ABSTRACT
Food environments may promote access to unhealthy foods, contributing to noncommunicable diseases in low- and middle- income countries (LMICs). This review assessed published evidence on the effects of food environment interventions on anthropometric (BMI and weight status) outcomes in school-aged children (5–9 y) and adolescents (10–19 y) (SACA) in LMICs. We summarized randomized controlled trials (RCTs) and quasi-experimental studies (QES) published since 2000 to August 2019 in the peer-reviewed and gray literature that assessed the effects of food-related behavioral and environmental interventions on diet-related health outcomes in SACA in LMICs. Electronic databases (MEDLINE, Embase, PsycINFO, Cochrane Library) were searched using appropriate keywords, Medical Subject Headings, and free text terms. Eleven RCTs and 6 QES met the inclusion criteria, testing multicomponent behavioral and environmental interventions in schools. Analysis of 6 RCTs (n = 17,054) suggested an overall effect on change in BMI [mean difference (MD): −0.11, 95% CI: −0.19 , −0.03], whereas there was no observed effect in 5 studies using endline BMI (n = 17,371) (MD: 0.05, 95% CI: −0.32, 0.21). There was no significant pooled effect among the 3 QES (n = 5,023) that reported differences in change in BMI or endline (MD: −0.37, 95% CI: −0.95, 0.22). There is limited evidence to support the modification of diet-related health outcomes through school-based food environment interventions in SACA in LMICs. Further studies are needed to understand the impact of school and community-based food environment interventions on nutritional status in this population.
Keywords: food environment, nutrition, diet, school-age children, adolescents, developing countries
Introduction
Malnutrition is one of the leading risk factors for morbidity and mortality globally (1). Since the Millennium Development Goal era, considerable effort has focused on eradicating undernourishment and improving health outcomes in children and adolescents through efforts in nutrition, supplementation, and fortification. However, recent shifts in global supply chains and foreign direct investments, and transformations in food processing, packaging, and distribution have drastically changed the landscape of food (2). In low- and middle-income countries (LMICs), as classified by the World Bank in terms of a country's gross national income (GNI) in United States Dollars per capita, there is greater accessibility and availability of cheap, fast-food, and convenience foods. Simultaneously, a significant portion of consumed food in LMICs is still acquired through domestic channels and informal unregistered vendors, such as wet markets and mobile vendors (2). The dynamic and opportunistic nature of the food environment leads to challenges in accurately estimating food availability, accessibility, and affordability in a given setting. For school-aged children and adolescents (SACA), elements of the food environment may increase reliance on, and greater preference for, nutrient-poor and ultraprocessed foods, including sugar-sweetened beverages, as well as increased unhealthy snacking and eating away from home (3, 4). These dietary patterns are believed to underlay the nutrition transition and double burden of malnutrition in many LMICs (5, 6).
Interventions designed to enhance food environments may be “settings-based,” implemented in schools, workplaces, community centers, and neighborhoods, or “sector-based,” implemented at a macrolevel (e.g., national supply chains and the private sector) (7). For SACA, school and work settings and the surrounding consumer spaces are influential food environments whereby their food choices and consumption are dictated by what is available and accessible (e.g., in cafeterias, vending machines, food vendors on or near school/work) (7, 8). The home microlevel environment is similarly important and influential in dietary intake and health outcomes in SACA, but is likely to be affected by a different set of policy levers and is therefore outside of the scope of the present review.
Food environment interventions are commonly classified as environmental or behavioral (9, 10). Environmental interventions focus on aspects of the environment that influence food choice, such as the natural and physical environments, legal and political, socioeconomic, and cultural environments (e.g., changes to the school cafeteria menu or decreased availability of snack foods in schools). Behavioral interventions place greater emphasis on individuals, often focusing on their knowledge, attitudes, perceptions, and preferences regarding food choice and dietary intake (e.g., nutrition counseling and education programs) (10). Interventions may overlap in terms of level of implementation and/or intervention modality. For example, nutritional labeling policies may be implemented at both the consumer and workplace levels, and aim to alter both the environment and behavior of the consumer.
The objective of this review was to examine interventions of the food environment and its impact on anthropometric and diet-related health outcomes in SACA in LMICs. To date, food environment research has mostly been conducted in high-income countries. However, food environments in LMICs differ from those in high-income settings in terms of their dynamic nature and infrastructure, providing unique challenges in effectively measuring and monitoring food environments (11). Thus, understanding if and how food environment interventions affect health outcomes in LMICs is crucial to provide strategic recommendations, and to encourage advocacy and further research in this area.
Definitions of the Food Environment
Food system
A system that embraces all the elements (environment, people, inputs, processes, infrastructure, institutions, markets, and trade) and activities that relate to the production, processing, distribution and marketing, preparation and consumption of food, and the outputs of these activities, including socioeconomic and environmental outcomes [High Level Panel of Experts (2)].
Food environment
The collective physical, economic, policy and sociocultural surroundings, opportunities, and conditions that influence people's food and beverage choices and nutritional status [International Network for Food and Obesity/Non-communicable Diseases (NCDs) Research, Monitoring, and Action Support (8)].
Food accessibility
This refers to proximity, density, and presence of retailers relative to individuals or organizations.
Food availability
This refers to both retailers and product availability within a given context.
Food pricing
From a market perspective, this is indicative of the market price of products. From a household or individual perspective, this equates to affordability (purchasing power).
Food promotion
Promotional advertising, marketing and branding, and packaging directed at individuals.
Food policy
This refers to policies, regulations, and guidelines related to the provision, sale, and marketing of food (i.e., national, regional, local) within consumer and organizational environments.
Methods
Search strategy and selection criteria
The search strategy was formulated using the Problem/Patient/Population, Intervention/Indicator, Comparison, Outcome (PICO) methodology, and use of Medical Subject Headings and keywords. A comprehensive search of the literature was conducted in the following databases: BiblioMap, Cochrane Central Register of Controlled Trials, Embase, PsycINFO, MEDLINE, and TRoPHI, as well as trials registered with the International Clinical Trials Registry Platform. The publication date range was established from January 2000 to August 2019 given the paucity of food environment research prior to 2000. Non-indexed (“grey”) literature was searched within the following organizational websites and databases, using keyword searches in the areas of health, health promotion, nutrition, and food environment: eLENA, Food and Agricultural Organization, International Food Policy and Research Institute, International Initiative for Impact Evaluation, International Network for Food and Obesity Research, Monitoring, and Action Support, National Cancer Institute, Epidemiology and Genomics Research Program, World Bank, World Food Programme, and World Obesity. No language restrictions or search filters were applied.
