Abstract
Background:
Recent years have witnessed wide applications of exergames to balance training among the older adults. However, research concerning balance training with the use of Kinect for Xbox has remained scarce. While previous studies have shown the positive effects of exergames on improving balance and preventing falling among the older adults, there has been a paucity of empirical evidence supporting the superiority of Kinect exercise to conventional exercise over balance training among the older adults. Therefore, this study aimed to compare the feasibility, safety, and effectiveness of Kinect exercise against conventional exercise over balance training among the community older adults.
Method:
A total of 20 participants were randomly assigned to the Kinect Exercise Group (N = 10) or the Conventional Exercise Group (N = 10) for a 5-week balance training (45 minutes a time, 2 times a week). Assessor blinding was employed to assess the participants’ performance before and after the treatment, including 30-Second Chair Stand Test (30-sec CST), Timed Up and Go (TUG), Functional Reach Test (FRT), and One-Leg Stance Test (OLST) respectively with eyes open and closed. Subjective feeling of the intensity of pain and side effects were recorded throughout the investigation period. Nonparametric statistics was used for data analysis.
Results:
Within-group comparison between the pre-test and post-test indicated that significant differences existed in all of the 5 tests (30-sec CST, TUG, FRT, OLST with eyes open, and OLST with eyes closed) in the Kinect exercise group. To the Conventional exercise group, however, significant differences were only observed in 30-sec CST, FRT and OLST with eyes open. With regard to between-group comparison, significant differences were only found in FRT.
Conclusion:
Such results indicated that both treatments were helpful in improving the participants’ balance performance, that Kinect exercise was more effective in terms of overall balance ability, and that Kinect exercise was particularly beneficial to functional reach enhancement in comparison with traditional exercise. Kinect exercise could be a feasible, safe, and effective alternative for dynamic balance training among older adults.
Keywords: balance training, exergames, Kinect, older adults
1. Introduction
Older adult population aged above 65 in Taiwan has been rising.[1] Age-related deterioration includes weak lower-limb muscles, decreased endurance, poor balance and posture control, slow walking speed, short stride, and decreased reaction capacity.[2] Older adults’ increased mobility difficulty, elongated reaction time, and declining quality in daily-activity participation result in accidental injuries, with the most common being caused by falling.[3] Gehlsen and Whaley[4] noted that balance control capability is significantly correlated with the incidence rate of falls. Furthermore, poor balance and postural stability are the most common problems related to falling.[5]
According to a long-term follow-up survey of the physical, psychological, and social lives of older adults in Taiwan, providing regular physical activity to older adults can help improve their daily life abilities, enhance their balance capacity, and reduce the incidence of fractures as well as the risk and mortality of other chronic diseases.[6] In addition, exercise increases physical activity, improves muscle strength, facilitates balance, and reduces risks of falls and fractures among older adults.[7,8]
Conventional exercises such as physical training,[9–11] strengthening exercise,[12] aerobic exercise,[13] Tai Chi,[14] and balance training[15] are effective ways to strengthen the lower-limb muscles, endurance, walking function, and balance ability of the older adults, thus preventing falling incidents. However, problems as poor exercise compliance, inadequate exercise intensity, and inability to effectively maintain training outcomes influence the success of interventions.[16–19]
Therefore, researchers and practitioners have directed their attention to other alternatives. Virtual reality (VR), compared with conventional exercise models, creates an interactive simulated environment capable of immersing users in a virtual setting and allowing them to interact with it. As technology advances, game technology has also undergone profound innovation and change, enabling it to be applied to balance training for older adults.[20,21]
Since their emergence, VR and exergames have been used as instruments for rehabilitation assessment and treatment.[22,23] Previous studies have shown how VR-based exergames positively affect participants’ motivation and pleasure.[24,25] In fact, exergames possess the following advantages over conventional physical exercise. First, exergames are more attractive and the nature of real-time interaction enhances players’ motivation. Players can simultaneously practice actions and cognitive skills when performing in-game tasks.[26,27] Second, exergames emphasize correct positions for particular body movements. That means players can focus on participating in a game and concentrate on in-game interactions without paying special attention to their movements.[28] Third, exergames can be played alone at home[29] or together with a small group.[30,31] Such an social function makes exergames more appealing to older adults.
In comparing motion capture controller among Vicon systems, Nintendo Wii, Sony Playstation EyeToy, and Xbox Kinect, Xbox Kinect (Microsoft Xbox 360, Redmond, WA) is considered the most appropriate system for this study. It does not require any specific controller and is equipped with a sensitive sensor, which provides accurate motion-capture.[32–34] The use of Xbox Kinect for balance training in older adults is not new. Previous examinations have proved the beneficial effects of using Xbox Kinect on improving the balance ability of older adults.[35–38]
Recently, studies focusing on older adults’ balance function using exergames (e.g., played on the Nintendo Wii) have verified the positive effects of such games on balance training and fall prevention.[20,22,30,39,40] Although the literature has shown that both exergames and traditional balance training were effective in improving balance,[41] studies comparing exergames with traditional physical balance exercises have shown mixed results.[42,43] While we hypothesized that Kinect exercise was more advantageous than conventional exercise in terms of functional balancing, such assumption required further empirical validation. To address this research gap, therefore, the purpose of the present study was to examine the effects of Kinect exercise on balance training against conventional physical exercise among community older adults.
2. Methods
2.1. Design
This study was an assessor-blind clinical trial in which participants were randomly assigned to a Kinect exercise group or conventional exercise group; blinding was only imposed on the evaluator. The participants were community older adults aged above 60. Ethical approval for this study (No. IRB-10709-001) was provided by the Institutional Review Board of Chi Mei Hospital, Taiwan, on October 22, 2018. Written informed consent from all of the participants was obtained before the intervention implementation. The research commenced once the participants comprehended the research purposes and experimental procedure.
