Abstract
Background:
There is no agreement about or understanding of what rehabilitation is; those who pay for it, those who provide it, and those who receive it all have different interpretations. Furthermore, within each group, there will be a variety of opinions. Definitions based on authority or on theory also vary and do not give a clear description of what someone buying, providing, or receiving rehabilitation can actually expect.
Method:
This editorial extracts information from systematic reviews that find rehabilitation to be effective, to discover the key features and to develop an empirical definition.
Findings:
The evidence shows that rehabilitation may benefit any person with a long-lasting disability, arising from any cause, may do so at any stage of the illness, at any age, and may be delivered in any setting. Effective rehabilitation depends on an expert multidisciplinary team, working within the biopsychosocial model of illness and working collaboratively towards agreed goals. The effective general interventions include exercise, practice of tasks, education of and self-management by the patient, and psychosocial support. In addition, a huge range of other interventions may be needed, making rehabilitation an extremely complex process; specific actions must be tailored to the needs, goals, and wishes of the individual patient, but the consequences of any action are unpredictable and may not even be those anticipated.
Conclusion:
Effective rehabilitation is a person-centred process, with treatment tailored to the individual patient’s needs and, importantly, personalized monitoring of changes associated with intervention, with further changes in goals and actions if needed.
Keywords: Rehabilitation description, content, process, therapy, person-centred
Introduction
What constitutes rehabilitation? Physiotherapy? Exercises? Something you receive ‘to get you better’? Many healthcare staff, when referring someone to rehabilitation, have little idea, maybe saying ‘they’ll sort out your problems for you’, or sometimes ‘they’ll work you really hard’. Commissioners, similarly, rarely understand what they are paying for; at most they expect a certain number of contact hours between a patient and a therapist and/or setting goals. Patients do not know what to expect.
Searching dictionaries or the Internet does not help much because the answers are imprecise and lack detail. Commissioners (for example) still would not know what they are paying for, how to assess its quality, or how to quantify it if depending on published definitions, such as one in a recent commissioning guide1 (Box 1), or others.2–4 Most definitions are not based on evidence.
Box 1.
|
A definition of rehabilitation
From NHS England’s guide on commissioning rehabilitation1 The goal: A modern healthcare system must do more than just stop people dying. It needs to equip them [patients] to live their lives, fulfil their maximum potential and optimise their contribution to family life, their community and society as a whole. The content: Rehabilitation achieves this by focusing on the impact that the health condition, developmental difficulty or disability has on the person’s life, rather than focusing just on their diagnosis. It involves working in partnership with the person and those important to them so that they can maximise their potential and independence, and have choice and control over their own lives. It is a philosophy of care that helps to ensure people are included in their communities, employment and education rather than being isolated from the mainstream and pushed through a system with ever-dwindling hopes of leading a fulfilling life. |
An empirical investigation into the phenomenon of rehabilitation might clarify the matter. This editorial reviews studies reporting that rehabilitation has a beneficial effect and asks: what aspects of the intervention being studied, rehabilitation, are common between the various studies investigating successful rehabilitation?
This approach is not new. It was used to investigate the nature of ‘stroke unit rehabilitation’ in 2002,5 and the 2013 review6 stated:
In summary, organised inpatient (stroke unit) care was characterised by: (1) co-ordinated multidisciplinary rehabilitation, (2) staff with a specialist interest in stroke or rehabilitation, (3) routine involvement of carers in the rehabilitation process and (4) regular programmes of education and training.
This editorial, based on systematic reviews and larger individual trials, identifies the features of rehabilitation found in studies showing that patients benefit. Its aim is to discover the main characteristics of effective ‘rehabilitation’. The results are presented in three domains:
Context: who may benefit, and does location matter?
Process: what are the common features of the process?
Interventions: what interventions are used?
It develops an evidence-based description of effective rehabilitation.
Context
This part investigates whether the benefits of rehabilitation are restricted to specific patient groups, or to delivery in specific locations.
What conditions are associated with benefit?
Systematic reviews have considered rehabilitation involving patients covering a large range of conditions, diseases, and ages, and in almost all groups a positive effect is shown. Patients can be helped by rehabilitation if they have the following:
Neurological conditions such as multiple sclerosis,12–14 stroke,6 motor neurone disease,15 and other conditions;16,17
Musculo-skeletal disorders such as fractures,18,19 hip and knee arthroplasty,20 and sub-acute or chronic back pain;21,22
The common feature among the wide variety of disease disorders listed above is that the patient has a continuing disability, often with several or many factors contributing to the situation.
The only reasonable conclusion must be that rehabilitation, whatever it is, is likely to benefit anyone with persistent disability associated with an illness, regardless of the underlying disease or disorder.
Is rehabilitation effective anywhere?
Rehabilitation has been found effective in most settings:
Probably in intensive care units (there are many reviews, with contrasting findings);25–28
Specialist rehabilitation inpatient wards;6
Nursing homes;31 and
It is specifically important to note that rehabilitation out of hospital, after discharge, is effective.32,35
Although the strength of the evidence varies, there seems little doubt that rehabilitation can have a beneficial effect wherever it is delivered. Direct comparisons between different settings have rarely been studied.
