Key Points
Question
Is dialectical behavior therapy for posttraumatic stress disorder (DBT-PTSD) superior to cognitive processing therapy (CPT) in reducing the severity of complex presentations of posttraumatic stress disorder associated with childhood abuse?
Findings
In this randomized clinical trial, treatments with DBT-PTSD and CPT both created large and significant improvements in PTSD severity, with improvement more pronounced under DBT-PTSD. The proportions achieving symptomatic remission were 58% in DBT-PTSD vs 41% in CPT, a significant difference.
Meaning
In this trial, patients with severe childhood abuse–associated complex posttraumatic stress disorder highly improved under both DBT-PTSD and CPT, with DBT-PTSD being superior to CPT.
This randomized clinical trial compares the efficacy of 2 therapies for childhood abuse–associated posttraumatic stress disorder in women by randomizing participants to receive dialectical behavior therapy for posttraumatic stress disorder or cognitive processing therapy.
Abstract
Importance
Childhood abuse significantly increases the risk of developing posttraumatic stress disorder (PTSD), often accompanied by symptoms of borderline personality disorder (BPD) and other co-occurring mental disorders. Despite the high prevalence, systematic evaluations of evidence-based treatments for PTSD after childhood abuse are sparse.
Objective
To compare the efficacy of dialectical behavior therapy for PTSD (DBT-PTSD), a new, specifically designed, phase-based treatment program, against that of cognitive processing therapy (CPT), one of the best empirically supported treatments for PTSD.
Design, Setting, and Participants
From January 2014 to October 2016, women who sought treatment were included in a multicenter randomized clinical trial with blinded outcome assessments at 3 German university outpatient clinics. The participants were prospectively observed for 15 months. Women with childhood abuse–associated PTSD who additionally met 3 or more DSM-5 criteria for BPD, including affective instability, were included. Data analysis took place from October 2018 to December 2019.
Interventions
Participants received equal dosages and frequencies of DBT-PTSD or CPT, up to 45 individual sessions within 1 year and 3 additional sessions during the following 3 months.
Main Outcomes and Measures
The predefined primary outcome was the course of the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) score from randomization to month 15. Intent-to-treat analyses based on dimensional CAPS-5 scores were complemented by categorical outcome measures assessing symptomatic remission, reliable improvement, and reliable recovery.
Results
Of 955 consecutive individuals assessed for eligibility, 193 were randomized (DBT-PTSD, 98; CPT, 95; mean [SD] age, 36.3 [11.1] years) and included in the intent-to-treat analyses. Analysis revealed significantly improved CAPS-5 scores in both groups (effect sizes: DBT-PTSD: d, 1.35; CPT: d, 0.98) and a small but statistically significant superiority of DBT-PTSD (group difference: 4.82 [95% CI, 0.67-8.96]; P = .02; d, 0.33). Compared with the CPT group, participants in the DBT-PTSD group were less likely to drop out early (37 [39.0%] vs 25 [25.5%]; P = .046) and had higher rates of symptomatic remission (35 [40.7%] vs 52 [58.4%]; P = .02), reliable improvement (53 [55.8%] vs 73 [74.5%]; P = .006), and reliable recovery (34 [38.6%] vs 52 [57.1%]; P = .01).
Conclusions and Relevance
These findings support the efficacy of DBT-PTSD and CPT in the treatment of women with childhood abuse–associated complex PTSD. Results pertaining to the primary outcomes favored DBT-PTSD. The study shows that even severe childhood abuse–associated PTSD with emotion dysregulation can be treated efficaciously.
Trial Registration
German Clinical Trials Register: DRKS00005578
Introduction
The experience of childhood abuse (CA), whether sexual and/or physical, increases the likelihood of mental disorders later in life, particularly posttraumatic stress disorder (PTSD) and borderline personality disorder (BPD).1,2,3,4,5,6 Cooccurrence of these 2 disorders is frequent: in epidemiological studies, 15% to 29% of individuals with PTSD also met criteria for BPD, while 17% to 53% of individuals with BPD reported PTSD.7,8,9,10 In clinical samples, BPD-PTSD comorbidity often exceeds 50%.11,12,13 Recent studies suggest that the experience of CA in particular results in complex presentations of PTSD, with high cooccurrence of these disorders.8,14
A recent meta-regression involving 51 randomized clinical trials found that patients with a history of CA and complex PTSD symptoms responded poorly to psychotherapy for PTSD.15 This might be because of trauma-associated morphological alterations of the central nervous system,16,17 increased dissociative features,18 or severe self-criticism,19 which might impede neural plasticity, emotional learning, and treatment motivation. The empirical base for a negative outcome of co-occurring BPD on treatment response is sparse. One study that investigated efficacy of cognitive behavioral therapy for survivors of childhood sexual abuse found that all the patients with co-occurring BPD dropped out of the cognitive behavioral therapy arm.20 Five studies21,22,23,24,25 documented no significant associations of BPD with treatment outcome; however, 3 of these studies21,22,23 had excluded patients with current self-injurious behavior. This exclusion corresponds to the frequent exclusion from PTSD trials of patients with severe psychopathology, such as suicidality, ongoing self-harm, and substance abuse.26,27
Conversely, a study28 showed that dialectical behavior therapy (DBT), one of the currently best-established treatments for BPD, did not significantly improve co-occurring PTSD. An attempt to address this problem has been made by adding prolonged exposure therapy to the standard DBT procedure.29 However, the dropout rates were high, and the data are limited.