2.2. Participants and recruitment
The recruitment criteria of the participants were as follows:
-
(1)
aged above 60 who lived in the same community;
-
(2)
having normal cognitive comprehension abilities and a score of at least 24 points on the Mini-Mental State Examination (MMSE);[44]
-
(3)
having undergone confirmations of disease history and health status through answering a health survey and the Physical Activity Readiness Questionnaire (PAR-Q)[45] to ensure safety of the training; (4) possessing normal comprehension and visual functions; and
-
(4)
being able to walk more than 10 minutes with or without the aid of an assistive device.
The exclusion criteria were as follows:
-
(1)
cognitive impairment;
-
(2)
diabetes mellitus and neuropathy or peripheral artery disease;
-
(3)
dyskinesia induced by orthopedic or neurological diseases; and
-
(4)
other neurological disorders or diseases.
2.3. Research process
The demographic data (e.g., sex, age, height, weight, and medical conditions) of eligible participants who agreed to participate were recorded. After an eligibility review with the participants that employed the MMSE and PAR-Q to confirm their health status, a pretest was conducted to determine their basic balance ability. Subsequently, the participants were randomly divided into 2 groups (Kinect exercise group and conventional exercise group) by drawing lots, after which the exercise intervention was implemented (Fig. 1).
Figure 1.
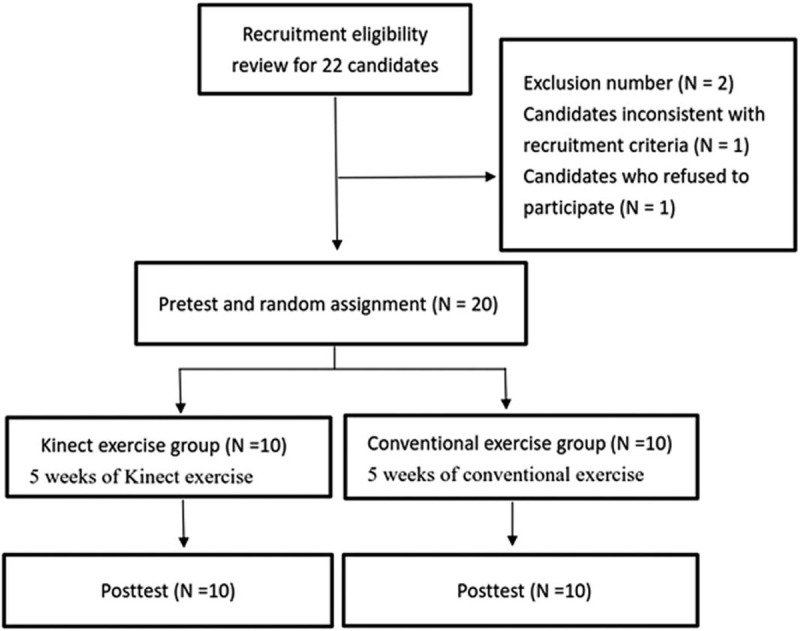
Research procedure.
The research purposes and procedure were explained in detail to all participants; they were entitled to know the post-training results and evaluation data. To maintain consistency during training, the research was conducted at the same community activity center, which also ensured that their performance was not susceptible to environmental disturbances and could be completed under the same conditions.
Before the experiment commenced, a 30-minute description and explanation session was held. Both groups were monitored by a qualified occupational therapist during 45-minute training sessions, which were conducted twice a week for consecutive 5 weeks.
2.4. Interventions
2.4.1. Kinect exercise group
The hardware devices used in this group were a Microsoft Kinect for Xbox 360, projector, and stopwatch; the game software was Your Shape: Fitness Evolved II (Chinese version).
For the basic training, the Zen Mode of Your Shape: Fitness Evolved I used by Kim et al[37] was referenced when selecting the exergames content. According to the occupational therapy analysis theory proposed by Hagedorn,[46] this study selected the games in Your Shape: Fitness Evolved II that were suitable for training older adults’ static and dynamic balance and lower-body endurance. After functional activity analysis was performed, this study selected the following exergames: Zen Energy, Yoga, Destination Bollywood, Cardio Boxing, Humana Vatality and Cardio.
The training was conducted in groups, with each session led by a participant who was responsible for operating the game and exercise. Other participants followed the movements. Each participant took turns to serve as the leader to ensure fair rotation until the research concluded (Fig. 2).
Figure 2.
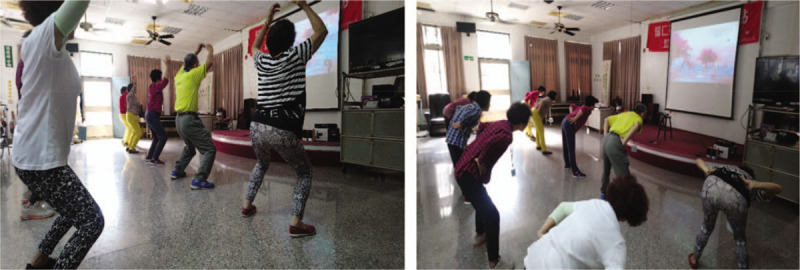
Kinect Exercise Group: exergames included Zen Energy, Yoga, Destination Bollywood, Cardio Boxing, Humana Vatality and Cardio.
Each exergame is described in the following paragraphs:
Zen Energy is a slow and gentle fitness game; some of its movements are similar to tai chi and yoga, and can train participants to shift their center of gravity and enhance lower-body strength to improve static balance.
Yoga is a relaxation and coordination game that emphasizes stretching, stability, coordination, and control. It can train the muscle coordination and stability of the core muscles and lower limbs.
Destination Bollywood uses brisk rhythms and dance moves, rhythmic dancing involving all limbs, and abdomen and hip exercises to train participants to shift their center of gravity and slow to fast movements, thereby enhancing dynamic balance.
Cardio Boxing is based on boxing moves combined with squatting, left–right weight shifting, and kicking in coordination with slow to fast beats. The game trains upper- and lower-limb muscle endurance as well as the ability to shift the body's center of gravity to enhance dynamic balance.
Humana Vatality and Cardio share similar contents, focusing on lower-limb muscle endurance and weight shifting. The games provide a variety of dynamic balance activities and focus on highly repetitive limb movements.
