Abstract
Objective:
Fear of deportation (FOD) is a prevalent concern among mixed-status families. Yet, our understanding of how FOD shapes human health and development is in its infancy. To begin to address this knowledge gap, we examined the relationship between household FOD, body mass index (BMI) percentiles and salivary uric acid (sUA), a biomarker related to oxidative stress/hypertension/metabolic syndrome, among 111 individuals living in Mexican-origin families.
Methods:
Participants were 65 children (2 months-17 years, 49% female) and 46 adults (20–58 years, 71% female) living in 30 Mexican-origin families with at least one immigrant parent in Phoenix, AZ. We recruited families using cluster probability sampling of 30 randomly selected census tracts with a high proportion of Hispanic/Latino immigrants. The head of household completed a survey containing demographic, FOD, and psychosocial measures. All family members provided saliva (later assayed for sUA) and anthropometric measures. Relationships between household FOD, BMI percentile, and sUA levels were estimated using multilevel models.
Results:
Higher levels of household FOD were associated with lower BMI percentiles and lower sUA levels between families, after controlling for social support and socioeconomic proxies.
Conclusion:
Key features of the social ecology in which mixed-status families are embedded are associated with individual differences in biological processes linked to increased risk for chronic disease.
1 |. INTRODUCTION
Fear of immigration enforcement remains a persistent stressor for Latinos in the US (Becerra, Androff, Cimino, Wagaman, & Blanchard, 2013; Cavazos-Rehg, Zayas, & Spitznagel, 2007; Theodore, 2013). Immigration enforcement policies in the US entail high surveillance from local law enforcement and exclusion from participation in public life among immigrants and their children (Nuñez & Heyman, 2007; Rodríguez, Young, & Wallace, 2015; Suro, Suárez-Orozco, & Canizales, 2015; Yoshikawa, Godfrey, & Rivera, 2008; Yoshikawa & Kholoptseva, 2013). Fear and anxiety result from the possibility of a family member’s detention by Immigration Customs and Enforcement (ICE), financial hardship resulting from a family member’s detention or deportation, and adversity from discrimination. In Arizona, immigration enforcement policies restrict families’ access to adequate transportation, secure employment, and participation in federal social welfare programs (Rodríguez, Young, & Wallace, 2015; Suro et al., 2015; Yoshikawa et al., 2008). Senate Bill 1070 (SB 1070) “Support Our Law Enforcement and Safe Neighborhoods Act” passed in the Arizona state senate in 2010 to allow local law enforcement to arrest persons they suspect to be unauthorized immigrants during lawful stops, detentions, and arrests.
Immigration enforcement policies often target Mexican-origin and Latino communities in the US (Aranda & Vaquera, 2015; Magãna & Lee, 2013). Since the implementation of SB 1070, the enforcement of this policy has created levels of fear and mistrust such that even US-born Latinos feel vulnerable and report poorer psychosocial wellbeing (Moya-Salas, Ayón, & Gurrola, 2013; Szkupinski-Quiroga, Medina, & Glick, 2014). Moreover, the criminalization of undocumented Latinos has been amplified during Donald J. Trump’s tenure as President of the United States, where he has signed an executive order to build a militarized wall along the US-Mexico border and seeks to increase the deportation of unauthorized immigrants by including those with minor criminal infractions (Executive Order No. 13767, 2017). Despite our understanding of the effects of immigration enforcement policies on fear and anxiety, mistrust and vulnerability, financial hardship, and adversity from discrimination, research examining the relationship between fear from immigration enforcement and biobehavioral health has been limited (see Holmes & Marcelli, 2012; Landale, Hardie, Oropesa, & Hillemeier, 2015; for exceptions). In this study, we begin to address this knowledge gap.
1.1 |. Conceptual issues
There are direct and indirect reasons to expect a relationship between fear of deportation and biobehavioral health. In contrast to their Latino and immigrant peers, families living with an undocumented immigrant are more likely to be living in poverty, experience adversity related to discrimination, have restricted access to social services (Rodríguez et al., 2015; Suro et al., 2015; Van Hook & Balistreri, 2006; Yoshikawa et al., 2008), have high food insecurity (Kalil & Chen, 2008), and face chronic uncertainty and concern about deportation of undocumented family members. In sum, given shifting policies at the state and federal level, now more than ever, the social ecologies of families living with an undocumented immigrant increase an individual’s risk for negative health outcomes.
In recent decades, technical advances have enabled the minimally invasive measurement of a broad spectrum of biological variables in oral fluid samples. Importantly, within the context of research on immigrants in particular, saliva collection is perceived as more culturally acceptable than traditional biospecimens such as blood, urine, hair, or tissue (Gorodischer, Burtin, Hwang, Levine, & Koren, 1994; McClure, Snodgrass, Martínez, & Eddy, 2013). The measurement of uric acid in saliva is among the most recent developments in salivary bioscience.
Uric acid (UA) is the end product of the metabolic break-down of purine nucleotides. High levels of UA may be caused by consumption of high fructose corn syrup, table sugar, or purine-rich proteins, rapid weight loss, and/or reduced excretion from the kidneys (Mueller, Kasl, Brooks, & Cobb, 1970). Higher levels of UA can be indicative of oxidative stress (Aschbacher et al., 2013; Baldree & Stapleton, 1997; De Oliveira & Burini 2012; De Oliveira, Moreto, Silveira, & Burini, 2013; Ishizaka, Yamakado, Toda, Tani, & Ishizaka, 2014), which has the potential to accelerate cellular aging (Epel, 2009). UA is a well-established biomarker associated with hypertension, metabolic syndrome (MetS), gout, and kidney stones (Zhao & Huang, 2015), and a suitable predictor of individual differences in chronic disease risk in adolescence and adulthood (Jones, Richey, Alpert, & Li, 2008; Mellen et al., 2006; Sun, Pei, Lue, & Chen, 2015; Wang et al., 2012). Studies report a strong positive association between UA measured in serum and in saliva (Zhao & Huang, 2015).
Evidence also suggests that psychosocial factors are related to UA levels via adverse health behaviors. Recent research has indicated that there is a relationship between UA and acute stress, temperament, disinhibition and psychiatric disorders characterized by impulsivity. For example, Kesebir, Yaylacı, Süner, and Gültekin (2014) examined serum UA in relation to self-reported temperament data in patients with bipolar disorder (BD), major depressive disorder (MDD) and healthy controls. They found elevated UA in those with BD and significantly lower UA among those with MDD. Lorenzi and colleagues (2010) examined serum UA in relation to temperament in Brazilian adult men and women, finding that elevated serum UA levels were significantly correlated with disinhibition (no fear) in both men and women. Related to these results, Sutin and colleagues (2014) found that elevated levels of serum UA were related to impulsivity and excitement-seeking in men and women. Lyngdoh and colleagues (2013), in the only longitudinal study of serum UA in adults, found a quadratic relationship between serum UA and social phobia (a form of chronic stress), where elevated levels of serum UA were related to lower social phobia only up to a certain concentration and period of time, after which increasing serum UA levels were no longer protective and were correlated with increased odds of patients reporting social phobia. There is also some indication that there is a difference in serum UA levels if people anticipate the stress, where unanticipated stress is significantly related to lower levels of serum UA (Rahe & Arthur, 1967; Rahe, Arthur & Clark 1968; Zir, McHugh, Rahe, Arthur, & Rubin, 1973). Although researchers are not sure whether UA is a cause or consequence of emotion-related psychopathology, Goodman and colleagues (2016) found that salivary uric acid (sUA) levels predicted hippocampal regulation of emotion during acute psychosocial stress.
Monitoring sUA levels in persons of Mexican-origin may also be of empirical interest because of the high prevalence of chronic disease in this population. For example, in the US, obesity among Mexican children ages 2–11 is the highest at 20.9%, in comparison to Whites (13.3%) and Blacks (18.8%) (Kaur, Lamb, & Ogden, 2015). Similarly, Latino adults have a higher prevalence of obesity than non-Hispanic Whites (Flegal, Carroll, Ogden, & Curtin, 2010). In comparison to other US-based racial and ethnic groups, Latino adolescents have the highest prevalence of MetS (Cook, Weitzman, Auinger, Nguyen, & Dietz, 2003; Sun et al., 2015). Having higher levels of UA in youth is associated with MetS in children and adolescents (Ford, Li, Cook, & Choi, 2007). Moreover, according to 2007–2010 NHANES data, Latino adults have 0.60 higher odds of having a history of passing kidney stones, than other racial and ethnic minority groups in the United States (Juraschek, Miller, & Gelber, 2013). In relation to mental health, although Hispanics/Latinos in the US have a similar susceptibility to mental health illness as the general population, they have disparities in access to mental health treatment and in the quality of that treatment.
