Abstract
Challenges in the management of ocular pain are an underappreciated topic. Currently available therapeutics lack both efficacy and clear guidelines for their use, with many also possessing unacceptable side effects. Promising novel agents would offer analgesic, anti-inflammatory, and possibly neuroprotective actions; have favorable ocular safety profiles; and show potential in managing neuropathic pain. Growing evidence supports a link between the endocannabinoid system (ECS) and a range of physiological and disease processes, notably those involving inflammation and pain. Both preclinical and clinical data suggest analgesic and anti-inflammatory actions of cannabinoids and ECS-modifying drugs in chronic pain conditions, including those of neuropathic origin. This review will examine existing evidence for the anatomical and physiological basis of ocular pain, specifically, ocular surface disease and the development of chronic ocular pain. The mechanism of action, efficacy, and limitations of currently available treatments will be discussed, and current knowledge related to ECS-modulation of ocular pain and inflammatory disease will be summarized. A perspective will be provided on the future directions of ECS research in terms of developing cannabinoid therapeutics for ocular pain.
Keywords: endocannabinoids, inflammation, neuropathic pain, ocular
Introduction
The eye is a unique sensory organ comprised of both neural and non-neural tissues that facilitate vision through the collection and modification of light, followed by photoreceptor activation and subsequent neural transmission to vision centers of the brain. The anterior segment includes the highly innervated cornea, as well as the iris, lens and anterior chamber, the latter of which is filled with aqueous humor (Figure 1A). The posterior segment includes the retina, optic nerve, and the posterior chamber, which is filled with gel-like vitreous humor. The eye consists of an outermost fibrous sclera, covered by a thin membranous conjunctiva at its anterior aspect, with a vascular choroid layer below the sclera and superficial to the innermost retina—covering a large portion of the posterior chamber [1,2]. Six extraocular muscles act to delicately coordinate the voluntary and reflexive movements of the eye [3].
Figure 1. Overview of anterior ocular anatomy and corneal histology.
Anterior ocular anatomy (A), with histologic cross-section of the cornea (B) and confocal microscopy of the corneal endothelium (C). Figure used with permission from [4].
The blood–ocular barrier isolates the ocular environment from the systemic circulation, formed through both the blood–retina and blood–aqueous barriers [5]. The human cornea is avascular and thinnest centrally (0.5 mm), increasing in thickness peripherally [6]. Six layers comprise the cornea (Figure 1B), beginning with an outermost non-keratinized stratified squamous epithelium, below which lies a thin acellular layer (Bowman layer) followed by stroma that comprises 80–85% of the corneal thickness [6]. The corneal endothelium is in direct contact with the aqueous humor in the anterior chamber, representing the innermost layer of the cornea. Of note, the cornea is one of the most innervated tissues in the body [7], which imparts a unique sensitivity. In addition to the cornea’s ability to provide a refractive surface, and its barrier action, this sensitivity plays an important physiological role in tear film maintenance, where sensing evaporation triggers tear production [8]. Corneal innervation emanates from the nasociliary branch of the ophthalmic division of the trigeminal nerve that extends to a plexiform arrangement of nerves beneath the basal layer of the corneal epithelium [6]. The nature of this exposed and highly innervated system underlies the range of ocular pain pathologies.
Mechanisms of ocular pain
Ocular pain that originates at ocular sites in the periphery is transmitted to sensory and emotional centers of the brain, forming the perception of pain. Specifically, ocular innervation originates from the ophthalmic division of the trigeminal nerve (cranial nerve V), with up to 450 free nerve endings of trigeminal sensory neurons in the epithelium of the cornea [9]. Nociceptors are the ‘noxious receptors’ and respond to a range of stimuli, including mediators of inflammation such as Substance P (SP), acetylcholine, bradykinin, or prostaglandins [10]. Those nociceptors that respond to multiple types of noxious stimuli are designated ‘polymodal’ [11]. As reported by Belmonte et al. [12], primary afferent nerve fibers in the cornea are either polymodal (70% of primary afferents), cold receptors (10%), or mechanoreceptors (20%). Cold receptors respond to low temperatures and may be involved with sensation of tear film evaporation [8], whereas mechanoreceptors respond to mechanical stimulation.
There are two main types of afferent neuronal fibers of nociceptors: Aδ- and C-fibers. Aδ fibers are myelinated and responsible for the transmission of noxious stimuli that leads to the perception of pain that is acute and localized. C-fibers are unmyelinated and responsible for the transmission of noxious information that results in a slow and diffuse pain [13]. Both Aδ- and C-fibers are present in the human cornea [14], with the majority being polymodal nociceptors [7]. When a nociceptor receives a stimulus of sufficient magnitude to surpass its activation threshold, neuronal membrane depolarization occurs [15]. This nociceptor depolarization occurs via several voltage-gated ion channels (sodium, calcium, and potassium), in addition to purinergic P2X families, acid-sensing ion channels, and members of the transient receptor potential (TRP) family of cation channels [16]. With sufficient nociceptors activated, this membrane depolarization generates action potentials in the primary afferent neurons, which synapse with second order neurons in the trigeminal brainstem complex before being transmitted to the higher centers responsible for emotional (amygdala, prefrontal cortex, periaqueductal gray, and hypothalamus) and sensory-discriminative (posterior thalamus, parabrachial nucleus, and insular cortex) aspects of the perception of pain [11,15,17–21].
With regard to corneal innervation, the primary afferent fibers form bundles around the limbus, which leads to the generation of a limbal plexus [22]. As illustrated in Figure 2, both myelinated Aδ and the smaller diameter C-fibers originate from the subepithelial plexus (SEP) [23]. C-fibers extend anteriorly to the outermost layers of the corneal epithelium, while Aδ fibers branch dichotomously from the SEP, travelling anteriorly to Bowman’s membrane and then inferiorly to the basal epithelial cells [23].
Figure 2. Depiction of human corneal epithelial innervation.
Outlines stromal nerve bundles, including both Aδ and C-fibers, below Bowman’s layer in the SEP that enters the corneal epithelium via the basal lamina and forms the basal epithelial plexus, with Aδ fibers extending horizontally and C-fibers extending anteriorly. Figure used with permission from [23].
Several key receptors present in corneal tissues contribute to the generation of pain signals. The TRP family of receptors, with notable members TRP vanilloid 1 (TRPV1) and TRP melastatin 8 (TRPM8), are cation channels present in the cornea that are implicated in sensory neurotransmission [24–32]. TRPM8, the so-called ‘cold receptor’, is the main receptor associated with cold somatosensation (temperatures < 25°C) but is also activated by menthol, icilin, and acetone [32–34]. Further, TRPM8 is proposed to play a physiological role in the sensation of tear film evaporation [8]. TRPV1 is the capsaicin-receptor, also activated by decreases in pH, temperatures above 43°C [35], a range of chemicals, hyperosmolarity, and mechanical stretch [36]. TRPV1 is known to modulate nociception, mediate innate immune responses and inflammation, as well as wound healing [37]. The activation of TRPV1 on nociceptive neurons leads to the generation of action potentials in addition to triggering the release of pain-inciting neuropeptides and inflammatory mediators [38]. In addition to the presence of TRPV1 throughout the human cornea (epithelial, stromal, and endothelial tissue) [29], TRPV1 is found on a range of peripheral nerve terminals as well as in the CNS [36]. Activation of TRPV1 through cross-talk with the cannabinoid 1 receptor (CB1R) has been reported, [30,39] and will be discussed in greater detail later in this review.
Other mediators of ocular pain include the vasoactive neuropeptides calcitonin gene-related peptide (CGRP) and SP, both known to modulate neurogenic inflammation in the eye [24,40,41]. SP and CGRP have been detected in sensory neurons in the cornea [9,24,42–46], and, following their release from activated nociceptive C-fibers [7,47], are associated with the transmission of pain, in addition to their pro-inflammatory actions [48,49]. As reported by Murata et al. [24], 37% of rat corneal neuronal somata in the ophthalmic division of the trigeminal nerve are TRPV1 positive (detected via immunofluorescence), with one third of these co-expressing substance P and the remainder co-expressing CGRP.
Ocular disease and ocular pain
Pain is defined by the International Association for the Study of Pain as an ‘unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ [50]. Ocular pain has both diverse presentations and etiologies, with the potential to drastically alter quality of life, particularly when chronic [51]. Further, the management of chronic ocular pain can be challenging due to its complex origins, as well as the limitations of currently available therapies [52].
A range of pathologies can lead to acute or chronic ocular pain, which contributes to the marked burden of the condition. These include traumatic injury to the tissues of the eye or higher order nerves, infections (e.g. infectious keratitis or endophthalmitis), inflammatory conditions (such as uveitis), or iatrogenic causes (damage from surgery or infection secondary to invasive procedures) [20,53]. Systemic autoimmune disease such as diabetes can result in the development of chronic neuropathic pain [8,53].
Neuropathic pain results from central and/or peripheral nerve damage or sensitization. Patients with neuropathic pain may experience spontaneous pain, pain in response to a stimulus that does not normally elicit pain (i.e. allodynia), or an increased pain response resulting from a stimulus that normally elicits pain (i.e. hyperalgesia) [54,55]. In neuropathic pain syndrome, both an increased level of afferent nerve firing and an abnormal response to afferent stimuli are observed [56]. Spontaneous pain can originate from injured areas along the length of the nerve, such as nerve terminals or the dorsal root ganglion (DRG) [57], in addition to potentially originating from undamaged surrounding nerves that are activated via ‘cross-talk’ with damaged nerves [58].
Regarding the anterior ocular surface, trauma to the cornea (surgery, abrasions, foreign bodies, chemical burns etc.) or infections such as herpes simplex virus (HSV) keratitis can lead to nerve damage, with resultant pain. Conditions of the posterior segment, such as scleritis or idiopathic orbital inflammation, can lead to deep ocular pain that may be severe [59]. Also relating to the posterior segment, optic neuritis, characterized by inflammation of the optic nerve, may be painful (particularly with eye movement) [60].
Dry eye disease (DED) is among the most common ocular diseases [61] and is associated with chronic dry eye-like pain (DELP). Several comprehensive reviews discuss the relation between DED and DELP in detail, such as Rosenthal et al. and Galor et al. [8,62]. Under normal physiologic conditions, the corneal surface is covered by a thin tear film, composed of a mucinous layer that originates from goblet cells in the conjunctiva, an aqueous layer superficial to the mucinous layer, and an outermost lipid layer [6]. The tear film plays a key barrier role and through the interface generated with the cornea, contributes significantly to ocular refractive power [6]. It is interesting that decreases in the parameters of tear production are not well associated with DELP [8,63,64]. Similarly, there is not a strong association between disorders of the meibomian glands and DELP—where meibomian glands normally supply the lipid component of the tear film [8,52]. Further, DELP exhibits characteristics of neuropathic sensitization of the cornea [8]. Several studies have suggested that TRPM8 receptors on the ocular surface are involved in sensing tear evaporation [65,66], suggesting an intricate role of TRPM8 in the physiological maintenance of a tear film. Significantly decreased tear production has been observed in TRPM8 knockout (Trpm8−/−) mice [65]. Through recording nerve terminal impulse activity in the mouse eye, this group additionally identified loss of cold responsiveness in TRPM8 knockouts.
Inflammatory pain is a form of nociceptive pain. The process of inflammation can, however, itself lead to the development of neuropathic pain [67–71]. This inflammatory neuronal damage can occur directly, such as in autoimmune neuropathy, or indirectly, such as from nerve compression, which may result in ischemic nerve injury. Neural sensitization and lowered pain thresholds occur with tissue damage, resulting in the release of a range of inflammatory mediators such as cytokines, bradykinin, SP and prostaglandins, which further contribute to neuronal sensitivity [56]. Ocular inflammation is a double-edged sword in that it plays a key role in antimicrobial defenses and wound healing, yet at the same time can be central in pathological processes that pose a threat to vision. The eye is uniquely isolated from the systemic immune system (‘immune-privileged’) via various barriers (physical, immunosuppressive factors, and active immune modulation) [72,73], which confers protection from the potentially damaging effects of immune infiltration [74]. At the same time, dendritic cells and resident macrophages in various ocular tissues, such as the cornea and choroid, act as sentinels of the innate immune system (an initial non-specific response) [75,76].
Current therapies for ocular pain and limitations
Commonly used topical agents in the management of ocular pain include anesthetics, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroids [77–79]. Neuropathic pain is treated with systemic agents aimed at modulating pain-signaling pathways, in order to increase nociceptor pain thresholds and decrease signaling. These include the gabapentinoids (‘GABAergics’), tricyclic antidepressants, and opioids [53]. Acute pain treatment is often initiated alongside disease-specific treatments, such as surgical management or antibiotics. Current pharmacological options for the treatment of neuropathic pain fall short due to inadequate efficacy and/or unacceptable side effects [80,81].
Topical ocular anesthetics (such as tetracaine or proparacaine) are sodium channel blockers, widely used in clinical practice, and can result in immediate and complete alleviation of pain that originates from the ocular surface. This efficacy is, however, contrasted by limits on duration of use, where continued application is well documented to lead to corneal melt [82]—an ulcerative process associated with breakdown of corneal epithelium and stroma [77].
Corticosteroids (such as prednisolone or dexamethasone) act as potent anti-inflammatory agents, through up-regulation of anti-inflammatory protein transcription and blockade of the translocation of pro-inflammatory transcription factors. Topical steroids remain key tools in decreasing ocular inflammation, which can be vision-saving [83]; however, their extended use is associated with significant side effects including cataract, glaucoma, delayed ocular healing, or secondary infections resulting from ocular immunosuppression [84]. Systemic steroids or other immunosuppressive agents are used in addition to NSAIDs in severe inflammatory conditions such as scleritis [85].
