Abstract
Introduction
The I-PASS Handoff Program is a comprehensive handoff curriculum that has been shown to decrease rates of medical errors and adverse events during patient handoffs. Frontline providers are the key individuals participating in handoffs of patient care. It is important they receive robust handoff training.
Methods
The I-PASS Mentored Implementation Handoff Curriculum frontline provider training materials were created as part of the original I-PASS Study and adapted for the Society of Hospital Medicine (SHM) I-PASS Mentored Implementation Program. The adapted materials embrace a flipped classroom approach with an emphasis on adult learning theory principles. The training includes an overview of I-PASS handoff techniques, TeamSTEPPS team communication strategies, verbal handoff simulation scenarios, and a printed handoff document exercise.
Results
As part of the SHM I-PASS Mentored Implementation Program, 2,735 frontline providers were trained at 32 study sites (16 adult and 16 pediatric) across North America. At the end of their training, 1,762 frontline providers completed the workshop evaluation form (64% response rate). After receiving the training, over 90% agreed/strongly agreed that they were able to distinguish a good- from a poor-quality handoff, articulate the elements of the I-PASS mnemonic, construct a high-quality patient summary, advocate for an appropriate environment for handoffs, and participate in handoff simulations. Universally, the training provided them with knowledge and skills relevant to their patient care activities.
Discussion
The I-PASS frontline training materials were rated highly by those trained and are an integral part of a successful I-PASS Handoff Program implementation.
Keywords: Handoffs, Residents, Advanced Care Providers, Safety, Quality Improvement, I-PASS, Nurse/Nurse Practitioner, Physician, Physician Assistant, Hospital Medicine, Internal Medicine, Pediatrics, Case-Based Learning, Flipped Classroom, Online/Distance Learning, Simulation
Educational Objectives
By the end of this activity, learners will be able to:
-
1.
Describe the importance of effective communication in reducing medical errors.
-
2.
Articulate the importance of effective team-training strategies to improve handoff communication.
-
3.
Illustrate how situation monitoring and situation awareness create a shared mental model to provide safe patient care.
-
4.
Demonstrate the ability to construct a high-quality patient summary including all essential components (summary statement, events leading up to admission, hospital course, ongoing assessment plan).
-
5.
Demonstrate use of the I-PASS mnemonic during a handoff simulation, as giver and receiver, and be rated as satisfactory by a trained observer.
Introduction
As duty-hour standards by the Accreditation Council for Graduate Medical Education (ACGME) have evolved over the past 15 years, the number of handoffs between resident physicians has increased.1 Handoffs are cited by leading regulatory and patient safety organizations as high-risk events that potentially put patients at risk for medical errors and adverse events.2 In order to address this risk, the ACGME now requires that residency programs provide residents with handoff training and monitor the quality of their handoff communication.1
In 2010, we launched the I-PASS Handoff Study at 11 institutions across North America.3-5 This study involved the implementation of a novel handoff bundle that included (1) the I-PASS mnemonic; (2) an interactive workshop to teach TeamSTEPPS teamwork and communication skills, as well as I-PASS handoff techniques; (3) simulation and role-play exercises to practice skills learned in the workshop; (4) a computer module to allow for independent learning; (5) a faculty development program; (6) handoff assessment tools designed to be used by faculty to observe handoffs and provide feedback to frontline providers to improve performance; and (7) a process and culture-change campaign featuring a logo, posters, and other visual reinforcement materials to ensure program adoption and sustainability. The original I-PASS Handoff Bundle included a comprehensive suite of educational materials with seven major complementary components that were published in MedEdPORTAL in 2013-2014.6-12 Implementation of this bundle at the study sites was associated with a 23% reduction in medical errors (24.5 vs. 18.8 per 100 admissions, p < .001) and a 30% reduction in preventable adverse events (4.7 vs. 3.3 per 100 admissions, p < .001). As evidence of successful implementation, significant increases across all sites were observed in inclusion of key information in written handoff documents (improvements in nine of nine prespecified key elements) and in verbal communications during handoffs (five of five key elements; p < .001 for all 14 comparisons).4 There were no significant changes in the duration of oral handoffs per patient (2.4 vs. 2.5 minutes, p = .55) or resident workflow, including patient-family contact and computer time.
