Dear Editor,
The anxiety and trauma associated with the tragic coronavirus disease pandemic coded, COVID-19 led many to indulge in various unorthodox preventive measures such as the extensive indiscriminate use of alcohol-based hand sanitizers (ABHS), abuse, misuse, overdose of prescription drugs like chloroquine, hydroxychloroquine and chloroquine phosphate globally. While some preventive measures are recommended and adopted, such as national lockdown, self-isolation, quarantine, stay-at-home model, avoidance of large gathering, social distancing, wearing of face-masks and hand gloves, periodic hand washing particularly with liquid soaps/detergents under running tap water, avoidance of touching the face among others, the use of ABHS has been more prominent. ABHS contains on average 60-70 % by weight of one or more alcohols. During the 2019/2020 COVID-19 pandemic, the use of ABHS was more renowned to the extent that some individuals recommended the application on the hands every 30 minutes for a period of at least 20 seconds while outside the home. Though, the periodic application of the hand sanitizers seems like an effective on-the-go solution to preventing the spread of the virus, many other associated hazards call for caution. Besides transdermal absorption leading to mortality and morbidity of varying degree; alcohol-alcohol adulteration, deliberate and unintentional ingestion of ABHS may result in respiratory depression, irreversible blindness, intoxication, cirrhosis, acidosis, headache, central nervous system depression, seizure, hypoglycemia, coma, or even death in some cases. The non-ABHS are equally not absolutely safe as many of them contain active agents that are allegedly carcinogenic, toxic, inducing microbial resistance and endocrine disruption. Considered together, this implies that while some may not die from contracting the disease, the preventive measures taken could lead to death or other forms of morbidity thereby revealing that there is indeed, death in preventive measures when done without cautionary measures. This study seeks to highlight some associated risks in the use of ABHS and non-ABHS, whilst advocating the use of safer or 'greener' alternative procedure for use as preventive measures particularly during the COVID-19 pandemic.
The sudden outbreak of the coronavirus disease epidemic preferably referred to as COVID-19 was a tragic global pandemic that claimed over 190,000 lives with over two million reported cases spreading across 210 countries within the first five months (December, 2019 - 24th April, 2020) of the outbreak across the globe (Worldometers, 2020[102]). While the highest toll of mortality remained in China, Italy, Spain and America as at the end of March, 2020, many Asian and tropical African countries such as Iran, South Africa, Algeria, Egypt, Nigeria and Cameroon had got their acrid taste of the pandemic. The fear, anxiety and emotional trauma associated with the outbreak of COVID-19 which started from the Wuhan Province in China in December 2019 was quite rattling, monumental and terrific as many erroneously regarded contracting the infection as a death penalty. In fact, infected individuals who recovered from the disease are stigmatized and disenfranchised, segregated and avoided. The long and short term implications of contracting the disease made citizens of most countries to intensify efforts at preventing the COVID-19 disease. While global mortality rate rose to 3.4 % in some countries (Worldometers, 2020[102]), the trauma associated with the infection had no limit. The incident obviously led to improvement in hand hygiene (HH) in order to curtail the spread of the virus. This has brought to limelight the prominence of alcohol-based hand sanitizer, ABHS and other non-alcohol based hand sanitizers as well as household disinfectants.
Common preventive measures against the COVID-19
As at this moment, there is no vaccine for the prevention of COVID-19. The best prevention is to avoid being exposed to the virus (Adhikari et al., 2020[1]). As a result of this, government and individuals adopted various measures in preventing the spread of the disease. The government and health sector' advocacy groups contributed tremendously to the spike in the use of various preventive methods such as city/town and national lockdown, self-isolation, quarantine, stay-at-home model, avoidance of crowd, social distancing, wearing of face-mask and hand gloves, periodic hand washing particularly with liquid soaps/detergents, use of ABHS, avoidance of touching the face among others. Following unsubstantiated claims, some individuals in the developing countries resulted to the overconsumption of acclaimed immune-boosting substances such as ginger, garlic, lemon fruits, and salt solution etc. Besides, some in the tropical countries believed that the hot weather could reduce the chances of survival of the virus, hence, they resulted to staying long hours in the bright day sunlight and/or periodic consumption of hot drinks such as water, tea and juice with the intention of providing an unhealthy high temperature environment for the survival of the infectious virus. Some other people resulted to the consumption of food or substances that increases the pH of the body to the alkaline region since there were unsubstantiated claims that the virus does not survive at alkalinic pH. Although viruses are sensitive to pH and temperature changes and cannot survive beyond a narrow range (Sturman et al., 1990[85]; Mi et al., 2019[62]), a crude means of achieving such could be more deadly than envisaged.
Moreover, the tentative approval by the United States tentative of chloroquine-based therapy as trial for the management of COVID-19 patients on compassionate ground (based on WHO guideline), led some individuals to an unethical practice of the indiscriminate consumption of chloroquine-based drugs as both prophylaxis and curative. Although, initial trials indicated some interesting positive results at minute doses (Gao et al., 2020[33]; Liu et al., 2020[54]; Singh et al., 2020[82]), reports are still premature and yet to be universally accepted. If clinical data confirm the antiviral activity of chloroquine-based drugs, the novel COVID-19 could become one of the cheapest and simplest to treat among infectious respiratory diseases. This is because the drugs are quite affordable (Raoult et al., 2020[73]). The affordability and accessibility of the chloroquine-based drugs partly led to the abuse with resultant lethality and health hazards which included abdominal discomfort, coma and even death in some cases (Wong et al., 2011[101]). In fact, the moderate dose of chloroquine can cause effects such as depression, psychosis, delirium, mood swing, personality change among others (Good and Shader, 1982[36]). The close derivative, hydroxychloroquine is also known to possess side effects such as retinal toxicity, cardiovascular toxicity, refractory shock and ventricular arrhythmias (Fung et al., 2007[32]; Rüther et al., 2007[76]; Marmor et al., 2016[60]; Tsang et al, 2019[91]). Meanwhile, chloroquine phosphate and a few other derivatives have been reported as potential anti-dote to COVID-19 infection (Gao et al., 2020[33]; Sahraei et al., 2020[78]).
Although, many of these preventive measures were often adopted, many of them frequently present mild to severe implications with only a few of them proving really potent and safe. In reality, some of the measures were quite detrimental to human health and it could result to death before even contracting the dreaded viral infection, COVID-19 (Choi et al., 2017[22]; Chan and Chan, 2018[20]). While all the measures adopted thus far have both their merits and demerits, this report focuses more on the chemistry of the death and the associated danger, particularly in the use of hand sanitizers and other applied preventive chemicals against the spread of COVID-19 as well as other germs.
Chemical compositions of household products for preventive measures against COVID-19
The advent of the COVID-19 outbreak marked the commencement of the surge in the series of industrial and domestic-made chemicals like the hand sanitizers, liquid soaps, disinfectants and others. The upsurge in the global consumption of hand sanitizers following the COVID-19 pandemic was unprecedentedly geometrical. The use of hand sanitizer became well renowned to the extent that some individuals apply on their hands every 30 minutes especially when outside the home. While the practice seems a plausibly effective on-the-go solution in the prevention of the spread of the viral infection, other serious dangers are quite associated. Although, microorganisms pervade almost everywhere human survives (Bhoonderowa et al., 2014[10]; Kõljalg et al., 2017[47]) and the use of sanitizers can help in minimizing their spread and deleterious effect on human, the frequent use may however pre-dispose users to some degree of fatality (Chan et al., 2017[21]; Chan and Chan, 2018[20]).