Studies were eligible if they included data collected in or after 2000 and measured the effects of a food environment intervention on ≥1 specific health outcome (listed below) in SACA (aged 5–19.9 y) living in LMICs. Preventive and management-based environmental interventions that were implemented at the school (or other organization), community, or market were included. Organizational interventions include changes to the school or workplace, whereas market-level interventions focus on the consumer retail environment and may include policy changes in taxation or marketing of food products. Community-level interventions include population policies and programs, such as public health campaigns to reduce advertising of unhealthy foods on television. Studies with multicomponent interventions that included an environmental and behavioral component (either together or in separate arms) were eligible for inclusion. Control groups included populations that were not exposed to the experimental intervention.
Eligible primary outcomes included anthropometric and diet-related health outcomes relevant to SACA: stunting (<2 SDs for height-for-age), wasting (<2 SDs for weight-for-height), BMI, lean mass, fat mass, waist circumference, waist-to-hip ratio, anemia, type 2 diabetes, metabolic syndrome, goiter, xeropthalmia, and night blindness.
SACA who were in school or out-of-school were eligible for inclusion. Studies were excluded if the population only consisted of individuals with a defined pre-existing illness (e.g., chronic and genetic diseases, metabolic, nutritional, and growth disorders, HIV, and tuberculosis). Studies that included participants beyond the eligible age range (e.g., 20–22 y or 1–4 y), where the mean age was <5 y or ≥20 y, or did not provide a mean age were also excluded.
The following types of study designs were eligible for inclusion: randomized controlled trials (RCTs), quasi-experimental studies (QES), nonrandomized controlled trials (NRCTs), controlled before-after studies, interrupted-time-series studies, and repeated measures studies, as well as large-scale program evaluations that assessed the efficacy and/or effectiveness of interventions. Mixed methods studies were also considered, but only quantitative aspects of those studies were included.
Study screening and data extraction
Following removal of duplicate studies, a multistage screening process was conducted to select eligible studies. Each title and abstract was assessed by a single reviewer. Full-text screening was conducted in duplicate according to the inclusion/exclusion criteria. De-duplication and title and abstract screening were managed using EndNote. Full-text screening and documentation of reasons for exclusion were managed using Covidence, a web-based platform for systematic review processes. Any disagreements were resolved by discussion, and where necessary, by consultation of a third review author. Data from included studies were independently coded and abstracted by two authors, using predefined data abstraction forms. Abstraction forms were matched and in the event of a disagreement, a third review author was consulted. See Supplementary Table 1 for details on variables extracted.
Data analysis
All reported outcomes were taken directly from published studies and publicly available information. Authors were contacted if there were discrepancies in reported data. For binary outcomes, we reported the risk ratio (RR) of outcomes in the intervention group compared with the control group. For continuous outcomes, we reported the mean difference (MD) using change scores (preferentially) or endline values, if the outcomes had been measured in the same way by all studies. We conducted random-effects meta-analyses to investigate the impact of interventions on BMI (kg/m2), zBMI (relative weight for child age), and prevalence of weight status (overweight, obesity, or combined). We also explored heterogeneity by age group, measure (endline or change scores), setting of intervention, risk of bias, duration of intervention (≤9 wk compared with >9 wk), and by study design (randomization compared with nonrandomization). Quality assessment was conducted in duplicate. Risk of bias of included studies was appraised using the adapted Cochrane Effective Practice and Organization of Care (EPOC) guidelines for randomized trials. QES were evaluated based on the Risk of Bias In Non-Randomized Studies of Interventions (ROBINS-I) (12). Both tools incorporated 5 domains of bias assessment including: selection, performance, attrition, detection, and outcome reporting. In terms of certainty of outcomes, we appraised BMI and weight status prevalence using Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) criteria (risk of bias, imprecision, indirectness, inconsistency, and publication bias) (13, 14). Quality was rated as low, medium, or high. Statistical analysis was conducted in Review Manager 5.3.
Results
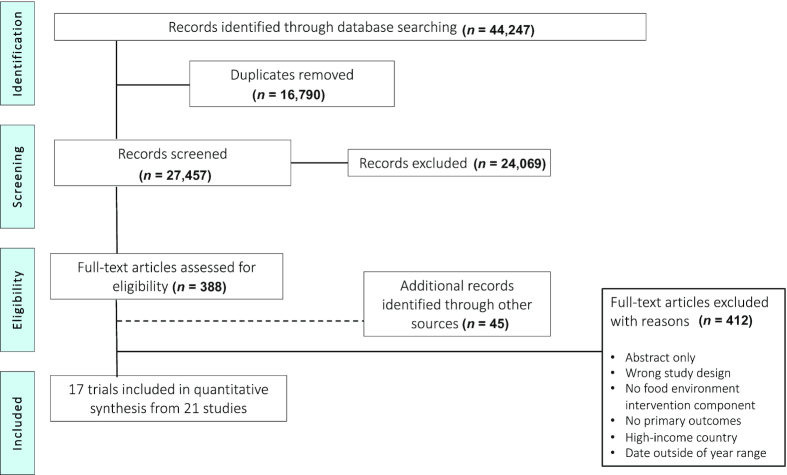
A database search generated 27,457 records after duplicates were removed. Screening of titles and abstracts identified 388 articles, and an additional 45 records from other sources, for full-text review. Of these, 17 trials (21 studies) met our inclusion criteria and were included in the analysis. Due to the following reasons, 412 studies were excluded: ineligible interventions (either inappropriate intervention type or no intervention present), outcomes (wrong primary outcomes), or study populations (not specific to ages 5–19 y). See Figure 1 for the flow of studies.
FIGURE 1.
Flow chart of study selection process.
Of the included trials, 11 were RCTs and 6 were QES. Three trials were conducted in China (15–17), while two studies were conducted in Thailand (18, 19) and two studies in Mexico (20, 21). The remaining trials were conducted in the following countries: Brazil (22), India (23), South Africa (24), Turkey (25), Malaysia (26), Lebanon (27), Tonga (28), Fiji (29), Iran (30), and Argentina (31) (Table 1). All studies were conducted in a school setting, of which 13 were in urban areas. The majority of studies did not indicate whether schools were private or public, apart from one study that included a mix of public and private schools, and two studies that were explicitly conducted in public schools. All studies evaluated multicomponent interventions, without disaggregating outcome data by component, and all studies included a control group. Behavioral interventions include components such as lifestyle modification comprising nutrition education and/or physical activity sessions with students and parents. Food environment interventions include components such as increasing the availability of healthy foods within the school (15–22, 24–29, 31), developing school policies regarding the sale or marketing of food (17–19, 23, 24, 28, 29), and promotion of healthy foods or water consumption (28, 29). The duration of interventions varied from 3 mo to 3 y. The total number of participants analyzed in the included studies was 28,457 children and adolescents (5–19.9 y). Fourteen trials included participants who were within the age range of 7–13 y. Three focused primarily on adolescents with an age range of 13–19 y.
