Summary
Objective
To analyze the effectiveness of exercise interventions on falls and fall-related fracture prevention among community-dwelling elderlies.
Methods
Literature search was conducted in Pubmed and Embase. Keywords used for literature search were “fracture” AND “fall” AND “exercise”. Randomized controlled trials involving community-dwelling elderlies older than 60 years old with physical exercises as intervention were included. A systematic review and meta-analysis was performed. The primary outcomes were falls and fractures.
Results
Twelve studies were included and 4784 participants were involved with a mean age of 75.4. The most common exercise interventions were strength and balance exercises. The results of meta-analysis of 11 studies showed that exercise intervention had beneficial effect on fall prevention (RR = 0.71, 95% CI, 0.62–0.82; I2 = 24%, p < 0.0001). The effect was better when exercise intervention applied to women participants (RR = 0.64, 95% CI, 0.49–0.83; I2 = 28%, p = 0.00009) compared to men and women participants (RR = 0.75, 95% CI, 0.64–0.89; I2 = 24%, p = 0.001). The results of meta-analysis of seven studies showed that physical exercise had significant effect on fracture prevention (RR = 0.54, 95% CI, 0.35–0.83; I2 = 25%, p = 0.005). However, the effect was significant when exercise intervention applied to women participants only (RR = 0.37, 95% CI, 0.20–0.67; I2 = 0%, p = 0.001) but not significant when exercise intervention applied to both genders (RR = 0.80, 95% CI, 0.58–1.09; I2 = 0%, p = 0.15).
Conclusion
Exercise interventions, especially the combination of strength and balance training, were effective in preventing falls. Resistance exercises and jumping exercises were effective for fracture prevention among community-dwelling older population. The effectiveness of exercise interventions on fracture prevention have more significant effect on women. Further studies are needed to test the effectiveness of exercise interventions in men.
Translational potential
The use of effective exercises or biophysical interventions including vibration therapy can be incorporated into Fracture Liaison Services to prevent future fall and fracture.
Keywords: Exercise, Fall, Fracture, Prevention, Systematic review
Introduction
A fragility fracture is defined as a fracture caused by low-energy trauma and is a common cause of morbidity and mortality in the elderly. The event occurs in up to half of females and one-third of males who are older than 50 years of age [1]. These fractures cause pain and disability in the elderly resulting in a huge and growing financial burden to our healthcare society. The annual direct costs attributable to fracture treatment in the European Union equates to approximately 24 billion EUROs. Including indirect costs such as long-term care and facture prevention therapies, this figure rises to 37 billion EUROs per year [2]. Fragility fractures are most common in patients with osteoporosis [3,4]. To decrease these costs, strategies in preventing primary and secondary falls and fractures are essential.
The concept of imminent fracture risk has also been highlighted in recent studies, with a significant increase in fracture risk in the first 2 years after an initial fracture [5,6]. This window of opportunity provides a golden period to prevent falls and fractures. With the development of Fracture Liaison Services, effective exercise interventions for rehabilitation and fall prevention should be incorporated [7,8]. Ultimately, these strategies will prevent further fractures and subsequent complications. Hip fractures are linked with 33% mortality in the first year and increased morbidity [9]. Loss of independence and deterioration of ambulatory capacity in activities of daily living (ADL) are common consequences after fragility fractures as it is strongly associated with the development of sarcopenia as well [10].
One of the key components of fracture prevention is taking the initiative to prevent falls in a targeted population [11]. There has been controversial evidence on exercise interventions in fracture prevention with previous meta-analysis studies being inconclusive due to the existence of publication bias [12]. However, more recent large-scale randomized controlled trials have provided new positive results [13,14], which may provide the latest evidence on the effectiveness of exercise interventions on fall and fracture prevention among elderlies. This is crucial for the incorporation of effective physiotherapy strategies in Fracture Liaison Services in the future. Therefore, the research question for this systematic review and meta-analysis was:
-
1.
What is the effectiveness of exercise interventions on falls and fall-related fracture prevention among community-dwelling elderlies?
Materials and methods
Identification and selection of studies
A literature search was conducted in Pubmed and Embase. Last access to both databases was 3 June 2019. PRISMA guidelines was used. The keywords used for literature search were “fracture” AND “fall” AND “exercise”. The inclusion criteria were 1) randomized controlled trials investigating the effect of exercise interventions, 2) participants older than 60 years of age in the community, 3) outcome measures of fall reported 4) outcome measures of fracture reported. Exclusion criteria were 1) absence of control group, 2) participants received medication interventions e.g. steroids, etc. 3) fall or fracture outcomes not reported, 4) review papers and 5) articles not in English.
Selection of studies
2 reviewers conducted selection of studies independently. Duplicates were removed. Title and abstracts were screened and irrelevant papers were removed based on inclusion and exclusion criteria. Full text of potential relevant papers was retrieved and assessed for eligibility. Disagreements were settled by discussion and consensus.
Data extraction and synthesis
Information from eligible studies were extracted and presented: 1) study design and sample size, 2) means age and gender, 3) characteristics of the exercise in intervention group 4) frequency, duration, mode of delivery of exercise program 5) follow-up period, 6) activities of control group 7) fall and fracture outcomes.