Currently, treatment of CA-associated PTSD mostly relies on established treatments that were developed for survivors of adult-onset trauma. Most treatment guidelines recommend prolonged exposure, cognitive processing therapy (CPT), or trauma-focused cognitive behavioral therapy,30,31,32 but there is debate on whether these treatments are sufficient for patients with CA-associated PTSD.33,34 Some authors favor phase-based treatments, focusing on emotion regulation before addressing traumatic memories,35,36,37,38,39 while others maintain that standard trauma-focused programs without additional components are sufficient.40,41 To date, no direct comparison has been carried out between standard PTSD therapies and specifically designed phase-based therapies.
Dialectical behavior therapy for PTSD (DBT-PTSD) is a prototypic phase-based treatment that is designed to meet the needs of survivors of CA with highly complex presentations of PTSD, including features of BPD. The first evaluation of this treatment supported its efficacy under residential treatment conditions.42,43 The present study aimed at testing the superiority of DBT-PTSD compared with CPT in outpatients. We chose CPT as the comparator treatment because it is a highly efficacious,41,44,45,46 non–phase-based, well-established therapy for PTSD that has been shown to be efficacious in treating CA-associated PTSD.44
Methods
Trial Design and Participants
The study was conducted at 3 sites in Germany. Approval was obtained from the applicable ethics committees (Medical Faculty Mannheim at Heidelberg University in Mannheim, Goethe University in Frankfurt, and Humboldt University in Berlin). Before randomization, participants provided written informed consent. Safety and data quality were independently monitored by the Coordination Centre for Clinical Trials, Heidelberg. The study protocol has been published elsewhere47 and is available in Supplement 2.
Inclusion criteria included female sex and gender identity; an age of 18 to 65 years; a diagnosis of PTSD (according to the DSM-5) following sexual or physical abuse before age 18 years; meeting 3 or more BPD criteria, including criterion 6 (affective instability); and availability for 1 year of outpatient treatment. Exclusion criteria included lifetime diagnoses of schizophrenia, bipolar I disorder, mental retardation, or severe psychopathology requiring immediate treatment in a different setting (eg, a body mass index <16.5); life-threatening suicide attempts within the last 2 months; current substance dependence (any usage within the last 2 months); medical conditions contradicting exposure protocol (eg, pregnancy); a highly unstable life situation (eg, homelessness); scheduled residential treatment; and receipt of either CPT or DBT-PTSD treatment during the last year. Patients with ongoing self-harm, suicidality, or high-risk behaviors were not excluded.
Participants were recruited from waiting lists of outpatient clinics in Mannheim, Frankfurt, and Berlin, Germany; through advertisements; and from therapists who had been informed about the study. Recruitment occurred from January 2014 to October 2016. Data analysis took place from October 2018 to December 2019.
Randomization and Masking
Web-based randomization software (http://randomizer.at) was used to assign participants in a 1:1 ratio to DBT-PTSD or CPT. Assessments were conducted by trained and experienced clinicians who were blinded to assignments.
Interventions
Detailed descriptions of the interventions were published elsewhere and are provided in the supplementary material (eAppendix in Supplement 1).41,42,47,48 Briefly, DBT-PTSD is a multicomponent phase-based program based on the principles, modes, and functions of standard DBT49 but supplemented by trauma-focused cognitive-behavioral interventions40,50 and specific techniques from compassion-focused therapy51 and acceptance and commitment therapy.52 Cognitive processing therapy is an established trauma-focused cognitive therapy aiming at challenging dysfunctional trauma-associated cognitions and emotions. Treatment, modified for this study, followed a session-by-session protocol. The first 4 sessions aimed at elaborating a case history, the patient’s specific problem behaviors, and emergency plans; the next 12 sessions encompassed the original 12 CPT core sessions; and the content of the remainder was derived from the patient’s individual stuck-point log.