TABLE 1.
Characteristics of included studies
| Author (year) | Country | Study design/duration | Participants | Intervention | Outcomes |
|---|---|---|---|---|---|
| Alvirde-Garcia (2013) (21) | Mexico | RCT; duration of the intervention: 3 y. Measurements were taken at years 1, 2, and 3 | 2 semirural communities (2 schools in Tenango del Vale and 3 schools in Santa Cruz) were selected with similar SES characteristics. The intervention group (Tenango del Vale) analyzed 816 students, while the comparison group (Santa Cruz) analyzed 408 students | Behavioral component: the intervention included nutrition education and increased physical activity (PA) for the pupils, lifestyle modification for parentsEnvironmental component: change in food items sold at schools’ canteens | Primary outcomes: BMI, prevalence of overweight, prevalence of obesity Secondary outcomes: dietary intake (calories from foods) |
| Amini (2016) (30) | Iran | cRCT; duration of the intervention: 18 wk. Measures were taken before and immediately after the intervention | 334 students, 167 in the intervention and 167 in the comparison group (grades 4–6) determined to be overweight or obese based on WHO standards, were recruited for the study. Analysis on 164 in the intervention and 163 in the comparison group | Behavioral component: the intervention included nutrition education and increased physical activity (PA) for the pupils, lifestyle modification for parents Environmental component: change in food items sold at the schools’ canteens | Primary outcomes: weight, height, BMI (z-score), waist circumference, hip circumference, trifold skin thickness Secondary outcomes: dietary intake (energy, fat, protein, carbohydrates, % energy from fat, % energy from carbohydrates) |
| Banchonhattakit (2009) (19) | Thailand | Quasi-experimental; duration of the intervention: 8 mo. Follow-up lasted 8 mo | 12 schools, with 375 students in the 5th grade (6 schools were the intervention group, N = 180 and 6 schools were the control group, N = 195) met the inclusion criteria | Behavioral component: the school network supported the implementation of the intervention, had monthly meetings, and consisted of parents, school administrators, teachers, and community leaders; a healthy diet, 30 min of daily PA Environmental component: changing school policies and improved school-lunch programs were promoted | Primary outcomes: overweight and obesity (as N/% in BMI categories) Secondary outcomes: frequency of consumption of fast food |
| Chawla (2017) (18) | Thailand | Quasi-experimental; duration of the intervention: 6 mo. Measures were taken before and immediately after the intervention | 453 students attending grades 4–5 were enrolled. Of these, 414 (206 in the intervention group, and 208 in the control group) were analyzed | Behavioral component: 7, 50-min sessions on life-skills including but not limited to, healthy eating guidance, physical exercise, and nutritional assessment. School and parental involvement, including increasing PA time, and 1-h workshops for families Environmental component: school food policy on food sold in schools; removal of vending machines | Primary outcomes: normal, overweight & obese status (as % within each BMI z-score) Secondary outcomes: mean lipid profile |
| Cao (2015) (16) | China | cRCT; duration of the intervention: 2 y. Measures were taken in January 2011 (pre-intervention), at a follow-up in January 2012, at a second follow-up in January 2013 and post-intervention in January 2014. The intervention ended in December 2013 | 26 primary schools, 2446 students in grade 1. The schools were divided into 3 groups according to average obesity prevalence. 7 schools with a high obesity prevalence (75th percentile), 12 schools between the 25th and 75th percentiles, and 7 schools below the 25th percentile. Of these, 1813 students were analyzed: 985 students in the intervention group and 828 students in the control group | Behavioral component: provision of health education for parents, caregivers and students, and provision of physical exercise activities during school for students Environmental component: reduction of fat content in the food provided at canteens, and increased availability of fruits and vegetables at school canteens | Primary outcomes: normal, overweight & obese (as N/% within each BMI z-score), BMI (z-score) |
| De Villiers (2016) (24) Substudy: Steyn (2015) (34) | South Africa | cRCT; duration of the intervention: 3 y | 16 schools with 1002 students in grades 4–6 were enrolled. Of these, 503 students were analyzed from the intervention group, while 499 were analyzed from the control group | Behavioral component: providing life orientation curriculum including nutrition; family and community involvement including educational events Environmental component: nutrition activities related to developing healthy school nutrition policies; improving tuck shops by making healthier options available; encouraging learners to bring healthy lunch boxes to school; encouraging the promotion of healthy foods at special events; and the initiation of vegetable gardens at schools | Primary outcomes: severe thinness, thinness, normal, overweight, obese (as N/% within each BMI z-score) |
| Fotu (2011) (28) | Tonga | Quasi-experimental; duration of the intervention: 3 y | Within 22 villages, 13 schools with 2479 students aged 11–19 y were selected | Behavioral component: capacity building with school staff and the community Environmental component: promotion of nutrition through media; development of a vegetable garden and canteen; repair of water tank; implementation of school food policiesDuration of intervention: 3 y | Primary outcomes: height, weight, normal, overweight, obesity (BMI as kg/m2 and z-score), fat mass Secondary outcomes: frequency of consumption, place of consumption, meal patterns |
| Habib-Mourad (2014) (27) | Lebanon | Quasi-experimental; duration of the intervention: 3 mo | 374 students in grades 4–5 (aged 9–11 y) were selected. Of these, there were 4 schools with 100 students (57 male, 43 female) analyzed in the intervention group and 4 schools with 100 students (53 male, 47 female) analyzed in the control group | Behavioral component: education sessions (1 per week/3 mo); family programme with health events Environmental component: changes in school food shops | Primary outcomes: BMI (as kg/m2), waist circumference Secondary outcomes: frequency of consumption; place of consumption; meal patterns; types of foods purchased |
| Herscovici (2013) (31) | Argentina | RCT; duration of the intervention: 6 mo | 6 schools, 405 students in grades 5–6 (ages 9–11 y). Of these, 369 were analyzed: 205 students in the intervention group and 164 students in the control group. At baseline, in the intervention group, 47.7% were male, and 52.3% were female. In the control group, 53.2% were male and 46.8% were female | Behavioral component: nutritional education to promote healthy eating, good habits and PA, physical exercise activities for the students, and an educational workshop aimed at parents and caregivers Environmental component: modifications to the school snack bar to provide 5 healthy food items | Primary outcomes: underweight, normal weight, overweight and obese (as N/%), BMI (kg/m2), BMI (z-score); Secondary outcomes: increased and decreased consumption of certain food and beverages |
