ABSTRACT
Background
The Healthy Eating Index–2015 (HEI-2015) score measures adherence to recommendations from the 2015–2020 Dietary Guidelines for Americans. The HEI-2015 was altered from the HEI-2010 by reclassifying sources of dietary protein and replacing the empty calories component with 2 new components: saturated fats and added sugars.
Objectives
Our aim was to assess whether the HEI-2015 score, along with 3 other previously defined indices, were associated with incident cardiovascular disease (CVD), CVD mortality, and all-cause mortality.
Methods
We conducted a prospective analysis of 12,413 participants aged 45–64 y (56% women) from the Atherosclerosis Risk in Communities (ARIC) Study. The HEI-2015, Alternative Healthy Eating Index–2010 (AHEI-2010), alternate Mediterranean (aMed) diet, and Dietary Approaches to Stop Hypertension Trial (DASH) scores were computed using the average dietary intakes of Visits 1 (1987–1989) and 3 (1993–1995). Incident CVD, CVD mortality, and all-cause mortality data were ascertained from baseline through 31 December, 2017. We used Cox proportional hazards models to estimate HRs and 95% CIs.
Results
There were 4509 cases of incident CVD, 1722 cases of CVD mortality, and 5747 cases of all-cause mortality over a median of 24–25 y of follow-up. Compared with participants in the lowest quintile of HEI-2015, participants in the highest quintile had a 16% lower risk of incident CVD (HR: 0.84; 95% CI: 0.76–0.93; P-trend < 0.001), 32% lower risk of CVD mortality (HR: 0.68; 95% CI: 0.58–0.80; P-trend < 0.001), and 18% lower risk of all-cause mortality (HR: 0.82; 95% CI: 0.75–0.89; P-trend < 0.001) after adjusting for demographic and lifestyle covariates. There were similar protective associations for AHEI-2010, aMed, and DASH scores, and no significant interactions by race.
Conclusions
Higher adherence to the 2015–2020 Dietary Guidelines for Americans was associated with lower risks of incident CVD, CVD mortality, and all-cause mortality among US adults.
Keywords: ARIC, dietary pattern, dietary score, cardiovascular disease, mortality
Introduction
The 2015–2020 Dietary Guidelines for Americans highlights the importance of healthy eating patterns that represent the totality of foods and beverages habitually consumed, rather than individual dietary components and nutrients that were emphasized in previous editions (1). The components within an eating pattern may have interactive and cumulative health effects and, therefore, eating patterns have the potential to prevent chronic disease to a greater extent than the modification of 1 component (2). The Healthy Eating Index (HEI), which was developed to reflect the Dietary Guidelines; the Alternative Healthy Eating Index (AHEI), which consists of dietary components associated with chronic diseases; the alternate Mediterranean (aMed) diet; and the Dietary Approaches to Stop Hypertension Trial (DASH) diet (3–6) are 4 common indices used in nutrition epidemiology to assess healthy dietary patterns. Although the 4 indices have overlapping components, they each uniquely capture different combinations of food groups and have distinctive scoring methods.
The HEI-2015, based on the most recent 2015–2020 Dietary Guidelines for Americans, was updated from the HEI-2010 by including legumes in 4 components rather than 2 and splitting the empty calories component (which included solid fats, alcohols, and added sugars) into 2 components: added sugars and saturated fats (3). While previous studies have assessed the associations between earlier versions of the HEI (HEI-2005, HEI-2010) and chronic disease and mortality (4, 7, 8), it is not yet known whether the HEI-2015 is associated with cardiovascular disease (CVD), CVD mortality, or all-cause mortality risks. A study in the Multiethnic Cohort found an inverse association between the HEI-2015 score and all-cause mortality, CVD mortality, and cancer mortality among men and women (9). However, generalizability was limited, as participants were recruited from Hawaii and Los Angeles. Additional studies are needed to confirm these findings in other populations, as well as to examine the association with incident CVD. Previous observational studies have suggested that adhering to healthy dietary patterns may reduce risks of CVD, diabetes, and mortality (4, 7, 10–14).
The primary objective of our analysis was to examine whether the recently published HEI-2015 score is associated with CVD, CVD mortality, and all-cause mortality risks in the Atherosclerosis Risk in Communities (ARIC) study, a community-based population consisting of black and white participants. We also examined the associations with other dietary pattern indices (AHEI-2010, aMed, and DASH) that are frequently used to assess diet quality and are relevant to dietary guidance in the US population.
Methods
The ARIC study was a community-based, prospective cohort of 15,792 participants, aged 45–64 y at baseline, from 4 US communities (Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and Minneapolis suburbs, Minnesota) who were enrolled and examined from 1987 to 1989 (Visit 1) (15). Participants were also seen in person at Visit 2 (1990–1992; n = 14,348), Visit 3 (1993–1995; n = 12,887), Visit 4 (1996–1998; n = 11,656), Visit 5 (2011–2013; n = 6538), and Visit 6 (2016–2017; n = 4003), and Visit 7 is ongoing. The ARIC study was approved by the Institutional Review Boards of participating institutions, and participants provided written informed consent at each clinical site.
Participants who were neither black nor white (n = 48), black from Washington County, Maryland (n = 33), and black from Minneapolis, Minnesota (n = 22), were excluded from our analysis due to small numbers that did not accurately represent the minority groups within these study centers. Individuals with a history of coronary heart disease (n = 763), stroke (n = 186), or heart failure (n = 594) at baseline were not included. We additionally excluded participants who were missing data on covariates of interest (n = 1302), participants with extreme energy intakes (women: <500 or >3500 kcal/d; men: <700 or >4500 kcal/d; n = 75), and participants with incomplete FFQs (n = 356). Our final study population consisted of 12,413 participants.
Measurement of dietary intake
Dietary intake was assessed using an interviewer-administered, 66-item FFQ that was modified from the 61-item Willett questionnaire and has been validated in ARIC (16–18). The FFQ was administered at Visit 1 (1987–1989) and Visit 3 (1993–1995). Participants were asked by trained interviewers to report the average frequency of consuming food items of a given portion size in the past year. The total energy and nutrient intake was calculated by multiplying the self-reported frequency and portion size of each food item by the nutritional content, using US Department of Agriculture data sources. Cumulative updating of the FFQ by incorporating both Visits 1 and 3 was used to reduce the within-person variation and represent the long-term dietary intake (19). The Visit 1 dietary intake was used for participants who had a CVD event or were censored between Visits 1 and 3, or for those who were missing Visit 3 dietary data. For participants who were censored after Visit 3, we used the mean of their Visit 1 and Visit 3 dietary intakes.