NSAIDs inhibit cyclooxygenase enzymes (COX-1 and COX-2), preventing the formation of certain eicosanoids, notably prostaglandins—which are inflammatory and nociceptive [86,87]. Topical ocular NSAIDs (such as nepafenac or ketorolac) are generally associated with a less significant toxicity profile than are corticosteroids [77]. There remain, however, concerns relating to ocular NSAID safety, particularly in the context of long-term use. The ocular toxicity of NSAIDs is associated with delayed healing [88] and ranges from epithelial erosion and corneal thinning, to corneal melt [77]. Systemic NSAIDs such as ibuprofen or naproxen are associated with inhibition of COX-1 mediated gastroprotective actions, resulting in increased risk of gastric ulceration and bleeds, in addition to increased cardiovascular risks and nephrotoxicity [89–91]. Topical and systemic NSAIDs are generally not considered to be options for the treatment of neuropathic pain. Acetaminophen, which acts differently than do NSAIDs, may play a limited role in pain management, particularly as an adjunctive agent, potentially acting through peripheral and central COX inhibition, in addition to central mechanisms including modulation of descending serotonergic pathways and ECS modulation [92].
Neuropathic pain generally requires systemic pain-modulating strategies, usually beginning with gabapentinoid agents (e.g. pregabalin, gabapentin) or certain antidepressants—namely the tricyclic antidepressants (TCAs) (e.g. amitriptyline, nortriptyline) or serotonin norepinephrine reuptake inhibitors (SNRIs) (e.g. venlafaxine, duloxetine) as first-line agents [93]. Second-line agents include tramadol—a weak opioid agonist and SNRI, and classical opioid receptor agonists (e.g. hydromorphone, fentanyl). The mechanisms of the gabapentinoids in neuropathic pain are not well defined; however, their blockade of voltage-gated calcium channels (VGCCs) on primary afferent neurons is believed to play a central role [94,95], which appears to be in-line with up-regulation of a specific VGCC subunit (α2δ) in the setting of nerve injury [96]. Use of a combination of these agents may achieve only moderate reductions in pain, and may carry a heavy side-effect burden, such as dizziness and somnolence for gabapentinoids, weight gain, daytime sedation and other anticholinergic effects for TCAs, or constipation, nausea, sweating and potential for clinically significant respiratory depression with the use of opioids [93].
The use of systemic cannabinoids is promising in managing chronic non-cancer pain, particularly when neuropathic in nature [97,98]. Cannabinoid-mediated analgesia arises from a range of peripheral and central mechanisms, including through modulation of descending inhibitory pain pathways, central neuronal modulation, neuroprotective mechanisms, and inhibition of prostaglandin synthesis [99]. Evidence supporting use of systemic cannabinoids for pain is reflected by their incorporation into the Canadian Pain Society guidelines as third line agents for chronic neuropathic pain [93]. There is, however, a clear need for further large-scale controlled clinical trials in order to establish both safety and efficacy of systemic cannabinoids [100–103]. With respect to the ocular use of cannabinoids and small molecular drugs that target the ECS, several recent studies have indicated that ECS-modifying drugs may be useful in the treatment of both ocular pain and inflammation, with options for local ocular delivery offering advantages over systemic cannabinoids, such as decreased systemic bioavailability and potentially improved target-site concentrations. The following sections will review current knowledge of the ECS, the presence of components of the ECS in the eye, and existing evidence for ECS modulation of ocular pain.
Overview of the endocannabinoid system
The ECS is a complex biological regulatory system, conserved among vertebrates, which regulates both systemic and CNS functions that include immune response, pain, neuronal activity, in addition to metabolic and cardiovascular functions [104–109]. Growing evidence also suggests that the ECS plays an important role in a range of disease processes [110]. The characterization of an endogenous cannabinoid system stemmed from the isolation of the psychoactive cannabinoid, THC (Δ9-tetrahydrocannabinol), from cannabis in 1964 by Gaioni and Mechoulam [111]. Identification of THC and the synthesis of synthetic cannabinoid ligands heralded the discovery and cloning of receptors for cannabinoids and facilitated identification of endogenous ligands. The two main endogenous bioactive lipids of the ECS, termed endocannabinoids, are anadamide (AEA) [112] and 2-arachidonoylglycerol (2-AG) [113]. Together with their respective biosynthetic and degradative enzymes, endocannabinoids and cannabinoid receptors constitute the ECS (Figure 1) [114].
The cannabinoid receptors include the CB1R—found in the CNS and ubiquitously expressed in systemic organs and tissues, and the cannabinoid type 2 receptor (CB2R)—highly localized to cells of the immune system. The first discovered cannabinoid receptor, CB1R, was cloned from rat brain cDNA in 1990 [115], and subsequent identification of CB2R was based on sequence homology with CB1R (44% amino acid homology is shared) [116]. Both CB1R and CB2R are G-protein coupled receptors (GPCRs), activated endogenously by endocannabinoids, the most well documented of which are AEA and 2-AG [117,118]. The endocannabinoids also bind to non-cannabinoid receptors, including TRPV1, G-protein coupled receptor 55 (GPR55) (Figure 1), GPR18 and peroxisome proliferator-activated receptors α, β/δ, and γ [119]. All tissues of the body, which have been examined to date, contain endocannabinoids [120].
Endocannabinoids are generated ‘on-demand’ via enzymatic catabolism of membrane lipids [121] (Figure 3). Specifically, AEA is formed through the enzymatic action of phospholipase D (NAPE-PLD) on phospholipid N-arachidonoyl phospahtidylethanolamine (NAPE) [120–122]. Synthesis of 2-AG begins with the generation of 1,2-diacylglycerol (DAG) via phospholipase C, where DAG is then converted to 2-AG via 1,2-diacylglycerol lipase (DAG lipase) [120,123,124]. Degradation of endocannabinoids also occurs through enzymatic action, and the localization of specific degradative enzymes dictates the duration of action of endocannabinoids (Figure 4) [108,120,125]. AEA is converted via hydrolysis to arachidonic acid and ethanolamine by the enzyme fatty acid amyl hydrolase (FAAH), and 2-AG is converted via hydrolysis to arachidonic acid and glycerol through the actions of monoacylglycerol (MAGL), and to a lesser extent α–β hydrolase domain protein 6 (ABHD-6) and ABHD-12 [120,126–130]. Both 2-AG and AEA act as substrates for arachidonic acid-metabolizing enzymes such as lipoxygenase enzyme subtypes or COX-2, where AEA also acts as a substrate for certain cytochrome P450 oxidase enzymes [131].
Figure 3. Overview of the ECS.
Highlights key endocannabinoids, cannabinoid receptors, and biosynthetic and degradative enzymes. NAPE: N-acyl-phosphatidylethanolamine; NAPE-PLD: N-acyl-phosphatidylethanolamine-specific phospholipase D; 2-AG: 2-arachidonoylglycerol; DAG: diacylglycerol; DAGL: diacylglycerol lipase; EMT: endocannabinoid membrane transporter – ? is to denote controversy surrounding the characterization of an EMT [132–137]. TRPV1: transient receptor potential cation channel subfamily V member 1; CB1: cannabinoid receptor 1; CB2: cannabinoid receptor 2; GPR55: G protein-coupled receptor 55; FAAH: fatty acid amide hydrolase; MAGL: monoacylglycerol lipase. Figure modified with permission from [114].
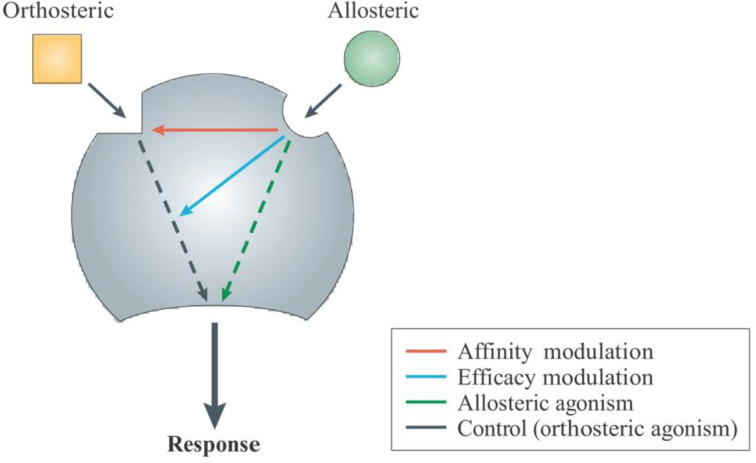
Figure 4. Mechanistic summary of allosteric receptor modulation.
Figure used with permissions from [138].
The well-known psychoactive actions of the cannabis plant arise largely from THC-mediated activation of CNS CB1Rs, which are coupled to Gαi protein-signaling pathways including adenylyl cyclase (AC), mitogen-activated protein kinase (MAPK), and cyclic adenosine monophosphate (cAMP) [108,118]. CB1R activation results in decreased synaptic neurotransmitter release mediated through presynaptic voltage-gated Ca2+ channel-inhibition [121]. The presence of CB2R on immune cells spans various populations, listed here in order of descending levels of receptor expression: natural killer cells, monocytes, polymorphonuclear leukocytes, and CD4+ and CD8+ lymphocytes [139]. In addition to expression on immune cells of the periphery, CB2R is also found in the CNS on microglia cells, glia and some neurons [140,141]. Activation of CB2R is not associated with CB1R-like behavioral effects, but in common with CB1R, activation of CB2R is associated with Gαi protein-coupled signaling pathways, inhibition of AC and decreases in cAMP levels as well as activation of MAPK pathways [108,117,142,143]. Growing evidence links CB2R activation with anti-inflammatory actions [108,144–148]. Further, increased levels of both endocannabinoids and CB2R expression have been observed in the setting of injury, indicative of the receptor’s involvement in endogenous protective mechanisms [149,150].
Ocular ECS and potential for modulation
No ECS-modulating agents are currently approved for ocular use. There is, however, a growing body of evidence indicating potential for ECS-modulation in the treatment of a range of ocular conditions. Both CB1R and CB2R have been identified in various tissues of the human eye, including the cornea (CB1R) [151], ciliary body and ciliary process, trabecular meshwork, retina, and iris [151–153] as well as in immune cells present in ocular tissues (CB2R) [139,154–157]. Both endocannabinoids (2-AG and AEA) and the enzymes involved in their synthesis and degradation have been identified in various tissues in human eyes, including the cornea, iris, retina, choroid, and ciliary body [157,158–165].
CB1R is of interest as an analgesic strategy, and the activation of CB2R is of particular interest in terms of its anti-inflammatory effects [108]. Alternate ECS-modulation strategies, such as allosteric modulation [166–170] or degradative enzyme inhibitors [171] may additionally be valuable in achieving site-specific cannabinoid actions and/or serve to elicit cannabinoid receptor effects while minimizing the side-effects that are associated with chronic administration of potent orthosteric agonists (i.e. the generation of tachyphylaxis) [157,164]. Ocular ECS-modulation is a promising potential target for a number of painful ocular diseases, and the development of appropriate preclinical models will be an important next step in assessing safety and efficacy of cannabinoids for ocular disease, particularly in terms of their long-term use.
ECS actions on ocular inflammation
Inflammation in the eye can lead to acute or chronic pain, the development of neuropathy, or contribute to vision loss [20,21]. A range of leukocyte populations express CB2Rs and studies in animal models have generated promising data, which indicates anti-inflammatory effects of CB2R-activation [144,146,147]. Though significant levels of CB2R have not been detected in corneal tissue under physiological conditions [172], CB2R-modulation is a promising target for corneal disease as the immune cells that express CB2R are recruited to the eye during ocular inflammation. Additionally, up-regulation of CB2R on resident immune cells and glia after injury may also be relevant for development of CB2R-selective drugs [173].
A commonly used animal model of ocular inflammation involves intraocular administration of endotoxin (lipopolysaccharide, LPS), termed endotoxin-induced uveitis (EIU). Administration of LPS results in an innate immune-mediated pan-ocular inflammation that mimics pathophysiological characteristics of anterior uveitis, an inflammatory condition of the uvea (encompassing the iris, ciliary body, and choroid), which is accompanied by pain and photophobia [146,147,174]. An EIU study examining cytokine and chemokine levels, as well as leukocyte–endothelial adherence in the microvasculature of the rat iris, as parameters of inflammation, compared ocular topical treatment with a CB2R-selective cannabinoid agonist to topical NSAID (nepafenac) and corticosteroids (prednisolone and dexamethasone) [146]. The CB2R-agonist resulted in decreased parameters of inflammation at 6 h, where, interestingly, similar anti-inflammatory actions were not observed with NSAID or corticosteroids. It is also noteworthy that CB1R activation may not be advantageous during EIU, as suggested by one study in rabbits that found AEA-induced increases in parameters of ocular inflammation and damage, which were attenuated with CB1R blockade (via AM251) [175].
Experimental autoimmune uveoretinitis is an antibody/adjuvant-triggered adaptive immune-mediated inflammation that induces pathological changes in-line with uveoretinitis [73,144]. Using this model, a selective CB2R-agonist (JWH 133) was found to suppress the disease progression and led to several immunosuppressive actions, including decreased cytokine/chemokine production, as well as decreased leukocyte rolling and infiltration in vasculature of the inflamed retina when delivered systemically [144]. The authors propose that these effects may result from CB2R-mediated inhibition of autoreactive T-cell activation, in addition to effects on leukocyte recruitment.
