Abstract
Within the past several decades, the emergence of new viral diseases with severe health complications and mortality is evidence of an age-dependent, compromised bodily response to abrupt stress with concomitantly reduced immunity. The new severe acute respiratory syndrome coronavirus 2, SARS-CoV-2, causes coronavirus disease 2019 (COVID-19). It has increased morbidity and mortality in persons with underlying chronic diseases and those with a compromised immune system regardless of age and in older adults who are more likely to have these conditions. While SARS-CoV-2 is highly virulent, there is variability in the severity of the disease and its complications in humans. Severe pneumonia, acute respiratory distress syndrome, lung fibrosis, cardiovascular events, acute kidney injury, stroke, hospitalization, and mortality have been reported that result from pathogen–host interactions. Hallmarks of aging, interacting with one another, have been proposed to influence health span in older adults, possibly via mechanisms regulating the immune system. Here, we review the potential roles of the hallmarks of aging, coupled with host–coronavirus interactions. Of these hallmarks, we focused on those that directly or indirectly interact with viral infections, including immunosenescence, inflammation and inflammasomes, adaptive immunosenescence, genomic instability, mitochondrial dysfunction, epigenetic alterations, telomere attrition, and impaired autophagy. These hallmarks likely contribute to the increased pathophysiological responses to SARS-CoV-2 among older adults and may play roles as an additive risk of accelerated biological aging even after recovery. We also briefly discuss the role of antiaging drug candidates that require paramount attention in COVID-19 research.
Keywords: COVID-19, Pandemic, Comorbidity, Aging, Hallmarks of aging, Antiaging
The recently emerged severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is distinguished phylogenetically from other coronaviruses (1), causing more severe upper respiratory tract infections, respiratory distress, and hospitalization. These symptoms often result in admissions to intensive care units, mechanical ventilation, as well as mortality (2,3), mainly in persons with compromised immune systems and/or comorbidities such as diabetes, hypertension, and cancer (4). Previous outbreaks of community-acquired pneumonia and severe respiratory disease from coronaviruses reported in 2003 and 2012 were caused by SARS-CoV-1 and the Middle East respiratory syndrome (MERS-CoV), respectively (5). The latest coronavirus disease 2019 (COVID-19) started in Wuhan, China (6), and with its high virulence capacity and fast transmissibility, primarily through aerosol droplets (7), rapidly spread around the world. COVID-19 can be asymptomatic or minimally symptomatic with or without fever, cough, shortness of breath, fatigue, and gastrointestinal symptoms. COVID-19 can progress to moderate or severe pneumonia, severe symptomatic acute respiratory distress syndrome, cardiovascular complications, kidney injury, stroke, and mortality (2,4,8,9). In laboratory examinations, most patients appeared to have “cytokine storm,” leukopenia, thrombocytopenia, and coagulopathy (2,10). Computed tomography depicted multifocal ground-glass opacities and subsegmental areas of consolidation and fibrosis—in some cases, even without overt clinical symptoms (11).
The silent spread of SARS-CoV-2 via asymptomatic cases likely increases transmission to all individuals, especially to older persons who are at higher risk for more severe complications (3) or abruptly develop stroke or cardiovascular incidents as the result of virus–host interactions. Therefore, understanding the variability in host responses to viral infection is likely to yield better clinical management among older adults (12,13).
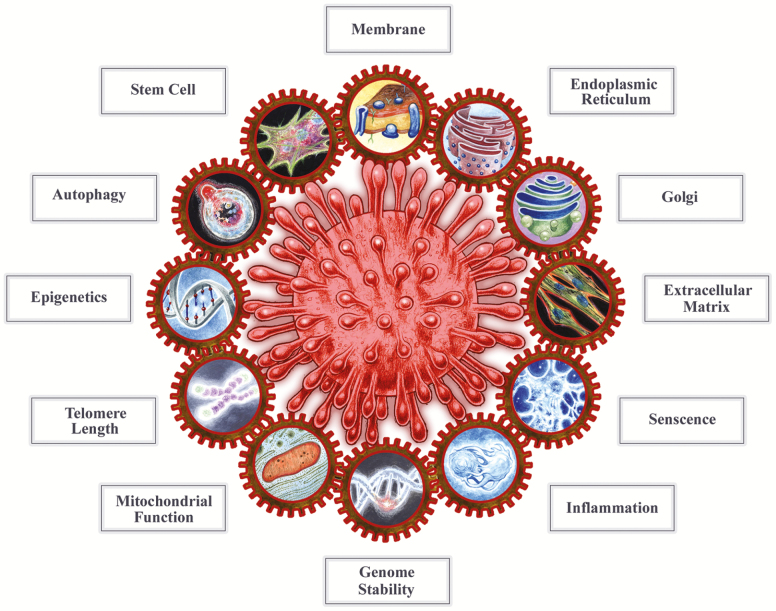
Normal aging includes changes at the cell, tissue, and organ levels (hallmarks of aging) that are known to contribute to morbidity, frailty, and mortality in the aging population. Hallmarks of aging, affecting one another, interfere with all aspects of cellular and system functions and play roles in chronic diseases (14–16) and interact directly or indirectly with the viral infection. Some of these hallmarks include immunosenescence, inflammation and inflammasomes, adaptive immunosenescence, genomic instability, mitochondrial dysfunction, epigenetic alterations, telomere attrition, and impaired autophagy that result in variability in reserve and adaptation capacity in response to stress. With the COVID-19 pandemic, consideration of these hallmarks when treating infected older patients may be critical to enhance positive outcomes (12,13). Here, we focus on some of the hallmarks of aging with regard to their potential roles in the host response to SARS-CoV-2 infection (Figure 1) and as possible underlying factors for poorer outcomes.
Figure 1.
The schematic figure implies the interaction between severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with the cell structures, clockwise including cell membrane, endoplasmic reticulum, Golgi, extracellular matrix, followed by hallmarks of aging such as senescence cells, inflammation, genome instability, mitochondrial function, telomere length, epigenetics, and stem cell exhaustion. The entire cell fitness is required to combat viral infection, and coronavirus engages cell systems.