Scoring of dietary patterns
HEI-2015, AHEI-2010, aMed, and DASH diet indices were used to assess adherence to healthy dietary patterns. The HEI-2015 score (ranging from 0–100 possible points) was created to assess adherence to the 2015–2020 US Dietary Guidelines for Americans, and consists of 13 components that were scored based on energy-adjusted food and nutrient intakes (Supplemental Table 1) (3). The AHEI-2010 score (0–110) was created to include foods, beverages, and nutrients associated with chronic diseases, based on previous literature (Supplemental Table 1) (4). The aMed score (0–9) was developed to assess adherence to a Mediterranean-style diet in the US population (Supplemental Table 1) (5). Due to the narrow range of scores in the aMed diet, as a sensitivity analysis, we modified the scoring using ranked distribution in quintiles for each component except alcohol, which was based on cutoffs (Supplemental Table 2). The range of possible scores for the modified aMed score was 9–45. The DASH score (8–40) was derived by Fung et al. (6) to reflect the DASH dietary pattern, which was tested in 2 randomized, controlled feedings trials (20, 21). The DASH score has 8 components that are each worth 5 points (Supplemental Table 1) (6).
Definition of outcomes
Our primary outcomes were incident CVD, CVD mortality, and all-cause mortality. Incident CVD events were a composite of incident coronary artery disease (CAD), incident stroke, and incident heart failure after Visit 1 through 31 December, 2017. CVD events were ascertained through: 1) annual telephone calls to cohort participants/proxies; 2) active surveillance of local hospital discharge records; 3) state death records; and 4) linkage to the National Death Index (15). Trained abstractors collected data on all CVD-related hospitalizations. CAD events were defined as a definite or probable myocardial infarction, fatal CAD by a physician review, or coronary revascularization (22). Definite or probable incident stroke was classified by physician reviewers and a computer algorithm, using criteria adapted from the National Survey of Stroke. Stroke was defined as a sudden neurologic insult of ≥24-h duration or a neurologic insult associated with death without evidence of a nonstroke cause of death. Heart failure was defined by a hospitalization or death with an International Classification of Diseases (ICD)-9 code 428 or ICD-10 code I50.
CVD mortality was defined as a death with CVD as the underlying cause (ICD-9 codes 390–459 or ICD-10 codes I00-I99). All-cause mortality was defined as any death subsequent to Visit 1 until the end of 2017, as determined by annual telephone calls, linkage to local hospital and state health department records, and linkage to the National Death Index.
Covariates
A questionnaire was administered to participants at baseline by trained interviewers to ascertain age, sex, race, education level, income level, physical activity [sport and nonsport exercise activity during leisure, from the Baecke questionnaire (23, 24)], smoking status, alcohol status, and medical history. Race and center were combined into a single variable (race center interaction term) given the nonuniform distribution of racial groups across centers. Education levels were categorized as less than high school, high school or equivalent, and college or higher. Income levels were categorized as an annual household income <$24,000, $24,000–49,999, and ≥$50,000. Smoking status and alcohol status were categorized as never, former, and current.
Statistical analysis
We summarized baseline characteristics of participants by quintiles of each dietary score. Differences in baseline characteristics by each score were assessed using the χ2 test and ANOVA. The correlations between dietary scores were calculated using Pearson's correlation. We used Cox proportional hazards regression models to calculate HRs and 95% CIs, to quantify the association between each dietary score and risks of CVD, CVD mortality, and all-cause mortality. We adjusted the analyses for potential confounders: age, sex, race center (interaction term), total energy intake, education level, income level, physical activity, and smoking status. Alcohol status was also adjusted for in analyses using HEI-2015 and DASH scores, because alcohol was not scored in those indices. We calculated P-trends using the median value of each quintile of a dietary score. HRs were calculated by quintiles of each dietary score and for each SD increase in a dietary score. We also conducted stratified analyses by race for each dietary score and tested for interactions using the likelihood ratio test. All analyses were performed using Stata (version 14.0; StataCorp).
Results
Participant characteristics
Baseline characteristics of the study population, according to lowest and highest quintiles of each dietary score, are shown in Table 1. Characteristics, by quintile, of each score are shown in Supplemental Tables 3–6. With respect to demographic and lifestyle characteristics, participants who had higher dietary scores were more likely to be female, have at least a college degree, have a higher income, never smoke, and be more physically active, compared to their counterparts with lower scores (Table 1). Supplemental Table 7 shows the mean consumption of individual HEI-2015 components, according to quintile. The correlation between dietary scores ranged from 0.59 (HEI-2015 and aMed) to 0.79 (HEI-2015 and DASH).
TABLE 1.