To achieve structural equality of the arms, both treatments included individual therapy, plus homework and telephone consultation as needed. All patients received up to 45 weekly sessions over a year, followed by a booster phase of 3 monthly sessions. Participants who missed 6 consecutive weekly sessions or had psychiatric hospitalizations of 2 weeks or longer were considered dropouts, unless they had achieved early remission. Early remission was achieved under predefined conditions, all of which had to be fulfilled: (1) the patient claimed recovery prior to session 45; (2) the therapist agreed; (3) the therapist’s supervisor agreed; and (4) a blinded rater assessed that the patient no longer met the PTSD diagnosis (Clinician-Administered PTSD Scale [CAPS-5] score).53
To ensure integrity of the treatments, prior to the study, participating therapists were trained in either DBT-PTSD or CPT in 4-day workshops led by the respective treatment developers. All therapists had regular team consultations. The arms were balanced with respect to therapists’ experience, age, and structural characteristics, such as the number of patients (eTable 1 in Supplement 1). Therapist adherence and competence were assessed by 2 independent raters (M.M.-E. and 1 nonauthor) who had received intensive training in both treatments and the rating procedure. They viewed a total of 258 videotapes (2 sessions from each patient who completed the study) and rated the therapists using scales that had been specifically developed to assess these characteristics in both arms. Interrater reliability for all scales yielded good to excellent results (intraclass correlations, 0.67-0.97).54,55
Diagnostic Procedures
Diagnoses of PTSD were established with the CAPS-5, co-occurring Axis I disorders with the Structured Clinical Interview for DSM-IV Axis I disorders,56 and BPD with the International Personality Disorder Examination.57 The concordance between the diagnoses of PTSD according to the CAPS-5 vs the Structured Clinical Interview was 100%. Interrater reliability for the diagnosis established with the CAPS-5 in the present sample was high (intraclass correlations, 0.81-0.89).58
Outcome Measures
The predefined primary outcome was the CAPS-5 score at 15 months, for which internal consistency (Cronbach α) was 0.93 in our sample.58 Secondary outcomes included all psychopathology scales assessed at all major assessments and the Global Assessment of Functioning.59 Rating scales included the PTSD Checklist for DSM-5,60 the Borderline Symptom List (short version [BSL-23]),61 the behavioral items of the BSL,62 the Beck Depression Inventory–II,63 and the Dissociation Tension Scale covering the last week64 with the subscales for duration and intensity.
Assessments and Missing Data
Full assessments were conducted before the start of therapy and after 3, 6, 9, 12, and 15 months. The primary analyses were conducted on the intent-to-treat (ITT) population, which included all participants who were randomized and fulfilled the criteria for participating. Missing items (≤10%) were imputed using stochastic regression imputation based on all other items from the respective scale.65,66 If more than 10% of the items were missing, multiple imputation on the scale level was applied. Given a nonmonotone missing pattern, the Markov chain Monte Carlo method was used for this purpose.67 Multiple imputation was based on the SAS procedures MI (1000 runs) and MIANALYZE. The ITT analyses were supplemented with analyses according to protocol. Details regarding missing data for the primary outcome are provided in eTable 2 in Supplement 1.
Statistical Analysis
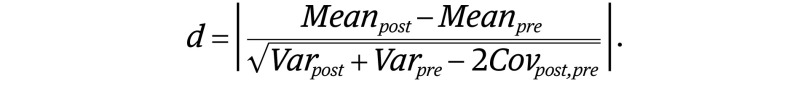
The planned sample size was determined a priori from a power analysis. As described by Bohus et al,47 an N of 180 or more would detect a medium-size superiority of DBT-PTSD over CPT with a statistical power of 0.80 or more. Mixed linear models were the predefined primary strategy for analyzing changes. Variables that were in line with the assumption of normality were modeled by the following mixed linear model (Equation 1) based on the unstructured covariance matrix:
 . .
|
Parameter estimation was based on restricted maximum likelihood estimates in SAS version 9.4 (SAS Institute) PROC MIXED. Potential misspecifications were checked by plotting marginal residuals against predicted means and using Q-Q plots. Mixed models were complemented with the following clinically meaningful measures: symptomatic remission, defined as no longer meeting the diagnostic criteria of PTSD according to DSM-5 vs not achieving this goal (ie, not experiencing remission or dropping out without having experienced remission); reliable improvement (on the CAPS-5), requiring that the improvement exceeds a threshold (calculated as SD[CAPSpre] × √2 × √(1 − reliability[CAPS]) × 1.96 = 7.29) compatible with chance variation and unreliability68; or reliable recovery, defined as reliable improvement plus symptomatic remission.69
Changes in percentages over time were evaluated using the McNemar test. Categorical data were compared using χ2 tests. All P values ≤.05 (2-tailed) were considered statistically significant. Effect sizes for comparisons of continuous data before and after the intervention were calculated per Equation 2:
 . .
|
Results
Patient Flow
Of 955 patients assessed for eligibility, 619 did not meet the inclusion criteria or met exclusion criteria, and 136 declined to participate (Figure 1). Of the 200 who were randomized, 7 were later excluded after they were found to be in violation of inclusion or exclusion criteria, in that they had no diagnosis of PTSD (n = 3), were pregnant at the time of randomization, had a brain tumor, had an established diagnosis of schizophrenia at the time of randomization, or did not have a female gender identity and sex. The final sample thus consisted of 193 participants (DBT-PTSD, 98; CPT, 95).