A recent study by Szczesniak et al. demonstrated anti-inflammatory actions of cannabinoids in proliferative vitreoretinopathy (PVR), an inflammatory condition that develops secondary to ocular trauma, or iatrogenic causes—commonly procedures used to correct retinal detachment [176,179]. In a mouse PVR model using intravitreal (IVT) dispase (to cleave the retinal basement membrane), treatment with a cannabidiol (CBD) analog, HU308, which selectively activates CB2R [177,178], led to decreased parameters of inflammation and improved histopathology [179]. This study by Szczesniak et al. found worsened histopathology and increased parameters of inflammation with CB2R-knockout or pharmacological blockade of CB2R (via AM630), indicating a tissue-protective and anti-inflammatory role of CB2R. Further, beneficial effects of HU308 (anti-inflammatory and improved histopathology) were absent when HU308 was administered to mice pretreated with a CB2R antagonist (AM630), indicating these actions of HU308 were CB2R-mediated.
ECS actions on ocular pain
There are limited yet promising lines of evidence indicating the potential for ECS-modulation in the management of ocular pain. A study in rats that elicited ocular pain (via ocular surface administration of mustard oil or a CO2 gas puff) found decreased neuronal activity of those corneal nerves that synapse in a specific medullary transition region, the trigeminal interpolaris/caudalis (Vi/Vc) following treatment with a non-selective CB1R/CB2R agonist (WIN55212-2) [180]. The authors related this action to the Vi/Vc’s role in corneal reflexes and anterior eye homeostasis.
Recently published data in a mouse model of corneal hyperalgesia found that three topically applied cannabinoids (Δ8THC, CBD, and HU-308) decreased corneal inflammation and corneal hyperalgesia, as determined by the evaluation of corneal neutrophil infiltration and behavioral testing, respectively [181]. All tested cannabinoids had both analgesic and anti-inflammatory actions in wild-type mice, with a CB1R-antagonist, AM251, blocking both the analgesic and anti-inflammatory effects of Δ8THC, suggesting that the effects of Δ8THC are mediated by CB1R activation [181]. The actions of the phytocannabinoid, CBD, however, did not result from CB1R or CB2R modulation (confirmed using AM251 and CB2R-knockout mice). Interestingly, concurrent administration of a 5-hydroxytryptamine subtype 1a (5-HT1A) receptor antagonist (WAY100635) ablated the effects of CBD. Both the analgesic and anti-inflammatory actions of the CB2-selective CBD analog, HU308, were absent in CB2R-knockout mice, supporting contributions of CB2R-mediated corneal anti-inflammatory and antinociceptive effects in this model [181].
The ocular actions of cannabinoids may involve non-cannabinoid receptors, as seen with potential CBD anti-inflammatory and analgesic actions that are mediated through 5-HT1A [181]. Further, the TRPV1 receptor has been found to co-localize with CB1R in both mouse corneal epithelium as well as human corneal epithelial cells, implying that CB1R may play an important role in modulating corneal TRPV1 activity [27,30]. Yang et al. [30] further identified reductions in both inflammatory infiltration of the corneal stroma and scarring in an injury model, following treatment with WIN55212-2. The authors proposed that these actions were through CB1R–TRPV1 interactions and involved TRPV1 receptor desensitization. Similarly, findings were reported by McDowell et al. [182] in rat DRG neurons where sensitization of TRPV1 (via nerve growth factor) was inhibited by CB1R-activation (via arachidonoyl-2’-chloroethylamide). Understanding the interaction between CB1R with TRPV1 may be valuable in developing therapeutics for ocular pain, as both receptors are present in ocular tissues and involved in ocular pain transmission.
Novel approaches to modulate the ocular ECS: cannabinoid receptor allosteric modulation and enzyme-inhibitors as indirect ECS agonists
As reviewed by Cairns et al., the potential for ECS modulation by exogenous endocannabinoids maybe limited due to their short duration of action [164,183,184]. In addition, ligands that bind to the orthosteric site in order to activate cannabinoid receptors are associated with psychoactive effects (via CB1R), dependence, and the development of tachyphylaxis when administered repeatedly [166,169,170,185]. Together, these underline the need for further exploration of novel ECS-modulatory strategies, including the use of allosteric ligands or enzyme inhibitors.
Figure 4 illustrates allosteric ligand modulation of receptors. Through binding ‘allosteric’ sites on the receptor—sites distinct from the orthosteric site, allosteric ligands can increase (positive allosteric modulators, PAMs) or decrease (negative allosteric modulators, NAMs) a receptor’s interaction with orthosteric agonists, thus altering ligand affinity, efficacy, potency, and/or dissociation [167,168,138]. In addition to PAMs and NAMs, there are ‘neutral’ allosteric ligands, which compete with ligands for allosteric site binding while not eliciting effects on response to orthosteric site ligand binding [167,168,138]. Cumulative evidence indicates multiple allosteric sites on GPCRs, which expands the range of modulatory strategies [168,169].
Allosteric ligands have several unique properties that contribute to their potential clinical utility. One such property is the tendency of allosteric sites to be more distinct from one another (via demonstrating less conservation between receptor subtypes) than are orthosteric sites [167,170]. This has been demonstrated for CB1R, where allosteric sites are believed to be located in variable regions [186–188], as compared with orthosteric site(s) found in more conserved regions [170,189–191]. Congrève et al. [168] suggest that an evolutionary pressure toward conservation of orthosteric sites, for the preservation of endogenous ligand signaling, is likely responsible and absent in the case of allosteric sites. This may lead to less off-target side effects from allosteric ligands compared with orthosteric ligands [192].
Biased ligands are able to elicit a shift toward a receptor conformation that favors specific signaling pathways [169]. Although biased signaling is not unique to allosteric ligands, this, along with the distinct nature of allosteric sites provides opportunities to develop novel therapeutics with improved specificity and reduced side effects [169,193–197]. Allosteric modulation of cannabinoid receptors is a complex and novel area for discovery. Illustrating this complexity is data indicating a range of possible outcomes of modulation. Studies have demonstrated the ability of allosteric modulators to possess both PAM and NAM actions. An example of this is with an allosteric modulator possessing PAM activity for CB1R orthosteric agonist binding, with concurrent NAM activity on CB1R-mediated inhibition of cAMP [169,198,199].
Tachyphylaxis represents an adaptive mechanism, characterized at the cellular level for cannabinoids by cannabinoid receptor desensitization and down-regulation, which, along with CB1R-mediated psychotropic actions, limits the clinical applications of CB1R orthosteric agonists [200]. Allosteric modulators have the potential to increase cannabinoid receptor activity without contributing to desensitization [164,166]. Novel strategies include allosteric modulation of endogenous endocannabinoid binding, and PAM-mediated potentiation of sub-threshold levels of exogenous agonists. With respect to CB1R, these strategies may reduce the development of tachyphylaxis following repeat cannabinoid receptor agonist treatment [201]. This likely has significant potential in developing novel ECS-modulating strategies, particularly for frequent and/or long-term use, such as in uveitis, glaucoma, or chronic ocular pain conditions. In support of this approach, a recent publication by Cairns et al. reported that topical application of a novel CB1R allosteric modulator, GAT229 [202], was able to reduce intraocular pressure (IOP) in a mouse model of glaucoma. Additionally, when combined with a CB1R agonist, WIN55212-2, at a subthreshold dose for reducing IOP, GAT229 was able to increase the efficacy and duration of action for WIN55212-2’s ocular hypotensive actions [203].
A second novel approach to ECS-modulation is through the inhibition of mechanisms by which endocannabinoid action is terminated. Enzyme inhibitors exert cannabimimetic actions through inhibiting the degradative enzymes responsible for endocannabinoid hydrolysis (predominant mechanism) or oxygenation [171,204]. As with allosteric modulators, an enzyme inhibitor strategy may result in site-specific effects. This is likely a result of increased endocannabinoid synthesis at the site of tissue injury [205]. Generally, endocannabinoids are short-lived, undergoing both rapid enzymatic degradation and uptake from the extracellular space [171,206,207]. Potential enzyme inhibitors may target FAAH, increasing the levels of AEA, and/or MAGL, ABHD-6, and ABHD-12—to increase the levels of 2-AG [171]. Toczek et al. [171] provide a comprehensive review of the ECS enzyme inhibitors examined in preclinical studies and clinical trials.
To date, endocannabinoid enzyme inhibitors have not been examined in the context of ocular pain and inflammation. That being said, there is considerable data indicating that they possess analgesic actions in neuropathic pain models [171]. The most work to-date has focused on FAAH inhibition and indicates the antinociceptive [208–213], neuroprotective [214,215] and analgesic actions [216] including in inflammatory pain models [217,218].
It is interesting that a peripherally restricted FAAH inhibitor, URB937, was shown to be antinociceptive in both inflammatory and peripheral nerve injury pain models, with both effects lost through CB1R blockade [219]. As suggested by the authors, these results indicate peripheral AEA actions via CB1R, which prevent signal transmission to higher centers in the CNS. This peripherally restricted FAAH inhibitor has been further shown to possess antinociceptive action in a migraine model (via systemic nitroglycerin) in rats [220]. There remains, however, a level of complexity to the effects of FAAH in pain. Carey et al. identified a pro-nociceptive phenotype (nocifensive behavior and hypersensitivities to mechanical and heat stimuli) with capsaicin challenge in mice with genetic knockout of FAAH, while the mice concurrently demonstrated an analgesic phenotype in response to models of inflammatory nociception [221]. Both TRPV1- and CB1R-antagonists ablated this pro-nociceptive phenotype, and the authors acknowledged the gaps in knowledge surrounding the range of active lipid signaling molecules that are metabolized by FAAH, with these data suggesting potential limitations of FAAH inhibition based on pain type [221]. Further, it is of value to acknowledge that attempts to examine systemic FAAH-inhibition in the setting of chronic pain have generated conflicting findings [222,223], including a drug candidate (PF-04457845, Pfizer) that was dropped after clearing Phase II clinical trials due to poor efficacy [224]. Several new FAAH inhibitors with improved efficacy are in development; however, this development was placed on hold pending an investigation of the pharmaceutical company Bial’s agent, 10-2474, which led to the development of severe neurological disorders during a phase I clinical trial in 5 of 6 subjects, with 1 death [225]. This complication is, however, suggested to have resulted from off-target and non-ECS related actions [226].
Enzyme inhibitors targeting MAGL have also generated promising data; however, these inhibitors have been associated with behavioral effects indicative of CB1R activation in the CNS [227]. While FAAH inhibitors have been reported to generate analgesia in preclinical models, these drugs, unlike MAGL inhibitors, have not generally been associated with behavioral effects [228,229]. These differences between FAAH- and MAGL- inhibitor action may in part be due to the full versus partial agonist actions of 2-AG and AEA, respectively [230].
JZL184 acts as a MAGL-specific inhibitor [229], which allows differentiation from FAAH-inhibition mediated effects [231], and has been shown to produce analgesia in various pain assays [229,232–237]. In a mouse model of orofacial neuropathic pain, induced via injury of the inferior orbital nerve, JZL184 reduced pain (increased threshold to mechanical stimulation) 2 h following administration [231].
Another MAGL-selective inhibitor, KML29, has reported anti-inflammatory and antinociceptive action [238]. Crowe et al. assessed low-dose KML29 in combination with a low-dose of the established neuropathic pain agent, gabapentin, in a mouse model of neuropathic pain (chronic constriction injury) [239]. The authors highlight this strategy as a method to limit side effect profiles of the individual agents, finding that treatment resulted in additive attenuation of mechanical allodynia (reduced with CB1R antagonist treatment) and synergistic reduction of cold allodynia (no effect with CB1R blockade) [239]. Along a similar line of investigation, Crowe et al. [240] assessed the combination of the NSAID diclofenac with JZL184, finding additive attenuation of cold allodynia, as well as synergistic reduction of mechanical allodynia, which was blocked with CB1R antagonist treatment. Also examining KLM29, Miller et al. [241] observed an ocular hypotensive effect in a mouse model, while JZL184 did not have an effect on IOP.
While endocannabinoid enzyme inhibitors have not been specifically examined in models of ocular inflammation and pain, Slusar et al. [214] examined the effect of FAAH inhibition with URB567 on the survival of retinal ganglion cells (RGCs), in a rat optic nerve axotomy model. The study demonstrated an increased survival of RGCs with URB597 treatment, an effect ablated following CB1R but not CB2R antagonist treatment. This group also identified significant increases in retinal AEA and decreased AEA metabolite levels following URB597 treatment.
Creative approaches to ECS modulation in the treatment of ocular pain and inflammation offer unique advantages over exogenous orthosteric modulation. A significant body of research indicates analgesic and antinociceptive actions of enzyme inhibitors, including of FAAH and MAGL, in neuropathic and other pain models. The actions of enzyme inhibitors specifically in the setting of ocular pathology have demonstrated promising data indicating neuroprotective and IOP-lowering actions, although examination of selective endocannabinoid enzyme inhibitors in relevant animal models of ocular inflammation and pain is now required in order to fully access the utility of this class of ECS-modulators. As the cellular uptake of endocannabinoids plays a role in termination of action, strategies to inhibit this process may also be valuable when attempting to prolong endocannabinoid action.
Conclusion
There is a definite need for novel pharmacological approaches to the management of ocular pain. In particular, ocular neuropathic pain is difficult to manage and may originate from non-ocular sites in the periphery and/or centrally. The ECS is present ubiquitously through the body, including a range of ocular tissues, and represents a promising target in the treatment of several physiological and pathophysiologic processes in the eye including, but not limited to, pain, inflammation, and neuronal damage. Modulating CB2R has immunomodulatory potential, whereas the activation of CB1R appears to contribute to both centrally and peripherally mediated analgesia. Novel drug strategies, namely the use of cannabinoid receptor allosteric modulators, biased ligands or through the inhibition of enzymes that degrade endocannabinoids, may be valuable targets in developing drugs that circumvent the limitations of orthosteric agonists at the cannabinoid receptors. Furthermore, ocular topical or regional administration of cannabinoids is a promising strategy for delivery. For cannabinoids administered via systemic or topical/regional routes alike, safety and efficacy must be further examined, particularly in the context of long-term use.