Assessment of methodological quality
The recommendation of the Cochrane Collaboration was followed to assess risk of bias among the six domains: Random sequence generation, allocation concealment, methods of ascertaining falls or fracture, blinding of fall assessment, blinding of participants and personnel and incomplete outcome data [15]. For each domain, ratings were low risk, high risk or unclear based on whether the specific domain was performed.
Data analysis
The rate ratio of falls and the rate ratio of fractures of each study were the primary outcome of interest to show the effectiveness of exercise intervention compared to control group. The corresponding data were extracted from each study, and if the rate ratio was not reported, it was calculated from the total number of falls or fracture divided by the total length of time falls or fractures were monitored (person years) in the two comparison groups as recommended by the Cochrane handbook (chapter 9) [16]. The rate ratio (RR) and standard error (SE) were calculated by software Comprehensive meta-analysis (CMA, NJ, USA) with 95% confidence intervals. The effect of physical exercise performed on falls and fractures prevention was analyzed by Review Manager (RevMan 5.1; Cochrane Community, London, UK) and forest plots were assembled for the two categories by using a random effect model. Heterogeneity was tested with Cochran's Q statistic and I square test quantified the degree of heterogeneity, which I square value of 25%, 50% and 75% represented low, moderate and high degrees of heterogeneity respectively.
Results
Flow of studies through the review
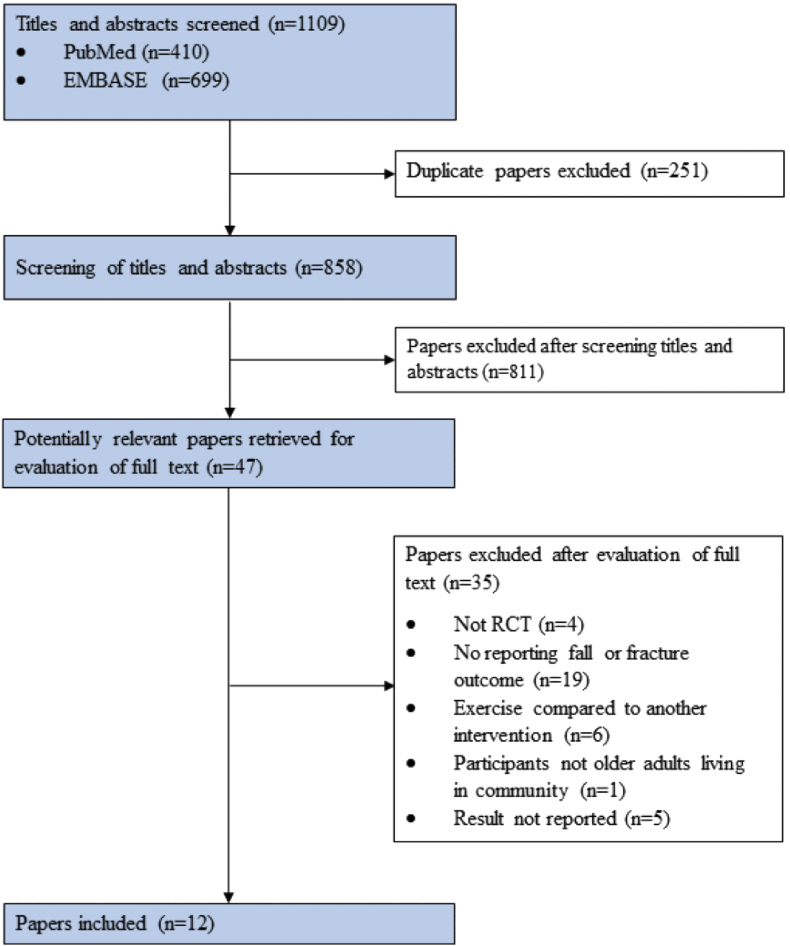
The search strategy yielded 1103 publications, of which 251 were excluded due to duplicates from Pubmed and Embase. Another 804 trials were excluded as the papers were not related to the topic. A total of 48 full text articles were reviewed for eligibility, 4 studies were excluded as they were not randomized controlled trials, 20 did not report any outcomes on falls or fractures. 6 studies compared two exercise interventions without control groups. 5 studies were study protocols. 1 study had participants living in nursing homes. A total of 12 studies remained for further analysis. Please refer to Fig. 1 for PRISMA diagram.
Fig. 1.
Flow chart of literature search result.
Characteristics of included studies
A total of 4784 individuals participated in all studies, with sample size ranging from 44 to 1635 participants. The majority of the participants were women with a mean age of 75.4 years. 5 studies [13,[17], [18], [19], [20]] involved women subjects only. 7 studies had an adherence rate more than 90%, whereas three studies had 85% adherence and two studies had approximately 70%. The studies were conducted in 7 countries, which were Finland [13,14,19], USA [21], Japan [20,22,23], Netherlands [24], Germany [17,18], Spain [25] and England [26] (see Table 1).
Table 1.