The exercise schedule for the Kinect group was as follows: Zen Energy and Yoga were employed as a warm up; Destination Bollywood was used for training for the first 3 sessions; and Cardio Boxing and Humana Vatality were used for the following 4 sessions. In the final 3 sessions, the training intensity was enhanced by introducing Humana Vatality and Cardio. All sessions included a 3-minute break and concluded with Zen Energy and Yoga.
Each session lasted for 45 minutes; the Kinect exercise group adopted a diverse sports game class to provide participants with an opportunity to sample different exergames, the purpose of which was primarily to train their static and dynamic balance as well as lower-limb muscle endurance.
2.4.2. Conventional exercise group
The training content for this group was based on a course designed by Campbell et al,[47] which was specifically designed for preventing falls among older women. The content of this course has been verified to effectively reduce the incidence of falls and improve the balance ability of older adults. Thus, it was adopted as the training framework for the conventional exercise group in the present study. A 2-stage exercise training intervention was planned. The first stage consisted of a 5-minute warmup, 15-minute training activity, and 3-minute break, whereas the second stage consisted of 12 minutes of exercise and 5 minutes of final relaxation. Each session lasted for 45 minutes. The warmup activity in the first stage comprised slow physical exercises and stretching. The training activity employed tempo music in conjunction with lower-body strengthening exercises, mark time exercises, sideways walking exercises, walking forward and backward, squat-to-stand exercises, and stepping and leg lifting. After the break, the second stage employed chairs as an assistive tool, which the participants leaned on while standing to train their static balance and lower-limb muscle endurance. This included tandem standing exercises, tandem walking, and 1-leg standing. Additional training such as sit-to-stand exercises, half squats, and leg lifting were performed when participants were sitting on the chair. Finally, the second stage concluded with slow stretches, breathing adjustment, and relaxation (Fig. 3). The activities in the conventional exercise group were also conducted in groups. All 10 sessions (i.e., twice a week for 5 weeks) included the aforementioned exercises and were guided by the same occupational therapist.
Figure 3.

Conventional Exercise Group: (A) lower-body strengthening exercise; (B) second stage employed chairs as an assistive tool to train their balance.
To compare the effects of Kinect exergames and conventional exercise on older adults’ balance ability, the 2 groups were respectively guided by the Kinect's built-in trainers (for the Kinect exercise group) and an occupational therapist (for the conventional exercise group). Despite the differences in training contents and activities, the objective was the same; that is, to provide exercise interventions that trained participants’ muscle strength and balance ability for post-intervention analysis of the results.
2.5. Outcome measures
The focus of the evaluation was to understand the overall balance ability of older adults aged above 60, by specifically examining performance of lower-body strength (a construct crucial to overall balance ability), walking speed and agility, and dynamic as well as static balance. A clinical assessment tool with favorable reliability and credibility was employed to record the participants’ performance. The lower-body strength used 30-second Chair Stand Test (30-sec CST), and functional balance assessments content included the Timed Up and Go test (TUG), Functional Reach Test (FRT), and One-Leg Stance Test (OLST) respectively with eyes open and closed. Assessments of the feasibility and safety of the exercises involved recording the participants’ overall participation rate, attendance rate, and subjective feelings of pain. A 10-cm visual analogue scale or verbal rating scale was used to record whether each exercise session caused joint pain, as well as whether adverse events (e.g., injuries, falls, and medical problems) or side effects (e.g., soreness, dizziness, nausea, and headaches) occurred during exercise. The test criteria and definitions were as follows:
30-sec CST: Participants sit in the middle of a chair with their back straightened (without leaning against the chair), feet on the ground, and hands crossed in front of their chests. Upon the researcher's signal, they stand and sit repeatedly for 30 seconds and the number of completions is recorded. The test–retest reliability (R = 0.92; 95% CI: 0.87–0.95) and validity (.71) of this experiment were favorable.[48]
TUG: Participants sit on a chair with their hands resting naturally in their laps and backs leaning against the chair. When the test commences, they stand without relying on the armrest, walk 3 m forward, and then turn back toward the chair and sit down; the researcher records the time required for the entire process. The test is repeated twice, and the average of the 2 results is recorded for further analysis. The sensitivity and specificity of the test were both 87%, indicating favorable test consistency; furthermore, its test–retest reliability was ICC = 0.98–0.99.[49]
FRT: Participants are asked to stand with their right side against a wall and lift their right hand upward until their arm is horizontal (90°), after which they clench their fists and reach forward in a progressive manner until their maximum limit. The difference between the final position of the third metacarpophalangeal joint and the initial position of the cloth ruler is recorded, which represents the distance (cm) that the participants can reach forward. During this process, they must not touch the wall, bend their feet, or take any steps. The measurement is conducted twice and the average of the 2 results is calculated. The inter- and intra-rate reliability scores of this test were .98 and .92, respectively.[50]
OLST: Participants stand on 1 foot (their dominant foot) under open and closed eye conditions, and the time that they can remain standing is recorded. Once timing commences, participants cross their arms in front of their chest and raise one of their feet up to a 90° level; their body must remain upright and their feet cannot touch. Participants must look directly at a target 3 m in front of them when standing with eyes open, whereas when their eyes are closed, timing commences after they confirm that they are standing on 1 foot with a stable posture and closed eyes. The timing is stopped when participants’ feet touch, their lifted foot is grounded, their hands move and the initial posture is not maintained, or their balance is lost. The tester provides participants with full protection throughout the test to prevent them from falling. The test is repeated twice, and the average of the results is recorded for further analysis. The intraclass correlation coefficient of this test was .73.[51]
Subjective feeling of pain: A 10-cm visual analogue scale or verbal rating scale is employed, which uses a 10-cm line. The left and right ends of the line are marked with 0 and 10 cm, denoting no pain and severe pain, respectively. Participants are asked to mark a position on the line that represents their pain, and the value is recorded. Alternatively, the tester can explain the meaning of 0 to 10 and allow verbal rating by patients. Results showed that the test–retest reliability of the numerical rating scale was ICC = .822, whereas the validity test indicated that the Spearman correlation of the criterion validity was .74–.95.[52]
2.6. Statistical analysis
Statistical analysis was conducted using IBM SPSS Statistics 24.0 and P < . 05 was considered statistically significant. Furthermore, all analyzed values were presented using medians (Q1–Q3). Nonparametric statistical analysis was adopted because of the relatively small sample size and the skewed distribution between the 2 groups. Descriptive statistics were applied to analyze the demographic data and evaluation items of the participants in each group. To compare the performance between the 2 groups, Fisher exact test was used in the category data (sex and diseases), whereas the Mann–Whitney U test was used to compare continuous data (age, height, and weight). The dependent variable (balance performance) in this study was subjected to intragroup comparison using the Wilcoxon signed-rank test, whereas a between-group comparison was performed using the Mann–Whitney U test.
