Abstract
Epidemiological data support the view that both obesity and cardiovascular diseases (CVD) account for a high proportion of total morbidity and mortality in adults throughout the world. Obesity and CVD have complex interplay mechanisms of genetic and environmental factors, including diet. Nutrition is an environmental factor and it has a predominant and recognizable role in health management and in the prevention of obesity and obesity-related diseases, including CVD. However, there is a marked variation in CVD in patients with obesity and the same dietary pattern. The different genetic polymorphisms could explain this variation, which leads to the emergence of the concept of nutrigenetics. Nutritional genomics or nutrigenetics is the science that studies and characterizes gene variants associated with differential response to specific nutrients and relating this variation to various diseases, such as CVD related to obesity. Thus, the personalized nutrition recommendations, based on the knowledge of an individual’s genetic background, might improve the outcomes of a specific dietary intervention and represent a new dietary approach to improve health, reducing obesity and CVD. Given these premises, it is intuitive to suppose that the elucidation of diet and gene interactions could support more specific and effective dietary interventions in both obesity and CVD prevention through personalized nutrition based on nutrigenetics. This review aims to briefly summarize the role of the most important genes associated with obesity and CVD and to clarify the knowledge about the relation between nutrition and gene expression and the role of the main nutrition-related genes in obesity and CVD.
Introduction
Obesity is an emerging noncommunicable disease associated with chronic low-grade inflammation, and the development of many obesity-related diseases, such as cardiovascular disease (CVD), type 2 diabetes mellitus, and a number of cancers [1]. Obesity has a multifactorial etiology, where lifestyle factors, including unhealthy dietary patterns, physical inactivity, and poor sleeping habits, are recognized to play a crucial role in both the development and progression of obesity and its comorbidities [1]. Nevertheless, in the so called obesogenic environments, up to 70% of the population variation in obesity may be attributed to genetic factors [2]. In this very complex scenario, there is growing evidence that the evaluation of gene–diet interactions in relation to obesity and CVD could currently represent an interesting field of application for innovative nutritional interventions for changing health behaviors.
The nutrigenetics is the science that explores the specific interactions between genes and nutrients and relating this variation to human health and to variable disease states, including obesity and CVD [3]. To date, through Genome-wide association studies (GWAS), the Human Genome Project has led to sequencing the entire human genome in order to identify genes and/or loci associated with a specific phenotype [4, 5]. The Human Genome Project led to the understanding of multiple mutual relations among genes, nutrition, and diseases [6]. In fact, the sequencing of the human genome has reported a significant genetic heterogeneity within the same human population groups. A number of single-nucleotide polymorphisms (SNPs) can have a relation to nutrition [7]. There is a bidirection relationship between genome and nutrition that may affect the individual’s diseases susceptibility [8]. In particular, on the one side, the genetic background of one person can define the metabolic response, nutritional state, and the susceptibility to nutrient-dependent or related diseases [9]. On the other side, the nutrients up- or downregulate the gene expression, and consequently, at the molecular level, the metabolic responses. These interactions between nutrition and genome have led to two new science branches, nutrigenetics and nutrigenomics [10]. However, it has to be underlined that the genetics can explain only a small part of the total variance of factors associated with CVD [5, 11].
In this context, specific nutrients, through the interaction with individual genetic characteristics, may lead to the up- or downregulation of specific metabolic pathways, which may contribute to the development of obesity and CVD [5]. The nutrigenetics studies provide the evidence of the association between SNPs and single nutrients. As an example, it has been previously reported higher high-density lipoprotein (HDL) cholesterol levels in carriers of the A allele for an SNP located in the promoter region of Apolipoprotein (APO) A1 after a diet rich in polyunsaturated fatty acids (PUFA) [12]. Similarly, the APO E polymorphisms, in particular the carriers of APO E4 isoform, have been associated with a higher risk of CVD and the carriers of these polymorphisms have a 46% increase in CVD risk compared with the carriers of the APO E3 isoform [13].
Beyond single nutrients, it is worthwhile to consider that the diet is a complex combination of several nutrients and foods with similar properties, thus it is very challenging, to separate the effect of a single nutrient from others, in free-living populations [14]. Very recently, the Food4Me project, a large randomized trial of 5562 European participants, investigated the hypothesis of personalized nutrition based on an individual’s genetic background [15]. The objective of this study was to investigate the effectiveness of three different types of dietary interventions. For this purpose, participants were randomly assigned to one of the following intervention groups for a 6-month period: diet based on the healthy eating guidelines, diet based on both the individual’s dietary intake and anthropometric measurements, including body mass index and waist circumference, and diet based on both anthropometric measurements and the individual’s dietary intake, and in addition on genotypic data, in particular related to five genetic variants in obesity-associated gene (FTO), fatty acid desaturase (FADS)-1, transcription factor 7-like 2, APO E, and methylenetetrahydrofolate reductase (MTHFR) [15]. In particular, the results of the Food4Me randomized controlled trial investigated the effect of the APO E genotype on response to the personalized dietary advice intervention. Data from this trial showed that the diet based on genotypic data resulted in a higher reduction of saturated fatty acids intake for the gene-based personalized nutrition targeted to APO E compared with standard dietary advice [16], and suggested this approach could improve the nutritional behavior, with favorable healthy consequences in the long term [16]. In particular, it is also remarkable to notice that the effect of adherence to a Mediterranean style diet on incidence of cardiovascular outcomes in type 2 diabetes [17–19] is also mediated by genetic influences.
Offering personalized diet advice based to the individual’s genetic susceptibility could be a promising strategy for preventing or treating obesity and obesity-related diseases, including CVD. Tailored dietary advice is the objective of precision nutrition, which is based on the study of nutrigenetics in order to identify the specific genetic factors able to explain the interindividual variability of the response to a specific dietary pattern [20]. To promote nutrigenetic studies, it is mandatory to increase the knowledge on this topic and to develop useful dietary and lifestyle recommendations to manage body weight and reduce CVD risk. Indeed, personalized nutrition recommendations based also on the individual’s genetic background might improve the outcomes of a specific dietary intervention and could represent a new dietary approach to prevent nutrition-related diseases and obesity complications. Given these premises, it is intuitive to understand that the elucidation of diet and gene interactions could support more specific and effective dietary interventions in both obesity and CVD prevention through personalized nutrition based on nutrigenetics. This review aims to briefly summarize the role of the most important genes associated with obesity and obesity-related CVDs.
Obesity and cardiovascular diseases (CVDs)
Obesity represents a major risk factor for CVD. One of the most important consequences of obesity is a widespread impairment of cardiovascular physiology as a result of structural and functional adaptations induced by obesity [21]. These adaptive mechanisms translate into profound hemodynamic alterations due to increases in blood volume, cardiac output, stroke volume, and heart rate, resulting in a progressive cardiac remodeling, in terms of left atrial enlargement, left ventricular (LV) dilation [22], and eccentric or concentric LV hypertrophy [23, 24].
It has been widely established that the excess of adipose tissue exerts a number of endocrine influences, including synthesis and release of hormones and cytokines [25]. Some of the latter, named adipokines, orchestrate several pathways related to the development of the well-known chronic low-grade inflammation which, in turn, is strongly related to the increased risk of CVD development [26] through its proatherogenic effect [27].
The excess of adipose tissue increases the epicardial adipose tissue (EAT) deposition that in turn has been recognized to play a pivotal role in the development of cardiovascular complications related to obesity [21]. Increased EAT is responsible for a local proatherogenic effect, resulting in increased risk of coronary heart disease and arrhythmias, including atrial fibrillation [28].
Interestingly, obesity-related alteration of the gut microbiota is responsible for triggering several inflammatory pathways, resulting in increased cardiometabolic risk [29], and production of metabolites related to cardiovascular risk. Emerging evidence, indeed, focused the attention on the trimethylamine N-oxide (TMAO), as a gut microbiota-derived metabolite recognized as a prognostic marker for obesity-related cardiovascular events beyond traditional risk factors [30]. In particular, scientific evidence demonstrated TMAO as a risk factor for atherosclerosis [31], stroke [32–35], and heart failure [36]. A recent study demonstrated a positive association between TMAO serum levels and both Visceral Adiposity Index and Fatty Liver Index as a gender-specific indicator of adipose dysfunction and predictor of nonalcoholic fatty liver disease, respectively [37].
Nutrigenetics for CVD prevention in patients with obesity
Over the past century, research established that lifestyle, including diet, strongly affects CVD risk [38–40]. For this reason, dietary recommendations have been the focus of public health campaigns aiming to reduce CVD risk [40–42]. Despite that effort, the expected reduction of mortality for CVD does not occur consistently, and this failure has been attributed, at least in part, to individual variability to dietary recommendation responsiveness and to different genetics, or possibly to the bidirectional interactions between both factors. The Human Genome Project [43] highlighted a plethora of genes and their end products, the proteins, which could be involved in these differential weight responses to diet. Nutrigenetics is the discipline that studies how genetic variability regulates individual differential responses to dietary regimens. It can be considered as a section of nutrigenomics, which, more widely, investigates interactions between nutrients and the genome [44], taking into account not only genetics, but also gene expression changes and epigenetics. Relevant improvements in the fields of nutrigenetics and nutrigenomics opened the possibility for personalized nutrition aimed to prevent major diseases, including CVD.
Epidemiologic studies demonstrated that a strong predisposition to CVD is due to individual genetics. Numerous familial and twin studies [45] supported this notion, together with large long-term cardiovascular cohort studies [46, 47]. GWAS identified dozens of genes/loci associated with atherosclerosis, many of which have been confirmed by independent investigations. Despite that, only about 30% of the estimated heritability variance could be explained by the identified susceptibility alleles [48]. To clarify the origin of this missing heritability, several limits of genetics studies have been hypothesized to be involved: lack of consideration of gene–gene interactions, limited study power to detect rare variants, and contribution of environmental factors, including nutritional habits among others.
