Abstract
Background
Maternal near miss refers to a very ill pregnant or delivered woman who nearly died but survived a complication during pregnancy, childbirth, or within 42 days of termination of pregnancy. Maternal death; the most catastrophic end is frequently described as just “tip of the iceberg,” whereas maternal near-miss as the “base.” Therefore, this study aimed at assessing the factors associated with maternal near-miss among women admitted in public hospitals of West Arsi zone, Ethiopia.
Methods
A facility-based unmatched case-control study was conducted from Mar 1 to Apr 30, 2019. Three hundred twenty-one (80 cases and 241 controls) study participants were involved in the study. Cases were recruited consecutively as they present, whereas controls were selected by systematic sampling method. Cases were women admitted to hospitals during pregnancy, delivery, or within 42 days of termination of pregnancy and fulfilled at least one of the maternal near-miss disease-specific criteria, while controls were women admitted and gave birth by normal vaginal delivery. The interviewer-administered structured questionnaire and data abstraction tool was used to collect data. Data were entered Epi data 3.1 and then transferred into SPSS 20 for analysis. Multivariable logistic regression was used, and the significance level was declared at p value ≤ 0.05.
Results
The major maternal near-miss morbidities were severe obstetric hemorrhage (32.5%), pregnancy-induced hypertensive disorders (31.3%), and obstructed labor (26.3%), followed by 6.3% and 3.8% of severe anemia and pregnancy-induced sepsis, respectively. The odds of maternal near miss were statistically significantly associated with women's lack of formal education [AOR = 2.24, 95% CI: (1.17, 4.31)]. Not attending antenatal care [AOR = 3.71, 95% CI: (1.10, 12.76)], having prior history of cesarean section [AOR = 3.53, 95% CI: (1.49, 8.36)], any preexisting chronic medical disorder [AOR = 2.04, 95% CI: (1.11, 3.78)], and having experienced first delay [AOR = 5.74, 95% CI: (2.93, 11.2)].
Conclusions
Maternal education, antenatal care, chronic medical disorders, previous cesarean section, and first delay of obstetric care-seeking were identified as factors associated with maternal near-miss morbidity. Therefore, this finding implies the need to get better with those factors, to preclude severe maternal complications and subsequent maternal mortality.
1. Introduction
Maternal death is the most catastrophic end that could happen to a pregnant woman. It is frequently described as just “tip of the iceberg” while maternal morbidity as the “base,” and for every woman who dies, many more will survive but often suffer from lifelong disabilities [1, 2]. World Health Organization (WHO) defines the maternal near-miss event as “a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy” [3, 4]. Thus, maternal near miss is increasingly used as an indicator of the quality of obstetric care and clinical practice. The practical implementation of this concept should provide a significant contribution to reduce maternal deaths and improve maternal health [4–6].
Globally, 303,000 maternal deaths were occurred in 2015, with the highest-burden being in sub-Saharan African countries [7]. In other words, women in sub-Saharan Africa have 1 in 39 risk of dying in childbirth compared to 1 in 3,800 in industrialized countries in their lifetime [5, 8]. Maternal mortality continues to be of great public health importance because many more women experience life-threatening complications [9, 10], during pregnancy, delivery, and postpartum complications [11]. Despite all the efforts on maternal health care, maternal near-miss, disabilities, and deaths were exceptionally high in developing countries, including Ethiopia [12].
Ethiopia is one of sub-Saharan Africa countries with the highest maternal mortality rate. According to the Ethiopian Demographic and Health Survey (EDHS, 2016) report, MMR is 412 per 100,000 live births, and for every maternal death, 10% to 15% of the women develop disability from pregnancy and pregnancy-related complications [13]. Ethiopia is one of five countries that account for half of the maternal deaths globally [14]; about 20,000 women die each year from pregnancy and childbirth complications [15]. A study done at Ayder Referral Hospital in Tigray showed that 22.7% near misses and MMR of 427 per 100,000 live births [16]. Besides, a retrospective review done in Ethiopia at Debre-Markos referral hospital found that 403 (29.7%) near-miss cases from a total of 1355 case notes reviewed in a five-year period [17].
Maternal near-miss complications are numerous and are estimated to be around 12 times more frequent than maternal deaths in Ethiopia [18]. However, the factors associated with it are not well-studied using the standardized WHO criteria to measure maternal near-miss. In addition, previously published studies conducted in the country relied on patient records review to assess factors of maternal near-miss [15–18]. Hence, these studies might be subjected to information bias due to incompleteness and poor quality of secondary data at the health facility. And also, the study design used was cross-sectional that has known limitations of ascertaining cause-effect relationships [16, 18]. Therefore, this study was carried out to assess factors associated with maternal near-miss among women admitted in public hospitals of West Arsi zone, Oromia region, Ethiopia, in 2019. The evidence generated through this study would be used by the local health planner, stakeholders working on maternal health programs.
2. Materials and Methods
2.1. Study Setting and Period
The study was conducted in West Arsi zone public hospitals from Mar 1 to Apr 30, 2019. The zones are found in Oromia regional state, Ethiopia. According to the 2007 national household census, the zone has a total population of 1,964,038, of whom 990,295 are women. The total number of women of reproductive age (15-49 years) is estimated to be 434,412 [19]. In the zone, there are four government hospitals, Shashemene Referral Hospital, Melka Oda General Hospital, Dodola General Hospital, and Kokosa Primary Hospital. And three private/NGO hospitals (Negele Arsi General Hospital, Feya Primary Hospital, and Gambo Primary Hospital). Additionally, there are 81 functional health centers, 351 functional health posts, 179 private clinics, 1NGO clinic, and 95 pharmacy/drug shop.
2.2. Study Design
An unmatched case-control study design was employed.