Figure 1. Patient Flow.
BPD indicates borderline personality disorder; CA, childhood abuse; CPT, cognitive processing therapy; DBT-PTSD, dialectical behavior therapy for posttraumatic stress disorder; PTSD, posttraumatic stress disorder.
Overall, 62 of the 193 participants (32.1%) withdrew, with significantly more dropouts in the CPT than the DBT-PTSD group (37 [39.0%] vs 25 [25.5%]; P = .046). In 10 individuals (CPT, 8; DBT-PTSD, 2; P = .06), the reason was psychiatric hospitalization of 2 weeks or more. The numbers of dropouts in CPT vs DBT-PTSD were 20 vs 11 individuals from the start of therapy to 3 months, 6 vs 6 individuals from 3 months to 6 months, 8 vs 5 individuals from 6 months to 9 months, 3 vs 3 individuals from 9 months to 12 months, and 0 vs 0 individuals from 12 months to 15 months.
Patient Characteristics
Sociodemographic and clinical characteristics of participants are provided in Table 1. Briefly, mean (SD) age was 36.3 (11.1) years. The mean (SD) age at first abuse was 7.7 (4.2) years, and the mean (SD) duration of the abuse was 6.9 (6.0) years. Psychotropic medication was prospectively monitored. By the end of the treatment, prescription rates in the 2 groups were similar for all medication classes except for neuroleptics (DBT-PTSD, 7 [8.0%]; CPT, 17 [21.8%]; uncorrected P = .02); however, this was nonsignificant after Bonferroni correction. Pre-to-post changes in psychotropic medication were uncorrelated with pre-to-post changes in the primary and secondary outcomes and not significantly associated with either symptomatic remission or dropout rates.
Table 1. Patient Characteristics and Psychotropic Medication.
| Characteristic | Participants, No. (%) | ||
|---|---|---|---|
| Entire sample | DBT-PTSD | CPT | |
| Age, mean (SD), y | 36.3 (11.1) | 37.0 (10.7) | 35.5 (11.4) |
| Educationa | |||
| No graduation or still at school | 11 (5.8) | 7 (7.2) | 4 (4.3) |
| Lower secondary school (Hauptschule) | 30 (15.8) | 16 (16.5) | 14 (15.1) |
| Intermediate secondary school (Mittlere Reife) | 67 (35.3) | 33 (34.0) | 34 (36.6) |
| High school graduation (Abitur) | 75 (39.5) | 37 (38.1) | 38 (40.9) |
| Other | 7 (3.7) | 4 (4.1) | 3 (3.2) |
| Marital statusb | |||
| Single | 95 (49.7) | 44 (45.8) | 51 (53.7) |
| Married or similar relationship | 49 (25.7) | 25 (26.0) | 24 (25.3) |
| Separated, divorced, or widowed | 47 (24.6) | 27 (28.1) | 20 (21.1) |
| No. of Axis I disorders, mean (SD) | |||
| Current | 3.25 (1.43) | 3.06 (1.31) | 3.44 (1.53) |
| Lifetime | 4.21 (1.54) | 4.07 (1.45) | 4.35 (1.62) |
| Co-occurring BPD | 93 (48.2) | 43 (43.9) | 50 (53.6) |
| BPD criteria, mean (SD), No. | 4.80 (1.64) | 4.68 (1.63) | 4.92 (1.65) |
| ≥1 Suicide attempt, lifetimec | 107 (57.5) | 58 (63.0) | 49 (52.1) |
| Nonsuicidal self-injury at least once in the last mod | 75 (39.1) | 40 (40.8) | 35 (37.2) |
| Index trauma | |||
| Sexual abuse or sexual and physical abuse | 144 (74.6) | 75 (76.5) | 69 (72.6) |
| Exclusively physical abuse | 49 (25.4) | 23 (23.5) | 26 (27.4) |
| Repeated abused | 174 (90.6) | 86 (88.7) | 88 (92.6) |
| Age at first abuse, mean (SD), y | 7.69 (4.21) | 7.67 (4.28) | 7.71 (4.16) |
| Duration of abuse, mean (SD), y | 6.90 (6.00) | 6.36 (5.16) | 7.44 (6.69) |
| Perpetrator known to the patient | 182 (94.3) | 94 (95.9) | 88 (92.6) |
| Additional sexual or physical abuse in adulthoode | 124 (67.8) | 66 (71.7) | 58 (63.7) |
| Prior psychotherapeutic or psychiatric treatment | 172 (89.1) | 85 (91.6) | 87 (86.7) |
| Psychotropic medication at baselinef | |||
| Any psychotropic medication | 133 (69.3) | 68 (69.4) | 65 (69.2) |
| Antidepressants | 103 (53.7) | 52 (53.1) | 51 (54.3) |
| Neuroleptics | 55 (28.7) | 24 (24.5) | 31 (33.0) |
| Mood stabilizersg | 4 (2.1) | 1 (1.0) | 3 (3.2) |
| Benzodiazepines | 14 (7.3) | 7 (7.1) | 7 (7.5) |
| Other psychotropic medication | 19 (9.9) | 7 (7.1) | 12 (12.8) |
| Psychotropic medication at postassessment | |||
| Any psychotropic medication | 84 (50.6) | 42 (47.7) | 42 (53.9) |
| Antidepressants | 64 (38.6) | 33 (37.5) | 31 (39.7) |
| Neuroleptics | 24 (14.5) | 7 (8.0) | 17 (21.8) |
| Mood stabilizersg | 1 (0.6) | 0 (0.0) | 1 (1.3) |
| Benzodiazepines | 8 (4.8) | 4 (4.6) | 4 (5.1) |
| Other psychotropic medication | 10 (6.0) | 5 (5.7) | 5 (6.4) |
| Change in psychotropic medication from before therapy to postassessment | 87 (52.4) | 45 (51.4) | 42 (53.9) |
Abbreviations: BPD, borderline personality disorder; CPT, cognitive processing therapy; DBT-PTSD, dialectical behavior therapy for posttraumatic stress disorder.
