Abstract
Studies show that vertebral fractures could predict the risk of hip fractures. We aimed to evaluate the potential benefits of whether the timing of vertebroplasty (VP) for vertebral fracture associated with the risk of hip fracture for hip replacement.
We identified 142,782 patients from the Taiwan National Health Insurance Database with thoracolumbar vertebral fracture (International Classification of Diseases, Ninth Revision, Clinical Modification:805.2–805.9) who were followed up from 2000 to 2013. These patients were divided into those who underwent VP (VP group) (International Classification of Diseases, Ninth Revision, Clinical Modification : 78.49) within 3 months and those who did not (non-VP group). After adjusting for the confounding factors, the Cox proportional hazards analysis was used to estimate the effect of early VP on reducing the risk of hip fracture. The difference in the risk of hip replacement, between the VP group and non-VP group was estimated using the Kaplan-Meier method with the log-rank test.
In the 14-year follow-up, the cumulative incidence rate of hip replacement in the VP group was lower than that in the non-VP group (0.362% and 0.533%, respectively, long-rank P < .001). There was a significant difference between the 2 groups since the first-year follow-up.
Our study showed that early VP performed to avoid progression of the kyphotic changes following thoracolumbar vertebral fracture may reduce the risk of hip fracture. These results, obtained from retrospective data, indicate that a prospective study is warranted.
Keywords: compression fracture, fall, hip fracture, pelvic incidence, sarcopenia, vertebroplasty
1. Introduction
Vertebral compression fractures and hip fractures are prevalent in the elderly population. Vertebral deformity could lead to complications of the respiratory and intra-abdominal organs and increase the risk of mortality. Further, hip fractures can decrease the quality of life and cause many morbidities. Vertebral compression fractures and hip fractures have high risk of mortality.[1–3] Taiwan, like other developed countries, is facing the challenge of an aging population. In 2011, 10.7% of the entire population was ≥ 65 years old; this figure is more than 14% in 2017.[4] Some authors concluded that a relationship between vertebral deformities and hip fracture that vertebral deformities have in prospective studies been reported as a risk factor for a future hip fracture.[5–8]
The objective of our study was to evaluate whether a relationship exists between hip fractures and the timing of restoration of vertebral deformities among population-based cohorts using the National Health Insurance Research Database at the National Health Research Institutes (NHIRD) in Taiwan. We hypothesized that early vertebroplasty (VP) performed to prevent the progression of kyphotic changes owing to thoracolumbar compression fracture (TLCF) would decrease the risk for a future hip fracture.
2. Methods
2.1. Data source
The National Health Insurance program in Taiwan is a compulsory single-payer program initiated in 1995, which covers nearly 99% of the 23.75 million residents of Taiwan. The NHIRD, contains all claims data of the beneficiaries and uses the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes to record diagnoses. We used the NHIRD strictly for research purposes. All data recorded in the database are double-encrypted to protect the confidentiality of the patients.
2.2. Study design
The study flow and patient characteristics with details of inclusion and exclusion criteria are shown in Figure 1. This retrospective population-based cohort study used NHIRD data collected between 2000 and 2013. The index date was defined as the first date in the database that indicated a diagnosis of TLCF (ICD-9-CM: 805.2–805.9). The exclusion criteria were as follows: a history of TLCF before the index date, a history of hip replacement (ICD-9-CM: 81.51, 51.52) before the index date, aged below 18 years, and unknown gender. These patients were divided into groups based on those who received VP (VP group) (ICD-9-CM: 78.49, repair of vertebral fracture) within 3 months and those who did not (non-VP group). Propensity score (PS) matching according to age, sex, and index date was performed on patients in the non-VP group randomly matched with those in the VP group (4 controls for each patient in the VP group) using the same exclusion criteria. At the end, the patients who underwent hip replacement (ICD-9-CM:81.51, 81.52) in both groups (VP and non-VP) were extracted. Using these criteria, 429 patients from the VP group and 2465 from the non-VP group who underwent hip replacement after TLCF were identified. Comorbidities in this study included diabetes mellitus (ICD-9-CM: 250), hypertension (ICD-9-CM: 401–405), depression (ICD-9-CM: 296.2–296.3, 296.82, 300.4, 311), renal disease (ICD-9-CM: 580–589), hyperlipidemia (ICD-9-CM: 580 - 589), pneumonia (ICD-9-CM: 480–486), injury (ICD-9-CM: 800–999, excluding 805.2–805.9), tumor (ICD-9-CM: 140–208), osteoporosis (ICD-9-CM: 733), ischemic heart disease (ICD-9-CM: 410–414), and stroke (ICD9-CM:430–438). We also examined the impact of the baseline sociodemographic characteristics, including age, sex, urbanization level, and Charlson comorbidity index score.