Given these premises, it is intuitive to understand that the elucidation of gene–diet interactions could support more specific and effective interventions for CVD preventions through personalized nutrition. Nutrigenetics, indeed, focusing on genetic variants able to explain differential responses to nutrients and/or dietetic interventions, can play a role in the prevention of cardiovascular events.
As previously mentioned, several studies highlighted that a substantial heterogeneity in response to dietary intervention actually exists, according to the different dietary component included [49–53], and molecular genetics, as soon as it developed, was addressed as the tool able to explain that variability. On the other hand, dietary reference values, such as the recommended dietary allowances, are designed for the general population assuming a Gaussian distribution of the different metabolic outcomes ensuing nutrients intake. Due to their different genetics, these reference values are not optimized for population subgroups, which may substantially diverge in the activity of transport proteins for a certain nutrient or in the activity of enzymes necessary to metabolize that micronutrient or requiring it as a cofactor. Despite a single SNP may have a relatively small effect in comparison with other known risk factors (such as family history for CVDs), several minor genetic variances in association with various environmental exposures (i.e., inadequate diet) could result in relevant changes in gene expression. As a result of the interactions between all these variables, the final phenotype could be affected by negligible changes or, on the contrary, by an increased risk due to the co-existence of these unfavorable conditions. This setting could be particularly alarming when involving pathways potentially able to promote atherogenesis (i.e., inflammation and/or lipid metabolisms) in high-CVD risk subjects, such as patients with obesity.
While nutrigenetic studies were almost all observational in the first era of this discipline, the number of interventional investigations including genetic variability for dietary responsiveness significantly increased in the last decades [54]. This aspect is noteworthy considering that one of the most popular accusations that skeptical researchers/physicians addressed to nutrigenetics and nutrigenomics was that clinical advice based on molecular nutrition was deduced by observational studies rather than interventional [55]. In this context, recent evidence coming from interventional studies involving nutrigenetics has identified specific pathways as potentially involved in heterogeneous dietary responses and consequentially able to promote or prevent CVD in susceptible patients.
Genetic variants affecting responsiveness to nutritional intervention tailored to reduce CVD risk in patients with obesity
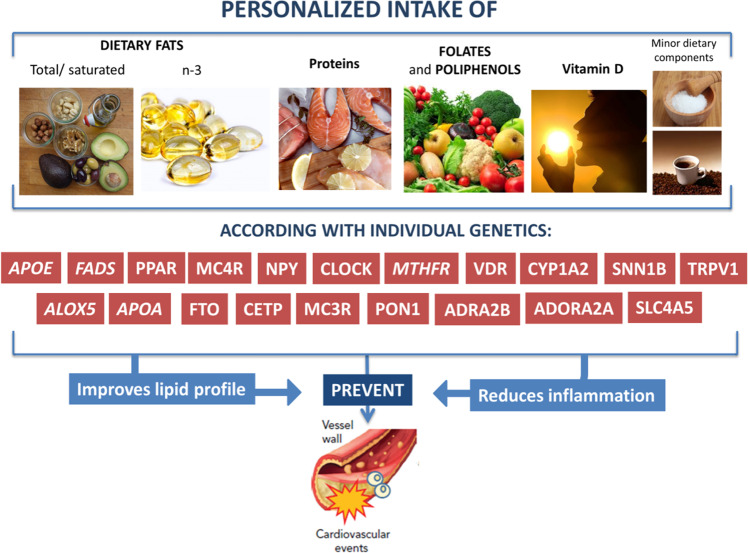
The following paragraph describes genetic contributions to pathways that should be considered to tailor personalized dietetic recommendations to prevent CVD in patients with obesity. Herein, we report recent evidence supporting the relationship between genetic variants and responsiveness to specific nutrients intake. In particular we focused on both observational studies and clinical trials (summarized in Table 1) investigating the effects of nutrients supplementation on cardiovascular outcomes, with the aim to identify applications of nutrigenetics in clinical practice. Graphical representation of personalized interventions tailored to reduce CVD risk in obese patients based on their individual responsiveness to specific nutrients or dietary plans are reported in Fig. 1.
Table 1.
Evidences from clinical trials.
| Reference | Study design | Population | Gene variants | Outcomes |
|---|---|---|---|---|
| Omega-3 supplementation | ||||
| [61] | DB, R, PC | Type 2 diabetics | CD36 (rs1527483), NOS3 (rs1799983), PPARG (rs1801282) | Diabetic CD36-G allele, PPARG-G allele, and NOS3-A allele carrier are better responders to omega-3 supplementation in improvement of lipid profile |
| [63] | DB, PC | Healthy subjects | ALOX5; genotypes: “dd,” “d5,” and “55” (“d” represents the deletion of 1 or 2 SP1 binding sites; “5” indicates the allele with 5 sites) | Increased levels of EPA, DHA, and omega-3 and reduced omega-6/omega-3 ratio and HDL particle concentrations in “d5” and “55” genotypes. Reduced TG in “d5” genotypes |
| [64] | DB, R, PC | Elderly | APO E4 | The expression of genes related to IFN is reduced only in carriers |
| [65] | DB | Healthy subjects | 12 tagging SNPs in FFAR4 | Omega-3 supplementation reduce HOMA-IR and fasting insulin in carriers of the major allele of several FFAR4 SNPs |
| [66] | DB | Healthy subjects | 31 SNPs in 6 genes associated with TG response to omega-3 supplementation | Variant carriers are nonresponder to omega-3 supplementation for control of TG serum levels |
| Folate supplementation | ||||
| [76] | DB | Subjects with hyperhomocysteinaemia | MTHFR and MTRR | SNPs rs1801133 and 1801131 in MTHFR and rs1801394 and rs162036 in MTRR are associated with the efficacy of folate supplementation for hyperhomocysteinaemia |
| Vitamin D supplementation | ||||
| [83] | DB | Type 2 diabetics | VDR polymorphism | Significantly improvements of metabolic profile in Taq-I GG genotype and Bsm-I TT genotype carriers |
| [84] | DB, R, PC | Postmenopausal women | SNP rs11185644 in RXRA | SNP in RXRA are associated with vitamin D3 dose-response |
| [85] | DB, R, C | Type 2 diabetics | Fok-I: alleles are defined as “F” (absence of the restriction site) or “f” (presence of the restriction site) | After supplementation, differences in 25(OH)D serum levels were significant between “ff” and “FF.” In “FF” carriers lower levels of inflammatory biomarkers were detected compared with “ff” and “Ff.” “ff” carriers are “low responders” to supplementation with 25(OH)D |
DB double-blind, R randomized PC placebo-controlled, C controlled, OL open label, EPA eicosapentaenoic acid, DHA docosahexaenoic acid, HDL high-density lipoprotein, TG triglycerides, HOMA-IR homeostasis model assessment of insulin resistance, IFN interferon, SNP single-nucleotide polymorphism.
Fig. 1. Nutrigenetics-personalized nutrition in obesity and cardiovascular diseases.
Graphical representation of personalized interventions tailored to reduce CVD risk in obese patients based on their individual responsiveness to specific nutrients or dietary plans. A personalized diet based on nutrigenomics lead to both improvement lipid profile and reduction of inflammation, and could act on cardiovascular prevention in patients with obesity.
Omega-3 fatty acids
Perturbed lipid metabolism and inflammation (which are both strongly associated with dietary patterns) [56, 57] are key players in atherosclerosis onset. Indeed, many of the identified genetic variants associated with CVD are mapped to genes directly or indirectly involved in the regulation of these two central pathways.
Numerous investigations about nutrigenetics and lipid metabolism regulation have been conducted [58]. Definitely the homeostasis of lipid profile depends on the interplay of intricate biochemical pathways involving several different enzymes, receptors, and other factors, through which the genetic variability could modulate the final lipid phenotype. These individual differences have not been considered in the guidelines to the general population, and this is reflected in the heterogeneous responses observed after nutritional interventions aimed to improve lipid profile.
Particularly relevant, both in terms of lipid profile regulation and inflammation reduction, is the intake of PUFA (i.e., omega-6 and omega-3 fatty acids), which has been linked to decrease in CVD risk. It has been extensively demonstrated that omega-3 fatty acids (eicosapentaenoic acid (EPA)/docosahexaenoic acid (DHA) above all) exert cardioprotective effects through reduction of triglyceride levels, by contrasting the pro-inflammatory eicosanoid storm, and decreasing platelet aggregation and blood pressure. However, intake of omega-3 fatty acids does not have the same effect in every subject. Indeed, genetic variations in the long-chain PUFA biosynthetic pathways affect levels of circulating and tissue PUFA together with other biomarkers and clinical endpoints of CVD. A comprehensive review of the diet–gene interactions and PUFA metabolism [59] describes as particularly relevant for CVD the genetic variations within the fatty acid desaturase FADS gene family (in particular FADS1 and FADS2, involved in the bioconversion of essential fatty acids to longer chained PUFA), fatty acid elongase (ELOVL2) (involved in DHA biosynthesis), phospholipase A (PLA2G4), and arachidonate 5-lipoxygenase (ALOX5) (that code for enzymes that mobilize and metabolize arachidonic acid). O’Neill and Minihane [60] summarized the existing evidence of FADS genotype influences on fatty acid status and cardiovascular health [60]. Current evidence demonstrates that carriers of FADS minor alleles have higher plasma and tissue levels of linoleic and α-linolenic acids, lower levels of arachidonic acid, EPA, and also lower level of DHA. This induces a reduced inflammatory status and CVD risk, and dietary total fat intake can modify this association. Despite the fact that effect size of this gene x nutrient interaction has not been measured, the authors suggested the usage of this genetic information to refine EPA and DHA recommendations (with higher intake recommended for FADS minor alleles carriers) [60].