1.2 |. Theoretical approach
The biopsychosocial approach to racial health disparities emphasizes the examination of acute and chronic stressors associated with the experiences of perceived racism (Dressler, Oths, & Gravlee, 2005). For the purposes of this article, we will use Andersen, Clark, and Williams (2012) definition of racism, which refers to “beliefs, attitudes, institutional arrangements, and acts that tend to denigrate individuals or groups because of phenotypic characteristics or ethnic group affiliation…[it can be] held by or perpetuated by members of a different racial/ethnic group (intergroup racism) and by members of the same racial/ethnic group (intragroup racism)” (p. 79). It builds on the stress-coping model proposed by Lazarus and Folkman (1984) and Selye’s (1976) theory of stress on the hypothalamic-pituitary-adrenal axis.
Specifically, the biopsychosocial approach posits that there are physiological and psychological responses to stress from perceived racism (Anderson, McNeilly, & Myers, 1991; Andersen, Kiecolt-Glaser, & Glaser, 1994; Dressler et al., 2005), but also the material deprivation from institutionalized forms of racism can create negative health outcomes in racial and ethnic minorities (Krieger, 2012). Our perspective emphasizes the biobehavioral effects of stress associated with the experiences of racism from immigration enforcement policies targeting people of Latino- and Mexican-origin as forms of institutionalized racism (Aranda & Vaquera, 2015; Massey, 2015). Biospecimens are often used in biopsychosocial research of racial and ethnic health disparities to demonstrate how diverse acute and chronic stressors from institutionalized and interpersonal racial discrimination are related to physiological responses to stress and the etiology of chronic disease (Harrell et al., 2011). However, in comparison to other racial/ethnic groups, there has been little biopsychosocial research examining how Latinos, including Mexicans, embody racial discrimination (e.g., McClure et al., 2010), much less from the institutional racism emanating from immigration enforcement policies.
1.3 |. Present study
In the present study, we explore the relationship between household fear of deportation (FOD) and sUA in 30 families of Mexican-origin with at least one immigrant parent. We examine whether household FOD is associated with sUA levels in Mexican-origin, mixed-status families because the precarious nature of immigration detention and deportation is a form of unanticipated psychosocial stress (Arbona et al., 2010; Cavazos-Reg et al., 2007; De Genova, 2002) and UA has been found to be inversely associated with unanticipated stress (Rahe & Arthur, 1967; Rahe, Rubin, Arthur, & Clark, 1968; Zir et al., 1973) and fear (Lorenzi, Borba, Dutra, & Lara, 2010). Moreover, FOD may be associated with UA because UA is a regulator of hippocampal activity (HCA), or one’s emotional response to stress (Goodman et al., 2016). As such, people who report more household fear of deportation may have less UA regulating their emotional response to the stress of having their family members (or themselves) detained and/or deported by immigration authorities.
1.4 |. Methods
Data are from a cross-sectional exploratory study of Latino families, with at least one immigrant parent, to examine household fear of deportation in relation to anthropometric, demographic, psychosocial, and salivary analyte data. Families were recruited during the summer/fall of 2014. We employed cluster probability sampling—the research team recruited families by going door-to-door in 30 randomly selected census tracts, with a high location quotient of foreign-born Hispanics/Latinos between 1.8 and 3.5 (range 0.4–3.6).
Families were eligible if they self-identified as Hispanic/ Latino and had at least one parent who was a Latin American immigrant. We excluded families if the head of household was <18 years of age, or if the head of household was incapable of providing consent for themselves or their children. Following recommendations by Granger et al. (2012) we excluded families who had one family member that had just visited the dentist in the last 24 hours; smoked or chewed tobacco; had open mouth sores or abrasions; was ill with an acute condition or chronic disease or a had a fever. Certain medications can also affect UA levels (see Moriwaki, 2014 for review), so we also excluded families in which anyone was taking prescription or over-the-counter medications, including NSAIDs, hormonal contraceptives, or beta-blockers. After the head of household and individual family members consented to participate, we gave each family a $50 gift card. Children under the age of 6 provided oral assent and children older than 6 years provided written assent. The university Institutional Review Board approved this study.
1.5 |. Participants
Participants (N = 111) were members of 30 Mexican-origin, low-income families among whom 48% reported an annual family income of <$20,000/year. Given the demographic makeup of Latinos in the City of Phoenix, all of the participating families were Mexican-origin. The typical family size was three to four persons, with the largest family having eight persons. The average number of children in each home was two to three. Although these families were typically headed by a single-mother, half lived with a male partner, who may not have been the biological father of the child (ren). The majority of families identified as mestizo (Indian and White). Fourteen families reported one or more fears of being deported; with obtaining a driver’s license being the most commonly reported fear (23.3%) (See Table 1). In this sample, there were 65 females and 46 males, 65 were children (2 months-17 years, 49% female) and 46 adults (20–58 years, 71% female).
TABLE 1.
Family characteristics
| Families N = 30 | |
|---|---|
| Family Size [R, (M)] | 2–8 persons (4.2) |
| Number of Children | 1–6 children (2.3) |
| Years in USA [M ± SD] | 10.69 ± 7.49 |
| Years in Phoenix | 9.91 ± 6.75 |
| Race/Ethnicity | |
| White | 7 (23.3%) |
| Moreno (Black, Hispanic-origin) | 5 (16.7%) |
| Mestizo (Indian & White) | 11 (36.7%) |
| Zambo (Black & Indian) | 7 (23.3%) |
| Marital Status | |
| Married | 23 |
| Living w/partner | 3 |
| Divorced/Separated | 4 |
| Annual Family Income | |
| <$20,000 | 16 (53.5%) |
| $20,000–$34,999 | 11 (36.7%) |
| $35,000–$49,999 | 3 (10.0%) |
| Home Ownership | |
| Rent | 28 (93.3%) |
| Own | 2 (6.7%) |
| Fear of Deportation | |
| Walking in public | 2 (6.7%) |
| Seeking help from government agencies | 4 (13.3%) |
| Reporting incidents to the police | 3 (10%) |
| Reporting personal incidents to police | 3 (10%) |
| Reporting to court (even with a summons) | 2 (6.7%) |
| Obtaining a driver’s license | 7 (23.3%) |
| Waiting at the corner for work | 3 (10%) |
| Had ≥1 fear | 14 families (47%) |
1.6 |. Measures
Saliva Collection and Assay:
Following recommendations by Granger and colleagues (Granger et al., 2007, 2012), participants were instructed not to have consumed food or liquids, or brushed their teeth prior to an hour of providing samples and they rinsed their mouth with water 10 minutes prior to sample donation. We collected 1.0–1.8 mL of whole saliva from family members older than 6 years of age by passive drool. For the youngest children, ages 2 months-5 years, saliva was collected while they sat on their parent’s lap as a research assistant held a saliva collection swab in their mouth for three minutes. To confirm sample volumes were sufficient, children’s saliva was expressed immediately after collection from each swab using a 5cc needleless syringe. All samples were then frozen on dry ice and transported to the University where they were stored at –80°C until the day of assay.
On the day of assay, samples were thawed, centrifuged to remove mucins, and assayed in duplicate for sUA using a commercially available enzymatic reaction kit specifically designed for use with saliva (Salimetrics, Carlsbad, CA). The assay used 10 μl test volume, had a range of sensitivity from 0.78 to 25 mg/dl, and average inter- and intra-assay coefficients of variation were 10% and 5%. The average of the duplicate tests were used in the descriptive analyses and for the multilevel models to assess the measurement error.
Anthropometric Measures:
After collecting the saliva samples, we measured each family member’s weight with a SECA 876 Portable Scale and their height with a SECA Portable Stadiometer to calculate their BMI. We also measured the smallest part of their waist and the widest part of their hips with a Gulick II measuring tape to calculate waist-to-hip circumference ratio, to assess abdominal adiposity. The participants retained form-fitting clothing when we weighed and measured them, but took off their shoes and heavier clothing. All measures were recorded in metric units.
Survey Measures:
After collecting the salivary and anthropometric measures, we administered an 80-item questionnaire to the head of household in the language of their choice. We used a tablet-based, interviewer-administered survey that included demographic items on family composition, total annual household income, home ownership, language use in multiple contexts for all family members, self-rated health of each family member, and each family member’s health insurance status. We also queried the head of household’s current employment status, highest educational attainment, and Spanish/English literacy.