| Koo (2018) (26) | Malaysia | Quasi-experimental; duration of the intervention: 3 mo | 83 students aged 9–11 y were selected. Of these, 31 were analyzed in the intervention group (58.1% male) and 32 were analyzed in the control group (46.9% male) | Behavioral component: education sessions (biweekly 30-min sessions); family education session (once, on diet counseling) Environmental component: changes in availability of whole grain foods | Primary outcomes: BMI (as z-score), fat mass %, waist circumference |
| Kremer (2011) (29) | Fiji | Quasi-experimental; duration of the intervention: 2 y | Students (N = 2948), aged 13–18 y from 14 schools (7 intervention and 7 control). Of these, there were 7 schools with 879 students (46.1% male) analyzed in the intervention group and 7 schools with 2069 students (43.4% male) analyzed in the control group | Behavioral component: nutrition education for students and parents; training on vegetable gardening, pot plant technology, healthy meal preparation, food display, provision of healthy lunch and snacks Environmental component: offering of breakfast at school canteen; development of school food policies and guidelines; promotion of healthy foods through media (posters); development of a school garden | Primary outcomes: weight, height, BMI (as prevalence, kg/m2 and z-score), fat mass Secondary outcomes: frequency of consumption, meal patterns |
| Liu (2018) (17) | China | cRCT; duration of the intervention: 1 y | 12 primary schools; 1889 students in grades 3–5 (ages 7–11 y). Of these, 930 students were analyzed in the intervention group and 959 in the control group. In the intervention group, 53% of the students were male and 47% were female. In the control group, 50.5% of the students were male and 49.5% were female | Behavioral component: education on health and nutrition for students and physical exercise activities Environmental component: school policies that do not permit sugar-sweetened beverages, snacks, and electronic products in school. Promotion of drinking water and improvement of school lunches offered at the school cafeteria | Primary outcomes: BMI (kg/m2), BMI (z-score), underweight, normal, overweight, and obesity (as N/% within BMI z-scores) Secondary outcomes: consumption (portions/day) and frequency of consumption (number of days per week) of certain food and beverages |
| Safdie (2013a) (35)Substudy: Safdie (2013b) (35) | Mexico | RCT; duration of the intervention: 18 mo | Students (N = 886) in grades 4–5 (mean age 9.7 y ± 0.7) were enrolled in the study. Of these, 830 students were analyzed (N = 252 in intervention basic, N = 254 in intervention plus, N = 354 in control) | Basic intervention: behavioral, environmental and physical activity components Plus intervention: same intervention as basic, except added financial and human resources Behavioral component: educational and skill-based workshops on nutrition for students; mass communication, and supportive resources provided for students and parents on 4 main behaviors including fruit and vegetable consumption, water consumption, engage in PA and pack a healthy lunch Environmental component: increase availability of healthier food sold at schools; ensure water availability; limiting the sale of sugar-sweetened beverages in the schoolPA component: PA promoted during recess and free time; improving the quality of physical education ≥50 min/wk; improving the school premises and providing sports equipment | Primary outcomes: weight, height, BMI (kg/m2), weight status (as prevalence of overweight and obesity) |
| Sevinc (2011) (25) | Turkey | RCT; duration of the intervention: 8 mo | Students (N = 6847) in grades 1–7 were enrolled in the study. Of these, 6771 students were analyzed (N = 2012 in intervention 1 group, N = 1938 in intervention 2 group, N = 2821 in control) | Intervention 1: behavioral component (PA program). PA program included physical education lessons 2 and 3 h/wk, depending on the day Intervention 2: behavioral and environmental component. Behavioral components included a healthy nutrition education program. The environmental component was distribution of boxed milk during mealtime, and increasing the supply of healthy eating options in the school canteen (including, water, freshly squeezed fruit juice, buttermilk, milk, and seasonal fruits) | Primary outcome: BMI (kg/m2) |
| Sichieri (2009) (22) | Brazil | cRCT; duration of the intervention: 9 mo | Students (N = 1140) aged 9–12 y (mean age: 10.9 ± 0.81), were enrolled in the study. Of these, 927 students were analyzed (N = 434 in intervention, N = 493 in control) | Behavioral component: healthy lifestyle education program that provided simple messages encouraging water consumption instead of sugar-sweetened carbonated beverages Environmental component: water bottles were provided to students and faculty | Primary outcomes: weight, height, BMI (kg/m2), weight status (as prevalence of underweight, overweight, and obese) Secondary outcomes: food group intake |
| Singhal (2010) (23) Substudy: Singhal (2011) (36) | India | RCT; duration of the intervention: 8 mo | Students (N = 209) in grade 11 (aged 15–17 y, mean age: 16.02 ± 0.55), mixed SES, were enrolled in the study. Of these, N = 201 students were analyzed (N = 99 in intervention, N = 102 in the control) | Behavioral component: promotion of nutrition education through lectures and focused group discussion; PA periods in school every week for 30 min; weekly individual counseling; health camp for teachers Environmental component: policy changes in the school which changed the school canteen menu to offer healthier alternatives; limiting the sale of carbonated drinks, high calorie foods, and noodles | Primary outcomes: weight, height, BMI (kg/m2), BMI (z-score), waist circumference, triceps skinfold thickness Secondary outcomes: food group intake, lipid profiles, place of consumption, hs-CRP, HOMA-IR, HOMA-bCF, disposition index, fasting insulin, plasma glucose |
| Xu (2017) (15) Substudy: Meng (2013) (37) | China | cRCT; duration of the intervention: 2 semesters (∼8 mo) | Students (N = 9867), aged 6–13 y, were enrolled in the study. Of these, 8573 were analyzed (N = 3476 in comprehensive intervention, N = 628 in nutrition education intervention, N = 605 PA intervention, N = 3398 in comprehensive control, and N = 466 in control group for nutrition education intervention and PA intervention groups) | Nutrition education intervention: behavioral component (nutrition handbook and courses on nutrition and health), environmental component (the school lunch cafeteria menu was evaluated periodically and nutrition suggestions were provided accordingly) PA intervention: a classroom-based physical activity program to promote exercise Comprehensive intervention: the nutrition education intervention combined with PA intervention | Primary outcomes: BMI (kg/m2), BMI (z-score) waist circumference, fat mass % Secondary outcomes: insulin, plasma glucose, lipid profiles |
cRCT, cluster randomized controlled trial; HOMA-IR, homeostasis model assessment - insulin resistance; HOMA-bCF, homeostasis model assessment - β cell function; hs-CRP, high-sensitivity C-reactive protein; PA, physical activity; RCT, randomized controlled trial; SES, socioeconomic status.