Following the original study, our group noted a number of key challenges to implementation of the original curriculum bundle that needed to be addressed in order to promote effective implementation of the program during spread to other institutions. In conjunction with the Society of Hospital Medicine (SHM) in the I-PASS Mentored Implementation Program, the curricular materials of the original handoff bundle were edited and refined.13,14 These refinements included adoption of the training materials for adult medicine patients and also for frontline providers who were not resident physicians (e.g., advanced practice providers). Additionally, the length of the training session was shortened, and higher-quality video training scenarios were created. As part of the SHM I-PASS Mentored Implementation Program, the newly refined and updated frontline provider handoff program was successfully implemented at 32 adult and pediatric residency programs and hospitals across North America.
The I-PASS Mentored Implementation Handoff Curriculum frontline provider training materials include the I-PASS core content video module, the patient summary and written handoff exercises (in both pediatric and adult versions), and all materials for the frontline provider in-person workshops (in both pediatric and adult versions). The materials for the frontline provider workshops include the workshop slide sets, an interactive guide for attendees, handoff simulation materials, associated workshop videos (which can be embedded into the workshop slides), and a workshop evaluation form. While the frontline provider training materials serve as an independent resource for training frontline providers at one's own institution, the members of the I-PASS Study Group recommend using them along with the other complementary I-PASS curricular modules available in MedEdPORTAL. The entire I-PASS Mentored Implementation Handoff Curriculum is a multifaceted collection of modules that provides training and strategic plans for every aspect of leading the culture change that is required to implement an effective handoff program that improves patient safety and outcomes. While the SHM I-PASS Mentored Implementation Program included mentorship from external experts for each site, we believe that we have compiled all of the critical training elements of the program, as well as expert tips for successful implementation and sustainment in this extensive module collection. This collection of modules will allow anyone to capably implement the program at their home institution.
Methods
Development of the Curriculum
The original I-PASS resident training materials were published in MedEdPORTAL in 2013.11 Since that time, we have received over 880 requests for these materials in MedEdPORTAL, plus more on the I-PASS Study website.15 We developed the original materials in a rigorous fashion in collaboration with a group of medical educators, patient safety experts, and health services researchers over a 1-year period using Kern's six steps for curriculum development.16 For the SHM I-PASS Mentored Implementation Program, all materials underwent rigorous revision based upon feedback, and we made the following edits to the former resident training materials:
-
1.
We adapted the name of the of the curriculum to include the term frontline provider instead of resident. We made this change to be more inclusive of other frontline providers who participate in handoffs, including hospitalists, advanced practice providers, and fellows.
-
2.
We revised the training program to include a flipped classroom approach after receiving feedback from site leaders after the original study that it was difficult to secure enough time and resources to train residents given the length of the original training session (3 hours).14 The flipped classroom approach required frontline providers to complete some prework to prepare them for the in-person training. As a result, we were able to shorten the training session from 3 hours to 90 minutes, thus allowing for greater feasibility and flexibility.
-
3.
We expanded the materials, originally developed for pediatric providers, to include cases and examples for providers who care for hospitalized adults.
-
4.
We created new, higher-quality, professional-grade training videos for various elements of the curriculum.
These revised materials were successfully deployed from 2015 to 2016 at the first wave of 16 sites for the SHM I-PASS Mentored Implementation Program. We elicited feedback from these sites, and edits were made to the curriculum for use by the subsequent 16 sites in the second wave.
Overview of the Curricular Materials
The I-PASS Mentored Implementation Handoff Curriculum: frontline provider training materials include the following:
-
1.
I-PASS core content video module (Appendix A; video references included in Appendix AB): This 24-minute introductory video module provides an overview of the main components of the I-PASS Handoff Program, including background on the I-PASS program, the I-PASS mnemonic, TeamSTEPPS techniques, video vignettes of handoffs, and sample printed handoff documents.