Data regarding education were available for 190 participants.
Marital status was available for 191 participants.
Data regarding suicide attempts (lifetime) were available for 186 participants.
Data regarding nonsuicidal self-injury and repeated abuse were available for 192 participants.
Data regarding additional sexual physical or sexual abuse in adulthood were available for 180 participants.
Data regarding psychotropic medication at pretherapy assessment were available for 192 participants; psychotropic medication at 15 months and change in psychotropic medication data were available for 166 participants.
Lithium, lamotrigine, carbamazepine, or valproate; atypical neuroleptics that are currently being used as mood stabilizers (ie, olanzapine, quetiapine, aripiprazole, risperidone, ziprasidone, asenapine, paliperidone, and lurasidone) have been subsumed under neuroleptics.
Treatment Integrity
Mean (SD) adherence to the respective manuals was good in both groups (DBT-PTSD, 4.1 [1.2] points; CPT, 3.9 [1.3] points). Mean (SD) therapeutic competence was likewise good (DBT-PTSD, 4.0 [0.9] points; CPT, 4.0 [0.9] points).
Primary Outcome
For both therapies, mean changes on the CAPS-5 score were significant, with unadjusted mean (SD) improvements of 19.4 (14.4) points (P < .001) in the DBT-PTSD group and 14.6 (14.8) points (P < .001) in the CPT group. These reductions correspond to large pre-to-post effect sizes (d, 1.35 and d, 0.98, respectively; Table 2). Comparisons of individual CAPS-5 scores before and after therapy (Figure 2) indicated that most participants in both groups showed improvement with respect to the primary outcome, and none showed reliable worsening.
Table 2. Primary and Secondary Outcome Data Before Therapy vs Postassessment.
| Measure | Mean (SD) | Effect size, Cohen d | Mixed linear models, β (SE) | Term | P value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Pretherapy | Postassessment | Intent-to-treat populationa | P value | Population according to protocolb | P value | ||||
| Clinician Administered PTSD Scale | |||||||||
| DBT-PTSD | 39.93 (10.84) | 20.56 (15.81) | 1.35 | NA | 1.66 | NA | β10 = −4.84 (0.73) | Time | <.001 |
| CPT | 40.96 (8.95) | 26.41 (16.04) | 0.98 | NA | 1.25 | NA | β01 = −0.30 (1.54) | Group | .85 |
| Comparison | NA | NA | 0.33 | .02 | 0.21 | .26 | β11 = 0.93 (0.47) | Group × time | .047 |
| Posttraumatic Stress Disorder Checklist for DSM-5 | |||||||||
| DBT-PTSD | 49.39 (11.46) | 23.82 (17.86) | 1.55 | NA | 2.34 | NA | β10 = −6.98 (0.89) | Time | <.001 |
| CPT | 49.54 (11.04) | 33.74 (19.60) | 0.90 | NA | 1.34 | NA | β01 = −1.24 (1.82) | Group | .50 |
| Between | NA | NA | 0.57 | <.001 | 0.46 | .04 | β11 = 1.86 (0.57) | Group × time | .001 |
| Dissociation Tension Scale–duration | |||||||||
| DBT-PTSD | 24.13 (16.88) | 14.04 (14.58) | 0.79 | NA | 1.23 | NA | β10 = −3.13 (0.74) | Time | <.001 |
| CPT | 23.96 (14.81) | 20.87 (18.08) | 0.20 | NA | 0.31 | NA | β01 = −0.57 (2.45) | Group | .82 |
| Comparison | NA | NA | 0.50 | <.001 | 0.30 | .20 | β11 = 1.17 (0.48) | Group × time | .02 |
| Dissociation Tension Scale–intensity | |||||||||
| DBT-PTSD | 2.82 (1.70) | 1.77 (1.70) | 0.82 | NA | 1.22 | NA | β10 = −0.30 (0.08) | Time | <.001 |
| CPT | 3.12 (1.62) | 2.61 (1.88) | 0.33 | NA | 0.55 | NA | β01 = 0.28 (0.27) | Group | .32 |
| Comparison | NA | NA | 0.39 | .007 | 0.20 | 0.41 | β11 = 0.09 (0.05) | Group × time | .09 |
| Borderline Symptom List–23 | |||||||||