Characteristics of included studies.
| Author and year | No. of participants | Participant selection criteria | Mean age | Type of exercise | Mode of delivery | Exercise frequency | Intervention duration | Follow-up period (month) | Comparison group | Rate ratio of fall or fracture (person year) |
|---|---|---|---|---|---|---|---|---|---|---|
| Karinkanta, 2015 | 72 | Lived independently at home, no osteoporosis | 73.3 | Resistance ex and balance-jumping ex | Group ex | 3 times per week | 12 months | 5 years (60 months) | No intervention | Fall: 0.49 Fracture: 0.26 |
| Korpelainen 2004 | 160 | Elderly women with low BMD at radius and hip | 72.8 | Jumping and balance ex | Group ex and home ex | Daily, 1 h group ex+ 20 min home ex | 6 months | 30 months | No intervention | Fall: 0.788 Fracture:0.339 |
| Gill, 2016 | 1635 | 70-79 yo short physical performance battery score <9, able to walk 400 m | 78.9 | Strength, flexibility and balance | Group and home ex | Group ex: 2 times per week Home ex: 3–4 times per week |
24–42 months | 2.6 years (31 months) | Educational program | Fracture:0.867 |
| Sakamoto, 2012 | 865 | Home dwelling elderly>75 years old | 80.5 | Single leg standing exercise | Supervised individual ex | 1 min per set, 3 sets a day, daily exercise | 6 months | No (6 months observation) | No intervention | Fall: 0.676 Fracture:0.404 |
| Smulders, 2010 | 92 | With osteoporosis and a fall history within 1 year | 71 | Balance, Walking ex, weight bearing ex, obstacle course, correction of gait | Group ex | 11 sessions during 5.5 weeks | 5.5 weeks | 12 months | No intervention | Fall: 0.626 Fracture:0.319 |
| Uusi-Rasi, 2015 | 205 | Home-dwelling women, at least one fall history in previous year, no use of vit D and no contraindication to ex | 74.2 | Balance challenge, weight-bearing, strengthening, agility and functional exercise | Supervised group ex | 2 times per week in first 12 months, once per week in another 12 months | 24 months | No, Monthly reported fall in the observation time 24 months |
No intervention | Fall: 0.98 |
| Kemmler, 2010 | 227 | 65-year-old or older, living independently in community | 69.1 | Dynamic balance training, strength, stretching and weight bearing ex | Group ex and home ex | Once per week, 120 min for group ex, 40 min for home ex | 18 months | No, observed in study time (18months) | Low- frequency and low intensity exercise, 60 min per week for 10 weeks and follow by rest for 10 weeks (18months duration) | Fall:0.54 Fracture:0.487 |
| Hauer, 2001 | 57 | Female geriatric patients admitted to acute care or inpatient reheb with history of injurious fall | 82 | Resistance training, progressive functional balance training | Group ex | 3 times per week | 3 months | 3 months | Placebo activities, eg: flexibility ex, ball games and memory tasks | Fall:0.753 |
| Suzuki, 2004 | 44 | Community dwelling elderly women | 78 | Strengthening, walking, balance and tai chi | Group ex and home ex | Group ex: 1 h session every two weeks Home ex: 2–3 times per week, 30 min per day |
6 months | 20 months | Pamphlet and advice on fall prevention | Fall:0.25 |
| Perula, 2012 | 404 | community-living elderly | 76.3 | Walking, balance, strengthen and flexibility | Group ex and home ex | Group ex: 5 sessions/weeks for 3 weeks, 90 min per session Home ex: 4 times per week, 30 min per sessions |
12 months | 12 months | Received brief piece of advice about fall prevention and information leaflet | Fall:0.73 |
| Kim, 2013 | 105 | Age>70, at least a fall experience in previous year | 77.8 | Strength and balance | Group ex | Twice per week, each session for 60 min | 3 months | 12 months | Took a 60 min educational class once a month for 3 months, class focused on undernutrition, cognitive function and oral hygiene | Fall: 0.486 Fracture:0.51 |
| Iliffe, 2014 | 845 | Age >65 community living elderly | 71 | Strengthening and balance, endurance, flexibility, functional floor skills and tai chi | Group ex and home ex | Group ex: 60 min weekly ex class Home ex: twice per week, 30 min per sessions |
24 weeks | 12months | No intervention | Fall: 0.74 |
Exercise characteristics and delivery
Exercise interventions were provided to all participants in the intervention groups. These include resistance or strength exercise, balance training, jumping exercise, flexibility exercise, weight-bearing exercise, gait training, agility exercise, functional exercise and Tai Chi. All studies had balance exercise. 9 studies [13,14,17,18,[20], [21], [22],25,26] combined balance and strengthening exercise. As for the remaining 3 studies, 1 study used balance exercise alone [19], 1 study used balance and jumping exercises [23] whilst 1 study combined balancing with weight bearing exercise [24]. 6 studies reported the mode of delivery with a combination of group and home exercises [[18], [19], [20], [21],25,26], 5 studies delivered via group form [13,14,17,22,24] and 1 study delivered exercise individually [23]. 5 studies [14,18,22,24,26] performed exercises 1–2 times per week, 3 studies [13,17,21] performed exercises 3–4 times per week. 2 studies [19,23] had daily exercise and 1 study performed group exercises every 2 weeks and home exercise 2–3 times per week [20]. Another study performed group exercise 5 sessions per week for the first three weeks and performed home exercises 4 times per week afterwards [25]. The total period of exercise intervention was up to 3 months in 2 studies [17,22], 6 months in 4 studies [19,20,23,26], 12 months in 2 studies [13,25], 18 months in 1 study [18], 24 months in 1 study [14] and 1.4 months for 1 study [24]. For 1 study [21], the period of exercise was up to 24 months–42 months depending on the enrollment of participants.