2.3. Source and Study Populations
Women who were admitted at selected hospitals during pregnancy, labor, or within the first 42 days of termination of pregnancy.
2.3.1. Selection of Cases
Cases were women who admitted to the hospitals due to pregnancy-related complications, deliver/abortion, or within 42 days of termination of pregnancy. And those who fulfill at least one of the five diagnostic maternal near-miss validated disease-specific criteria proposed by WHO, Filippi et al., and Say et al. [4, 20, 21]. Obstructed labor (uterine rupture, impending rupture like prolonged labor with previous C.S., emergency C.S.), hemorrhage (severe obstetric hemorrhage leading to shock, emergency hysterectomy, coagulation defects, and/or blood transfusion of at least one units), pregnancy-induced hypertension disorders (severe preeclampsia or eclampsia), sepsis (septic abortion, infections including hyper or hypothermia or a clear source of infection and clinical signs of septic shock), and severe anemia (including low hemoglobin <6 g/dl or clinical signs of severe anemia in women without hemorrhage).
2.3.2. Selection of Controls
Controls were those women who admitted to the same hospital with normal labor and gave birth in normal vaginal delivery without complications.
2.4. Sample Size Determination
The sample size was calculated using Epi Info version 7 software package designed for an unmatched case-control study. The following assumptions were made during calculating sample size: 95% confidence level, 80% power, and a case to control the ratio of 1 : 3. The sample size calculated for main exposure variables associated with near maternal miss using variables from different kinds of literature. Then, variable resulted in a high sample size were taken. Delay to reach the place of health care was the main exposure variable for maternal near miss that provided the maximum sample size, which was taken from the study done in Northern Ethiopia [22]. According to the study, 40.5% of controls delay for >60 minutes in reaching the final place of care, while 60.2% of cases delay for >60 minutes. This gives a total sample size of 292 (73 cases and 219 controls). By taking a 10% nonresponse rate, the final sample size was 321 (80 cases and 241controls).
2.5. Sampling Technique
The sample size was proportionally allocated for each public hospitals in the zone based on their number client flow. Then, cases were recruited consecutively as they present, whereas controls were selected by systematic sampling method with an interval of five (k = 1309/241 = 5).
2.6. Data Collection Tools
The questionnaire and near-miss data abstraction tools were adapted from different literature [4, 15, 21]. For the identification of cases, the WHO disease-specific criteria were used. The near-miss data abstraction tool was constructed for the case and control identification from medical records. The questionnaire was composed of four main parts: -mothers' socioeconomic and demographic factors, reproductive health and obstetric characteristics, previous chronic medical history, and obstetric health care delays.
2.7. Data Collection Technique and Procedure
Exit interviews were conducted by trained data collectors using structured; pretested questionnaires. Identifying cases and collecting information which could not be obtained by interview like the diagnosis of obstetric complications, laboratory investigation, and management were extracted from patient medical records and discharge summaries. Eight midwife nurses who have experience on obstetric care (two midwives per hospital) and who can speak the local language were recruited as data collectors. Four nurses who have bachelor's degree holders were recruited as supervisors.
2.8. Operational Definitions
2.8.1. Maternal Near Miss
Admitted women with at least one of the following obstetric diagnosis: severe preeclampsia or eclampsia, severe hemorrhage, dystocia (uterine rupture, impending uterine rupture like prolonged labor with previous cesarean section, and emergency C.S. delivery), severe anemia (hemoglobin<6 g/dl), and sepsis (puerperal sepsis, chorioamnionitis, and septic abortion) [3, 4, 21].
2.8.2. The First Phase (Referral Status)
The period between arrival at the first health facility and arrival at the current study hospital. Accepted time spent between arrival and the first examination is usually set not more than 60 minutes.
2.8.3. The Second Phase
The time spent between arrival at the final current study hospital and the first examination, followed by the time spent between the first examinations and receiving the first care. Accepted time spent between examination and receiving first care is usually set not more than 30 minutes. Therefore, the third delay is a delay in at least one phase delay of the two-third delay phases. The delay in referral from various health facilities and multiple referrals were included in the third delay within intermediate health facilities.
2.8.4. Well-Birth Prepared
Defined as having taken at least 3 of the four actions (bought childbirth materials, saved money, identified transport, identified skilled provider or health facility).
2.9. Data Quality Assurance Techniques
Training was given for data collectors and supervisors for one day on interview techniques, confidentiality of the information, and informed consent. The pretest was conducted in Robe hospital, using 5% of the sample size who fulfill the inclusion criteria, and feedbacks were incorporated accordingly. The data completeness and consistency were checked by supervisors on a daily basis.
2.10. Data Management and Analysis
The data were entered and cleaned using Epi data version 3.1, then exported to SPSS version 20 for further analysis. Univariate analysis: proportions, frequencies, and averages were calculated for study variables to compare cases and controls. Bivariable and multivariable logistic regression were to identify predictor variables for maternal near miss. All variables having a p value ≤ 0.25 in the bivariate analysis were considered for multivariable logistic regression model. The Hosmer and Lemeshow goodness of fit test was used to determine whether the model adequately describes the data and the model adequately fitted for the final model (p = 0.108). Confounders were controlled with multivariable logistic regression, and multicollinearity was also checked with a correlation matrix. Adjusted odds ratio (AOR) with 95% CI was estimated to assess the presence and strength of associations, and statistical significance was declared at a p value ≤ 0.05.