3. Results
3.1. Demographic data and pretest values of participants
3.1.1. Recruitment and baseline characteristics
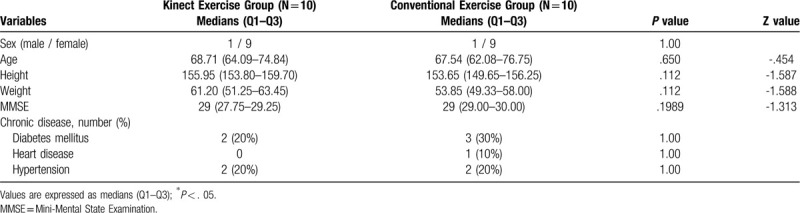
A total of 22 older adults were recruited into this study; 1 was absent during the pretest and was thus excluded, as was another with severe heart disease whose condition did not meet the recruitment criteria. Ultimately, 20 older adults participated in this study and were randomly assigned to the Kinect exercise group (1 male and 9 females, median (Q1–Q3) = 68.71 (64.09–74.84)) and conventional exercise group (1 male and 9 females, median (Q1–Q3) = 67.54 (62.08–76.75)). The overall participation rate of the 2 groups were 100% and 96%, respectively, and the between-group comparison showed that neither group had statistically significant differences in terms of demographic data, such as age, height, weight, MMSE score, and chronic disease (see Table 1).
Table 1.
Analysis of participants’ demographic data.
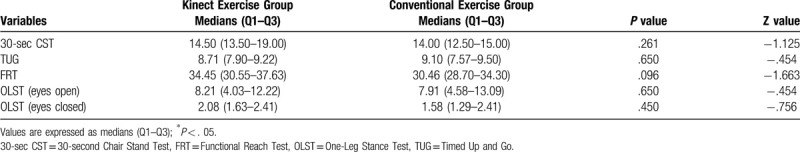
Statistical analysis of the pretest results of the 2 groups revealed that the 30-sec CST, TUG, FRT, OLST respectively with open and closed eyes did not achieve between-group significant differences. All parameter data presented a consistent benchmark before the training (see Table 2).
Table 2.
Pretest between-group comparison of assessments.
3.1.2. Functional balance test values
Table 3 presents the within-group analysis results for the 2 groups after 5 weeks of training. The Kinect exercise group achieved significant differences in the results of the 30-sec CST (P = .005), TUG (P = .005), FRT (P = .005), OLST with eyes open (P = .005), and OLST with eyes closed (P = .005).
Table 3.
Within-group pretest and post-test comparisons of the 2 groups’ assessment data.
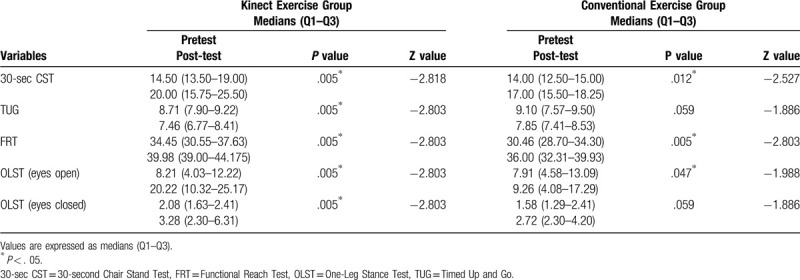
The within-group analysis of the test results of the conventional exercise group indicated that the participants displayed significant improvements in the 30-sec CST (P = .012), FRT (P = .005), and OLST with eyes open (P = .047), whereas significant differences were not achieved in the TUG (P = .059) and OLST with eyes closed (P = .059).
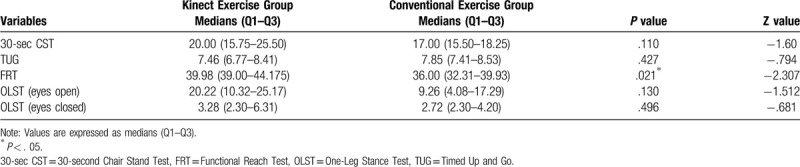
The between-group comparison showed that a significant difference was only observed in FRT (P = .021). Despite other evaluated items showing significant progress in the within-group comparison of the Kinect exercise group, they did not achieve a significant with those of the conventional exercise group in the between-group comparison (see Table 4).
Table 4.
Post-test between-group comparison of participants’ assessed items.
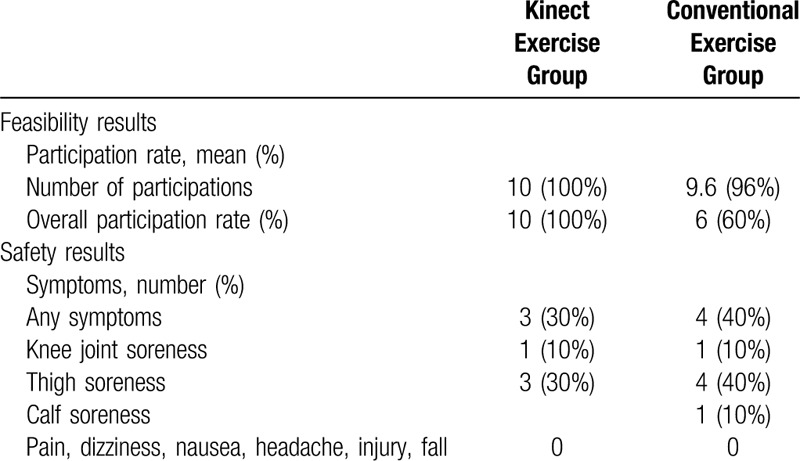
3.1.3. Feasibility and safety record
The conventional exercise group had an overall participation rate of 96%, with 6 participants attending every training session whereas the other 4 each absent once due to regular medical checkups and personal affairs. The Kinect exercise group had a 100% overall participation rate, with all the participants attending the entire training.
