Abstract
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has emerged as a new threat to healthcare systems. In this setting, heart failure units have faced an enormous challenge: taking care of their patients while at the same time avoiding patients' visits to the hospital.
Objective
The aim of this study was to evaluate the results of a follow-up protocol established in an advanced heart failure unit at a single center in Spain during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
During March and April 2020, a protocolized approach was implemented in our unit to reduce the number of outpatient visits and hospital admissions throughout the maximum COVID-19 spread period. We compared emergency room (ER) visits, hospital admissions, and mortality with those of January and February 2020.
Results
When compared to the preceding months, during the COVID pandemic there was a 56.5% reduction in the ER visits and a 46.9% reduction in hospital admissions, without an increase in mortality (9 patients died in both time periods). A total of 18 patients required a visit to the outpatient clinic for decompensation of heart failure or others.
Conclusion
Our study suggests that implementing an active-surveillance protocol in acutely decompensated heart failure units during the SARS-CoV-2 pandemic can reduce hospital admissions, ER visits and, potentially, viral transmission, in a cohort of especially vulnerable patients.
Keywords: Heart failure, Heart failure unit, COVID-19, SARS-CoV-2, Coronavirus
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has emerged as a new threat to healthcare systems and to the world's population, particularly to the elderly and those with chronic comorbidities [1]. In this setting, heart failure units (HFU) have faced an enormous challenge: taking care of their patients while at the same time avoiding patients' visits to the hospital. Many of these units have had to reinvent themselves, prioritizing telephone calls and telemonitoring.
The aim of this study was to evaluate the results of a follow-up protocol established in a HFU at a single center in Spain during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
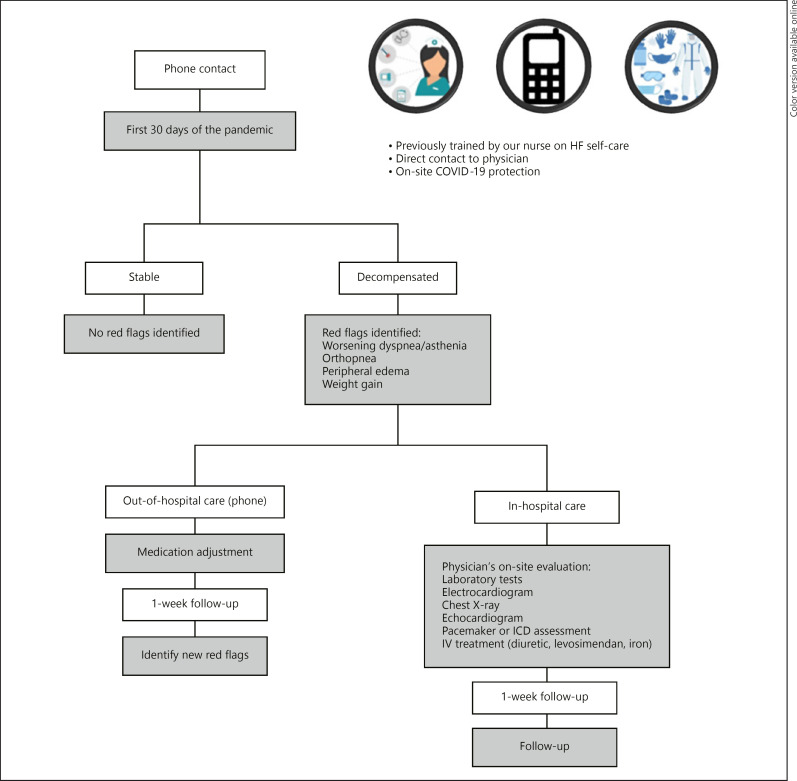
During March and April 2020, a protocolized approach was implemented in our unit to reduce the number of outpatient visits and hospital admissions throughout the maximum COVID-19 spread period. All patients were contacted by phone call during the first month of the pandemic by one of the four physicians in our unit. All patients had been previously trained by our nurse to take daily blood pressure, heart rate and weight, as well as to identify heart failure red flags (worsening dyspnea or orthopnea, peripheral edema, or weight gain, amongst others) [2]. Patients who reported signs or symptoms of acutely decompensated heart failure were classified into two groups: those who could be managed remotely and those who required physician's on-site evaluation and/or further testing, including laboratory tests, electrocardiogram, chest X-ray, echocardiogram, pacemaker, or implantable cardioverter defibrillator (ICD) assessment. Patients who fell in the first group had their medication adjusted, and a follow-up call was scheduled within a week, whereas those in the second group were evaluated in our outpatient clinic, where intravenous therapies (furosemide, levosimendan, or iron) could be administered and the necessary tests performed, all on the same day. Universal protection measures were adopted to avoid potential SARS-CoV-2 transmission during these visits. Moreover, a phone line was available for the patients to directly contact a physician from our unit during working hours from Monday to Friday (Fig. 1).