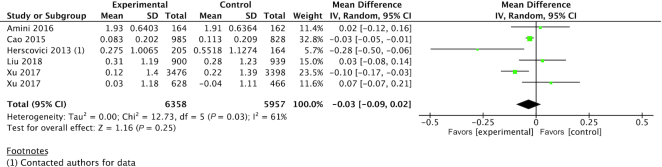
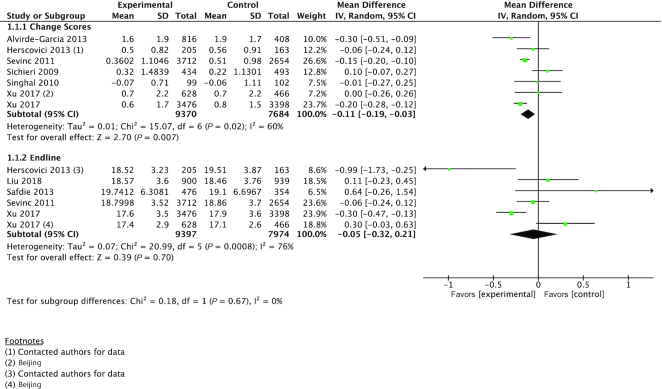
A pooled analysis of 5 studies (n = 12,315) measuring the effect of the intervention on mean BMI (z-score) at endline showed no overall effect [MD: −0.03 (95% CI: −0.09, 0.02)] (Figure 2). Likewise, a separate analysis that was limited to studies comparing the effect of the intervention on BMI (kg/m2) at endline produced similar null results [5 studies, n = 17,371, MD: −0.05 (95% CI: −0.32, 0.21)] (Figure 3). However, in an analysis of 6 studies (n = 17,054) in which BMI mean change was reported, there was a protective effect of the intervention [MD: −0.11 (95% CI: −0.19 −0.03)] (Figure 3). Importantly, the 2 largest RCTs, Sevinc et al. (25) (n = 6,366) and Xu et al. (15) (n = 6,874) did observe a small magnitude of effect on BMI, favoring an attenuated increase in BMI with the intervention [Xu et al. (15) change score MD: −0.20 (95% CI: −0.28, −0.12); endline MD: −0.30 (95% CI: −0.47, −0.13); Sevinc et al. (25) change score MD: −0.15 (95% CI: −0.20, −0.10); endline MD: −0.06 (95% CI: −0.24, 0.12)] (Figure 3).
FIGURE 2.
Forest plot of comparison: randomized controlled trial food environment interventions versus control. Mean difference in BMI (z-score) from baseline to post-intervention using endline values.
FIGURE 3.
Forest plot of comparison: randomized controlled trial food environment interventions versus control. Mean difference in BMI from baseline to post-intervention using change scores and endline values.
No significant differences between intervention and control groups were found for weight status outcomes, reported as prevalence of overweight [n = 11,796; RR: 0.96 (95% CI: 0.87, 1.05)], obesity [n = 13,635; RR: 0.92 (95% CI: 0.79, 1.07)], or overweight and obesity [n = 11,725; RR: 0.92 (95% CI: 0.80, 1.05)] using RCT data (Supplementary Figures S1–3).
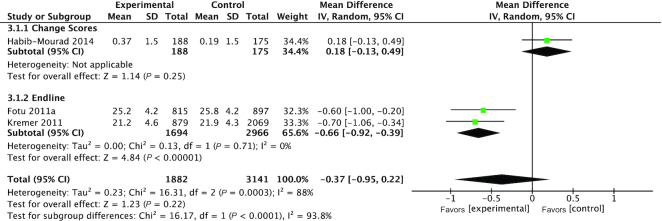
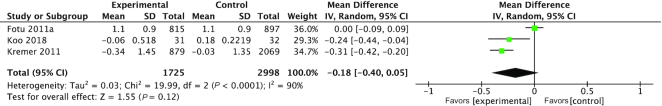
Pooled analysis of BMI from 3 QES [change score or endline (n = 5023)] suggested no significant differences between intervention and control populations [MD: −0.37 (95% CI: −0.95, 0.22)] (Figure 4) and as z-scores (n = 4,723) [MD: −0·.8 (95% CI: −0.40, 0.05)] (Figure 5).
FIGURE 4.
Forest plot of comparison: quasi-experimental interventions versus control. Mean difference in BMI from baseline to post-intervention using change scores and endline values.
FIGURE 5.
Forest plot of comparison: quasi-experimental interventions versus control. Mean difference in BMI (z-score) from baseline to post-intervention using endline values.
A similar finding was noted for 2 QES in terms of prevalence of obese participants [n = 4660; RR: 0.95 (95% CI: 0.74, 1.23)] and combined prevalence of overweight and obese participants [n = 2501; RR: 0.95 (95% CI 0.88, 1.03)]. However, there was a 11% reduced risk of becoming overweight compared with the control [2 studies, n = 4660; RR: 0.89 (95% CI: 0.81, 0.99)] (Supplementary Figures S4–6).
Discussion
The purpose of this review was to determine the impact of food environment interventions on diet-related health outcomes of SACA in LMICs. Pooled analyses showed a small significant effect on reduction in BMI, which aligns with similar systematic reviews of studies conducted in high-income countries (32). Furthermore, the two largest RCTs both showed significant attenuations in the increase in BMI in the intervention groups compared with the control groups. However, the effects were inconsistent and there was substantial heterogeneity across studies in terms of study design (randomization, blinding, duration, and complexity of intervention components), measurement tools, and populations. Given the complexity and upstream nature of food environment interventions, there is an inherent dilution bias (33). Controlling the dose of exposure within a food environment intervention poses logistical difficulty and can be contaminated by other environments and elements, such as the household food environment, consumer behavior, attitudes, and preferences.