SARS-CoV-2 Virology
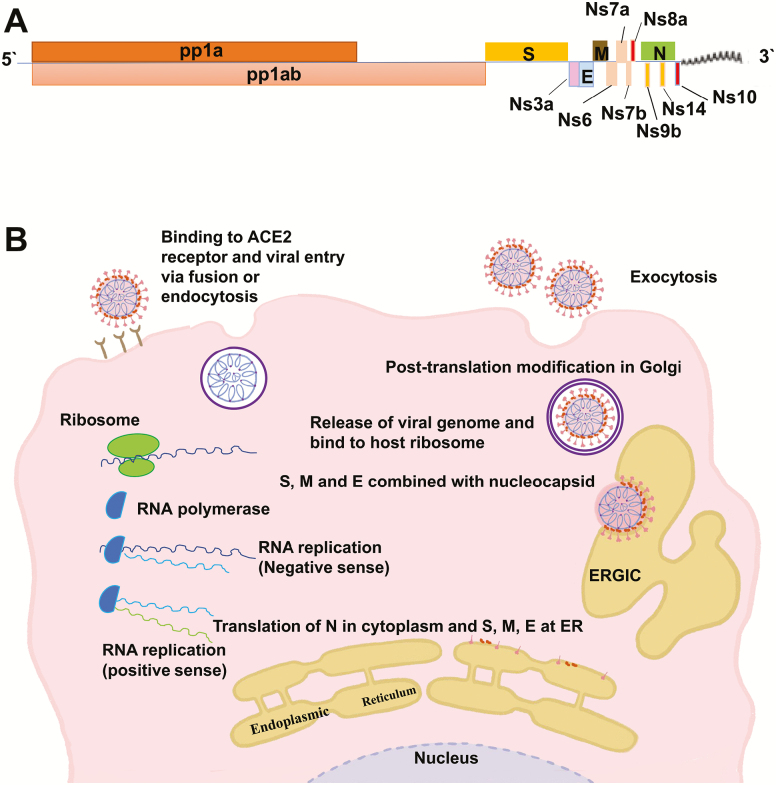
Classified within the Coronaviridae family, SARS-CoV-2 shares the main common characteristics of this family. Coronaviruses are enveloped with large (∼30-kb) single-stranded positive-sense RNA (17). Their genome is divided into two parts, 5′ two-thirds and 3′ one-third, with the former including open reading frames (ORF1a and ORF1b) that encode pp1a and pp1ab, two large polyproteins that can be cleaved to nonstructural proteins (nsp1–16) required for the synthesis of new viral genetic material. The rest of the genome includes genes that encode the structural proteins to produce virions and accessory genes that play a role in the host response (17).
Structural proteins include the spike (S) glycoprotein, known for its pathogenicity, that comprises two functional subunits: S1 as the receptor-binding domain and S2 that mediates fusion between the virus envelope and host cell membrane. Other coronavirus proteins include nucleocapsid (N), involved in genome replication; a membrane (M) protein from the host endoplasmic reticulum or Golgi responsible for virus assembly; and the envelope protein (E) (Figure 2A; Table 1). SARS-CoV-2 highly resembles SARS-CoV-1, sharing 77% similarity with the residual amino acids of the S protein (1). Also, the similarity of N, M, and 3a proteins in SARS-CoV-1 and SARS-CoV-2 implies a similar pathogenic pathway. SARS-CoV-2 binds to the angiotensin-converting enzyme 2 (ACE2), a cell surface receptor that converts the vasopressor octapeptide angiotensin-II to the vasodilator angiotensin 1-7 and is highly expressed in the vascular endothelia, lung, kidney, small intestine epithelial cells, immune cells, and testis (18,19). Following binding to ACE2, the virus enters the cell through either an endosome (in acidic environments) or by S glycoprotein cleavage with host cell proteases, such as TMPRSS2 and furin (20–22). Using their own RNA polymerase, coronaviruses replicate their genome in the host cell cytoplasm and employ the host ribosome machinery to produce proteins. Subsequent viral assembly occurs in the host endoplasmic reticulum–Golgi intermediate complex and mature virions are released through a secretory mechanism in smooth-walled vesicles, resulting in endoplasmic reticulum stress (Figure 2B).
Figure 2.
(a) Key SARS CoV-2 proteins implicated in COVID-19. The viral genome encodes 29 proteins among which at least 13 have been implicated in its virulence. (b) Coronavirus structure, cell entry, and replication. ACE2 = angiotensin-converting enzyme 2; ERGIC = endoplasmic reticulum–Golgi intermediate compartment; ER = endoplasmic reticulum.
Table 1.
COVID-19 Structural, Nonstructural, and Accessory Proteins
| Replication Phase | Host Factor | Virus Factor | Function |
|---|---|---|---|
| Binding and entry | ACE2 | Spike glycoprotein (S) | Cellular receptor |
| Viral transcription/replication, ribosome frameshift | Replicase polyprotein 1a (R1a) | ||
| Viral transcription/replication, ribosome frameshift | Replicase polyprotein 1ab (R1ab) | ||
| Protein 3a | Independent budding | Induction of apoptosis | |
| Protein 3b | Inhibition of type I interferons, induction of apoptosis | ||
| Envelope small membrane protein (E) | Independent budding | ||
| Membrane protein (M) | Virion morphogenesis | ||
| Nonstructural protein 6 (NS6) | Inhibition of type I interferons, alteration in cellular DNA synthesis | ||
| Nonstructural protein 7a (Ns7a) | Activate inflammation (MAPK-8) and NF-κB pathways | ||
| Ns7b | Unknown | ||
| Ns8a | Induction of apoptosis, alteration in cellular DNA synthesis | ||
| Nucleoprotein (N) | Viral genome packaging | ||
| Ns14 | Exonuclease and repair activity | ||
| Ns9b | Unknown | ||
| Ns10 | Unknown | ||
| IFITM (interferon-induced transmembrane) | Inhibits cell entry | ||
| TMPRSS2 (transmembrane protease serine 2) | Cleaves and activates S protein | ||
| Furin | Cleaves and activates S protein | ||
| Genome replication and transcription | GSK3 (glycogen synthase kinase 3) | Phosphorylates N protein and facilitates viral replication | |
| Translation of structural proteins | N-linked glycosylation enzymes in Golgi | Modifies S and M protein; N-linked glycosylation of the S protein facilitates lectin-mediated virion attachment and constitutes some neutralizing epitopes | |
| Endoplasmic reticulum chaperones | Proper folding and maturation of protein |
Note: ACE2 = angiotensin-converting enzyme 2; COVID-19 = coronavirus disease 2019.
Hallmarks of Aging and COVID-19
Innate Immunosenescence, Inflammation, and Inflammasomes
The human body uses pattern recognition receptors to identify pathogen-associated molecular patterns and endogenous danger (or damage)-associated molecular patterns. The most well-known pattern recognition receptors include the Toll-like receptors (TLRs), cytoplasmic retinoic acid-inducible gene I (RIG-I), the RIG-I-like receptor (RLR), and the nucleotide-binding oligomerization domain-like receptor (NLR). TLRs such as TLR7 are induced in response to recognized particles (23,24), including single-stranded RNA viruses, and stimulate proinflammatory cytokines and interferons (IFNs) type I and III (25). The latter, released from virus-infected cells, upregulates IFN-stimulated genes, which is a first step in limiting viral entry or viral replication (26). At later stages, IFNs can inhibit viral assembly, the viral spread, and modulate the immune system by promoting macrophage, natural killer (NK)-, T-, and B-cell activities (27). It has been suggested that coronavirus can antagonize IFNs and thereby evade the immune system (28).