Does stage or prognosis of disease affect effectiveness?
Categorization of disabling disorders by prognosis and stage is difficult, and the categories suggested are not as distinct as they appear. Moreover, the effects of development (in children) and aging (in older adults) lead to changes in disability and/or rehabilitation needs. Nonetheless, there is evidence that rehabilitation is beneficial in the following:
The later, more stable phases of acute onset disorders: stroke;38
Diseases that have a slow or fluctuant onset and are progressive to a greater or lesser degree: multiple sclerosis,12–14 osteoarthritis,39 chronic back pain;21
Diseases that are more inexorably progressive: Parkinson’s disease17 and Alzheimer’s disease.40,41
One may conclude that rehabilitation is likely to be beneficial to a person with disability at any stage of their illness and whatever the nature of their prognosis, including when receiving palliative care: rehabilitation can benefit people with advanced cancer.42
Does age limit effectiveness?
There are few trials of rehabilitation (in contrast to trials on specific interventions) involving children, and no reviews were identified. The studies already referred to have included people of all ages from teenagers through to the very old and frail. There is no reason to doubt that rehabilitation is effective at any age, though there is little evidence for children.
Process
The second part of this review investigates what features of the process are common across the studies showing benefit.
Using the biopsychosocial model of illness
The use of a biopsychosocial framework43 is mentioned or implied in almost all reviews and articles. This characteristic is inextricably intertwined with multidisciplinary teamwork44 because any process based on the biopsychosocial model necessarily considers a wide range of factors, requiring input from several different professions. Conversely, any team covering the range of factors in the model necessarily uses a single framework for analysis and communication.
The use of this model43 is perhaps the defining characteristic of rehabilitation and distinguishes it from most other medical specialist services. Other healthcare services using the biopsychosocial model, to a greater or lesser extent, are psychiatry, including learning disability and liaison psychiatry services; palliative care; chronic pain services; geriatrics; and probably community paediatrics.
Practicing multidisciplinary teamwork
In almost all the studies and reviews of rehabilitation, the involvement of a multidisciplinary team44 is mentioned explicitly or, if not, it is implied. The important features associated with multidisciplinary teamwork are also expanded upon in the stroke rehabilitation reviews.5,6
The need for and characteristics of multidisciplinary teams has been reviewed recently.44 Studies suggest that, in healthcare, teamwork is generally associated with a better outcome,45 and an observational study on stroke rehabilitation teams46 found a relationship between better outcome and three team features:
Being oriented towards achieving tasks;
Extent of order and organization;
Use of good-quality information.
Another study on stroke rehabilitation teams47 found that effectiveness improved as the quality of team meetings improved in terms of the following:
Communication;
Coordination;
Contributions being equal;
Mutual support;
Commitment of members to team goals;
Cohesion (team spirit).
The evidence thus strongly suggests that successful rehabilitation depends upon a multidisciplinary team being involved. It is important to stress that a team is not just a collection of people who happen to be working with a specific patient; a team works together with each other over time and with many patients.44
It is also important to recognize that the team must have specialist expertise (knowledge and skills) in the problems that they see. In the case of stroke unit rehabilitation, this was related to stroke,5,6 but in other setting, it might be a condition, such as chronic pain or spinal cord injury, or a particular intervention such as assistive technology, or some other particular aspect of rehabilitation. Acquiring and maintaining specialist expertise requires continuing multidisciplinary education and training (i.e. training in areas outside each person’s limited professional field).5,6
Other important characteristics associated with effective teamwork44 include the following:
- Having regular team meetings, both
- About individual patients, and
- About team functioning and processes.
- Using the setting of goals to:
- Motivate the patient and team members.
- Ensure co-ordination of actions between different people and over time.
- Working collaboratively to
- Support each other’s interventions.
- Share information, including specific knowledge and skills.
Using structured protocols
Just as the evolution of the biomedical model of illness led to a very standardized way of approaching the biomedical aspects of illness, with great success, so a structured careful, almost obsessional approach arising from considering all factors within the biopsychosocial model of illness is an important aspect of rehabilitation’s success. The team’s use of structured approaches to common problems, be that assessing a person’s losses and abilities, or reacting to challenging behaviours, or communicating and reporting on clinical matters is part of the ‘coordinated approach’ identified in stroke services.5
The effectiveness of structured protocols is perhaps illustrated most powerfully in the field of spinal cord injury rehabilitation.36,37 Between 1935 and 1955, the prognosis for someone with a spinal cord injury was transformed from an early death, secondary to sepsis and renal failure, to returning to community living and employment with a reasonable (but not yet fully normal) life expectancy. This arose in the absence of any treatment for the injury or transformative medical advance relating to the ‘complications’ that killed people. Using structured protocols may also account for the reduced mortality associated with stroke unit care.6
Being person-centred (and family-centred)
Two characteristics of successful stroke rehabilitation were ‘routine involvement of carers in the rehabilitation process’,6 and routine provision of ‘information on stroke disease, rehabilitation, and recovery’ to both the patient and the family.5 Being person-centred is also consistent with both goal-setting and shared decision-making, both processes that are widely advocated although perhaps lacking the evidence needed to make a strong case for them.48–50
There is a close overlap between being person-centred and rehabilitation. Before discuss it further, we need to consider two groups of interventions, those which:
Are effective and applicable across the majority of rehabilitation services;
Are specific to certain conditions.