-
2.Patient summary and written handoff exercises: These self-study materials are intended to be completed prior to the in-person I-PASS frontline provider training workshop. These exercises include an opportunity to develop an effective patient summary in the I-PASS structure after reviewing a patient case.
-
•Patient summary and written handoff exercise, pediatric version (Appendix B).
-
•Patient summary and written handoff exercise, adult version (Appendix C).
-
•
-
3.Frontline provider workshop materials (pediatric and adult versions): The following educational materials are intended to be used during the 90-minute in-person workshop. Materials include an in-depth introduction to the TeamSTEPPS team communication strategies via illustrative videos, a video vignette demonstrating a poor handoff with associated discussion points, and a team-based handoff video vignette. During the latter part of the 90-minute workshop, participants are organized into groups of three in order to complete three separate handoff simulation exercises. In this small-group activity, each participant is given the opportunity to be the giver, receiver, and observer/evaluator of a handoff.
-
•Frontline provider workshop, pediatric version (Appendix D).
-
•Frontline provider workshop interactive guide, pediatric version (Appendix E).
-
•Handoff simulation materials, pediatric versions: handoff simulation participant 1 packet, pediatric version (Appendix F); handoff simulation participant 2 packet, pediatric version (Appendix G); handoff simulation participant 3 packet, pediatric version (Appendix H); and simulation facilitator packet, pediatric version (Appendix I).
-
•Workshop videos (embedded in workshop slides, copies also provided in case any need to be reinserted): TeamSTEPPS brief video, pediatric version (Appendix J); TeamSTEPPS debrief video, pediatric version (Appendix K); TeamSTEPPS huddle video, pediatric version (Appendix L); TeamSTEPPS cross-monitoring and feedback video, pediatric version (Appendix M); TeamSTEPPS assertive statement video, pediatric version (Appendix N); and team handoff scenario video (Appendix O).
-
•Frontline provider workshop evaluation form (Appendix P).
-
•Frontline provider workshop, adult version (Appendix Q).
-
•Frontline provider workshop interactive guide, adult version (Appendix R).
-
•Handoff simulation materials, adult versions: handoff simulation participant 1 packet, adult version (Appendix S); handoff simulation participant 2 packet, adult version (Appendix T); handoff simulation participant 3 packet, adult version (Appendix U); and simulation facilitator packet, adult version (Appendix V).
-
•Workshop videos (embedded in workshop slides, copies also provided in case any need to be reinserted): TeamSTEPPS brief video, adult version (Appendix W); TeamSTEPPS debrief video, adult version (Appendix X); TeamSTEPPS huddle video, adult version (Appendix Y); TeamSTEPPS cross-monitoring and feedback video, adult version (Appendix Z); TeamSTEPPS assertive statement video, adult version (Appendix AA); and team handoff scenario video (Appendix O).
-
•Frontline provider workshop evaluation Form (Appendix P).
-
•
How to Implement This Curriculum
We designed the I-PASS Mentored Implementation Handoff Curriculum frontline provider training materials to assist both those just starting to implement a handoff program for frontline providers and those seeking additional resources and guidance for handoff improvement initiatives already in progress. During our program, the I-PASS site leaders at a given site led all training efforts. Our site leaders were residency program directors, division or section directors, chief residents, faculty members, hospital quality improvement leaders, or designated institutional officials. As site leaders, these individuals were responsible for thinking through the current state of shift-to-shift handoffs at the institution, developing the goals for process improvement, training frontline providers and champions, and creating a system of observation, feedback, and data tracking to ensure successful implementation of the handoff program. Given the various responsibilities of a site leader, many site leaders recruited I-PASS champions, typically faculty/attending physicians, chief residents, or other key educators, to assist with deploying the training efforts for frontline providers. All of these champions completed the I-PASS champion training and were well versed in the curriculum.
At all of our sites, the rollout of frontline provider training occurred 1-2 months before the official go-live of the handoff program and took place in the following order:
-
1.