3. Results
3.1. Sociodemographic and Economic Characteristics of Women
The mean (±SD) age of cases and controls was 27.56 (±6.0) and 27.0 (±5.43) years, respectively. However, the mean age difference between cases and controls was not statistically significant p = 0.105. The majority of cases were an urban residence, 53 (66.2%), and nearly half of controls 116 (48.1%) were rural residents. Of the total respondents, 294 (91.6%) of them were currently in marital union. Concerning educational status, 38 (47.5%) cases and 51 (21.2%) controls had no formal education. Regarding transportation, 48 (60%) cases and 180 (74.7%) controls have access to transportation (Table 1).
Table 1.
Sociodemographic and economic characteristics of women admitted in Western Arsi zone public hospitals, Ethiopia, 2020.
| Characteristics | Cases (n = 80) | Controls (n = 241) | Total (n = 321) | Chi-square | p value |
|---|---|---|---|---|---|
| Residence | |||||
| Rural | 53 (66.2) | 116 (48.1) | 169 (52.6) | 7.908 | 0.005 |
| Urban | 27 (33.8) | 125 (51.9) | 152 (47.4) | ||
| Women's age | |||||
| <20 year | 9 (11.2) | 29 (12.0) | 38 (11.8) | 4.499 | 0.105 |
| 20-34 year | 52 (65.0) | 179 (74.3) | 231 (72.0) | ||
| ≥35 year | 19 (23.8) | 33 (13.7) | 52 (16.2) | ||
| Mean (±SD) | 27.56 (±6.0) | 27.0 (±5.43) | |||
| Current marital status | |||||
| Not in marital union | 8 (10.0) | 19 (7.9) | 27 (8.4) | 0.349 | 0.555 |
| In marital union | 72 (90.0) | 222 (92.1) | 294 (91.6) | ||
| Women's education | |||||
| No formal education | 38 (47.5) | 51 (21.2) | 89 (27.7) | 24.97 | <0.001 |
| Primary education | 29 (36.2) | 98 (40.7) | 127 (39.6) | ||
| Secondary education | 11 (13.8) | 63 (26.1) | 74 (23.0) | ||
| Higher education | 2 (2.5) | 29 (12.0) | 31 (9.7) | ||
| Husband's education (n = 313) | |||||
| No formal education | 21 (27.3) | 55 (23.3) | 76 (24.3) | 5.299 | 0.151 |
| Primary education | 32 (41.5) | 78 (33.0) | 110 (35.1) | ||
| Secondary education | 16 (20.8) | 53 (22.5) | 69 (22.0) | ||
| Higher education | 8 (10.4) | 50 (21.2) | 58 (18.6) | ||
| Monthly income | |||||
| ≤1000 ETB | 29 (36.2) | 57 (23.7) | 86 (26.8) | 5.639 | 0.131 |
| 1001–2000 ETB | 15 (18.8) | 46 (19.0) | 61 (19.0) | ||
| 2001–3000 ETB | 12 (15.0) | 38 (15.8) | 50 (15.6) | ||
| ≥3001 ETB | 24 (30.0) | 100(41.5) | 124 (38.6) | ||
| Distance to nearest F.H. | |||||
| >60 minutes | 31 (38.8) | 51 (21.2) | 82 (25.5) | 9.769 | 0.002 |
| ≤60 minutes | 49 (61.2) | 190 (78.8) | 239 (74.5) | ||
| Road access | |||||
| Yes | 61 (76.2) | 201 (83.4) | 262 (81.6) | 2.048 | 0.152 |
| No | 19 (23.8) | 40 (16.6) | 59 (18.4) | ||
| Transportation access | |||||
| Yes | 48 (60.0) | 180 (74.7) | 228 (71.1) | 5.305 | 0.021 |
| No | 32 (40.0) | 61 (25.3) | 93 (28.9) |
3.2. Reproductive and Obstetric Related Characteristics of Study Participants
The proportion of early marriage among near-miss groups and control groups was comparable 31.2% and 29.2%, respectively. In terms of the history of caesarian section, 18 (22.5%) cases and 21 (8.7%) controls had at least one history of the previous caesarian section. Likewise, the history of prior abortion was 6.2% and 12% among cases and controls, respectively (Table 2).
Table 2.
Reproductive and obstetric characteristics of women admitted in Western Arsi zone public hospitals, Ethiopia, 2020.
