychiatry. 2015;72(6):576–583. doi: 10.1001/jamapsychiatry.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beronio K, Glied S, Frank R. How the affordable care act and mental health parity and addiction equity act greatly expand coverage of behavioral health care. J Behav Health ServRes. 2014;41(4):410–428.doi: 10.1007/s11414-014-9412-0. [DOI] [PubMed] [Google Scholar]
- 26.Improving the quality of health care for mental and substance-use conditions: quality chasm series. Inst Med. Available at: http://www.iom.edu/Reports/2005/Improving-the-Quality-of-Health-Care-for-Mental-and-Substance-Use-Conditions-Quality-Chasm-Series.aspx Accessed January 3, 2014. [PubMed]
- 27.Barry CL, Huskamp HA. Moving beyond parity — mental health and addiction care under the ACA. N Engl JMed. 2011;365(11):973–975. doi: 10.1056/NEJMp1108649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mechanic D. Seizing opportunities under the affordable care act for transforming the mental and behavioral health system. Health Aff (Millwood). 2012;31(2):376–382. 40. doi: 10.1377/hlthaff.2011.0623. [DOI] [PubMed] [Google Scholar]
- 29.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home; February 2007. Available at: http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf Accessed July 23, 2015. [Google Scholar]
- 30.Baird M, Blount A, Brungardt S, et al. Joint principles: integrating behavioral health care into the patient-centered medical home. Ann Fam Med. 2014;12(2):183–185. doi: 10.1370/afm.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Young J, Gilwee J, Holman M, Messier R, Kelly M, Kessler R. Mental health, substance abuse, and health behavior intervention as part of the patient-centered medical home: a case study. Transl Behav Med. 2012;2(3):345–354. doi: 10.1007/s13142-012-0148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waitzkin H, Williams RL, Bock JA, McCloskey J, Willging C, Wagner W. Safety-net institutions buffer the impact of Medicaid managed care: a multi-method assessment in a rural state. Am J Public Health. 2002;92(4):598–610. doi: 10.2105/AJPH.92.4.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ku L, Jones K, Shin P, Bruen B, Hayes K. The states’ next challenge—securing primary care for expanded Medicaid 46. populations. N Engl J Med. 2011;364(6):493–495. [DOI] [PubMed] [Google Scholar]
- 34.Newkirk II VR, Damico A. The Affordable Care Act and Insurance Coverage in Rural Areas. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2014. Available at: http://kff.org/uninsured/issue-brief/the-affordable-care-act-and-insurance-coverage-in-rural-areas/ Accessed March 9, 2015. [Google Scholar]
- 35.Gale JA, Edmund S. The Provision of Mental Health Services 48. by Rural Health Clinics Portland, ME: Maine Rural Health Research Center; 2010. Available at: http://muskie.usm.maine.edu/Publications/rural/WP43/Rural-Health-Clinics-Mental-Health-Services.pdf Accessed July 23, 2015. [Google Scholar]
- 36.Himelhoch S, Ehrenreich M. Psychotherapy by primary-care providers: results of a national sample. Psychosomatics. 2007;48(4):325–330. [DOI] [PubMed] [Google Scholar]
- 37.Borders TF, Booth BM. Research on rural residence and access to drug abuse services: where are we and where do we go? J Rural Health. 2007;23(s1):79–83. [DOI] [PubMed] [Google Scholar]
- 38.Anderson RL, Josephine Gittler JD. Unmet need for community-based mental health and substance use treatment among rural adolescents. Community Ment Health J. 2005;41(1):35–49. doi: 10.1007/s10597-005-2598-0. [DOI] [PubMed] [Google Scholar]
- 39.Dotson JAW, Roll JM, Packer RR, Lewis JM, McPherson S, Howell D. Urban and rural utilization of evidence-based practices for substance use and mental health disorders: variations in evidence-based practice utilization. J Rural Health. 2014;30(3):292–299. doi: 10.1111/jrh.12068. [DOI] [PubMed] [Google Scholar]
- 40.Booth BM, Kirchner JE, Fortney J, Ross R, Rost K. Rural at-risk drinkers: correlates and one-year use of alcoholism treatment services. J Stud Alcohol. 2000;61:267–277. [DOI] [PubMed] [Google Scholar]
- 41.Rost K, Fortney J, Zhang M, Smith J, Smith GRS Jr. Treatment of Depression in Rural Arkansas: Policy Implications for Improving Care. J Rural Health. 1999;15(3):308–315. doi: 10.1111/j.1748-0361.1999.tb00752.x. [DOI] [PubMed] [Google Scholar]
- 42.Borders TF, Booth BM, Stewart KE, Cheney AM, Curran GM. Rural/urban residence, access, and perceived need for treatment among African American cocaine users: perceived need for drug use treatment. J Rural Health. 2015;31(1):98–107. doi: 10.1111/jrh.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Penchansky R, Thomas J. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–140. [DOI] [PubMed] [Google Scholar]