Interventions – 1
The interventions mentioned most often in reviews are exercise, education, the giving of information, and providing psychosocial support. For example, in cardiac rehabilitation, a recent review identified five core components of an effective programme.51 Three of the components are applicable to almost all conditions – exercise training, psychosocial management, and patient education. Two could be considered more specific to cardiac disease, nutritional counselling and risk factor modification, but alternatively they could be considered specific aspects of patient education. One study suggested psychosocial support was an essential part of respiratory rehabilitation,52 but there is little further evidence as to the meaning or content of ‘psychosocial support’. Exercise and education will be discussed further.
Exercise
Exercise, as used in rehabilitation research, carries two meanings. The first concerns undertaking muscular, physical activities that are associated with increased energy consumption and cardio-respiratory work. The second concerns the performance of a specified activity, usually practicing it to improve performance. Often the two will coincide, with undertaking the task-related practice of walking being a good example.
The benefits of ‘exercise’ as reported in studies may therefore arise from:
Practicing a functional activity, by repeatedly performing it, and
Undertaking more muscular work, increasing cardio-respiratory work.
There is strong evidence supporting task-oriented and task-specific training after stroke,53 with the majority of the benefit being found in improved performance of the specific task. There is probably a dose–response relationship,54,55 but in practice, the extra amount of direct therapy time needed to make a difference is too large to be feasible.56 The practice of the activity, rather than direct therapy input, is probably the main factor leading to benefit. The general principle of task-oriented training (i.e. practicing a functional activity) applies across all rehabilitation, because it is a principle underlying learning.
There is also reasonable evidence supporting the benefits associated with exercise that increases cardio-respiratory work. The benefits not only include better cardio-respiratory function,8–11 but extend well beyond cardio-respiratory fitness.10,11,39,57 Exercise may help patients with chronic fatigue,58 low back pain,59 osteoarthritis of hip or knee,39 ankle sprains,60 cardiac problems,10 chronic obstructive pulmonary disease,8 and many more conditions, often ‘with or without education and/or psychological support’.8
Education and self-management
The specific effect of education is not often studied separately. One review suggested education improved quality of life in people with cardiac disease.61
However, self-management by a patient with a long-term disabling condition depends on education, and there is evidence to support teaching self-management strategies for:
Chronic obstructive pulmonary disease,62 improving quality of life, reducing hospital admissions, but possibly increasing mortality;63
Stroke, improving quality of life;64
Fatigue in people with fatigue associated with cancer and its treatment.65,66
The common components of successful community-based programmes67 are also mostly achieved through education about:
The disease, and management of symptoms and medication;
Core self-management skills;
Exercise programme;
Self-relaxation training.
In summary, there is good evidence that practicing functional activities and undertaking cardio-respiratory exercise are both important interventions in any rehabilitation service. Education is also an important intervention, although its content is less well established; it probably always includes knowledge about the disease; its causes, prognosis, and treatments; and teaching skills in relation to self-management. Education may also cover managing the emotional aspects of the illness. Teaching about prognosis will, importantly, ensure that the expectations of the patient and family are appropriate.
Interventions – 2
The range of actions undertaken by a rehabilitation service is dramatically illustrated by the detailed description of the content of a rehabilitation programme to be undertaken in intensive care units, being evaluated in a trial. No fewer than 12 separate components were identified.68 Descriptions of other evaluated rehabilitation programmes illustrate the number and variety of actions that constitute a part of the patient’s overall rehabilitation.69,70
Thus rehabilitation is definitely a complex intervention, one in which cause–effect relationships are difficult to establish, are often non-linear, and often interact (not always beneficially). Table 1 illustrates its complexity of rehabilitation as assessed using one set of characteristics used to measure the spectrum of complexity.71
Table 1.