Fig. 1.
Implemented protocol to reduce the number of outpatient visits and hospital admissions throughout the COVID-19 pandemic.
In order to perform the study, we retrospectively reviewed all 368 patients who were being followed in our HFU between January 1 and April 30, 2020. Demographic, clinical, and analytical data were collected and subsequently analyzed. For the analysis, we compared the months of January and February 2020, when regular hospital activity took place, with March and April 2020, the peak of the COVID-19 pandemic in our country. We sought to compare all-cause mortality, emergency department visits, and hospital admissions between those time periods.
Results
Regarding patients' basal characteristics, median age was 75.9 years (interquartile range [IQR] 65.7–84.3), and 66.7% were male. The most common cause of heart failure was ischemic cardiomyopathy (42%), followed by idiopathic cardiomyopathy (19.8%). Median left ventricular ejection fraction was 40% (IQR 32–55), 45.9% had left ventricular ejection fraction <40%, and median B-type natriuretic peptide (last B-type natriuretic peptide determined in our outpatient clinic before the pandemic) was 160 pg/mL (IQR 80–504). The majority of our patients were symptomatic, in NYHA class II, III or IV (65.8%), and all of them (100%) had been admitted at least once to the hospital for acutely decompensated heart failure in the past year (Table 1).
Table 1.
Basal characteristics and treatment of HFU patients
| All patients (n = 368) | COVID-19 period (March and April, 2020) |
||||
|---|---|---|---|---|---|
| ER (n = 30) | hospitalization (n = 26) | death (n = 9) | |||
| Age, years | 73.8; 13.7 | 77.0; 9.1 | 76.5; 9.0 | 82.2; 6.7 | |
| Female sex | 159 (33.3) | 11 (36.7) | 8 (30.8) | 3 (33.3) | |
| Risk factors | |||||
| Hypertension | 354 (81.6) | 23 (82.1) | 21 (87.5) | 6 (75) | |
| Diabetes | 175 (35.8) | 15 (50) | 13 (50) | 4 (44.4) | |
| Dyslipidemia | 279 (66.3) | 18 (66.7) | 18 (72) | 6 (75) | |
| HF data | |||||
| LVEF, % | 43.3; 13.7 | 46.2; 14.1 | 45.3; 14.1 | 50.8; 10.2 | |
| Patients with HFrEF | 224 (45.8) | 9 (30) | 9 (34.6) | 2 (22.2) | |
| Ischemic etiology of HF | 125 (25.6) | 3 (10) | 2 (7.7) | 2 (22.2) | |
| NYHA class | |||||
| I | 145 (34.2) | 6 (20) | 2 (8.7) | 0 (0) | |
| II | 180 (42.5) | 16 (53.3) | 12 (52.2) | 5 (55.5) | |
| III | 88 (20.8) | 7 (23.3) | 7 (30.4) | 4 (45.5) | |
| IV | 11 (2.6) | 1 (3.3) | 2 (8.7) | 0 (0) | |
| Previous BNP, pg/mL | 496; 1399 | 285; 527 | 449; 569 | 217; 197 | |
| Episode peak BNP, pg/mL | − | 1,657; 1240 | 1,623; 1417 | 1,881; 1839 | |
| Previous creatinine, g/dL | 1.27; 0.64 | 1.24; 0.44 | 1.51; 0.91 | 1.22; 0.50 | |
| Episode peak creatinine, g/dL | − | 1.70; 0.79 | 2.65; 2.29 | 2.04; 1.1 | |
| Previous hemoglobin, g/dL | 13.6; 2.0 | 12.9; 2.1 | 12.8; 2.1 | 12.6; 3.2 | |
| Episode minimum hemoglobin, g/dL | − | 11.7; 2.4 | 10.9; 2.6 | 11.7; 3.3 | |
| Previous treatment | |||||
| ACEIs/ARBs | 201 (41.1) | 9 (30) | 10 (38.5) | 1 (11.1) | |
| Sacubitril/valsartan | 207 (42.3) | 12 (40) | 11 (42.3) | 4 (44.4) | |
| Beta-blockers | 402 (82.2) | 26 (86.7) | 23 (88.5) | 7 (77.8) | |
| MRA | 284 (58.1) | 17 (56.7) | 12 (46.2) | 3 (33.3) | |
| ICD | 78 (16.3) | 4 (13.3) | 8 (30.8) | 1 (11.1) | |
| CRT | Furosemide dose | 78 (16.3) | 3 (10) | 7 (26.9) | 2 (22.2) |
| ≤40 mg/day | 144 (50.9) | 7 (36.8) | 7 (36.8) | 3 (42.9) | |
| 40–120 mg/day | 112 (39.6) | 9 (47.4) | 9 (47.4) | 4 (57.1) | |
| >120 mg/day | 27 (9.5) | 3 (15.8) | 3 (15.8) | 0 (0) | |
| Ambulatory inotropes (levosimendan) | 10 (2.1) | 2 (6.7) | 3 (11.5) | 1 (11.1) | |