No accidents or medical problems occurred during the research. The most common post-exercise symptom among the participants was soreness, and all symptoms disappeared after rest; thus, they did not affect the research. Side effects occurred 12 times in the conventional exercise group, including knee joint soreness (2 times), thigh soreness (9 times), and calf soreness (1 time). By contrast, side effects occurred 6 times in the Kinect exercise group, including knee joint soreness (2 times) and thigh soreness (4 times). Neither group showed any signs of dizziness, nausea, headache, injury, or fall (see Table 5).
Table 5.
Feasibility and safety statistics.
4. Discussion
4.1. Main results
This study recruited 20 older adults aged above 60 who lived in the same community, with them randomly assigned to the Kinect exercise group or the conventional exercise group. To both groups, exercise training was conducted twice a week for a total of 5 weeks. The results in Table 3 showed that the participants in the Kinect exercise group made significant improvement in all of the 5 tests, including 30-sec CST, TUG, FRT, OLST with eyes open, and OLST with eyes closed. Those in the conventional exercise group, likewise, showed improvement in 30-sec CST, FRT, and OLST with eyes open at a significant level. Taken together, both exercise designs were particularly beneficial to balance ability enhancement in the 30-sec CST, FRT, and OLST with eyes open. A further analysis of the overall balance ability between the 2 groups suggested that after 5 weeks of exercise training, the Kinect exercise group outperformed the conventional exercise group in FRT. Significant between-group differences in other areas were not observed.
Such results indicated that both treatments were helpful in improving the participants’ balance performance. Furthermore, Kinect exercise was more effective in terms of overall balancing presentation, as evidenced in the participants’ improvement in all of the 5 tests. Last but the least, Kinect exercise was particularly beneficial to functional reach enhancement in comparison with traditional exercise.
4.2. Lower-body strength and functional balance performance
The 30-sec CST test was employed to assess the participants’ lower-body strength, a construct crucial to overall balance ability. As shown in previous studies, the number of falls increases by 35% to 40% when an individual reaches 60 years old, mainly due to reduced muscle strength and balance.[53–55] The literature has also revealed that lack of physical activity may result in lower-limb weakening and impairment of balance, which has been found to be significant predictors of falls in community-dwelling elderly.[56] The older adults in both groups of this study showed improvement in the 30-sec CST. That is because the training session for both groups involved lower-limb training. Therefore, their improvement in such aspect was as expected.
TUG performance includes multiple factors as agility, lower-limb strength, balance ability and walking speed. TUG provides information about mobility because it covers actions commonly seen in daily lives, such as standing from a seated position, walking, changing the direction.[57] In this study, TUG improvement was only observed in the Kinect exercise group. A potential reason for such an improvement only located in the Kinect exercise group is that interactive video games attracted the older adults and helped them to increase functional activity performance by engaging in position changing movements and maintaining postural control, echoing previous studies that increase in more accurate postural control contributed to an improvement in dynamic balance, muscle strength reinforcement, and role of mirror neurons.[25] Furthermore, this finding aligned with previous studies in that higher motivation and interest led to awareness of balance control.[58] Overall speaking, Kinect exergames played a crucial role in helping older adults to enhance their TUP performance.
As regards the One Leg Stance Test (OLST), a standardized test that measures static balance,[55] the results of the present study showed that the static balance of both groups improved with the participants’ eyes open. The participants in the Kinect exercise group also improved with eyes closed. Since the exercise in both groups required 1 leg standing and weight shifting practices, the participants therefore improved their static balance. However, as Kinect exercise required repeated shifting of body weight between 2 legs, this kind of exercise might improve the proprioception of the knee joints,[59] leading to significant improvement in OLST with eyes closed in the Kinect exercise group. Besides, the physiological demand of the Kinect exergames might help fortify the static balance and posture control.
Functional Reach Test (FRT) is a clinical outcome measure and assessment tool for ascertaining dynamic balance in 1 simple task. The FRT is a quick single-task dynamic test defined as the maximal distance one can reach forward beyond arm's length, while maintaining a fixed base of support in the standing position.[50] While both groups improved in the dynamic balance tests, Kinect exercise, in comparison, was more effective in enhancing the participants’ dynamic balance, aligning with findings from previous studies.[36,50,58] One possible reason may lie in the various changes in posture and weight shifts required by Kinect exergames. The advantages of Xbox Kinect are its accurate motion capture and visual feedback.[32–34] Combined with specific motion tasks, it enabled the participants to match the trainer's actions on screen, such as bend forward, prompt change of motion, and weight shifts. Therefore, in addition to achieving balance control during exercises, the Xbox Kinect enabled the participants to attain more efficient and correct movement or posture through visual feedback. Moreover, the participants took turns to serve as the leader during the group exercise, which further motivated them to improve their performance through mutual encouragement.
Except for the FRT test, no significant differences were observed in other tests between the 2 groups. This result may have been caused by the similar training concept despite the different training activity contents and methods designed for the 2 groups; that is, to improve the participants’ ability of weight shift, lower-body strength and endurance, posture control, and balance performance. In fact, relevant studies on exergames have also yielded similar results in which no significant differences were observed in the effects between exergames and conventional balance training on certain areas.[60–63]
4.3. Feasibility and safety discussion
The conventional and Kinect exercise groups had overall participation rates of 96% and 100%. This may be related to the group exercise approach adopted in this study, under which the participants could interact and enhance their friendships when they exercised together. This in turn resulted in greater group cohesion. In this study, the participants encouraged and reminded each other of the time of the activity, thus increasing the overall participation rate.