Complexity of rehabilitation, based on Wells et al.71
| n | Complexity characteristic | Interventions in rehabilitation |
|---|---|---|
| 1 | Number of components within it | Multiple components, both in processes and in actions undertaken |
| 2 | Its quantity and/or intensity | Depends entirely upon the patient’s specific situation and problem(s); no ‘standard’ dose of any component |
| 3 | Ability to specify the components | The component processes need to identify and then solve problems defined, but the actions needed cannot be specified at the start of rehabilitation |
| 4 | Confidence in identification of its active component | In almost every case, it is impossible to be even partially certain about the active component, and it is likely that one action influences several factors within the individual patient’s situation |
| 5 | Timing of actions involved | Multiple actions over time, with interdependence and often also dependent upon a correct sequence |
| 6 | Number of people involved in its delivery | Usually large, sometimes very large |
| 7 | Extent to which responsibility for intervention can be delineated | Low ability to delineate responsibility, and team members and others often share responsibility for actions and goals |
| 8 | Number of different (professional) groups involved | Large number of different professional groups involved, often coming from outside the ‘core team’ |
| 9 | Technical/professional skill involved | Depends upon specialist knowledge and skills in initial assessment and analysis, in practical treatment processes and in broader psychological and communication spheres |
| 10 | Extent of human interaction needed to deliver it | Almost totally dependent on human interaction; interpersonal relationships with the patient, family members, and other involved professionals are all crucial |
| 11 | Number of settings and organizations involved | May be delivered in many settings consecutively or together and will almost always involve working across geographic and organizational boundaries |
| 12 | Degree of patient involvement and participation needed | Patient engagement is essential at all times, with the exception of patients who are unconscious |
| 13 | Sphere of impact of the actions | The processes and the effects of actions both involve many people surrounding the patient |
| 14 | Ability to define and measure main outcome(s) | Many important outcomes are difficult to define precisely, and most are only measurable through patient report. E.g. Quality of life, life satisfaction, social integration. The patient’s own goals may not be measurable |
An interesting example of the difficulty in defining the ‘active ingredient’ comes from a trial of adding week-end therapy to an inpatient programme.72 The trial found a small benefit which, at first glance, might be attributed to the extra hour of therapy. However, the associated qualitative study73 found that ‘The patient-therapist interaction was more important to the patient than the amount or content of their physiotherapy’. More importantly, they reported that ‘Saturday therapy changed patients’ perceptions of weekends in rehabilitation’, so that patients in the experimental group practised more on Sundays too! The effectiveness was probably secondary to a change in the patient’s perception and expectation (of rehabilitation), not giving extra time.
The complexity of rehabilitation leads to a difficulty faced by both service providers and commissioners. There are very many potential actions that might benefit a patient, but often there is either no evidence available about their effectiveness, or the available evidence is weak or unsupportive.
When evidence of benefit is weak, inconclusive or even negative, it does not necessarily mean that the intervention should not be used (unless harm has been demonstrated). First, it may be that a small number of patients respond well, with the rest being unaffected, such that benefit cannot be detected. Second, the intervention may only help as one component of a bundle of care. Bundles of care are common, such as those for reducing infection74 or errors in surgery.75 Often the individual components in a bundle have not been tested separately.
Conundrum and solution
There is, therefore, a conundrum. Rehabilitation as a process is beneficial. Some interventions that are common to all fields of rehabilitation have been identified. But the evidence base for specific interventions in any particular group of patients is weak or absent, with few exceptions.
To resolve this conundrum, the rehabilitation team must, for each patient::
Use a collection of interventions to meet the patient’s specific needs, taking into account all aspects of his or her situation, wishes, values, and so on;
Evaluate the patient’s rehabilitation programme on a planned, ongoing basis using simple targeted measures at appropriate intervals.
That rehabilitation should be so specific to the patient follows from the trite but vital observation that every patient is different. In the context of a single drug or an operation set within a biomedical model, these differences may not matter. In rehabilitation, which is set within the biopsychosocial model, it is inevitable that many, if not, most actions need tailoring to a patient’s situation. Therefore, no two patients will have exactly the same rehabilitation package, and no two patients will respond in exactly the same, predictable way. Consequently, when evaluating rehabilitation, each patient needs a tailored package of assessments to evaluate and alter the package, the timing of these assessments also being appropriate to the situation. The process should use a few simple measures only, often to include checking for harm (e.g. sedation from a drug used).
One term used to encompass this approach is person-centred care. This phrase has many meanings. Two reviews illustrate what the phrase encompasses.
One review76 focused on the values and attitudes associated with person-centred care, suggesting it requires an organizational culture with six characteristics:
Respecting the patient’s perspective;
Being compassionate;
Recognizing the importance of interpersonal relationships both within the patient’s social groups and also between the rehabilitation team and the patient;
Prioritizing a patient’s participation in social and/or meaningful activities;
Recognizing the patient’s role as a citizen; and
Focusing on a patients strengths and abilities.
A second paper77 focused on the necessary processes, identifying eight characteristics:
An individualized set of goals derived from the patient’s preferences;
Ongoing review of the goals and planned actions;
Use of an interprofessional team (to include the patient);
Identification of a key-worker as a single point of contact;
Coordination between all people and organizations involved;
Good communication and sharing of infor-mation;
Education and training of both healthcare staff and the patient and family; and
Performance measurement and quality-control using feedback from patients.