In order to assess the family’s ancestry, we first asked the head of household’s country of origin. If the head of household was US-born then we asked for the immigrant family member’s country of origin. We modified the race/ ethnicity item on the survey to include the four US Office of Management and Budget categories (i.e., “White non-Hispanic”) and the Latin American caste categories, which take into consideration racial inter-marriage. For example, persons of White and Black admixture self-identify as mulatto, those mixed with White and Indian identify as mestizo, those mixed with Indian and African descent identified as zambo, and those that identified as African descent were moreno (Candelario, 2007).
Social Support Scale:
The social support scale administered in this study was Boehnert, Bradshaw, and Latkin’s (2009) adaptation of the Arizona Social Support Inventory by Barrera and Gottlieb (1981). The scale consisted of six items discerning instrumental forms of social support along four dimensions: personal advice, informational, health, and financial support using a 5-point Likert-type scale (0 = Definitely not/4 = Definitely yes). The scale was administered by the first author in a cardiovascular risk assessment of Latina/o immigrants in Baltimore in 2011–2012 and had face and construct validity in that sample (Martínez, Juon, Levine, Lyford-Pike, & Peters, 2014) and in the present study, had a high Cronbach’s alpha (α = 0.84), indicating reliability.
Fear of Deportation Questionnaire:
To assess fear of deportation at the household level, we modified an existing seven-item questionnaire, the Fear of Deportation Questionnaire (α = 0.70) created by Arbona and colleagues at multiple Texas universities (2010). The fear of deportation questionnaire discerns if the respondent avoided seeking government services, attending court, reporting crimes done to others or oneself, or being in public for fear of deportation. Every affirmative answer receives a one point (0 = no avoidance of the activity for fear of deportation/1 = yes avoidance of the activity for fear of deportation) with a maximum of seven points. We modified the Arbona and colleagues fear of deportation questionnaire to a family-level variable by asking whether the respondent or someone in their family avoided the above activities for fear of deportation. For example, “Have you or someone in your family avoided asking for help from government agencies for fear of being deported?”
Arbona and colleagues sampled mostly Mexican and some Central America immigrants from two major cities in Texas. Arizona and Texas share similar histories and demographics as Southwestern borderland states with a strong presence of border patrol and primarily Mexican immigrants and Mexican Americans. Given that our sample in Phoenix is similar to the one in Arbona and colleagues’ study, we believe this questionnaire was culturally appropriate. An exploratory factor analysis revealed that all seven items had strong factor loadings (≥0.5) along two factors that explained 90% and 28% of the variance respectively (results not shown here).
1.7 |. Analytic strategy
To discern the relationship between sUA with household fear of deportation we estimated an exploratory multilevel mediation model in which age, gender, log BMI percentile and identifying as zambo predicted log mean SUA levels within families. At the second level we estimated whether household fear of deportation (FOD) predicted family’s log BMI percentiles and social support score, and in turn, sUA mean levels between families (see Figure 1). In order to account for the developmental and gender differences in sUA levels among family members (Martínez, Ruelas, & Granger, 2016), we estimated two additional models that utilized the difference of an individual’s mean sUA levels from the sample mean sUA level for their gender and age category (infants <2, early childhood 2–5, middle childhood 6–12, adolescence 13–18, and adulthood 191). We called this adjusted variable DiffsUA in the tables. We compared results between log mean sUA levels and the DiffsUA levels as an additional check of robustness.
FIGURE 1.
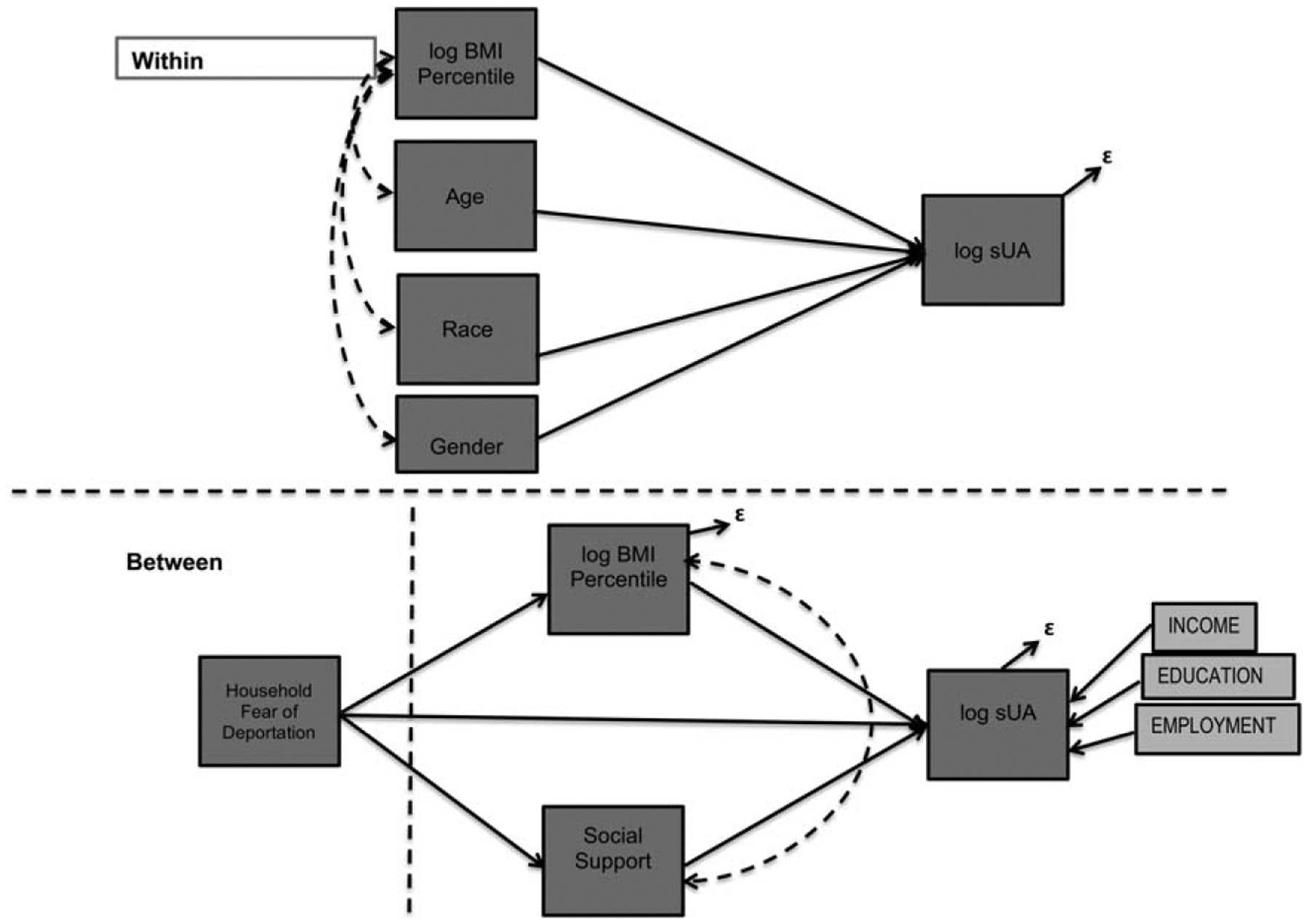
Exploratory Multilevel Mediation: Fear of Deportation in relation to BMI Percentile, Social Support, Socioeconomic Status and sUA
Since epidemiological studies report lower levels of serum UA in adults who have more social support (Thomas, Goodwin, & Goodwin, 1985), we examined whether social support mediated the effects of household FOD on mean sUA levels. Given that obesity is a key mediator in the pathway between stress-induced oxidative stress (Baldree & Stapleton, 1997; Epel, 2009) we also included it as a mediator between families, while controlling for socioeconomic proxies (e.g., total annual household income, head of household’s highest educational level, and employment status) as covariates of sUA. The proxies for household socioeconomic status were not estimated as covariates of household fear of deportation because they were not strongly correlated (See Table 2).
TABLE 2.