Acknowledgements
The authors would like to thank Dr Anna-Maria Szczesniak for her assistance editing this review, as well as Dinesh Thapa for his assistance with photo editing software.
Abbreviations
- 2-AG
2-arachidonoylglycerol
- 5-HT1A
5-hydroxytryptamine receptor 1A
- ABHD
α–β hydrolase domain
- AC
adenylyl cyclase
- AEA
anadamide
- cAMP
cyclic adenosine monophosphate
- CB1R
cannabinoid 1 receptor
- CB2R
cannabinoid 2 receptor
- cDNA
complementary deoxyribonucleic acid
- CGRP
calcitonin gene related peptide
- CNS
central nervous system
- COX-1 and -2
cyclooxygenase 1 and cyclooxygenase 2
- DAG
diacylglycerol
- DAGL
diacylglycerol lipase
- DED
dry eye disease
- DELP
dry eye-like pain
- DRG
dorsal root ganglion
- ECS
endocannabinoid system
- EIU
endotoxin-induced uveitis
- EMT
endocannabinoid membrane transporter
- FAAH
fatty acid amide hydrolase
- GPCR
G protein-coupled receptor
- GPR55
G protein-coupled receptor 55
- HSV
herpes simplex virus
- IOP
intraocular pressure
- LPS
lipopolysaccharide
- MAGL
monoacylglycerol lipase
- MAPK
mitogen-activated protein kinase
- NAM
negative allosteric modulator
- NAPE
N-acyl-phosphatidylethanolamine
- NAPE-PLD
N-acyl-phosphatidylethanolamine-specific phospholipase D
- NSAID
non-steroidal anti-inflammatory drug
- PAM
positive allosteric modulator
- PVR
proliferative vitreoretinopathy
- RGC
retinal ganglion cell
- SEP
subepithelial plexus
- SNRI
serotonin norepinephrine reuptake inhibitor
- SP
substance P
- TCA
tricyclic antidepressant
- THC
tetrahydrocannabinol
- TRP
transient receptor potential
- TRPV1
transient receptor potential vanilloid 1
- TRPM8
transient receptor potential melastatin 8
- VGCC
voltage-gated calcium channel
- Vi/Vc
trigeminal interpolaris/caudalis
Author Contribution
M.E.M.K. contributed to writing and edited the review. J.D.L. wrote the majority of the review.
Competing Interests
Melanie Kelly is a director and the Chief Scientific Officer of Panag Pharma, Halifax, NS. Melanie Kelly holds patent WO2015/074137.
Funding
The authors declare that there are no sources of funding to be acknowledged.
References
- 1.Kiel J.W. (2010) Anatomy. In: The Ocular Circulation, Morgan & Claypool Life Sciences, San Rafael (CA) [PubMed] [Google Scholar]
- 2.Kels B.D., Grzybowski A. and Grant-Kels J.M. (2015) Human ocular anatomy. Clin. Dermatol. 33, 140–146 10.1016/j.clindermatol.2014.10.006 [DOI] [PubMed] [Google Scholar]
- 3.Spencer R.F. and Porter J.D. (2006) Biological organization of the extraocular muscles. Prog. Brain Res. 151, 43–80 10.1016/S0079-6123(05)51002-1 [DOI] [PubMed] [Google Scholar]
- 4.Navaratnam J., Utheim T.P., Rajasekhar V.K. and Shahdadfar A. (2015) Substrates for expansion of corneal endothelial cells towards bioengineering of human corneal endothelium. J. Funct. Biomater. 6, 917–945 10.3390/jfb6030917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunha-Vaz J., Bernardes R. and Lobo C. (2011) Blood-retinal barrier. Eur. J. Ophthalmol. 21, S3–S9 10.5301/EJO.2010.6049 [DOI] [PubMed] [Google Scholar]
- 6.DelMonte D.W. and Kim T. (2011) Anatomy and physiology of the cornea. J. Cataract Refract. Surg. 37, 588–598 10.1016/j.jcrs.2010.12.037 [DOI] [PubMed] [Google Scholar]
- 7.Belmonte C., Acosta M.C. and Gallar J. (2004) Neural basis of sensation in intact and injured corneas. Exp. Eye Res. 78, 513–525 10.1016/j.exer.2003.09.023 [DOI] [PubMed] [Google Scholar]
- 8.Rosenthal P. and Borsook D. (2016) Ocular neuropathic pain. Br. J. Ophthalmol. 100, 128–134 10.1136/bjophthalmol-2014-306280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Müller L.J., Marfurt C.F., Kruse F. and Tervo T.M. (2003) Corneal nerves: structure, contents and function. Exp. Eye Res. 76, 521–542 10.1016/S0014-4835(03)00050-2 [DOI] [PubMed] [Google Scholar]
- 10.Belmonte C., Garcia-Hirschfeld J. and Gallar J. (1997) Neurobiology of ocular pain. Prog. Ret. Eye Res. 16, 117–156 10.1016/S1350-9462(96)00027-4 [DOI] [Google Scholar]
- 11.Brooks J. and Tracey I. (2005) From nociception to pain perception: imaging the spinal and supraspinal pathways. J. Anat. 207, 19–33 10.1111/j.1469-7580.2005.00428.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belmonte C., Aracil A., Acosta M.C., Luna C. and Gallar J. (2004) Nerves and sensations from the eye surface. Ocul. Surf. 2, 248–253 10.1016/S1542-0124(12)70112-X [DOI] [PubMed] [Google Scholar]
- 13.Basbaum A.I., Bautista D.M., Scherrer G. and Julius D. (2009) Cellular and molecular mechanisms of pain. Cell 139, 267–284 10.1016/j.cell.2009.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müller L.J., Vrensen G.F., Pels L., Cardozo B.N. and Willekens B. (1997) Architecture of human corneal nerves. Invest. Ophthalmol. Vis. Sci. 38, 985–994 [PubMed] [Google Scholar]
- 15.Basbaum A.I. and Jessell T. (2000) The perception of pain. In Principles of Neuroscience (Kandel E.R., Schwartz J. and Jessell T., eds), pp. 472–491, Appleton and Lange, New York [Google Scholar]
- 16.Benarroch E.E. (2015) Ion channels in nociceptors: recent developments. Neurology 84, 1153–1164 10.1212/WNL.0000000000001382 [DOI] [PubMed] [Google Scholar]
- 17.Hirata H., Takeshita S., Hu J.W. and Bereiter D.A. (2000) Cornea-responsive medullary dorsal horn neurons: modulation by local opioids and projections to thalamus and brain stem. J. Neurophysiol. 84, 1050–1061 10.1152/jn.2000.84.2.1050 [DOI] [PubMed] [Google Scholar]
- 18.Panneton W.M., Hsu H. and Gan Q. (2010) Distinct central representations for sensory fibers innervating either the conjunctiva or cornea of the rat. Exp. Eye Res. 90, 388–396 10.1016/j.exer.2009.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aicher S.A., Hermes S.M. and Hegarty D.M. (2013) Corneal afferents differentially target thalamic- and parabrachial-projecting neurons in spinal trigemina nucleus caudalis. Neuroscience 232, 182–193 10.1016/j.neuroscience.2012.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Belmonte C., Acosta M.C., Merayo-Lloves J. and Gallar J. (2015) What causes eye pain? Curr. Ophthalmol. Rep. 3, 111–121 10.1007/s40135-015-0073-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goyal S. and Hamrah P. (2016) Understanding neuropathic corneal pain— gaps and current therapeutic approaches. Sem. Ophthalmol. 31, 59–70 10.3109/08820538.2015.1114853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Aqaba M.A., Fares U., Suleman H., Lowe J. and Dua H.S. (2010) Architecture and distribution of human corneal nerves. Br. J. Ophthalmol. 94, 784–789 10.1136/bjo.2009.173799 [DOI] [PubMed] [Google Scholar]
- 23.Guthoff R.F., Wienss H., Hahnel C. and Wree A. (2005) Epithelial innervation of human cornea: a three-dimensional study using confocal laser scanning fluorescence microscopy. Cornea 24, 608–613 10.1097/01.ico.0000154384.05614.8f [DOI] [PubMed] [Google Scholar]
- 24.Murata Y. and Masuko S. (2006) Peripheral and central distribution of TRPV1, substance P and CGRP of rat corneal neurons. Brain Res. 1085, 87–94 10.1016/j.brainres.2006.02.035 [DOI] [PubMed] [Google Scholar]
- 25.Zhang F., Yang H., Wang Z., Mergler S., Liu H. and Kawakita T. (2007) Transient receptor potential vanilloid 1 activation induces inflammatory cytokine release in corneal epithelium through MAPK signaling. J. Cell. Physiol. 213, 730–739 10.1002/jcp.21141 [DOI] [PubMed] [Google Scholar]
- 26.Mergler S., Pleyer U., Reinach P., Bednarz J., Dannowski H., Engelmann K. et al. (2005) EGF suppresses hydrogen peroxide induced Ca2+ influx by inhibiting L-type channel activity in cultured human corneal endothelial cells. Exp. Eye Res. 80, 285–293 10.1016/j.exer.2004.09.012 [DOI] [PubMed] [Google Scholar]
- 27.Mergler S., Valtink M., Coulson-Thomas V.J., Lindemann D., Reinach P.S., Engelmann K. et al. (2010) TRPV channels mediate temperature-sensing in human corneal endothelial cells. Exp. Eye. Res. 90, 758–770 10.1016/j.exer.2010.03.010 [DOI] [PubMed] [Google Scholar]
- 28.Mergler S., Garreis F., Sahlmüller M., Reinach P.S., Paulsen F. and Pleyer U. (2011) Thermosensitive transient receptor potential channels in human corneal epithelial cells. J. Cell Physiol. 226, 1828–1842 10.1002/jcp.22514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mergler S., Valtink M., Takayoshi S., Okada Y., Miyajima M. and Saika S. (2014) Temperature-sensitive transient receptor potential channels in corneal tissue layers and cells. Ophthalmic Res. 52, 151–159 10.1159/000365334 [DOI] [PubMed] [Google Scholar]
- 30.Yang Y., Yang H., Wang Z., Varadaraj K., Kimari S.S. and Mergler S., Cannabinoid receptor 1 suppresses transient receptor potential vanilloid 1-induced inflammatory responses to corneal injury. Cell. Signal. 25, 501–511 10.1016/j.cellsig.2012.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quallo T., Vastani N., Horridge E., Gentry C., Parra A. and Moss S. (2015) TRPM8 is a neuronal osmosensor that regulates eye blinking in mice. Nat. Commun. 6, 7150 10.1038/ncomms8150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lucius A., Khajavi N., Reinach P.S., Köhrle J., Dhandapani P. and Huimann P. (2016) 3-Iodothyronamine increases transient receptor potential melastatin channel 8 (TRPM8) activity in immortalized human corneal epithelial cells. Cell. Signal. 28, 136–147 10.1016/j.cellsig.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 33.Caspani O., Zurborg S., Labuz D. and Heppenstall P.A. (2009) The contribution of TRPM8 and TRPA1 channels to cold allodynia and neuropathic pain. PLoS One 4, e7383 10.1371/journal.pone.0007383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olsen R.V., Andersen H.H., Møller H.G., Eskelund P.W. and Arendt-Nielsen L. (2014) Somatosensory and vasomotor manifestations of individual and combined stimulation of TRPM8 and TRPA1 using topical L-menthol and trans-cinnamaldehyde in healthy volunteers. Eur. J. Pain. 18, 1333–1342 10.1002/j.1532-2149.2014.494.x [DOI] [PubMed] [Google Scholar]
- 35.Stenholm E., Bongenhielm U., Ahlquist M. and Fried K. (2002) VRl- and VRL-l-like immunoreactivity in normal and injured trigeminal dental primary sensory neurons of the rat. Acta Odontol. Scand. 60, 72–79 10.1080/000163502753509455 [DOI] [PubMed] [Google Scholar]
- 36.Okada Y., Reinach P.S. and Shirai K. (2015) Transient receptor potential channels and corneal stromal inflammation. Cornea 34, S136–S141 10.1097/ICO.0000000000000602 [DOI] [PubMed] [Google Scholar]
- 37.Martínez-García M.C., Martínez T., Pañeda C., Gallego P., Jimenez A.I. and Merayo J. (2013) Differential expression and localization of transient receptor potential vanilloid 1 in rabbit and human eyes. Histol. Histopathol. 28, 1507–1516 [DOI] [PubMed] [Google Scholar]
- 38.Jara-Oseguera A., Simon S.A and Rosenbaum T. (2008) TRPV1: on the road to pain relief. Curr. Mol. Pharmacol. 1, 255–269 10.2174/1874467210801030255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tóth A., Blumberg P.M. and Boczán J. (2009) Anandamide and the vanilloid receptor (TRPV1). Vitam. Horm. 81, 389–419 [DOI] [PubMed] [Google Scholar]
- 40.Beuerman R.W. and Stern M.E. (2005) Neurogenic inflammation: a first line of defense for the ocular surface. Ocul. Surf. 3, S203–S206 10.1016/S1542-0124(12)70256-2 [DOI] [PubMed] [Google Scholar]
- 41.Mantelli F., Massaro-Giordano M., Macchi I., Lambiase A. and Bonini S. (2013) The cellular mechanisms of dry eye: From pathogenesis to treatment. J. Cell Physiol. 228, 2253–2256 10.1002/jcp.24398 [DOI] [PubMed] [Google Scholar]
- 42.Tervo K., Tervo T.M.T., Eranko L., Vannas A., Cuello A.C. and Eranko O. (1982) Substance P immunoreactive nerves in the human cornea and iris. Invest. Ophthalmol. Vis. Sci. 23, 671–674 [PubMed] [Google Scholar]
- 43.Stone R.A. and Kuwayama Y. (1985) Substance P-like immunoreactive nerves in the human eye. Arch. Ophthalmol. 103, 1207–1211 10.1001/archopht.1985.01050080119031 [DOI] [PubMed] [Google Scholar]
- 44.Jones M.A. and Marfurt C.F. (1991) Calcitonin gene-related peptide and corneal innervation: a developmental study in the rat. J. Comp. Neurol. 313, 132–150 10.1002/cne.903130110 [DOI] [PubMed] [Google Scholar]
- 45.Marfurt C.F., Murphy C.J. and Florczak J.L. (2001) Morphology and neurochemistry of canine corneal innervation. Invest. Ophthalmol. Vis. Sci. 42, 2242–2251 [PubMed] [Google Scholar]