| DBT-PTSD | 2.01 (0.82) | 1.14 (0.86) | 1.11 | NA | 1.4 | NA | β10 = −0.25 (0.04) | Time | <.001 |
| CPT | 2.04 (0.80) | 1.63 (0.95) | 0.47 | NA | 0.72 | NA | β01 = −0.001 (0.12) | Group | .99 |
| Comparison | NA | NA | 0.55 | <.001 | 0.27 | .22 | β11 = 0.08 (0.03) | Group × time | .003 |
| Borderline Symptom List–behavioral items | |||||||||
| DBT-PTSD | 0.34 (0.33) | 0.18 (0.18) | 0.54 | NA | 0.76 | NA | NAc | NAc | NAc |
| CPT | 0.31 (0.28) | 0.29 (0.25) | 0.08 | NA | 0.34 | NA | |||
| Comparison | NA | NA | 0.50 | <.001 | 0.39 | .06 | |||
| Beck Depression Inventory–II | |||||||||
| DBT-PTSD | 33.24 (11.20) | 21.57 (14.04) | 0.98 | NA | 1.37 | NA | β10 = −3.20 (0.78) | Time | <.001 |
| CPT | 34.10 (10.81) | 26.99 (15.09) | 0.48 | NA | 0.76 | NA | β01 = 0.33 (1.93) | Group | .86 |
| Comparison | NA | NA | 0.32 | .02 | 0.17 | .45 | β11 = 0.86 (0.49) | Group × time | .09 |
| Global Assessment of Functioning | |||||||||
| DBT-PTSD | 50.75 (9.14) | 60.13 (13.95) | 0.67 | NA | 1.12 | NA | β10 = 2.38 (0.62) | Time | <.001 |
| CPT | 49.19 (7.69) | 55.25 (12.55) | 0.51 | NA | 0.87 | NA | β01 = −0.71 (1.39) | Group | .61 |
| Comparison | NA | NA | 0.26 | .08 | 0.27 | .16 | β11 = −0.52 (0.40) | Group × time | .20 |
Abbreviations: CPT, cognitive processing therapy; DBT-PTSD, dialectical behavior therapy for posttraumatic stress disorder; NA, not applicable; PTSD, posttraumatic stress disorder.
Intent-to-treat: n = 98 (DBT-PTSD), and n = 95 (CPT), respectively; besides the Dissociation Tension Scale–duration under CPT and the Borderline Symptom List–behavioral items under CPT all pre-to-post effect sizes d were statistically different from 0.
According to protocol: n = 73 (DBT-PTSD), and n = 58 (CPT), respectively; besides the Dissociation Tension Scale–duration under CPT, all pre-to-post effect sizes d were statistically different from 0.
Mixed linear models for the Borderline Symptom List–behavioral items are not reported because the assumption of linearity was not met and the Newton-Raphson algorithms used in generalized linear models did not consistently converge during the procedure of multiple imputation.
Figure 2. Individual Participant Scores.
Total Clinician-Administered PTSD Scale for DSM-5 (CAPS) scores of participants randomized to dialectical behavioral therapy for posttraumatic stress disorder (DBT-PTSD) or cognitive processing therapy (CPT) (intent-to-treat population) before therapy (month 0) vs postassessment (month 15). Values below the main diagonal indicate improvements; the dotted diagonals represent reliable change.
Between-group comparison of the predefined primary outcome favored DBT-PTSD. For the ITT population, the mean change on the CAPS-5 scores was larger for DBT-PTSD than CPT, albeit with a small effect size (d, 0.33; P = .02). Similarly, the mixed linear model indicated a steeper slope of linear improvements for DBT-PTSD (β11, 0.93 ± 0.47; P = .047; Table 2 and Figure 3). The more pronounced decline of CAPS-5 scores in the DBT-PTSD group was mirrored by a higher percentage of participants achieving symptomatic remission (52 of 89 observed cases [58.4%] vs 35 of 86 observed cases [40.7%]; P = .02), reliable improvement (73 [74.5%] vs 53 [55.8%]; P = .006), and reliable recovery (52 of 91 observed cases [57.1%] vs 34 of 88 observed cases [38.6%]; P = .01). However, the percentage of participants achieving early remission was higher for CPT than DBT-PTSD (9 [9.5%] vs 2 [2.0%]; P = .03).