The diverse dimensions of the food environment lead to a variety of interventions that may be designed and implemented. However, among studies in the present review, the most commonly addressed food environment dimension was availability. Of the 17 trials included in the analysis, 15 (6 QES and 9 RCTs) involved an intervention or intervention component that changed food availability in school settings. Typically, an intervention increased the availability of healthy food items and removed unhealthy items from the cafeteria and vendors on the school property. Most study interventions examined multiple food environment dimensions. For example, the intervention by Fotu et al. (28) addressed the promotion and availability of healthy food products, as well as school policies on food vendors on school property. The multifaceted design of these interventions limited the ability to disentangle outcome data by dimension. Interventions also targeted food promotion, accessibility, and policy. No study intervention captured data on pricing or spending patterns of SACA. Understandably, the unregulated and the unstable nature of food vendors in LMICs lends to inconsistent pricing and insufficient cost regulation, a possibly difficult metric. Additionally, spending by SACA is influenced by factors beyond their control, including household socioeconomic status, and whether they receive spending money from parents and guardians.
All studies in this review used multicomponent interventions, consisting of both a behavioral component (e.g., a nutrition education program) and an environmental component, defined as any policy or physical change to the environment, which affects one or more of the food environment dimensions. None of the studies disaggregated outcome data based on the discrete behavioral and environmental components, providing a limited ability to analyze and understand the environment-specific effects on health outcomes in this age group. However, we acknowledge the logistical difficulties in disentangling environmental from behavioral components. Behavior change and effects on diet-related health outcomes, such as BMI, may be dependent on greater intervention duration. In this review, duration ranged from 3 mo to 3 y, with half of the studies (n = 8) implementing interventions with a duration of 9 mo or less.
Beyond school premises, the consumer food environment, including social media, presents numerous additional opportunities for children (particularly older children) to dilute the effect of school-based interventions (32). Future research may consider a factorial or multiarm RCT study design, whereby school and community-based interventions, using both environmental and behavioral-type components, can be both disaggregated and combined, to compare and contrast their effects.
A major limitation of this review is the lack of generalizability of the results. First, none of the studies were conducted in low- or lower-middle income countries; all were conducted in upper-middle income countries, although it is noted that conditions and contexts amongst the upper middle-income countries may differ. In addition, the majority (13 of 17) of studies were conducted in urban settings. Yet, according to recent World Bank estimates, 41.8% of the global population aged 0–14 y and ∼11% of females and male aged 15–19 y live in low-income settings (38). Estimates also show that just less than half of the global population (44.7%) live in rural areas. All of the studies implemented interventions at the school level, such that the findings of this review cannot be extrapolated to other community settings. The rationale for school-level interventions assumes that most children and adolescents attend school and therefore will be reached by the program. However, in many LMICs, there may be limitations to official registration and regular attendance of students, for reasons including gender biases in school enrollments, financial limitations, and child labor (39).
The robustness of pooled analyses was greatly limited by the heterogeneity of food environment exposures and diet-related health outcomes measured across the studies. For example, although the majority of studies measured BMI, it was variably reported using the original units (kg/m2) or normalized as a z-score (with an inconsistent use of WHO Growth Standards), and some studies reported endline averages whereas others compared groups with respect to interval changes (Table 2). Furthermore, all studies included both SACA without disaggregating outcome data between different age groups or between boys and girls. This is an important consideration given the unique transition from childhood to adolescence, which is marked by specific physiological changes, mental and socioemotional development, and increased behavioral autonomy and choice (40).
TABLE 2.
Included studies by outcome reported
| Author (year) | BMI (z-score) | BMI (kg/m2) change score | BMI (kg/m2) endline | Prevalence of overweight | Prevalence of obesity | Prevalence of overweight and obesity |
|---|---|---|---|---|---|---|
| Randomized Controlled Trials | ||||||
| Alvirde-Garcia (2013) (21) | x | |||||
| Amini (2016) (30) | x | |||||
| Cao (2015) (16) | x | x | x | |||
| De Villiers (2016) (24) Substudy: Steyn (2015) (34) | x | x | x | |||
| Herscovici (2013) (31) | x | x | x | |||
| Liu (2018) (17) | x | x | x | x | ||
| Safdie (2013a) (20) Substudy: Safdie (2013b) (35) | x | |||||
| Sevinc (2011) (25) | x | x | ||||
| Sichieri (2009) (22) | x | x | x | |||
| Singhal (2010) (23) Substudy: Singhal (2011) (36) | x | |||||
| Xu (2017) (15) Substudy: Meng (2013) (37) | x | x | x | x | x | x |
| Quasi-experimental Studies | ||||||
| Banchonhattakit (2009) (19) | x | |||||
| Chawla (2017) (18) | x | |||||
| Fotu (2011) (28) | x | x | x | x | x | |
| Habib-Mourad (2014) (27) | x | |||||
| Koo (2018) (26) | x | |||||
| Kremer (2011) (29) | x | x | x | x | ||
Based on EPOC, ROBINS-I, and GRADE criteria, both RCTs and QES in this review were downgraded due to unclear or high risk of disclosure of random sequence generation and indirectness of the intervention. It should be noted that although lack of blinding of both personnel and participants of the intervention is usually a reason for downgrading, it is not always appropriate nor possible. In certain cases, it is not possible to completely blind participants, such as in a food environment intervention that changes the availability of consumed items offered in the cafeteria. Lastly, other methodological limitations of food environment research include the assurance of appropriate and ethical randomization in RCTs and the lack of feasibility of geographical separation between intervention and control groups in QES to control for contamination (41).
Conclusions
In summary, this systematic review yielded limited evidence to support a beneficial effect of food environment interventions on anthropometric and weight-status outcomes in SACA in LMICs. Pooled analyses were difficult to interpret given the between-study heterogeneity in design, food environment metrics, outcome reporting, and effect sizes. Future work should identify key components of the food environment that may be amenable to modification by well-designed and feasible interventions, tested in the context of RCTs that are powered to examine effects on health outcomes of public health relevance including obesity and other noncommunicable diseases, and micronutrient deficiencies. As the number of SACA increases globally (40), it is critical that these knowledge and data gaps are addressed to guide future policies and programs in LMICs.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to acknowledge Michelle Gaffey for her assistance in the protocol development. The authors’ contributions were as follows—ZAB and DR: conceptualized the systematic review; BC, CO, EK, DR, and ZAB: have content expertise in the area of global child health and nutrition; EK, DR, and ZAB: have expertise and experience in conducting systematic reviews and meta-analyses, as well as in statistical methods, particularly those methods used in clinical research and epidemiology; BC and CO: conducted the search, retrieved and extracted all data in the systematic review; BC: conducted the meta-analyses; BC and CO: wrote the draft manuscript; EK, DR, and ZAB: assisted in editing the final version; and all authors: read and approved the final version of the manuscript.