Follow-up periods
4 studies had follow-up of 12 months [22,[24], [25], [26]], 2 studies had follow-up of 30 months [19,21] and 3 studies [14,18,23] had no follow up post-intervention and recorded fall or fracture incidence during the intervention period. The remaining studies had follow up at 3 months [17], 20 months [20] and 60 months [13].
Control group activities
In the control groups, there were no interventions in 6 studies [13,14,19,23,24,26]. Other studies used alternative activities including health education workshops [21], ball games and memory tasks [17], and pamphlet and advice on fall prevention [20,25]. 1 study gave a low-frequency, low-intensity task for 60 min per week for 10 weeks followed by 10 weeks of rest. The tasks included relaxation, games, dances, body sensitivity, deep breathing and general coordination [18]. The control group of another study [22] took a 60-min class once per month for 3 months focusing on nutrition, cognitive function and oral hygiene.
Risk of bias
The risk of bias of all studies were assessed. All studies performed randomized allocation and allocation concealment with low risk of bias. As for reporting bias, most studies had low risk of bias with participants using fall calendars [14,17,18,22,24,26], medical records [13,21] and by interview [20]. In 1 study, participants were asked whether a fall had occurred during follow-up [19] and another study only assessed the incidence of fall by asking participants every 3 months without record in a calendar, which has a risk of recall bias in elderlies [25]. One study did not report on the method of fall or fracture reporting [23], and risk of bias was unclear. For performance bias, 7 studies had both participants and outcome assessors blinded [13,14,18,19,22,25,26], 1 study had participants blinded only [21] and the remaining four studies [17,20,23,24] did not have any information regarding blinding. The majority of studies had low attrition bias and detection bias. There were minimal loss of subjects. The assessment of risk of bias in the included studies is in Table 2. 1 study did not report data related to number of fall and fracture rates and was therefore excluded from meta-analysis [21].
Table 2.
Assessment of risk of bias in included studies.
| Trial | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting falls/fracture | Other bias |
|---|---|---|---|---|---|---|---|
| Karinkanta, 2015 | Low | Low | Low | Low | Low | Low | Low |
| Korpelainen, 2004 | Low | Low | Low | Low | Low | High | Low |
| Gill, 2016 | Low | Low | High | Low | Low | Low | Low |
| Sakamoto, 2012 | Low | Low | Unclear | Unclear | Low | Unclear | Low |
| Smulders, 2010 | Low | Low | Unclear | Low | Low | Low | Low |
| Uusi-Rasi, 2015 | Low | Low | Low | Low | Low | Low | Low |
| Kemmler, 2010 | Low | Low | Low | Low | Low | Low | Low |
| Hauer, 2001 | Low | Low | Unclear | Low | High | Low | Low |
| Suzuki, 2004 | Low | Low | Unclear | Low | Low | Low | Low |
| Perula. 2012 | Low | Low | Low | low | Low | High | Low |
| Kim, 2013 | Low | Low | Low | Low | Low | Low | Low |
| Iliffe, 2014 | Low | Low | Low | Low | High | Low | Low |
Meta-analysis
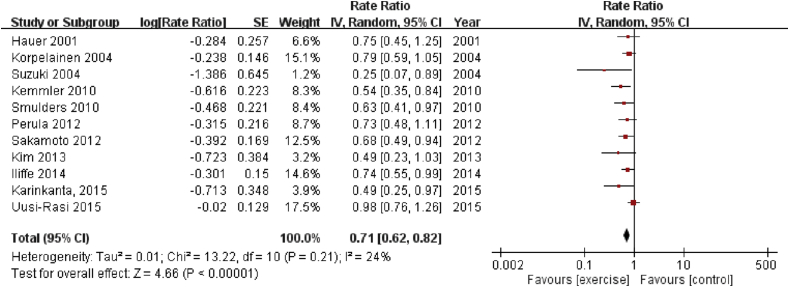
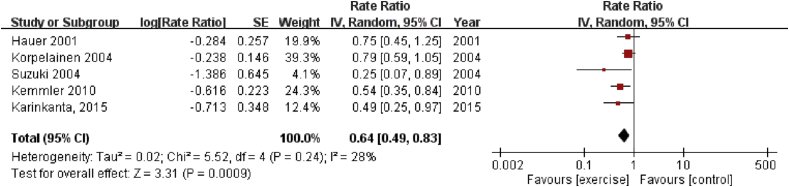