RIG-I-like receptors, which reside on mitochondria, can detect RNA viruses and activate mitochondrial antiviral-signaling proteins. Mitochondrial antiviral-signaling proteins, in turn, increase proinflammatory cytokines including interleukin (IL)-6, tumor necrosis factor-α (TNF-α) that are related to nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, interferon regulatory factors, and inflammasome-related cytokines (IL-1β and IL-18) (23). Elevated inflammasome pathways in normal aging have been associated with age-related chronic diseases (29,30). By further stimulating inflammasome pathway activity, viral infections can exacerbate age-related impairment of immunological responses. With aging, the decline in innate immunity attenuates IFN responses to viral infection in neutrophils, monocytes and macrophages, and NK cells (24,27,31,32). Moreover, costimulatory signals are reduced from the antigen-presenting cells, including macrophages, B cells, NK, and dendritic cells that are required to activate T cells (32).
Coronaviruses have been shown to activate both the NLRP3 inflammasome and the NF-κB pathway (33,34). Of particular importance are elevated levels of TNF-α-converting enzyme (TACE), a proteolytic enzyme in the processing of TNF-α, TNF receptors (TNFRs), and ACE2. Both ACE2 and TACE levels are associated with poor prognosis in heart failure. In addition, TNFR-1 and TNFR-2 are strongly associated with kidney failure in older adults (35). ACE2 is an enzyme that promotes the formation of angiotensin 1-7, which has anti-inflammatory functions (36–38). However, ACE2 expression levels in human aging and ACE2 activity upon SARS-CoV-2 infection remain to be elucidated.
Moreover, in response to viral infections, plasminogen activator inhibitor-1 level increases to neutralize proteases such as TMPRSS2 and thus reduces the infectivity. Transforming growth factor-beta (TGF-beta) increases in response to persistent inflammation, and is known to trigger SERPINE1 expression, the gene encoding plasminogen activator inhibitor-1, which further increases TGF-beta levels (26). Of note, increased plasminogen activator inhibitor-1 level, a known marker of senescence (39), may increase thromboembolism and coagulopathy, which are risk factors for acute cardiovascular events and stroke (26). Similar to MESR-CoV, SARS-CoV-2 also has been reported to have a furin-like cleavage site (40). Furin, another host cell protease, stimulates both NLRP3 and NF-κB inflammatory pathways and activates TGF-beta (41). Notably, TGF-beta and growth differentiation factor 15, a member of TGF-beta superfamily, are known markers associated with aging (42) as well as significant prognostic markers in acute respiratory distress syndrome (43,44).
Adaptive Immunosenescence
Adaptive immunity that identifies and responds to specific pathogens includes humoral and cellular immunities, which are mediated by B cells, and CD8+ and CD4+ T cells, respectively. B lymphocytes are triggered to differentiate into immunoglobin-producing plasma cells by cytokine production from CD4+ cells (42). Increased levels of all immunoglobulins (Ig), including IgA from respiratory mucosal cells, IgM, and IgG, have been reported in response to coronavirus (23). IgM is the first antibody secreted in response to acute viral infection. IgG, produced later and enhanced upon reinfection, facilitates phagocytosis of infected cells and antibody-dependent cellular toxicity by both NK and CD8+ cells (45). With aging, there is a shift from the naïve toward memory B cells, alterations in the key stimulatory factors mediating the B-cell response to antigens, as well as reduced capacity for antigen recognition sites on antibodies to recognize novel pathogens. Moreover, in response to antiviral vaccines, long-lived plasma cells decrease (46).
With aging, in addition to the decreased number of naïve T cells, communication between T cells and antigen-presenting cells, which is required to convert naïve T cells to memory cells, is reduced (47).
Upon viral infection, the activated cytotoxic CD8+ cells release the lysing enzymes to degrade infected cells and viral genomes. If CD8+ cells fail to eliminate the virus, cytokines released from CD4+ T effector cells induce augmented inflammatory responses (48). Decreased numbers of naïve CD8+ T cells and reduced T-cell receptor diversity—as well as alterations in distribution and function of effector, memory, and regulatory CD8+ T cells—lead to impaired recognition of new antigens and accumulation of dysfunctional memory T cells (49–51). Of note, transcription factor FOXO3 that is expressed on T cells was shown to play an essential role in the regulation of T-cell functions in response to pathogens (52).
Notably, an age-dependent sex discrepancy in immune systems has been demonstrated (53), and the incidence of coronavirus infection has also been reported to be higher in men than women. With SARS-CoV-1, viral titers and the accumulation of inflammatory monocytes and neutrophils in the lungs were higher among men than women (54,55). A study of epigenomics and transcriptomics of immune cells has suggested a bimodal reduction in B-cell function in men, first in the early 30s and then at age 65 years and older (53). The sex- and age-dependent immune cell-specific epigenetic and transcriptomic discrepancy can also underlie the sex and age differences in severity of COVID-19 symptoms. Moreover, estrogen receptor signaling (56), variability in testosterone levels, and androgen receptor expression have been implicated in the variability of immune responses (57). Notably, androgen receptor element genes are upstream to the TMPRSS2 transcription start site and regulate its expression (58). While more rigorous epidemiological data on sex and age distribution of COVID-19 are warranted (59), more investigation on sex- and age-dependent immune response to RNA viral infections will shed more light on COVID-19 severity.
DNA Repair and Genomic Instability
The accumulation of somatic mutations, genomic instability, and attenuated DNA repair have been shown in aging immune cells. The overexpression of oxidative stress seen with a viral infection, along with attenuated DNA repair capacity, could accelerate genome instability and apoptosis in noninfected cells (60,61).