Correlations between natural log of mean sUA levels and study covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. LsUA | - | ||||||||||
| 2. sUADiff | 0.80** | - | |||||||||
| 3. LBMI Percentile | 0.28** | 0.24** | - | ||||||||
| 4. BMI Percentile | 0.18* | 0.12 | 0.43** | - | |||||||
| 5. Age | 0.15 | 0.07 | 0.75** | 0.04 | - | ||||||
| 6. Fear of Deportation | −0.31** | −0.27** | −0.17* | −0.02 | −0.16* | - | |||||
| 7. Social Support | −0.12 | −0.18* | −0.15 | −0.20** | 0.17* | 0.08 | - | ||||
| 8. Income | −0.14 | −0.14 | 0.09 | 0.06 | 0.17* | 0.07 | 0.39** | - | |||
| 9. Un/Employmenta | 0.09 | −0.06 | 0.17* | 0.01 | 0.18* | −0.08 | 0.12 | 0.31** | - | ||
| 10. Educational Level | 0.18* | 0.01 | 0.13 | −0.03 | 0.10 | 0.17* | 0.11 | 0.08 | 0.24** | - | |
| 11. Genderb | 0.02 | 0.03 | 0.19** | 0.04 | 0.15 | −0.21** | −0.03 | 0.03 | 0.02 | −0.11 | - |
| 12. Blackc | −0.14 | −0.13 | −0.04 | −0.13 | 0.04 | 0.12 | 0.02 | 0.09 | 0.08 | −0.07 | 0.08 |
| 13. Mestizoc | −0.17 | −0.18* | 0.01 | 0.26** | −0.12 | 0.07 | 0.04 | 0.04 | 0.22** | 0.07 | −0.05 |
| 14. Morenoc | −0.04 | 0.04 | 0.01 | −0.04 | 0.04 | 0.13 | 0.08 | 0.24** | 0.07 | 0.15 | −0.16 |
| 15. Zamboc | 0.18* | 0.18* | −0.01 | −0.08 | −0.12 | −0.23** | −0.24** | −0.35** | −0.25** | 0.09 | 0.03 |
Employment (0 = Unemployed, 1 = employed ≥20 hours/week).
Gender (0 = Male, 1 = Female).
Spearman rank correlation.
L: log transformation.
Diff sUA: (Individual sUA levels – age-and-gender-specific mean sUA level).
P<.05,
P<.10.
With regard to controlling for adiposity within families, we estimated the model using individual BMI percentiles, as designated by the Centers for Disease Control (Flegal et al., 2010; Kuczmarski et al., 2000) instead of raw BMI scores because the standards that designate normal, overweight and obese are different between children and adults, and are age- and-gender-specific among children. Since there was very little variance in waist-to-hip circumference ratio (0.97 ± 0.04 cm2), this variable was excluded from the within-level models (Table 3). Since mean sUA levels were positively skewed, we used the natural log transformation for statistics where a normal distribution was needed. The adjusted variable, DiffsUA, was normally distributed and did not require transformation. The models were estimated using full information maximum likelihood (Enders, 2010) and the fit between the model and observed data was acceptable (i.e., CFI was greater than .95 (.90), RMSEA was less than .05 (.08), and SRMR was less than (.05). Descriptive statistics were conducted using Stata 12.1, and multilevel mediation models were estimated using MPlus 7.2.
TABLE 3.
Anthropometric measures and sUA levels by age and gender, N = 111
| Age | <2 years | 2–5 years | 6–12 years | 13–18 years | 19+ years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | M | F | M | F | M | F | M | F | M | F |
| N | 4 | 3 | 9 | 12 | 12 | 12 | 8 | 5 | 13 | 33 |
| BMI (kg/m2) | 18.34 ± 4.00 | 18.34 ± 2.55 | 15.94 ± 1.57 | 18.44 ±3.64 | 20.05 ± 5.26 | 19.08 ± 4.63 | 23.5 ± 5.80 | 20.98 ± 3.84 | 29.98 ± 2.37a | 32.51 ± 7.76 |
| [M ± SD] (Range) | (16.0–24.3) | (15.4–20.1) | (13.8–18.3) | (13.1–25.8) | (14.3–32.2) | (15.4–31.2) | (18.8–37.1) | (16.4–25.8) | (26.3–34.9) | (20.1–50) |
| BMI Percentilea,b | 0.43 ± 0.38 | 0.82 ± 0.23 | 0.55 ± 0.36 | 0.73 ± 0.33 | 0.71 ± 0.32 | 0.71 ± 0.21 | 0.66 ± 0.17 | 0.59 ± 0.41 | 0.70 ± 0.20 | 0.71 ± 0.23 |
| [M ± SD] (Range) | (0.13–0.99) | (0.55–0.97) | (0.02–0.95) | (0.03–0.99) | (0.04–0.99) | (0.39–0.99) | (0.45–0.99) | (0.05–0.94) | (0.23–0.93) | (0.19–0.99) |
| Waist:Hip(cm) | 0.99 ± 0.04 | 0.96 ± 0.03 | 0.95 ± 0.05 | 0.95 ± 0.06 | 0.92 ± 0.07 | 0.87 ± 0.05 | 0.91 ± 0.07 | 0.86 ± 0.04 | 0.97 ± 0.04 | 0.87 ± 0.06 |
| [M ± SD] (Range) | (0.932–1.02) | (0.927–0.98) | (0.89–1.03) | (0.86–1.06) | (0.79–1.02) | (0.79–0.99) | (0.79–0.98) | (0.81–0.90) | (0.92–1.06) | (0.69–1.02) |
| sUA (pg/mL) | 2.12 ± 0.98 | 1.11 ± 0.68 | 2.06 ± 1.35 | 3.09 ± 1.09a | 1.52 ± 1.03 | 1.53 ± 1.12 | 1.98 ± 1.30 | 1.51 ± 0.75 | 3.10 ± 2.00 | 2.17 ± 1.29 |
| [M ± SD] (Range) | (1.31–3.51) | (0.46–1.82) | (0.70–5.09) | (1.18–5.34) | (0.37–4.04) | (0.35–4.38) | (0.096–3.81) | (0.80–2.72) | (0.81–7.86) | (0.41–5.45) |
Descriptive statistics calculated in Stata 12.1.
Body Mass Index (BMI).
M (Male) F (Female).
CDC/NCHS age-sex-specific growth charts youth 2–20 years of age, available at: http://www.cdc.gov/nccdphp/dnpa/growthcharts/training/modules/module2/text/module2print.pdf.
Adult BMI percentiles based on NHANES 2007–2008 data available at: https://www.cdc.gov/nchs/data/hestat/obesity_adult_07_08/obesity_adult_07_08.pdf.
2 |. RESULTS
Individual log mean sUA levels were correlated with log BMI (ρ = 0.28, P < .05) and marginally related to BMI percentiles (ρ = 0.18, P = .06), identification as zambo (ρ = 0.18, P < .10), and educational level (ρ = 0.18, P < .10). There were inverse relationships between household fear of deportation (FOD) with the main dependent variables, individual log mean sUA levels (ρ= −0.31, P < .05) and the different mean age-gender-specific sUA levels (DiffsUA: ρ= −0.27, P < .05). Household fear of deportation was also inversely related to identifying as zambo (ρ= −0.23, P < .05) and male (ρ = 20.25, P < .05) (See Table 2).
Before running our comprehensive multilevel models, we conducted further exploratory analyses on some variables in relationship to individual log BMI percentiles and log mean sUA levels. First, we examined the relationship between each fear of deportation dimension (e.g., fear of being in public, seeking help from government agencies, obtaining a driver’s license, reporting infractions to the police, and going to court) in relation to individual BMI percentiles and mean sUA levels to discern whether this inverse relationship was present among all items. Five of the seven fear of deportation items were inversely related to BMI percentile and sUA levels.
Second, we decided to estimate racial self-identification at the within- instead of between-family level because some family members did not identify with the same race/ethnicity as their kin. The multilevel model that included all of the individual race/ethnicity categories did not converge, so we estimated the model with each race/ethnicity category separately. Third, we examined whether time in the US or Phoenix was related to any of the anthropometric measures, social support, and household fear of deportation. Time in the US and time in Phoenix were not significantly related to BMI, BMI percentiles, sUA levels, or fear of deportation, so they were excluded from the multilevel models (analyses not shown here).
In the comprehensive multilevel model (Table 4, Model 1), an individual family member’s age, log BMI percentile, gender, or race/ethnicity, were not related to another family member’s log sUA levels within families. Social support was not related to log mean sUA levels (β = 0.01, P = .99) between families, nor was the presence of social support related to other variables’ relationship to log mean sUA levels. Between families, household FOD was inversely related to log BMI percentiles (β= −0.04, P = .03) and log mean sUA levels (β= −0.12, P = .02), after controlling for the head of household’s education and employment status and total household annual income (Table 4, Model 1). In the comprehensive model with DiffsUA as the dependent variable, family BMI percentile was not related to sUA or household FOD (Table 4, Model 4).