Three to 4 weeks before the in-person workshop: Site leaders distributed the I-PASS core content video module and the patient summary and written handoff exercise to frontline providers for completion. Some sites showed the video during a regular meeting time or sent a link to the video (posted on a hospital shared drive or another online format). Videos were found to play well on standard media players such as Windows Media Player or QuickTime. Site leaders shared the patient summary and written handoff exercise either electronically or via hard copy. They also reminded frontline providers via email and at meetings about the importance of completing both tasks before the in-person workshop.
-
2.
In-person workshop: During the in-person workshop, site leaders facilitated the frontline provider workshop, which included the seven embedded video scenarios. Videos were embedded into the slides before distribution to the sites; however, if the videos did not format correctly, some site leaders had to download them to their own computer hard drives and embed them again themselves. A media player was not required to play videos embedded into the slides; however, if the videos needed to be viewed outside of the slides, they played well on standard media players such as Windows Media Player or QuickTime.
-
3.
Our site leaders noted that optimal workshop training occurred in a large conference room with audiovisual capabilities that allowed for appropriate viewing of slides and videos. At the end of the didactic workshop, the workshop facilitator split the frontline providers into groups of three, and they participated in the three handoff simulation scenarios. I-PASS champions observed each small group of three and provided feedback.
-
4.
Upon completion of the in-person training: Frontline providers completed the frontline provider workshop evaluation form at the end of the workshop. This feedback was critical for improvement and spread efforts at each site.
Handouts were required for the in-person workshop. Site leaders printed the following handouts in advance of the in-person workshops:
-
1.
Frontline provider workshop interactive guide: One copy was printed per attendee. This handout contained key exercises that were incorporated into the in-person workshop session.
-
2.
Handoff simulation materials: Site leaders divided the expected number of attendees by three; this was the number of small groups that were present at the in-person workshop. Handoff simulation participant 1, 2, and 3 packets were printed and individually stapled. Copies of each of these packets were joined with a paper clip to form larger packet. Site leaders distributed these larger packets to each small group of three during the handoff simulation time at the in-person workshop.
-
3.
Simulation facilitator packet: Site leaders printed a copy of this packet for each I-PASS champion recruited to assist with the handoff simulation scenarios during the in-person workshop.
-
4.
Frontline provider workshop evaluation form: Site leaders printed one copy per attendee.
Given the complexity and time line of the deployment of this training program, our site leaders noted that it was important to continually check in with and remind frontline providers about the importance of the implementation of the program and time needed to train providers, see practice change, and sustain that change. Best-practice recommendations and expert advice about how to change via novel implementation methods were compiled into a companion publication in MedEdPORTAL, the I-PASS Mentored Implementation Handoff Curriculum implementation guide and resources.17
Measurement of the Impact of the Curriculum
At the conclusion of the in-person workshop, frontline providers at all of the 32 SHM I-PASS sites completed an evaluation of the curriculum. Site leaders distributed the evaluations either in paper form or as a link to a REDCap survey tool, via either a tiny URL or a QR code at the end of the in-person workshop. The surveys contained various questions about the frontline providers’ confidence in executing various skills related to the curriculum, as well as the quality of the training experiences. Reponses to these questions were collected on a 5-point Likert-type agreement scale. We dichotomized the results into strongly agree/agree, neutral, and disagree/strongly disagree for analysis. Site leaders also collected the number of frontline providers trained as part of the program.