Clinical trials investigating the different responsiveness to omega-3 supplementation focused on various gene variants, including cluster of differentiation (CD)36 [61], nitric oxide synthase (NOS)3 [62], peroxisome proliferator-activated receptor gamma (PPARG) [61], ALOX5 [63], APOE4 [64], free fatty acid receptor (FFAR)4 [65], and genes associated with triglycerides response to omega-3 supplementation [66]. More specifically, people with diabetes carrying the following alleles CD36-G, NOS3-A, and PPARG-G are better responders to omega-3 supplementation in the improvement of lipid profile [61]. In elderly people carrying the gene variant APOE4, supplementation with omega-3, significantly reduces the expression of genes related to interferon [64].
Further studies have been conducted on healthy individuals. Although these people are not at high-CVD risk, these studies are useful to elucidate the different role of omega-3 supplementation on the basis of genotype on cardiovascular outcomes. Armstrong et al. [63] studied three different genotypes indicated as “ALOX5-dd,” “ALOX5-d5,” and “ALOX5-55”, where “d” represents the deletion of one or two SP1 binding sites and “5” indicates the allele with five sites in 98 subjects. After 6-week treatment with 5 g fish oil daily, increased levels of EPA, DHA, and omega-3 and reduced omega-6/omega-3 ratio and HDL cholesterol particle concentrations were observed in “d5” and “55” genotypes; in addition, reduced serum levels of triglycerides were observed in “d5” genotypes [63]. More recently, in 208 subjects treated with 5 g fish oil for 6 weeks, Vallée Marcotte et al. identified 31 SNPs in six genes related to control of triglyceride levels in response to supplementation with omega-3 fatty acids that confer nonresponsiveness to treatment [66]. Interestingly, the same research group previously demonstrated that supplementation with 3 g omega-3 fatty acids daily for 6 weeks significantly reduced insulin resistance and fasting insulin in carriers of the major allele of several FFAR4 SNPs [65].
Folate
It is well known that both micronutrient deficiency and abundance can alter the genome stability, thus impacting nutrient–nutrient and gene–nutrient interactions (which is influenced by the genotype) [67]. SNPs can influence micronutrient status and chronic diseases related to their metabolism. Consequently, (micro)nutrients have the potential to increase or reduce the chances of disease onset through regulation of these interactions.
A pivotal example is the regulation of homocysteine levels by folate intake. Plasma homocysteine is an integrated marker of one carbon metabolism and is inversely correlated with folate, vitamin B6 and B12 intake, while it is positively associated with alcohol consumption [68]. The accumulation of homocysteine is a predictor of CVD risk [69, 70]. Several mechanisms have been postulated to promote CVD onset, and promotion of inflammation is one of them [71]. Plasma homocysteine has a heritability estimate of 8–57% [72, 73]. One of the most investigated variants associated with increased plasma homocysteine is the C677T polymorphism (rs1801133) in 5,10 MTHFR gene. Carriers of the T allele display reduced ability to convert methylenetetrahydrofolate to methyl-tetrahydrofolate, which is responsible for the impairment in the homeostasis of the one carbon cycle pathway [74]. A recent meta-analysis confirmed that not only TT genotype is associated with higher plasma homocysteine levels and lowered serum folate, but also to a reduced response to short-term folate supplementation [75]. These data support the necessity to identify MTHFR TT carriers in order to ensure them an adequate folate intake able to override genetic effects (that could lead them to increased risk to develop CVD) minimizing any adverse outcomes. Indeed, it has been demonstrated that efficacy of hyperhomocysteinaemia treatment with folate supplementation depends on MTHFR genotype [76].
A prospective cohort study was performed on subjects with hyperhomocysteinaemia in order to evaluate how polymorphisms of genes related to folate metabolism change the efficacy of supplementation with folic acid [76]. Subjects were administered 5 mg folate daily for 90 days and homocysteine levels were measured before and after treatment. In addition, SNPs in MTHFR and MTRR genes were evaluated. After treatment, the efficacy of folate supplementation in reducing homocysteine levels was higher in participants carrying the SNPs rs1801133 and rs1801131 in MTHFR and rs1801394 and rs162036 in MTRR [76].
Vitamin D
Another micronutrient whose homeostasis is important to prevent CVD is vitamin D. While deficiency of this vitamin was previously related mainly to skeletal complications (osteoporosis, osteomalacia, osteopenia, and bone fractures), recent evidence reported that vitamin D deficiency has been associated to several nonskeletal diseases such as cancer, neurological disorders, metabolic diseases, and CVD [77]. Indeed, a meta-analysis involving 65,994 participants demonstrated a linear and inverse association between circulating vitamin D levels and CVD risk [78], supporting the hypothesis that vitamin D levels should be taken into account when planning a dietary regimen aimed to prevent CVD risk. This issue appears as particularly relevant in the obese population, which is not only more prone to CVD, but also to vitamin D deficiency (vitamin D deficiency prevalence is 35% higher in patients with obesity than in the eutrophic population) due to vitamin D lipophilic properties [79]. Despite circulating 25-hydroxy vitamin D concentrations being mainly determined by sun exposure followed by diet [80], growing evidence suggests that genetic factors could also play a role in determining vitamin D levels. A genome-wide association study identified some common genetic determinants of vitamin D insufficiency (rs2282679, rs12785878, rs10741657, and rs6013897) near to genes regulating cholesterol synthesis, hydroxylation, and vitamin D transport [81]. Furthermore, several SNPs located in the gene encoding for the vitamin D receptor (VDR) (Taq-I, Bsm-I, Apa-I, and Fok-I) [82] were also associated with different responses to vitamin D treatment [83]. Therefore, a nutrigenetic assessment could represent an additional tool to tailor vitamin D supplementation in order to prevent CVD.
The different response to vitamin D supplementation on the base of gene variants has been investigated in postmenopausal women with overweight and obesity [84] and in people with obesity and type 2 diabetes [83, 85]. Recent evidence suggests that SNPs in the vitamin D-related receptor genes are responsible for a different response to treatment. In particular, in 2207 postmenopausal women with overweight and obesity, the SNP rs11185644 in retinoid X receptor alpha (RXRA) has been demonstrated to be significantly associated with dose–response variation of 25(OH) serum levels to vitamin D supplementation [84]; in 204 people with type 2 diabetes, VDR polymorphisms have been investigated, showing that supplementation with 2000IU vitamin D daily for 12 months significantly improved the metabolic profile in Taq-I GG and Bsm-I TT genotype carriers [83]. Moreover, Neyestani et al. studied the different response to vitamin D in 140 people with type 2 diabetes carrying the VDR polymorphism Fok-I, the alleles of which have been defined as “F” (in case of absence of the restriction site) and “f” (in case of presence of the restriction site). After 12 weeks of treatment with 500 IU vitamin D/day, significant differences in 25(OH)D serum levels have been noted between “ff” and “FF,” in particular, the higher increment in serum 25(OH)D was found in “FF” (25(OH)D serum levels increment: FF > Ff > ff). Interestingly, lower levels of inflammatory biomarkers, including c-reactive protein and interleukin-6, were detected in “FF” carriers compared with “ff” and “Ff.” The authors, thus, conclude that “ff” carriers are “low responders” to vitamin D supplementation [85].
Dietary pattern
Extending the inquiry about fat intake and CVD, it is interesting to pay attention to the diatribe between low-fat and low-carb diets, which has recently become a hot topic in dietetics. In fact, while low-fat diets have been strongly promoted as antiatherogenic during the last decades, interesting evidence about use of low-carb diets is recently emerging [86]. Several nutrigenetic studies, with the inclusion of different genetic alleles, discussed the use of high-fat or low-fat diets in tailored nutritional approaches aimed to improve weight loss, lipid profile, and glycaemic control [87–91]. Most of the investigated genes were related to food intake control and regulation of energy homeostasis (i.e., FTO and MC3R) or glucose and lipid metabolism (i.e., ADIPOQ and CETP) [89, 92, 93]. Interestingly, genetic variants in the FTO and MC4R, both associated with appetite and food craving, have also been investigated for differential satiety in response to dietary protein intake [94, 95]. Heterogeneous responses after low energy diets were also observed in terms of weight loss and inflammation reduction according to FTO, PPAR, and NPY [96, 97], suggesting that different dietetic regimens in terms of macronutrients should be optimized to effectively reduce inflammation and improve lipid profile in subjects with different genetic backgrounds.
In addition, other nutrigenetic studies have reported some individual variations in the response to the Mediterranean diet [98–100]. Among dietary patterns, the Mediterranean diet is considered one of the healthiest in the world [101]. The Mediterranean diet is characterized by a high consumption of healthy food (e.g., extra virgin olive oil, fish, fruits and vegetables, legumes, unrefined cereals) [101]. This dietary pattern plays a key role not only in the prevention of a number of chronic diseases, including CVD and metabolic syndrome [102, 103], but in providing an important contribution to weight loss [104], contributing to prevent and treat obesity [105]. It is remarkable to notice that it has been recognized that the effect of adherence to the Mediterranean diet on cardiovascular outcomes [17–19] or others [106, 107] is also modulated by genetic influences (i.e., SNPs located in the genes NLRP3, CLOCK, MC4R, FTO, and PPAR). Garaulet et al., in a total of 1287 people with overweight and obesity, analyzed the anthropometric measurements and PERILIPIN1 (PLIN1) genotypes, including 6209T>C (rs2289487), 11482G>A (rs894160), 13041A>G (rs2304795), and 14995A>T (rs1052700) after the Mediterranean diet and weight-loss progression. The PLIN1 locus was associated with variability in response to a weight-loss program based on a Mediterranean diet. In particular, carrying the minor C allele at the PLIN1 6209T>C was associated with a better weight-loss response (p = 0.035) after 28 weeks of treatment and the probability of being a better responder evaluated as percentage of weight loss ≥ 7.5%, was 33% higher among C than among TT carriers (p = 0.017) [98].