Figure 3. Dimensional and Categorical Treatment Outcomes.

Scores and categories are based on Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) scores for dialectical behavioral therapy for posttraumatic stress disorder (DBT-PTSD; dark color) and cognitive processing therapy (CPT; light color). Error bars indicate standard errors of means. A, Course of mean CAPS scores from before therapy (month 0) to postassessment (month 15). B, Rates of symptomatic remission from the diagnosis of PTSD (not meeting the full criteria of posttraumatic stress disorder (PTSD) in the CAPS-5) of reliable improvement (improvement from before to after therapy that exceeds a threshold compatible with the unreliability of measurement) and reliable recovery (reliable improvement plus symptomatic remission).
Secondary Outcomes
Changes in the PTSD Checklist for DSM-5 were large in both groups. Mean changes in the ITT population were larger for the DBT-PTSD group (DBT-PTSD: d, 1.55; CPT: d, 0.90; between-group effect size d, 0.57; P < .001). This finding was supported by the significant group × time interaction in the mixed linear model, indicating a more pronounced improvement in the DBT-PTSD group for self-rated severity of PTSD symptoms (β11, 1.86 ± 0.57; P = .001).
Findings regarding dissociation were less homogeneous. While duration of dissociative symptoms (Dissociation Tension Scale) declined in both groups, decline in the intensity of dissociative symptoms was significant only for DBT-PTSD. Mean changes were large for DBT-PTSD (d, 0.79 and d, 0.82 for the duration and intensity of dissociation, respectively) and small for CPT (d, 0.20 and d, 0.33, respectively). Between-group effect sizes were significant for both duration and intensity of dissociation (d, 0.50; P < .001; d, 0.39; P = .007). Mixed linear models partially supported these findings (β11, 0.09 ± 0.05; P = .02 and β11, 1.17 ± 0.48, respectively; P = .09 for the group × time interactions; Table 2).
Pre-to-post effect sizes in the BSL-23 were large for DBT-PTSD (d, 1.11) and medium for CPT (d, 0.47). The difference between the groups was significant (between-group effect size: d, 0.55; P < .001). While the BSL–behavioral items score involving frequencies of dysfunctional behaviors, such as self-harm, high-risk behaviors, or consumption of drugs, declined in both groups, the decline in the DBT-PTSD group was significant (d, 0.54; P < .001), while that for CPT was not (d, 0.08; P = .42). This decline was more pronounced under DBT-PTSD (between-group effect size: d, 0.50; P < .001).
Improvements of Beck Depression Inventory–II scores were large for DBT-PTSD (d, 0.98) and medium for CPT (d, 0.48). This difference of pre-to-post differences was small and significant (d, 0.32; P = .02), but the group × time interaction in the mixed linear model was not significant. With respect to the Global Assessment of Functioning, medium improvements were observed (DBT-PTSD: d, 0.67; CPT: d, 0.51), but there were no significant between-group effects (Table 2). The means (SDs) for all dimensional scales and assessment points and the length of hospitalization by condition are provided in eTable 3 and 4 in Supplement 1, respectively.
Results pertaining to the analyses according to protocol are summarized in Table 2. No differences in any outcome variables were noted between the 3 sites (eTable 5 in Supplement 1).
No suicides occurred during the observation period. One suicide attempt was noted in the CPT group.
Discussion
Dialectical behavior therapy for PTSD (DBT-PTSD) is designed as a phase-based treatment specifically for patients with highly symptomatic CA-associated PTSD and complicating conditions, such as emotion dysregulation and other features of BPD. This randomized clinical trial compared the efficacy of DBT-PTSD with that of CPT, which is one of the best available treatments for PTSD but is not specifically designed for this population. Improvements in the primary outcome measure were large and significant for both treatments but more pronounced in the DBT-PTSD group. The same results were seen for other aspects of psychopathology closely associated with a history of CA, such as dissociation, self-harm, and high-risk behaviors. Furthermore, participants in the DBT-PTSD group were more likely to achieve symptomatic remission, reliable improvement, and reliable recovery and were less likely to drop out of treatment.
The large pre-to-post effect sizes in both treatment groups parallel the effect sizes observed in previous studies of both CPT and DBT-PTSD.41,42,43,44,70 Similarly, the low rates of suicidal acts and the absence of significant symptom exacerbations in both groups are in line with previous studies.
Cognitive processing therapy did not perform as well as it has in PTSD studies in general.41,44 This might be because of the relatively high dropout rate within the first 3 months. It is unclear how sessions 1 to 4, which were added to the CPT protocol for safety reasons, affected treatment dropout. On the other hand, high dropout rates might be explained by clinical characteristics of the study population (in that all participants met at least 3 BPD criteria, including affective instability, and 48% had co-occurring BPD). These characteristics might require specifically tailored interventions for this population, as provided by DBT-PTSD.