In the conventional exercise group, side effects occurred 12 times (overall incidence rate = 12.5%): knee joint soreness (2 times), thigh soreness (9 times), and calf soreness (1 time). By contrast, in the Kinect exercise group, side effects occurred 6 times (overall incidence rate = 6%): knee joint soreness (2 times) and thigh soreness (4 times). Neither groups exhibited any signs of dizziness, nausea, headache, injury, or falls. Brasington[64] and Bonis[65] noted that few studies have observed videogame-related tendinitis (known as “Nintendinitis” and “Wiitis”); that is, muscle damage and pain caused by Wii video games because of their use of sensors. However, users are not required to wear sensors when playing Kinect exergames, and thus, they do not exhibit any upper-arm tendinitis. Additionally, Holden[66] mentioned that users immersed in VR may experience symptoms such as dizziness, nausea, headache, and sweating, which are known as cybersickness. However, the use of a projection screen with Kinect exergames did not result in any dizziness, nausea, headache, injury, or falls in the present study.
The side effects observed in the Kinect exercise group were (in the order of their occurrence) thigh and knee joint soreness, whereas those observed in the conventional exercise group were thigh, knee joint, and calf soreness. All participants experienced lower-limb soreness, which improved after a break and did not extend into the next activity. The conventional exercise involved highly repetitive stepping movements and exercises that focused on lower-limb strengthening, which resulted in more thigh soreness. Additionally, the soreness in both groups occurred during the first few weeks of exercise, which might be caused by the change in the participants’ living habits and increased exercise time. Accordingly, the symptoms subsided after they adapted to the training exercise. Severe side effects such as injury and fall did not occur during exercise in either group.
In this study, both exercise designs were effective in improving the older adults’ balance ability, Kinect exergames were more comprehensive than conventional exercise in balance ability development, and the use of Kinect exergames contributed to particular functional reach enhancement. Such results reflect the benefits of virtual interactive contexts created by the Kinect exergames, such as group cohesion and liberation from wearing sensors, which respectively promoted long-term exercise and avoided discomfort and inconvenience.
4.4. Research limitations and prospects
-
1.
The limitations of this study were as follows:
-
(1)
The small number of participants meant that this study's interpretation and analysis cannot be extended to the general older adult population. The sample size was limited to 20 older adults, including 2 males and 18 females. Persuasive results might not be generated from a small sample size and unbalanced gender ratio, thus making it challenging to extrapolate the current results to other populations.
-
(2)
Some arguments in this study lacked the support of concrete evidence and can only be regarded as preliminary results. Thus, more in-depth research is required for further exploration and clarification.
-
(3)
This experiment focused on community older adults; thus, the results cannot be extended to older adults in other types of institution.
-
(1)
-
2.
Prospects
-
(1)
Future studies should increase the number of participants to enhance generalizability. Moreover, accurate and objective assessment instruments (e.g., strain gauge devices, ambulant accelerometer devices, and computerized dynamic posturography) should be incorporated and applied to community groups with different lifestyles to validate the effects of different exercise interventions.
-
(2)
This study attained preliminary results on the use of Kinect exergames for training community older adults. Future studies are suggested to explore whether Kinect exergames can be used by older adults at home; that is, they should investigate the feasibility and convenience of older adults’ self-training at home as well as their compliance with exergames.
-
(1)
5. Conclusion
The findings of this study indicated that after 5 weeks of intervention, the community older adults in both groups exhibited significant improvement in balance performance. While both interventions were effective, the Kinect exercise group demonstrated enhancement in more tests assessing balance ability, when compared with the conventional exercise group. A further probe into how Kinect exergames differed from conventional physical exercise revealed the significant effects of Kinect exergames on functional reach. Additional benefits observed in this study also suggested the use of Kinect exercise as a feasible, safe, and effective training method for improving community older adults’ balance, promoting group cohesion, and increasing motivation to exercise.
Author contributions
Conceptualization: Chi-Min Yang, Hao-Chiang Koong Lin.
Data curation: Shu-Yu Yang.
Formal analysis: Yi-Chen Chen.
Resources: Jun (Scott) Chen Hsieh, Hao-Chiang Koong Lin.
Validation: Hao-Chiang Koong Lin.
Writing – original draft: Chi-Min Yang.
Writing – review & editing: Chi-Min Yang, Jun (Scott) Chen Hsieh.
Footnotes
Abbreviations: 30-sec CST = 30-second Chair Stand Test, FRT = Functional Reach Test, MMSE = Mini-Mental State Examination, OLST = One-Leg Stance Test, PAR-Q = Physical Activity Readiness Questionnaire, TUG = timed up and go, VR = virtual reality.