The Food4Me Study demonstrated the beneficial effects of higher adherence to the Mediterranean diet after 6 months, also in the presence of an elevated genetic risk evaluated with a Genetic Risk Score, on anthropometric and biochemical markers. In particular, the authors found a greater reduction in body mass index and plasma glucose levels in the participants with a high genetic risk score when they had a higher adherence to the Mediterranean diet [99].
Very recently, Di Renzo et al., on a sample of 188 people divided into two groups, control group, and Mediterranean diet group, analyzed the FTO rs9939609 allele and the difference in body composition at baseline and after 4-week nutritional intervention in order to see if the FTO polymorphism could influence the response to a Mediterranean diet treatment [100]. The authors found significant relations of the variation of total body fat with the diet–gene interaction (p = 0.04). Of interest, FTO was associated with the variation of body composition in particular total body water (p = 0.02) concluding that whereas the Mediterranean diet is a good dietary treatment to reduce total body fat, data about FTO remain uncertain. Understanding the influence of FTO on body composition during dietary treatments is important to decide whether its effect has to be taken into consideration during both development of nutritional plans and patient monitoring.
Other dietary factors
Other dietary factors proposed to be useful as adjuvant for their potential anti-inflammatory effect (associated with antioxidant activity and inhibition of enzymes involved in eicosanoids production) are the polyphenols [108]. Studies showed that polyphenols intake can prevent CVD onset thanks to their antioxidant and antiatherosclerotic activity [109, 110]. It was recently demonstrated that supplementation with polyphenols from grape significantly reduced the serum levels of TMAO, an emerging risk factor for CVD [111, 112]. An interesting nutrigenetic association for the individual response to polyphenols intake has been attributed to the gene encoding for PON1 enzyme (a glycoprotein able to protect lipoproteins from oxidation and consequently strongly associated with HDL cholesterol antioxidant and anti-inflammatory activity). SNPs in the PON1 gene have been associated with susceptibility to CVD and atherosclerosis [113], but this association was interestingly linked to polyphenols and anthocyanins consumption [108]. In particular PON1 variants (rs854549, rs854552, rs854571, and rs854572) could identify subjects who effectively take advantage from targeted polyphenols dietary intake in terms of CVD prevention.
Coffee, and in general caffeine, intake is another issue that is commonly linked to cardiovascular outcomes. Interestingly, an observational study reported that coffee intake is negatively associated with metabolic syndrome prevalence, waist circumference, blood pressure, HDL cholesterol, LDL cholesterol, and triglycerides levels in psoriatic patients [114], suggesting the potential protective role of moderate (2–3 cups per day) consumption of coffee, probably due to the high amount of polyphenols. However, considering that there is no completely clear epidemiological evidence about the link between habitual coffee intake and the development of hypertension [115], nutrigenetic interactions are proposed as potentially able to explain part of the interindividual variability in the cardiovascular effects of coffee drinking. Several polymorphisms located in genes regulating caffeine metabolism (i.e., CYP1A2) or encoding for adenosine and adrenergic receptors (i.e., ADORA2A, ADRA1A, ADRA2B, ADRB1, ADRB2, and ADRB3) have been suggested to explain these heterogeneous cardiovascular effects of coffee consumption. Slow metabolizers of caffeine according to CYP1A2 genotype, in particular, displayed tachycardia, increased aortic stiffness, higher pulse wave velocity, vascular inflammation, and increased catecholamines after 3 h from caffeine consumption in comparison with the fast metabolizers [116]. Despite numerous studies investigating genotype mediated effects of caffeine on CVD risk, contrasting evidence emerged [117].
Limits and pitfalls of nutrigenetic approach to prevent CVDs
Several authors raised the question about the need for tailored nutrition in CVD prevention [118, 119]. Most of them concluded that, while it would be a promising field for the near future, there is a need for more evidence in our understanding of gene–nutrient interactions before it would be possible to translate these data into clinical practice [120]. Nevertheless, by now, it is impossible to ignore the potential implications of nutrigenetics on public health (including CVD prevention) in terms of (i) definition of personalized dietary requirement identification; (ii) identification of nutrient intake combinations ideal for the homeostasis of specific genomic profiles; (iii) better understanding of epidemiological data, clarifying the origin of the heterogeneous responses measured in populations after specific dietary intervention; and (iv) optimized intervention and prevention strategies [67].
As a matter of fact, despite a noteworthy body of scientific evidence on gene–diet interactions determining CVD phenotypes which clearly demonstrated that genetic influence on CVDs is mediated by diet, moving from bench to bed-side still actually represents a challenge for personalized nutrition. This is, at least in part, due to intrinsic limits of nutrigenetic studies (such as neglecting the possible overall interactions between numerous gene variants [121] with different nutritional interactions) and the lack of systematic review and meta-analysis of gene–diet interactions. These studies are mandatory to better estimate the effect size of gene–diet interactions and to identify the most predictive variants for which genotyping should be recommended. In this contest, Corella et al. [122] recently published a guide for upcoming studies and implementations necessary to overcome the current limits in nutrigenetics, while Grimaldi et al. proposed a guideline to evaluate the scientific evidence for genotype-based dietary advice in order to correctly introduce them into clinical practice [123].
Another aspect that could limit application of nutrigenetics is that the prevalence of the analyzed SNPs varies significantly among different ethnic groups and the association with the identified phenotype is not always confirmed in populations of different ethnicities. Furthermore, while communicating nutrigenetic data seems to promote motivation and adherence to diets [124], a recent systematic review demonstrated that to communicate the genetic risk of cardiometabolic disorders does not significantly impact motivation and actual engagement in preventative lifestyle modification and clinical outcome [125]. This suggests that the mediation of nutritionists and physicians is mandatory to correctly translate nutrigenetic information into clinical advice and to obtain real benefits for patients.
Conclusion
Undeniably, nutrigenetics is still in infancy with respect to research conducted on CVD prevention and therapy; nevertheless, the development of high-throughput (and cheaper) technologies and the increasing number of intervention studies including also nutrigenetic analysis have strongly contributed to produce consistent results [88, 126–129]. This promising landscape would be further enhanced by the co-application of other “omics” disciplines (i.e., epigenomics, nutrigenomics, metabolomics, lipidomics, transcriptomics, and proteomics). Dogan et al., for instance, recently demonstrated the ability of an integrated approach to successfully model symptomatic coronary heart disease status by integrating genetic, epigenetic and phenotype data from the Framingham Heart Study [126]. This inclusive approach is actually converting personalized nutrition and medicine into a reality, particularly in the field of CVD prevention in obesity.
Acknowledgements
Obesity Programs of nutrition, Education, Research and Assessment (OPERA) group members served as collaborators and approved the final version of the manuscript: Colao Annamaria, Savastano Silvia, Barrea Luigi, Muscogiuri Giovanna, Alviggi Carlo, Angrisani Luigi, Annunziata Giuseppe, Beguinot Francesco, Belfiore Annamaria, Belfiore Antonino, Bellastella Giuseppe, Biondi Bernadette, Bonaduce Domenico, Bordoni Laura, Brasacchio Caterina, Capaldo Brunella, Caprio Massimiliano, Cataldi Mauro, Cignarelli Angelo, Cittadini Antonello, Conforti Alessandro, Cuomo Rosario, De Placido Giuseppe, De Siena Marina, Di Carlo Costantino, Di Luigi Luigi, Di Nisio Andrea, Di Renzo Laura, Di Somma Carolina, Docimo Ludovico, Donini Lorenzo Maria, Federici Massimo, Foresta Carlo, Gabbianelli Rosita, Gambineri Alessandra, Gastaldelli Amalia, Giallauria Francesco, Giardiello Cristiano, Gnessi Lucio, Guida Brunella, Laudisio Daniela, Lenzi Andrea, Macchia Paolo Emidio, Manno Emilio, Marzullo Paolo, Migliaccio Silvia, Muratori Fabrizio, Musella Mario, Nardone Gerardo, Nicasto Vincenzo, Piazza Luigi, Pilone Vincenzo, Pivari Francesca, Pivonello Rosario, Pugliese Gabriella, Riccardi Gabriele, Ritieni Alberto, Salzano Ciro, Sanduzzi Alessandro, Sbraccia Paolo, Sesti Giorgio, Soldati Laura, Taglialatela Maurizio, Trimarco Bruno, Tuccinardi Dario.
Funding
The 2019 OPERA meeting was organized by Panta Rei Srl and sponsored by Novo Nordisk, Therascience, Bruno Pharma, Merck, Savio Pharma Italia Srl, IBSA Institut Biochimique SA, Bioitalia Srl, Cohesion Pharmaceutical, and Specchiasol Srl. Publication of this article as part of a supplement was sponsored by Panta Rei Srl, Naples, Italy. The meeting sponsors and organizer did not have access to the manuscripts and the authors maintained control of the content.