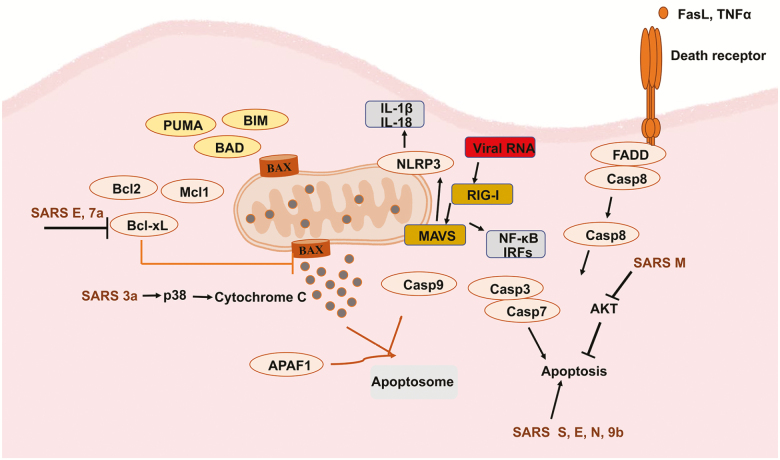
Among DNA repair mechanisms, p53 plays a vital role in response to low levels of stress and protects cells from oxidative damage. Conversely, higher levels of oxidative stress (eg, increased inflammatory responses secondary to viral infection) result in persistent activation of p53 and increased mitochondrial outer membrane permeability, which in turn leads to apoptosis (Figure 3) (62). Although p53 can downregulate coronavirus replication via regulation of the cell cycle (63), the coronavirus papain-like protease degrades p53 and allows replication of infected cells (64). Further, the DNA damage response can play a role in the pathogenesis of RNA viruses through induction of apoptosis, deleterious somatic mutations, and excessive stimulation of inflammatory immune responses (Figure 3) (65). Additionally, coronavirus can inhibit the activity of the cyclin-dependent protein complex, resulting in inactivation of the retinoblastoma protein, which is an important tumor suppressor protein and cell cycle check (66).
Figure 3.
Mitochondria, outer membrane permeability, and apoptosis pathways. Apoptosis induced by coronavirus infection, including intrinsic and extrinsic apoptosis. FasL = Fas ligand; TNF-α = tumor necrosis factor-alpha. Antiapoptotic factors: Bcl-xL = Bcl-2-like protein 1; Bcl2 = B-cell lymphoma 2; Mcl1 = myeloid cell leukemia 1. Proapoptotic factors: PUMA = p53-upregulated modulator of apoptosis; BAD = Bcl2-associated agonist of cell death; BAX = Bcl2-associated X; BIM = Bcl2-interacting mediator of cell death; APAF1 = apoptotic peptidase-activating factor 1; Casp = caspase; FADD = Fas-associated via death domain; AKT = RAC-alpha serine/threonine protein kinase; IL = interleukin; IRFs = interferon regulatory factors; MAVS = mitochondrial antiviral-signaling proteins; NF-κB = nuclear factor kappa-light-chain-enhancer of activated B cells; RIG-I = retinoic acid-inducible gene I; SARS = severe acute respiratory syndrome (70).
Of note, coronavirus accessory proteins such as the 7a protein also mediate apoptosis by interfering with Bcl-X (an antiapoptotic protein); additionally, coronavirus accessory proteins 3a and 9b, as well as structural proteins such as S, E, M, and N modulate apoptosis by inducing endoplasmic reticulum stress and activating the p38 MAPK pathway (Figure 3) (67,68).
Collectively, adverse cellular responses to DNA damage and diminished DNA repair capacity have been associated with genome instability and a decline in immune system function. This hallmark of aging not only is likely to be a risk for poor outcomes in older adults but also is likely to be amplified by coronavirus infection.
Mitochondrial Dysfunction
Mitochondria, through several functions, play pivotal roles in cell homeostasis. They play a powerhouse role with metabolic oxidation via the tricarboxylic acid cycle and the production of adenosine triphosphate via the electron transport chain and the beta-oxidation of fatty acids. With aging, mitochondrial phosphorylation capacity is decreased. Accordingly, the increased energy expenditure secondary to a cytokine storm can lead to a nonadaptive state, overwhelming the metabolic reserve capacity of mitochondria among older adults who have COVID-19. As a normal body function against pathogens, mitochondria also produce reactive oxygen species (ROS) (69). However, excessive ROS production can be damaging in a similar way to encountering coronavirus infection (70). Moreover, augmented ROS production, known as one of the contemporary theories of aging, has been associated with age-related diseases and decreased life span (71). Though diminished with aging, detoxifying systems including catalase, superoxide dismutase, glutathione peroxidase, and glutathione reductase with selenium and magnesium as their cofactors (72), vitamins E and C, and coenzyme Q10 all help minimize ROS-induced tissue damage (73). Supplementation with coenzyme Q10, an integral part of the mitochondrial respiratory chain, has been linked with antioxidant activity, less severe respiratory viral infections, and less severe inflammatory response (74).
As mentioned above, mitochondria regulate innate and adaptive immunity (eg, viral RNA activates mitochondrial antiviral-signaling proteins via RIG-I on mitochondria), which in turn stimulate NF-κB, NLRP3 pathways, and interferon regulatory factors. Mitochondria also mediate cytotoxic responses to lung cell stress (75,76).
Together, the combination of impaired respiration, diminished adenosine triphosphate production, increased ROS, and reduced detoxification capacity with dysregulated immune functions seems likely to play a pivotal role in the increased inflammation and severity of COVID-19.
Epigenetic Alterations
With aging, epigenomic alterations play a pivotal role in distinguishing immune cell phenotypes and regulating inflammatory responses to intrinsic or extrinsic stressors. Age is one of the main drivers of variations in chromatin structure measured by the assay for transposase-accessible chromatin with high-throughput sequencing (ATAC-seq) (53). Specific epigenetic modifications such as chromatin accessibility via histone acetylation/methylation play essential roles in response to viral infection (77–79). Shared epigenomic patterns of aging result in decreases in naïve T cells and increases in monocytes and cytotoxic cell functions. However, the magnitude of alterations is more significant in men than in women, with an accompanied loci-specific methylation decline in the B cells (53). As such, sex and age differences in epigenetic patterns of immune cells, in part, can explain variability in the severity of COVID-19.
Moreover, the epigenetic changes in CpG-sites located in subtelomeric regions that control innate immunity can mediate inflammatory responses to COVID-19. Chronic viral infection can accelerate aging as measured by the “epigenetic clock” (80). It remains to be elucidated whether these epigenetic clocks based on chronological or biological age (80,81) can predict the severity of COVID-19 and subsequent exacerbation of chronic diseases in COVID-19 survivors.