Baseline characteristics of Atherosclerosis Risk in Communities participants in lowest and highest quintiles of dietary scores1
| HEI-2015 | AHEI-2010 | aMed | DASH | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Q1: 602 | Q5: 81 | Q1: 37 | Q5: 67 | Q1: 2 | Q5: 6 | Q1: 18 | Q5: 30 |
| n | 2483 | 2482 | 2483 | 2482 | 2381 | 3071 | 3094 | 2398 |
| Age, y | 54 ± 6 | 55 ± 6 | 53 ± 6 | 55 ± 6 | 53 ± 6 | 54 ± 6 | 53 ± 6 | 55 ± 6 |
| Female, % | 40 | 70 | 49 | 63 | 57 | 55 | 41 | 73 |
| Black, % | 23 | 21 | 28 | 17 | 19 | 24 | 36 | 14 |
| Education level, % | ||||||||
| <High school | 31 | 13 | 29 | 13 | 25 | 16 | 34 | 13 |
| High school or equivalent | 44 | 39 | 43 | 40 | 46 | 38 | 42 | 38 |
| ≥College | 25 | 47 | 28 | 47 | 29 | 46 | 25 | 49 |
| Annual household income, % | ||||||||
| <$24,000 | 40 | 31 | 42 | 30 | 37 | 32 | 45 | 29 |
| $24,000–$49,999 | 39 | 38 | 38 | 39 | 40 | 37 | 38 | 39 |
| ≥$50,000 | 21 | 32 | 21 | 31 | 23 | 30 | 17 | 32 |
| Smoking status, % | ||||||||
| Never smoker | 31 | 49 | 40 | 43 | 40 | 45 | 33 | 50 |
| Former smoker | 29 | 35 | 27 | 37 | 28 | 35 | 29 | 35 |
| Current smoker | 40 | 15 | 33 | 20 | 32 | 20 | 38 | 15 |
| Alcohol status, % | ||||||||
| Never drinker | 19 | 26 | 27 | 21 | 23 | 24 | 24 | 24 |
| Former drinker | 21 | 16 | 22 | 15 | 20 | 16 | 21 | 16 |
| Current drinker | 60 | 58 | 51 | 64 | 57 | 60 | 55 | 60 |
| Physical activity index score3 | 2.3 ± 0.7 | 2.7 ± 0.8 | 2.3 ± 0.7 | 2.7 ± 0.8 | 2.3 ± 0.8 | 2.6 ± 0.8 | 2.2 ± 0.7 | 2.7 ± 0.8 |
| Total energy intake, kcal/d | 1633 ± 602 | 1330 ± 418 | 1400 ± 497 | 1626 ± 479 | 1312 ± 467 | 1672 ± 515 | 1620 ± 562 | 1403 ± 424 |
Values for categorical variables are given as percentages; for continuous variables, means ± SDs. AHEI, Alternative Healthy Eating Index; aMed, alternate Mediterranean diet; DASH, Dietary Approaches to Stop Hypertension Trial; HEI, Healthy Eating Index; Q, quintile.
Median score of quintile.
Physical activity index scores were calculated based on intensity and time of sport and nonsport exercise during leisure time; 1 is lowest and 5 is highest.
Dietary patterns and risks
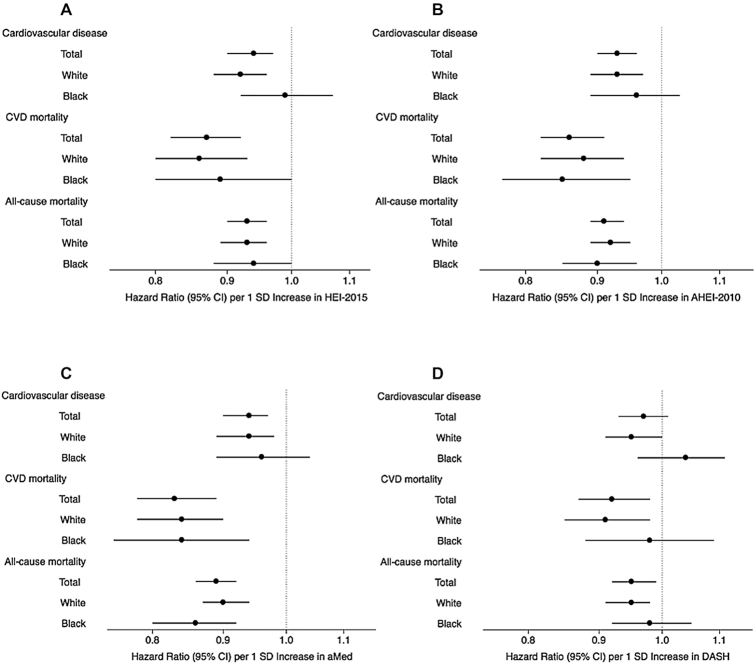
During a median follow-up time of 24 y, 4509 cases of incident CVD occurred. After adjustment for age, sex, race center, total energy intake, education level, income level, physical activity, smoking status, and alcohol status, participants in the highest quintile of HEI-2015 had a 16% (HR: 0.84; 95% CI: 0.76–0.93) lower risk of incident CVD, compared to participants in quintile 1 (Tables 2–5). Participants in the highest quintiles of AHEI-2010, aMed, and DASH had, respectively, 15% (HR: 0.85; 95% CI: 0.77–0.93), 16% (HR: 0.84; 95% CI: 0.77–0.93), and 11% (HR: 0.89: 95% CI: 0.81–0.99) lower risks of CVD, compared to participants in the lowest quintiles. For each additional increase in the SD of a dietary score, the risk of CVD was reduced by 3–7% (Figure 1).
TABLE 2.
Risks, by quintiles, of Healthy Eating Index among Atherosclerosis Risk in Communities participants1
| Q1: 602 (n = 2483) | Q2: 67 (n = 2483) | Q3: 71 (n = 2482) | Q4: 75 (n = 2483) | Q5: 81 (n = 2482) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 1041 | 913 | 904 | 845 | 806 | — |
| Incidence rate4 | 22.1 | 17.8 | 17.0 | 15.5 | 14.5 | — |
| HR (95% CI) | 1 (ref.) | 0.87 (0.79–0.95) | 0.89 (0.81–0.98) | 0.84 (0.77–0.93) | 0.84 (0.76–0.93) | <0.001 |
| CVD mortality | ||||||
| Cases, n | 425 | 372 | 338 | 309 | 278 | — |
| Incidence rate4 | 8.3 | 7.0 | 6.2 | 5.6 | 5.0 | — |
| HR (95% CI) | 1 (ref.) | 0.81 (0.71–0.94) | 0.75 (0.65–0.87) | 0.76 (0.65–0.89) | 0.68 (0.58–0.80) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 1333 | 1225 | 1096 | 1063 | 1030 | — |
| Incidence rate4 | 25.7 | 22.7 | 19.7 | 19.0 | 18.2 | — |
| HR (95% CI) | 1 (ref.) | 0.90 (0.83–0.97) | 0.85 (0.78–0.92) | 0.87 (0.80–0.95) | 0.82 (0.75–0.89) | <0.001 |
Cox proportional hazards models used to estimate HRs and 95% CIs were adjusted for age, sex, race center (interaction term), total energy intake, education level, income level, physical activity, and smoking status, as well as alcohol status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 5.
