Abstract
Background:
Anxiety and depressive disorders are often characterized by perceived social disconnection, yet evidence-based treatments produce only modest improvements in this domain. The well-established link between positive affect (PA) and social connectedness suggests that directly targeting PA in treatment may be valuable.
Method:
A secondary analysis of a waitlist-controlled trial (N=29) was conducted to evaluate treatment response and process of change in social connectedness within a 10-session positive activity intervention protocol—Amplification of Positivity (AMP)—designed to increase PA in individuals seeking treatment for anxiety or depression (ClinicalTrials.gov Identifier: NCT02330627). Perceived social connectedness and PA/negative affect (NA) were assessed throughout treatment. Time-lagged multilevel mediation models examined the process of change in affect and connectedness throughout treatment.
Results:
The AMP group displayed significantly larger improvements in social connectedness from pre- to post-treatment compared to waitlist; improvements were maintained through 6-month follow-up. Within the AMP group, increases in PA and decreases in NA both uniquely predicted subsequent increases in connectedness throughout treatment. However, experiencing heightened NA throughout treatment attenuated the effect of changes in PA on connectedness. Improvements in connectedness predicted subsequent increases in PA, but not changes in NA.
Conclusions:
These preliminary findings suggest that positive activity interventions may be valuable for enhancing social connectedness in individuals with clinically impairing anxiety or depression, possibly through both increasing positive emotions and decreasing negative emotions.
Keywords: Anxiety, depression, positive activity intervention, social connectedness, affect, randomized controlled trial
Feeling connected to others is a fundamental human need (Baumeister & Leary, 1995)—one that confers important health benefits, including mitigating the adverse effects of stress, enhancing immune function, and promoting life satisfaction (Chu, Saucier & Hafner, 2010; Cohen, 2004; Eisenberger & Cole, 2012; Lyubomirsky, King, & Diener, 2005; Umbersen & Montez, 2010). Social disconnection and loneliness increase risk for early mortality to a degree comparable with well-established health risk factors such as obesity and smoking (Cacioppo & Cacioppo, 2018; Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015; Holt-Lunstad, Smith, & Layton, 2010). Social disconnection is common in anxiety and depressive disorders (Beck, 2010; McKnight & Kashdan, 2009; Olatunji, Cisler, & Tolin, 2007; Saris, Aghajani, van der Werff, van der Wee, & Pennix, 2017); individuals diagnosed with these conditions often have fewer and lower quality social connections, report lower levels of perceived social support, and are more likely to be socially isolated than their non-anxious, non-depressed counterparts. Identifying treatment approaches that can improve social connectedness in anxiety and depressive disorders is therefore an important public health endeavor.
Contemporary treatments for anxiety and depression improve facets of social connectedness; however, improvements tend to be modest and do not match the much larger changes typically observed for symptoms (Eng, Coles, Heimberg, & Safren, 2005; Hofmann, Wu, & Boettcher, 2014; McKnight & Kashdan, 2009). For example, a meta-analysis examining the effect of cognitive behavioral therapy (CBT) on quality of life for individuals with anxiety disorders found modest improvements in social quality of life (Hedges’ g = 0.25) that were significantly smaller than improvements in other quality of life domains (e.g., psychological) and symptoms (Hofmann et al., 2014). A meta-analysis in depression (Renner, Cuijpers, & Huibers, 2014) revealed small to medium improvements in measures of social disability across psychotherapies (Hedge’s g = 0.46), including CBT and Interpersonal Psychotherapy (IPT; Markowitz & Weissman, 2004)—an empirically supported treatment that explicitly targets social functioning through identifying and addressing a core interpersonal problem (i.e., grief, role transition, role dispute, or interpersonal deficits) thought to maintain depression. Even after remission from anxiety or depression, impairments in numerous domains of social functioning persist (e.g., loneliness, social support, network size; Saris et al., 2017). Thus, while current treatments are effective in decreasing symptoms of anxiety and depression, they do not fully ameliorate impairments in social connectedness.
A treatment’s ability to enhance social connectedness depends on how well it can target the mechanisms that promote adaptive social bonds. It is well known that our emotions, both positive and negative, influence our capacity to connect with others (Keltner & Kring, 1998). Excessive negative affect—produced by over-activation of the negative valence (avoidance/aversive) system (Elliot, 2006; Gray, 1987; Lang, 1995)—can lead to lower participation in social activities, diminished engagement in social relationships, and ultimately poorer interpersonal outcomes (e.g., loneliness, diminished relationship satisfaction; Gable & Berkman, 2008; Impett et al., 2010; Trew, 2011). Heightened positive affect—generated by the positive valence (approach/appetitive) system—facilitates positive social connections (Fredrickson, Cohn, Coffey, Pek, & Finkel, 2008; Kok et al., 2013; Waugh & Fredrickson, 2006; see Ramsey & Gentzler, 2015, for a review), above and beyond negative affective experiences (Strong & Aron, 2006), by guiding people toward (e.g., coordinating social initiation behaviors) and enhancing responsiveness to situations that offer the potential for social reward (Fredrickson, 2013; Gable & Berkman, 2008; Gable & Reis, 2010; Lyubomirsky et al., 2005).
Evidence-based treatments for anxiety and depression (e.g., cognitive behavioral therapy) are efficacious in reducing negative emotions and symptoms (e.g., Craske, Treanor, Conway, Zbozinek, & Vervliet, 2014; Cuijpers et al, 2013; Hofmann & Smits, 2008). Yet individuals with depression and anxiety also display aberrant functioning of the positive valence system, including low positive affect, diminished approach motivation and behavior, and reduced behavioral and neural reactivity to rewards (for reviews, see Carl, Soskin, Kerns, & Barlow, 2013; Craske, Meuret, Ritz, Treanor, & Dour, 2016; Dillon et al., 2014; Trew, 2011). Although current interventions improve positive affect and deliberately target it to some extent (e.g., behavioral activation), treatment effects tend to be modest (small to medium sized effects; all psychotherapies combined, Boumparis, Karyotaki, Kleiboer, Hofmann, & Cuijpers, 2016; cognitive behavioral therapy, Dunn et al., 2020; Kring, Persons, & Thomas, 2007; acceptance and commitment therapy, Sewart et al., 2019; mindfulness-based therapy, Strege, Swain, Bochicchio, Valdespino, & Richey, 2018). For example, a large randomized controlled trial comparing cognitive therapy, pharmacotherapy, and their combination for depression (Hollon et al., 2014) revealed that participants displayed post-treatment levels of positive affect that were significantly below community norms, despite returning to normative levels of negative affect (Dunn et al., 2020). Even behavioral activation, which focuses on increasing exposure to rewarding activities, has modest effects on positive affect and related clinical outcomes (i.e., anhehonia; Dichter et al., 2009; Moore et al., 2013). Many well-established intervention approaches may therefore only partially upregulate positive emotions, which are a key ingredient for building social connections.
We previously designed and evaluated a 10-session clinician-administered positive activity intervention protocol—Amplification of Positivity (AMP)—for individuals with clinically impairing anxiety or depression, with the intent to specifically target the positive valence system and increase positive affect (Taylor, Lyubomirsky, & Stein, 2017). Positive activities refer to intentional and repeated practices adapted from exercises developed within the field of positive psychology to promote positive thoughts, behaviors, and emotions in populations not selected for clinical characteristics (Layous, Chancellor, & Lyubomirsky, 2014; Lyubomirsky & Layous, 2013; Seligman, Steen, Park, & Peterson, 2005). Although several activities within the AMP protocol share conceptual elements with established treatments for depression and anxiety, such as planning pleasurable and meaningful activities (shared with Behavioral Activation; Jacobson, Martell, & Dimidjian, 2001) and affirming core values (shared with Acceptance and Commitment Therapy; Hayes, Luoma, Bond, Masuda, & Lillis, 2006), the majority of activities are not explicitly included within established clinical interventions (e.g., counting one’s blessings, Emmons & McCullough, 2003; performing acts of kindness, Nelson, Layous, Cole, & Lyubomirsky, 2016; noticing and amplifying positive events, Jose, Lim, & Bryant, 2012). Results of a waitlist-controlled randomized clinical trial revealed that AMP significantly increased positive emotions as well as decreased negative emotions and symptoms of anxiety and depression (all within- and between-group AMP effects on the composite outcomes were large; Cohen’s d > .90; Taylor, Lyubomirsky et al., 2017).