Figure 1.
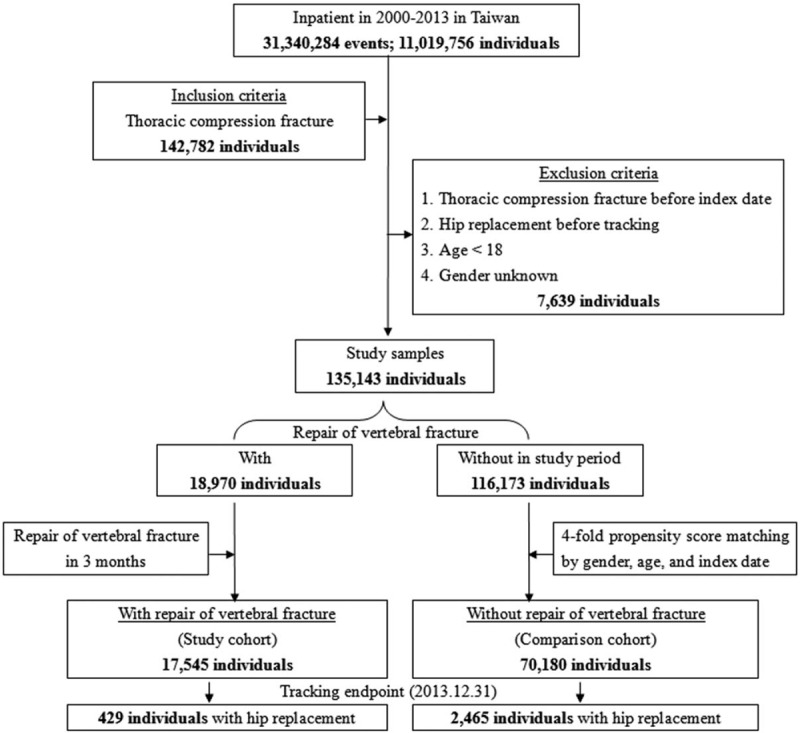
The flowchart of study sample selection from National Health Insurance Research Database in Taiwan.
2.3. Statistical analysis
Baseline distributions of the demographic characteristics and comorbidities were compared between the patients in the VP and non-VP groups using the χ2 test for categorical variables and the t-test for continuous variables. The incidence density of hip replacement (per 105 person-years) was calculated in both cohorts. Additionally, we calculated the incidence rate ratio of hip replacement for each variable. Univariate and multivariate Cox proportional hazards regression models were used to analyze the influence of early VP after TLCF (VP group) on the risk of hip replacement, which was expressed as a hazard ratio (HR) with a 95% confidence interval (CI), using non-VP patients as the reference. Multivariate models were controlled for a considerable range of independent variables: age, sex, diabetes mellitus (DM), hypertension (HTN), depression, renal disease, hyperlipidemia, pneumonia, injury, tumor, osteoporosis, ischemic heart disease (IHD), stroke, Charlson comorbidity index score, season, city location, urbanization, and level of care. After stratifying by age, sex, comorbidities, and follow-up time, the Cox models were used to compare the risk of hip replacement between the patients in the VP and non-VP groups. Cumulative incidence curves of the risk of hip replacement for the 2 cohorts were assessed using the Kaplan–Meier analysis. Differences between cohorts were evaluated using the log-rank test. All data were analyzed using the SAS statistical software (Version 9.3 for Windows). A 2-tailed P < .05 was considered significant.
2.4. Ethics statement
We employed the NHIRD-encrypted patient personal information system to protect patient privacy; therefore, patient consent was not required to access the NHIRD. This study was approved by the Institutional Review Board of the Tri-Service General Hospital. (TSGHIRB No. 2–105–05–082).
3. Results
During 2000–2013, 142,782 TLCF patients were enrolled in this study in accordance with our inclusion criteria; hip replacement was observed in 429 of 17,545 VP patients and in 2,465 of 70,180 non-VP patients (2.445% versus 3.512%, P < .001). The baseline demographic characteristics and comorbidities are as presented in Table 1. In both cohorts, approximately 67.22% patients were ≥65 years of age and 67.77% of the patients were women. The major coexisting diseases were HTN (20.51%) and DM (15.35%), injury (30.88%), and osteoporosis (20.65%).