- 46.Müller L.J. and Klooster J. (2001) Distribution of substance P (SP) and calcitonin gene related peptide (GGRP) in human corneal nerves. Invest. Ophthalmol. Vis. Sci. 42, S28 [Google Scholar]
- 47.Schlereth T., Schukraft J., Krämer-Best H.H., Geber C., Ackermann T. and Birklein F. (2016) Interaction of calcitonin gene related peptide (CGRP) and substance P (SP) in human skin. Neuropeptides 59, 57–62 10.1016/j.npep.2016.06.001 [DOI] [PubMed] [Google Scholar]
- 48.Harrison S. and Geppetti P. (2001) Substance p. Int. J. Biochem. Cell Biol. 33, 555–576 10.1016/S1357-2725(01)00031-0 [DOI] [PubMed] [Google Scholar]
- 49.Donkin J.J., Turner R.J., Hassan I. and Vink R. (2007) Substance P in traumatic brain injury. Prog. Brain Res. 161, 97–109 10.1016/S0079-6123(06)61007-8 [DOI] [PubMed] [Google Scholar]
- 50.IASP (2010) Diagnosis and classification of neuropathic pain epidemiology and impact of neuropathic pain. Pain Medicine XVIII, 1–6 [Google Scholar]
- 51.Pouyeh B., Viteri E., Feuer W., Lee D.J., Florez H., Fabian J.A. et al. (2012) Impact of ocular surface symptoms on quality of life in a United States veterans affairs population. Am. J. Ophthalmol. 153, 1061–1066 10.1016/j.ajo.2011.11.030 [DOI] [PubMed] [Google Scholar]
- 52.Galor A., Levitt R.C., Felix E.R., Martin E.R. and Sarantopoulos C.D. (2015) Neuropathic ocular pain: an important yet underevaluated feature of dry eye. Eye 29, 301–312 10.1038/eye.2014.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dieckmann G., Goyal S. and Hamrah P. (2017) Neuropathic corneal pain: approaches for management. Ophthalmology 124, S34–S47 10.1016/j.ophtha.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bridges D., Thompson S.W. and Rice A.S. (2001) Mechanisms of neuropathic pain. Br. J. Anaesth. 87, 12–26 10.1093/bja/87.1.12 [DOI] [PubMed] [Google Scholar]
- 55.Jensen T.S. and Finnerup N.B. (2014) Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. Lancet Neurol. 13, 924–935 10.1016/S1474-4422(14)70102-4 [DOI] [PubMed] [Google Scholar]
- 56.Yaksh T.L. and Wiese A.J.A. (2014) Survey of systems involved in nociceptive processing. In Comprehensive Treatment of Chronic Pain by Medical, Interventional, and Integrative Approaches (Deer T.R., Leong M.S., Buvanendran A., Gordin V., Kim P.S., Panchal S.J. and Ray A., eds), Springer, Berlin, The American Academy of Pain Medicine Textbook on Pain Management 9 [Google Scholar]
- 57.Wall P.D. and Devor M. (1983) Sensory afferent impulses originate from dorsal root ganglia as well as the periphery in normal and nerve injured rats. Pain 17, 321–339 10.1016/0304-3959(83)90164-1 [DOI] [PubMed] [Google Scholar]
- 58.Bennett M. (2010) Neuropathic Pain, Oxford University Press [Google Scholar]
- 59.Waldman C.W, Waldman S.D. and Waldman R.A. (2014) A practical approach to ocular pain for the non-ophthalmologist. Pain Manag. 4, 413–426 10.2217/pmt.14.38 [DOI] [PubMed] [Google Scholar]
- 60.Toosy A.T., Mason D.F. and Miller D.H. (2014) Optic neuritis. Lancet Neurol. 13, 83–99 10.1016/S1474-4422(13)70259-X [DOI] [PubMed] [Google Scholar]
- 61.Gayton J.L. (2009) Etiology, prevalence, and treatment of dry eye disease. Clin. Ophthalmol. 3, 405–412 10.2147/OPTH.S5555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galor A., Moein H.R., Lee C., Rodriguez A., Felix A.R., Sarantopolous K.D. et al. (2018) Neuropathic pain and dry eye. Ocul. Surf. 16, 31–44 10.1016/j.jtos.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mainstone J.C., Bruce A.S. and Golding T.R. (1996) Tear meniscus measurement in the diagnosis of dry eye. Curr. Eye Res. 15, 653–661 10.3109/02713689609008906 [DOI] [PubMed] [Google Scholar]
- 64.Nichols K.K., Nichols J.J. and Mitchell G.L. (2004) The lack of association between signs and symptoms in patients with dry eye disease. Cornea 23, 762–770 10.1097/01.ico.0000133997.07144.9e [DOI] [PubMed] [Google Scholar]
- 65.Parra A., Madrid R., Echevarria D., del Olmo S., Morenilla-Palao C. and Acosta M.C. (2010) Ocular surface wetness is regulated by TRPM8-dependent cold thermoreceptors of the cornea. Nat. Med. 16, 1396–1399 10.1038/nm.2264 [DOI] [PubMed] [Google Scholar]
- 66.Hirata H. and Oshinsky M.L. (2012) Ocular dryness excites two classes of corneal afferent neurons implicated in basal tearing in rats: involvement of transient receptor potential channels. J. Neurophysiol. 107, 1199–1209 10.1152/jn.00657.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moalem G. and Tracey D.J. (2006) Immune and inflammatory mechanisms in neuropathic pain. Brain Res. Rev. 51, 240–264 10.1016/j.brainresrev.2005.11.004 [DOI] [PubMed] [Google Scholar]
- 68.Schomberg D., Ahmed M., Miranpuri G., Olson J. and Resnick D.K. (2012) Neuropathic pain: role of inflammation, immune response, and ion channel activity in central injury mechanisms. Ann. Neurosci. 19, 125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ellis A. and Bennett D.L. (2013) Neuroinflammation and the generation of neuropathic pain. Br. J. Anaesth. 111, 26–37 10.1093/bja/aet128 [DOI] [PubMed] [Google Scholar]
- 70.Kerstman E., Ahn S., Battu S., Tariq S. and Grabois M. (2013) Neuropathic pain. Handb. Clin. Neurol. 110, 175–187 10.1016/B978-0-444-52901-5.00015-0 [DOI] [PubMed] [Google Scholar]
- 71.Sommer C., Leinders M. and Üçeyler N. (2018) Inflammation in the pathophysiology of neuropathic pain. Pain 159, 595–602 [DOI] [PubMed] [Google Scholar]
- 72.Cooper B.A., Holekamp N.M., Bohigian G. and Thompson P.A. (2003) Case-control study of endophthalmitis after cataract surgery comparing scleral tunnel and clear corneal wounds. Am. J. Ophthalmol. 136, 300–305 10.1016/S0002-9394(03)00202-2 [DOI] [PubMed] [Google Scholar]
- 73.Taylor A.W. (2009) Ocular immune privilege. Eye 23, 1885–1889 10.1038/eye.2008.382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vallejo-Garcia J.L., Asencio-Duran M., Pastora-Salvador N., Vinci-Guerra P. and Romano M.R. (2012) Role of inflammation in endophthalmitis. Mediators Inflamm., 2012, 10.1155/2012/196094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McMenamin P.G., Crewe J., Morrison S. and Holt P.G. (1994) Immunomorphologic studies of macrophages and MHC class II-positive dendritic cells in the iris and ciliary body of the rat, mouse, and human eye. Invest. Ophthalmol. Vis. Sci. 35, 3234–3250 [PubMed] [Google Scholar]
- 76.Li S., Li B., Jiang H., Wang Y., Qu M. and Duan H. (2013) Macrophage depletion impairs corneal wound healing after autologous transplantation in mice. PLoS One 8, e61799 10.1371/journal.pone.0061799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gaynes B.I. and Onyekwuluje A. (2008) Topical ophthalmic NSAIDs: a discussion with focus on nepafenac ophthalmic suspension. Clin. Ophthalmol. 2, 355–368 10.2147/OPTH.S1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim S.J., Flach A.J. and Jampol L.M. (2010) Nonsteroidal anti-inflammatory drugs in ophthalmology. Surv. Ophthalmol. 55, 108–133 10.1016/j.survophthal.2009.07.005 [DOI] [PubMed] [Google Scholar]
- 79.Wilson D.J., Schutte S.M. and Abel S.R. (2015) Comparing the efficacy of ophthalmic NSAIDs in common indications: a literature review to support cost-effective prescribing. Ann. Pharmacother. 49, 727–734 10.1177/1060028015574593 [DOI] [PubMed] [Google Scholar]
- 80.Gallagher R.M. and Rosenthal L.J. (2008) Chronic pain and opiates: balancing pain control and risks in long-term opioid treatment. Arch. Phys. Med. Rehabil. 89, S77–S82 10.1016/j.apmr.2007.12.003 [DOI] [PubMed] [Google Scholar]
- 81.Nightingale S. (2012) The neuropathic pain market. Nat. Rev. Drug Discov. 11, 101–102 10.1038/nrd3624 [DOI] [PubMed] [Google Scholar]
- 82.Wolf E.J., Kleiman L.Z. and Schrier A. (2007) Nepafenac-associated corneal melt. J. Cataract Refract Surg. 33, 1974–1975 10.1016/j.jcrs.2007.06.043 [DOI] [PubMed] [Google Scholar]
- 83.Comstock T.L. and Decory H.H. (2012) Advances in corticosteroid therapy for ocular inflammation: loteprednol etabonate. Int. J. Inflam. 2012, 789623 10.1155/2012/789623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Duvall B. and Kershner R. (2006) Ophthalmic Medications and Pharmacology, 2nd ed., Slack, Thorofare, N.J. [PubMed] [Google Scholar]
- 85.Beardsley R.M., Suhler E.B., Rosenbaum J.T. and Lin P. (2013) Pharmacotherapy of scleritis: current paradigms and future directions. Expert Opin. Pharmacother. 14, 411–424 10.1517/14656566.2013.772982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cashman J.N. (1996) The mechanisms of action of NSAIDs in analgesia. Drugs 52, 13–23 10.2165/00003495-199600525-00004 [DOI] [PubMed] [Google Scholar]
- 87.Vane J.R. and Botting R.M. (1998) Mechanism of action of nonsteroidal anti-inflammatory drugs. Am. J. Med. 104, 2S–8S 10.1016/S0002-9343(97)00203-9 [DOI] [PubMed] [Google Scholar]
- 88.Gaynes B.I. and Fiscella R. (2002) Topical non-steroidal anti-inflammatory drugs for ophthalmic use. Drug Saf. 25, 2334–2350 10.2165/00002018-200225040-00002 [DOI] [PubMed] [Google Scholar]
- 89.Murray M.D. and Brater D.C. (1993) Renal toxicity of the non-steroidal anti-inflammatory drugs. Annu. Rev. Pharmacol. Toxicol. 33, 435–465 10.1146/annurev.pa.33.040193.002251 [DOI] [PubMed] [Google Scholar]
- 90.Hawkey C.J. and Langman M.J. (2003) Non-steroidal anti-inflammatory drugs: overall risks and management. Complementary roles for COX-2 inhibitors and proton pump inhibitors. Gut 52, 600–608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Trelle S., Reichenbach S., Wandel S., Hildebrand P., Tschannen B. and Villiger P.M (2011) Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ 342, c7086 10.1136/bmj.c7086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jóźwiak-Bebenista M. and Nowak J.Z. (2014) Paracetamol: mechanism of action, applications and safety concern. Acta Pol. Pharm. 71, 11–23 [PubMed] [Google Scholar]
- 93.Moulin D., Boulanger A., Clark A.J, Clarke H., Dao T. and Finley G.A (2014) Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian Pain Society. Pain Res. Manag. 19, 328–335 10.1155/2014/754693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Freynhagen R., Strojek K., Griesing T., Whalen E. and Balkenohl M. (2005) Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomised, double-blind, multicentre, placebo-controlled trial of flexible- and fixed-dose regimens. Pain 115, 254–263 10.1016/j.pain.2005.02.032 [DOI] [PubMed] [Google Scholar]
- 95.Bian F., Li Z., Offord J., Davis M.D., McCormick J. and Taylor C.P. (2006) Calcium channel alpha2-delta type 1 subunit is the major binding protein for pregabalin in neocortex, hippocampus, amygdala, and spinal cord: an ex vivo autoradiographic study in alpha2-delta type 1 genetically modified mice. Brain Res. 1075, 68–80 10.1016/j.brainres.2005.12.084 [DOI] [PubMed] [Google Scholar]
- 96.Li C.Y., Song Y.H., Higuera E.S. and Luo Z.D. (2004) Spinal dorsal horn calcium channel alpha2delta-1 subunit upregulation contributes to peripheral nerve injury-induced tactile allodynia. J. Neurosci. 24, 8494–8499 10.1523/JNEUROSCI.2982-04.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rahn E.J. and Hohmann A.G. (2009) Cannabinoids as pharmacotherapies for neuropathic pain: from the bench to the bedside. Neurotherapeutics 6, 713–737 10.1016/j.nurt.2009.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lynch M.E. and Campbell F. (2011) Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials. Br. J. Clin. Pharmacol. 72, 735–744 10.1111/j.1365-2125.2011.03970.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Aggarwal S.K., Carter G.T., Sullivan M.D., Zumbrunnen C., Morrill R. and Mayer J.D. (2009) Medicinal use of cannabis in the United States: historical perspectives, current trends, and future directions. J. Opioid. Manag. 5, 153–168 10.5055/jom.2009.0016 [DOI] [PubMed] [Google Scholar]