The similarities between rehabilitation and person-centred care is obvious, and there is also evidence that care described as person-centred is effective,78,79 but not always.80,81
Finally, this person-centred approach has already been recognized in one definition of rehabilitation, adopted by the American Thoracic Society (ATS) and the European Respiratory Society (ERS)4 in 2013:
Pulmonary rehabilitation is a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors.
Conclusion
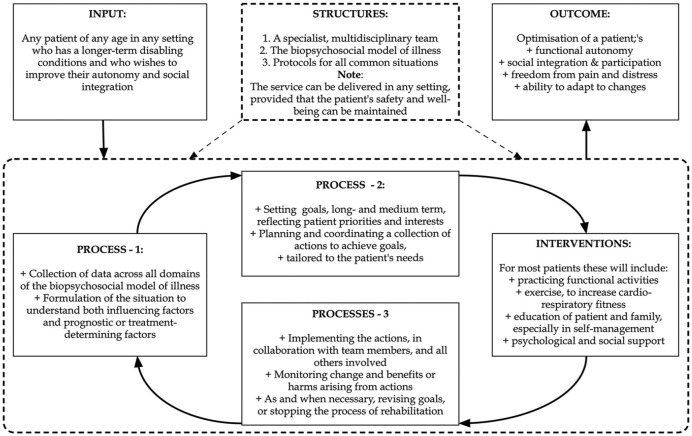
A definition of rehabilitation derived from the evidence reviewed is given in Box 2, and Figure 1 outlines the process of rehabilitation that follows from it. The important features that characterize effective rehabilitation are as follows:
Box 2.
|
An evidence-based description of effective rehabilitation
The goal. To optimize a patient’s self-rated quality of life and degree of social integration through optimizing independence in activities, minimizing pain and distress, and optimizing the ability to adapt and respond to changes in circumstances. Patients and places: Rehabilitation may • Benefit anyone with a long-term disabling illness at any stage of that illness; • Be delivered in any setting. The content. Rehabilitation: • Is a problem-solving process, framed in the context of the holistic biopsychosocial model of illness, delivered in a person-centred way, and requiring: ○ An expert, multidisciplinary team, setting collaborative team-based goals; ○ A formulation of the situation, covering all domains of the biopsychosocial model; ○ Close, collaborative working across all boundaries, professional, organizational, and geographic; ○ Ongoing monitoring of change and effects of interventions. • Will almost always use the following general approaches to management ○ Repeated practice of functional activities; ○ General exercise that increases cardio-respiratory work; ○ Education with an emphasis upon self-management; ○ Psycho-social support (not well defined yet). • and always involves a large number of specific actions tailored to the patient’s priorities and specific needs and goals, ○ Covering (if necessary) all domains of the biopsychosocial model of illness; ○ Being evaluated regularly for their benefits and harms, to determine whether they should be continued, changed, or abandoned. |
Figure 1.
Rehabilitation: who benefits, what structures are needed, what processes occur, and what is the outcome?
Basing the process on the biopsychosocial model of illness;
Having an expert multidisciplinary team, which uses structured protocols to ensure a consistent, comprehensive approach.
Undertaking a comprehensive (holistic) initial (diagnostic) assessment to achieve a full under-standing of the patient’s situation, both the factors that influence it and the factors that may determine interventions;
Using many different interventions tailored to the particular patient;
Monitoring the changes arising in association with these interventions, evaluating them against goals, and checking for potential harms.
Commissioners, organizations responsible for the quality of a rehabilitation service provided, and patients considering a rehabilitation service now have an evidence-based set of criteria to measure the quality of a service (See also supplementary figure).
Supplemental Material
Supplemental material, 20-01-15_supp_data_figure for What is rehabilitation? An empirical investigation leading to an evidence-based description by Derick T Wade in Clinical Rehabilitation
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Derick T Wade  https://orcid.org/0000-0002-1188-8442
https://orcid.org/0000-0002-1188-8442
Supplemental Material: Supplemental material for this article is available online.
References
- 1. NHS England. Commissioning guidance for rehabilitation. Publications Gateway reference no: 04919, https://www.england.nhs.uk/wp-content/uploads/2016/04/rehabilitation-comms-guid-16-17.pdf (accessed 2 December 2019).