- 44.Rost K, Adams S, Xu S, Dong F. Rural-urban differences in hospitalization rates of primary care patients with depression. Psychiatr Serv. 2007;58(4):503–508. [DOI] [PubMed] [Google Scholar]
- 45.Ziller EC, Anderson NJ, Coburn AF. Access to rural mental health services: service use and out-of-pocket costs: access to rural mental health services. J Rural Health. 2010;26(3):214–224. doi: 10.1111/j.1748-0361.2010.00291.x. [DOI] [PubMed] [Google Scholar]
- 46.Fortney JC, Harman JS, Xu S, Dong F. The association between rural residence and the use, type, and quality of depression care: rural residence and depression care. J Rural Health. 2010;26(3):205–213. doi: 10.1111/j.1748-0361.2010.00290.x. [DOI] [PubMed] [Google Scholar]
- 47.McAuliffe WE, LaBrie R, Woodworth R, Zhang C, Dunn RP. State substance abuse treatment gaps. Am J Addict. 2003;12(2):101–121. doi: 10.1080/10550490390201371. [DOI] [PubMed] [Google Scholar]
- 48.Borders TF, Booth BM. Rural, suburban, and urban variations in alcohol consumption in the United States: findings from the National Epidemiologic Survey on alcohol and related conditions. J Rural Health. 2007;23(4):314–321. [DOI] [PubMed] [Google Scholar]
- 49.Rossen LM, Khan D, Warner M. Trends and geographic patterns in drug-poisoning death rates in the U.S., 1999–2009. Am JPrevMed. 2013;45(6):e19–e25. doi: 10.1016/j.amepre.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rossen LM, Khan D, Warner M. Hot spots in mortality from drug poisoning in the United States, 2007–2009. Health Place. 2014;26:14–20. doi: 10.1016/j.healthplace.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.University of Washington Rural Health Research Center. Rural-Urban Commuting Area Codes. 2005. Available at: http://depts.washington.edu/uwruca/ruca-codes.php Accessed February 9, 2015.
- 52.University of North Dakota Center for Rural Health. Rural-Urban Commuting Areas Version 3.10. 2014. Available at: http://ruralhealth.und.edu/ruca Accessed February 9, 2015.
- 53.United States Census Bureau. State and County QuickFacts. July 2014. Available at: http://www.census.gov/quickfacts/table/PST045214/00,46 Accessed July 23, 2015.
- 54.United States Census Bureau. 2013. American Community Survey. Available at: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk Accessed January 7, 2015.
- 55.Kroenke K, Spitzer R, Williams J, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 56.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. [DOI] [PubMed] [Google Scholar]
- 57.Kroenke K, Spitzer RL, Williams JB, Monahan P, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 58.Prins A, Ouimette P, Kimerling R, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry. 2004;9(1):9–14. doi: 10.1185/135525703125002360. [DOI] [Google Scholar]
- 59.Bush KR, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. Ambulatory Care Quality Improvement Project. The AUDIT Alcohol Consumption Questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 60.Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT): validation in a female veterans affairs patient population. Arch Intern Med. 2003;163(7):821. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- 61.Bradley KA, Bush KR, McDonell MB, Malone T, Fihn SD. Ambulatory Care Quality Improvement Project. Screening for problem drinking: Comparison of CAGE and AUDIT. J Gen Intern Med. 1998;13(6):379–388. doi: 10.1046/j.1525-1497.1998.00118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUH_resultsPDFWHTML2013/Web/NSDUHresults2013.pdf Accessed February 9, 2015. [Google Scholar]
- 63.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Questionnaire. 2013. Available at: http://www.cdc.gov/brfss/questionnaires.htm Accessed February 9, 2015. [Google Scholar]
- 64.Agency for Healthcare Research and Quality. CAHPS Health Plan Survey. Available at: https://cahps.ahrq.gov/health_plan/ Accessed February 9, 2015. [Google Scholar]
- 65.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire. Hyattsville, Maryland: U.S: Department of Health and Human Services, Centers for Disease Control and Prevention; 2013. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2013-2014/questionnaires13_14.htm Accessed July 23, 2015. [Google Scholar]
- 66.Agency for Healthcare Research and Quality. CAHPS CAinician & Group Survey, Adult Primary Care Instrument. Rockville, MD; 2008. Available at: https://www.cahps.ahrq.gov/surveys-guidance/cg/instructions/index.html Accessed July 23, 2015. [Google Scholar]
- 67.Wright BJ, Carlson MJ, Edlund T, DeVoe J, Gallia C, Smith J. The impact of increased cost sharing on medicaid enrollees. Health Aff (Millwood). 2005;24(4):1106–1116. doi: 10.1377/hlthaff.24.4.1106. [DOI] [PubMed] [Google Scholar]