- 100.Bellnier T., Brown G.W. and Ortega T.R. (2018) Preliminary evaluation of the efficacy, safety, and costs associated with the treatment of chronic pain with medical cannabis. Ment. Health Clin. 8, 110–115 10.9740/mhc.2018.05.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Casey S.L and Vaughan C.W. (2018) Plant-based cannabinoids for the treatment of chronic neuropathic pain. Medicines 2018, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Davis M.P. (2018) Cancer-related neuropathic pain: review and selective topics. Hematol. Oncol. Clin. North Am. 32, 417–431 10.1016/j.hoc.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 103.O’Brien M. and McDougall J.J. (2018) Cannabis and joints: scientific evidence for the alleviation of osteoarthritis pain by cannabinoids. Curr. Opin. Pharmacol. 40, 104–109 10.1016/j.coph.2018.03.012 [DOI] [PubMed] [Google Scholar]
- 104.Bernard C., Milh M., Morozov Y.M., Ben-Ari Y., Freund T.F. and Gozlan H. (2005) Altering cannabinoid signaling during development disrupts neuronal activity. Proc. Natl. Acad. Sci. U.S.A. 102, 9388–9393 10.1073/pnas.0409641102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pandey R., Mousawy K., Nagarkatti M. and Nagarkatti P. (2009) Endocannabinoids and immune regulation. Pharmacol. Res. 60, 85–92 10.1016/j.phrs.2009.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pacher P. and Kunos G. (2013) Modulating the endocannabinoid system in human health and disease–successes and failures. FEBS J. 280, 1918–1943 10.1111/febs.12260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Silvestri C. and Di Marzo V. (2013) The endocannabinoid system in energy homeostasis and the etiopathology of metabolic disorders. Cell Metab. 17, 475–490 10.1016/j.cmet.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 108.Pertwee R.G. (2015) Endocannabinoids and their pharmacological actions. Handb. Exp. Pharmacol. 231, 1–37 10.1007/978-3-319-20825-1_1 [DOI] [PubMed] [Google Scholar]
- 109.Pacher P., Steffens S., Haskó G., Schindler T.H. and Kunos G. (2018) Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev. Cardiol. 15, 151–166 10.1038/nrcardio.2017.130 [DOI] [PubMed] [Google Scholar]
- 110.Mechoulam R., Hanus L.O., Pertwee R. and Howlett A.C. (2014) Early phytocannabinoid chemistry to endocannabinoids and beyond. Nat. Rev. Neurosci. 15, 757–776 10.1038/nrn3811 [DOI] [PubMed] [Google Scholar]
- 111.Gaoni Y. and Mechoulam R. (1964) Isolation, structure, and partial synthesis of an active constituent of Hashish. J. Am. Chem. Soc. 86, 1646–1647 10.1021/ja01062a046 [DOI] [Google Scholar]
- 112.Devane W.A., Hanus L., Breuer A., Pertwee R.G., Stevenson L.A. and Griffin G. (1992) Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258, 1946–1949 10.1126/science.1470919 [DOI] [PubMed] [Google Scholar]
- 113.Mechoulam R., Ben-Shabat S., Hanus L., Ligumsky M. and Kaminsky M.E (1995) Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem. Pharmacol. 50, 83–90 10.1016/0006-2952(95)00109-D [DOI] [PubMed] [Google Scholar]
- 114.Schicho R. and Storr M. (2013) Patients with IBD find symptom relief in FAAH: fatty acid amide hydrolase; MAGL: monoacylglycerol lipase. Nat. Rev. Gastroenterol. Hepatol., 11, 142–143, 10.1038/nrgastro.2013.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Matsuda L.A., Lolait S.J., Brownstein M.J., Young A.C. and Bonner T.I. (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346, 561e4 10.1038/346561a0 [DOI] [PubMed] [Google Scholar]
- 116.Munro S., Thomas K.L. and Abu-Shaar M. (1993) Molecular characterization of a peripheral receptor for cannabinoids. Nature 365, 61–65 10.1038/365061a0 [DOI] [PubMed] [Google Scholar]
- 117.Howlett A.C., Barth F., Bonner T.I., Cabral G., Casellas P. and Devane W.A. (2002) International Union of Pharmacology: XXVII. Classification Of Cannabinoid Receptors. Pharmacol. Rev. 54, 161–202 [DOI] [PubMed] [Google Scholar]
- 118.Pertwee R.G. (2010) Receptors and channels targeted by synthetic cannabinoid receptor agonists and antagonists. Curr. Med. Chem. 17, 1360–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Alexander S.P. and Kendall D.A. (2007) The complications of promiscuity: endocannabinoid action and metabolism. Br. J. Pharmacol. 152, 602–623 10.1038/sj.bjp.0707456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hillard C.J. (2017) Circulating endocannabinoids: from whence do they come and where are they going? Neuropsychopharmacology 43, 145–172, 10.1038/npp.2017.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hillard C.J. (2015) The endocannabinoid signaling system in the CNS: a primer. Int. Rev. Neurobiol. 125, 1–47 10.1016/bs.irn.2015.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Piomelli D., Beltramo M., Giuffrida A. and Stella N. (1998) Endogenous cannabinoid signaling. Neurobiol. Dis. 5, 462–473 10.1006/nbdi.1998.0221 [DOI] [PubMed] [Google Scholar]
- 123.Stella N., Schweitzer P. and Piomelli D. (1997) A second endogenous cannabinoid that modulates long-term potentiation. Nature 388, 773–778 10.1038/42015 [DOI] [PubMed] [Google Scholar]
- 124.Goparaju S.K., Ueda N., Taniguchi K. and Yamamoto S. (1999) Enzymes of porcine brain hydrolyzing 2-arachidonoylglycerol, an endogenous ligand of cannabinoid receptors. Biochem. Pharmacol. 57, 417–423 10.1016/S0006-2952(98)00314-1 [DOI] [PubMed] [Google Scholar]
- 125.Storr M.A., Keenan C.M., Emmerdinger D., Zhang H., Yüce B. and Sibaev A. (2008) Targeting endocannabinoid degradation protects against experimental colitis in mice: involvement of CB1 and CB2 receptors. J. Mol. Med. 86, 925–936 10.1007/s00109-008-0359-6 [DOI] [PubMed] [Google Scholar]
- 126.Cravatt B.F., Giang D.K., Mayfield S.P., Boger D.L., Lerner R.A. and Gilula N.B. (1996) Molecular characterization of an enzyme that degrades neuromodulatory fatty-acid amides. Nature 384, 83–87 10.1038/384083a0 [DOI] [PubMed] [Google Scholar]
- 127.Cravatt B.F., Demarest K., Patricelli M.P., Bracey M.H., Giang D.K., Martin B.R. et al. (2001) Supersensitivity to anandamide and enhanced endogenous cannabinoid signaling in mice lacking fatty acid amide hydrolase. Proc. Natl. Acad. Sci. U.S.A. 98, 9371–9376 10.1073/pnas.161191698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Blankman J.L., Simon G.M. and Cravatt B.F. (2007) A comprehensive profile of brain enzymes that hydrolyze the endocannabinoid 2-arachidonoylglycerol. Chem. Biol. 14, 1347–1356 10.1016/j.chembiol.2007.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Burstein S.H. and Zurier R.B. (2009) Cannabinoids, endocannabinoids, and related analogs in inflammation. AAPS J. 11, 109–119 10.1208/s12248-009-9084-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Savinainen J.R., Saario S.M. and Laitinen J.T. (2012) The serine hydrolases MAGL, ABHD6 and ABHD12 as guardians of 2-arachidonoylglycerol signalling through cannabinoid receptors. Acta Physiol. 204, 267–276 10.1111/j.1748-1716.2011.02280.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Urquhart P., Nicolaou A. and Woodward D.F. (2015) Endocannabinoids and their oxygenation by cyclo-oxygenases, lipoxygenases and other oxygenases. Biochim. Biophys. Acta 1851, 366–376 10.1016/j.bbalip.2014.12.015 [DOI] [PubMed] [Google Scholar]
- 132.De Petrocellis L., Bisogno T., Maccarrone M., Davis J.B., Finazzi-agro A. and Di Marzo V. (2001) The activity of anandamide at vanilloid VR1 receptors requires facilitated transport across the cell membrane and is limited by intracellular metabolism. J. Biol. Chem. 276, 12856–12863 10.1074/jbc.M008555200 [DOI] [PubMed] [Google Scholar]
- 133.Hillard C.J. and Jarrahian A. (2003) Cellular accumulation of anandamide: consensus and controversy. Br. J. Pharmacol. 140, 802–808 10.1038/sj.bjp.0705468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moore S.A., Nomikos G.G., Dickason-Chesterfield A.K., Schober D.A., Schaus J.M. and Ying B.P (2005) Identification of a high-affinity binding site involved in the transport of endocannabinoids. Proc. Natl. Acad. Sci. U.S.A. 102, 17852–17857 10.1073/pnas.0507470102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Guindon J. and Hohmann A.G. (2009) The endocannabinoid system and pain. CNS Neurol. Disord. Drug Targets 8, 403–421 10.2174/187152709789824660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chicca A., Marazzi J., Nicolussi S. and Gertsch J. (2012) Evidence for bidirectional endocannabinoid transport across cell membranes. J. Biol. Chem. 287, 34660–34682 10.1074/jbc.M112.373241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fowler C.J. (2013) Transport of endocannabinoids across the plasma membrane and within the cell. FEBS J. 280, 1895–1904 10.1111/febs.12212 [DOI] [PubMed] [Google Scholar]
- 138.Conn P.J., Christopoulos A. and Lindsley C.W. (2009) Allosteric modulators of GPCRs: a novel approach for the treatment of CNS disorders. Nat. Rev. Drug Discov. 8, 41–54 10.1038/nrd2760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Galiègue S., Mary S., Marchand J., Dussossoy D., Carrière D., Carayon P. et al. (1995) Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur. J. Biochem. 232, 54–61 10.1111/j.1432-1033.1995.tb20780.x [DOI] [PubMed] [Google Scholar]
- 140.Maccarrone M., Bab I., Bíró T., Cabral G.A., Dey S.K. and Di Marzo V. (2015) Endocannabinoid signaling at the periphery: 50 years after THC. Trends Pharmacol. Sci. 36, 277–296 10.1016/j.tips.2015.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Van Sickle M.D., Duncan M., Kingsley P.J., Mouihate A., Urbani P. and Mackie K. (2005) Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science 310, 329–332 10.1126/science.1115740 [DOI] [PubMed] [Google Scholar]
- 142.Devane W.A., Dysarz F.A., Johnson M.R., Melvin L.S. and Howlett A.C. (1988) Determination and characterization of a cannabinoid receptor in rat brain. Mol. Pharmacol. 34, 605–613 [PubMed] [Google Scholar]
- 143.Howlett A.C. (2005) Cannabinoid receptor signaling. Handb. Exp. Pharmacol. 168, 53–79 10.1007/3-540-26573-2_2 [DOI] [PubMed] [Google Scholar]
- 144.Xu H., Cheng C.L., Chen M., Manivannan A., Cabay L. and Pertwee R.G. (2007) Anti-inflammatory property of the cannabinoid receptor-2-selective agonist JWH-133 in a rodent model of autoimmune uveoretinitis. J. Leukoc. Biol. 82, 532–541 10.1189/jlb.0307159 [DOI] [PubMed] [Google Scholar]
- 145.Wright K.L., Duncan M. and Sharkey K.A. (2008) Cannabinoid CB2 receptors in the gastrointestinal tract: a regulatory system in states of inflammation. Br. J. Pharmacol. 153, 263–270 10.1038/sj.bjp.0707486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Toguri J.T., Lehmann C., Laprairie R.B., Szczesniak A.M., Zhou J. and Denovan-Wright E.M. (2014) Anti-inflammatory effects of cannabinoid CB2 receptor activation in endotoxin-induced uveitis. Br. J. Pharmacol. 171, 1448–1461 10.1111/bph.12545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Toguri J.T., Moxsom R., Szczesniak A.M., Zhou J., Kelly M. E.M. and Lehmann C. (2015) Cannabinoid 2 receptor activation reduces leukocyte adhesion and improves capillary perfusion in the iridial microvasculature during systemic inflammation. Clin. Hemorheol. Microcirc. 61, 237–249 10.3233/CH-151996 [DOI] [PubMed] [Google Scholar]
- 148.Gómez-Gálvez Y., Palomo-Garo C., Fernández-Ruiz J. and García C. (2016) Potential of the cannabinoid CB2 receptor as a pharmacological target against inflammation in Parkinson’s disease. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 64, 200–208 10.1016/j.pnpbp.2015.03.017 [DOI] [PubMed] [Google Scholar]
- 149.Steffens S. and Pacher P. (2012) Targeting cannabinoid receptor CB2 in cardiovascular disorders: Promises and controversies. Br. J. Pharmacol. 167, 313–323 10.1111/j.1476-5381.2012.02042.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rom S. and Persidsky Y. (2013) Cannabinoid receptor 2: potential role in immunomodulation and neuroinflammation. J. Neuroimmune Pharmacol. 8, 608–620 10.1007/s11481-013-9445-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Straiker A.J., Maguire G., Mackie K. and Lindsey J. (1999) Localization of cannabinoid CB1 receptors in the human anterior eye and retina. Invest. Ophthalmol. Vis. Sci. 40, 2442–2448 [PubMed] [Google Scholar]
- 152.Porcella A., Maxia C., Gessa G.L. and Pani L. (2000) The human eye expresses high levels of CB1 cannabinoid receptor mRNA and protein. Eur. J. Neurosci. 12, 1123–1127 10.1046/j.1460-9568.2000.01027.x [DOI] [PubMed] [Google Scholar]