| Characteristics | Cases (n = 80) | Controls (n = 241) | Total (n = 321) | Chi-square | p value |
|---|---|---|---|---|---|
| ANC visits | |||||
| No visit at all | 47 (58.8) | 48 (19.9) | 95 (29.6) | 43.469 | <0.001 |
| At least one visit | 33 (41.2) | 193 (80.1) | 226 (70.4) | ||
| Timing of ANC booking (n = 226) | |||||
| Early booking (≤12 weeks) | 6 (18.2) | 57 (29.5) | 63 (27.9) | 1.806 | 0.179 |
| Late booking (>12 weeks) | 27 (81.8) | 136 (70.5) | 163 (72.1) | ||
| Gravidity | |||||
| 1 | 27 (33.8) | 44 (18.3) | 71 (22.1) | 8.369 | 0.015 |
| 2-4 | 33 (41.2) | 123 (51.0) | 156 (48.6) | ||
| ≥5 | 20 (25.0) | 74 (30.7) | 94 (29.3) | ||
| Parity | |||||
| 0 | 27 (33.8) | 52 (21.6) | 79 (24.6) | 4.957 | 0.084 |
| 1-4 | 36 (45.0) | 134 (55.6) | 170 (53.0) | ||
| ≥5 | 17 (21.2) | 55 (22.8) | 72 (22.4) | ||
| Ever had abortion | |||||
| Yes | 5 (6.2) | 29 (12.0) | 34 (10.6) | 2.121 | 0.145 |
| No | 75 (93.8) | 212 (88.0) | 287 (89.4) | ||
| History of previous cesarean section | |||||
| Yes | 18 (22.5) | 21 (8.7) | 39 (12.1) | 10.695 | 0.001 |
| No | 62 (77.5) | 220 (91.3) | 282 (87.9) | ||
| Undergone female genital mutilation | |||||
| Yes | 60 (75.0) | 170 (70.5) | 230 (71.7) | 0.588 | 0.443 |
| No | 20 (25.0) | 71 (29.5) | 91 (28.3) | ||
| Age at first marriage(n = 313) | |||||
| Age ≤ 18 years | 24 (31.2) | 69 (29.2) | 93 (29.7) | 0.104 | 0.747 |
| Age > 18 years | 53 (68.8) | 167 (70.8) | 220 (70.3) | ||
| Age at first pregnancy | |||||
| <16 | 9 (11.2) | 12 (5.0) | 21 (6.5) | 3.887 | 0.143 |
| 16-19 | 33 (41.2) | 104 (43.2) | 137 (42.7) | ||
| ≥20 | 38 (47.5) | 125 (51.9) | 163 (50.8) | ||
| Birth interval (n = 268) | |||||
| ≥24 months | 44 (83.0) | 176 (81.9) | 220 (82.1) | 0.039 | 0.844 |
| <24 months | 9 (17.0) | 39(18.1) | 48 (17.9) | ||
| Current pregnancy planned | |||||
| Yes | 66 (82.5) | 209 (86.7) | 275 (85.7) | 0.872 | 0.350 |
| No | 14 (17.5) | 32 (13.3) | 46 (14.3) | ||
| Well birth prepared | |||||
| Yes | 39 (48.8) | 123 (51.0) | 162 (50.5) | 0.126 | 0.723 |
| No | 41 (51.2) | 118 (49.0) | 159 (49.5) |
3.3. Preexisting Chronic Medical Disorders and Maternal Obstetric Health Care Delays
History of at least one chronic preexisting medical disorder was reported in half (51.2%) of cases and one third (32.8%) of controls. Majority 220 (68.5%) were self-referred from home, while 40% of cases and 28.6% of controls referred from health facilities, respectively.
More than half (55%) of near-miss cases delayed >4 hours for deciding to go to the health facility compared to controls (12.4%) (Table 3).
Table 3.
Preexisting chronic medical disorders and maternal obstetric health care delays among women admitted in Western Arsi zone public hospitals, Ethiopia, 2020.
| Characteristics | Cases (n = 80) | Controls (n = 241) | Total (n = 321) | Chi-square | p value |
|---|---|---|---|---|---|
| Referral status | |||||
| Health facility referred | 32 (40.0) | 69 (28.6) | 101 (31.5) | 3.600 | 0.058 |
| Self-referred from home | 48 (60.0) | 172 (71.4) | 220 (68.5) | ||
| Means of transportation | |||||
| Ambulance | 32 (40.0) | 73 (30.3) | 105 (32.7) | 2.573 | 0.109 |
| Other than ambulance∗∗ | 48 (60.0) | 168 (69.7) | 216 (67.3) | ||
| First delay | |||||
| Yes | 44 (55.0) | 30 (12.4) | 74 (23.1) | 61.308 | <0.001 |
| No | 36 (45.0) | 211 (87.6) | 247 (76.9) | ||
| Second delay | |||||
| Yes | 24 (30.0) | 56 (23.2) | 80 (24.9) | 1.468 | 0.226 |
| No | 56 (70.0) | 185 (76.8) | 241 (75.1) | ||
| Third delay | |||||
| Yes | 21 (26.2) | 54 (22.4) | 75 (23.4) | 0.495 | 0.481 |
| No | 59 (73.8) | 187 (77.6) | 246 (76.6) | ||
| Previous chronic hypertension | |||||
| Yes | 16 (20.0) | 26 (10.8) | 42 (13.1) | 4.482 | 0.034 |
| No | 64 (80.0) | 215 (89.2) | 279 (86.9) | ||
| Previous anemia | |||||
| Yes | 22 (27.5) | 40 (16.6) | 62 (19.3) | 4.581 | 0.032 |
| No | 58 (72.5) | 201(83.4) | 259 (80.7) | ||
| HIV positive | |||||
| Yes | 9 (11.2) | 12 (5.0) | 21 (6.5) | 3.863 | 0.049 |
| No | 71 (88.8) | 229 (95.0) | 300 (93.5) | ||
| History of maternal cardiac disease | |||||
| Yes | 12 (15.0) | 15 (6.2) | 27 (8.4) | 6.005 | 0.014 |
| No | 68 (85.0) | 226 (93.8) | 294 (91.6) | ||
| History of diabetic mellitus | |||||
| Yes | 9 (11.2) | 17 (7.1) | 26 (8.1) | 1.421 | 0.233 |
| No | 71 (88.8) | 224 (92.9) | 295 (91.9) | ||
| At least one preexisting medical problem | |||||
| Yes | 41 (51.2) | 79 (32.8) | 120 (37.4) | 8.753 | 0.003 |
| No | 39 (48.8) | 162 (67.2) | 201 (62.6) |
∗∗Other than ambulance includes public transport, private transport, on the walk, and carried by men.
3.4. Clinical Characteristics of Near Misses
Among 80 near-miss cases, the most complications were severe obstetric hemorrhage(32.5%), followed by severe pregnancy-induced hypertensive disorders (31.3%). Most of near misses (79%) had occurred before hospital admission. The remaining 21% occurred during or after admission to the hospitals (Figure 1).
Figure 1.