Risks, by quintiles, of Dietary Approaches to Stop Hypertension Trial among Atherosclerosis Risk in Communities participants1
| Q1: 182 (n = 3094) | Q2: 22 (n = 2447) | Q3: 25 (n = 2791) | Q4: 27 (n = 1683) | Q5: 30 (n = 2398) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 1248 | 908 | 998 | 602 | 753 | — |
| Incidence rate4 | 20.7 | 17.8 | 16.6 | 16.6 | 13.9 | — |
| HR (95% CI) | 1 (ref.) | 0.97 (0.89–1.05) | 0.99 (0.91–1.08) | 1.00 (0.90–1.11) | 0.89 (0.81–0.99) | 0.1 |
| CVD mortality | ||||||
| Cases, n | 534 | 336 | 357 | 211 | 284 | — |
| Incidence rate4 | 8.3 | 6.4 | 5.8 | 5.6 | 5.2 | — |
| HR (95% CI) | 1 (ref.) | 0.90 (0.78–1.03) | 0.91 (0.79–1.05) | 0.91 (0.77–1.07) | 0.79 (0.68–0.93) | 0.01 |
| All-cause mortality | ||||||
| Cases, n | 1637 | 1156 | 1221 | 729 | 1004 | — |
| Incidence rate4 | 25.0 | 21.6 | 19.5 | 19.3 | 18.3 | — |
| HR (95% CI) | 1 (ref.) | 0.94 (0.87–1.02) | 0.96 (0.88–1.03) | 0.93 (0.85–1.02) | 0.88 (0.80–0.96) | 0.01 |
Cox proportional hazards models used to estimate HRs and 95% CIs were adjusted for age, sex, race center (interaction term), total energy intake, education level, income level, physical activity, and smoking status, as well as alcohol status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
FIGURE 1.
HRs (on logarithmic scale) of CVD, CVD mortality, and all-cause mortality per 1 SD increase of each dietary score among ARIC participants, stratified by race. (A) HEI-2015; (B) AHEI-2010; (C) aMed; and (D) DASH. SD for HEI-2015 = 8.3; AHEI-2010 = 11.8; aMed = 1.8; and DASH = 4.9. Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, race center (interaction term), total energy intake, education level, income level, physical activity, and smoking status. HEI-2015 and DASH scores were additionally adjusted for alcohol status. AHEI, Alternative Healthy Eating Index; aMed, alternate Mediterranean diet; ARIC, Atherosclerosis Risk in Communities; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension Trial; HEI, Healthy Eating Index.
TABLE 3.
Risks, by quintiles, of Alternative Healthy Eating Index among Atherosclerosis Risk in Communities participants1
| Q1: 372 (n = 2483) | Q2: 45 (n = 2483) | Q3: 51 (n = 2482) | Q4: 57 (n = 2483) | Q5: 67 (n = 2482) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 987 | 955 | 860 | 852 | 855 | — |
| Incidence rate4 | 19.9 | 18.7 | 16.3 | 15.9 | 15.6 | — |
| HR (95% CI) | 1 (ref.) | 0.96 (0.87–1.05) | 0.84 (0.77–0.93) | 0.84 (0.77–0.92) | 0.85 (0.77–0.93) | <0.001 |
| CVD mortality | ||||||
| Cases, n | 420 | 346 | 327 | 333 | 296 | — |
| Incidence rate4 | 8.0 | 6.5 | 6.0 | 6.1 | 5.3 | — |
| HR (95% CI) | 1 (ref.) | 0.85 (0.74–0.98) | 0.83 (0.72–0.96) | 0.78 (0.67–0.90) | 0.66 (0.57–0.77) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 1203 | 1214 | 1148 | 1107 | 1075 | — |
| Incidence rate4 | 22.8 | 22.4 | 20.9 | 20.0 | 19.0 | — |
| HR (95% CI) | 1 (ref.) | 0.95 (0.88–1.03) | 0.92 (0.85–1.00) | 0.84 (0.78–0.92) | 0.80 (0.73–0.87) | <0.001 |
Cox proportional hazards models used to estimate HRs and 95% CIs were adjusted for age, sex, race center (interaction term), total energy intake, education level, income level, physical activity, and smoking status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 4.
Risks, by quintiles, of alternate Mediterranean diet among Atherosclerosis Risk in Communities participants1
| Q1: 22 (n = 2381) | Q2: 3 (n = 2216) | Q3: 4 (n = 2501) | Q4: 5 (n = 2244) | Q5: 6 (n = 3071) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 892 | 809 | 927 | 813 | 1068 | — |
| Incidence rate4 | 18.2 | 17.6 | 17.7 | 17.1 | 15.9 | — |
| HR (95% CI) | 1 (ref.) | 0.93 (0.84–1.02) | 0.94 (0.86–1.03) | 0.91 (0.82–1.00) | 0.84 (0.77–0.93) | <0.001 |
| CVD mortality | ||||||
| Cases, n | 353 | 330 | 342 | 308 | 389 | — |
| Incidence rate4 | 6.9 | 6.9 | 6.3 | 6.3 | 5.6 | — |
| HR (95% CI) | 1 (ref.) | 0.94 (0.81–1.09) | 0.86 (0.74–0.99) | 0.77 (0.66–0.91) | 0.66 (0.57–0.77) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 1123 | 1046 | 1191 | 1040 | 1347 | — |
| Incidence rate4 | 21.8 | 21.7 | 21.7 | 20.8 | 19.3 | — |
| HR (95% CI) | 1 (ref.) | 0.93 (0.86–1.01) | 0.93 (0.86–1.01) | 0.84 (0.77–0.91) | 0.76 (0.70–0.83) | <0.001 |
Cox proportional hazards models used to estimate HRs and 95% CIs were adjusted for age, sex, race center (interaction term), total energy intake, education level, income level, physical activity, and smoking status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
There were 1722 deaths due to CVD during a median follow-up of 25 y. After adjustment for covariates, participants in the highest quintiles of HEI-2015, AHEI-2010, aMed, and DASH scores had, respectively, 32% (HR: 0.68; 95% CI: 0.58–0.80), 34% (HR: 0.66; 95% CI: 0.57–0.77), 34% (HR: 0.66; 95% CI: 0.57–0.77), and 21% (HR: 0.79; 95% CI: 0.68–0.93) lower risks of CVD mortality (Tables 2–5). Each additional increase in the SD of a dietary score reduced the risk of CVD mortality by 8–17% (Figure 1).