TABLE 4.
Exploratory Multilevel Models of household fear of deportation in relation to salivary uric acid (sUA) in Mexican-origin families
| Model 1 | Model 2 | Model 3 | Within Y=Diff sUAd | Model 4 | Model 5 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Within Y=LsUAc | β | SE | P | β | SE | p | β | SE | P | β | SE | P | β | SE | P | |||
| Age | 0.003 | 0.004 | .45 | 0.003 | 0.004 | .43 | Age | −0.02 | 0.17 | .90 | −0.06 | 0.16 | .68 | |||||
| Gendera | −0.11 | 0.14 | .42 | −0.11 | 0.14 | .44 | Gender | −0.14 | 0.10 | .17 | −0.11 | 0.10 | .26 | |||||
| LBMIP | 0.31 | 0.26 | .23 | 0.30 | 0.26 | .24 | 0.30 | 0.29 | .29 | BMIP | 0.08 | 0.20 | .71 | 0.08 | 0.19 | .67 | ||
| Zambo | 0.08 | 0.15 | .41 | 0.10 | 0.14 | .48 | Zambo | −0.02 | 0.12 | .95 | ||||||||
| RV = 0.42 | RV=0.42 | RV=0.44 | RV=0.98 | RV=0.98 | ||||||||||||||
| Between§ Y=LsUA | β | SE | P | β | SE | P | β | SE | P | Between§ Y=Diff sUA | β | SE | P | β | SE | P | ||
| Social Support | 0.01 | 0.16 | .99 | Social Support | 0.03 | 0.43 | .94 | |||||||||||
| Household Fear of Deportation | −0.12 | 0.05 | .02 | −0.12 | 0.05 | .02 | −0.09 | 0.05 | .05 | Household Fear of Deportation | −0.68 | 0.27 | .01 | −0.63 | 0.25 | .01 | ||
| LBMIP | 1.23 | 0.78 | .11 | 1.28 | 0.72 | .07 | 1.85 | 0.81 | .02 | BMIP | 0.59 | 0.56 | .29 | 0.71 | 0.36 | .05 | ||
| Education | 0.12 | 0.05 | .02 | 0.13 | 0.05 | .01 | Education | 0.17 | 0.22 | .46 | ||||||||
| Income | −0.42 | 0.30 | .09 | −0.16 | 0.10 | .11 | Income | −0.31 | 0.31 | .31 | ||||||||
| Employmentb | 0.15 | 0.25 | .47 | Employment | −0.14 | 0.27 | .60 | |||||||||||
| Y=BMIP | RV = 0.001 | RV=0.001 | RV=0.001 | Y=BMIP | RV=0.05 | RV=0.05 | ||||||||||||
| Social Support | 0.10 | 0.68 | .95 | Social Support | 0.16 | 0.14 | .26 | |||||||||||
| Household Fear of Deportation | −0.04 | 0.02 | .03 | −0.04 | 0.02 | 0.05 | Household Fear of Deportation | −0.06 | 0.20 | .78 | ||||||||
| RV = 0.01 | RV 0.01 | RV 0.01 | RV=0.05 | |||||||||||||||
Between families, as in Figure 1.
β= beta coefficient RV = Residual Variance.
SE = standard error P = P-value.
Gender (0 = Male, 1 = Female).
Head of Household Employment (0 = Unemployed, 1 = employed ≥20 hours/week).
Natural log transformation for sUA.
Diff sUA: (Individual sUA level – age category-and-gender-specific mean sUA level).
In Model 2, we omitted social support as a mediating variable between household FOD and log mean sUA levels. We also excluded the head of household’s employment status as a covariate of log mean sUA levels because of its low correlation (ρ = 0.09, Table 2) and high P-value (P = .47, Table 4, Model 1). Similar to Model 1, an individual family member’s age, BMI percentile, gender, or race/ethnicity are not related to another family member’s log sUA levels within families. In the absence of social support and the head of household’s employment status, the association between household FOD and log BMI percentile on family’s log mean sUA levels were similar to Model 1.
In Model 3, we examine the total direct and total indirect effect of household FOD and log BMI percentiles between families to determine whether BMI percentile is a mediator between household FOD and log mean sUA levels. Age, gender, and self-identifying as zambo were omitted because of their weak beta coefficients and high p-values within families’ sUA levels. The total direct effect of household fear of deportation on log mean sUA levels was significant (β= −0.17, P < .01). The estimate of the direct effect between household FOD and log mean sUA levels declined (γxy= −0.09, P < .05) as the estimated paths for indirect effects (βxz= −0.04, P = .04, γzy = 1.85, P = .02) increased (Figure 2). Log BMI percentile appears to be a partial mediator for the relationship between household FOD and log mean sUA levels between families of Mexican-origin, as the direct path between household FOD and sUA levels remained significant (Table 4, Model 3). Between families, for every item answered affirmatively on the FOD questionnaire, log BMI percentile decreased by 4%, in turn, decreasing log mean sUA levels by 15%. Nevertheless, in comparing Model 2 to Model 3, lower annual household income and head of household’s higher educational attainment strengthened the direct effect of household FOD on log mean sUA levels (β= −0.12, P = .02 vs. β= −0.09, P = .05), and weakened the effect of family’s log BMI percentile on log mean sUA levels between families (β = 1.28, P = .07 vs. β = 1.85, P = 0.02) (Table 4, see Models 2 and 3).
FIGURE 2.
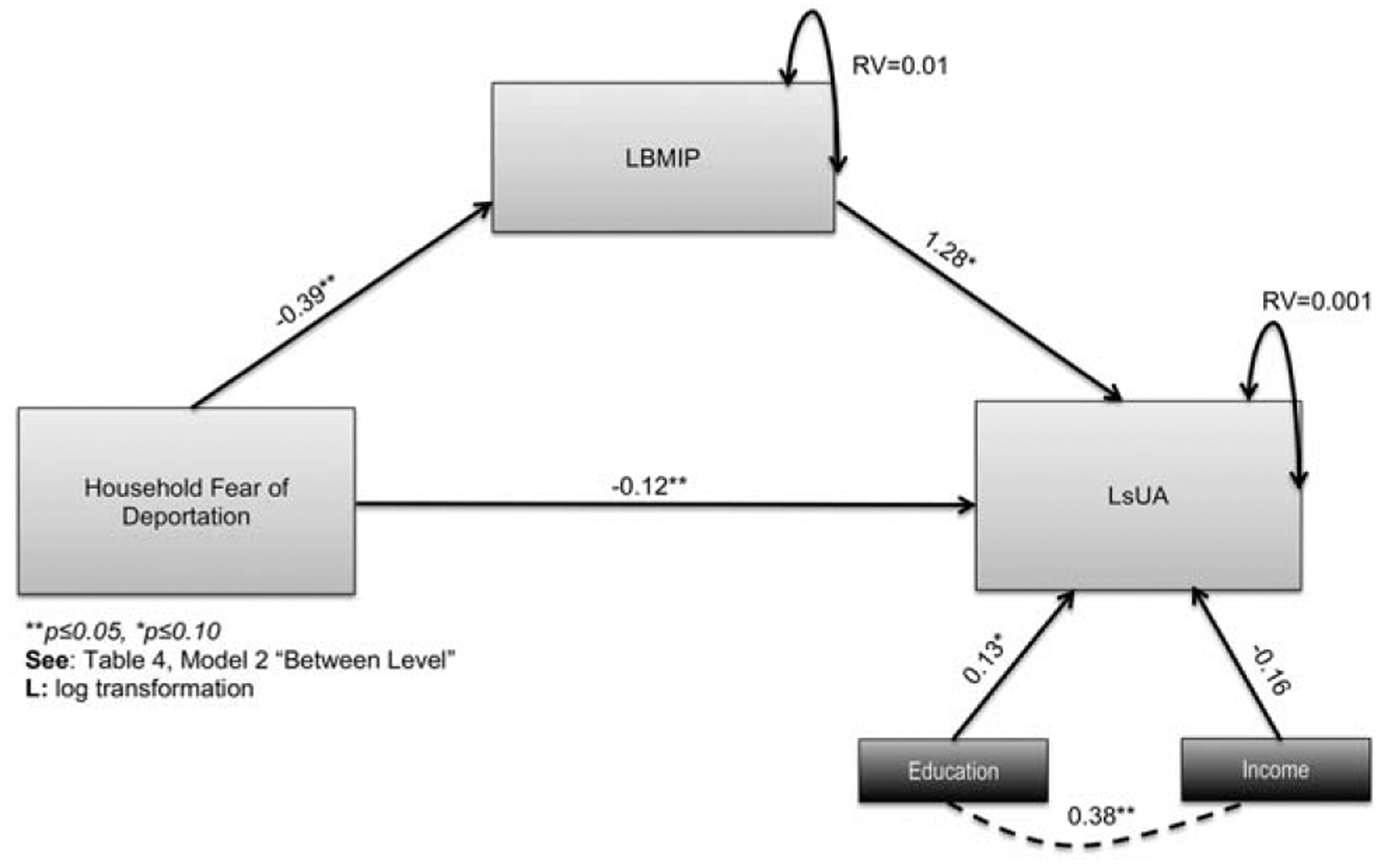
Exploratory Multilevel Mediation of Household Fear of Deportation in relation to BMI Percentile and sUA between Mexican-origin Families
However, when we examine the adjusted DiffsUA results, family BMI percentile is not a mediator between household FOD and sUA levels because they are not related to one another (βxz= −0.06, P = .78). Even with the adjustment of individual and family sUA levels to reflect developmental- and gender-specific differences between family members, we find that BMI percentile (β = 0.71, P = .05) and household FOD (β= −0.63, P = 0.01) continue to be related to differences in sUA levels between families (see Table 4, Model 5).