Various sub-standard brands of hand sanitizers flooded both offline and online markets in the developed and developing countries. Besides the hike in the prices of these household products, their acquisition could be tantamount to self-purchase of quicker “death”. While the chemical composition of the various household antiviral preventive products used is sometimes regional or country-based, some chemicals are more accessible and universal to all. Some of them are thus discussed herein.
Hand sanitizers and disinfecting soaps
Hand sanitizers are hygienic products that are applied on the hands to prevent the spread of microorganisms like viruses, bacterial and fungi such as coronaviruses, rhinoviruses, influenza viruses, herpes simplex virus, ebola virus, Staphylococcus aureus, Enterococcus faecalis, Escherichia coli, traveller diarrhoea among others, especially where access to water is limited (Fendler et al., 2002[30]; Conover and Gibson, 2016[24]; Wolfe et al., 2017[100]; Thaddeus et al., 2018[87]; Kuenzli et al., 2019[50]). Hand sanitizers, though, originally developed for the healthcare sector (Ascenzi, 1995[3]; Block, 2001[12]), it has become a routine for many people to carry hand sanitizer with them at all times, especially during the recent disease outbreak.
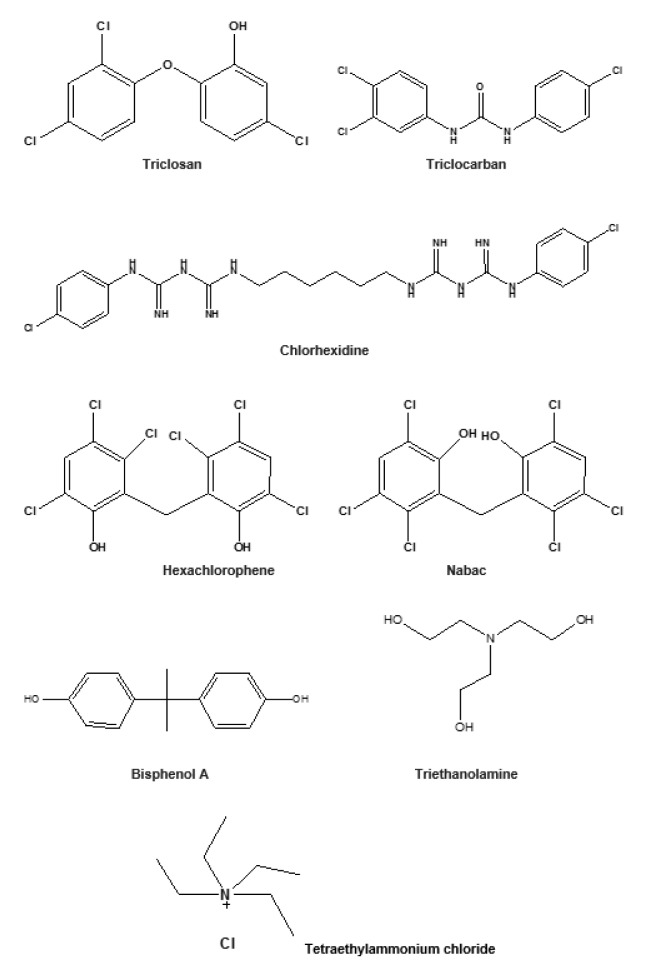
Industrial and home-made hand sanitizers are made of various chemical compositions subject to what is locally available. A brief check of brands on the internet, local markets and the literatures indicated two main categories of sanitizers; alcohol-based and non-alcohol-based hand sanitizers (NABHS). The alcohol-based hand sanitizers (ABHS) are primarily composed of alcohols such as either ethanol, isopropyl alcohol, propan-1-ol or propan-2-ol; and additives such as colorants, stabilizers, fragrance and sometimes preservatives which may include formaldehyde, parabens among other chemicals (Luby et al., 2004[57], 2005[56]; Kramer et al., 2007[48]; Napolitani et al., 2020[65]). Other chemicals usually added for various purposes include polyacrylic acid, glycerin, carbomer, propylene glycol, triethanolamine (trolamine), tetraethylammonium chloride, dichlorodimethylphenol (Figure 1(Fig. 1)), chlorine, deionized water, and extract of plants (Wolfe et al., 2017[100]; Thaddeus et al., 2018[87]; Surini et al., 2018[86]). The World Health Organization guideline for the preparation of ABHS revealed the composition to be 80 % ethanol, 1.45 % glycerol and 0.125 % hydrogen peroxide or 75 % isopropyl alcohol, 1.45 % glycerol and 0.125 % hydrogen peroxide (WHO, 2010[97]). On the other hand, the non-alcohol based hand sanitizers (NABHS) are made up of various chemicals similar to the component found in the alcohol-based type with the exclusion of alcohol. However, anti-microbial or disinfecting agents such as triclosan (TCS), triclocarban, sodium hypochlorite, chlorhexidine, benzalkonium chloride and benzithonium chloride are often added (Hayat and Munnawar, 2016[42]; Bondurant et al., 2019[13]).
Figure 1. Some active agents used in sanitizers and disinfectants.
Some of the chemicals used in various disinfectants include chloroxyphenol B, oleum aromaticum, triclosan, triethanolamine, tetraethylammonium, dichlorodimethylphenol, chlorine, etc. It is quite imperative that antimicrobial agents, disinfectants and antiseptics substances possess strong activities against the pathogens including the biofilm-forming pathogens, else antimicrobial resistance could easily develop (Bridier et al., 2011[16]; Hauser et al., 2016[41]; Ghanem et al., 2018[35]). The assumption has led to the use of extremely strong and sometimes hazardous chemicals as disinfectants. For effectiveness or improved potency, combinations of two or more active ingredients are often used in some anti-viral disinfectants (Ahmed et al., 2020[2]).
A newly developed NABHS which contains only 14 % alcohol by volume and usually applied in small volume was reported to work synergistically with the other active agent in the sanitizer via a system called “quad system technology” to kill the virus and other germs (Cavage, 2010[17]).
Generally, in ABHS, formulations with ethanol between 60 and 95 % are known to be significantly effective in preventing spread of microbial infections (Kramer et al., 2002[49]) and are generally regarded safe (FDA, 1994[29]). WHO recommends washing of hands under running tap water, and when the resources for that is not available, ABHS comes handy. However, the ABHS are recommended over the use of soap due to its ease of use and capability in stalling microbial spread (WHO 2009[98]; Hayat and Munnawar, 2016[42]). However, some other potential alternatives such as nonorganic antibiotics and organic or natural biocides have been proposed in place of triclosan due to some of the reported side effects (Kim et al., 2007[46]).
Associated hazards with ABHS for the prevention of COVID-19
Many ABHS carry a lot of risks. First, most ABHS contain alcohols in excess of 60 % which made them to be classified as Class I Flammable Liquid substance as a result of their flash point below 100 °C Fahrenheit (Kramer et al., 2002[49]; FDA, 2020[28]). Precisely, ethanol 80 % (v/v) and isopropyl alcohol 75 % (v/v) have flash points of 17.5 °C and 19 °C, respectively (WHO, 2020[95]). This quite indicates that the products can ignite at relatively low temperatures.