Quantitative values are expressed as mean; SD, and qualitative values as number (percentages). LVEF, left-ventricular ejection fraction. HFrEF, heart failure with reduced ejection fraction. HF, heart failure. NYHA, New York Heart Failure Association. BNP, B-type natriuretic peptide. ACEIs, angiotensin-converting enzyme inhibitors. ARBs, aldosterone receptor blockers. MRA, mineralocorticoid receptor antagonists. ICD, implantable cardioverter defibrillator. CRT, cardiac resynchronization therapy.
During the 2 months immediately preceding the pandemic (January and February 2020), there were a total of 69 emergency room (ER) visits, 49 hospital admissions, and 9 deaths in our HFU cohort, whereas in the second period analyzed, there were a total of 30 ER visits, 26 hospital admissions, and 9 deaths. Of the 9 deaths during the COVID pandemic, 2 were due to SARS-CoV-2 infection, 2 were of cardiac origin, and 5 of non-cardiac origin. A total of 13 patients presented symptoms suggestive of COVID infection (fever, cough, sore throat, headache, anosmia, and ageusia), 6 underwent reverse transcriptase-polymerase chain reaction test in a throat swab, but only 4 were positive.
As to the activity in our unit, on top of the proactive telephone approach from the unit described earlier, 18 patients required a visit to the outpatient clinic (4 ICD or TRC checks, 4 administrations of intravenous diuretics, 5 for levosimendan, and 1 for IV iron, 1 blood transfusion, 14 blood tests, 1 electrical cardioversion, and 1 chest X-ray). A total of 50 patients contacted us via the direct phone line we provided them.
When compared to the preceding months, during COVID pandemic there was a 56.5% reduction in the ER visits and a 46.9% reduction in hospital admissions in our cohort of patients, which is clearly an outstanding achievement, taking into account that hospitals are considered to be hot spots for viral transmission. However, mortality remained the same. We did not expect to see a reduction in mortality, due to the fact that it is a HFU cohort with an intrinsically high mortality rate. Only 4 out of 368 patients (0.01%) tested positive for COVID-19 infection, which is a very low rate taking into account the high-risk population we are referring to. This probably reflects our efforts in keeping patients at home as much as possible, limiting visits to the hospital to those cases strictly necessary.
Conclusion
Our study suggests that implementing an active-surveillance protocol in HFUs during the SARS-CoV-2 pandemic can reduce hospital admissions, ER visits and, potentially, viral transmission, in a cohort of especially vulnerable patients.
Statement of Ethics
The study was approved by the Ethics Committee of University Hospital Ramon y Cajal (Madrid, Spain), and informed consent was waived.
Disclosure Statement
The authors report no relationships that could be construed as a conflict of interest.
Funding Sources
The authors received no specific funding for this work.
Author Contributions
All authors conceived the study and analyzed the data. M.J.-B.B. and D.C.P. wrote the first draft of the manuscript, and all authors critically appraised and revised the manuscript. G.L.A.S. is the guarantor for the study.
References
- 1.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 Feb;323((11)):1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strömberg A, Mårtensson J, Fridlund B, Levin LA, Karlsson JE, Dahlström U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective, randomised trial. Eur Heart J. 2003 Jun;24((11)):1014–23. doi: 10.1016/s0195-668x(03)00112-x. [DOI] [PubMed] [Google Scholar]