Our goal in the current research was to conduct a secondary analysis of that trial to evaluate the effects of the AMP protocol on social connectedness in individuals seeking treatment for anxiety or depression. Research from affective and relational science demonstrates that positive activities increase perceived social connectedness and positive relationship functioning (e.g., relationship satisfaction) in non-clinical samples (Algoe, Fredrickson, & Gable, 2013; O’Connell, Shea, & Gallagher, 2016; Nelson et al., 2016), and in those with elevated social anxiety (Alden & Trew, 2013). They also have been shown to facilitate specific social affiliative behaviors and generate positive interpersonal transactions (Algoe, 2019). For example, inducing gratitude led individuals to spend more time with the person they felt grateful toward and to engage in socially inclusive behaviors involving that person, even at a cost to themselves (Bartlett, Condon, Cruz, Baumann, & Desteno, 2012). Moreover, relationally focused positive activities (e.g., doing kind acts for others) tend to generate stronger effects than engaging in self-focused positive activities (i.e., engaging in kind acts for oneself; Nelson et al., 2016; O’Connell et al., 2016).
Considering the literature above, the current research tested two hypotheses: (1) that the AMP regimen resulted in greater increases in perceived social connectedness compared to waitlist control, and (2) that predicted increases in social connectedness over the course of completing AMP would be accounted for by preceding increases in positive affect as well as decreases in negative affect. Measures of affect and perceived social connectedness were administered throughout treatment, thereby permitting a temporal analysis of change in each outcome as well as examining unique variance accounted for above and beyond the other variables. Finally, given prior experimental research demonstrating that positive and negative emotions interact in predicting changes in connectedness during social affiliation (Taylor, Pearlstein, & Stein, 2017), we explored whether changes in positive affect interacted with changes in negative affect in predicting subsequent changes in connectedness. This exploratory analysis may inform boundary conditions at which positive or negative emotions are more or less potent contributors to changes in connectedness in the context of treatment.
Method
Participants
Participants were individuals seeking treatment for anxiety or depression recruited through clinical referrals, as well as posted announcements in community and online settings (e.g., ResearchMatch.org). Inclusion criteria1 were (1) age 18 to 55 and (2) clinically elevated symptoms of anxiety (score of 8 or higher on the Overall Anxiety Severity and Impairment Scale [OASIS; Campbell-Sills et al., 2009]) or depression (score of 10 or higher on the Patient Health Questionnaire-9 [PHQ-9; Kroenke, Spitzer, & Williams, 2001]). Exclusion criteria were intended to ensure that participants could safely complete the procedures and to minimize confounding interpretation of our findings (e.g., concomitant treatments): (1) pharmacological treatments (e.g., anxiolytics, antidepressants; past 6 weeks); (2) concurrent psychotherapy (past 6 weeks); (3) current active suicidal ideation; (4) history of major neurological disorder or moderate to severe traumatic brain injury; (5) moderate alcohol or marijuana use disorder (past year); mild substance use disorder (all other drugs except for alcohol or marijuana; past year); (6) bipolar I or psychotic disorders; and (7) characteristics that compromise MRI safety (e.g., metal in body). Diagnostic interviews were conducted using the Mini International Neuropsychiatric Interview for DSM-5 (MINI Version 7.0.0.0).2
A total of 29 participants were randomized to either the immediate AMP protocol (n=16) or delayed treatment (waitlist) group (WL; n=13). One participant in the AMP group discontinued treatment following session 7, and one participant in the WL group initiated treatment outside of the study following randomization and therefore was excluded from the analyses. Four WL participants initiated the AMP protocol following the post-assessment. See Supplemental Figure 1 for participant enrollment statistics and progress through the study. The demographic and clinical composition reflected a diverse, community-based treatment-seeking sample. Demographic characteristics were as follows: age (M = 29.4, SD = 11.9), gender (11 men; 17 women), race (71% White, 21% Asian, 4% Native American, 4% Pacific Islander), and ethnicity (21% Hispanic). Participants met criteria for a range of DSM-5 conditions (note that percentages sum to > 100%, given high comorbidity across the sample): major depressive disorder (current; 57%), social anxiety disorder (57%), generalized anxiety disorder (39%), panic disorder (7%), posttraumatic stress disorder (21%), eating disorder (11%), obsessive compulsive disorder (4%), mild alcohol use disorder (7%), and mild marijuana use disorder (4%). As reported in Taylor, Lyubomirsky et al. (2017), no group differences were observed on any of the assessed demographic or clinical characteristics other than a greater proportion of participants in the AMP group reported receiving prior psychological treatment compared to WL participants (88% vs. 50%). See Supplemental Table 1.
Measures
Participants completed a battery of reliable and valid self-report measures assessing positive and negative affect, symptoms (anxiety and depression), psychological well-being, and social connectedness. The secondary analysis reported in this paper focuses on positive and negative affect, and social connectedness.
Social Connectedness.
Participants completed the 20-item Social Connectedness Scale–Revised (SCS-R; Lee et al., 2001) pre- and post-assessment (both groups), and prior to treatment sessions 1, 3, 5, 7, and 9, as well as at 3- and 6-month follow-up for participants completing the AMP protocol. The SCS-R measures a psychological sense of belonging, or how individuals cognitively construe interpersonal closeness with others in their social world. The SCS-R uses a 6-point rating scale (1 = strongly disagree to 6 = strongly agree). Sample items include “I am able to connect with other people”; “I feel close to other people”; and “I don’t feel I participate with anyone or any group” (reverse scored). The SCS-R displays high internal consistency, test-retest reliability (examined over a 1-month period), and convergent validity (Lee et al., 2001). See Table 2 for descriptive summaries and Cronbach’s α at each assessment visit.
Table 2.
Means and Standard Deviations of Outcome Variables Throughout the AMP Program.
| Assessment | PANAS-PA | PANAS-NA | SCS-R |
|---|---|---|---|
| Baseline | 24.20 (7.88) α = .90 | 26.25 (8.14) α = .89 | 66.70 (12.08) α = .86 |
| Session 1 | 24.38 (6.78) α = .89 | 22.31 (8.24) α = .89 | 67.75 (12.81) α = .83 |
| Session 2 | 25.24 (6.17) α = .89 | 20.35 (6.84) α = .88 | -- |
| Session 3 | 25.58 (6.92) α = .90 | 19.53 (7.38) α = .87 | 71.11 (14.07) α = .89 |
| Session 4 | 26.84 (6.82) α = .90 | 19.74 (8.41) α = .94 | -- |
| Session 5 | 28.05 (6.50) α = .89 | 18.79 (8.66) α = .94 | 74.83 (13.94) α = .90 |
| Session 6 | 26.85 (7.00) α = .89 | 19.00 (9.25) α = .95 | -- |
| Session 7 | 28.53 (6.53) α = .88 | 16.37 (3.92) α = .73 | 77.21 (11.39) α = .84 |
| Session 8 | 26.84 (6.20) α = .89 | 18.00 (4.37) α = .67 | -- |
| Session 9 | 30.11 (6.90) α = .89 | 16.33 (4.30) α = .76 | 78.11 (13.37) α = .89 |
| Session 10 | 32.58 (6.77) α = .87 | 15.79 (4.53) α = .78 | -- |
| Post-Assessment | 32.58 (6.81) α = .93 | 16.00 (3.68) α = .92 | 83.68 (14.16) α = .94 |
Note. AMP = Amplification of Positivity; PANAS = Positive and Negative Affect Schedule; PA = Positive Affect; NA = Negative Affect; SCS-R = Social Connectedness Scale Revised; α = Cronbach’s alpha.
Positive and Negative Affect.