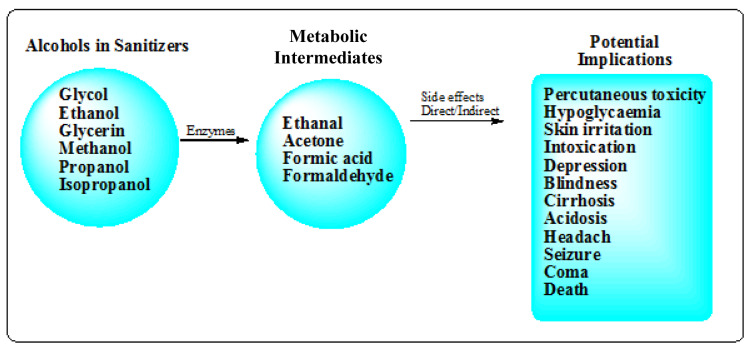
Hence, ABHS increase the risk of fire accidents. Although, ABHS are a more accessible and usually a preferred choice for many people during epidemics like the COVID-19 compared to choices like the towelettes (Rai et al., 2017[72]), yet they carry their own significant risks. The risk associated with the use of the ABHS includes accidental poisoning via ingestion, fire hazard, organ toxicity via absorption through the skin among others (Figure 2(Fig. 2)). Children are often attracted to the nature, smell and cool feel of alcohol on the skin and series of accidental poisonings, including fatal ones in child ren have been reported (Chan and Chan, 2018[20]). For instance, investigation carried out on young children who swallowed ABHS revealed that they were diagnosed of apnea, acidosis and some even went into coma (Rayar and Ratnapalan, 2013[74]). It has been established that younger children have decreased liver glycogen stores, which increases their risk of developing hypoglycemia and have various pharmacokinetic factors, which make them more susceptible to developing toxicity from alcohol (Tran et al., 2007[89]; Marek and Kraft, 2014[59]).
Figure 2. Potential health hazards of ingested or skin-absorbed alcohols in ABHS.
In addition, alcohol-alcohol dilution is a major contamination in the industry. A more affordable alcohol with similar physical properties is sometimes used to adulterate another alcohol for pecuniary profit. If the ethanol for instance, is adulterated with other toxic alcohols such as methanol, irreversible blindness, coma or even death could result (Gormley et al., 2012[37]; Forrester, 2015[31]; Moore, 2019[63]). Methanol is known to be more lethal than ethanol as unintentional ingestion by children and deliberate consumption by older subjects often lead to poisoning requiring prompt antidotal therapy, critical care in addition to other supporting therapy (Chan and Chan, 2018[20]). Methanol is reportedly more toxic when inhaled, or exposed to human orally or through the skin. Alcohol concentration in the blood could increase via absorption through the skin when used frequently. Due to its toxicity, it is therefore strongly not recommended for use in hand sanitizers. However, some reports indicated that such contaminations have been observed in ABHS (Mowry et al., 2015[64]; Chan and Chan, 2018[20]). Transdermal poisoning resulting from skin absorption of methanol is well reported (Qiao and Guo, 1992[71]; Ryu et al., 2016[77]). In fact, exposure to methanol was reported to cause multiple sclerosis (Henzi, 1984[43]). Other types of alcohol-alcohol intoxication and poisoning have been reported (Chan et al., 2017[21]; Chan and Chan, 2018[20]).
The commonly used alcohol in ABHS, ethanol, is a known toxicant and central nervous (CNS) depressant capable of inducing hypoglycemia (Baum 2017[9]; Moore, 2019[63]). The use of isopropanol-based hand sanitizers carries equal or even greater risk than ethanol-based counterparts. Isopropanol besides being intoxicating, it is converted in the liver to acetone (propanone) which causes greater CNS depression than ethanol (Litovitz, 1986[53]). Various deaths and morbidities associated with ABHS have been reported (Gormley et al., 2012[37]; Darracq et al., 2013[25]; Jones et al., 2013[45]; Forrester, 2015[31]; Basyal et al., 2018[8]; Moore, 2019[63]). Interestingly, there has been emerging cases of alcohol-tolerant microorganisms which therefore cast aspersion on the future of the use of alcohol in hand sanitizers (Pidot et al., 2018[70]; Bondurant et al., 2019[14]). It is predicted that more organisms would develop resistance to alcohol in the near future if indiscriminate discharge to the environment is not controlled.
Other adverse health effects that could result from both ABHS and NABHS include ocular irritation, vomiting, conjunctivitis, oral irritation, cough, and abdominal pain (Qiao and Guo, 1992[71]; Choi et al., 2017[22]; Chan and Chan, 2018[20]). In some rare scenario, adverse effects could include acidosis, respiratory depression, headache, hypoglycemia, irreversible blindness, central nervous system depression, seizure, coma and death (Figure 2(Fig. 2)). These effects are noted to be more severe in ABHS (Bonner, 2017[15]; Choi et al., 2017[22]; Chan and Chan, 2018[20]). The continuous use or overuse of hand sanitizers can cause chronic irritation and severe skin breakdown among other effects (Qiao and Guo, 1992[71]), especially in children. A study that reported the incidences of poisoning associated with ABHS between 2011 and 2014 indicated that children below 12 years had incidences of over 70,000 exposures to hand sanitizers, of which 92 % are due to ABHS with only 8 % NABHS exposure (Bonner, 2017[15]).
Furthermore, the continuous topical application of ethanol on the skin was reported to lower skin barrier functions, thereby rending the membrane highly susceptible to harmful chemicals in soaps and cosmetics (Lachenmeier, 2008[51]). Moreso, percutaneous toxicity could also occur in children with lacerated skin (Lachenmeier, 2008[51]). In fact, the potential for abuse of ABHS has raised more concern now than before. Although, ABHS seem easier to use and proved higher efficiency than some detergent-based sanitizers, the repeated exposure of users to the ABHS calls for caution (Perez et al., 2019[69]).
Environmental hazards of triclosan in hand sanitizers and liquid soaps
Triclosan (TCS: 2, 4, 4'-trichloro-2'-hydroxydiphenyl ether) is a universal antimicrobial agent that has found its way into many pharmaceuticals and personal care products as well as in the promotion of growth in animal including aquatic species (Daughton and Ternes, 1999[26]). It is used as antibacterial agent in many consumers' and household products such as medicated soaps, hand sanitizers, deodorants, toothpastes, air fresheners and other cosmetic products (Sethuraman et al., 2014[80]). It is currently being considered as an emerging contaminant (Wang et al., 2018[93]).
Triclosan with its related compound, triclocarban (Figure 1(Fig. 1)) used in consumer's products such as liquid soaps and hand sanitizers previous mentioned is of paramount concerns to scientists due to its long persistency in the environment (FDA, 2016[27]; USGS, 2016[92]). Its ability to cause disruption of the endocrine (hormone) system is still being evaluated and already recommended to be avoided (Bonner, 2017[15]; Stoker et al., 2010[84]). It was classed as a pesticide in the National Pesticide Information Retrieval System (NPIRS [Triclosan], 2020[67]) of the United States. Previously, hexachlorophene, an organochlorine compound known as Nabac (Figure 1(Fig. 1)) with structural similarity to triclosan had been banned as disinfectant by the FDA following health concerns due to the allegedly associated teratogenicity (IARC, 1998[44]; Halden, 2014[39]). TCS together with bisphenol A were reported to possess potential to weaken the immune system (Clayton et al., 2011[23]). TCS is reported to cause oxidative stress and induce genotoxicity in goldfish, suggesting a potential ecotoxicological risk to aquatic ecosystems (Stasinakis et al., 2008[83]; Halden, 2014[39]; Silva et al., 2015[81]). TCS has been reported as persistent organic pollutants that are retained for months or years in water bodies (Lygina et al., 2013[58]).