- 153.Stamer W.D., Golightly S.F., Hosohata Y., Ryan E.P., Porter A.C. and Varga E. (2001) Cannabinoid CB1 receptor expression, activation and detection of endogenous ligand in trabecular meshwork and ciliary process tissues. Eu. J. Pharmacol. 431, 277–286 10.1016/S0014-2999(01)01438-8 [DOI] [PubMed] [Google Scholar]
- 154.Yazulla S. (2008) Endocannabinoids in the retina: from marijuana to neuroprotection. Prog. Retin. Eye Res. 27, 501–526 10.1016/j.preteyeres.2008.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Bouskila J., Javadi P., Casanova C., Ptito M. and Bouchard J.F. (2013) Müller cells express the cannabinoid CB2 receptor in the vervet monkey retina. J. Comp. Neurol. 521, 2399–2415 10.1002/cne.23333 [DOI] [PubMed] [Google Scholar]
- 156.Bouskila J., Harrar V., Javadi P., Beierschmitt A., Palmour R. and Casanova C. (2016) Cannabinoid Receptors CB1 and CB2 modulate the electroretinographic waves in vervet monkeys. Neural Plast. 2016, 1253245 10.1155/2016/1253245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Toguri J.T., Caldwell M. and Kelly M.E. (2016) Turning down the thermostat: modulating the endocannabinoid system in ocular inflammation and pain. Front. Pharmacol. 7, 304 10.3389/fphar.2016.00304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chen J., Matias I., Dinh T., Lu T., Venezia S. and Nieves A. (2005) Finding of endocannabinoids in human eye tissues: implications for glaucoma. Biochem. Biophys. Res. Commun. 330, 1062–1067 10.1016/j.bbrc.2005.03.095 [DOI] [PubMed] [Google Scholar]
- 159.Hu S.S., Arnold A., Hutchens J.M, Radicke J., Cravatt B.F. and Wager-Miller J. (2010) Architecture of cannabinoid signaling in mouse retina. J. Comp. Neurol. 518, 3848–3866 10.1002/cne.22429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bouskila J., Burke M.W., Zabouri N., Casanova C., Ptito M. and Bouchard J.F. (2012) Expression and localization of the cannabinoid receptor type 1 and the enzyme fatty acid amide hydrolase in the retina of vervet monkeys. Neuroscience 202, 117–130 10.1016/j.neuroscience.2011.11.041 [DOI] [PubMed] [Google Scholar]
- 161.Cécyre B., Zabouri N., Huppé-Gourgues F., Bouchard J.F. and Casanova C. (2013) Roles of cannabinoid receptors type 1 and 2 on the retinal function of adult mice. Invest. Ophthalmol. Vis. Sci. 54, 8079–8090 10.1167/iovs.13-12514 [DOI] [PubMed] [Google Scholar]
- 162.Cécyre B., Thomas S., Ptito M., Casanova C. and Bouchard J.F. (2014) Evaluation of the specificity of antibodies raised against cannabinoid receptor type 2 in the mouse retina. Naunyn Schmiedebergs Arch. Pharmacol. 387, 175–184 10.1007/s00210-013-0930-8 [DOI] [PubMed] [Google Scholar]
- 163.Bouchard J.F., Casanova C., Cécyre B. and Redmond W.J. (2016) Expression and function of the endocannabinoid system in the retina and the visual brain. Neural Plast. 2016, 9247057 10.1155/2016/9247057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Cairns E.A., Toguri T.J., Porter R.F., Szczesniak A-M. and Kelly M.E.M. (2016) Seeing over the horizon: targeting the endocannabinoid system for the treatment of ocular disease. J. Basic Clin. Physiol. Pharmacol. 27, 253–265 10.1515/jbcpp-2015-0065 [DOI] [PubMed] [Google Scholar]
- 165.Toguri T.J., Leishman E., Szczesniak A.M., Laprairie R., Oehler O. and Straiker A. (2018) Inflammation and CB2 signaling drive novel changes in the ocular lipidome and regulate immune cell activity in the eye. Prostaglandins Other Lipid Mediat., in press [DOI] [PubMed] [Google Scholar]
- 166.Ross R.A. (2007) Allosterism and cannabinoid CB(1) receptors: the shape of things to come. Trends Pharmacol. Sci. 28, 567–572 10.1016/j.tips.2007.10.006 [DOI] [PubMed] [Google Scholar]
- 167.Wootten D., Christopoulos A. and Sexton P.M. (2013) Emerging paradigms in GPCR allostery: implications for drug discovery. Nat. Rev. Drug Discov. 12, 630–644 10.1038/nrd4052 [DOI] [PubMed] [Google Scholar]
- 168.Congrève M., Oswald C. and Marshall F.H. (2017) Applying Structure-Based Drug Design Approaches to Allosteric Modulators of GPCRs. Trends Pharmacol. Sci. 38, 837–847 10.1016/j.tips.2017.05.010 [DOI] [PubMed] [Google Scholar]
- 169.Alaverdashvili M. and Laprairie R.B. (2018) The future of type 1 cannabinoid receptor allosteric ligands. Drug Metab. Rev. 50, 14–25 10.1080/03602532.2018.1428341 [DOI] [PubMed] [Google Scholar]
- 170.Dopart R., Lu D., Lichtman A.H. and Kendall D.A. (2018) Allosteric modulators of cannabinoid receptor 1: developing compounds for improved specificity. Drug Metab. Rev. 50, 3–13 10.1080/03602532.2018.1428342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Toczek M. and Malinowska B. (2018) Enhanced endocannabinoid tone as a potential target of pharmacotherapy. Life Sci., 204, 20–45 10.1016/j.lfs.2018.04.054 [DOI] [PubMed] [Google Scholar]
- 172.Murataeva N., Li S., Oehler O., Miller S., Dhopeshwarkar A. and Hu S.S.-J. (2015) Cannabinoid-induced chemotaxis in bovine corneal epithelial cells. Invest. Opthalmol. Vis. Sci. 56, 3304–3313 10.1167/iovs.14-15675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ashton J.C. and Glass M. (2007) The cannabinoid CB2 receptor as a target for inflammation-dependent neurodegeneration. Curr. Neuropharmacol. 5, 73–80 10.2174/157015907780866884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Agrawal R.V., Murthy S., Sangwan V. and Biswas J. (2010) Current approach in diagnosis and management of anterior uveitis. Indian J. Ophthalmol. 58, 11–19 10.4103/0301-4738.58468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Altinsoy A., Dileköz E., Kul O., Ilhan S.Ö., Tunccan O.G. and Seven I. (2011) A cannabinoid ligand, anandamide, exacerbates endotoxin-induced uveitis in rabbits. J. Ocul. Pharmacol. Ther. 27, 545–552 10.1089/jop.2011.0049 [DOI] [PubMed] [Google Scholar]
- 176.Pastor J.C. (1998) Proliferative vitreoretinopathy: an overview. Surv.. Ophthalmol. 43, 3e18. [DOI] [PubMed] [Google Scholar]
- 177.Hanuš L., Breuer A., Tchilibon S., Shiloah S., Goldenberg D. and Horowitz M. (1999) HU-308: a specific agonist for CB(2), a peripheral cannabinoid receptor. Proc. Natl. Acad. Sci. U.S.A. 96, 14228–14233 10.1073/pnas.96.25.14228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Soethoudt M., Grether U. and Fingerle J. (2017) Cannabinoid CB receptor ligand profiling reveals biased signalling and off-target activity. Nat. Commun. 8, 13958 10.1038/ncomms13958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Szczesniak A., Porter R.F., Toguri J.T., Borowska-Fielding J., Gebremeskel S. and Siwakoti A. (2017) Cannabinoid 2 receptor is a novel anti-inflammatory target in experimental proliferative vitreoretinopathy. Neuropharmacology 113, Part B, 627–638 10.1016/j.neuropharm.2016.08.030 [DOI] [PubMed] [Google Scholar]
- 180.Bereiter D.A., Bereiter D.F. and Hirata H. (2002) Topical cannabinoid agonist, WIN55,212-2, reduces cornea-evoked trigeminal brainstem activity in the rat. Pain 99, 547–556 10.1016/S0304-3959(02)00271-3 [DOI] [PubMed] [Google Scholar]
- 181.Thapa D., Cairns E., Szczesniak A.M., Toguri J.T., Caldwell M. and Kelly M.E.M. (2018) The Cannabinoids ∆8THC, CBD, and HU-308 act via distinct receptors to reduce corneal pain and inflammation. Cannabis Cannabinoid Res. 3, 291–307 10.1089/can.2017.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.McDowell T.S., Wang Z.Y., Singh R. and Bjorling D. (2013) CB1 cannabinoid receptor agonist prevents NGF-induced sensitization of TRPV1 in sensory neurons. Neurosci. Lett. 551, 34–38 10.1016/j.neulet.2013.06.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Njie Y.F., Qiao Z., Xiao Z., Wang W. and Song Z.H. (2008) N-Arachidonyletha- nolamide-induced increase in aqueous humor outflow facility. Invest. Ophthalmol. Vis. Sci. 49, 4528–4534 10.1167/iovs.07-1537 [DOI] [PubMed] [Google Scholar]
- 184.Hudson B.D., Beazley M., Szczesniak A.M., Straiker A. and Kelly M.E. (2011) Indirect sympatholytic actions at beta-adrenoceptors account for the ocular hypotensive actions of cannabinoid receptor agonists. J. Pharmacol. Exp. Ther. 339, 757–767 10.1124/jpet.111.185769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Janero D.R. and Thakur G.A. (2016) Leveraging allostery to improve G protein-coupled receptor (GPCR)-directed therapeutics: cannabinoid receptor 1 as discovery target. Exp. Opin. Drug Discov. 11, 1223–1237 10.1080/17460441.2016.1245289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Fay J.F. and Farrens D.L. (2013) The membrane proximal region of the cannabinoid receptor CB1 N-terminus can allosterically modulate ligand affinity. Biochemistry 52, 8286–8294 10.1021/bi400842k [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Shore D.M., Baillie G.L., Hurst D.H., Navas F., Seltzman H.H. and Marcu J.P. (2014) Allosteric modulation of a cannabinoid G protein-coupled receptor binding site elucidation and relationship to G protein signaling. J. Biol. Chem. 289, 5828–5845 10.1074/jbc.M113.478495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Stornaiuolo M., Bruno A., Botta L., La Regina G., Cosconati S. and Silvestri R. (2015) Endogenous vs exogenous allosteric modulators in GPCRs: a dispute for shuttling CB1 among different membrane microenvironments. Sci. Rep. 5, 15453 10.1038/srep15453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hua T., Vemuri K., Pu M., Qu L., Han G.W. and Wu Y. (2016) Crystal structure of the human cannabinoid receptor CB1. Cell 167, 750–762 10.1016/j.cell.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Shao Z., Yin J., Chapman K., Grzemska M., Clark L. and Wang J. (2016) High-resolution crystal structure of the human CB1 cannabinoid receptor. Nature 540, 602–606 10.1038/nature20613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hua T., Vemuri K., Nikas S.P., Laprairie R.B., Wu Y. and Qu L. (2017) Crystal structures of agonist-bound human cannabinoid receptor CB1. Nature 547, 468–471 10.1038/nature23272 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 192.Nguyen T., Li J.X., Thomas B.F., Wiley J.L., Kenakin T.P. and Zhang Y. (2016) Allosteric modulation: an alternate approach targeting the cannabinoid CB1 receptor. Med. Res. Rev. 37, 441–474 10.1002/med.21418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Cawston E.E., Redmond W.J., Breen C.M., Grimsey N.L., Connor M. and Glass M. (2013) Real-time characterization of cannabinoid receptor 1 (CB1) allosteric modulators reveals novel mechanism of action. Br. J. Pharmacol. 170, 893–907 10.1111/bph.12329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Khajehali E., Malone D.T., Glass M., Sexton P.M., Christopoulos A. and Leach K. (2015) Biased agonism and biased allosteric modulation at the CB1 cannabinoid receptor. Mol. Pharmacol. 88, 368–379 10.1124/mol.115.099192 [DOI] [PubMed] [Google Scholar]
- 195.Laprairie R.B., Bagher A.M., Kelly M.E.M. and Denovan-Wright E.M. (2016) Biased type 1 cannabinoid receptor signaling influences neuronal viability in a cell culture model of Huntington disease. Mol. Pharmacol. 89, 364–275 10.1124/mol.115.101980 [DOI] [PubMed] [Google Scholar]
- 196.Laprairie R.B., Bagher A.M. and Denovan-Wright E.M. (2016) Cannabinoid receptor ligand bias: implications in the central nervous system. Curr. Opin. Pharmacol. 32, 32–43 10.1016/j.coph.2016.10.005 [DOI] [PubMed] [Google Scholar]
- 197.Kulkarni P.M., Ranade A., Garai S. and Thakur G.A. (2017) Microwave-accelerated conjugate addition of 2-arylindoles to substituted b-nitrostyrenes in the presence of ammonium trifluoroacetate: an efficient approach for the synthesis of a novel class of CB1 cannabinoid receptor allosteric modulators. J. Heterocycl. Chem. 54, 2079–2084 10.1002/jhet.2861 [DOI] [Google Scholar]
- 198.Price M.R., Baillie G.L., Thomas A., Stevenson L.A., Easson M. and Goodwin R. (2005) Allosteric modulation of the cannabinoid CB1 receptor. Mol. Pharmacol. 68, 1484–1495 10.1124/mol.105.016162 [DOI] [PubMed] [Google Scholar]