Participants completed the 20-item Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) pre- and post-assessment (both groups), as well as prior to each treatment session throughout the PAI protocol, in order to assess activated forms of positive and negative affect “during the past week.” The PANAS has high internal consistency and temporal stability (trait version), and correlational data and confirmatory factor analyses support its validity (Crawford & Henry, 2004). See Table 2 for descriptive summaries and Cronbach’s α at each assessment visit.
Procedure
Data originated from a randomized controlled trial comparing the AMP protocol to a WL control condition (see Taylor, Lyubomirsky et al., 2017, for additional details regarding the study procedures). Participants randomly assigned to the immediate treatment group were assessed before, during, and after treatment, as well as 3 and 6 months following the post-assessment. WL participants were assessed at the beginning and end of the 10-week WL period, after which they were offered treatment. For WL participants who initiated the AMP protocol (n=4), their WL post-assessment data served as their baseline assessment data for the within-group treatment analyses.
Treatment
Amplification of Positivity (AMP).
The AMP protocol consisted of 10, 60-minute individual treatment sessions delivered by therapists with over 10 years of experience treating individuals with anxiety or depression. Treatment began with a 30-minute orientation at the start of the first session to acquaint the therapist and patient, and set goals for treatment. A treatment manual was developed based on prior literature on positive activity interventions and emotion science findings regarding the function of positive thoughts, emotions, and behaviors. See Supplemental Table 2 for a summary of each treatment module. Handouts accompanied each module, which included instructions and space to complete the written portion of a given activity. The structure of each session followed traditional behavioral treatment regimens, including reviewing completion of the prior week’s exercises, troubleshooting issues that arose during exercise completion, introducing material about a new positive activity and planning between-session exercises. Therapists met weekly to review ongoing cases and treatment adherence; however, treatment fidelity was not formally assessed.
Waitlist (WL).
Waitlist participants completed the pre- and post-assessments at a 10-week interval. Treatment was offered to these individuals after the post-assessment.
Overview of Statistical Analyses
All analyses were conducted using SPSS version 26. Our first question examined group differences in perceived social connectedness following AMP or WL. SCS-R scores were submitted to an analysis of covariance (ANCOVA) to test group differences at post-treatment, controlling for participants’ pre-treatment scores (Van Breukelen, 2006; Vickers & Altman, 2001). This analysis approach was used to remain consistent with the primary outcomes paper, and because WL participants only completed assessments at pre- and post-treatment rather than repeatedly throughout the 10-week period. We confirmed that assumptions underlying ANCOVA were met: independence of the covariate [pre-treatment scores] and treatment group, t(26) = 1.52, p = .14, and homogeneity of regression slopes such that the covariate (baseline SCS-R scores) and treatment group did not interact in predicting the outcome, F(1, 24) = .00, p = 1.0, η2p = .00. Analyses were conducted on an intent-to-treat (ITT) basis. Mid-treatment (session 5) data were used for the post-assessment for the one participant who discontinued treatment following session 7. The magnitude of treatment response was established by calculating (1) within-group effect sizes = (post-assessment mean minus pre-assessment mean)/([pre-assessment standard deviation + post-treatment standard deviation]/2) (referred to as Cohen’s dav; see Lakens, 2013); and (2) between-group controlled effect sizes = (post-assessment AMP covariance adjusted mean minus post-assessment WL covariance adjusted mean)/pooled standard deviation.
Our second question examined whether changes in social connectedness over the course of treatment were accounted for by changes in positive affect (PA), negative affect (NA), or both. This analysis focused on all participants who initiated the AMP protocol (n=20), including those initially randomized to the AMP group (n=16), as well as those from the WL group who subsequently enrolled in the AMP protocol (n=4).3 We asked the question: Did increases in PA, decreases in NA, or both account for subsequent increases in connectedness throughout the course of the AMP protocol? The within-treatment (session by session) data formed a multilevel structure such that repeated measures collected over time were nested within participants. The lower level (Level 1) data comprised repeated measures of PA and NA (PANAS) collected prior to each treatment session, and perceived social connectedness (SCS-R) collected prior to sessions 1, 3, 5, 7, and 9. Level 1 data were nested within upper level units (Level 2; i.e., participants). This data structure is appropriate for hierarchical linear modeling approaches.
Post-treatment follow-up data was not included in these analyses.
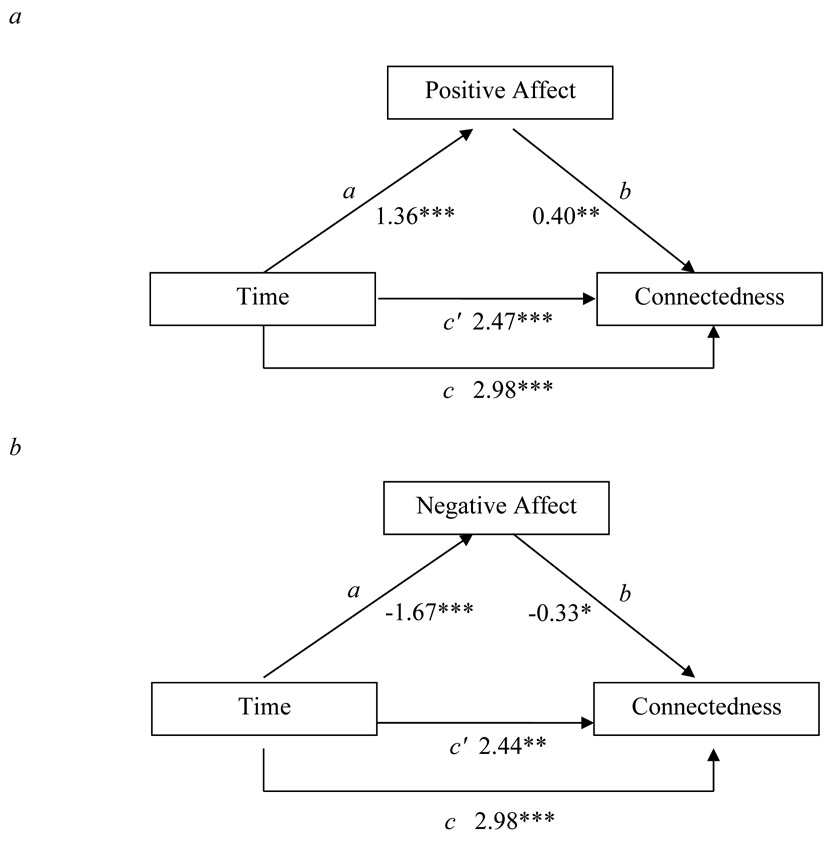
Our primary model tested whether changes in PA or NA accounted for subsequent changes in perceived social connectedness (see Figure 2). We first examined the slopes in connectedness (see Figure 2, path c) and PA and NA over time (see Figure 2a and 2b, respectively, path a) to confirm that social connectedness and PA increased over treatment, and NA decreased over treatment. Mediation analyses were then used to examine whether changes in PA and/or NA accounted for predicted increases in social connectedness over the course of treatment. A lower level mediation approach was used because of the longitudinal nature of the data—that is, the predictor variable (time) and mediators (affect) were Level 1 variables measured repeatedly throughout treatment (Bauer, Preacher, & Gil, 2006; Kenny, Korchmaros, & Bolger, 2003). Each mediator (PANAS-PA and NA) was first entered in separate models to establish the presence of indirect effects independent of the effects of changes in the other variable. Significant indirect effects were followed by a more conservative analysis in which both PA and NA scores were entered together in a model to establish unique variance accounted for by each variable in predicting change in connectedness. We also explored whether PA and NA interacted in predicting subsequent connectedness. Variables were centered at the sample mean prior to computing the interaction term. The mediator and outcome variable were time lagged (Aderka, Foa, Applebaum, Shafran, & Gilboa-Schechtman, 2011; Bomyea et al., 2015) in order to conduct a more rigorous test of mediation in which the mediator temporally precedes the outcome (Kazdin, 2007). That is, we examined whether changes in the mediator at time t accounted for changes in the outcome at time t + 1. Note that all models described above were time-lagged. That is, we examined the slope of the hypothesized intervening variables (PA and NA) at time t, whereas the slope of the outcome (perceived social connectedness) was examined at time t+1. Because SCS-R outcomes were collected every other session, models only included PANAS data from the relevant prior session (e.g., PANAS at session 2 predicting SCS-R at session 3; PANAS at session 4 predicting SCS-R at session 5 etc.). We also examined on an exploratory basis whether social connectedness at time t accounted for changes in positive and negatives emotions at time t + 1. This analysis would elucidate possible bi-directional relationships between change in affect and perceived connectedness throughout treatment. We screened for outliers within the multilevel modeling framework using the R package influence.ME (Nieuwenhuis, Pelzer, & Grotenhuis, 2012) and found no evidence of influential outlying data (all Cook’s distance < 1; Tabachnick & Fidell, 2007).