Table 1.
Demographic characteristics and comorbidities in TLCF patients who did or did not receive VP in 3 mo.
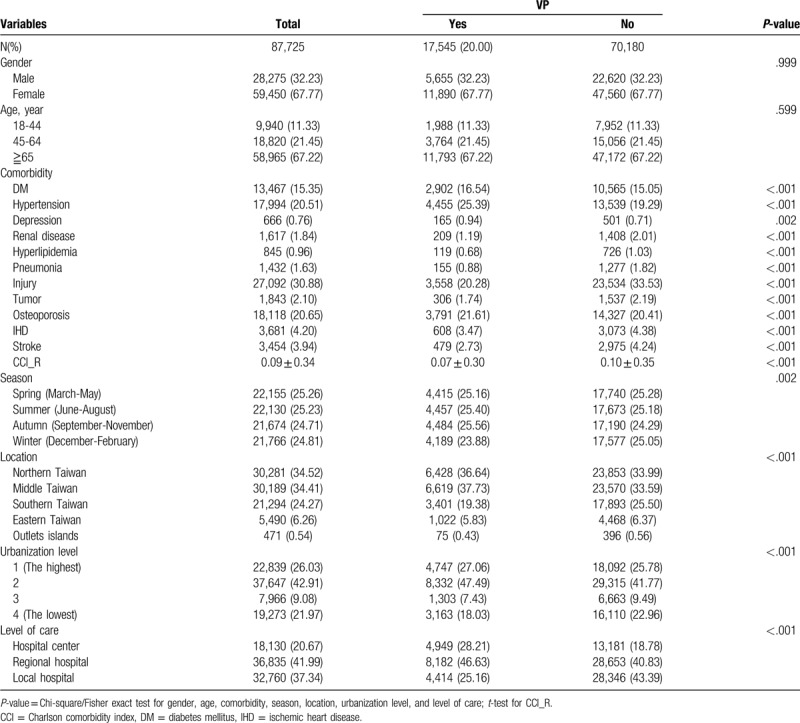
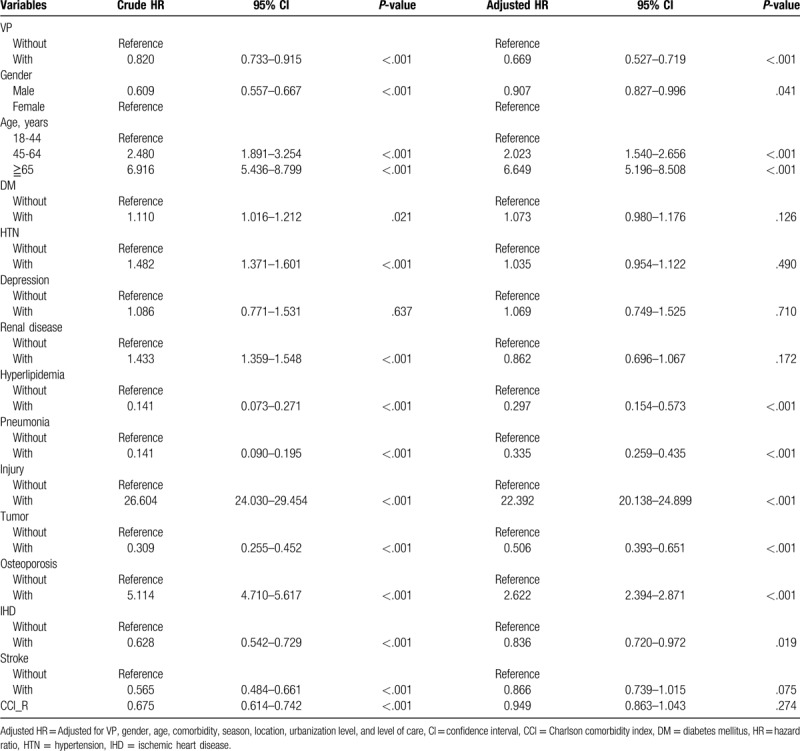
Table 2 describes the 14-year follow-up of the demographic characteristics and incidence of morbidity. The incidence of renal disease, pneumonia, injury, tumor, IHD, and stroke in the VP group was lower than that in the non-VP group (3.69% versus 5.92%, 7.73% versus 11.93%, 18.08% versus 24.21%, 7.06% versus 8.60%, 6.73% versus 7.71%, 5.66% versus 7.92%). After adjusting for the confounding factors, such as age, comorbidities, residence of urbanization and locations, seasons, level of care, and insured premiums, the risk of hip replacement in the VP group was lower than that in the non-VP group (adjusted HR, 0.669, 95% CI [0.527, 0.719], P < .001) (Table 3). Female sex (adjusted HR, 1.103, 95% CI, 1.004–1.209, P < .041), age ≥ 65 years (adjusted HR, 6.649, 95% CI, 5.196–8.508, P < .001), injury (adjusted HR, 22.392, 95% CI, 20.138–24.899, P < .001), and osteoporosis (adjusted HR, 2.262, 95% CI, 2.394–2.871, P < .001) with TLCF were associated with an increased risk of hip replacement.