We documented 5747 deaths due to any cause over a median follow-up time of 25 y. The highest quintiles of HEI-2015, AHEI-2010, aMed, and DASH scores were, respectively, associated with 18% (HR: 0.82; 95% CI: 0.75–0.89), 20% (HR: 0.80; 95% CI: 0.73–0.87), 24% (HR: 0.76; 95% CI: 0.70–0.83), and 12% (HR: 0.88; 95% CI: 0.80–0.96) lower risks of all-cause mortality, after adjustment for covariates (Tables 2–5). Each additional SD increase in a dietary score was associated with a 4–11% lower risk of all-cause mortality (Figure 1).
Sensitivity analyses
When we stratified our analyses by race, we found similar relative measures of association between white and black participants (P-interactions > 0.05; Tables 6–13). The estimates for whites were similar to the estimates for the total population (Tables 6–9). However, for black participants, none of the dietary patterns were associated with CVD (Tables 10–13; Figure 1). Among black participants, the AHEI-2010 and aMed were associated with reduced risks of CVD mortality and all-cause mortality, and the DASH score was not significantly associated with any of the outcomes.
TABLE 6.
Risks, by quintiles, of Healthy Eating Index among white Atherosclerosis Risk in Communities participants1
| Q1: 602 (n = 1914) | Q2: 67 (n = 1835) | Q3: 71 (n = 1822) | Q4: 75 (n = 1939) | Q5: 81 (n = 1963) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 794 | 667 | 639 | 625 | 602 | — |
| Incidence rate4 | 21.3 | 17.3 | 16.1 | 14.5 | 13.5 | — |
| HR (95% CI) | 1 (ref.) | 0.89 (0.80–0.99) | 0.88 (0.79–0.98) | 0.82 (0.74–0.92) | 0.82 (0.73–0.92) | <0.001 |
| CVD mortality | ||||||
| Cases, n | 293 | 244 | 219 | 208 | 196 | — |
| Incidence rate4 | 7.3 | 6.1 | 5.4 | 4.7 | 4.4 | — |
| HR (95% CI) | 1 (ref.) | 0.82 (0.69–0.98) | 0.76 (0.63–0.91) | 0.79 (0.66–0.96) | 0.66 (0.54–0.81) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 994 | 870 | 763 | 801 | 792 | — |
| Incidence rate4 | 24.3 | 21.5 | 18.4 | 18.0 | 17.5 | — |
| HR (95% CI) | 1 (ref.) | 0.92 (0.84–1.01) | 0.85 (0.77–0.94) | 0.89 (0.81–0.98) | 0.81 (0.74–0.90) | <0.001 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status, as well as alcohol status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 13.
Risks, by quintiles, of Dietary Approaches to Stop Hypertension Trial among black Atherosclerosis Risk in Communities participants1
| Q1: 182 (n = 1121) | Q2: 22 (n = 619) | Q3: 25 (n = 578) | Q4: 27 (n = 293) | Q5: 30 (n = 329) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 456 | 245 | 240 | 121 | 120 | — |
| Incidence rate4 | 21.6 | 19.8 | 19.7 | 20.0 | 17.3 | — |
| HR (95% CI) | 1 (ref.) | 1.03 (0.88–1.20) | 1.12 (0.85–1.32) | 1.15 (0.93–1.41) | 1.01 (0.82–1.25) | 0.3 |
| CVD mortality | ||||||
| Cases, n | 239 | 111 | 112 | 51 | 49 | — |
| Incidence rate4 | 10.6 | 8.7 | 9.0 | 8.2 | 6.9 | — |
| HR (95% CI) | 1 (ref.) | 1.00 (0.79–1.25) | 1.06 (0.84–1.33) | 1.02 (0.74–1.39) | 0.87 (0.63–1.20) | 0.7 |
| All-cause mortality | ||||||
| Cases, n | 641 | 319 | 277 | 138 | 152 | — |
| Incidence rate4 | 28.2 | 24.8 | 22.2 | 21.8 | 21.2 | — |
| HR (95% CI) | 1 (ref.) | 1.00 (0.88–1.15) | 1.00 (0.87–1.16) | 1.01 (0.83–1.22) | 0.93 (0.77–1.12) | 0.6 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status, as well as alcohol status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 9.
Risks, by quintiles, of Dietary Approaches to Stop Hypertension Trial among white Atherosclerosis Risk in Communities participants1
| Q1: 182 (n = 1973) | Q2: 22 (n = 1828) | Q3: 25 (n = 2213) | Q4: 27 (n = 1390) | Q5: 31 (n = 2069) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 792 | 663 | 758 | 481 | 633 | — |
| Incidence rate4 | 20.2 | 17.2 | 15.8 | 15.9 | 13.4 | — |
| HR (95% CI) | 1 (ref.) | 0.93 (0.84–1.03) | 0.94 (0.85–1.04) | 0.96 (0.85–1.08) | 0.86 (0.77–0.97) | 0.03 |
| CVD mortality | ||||||
| Cases, n | 295 | 225 | 245 | 160 | 235 | — |
| Incidence rate4 | 7.0 | 5.6 | 5.0 | 5.1 | 5.0 | — |
| HR (95% CI) | 1 (ref.) | 0.86 (0.72–1.02) | 0.85 (0.72–1.02) | 0.87 (0.71–1.06) | 0.78 (0.64–0.94) | 0.01 |
| All-cause mortality | ||||||
| Cases, n | 996 | 837 | 944 | 591 | 852 | — |
| Incidence rate4 | 23.4 | 20.6 | 18.8 | 18.8 | 17.8 | — |
| HR (95% CI) | 1 (ref.) | 0.91 (0.83–1.00) | 0.93 (0.85–1.02) | 0.91 (0.81–1.01) | 0.86 (0.77–0.95) | 0.01 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status, as well as alcohol status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 10.
Risks, by quintiles, of Healthy Eating Index among black Atherosclerosis Risk in Communities participants1
| Q1: 602 (n = 569) | Q2: 67 (n = 648) | Q3: 71 (n = 660) | Q4: 75 (n = 544) | Q5: 81 (n = 519) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 247 | 246 | 265 | 220 | 204 | — |
| Incidence rate4 | 24.9 | 19.1 | 19.4 | 19.5 | 18.6 | — |
| HR (95% CI) | 1 (ref.) | 0.81 (0.68–0.97) | 0.90 (0.76–1.08) | 0.93 (0.77–1.12) | 0.94 (0.77–1.15) | 0.9 |
| CVD mortality | ||||||
| Cases, n | 132 | 128 | 119 | 101 | 82 | — |
| Incidence rate4 | 12.2 | 9.6 | 8.5 | 8.8 | 7.3 | — |
| HR (95% CI) | 1 (ref.) | 0.80 (0.62–1.02) | 0.74 (0.57–0.95) | 0.75 (0.58–0.99) | 0.76 (0.57–1.02) | 0.04 |
| All-cause mortality | ||||||
| Cases, n | 339 | 355 | 333 | 262 | 238 | — |
| Incidence rate4 | 30.9 | 26.3 | 23.6 | 22.5 | 20.9 | — |
| HR (95% CI) | 1 (ref.) | 0.84 (0.73–0.98) | 0.83 (0.71–0.97) | 0.83 (0.70–0.98) | 0.85 (0.71–1.01) | 0.05 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status, as well as alcohol status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 7.