How to cite this article: Yang CM, Chen Hsieh JS, Chen YC, Yang SY, Lin HC. Effects of Kinect exergames on balance training among community older adults: A randomized controlled trial. Medicine. 2020;99:28(e21228).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Department of Manpower Planning, Council for Economic Planning and Development. Taiwan population projections from 2010 to 2060. Taipei, Taiwan, ROC: Council for Economic Planning and Development, Executive Yuan; 2010. [Google Scholar]
- [2].Lang PO, Michel JP, Zekry D. Frailty syndrome: a transitional state in a dynamic process. Gerontology 2009;55:539–49. [DOI] [PubMed] [Google Scholar]
- [3].Muravchick S. Physiological changes of aging. ASA refresher courses in anesthesiology 2003;31:139–50. [Google Scholar]
- [4].Gehlsen GM, Whaley MH. Falls in the elderly: part II, balance, strength, and the flexibility. Arch Phys Med Rehabil 1990;71:735–41. [PubMed] [Google Scholar]
- [5].Drootin M. Panel on prevention of falls in older persons, American Geriatrics Society and British Geriatrics Society: summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148–57. [DOI] [PubMed] [Google Scholar]
- [6].Health Promotion Administration, Ministry of Health and Welfare. Long-Term Follow-Up (7th) Survey of Physical, Psychological, And Social Life Status of Middle-Aged and Elderly People in Taiwan. Taipei City: Health Promotion Administration, Ministry of Health and Welfare; 2011. [Google Scholar]
- [7].Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].American College of Sports Medicine. Physical activity programs and behavior counseling in older adult populations. Med Sci Sports Exerc. 2004;36:1997-2003. [DOI] [PubMed] [Google Scholar]
- [9].Rydwik E, Frändin K, Akner G. Effects of physical training on physical performance in institutionalised elderly patients (70+) with multiple diagnoses. Age Ageing 2004;33:13–23. [DOI] [PubMed] [Google Scholar]
- [10].Steadman J, Donaldson N, Kalra L. A randomized controlled trial of an enhanced balance training program to improve mobility and reduce falls in elderly patients. J Am Geriatr Soc 2003;51:847–52. [DOI] [PubMed] [Google Scholar]
- [11].Kobayashi R, Nakadaira H, Ishigami K, et al. Effects of physical exercise on fall risk factors in elderly at home in intervention trial. Environ Health Prev Med 2006;11:250–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Schlicht J, Camaione DN, Owen SV. Effect of intense strength training on standing balance, walking speed, and sit-to-stand performance in older adults. J Gerontol A Biol Sci Med Sci 2001;56:M281–6. [DOI] [PubMed] [Google Scholar]
- [13].Shigematsu R, Chang M, Yabushita N, et al. Dance-based aerobic exercise may improve indices of falling risk in older women. Age Ageing 2002;31:261–6. [DOI] [PubMed] [Google Scholar]
- [14].Liu H, Frank A. Tai chi as a balance improvement exercise for older adults: a systematic review. J Geriatr Phys Ther 2010;33:103–9. [PubMed] [Google Scholar]
- [15].Shimada H, Uchiyama Y, Kakurai S. Specific effects of balance and gait exercises on physical function among the frail elderly. Clin Rehabil 2003;17:472–9. [DOI] [PubMed] [Google Scholar]
- [16].Day L, Hill KD, Stathakis VZ, et al. Impact of Tai-Chi on falls among preclinically disabled older people. A randomized controlled trial. J Am Med Dir Assoc 2015;16:420–6. [DOI] [PubMed] [Google Scholar]
- [17].Lee HC, Chang KC, Tsauo JY, et al. Effects of a multifactorial fall prevention program on fall incidence and physical function in community-dwelling older adults with risk of falls. Arch Phys Med Rehabil 2013;94:606–15. [DOI] [PubMed] [Google Scholar]
- [18].Sohng KY, Moon JS, Song HH, et al. Fall prevention exercise program for fall risk factor reduction of the community-dwelling elderly in Korea. Yonsei Med J 2003;44:883–91. [DOI] [PubMed] [Google Scholar]
- [19].Tiedemann A, O’Rourke S, Sherington C. How is a yoga-based fall prevention program perceived by older people? J Sci Med Sport 2014;18:e94. [Google Scholar]
- [20].Bieryla KA, Dold NM. Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clin Interv Aging 2013;8:775–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Griffin M, Shawis T, Impson R, et al. Using the Nintendo Wii as an intervention in a falls prevention group. J Am Geriatr Soc 2012;60:385–7. [DOI] [PubMed] [Google Scholar]
- [22].Fu AS, Gao KL, Tung AK, et al. Effectiveness of exergaming training in reducing risk and incidence of falls in frail older adults with a history of falls. Arch Phys Med Rehabil 2015;96:2096–102. [DOI] [PubMed] [Google Scholar]
- [23].Schultheis MT, Rizzo AA. The application of virtual reality technology in rehabilitation. Rehabil Psychol 2001;46:296–311. [Google Scholar]
- [24].Merians AS, Jack D, Boian R, et al. Virtual reality-augmented rehabilitation for patients following stroke. Phys Ther 2002;82:898–915. [PubMed] [Google Scholar]
- [25].Hung JW, Chou CX, Hsieh YW, et al. Randomized comparison trial of balance training by using exergaming and conventional weight-shift therapy in patients with chronic stroke. Arch Phys Med Rehabil 2014;95:1629–37. [DOI] [PubMed] [Google Scholar]
- [26].Skjæret N, Nawaz A, Morat T, et al. Exercise and rehabilitation delivered through exergames in older adults: an integrative review of technologies, safety and efficacy. Int J Med Inform 2016;85:1–6. [DOI] [PubMed] [Google Scholar]
- [27].Van Diest M, Lamoth CJ, Stegenga J, et al. Exergaming for balance training of elderly: state of the art and future developments. J Neuroeng Rehabil 2013;10:101–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Proffitt R, Lange B, Chen C, et al. A comparison of older adults’ subjective experiences with virtual and real environments during dynamic balance activities. J Aging Phys Act 2015;23:24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Brox E, Luque LF, Evertsen GJ, et al. Exergames for elderly: social exergames to persuade seniors to increase physical activity. Paper presented at: The 5th International ICST Conference on Pervasive Computing Technologies for Healthcare; May 23-26, 2011; Dublin, Ireland. [Google Scholar]
- [30].Keogh JW, Power N, Wooller L, et al. Physical and psychosocial function in residential aged-care elders: effect of Nintendo Wii sports games. J Aging Phys Act 2014;22:235–44. [DOI] [PubMed] [Google Scholar]