Author contributions
The authors’ responsibilities were as follows: LB, GA, LB, and SS were responsible for the concept of this paper and drafted the manuscript; GM, AC, and SS provided a critical review of the paper. LB, GA, and LB are equally contributed to this work. OPERA Group members participated to the revision of the manuscript. All authors and OPERA Group Members contributed to and agreed on the final version of the manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Karczewski J, Sledzinska E, Baturo A, Jonczyk I, Maleszko A, Samborski P, et al. Obesity and inflammation. Eur Cytokine Netw. 2018;29:83–94. doi: 10.1684/ecn.2018.0415. [DOI] [PubMed] [Google Scholar]
- 2.Goodarzi MO. Genetics of obesity: what genetic association studies have taught us about the biology of obesity and its complications. Lancet. 2018;6:223–36. doi: 10.1016/S2213-8587(17)30200-0. [DOI] [PubMed] [Google Scholar]
- 3.Ordovas JM, Corella D. Nutritional genomics. Ann Rev Genom Hum Genet. 2004;5:71–118. doi: 10.1146/annurev.genom.5.061903.180008. [DOI] [PubMed] [Google Scholar]
- 4.Webb TR, Erdmann J, Stirrups KE, Stitziel NO, Masca NG, Jansen H, et al. Systematic evaluation of pleiotropy identifies 6 further loci associated with coronary artery disease. J Am Coll Cardiol. 2017;69:823–36. doi: 10.1016/j.jacc.2016.11.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vazquez-Vidal I, Desmarchelier C, Jones PJH. Nutrigenetics of blood cholesterol concentrations: towards personalized nutrition. Curr Cardiol Rep. 2019;21:38. doi: 10.1007/s11886-019-1124-x. [DOI] [PubMed] [Google Scholar]
- 6.El-Sohemy A. Nutrigenetics. Forum Nutr. 2007;60:25–30. doi: 10.1159/000107064. [DOI] [PubMed] [Google Scholar]
- 7.Williams CM, Ordovas JM, Lairon D, Hesketh J, Lietz G, Gibney M, et al. The challenges for molecular nutrition research 1: linking genotype to healthy nutrition. Genes Nutr. 2008;3:41–9. doi: 10.1007/s12263-008-0086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gregori D, Foltran F, Verduci E, Ballali S, Franchin L, Ghidina M, et al. A genetic perspective on nutritional profiles: do we still need them? J Nutrigenet Nutrigenomics. 2011;4:25–35. doi: 10.1159/000322569. [DOI] [PubMed] [Google Scholar]
- 9.Elsamanoudy AZ, Mohamed Neamat-Allah MA, Hisham Mohammad FA, Hassanien M, Nada HA. The role of nutrition related genes and nutrigenetics in understanding the pathogenesis of cancer. J Microsc Ultrastruct. 2016;4:115–22. doi: 10.1016/j.jmau.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeBusk RM, Fogarty CP, Ordovas JM, Kornman KS. Nutritional genomics in practice: where do we begin? J Am Dietetic Association. 2005;105:589–98. doi: 10.1016/j.jada.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Elder SJ, Lichtenstein AH, Pittas AG, Roberts SB, Fuss PJ, Greenberg AS, et al. Genetic and environmental influences on factors associated with cardiovascular disease and the metabolic syndrome. J Lipid Res. 2009;50:1917–26. doi: 10.1194/jlr.P900033-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ordovas JM, Corella D, Cupples LA, Demissie S, Kelleher A, Coltell O, et al. Polyunsaturated fatty acids modulate the effects of the APOA1 G-A polymorphism on HDL-cholesterol concentrations in a sex-specific manner: the Framingham Study. Am J Clin Nutr. 2002;75:38–46. doi: 10.1093/ajcn/75.1.38. [DOI] [PubMed] [Google Scholar]
- 13.Xu M, Zhao J, Zhang Y, Ma X, Dai Q, Zhi H, et al. Apolipoprotein E gene variants and risk of coronary heart disease: a meta-analysis. BioMed Res Int. 2016;2016:3912175. doi: 10.1155/2016/3912175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tapsell LC, Neale EP, Satija A, Hu FB. Foods, nutrients, and dietary patterns: interconnections and implications for dietary guidelines. Adv Nutr. 2016;7:445–54. doi: 10.3945/an.115.011718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Celis-Morales C, Livingstone KM, Marsaux CF, Forster H, O’Donovan CB, Woolhead C, et al. Design and baseline characteristics of the Food4Me study: a web-based randomised controlled trial of personalised nutrition in seven European countries. Genes Nutr. 2015;10:450. doi: 10.1007/s12263-014-0450-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fallaize R, Celis-Morales C, Macready AL, Marsaux CF, Forster H, O’Donovan C, et al. The effect of the apolipoprotein E genotype on response to personalized dietary advice intervention: findings from the Food4Me randomized controlled trial. Am J Clin Nutr. 2016;104:827–36. doi: 10.3945/ajcn.116.135012. [DOI] [PubMed] [Google Scholar]
- 17.Corella D, Asensio EM, Coltell O, Sorli JV, Estruch R, Martinez-Gonzalez MA, et al. CLOCK gene variation is associated with incidence of type-2 diabetes and cardiovascular diseases in type-2 diabetic subjects: dietary modulation in the PREDIMED randomized trial. Cardiovasc Diabetol. 2016;15:4. doi: 10.1186/s12933-015-0327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ortega-Azorin C, Sorli JV, Estruch R, Asensio EM, Coltell O, Gonzalez JI, et al. Amino acid change in the carbohydrate response element binding protein is associated with lower triglycerides and myocardial infarction incidence depending on level of adherence to the Mediterranean diet in the PREDIMED trial. Circulation. 2014;7:49–58. doi: 10.1161/CIRCGENETICS.113.000301. [DOI] [PubMed] [Google Scholar]
- 19.Roncero-Ramos I, Rangel-Zuniga OA, Lopez-Moreno J, Alcala-Diaz JF, Perez-Martinez P, Jimenez-Lucena R, et al. Mediterranean diet, glucose homeostasis, and inflammasome genetic variants: The CORDIOPREV Study. Mol Nutr Food Res. 2018;62:e1700960. doi: 10.1002/mnfr.201700960. [DOI] [PubMed] [Google Scholar]
- 20.de Toro-Martin J, Arsenault BJ, Despres JP, Vohl MC. Precision nutrition: a review of personalized nutritional approaches for the prevention and management of metabolic syndrome. Nutrients. 2017;9:913–41. doi: 10.3390/nu9080913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019;92:98–107. doi: 10.1016/j.metabol.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci. 2001;321:225–36. doi: 10.1097/00000441-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Chakko S, Mayor M, Allison MD, Kessler KM, Materson BJ, Myerburg RJ. Abnormal left ventricular diastolic filling in eccentric left ventricular hypertrophy of obesity. Am J Cardiol. 1991;68:95–8. doi: 10.1016/0002-9149(91)90718-z. [DOI] [PubMed] [Google Scholar]
- 24.Lavie CJ, Milani RV, Ventura HO, Cardenas GA, Mehra MR, Messerli FH. Disparate effects of left ventricular geometry and obesity on mortality in patients with preserved left ventricular ejection fraction. Am J Cardiol. 2007;100:1460–4. doi: 10.1016/j.amjcard.2007.06.040. [DOI] [PubMed] [Google Scholar]
- 25.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–56. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 26.Nakamura K, Fuster JJ, Walsh K. Adipokines: a link between obesity and cardiovascular disease. J Cardiol. 2014;63:250–9. doi: 10.1016/j.jjcc.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koh KK, Park SM, Quon MJ. Leptin and cardiovascular disease: response to therapeutic interventions. Circulation. 2008;117:3238–49. doi: 10.1161/CIRCULATIONAHA.107.741645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guglielmi V, Sbraccia P. Epicardial adipose tissue: at the heart of the obesity complications. Acta Diabetol. 2017;54:805–12. doi: 10.1007/s00592-017-1020-z. [DOI] [PubMed] [Google Scholar]
- 29.Bleau C, Karelis AD, St-Pierre DH, Lamontagne L. Crosstalk between intestinal microbiota, adipose tissue and skeletal muscle as an early event in systemic low-grade inflammation and the development of obesity and diabetes. Diabetes/Metab Res Rev. 2015;31:545–61. doi: 10.1002/dmrr.2617. [DOI] [PubMed] [Google Scholar]
- 30.Li XS, Obeid S, Klingenberg R, Gencer B, Mach F, Raber L, et al. Gut microbiota-dependent trimethylamine N-oxide in acute coronary syndromes: a prognostic marker for incident cardiovascular events beyond traditional risk factors. Eur Heart J. 2017;38:814–24. doi: 10.1093/eurheartj/ehw582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Randrianarisoa E, Lehn-Stefan A, Wang X, Hoene M, Peter A, Heinzmann SS, et al. Relationship of serum trimethylamine n-oxide (TMAO) levels with early atherosclerosis in humans. Sci Rep. 2016;6:26745. doi: 10.1038/srep26745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haghikia A, Li XS, Liman TG, Bledau N, Schmidt D, Zimmermann F, et al. Gut microbiota-dependent trimethylamine N-oxide predicts risk of cardiovascular events in patients with stroke and is related to proinflammatory monocytes. Arterioscler Thromb Vasc Biol. 2018;38:2225–35. doi: 10.1161/ATVBAHA.118.311023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liang Z, Dong Z, Guo M, Shen Z, Yin D, Hu S, et al. Trimethylamine N-oxide as a risk marker for ischemic stroke in patients with atrial fibrillation. J Biochem Mol Toxicol. 2019;33:e22246. doi: 10.1002/jbt.22246. [DOI] [PubMed] [Google Scholar]