Figure 2.
Results of the hypothesized mediation models with the effect of time on change in social connectedness mediated by change in positive affect (PA, Figure 2a) and change in negative affect (NA, Figure 2b; p < 0.001, **p < 0.01, *p < .05).
To test for significant mediation (i.e., the indirect effect of time on connectedness through change in affect), we examined the product of the coefficients for the effects of the a and b paths through the construction of asymmetric confidence intervals, given that the ab path tends to be asymmetric (MacKinnon, Fairchild, & Fritz, 2007; MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). If the 95% confidence interval does not include zero, the mediated effect is considered significant (MacKinnon, Lockwood, & Williams, 2004). The program PRODCLIN (MacKinnon et al., 2007) was used to calculate the asymmetric confidence limits for our analyses.
Results
Changes in Social Connectedness
Table 1 presents the means and standard deviations for the SCS-R for AMP and WL groups. Results of the ANCOVA conducted on the SCS-R revealed that individuals in the AMP group demonstrated significantly greater perceived social connectedness at post-treatment compared to participants in the WL group, F(1, 25) = 7.49, p = .011, η2p = .23 (Cohen’s d = 1.07). The magnitude of within-group improvements in social connectedness from pre- to post-assessment was large for the PAI group (Cohen’s dav = 1.28) and small-to-medium for the WL group (Cohen’s dav = 0.48).
Table 1.
Descriptive summaries of the SCS-R for the AMP (n=16) and WL (n=12) groups.
| Measure | Pre-assessment M (SD) |
Post-assessment M (SD) |
3-month follow-up M(SD)a |
6-month follow-up M (SD)a |
|---|---|---|---|---|
| SCS-R | ||||
| PAI | 66.31 (12.59) | 83.38 (14.00) | 86.47 (16.52) | 84.60 (16.25) |
| WL | 58.83 (13.34) | 65.50 (14.63) | ||
Note. AMP = Amplification of Positivity; WL = Waitlist; SCS-R = Social Connectedness Scale Revised.
Treatment completers only (n=15).
Results of the repeated measures ANOVA (Time: pre, post, 3- and 6-month follow-up) conducted on the SCS-R within the AMP group4 revealed a significant main effect of Time, F(1.657, 23.194) = 15.49, p < .001, η2p = .53. Follow-up contrasts using the Sidák adjustment for multiple comparisons indicated that the AMP group displayed significant improvements in social connectedness from pre-assessment to each of the subsequent assessment points (all ps < .01). Post-treatment and follow-up scores did not significantly differ (all ps > .05), which indicated that initial gains were maintained up to 6-months following the end of treatment (see Figure 1).
Figure 1.
Change in social connectedness (SCS-R) in the Amplification of Positivity (AMP) vs. waitlist (WL) groups. Error bars represent ±1 standard error.
We evaluated clinically significant change in social connectedness following Jacobson and Truax (1991). A participant was classified as meeting criteria for clinically significant change if (1) their post-treatment SCS-R score fell closer to the mean of the normative population (M = 88.02, SD = 16.82 from Lee et al., 2001, study 1)5 than to the mean of the clinical population (M = 63.11, SD = 13.22 in the current sample), and (2) if they displayed a statistically reliable improvement in SCS-R scores from pre- to post-assessment using the reliable change index (RCI > 1.96)—calculated as the difference in post- minus pre-treatment scores divided by Sdiff, wherein Sdiff = √(2 x SE2), and SE = S1 x √(1 – rxx) with S1 being SD at baseline and rxx being reliability of the scale. In our sample Sdiff = 7.00. The proportion of participants who achieved clinically significant improvement on the SCS-R was 56% (9/16) in the AMP group and 17% (2/12) in the WL group, Fisher’s exact = .054. No participants met criteria for clinically significant deterioration (defined by RCI < −1.96).
Changes in Affect as a Mediator of Increases in Connectedness Throughout Treatment
Table 2 presents the means and standard deviations for the outcome measures at each assessment point in all participants who initiated AMP. Zero-order Pearson’s correlations between the outcomes at baseline are presented in Supplemental Table 3. Results of the hypothesized mediation models are presented in Figure 2. Table 2 displays outcomes of the statistical analyses for each of these models. Consistent with the above and previously reported outcomes (Taylor, Lyubomirsky et al., 2017), time significantly predicted PANAS-PA and NA, as well as SCS-R ratings, such that participants reported feeling increasing levels of PA and connectedness, as well as decreasing levels of NA as treatment progressed (all p < .001).
Increases in PA predicted subsequent increases in social connectedness when entered in the multilevel model together with time (B = 0.40, p = .005, path b, Figure 2a). Time remained a significant predictor of increases in social connectedness when controlling for change in PA (B = 2.47, p < .001, path c’, Figure 2a). The mediation analysis revealed that the indirect effect (ab) of time on connectedness through increases in PA was significant (ab = .5440; 95% CI [.1538, 1.04742]).
Decreases in NA significantly predicted increases in connectedness when entered in the multilevel model together with time (B = −.33, p = .024, path b, Figure 2b). The direct effect of time on increases in social connectedness remained significant when controlling for change in negative affect (B = 2.44, p = .001, path c’, Figure 2b). The mediation analysis revealed that the indirect effect (ab) of time on connectedness through decreases in NA was significant (ab = .5511; 95% CI [.09437, 1.08638]).
Positive and negative affect concurrently predicting social connectedness.
Correlations revealed that PA and NA were not significantly associated at baseline, r = .05, p = .84. To determine the unique variance accounted for by PA and NA in predicting social connectedness, we examined the indirect effect of time on connectedness through concurrent changes in both PA and NA. Results of this analysis revealed that increases in PA significantly predicted increases in social connectedness when simultaneously accounting for time and changes in NA (B = .36, p = .012, path b1, Table 2, Model 4). The indirect effect (ab) of time on connectedness through increases in PA remained significant when accounting for change in NA (ab = .4896; 95% CI [.1099, .9776]). Change in NA was a marginally significant predictor of changes in connectedness over the course of treatment when accounting for concurrent changes in PA and time (B = −28, p = .058, path b2, Table 2, Model 4). The indirect effect (ab) of time on connectedness through decreases in NA was no longer significant when accounting for change in PA (ab = .4676; 95% CI [−.01614, 1.02119]. The direct effect of time on social connectedness remained significant when controlling for change in PA and NA (B = 2.05, p = .003, path c’, Table 2).
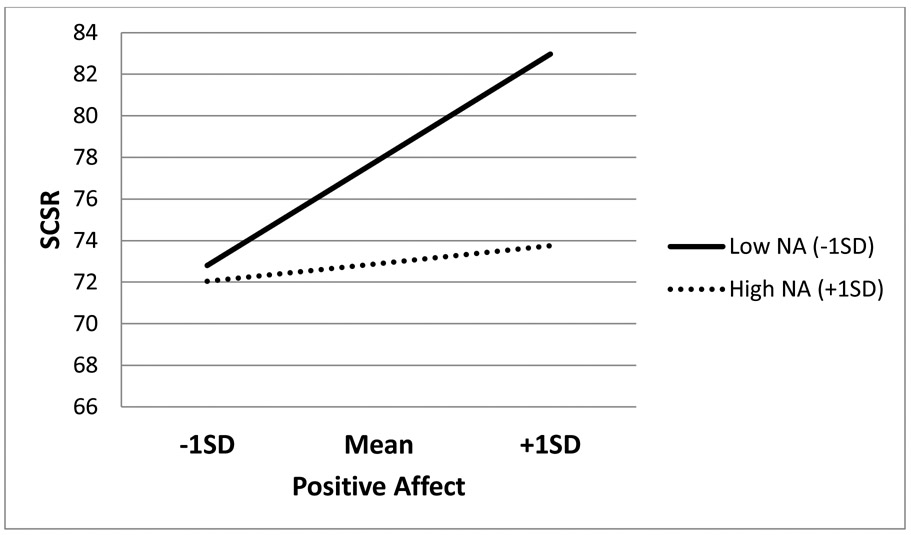
Interaction of positive and negative affect predicting social connectedness.