Table 2.
Demographic characteristics and comorbidities in TLCF patients who did or did not receive VP in 3 mo after 14 yr follow-up.
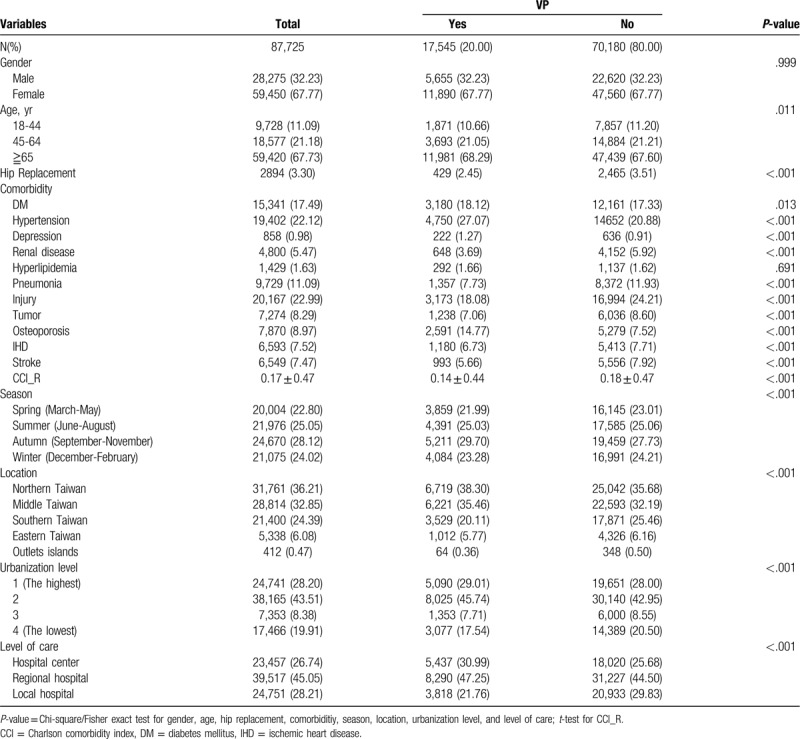
Table 3.
Risk of the hip replacement at the end of follow-up by using Cox regression.
In the stratified subgroup analysis, compared with the non-VP group, the risk reduction in the VP group was apparent in both males and females, all 3 age groups, with or without the following comorbidities: DM, HTN, depression, pneumonia, injury, osteoporosis, IHD, and stroke. Absence of renal disease, hyperlipidemia, and tumor in the VP group was associated with a significantly decreased risk of hip replacement. (Table 4). The mean duration of hip replacement was 3.40 ± 2.93 years in the VP group and 2.78 ± 2.55 years in the non-VP group (data not shown in the table). The Kaplan–Meier method was used to evaluate the cumulative incidence. The cumulative incidence rate of hip replacement in the VP group was lower than that in the non-VP group (0.362% and 0.533%, respectively, Long-rank P < .001) (Fig. 2). There was a significant difference between the 2 groups since the first-year follow-up.
Table 4.
Risk of the hip replacement at the end of follow-up stratified by using Cox regression.