Notes
Supported by the Joannah and Brian Lawson Centre for Child Nutrition, The University of Toronto, Canada; Award: 0001/2017/471141. The funders had no role in the design, implementation, analysis, or interpretation of results.
Supplemental Table 1 and Supplemental Figures 1–6 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn/.
Author disclosures: The authors report no conflicts of interest.
Abbreviations used: CI, Confidence Interval; EPOC, Effective Practice and Organization of Care; GRADE, Grading of Recommendations, Assessment, Development, and Evaluations; LMIC, low- and middle- income country; MD, mean difference; QES, quasi-experimental studies; RCT, randomized controlled trial; ROBINS-I, Risk of Bias In Non-Randomized Studies of Interventions; RR, risk ratio; SACA, school-aged children and adolescents.
Contributor Information
Bianca Carducci, Email: bianca.carducci@sickkids.ca, Centre for Global Child Health, Hospital for Sick Children; Peter Gilgan Centre for Research, and Learning (PGCRL), Toronto, ON, Canada; Department of Nutritional Sciences, University of Toronto, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada.
Christina Oh, Centre for Global Child Health, Hospital for Sick Children; Peter Gilgan Centre for Research, and Learning (PGCRL), Toronto, ON, Canada.
Emily C Keats, Centre for Global Child Health, Hospital for Sick Children; Peter Gilgan Centre for Research, and Learning (PGCRL), Toronto, ON, Canada.
Daniel E Roth, Centre for Global Child Health, Hospital for Sick Children; Peter Gilgan Centre for Research, and Learning (PGCRL), Toronto, ON, Canada; Department of Nutritional Sciences, University of Toronto, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada; Department of Pediatrics, University of Toronto, Toronto, Ontario, Canada; Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada.
Zulfiqar A Bhutta, Centre for Global Child Health, Hospital for Sick Children; Peter Gilgan Centre for Research, and Learning (PGCRL), Toronto, ON, Canada; Department of Nutritional Sciences, University of Toronto, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada; Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada; Centre of Excellence in Women and Child Health, Aga Khan University, Karachi, Pakistan.
References
- 1. Food and Agriculture Organization, International Fund for Agricultural Development, United Nations Children's Fund, World Food Programme and World Health Organization. The State of Food Security and Nutrition in the World 2018: Building Climate Resilience for Food Security and Nutrition 2018. [Internet]. Rome: Food and Agriculture Organization; 2018. Available from: http://www.fao.org/3/I9553EN/i9553en.pdf. [Google Scholar]
- 2. High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. Nutrition and Food systems. [Internet]. Rome: Committee on World Food Security; 2017. Available from:http://www.fao.org/3/a-i7846e.pdf.
- 3. Baker P, Friel S. Food systems transformations, ultra-processed food markets and the nutrition transition in Asia. Global Health. 2016;12(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Popkin BM, Reardon T. Obesity and the food system transformation in Latin America. Obes Rev. 2018;19(8):1028–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. International Food Policy Research Institute. 2017 Global Food Policy Report. [Internet]. Washington, DC: International Food Policy Research Institute; 2017. Available from: https://www.ifpri.org/publication/2017-global-food-policy-report. [Google Scholar]
- 6. Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, James WP, Wang Y, McPherson K. Child and adolescent obesity: part of a bigger picture. Lancet. 2015;385(9986):2510–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev. 2002;3(4):289–301. [DOI] [PubMed] [Google Scholar]
- 8. Swinburn B, Sacks G, Vandevijvere S, Kumanyika S, Lobstein T, Neal B, Barquera S, Friel S, Hawkes C, Kelly B et al.. INFORMAS (International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support): overview and key principles. Obes Rev. 2013;14(Suppl 1):1–12. [DOI] [PubMed] [Google Scholar]
- 9. Roberto CA, Swinburn B, Hawkes C, Huang TT, Costa SA, Ashe M, Zwicker L, Cawley JH, Brownell KD. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385(9985):2400–9. [DOI] [PubMed] [Google Scholar]
- 10. Hawkes C, Jewell J, Allen K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING Framework. Obes Rev. 2013;14(Supplement 2):159–68. [DOI] [PubMed] [Google Scholar]
- 11. Turner C, Kalamatianou S, Drewnowski A, Kulkarni B, Kinra S, Kadiyala S. Food environment research in low- and middle-income countries: a systematic scoping review. Adv Nutr. 2019;11(2):387–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry S, Altman DG, Ansari MT, Boutron I et al.. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Presenting results and ‘Summary of findings’ tables. In: Higgins JPT and Green S.editors. Cochrane Handbook for Systematic Reviews of Interventions. West Sussex: John Wiley & Sons; 2008. p. 335–58. [Google Scholar]
- 14. Guyatt GH, Oxman AD, Vist GE, Kunz R, Kalck-Ytter Y, Alonso-Coello P, Schunemann HJ; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xu H, Li Y, Zhang Q, Hu XL, Liu A, Du S, Li T, Guo H, Li Y, Xu G et al.. Comprehensive school-based intervention to control overweight and obesity in China: a cluster randomized controlled trial. Asia Pac J Clin Nutr. 2017;26(6):1139–51. [DOI] [PubMed] [Google Scholar]
- 16. Cao ZJ, Wang SM, Chen Y. A randomized trial of multiple interventions for childhood obesity in China. Am J Prev Med. 2015;48(5):552–60. [DOI] [PubMed] [Google Scholar]
- 17. Liu Z, Li Q, Maddison R, Ni Mhurchu C, Jiang Y, Wei DM, Cheng L, Cheng Y, Wang D, Wang HJ. A school-based comprehensive intervention for childhood obesity in China: a cluster randomized controlled trial. Child Obes. 2019;15(2):105–15. [DOI] [PubMed] [Google Scholar]
- 18. Chawla N, Panza A, Sirikulchayanonta C, Kumar R, Taneepanichskul S. Effectiveness of a school-based multicomponent intervention on nutritional status among primary school children in Bangkok, Thailand. J Ayub Med Coll Abbottabad. 2017;29(1):13–20. [PubMed] [Google Scholar]