The interaction of PA x NA significantly predicted changes in connectedness (B = −.040, p = .005, path b1*b2, Table 2, Model 5). An examination of the pattern of estimated means from the multilevel model revealed that the association between PA and increases in connectedness was attenuated at higher levels of NA, and conversely, that the relationship between decreases in NA and increases in connectedness was diminished at lower levels of PA (see Figure 3).
Figure 3.
Estimated social connectedness scores (SCS-R) at the mid-point of treatment plotted at different levels of positive affect (PA) and negative affect (NA), that is, at one standard deviation below and above the sample mean.
Change in social connectedness predicting change in affect throughout treatment.
We also explored whether social connectedness at time t accounted for changes in PA and NA at time t + 1. Results revealed that increases in social connectedness predicted subsequent increases in PA when entered in the multilevel model together with time (B = .19, p = .001, path b). Those effects remained robust when controlling for NA at time t. This was a significant mediating effect (ab = .2412; 95% CI [.07398, .4631]). In contrast, changes in social connectedness did not predict later changes in NA (B = −.04, p = .47, path b).
Discussion
The current research examined changes in perceived social connectedness in the context of a positive activity intervention protocol—Amplification of Positivity (AMP)—for individuals seeking treatment for anxiety or depression (Taylor, Lyubomirsky et al., 2017). Consistent with predictions, participants in the AMP group reported significantly higher social connectedness following treatment than those in the control group. AMP-related increases in connectedness were maintained up to 6 months following treatment. More than half (56%) of AMP participants met criteria for clinically significant change—approximating response rates achieved on primary symptom outcomes in empirically established psychosocial treatments for anxiety (Loerinc et al., 2015) and depression (Cuijpers et al., 2014). Thus, the current findings provide preliminary evidence that the social connectedness-related benefits of positive activities previously demonstrated in non-clinical (Algoe et al., 2013; Bartlett et al., 2012; O’Connell et al., 2016; Nelson et al., 2016; Williams & Bartlett, 2015) and non-diagnosed elevated symptom samples (Alden & Trew, 2013) also extend to clinical populations. Limitations of the small sample and waitlist control group notwithstanding, these findings are encouraging given that social disconnection is a common and debilitating feature of anxiety and depression that is only partially ameliorated by existing treatments (e.g., Hofmann et al., 2014; Renner et al., 2016) and persists despite symptom remission (Saris et al., 2017).
Although the AMP regimen was intended to specifically upregulate positive valence processes, it was previously shown to decrease negative affect to a magnitude comparable to increases in positive affect (Taylor, Lyubomirsky et al., 2017), a finding consistent with extant literature (Boiler et al., 2013; Chakhssi, Kraiss, Sommers-Spijkerman, & Bohlmeijer, 2018; Sin & Lyubomirsky, 2009). The current secondary analysis revealed that both increases in positive affect and decreases in negative affect each predicted subsequent increases in connectedness throughout treatment—although associations were somewhat less robust for negative affect when considered in the same regression model alongside positive affect. These findings align with prior research suggesting that both positive affect (e.g. Fredrickson, 2013; Lyubomirsky et al., 2005) and negative affect (e.g. Keltner & Kring, 1998) contribute to social connections, and that positive affect may especially so (see Clark & Watson, 1988; Watson, Clark, McIntyre, & Hamaker, 1992; Taylor, Pearlstein et al., 2017; Taylor, Pearlstein, & Stein, 2020).
Current empirically supported treatments for anxiety and depression predominately aim to decrease negative affect. Although several of these interventions (e.g., cognitive behavioral therapy) include components that encourage engagement in positive activities to build a sense of pleasure or mastery, improvement in positive affect tends to be modest and does not always match changes in negative affect or symptoms, nor return to normative levels, on average (Dunn et al., 2020; Kring et al., 2007; Sewart et al., 2019; Strege et al., 2018). These treatments may therefore facilitate gains in social functioning largely through their success at reducing negative emotions or symptoms. Treatment regimens such as AMP, which explicitly target the upregulation of positive emotions through a wide variety of techniques (see also Craske et al., 2019; Dunn et al., 2019) may offer a different pathway or possibly added benefit for enhancing social connectedness. The current findings are consistent with the body of affective and relational literature cited above suggesting that effectively altering both positive and negative emotion in treatment may yield optimal outcomes for social relationship functioning. Knowing where a given individual lies along positive and negative affect continuums would potentially offer a more personalized and efficient approach to targeting mechanisms underpinning social disconnection.
Also in line with the notion that both positive and negative affect influence social connectedness, the current study revealed that continuing to experience heightened negative affect throughout treatment appeared to inhibit the influence of positive emotions on subsequent feelings of social connectedness; conversely, continuing to experience blunted positive affect attenuated the association between changes in negative affect and connectedness. Those findings converge with a nascent literature in clinically anxious samples suggesting that social connectedness that develops during relationship formation is accounted for by increases in positive affect, but less so when individuals concurrently experience high levels of negative affect (i.e., anxiety; Taylor, Pearlstein et al., 2017). It may be that the mechanisms that underpin the positive valence system-social connectedness link (e.g., social approach behavior, responsiveness to positive social cues) are inhibited when negative emotions are too high. Treatment-related improvements that occur along only one affective dimension may therefore have limited impact on connectedness if dysfunction in the other affective dimension persists. Our findings underscore the importance of monitoring and targeting both types of emotions in treatment and suggest that for individuals continuing to experience high negative affect or low positive affect, alternative targeted treatment strategies may be warranted. Additional research is needed to test the efficacy of combining different treatment strategies that directly target positive vs. negative affect, as well as the optimal timing for implementing those strategies. Although the AMP regimen tested herein was originally developed to serve as a standalone treatment, it may also have utility as an augmentation strategy following completion of extant treatments for those individuals who experience remaining impairment in positive affect or social connectedness. Moreover, because the positive activities within the current protocol are relatively straightforward in nature, AMP may lend itself to other implementation formats that may be less resource-intensive than individual sessions with a clinician (e.g., group psychotherapy, self-guided computer- or phone-based application).
Finally, increases in connectedness were shown to predict subsequent increases in positive affect. This finding is consistent with empirically supported theoretical accounts of a bidirectional, self-perpetuating “upward spiral,” wherein increases in positive affect strengthen social connections, which in turn promote further amplification of positive affect (Fredrickson & Joiner, 2002; Ramsey & Gentzler, 2015). Changes in social connectedness did not, however, significantly predict subsequent changes in negative affect, although the relationship was in the expected direction (i.e., increases in connectedness were associated with decreases in negative affect). Those findings suggest that variables other than social connectedness accounted for the reduction in negative affect observed over the course of AMP; however, the small sample size also limited power to detect more modest associations. Together, the present results dovetail with previous studies examining prospective, bi-directional relationships between affect, social connectedness, and symptoms of anxiety and depression. For example, naturally occurring improvements in positive social functioning (e.g., connectedness, social group integration) predict reduced subsequent risk for depression (Cruwys et al., 2013; Czyz, Liu, & King, 2012). Other longitudinal research suggests that anxiety can give rise to depression specifically when anxious avoidance leads individuals to abandon positive experiences and develop social anhedonia—a common correlate of diminished connectedness (Winer et al., 2017). Additional work suggests that discordance between positive affective experience vs. behavior relates to increased likelihood of developing depression and diminished well-being over time, in part by disrupting social connectedness (Mauss et al., 2011; although for a discussion on important cultural differences see Su, Lee, & Oishee, 2013). The current study contributes to this wider body of research and is the first, to our knowledge, to examine the temporal process of change in affect and social connectedness throughout treatment. Further elucidating the mechanisms that account for the observed associations (e.g., reduced avoidance of positive activities, increased positive emotion concordance) is an important direction for future research.