Toxicity and side-effects of disinfectants, adulterated and sub-standard chemicals in soaps and hand sanitizers on the users
Antibiotics abuse, overuse and misuse of soaps and hand sanitizers is often responsible for effects such as antibiotics resistance and endocrine disruption (Atolani et al. 2016[7]; Lu et al., 2018[55]). TCS, a typical antibiotic is commonly used in many soap preparations and some hand sanitizers are known to produce high anti-microbial efficiency. However, many studies have implicated it as a source of induction of antibiotic resistant microorganisms as the use of only 0.2 mg/L TCS for only 30 days can cause multi-drug resistance to Escherichia coli and Staphylococcus aureus of which similar effects were not reported for chlorhexidine or hydrogen peroxide-based agents (Westgate et al., 2016[94]).
The use of alcohol in ABHS is equally not absolutely safe as it can easily be absorbed through the skin. Reports indicated that blood concentration of ethanol could reach 2.3 % within 90 minutes of use of ABHS (Kramer et al., 2007[48]). In the study, ethanol and acetaldehyde concentrations were as high as 1.7 and 1.95 mg/L respectively. Ethanol is often converted to acetaldehyde which is also absorbed into the blood stream (Thompson et al., 2005[88]; NPIRS [Ethanol] 2020[67]). The metabolic products are often more toxic in the human system. High concentration of ethanol in human blood ingested via consumption of alcoholic beverages is known to cause both short-term and long-term toxicity such as inebriation and liver cirrhosis. Hence, the use of ABHS could invariably lead to increased concentration of alcohol in human blood (Kramer et al., 2007[48]).
There are increasing incidences of intentional ingestion of ethanol-containing hand sanitizers especially by alcohol addicts (Gormley et al., 2012[37]). Since children are attracted to the scent, bright coloration and the attractive packaging of ABHS, they are generally more at risk (Rayar and Ratnapalan, 2013[74]). Within 2011 - 2016, U.S. poison control centers reported over 100,000 calls with regards to children exposure to hand sanitizer (Georgia Poison Center, 2015[34]; CDC, 2020[18]).The intoxication by the ingestion of hand sanitizers is a major overlooked risk seeking urgent attention globally (Jones et al., 2013[45]; Raza et al., 2014[75]; Moore, 2019[63]). High degree of morbidity and mortality are risks associated with the use of ABHS (Santos et al., 2017[79]). Therefore, following the proliferation in the production of ABHS due to the COVID-19 pandemic, there is an obvious need for global caution and conscientiousness in the acquisition and utilization of hand sanitizers.
Soaps and ABHS: efficiency versus safety potential
It was reported that most germs or microbial pathogens cannot survive adequate washing with liquid soaps. The structure of most pathogenic bacterial and virus is less resistant to the potency of the alkalinity, the corrosive nature and membrane-shattering ability of most liquid soaps. While the proper washing with the liquid soaps kills the pathogens up to 99.9 % the rinsing with clean water helps to eliminate the dead organisms from hands. Most liquid soaps are water-based; hence, this naturally reduces the skin penetrating effect of some of the components compared to ABHS. Most hand-sanitizers usually organic-based are also known to kill pathogen up to 99.9 % when effectively rubbed on the hand, but the absorption potential through human skin to some vital organs such as the kidney and liver could result to toxicities such as nephrotoxicity, cirrhosis among others (Kramer et al., 2007[48]; Choi et al., 2017[22]; Chan and Chan, 2018[20]).
Since HH is of paramount importance to the prevention of the spread of virus and other germs, the use of safe hand rub, soap, or sanitizers is imperative. Due to associated toxicities and side effects, some hand rubs, soaps and sanitizers contain some chemical compounds which may only be most appropriate for use on non-skin surfaces such as the surfaces of furniture, door handles, walls, phones, glass, toilet zincs, metal tools, vehicles exteriors, electronic gadgets, hospital equipment among others and not on human skin.
In order to underscore the relevance of alcohol in disinfection of non-skin objects, a study reported that a single cleaning with an alcohol wipe proved higher potency than the alcohol-based hand rub in decontamination of stethoscopes used in hospitals (Mehta et al., 2010[61]). Other studies also showed that use of hand sanitizers used outside hospital environment do not show superior benefit to soap (Oughton et al., 2009[68]; CDC, 2020[19]). Hence, washing with soap and warm water with good HH may adequately suffice for homes and as well eliminate exposure to hazardous chemicals and consecutive release to the environment (Wolf et al., 2018[99]). The CDC and some other reports indicated that besides preserving good environmental flora, washing with soap and water produces better or equivalent results compared to ABHS sanitizers at removing or killing certain types of virus such as the noroviruses and other germs (Grayson et al., 2009[38]; Blaney et al., 2011[11]; Bondurant et al., 2019[13]; CDC, 2020[18]).
Impact of excessive use of hand sanitizers on the environment
Hand sanitizers usually end-up being deposited in high concentrations of the constituting chemical residues (contaminants) in the environmental soil and water bodies. High concentration of these chemicals released in the environment could trigger multi-drug resistance (Westgate et al., 2016[94]). Antimicrobial resistance is obviously a major public health concern globally. The World Health Organization (WHO) reported that about 700,000 people died due to antimicrobial-resistant infections every year (WHO, 2019[96]). It is further predicted that the death due to antimicrobial-resistant infections could reach 10 million annually by 2050 if no concrete action is taken now (WHO, 2019[96]).
Preference for the use of ordinary soap or liquid soap for hand sanitizing
Experiment has revealed that washing with ordinary soap solution is effective at killing and eliminating the virus and other germs in the hand. The fatty outer surface of the virus is denatured by the soap molecule and that process leads to the destruction of the virus which is washed away by water. It is worth mentioning that hand washing with soap solution and rinsing with water (preferably warm water) will kill and eliminate the germs from the surface, using of ABHS will kill the organism without eliminating them from the surface. The use of soap and water must be a preferred choice when the hand is visibly or grossly contaminated. ABHS also do not remove pesticide from the hand (CDC, 2020[18]). The use of ABHS in such instances could make the hand so messy and unpleasant. In fact, the Food and Drug Administration (FDA) of the United States already banned the use of triclosan in antibacterial soaps (IARC, 1998[44]; Halden, 2014[39]).
Modern natural “Green” hand sanitizers as preferred alternative to ABHS
Recent advances in the cosmetic industry have led to the production of safe hand sanitizers obtained via green process. This involved the incorporation of safe natural antiseptic agents into soaps, hand rubs or NABHS in place of the synthetic ones that are associated with multiple side effects. Natural products such as plant extracts, exudates, purified isolates and essential oils have been proposed as germ-killers in hand sanitizers, soaps and other cosmetics and body care products (Ningsih et al., 2017[66]; Hartatik, 2014[40]; Lateh, 2015[52]; Surini et al., 2018[86]; Zubair et al., 2018[103][104]; Atolani et al., 2019[6][5]; 2020[4]). Natural products such as coconut oil have been used to produce hand sanitizers with enhanced cosmetic properties (Tran et al., 2019[90]). Such green alternative will preserve the natural environment and the skin of people (Atolani et al., 2016[7]).
Recommendations for use of alcohol-based hand sanitizers and soaps
Following the multiple side-effects associated with the use of ABHS and some liquid soaps due to the “unsafe” active agents in them, the following recommendations have become inevitable:
Manufacturers and Health care providers should advocate the potential dangers associated with abuse, overuse and misuse of ABHS and antibacterial active soaps.