Results
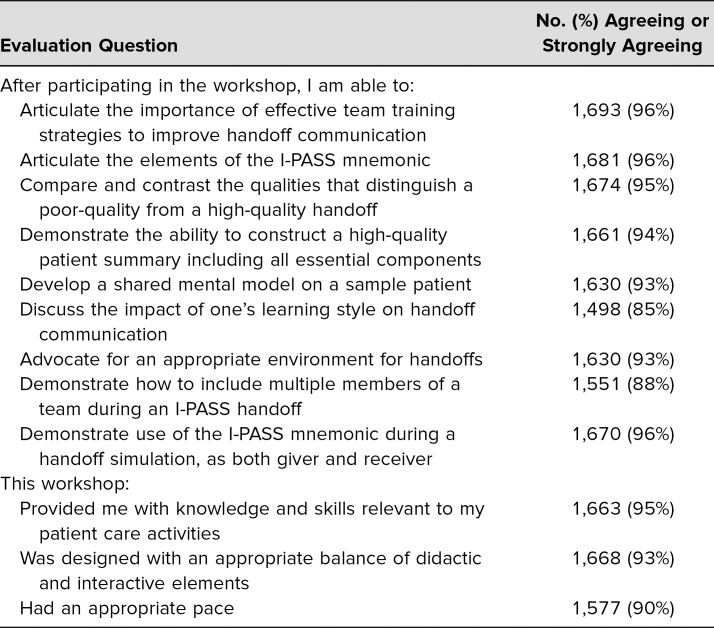
As part of the SHM I-PASS Mentored Implementation Program's frontline training program, we trained 2,735 frontline providers at 32 sites across North America. This group included frontline providers who cared for both hospitalized children and adults. At the end of the training, 1,762 frontline providers completed the workshop evaluation form (64% response rate). Frontline provider responses from the workshop evaluation form are detailed in the Table.
Table. I-PASS Frontline Provider Workshop Evaluation Form Responses (N = 1,762).
Discussion
In response to increasing regulatory requirements around handoff education and supervision for trainees in undergraduate and graduate medical education,1 as well as the recognition that handoffs are high-risk events for errors in patient care,2 the I-PASS Mentored Implementation Handoff Curriculum frontline provider training materials were created following a 6-year collaborative effort to develop a handoff training program that would be targeted, effective, and flexible for those on the front lines of patient care. The results from the original I-PASS Handoff Study showed a great impact of the curriculum on patient safety without adverse consequences on resident physician workflow.4 However, that curriculum was noted to require a significant amount of in-person training time (3 hours) and was mainly focused on training pediatric residents at academic or university-based institutions. The program subsequently underwent significant revision as part of the SHM I-PASS Mentored Implementation Program and is now an effective and efficient training resource for any type of frontline provider regardless of training level, specialty, institution, or type of patients. Data from the SHM I-PASS Mentored Implementation Program showed that the vast majority of the 1,762 frontline providers who completed evaluations felt that the training provided them with knowledge and skills relevant to their patient care activities, was an appropriate balance of didactic and interactive elements, and was appropriately paced for learning. Participants overwhelmingly noted that after receiving the training, they were able to distinguish a good- from a poor-quality handoff, articulate the elements of the I-PASS mnemonic, demonstrate how to share one's mental model about a patient, construct a high-quality patient summary, advocate for an appropriate environment for handoffs, and participate as a handoff giver and receiver during handoff simulations.
While the resources in this module will be of great value to those looking to train frontline providers of patient care in handoff communication, we would like to share some key lessons learned that are critical for successful implementation and sustainment of the program at one's own institution.
-
1.
Culture change takes time: While there is often a great deal of excitement immediately following the implementation of the I-PASS Handoff Program at an institution, that excitement can wane with time. This can lead frontline providers to return to old handoff habits for the sake of ease or familiarity. In addition, opponents of the program can become a powerful voice against change and further inhibit efforts. With resident physicians, we have found that it often takes 3-5 years of concerted culture-change effort in order to consistently change handoff practices. Because most residencies are typically 3-5 years in length, it takes that much time for a full generation of residents to standardize new handoff practices. After 3-5 years, one has a contingent of residents who have been taught a practice from day one of residency and therefore do not know a different way of practicing. Culture change is difficult and takes time; patience and perseverance are key.
-
2.
Frontline providers need feedback: Individuals are motivated by data. Therefore, the more one can share various outcome metrics from the I-PASS Handoff Program with frontline providers (e.g., adherence rates to all five elements of the I-PASS mnemonic, length of handoff communication, adverse events related to handoff failures, etc.), the more successful the implementation will be because frontline providers will be motivated to change behaviors. Sharing data in tables or run charts in highly visible locations (e.g., conference rooms, lecture halls, lounges, via email, etc.) where frontline providers spend a great deal of time is an effective way to provide feedback to encourage behavior change. Such data can be provided weekly or monthly; it just needs to be done regularly and be highly publicized. Often, frontline providers will also respond to making a competition out of performance and rewarding those with exemplary performance.