Risks, by quintiles, of Alternative Healthy Eating Index among white Atherosclerosis Risk in Communities participants1
| Q1: 372 (n = 1800) | Q2: 45 (n = 1817) | Q3: 51 (n = 1886) | Q4: 57 (n = 1906) | Q5: 67 (n = 2064) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 700 | 665 | 632 | 638 | 692 | — |
| Incidence rate4 | 18.9 | 17.5 | 15.5 | 15.4 | 15.0 | — |
| HR (95% CI) | 1 (ref.) | 0.95 (0.86–1.06) | 0.84 (0.75–0.94) | 0.85 (0.76–0.95) | 0.84 (0.75–0.93) | <0.001 |
| CVD mortality | ||||||
| Cases, n | 256 | 210 | 232 | 226 | 236 | — |
| Incidence rate4 | 6.6 | 5.3 | 5.5 | 5.3 | 5.0 | — |
| HR (95% CI) | 1 (ref.) | 0.85 (0.70–1.02) | 0.90 (0.75–1.08) | 0.83 (0.69–1.00) | 0.68 (0.56–0.82) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 812 | 863 | 844 | 826 | 875 | — |
| Incidence rate4 | 20.6 | 21.4 | 19.9 | 19.2 | 18.4 | — |
| HR (95% CI) | 1 (ref.) | 1.01 (0.91–1.11) | 0.96 (0.87–1.06) | 0.89 (0.81–0.98) | 0.82 (0.74–0.90) | <0.001 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 8.
Risks, by quintiles, of alternate Mediterranean diet among white Atherosclerosis Risk in Communities participants1
| Q1: 22 (n = 1926) | Q2: 3 (n = 1678) | Q3: 4 (n = 1887) | Q4: 5 (n = 1655) | Q5: 6 (n = 2327) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 711 | 588 | 676 | 578 | 774 | — |
| Incidence rate4 | 17.6 | 16.4 | 16.8 | 16.3 | 15.1 | — |
| HR (95% CI) | 1 (ref.) | 0.90 (0.81–1.01) | 0.93 (0.84–1.04) | 0.91 (0.82–1.02) | 0.83 (0.74–0.92) | <0.001 |
| CVD mortality | ||||||
| Cases, n | 247 | 210 | 237 | 198 | 268 | — |
| Incidence rate4 | 5.9 | 5.7 | 5.7 | 5.4 | 5.1 | — |
| HR (95% CI) | 1 (ref.) | 0.87 (0.72–1.05) | 0.92 (0.77–1.11) | 0.79 (0.65–0.95) | 0.65 (0.54–0.78) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 876 | 744 | 855 | 740 | 1005 | — |
| Incidence rate4 | 20.7 | 19.9 | 20.3 | 19.8 | 18.8 | — |
| HR (95% CI) | 1 (ref.) | 0.88 (0.80–0.98) | 0.93 (0.84–1.02) | 0.84 (0.76–0.93) | 0.77 (0.70–0.85) | <0.001 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 11.
Risks, by quintiles, of Alternative Healthy Eating Index among black Atherosclerosis Risk in Communities participants1
| Q1: 372 (n = 683) | Q2: 45 (n = 666) | Q3: 51 (n = 596) | Q4: 57 (n = 577) | Q5: 66 (n = 418) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 287 | 290 | 228 | 214 | 163 | — |
| Incidence rate4 | 22.8 | 22.2 | 18.9 | 17.6 | 18.5 | — |
| HR (95% CI) | 1 (ref.) | 0.99 (0.84–1.16) | 0.88 (0.74–1.05) | 0.86 (0.72–1.03) | 0.96 (0.78–1.18) | 0.3 |
| CVD mortality | ||||||
| Cases, n | 164 | 136 | 95 | 107 | 60 | — |
| Incidence rate4 | 12.3 | 9.9 | 7.7 | 8.6 | 6.6 | — |
| HR (95% CI) | 1 (ref.) | 0.87 (0.69–1.09) | 0.74 (0.57–0.96) | 0.75 (0.58–0.96) | 0.68 (0.50–0.92) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 391 | 351 | 304 | 281 | 200 | — |
| Incidence rate4 | 29.1 | 25.3 | 24.3 | 22.4 | 21.8 | — |
| HR (95% CI) | 1 (ref.) | 0.85 (0.73–0.98) | 0.85 (0.73–0.99) | 0.76 (0.65–0.89) | 0.79 (0.66–0.94) | <0.001 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
TABLE 12.
Risks, by quintiles, of alternate Mediterranean diet among black Atherosclerosis Risk in Communities participants1
| Q1: 22 (n = 455) | Q2: 3 (n = 538) | Q3: 4 (n = 614) | Q4: 5 (n = 589) | Q5: 6 (n = 744) | P-trend3 | |
|---|---|---|---|---|---|---|
| Cardiovascular disease | ||||||
| Cases, n | 181 | 221 | 251 | 235 | 294 | — |
| Incidence rate4 | 21.1 | 21.9 | 20.7 | 19.5 | 18.6 | — |
| HR (95% CI) | 1 (ref.) | 1.03 (0.85–1.26) | 0.98 (0.71–1.19) | 0.94 (0.77–1.15) | 0.95 (0.78–1.15) | 0.4 |
| CVD mortality | ||||||
| Cases, n | 106 | 120 | 105 | 110 | 121 | — |
| Incidence rate4 | 11.6 | 11.3 | 8.3 | 8.9 | 7.5 | — |
| HR (95% CI) | 1 (ref.) | 1.05 (0.81–1.37) | 0.74 (0.56–0.97) | 0.79 (0.60–1.05) | 0.72 (0.54–0.95) | <0.001 |
| All-cause mortality | ||||||
| Cases, n | 247 | 302 | 336 | 300 | 342 | — |
| Incidence rate4 | 26.8 | 28.3 | 26.4 | 23.9 | 20.8 | — |
| HR (95% CI) | 1 (ref.) | 1.06 (0.90–1.26) | 0.93 (0.79–1.10) | 0.84 (0.71–1.00) | 0.75 (0.63–0.90) | <0.001 |
Cox proportional hazards models to estimate HRs and 95% CIs were adjusted for age, sex, center, total energy intake, education level, income level, physical activity, and smoking status. CVD, cardiovascular disease; Q, quintile; ref., reference.