The habitual use of ABHS must be deliberately avoided. As much as it is possible, its use should be occasional when other options such as soap and warm water are not available. This would impact safety of both users and the environment.
Users should only purchase small amount of ABHS at a time to avoid overt addiction and abuse due to the surplus.
The use of hand sanitizer should be limited to only the finger and wrist region as absorption via the arm and other body parts could be increased thereby raising blood alcohol concentration within a short time.
When the use of ABHS is unavoidable, users should ensure use of low concentration alcohol at an average of 60-70 % as higher concentrations could be more deleterious.
The ABHS should be kept far away from heat, flame, spark-source or any oxidizing agents to avoid fire incidence since they are flammable.
Children should not be allowed direct access to ABHS as the fatality of accidental ingestion in children is worse and incidences are on the rise.
In case of liquid soaps; soaps with triclosan or triclocarban and other questionable safety profile should be avoided.
There should be incorporation of skin protecting emollient in ABHS and liquid soap in order to prevent after-use skin dryness, skin breaking/cracking as well as reduce alcohol penetration through the skin.
General cleanliness and good hygiene is imperative to keep microbial infections at bay. Consistent tidiness will minimize the need for repetitive use of liquid soaps and ABHS.
Conclusions
The enormous release of adulterated and uncontrolled infection-preventing household products such as the antibacterial active liquid soap and ABHS in the global markets have several potential adverse health effects on human such as dehydrated skin, irritation, poisoning, and cancer among others. Thus, the careful adoption of hand washing with selected safe liquid soap should be encouraged by all. Improvement in hand hygiene is akin to the containment of the spread of germs, including the ravaging viral infection, COVID-19. However, when the use of hand sanitizer is inevitable, consumers should be cautious of the chemical constituents as well as the concentration of each constituent. These measures are important to the prevention of avoidable implications such as unintentional or deliberate ingestion or chemical absorption through the skin which could lead to incidences such as irreversible blindness, depression, intoxication, liver cirrhosis, acidosis, headache, central nervous system depression, seizure, hypoglycemia, coma and death. While preventing infections such as the COVID-19 and other microbial-induced infections, slow and systematic death should be meticulously avoided. Otherwise, the prevention mode could lead to higher fatality than the infection being avoided.
Notes
Olubunmi Atolani and Oluyomi Stephen Adeyemi (Department of Biochemistry, Medicinal Biochemistry, Infectious Diseases, Nanomedicine & Toxicology Laboratory, Landmark University, PMB 1001, Omu-Aran 251101, Kwara State, Nigeria; E-mail: yomibowa@yahoo.com) equally contributed as corresponding author.
Acknowledgements
Authors appreciate Ton Duc Thang University, Ho Chi Minh City as well as the University of Ilorin, Ilorin, Nigeria.
References
- 1.Adhikari S, Meng S, Wu Y, Mao Y, Ye R, Wang Q, et al. Epidemology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect Dis Pov. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed K, Ahmed H, Ahmed FA, Ali AA, Akbar J, Rana J, et al. Analysis of anti-microbial and anti-biofilm activity of hand washes and sanitizers against S. aureus and P. aeruginosa. J Pak Med Assoc. 2020;70:100–104. doi: 10.5455/JPMA.2776. [DOI] [PubMed] [Google Scholar]
- 3.Ascenzi JM. Handbook of disinfectants and antiseptics. New York, NY: CRC Press; 1995. [Google Scholar]
- 4.Atolani O, Areh ET, Oguntoye OS, Zubair MF, Fabiyi OA, Oyegoke RA, et al. Chemical characterization, antioxidant, cytotoxicity, anti-toxoplasmagondii and antimicrobial potentials of the Citrus sinensis seed oil for sustainable cosmeceutical production. Heliyon. 2020;6(2):e03399. doi: 10.1016/j.heliyon.2020.e03399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atolani O, Areh ET, Oguntoye OS, Zubair MF, Fabiyi OA, Oyegoke RA, et al. Chemical composition, antioxidant, anti-lipooxygenase, antimicrobial, anti-parasite and cytotoxicity of Polyalthia longifolia seed oil. Med Chem Res. 2019;22:12. [Google Scholar]
- 6.Atolani O, Oguntoye H, Areh ET, Adeyemi OS, Kambizi L. Chemical composition, anti-toxoplasma, cytotoxicity, antioxidant, and anti-inflammatory potential of Cola gigantea seed oil. Pharm Biol. 2019;57:154–60. doi: 10.1080/13880209.2019.1577468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atolani O, Olabiyi ET, Issa AA, Azeez HT, Onoja EG, Ibrahim SO, et al. Green synthesis and characterization of natural antiseptic soaps from the oils of underutilized tropical seed. Sust Chem Pharm. 2016;4:32–9. [Google Scholar]
- 8.Basyal S, Bachan M, Khan Z, Siegel R. 1096: Alcohol intoxication in a secured hospital unit. Crit Care Med. 2018;46(1):531. [Google Scholar]
- 9.Baum CR. Ethanol intoxication in children: epidemiology, estimation of toxicity, and toxic effects. [17 April 2017]. Available from: https://www.uptodate.com/contents/ethanolintoxication-in-children-epidemiology-estimation-of-toxicity-and-toxiceffects.
- 10.Bhoonderowa A, Gookool S, Biranjia-Hurdoyal SD. The importance of mobile phones in the possible transmission of bacterial infections in the community. J Commun Health. 2014;39:965–967. doi: 10.1007/s10900-014-9838-6. [DOI] [PubMed] [Google Scholar]
- 11.Blaney DD, Daly ER, Kirkland KB, Tongren JE, Kelso PT, Talbot EA. Use of alcohol-based hand sanitizers as a risk factor for norovirus outbreaks in long-term care facilities in northern New England: December 2006 to March 2007. Am J Infect Control. 2011;39:296–301. doi: 10.1016/j.ajic.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Block SS. Disinfection, sterilization, and preservation. soil science. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 13.Bondurant S, McKinney T, Bondurant L, Fitzpatrick L. Evaluation of a benzalkonium chloride hand sanitizer in reducing transient Staphylococcus aureus bacterial skin contamination in health care workers. Am J Infect Contr. 2019;47:1–5. doi: 10.1016/j.ajic.2019.08.030. [DOI] [PubMed] [Google Scholar]
- 14.Bondurant SW, Duley CM, Harbell JW. Demonstrating the persistent antibacterial efficacy of a hand sanitizer containing benzalkonium chloride on human skin at 1, 2, and 4 hours after application. Am J Infect Contr. 2019;47:928–32. doi: 10.1016/j.ajic.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Bonner L. CDC report calls attention to hand sanitizer risk in children. Pharm Today. 2017;23(5):34. [Google Scholar]
- 16.Bridier A, Briandet R, Thomas V, Dubois-Brissonnet F. Resistance of bacterial biofilms to disinfectants: a review. Biofouling. 2011;27:1017–1032. doi: 10.1080/08927014.2011.626899. [DOI] [PubMed] [Google Scholar]
- 17.Cavage WM. Flammability test of alcohol-based hand sanitizer. Washington, DC: Federal Aviation Administration; 2010. Available from: https://www.fire.tc.faa.gov/pdf/TN10-19.pdf. [Google Scholar]
- 18.CDC, Centers for Disease Control and Prevention. Show Me the Science – When & how to use hand sanitizer in community settings. 2020. [19 April, 2020]. Available from: https://www.cdc.gov/handwashing/show-me-the-science-hand-sanitizer.html#one.