- 199.Ahn K.H., Mahmoud M.M. and Kendall D.A. (2012) Allosteric modulator ORG27569 induces CB1 cannabinoid receptor high affinity agonist binding state, receptor internalization, and Gi protein-independent ERK1/2 kinase activation. J. Biol. Chem. 287, 12070–12082 10.1074/jbc.M111.316463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Burston J.J., Wiley J.L., Craig A.A., Selley D.E. and Sim-selley L.J. (2010) Regional enhancement of cannabinoid CB receptor desensitization in female adolescent rats following repeated Delta-tetrahydrocannabinol exposure. Br. J. Pharmacol. 161, 103–112 10.1111/j.1476-5381.2010.00870.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Russo EB. (2008) Cannabinoids in the management of difficult to treat pain. Ther. Clin. Risk Manag. 4, 245–259 10.2147/TCRM.S1928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Laprairie R.B., Kulkarni P.M., Deschamps J.R., Kelly M.E.M., Janero D.R. and Cascio M.G (2017) Enantiospecific Allosteric Modulation of Cannabinoid 1 Receptor. ACS Chem. Neurosci. 8, 1188–1203 10.1021/acschemneuro.6b00310 [DOI] [PubMed] [Google Scholar]
- 203.Cairns E.A., Szczesniak A.M., Straiker A.J., Kulkarni P.M., Pertwee R.G. and Thakur G.A (2017) The in vivo effects of the CB-positive allosteric modulator GAT229 on intraocular pressure in ocular normotensive and hypertensive mice. J. Ocul. Pharmacol. Ther. 33, 582–590 10.1089/jop.2017.0037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Di Marzo V. (2008) Targeting the endocannabinoid system: to enhance or reduce? Nat. Rev. Drug. Discov. 7, 438–455 10.1038/nrd2553 [DOI] [PubMed] [Google Scholar]
- 205.Sagar D.R., Burston J.J., Woodhams S.G. and Chapman V. (2012) Dynamic changes to the endocannabinoid system in models of chronic pain. Philos. Trans. Royal Soc. B 367, 3300–3311 10.1098/rstb.2011.0390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Fonseca B.M., Costa M.A., Almada M., Correia-da-Silva G. and Teixeira N.A. (2013) Endogenous cannabinoids revisited: a biochemistry perspective. Prostaglandins Other Lipid Mediat. 102-103, 13–30 10.1016/j.prostaglandins.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 207.Murataeva N., Straiker A. and Mackie K. (2014) Parsing the players: 2-arachidonoylglycerol synthesis and degradation in the CNS. Br. J. Pharmacol. 171, 1379–1391 10.1111/bph.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Russo E.B. (2007) History of cannabis and its preparations in saga, science, and sobriquet. Chem. Biodivers. 4, 1614–1648 10.1002/cbdv.200790144 [DOI] [PubMed] [Google Scholar]
- 209.Kinsey S.G., Long J.Z., O’Neal S.T., Abdullah R.A., Poklis J.L. and Boger D.L (2009) Blockade of endocannabinoid-degrading enzymes attenuates neuropathic pain. J. Pharmacol. Exp. Ther. 330, 902–910 10.1124/jpet.109.155465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Kinsey S.G., Long J.Z., Cravatt B.F. and Lichtman A.H. (2010) Fatty acid amide hydrolase and monoacylglycerol lipase inhibitors produce anti-allodynic effects in mice through distinct cannabinoid receptor mechanisms. J. Pain 11, 1420–1428 10.1016/j.jpain.2010.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Zubrzycki M., Janecka A., Liebold A., Ziegler M. and Zubrzycka M. (2017) Effects of centrally administered endocannabinoids and opioids on orofacial pain perception in rats. Br. J. Pharmacol. 174, 3780–3789 10.1111/bph.13970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Flannery L.E., Kerr D.M., Finn D.P. and Roche M. (2018) FAAH inhibition attenuates TLR3-mediated hyperthermia, nociceptive- and anxiety-like behaviour in female rats. Behav. Brain. Res. 353, 11–20 10.1016/j.bbr.2018.06.030 [DOI] [PubMed] [Google Scholar]
- 213.Jiang H.X., Ke B.W., Liu J., Ma G., Hai K.R. and Gong D.Y (2018) Inhibition of fatty acid amide hydrolase improves depressive-like behaviors independent of its peripheral antinociceptive effects in a rat model of neuropathic pain. Anesth. Analg. 10.1213/ANE.0000000000003563 [DOI] [PubMed] [Google Scholar]
- 214.Slusar J.E., Cairns E.A., Szczesniak A.M., Bradshaw H.B., Di Polo A. and Kelly M.E. (2013) The fatty acid amide hydrolase inhibitor, URB597, promotes retinal ganglion cell neuroprotection in a rat model of optic nerve axotomy. Neuropharmacology 72C, 116–125 10.1016/j.neuropharm.2013.04.018 [DOI] [PubMed] [Google Scholar]
- 215.Cuccurazzu B., Zamberletti E., Nazzaro C., Prini P., Trusel M. and Grilli M. (2018) Adult cellular neuroadaptations induced by adolescent THC exposure in female rats are rescued by enhancing anandamide signaling. Int. J. Neuropsychopharmacol. 10.1093/ijnp/pyy057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Piomelli D., Tarzia G., Duranti A., Tontini A., Mor. M. and Compton T.R. (2006) Pharmacological profile of the selective FAAH inhibitor KDS-4103 (URB597). CNS Drug Rev. 12, 21–38 10.1111/j.1527-3458.2006.00021.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Jayamanne A., Greenwood R., Mitchell V.A., Aslan S., Piomelli D. and Vaughan C.W. (2006) Actions of the FAAH inhibitor URB597 in neuropathic and inflammatory chronic pain models. Br. J. Pharmacol. 147, 281–288 10.1038/sj.bjp.0706510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.McDougall J.J., Muley M.M., Philpott H.T., Reid A. and Krustev E. (2017) Early blockade of joint inflammation with a fatty acid amide hydrolase inhibitor decreases end-stage osteoarthritis pain and peripheral neuropathy in mice. Arthritis Res. Ther. 19, 106 10.1186/s13075-017-1313-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Clapper J.R., Moreno-Sanz G., Russo R., Guijarro A., Vacondio F. and Duranti A. (2010) Anandamide suppresses pain initiation through a peripheral endocannabinoid mechanism. Nat. Neurosci. 13, 1265–1270 10.1038/nn.2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Greco R., Bandiera T., Mangione A.S., Demartini C., Siani F. and Nappi G. (2015) Effects of peripheral FAAH blockade on NTG-induced hyperalgesia–evaluation of URB937 in an animal model of migraine. Cephalalgia 35, 1065–1076 10.1177/0333102414566862 [DOI] [PubMed] [Google Scholar]
- 221.Carey L.M., Slivicki R.A., Leishman E., Cornett B., Mackie K. and Bradshaw H. (2016) A pro-nociceptive phenotype unmasked in mice lacking fatty-acid amide hydrolase. Mol. Pain, 10.1177/1744806916649192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Mallet C., Dubray C. and Dualé C. (2016) FAAH inhibitors in the limelight, but regrettably. Int. J. Clin. Pharmacol. Ther. 54, 498–501 10.5414/CP202687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Wagenlehner F.M.E., Van till J.W.O., Houbiers J.G.A., Martina R.V., Cerneus D.P. and Melis J.H.J.M (2017) Fatty acid amide hydrolase inhibitor treatment in men with chronic prostatitis/chronic pelvic pain syndrome: an adaptive double-blind. Randomized Controlled Trial. Urol. 103, 191–197 [DOI] [PubMed] [Google Scholar]
- 224.Huggins J.P., Smart T.S., Langman S., Taylor L. and Young T. (2012) An efficient randomised, placebo-controlled clinical trial with the irreversible fatty acid amide hydrolase-1 inhibitor PF-04457845, which modulates endocannabinoids but fails to induce effective analgesia in patients with pain due to osteoarthritis of the knee. Pain 153, 1837–1846 10.1016/j.pain.2012.04.020 [DOI] [PubMed] [Google Scholar]
- 225.Kerbrat A., Ferré J.C., Fillatre P., Ronzière T., Vannier S. and Carsin-Nicol B. (2016) Acute Neurologic Disorder from an Inhibitor of Fatty Acid Amide Hydrolase. N. Engl. J. Med. 375, 1717–1725 10.1056/NEJMoa1604221 [DOI] [PubMed] [Google Scholar]
- 226.van Esbroeck A.C.M., Janssen A.P.A., Cognetta A.B., Ogasawara D., Shpak G. and van der Kroeg M. (2017) Activity-based protein profiling reveals off-target proteins of the FAAH inhibitor BIA 10-2474. Science 356, 1084–1087 10.1126/science.aaf7497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Wiley J.L. and Martin B.R. (2003) Cannabinoid pharmacological properties common to other centrally acting drugs. Eur. J. Pharmacol. 471, 185–193 10.1016/S0014-2999(03)01856-9 [DOI] [PubMed] [Google Scholar]
- 228.Lichtman A.H., Leung D., Shelton C.C., Saghatelian A., Hardouin C. and Boger D.L (2004) Reversible inhibitors of fatty acid amide hydrolase that promote analgesia: evidence for an unprecedented combination of potency and selectivity. J. Pharmacol. Exp. Ther. 311, 441–448 10.1124/jpet.104.069401 [DOI] [PubMed] [Google Scholar]
- 229.Long J.Z., Li W., Booker L., Burston J.J., Kinsey S.G. and Schlosburg J.E (2009) Selective blockade of 2-arachidonoylglycerol hydrolysis produces cannabinoid behavioral effects. Nat. Chem. Biol. 5, 37–44 10.1038/nchembio.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Gonsiorek W., Lunn C., Fan X., Narula S., Lundell D. and Hipkin R.W. (2000) Endocannabinoid 2-arachidonyl glycerol is a full agonist through human type 2 cannabinoid receptor: antagonism by anandamide. Mol. Pharmacol. 57, 1045–1050 [PubMed] [Google Scholar]
- 231.Kamimura R., Hossain M.Z., Unno S., Ando H., Masuda Y. and Takahashi K. (2018) Inhibition of 2-arachydonoylgycerol degradation attenuates orofacial neuropathic pain in trigeminal nerve-injured mice. J. Oral Sci. 60, 37–44 10.2334/josnusd.17-0005 [DOI] [PubMed] [Google Scholar]
- 232.Spradley J.M., Guindon J. and Hohmann A.G. (2010) Inhibitors of monoacylglycerol lipase, fatty-acid amide hydrolase and endocannabinoid transport differentially suppress capsaicin-induced behavioral sensitization through peripheral endocannabinoid mechanisms. Pharmacol. Res. 62, 249–258 10.1016/j.phrs.2010.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Guindon J., Guijarro A., Piomelli D. and Hohmann A.G. (2011) Peripheral antinociceptive effects of inhibitors of monoacylglycerol lipase in a rat model of inflammatory pain. Br. J. Pharmacol. 163, 1464–1478 10.1111/j.1476-5381.2010.01192.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Woodhams S., Wong A., Barrett D., Bennett A., Chapman V. and Alexander S. (2012) Spinal administration of the monoacylglycerol lipase inhibitor JZL184 produces robust inhibitory effects on nociceptive processing and the development of central sensitization in the rat. Br. J. Pharmacol. 167, 1609–1619 10.1111/j.1476-5381.2012.02179.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ghosh S., Wise L.E., Chen Y., Gujjar R., Mahadevan A. and Cravatt B.F (2013) The monoacylglycerol lipase inhibitor JZL184 suppresses inflammatory pain in the mouse carrageenan model. Life Sci. 92, 498–505 10.1016/j.lfs.2012.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Guindon J., Lai Y., Takacs S.M., Bradshaw H.B. and Hohmann A.G. (2013) Alterations in endocannabinoid tone following chemotherapy-induced peripheral neuropathy: effects of endocannabinoid deactivation inhibitors targeting fatty-acid amide hydrolase and monoacylglycerol lipase in comparison to reference analgesics following cisplatin treatment. Pharmacol. Res. 67, 94–109 10.1016/j.phrs.2012.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Khasabova I.A., Yao X., Paz J., Lewandowski C.T., Lindberg A.E. and Coicou L. (2014) JZL184 is anti-hyperalgesic in a murine model of cisplatin-induced peripheral neuropathy. Pharmacol. Res. 90, 67–75 10.1016/j.phrs.2014.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Ignatowska-Jankowska B.M., Ghosh S., Crowe M.S., Kinsey S.G., Niphakis M.J. and Abdullah R.A (2014) In vivo characterization of the highly selective monoacylglycerol lipase inhibitor KML29: antinociceptive activity without cannabimimetic side effects. Br. J. Pharmacol. 171, 1392–1407 10.1111/bph.12298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Crowe M.S., Wilson C.D., Leishman E., Prather P.L., Bradshaw H.B. and Banks M.L (2017) The monoacylglycerol lipase inhibitor KML29 with gabapentin synergistically produces analgesia in mice. Br. J. Pharmacol. 174, 4523–4539 10.1111/bph.14055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Crowe M.S., Leishman E., Banks M.L., Gujjar R., Mahadevan A. and Bradshaw H.B (2015) Combined inhibition of monoacylglycerol lipase and cyclooxygenases synergistically reduces neuropathic pain in mice. Br. J. Pharmacol. 172, 1700–1712 10.1111/bph.13012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Miller S., Leishman E., Hu S.S., Elghouche A., Daily L. and Murataeva N. (2016) Harnessing the Endocannabinoid 2-arachidonoylglycerol to lower intraocular pressure in a murine model. Invest. Ophthalmol. Vis. Sci. 257, 3287–3296 10.1167/iovs.16-19356 [DOI] [PMC free article] [PubMed] [Google Scholar]