Telomere Attrition
Telomeres, which are repetitive nucleotides (TTAGGG)n at the ends of each chromosome, play a role in maintaining genome stability and regulate innate immunity in response to viral infection. Regions near telomeres called subtelomeres contain CG-enriched genes that regulate innate immunity (82). Influenced by telomere length, these genes regulate telomere repeat-containing RNA (TERRA) transcription, and their expression can be upregulated in response to viral infection via activation of interferon-stimulated genes. Therefore, diverse telomere lengths often observed with aging immune cells (83) can underlie differential responses to viral challenge (82). Another consequence of telomere attrition is the premature induction of genome instability in viral-specific CD8+ memory T cells that results in senescent or antiapoptotic cells (84). Thus, telomere attrition, coupled with dysregulated innate and adaptive immune responses to viral infection, is another hallmark of aging that can contribute to the severe outcomes in older adults with COVID-19.
Impaired Autophagy
The process of autophagy is modified by aging and thus can play a role in controlling viral infection through diminished viral degradation, as well as by dysregulating innate and adaptive immunity (85).
The autophagy process includes the functions of several protein complexes. In the absence of stress, the mTORC1/ULK1/2 complex inhibits the initiation of autophagy. Under stress, including viral infections, mTORC1 is inhibited, which subsequently activates a series of proteins that result in the induction of autophagy and virion encapsulation and degradation of viral particles (86).
Moreover, autophagy regulates the bridge between the innate and adaptive immune responses to viral infection by inducing antigen-presenting cells such as B cells, macrophages, and dendritic cells. Antigen-presenting cells, in turn, present viral antigens to CD4+ T cells to release cytokines and regulate adaptive immune responses. The early autophagic process induces the release of interferon-gamma (IFN-γ) from CD4+ T cells to promote CD8+ T cells, NK cells, and macrophages in response to viral infection (87). Moreover, the autophagic process controls the inflammatory response, preventing the accumulation of ROS and the inflammasome pathway via targeting pro-IL-1β for lysosomal degradation (88). While some viruses evade the direct autophagy-mediated function, immune-mediated effects of autophagy can still control viral infection and inflammatory-mediated tissue damage. Therefore, impaired autophagy, a hallmark of aging, possibly contributes to the severity of COVID-19 and poor outcomes in older patients. Niclosamide and valinomycin, two FDA-approved drugs for other purposes, enhance autophagy, and diminish viral replication (89). However, the antiviral effect of polyamines, such as spermidine, a bolster of autophagy, has been debated (90). Of note, rapamycin and its analogs, and also Vitamin D3, drugs with suggestive antiaging effects, have antiviral efficacy by increasing autophagy (91). Despite its immunosuppressive effects in transplant patients, rapamycin inhibition of mTORC1 improves immune function in older adults and increases the response to vaccines; some clinical trials using rapamycin have shown no serious side effects in humans (92–95). Therefore, rapamycin, by improving immunity, is expected to improve outcomes in older adults with COVID-19.
Interventions to Mitigate COVID-19 in Aging
Clinical manifestations of COVID-19 have indicated that host–virus interactions such as cytokine storm and coagulopathy, underlying comorbidities, and possibly polypharmacy are all possible culprits for the spectrum of COVID-19 severity. To combat both acute and chronic conditions related to COVID-19, enhancing response to the vaccine and antiviral therapies, using drugs that boost immune system response and enhance body system health is warranted. Older adults with an attenuated response to vaccine or antiviral medications might skew the pandemic figure toward epidemy in the older population. Therefore, some antiaging modalities possibly attenuate the severity of COVID-19 and increase response to vaccines when they become available. Thus, combating SARS-CoV-2 requires methods that go beyond direct targeting of the virus to include those approaches that support bodily system function via improving immunity, especially in older adults.
As such, interfering with pathways associated with the hallmarks of aging has the potential to improve the response to antiviral drugs (96). Potential drugs include agents that reduce mitochondrial ROS production and boost the immune system. Rapamycin has been shown to increase the immune response to the influenza vaccine and boost immune function in older adults (93,94). Metformin, an old antidiabetic drug and also a candidate antiaging modality, interferes with viral replication and host–viral interactions (97). Increasing Sirt6, an enzyme regulating multiple age-related signaling pathways, has been shown to reduce the immense inflammatory response to the fatal dengue virus infection (98). Some of the chloroquine-related family drugs, which are treatment candidates for prevention and treatment of COVID-19, also interfere with beta-galactosidase, a marker of senescence in cells (99). However, the efficacy and safety of chloroquine drugs in older adults require more data.
Although lists of drugs and vitamins have been suggested (100), at this writing, none of the ongoing clinical trials has considered recruiting older patients. Thus, the impact of all potential therapies and safety in older adults remains to be determined. We suggest an accelerated understanding of the interactions between COVID-19 and the host hallmarks of aging in order to identify biomarkers with which to screen individuals at higher risk. Understanding the mechanisms of COVID-19 will likely arise from comparing the disease risks and response to treatments in young men and women with COVID-19 versus older patients—to do this, we need to include older adults in clinical trials.
Conclusion
The COVID-19 outbreak is a worldwide public health problem with health consequences that are likely to persist for many years. Currently, older adults and patients with comorbidities and other unknown risk factors have developed more severe and critical complications, and therefore are at higher mortality risk. Both the incidence and severity of disease appear to be more prominent in men than women, which can be partially explained by both age-dependent and -independent sex dimorphism in the immune system. Coronaviruses use host factors for replication; these factors are affected by age and the same mechanisms as those linked with the hallmarks of aging. Some of the hallmarks of aging, coupled with immune system responses and comorbidities, seem likely to play a pivotal role in the severity of COVID-19. Innate immunity with cytokine storms, coagulopathy, neutralizing antibodies; cellular immune responses such as CD4+ and CD8+ T cells, B cells, NK cells, monocytes and macrophages, and inflammatory host responses; along with specific virus antigen epitopes—all have interactive roles in disease development. Diminished reserves and stress response capacity, coupled with the reduced immune response to vaccines, place older adults at higher risk for critical health complications and mortality, especially during times of acute stress. Together with antiviral interventions, the key hallmarks of aging can offer insights for the identification and treatment of patients most at risk and help elucidate the basis for age and sex differences in response to such stressors. Application of candidate antiaging drugs such as rapamycin and metformin, and antiviral drugs with potential senolytic effects possibly boost the immune system of older adults. Further investigation requires immediate attention. Such drugs can also prevent the possible post-COVID-19 accumulation of morbidities and accelerated biology of aging.
Acknowledgments
We thank Neda Hajmomeni for the art applied in Figures 2b and 3. S.S. performed a literature review, wrote, and edited the manuscript. J.M.H. performed a literature review, contributed to the writing, and edited the manuscript. We applaud all researchers and health care workers involved in the COVID-19 pandemic. The exclusion of related references reflects the limited number of references we could cite.
Funding
National Institute on Aging-Biology (grant/award number: K01AG059898).
Conflict of Interest
None reported.