- 19.CDC, Centers for Disease Control and Prevention Healthcare providers. Clean hands count for healthcare providers. 2020. [15 April, 2020]. Available from: https://www.cdc.gov/handhygiene/providers/index.html.
- 20.Chan APL, Chan TYK. Methanol as an unlisted ingredient in supposedly alcohol-based hand rub can pose serious health risk. Int J Environ Res Public Health. 2018;15:1440. doi: 10.3390/ijerph15071440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan GCK, Chan JCM, Szeto CC, Chow KM. Mixed isopropanol-methanol intoxication following ingestion of alcohol-Based hand rub solution. Clin Nephrol. 2017;88:218–20. doi: 10.5414/CN109103. [DOI] [PubMed] [Google Scholar]
- 22.Choi JH, Lee SK, Gil YE, Ryu J, Jung-Choi K, Kim H, et al. Neurological complications resulting from non-oral occupational methanol poisoning. J Korean Med Sci. 2017;32:371–6. doi: 10.3346/jkms.2017.32.2.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clayton EM, Todd M, Dowd JB, Aiello AE. The impact of bisphenol A and triclosan on immune parameters in the U.S. population, NHANES 2003-2006. Environ Health Perspect. 2011;119:390–396. doi: 10.1289/ehp.1002883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conover DM, Gibson KE. Comparison of two plain soap types for removal of bacteria and viruses from hands with specific focus on food service environments. Food Contr. 2016;69:141–146. [Google Scholar]
- 25.Darracq M, Ghafouri N, Pesce A, Cantrell FL. Hand sanitizer intoxication following a crude extraction method. Am J Drug Alcohol Abuse. 2013;39:217–218. doi: 10.3109/00952990.2013.773335. [DOI] [PubMed] [Google Scholar]
- 26.Daughton CG, Ternes TA. Pharmaceuticals and personal care products in the environment: Agents of subtle change? Environ Health Perspect. 1999;107:907–38. doi: 10.1289/ehp.99107s6907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.FDA, Food and Drug Administration. Silver Spring, MD: FDA; 2016. [16th April, 2020]. 5 Things to know about Triclosan. Available from: https://www.fda.gov/consumers/consumer-updates/5-things-know-about-triclosan. [Google Scholar]
- 28.FDA, Food and Drug Administration. Silver Spring, MD: FDA; 2020. [16th April, 2020]. Policy for temporary compounding of certain alcohol-based hand sanitizer products during the public health emergency immediately in effect guidance for industry. Available from: https://www.fda.gov/media/136118/download. [Google Scholar]
- 29.FDA, Food and Drug Administration. Tentative final monograph for healthcare antiseptic drug products;proposed rule. Fed Reg. 1994;59:31441–31452. [Google Scholar]
- 30.Fendler EJ, Ali Y, Hammonda BS, Lyons MK, Kelley MB, Vowell NA. The impact of alcohol hand sanitizer use on infection rates in an extended care facility. Am J Infect Contr. 2002;30:226–233. doi: 10.1067/mic.2002.120129. [DOI] [PubMed] [Google Scholar]
- 31.Forrester M. Characteristics of hand sanitizer ingestions by adolescents reported to poison centers. Int J Adolesc Med Health. 2015;27(1):69–72. doi: 10.1515/ijamh-2014-0014. [DOI] [PubMed] [Google Scholar]
- 32.Fung HT, Lam KK, Wong OF, Lau B, Kam CW. Case of fatal hydroxychloroquine overdose. Hong Kong J Emerg Med. 2007;14(1):53–57. [Google Scholar]
- 33.Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. BioScience Trends. 2020;14(1):1047. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 34.Georgia Poison Center. Hand sanitizer. 2015. [19th April, 2020]. Available from: https://www.georgiapoisoncenter.org/poisons/in-the-news/alerts-recent-trends/hand-sanitizer/
- 35.Ghanem B, Haddadin RN, Control I. Multiple drug resistance and biocide resistance in Escherichia coli environmental isolates from hospital and household settings. J Antimicrob Resist. 2018;7:47. doi: 10.1186/s13756-018-0339-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Good MI, Shader RI. Lethality and behavioral side effects of chloroquine. J Clin Psychopharmacol. 1982;2:40–7. doi: 10.1097/00004714-198202000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Gormley NJ, Bronstein AC, Rasimas JJ, Pao M, Wratney AT, Sun J, et al. The rising incidence of intentional ingestion of ethanol-containing hand sanitizers. Crit Care Med. 2012;40:290–294. doi: 10.1097/CCM.0b013e31822f09c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grayson ML, Melvani S, Druce J, Barr IG, Ballard SA, Johnson PD, et al. Efficacy of soap and water and alcohol-based hand-rub preparations against live H1N1 influenza virus on the hands of human volunteers. Clin Infect Dis. 2009;48:285–291. doi: 10.1086/595845. [DOI] [PubMed] [Google Scholar]
- 39.Halden RU. On the need and speed of regulating triclosan and triclocarban in the United States. Environ Sci Technol. 2014;48:3603–11. doi: 10.1021/es500495p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hartatik P. Formulation of antiseptic gel preparation of essential lavender flower oil (Lavandula angustifolia Miller) with carbopol base and antibacterial activity against Staphylococcus aureus (Thesis) Surakarta: Faculty of Pharmacy, Universitas Muhammadiyah; 2014. [Google Scholar]
- 41.Hauser AR, Mecsas J, Moir DT. Beyond antibiotics: New therapeutic approaches for bacterial infections. Clin Infect Dis. 2016;63:89–95. doi: 10.1093/cid/ciw200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hayat A, Munnawar F. Antibacterial effectiveness of commercially available hand sanitizers. Int J Biol Biotech. 2016;13:427–431. [Google Scholar]
- 43.Henzi H. Chronic methanol poisoning with the clinical and pathologic-anatomical features of multiple sclerosis. Med Hypotheses. 1984;13:63–75. doi: 10.1016/0306-9877(84)90131-2. [DOI] [PubMed] [Google Scholar]
- 44.IARC, International Agency for Research on Cancer. Hexachlorophene - Summaries and evaluations. IPCS Inchem. 1998;20:241. Available from: http://www.inchem.org/documents/iarc/vol20/hexachlorophene.html. [Google Scholar]
- 45.Jones R, Schuhmann L, El-Mallakh R. A patient who prefers to imbibe ethanol-based hand sanitizer over traditional alcoholic beverages. Am J Addict. 2013;22:148–149. doi: 10.1111/j.1521-0391.2013.00309.x. [DOI] [PubMed] [Google Scholar]
- 46.Kim JS, Kuk E, Yu KN, Kim J, Park SJ, Lee HJ, et al. Antimicrobial effects of silver nanoparticles. Nanomedicine. 2007;3:137–47. doi: 10.1016/j.nano.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 47.Kõljalg S, Mändar R, Sõber T, Rööp T, Mändar R. High level bacterial contamination of secondary school students’ mobile phones. GERMS. 2017;7(2):73–77. doi: 10.18683/germs.2017.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kramer A, Below H, Bieber N, Kampf G, Toma CD, Huebner N, et al. Quantity of ethanol absorption after excessive hand disinfection using three commercially available hand rubs is minimal and below toxic levels for humans. BMC Infect Dis. 2007;7:117. doi: 10.1186/1471-2334-7-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kramer A, Rudolph P, Kampf G, Pittet D. Limited efficacy of alcohol-based hand gels. Lancet. 2002;359:1489–1490. doi: 10.1016/S0140-6736(02)08426-X. [DOI] [PubMed] [Google Scholar]