The residual variance for both log BMI percentiles (RV = 0.01, P = .23) and log mean sUA levels (RV = 0.001, P = .99) in Model 3 were low and insignificant, indicating that household FOD and BMI percentile account for much of the variance in log sUA levels between families, even after controlling for socioeconomic indicators and social support. Nevertheless, other variables are worth exploring in understanding the relationship between household fear of deportation, BMI percentiles and sUA levels, which we will discuss below. The final mediation model (Table 4, Model 3) and adjusted DiffsUA model (Table 4, Model 5) showed good model fit with an RMSEA = 0.00, CFI/TLI = 1.00, and SRMRwithin =0.000, SRMRbetween =0.000
3 |. DISCUSSION
In a multilevel analysis with families as the main unit of analysis, we consistently found that more psychosocial stress from household fear of deportation was related to lower BMI percentiles and lower sUA levels between families. These findings support prior research finding adverse health effects from fear of immigration enforcement policies (Aranda & Vaquera, 2015; Arbona et al., 2010; Cavazos-Rehg et al., 2007; Vargas, Sanchez, & Juárez, 2017). Similar to extant research finding lower levels of UA in relation to fear (Lorenzi et al., 2010) and unanticipated stress (Rahe & Arthur, 1967; Rahe et al., 1968; Zir et al., 1973), we found that more household fear of deportation was related to lower sUA levels between families. However, we are cautious to relegate causality to these findings because sUA is also mediated by health behaviors and material conditions; there are several factors that need to be taken into consideration when interpreting these results.
First, we found that more household fear of deportation was related to lower BMI percentiles between families. There are studies that demonstrate that anxiety and enduring negative emotional situations are strongly related to undereating and unconscious appetite (Macht, 2008). It is possible that fear of deportation of another family member or oneself, along with other stressors related to migrant illegality (De Genova, 2002), may lead to negative emotions that suppress appetite. Moreover, persons living in homes reporting more fear of deportation may also have fewer material resources. Given that undocumented immigrants are unauthorized to work, have a driver’s license (with the exception of DACA recipients), or participate in publicly-funded welfare programs (e.g., SNAP) in Arizona, they may have less disposable income to buy food, partly explaining the lower BMI percentiles in these families.
Related to the lower BMI percentiles, Mexican-origin families often live in “entrapped communities” (Nuñez & Heyman, 2007) to avoid chronic surveillance from police and immigration enforcement. These communities tend to have fewer retail food environments (Nuñez & Heyman, 2007; Sharkey & Dean, 2012). Therefore, state immigration policies may indirectly shape food environments, healthy food access, purchasing behaviors and dietary practices. Future studies should inquire about food security, participation in food assistance programs, and the proportion of household income used toward food in order to provide a comprehensive examination of the social determinants of BMI percentiles in mixed-status families in relationship to household fear of deportation.
Second, in this study social support was not related to household fear of deportation or sUA levels, despite other research (Thomas et al., 1985) finding that stronger social support was related to lower serum UA levels, independent of age and weight. For the future, we will consider examining whether other protective factors may mitigate the effect of fear of deportation on salivary biomarkers, such as religious coping (Read-Wahidi & DeCaro, 2017) and civic engagement. The social support scale we used may not capture other ways that members of mixed-status Latino families receive support from others in the context of restrictions shaped by local immigration enforcement policies.
Third, individual serum UA levels can increase after vigorous exercise, the consumption of alcohol, purine-rich proteins, and fructose (Choi, Ford, Gao, & Choi, 2008; Choi et al., 2005; Viazzi, Genovesi, Ambruzzi, and Giussani, 2015), and decreases with the consumption of dairy in adults (Choi et al., 2005) and breast milk in infants (Kuchan, Ostrom, Smith, & Hu, 2000). Given the strong association between serum and salivary UA levels, it is possible that sUA levels are also influenced by diet. Logistical and practical constraints coordinating home visits with these families made it difficult to expect families in the study to fast before saliva collection. Nevertheless, an inclusion criterion was for no participant to have consumed food or beverages, other than water, the hour before we collected the first saliva sample. For future studies of sUA, it would be valuable to incorporate diet quality data, require participants to fast, or both.
3.1 |. Limitations
Some of the limitations include the small sample size, the lack of longitudinal data, and the lack of established population means for sUA in children and adults. This was a cross-sectional study, and we need longitudinal data to ascertain: (i) at what point immigration enforcement policies are considered anticipated stressors by mixed-status families, and (ii) at what point sUA manifests reduced hippocampal activity or chronic disease. One limitation of using the difference of an individual’s sUA levels from the sample mean sUA level for their gender and age category is that, unlike body mass index, there are no population-based studies documenting mean sUA levels in adults or children. We are one of the first researchers examining this novel salivary biomarker. Ideally, we would compare the distribution of sUA in our sample to the ones in the population to account for the developmental differences in the family sUA levels in the multilevel model.
3.2 |. New contribution to the literature
We address recent requests to examine how immigration enforcement policies are related to the health outcomes (Hardy et al., 2012; Martinez et al., 2015; Rhodes et al., 2015) of family members living with unauthorized immigrants, such as children in mixed-status households (Landale et al., 2015; Suro et al., 2015). We also contribute to the biopsychosocial approach to racial disparities by demonstrating that household fear of deportation may also be related to biobehavioral health, through sUA. In conclusion, the relationship between household fear of deportation and physiological health outcomes between families is complex, and must take into consideration anthropometric, demographic, and socio-environmental variables.
ACKNOWLEDGMENTS
We would like to thank the laboratory staff at the Institute for Interdisciplinary Salivary Bioscience Research and the reviewers who provided valuable feedback on this manuscript. We also would like to thank the families who participated in this study, and Salimetrics for the donation of some of the reagents.
Funding information This project received funding from the ASU College of Liberal Arts and Sciences Seed Funding Mechanism, the Program for Transborder Communities seed grant, and the NIH Loan Repayment Program 2018-2020 (L60 MD011867).
Footnotes
DISCLOSURE STATEMENT
In the interest of full disclosure we note that DAG is the founder and chief scientific and strategy advisor at Salimetrics LLC and Salivabio LLC and that the nature of these relationships is managed by the policies of the committees on conflict of interest at the Johns Hopkins University School of Medicine and the University of California at Irvine.