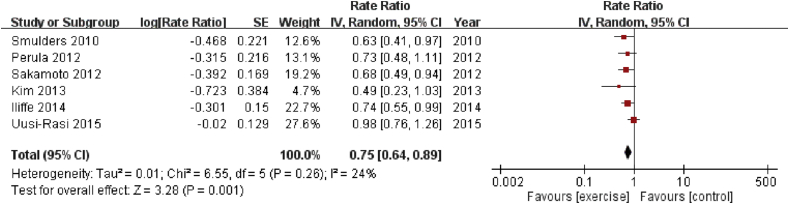
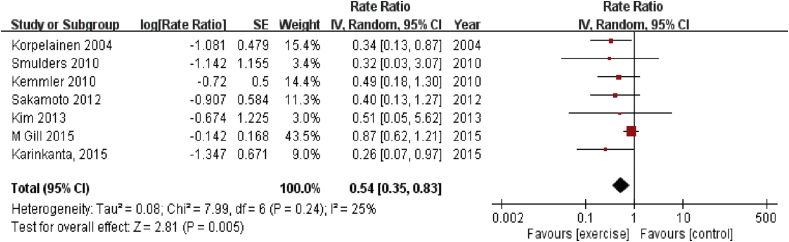
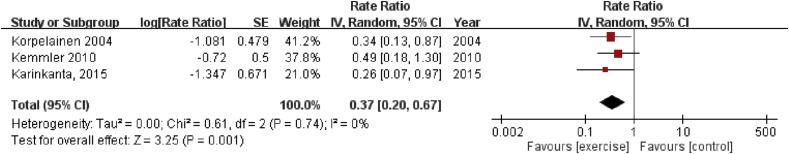
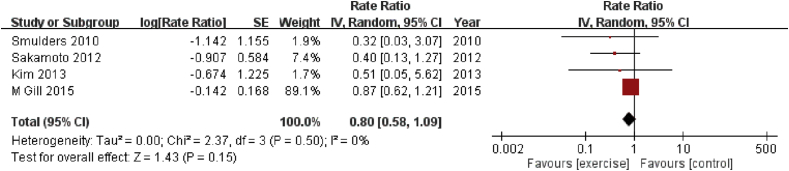
The results of the meta-analysis of all 11 studies [13,14,[17], [18], [19], [20],[22], [23], [24], [25], [26]] showed that exercise intervention had significant beneficial effect on fall prevention (RR = 0.71, 95% CI, 0.62–0.82; I2 = 24%, p < 0.0001) (Fig. 2). The effect was even better when exercise intervention was performed on women participants [13,[17], [18], [19], [20]] (RR = 0.64, 95% CI, 0.49–0.83; I2 = 28%, p = 0.00009) (Fig. 4) compared to both genders [14,[22], [23], [24], [25], [26]] (RR = 0.75, 95% CI, 0.64–0.89; I2 = 24%, p = 0.001) (Fig. 5). The results of meta-analysis of the 7 studies [13,18,19,[21], [22], [23], [24]] showed that physical exercise also had a significant effect on fracture prevention (RR = 0.54, 95% CI, 0.35–0.83; I2 = 25%, p = 0.005) (Fig. 3). The effect was significant when exercise intervention was applied to women participants only [14,18,19] (RR = 0.37, 95% CI, 0.20–0.67; I2 = 0%, p = 0.001) (Fig. 6) but not significant when exercise intervention was performed on both genders [[21], [22], [23], [24]] (RR = 0.80, 95% CI, 0.58–1.09; I2 = 0%, p = 0.15) (Fig. 7).
Fig. 2.
Overall effect of exercise intervention on fall prevention.
Fig. 4.
Overall effect of exercise intervention on fall prevention in women only.
Fig. 5.
Overall effect of exercise intervention on fall prevention in both gender.
Fig. 3.
Overall effect of exercise intervention on fracture prevention.
Fig. 6.
Overall effect of exercise intervention on fracture prevention in women only.
Fig. 7.
Overall effect of exercise intervention on fracture prevention in both gender.
Discussion
This meta-analysis showed that exercise intervention produced positive effect on fall prevention and reduction of fractures in elderlies. The exercise regimen used by participants were mostly a combination of resistance or strengthening training with balance exercises [13,14,17,18,[20], [21], [22],25,26], with the incidence of fall significantly reduced. Muscle strength and balance are key elements for preventing falls from muscle weakness and sarcopenia [27]. There is strong evidence supporting strengthening or resistance exercises to enhance quadriceps which acts as a static and dynamic balancer for older people [28]. Lower limb muscle strength is crucial for mobility and physical function [29]. Therefore, these exercises are important and should be involved in multi-component exercises intervention, and can play an important role in fall prevention programs [30]. Almost all hip and wrist fractures and approximately 30% of vertebral fractures are caused by falls [31]. Balance exercises are an alternative type of training which aims to prevent falls. There are different ways to deliver balance exercise among studies but the principles are similar. Exercises that decrease the base of support, shift the center of mass side-to-side, stepping up and down with minimal hand support, single leg stance, tandem walking, obstacle courses, and Tai Chi are commonly performed [13,14,[17], [18], [19], [20], [21], [22], [23], [24], [25], [26]].