Median score of quintile.
Trend was tested using the median value within each quintile.
Crude incidence rate per 1000 person-years.
In our sensitivity analysis, using a modified version of the aMed score for a wider distribution of scores, results were similar to the original aMed scoring (Supplemental Table 8).
Discussion
In our analysis of 12,413 participants from the ARIC study, we observed inverse associations for the HEI-2015 score and incident CVD, CVD mortality, and all-cause mortality. Findings for the AHEI-2010 and aMed were generally consistent and DASH was slightly weaker but still consistent, compared to the HEI-2015. The strongest associations were observed for CVD mortality, in which the highest adherence (quintile 5) to the healthy dietary patterns were associated with 21–34% reductions in risk, compared to participants with the lowest adherence (quintile 1). Participants in quintile 5 had 11–16% reduced risks for incident CVD and 12–24% reduced risks of all-cause mortality, compared to participants in quintile 1. Results were significant for almost all quintiles, suggesting that even small improvements in diet quality may reduce risks of CVD and mortality.
Our results were consistent with previous studies that reported inverse associations between healthy dietary patterns and CVD, CVD mortality, and all-cause mortality (7, 12). The Dietary Patterns Methods Project used a standardized approach to synthesize findings from 3 cohorts (NIH-American Association of Retired Persons Diet and Health Study, the Multiethnic Cohort, and the Women's Health Initiative Observational Study) to assess the associations between HEI-2010, AHEI-2010, aMed, and DASH scores and risks of CVD mortality, cancer mortality, and all-cause mortality (7). The authors observed 11–28% reductions in risks of death from all causes, CVD, and cancer when comparing the highest quintile of dietary scores to the lowest quintile, after adjusting for similar confounders as those used in our study (7). Other studies have found similar protective findings for cardiovascular events and total and cardiovascular mortality with the HEI (4, 8), AHEI (4, 8, 25), Mediterranean diet (13, 26), and DASH diet (6, 8) indices. The majority of these studies were conducted in Caucasian cohorts; therefore, generalizability was limited and it was unclear whether the associations were replicable among black participants. Our analysis in ARIC found that the associations between HEI-2015 scores and incident CVD, CVD mortality, and all-cause mortality were similar in direction and magnitude for white and black participants, and there were no significant interactions. However, there were no significant associations between dietary scores and CVD among black participants. This may be due to the small sample size of black participants (24% of the entire study population).
Although some of these scores have been previously examined, a novel aspect of this study was the use of the HEI-2015 index, which was updated from the HEI-2010 with the release of the 2015–2020 Dietary Guidelines for Americans. The HEI-2015 differs from the previous version by including legumes in the scoring of 4 components (total vegetables, greens and beans, total protein, and seafood and plant protein) rather than 2 and separating the empty calories (solid fats, alcohols, and added sugars) component into 2 separate components (saturated fats and added sugars) (3). To date, 1 study in the Multiethnic Cohort has examined the associations between the HEI-2015 and all-cause, CVD, and cancer mortality, and found inverse associations similar to those found in our study (9). In their study, they found that the risk of all-cause mortality was 21% lower (HR for quintile 5 compared with 1: 0.79; 95% CI: 0.76–0.82) for both men and women and the risks of CVD mortality were 24% lower (HR: 0.76; 95% CI: 0.71–0.82) for men and 25% lower (HR: 0.75; 95% CI: 0.70–0.81) for women (9). In our study, we also found a stronger association between healthy diet and CVD mortality, compared to all-cause mortality.
In the present study, all 4 indices performed similarly with regards to risks of incident CVD, CVD mortality, and all-cause mortality, suggesting that each of these healthy dietary patterns can be recommended and incorporated into healthy lifestyles, despite some differences in scoring criteria. There are some similarities and differences worth highlighting. All 4 indices included vegetables, fruits, and whole grains. Components that were unique to the HEI-2015 included refined grains, all dairy, the unsaturated/saturated fat ratio, saturated fats, and added sugars. Component groups that were not defined as 1 of the 13 groups in the HEI-2015 but were, to a variable extent, in the other 3 scores included low-fat dairy, sugar-sweetened beverages, nuts and legumes, red/processed meat, fish, trans fat, long-chain fats, polyunsaturated fats, and alcohol. Additionally, some food items contributed to multiple components; for example, whole fruits were counted in 2 components (total fruits and whole fruits) and beans were counted in 4 components (total vegetables, greens and beans, total protein, and seafood and plant proteins).
Along with the previous literature, our findings confirm the legitimacy of using dietary patterns as a holistic measure of overall dietary intake and highlight the importance of national dietary guidelines. Although the HEI-2015 appeared to have the strongest associations with the outcomes of all 4 dietary indices assessed, the differences among HRs between indices were marginal and, therefore, we cannot conclude that the HEI-2015 is superior in that regard. However, the HEI index may be considered a strong index, because it is constantly being improved upon with each update of the Dietary Guidelines, as our scientific knowledge and understanding of diets and health are cumulating.
A limitation of this study was self-reported dietary intakes, which may have resulted in measurement errors. However, the FFQs were administered in person by trained interviewers. Furthermore, we used a cumulative average approach to make use of 2 FFQs that were administered ∼6 y apart, when available, in order to use a more precise estimate of diet. Another limitation is that, although food intakes were most likely correctly ranked because of the nature of the FFQ, nutrient intakes were most likely underestimated. Despite adjusting for many covariates that were potential confounders, it is possible that there was still residual confounding. Associations between individual components of the scores were not examined in this analysis, given our focus on a holistic measure of diet that accounts for potential interactions between components. Our findings suggest that there are different ways to define a healthy dietary pattern, and they may each have similar effects on clinical outcomes.