- 19. Banchonhattakit P. Effectiveness of school network for childhood obesity prevention. Southeast Asian J Trop Med Public Health. 2009;40(4):816–34. [PubMed] [Google Scholar]
- 20. Safdie M, Jennings-Aburto N, Levesque L, Janssen I, Campirano-Nunez F, Lopez-Olmedo N, Aburto T, Rivera JA. Impact of a school-based intervention program on obesity risk factors in Mexican children. Salud Publica Mex. 2013;55(3):374–87. [DOI] [PubMed] [Google Scholar]
- 21. Alvirde-Garcia U, Henao-Moran S, Gomez-Perez FJ, Aguilar-Salinas CA. Resultados de un programa comunitario de intervención en el estilo de vida en niños. Salud Publica Mex. 2013;55(3):406–14. [PubMed] [Google Scholar]
- 22. Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomized trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12(2):197–202. [DOI] [PubMed] [Google Scholar]
- 23. Singhal N, Misra A, Shah P, Gulati S. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr. 2010;64(4):364–73. [DOI] [PubMed] [Google Scholar]
- 24. De Villiers A, Steyn NP, Draper CE, Hill J, Gwebushe N, Lambert EV, Lombard C. Primary school children's nutrition knowledge, self-efficacy, and behavior, after a three-year healthy lifestyle intervention (HealthKick). Ethn Dis. 2016;26(2):171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sevinc O, Bozkurt AI, Gundogdu M, Bas Aslan U, Agbuga B, Aslan S, Dikbas E, Gokce Z. Evaluation of the effectiveness of an intervention program on preventing childhood obesity in Denizli, Turkey. Turk J Med Sci. 2011;41(6):1097–105. [Google Scholar]
- 26. Koo HC, Poh BK, Abd Talib R. The GReat-ChildTM Trial: a quasi-experimental intervention on whole grains with healthy balanced diet to manage childhood obesity in Kuala Lumpur, Malaysia. Nutrients. 2018;10(2):156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Habib-Mourad C, Ghandour LA, Moore HJ, Nabhani-Zeidan M, Adetayo K, Hwalla N, Summerbell C. Promoting healthy eating and physical activity among school children: findings from Health-E-PALS, the first pilot intervention from Lebanon. BMC Public Health. 2014;14 Article no: 940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fotu KF, Millar L, Mavoa H, Kremer P, Moodie M, Snowdon W, Utter J, Vivili P, Schultz JT, Malakellis M et al.. Outcome results for the Ma'alahi Youth Project, a Tongan community-based obesity prevention programme for adolescents. Obes Rev. 2011;12(Suppl 2):41–50. [DOI] [PubMed] [Google Scholar]
- 29. Kremer P, Waqa G, Vanualailai N, Schultz JT, Roberts G, Moodie M, Mavoa H, Malakellis M, McCabe MP, Swinburn BA. Reducing unhealthy weight gain in Fijian adolescents: results of the Healthy Youth Healthy Communities study. Obes Rev. 2011;12(Suppl 2):29–40. [DOI] [PubMed] [Google Scholar]
- 30. Amini M, Djazayery A, Majdzadeh R, Taghdisi MH, Sadrzadeh-Yeganeh H, Abdollahi Z, Hosseinpour-Niazi N, Chamari M, Nourmohammadi M. A school-based intervention to reduce excess weight in overweight and obese primary school students. Biol Res Nurs. 2016;18(5):531–40. [DOI] [PubMed] [Google Scholar]
- 31. Herscovici R, Kovalskys I, De Gregorio MJ. Gender differences and a school-based obesity prevention program in Argentina: a randomized trial. Rev Panam Salud Publica. 2013;34(2):75–81. [PubMed] [Google Scholar]
- 32. Driessen CE, Cameron AJ, Thornton LE, Lai SK, Barnett LM. Effect of changes to the school food environment on eating behaviours and/or body weight in children: a systematic review. Obes Rev. 2014;15(12):968–82. [DOI] [PubMed] [Google Scholar]
- 33. Lindholm L, Rosen M. What is the “golden standard” for assessing population-based interventions? – Problems of dilution bias. J Epidemiol Community Health. 2000;54(8):617–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Steyn NP, de Villiers A, Gwebushe N, Draper CE, Hill J, de Waal M, Dalais L, Abrahams Z, Lombard C, Lambert EV. Did HealthKick, a randomised controlled trial primary school nutrition intervention improve dietary quality of children in low-income settings in South Africa?. BMC Public Health. 2015;15:948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Safdie M, Levesque L, Gonzalez-Casanova I, Salvo D, Islas A, Hernandez-Cordero S, Bonvecchio A, Rivera JA. Promoting healthful diet and physical activity in the Mexican school system for the prevention of obesity in children. Salud Publica Mex. 2013;55(Suppl 3):357–73. [DOI] [PubMed] [Google Scholar]
- 36. Singhal N, Misra A, Shah P, Gulati S, Bhatt S, Sharma S, Pandey RM. Impact of intensive school-based nutrition education and lifestyle interventions on insulin resistance, beta-cell function, disposition index, and subclinical inflammation among Asian Indian adolescents: a controlled intervention study. Metab Syndr Relat Disord. 2011;9(2):143–50. [DOI] [PubMed] [Google Scholar]
- 37. Meng L, Xu H, Liu A, van Raaij J, Bemelmans W, Hu X, Zhang Q, Du S, Fang H, Ma J et al.. The costs and cost-effectiveness of a school-based comprehensive intervention study on childhood obesity in China. PLoS One. 2013;8(10):e77971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. World Bank Group. World Bank Group Open Data. [Internet]. Washington: World Bank Group; 2019. Available from:; https://data.worldbank.org/. [Google Scholar]
- 39. United Nations Educational, Scientific and Cultural OrganizationInstitute for Statistics (UIS). One in Five Children, Adolescents and Youth is Out of School. [Internet]. Montreal and Paris: UIS; 2018. Available from:; http://uis.unesco.org/sites/default/files/documents/fs48-one-five-children-adolescents-youth-out-school-2018-en.pdf. [Google Scholar]
- 40. World Health Organization. Implementing Effective Actions to Improving Adolescent Nutrition. [Internet]. Geneva: World Health Organization; 2018. Available from: https://apps.who.int/iris/bitstream/handle/10665/260297/9789241513708-eng.pdf. [Google Scholar]
- 41. Sanson-Fisher RW, Bonevski B, Green LW, D'Este C. Limitations of the randomized controlled trial in evaluating population-based health interventions. Am J Prev Med. 2007;33(2):155–61. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.