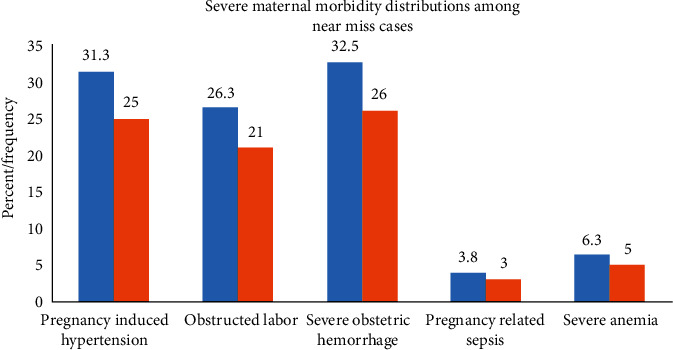
Maternal morbidity among near-miss cases admitted in Western Arsi zone public hospitals, Ethiopia, 2020.
3.5. Factors Associated with Maternal Near Misses among Women Admitted in Public Hospitals
Women with no formal education had two times [AOR = 2.24, 95% CI: (1.17, 4.31)] higher odds of developing maternal near-miss compared to women with formal education. Similarly, women who did not have an antenatal care follow-up had 3.71 times [AOR = 3.71, 95% CI: (1.10, 12.76)] greater odds of developing maternal near-miss compared to women who had four and more antenatal visits. The odds of maternal near-miss was 3.53 times [AOR = 3.53, 95% CI: (1.49, 8.36)] greater among women with a history of previous cesarean section as compared to women who had no history of previous cesarean section.
Moreover, women who had at least one preexisting medical disorder had two times [AOR = 2.04, 95% CI: (1.11, 3.78)] increased odds of maternal near miss compared to their counterparts. Delay to seek obstetric health care (first delay) was strongly associated with maternal near miss. The odds of maternal near-miss among women who delayed more than 4 hours at home were 5.74 times higher compared to those who decided to seek health care within 4 hours [AOR = 5.74, 95% CI: (2.93, 11.2)] (Table 4).
Table 4.
Factors associated with maternal near miss in multivariable logistic regression analysis, among women in West Arsi zone public hospitals, Ethiopia, 2019.
| Factor variables | Maternal near miss | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Cases (n = 80) | Control (n = 241) | |||
| Place of residence | ||||
| Rural | 53 (66.2) | 116 (48.1) | 2.11 (1.24, 3.58) | 0.64 (0.31, 1.34) |
| Urban® | 27 (33.8) | 125 (51.9) | 1.00 | 1.00 |
| Maternal education | ||||
| No formal education | 38 (47.5) | 51 (21.2) | 3.37 (1.97, 5.76) | 2.24 (1.17, 4.31) ∗∗ |
| Formal education® | 42 (52.5) | 190 (78.8) | 1.00 | 1.00 |
| Monthly income | ||||
| ≤1000 ETB | 29 (36.2) | 57 (23.7) | 2.12 (1.13, 3.98) | 1.81 (0.79, 4.08) |
| 1001–2000 ETB | 15 (18.8) | 46 (19.0) | 1.36 (0.65, 2.82) | 1.61 (0.64, 4.07) |
| 2000–3000 ETB | 12 (15.0) | 38 (15.8) | 1.32 (0.59, 2.89) | 2.22 (0.84, 5.87) |
| ≥3001® ETB | 24 (30.0) | 100 (41.5) | 1.00 | 1.00 |
| Distance to nearest facility | ||||
| >60 minutes | 31 (38.8) | 51 (21.2) | 2.35 (1.36, 4.07) | 1.14 (0.46, 2.78) |
| ≤60 minutes® | 49 (61.2) | 190 (78.8) | 1.00 | 1.00 |
| Transportation access | ||||
| No | 32 (40.0) | 61 (25.3) | 1.96 (1.15, 3.35) | 0.78 (0.35, 1.74) |
| Yes® | 48 (60.0) | 180 (74.7) | 1.00 | 1.00 |
| ANC visit | ||||
| 0 | 47 (58.8) | 48 (19.9) | 10.3 (3.41, 30.9) | 3.71 (1.1, 12.76)∗∗ |
| 1 | 11 (13.7) | 36 (14.9) | 3.21(0.94, 10.92) | 2.48 (0.66, 9.37) |
| 2-3 | 18 (22.5) | 115 (47.8) | 1.64 (0.53, 5.13) | 0.92 (0.26, 3.27) |
| ≥4® | 4 (5.0) | 42 (17.4) | 1.00 | 1.00 |
| History of previous C.S. | ||||
| Yes | 18 (22.5) | 21 (8.7) | 3.04 (1.53, 6.10) | 3.53 (1.49, 8.36)∗∗ |
| No® | 62 (77.5) | 220 (91.3) | 1.00 | 1.00 |
| Preexisting medical disorders | ||||
| Yes | 41 (51.2) | 79 (32.8) | 2.16 (1.29, 3.61) | 2.04 (1.11, 3.78)∗∗ |
| No® | 39 (48.8) | 162 (67.2) | 1.00 | 1.00 |
| Means of transportation | ||||
| Ambulance | 32 (40.0) | 73 (30.3) | 1.53 (0.91, 2.59) | 1.76 (0.93, 3.31) |
| Not ambulance® | 48 (60.0) | 168 (69.7) | 1.00 | 1.00 |
| Referral status | ||||
| Health facility referred | 32 (40.0) | 69 (28.6) | 1.66 (0.98, 2.81) | 1.47 (0.72, 3.01) |
| Self-referred from home® | 48 (60.0) | 172 (71.4) | 1.00 | 1.00 |
| First delay | ||||
| Yes | 44 (55.0) | 30 (12.4) | 8.59 (4.79, 15.4) | 5.74 (2.93, 11.2)∗∗ |
| No® | 36 (45.0) | 211 (87.6) | 1.00 | 1.00 |
∗∗Statistically significant variables in multiple logistic regressions at p value ≤ 0.05. ®: Reference category.