- [31].Lund HH, Jessen JD. Effects of short-term training of community-dwelling elderly with modular interactive tiles. Games Health J 2014;3:277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Clark RA, Pua YH, Fortin K, et al. Validity of the Microsoft Kinect for assessment of postural control. Gait Posture 2012;36:372–7. [DOI] [PubMed] [Google Scholar]
- [33].Fraile SH, Browne J, Brox E, et al. Suitability analysis of commercial open-source driven motion sensor devices applied to exergames for the elderly. Paper presented at: Ambient Assisted Living Forum 2012; September 24-27, 2012; Eindhoven, holland. [Google Scholar]
- [34].Van Diest M, Stegenga J, Wörtche HJ, et al. Suitability of Kinect for measuring whole body movement patterns during exergaming. J Biomech 2014;47:2925–32. [DOI] [PubMed] [Google Scholar]
- [35].Grigorova-Petrova K, Dimitrova A, Lubenova D, et al. Feasibility of interactive video games for influence on balance in institutionalized elderly people. J Phys Educ Sport 2015;15:429–32. [Google Scholar]
- [36].Sato K, Kuroki K, Saiki S, et al. Improving walking, muscle strength, and balance in the elderly with an exergame using Kinect: a randomized controlled trial. Games Health J 2015;4:161–7. [DOI] [PubMed] [Google Scholar]
- [37].Kim J, Son J, Ko N, et al. Unsupervised virtual reality-based exercise program improves hip muscle strength and balance control in older adults: a pilot study. Arch Phys Med Rehabil 2013;94:937–43. [DOI] [PubMed] [Google Scholar]
- [38].Hsieh WM, Chen CC, Wang SC, et al. Virtual reality system based on Kinect for the elderly in fall prevention. Technol Health Care 2014;22:27–36. [DOI] [PubMed] [Google Scholar]
- [39].Whyatt C, Merriman NA, Young WR, et al. A Wii bit of fun: a novel platform to deliver effective balance training to older adults. Games Health J 2015;4:423–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Park EC, Kim SG, Lee CW. The effects of virtual reality game exercise on balance and gait of the elderly. J Phys Ther Sci 2015;27:1157–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Valenzuela T, Okubo Y, Woodbury A, et al. Adherence to technology-based exercise programs in older adults: a systematic review. J Geriatr Phys Ther 2018;41:49–61. [DOI] [PubMed] [Google Scholar]
- [42].Brumels KA, Blasius T, Cortright T, et al. Comparison of efficacy between traditional and video game based balance programs. Clin Kines (Online) 2008;62:26–31. [Google Scholar]
- [43].Vernadakis N, Gioftsidou A, Antoniou P, et al. The impact of Nintendo Wii to physical education students’ balance compared to the traditional approaches. Comput Educ 2012;59:196–205. [Google Scholar]
- [44].Folstein MF, Folstein SE, McHung PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- [45].Thomas S, Reading J, Shephard RJ. Revision of the physical activity readiness questionnaire (PAR-Q). Can J Sport Sci 1992;17:338–45. [PubMed] [Google Scholar]
- [46].Hagedorn R. Tools for Practice in Occupational Therapy: A Structured Approach to Core Skills and Processes. London, England: Churchill Livingstone; 2000. [Google Scholar]
- [47].Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315:1065–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 1999;70:113–9. [DOI] [PubMed] [Google Scholar]
- [49].Langley FA, Mackintosh SF. Functional balance assessment of older community dwelling adults: a systematic review of the literature. Internet J Allied Health Sci Pract 2007;5:1–1. [Google Scholar]
- [50].Duncan PW, Weiner DK, Chandler J, et al. Functional reach: a new clinical measure of balance. J Gerontol 1990;45:M192–7. [DOI] [PubMed] [Google Scholar]
- [51].Hanke TA, Rogers MW. Reliability of ground reaction force measurements during dynamic transitions from bipedal to single-limb stance in healthy adults. Phys Ther 1992;72:810–6. [DOI] [PubMed] [Google Scholar]
- [52].Li L, Liu X, Herr K. Postoperative pain intensity assessment: a comparison of four scales in Chinese adults. Pain Med 2007;8:223–34. [DOI] [PubMed] [Google Scholar]
- [53].Hornbrook MC, Stevens VJ, Wingfield DJ, et al. Preventing falls among community-dwelling older persons: results from a randomized trial. Gerontologist 1994;34:16–23. [DOI] [PubMed] [Google Scholar]
- [54].Quail GC. An approach to the assessment of falls in the elderly. Aust Fam Physician 1994;23:873–6. [PubMed] [Google Scholar]
- [55].Milanović Z, Pantelić S, Trajković N, et al. Age related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging 2013;8:549–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Chu LW, Chi I, Chiu AY. Incidence and predictors of falls in the Chinese elderly. Ann Acad Med Singapore 2005;34:60–72. [PubMed] [Google Scholar]
- [57].Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000;80:896–903. [PubMed] [Google Scholar]
- [58].Chow DH, Mann SK. Effect of cyber-golfing on balance amongst the elderly in Hong Kong: a pilot randomised trial. Hong Kong J Occup Th 2015;26:9–13. [Google Scholar]
- [59].Tsang WW, Hui-Chan CW. Effects of exercise on joint sense and balance in elderly men: Tai Chi versus golf. Med Sci Sports Exerc 2004;36:658–67. [DOI] [PubMed] [Google Scholar]
- [60].Franco JR, Jacobs K, Inzerillo C, et al. The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol Health Care 2012;20:95–115. [DOI] [PubMed] [Google Scholar]
- [61].Singh DK, Rajaratnam BS, Palaniswamy V, et al. Participating in a virtual reality balance exercise program can reduce risk and fear of falls. Maturitas 2012;73:239–43. [DOI] [PubMed] [Google Scholar]
- [62].Singh DKA, Rajaratnam BS, Palaniswamy V, et al. Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric 2012;16:141–6. [DOI] [PubMed] [Google Scholar]
- [63].Choi SD, Guo L, Kang D, et al. Exergame technology and interactive interventions for elderly fall prevention: a systematic literature review. Appl Ergon 2017;65:570–81. [DOI] [PubMed] [Google Scholar]
- [64].Brasington R. Nintendinitis. N Engl J Med 1990;322:1473–4. [PubMed] [Google Scholar]
- [65].Bonis J. Acute wiiitis. N Engl J Med 2007;356:2431–2. [DOI] [PubMed] [Google Scholar]
- [66].Holden MK. Virtual environments for motor rehabilitation. Cyberpsychol Behav 2005;8:187–211. [DOI] [PubMed] [Google Scholar]