REFERENCES
- Andersen BL, Kiecolt-Glaser JK, & Glaser R (1994). A biobehavioral model of cancer stress and disease course. American Psychologist, 49(5), 389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson NB, McNeilly M, & Myers H (1991). Autonomic reactivity and hypertension in Blacks: A review and proposed model. Ethnicity and Disease, 1(2), 154–170. [PubMed] [Google Scholar]
- Aranda E, & Vaquera E (2015). Racism, the immigration regime, and the implications for racial inequality in the lives of undocumented young adults. Sociology of Race and Ethnicity, 1, 88–104. [Google Scholar]
- Arbona C, Olvera N, Rodriguez N, Hagan J, Linares A, & Wiesner M (2010). Acculturative stress among undocumented Latino immigrants in the United States. Hispanic Journal of Behavioral Sciences, 32(3), 362–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbacher K, O’donovan A, Wolkowitz OM, Dhabhar FS, Su Y, & Epel ES (2013). Good stress, bad stress and oxidative stress: Insights from anticipatory cortisol reactivity. Psycho-neuroendocrinology, 38(9), 1698–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldree LA, & Stapleton FB (1997). Uric acid metabolism in children. Pediatric Clinical Nutrition of America, 37(1), 391–418. [DOI] [PubMed] [Google Scholar]
- Barrera MJ, & Gottlieb BH (1981). Social support in the adjustment of pregnant adolescents: Assessment issues In Gottlieb BH (Ed.), Social networks and social support (pp. 69–96). [Google Scholar]
- Beverly Hills CA: Sage Publications. Becerra D, Androff D, Cimino A, Wagaman MA, & Blanchard KN (2013). The impact of perceived discrimination and immigration policies upon perceptions of quality of life among Latinos in the United States. Race and Social Problems, 5(1), 65–78. [Google Scholar]
- Boehnert A,SB, Bradshaw CP, & Latkin CA (2009). A social network perspective on heroin and cocaine use among adults: Evidence of bidirectional influences. Addiction, 104(7), 1210–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candelario GEB (2007). Color matters: Latina/o racial identities and life chances In Flores J & Rosaldo R (Eds.), A companion to Latina/O studies (pp. 337–350). Malden, MA: Blackwell Publishing. [Google Scholar]
- Cavazos-Rehg PA, Zayas LH, & Spitznagel EL (2007). Legal status, emotional well-being and subjective health status of Latino immigrants. Journal of the National Medical Association, 99(10), 1126. [PMC free article] [PubMed] [Google Scholar]
- Choi HK, Liu S, & Curhan G (2005). Intake of purine-rich foods, protein, and dairy products and relationship to serum levels of uric acid: The Third National Health and Nutrition Examination Survey. Arthritis & Rheumatism, 52(1), 283–289. [DOI] [PubMed] [Google Scholar]
- Choi JWJ, Ford ES, Gao X, & Choi HK (2008). Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: The Third National Health and Nutrition Examination survey. Arthritis Care & Research, 59(1), 109–116. [DOI] [PubMed] [Google Scholar]
- Clark R, Andersen NB, Clark VR, & Williams DR (2012). Racism as a stressor for African Americans: A biopsychosocial approach In LaVeist TA & Isaac LA (Eds.), Race, ethnicity and health: A public health reader. (pp. 79–103). San Francisco: Jossey-Bass. [Google Scholar]
- Cook S, Weitzman M, Auinger P, Nguyen M, & Dietz WH (2003). Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988–1994. Archives of Pediatric Adolescent Medicine, 15(3), 821–827. [DOI] [PubMed] [Google Scholar]
- De Genova N (2002). Migrant “illegality” and deportability in everyday life. Annual Review of Anthropology, 31(1), 419–447. [Google Scholar]
- De Oliveira EP, & Burini RC (2012). High plasma uric acid concentration: Causes and consequences. Diabetes and Metabolic Syndrome, 4(1), 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Oliveira EP, Moreto F, Silveira LV, & Burini RC (2013). Dietary, anthropometric, and biochemical determinants of uric acid in free-living adults. Nutrition Journal, 12, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler W, Oths KS, & Gravlee CC (2005). Race and ethnicity in public health research: Models to explain health disparities. American Review of Anthropology, 34, 231–252. [Google Scholar]
- Enders CK (2010). Applied missing data. New York: The Guilford Press. [Google Scholar]
- Epel ES (2009). Psychological and metabolic stress: A recipe for accelerated cellular aging? Hormones, 8(1), 7–22. [DOI] [PubMed] [Google Scholar]
- Executive Order, No. 13767. 82 FR 8793. Border Security and Immigration Enforcement Improvements 25 January 2017. [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, & Curtin LR (2010). Prevalence and trends in obesity among US adults, 1999–2008. Journal of the American Medical Association, 303, 235–241. [DOI] [PubMed] [Google Scholar]
- Ford ES, Li C, Cook S, & Choi HK (2007). Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation, 115(19), 2526–2532. [DOI] [PubMed] [Google Scholar]
- Goodman AM, Wheelock MD, Harnett NG, Mrug S, Granger DA, & Knight DC (2016). The hippocampal response to psychosocial stress varies with salivary uric acid level. Neuroscience, 339, 396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorodischer R, Burtin P, Hwang P, Levine M, & Koren G (1994). Saliva versus blood sampling for therapeutic drug monitoring in children: Patient and parental preferences and an economic analysis. Therapeutic Drug Monitor, 16(5), 437–443. [DOI] [PubMed] [Google Scholar]
- Granger DA, Fortunato CK, Beltzer EK, Virag M, Bright MA, & Out D (2012). Focus on methodology: Salivary bioscience and research on adolescence: An integrated perspective. Journal of Adolescence, 35(4), 1081–1095. [DOI] [PubMed] [Google Scholar]
- Granger DA, Kivlighan KT, Fortunato C, Harmon AG, Hibel LC, Schwartz EB, & Whembolua GL (2007). Integration of salivary biomarkers into developmental and behaviorally-oriented research: Problems and solutions for collecting specimens. Physiology & Behavior, 92(4), 583–590. [DOI] [PubMed] [Google Scholar]
- Hardy LJ, Getrich CM, Quezada JC, Guay A, Michalowski RJ, & Henley E (2012). A call for further research on the impact of state-level immigration policies on public health. American Journal of Public Health, 102(7), 1250–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell JP, Burford TI, Cage BN, Nelson TM, Shearon S, Thompson A, & Green S (2011). Multiple pathways linking racism to health outcomes. DuBois Review: Social Science Research on Race, 8(1), 143–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes LM, & Marcelli EA (2012). Neighborhoods and systemic inflammation: High CRP among legal and unauthorized Brazilian migrants. Health & Place, 18(3), 683–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishizaka Y, Yamakado M, Toda A, Tani M, & Ishizaka N (2014). Relationship between serum uric acid and serum oxidative stress markers in the Japanese general population. Nephron Clinical Practice, 128(1–2), 49–56. [DOI] [PubMed] [Google Scholar]
- Jones DP, Richey PA, Alpert BS, & Li R (2008). Serum uric acid and ambulatory blood pressure in children with primary hypertension. Pediatric Research, 64(5), 556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juraschek SP, Miller ER, & Gelber AC (2013). Body mass index, obesity, and prevalent gout in the United States in 1988–1994 and 2007–2010. Arthritis Care & Research, 65(1), 127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalil A, & Chen J (2008). “Mother’s citizenship status and household food insecurity among low-income children of immigrants” In Yoshikawa Hand Way N, (Eds.) “Beyond the Family: Contexts of Immigrant Children’s Development.” New Directions for Child and Adolescent Development, 121, 43–62. [DOI] [PubMed] [Google Scholar]
- Kasl SV, Gore S, & Cobb S (1975). The experience of losing a job: Reported changes in health, symptoms and illness behavior. Psychosomatic Medicine, 37(2), 106–122. [DOI] [PubMed] [Google Scholar]
- Kaur J, Lamb MM, & Ogden CL (2015). The association between food insecurity and obesity in children—The National Health and Nutrition Examination Survey. Journal of the Academy of Nutrition and Dietetics, 115(5), 751–758. [DOI] [PubMed] [Google Scholar]
- Kesebir S, Yaylacı ET, Süner Ö, & Gültekin BK (2014). Uric acid levels may be a biological marker for the differentiation of unipolar and bipolar disorder: The role of affective temperament. Journal of Affective Disorders, 165, 131–134. [DOI] [PubMed] [Google Scholar]
- Krieger N (2012). Methods for the scientific study of discrimination and health: An ecosocial approach. American Journal of Public Health, 102(5), 936–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuchan MJ, Ostrom KM, Smith C, & Hu PE (2000). Influence of purine intake on uric acid excretion in infants fed soy infant formulas. Journal of the American College of Nutrition, 19, 16. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei Z, … Johnson CL (2000). CDC growth charts: United States. Advance Data, 314, 1–27. [PubMed] [Google Scholar]