References
- 1. Li C, Yang Y, Ren L. Genetic evolution analysis of 2019 novel coronavirus and coronavirus from other species. Infect Genet Evol. 2020;82:104285. doi: 10.1016/j.meegid.2020.104285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. J AMA. 2020;323:1545–1546. doi: 10.1001/jama.2020.4031 [DOI] [PubMed] [Google Scholar]
- 4. Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020. doi: 10.1111/all.14238 [DOI] [PubMed] [Google Scholar]
- 5. Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. 2019;16:69. doi: 10.1186/s12985-019-1182-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 7. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109: 531–538. doi: 10.1007/s00392-020-01626-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929 [DOI] [PubMed] [Google Scholar]
- 10. Yao Z, Zheng Z, Wu K, Junhua Z. Immune environment modulation in pneumonia patients caused by coronavirus: SARS-CoV, MERS-CoV and SARS-CoV-2. Aging (Albany NY). 2020;12:7639–7651. doi: 10.18632/aging.103101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Le Couteur DG, Anderson RM, Newman AB. COVID-19 is a disease of older people. J Gerontol A Biol Sci Med Sci. 2020.doi: 10.1093/gerona/glaa077 [DOI] [Google Scholar]
- 13. Promislow DEL. A geroscience perspective on COVID-19 mortality. J Gerontol A Biol Sci Med Sci. 2020. doi: 10.1093/gerona/glaa094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell. 2014;159:709–713. doi: 10.1016/j.cell.2014.10.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ferrucci L, Gonzalez-Freire M, Fabbri E, et al. Measuring biological aging in humans: a quest. Aging Cell. 2020;19:e13080. doi: 10.1111/acel.13080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Luk HKH, Li X, Fung J, Lau SKP, Woo PCY. Molecular epidemiology, evolution and phylogeny of SARS coronavirus. Infect Genet Evol. 2019;71:21–30. doi: 10.1016/j.meegid.2019.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444–1448. doi: 10.1126/science.abb2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Matsuyama S, Nagata N, Shirato K, Kawase M, Takeda M, Taguchi F. Efficient activation of the severe acute respiratory syndrome coronavirus spike protein by the transmembrane protease TMPRSS2. J Virol. 2010;84:12658–12664. doi: 10.1128/JVI.01542-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Iwata-Yoshikawa N, Okamura T, Shimizu Y, Hasegawa H, Takeda M, Nagata N. TMPRSS2 contributes to virus spread and immunopathology in the airways of murine models after coronavirus infection. J Virol. 2019;93:e01815–18. doi: 10.1128/JVI.01815-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e278. doi: 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li G, Fan Y, Lai Y, et al. Coronavirus infections and immune responses. J Med Virol. 2020;92:424–432. doi: 10.1002/jmv.25685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pillai PS, Molony RD, Martinod K, et al. Mx1 reveals innate pathways to antiviral resistance and lethal influenza disease. Science. 2016;352:463–466. doi: 10.1126/science.aaf3926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015 [DOI] [PubMed] [Google Scholar]
- 26. Dittmann M, Hoffmann HH, Scull MA, et al. A serpin shapes the extracellular environment to prevent influenza A virus maturation. Cell. 2015;160:631–643. doi: 10.1016/j.cell.2015.01.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kawai T, Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol. 2010;11:373–384. doi: 10.1038/ni.1863 [DOI] [PubMed] [Google Scholar]
- 28. Nelemans T, Kikkert M. Viral Innate immune evasion and the pathogenesis of emerging RNA virus infections. Viruses. 2019;11:961. doi: 10.3390/v11100961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Franceschi C, Bonafè M, Valensin S, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2000;908:244–254. doi: 10.1111/j.1749-6632.2000.tb06651.x [DOI] [PubMed] [Google Scholar]
- 30. Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15:505–522. doi: 10.1038/s41569-018-0064-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Molony RD, Malawista A, Montgomery RR. Reduced dynamic range of antiviral innate immune responses in aging. Exp Gerontol. 2018;107:130–135. doi: 10.1016/j.exger.2017.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mahbub S, Brubaker AL, Kovacs EJ. Aging of the innate immune system: an update. Curr Immunol Rev. 2011;7:104–115. doi: 10.2174/157339511794474181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477–489. doi: 10.1038/s41577-019-0165-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhao C, Zhao W. NLRP3 inflammasome-a key player in antiviral responses. Front Immunol. 2020;11:211. doi: 10.3389/fimmu.2020.00211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Salimi S, Shardell MD, Seliger SL, Bandinelli S, Guralnik JM, Ferrucci L. Inflammation and trajectory of renal function in community-dwelling older adults. J Am Geriatr Soc. 2018;66:804–811. doi: 10.1111/jgs.15268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ruiz-Ortega M, Lorenzo O, Suzuki Y, Rupérez M, Egido J. Proinflammatory actions of angiotensins. Curr Opin Nephrol Hypertens. 2001;10:321–329. doi: 10.1097/00041552-200105000-00005 [DOI] [PubMed] [Google Scholar]
- 37. Nikolich-Zugich J, Knox KS, Rios CT, Natt B, Bhattacharya D, Fain MJ. SARS-CoV-2 and COVID-19 in older adults: what we may expect regarding pathogenesis, immune responses, and outcomes. Geroscience. 2020;42:505–514. doi: 10.1007/s11357-020-00186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Koff WC, Williams MA. Covid-19 and immunity in aging populations—a new research agenda. N Engl J Med. 2020. doi: 10.1056/NEJMp2006761 [DOI] [PubMed] [Google Scholar]
- 39. Vaughan DE, Rai R, Khan SS, Eren M, Ghosh AK. Plasminogen activator inhibitor-1 is a marker and a mediator of senescence. Arterioscler Thromb Vasc Biol. 2017;37:1446–1452. doi: 10.1161/ATVBAHA.117.309451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Coutard B, Valle C, de Lamballerie X, Canard B, Seidah NG, Decroly E. The spike glycoprotein of the new coronavirus 2019-nCoV contains a furin-like cleavage site absent in CoV of the same clade. Antiviral Res. 2020;176:104742. doi: 10.1016/j.antiviral.2020.104742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dubois CM, Blanchette F, Laprise MH, Leduc R, Grondin F, Seidah NG. Evidence that furin is an authentic transforming growth factor-beta1-converting enzyme. Am J Pathol. 2001;158:305–316. doi: 10.1016/s0002-9440(10)63970-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nikolich-Žugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol. 2018;19:10–19. doi: 10.1038/s41590-017-0006-x [DOI] [PubMed] [Google Scholar]