- 2. Wade DT, De Jong B. Recent advances in rehabilitation. BMJ 2000; 320: 1355–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wade DT. Rehabilitation – a new approach: part four: a new paradigm, and its implications. Clin Rehabil 2016; 30(2): 109–118. [DOI] [PubMed] [Google Scholar]
- 4. Spruit MA, Singh SJ, Garvey C, et al. An Official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188(8): e13–e64. [DOI] [PubMed] [Google Scholar]
- 5. Langhorne P, Pollock A. What are the components of effective stroke unit care? Age Ageing 2002; 31(5): 365–371. [DOI] [PubMed] [Google Scholar]
- 6. Stroke Unit Trialists’ Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013; 9: CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Puhan MA, Gimeno-Santos E, Cates CJ, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2016; 12: CD005305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2: CD003793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dowman L, Hill CJ, Holland AE. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst Rev 2014; 10: CD006322. [DOI] [PubMed] [Google Scholar]
- 10. Anderson L, Taylor RS. Cardiac rehabilitation for people with heart disease: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev 2014; 12: CD011273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shields GE, Wells A, Doherty P, et al. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart 2018; 104: 1403–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2019; 1: CD012732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Boesen F, Norgaard M, Skjerbaek AG, et al. Can inpatient multidisciplinary rehabilitation improve health-related quality of life in MS patients on the long term – The Danish MS Hospitals Rehabilitation Study. Mult Scler. Epub ahead of print 5 November 2019. DOI: 10.1177/1352458519884244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Boesen F, Norgaard M, Trenel P, et al. Longer term effectiveness of inpatient multidisciplinary rehabilitation on health-related quality of life in MS patients: a pragmatic randomized controlled trial – The Danish MS Hospitals Rehabilitation Study. Mult Scler 2018; 24(3): 340–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rooney J, Byrne S, Heverin M, et al. A multidisciplinary clinic approach improves survival in ALS: a comparative study of ALS in Ireland and Northern Ireland. J Neurol Neurosurg Psychiatry 2015; 86(5): 496–501. [DOI] [PubMed] [Google Scholar]
- 16. Turner-Stokes L, Pick A, Nair A, et al. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database Syst Rev 2015; 12: CD004170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ferrazzoli D, Ortelli P, Zivi I, et al. Efficacy of intensive multidisciplinary rehabilitation in Parkinson’s disease: a randomised controlled study. J Neurol Neurosurg Psychiatry 2018; 89(8): 828–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nordstrom P, Thorngren KG, Hommel A, et al. Effects of geriatric team rehabilitation after hip fracture: meta-analysis of randomized controlled trials. J Am Med Dir Assoc 2018; 19(10): 840–845. [DOI] [PubMed] [Google Scholar]
- 19. Handoll HHG, Cameron ID, Mak JCS, et al. Multi-disciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev 2009; 4: CD007125. [DOI] [PubMed] [Google Scholar]
- 20. Khan F, Ng L, Gonzalez S, et al. Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database Syst Rev 2008; 2: CD004957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev 2014; 9: CD000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marin TJ, Van Eerd D, Irvin E, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Syst Rev 2017; 6: CD002193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Olsson Moller U, Beck I, Ryden L, et al. A comprehensive approach to rehabilitation interventions following breast cancer treatment – a systematic review of systematic reviews. BMC Cancer 2019; 19(1): 472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Scott DA, Mills M, Black A, et al. Multidimensional rehabilitation programmes for adult cancer survivors. Cochrane Database Syst Rev 2013; 3: CD007730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tipping CJ, Harrold M, Holland A, et al. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med 2017; 43(2): 171–183. [DOI] [PubMed] [Google Scholar]
- 26. Arias-Fernandez P, Romero-Martin M, Gomez-Salgado J, et al. Rehabilitation and early mobilization in the critical patient: systematic review. J Phys Ther Sci 2018; 30(9): 1193–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fuke R, Hifumi T, Kondo Y, et al. Early rehabilitation to prevent post-intensive care syndrome in patients with critical illness: a systematic review and meta-analysis. BMJ Open 2018; 8: e019998, https://bmjopen.bmj.com/content/8/5/e019998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. Cochrane Database Syst Rev 2018; 3: CD010754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Doig E, Fleming J, Kuipers P, et al. Comparison of rehabilitation outcomes in day hospital and home settings for people with acquired brain injury – a systematic review. Disabil Rehabil 2010; 32(25): 2061–2077. [DOI] [PubMed] [Google Scholar]
- 30. Forster A, Young J, Langhorne P. Systematic review of day hospital care for elderly people. BMJ 1999; 318(7187): 837–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev 2013; 2: CD004294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Langhorne P, Baylan S. Early supported discharge services for people with acute stroke. Cochrane Database Syst Rev 2017; 7: CD000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Blair J, Corrigall H, Angus N, et al. Home versus hospital-based cardiac rehabilitation: a systematic review. Rural Remote Health 2011; 11(2): 1532, https://www.rrh.org.au/journal/article/1532/ [PubMed] [Google Scholar]