- 68.Carlson MJ, DeVoe J, Wright BJ. Short-term impacts of coverage loss in a medicaid population: early results from a prospective cohort study of the Oregon health plan. Ann FamMed. 2006;4(5):391–398. doi: 10.1370/afm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Interian A, Ang A, Gara MA, Link BG, Rodriguez MA, Vega WA. Stigma and depression treatment utilization among Latinos: utility of four stigma measures. Psychiatr ServWash DC. 2010;61(4):373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine Definition of Disparities: an application to mental health care. Health ServRes. 2006;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. Accessed June 24, 2015. [Google Scholar]
- 72.Gfroerer JC, Larson SL, Colliver JD. Drug use patterns and trends in rural communities. J Rural Health. 2007;23(s1):10–15. [DOI] [PubMed] [Google Scholar]
- 73.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 74.Aday LA, Andersen R. A framework for the study of access to medical care. Health ServRes. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- 75.Edlund MJ, Untitzer J, Curran GM. Perceived need for alcohol, drug, and mental health treatment. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):480–487. doi: 10.1007/s00127-006-0047-1. [DOI] [PubMed] [Google Scholar]
- 76.Edlund M, Booth B, Feldman Z. Perceived need for treatment for alcohol use disorders: results from two national surveys. Psychiatr Serv. 2009;60(12): 1618–1628. doi: 10.1176/appi.ps.60.12.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. JAMA Psychiatry. 2002;59(1):77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 78.Falck RS, Wang J, Carlson RG, Krishnan LL, Leukefeld C, Booth BM. Perceived need for substance abuse treatment among illicit stimulant drug users in rural areas of Ohio, Arkansas, and Kentucky. Drug Alcohol Depend. 2007;91(2–3):107–114. doi: 10.1016/j.drugalcdep.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decision. July 2015. Available at: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ Accessed July 24, 2015.
- 80.Thielke S, Vannoy S, Uniitzer J. Integrating mental health and primary care. Prim Care Clin OffPract. 2007;34(3):571–592. doi: 10.1016/j.pop.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 81.Davis M, Balasubramanian BA, Waller E, Miller BF, Green LA, Cohen DJ. Integrating behavioral and physical health care in the real world: early lessons from advancing care together. J Am Board Fam Med. 2013;26(5):588–602. [DOI] [PubMed] [Google Scholar]
- 82.Thomas K, Ellis A, Konrad T, Holzer C, Morrissey J. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009; 60(10):1323–1328. doi: 10.1176/appi.ps.60.10.1323. [DOI] [PubMed] [Google Scholar]
- 83.Bischoff RJ, Hollist CS, Smith CW, Flack P. Addressing the mental health needs of the rural underserved: Findings from a multiple case study of a behavioral telehealth project. Contemp Fam Ther. 2004;26(2): 179–198. [Google Scholar]
- 84.Grubaugh AL, Cain GD, Elhai JD, Patrick SL, Frueh BC. Attitudes toward medical and mental health care delivered via telehealth applications among rural and urban primary care patients. JNervMentDis. 2008; 196(2):166–170. doi: 10.1097/NMD.0b013e318162aa2d. [DOI] [PubMed] [Google Scholar]
- 85.Swinton JJ, Robinson WD, Bischoff RJ. Telehealth and rural depression: physician and patient perspectives. Fam SystHealth. 2009;27(2):172–182. doi: 10.1037/a0016014. [DOI] [PubMed] [Google Scholar]
- 86.Broffman L, Spurlock M, Dulacki K, et al. Understanding treatment gaps for mental health, alcohol, and drug use in South Dakota: a qualitative study of rural perspectives. J Rural Health. In Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Asch D, Jedrziewski M, Christakis N. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. [DOI] [PubMed] [Google Scholar]
- 88.Baruch Y, Holtom BC. Survey response rate levels and trends in organizational research. Hum Relat. 2008; 61(8):1139–1160. doi: 10.1177/0018726708094863. [DOI] [Google Scholar]
- 89.Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805–1806. [DOI] [PubMed] [Google Scholar]
- 90.Caton C, Dominguez B, Schanzer B, et al. Risk factors for long-term homelessness: findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005;95(10):1753–1759. doi: 10.2105/AJPH.2005.063321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.United States Department of Housing and Urban Development. The 2010 Annual Homeless Assessment Report to Congress.; 2011. Available at: https://www.hud_exchange.info/resources/documents/2010Homeless_AssessmentReport.pdf Accessed July 23, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.