Our study findings should be considered alongside the following limitations. The effect of the AMP regimen was evaluated in a small sample and compared to a no intervention (waitlist) group that only completed measures at pre- and post-treatment (cf. repeated measures throughout treatment), which introduces several caveats. First, the chosen sample may not be representative of the target population and may produce outcomes that over- or underestimate the true treatment effect. It also increases the likelihood of baseline group differences (in this case, engagement in prior psychosocial treatment), the influence of which cannot be adequately determined. Second, the multilevel models tested herein separately evaluated main effects mediational pathways, as well as the interaction of PA and NA in predicting social connectedness. Larger samples are needed to test integrated moderated mediation models to determine whether PA accounts for subsequent increases in connectedness, but only at lower levels of NA. Third, the waitlist group displayed small-to-medium sized improvements in social connectedness—outcomes that may reflect naturally occurring fluctuations in connectedness, improvement due to treatment expectancy (i.e., the promise of eventual treatment), or sampling bias. Future studies should be carried out in larger samples with a more substantive comparison group that could help account for common therapeutic effects (e.g., therapist attention, patient expectations) and reconcile these issues. Fourth, administering more frequent repeated assessments throughout treatment and follow-up in both AMP and control groups would permit the use of longitudinal statistical models (e.g., multilevel modeling) to compare treatment effects, which is the preferred statistical approach for clinical trials favored over other methods used to handle attrition (e.g., last observation carried forward) that may over- or underestimate treatment effects; it would also account for the potential impact of repeated measurement or demand characteristics on the study outcomes, and should lead to greater precision of model estimates for the time-lagged analyses.
In terms of treatment integrity, although therapists followed a structured manual and were monitored closely during weekly supervision, AMP fidelity and adherence were not formally assessed. Further, all measures were self-reported, and perceived social connectedness does not capture the full complexity of an individual’s social functioning. Although subjective measures of social functioning (e.g., loneliness) correlate with behavioral measures (e.g., social network size, frequency of engaging in social activities), these indices are not fully redundant (Saris et al., 2017), suggesting that examining AMP-related changes in other indices of social functioning could offer incremental value beyond self-report alone. In addition, although the SCS-R demonstrated sensitivity to change when measured on a bi-weekly basis throughout treatment, it is likely that changes in some aspects of social functioning, including perceived connectedness, unfold over months or years. Research is therefore needed to clarify the long-term trajectory of change in different social outcomes (e.g., frequency of participation in social activities, satisfaction with social relationships, social support). Finally, some AMP participants continued to endorse feeling socially disconnected post-treatment—scoring below the scale mid-point—suggesting that additional AMP sessions or alternative treatment may be needed for some individuals.
The perception that we are connected to others is a basic human need that is linked to mental and physical well-being (Cacioppo & Cacioppo, 2018; Holt-Lunstad et al., 2010, 2015; Lyubomirsky et al., 2005). The current findings provide initial support for the idea that positive activities may be valuable for enhancing social connectedness in individuals with clinically impairing anxiety or depression. Although the positive emotion system served as the primary target of the current AMP protocol, increases in positive emotions as well as decreases in negative emotions accounted for subsequent increases in connectedness, suggesting multiple pathways through which connectedness can be enhanced. Because social disconnection is common across a wide range of psychiatric conditions and existing treatments leave room for improvement for many patients in this domain (Hofmann et al., 2014; McKnight & Kashdan, 2009), continued development and evaluation of transdiagnostic interventions designed to promote stronger social connections is needed. Elucidating the boundary conditions of who stands to benefit from positive activity protocols within the social domain is needed to empirically define their transdiagnostic parameters, and to inform how positive activities can be improved or combined with other interventions to optimally modify the mechanisms that underpin social disconnection across psychopathologies.
Supplementary Material
Table 3.
Summary of Multilevel Regression Analyses for Positive Affect, Negative Affect, and Their Interaction Predicting Social Connectedness Throughout Treatment.
| Model | Path | Predictor | Outcome | B | SE B | t | p |
|---|---|---|---|---|---|---|---|
| 1 | c | Time | SCS-R | 2.98 | .59 | 5.04 | <.001 |
| 2 | a | Time | PA | 1.36 | .32 | 4.30 | <.001 |
| b | PA | SCS-R | .40 | .14 | 2.86 | .005 | |
| c' | Time | SCS-R | 2.47 | .59 | 4.21 | <.001 | |
| 3 | a | Time | NA | −1.67 | .29 | −5.70 | <.001 |
| b | NA | SCS-R | −.33 | .14 | −2.30 | .024 | |
| c' | Time | SCS-R | 2.44 | .64 | 3.83 | .001 | |
| 4 | b1 | PA | SCS-R | .36 | .14 | 2.57 | .012 |
| b2 | NA | SCS-R | −.28 | .15 | −1.92 | .058 | |
| c' | Time | SCS-R | 1.03 | .31 | 3.31 | .003 | |
| 5 | b1 | PA | SCS-R | .40 | .14 | 2.93 | .004 |
| b2 | NA | SCS-R | −.33 | .14 | −2.34 | .022 | |
| b1*b2 | PA*NA | SCS-R | −.040 | .014 | −2.88 | .005 | |
| c' | Time | SCS-R | 1.81 | .62 | 2.92 | .007 |
Note. The grey shading highlights the central predictor(s) evaluated within the specified regression model. PA = positive affect; NA = negative affect; SCS-R = Social Connectedness Scale Revised.
Acknowledgments
Funding: This research was supported by grants awarded to Charles T. Taylor from the University of California, San Diego, National Institute of Health Clinical and Translational Science Awards Program Grant UL1TR001442, and from the National Institute of Mental Health R61MH113769.
Footnotes
Participants completed a functional magnetic resonance imaging (fMRI) scan at pre- and post-assessment (data presented elsewhere). Several of the eligibility criteria were implemented to ensure MRI safety and minimize confounding of the imaging findings (e.g., the upper age range was restricted due to changes in brain function that occur later in life).
We thank David Sheehan for giving us permission to use a preliminary version of the MINI for DSM-5 in this study.
We repeated the multilevel modeling analyses without including the four WL subjects who completed treatment following the WL period (i.e., AMP participants only). The pattern of findings and statistical significance was consistent with those reported in the main text for the full analysis sample.
All treatment completers (n=15) finished at least one follow-up assessment (n=14 at 3- and 6-month follow-up sessions). Missing data at a given follow-up assessment point were substituted using data from a participant’s last available assessment point (i.e., last observation carried forward). Note that the Greenhouse-Geisser corrected degrees of freedom were used given that Mauchly’s test of sphericity was significant, x2(5) = 18.86, p = .002.
We repeated the clinically significant change analysis using normative data from study 2 (M = 89.84, SD = 15.44) and study 3 (M = 91.90, SD = 14.83) reported in Lee et al. (2001). Results were identical to those reported in the main text using study 1 data.
Conflict of Interest: Sarah Pearlstein and Sanskruti Kakaria declare no conflicts of interest. Charles T. Taylor declares that in the past 3 years he has been a paid consultant for Homewood Health, and receives payment for editorial work for UpToDate. Murray B. Stein declares that in the past 3 years he has been a paid consultant for Actelion, Aptinyx, Bionomics, Janssen, Neurocrine, Pfizer, and Resilience Therapeutics, and receives payment for editorial work for UpToDate and the journals Biological Psychiatry and Depression and Anxiety. Sonja Lyubomirsky declares that in the past 3 years she has been a paid lecturer for the Cleveland Clinic, Healthworld Ltd., and Metagenics, as well as a paid consultant for Biogen Idec.