- 34. Hillier S, Inglis-Jassiem G. Rehabilitation for community-dwelling people with stroke: home or centre based? A systematic review. Int J Stroke 2010; 5: 178–186. [DOI] [PubMed] [Google Scholar]
- 35. Verweij L, van de Korput E, Daams JG, et al. Effects of postacute multidisciplinary rehabilitation including exercise in out-of-hospital settings in the aged: systematic review and meta-analysis. Arch Phys Med Rehabil 2019; 100(3): 530–550. [DOI] [PubMed] [Google Scholar]
- 36. Donovan WH. Spinal cord injury – past, present, and future. J Spinal Cord Med 2007; 30: 85–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Silver JR. History of the treatment of spinal injuries. Postgrad Med J 2005; 81(952): 108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bunketorp-Käll L, Lundgren-Nilsson Å, Samuelsson H, et al. Long-term improvements after multimodal rehabilitation in late phase after stroke. Stroke 2017; 48: 1916–1924. [DOI] [PubMed] [Google Scholar]
- 39. Hurley M, Dickson K, Hallett R, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev 2018; 4: CD010842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Madureira BG, Pereira MG, Avelino PR, et al. Efeitos de programas de reabilitação multidisciplinar no tratamento de pacientes com doença de Alzheimer: uma revisão sistemática. [Effects of multidisciplinary rehabilitation programs on treatment of patients with Alzheimer’s disease: a systematic review]. Cad Saúde Colet 2018; 26: 222–232, http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414-462X2018000200222 [Google Scholar]
- 41. Sá CDC, Silva DFD, Bigongiari A, et al. Eficácia da reabilitação cognitiva na melhoria e manutenção das atividades de vida diária em pacientes com doença de Alzheimer: uma revisão sistemática da literatura [Efficacy of cognitive rehabilitation in improving and maintaining daily living activities in patients with Alzheimer’s disease: a systematic review of literature]. J Bras Psiquiatr 2019; 68: 153–160, http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0047-20852019000300153 [Google Scholar]
- 42. Salakari MRJ, Surakka T, Nurminen R, et al. Effects of rehabilitation among patients with advances cancer: a systematic review. Acta Oncol 2015; 54(5): 618–628. [DOI] [PubMed] [Google Scholar]
- 43. Wade DT, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil 2017; 31(8): 995–1004. [DOI] [PubMed] [Google Scholar]
- 44. Wade DT. A teamwork approach to neurological rehabilitation. In: Dietz V, Ward NS. (eds) Oxford textbook of neurorehabilitation. 2nd ed Oxford: Oxford University Press, 2020, pp. 9–21. [Google Scholar]
- 45. Choi BCK, Pak AP. Multidisciplinary, interdisciplinary, and transdisciplinary in health research, services, education, and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med 2006; 29: 351–364. [PubMed] [Google Scholar]
- 46. Strasser DC, Falconer JA, Herrin JS, et al. Team functioning and patient outcomes in stroke rehabilitation. Arch Phys Med Rehabil 2005; 86(3): 403–409. [DOI] [PubMed] [Google Scholar]
- 47. Tyson SF, Burton L, McGovern A. The effect of a structured model for stroke rehabilitation multi-disciplinary team meetings on functional recovery and productivity: a phase I/II proof of concept study. Clin Rehabil 2015; 29(9): 920–925. [DOI] [PubMed] [Google Scholar]
- 48. Levack WMM, Weatherall M, Hay-Smith EJC, et al. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst Rev 2015; 7: CD009727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. Med Decis Making 2015; 35(1): 114–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rose A, Rosewilliam S, Soundy A. Shared decision making within goal setting in rehabilitation settings: a systematic review. Patient Educ Couns 2017; 100(1): 65–75. [DOI] [PubMed] [Google Scholar]
- 51. Kabboul NN, Tomlinson G, Francis TA, et al. Comparative effectiveness of the core components of cardiac rehabilitation on mortality and morbidity: a systematic review and network meta-analysis. J Clin Med 2018; 7(12): E514, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306907/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lacasse Y, Guyatt GH, Goldstein RS. The components of a respiratory rehabilitation program: a systematic overview. Chest 1997; 111(4): 1077–1088. [DOI] [PubMed] [Google Scholar]
- 53. Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014; 9(2): e87987, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0087987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Veerbeek JM, Koolstra M, Ket JC, et al. Effects of augmented exercise therapy on outcome of gait and gait-related activities in the first 6 months after stroke. Stroke 2011; 42(11): 3311–3315. [DOI] [PubMed] [Google Scholar]
- 55. Lohse KR, Lang CE, Boyd LA. Is more better? Using metadata to explore dose–response relationships in stroke rehabilitation. Stroke 2014; 45(7): 2053–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Schneider EJ, Lannin NA, Ada L, et al. Increasing the amount of usual rehabilitation improves activity after stroke: a systematic review. J Physiother 2016; 62(4): 182–187. [DOI] [PubMed] [Google Scholar]
- 57. Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016; 1: CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Larun L, Brurberg KG, Odgaard-Jensen J, et al. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst Rev 2017; 4: CD003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Searle A, Spink M, Ho A, et al. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin Rehabil 2015; 29(12): 1155–1167. [DOI] [PubMed] [Google Scholar]