- 50.Kuenzli E, Jaeger VK, DeCrom S, Sydow V, Muigg V, Frei R, et al. Impact of alcohol-based hand-gel sanitizer and hand hygiene advice on travellers’ diarrhoea and colonization with extended-spectrum betalactamase-producing Enterobacteriaceae: A randomised, controlled trial. Travel Med Infect Dis. 2019;32:101475. doi: 10.1016/j.tmaid.2019.101475. [DOI] [PubMed] [Google Scholar]
- 51.Lachenmeier DW. Safety evaluation of topical applications of ethanol on the skin and inside the oral cavity. J Occup Med Toxicol. 2008;3(1):26. doi: 10.1186/1745-6673-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lateh MS. Formulation of gel sanitizer handicraft preparation of ethanol acid gelugur fruit (Garcinia atroviridis Griff Et Anders) as antibacterial to Staphylococcus aureus (Thesis) Surakarta: Faculty of Pharmacy, Universitas Muhammadiyah; 2015. [Google Scholar]
- 53.Litovitz T. The alcohols: ethanol, methanol, isopropanol, ethylene glycol. Pediatr Clin North Am. 1986;33:311–323. doi: 10.1016/s0031-3955(16)35004-0. [DOI] [PubMed] [Google Scholar]
- 54.Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lu J, Jin M, Nguyen SH, Mao L, Li J, Coin LJ, et al. Non-antibiotic antimicrobial triclosan induces multiple antibiotic resistance through genetic mutation. Environ Int. 2018;118:257–65. doi: 10.1016/j.envint.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 56.Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, et al. The effect of handwashing on child health: a randomized controlled trial. Lancet. 2005;366:225–233. doi: 10.1016/S0140-6736(05)66912-7. [DOI] [PubMed] [Google Scholar]
- 57.Luby SP, Agboatwalla M, Painter J, Altaf A, Billhimer WL, Hoekstra RM. Effect of intensive handwashing promotion on childhood diarrhea in high-risk communities in Pakistan: a randomized controlled trial. JAMA. 2004;291:2547–2554. doi: 10.1001/jama.291.21.2547. [DOI] [PubMed] [Google Scholar]
- 58.Lygina O, Lyubchik A, Neng N, Sharipova A, Issakhov M, Nogueira J, et al. Review of current situation with triclosan’s harmful disinfection by-products pathways into environme. Sci Israel Technol Adv. 2013;15:49–64. [Google Scholar]
- 59.Marek E, Kraft WK. Ethanol pharmacokinetics in neonates and infants. Curr Ther Res Clin Exp. 2014;76:90–7. doi: 10.1016/j.curtheres.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marmor MF, Kellner U, Lai TYY, Melles RB, Mieler WF. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy. Ophthalmology. 2016;123:1386–94. doi: 10.1016/j.ophtha.2016.01.058. [DOI] [PubMed] [Google Scholar]
- 61.Mehta AK, Halvosa JS, Gould CV, Steinberg JP. Efficacy of alcohol-based hand rubs in the disinfection of stethoscopes. Infect Contr Hosp Epidemiol. 2010;31:870–2. doi: 10.1086/655437. [DOI] [PubMed] [Google Scholar]
- 62.Mi D, Ou X, Li P, Peng G, Liu Y, Guo R, et al. Glycine 29 is critical for conformational changes of spike glycoprotein of MHV-A59 triggered by either receptor binding or high pH. J Virol. 2019;93(20):e01046–e01019. doi: 10.1128/JVI.01046-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moore DJE. Intoxication by hand sanitizer. J Emerg Nurs. 2019;45:218–219. doi: 10.1016/j.jen.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 64.Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd annual report. Clin Toxicol. 2015;53:962–1146. doi: 10.3109/15563650.2015.1102927. [DOI] [PubMed] [Google Scholar]
- 65.Napolitani M, Bezzini D, Moirano F, Bedogni C, Messina G. Methods of disinfecting stethoscopes: Systematic review. Int J Environ Res Public Health. 2020;17(6):1856. doi: 10.3390/ijerph17061856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ningsih DR, Zusfahair Z, Kartika D, Fatoni A. Formulation of handsanitizer with antibacterials substance from n-hexane extract of soursop leaves (Annona muricata Linn) MJFAS (Malaysian Journal of Fundamental and Applied Sciences) 2017;13:1–5. [Google Scholar]
- 67.NPIRS. National Pesticide Information Retrieval System. [Triclosan;Ethanol.] (NPIRS) 2020. [17 April 2020]. Available from: http://npirspublic.ceris.purdue.edu/ppis/chemical.aspx.
- 68.Oughton MT, Loo VG, Dendukuri N, Fenn S, Libman MD. Hand hygiene with soap and water is superior to alcohol rub and antiseptic wipes for removal of Clostridium difficile. Infect Contr Hosp Epidemiol. 2009;30:939–944. doi: 10.1086/605322. [DOI] [PubMed] [Google Scholar]
- 69.Perez LG, Ramanantsoa C, Beaudron A, Delchet CH, Penn P, Comacle P. Efficacy of an ethanol-based hand sanitizer for the disinfection of blood pressure cuffs. Int J Environ Res Public Health. 2019;16:4342. doi: 10.3390/ijerph16224342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pidot SJ, Gao W, Buultjens AH, Monk IR, Guerillot R, Carter GP, et al. Increasing tolerance of hospital Enterococcus faecium to handwash alcohols. Sci Transl Med. 2018;10:452. doi: 10.1126/scitranslmed.aar6115. [DOI] [PubMed] [Google Scholar]
- 71.Qiao JS, Guo LM. Six cases of methanol poisoning caused by skin absorption. J Henan Med Univ. 1992;27:186–7. [Google Scholar]
- 72.Rai H, Knighton S, Zabarsky TF. Comparison of ethanol hand sanitizer versus moist towelette packets for mealtime patient hand hygiene. Am J Infect Contr. 2017;45:1033–1034. doi: 10.1016/j.ajic.2017.03.018. [DOI] [PubMed] [Google Scholar]
- 73.Raoult D, Rolain J, Colson P. Chloroquine for the 2019 novel coronavirus SARS-CoV-2. Int J Antimicrob Agents. 2020;55:1–2. doi: 10.1016/j.ijantimicag.2020.105923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rayar P, Ratnapalan S. Pediatric ingestions of house hold products containing ethanol: A review. Clin Pediatr (Phila) 2013;52:203–209. doi: 10.1177/0009922812470970. [DOI] [PubMed] [Google Scholar]
- 75.Raza M, Patel A, Schleifer S, Eljarrah F. Access to alcohol in hand sanitizer in a substance abuse treatment program: A potentially overlooked risk. J Addict Med. 2014;8:216–217. doi: 10.1097/ADM.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 76.Rüther K, Foerster J, Berndt S, Schroeter J. Chloroquine/hydroxychloroquine: Variability of retinotoxic cumulative doses. Ophthalmologe. 2007;104:875–9. doi: 10.1007/s00347-007-1560-7. [DOI] [PubMed] [Google Scholar]