All procedures performed involving human participants were in accordance with the ethical standards of the University of California San Diego Human Research Protection Program and with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
References
- Aderka IM, Foa EB, Applebaum E, Shafran N, & Gilboa-Schechtman E (2011). Direction of influence between posttraumatic and depressive symptoms during prolonged exposure therapy among children and adolescents. Journal of Consulting and Clinical Psychology, 79(3), 421–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alden LE, & Trew JL (2013). If it makes you happy: Engaging in kind acts increases positive affect in socially anxious individuals. Emotion, 13(1), 64–75. [DOI] [PubMed] [Google Scholar]
- Algoe SB (2019). Positive interpersonal processes. Current Directions in Psychological Science, 28(2), 183–188. [Google Scholar]
- Algoe SB, Fredrickson BL, & Gable SL (2013). The social functions of the emotion of gratitude via expression. Emotion, 13(4), 605–609. [DOI] [PubMed] [Google Scholar]
- Bartlett MY, Condon P, Cruz J, Baumann J, & Desteno D (2012). Gratitude: Prompting behaviours that build relationships. Cognition & Emotion, 26(1), 2–13. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, & Gil KM (2006). Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods, 11(2), 142–163. [DOI] [PubMed] [Google Scholar]
- Beck JG (2014). Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment. Washington: American Psychological Association. [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, & Bohlmeijer E (2013). Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health, 13, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bomyea J, Ramsawh H, Ball T, Taylor C, Paulus M, Lang A, & Stein M (2015). Intolerance of uncertainty as a mediator of reductions in worry in a cognitive behavioral treatment program for generalized anxiety disorder. Journal of Anxiety Disorders, 33, 90–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boumparis N, Karyotaki E, Kleiboer A, Hofmann SG, & Cuijpers P (2016). The effect of psychotherapeutic interventions on positive and negative affect in depression: A systematic review and meta-analysis. Journal of Affective Disorders, 202, 153–162. [DOI] [PubMed] [Google Scholar]
- Breukelen GJ (2006). ANCOVA versus change from baseline had more power in randomized studies and more bias in nonrandomized studies. Journal of Clinical Epidemiology, 59(9), 920–925. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, & Cacioppo S (2018). The growing problem of loneliness. Lancet, 391(10119), 426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Norman SB, Craske MG, Sullivan G, Lang AJ, Chavira DA, … Stein MB (2009). Validation of a brief measure of anxiety-related severity and impairment: The overall anxiety severity and impairment scale (OASIS). Journal of Affective Disorders, 112(1-3), 92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carl JR, Soskin DP, Kerns C, & Barlow DH (2013). Positive emotion regulation in emotional disorders: A theoretical review. Clinical Psychology Review, 33(3), 343–360. [DOI] [PubMed] [Google Scholar]
- Chakhssi F, Kraiss JT, Sommers-Spijkerman M, & Bohlmeijer ET (2018). The effect of positive psychology interventions on well-being and distress in clinical samples with psychiatric or somatic disorders: A systematic review and meta-analysis. BMC Psychiatry, 18, 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu PS, Saucier DA, & Hafner E (2010). Meta-analysis of the relationships between social support and well-being in children and adolescents. Journal of Social and Clinical Psychology, 29(6), 624–645. [Google Scholar]
- Clark LA, & Watson D (1988). Mood and the mundane: Relations between daily life events and self-reported mood. Journal of Personality and Social Psychology, 54(2), 296–308. [DOI] [PubMed] [Google Scholar]
- Cohen S (2004). Social relationships and health. American Psychologist, 59(8), 676–684. [DOI] [PubMed] [Google Scholar]
- Craske MG, Meuret AE, Ritz T, Treanor M, & Dour HJ (2016). Treatment for anhedonia: A neuroscience driven approach. Depression and Anxiety, 33(10), 927–938. [DOI] [PubMed] [Google Scholar]
- Craske MG, Meuret AE, Ritz T, Treanor M, Dour HJ & Rosenfield D (2019). Positive affect treatment for depression and anxiety: A randomized clinical trial for a core feature of anhedonia. Journal of Consulting and Clinical Psychology, 87(5), 457–471. [DOI] [PubMed] [Google Scholar]
- Craske MG, Treanor M, Conway CC, Zbozinek T, & Vervliet B (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford JR, & Henry JD (2004). The positive and negative affect schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 43(3), 245–265. [DOI] [PubMed] [Google Scholar]
- Cruwys T, Dingle GA, Haslam C, Haslam SA, Jetten J, & Morton TA (2013). Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Social Science & Medicine, 98, 179–186. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, & Dobson KS (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. The Canadian Journal of Psychiatry, 58(7), 376–385. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Karyotaki E, Weitz E, Andersson G, Hollon SD, & van Straten A (2014). The effects of psychotherapies for major depression in adults on remission, recovery and improvement: A meta-analysis. Journal of Affective Disorders, 159, 118–126. [DOI] [PubMed] [Google Scholar]
- Czyz EK, Liu Z, & King CA (2012). Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. Journal of Clinical Child & Adolescent Psychology, 41(2), 214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dichter GS, Felder JN, Petty C, Bizzell J, Ernst M, & Smoski MJ (2009). The effects of psychotherapy on neural responses to rewards in major depression. Biological Psychiatry, 66, 886–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon DG, Rosso IM, Pechtel P, Killgore WD, Rauch SL, & Pizzagalli DA (2013). Peril and pleasure: An RDoC-inspired examination of threat responses and reward processing in anxiety and depression. Depression and Anxiety, 31(3), 233–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn BD, German RE, Kazanov G, Zu C, Hollon SD & DeRubeis RJ (2020) Changes in positive and negative affect during pharmacological treatment and cognitive therapy for major depressive disorder - A secondary analysis of two randomized controlled trials. Clinical Psychological Science, 8, 36–51. [Google Scholar]
- Dunn BD, Widnall E, Reed N, Owens C, Campbell J, & Kuyken W (2019). Bringing light into darkness: A multiple baseline mixed methods case series evaluation of Augmented Depression Therapy (ADepT). Behaviour Research and Therapy, 120, 103418. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, & Cole SW (2012). Social neuroscience and health: Neurophysiological mechanisms linking social ties with physical health. Nature Neuroscience, 15(5), 669–674. [DOI] [PubMed] [Google Scholar]
- Elliot AJ (2006). The hierarchical model of approach-avoidance motivation. Motivation and Emotion, 30(2), 111–116. [Google Scholar]
- Emmons RA, & Mccullough ME (2003). Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology, 84(2), 377–389. [DOI] [PubMed] [Google Scholar]
- Eng W, Coles ME, Heimberg RG, & Safren SA (2005). Domains of life satisfaction in social anxiety disorder: Relation to symptoms and response to cognitive-behavioral therapy. Journal of Anxiety Disorders, 19(2), 143–156. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (2013). Positive emotions broaden and build. Advances in Experimental Social Psychology, 47, 1–53. [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, & Finkel SM (2008). Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95(5), 1045–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, & Joiner T (2002). Positive emotions trigger upward spirals toward emotional wellbeing. Psychological Science, 13, 172–175. [DOI] [PubMed] [Google Scholar]
- Gable SL, & Berkman ET (2008). Making connections and avoiding loneliness: Approach and avoidance social motives and goals In Elliot AJ (Ed.), Handbook of approach and avoidance motivation (pp. 203–216). New York: Psychology Press. [Google Scholar]
- Gable SL, & Reis HT (2010). Good news! Capitalizing on positive events in an interpersonal context. Advances in Experimental Social Psychology, 42, 195–257. [Google Scholar]
- Gray JA (1987). The psychology of fear and stress (2nd ed.). New York: Cambridge University Press. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 1–25. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, & Smits JA (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. The Journal of Clinical Psychiatry, 69(4), 621–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Wu JQ, & Boettcher H (2014). Effect of cognitive-behavioral therapy for anxiety disorders on quality of life: A meta-analysis. Journal of Consulting and Clinical Psychology, 82(3), 375–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, DeRubeis RJ, Fawcett J, Amsterdam JD, Shelton RC, Zajecka J, … & Gallop R (2014). Effect of cognitive therapy with antidepressant medications vs antidepressants alone on the rate of recovery in major depressive disorder: a randomized clinical trial. JAMA Psychiatry, 71, 1157–1164. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10, 227–237. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7, e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR, & Dimidjian S (2001). Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice, 8, 255–270. [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. [DOI] [PubMed] [Google Scholar]