4. Discussion
In this study, women who did not have formal education had higher odds of near maternal miss compared to those who had formal education. This is comparable with studies in Bolivia, Morocco, Brazil, and Northern Ethiopia [19, 22–24], where illiterate mothers had higher odds of the maternal near miss. Possibly women with no formal education lack access to relevant information, which in one or another way may influence mothers' awareness of the obstetric complications and the need to seek better medical services. However, studies were done in Uganda, Ile-Ife Nigeria, Northeast Brazil, and Erbil city. Iraq [25–28] showed no significant association between women's education and maternal near-miss, and this is might be due to the study setting and study time difference.
Lack of antenatal care visits was the strong Factor associated with maternal near-miss in this study. This finding was parallel with the studies conducted in Bolivia, Pakistan, Morocco, and Iraq [19, 23, 25, 29, 30]. The study in Nigeria and Jimma University teaching hospital in Ethiopia also confirm the optimal number of antenatal care attendance as a protective factor against the severe maternal outcome and near miss. Furthermore, studies in Northeast Brazil as well as at Ayder teaching hospital Mekelle and Debra-Markos referral hospital in Ethiopia showed that women who had no antenatal visits were more likely to develop maternal near-miss [16, 17, 28]. This might be antenatal care is the most favorable contact point for mothers to get more information about the pregnancy. As well as discussion with health professionals on danger signs of pregnancy and delivery.
Consistence with previous studies in Netherland, Northeast Brazil South Africa, and Ethiopia [20, 28, 31–33], there was a higher risk of maternal near-miss among women with a prior history of cesarean section compared to their counterparts. Nevertheless, a study done in Tanzania showed that previous cesarean deliveries and maternal near-miss has no association [34]. This might be due to the difference in population, number, and quality of the recurrent cesarean section, and health service delivery systems. Giving the impression for a previous caesarian section delivery is critical because this kind of delivery, most of the time justified in case of health threats, which perhaps reoccur during the mother's subsequent pregnancy. As well, the previous cesarean section leads to increased risks of uterine rupture and hemorrhage due to uterine scar tissue during the next vaginal delivery. This implies cesarean section delivery especially elective nonmedical cesarean section should have to be reduced to the acceptable level [35] and avoid the misconception “once a cesarean section, always a cesarean section” to reduce the threats related with delivery.
Maternal near-miss was significantly associated with a history preexisting chronic medical disorder. This finding is comparable with studies in Iraq, Netherlands, and Uganda [25, 27, 32]. It was reported that the history of anemic resulted in maternal near maternal miss in countries like Ghana, Nigeria, and Sudan [26, 36–38]. Similarly, the history of prior chronic hypertension was associated with a high risk of maternal miss from studies in Brazil, Nigeria, and Ethiopia [26, 39]. In contrast, a study carried out on “applying the new concept of a maternal near-miss in an intensive care unit” illustrates preexisting medical morbidity has not increased the risk of maternal near-miss [40]. This inconsistency might be due to the difference in the approach used to diagnose near-miss cases like exclusively using management-based diagnosis (admission to intensive care unit) in such studies.
Likewise, the present study revealed that near-miss cases women were more likely to have a first delay (delay in deciding for health care) than their counterparts. This is in line with studies done in Morocco, Ile-Ife Nigeria, and Ethiopia [19, 26, 31]. Whereas second and third delays were not significantly associated with maternal near miss. This might be the fact that second and third delays would be more or less managed with improved ambulance services and due to the availability of enhanced comprehensive obstetric services in the current study hospitals as per the Ethiopian Ministry of Health recommendation. Finally, the findings of this study should be interpreted in light of its limitation. Although a disease-specific criterion was used to ascertain near-miss cases as per WHO recommendation for developing countries, the identification of cases using such criteria is less rigorous. In addition, there might be misclassification bias even though the identified cases were verified by senior physicians working in the study hospitals.
5. Conclusion
This study identified that women's with no formal education, lack of antenatal care visits, preexisting maternal chronic medical disorders, history of previous cesarean section, and first delay of obstetric care-seeking were factors associated with a maternal near miss. These findings had better recommend in rural areas, especially where there are high numbers of mothers with no formal education; focusing on the coverage of maternity service is a crucial step to avert serious maternal complications through strengthening health extension packages and scaling up of antenatal care. Furthermore, health facilities found in the zone better provide a quality antenatal care in order to identify high-risk women and prevent maternal near-miss morbidity. Those women who had a prior history of cesarean section and any preexisting medical disease must actively be recognized during pregnancy to prevent occurrence of maternal near miss. Finally, we recommend a longitudinal multicentre study to generate a more stable and more comprehensive national illustration of the maternal near miss.
Acknowledgments
We would like to thank the Hawassa University College of Medicine and Health Science for funding this thesis work. My pleasure typically goes to study participants and data collectors for their valuable time, commitment, and more of their support in all. We would like to show my appreciation for the West Arsi zone health department and hospitals for their cooperation in the process of data collection.
Abbreviations
- ANC:
Antenatal care
- AOR:
Adjusted odds ratio
- COR:
Crude odd ratio
- C.S.:
Cesarean section
- EDHS:
Ethiopia demographic and health survey
- MMR:
Maternal mortality ratio
- MNM:
Maternal near miss
- SDG:
Sustainable development goal
- WHO:
World Health Organization.
Data Availability
Data is not available for online access. However, readers who wish to gain access to the data can write to the corresponding author Feleke Hailemichael Astawesegn at felekeh86@gmail.com.