Our results concur with a previous review performed by Gillespie et al., in 2012 [32], which reported that the prevention of falls amongst community dwelling older adults included strengthening exercise and balance training. However, further to the analysis, our current study also investigated the effect of exercise interventions on fracture prevention. The occurrence of a fracture significantly affects clinical outcomes and healthcare costs. Ensuring the optimal exercise intervention for fracture prevention allows the potential incorporation into our Fracture Liaison Services [33]. It is important to have effective prevention of secondary fractures as the mortality is significantly higher.
Bone fragility is generally considered a major contributing factor of fracture occurrence [34]. However, deterioration of lower limb strength, loss of balancing ability and fall episodes may be the biggest risk factors causing fractures in the elderly [11]. An effective fall prevention exercise program is as important as treating bone health amongst elderlies [35]. In fact, exercises have been shown to bring positive effects in patients with osteoporosis [35], osteonecrosis [36], etc. This meta-analysis provides evidence that effective exercise programs are effective in fall prevention and benefit in reducing fractures. The meta-analysis by Kemmler et al. [12] showed some beneficial effect of exercises on fractures prevention among elderly but was not significant due to publication bias. Heterogeneity of trial results were also a major problem. Falls were not analyzed in the study and the meta-analysis comprised of both randomized controlled trials and non-randomized controlled trials. With the recent publications of further randomized controlled trials in this topic, we were able to conduct an updated review. The result of the current meta-analysis is focused on both fall and fall-related fractures with only randomized controlled trials to decrease risks of bias.
Our subgroup analysis showed exercise intervention was effective in preventing falls when applied to either women or both genders. But the effect of fracture prevention was significant in women only and not significant when both genders were involved. The result showed that the effectiveness of exercise on fracture prevention may be different between men and women. The study by Woo et al. [37] compared the effect of Tai Chi and resistance exercise on bone mineral density (BMD) changes between older men and women. The result showed no positive effects on BMD changes in men but significant BMD changes at the hip in women subjects. Our previous animal studies have shown that estrogen may play an important role. Ovariectomized rats, which are estrogen deficient, has higher response to mechanical stimulation as compared to sham rats [38]. However, further research is needed in order to understand the exact mechanisms. For these reasons, more effective strategies may be required to prevent falls and fractures in male patients. Currently there is lack of studies focusing on the effectiveness of exercises in men. Recent studies have been investigating the use of vibration therapy as an intervention to prevent falls in fragility fracture patients [39]. Vibration therapy is a biophysical intervention which is non-invasive and has been proven to have positive effects in quadricep muscle strength, balancing and gait speed.
Based on our results, the most effective exercises in preventing falls are strengthening and balance exercises, which is highlighted in most studies. Suzuki et al. showed balancing exercises with Tai Chi and strengthening exercises for a 6 month period had the lowest rate ratio in the prevention of falls [20]. As for the prevention of fractures, resistance exercises and balance-jumping exercises are most effective. Karinkanta et al. showed that these exercises for 12 months had the lowest rate ratio for fractures [14]. The strengths of this study are that it is composed of randomized controlled trials only, therefore reducing bias. The analysis is also more updated with the recent publishment of several studies. There are some limitations in this study. For the outcome measures, some studies did not apply fall calendars to record fall events which is a well-established method in collecting fall data. This may cause inaccuracies in the fall incidence rate [40]. There was also heterogeneity in follow-up periods between studies.
Conclusion
In conclusion, our results show that physical exercise can prevent falls and fall related fractures in elderlies. There are two important components for fall prevention which are balance and strength training and should be involved in fall prevention programs. Future incorporation of resistance exercises and balance-jump exercises into Fracture Liaison Services should be performed. Currently, the exact mechanisms as to why the effectiveness of exercise interventions on fracture prevention have more significant effect on women is still unclear. Further studies are also needed to test the effectiveness of exercise interventions in men in terms of fall and fracture prevention.
Conflict of Interest
The authors have no conflicts of interest to disclose in relation to this article.
Acknowledgement
This study was supported by the Hong Kong Research Grants Council Early Career Scheme (Reference no. 24108519).
Contributor Information
R.M.Y. Wong, Email: ronaldwong@ort.cuhk.edu.hk.
K.C. Chong, Email: kcchong117@gmail.com.
S.W. Law, Email: lawsw@ort.cuhk.edu.hk.
W.T. Ho, Email: percyho@link.cuhk.edu.hk.
J. Li, Email: 1155134059@link.cuhk.edu.hk.
C.S. Chui, Email: elvis_chui@cuhk.edu.hk.
S.K.H. Chow, Email: skhchow@cuhk.edu.hk.
W.H. Cheung, Email: louischeung@cuhk.edu.hk.