-
3.
Allow space for innovation and customization: While a fair amount of consistency and structure is critical for a handoff communication program, allowing frontline providers a bit of room to customize the handoff and make it their own can help enhance buy-in. For example, one can allow frontline providers some flexibility in adapting the verbal or written patient summary section based upon the unique characteristics of a patient population they care for (e.g., ICU patients, neonates, geriatric patients, etc.) or let them adapt who is responsible for what communication depending upon the number of people who attend a verbal handoff. If frontline providers are allowed to innovate and customize the program while maintaining key elements of the I-PASS mnemonic, they are more likely to see it as a process that fits their needs and workflow. Enhancing this kind of buy-in is key for acceptance and sustainment of the program.
Following the implementation of the SHM I-PASS Mentored Implementation Program, we noted the following limitations to the frontline provider training materials. First, while expanded to include scenarios for providers who care for adults, the simulation scenarios for the in-person training workshop do not include scenarios around surgical, critical care, subspecialty, and emergency department patients. Second, the evaluation of the curriculum does not include implementation or safety outcomes. Finally, the program has only been implemented in pediatric and internal medicine residency programs in North America, therefore limiting its generalizability to other residency training programs and community institutions. Despite the lack of specialty and patient-type diversity in the simulation scenarios for the in-person workshop, we do feel the provided template could be easily adapted with scenarios personalized for the provider, location, and patient type. Although this program has been implemented only in pediatric and internal medicine residency training programs, we do know of many other subspecialty programs that have obtained the curriculum and adapted it to fit their needs, based upon anecdotal reports as well download statistics from the first I-PASS Handoff Curriculum published in MedEdPORTAL.7,11
In closing, the I-PASS Mentored Implementation Handoff Curriculum frontline provider training materials are a robust, evidence-based, well-tested, and feasible set of educational materials that one can use for training frontline providers in structured handoff communication. The materials have been used in diverse institutions and settings across North America, thus speaking to their universal nature and adaptability. This module, which is one facet of the larger I-PASS Mentored Implementation Handoff Curriculum, also meets the needs of those seeking to comply with regulatory requirements from accrediting agencies. Future work of the I-PASS Study Group will focus on continued dissemination of the curricular materials and reflection on how to continue to meet the learning needs of frontline providers in a wide range of specialties and health care institutions across the globe.
Appendices
- I-PASS Core Content Video.wmv
- Patient Summary & Written Handoff Exercise-Pediatric.pdf
- Patient Summary & Written Handoff Exercise-Adult.pdf
- Frontline Provider Workshop-Pediatric.pptx
- Frontline Provider Workshop Interactive Guide-Pediatric.pdf
- Handoff Simulation Participant 1 Packet-Pediatric.pdf
- Handoff Simulation Participant 2 Packet-Pediatric.pdf
- Handoff Simulation Participant 3 Packet-Pediatric.pdf
- Simulation Facilitator Packet-Pediatric.pdf
- TeamSTEPPS Brief Video-Pediatric.wmv
- TeamSTEPPS Debrief Video-Pediatric.wmv
- TeamSTEPPS Huddle Video-Pediatric.wmv
- TeamSTEPPS Cross-Monitoring & Feedback Video-Pediatric.wmv
- TeamSTEPPS Assertive Statement Video-Pediatric.wmv
- Team Handoff Scenario.wmv
- Frontline Provider Workshop Evaluation Form.pdf
- Frontline Provider Workshop-Adult.pptx
- Frontline Provider Workshop Interactive Guide-Adult.pdf
- Handoff Simulation Participant 1 Packet-Adult.pdf
- Handoff Simulation Participant 2 Packet-Adult.pdf
- Handoff Simulation Participant 3 Packet-Adult.pdf
- Simulation Facilitator Packet-Adult.pdf
- TeamSTEPPS Brief Video-Adult.wmv
- TeamSTEPPS Debrief Video-Adult.wmv
- TeamSTEPPS Huddle Video-Adult.wmv
- TeamSTEPPS Cross-Monitoring & Feedback Video-Adult.wmv
- TeamSTEPPS Assertive Statement Video-Adult.wmv
- References for I-PASS Core Content Video.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Acknowledgments
Drs. O'Toole and Hepps are co-primary authors on this publication.