Ethical Approval
Ethical clearance and the supportive letter were obtained from the Hawassa University College of Medicine and Health Science Institutional Review Board (IRB). Written permission was obtained from the Oromia Regional Health Bureau and West Arsi Zone Health Department and participating hospitals. Informed consent was directly obtained from study participants after they stabilized from their clinical emergency (on discharge to home), explaining the objectives of the study. Confidentiality was assured for the information provided. Participation in the study was also on voluntary bases.
Conflicts of Interest
The authors declare that they have no competing interests. FN is a lecturer in the Department of Public Health, College of Medicine and Health Sciences, Maddawalabo University; FH and NC are lecturers in the School of Public Health, College of Medicine and Health Sciences, Hawassa University.
Authors' Contributions
F.N. was involved in conception, designing the study, writing proposal, analysis, interpretation of data, and manuscript writing. F.H. and N.C. were involved in designing the study, writing proposal, analysis, interpretation of data, and manuscript writing. All authors agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
References
- 1.Ashford L. Hidden Suffering: Disabilities from Pregnancy and Childbirth in Less Developed Countries. Population Reference Bureau; 2002. https://www.prb.org/wp-content/uploads/2002/08/HiddenSuffering_FrBW.pdf. [Google Scholar]
- 2.Kalhan M., Singh S., Punia A., Prakash J. Maternal near-miss audit: lessons to be learnt. International Journal of Applied and Basic Medical Research. 2017;7(2):85–87. doi: 10.4103/2229-516X.205815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization, Department of Reproductive Health and Research. the WHO near-miss approach for maternal health. Geneva, Switzerland: World Health Organization; 2011. Evaluating the quality of care for severe pregnancy complications. [Google Scholar]
- 4.Say L., Souza J. P., Pattinson R. C. Maternal near miss – towards a standard tool for monitoring quality of maternal health care. Best Practice & Research Clinical Obstetrics & Gynaecology. 2009;23(3):287–296. doi: 10.1016/j.bpobgyn.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Trends in Maternal Mortality: 1990 to 2013 Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 6.Requejo J. H., Bryce J., Barros A. J. D., et al. Countdown to 2015 and beyond: fulfilling the health agenda for women and children. The Lancet. 2015;385(9966):466–476. doi: 10.1016/S0140-6736(14)60925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Trends in maternal mortality: 1990-2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization; 2015. [Google Scholar]
- 8.World Health Organization. Trends in maternal mortality: 1990 to 2010. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 9.Creanga A. A., Syverson C., Seed K., Callaghan W. M. Pregnancy-related mortality in the United States, 2011-2013. Obstetrics & Gynecology. 2017;130(2):366–373. doi: 10.1097/aog.0000000000002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grobman W. A., Bailit J. L., Rice M. M., et al. Frequency of and Factors Associated With Severe Maternal Morbidity. Obstetrics & Gynecology. 2014;123(4):804–810. doi: 10.1097/aog.0000000000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Callaghan W. M., Creanga A. A., Kuklina E. V. Severe Maternal Morbidity Among Delivery and Postpartum Hospitalizations in the United States. Obstetrics & Gynecology. 2012;120(5):1029–1036. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 12.Prata N., Passano P., Sreenivas A., Gerdts C. E. Maternal mortality in developing countries: challenges in scaling-up priority interventions. Women’s Health. 2010;6(2):311–327. doi: 10.2217/whe.10.8. [DOI] [PubMed] [Google Scholar]
- 13.Central Statistical Agency [Ethiopia] Key Indicators Report. Addis Ababa and Rockville: Central Statistical Agency and ICF International; 2016. Ethiopia Demographic and Health Survey 2016. [Google Scholar]
- 14.Hogan M. C., Foreman K. J., Naghavi M., et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. The Lancet. 2010;375(9726):1609–1623. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- 15.Federal Democratic Republic of Ethiopia Ministry of Health. Maternal Death Surveillance and Response (MDSR) Technical Guideline. Addis Ababa, Ethiopia: Ministry of Health; 2014. http://mdsr-action.net/wp-content/uploads/2016/11/Ethiopia-MDSR-revised-guidelines.pdf. [Google Scholar]
- 16.Berhane G., Gessessew A., Van Roosmalen J., Van Den Akker T. Obstetric near-miss and maternal death: the case of Ayder teaching hospital, Mekelle, Ethiopia. Ethiopian Journal of Reproductive Health. 2012;6(1):56–63. [Google Scholar]
- 17.Gedefaw M., Gebrehana H., Gizachew A., Taddess F. Assessment of Maternal Near Miss at Debre Markos Referral Hospital, Northwest Ethiopia: Five Years Experience. Open Journal of Epidemiology. 2014;4(4):199–207. doi: 10.4236/ojepi.2014.44026. [DOI] [Google Scholar]
- 18.Gebrehiwot Y., Tewolde B. T. Improving maternity care in Ethiopia through facility based review of maternal deaths and near misses. International Journal of Gynecology & Obstetrics. 2014;127:S29–S34. doi: 10.1016/j.ijgo.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 19.Assarag B., Dujardin B., Delamou A., Meski F.-Z., De Brouwere V. Determinants of Maternal Near-Miss in Morocco: Too Late, Too Far, Too Sloppy? PLOS ONE. 2015;10(1):p. e0116675. doi: 10.1371/journal.pone.0116675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Filippi V., Ronsmans C., Gohou V., et al. Maternity wards or emergency obstetric rooms? Incidence of near-miss events in African hospitals. Acta Obstetricia et Gynecologica Scandinavica. 2005;84(1):11–16. doi: 10.1111/j.0001-6349.2005.00636.x. [DOI] [PubMed] [Google Scholar]