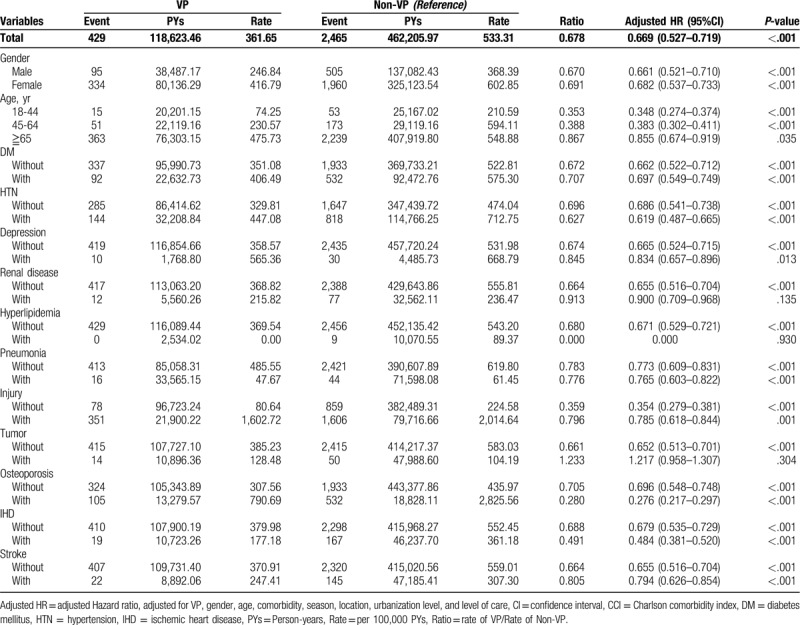
Figure 2.
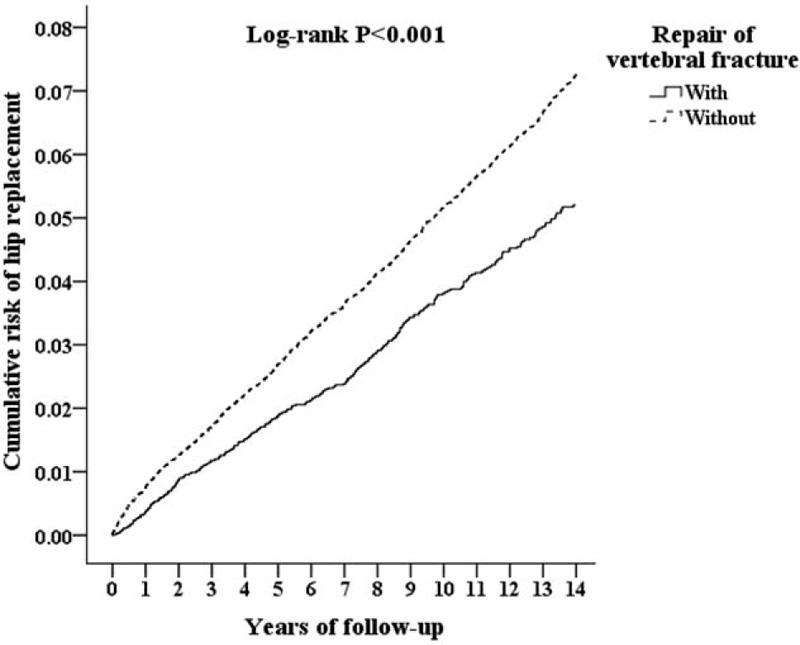
Kaplan-Meier for cumulative risk of hip replacement among aged 18 and over stratified by repair of vertebral fracture (VP) with log-rank test.
4. Discussion
This nationwide population-based retrospective study showed that the patient with thoracolumbar compression fracture (TLCF) who received VP within 3 months had a lower risk of hip replacement than had the patient with TLCF who did not receive VP within 3 months. To our knowledge, this is the first study to report on the association between the timing of VP intervention and the risk of hip replacement. Prospective studies have shown that vertebral deformities are a risk factor for a future hip fracture.[5–8] Our study indicates that early VP to prevent progression of the kyphotic change in TLCF may play an important role in decreasing hip joint degeneration and the hip fractures.