- 43. Tanaka T, Biancotto A, Moaddel R, et al. ; CHI Consortium Plasma proteomic signature of age in healthy humans. Aging Cell. 2018;17:e12799. doi: 10.1111/acel.12799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Clark BJ, Bull TM, Benson AB, et al. ; ARDS Network Investigators Growth differentiation factor-15 and prognosis in acute respiratory distress syndrome: a retrospective cohort study. Crit Care. 2013;17:R92. doi: 10.1186/cc12737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sullivan JA, Kim EH, Plisch EH, Peng SL, Suresh M. FOXO3 regulates CD8 T cell memory by T cell-intrinsic mechanisms. PLoS Pathog. 2012;8:e1002533. doi: 10.1371/journal.ppat.1002533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Frasca D, Diaz A, Romero M, Blomberg BB. The generation of memory B cells is maintained, but the antibody response is not, in the elderly after repeated influenza immunizations. Vaccine. 2016;34:2834–2840. doi: 10.1016/j.vaccine.2016.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sprent J, Surh CD. Normal T cell homeostasis: the conversion of naive cells into memory-phenotype cells. Nat Immunol. 2011;12:478–484. doi: 10.1038/ni.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. van de Sandt CE, Barcena M, Koster AJ, et al. Human CD8(+) T cells damage noninfected epithelial cells during influenza virus infection in vitro. Am J Respir Cell Mol Biol. 2017;57:536–546.doi: 10.1165/rcmb.2016-0377OC [DOI] [PubMed] [Google Scholar]
- 49. Bektas A, Schurman SH, Sen R, Ferrucci L. Human T cell immunosenescence and inflammation in aging. J Leukoc Biol. 2017;102:977–988. doi: 10.1189/jlb.3RI0716-335R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Britanova OV, Putintseva EV, Shugay M, et al. Age-related decrease in TCR repertoire diversity measured with deep and normalized sequence profiling. J Immunol. 2014;192:2689–2698. doi: 10.4049/jimmunol.1302064 [DOI] [PubMed] [Google Scholar]
- 51. Pawelec G. Hallmarks of human “immunosenescence”: adaptation or dysregulation? Immun Ageing. 2012;9:15. doi: 10.1186/1742-4933-9-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Birkenkamp KU, Coffer PJ. FOXO transcription factors as regulators of immune homeostasis: molecules to die for? J Immunol. 2003;171:1623–1629. doi: 10.4049/jimmunol.171.4.1623 [DOI] [PubMed] [Google Scholar]
- 53. Márquez EJ, Chung CH, Marches R, et al. Sexual-dimorphism in human immune system aging. Nat Commun. 2020;11:751. doi: 10.1038/s41467-020-14396-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Karlberg J, Chong DS, Lai WY. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol. 2004;159:229–231. doi: 10.1093/aje/kwh056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Alghamdi IG, Hussain II, Almalki SS, Alghamdi MS, Alghamdi MM, El-Sheemy MA. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417–423. doi: 10.2147/IJGM.S67061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kadel S, Kovats S. Sex hormones regulate innate immune cells and promote sex differences in respiratory virus infection. Front Immunol. 2018;9:1653. doi: 10.3389/fimmu.2018.01653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Traish A, Bolanos J, Nair S, Saad F, Morgentaler A. Do androgens modulate the pathophysiological pathways of inflammation? Appraising the contemporary evidence. J Clin Med. 2018;7:549. doi: 10.3390/jcm7120549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Shen LW, Mao HJ, Wu YL, Tanaka Y, Zhang W. TMPRSS2: a potential target for treatment of influenza virus and coronavirus infections. Biochimie. 2017;142:1–10. doi: 10.1016/j.biochi.2017.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bhopal R. Covid-19 worldwide: we need precise data by age group and sex urgently. BMJ. 2020;369:m1366. doi: 10.1136/bmj.m1366 [DOI] [PubMed] [Google Scholar]
- 60. Vijg J, Dong X, Milholland B, Zhang L. Genome instability: a conserved mechanism of ageing? Essays Biochem. 2017;61:305–315. doi: 10.1042/EBC20160082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhang L, Dong X, Lee M, Maslov AY, Wang T, Vijg J. Single-cell whole-genome sequencing reveals the functional landscape of somatic mutations in B lymphocytes across the human lifespan. Proc Natl Acad Sci USA. 2019;116:9014–9019. doi: 10.1073/pnas.1902510116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Shibue T, Suzuki S, Okamoto H, et al. Differential contribution of Puma and Noxa in dual regulation of p53-mediated apoptotic pathways. EMBO J. 2006;25:4952–4962. doi: 10.1038/sj.emboj.7601359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ma-Lauer Y, Carbajo-Lozoya J, Hein MY, et al. p53 down-regulates SARS coronavirus replication and is targeted by the SARS-unique domain and PLpro via E3 ubiquitin ligase RCHY1. Proc Natl Acad Sci USA. 2016;113:E5192–E5201. doi: 10.1073/pnas.1603435113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Yuan L, Chen Z, Song S, et al. p53 degradation by a coronavirus papain-like protease suppresses type I interferon signaling. J Biol Chem. 2015;290:3172–3182. doi: 10.1074/jbc.M114.619890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ryan EL, Hollingworth R, Grand RJ. Activation of the DNA damage response by RNA viruses. Biomolecules. 2016;6:2. doi: 10.3390/biom6010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yuan X, Yao Z, Wu J, et al. G1 phase cell cycle arrest induced by SARS-CoV 3a protein via the cyclin D3/pRb pathway. Am J Respir Cell Mol Biol. 2007;37:9–19. doi: 10.1165/rcmb.2005-0345RC [DOI] [PubMed] [Google Scholar]
- 67. Tan YX, Tan TH, Lee MJ, et al. Induction of apoptosis by the severe acute respiratory syndrome coronavirus 7a protein is dependent on its interaction with the Bcl-XL protein. J Virol. 2007;81:6346–6355. doi: 10.1128/JVI.00090-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Liu DX, Fung TS, Chong KK, Shukla A, Hilgenfeld R. Accessory proteins of SARS-CoV and other coronaviruses. Antiviral Res. 2014;109:97–109. doi: 10.1016/j.antiviral.2014.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Breda CNS, Davanzo GG, Basso PJ, Saraiva Câmara NO, Moraes-Vieira PMM. Mitochondria as central hub of the immune system. Redox Biol. 2019;26:101255. doi: 10.1016/j.redox.2019.101255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Fung TS, Liu DX. Human coronavirus: host-pathogen interaction. Annu Rev Microbiol. 2019;73:529–557. doi: 10.1146/annurev-micro-020518-115759 [DOI] [PubMed] [Google Scholar]