- 34.Nie J, Xie L, Zhao BX, Li Y, Qiu B, Zhu F, et al. Serum trimethylamine N-oxide concentration is positively associated with first stroke in hypertensive patients. Stroke. 2018;49:2021–8. doi: 10.1161/STROKEAHA.118.021997. [DOI] [PubMed] [Google Scholar]
- 35.Wu C, Li C, Zhao W, Xie N, Yan F, Lian Y, et al. Elevated trimethylamine N-oxide related to ischemic brain lesions after carotid artery stenting. Neurology. 2018;90:e1283–e1290. doi: 10.1212/WNL.0000000000005298. [DOI] [PubMed] [Google Scholar]
- 36.Tang WH, Wang Z, Fan Y, Levison B, Hazen JE, Donahue LM, et al. Prognostic value of elevated levels of intestinal microbe-generated metabolite trimethylamine-N-oxide in patients with heart failure: refining the gut hypothesis. J Am Coll Cardiol. 2014;64:1908–14. doi: 10.1016/j.jacc.2014.02.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barrea L, Annunziata G, Muscogiuri G, Di Somma C, Laudisio D, Maisto M, et al. Trimethylamine-N-oxide (TMAO) as novel potential biomarker of early predictors of metabolic syndrome. Nutrients. 2018;10:1971–90. doi: 10.3390/nu10121971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.LaRocca TJ, Martens CR, Seals DR. Nutrition and other lifestyle influences on arterial aging. Ageing Res Rev. 2017;39:106–19. doi: 10.1016/j.arr.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhatnagar A. Environmental determinants of cardiovascular disease. Circ Res. 2017;121:162–80. doi: 10.1161/CIRCRESAHA.117.306458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Masana L, Ros E, Sudano I, Angoulvant D, lifestyle expert working group Is there a role for lifestyle changes in cardiovascular prevention? What, when and how? Atheroscler Suppl. 2017;26:2–15. doi: 10.1016/S1567-5688(17)30020-X. [DOI] [PubMed] [Google Scholar]
- 41.Khanji MY, van Waardhuizen CN, Bicalho VVS, Ferket BS, Hunink MGM, Petersen SE. Lifestyle advice and interventions for cardiovascular risk reduction: a systematic review of guidelines. Int J Cardiol. 2018;263:142–51. doi: 10.1016/j.ijcard.2018.02.094. [DOI] [PubMed] [Google Scholar]
- 42.Torres N, Guevara-Cruz M, Velazquez-Villegas LA, Tovar AR. Nutrition and atherosclerosis. Arch Med Res. 2015;46:408–26. doi: 10.1016/j.arcmed.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 43.Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG, et al. The sequence of the human genome. Science. 2001;291:1304–51. doi: 10.1126/science.1058040. [DOI] [PubMed] [Google Scholar]
- 44.Bordoni L, Gabbianelli R. Primers on nutrigenetics and nutri(epi)genomics: origins and development of precision nutrition. Biochimie. 2019;160:156–71. doi: 10.1016/j.biochi.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 45.Lloyd-Jones DM, Nam BH, D’Agostino RB, Sr., Levy D, Murabito JM, Wang TJ, et al. Parental cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults: a prospective study of parents and offspring. JAMA. 2004;291:2204–11. doi: 10.1001/jama.291.18.2204. [DOI] [PubMed] [Google Scholar]
- 46.Govindaraju DR, Adrienne Cupples L, Kannel WB, O’Donnell CJ, Atwood LD, D’Agostino RB, Sr., et al. Genetics of the Framingham Heart Study population. Adv Genet. 2008;62:33–65. doi: 10.1016/S0065-2660(08)00602-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Larson MG, Atwood LD, Benjamin EJ, Cupples LA, D’Agostino RB, Sr., Fox CS, et al. Framingham Heart Study 100K project: genome-wide associations for cardiovascular disease outcomes. BMC Med Genet. 2007;8(Suppl 1):S5. doi: 10.1186/1471-2350-8-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Consortium CAD, Deloukas P, Kanoni S, Willenborg C, Farrall M, Assimes TL, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013;45:25–33. doi: 10.1038/ng.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Borel P, Desmarchelier C, Nowicki M, Bott R. A combination of single-nucleotide polymorphisms is associated with interindividual variability in dietary beta-carotene bioavailability in healthy men. J Nutr. 2015;145:1740–7. doi: 10.3945/jn.115.212837. [DOI] [PubMed] [Google Scholar]
- 50.Borel P, Desmarchelier C, Nowicki M, Bott R. Lycopene bioavailability is associated with a combination of genetic variants. Free Radic Biol Med. 2015;83:238–44. doi: 10.1016/j.freeradbiomed.2015.02.033. [DOI] [PubMed] [Google Scholar]
- 51.Borel P, Desmarchelier C, Nowicki M, Bott R, Tourniaire F. Can genetic variability in alpha-tocopherol bioavailability explain the heterogeneous response to alpha-tocopherol supplements? Antioxid Redox Signal. 2015;22:669–78. doi: 10.1089/ars.2014.6144. [DOI] [PubMed] [Google Scholar]
- 52.Desmarchelier C, Martin JC, Planells R, Gastaldi M, Nowicki M, Goncalves A, et al. The postprandial chylomicron triacylglycerol response to dietary fat in healthy male adults is significantly explained by a combination of single nucleotide polymorphisms in genes involved in triacylglycerol metabolism. J Clin Endocrinol Metab. 2014;99:E484–8. doi: 10.1210/jc.2013-3962. [DOI] [PubMed] [Google Scholar]
- 53.Luft FC, Weinberger MH. Heterogeneous responses to changes in dietary salt intake: the salt-sensitivity paradigm. Am J Clin Nutr. 1997;65(2 Suppl):612S–617S. doi: 10.1093/ajcn/65.2.612S. [DOI] [PubMed] [Google Scholar]
- 54.Ferguson LR, De Caterina R, Gorman U, Allayee H, Kohlmeier M, Prasad C, et al. Guide and position of the international society of nutrigenetics/nutrigenomics on personalised nutrition: part 1—fields of precision nutrition. J Nutrigenet Nutrigenomics. 2016;9:12–27. doi: 10.1159/000445350. [DOI] [PubMed] [Google Scholar]
- 55.Wittwer J, Rubio-Aliaga I, Hoeft B, Bendik I, Weber P, Daniel H. Nutrigenomics in human intervention studies: current status, lessons learned and future perspectives. Mol Nutr Food Res. 2011;55:341–58. doi: 10.1002/mnfr.201000512. [DOI] [PubMed] [Google Scholar]
- 56.Ross LJ, Barnes KA, Ball LE, Mitchell LJ, Sladdin I, Lee P, et al. Effectiveness of dietetic consultation for lowering blood lipid levels in the management of cardiovascular disease risk: A systematic review and meta-analysis of randomised controlled trials. Nutr Diet. 2019;76:199–210. doi: 10.1111/1747-0080.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shivappa N, Godos J, Hebert JR, Wirth MD, Piuri G, Speciani AF, et al. Dietary inflammatory index and cardiovascular risk and mortality-a meta-analysis. Nutrients. 2018;10:200–15. doi: 10.3390/nu10020200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ordovas JM, Corella D. Genetic variation and lipid metabolism: modulation by dietary factors. Curr Cardiol Rep. 2005;7:480–6. doi: 10.1007/s11886-005-0067-6. [DOI] [PubMed] [Google Scholar]
- 59.Chilton FH, Murphy RC, Wilson BA, Sergeant S, Ainsworth H, Seeds MC, et al. Diet-gene interactions and PUFA metabolism: a potential contributor to health disparities and human diseases. Nutrients. 2014;6:1993–2022. doi: 10.3390/nu6051993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O’Neill CM, Minihane AM. The impact of fatty acid desaturase genotype on fatty acid status and cardiovascular health in adults. Proc Nutr Soc. 2017;76:64–75. doi: 10.1017/S0029665116000732. [DOI] [PubMed] [Google Scholar]
- 61.Zheng JS, Chen J, Wang L, Yang H, Fang L, Yu Y, et al. Replication of a gene-diet interaction at CD36, NOS3 and PPARG in response to omega-3 fatty acid supplements on blood lipids: a double-blind randomized controlled trial. EBioMedicine. 2018;31:150–6. doi: 10.1016/j.ebiom.2018.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferguson JF, Phillips CM, McMonagle J, Perez-Martinez P, Shaw DI, Lovegrove JA, et al. NOS3 gene polymorphisms are associated with risk markers of cardiovascular disease, and interact with omega-3 polyunsaturated fatty acids. Atherosclerosis. 2010;211:539–44. doi: 10.1016/j.atherosclerosis.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 63.Armstrong P, Kelley DS, Newman JW, Staggers FE, Sr., Hartiala J, Allayee H, et al. Arachidonate 5-lipoxygenase gene variants affect response to fish oil supplementation by healthy African Americans. J Nutr. 2012;142:1417–28. doi: 10.3945/jn.112.159814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matualatupauw JC, Radonjic M, van de Rest O, de Groot LC, Geleijnse JM, Muller M, et al. Apolipoprotein E genotype status affects habitual human blood mononuclear cell gene expression and its response to fish oil intervention. Mol Nutr Food Res. 2016;60:1649–60. doi: 10.1002/mnfr.201500941. [DOI] [PubMed] [Google Scholar]