The concept of spinal alignment was developed by including the pelvis because spinal pathology, balance, and alignment are intertwined with the pelvis and lower extremities. The coordination among spinopelvic parameters is therefore of significant importance. A compensatory mechanism would trigger sagittal plane imbalance, such as hip extension, knee flexion, and an increase in pelvic incidence (PI) and pelvic tilt.[9] Further, it leads the pelvis to posteriorly rotate to preserve adequate sagittal balance, which results in an increased PI(Fig. 3). PI remains a key parameter in the sagittal spinal alignment and related deformities.[10,11]. Degenerative kyphosis and vertebral compression fracture are common in the elderly. TLCF causes kyphosis that moves the center of gravity forward and increases the load on the front column of the spine.[12] Subsequently, it results in a decrease in lumbar lordosis and the posterior tilt of the pelvis. This causes a deficiency in the anterior coverage of the acetabulum. However, the deficient coverage of anterior acetabulum applies more pressure on the femoral head, which leads to subchondral insufficiency fracture of the femoral head, necessitating hip replacement.[13–15] This posterior tilt of the pelvis results in decreased apparent femoral head coverage by creating a more articular surface of the acetabulum. Tsuchie et al. reported a case of non-traumatic anterior subluxation of bilateral femurs in a patient with severe compensatory posterior pelvic tilt. This anterior uncovering of the anterosuperior aspect of the femoral head by the acetabulum may create a dysplastic hip and could potentially be an etiological factor in the development of osteoarthritis of the hip, which is a potential risk factor of THR. VP performed after TLCF may not improve the kyphosis significantly, but it prevents the progression of kyphosis compared to the conservative treatment. This reduces the complications due to kyphosis.[16] Thus, TLCF causing sagittal plane imbalance could lead hip degeneration and may necessitate hip replacement.
Figure 3.
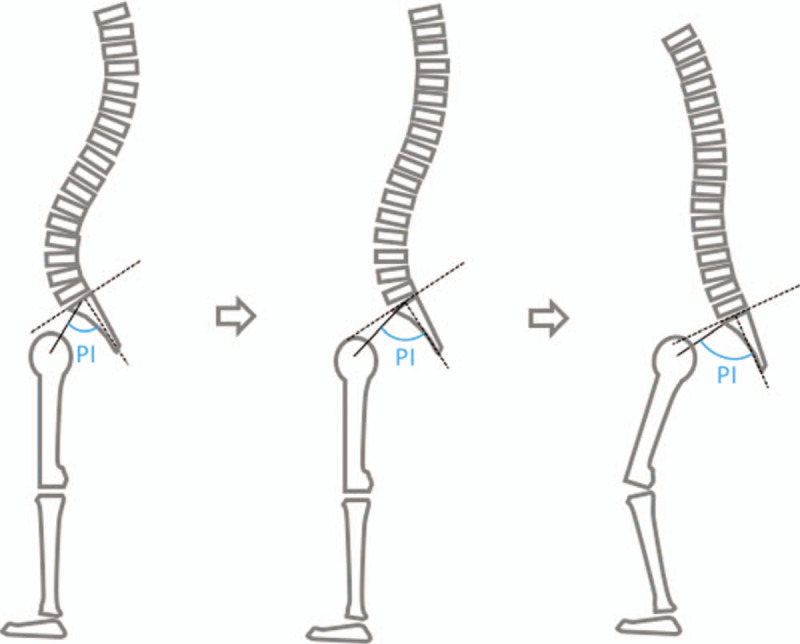
Increasing pelvis incidence with progressive kyphosis.
Patients with TLCF have gait patterns that significantly deviate from normal gait patterns after 6 months of conservative treatment, potentially increasing their risk of falls.[17] Furthermore, a good spinal sagittal alignment reduces the risk of falling, and positive sagittal balance is a radiographic parameter that is most highly correlated with adverse health outcomes.[18] Poor spinal sagittal alignment is related to body imbalance and altered vision field. When the body trunk bends forward, the direction of the vision line goes downward, impairing the ability to quickly grasp circumstances and possibly causing loss of balance, leading to falls.[19] Falls that result in fractures reduce the quality of life. Elderly people (aged 65 years and older) in USA and Japan fall approximately 30% and 20% each year, respectively.[20] Spinal deformity, which limits the activities of daily living and impairs the quality of life, is also considered an the important cause of falls. that a loss of lumbar lordosis, an increase in spinal inclination, and a postural imbalance were significantly higher in subjects with falls than in those without falls.[21] Similar to many previous studies, our report revealed that osteoporosis is a significant risk factor for TLCF. Additionally, osteoporotic hip fractures typically occur in the elderly population and result from low energy trauma injuries such as a fall from standing. Thus, early VP may restore the spinal alignment to avoid progression to spinal deformity, thereby reducing the risk of fall that may cause hip fractures.