- 77.Ryu J, Lim KH, Ryu DR, Lee HW, Yun JY, Kim SW, et al. Two cases of methyl alcohol intoxication by subchronic inhalation and dermal exposure during aluminum CNC cutting in a small-sized subcontracted factory. Ann Occup Environ Med. 2016;28:65. doi: 10.1186/s40557-016-0153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sahraei Z, Shabani M, Shokouhi S, Saffaei A. Aminoquinolines against coronavirus disease 2019 (COVID-19): Chloroquine or hydroxychloroquine. Int J Antimicrob Agents. 2020;55(4):105945. doi: 10.1016/j.ijantimicag.2020.105945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Santos C, Kieszak S, Wang A, Law R, Schier J, Wolkin A. Reported adverse health effects in children from ingestion of alcohol-based hand sanitizers – United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2017;66(8):223–226. doi: 10.15585/mmwr.mm6608a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sethuraman S, Kumar TR, Vivekananthan T. Effect of triclosan on histopathological changes in the hepatopancreas of zebra fish Brachydanio rerio hamilton-buchman. Asian J Biochem Pharmacol Res. 2014;4:2231–560. [Google Scholar]
- 81.Silva ARR, Cardoso DN, Cruz A, Lourenço J, Mendo S, Soares AMV, et al. Ecotoxicity and genotoxicity of a binary combination of triclosan and carbendazim to Daphnia magna. Ecotoxicol Environ Saf. 2015;115:279–90. doi: 10.1016/j.ecoenv.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 82.Singh AK, Singh A, Shaikh A, Singh R, Misra A. Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: A systematic search and a narrative review with a special reference to India and other developing countries. Diabetes Metab Syndr. 2020;14:241–246. doi: 10.1016/j.dsx.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stasinakis AS, Mamais D, Thomaidis NS, Danika E, Gatidou G, Lekkas TD. Inhibitory effect of triclosan and nonylphenol on respiration rates and ammonia removal in activated sludge systems. Ecotoxicol Environ Saf. 2008;70:199–206. doi: 10.1016/j.ecoenv.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 84.Stoker TE, Gibson EK, Zorrilla LM. Triclosan exposure modulates estrogen-dependent responses in the female wistar rat. Toxicol Sci. 2010;117:45–53. doi: 10.1093/toxsci/kfq180. [DOI] [PubMed] [Google Scholar]
- 85.Sturman LS, Ricard CS, Holmes KV. Conformational change of the coronavirus peplomer glycoprotein at pH 8.0 and 37°C correlates with virus aggregation and virus-induced cell fusion. J Virol. 1990;64:3042–3050. doi: 10.1128/jvi.64.6.3042-3050.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Surini S, Amirtha NI, Lestari DC. Formulation and effectiveness of a hand sanitizer gel produced using Salam bark extract. Int J Appl Pharm. 2018;10:216–220. [Google Scholar]
- 87.Thaddeus N, Francis E, Jane O, Obumneme A, Okechukwu E. Effects of some common additives on the antimicrobial activities of alcohol-based hand sanitizers. Asian Pac J Trop Med. 2018;11:222–226. [Google Scholar]
- 88.Thompson A, Griffin P, Stuetz R, Cartmell E. The fate and removal of triclosan during wastewater treatment. Water Environ Res. 2005;77:63–7. doi: 10.2175/106143005x41636. [DOI] [PubMed] [Google Scholar]
- 89.Tran MN, Wu AH, Hill DW. Alcohol dehydrogenase and catalase content in perinatal infant and adult livers: potential influence on neonatal alcohol metabolism. Toxicol Lett. 2007;169:245–252. doi: 10.1016/j.toxlet.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 90.Tran TH, Huyen TTT, Pham HQ, Vu-Quang H, Nguyen TD, Van-Thinh P, et al. Production process of hand sanitizer from Vietnamese coconut oil. Asian J Chem. 2019;31:1200–1206. [Google Scholar]
- 91.Tsang AC, Ahmadi S, Hamilton J, Gao J, Virgili G, Coupland SG, et al. The diagnostic utility of multifocal electroretinography in detecting chloroquine and hydroxychloroquine retinal toxicity. Am J Ophthalmol. 2019;206:132–139. doi: 10.1016/j.ajo.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 92.USGS, United States Geological Survey. Contaminants of emerging concern in the environment. [19 April, 2020]. Available from: http://toxics.usgs.gov/investigations/cec/index.php.
- 93.Wang AF, Xu R, Zheng F, Liu H. Effects of triclosan on acute toxicity, genetic toxicity and oxidative stress in goldfish Carassius auratus. Exp Anim. 2018;67:219–27. doi: 10.1538/expanim.17-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Westgate R, Grasha P, Maillard J. Use of a predictive protocol to measure the antimicrobial resistance risks associated with biocidal product usage. Am J Infect Contr. 2016;44:458–64. doi: 10.1016/j.ajic.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 95.WHO, World Health Organisation. Geneva: WHO Press; 2020. [19 April 2020]. Alcohol-based handrub risks/hazards. Available from: https://www.who.int/gpsc/tools/faqs/abhr2/en/ [Google Scholar]
- 96.WHO, World Health Organisation. Geneva: WHO Press; 2019. [17 April 2020]. New report calls for urgent action to avert antimicrobial resistance crisis. Available from: https://www.who.int/news-room/detail/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis. [Google Scholar]
- 97.WHO, World Health Organization. Geneva: WHO Press; 2010. [22 April 2020]. Guide to local production: WHO-recommended handrub formulations, Revised April, 2010. Available from: https://www.who.int/gpsc/5may/Guide_to_Local_Production.pdf. [Google Scholar]
- 98.WHO, World Health Organization. WHO guidelines on hand hygiene in health care. First global patient safety challenge clean care is safer care. Geneva: WHO Press; 2009. [PubMed] [Google Scholar]
- 99.Wolf J, Hunter PR, Freeman MC, Cumming O, Clasen T, Bartram J, et al. Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: updated meta-analysis and meta-regression. Trop Med Int Health. 2018;23:508–25. doi: 10.1111/tmi.13051. [DOI] [PubMed] [Google Scholar]
- 100.Wolfe MK, Gallandat K, Daniels K, Desmarais AM, Scheinman P, Lantagne D. Handwashing and Ebola virus disease outbreaks: A randomized comparison of soap, hand sanitizer, and 0.05% chlorine solutions on the inactivation and removal of model organisms Phi6 and E. coli from hands and persistence in rinse water. PLoS ONE. 2017;12(2):e0172734. doi: 10.1371/journal.pone.0172734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wong O, Chan Y, Lam S, Fung H, Ho J. Clinical experience in the use of intravenous lipid emulsion in hydroychloroquine and chloroquine overdose with refractory shock. Hong Kong J Emerg Med. 2011;18:243–8. [Google Scholar]
- 102.Worldometers records. COVID-19 Coronavirus pandemic. 2020. [24 April, 2020]. Available from: https://www.worldometers.info/coronavirus/
- 103.Zubair MF, Atolani O, Ibrahim SO, Oguntoye OS, Abdulrahim HA, Oyegoke RA, et al. Chemical and biological evaluations of potent antiseptic cosmetic products obtained from Momordica charantia seed oil. Sust Chem Pharm. 2018;9:35–41. [Google Scholar]
- 104.Zubair MF, Atolani O, Ibrahim SO, Oguntoye OS, Oyegoke RA, Olatunji GA. Fatty acids composition, antimicrobial potential and cosmeceutical utilization of Prosopis africana seed oil. J Mex Chem Soc. 2018;62(3):39–50. [Google Scholar]