- 65.Vallee Marcotte B, Cormier H, Rudkowska I, Lemieux S, Couture P, Vohl MC, et al. Polymorphisms in FFAR4 (GPR120) gene modulate insulin levels and sensitivity after fish oil supplementation. J Pers Med. 2017;7:15–27. doi: 10.3390/jpm7040015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vallee Marcotte B, Guenard F, Lemieux S, Couture P, Rudkowska I, Calder PC, et al. Fine mapping of genome-wide association study signals to identify genetic markers of the plasma triglyceride response to an omega-3 fatty acid supplementation. Am J Clin Nutr. 2019;109:176–85. doi: 10.1093/ajcn/nqy298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reddy VS, Palika R, Ismail A, Pullakhandam R, Reddy GB. Nutrigenomics: opportunities & challenges for public health nutrition. Indian J Med Res. 2018;148:632–41. doi: 10.4103/ijmr.IJMR_1738_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Selhub J. Folate, vitamin B12 and vitamin B6 and one carbon metabolism. J Nutr Health Aging. 2002;6:39–42. [PubMed] [Google Scholar]
- 69.Ridker PM, Shih J, Cook TJ, Clearfield M, Downs JR, Pradhan AD, et al. Plasma homocysteine concentration, statin therapy, and the risk of first acute coronary events. Circulation. 2002;105:1776–9. [PubMed] [Google Scholar]
- 70.Selhub J. The many facets of hyperhomocysteinemia: studies from the Framingham cohorts. J Nutr. 2006;136(6 Suppl):1726S–30S. doi: 10.1093/jn/136.6.1726S. [DOI] [PubMed] [Google Scholar]
- 71.Djuric D, Jakovljevic V, Zivkovic V, Srejovic I. Homocysteine and homocysteine-related compounds: an overview of the roles in the pathology of the cardiovascular and nervous systems. Can J Physiol Pharmacol. 2018;96:991–1003. doi: 10.1139/cjpp-2018-0112. [DOI] [PubMed] [Google Scholar]
- 72.Cesari M, Burlina AB, Narkiewicz K, Sartori MT, Sacchetto A, Rossi GP. Are fasting plasma homocyst(e)ine levels heritable? A study of normotensive twins. J Investig Med. 2000;48:351–8. [PubMed] [Google Scholar]
- 73.Vermeulen SH, van der Vleuten GM, de Graaf J, Hermus AR, Blom HJ, Stalenhoef AF, et al. A genome-wide linkage scan for homocysteine levels suggests three regions of interest. J Throm Haemost. 2006;4:1303–7. doi: 10.1111/j.1538-7836.2006.01977.x. [DOI] [PubMed] [Google Scholar]
- 74.Hazra A, Kraft P, Lazarus R, Chen C, Chanock SJ, Jacques P, et al. Genome-wide significant predictors of metabolites in the one-carbon metabolism pathway. Hum Mol Genet. 2009;18:4677–87. doi: 10.1093/hmg/ddp428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Colson NJ, Naug HL, Nikbakht E, Zhang P, McCormack J. The impact of MTHFR 677 C/T genotypes on folate status markers: a meta-analysis of folic acid intervention studies. Eur J Nutr. 2017;56:247–60. doi: 10.1007/s00394-015-1076-x. [DOI] [PubMed] [Google Scholar]
- 76.Du B, Tian H, Tian D, Zhang C, Wang W, Wang L, et al. Genetic polymorphisms of key enzymes in folate metabolism affect the efficacy of folate therapy in patients with hyperhomocysteinaemia. Br J Nutr. 2018;119:887–95. doi: 10.1017/S0007114518000508. [DOI] [PubMed] [Google Scholar]
- 77.Kheiri B, Abdalla A, Osman M, Ahmed S, Hassan M, Bachuwa G. Vitamin D deficiency and risk of cardiovascular diseases: a narrative review. Clin Hypertens. 2018;24:9. doi: 10.1186/s40885-018-0094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pilz S, Tomaschitz A, Drechsler C, Zittermann A, Dekker JM, Marz W. Vitamin D supplementation: a promising approach for the prevention and treatment of strokes. Curr Drug Targets. 2011;12:88–96. doi: 10.2174/138945011793591563. [DOI] [PubMed] [Google Scholar]
- 79.Pereira-Santos M, Costa PR, Assis AM, Santos CA, Santos DB. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. 2015;16:341–9. doi: 10.1111/obr.12239. [DOI] [PubMed] [Google Scholar]
- 80.Savastano S, Barrea L, Savanelli MC, Nappi F, Di Somma C, Orio F, et al. Low vitamin D status and obesity: role of nutritionist. Rev Endocr Metab Disord. 2017;18:215–25. doi: 10.1007/s11154-017-9410-7. [DOI] [PubMed] [Google Scholar]
- 81.Wang TJ, Zhang F, Richards JB, Kestenbaum B, van Meurs JB, Berry D, et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 2010;376:180–8. doi: 10.1016/S0140-6736(10)60588-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Uitterlinden AG, Fang Y, Van Meurs JB, Pols HA, Van Leeuwen JP. Genetics and biology of vitamin D receptor polymorphisms. Gene. 2004;338:143–56. doi: 10.1016/j.gene.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 83.Al-Daghri NM, Mohammed AK, Al-Attas OS, Ansari MGA, Wani K, Hussain SD, et al. Vitamin D receptor gene polymorphisms modify cardiometabolic response to vitamin D supplementation in T2DM patients. Sci Rep. 2017;7:8280. doi: 10.1038/s41598-017-08621-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang M, Zhao LJ, Zhou Y, Badr R, Watson P, Ye A, et al. SNP rs11185644 of RXRA gene is identified for dose-response variability to vitamin D3 supplementation: a randomized clinical trial. Sci Rep. 2017;7:40593. doi: 10.1038/srep40593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Neyestani TR, Djazayery A, Shab-Bidar S, Eshraghian MR, Kalayi A, Shariatzadeh N, et al. Vitamin D receptor Fok-I polymorphism modulates diabetic host response to vitamin D intake: need for a nutrigenetic approach. Diabetes Care. 2013;36:550–6. doi: 10.2337/dc12-0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hu T, Bazzano LA. The low-carbohydrate diet and cardiovascular risk factors: evidence from epidemiologic studies. Nutr Metab Cardiovasc Dis. 2014;24:337–43. doi: 10.1016/j.numecd.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gardner CD, Trepanowski JF, Del Gobbo LC, Hauser ME, Rigdon J, Ioannidis JPA, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: The DIETFITS Randomized Clinical Trial. JAMA. 2018;319:667–79. doi: 10.1001/jama.2018.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sun D, Heianza Y, Li X, Shang X, Smith SR, Bray GA, et al. Genetic, epigenetic and transcriptional variations at NFATC2IP locus with weight loss in response to diet interventions: The POUNDS Lost Trial. Diabetes Obes Metab. 2018;20:2298–303. doi: 10.1111/dom.13333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Qi Q, Durst R, Schwarzfuchs D, Leitersdorf E, Shpitzen S, Li Y, et al. CETP genotype and changes in lipid levels in response to weight-loss diet intervention in the POUNDS LOST and DIRECT randomized trials. J Lipid Res. 2015;56:713–21. doi: 10.1194/jlr.P055715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Goni L, Qi L, Cuervo M, Milagro FI, Saris WH, MacDonald IA, et al. Effect of the interaction between diet composition and the PPM1K genetic variant on insulin resistance and beta cell function markers during weight loss: results from the Nutrient Gene Interactions in Human Obesity: implications for dietary guidelines (NUGENOB) randomized trial. Am J Clin Nutr. 2017;106:902–8. doi: 10.3945/ajcn.117.156281. [DOI] [PubMed] [Google Scholar]
- 91.Santos JL, De la Cruz R, Holst C, Grau K, Naranjo C, Maiz A, et al. Allelic variants of melanocortin 3 receptor gene (MC3R) and weight loss in obesity: a randomised trial of hypo-energetic high- versus low-fat diets. PLoS ONE. 2011;6:e19934. doi: 10.1371/journal.pone.0019934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.de Luis DA, Izaola O, Primo D, Aller R, Ortola A, Gomez E, et al. The association of SNP276G>T at adiponectin gene with insulin resistance and circulating adiponectin in response to two different hypocaloric diets. Diabetes Res and Clin Pract. 2018;137:93–99. doi: 10.1016/j.diabres.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 93.Zheng Y, Huang T, Zhang X, Rood J, Bray GA, Sacks FM, et al. Dietary fat modifies the effects of FTO genotype on changes in insulin sensitivity. J Nutr. 2015;145:977–82. doi: 10.3945/jn.115.210005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Huang T, Zheng Y, Hruby A, Williamson DA, Bray GA, Shen Y, et al. Dietary protein modifies the effect of the MC4R genotype on 2-year changes in appetite and food craving: The POUNDS Lost Trial. J Nutr. 2017;147:439–44. doi: 10.3945/jn.116.242958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Huang T, Qi Q, Li Y, Hu FB, Bray GA, Sacks FM, et al. FTO genotype, dietary protein, and change in appetite: the preventing overweight using novel dietary strategies trial. Am J Clin Nutr. 2014;99:1126–30. doi: 10.3945/ajcn.113.082164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Curti ML, Rogero MM, Baltar VT, Barros CR, Siqueira-Catania A, Ferreira SR. FTO T/A and peroxisome proliferator-activated receptor-gamma Pro12Ala polymorphisms but not ApoA1-75 are associated with better response to lifestyle intervention in Brazilians at high cardiometabolic risk. Metab Syndr Relat Disord. 2013;11:169–76. doi: 10.1089/met.2012.0055. [DOI] [PubMed] [Google Scholar]
- 97.de Luis DA, Izaola O, de la Fuente B, Primo D, Aller R. Polymorphism of neuropeptide Y gene rs16147 modifies the response to a hypocaloric diet on cardiovascular risk biomarkers and adipokines. J Hum Nutr Diet. 2017;30:159–65. doi: 10.1111/jhn.12406. [DOI] [PubMed] [Google Scholar]