- 60. Bleakley CM, Taylor JB, Dischiavi SL, et al. Rehabilitation exercises reduce reinjury post ankle sprain, but the content and parameters of an optimal exercise program have yet to be established: a systematic review and meta-analysis. Arch Phys Med Rehabil 2019; 100(7): 1367–1375. [DOI] [PubMed] [Google Scholar]
- 61. Anderson L, Brown JPR, Clark AM, et al. Patient education in the management of coronary heart disease. Cochrane Database Syst Rev 2017; 6: CD008895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Murphy LA, Harrington P, Taylor SJ, et al. Clinical-effectiveness of self-management interventions in chronic obstructive pulmonary disease: an overview of reviews. Chron Respir Dis 2017; 14(3): 276–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lenferink A, Brusse-Keizer M, van der Valk PD, et al. Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017; 8: CD011682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Fryer CE, Luker JA, McDonnell MN, et al. Self management programmes for quality of life in people with stroke. Cochrane Database Syst Rev 2016; 8: CD010442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cheng KKF, Lim YTE, Koh ZM, et al. Home-based multidimensional survivorship programmes for breast cancer survivors. Cochrane Database Syst Rev 2017; 8: CD011152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Huang J, Han Y, Wei J, et al. The effectiveness of the Internet-based self-management program for cancer-related fatigue patients: a systematic review and meta-analysis. Clin Rehabil 2019; 34(3): 287–298. [DOI] [PubMed] [Google Scholar]
- 67. Mulligan H, Wilkinson A, Chen D, et al. Components of community rehabilitation programme for adults with chronic conditions: a systematic review. Int J Nurs Stud 2019; 97: 114–129. [DOI] [PubMed] [Google Scholar]
- 68. Ramsay P, Salisbury LG, Merriweather JL, et al. A rehabilitation intervention to promote physical recovery following intensive care: a detailed description of construct development, rationale and content together with proposed taxonomy to capture processes in a randomised controlled trial. Trials 2014; 15: 38, http://www.trialsjournal.com/content/15/1/38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Schmidt AM, Terkildsen Maindal H, Laurberg TB, et al. The Sano study: justification and detailed description of a multidisciplinary biopsychosocial rehabilitation programme in patients with chronic low back pain. Clin Rehabil 2018; 32(11): 1431–1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Westerhof-Evers HJ, Visser-Keizer AC, Fasotti L, et al. Social cognition and emotion regulation: a multifaceted treatment (T-ScEmo) for patients with traumatic brain injury. Clin Rehabil 2019; 33(5): 820–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wells M, Williams B, Treweek S, et al. Intervention description is not enough: evidence from an in-depth multiple case study on the untold role and impact of context in randomised controlled trials of seven complex interventions. Trials 2012; 13(1): 95, http://www.trialsjournal.com/content/13/1/95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Peiris CL, Taylor NF, Shields N. Additional Saturday Allied Health Services increase habitual physical activity among patients receiving inpatient rehabilitation for lower limb orthopedic conditions: a randomized controlled trial. Arch Phys Med Rehabil 2012; 93(8): 1365–1370. [DOI] [PubMed] [Google Scholar]
- 73. Peiris CL, Taylor NF, Shields N. Patients value patient-therapist interactions more than the amount or content of therapy during inpatient rehabilitation: a qualitative study. J Physiother 2012; 58(4): 261–268. [DOI] [PubMed] [Google Scholar]
- 74. Hsu C-D, Cohn I, Caban R. Reduction and sustainability of cesarean section surgical site infection: an evidence-based, innovative, and multidisciplinary quality improvement intervention bundle program. Am J Infect Control 2016; 44(11): 1315–1320. [DOI] [PubMed] [Google Scholar]
- 75. Chaudhary N, Varma V, Kapoor S, et al. Implementation of a surgical safety checklist and postoperative outcomes: a prospective randomized controlled study. J Gastrointest Surg 2015; 19(5): 935–942. [DOI] [PubMed] [Google Scholar]
- 76. Waters RA, Buchanan A. An exploration of person-centred concepts in human services: a thematic analysis of the literature. Health Policy 2017; 121(10): 1031–1039. [DOI] [PubMed] [Google Scholar]
- 77. The American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: a definition and essential elements. J Am Geriatr Soc 2016; 64(1): 15–18. [DOI] [PubMed] [Google Scholar]
- 78. Olsson L-E, Jakobsson Ung E, Swedberg K, et al. Efficacy of person-centred care as an intervention in controlled trials – a systematic review. J Clin Nurs 2013; 22(3-4): 456–465. [DOI] [PubMed] [Google Scholar]
- 79. Ballard C, Corbett A, Orrell M, et al. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: a cluster-randomised controlled trial. PLoS Med 2018; 15(2): e1002500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Spoorenberg SLW, Wynia K, Uittenbroek RJ, et al. Effects of a population-based, person-centred and integrated care service on health, wellbeing and self-management of community-living older adults: a randomised controlled trial on Embrace. PLoS ONE 2018; 13(1): e0190751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Guidetti S, Ranner M, Tham K, et al. A ‘client-centred activities of daily living’ intervention for persons with stroke: one-year follow-up of a randomized controlled trial. J Rehabil Med 2015; 47(7): 605–611, http://www.medicaljournals.se/jrm/content/html/10.2340/16501977-1981 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 20-01-15_supp_data_figure for What is rehabilitation? An empirical investigation leading to an evidence-based description by Derick T Wade in Clinical Rehabilitation