Although osteoporosis is prevalent in subjects with vertebral fracture and hip fracture, sarcopenia is another key point. People with sarcopenia have a 3-fold increased risk for a fall[22] and patients with TLCF also often develop sarcopenia, which is a condition characterized by loss of skeletal muscle mass and strength, along with physical dysfunction and a risk of death. Takahashi, K., et al reported that patients with TLCF have significantly decreased muscle mass, and the prevalence of sarcopenia in these patients is 22.7% to 43.7%, which is higher than the prevalence of other orthopedic disorders.[23] The prevalence of hip fracture is higher in the elderly people with reduced muscle mass index and sarcopenia. Many studies have observed the effect of sarcopenia on hip fracture. Sarcopenia usually affects older people because they consume lower concentrations of proteins owing to the catabolic condition of inflammatory diseases that they develop and low appetite. The risk factor of muscle weakness associated with a hip fracture in elderly is determined by the decrease in total body muscle mass and the rate of muscle loss.[24] According to the study of the Asian Working Group for Sarcopenia, patients has described a prevalence of 73.6% in men and 67.7% in women with hip fracture in Hong Kong.[25] Studies have shown the important role of sarcopenia in the incidence of hip fractures among elderly people, even if osteoporosis is not observed. One of the main treatment strategy of sarcopenia is exercise activity with muscle resistance training. Hence, early VP reduces pain, improves mobility, and reduces the risk of fall, which may decrease the risk of sarcopenia-related hip fracture.
This study had several limitations. First, the etiology of TLCF may be osteoporosis, cancer, and trauma of infection. The health insurance data we utilized did not classify the etiology of TLCF in order to analyze them. Second, the surgical interventions of TLCF may be VP or kyphoplasty. Kyphoplasty may correct the local kyphotic angle more than VP did. However, the influence of the spinal sagittal alignment is controversial. Our study could not conclude the results of the different types of surgical interventions. And the last, although osteoporosis is a crucial risk factor for vertebral fracture and hip fracture, we do not discuss the correlation between the use of anti-osteoporotic medication and the risk of hip replacement. Further studies are required for this issue.
5. Conclusions
Vertebral compression fracture and hip fracture are major public health issues, with an increasing incidence owing to the increase in the elderly population. Hip fractures can lead to poor quality of life, and increased mobility and mortality, which increases medical and care costs. Thus, methods to prevent hip fracture are an important issue. In our population-based cohort study, we found that patients with TLCF who received VP within 3 months had a lower risk of hip replacement than those with TLCF who did not receive VP within 3 months. We concluded that early VP in patients with TLCF may reduce the risk of hip fracture.
Acknowledgments
The authors would like to thank the reviewers of this paper for the invaluable comments and their host institution for the opportunity to pursue this research.
Author contributions
L-CZ wrote the manuscript, contributed to discussion, edited whole paper; T-CT developed the hypothesis, contributed to discussion; C-HC analyzed data, contributed to discussion; L-CC contributed to discussion; O-CY contributed to discussion; C-CL contributed to discussion; C-NF contributed to discussion; C-TT contributed to discussion; H-DY contributed to discussion; M-HI contributed to discussion; L-MY contributed to discussion; C-YH developed the hypothesis, contributed to discussion, edited whole paper; C-WC developed the hypothesis, contributed to discussion, edited whole paper; J-DT developed the hypothesis, contributed to discussion, edited whole paper
Footnotes
Abbreviations: CI = confidence interval, DM = diabetes mellitus, HTN = hypertension, ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification, NHIRD = National Health Insurance Research Database, PI = pelvic incidence, TLCF = thoracolumbar compression fracture, VP = vertebroplasty.
How to cite this article: Li CZ, Li CC, Tang CT, Chung CH, Ou CY, Chen CL, Chen NF, Chung TT, Hueng DY, Ma HI, Liu MY, Chen YH, Chien WC, Ju DT. Association of early vertebroplasty with risk of hip replacement: a nationwide population-based cohort study in Taiwan. Medicine. 2020;99:27(e20926).
We employed the NHIRD-encrypted patient personal information system to protect patient privacy; therefore, patient consent was not required to access the NHIRD. This study was approved by the Institutional Review Board of the Tri-Service General Hospital. (TSGHIRB No. 2-105-05-082).
Consent for publication: Not applicable.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
This study was supported by the Tri-Service General Hospital Research Foundation (TSGH-B-109010), and the sponsor has no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
The data that support the findings of this study are available from a third party, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the third party.