- Jose PE, Lim BT, & Bryant FB (2012). Does savoring increase happiness? A daily diary study. Journal of Positive Psychology, 7(3), 176–187. [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3(1), 1–27. [DOI] [PubMed] [Google Scholar]
- Keltner D, & Kring AM (1998). Emotion, social function, and psychopathology. Review of General Psychology, 2, 320–342. [Google Scholar]
- Kenny DA, Korchmaros JD, & Bolger N (2003). Lower level mediation in multilevel models. Psychological Methods, 8(2), 115–128. [DOI] [PubMed] [Google Scholar]
- Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, … Fredrickson BL (2013). How positive emotions build physical health. Psychological Science, 24(7), 1123–1132. [DOI] [PubMed] [Google Scholar]
- Kring AM, Persons JB, & Thomas C (2007). Changes in affect during treatment for depression and anxiety. Behaviour Research and Therapy, 45(8), 1753–1764. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakens D (2013). Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4, 863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang PJ (1995). The emotion probe: Studies of motivation and attention. American Psychologist, 50(5), 372–385. [DOI] [PubMed] [Google Scholar]
- Layous K, Chancellor J, & Lyubomirsky S (2014). Positive activities as protective factors against mental health conditions. Journal of Abnormal Psychology, 123(1), 3–12. [DOI] [PubMed] [Google Scholar]
- Lee RM, Draper M, & Lee S (2001). Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: Testing a mediator model. Journal of Counseling Psychology, 48(3), 310–318. [Google Scholar]
- Loerinc AG, Meuret AE, Twohig MP, Rosenfield D, Bluett EJ, & Craske MG (2015). Response rates for CBT for anxiety disorders: Need for standardized criteria. Clinical Psychology Review, 42, 72–82. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, King L, & Diener E (2005). The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin, 131(6), 803–855. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, & Layous K (2013). How do simple positive activities increase wellbeing? Current Directions in Psychological Science, 22, 57–62. [Google Scholar]
- Mackinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz JC, & Weissman MM (2004). Interpersonal psychotherapy: Principles and applications. World Psychiatry, 3(3), 136. [PMC free article] [PubMed] [Google Scholar]
- Mauss IB, Shallcross AJ, Troy AS, John OP, Ferrer E, Wilhelm FH, & Gross JJ (2011). Don't hide your happiness! Positive emotion dissociation, social connectedness, and psychological functioning. Journal of Personality and Social Psychology, 100(4), 738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcknight PE, & Kashdan TB (2009). The importance of functional impairment to mental health outcomes: A case for reassessing our goals in depression treatment research. Clinical Psychology Review, 29(3), 243–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore RC, Chattillion EA, Ceglowski J, Ho J, von Känel R, Mills PJ, … Mausbach BT (2013). A randomized clinical trial of behavioral activation (BA) therapy for improving psychological and physical health in dementia caregivers: Results of the Pleasant Events Program (PEP). Behaviour Research and Therapy, 51, 623–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson SK, Layous K, Cole SW, & Lyubomirsky S (2016). Do unto others or treat yourself? The effects of prosocial and self-focused behavior on psychological flourishing. Emotion, 16(6), 850–861. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuis R, Te Grotenhuis M, & Pelzer B (2012). “influence.ME: Tools for detecting influential data in mixed effects models.” R Journal, 4(2), 38–47. [Google Scholar]
- O’Connell BH, O’Shea D, & Gallagher S (2016). Enhancing social relationships through positive psychology activities: A randomised controlled trial. The Journal of Positive Psychology, 11(2), 149–162. [Google Scholar]
- Olatunji BO, Cisler JM, & Tolin DF (2007). Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review, 27(5), 572–581. [DOI] [PubMed] [Google Scholar]
- Ramsey MA, & Gentzler AL (2015). An upward spiral: Bidirectional associations between positive affect and positive aspects of close relationships across the life span. Developmental Review, 36, 58–104. [Google Scholar]
- Renner F, Cuijpers P, & Huibers MJH (2014). The effect of psychotherapy for depression on improvements in social functioning: a meta-analysis. Psychological Medicine, 44(14), 2913–2926. [DOI] [PubMed] [Google Scholar]
- Saris IMJ, Aghajani M, van der Werff SJA, van der Wee NJA, & Penninx BWJH (2017). Social functioning in patients with depressive and anxiety disorders. Acta Psychiatrica Scandinavica, 136(4), 352–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman ME, Steen TA, Park N, & Peterson C (2005). Positive psychology progress: Empirical validation of interventions. American Psychologist, 60(5), 410–421. [DOI] [PubMed] [Google Scholar]
- Sewart AR, Niles AN, Burklund LJ, Saxbe DE, Lieberman MD, & Craske MG (2019). Examining positive and negative affect as outcomes and moderators of cognitive-behavioral therapy and acceptance and commitment therapy for social anxiety disorder. Behavior Therapy, 56, 1112–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. [DOI] [PubMed] [Google Scholar]
- Strege MV, Swain D, Bochicchio L, Valdespino A, & Richey JA (2018). A pilot study of the effects of mindfulness-based cognitive therapy on positive affect and social anxiety symptoms. Frontiers in Psychology, 9, 866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong G, & Aron A (2006). The effect of shared participation in novel and challenging activities on experienced relationship quality: Is it mediated by high positive affect? In Vohs KD & Finkel EJ (Eds.), Intrapersonal processes in interpersonal relationships (pp. 342–359). New York: Guilford. [Google Scholar]
- Su JC, Lee RM, & Oishi S (2013). The role of culture and self-construal in the link between expressive suppression and depressive symptoms. Journal of Cross-Cultural Psychology, 44(2), 316–331. [Google Scholar]
- Tabachnick BG, & Fidell LS (2007). Using multivariate statistics (5th ed.). Boston, MA: Allyn & Bacon/Pearson Education. [Google Scholar]
- Taylor CT, Lyubomirsky S, & Stein MB (2017). Upregulating the positive affect system in anxiety and depression: Outcomes of a positive activity intervention. Depression and Anxiety, 34(3), 267–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CT, Pearlstein SL, & Stein MB (2017). The affective tie that binds: Examining the contribution of positive emotions and anxiety to relationship formation in social anxiety disorder. Journal of Anxiety Disorders, 49, 21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CT, Pearlstein SL, & Stein MB (2020). A tale of two systems: Testing a positive and negative valence systems framework to understand social disconnection across anxiety and depressive disorders. Journal of Affective Disorders, 266, 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo AR, Choi H, & Valenstein M (2013). Social relationships and depression: Ten-year follow-up from a nationally representative study. PLoS One, 8, e62396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trew JL (2011). Exploring the roles of approach and avoidance in depression: An integrative model. Clinical Psychology Review, 31(7), 1156–1168. [DOI] [PubMed] [Google Scholar]
- Umbersen D, & Montez JK (2010). Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior, 51(Suppl), S54–S66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers AJ, & Altman DG (2001). Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ, 323(7321), 1123–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, McIntyre CW, & Hamaker S (1992). Affect, personality, and social activity. Journal of Personality and Social Psychology, 63, 1011–1025. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Waugh CE, & Fredrickson BL (2006). Nice to know you: Positive emotions, self–other overlap, and complex understanding in the formation of a new relationship. The Journal of Positive Psychology, 1(2), 93–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LA, & Bartlett MY (2015). Warm thanks: Gratitude expression facilitates social affiliation in new relationships via perceived warmth. Emotion, 15(1), 1–5. [DOI] [PubMed] [Google Scholar]
- Winer ES, Bryant J, Bartoszek G, Rojas E, Nadorff MR, & Kilgore J (2017). Mapping the relationship between anxiety, anhedonia, and depression. Journal of Affective Disorders, 221, 289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.