The I-PASS Study Education Executive Committee members are Amy J. Starmer, MD, MPH, Co-chair; Nancy D. Spector, MD, Co-chair; James F. Bale, Jr., MD; Zia Bismilla, MD, MEd; Sharon Calaman, MD; Maitreya Coffey, MD; F. Sessions Cole, MD; Lauren A. Destino, MD; Jennifer L. Everhart, MD; Jennifer Hepps, MD; Christopher P. Landrigan, MD, MPH; Joseph O. Lopreiato, MD, MPH; Elizabeth L. Noble; Jennifer K. O'Toole, MD, MEd; Shilpa J. Patel, MD; Glenn Rosenbluth, MD; Theodore C. Sectish, MD; Rajendu Srivastava, MD, MPH; Adam T. Stevenson, MD; Lisa L. Tse; Daniel C. West, MD; and Clifton E. Yu, MD.
Disclosures
Drs. O'Toole, Patel, Rosenbluth, and Calaman have consulted with and hold stock in the I-PASS Patient Safety Institute, a company that trains institutions in best handoff practices and aids in their implementation. Drs. Spector, Sectish, Landrigan, West, Srivastava, and Starmer hold equity in and have consulted for the I-PASS Patient Safety Institute.
Funding/Support
Agency for Healthcare Research and Quality (Award 1R18HS023291): Dr. Christopher P. Landrigan.
Ethical Approval
Reported as not applicable.
References
- 1.Requirements Common Program. Accreditation Council for Graduate Medical Education website. Accessed July 24, 2018. http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements [Google Scholar]
- 2.communication Inadequate hand-off. Sentinel Event Alert. 2017;(58):1–6. [PubMed] [Google Scholar]
- 3.Starmer AJ, Spector ND, Srivastava R, et al.; I-PASS Study Group. I-PASS, a mnemonic to standardize verbal handoffs. Pediatrics. 2012;129(2):201–204. 10.1542/peds.2011-2966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starmer AJ, Spector ND, Srivastava R, et al.; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812. 10.1056/NEJMsa1405556 [DOI] [PubMed] [Google Scholar]
- 5.Starmer AJ, O'Toole JK, Rosenbluth G, et al.; I-PASS Study Education Executive Committee. Development, implementation, and dissemination of the I-PASS Handoff Curriculum: a multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876–884. 10.1097/ACM.0000000000000264 [DOI] [PubMed] [Google Scholar]
- 6.Calaman S, Spector ND, Starmer AJ, et al.; I-PASS Education Executive Committee. I-PASS Handoff Curriculum: computer module. MedEdPORTAL. 2013;9:9337. 10.15766/mep_2374-8265.9337 [DOI] [Google Scholar]
- 7.Calaman S, Hepps J, Spector ND, et al.; I-PASS Education Executive Committee. I-PASS Handoff Curriculum: handoff simulation exercises. MedEdPORTAL. 2013;9:9402. 10.15766/mep_2374-8265.9402 [DOI] [Google Scholar]
- 8.O'Toole J, Sectish T, Starmer AJ, et al.; I-PASS Education Executive Committee. I-PASS Handoff Curriculum: faculty development resources. MedEdPORTAL. 2013;9:9540. 10.15766/mep_2374-8265.9540 [DOI] [Google Scholar]
- 9.O'Toole J, Calaman S, Everhart J, et al. I-PASS Handoff Curriculum: medical student workshop. MedEdPORTAL. 2014;10:9854. 10.15766/mep_2374-8265.9854 [DOI] [Google Scholar]