References
- [1].Balkarli H, et al. Treatment of osteoporotic vertebral compression fractures with percutaneous vertebroplasty under local anesthesia: clinical and radiological results. Int J Clin Exp Med 2015;8:16287–93. [PMC free article] [PubMed] [Google Scholar]
- [2].Lin JH, et al. Early vertebroplasty associated with a lower risk of mortality and respiratory failure in aged patients with painful vertebral compression fractures: a population-based cohort study in Taiwan. Spine J 2017;17:1310–8. [DOI] [PubMed] [Google Scholar]
- [3].Pongchaiyakul C, et al. Asymptomatic vertebral deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective study. J Bone Miner Res 2005;20:1349–55. [DOI] [PubMed] [Google Scholar]
- [4].Lee TC, et al. One-year readmission risk and mortality after hip fracture surgery: a national population-based study in Taiwan. Aging Dis 2017;8:402–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hasserius R, et al. Hip fracture patients have more vertebral deformities than subjects in population-based studies. Bone 2003;32:180–4. [DOI] [PubMed] [Google Scholar]
- [6].Schousboe JT, et al. Association between prior non-spine non-hip fractures or prevalent radiographic vertebral deformities known to be at least 10 years old and incident hip fracture. J Bone Miner Res 2006;21:1557–64. [DOI] [PubMed] [Google Scholar]
- [7].Melton LJ, 3rd, et al. Vertebral fractures predict subsequent fractures. Osteoporos Int 1999;10:214–21. [DOI] [PubMed] [Google Scholar]
- [8].Black DM, et al. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of osteoporotic fractures research group. J Bone Miner Res 1999;14:821–8. [DOI] [PubMed] [Google Scholar]
- [9].Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 2010;19:1824–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Vrtovec T, et al. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J 2012;12:433–46. [DOI] [PubMed] [Google Scholar]
- [11].Fechtenbaum J, et al. Sagittal balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos Int 2016;27:559–67. [DOI] [PubMed] [Google Scholar]
- [12].Yokoyama K, et al. Postoperative change in sagittal balance after Kyphoplasty for the treatment of osteoporotic vertebral compression fracture. Eur Spine J 2015;24:744–9. [DOI] [PubMed] [Google Scholar]
- [13].Gebhart JJ, et al. Relationship between pelvic incidence and osteoarthritis of the hip. Bone Joint Res 2016;5:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yoshimoto H, et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 2005;30:1650–7. [DOI] [PubMed] [Google Scholar]
- [15].Jo WL, et al. Decreased lumbar lordosis and deficient acetabular coverage are risk factors for subchondral insufficiency fracture. J Korean Med Sci 2016;31:1650–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Balkarli H, et al. An evaluation of the functional and radiological results of percutaneous vertebroplasty versus conservative treatment for acute symptomatic osteoporotic spinal fractures. Injury 2016;47:865–71. [DOI] [PubMed] [Google Scholar]
- [17].Jacobs E, et al. Gait in patients with symptomatic osteoporotic vertebral compression fractures over 6 months of recovery. Aging Clin Exp Res 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lee BH, et al. Spinal sagittal balance status affects postoperative actual falls and quality of life after decompression and fusion in-situ surgery in patients with lumbar spinal stenosis. Clin Neurol Neurosurg 2016;148:52–9. [DOI] [PubMed] [Google Scholar]
- [19].Imagama S, et al. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J 2013;22:1346–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sakita M, et al. Falls and fall prevention in elderly people: summary of recent reviews. J of Health Promotion and Physical Therapy 2015;4:161–9. [Google Scholar]
- [21].Ishikawa Y, et al. Spinal sagittal contour affecting falls: cut-off value of the lumbar spine for falls. Gait Posture 2013;38:260–3. [DOI] [PubMed] [Google Scholar]
- [22].Hadjimichael AC. Hip fractures in the elderly without osteoporosis, Journal of Frailty. Sarcopenia and Falls 2018;03:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Takahashi K, et al. Correlation among sarcopenia, malnutrition and activities of daily living in patients with vertebral compression fractures: a comparison based on admission and discharge parameters evaluating these conditions. J Phys Ther Sci 2018;30:1401–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chen LK, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 2014;15:95–101. [DOI] [PubMed] [Google Scholar]
- [25].Ho AW, et al. Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric patients with hip fracture and its correlation with different factors. Hong Kong Med J 2016;22:23–9. [DOI] [PubMed] [Google Scholar]