- 71. Harman D. The free radical theory of aging. Antioxid Redox Signal. 2003;5:557–561. doi: 10.1089/152308603770310202 [DOI] [PubMed] [Google Scholar]
- 72. Espinoza SE, Guo H, Fedarko N, et al. Glutathione peroxidase enzyme activity in aging. J Gerontol A Biol Sci Med Sci. 2008;63:505–509. doi: 10.1093/gerona/63.5.505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Barcelos IP, Haas RH. CoQ10 and aging. Biology (Basel). 2019;8:28. doi: 10.3390/biology8020028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Chase M, Cocchi MN, Liu X, Andersen LW, Holmberg MJ, Donnino MW. Coenzyme Q10 in acute influenza. Influenza Other Respir Viruses. 2019;13:64–70. doi: 10.1111/irv.12608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Mills EL, Kelly B, O’Neill LAJ. Mitochondria are the powerhouses of immunity. Nat Immunol. 2017;18:488–498. doi: 10.1038/ni.3704 [DOI] [PubMed] [Google Scholar]
- 76. Schumacker PT, Gillespie MN, Nakahira K, et al. Mitochondria in lung biology and pathology: more than just a powerhouse. Am J Physiol Lung Cell Mol Physiol. 2014;306:L962–L974. doi: 10.1152/ajplung.00073.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Feser J, Tyler J. Chromatin structure as a mediator of aging. FEBS Lett. 2011;585:2041–2048. doi: 10.1016/j.febslet.2010.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Moskowitz DM, Zhang DW, Hu B, et al. Epigenomics of human CD8 T cell differentiation and aging. Sci Immunol. 2017;2:eaag0192. doi: 10.1126/sciimmunol.aag0192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ucar D, Márquez EJ, Chung CH, et al. The chromatin accessibility signature of human immune aging stems from CD8+ T cells. J Exp Med. 2017;214:3123–3144. doi: 10.1084/jem.20170416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Boulias K, Lieberman J, Greer EL. An epigenetic clock measures accelerated aging in treated HIV infection. Mol Cell. 2016;62:153–155. doi: 10.1016/j.molcel.2016.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Lu AT, Quach A, Wilson JG, et al. DNA methylation GrimAge strongly predicts lifespan and healthspan. Aging (Albany NY). 2019;11:303–327. doi: 10.18632/aging.101684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Wang Z, Deng Z, Tutton S, Lieberman PM. The telomeric response to viral infection. Viruses. 2017;9:218. doi: 10.3390/v9080218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Heidinger BJ, Blount JD, Boner W, Griffiths K, Metcalfe NB, Monaghan P. Telomere length in early life predicts lifespan. Proc Natl Acad Sci USA. 2012;109:1743–1748. doi: 10.1073/pnas.1113306109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Bellon M, Nicot C. Telomere dynamics in immune senescence and exhaustion triggered by chronic viral infection. Viruses. 2017;9:289. doi: 10.3390/v9100289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Cuervo AM, Macian F. Autophagy and the immune function in aging. Curr Opin Immunol. 2014;29:97–104. doi: 10.1016/j.coi.2014.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Tang SW, Ducroux A, Jeang KT, Neuveut C. Impact of cellular autophagy on viruses: insights from hepatitis B virus and human retroviruses. J Biomed Sci. 2012;19:92. doi: 10.1186/1423-0127-19-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Boehm U, Klamp T, Groot M, Howard JC. Cellular responses to interferon-gamma. Annu Rev Immunol. 1997;15:749–795. doi: 10.1146/annurev.immunol.15.1.749 [DOI] [PubMed] [Google Scholar]
- 88. Dong X, Levine B. Autophagy and viruses: adversaries or allies? J Innate Immun. 2013;5:480–493. doi: 10.1159/000346388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Gassen NC, Niemeyer D, Muth D, et al. SKP2 attenuates autophagy through Beclin1-ubiquitination and its inhibition reduces MERS-coronavirus infection. Nat Commun. 2019;10:5770. doi: 10.1038/s41467-019-13659-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Li MM, MacDonald MR. Polyamines: small molecules with a big role in promoting virus infection. Cell Host Microbe. 2016;20:123–124. doi: 10.1016/j.chom.2016.07.012 [DOI] [PubMed] [Google Scholar]
- 91. Stallone G, Infante B, Prisciandaro C, Grandaliano G. mTOR and aging: an old fashioned dress. Int J Mol Sci. 2019;20:2774. doi: 10.3390/ijms20112774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Keating R, Hertz T, Wehenkel M, et al. The kinase mTOR modulates the antibody response to provide cross-protective immunity to lethal infection with influenza virus. Nat Immunol. 2013;14:1266–1276. doi: 10.1038/ni.2741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Mannick JB, Del Giudice G, Lattanzi M, et al. mTOR inhibition improves immune function in the elderly. Sci Transl Med. 2014;6:268ra179. doi: 10.1126/scitranslmed.3009892 [DOI] [PubMed] [Google Scholar]
- 94. Mannick JB, Morris M, Hockey HP, et al. TORC1 inhibition enhances immune function and reduces infections in the elderly. Sci Transl Med. 2018;10:eaaq1564. doi: 10.1126/scitranslmed.aaq1564 [DOI] [PubMed] [Google Scholar]
- 95. Kraig E, Linehan LA, Liang H, et al. A randomized control trial to establish the feasibility and safety of rapamycin treatment in an older human cohort: immunological, physical performance, and cognitive effects. Exp Gerontol. 2018;105:53–69. doi: 10.1016/j.exger.2017.12.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Barzilai N, Crandall JP, Kritchevsky SB, Espeland MA. Metformin as a tool to target aging. Cell Metab. 2016;23:1060–1065. doi: 10.1016/j.cmet.2016.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Moser TS, Schieffer D, Cherry S. AMP-activated kinase restricts Rift Valley fever virus infection by inhibiting fatty acid synthesis. PLoS Pathog. 2012;8:e1002661. doi: 10.1371/journal.ppat.1002661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Li P, Jin Y, Qi F, et al. SIRT6 acts as a negative regulator in dengue virus-induced inflammatory response by targeting the DNA binding domain of NF-κB p65. Front Cell Infect Microbiol. 2018;8:113. doi: 10.3389/fcimb.2018.00113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Sargiacomo C, Sotgia F, Lisanti MP. COVID-19 and chronological aging: senolytics and other anti-aging drugs for the treatment or prevention of corona virus infection? Aging (Albany NY). 2020;12:6511–6517. doi: 10.18632/aging.103001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Zhou Y, Hou Y, Shen J, Huang Y, Martin W, Cheng F. Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discov. 2020;6:14. doi: 10.1038/s41421-020-0153-3 [DOI] [PMC free article] [PubMed] [Google Scholar]