- 10.Rosenbluth G, Patel SJ, Destino LA, et al.; I-PASS Education Executive Committee. I-PASS Handoff Curriculum: campaign toolkit. MedEdPORTAL. 2013;9:9397. 10.15766/mep_2374-8265.9397 [DOI] [Google Scholar]
- 11.Spector ND, Starmer AJ, Allen AD, et al.; I-PASS Education Executive Committee. I-PASS Handoff Curriculum: core resident workshop. MedEdPORTAL. 2013;9:9311. 10.15766/mep_2374-8265.9311 [DOI] [Google Scholar]
- 12.Starmer AJ, Landrigan C, Srivastava R, et al.; I-PASS Education Executive Committee. I-PASS Handoff Curriculum: faculty observation tools. MedEdPORTAL. 2013;9:9570. 10.15766/mep_2374-8265.9570 [DOI] [Google Scholar]
- 13.Maynard GA, Budnitz TL, Nickel WK, et al. Mentored implementation: building leaders and achieving results through a collaborative improvement model. Jt Comm J Qual Patient Saf. 2012;38(7):301–310. 10.1016/S1553-7250(12)38040-9 [DOI] [PubMed] [Google Scholar]
- 14.Sharma N, Lau CS, Doherty I, Harbutt D. How we flipped the medical classroom. Med Teach. 2015;37(4):327–330. 10.3109/0142159X.2014.923821 [DOI] [PubMed] [Google Scholar]
- 15.I-PASS Study Group website. Accessed July 5, 2016. http://ipassstudygroup.com/home
- 16.Kern DE, Thomas PA, Hughes MT. Curriculum Development for Medical Education: a Six-Step Approach. 2nd ed. Johns Hopkins University Press; 2009. [Google Scholar]
- 17.O'Toole JK, Starmer AJ, Calaman S, et al; for I-PASS Study Education Executive Committee. I-PASS Mentored Implementation Handoff Curriculum: implementation guide and resources. MedEdPORTAL. 2018;14:10736. 10.15766/mep_2374-8265.10736 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- I-PASS Core Content Video.wmv
- Patient Summary & Written Handoff Exercise-Pediatric.pdf
- Patient Summary & Written Handoff Exercise-Adult.pdf
- Frontline Provider Workshop-Pediatric.pptx
- Frontline Provider Workshop Interactive Guide-Pediatric.pdf
- Handoff Simulation Participant 1 Packet-Pediatric.pdf
- Handoff Simulation Participant 2 Packet-Pediatric.pdf
- Handoff Simulation Participant 3 Packet-Pediatric.pdf
- Simulation Facilitator Packet-Pediatric.pdf
- TeamSTEPPS Brief Video-Pediatric.wmv
- TeamSTEPPS Debrief Video-Pediatric.wmv
- TeamSTEPPS Huddle Video-Pediatric.wmv
- TeamSTEPPS Cross-Monitoring & Feedback Video-Pediatric.wmv
- TeamSTEPPS Assertive Statement Video-Pediatric.wmv
- Team Handoff Scenario.wmv
- Frontline Provider Workshop Evaluation Form.pdf
- Frontline Provider Workshop-Adult.pptx
- Frontline Provider Workshop Interactive Guide-Adult.pdf
- Handoff Simulation Participant 1 Packet-Adult.pdf
- Handoff Simulation Participant 2 Packet-Adult.pdf
- Handoff Simulation Participant 3 Packet-Adult.pdf
- Simulation Facilitator Packet-Adult.pdf
- TeamSTEPPS Brief Video-Adult.wmv
- TeamSTEPPS Debrief Video-Adult.wmv
- TeamSTEPPS Huddle Video-Adult.wmv
- TeamSTEPPS Cross-Monitoring & Feedback Video-Adult.wmv
- TeamSTEPPS Assertive Statement Video-Adult.wmv
- References for I-PASS Core Content Video.docx
All appendices are peer reviewed as integral parts of the Original Publication.