- Landale NS, Hardie JH, Oropesa RS, & Hillemeier MM (2015). Behavioral functioning among Mexican-origin children does parental legal status matter? Journal of Health and Social Behavior, 56(1), 2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping. New York: Springer. [Google Scholar]
- Lorenzi TM, Borba DL, Dutra G, & Lara DR (2010). Association of serum uric acid levels with emotional and affective temperaments. Journal of Affective Disorders, 121(1), 161–164. [DOI] [PubMed] [Google Scholar]
- Lyngdoh T, Bochud M, Glaus J, Castelao E, Waeber G, Vollenweider P, & Preisig M (2013). Associations of serum uric acid and SLC2A9 variant with depressive and anxiety disorders: A population-based study. PloS One, 8(10), e76336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macht M (2008). How emotions affect eating: A five-way model. Appetite, 50(1), 1–11. [DOI] [PubMed] [Google Scholar]
- McClure HH, Snodgrass JJ, Martínez CR, & Eddy JM (2013). Integrating biomarkers into research with Latino immigrants in the United States. Advances in Anthropology, 3, 112–120. [Google Scholar]
- McClure HH, Snodgrass JJ, Martinez CR, Eddy JM, Jiménez RA, & Isiordia LE (2010). Discrimination, psychosocial stress, and health among Latin American immigrants in Oregon. American Journal of Human Biology, 22(3), 421–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña L, & Lee E (2013). Latino politics and Arizona’s immigration law SB 1070. New York: Springer. [Google Scholar]
- Martínez AD, Juon HS, Levine DM, Lyford-Pike V, & Peters S (2014). The association between nutrition transition score and measures of obesity: Results from a cross-sectional study among Latina/o immigrants in Baltimore. Globalization and Health, 10(1), 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez AD, Ruelas L, & Granger DA (2016). Association between body mass index and salivary uric acid among Mexican-origin infants, youth and adults: Gender and developmental differences. Developmental Psychobiology, 59(2), 225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Wu E, Sandfort T, Dodge B, Carballo-Dieguez A, Pinto R, … Chavez-Baray S (2015). Evaluating the impact of immigration policies on health status among undocumented immigrants: A systematic review. Journal of Immigrant and Minority Health, 17(3), 947–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey D (2015). The real hispanic challenge. Pathways: A magazine on poverty, inequality, and social policy. Volume 7 (Spring), 3–7. [Google Scholar]
- Mellen PB, Bleyer AJ, Erlinger TP, Evans GW, Nieto FJ, Wagenknecht LE, … Herrington DM (2006). Serum uric acid predicts incident hypertension in a bi-ethnic cohort: The atherosclerosis risk in communities in communities study. Hypertension, 49, 1037–1042. [DOI] [PubMed] [Google Scholar]
- Moriwaki Y (2014). Effects on uric acid metabolism of the drugs except the anti-hyperuricemics. Journal of Bioequivalence & Bio-availability, 6(1), 10. [Google Scholar]
- Moya-Salas L, Ayón C, & Gurrola M (2013). Estamos traumados: The effect of anti-immigrant sentiment and policies on the mental health of Mexican immigrant families. Journal of Community Psychology, 41(8), 1005–1020. [Google Scholar]
- Mueller EF, Kasl SV, Brooks G, & Cobb S (1970). Psychosocial correlates of serum urate levels. Psychological Bulletin, 73 (4), 238. [DOI] [PubMed] [Google Scholar]
- Nuñez GG, & Heyman JM (2007). Entrapment processes and immigrant communities in a time of heightened border vigilance. Human Organization, 66(4), 354–265. [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA, 307(5), 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overview of the CDC Growth Charts. Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health Examination statistics. Retrieved from http://www.cdc.gov/nccdphp/dnpa/growthcharts/training/modules/module2/text/module2 [Google Scholar]
- Rahe RH, & Arthur RJ (1967). Stressful underwater demolition training: Serum urate and cholesterol variability. JAMA, 202, 1052–1054. [PubMed] [Google Scholar]
- Rahe RH, Rubin RT, Arthur RJ, & Clark BR (1968). Serum uric acid and cholesterol variability: A comprehensive view of underwater demolition team training. JAMA, 206, 2875–2880. [PubMed] [Google Scholar]
- Read-Wahidi MR, & DeCaro JA (2017). Guadalupan devotion as a moderator of psychosocial stress among Mexican immigrants in the rural Southern United States. Medical Anthropology Quarterly. DOI: 10.1111/maq.12372. [DOI] [PubMed] [Google Scholar]
- Rhodes S, Mann L, Siman FM, Song E, Alonzo J, Downs M, … Hall M. (2015). The impact of local immigration enforcement policies on the health of immigrant Hispanic/Latinos in the United States. American Journal of Public Health, 105(2), 329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez MA, Young M, & Wallace SP (2015, April). Creating conditions to support healthy people: State policies that affect the health of undocumented immigrants and their families. Los Angeles, California: University of California Global Health Institute. [Google Scholar]
- Salimetrics. Salivary uric acid enzymatic assay kit. Carlsbad, CA: Retrieved on 2 February 2016 at: https://www.salimetrics.com/assets/documents/1-3802.pdf [Google Scholar]
- Selye H (1976). The stress of life. New York: McGraw-Hill. [Google Scholar]
- Sharkey J, & Dean WR (2012). The Influence of Community Retail Food Environment on Household Food Access, Food Choice, and Dietary Intake of Mexican-origin Children in Colonias along the South Texas Border with Mexico. Retrieved on February 21, 2015 at: http://srdc.msstate.edu/ridge/projects/recipients/12_sharkey_final.pdf
- Sun HL, Pei D, Lue KH, & Chen YL (2015). Uric acid levels can predict metabolic syndrome and hypertension in adolescents: A 10-year longitudinal study. PLoS One, 10(11), [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suro R, Suárez-Orozco MM, & Canizales S (2015, April). Removing insecurity: How American children will benefit from President Obama’s Executive Action on Immigration. University of Southern California Sol Price School of Public Policy, Tomás Rivera Policy Institute, USC/UCLA. Retrieved on April 27, 2015 from: http://trpi.org/pdfs/research_report.pdf. [Google Scholar]
- Sutin AR, Cutler RG, Camandola S, Uda M, Feldman NH, Cucca F, … Terracciano A (2014). Impulsivity is associated with uric acid: Evidence from humans and mice. Biological Psychiatry, 75(1), 31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkupinski-Quiroga SS, Medina DM, & Glick J (2014). In the belly of the beast effects of anti-immigration policy on Latino Community members. American Behavioral Scientist, 58(13), 1723–1174. [Google Scholar]
- Theodore N (2013, May). Insecure Communities: Latino Perceptions of Police Involvement in Immigration Enforcement. Policy Link. Retrieved at: http://www.policylink.org/sites/default/files/INSECURE_COMMUNITIES_REPORT_FINAL.PDF
- Thomas PD, Goodwin JM, & Goodwin JS (1985). Effect of social support on stress-related changes in cholesterol level, uric acid level, and immune function in an elderly sample. American Journal of Psychiatry, 142(6), 735–737. [DOI] [PubMed] [Google Scholar]
- Van Hook J & Balistreri KS (2006). Ineligible parents, eligible children: food stamps receipt, allotments, and food insecurity among children of immigrants. Social Science Research, 35, 228–251. [Google Scholar]
- Vargas ED, Sanchez GR, & Juárez M (2017). Fear by association: Perceptions of anti-immigrant policy and health outcomes. Journal of Health Politics, Policy and Law, 42(3), 459–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viazzi F, Genovesi S, Ambruzzi M, & Giussani M (2015). Sugar, fructose, uric acid and hypertension in children and adolescents. Italian Journal of Pediatrics, 41, 72–76.26444666 [Google Scholar]
- Wang JY, Chen YL, Hsu CH, Tang SH, Wu CZ, & Pei D (2012). Predictive value of serum uric acid levels for the diagnosis of metabolic syndrome in adolescents. The Journal of Pediatrics, 161(4), 753–756. [DOI] [PubMed] [Google Scholar]
- Yoshikawa H, Godfrey EB, & Rivera AC (2008). Access to institutional resources as a measure of social exclusion: Relations with family process and cognitive development in the context of immigration. New Directions in Child and Adolescent Development, 121, 73–96. [DOI] [PubMed] [Google Scholar]
- Yoshikawa H, & Kholoptseva J (2013, March). Unauthorized immigrant parents and their children’s development: A summary of the evidence. Washington, DC: Migration Policy Institute. [Google Scholar]
- Zhao J, & Huang Y (2015). Salivary uric acid as a noninvasive biomarker for monitoring the efficacy of urate-lowering therapy in a patient with chronic gouty arthropathy. Clinical Chimica Acta, 450, 115–120. [DOI] [PubMed] [Google Scholar]
- Zir LM, McHugh WB, Rahe RH, Arthur RJ, & Rubin RT (1973). Renal excretion of uric acid. Alterations during stressful underwater demolition-team training. Archives of Internal Medicine, 132, 808–812. [PubMed] [Google Scholar]