- 98.Garaulet M, Vera B, Bonnet-Rubio G, Gomez-Abellan P, Lee YC, Ordovas JM. Lunch eating predicts weight-loss effectiveness in carriers of the common allele at PERILIPIN1: the ONTIME (Obesity, Nutrigenetics, Timing, Mediterranean) study. Am J Clin Nutr. 2016;104:1160–6. doi: 10.3945/ajcn.116.134528. [DOI] [PubMed] [Google Scholar]
- 99.San-Cristobal R, Navas-Carretero S, Livingstone KM, Celis-Morales C, Macready AL, Fallaize R, et al. Mediterranean diet adherence and genetic background roles within a web-based nutritional intervention: The Food4Me Study. Nutrients. 2017;9:1107–24. doi: 10.3390/nu9101107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Di Renzo L, Cioccoloni G, Falco S, Abenavoli L, Moia A, Sinibaldi Salimei P, et al. Influence of FTO rs9939609 and Mediterranean diet on body composition and weight loss: a randomized clinical trial. J Transl Med. 2018;16:308. doi: 10.1186/s12967-018-1680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72:30–43. doi: 10.1038/ejcn.2017.58. [DOI] [PubMed] [Google Scholar]
- 102.Widmer RJ, Flammer AJ, Lerman LO, Lerman A. The Mediterranean diet, its components, and cardiovascular disease. Am J Med. 2015;128:229–38. doi: 10.1016/j.amjmed.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mayneris-Perxachs J, Sala-Vila A, Chisaguano M, Castellote AI, Estruch R, Covas MI, et al. Effects of 1-year intervention with a Mediterranean diet on plasma fatty acid composition and metabolic syndrome in a population at high cardiovascular risk. PLoS ONE. 2014;9:e85202. doi: 10.1371/journal.pone.0085202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Esposito K, Kastorini CM, Panagiotakos DB, Giugliano D. Mediterranean diet and weight loss: meta-analysis of randomized controlled trials. Metab Syndr Relat Disord. 2011;9:1–12. doi: 10.1089/met.2010.0031. [DOI] [PubMed] [Google Scholar]
- 105.Bendall CL, Mayr HL, Opie RS, Bes-Rastrollo M, Itsiopoulos C, Thomas CJ. Central obesity and the Mediterranean diet: a systematic review of intervention trials. Crit Rev Food Sci Nutr. 2018;58:3070–84. doi: 10.1080/10408398.2017.1351917. [DOI] [PubMed] [Google Scholar]
- 106.Garcia-Calzon S, Martinez-Gonzalez MA, Razquin C, Corella D, Salas-Salvado J, Martinez JA, et al. Pro12Ala polymorphism of the PPARgamma2 gene interacts with a mediterranean diet to prevent telomere shortening in the PREDIMED-NAVARRA randomized trial. Circulation. 2015;8:91–9. doi: 10.1161/CIRCGENETICS.114.000635. [DOI] [PubMed] [Google Scholar]
- 107.Ortega-Azorin C, Sorli JV, Asensio EM, Coltell O, Martinez-Gonzalez MA, Salas-Salvado J, et al. Associations of the FTO rs9939609 and the MC4R rs17782313 polymorphisms with type 2 diabetes are modulated by diet, being higher when adherence to the Mediterranean diet pattern is low. Cardiovasc Diabetol. 2012;11:137. doi: 10.1186/1475-2840-11-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hussain T, Tan B, Yin Y, Blachier F, Tossou MC, Rahu N. Oxidative stress and inflammation: what polyphenols can do for us? Oxid Med Cell Longev. 2016;2016:7432797. doi: 10.1155/2016/7432797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kowalska K, Socha E, Milnerowicz H. Review: the role of paraoxonase in cardiovascular diseases. Ann Clin Lab Sci. 2015;45:226–33. [PubMed] [Google Scholar]
- 110.Rizzi F, Conti C, Dogliotti E, Terranegra A, Salvi E, Braga D, et al. Interaction between polyphenols intake and PON1 gene variants on markers of cardiovascular disease: a nutrigenetic observational study. J Transl Med. 2016;14:186. doi: 10.1186/s12967-016-0941-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Annunziata G, Maisto M, Schisano C, Ciampaglia R, Narciso V, Hassan STS, et al. Effect of grape pomace polyphenols with or without pectin on TMAO serum levels assessed by LC/MS-based assay: a preliminary clinical study on overweight/obese subjects. Front Pharmacol. 2019;10:575. doi: 10.3389/fphar.2019.00575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Annunziata G, Maisto M, Schisano C, Ciampaglia R, Narciso V, Tenore GC, et al. Effects of grape pomace polyphenolic extract (Taurisolo((R) in reducing TMAO serum levels in humans: preliminary results from a randomized, placebo-controlled, cross-over study. Nutrients. 2019;11:139–50. doi: 10.3390/nu11010139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shunmoogam N, Naidoo P, Chilton R. Paraoxonase (PON)-1: a brief overview on genetics, structure, polymorphisms and clinical relevance. Vasc Health Risk Manag. 2018;14:137–43. doi: 10.2147/VHRM.S165173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Barrea L, Muscogiuri G, Di Somma C, Annunziata G, Megna M, Falco A, et al. Coffee consumption, metabolic syndrome and clinical severity of psoriasis: good or bad stuff? Arch Toxicol. 2018;92:1831–45. doi: 10.1007/s00204-018-2193-0. [DOI] [PubMed] [Google Scholar]
- 115.Renda G, De Caterina R. Coffee and hypertension: a focus on contrasting acute and chronic effects and nutrigenetics. In: Preedy VR, editor. Coffee in health and disease prevention. Academic Press; 2015. p. 395–402. 10.1016/C2012-0-06959-1.
- 116.Palatini P, Ceolotto G, Ragazzo F, Dorigatti F, Saladini F, Papparella I, et al. CYP1A2 genotype modifies the association between coffee intake and the risk of hypertension. J Hypertens. 2009;27:1594–601. doi: 10.1097/HJH.0b013e32832ba850. [DOI] [PubMed] [Google Scholar]
- 117.Mesas AE, Leon-Munoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr. 2011;94:1113–26.. doi: 10.3945/ajcn.111.016667. [DOI] [PubMed] [Google Scholar]
- 118.Simopoulos AP. Nutrigenetics/nutrigenomics. Ann Rev Public Health. 2010;31:53–68. doi: 10.1146/annurev.publhealth.031809.130844. [DOI] [PubMed] [Google Scholar]
- 119.Fenech M, El-Sohemy A, Cahill L, Ferguson LR, French TA, Tai ES, et al. Nutrigenetics and nutrigenomics: viewpoints on the current status and applications in nutrition research and practice. J Nutrigenet Nutrigenomics. 2011;4:69–89. doi: 10.1159/000327772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Juma S, Imrhan V, Vijayagopal P, Prasad C. Prescribing personalized nutrition for cardiovascular health: are we ready? J Nutrigenet Nutrigenomics. 2014;7:153–60. doi: 10.1159/000370213. [DOI] [PubMed] [Google Scholar]
- 121.Bordoni L, Marchegiani F, Piangerelli M, Napolioni V, Gabbianelli R. Obesity-related genetic polymorphisms and adiposity indices in a young Italian population. IUBMB Life. 2017;69:98–105. doi: 10.1002/iub.1596. [DOI] [PubMed] [Google Scholar]
- 122.Corella D, Coltell O, Mattingley G, Sorli JV, Ordovas JM. Utilizing nutritional genomics to tailor diets for the prevention of cardiovascular disease: a guide for upcoming studies and implementations. Expert Rev Mol Diagn. 2017;17:495–513. doi: 10.1080/14737159.2017.1311208. [DOI] [PubMed] [Google Scholar]
- 123.Grimaldi KA, van Ommen B, Ordovas JM, Parnell LD, Mathers JC, Bendik I, et al. Proposed guidelines to evaluate scientific validity and evidence for genotype-based dietary advice. Genes Nutr. 2017;12:35. doi: 10.1186/s12263-017-0584-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Arkadianos I, Valdes AM, Marinos E, Florou A, Gill RD, Grimaldi KA. Improved weight management using genetic information to personalize a calorie controlled diet. Nutr J. 2007;6:29. doi: 10.1186/1475-2891-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Li SX, Ye Z, Whelan K, Truby H. The effect of communicating the genetic risk of cardiometabolic disorders on motivation and actual engagement in preventative lifestyle modification and clinical outcome: a systematic review and meta-analysis of randomised controlled trials. Br J Nutr. 2016;116:924–34. doi: 10.1017/S0007114516002488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dogan MV, Grumbach IM, Michaelson JJ, Philibert RA. Integrated genetic and epigenetic prediction of coronary heart disease in the Framingham Heart Study. PLoS ONE. 2018;13:e0190549. doi: 10.1371/journal.pone.0190549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Irvin MR, Zhi D, Aslibekyan S, Claas SA, Absher DM, Ordovas JM, et al. Genomics of post-prandial lipidomic phenotypes in the Genetics of Lipid lowering Drugs and Diet Network (GOLDN) study. PLoS ONE. 2014;9:e99509. doi: 10.1371/journal.pone.0099509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lai CQ, Smith CE, Parnell LD, Lee YC, Corella D, Hopkins P, et al. Epigenomics and metabolomics reveal the mechanism of the APOA2-saturated fat intake interaction affecting obesity. Am J Clin Nutr. 2018;108:188–200. doi: 10.1093/ajcn/nqy081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Perfilyev A, Dahlman I, Gillberg L, Rosqvist F, Iggman D, Volkov P, et al. Impact of polyunsaturated and saturated fat overfeeding on the DNA-methylation pattern in human adipose tissue: a randomized controlled trial. Am J Clin Nutr. 2017;105:991–1000. doi: 10.3945/ajcn.116.143164. [DOI] [PubMed] [Google Scholar]