References
- 1.Cummings S.R., Melton L.J. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 2.Hernlund E., Svedbom A., Ivergård M., Compston J., Cooper C., Stenmark J. Osteoporosis in the European union: medical management, epidemiology and economic burden. A report prepared in collaboration with the international osteoporosis foundation (IOF) and the European federation of pharmaceutical industry associations (efpia) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouxsein M.L., Kaufman J., Tosi L., Cummings S., Lane J., Johnell O. Recommendations for optimal care of the fragility fracture patient to reduce the risk of future fracture. J Am Acad Orthop Surg. 2004;12(6):385–395. doi: 10.5435/00124635-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Suen P.K., Qin L. Sclerostin, an emerging therapeutic target for treating osteoporosis and osteoporotic fracture: a general review. J Orthop Translat. 2016;4:1–13. doi: 10.1016/j.jot.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonafede M., Shi N., Barron R., Li X., Crittenden D., DJAoo Chandler. Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. 2016;11(1):26. doi: 10.1007/s11657-016-0280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roux C., Briot K. Imminent fracture risk. Osteoporos Int. 2017;28(6):1765–1769. doi: 10.1007/s00198-017-3976-5. [DOI] [PubMed] [Google Scholar]
- 7.Bonanni S., Sorensen A.A., Dubin J., Drees B. The role of the fracture liaison service in osteoporosis care. Mo Med. 2017;114(4):295–298. [PMC free article] [PubMed] [Google Scholar]
- 8.Wong R.M.Y., Ho W.T., Law S.W., Li W., Chau W.W., Chow S.K.H. Fragility fractures and imminent fracture risk in Hong Kong: one of the cities with longest life expectancies. Arch Osteoporos. 2019;14(1):104. doi: 10.1007/s11657-019-0648-4. [DOI] [PubMed] [Google Scholar]
- 9.Roche J.J., Wenn R.T., Sahota O., Moran C.G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong R.M.Y., Wong H., Zhang N., Chow S.K.H., Chau W.W., Wang J. The relationship between sarcopenia and fragility fracture-a systematic review. Osteoporos Int. 2019;30(3):541–553. doi: 10.1007/s00198-018-04828-0. [DOI] [PubMed] [Google Scholar]
- 11.Jarvinen T.L., Sievanen H., Khan K.M., Heinonen A., Kannus P. Shifting the focus in fracture prevention from osteoporosis to falls. BMJ. 2008;336(7636):124–126. doi: 10.1136/bmj.39428.470752.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kemmler W., Haberle L., von Stengel S. Effects of exercise on fracture reduction in older adults: a systematic review and meta-analysis. Osteoporos Int. 2013;24(7):1937–1950. doi: 10.1007/s00198-012-2248-7. [DOI] [PubMed] [Google Scholar]
- 13.Karinkanta S., Kannus P., Uusi-Rasi K., Heinonen A., Sievanen H. Combined resistance and balance-jumping exercise reduces older women's injurious falls and fractures: 5-year follow-up study. Age Ageing. 2015;44(5):784–789. doi: 10.1093/ageing/afv064. [DOI] [PubMed] [Google Scholar]
- 14.Uusi-Rasi Kirsti, Patil Radhika, Karinkanta Saija, Kannus Pekka, Tokola Kari, Lamberg-Allardt Christel. Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Intern Med. 2015;175(5):703–711. doi: 10.1001/jamainternmed.2015.0225. [DOI] [PubMed] [Google Scholar]
- 15.Higgins Julian P.T., Altman Douglas G., Gøtzsche Peter C., Jüni Peter, Moher David, Oxman Andrew D. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Julian, editor. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; Chichester, West Sussex ; Hoboken NJ: 2008. ©2008; 2008. [Google Scholar]
- 17.Hauer K., Rost B., Rutschle K., Opitz H., Specht N., Bartsch P. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc. 2001;49(1):10–20. doi: 10.1046/j.1532-5415.2001.49004.x. [DOI] [PubMed] [Google Scholar]
- 18.Kemmler W., von Stengel S., Engelke K., Haberle L., Kalender W.A. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: the randomized controlled senior fitness and prevention (SEFIP) study. Arch Intern Med. 2010;170(2):179–185. doi: 10.1001/archinternmed.2009.499. [DOI] [PubMed] [Google Scholar]
- 19.Korpelainen R., Keinanen-Kiukaanniemi S., Heikkinen J., Vaananen K., Korpelainen J. Effect of impact exercise on bone mineral density in elderly women with low BMD: a population-based randomized controlled 30-month intervention. Osteoporos Int. 2006;17(1):109–118. doi: 10.1007/s00198-005-1924-2. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki T., Kim H., Yoshida H., Ishizaki T. Randomized controlled trial of exercise intervention for the prevention of falls in community-dwelling elderly Japanese women. J Bone Miner Metabol. 2004;22(6):602–611. doi: 10.1007/s00774-004-0530-2. [DOI] [PubMed] [Google Scholar]
- 21.Gill T.M., Pahor M., Guralnik J.M., McDermott M.M., King A.C., Buford T.W. Effect of structured physical activity on prevention of serious fall injuries in adults aged 70-89: randomized clinical trial (LIFE Study) BMJ. 2016;352:i245. doi: 10.1136/bmj.i245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim H., Yoshida H., Suzuki T. Falls and fractures in participants and excluded non-participants of a fall prevention exercise program for elderly women with a history of falls: 1-year follow-up study. Geriatr Gerontol Int. 2014;14(2):285–292. doi: 10.1111/ggi.12095. [DOI] [PubMed] [Google Scholar]