- 21.Witteveen T., Bezstarosti H., de Koning I., et al. Validating the WHO maternal near miss tool: comparing high- and low-resource settings. BMC pregnancy and childbirth. 2017;17(1):p. 194. doi: 10.1186/s12884-017-1370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mekango D. E., Alemayehu M., Gebregergs G. B., Medhanyie A. A., Goba G. Determinants of maternal near miss among women in public hospital maternity wards in Northern Ethiopia: a facility based case-control study. PLOS ONE. 2017;12(9):p. e0183886. doi: 10.1371/journal.pone.0183886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rööst M., Altamirano V. C., Liljestrand J., Essén B. Does antenatal care facilitate utilization of emergency obstetric care? A case-referent study of near-miss morbidity in Bolivia. Acta Obstetricia et Gynecologica Scandinavica. 2010;89(3):335–342. doi: 10.3109/00016340903511050. [DOI] [PubMed] [Google Scholar]
- 24.Souza J. P., Cecatti J. G., Parpinelli M. A., et al. Maternal morbidity and near miss in the community: findings from the 2006 Brazilian demographic health survey. BJOG : An International Journal of Obstetrics and Gynaecology. 2010;117(13):1586–1592. doi: 10.1111/j.1471-0528.2010.02746.x. [DOI] [PubMed] [Google Scholar]
- 25.Akrawi V. S., Al-Hadithi T. S., Al-Tawil N. G. Major Determinants of Maternal Near-Miss and Mortality at the Maternity Teaching Hospital, Erbil city, Iraq. Oman Medical Journal. 2017;32(5):386–395. doi: 10.5001/omj.2017.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adeoye I. A., Onayade A. A., Fatusi A. O. Incidence, determinants and perinatal outcomes of near miss maternal morbidity in Ile-Ife Nigeria: a prospective case control study. BMC Pregnancy and Childbirth. 2013;13(1) doi: 10.1186/1471-2393-13-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakimuli A., Nakubulwa S., Kakaire O., et al. Maternal near misses from two referral hospitals in Uganda: a prospective cohort study on incidence, determinants and prognostic factors. BMC Pregnancy and Childbirth. 2016;16(1) doi: 10.1186/s12884-016-0811-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galvão L. P. L., Alvim-Pereira F., de Mendonça C. M. M., et al. The prevalence of severe maternal morbidity and near miss and associated factors in Sergipe, Northeast Brazil. BMC Pregnancy and Childbirth. 2014;14(1) doi: 10.1186/1471-2393-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Souza J. P., Cecatti J. G., Faundes A., et al. Maternal near miss and maternal death in the 2005 WHO global survey on maternal and perinatal health. Bulletin of the World Health Organization. 2010;88(2):113–119. doi: 10.2471/BLT.08.057828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Villar J., Carroli G., Zavaleta N., et al. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ. 2007;335(7628):1025–1035. doi: 10.1136/bmj.39363.706956.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kasahun A. W., Wako W. G. Predictors of maternal near miss among women admitted in Gurage zone hospitals, South Ethiopia, 2017: a case control study. BMC Pregnancy and Childbirth. 2018;18(1):p. 260. doi: 10.1186/s12884-018-1903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanegem N. V., Miltenburg A. S., Zwart J. J., Bloemenkamp K. W. M., Roosmalen J. V. Severe acute maternal morbidity in asylum seekers: a two-year nationwide cohort study in the Netherlands. Acta Obstetricia et Gynecologica Scandinavica. 2011;90(9):1010–1016. doi: 10.1111/j.1600-0412.2011.01140.x. [DOI] [PubMed] [Google Scholar]
- 33.Maswime S., Buchmann E. J. Why women bleed and how they are saved: a cross-sectional study of caesarean section near-miss morbidity. BMC Pregnancy and Childbirth. 2017;17(1):p. 15. doi: 10.1186/s12884-016-1182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Litorp H., Kidanto H. L., Rööst M., Abeid M., Nyström L., Essén B. Maternal near-miss and death and their association with caesarean section complications: a cross-sectional study at a university hospital and a regional hospital in Tanzania. BMC Pregnancy and Childbirth. 2014;14(1) doi: 10.1186/1471-2393-14-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ugwumadu A. Does the Maxim “Once a Caesarean, Always a Caesarean” Still Hold True? PLoS Medicine. 2005;2(9):p. e305. doi: 10.1371/journal.pmed.0020305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tunçalp Ö., Hindin M. J., Adu-Bonsaffoh K., Adanu R. M. Assessment of maternal near-miss and quality of care in a hospital-based study in Accra, Ghana. International Journal of Gynecology & Obstetrics. 2013;123(1):58–63. doi: 10.1016/j.ijgo.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Ali A. A. A., Khojali A., Okud A., Adam G. K., Adam I. Maternal near-miss in a rural hospital in Sudan. BMC Pregnancy and Childbirth. 2011;11(1) doi: 10.1186/1471-2393-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nair M., Choudhury M. K., Choudhury S. S., et al. Association between maternal anaemia and pregnancy outcomes: a cohort study in Assam, India. BMJ Global Health. 2016;1(1):p. e000026. doi: 10.1136/bmjgh-2015-000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Moraes A. P. P., Barreto S. M., Passos V. M. A., Golino P. S., Costa J. E., Vasconcelos M. X. Severe maternal morbidity: a case-control study in Maranhao, Brazil. Reproductive Health. 2013;10(1) doi: 10.1186/1742-4755-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lotufo F., Parpinelli M., Haddad S., Surita F., Cecatti J. Applying the new concept of maternal near-miss in an intensive care unit. Clinics. 2012;67(3):225–230. doi: 10.6061/clinics/2012(03)04. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is not available for online access. However, readers who wish to gain access to the data can write to the corresponding author Feleke Hailemichael Astawesegn at felekeh86@gmail.com.