There were several strengths in our study, including the use of trained interviewers to administer the FFQ, a prospective design, a relatively long follow-up period, rigorous ascertainment of CVD morbidity and mortality through active ascertainment and linkage to death records, and a large cohort with sufficient power to detect statistically significant associations.
In conclusion, we found that a higher diet quality, characterized by the HEI-2015 and 3 other dietary indices, was associated with reduced risks of incident CVD, CVD mortality, and all-cause mortality in a prospective cohort of 12,413 black and white adults. Our findings add evidence to the protective associations between the HEI-2015 score and cardiovascular and death outcomes, as well as corroborate previous literature on the AHEI-2010, aMed, and DASH scores.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—EAH, CMR: designed the research plan, analyzed the data, and had primary responsibility for the final content; EAH: wrote the paper; and all authors: read and approved the final manuscript.
Notes
The Atherosclerosis Risk in Communities (ARIC) Study has been funded in whole or in part with federal funds from the National Heart, Lung, and Blood Institute, NIH, and the Department of Health and Human Services (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700004I, and HHSN268201700005I).
Author disclosures: LMS, JC, and LJA, no conflicts of interest. EAH is supported by a grant from the NIH/National Heart, Lung, and Blood Institute (training grant T32 HL007024). CMR is supported by a mentored research scientist development award from the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK107782) and a grant from the National Heart, Lung, and Blood Institute (R21 HL143089).
Supplemental Tables 1–8 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn.
Abbreviations used: AHEI, Alternative Healthy Eating Index; aMed, alternate Mediterranean diet; ARIC, Atherosclerosis Risk in Communities; CAD, coronary artery disease; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension Trial; HEI, Healthy Eating Index; ICD, International Classification of Diseases.
References
- 1. US Department of Health and Human Services, US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. [Internet]. Available from: http://health.gov/dietaryguidelines/2015/guidelines/. [Google Scholar]
- 2. Hu FB. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9. [DOI] [PubMed] [Google Scholar]
- 3. Krebs-Smith SM, Pannucci TE, Subar AF, Kirkpatrick SI, Lerman JL, Tooze JA, Wilson MM, Reedy J. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N, Willett WC, Hu FB. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2005;82(1):163–73. [DOI] [PubMed] [Google Scholar]
- 6. Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20. [DOI] [PubMed] [Google Scholar]
- 7. Liese AD, Krebs-Smith SM, Subar AF, George SM, Harmon BE, Neuhouser ML, Boushey CJ, Schap TE, Reedy J. The Dietary Patterns Methods Project: Synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145(3):393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating index, the Dietary Approaches to Stop Hypertension score, and health outcomes: A systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780–800.e5. [DOI] [PubMed] [Google Scholar]
- 9. Panizza CE, Shvetsov YB, Harmon BE, Wilkens LR, Le Marchand L, Haiman C, Reedy J, Boushey CJ. Testing the predictive validity of the healthy eating Index-2015 in the multiethnic cohort: Is the score associated with a reduced risk of all-cause and cause-specific mortality?. Nutrients. 2018;10(4):E452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rodriguez-Monforte M, Flores-Mateo G, Sanchez E. Dietary patterns and CVD: A systematic review and meta-analysis of observational studies. Br J Nutr. 2015;114(9):1341–59. [DOI] [PubMed] [Google Scholar]
- 11. Jannasch F, Kroger J, Schulze MB. Dietary patterns and type 2 diabetes: A systematic literature review and meta-analysis of prospective studies. J Nutr. 2017;147(6):1174–82. [DOI] [PubMed] [Google Scholar]
- 12. Akbaraly TN, Ferrie JE, Berr C, Brunner EJ, Head J, Marmot MG, Singh-Manoux A, Ritchie K, Shipley MJ, Kivimaki M. Alternative healthy eating index and mortality over 18 y of follow-up: Results from the Whitehall II cohort. Am J Clin Nutr. 2011;94(1):247–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol. 2014;25(1):20–6. [DOI] [PubMed] [Google Scholar]
- 14. Tobias DK, Hu FB, Chavarro J, Rosner B, Mozaffarian D, Zhang C. Healthful dietary patterns and type 2 diabetes mellitus risk among women with a history of gestational diabetes mellitus. Arch Intern Med. 2012;172(20):1566–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The Atherosclerosis Risk in Communities (ARIC). Study: Design and objectives. The ARIC investigators Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 16. Stevens J, Metcalf PA, Dennis BH, Tell GS, Shimakawa T, Folsom AR. Reliability of a food frequency questionnaire by ethnicity, gender, age and education. Nutrition Research. 1996;16(5):735–45. [Google Scholar]
- 17. Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. [DOI] [PubMed] [Google Scholar]
- 18. Shimakawa T, Sorlie P, Carpenter MA, Dennis B, Tell GS, Watson R, Williams OD. Dietary intake patterns and sociodemographic factors in the atherosclerosis risk in communities study.Prev Med. 1994;23(6):769–80. [DOI] [PubMed] [Google Scholar]
- 19. Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, Willett WC. Dietary fat and coronary heart disease: A comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149(6):531–40. [DOI] [PubMed] [Google Scholar]
- 20. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM et al.. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117–24. [DOI] [PubMed] [Google Scholar]
- 21. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton 3rd DG et al.. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344(1):3–10. [DOI] [PubMed] [Google Scholar]
- 22. White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) study: Methods and initial two years' experience. J Clin Epidemiol. 1996;49(2):223–33. [DOI] [PubMed] [Google Scholar]
- 23. Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–42. [DOI] [PubMed] [Google Scholar]
- 24. Folsom AR, Arnett DK, Hutchinson RG, Liao F, Clegg LX, Cooper LS. Physical activity and incidence of coronary heart disease in middle-aged women and men. Med Sci Sports Exerc. 1997;29(7):901–9. [DOI] [PubMed] [Google Scholar]
- 25. Shivappa N, Hebert JR, Kivimaki M, Akbaraly T. Alternative Healthy Eating Index 2010, dietary inflammatory index and risk of mortality: Results from the Whitehall II cohort study and meta-analysis of previous DII and mortality studies. Br J Nutr. 2017;118(3):210–21. [DOI] [PubMed] [Google Scholar]
- 26. Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189–96. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.