- 23.Sakamoto K., Endo N., Harada A., Sakada T., Tsushita K., Kita K. Why not use your own body weight to prevent falls? A randomized, controlled trial of balance therapy to prevent falls and fractures for elderly people who can stand on one leg for </=15 s. J Orthop Sci. 2013;18(1):110–120. doi: 10.1007/s00776-012-0328-3. [DOI] [PubMed] [Google Scholar]
- 24.Smulders E., Weerdesteyn V., Groen B.E., Duysens J., Eijsbouts A., Laan R. Efficacy of a short multidisciplinary falls prevention program for elderly persons with osteoporosis and a fall history: a randomized controlled trial. Arch Phys Med Rehabil. 2010;91(11):1705–1711. doi: 10.1016/j.apmr.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Perula L.A., Varas-Fabra F., Rodriguez V., Ruiz-Moral R., Fernandez J.A., Gonzalez J. Effectiveness of a multifactorial intervention program to reduce falls incidence among community-living older adults: a randomized controlled trial. Arch Phys Med Rehabil. 2012;93(10):1677–1684. doi: 10.1016/j.apmr.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 26.Iliffe S., Kendrick D., Morris R., Masud T., Gage H., Skelton D. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess. 2014;18(49):1–105. doi: 10.3310/hta18490. vii-xxvii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carter N.D., Kannus P., Khan K.M. Exercise in the prevention of falls in older people: a systematic literature review examining the rationale and the evidence. Sports Med. 2001;31(6):427–438. doi: 10.2165/00007256-200131060-00003. [DOI] [PubMed] [Google Scholar]
- 28.Carter N.D., Khan K.M., Mallinson A., Janssen P.A., Heinonen A., Petit M.A. Knee extension strength is a significant determinant of static and dynamic balance as well as quality of life in older community-dwelling women with osteoporosis. Gerontology. 2002;48(6):360–368. doi: 10.1159/000065504. [DOI] [PubMed] [Google Scholar]
- 29.Liu C.J., Latham N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;(3):CD002759. doi: 10.1002/14651858.CD002759.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker M.K., Atlantis E., Fiatarone Singh M.A. Multi-modal exercise programs for older adults. Age Ageing. 2007;36(4):375–381. doi: 10.1093/ageing/afm054. [DOI] [PubMed] [Google Scholar]
- 31.Parkkari J., Kannus P., Palvanen M., Natri A., Vainio J., Aho H. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int. 1999;65(3):183–187. doi: 10.1007/s002239900679. [DOI] [PubMed] [Google Scholar]
- 32.Gillespie L.D., Robertson M.C., Gillespie W.J., Sherrington C., Gates S., Clemson L.M. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong R.M.Y., Law S.W., Lee K.B., Chow S.K.H., Cheung W.H. Secondary prevention of fragility fractures: instrumental role of a fracture liaison service to tackle the risk of imminent fracture. Hong Kong Med J. 2019;25(3):235–242. doi: 10.12809/hkmj187593. [DOI] [PubMed] [Google Scholar]
- 34.Wong R.M.Y., Choy M.H.V., Li M.C.M., Leung K.S., Chow S.K.-H., Cheung W.H. A systematic review of current osteoporotic metaphyseal fracture animal models. Bone Joint Res. 2018;7(1):6–11. doi: 10.1302/2046-3758.71.BJR-2016-0334.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chow T.H., Lee B.Y., Ang A.B.F., Cheung V.Y.K., Ho M.M.C., Takemura S. The effect of Chinese martial arts Tai Chi Chuan on prevention of osteoporosis: a systematic review. J Orthop Translat. 2018;12:74–84. doi: 10.1016/j.jot.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao D., Zhang F., Wang B., Liu B., Li L., Kim S.Y. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version) J Orthop Translat. 2020;21:100–110. doi: 10.1016/j.jot.2019.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woo J., Hong A., Lau E., Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36(3):262–268. doi: 10.1093/ageing/afm005. [DOI] [PubMed] [Google Scholar]
- 38.Chow S.K., Leung K.S., Qin J., Guo A., Sun M., Qin L. Mechanical stimulation enhanced estrogen receptor expression and callus formation in diaphyseal long bone fracture healing in ovariectomy-induced osteoporotic rats. Osteoporos Int. 2016;27(10):2989–3000. doi: 10.1007/s00198-016-3619-2. [DOI] [PubMed] [Google Scholar]
- 39.Wong R.M.Y., Ho W.T., Tang N., Tso C.Y., Ng W.K.R., Chow S.K. A study protocol for a randomized controlled trial evaluating vibration therapy as an intervention for postural training and fall prevention after distal radius fracture in elderly patients. Trials. 2020;21(1):95. doi: 10.1186/s13063-019-4013-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hannan M.T., Gagnon M.M., Aneja J., Jones R.N., Cupples L.A., Lipsitz L.A. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the MOBILIZE Boston Study. Am J Epidemiol. 2010;171(9):1031–1036. doi: 10.1093/aje/kwq024. [DOI] [PMC free article] [PubMed] [Google Scholar]