Strengths
Strengths of this study included measures to control for potentially confounding variables. Both groups received equal dosage and frequency of therapy, the process of therapist training was guided by the treatment developers, training and experience of the therapists were balanced across treatment groups, and structured observer-based scales were used to assess treatment integrity. In line with the updated CONSORT statement, randomization was concealed to all persons involved,71 and raters were blinded.
We tried to balance developers’ bias by including the CPT developer (P.A.R.) as a senior trainer and consultant for CPT supervisors. Therapists in both groups had similar experience and competence and received the same amounts of training and supervision. Assessments of adherence and competence revealed good treatment integrity to both manuals.
Limitations
Nevertheless, allegiance effects cannot be completely ruled out, and the findings need to be replicated by independent research groups. In the DBT-PTSD arm, the treatment developers were part of the consultation teams, while in the CPT arm, the supervisors were experienced in cognitive behavior therapy but did not have more experience in CPT than the therapists.
We emphasize that the study population consisted of patients whose PTSD was associated with CA and who had severe problems in emotion regulation and features of BPD, so the findings cannot be extended to PTSD in general. It also remains unknown whether our results can be generalized to patients of any age, sex, or gender identity. It is further unclear whether the improvements achieved and the superiority of DBT-PTSD over CPT will persist in the long term. These limitations should be addressed by future research.
Given the dropout rate of 32%, the results may be affected by attrition bias. To minimize potential bias, the primary analysis was based on the ITT sample.
Finally, the observed effects might have been confounded by intercurrent treatments. However, this seems unlikely since, with the exception of inpatient crisis interventions, only CPT and DBT-PTSD were allowed during the study period. Use of medication was unrestricted, but neither hospitalization nor changes in psychotropic medication were significantly associated with the outcome variables.
Conclusions
The study shows that even severe forms of CA-associated PTSD that include multiple co-occurring mental disorders and emotion dysregulation can be treated efficaciously. Future studies should strive for a better definition of patient groups that might profit from current therapies. In particular, additional research is required to test whether treatment efficacy might extend beyond adult women, and whether the DBT-PTSD protocol could be condensed to reduce cost burdens and patient burdens and facilitate dissemination.
eAppendix. Description of study treatments.
eTable 1. Therapist characteristics.
eTable 2. Number of observed cases per assessment for the primary outcome (CAPS).
eTable 3. Means and standard deviations (SD) for the primary and secondary outcome data at all assessments.
eTable 4. Hospitalization during treatment.
eTable 5. Potential impact of the study site on the change scores of primary and secondary assessments of outcome.
Translated Study Protocol.
Data Sharing Statement.
References
- 1.Cutajar MC, Mullen PE, Ogloff JR, Thomas SD, Wells DL, Spataro J. Psychopathology in a large cohort of sexually abused children followed up to 43 years. Child Abuse Negl. 2010;34(11):813-822. doi: 10.1016/j.chiabu.2010.04.004 [DOI] [PubMed] [Google Scholar]
- 2.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68-81. doi: 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- 3.Hailes HP, Yu R, Danese A, Fazel S. Long-term outcomes of childhood sexual abuse: an umbrella review. Lancet Psychiatry. 2019;6(10):830-839. doi: 10.1016/S2215-0366(19)30286-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197(5):378-385. doi: 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pérez-Fuentes G, Olfson M, Villegas L, Morcillo C, Wang S, Blanco C. Prevalence and correlates of child sexual abuse: a national study. Compr Psychiatry. 2013;54(1):16-27. doi: 10.1016/j.comppsych.2012.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Arch Gen Psychiatry. 2010;67(7):712-719. doi: 10.1001/archgenpsychiatry.2010.71 [DOI] [PubMed] [Google Scholar]
- 7.Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533-545. doi: 10.4088/JCP.v69n0404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scheiderer EM, Wood PK, Trull TJ. The comorbidity of borderline personality disorder and posttraumatic stress disorder: revisiting the prevalence and associations in a general population sample. Borderline Personal Disord Emot Dysregul. 2015;2(1):11. doi: 10.1186/s40479-015-0032-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pagura J, Stein MB, Bolton JM, Cox BJ, Grant B, Sareen J. Comorbidity of borderline personality disorder and posttraumatic stress disorder in the U.S. population. J Psychiatr Res. 2010;44(16):1190-1198. doi: 10.1016/j.jpsychires.2010.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;62(6):553-564. doi: 10.1016/j.biopsych.2006.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heffernan K, Cloitre M. A comparison of posttraumatic stress disorder with and without borderline personality disorder among women with a history of childhood sexual abuse: etiological and clinical characteristics. J Nerv Ment Dis. 2000;188(9):589-595. doi: 10.1097/00005053-200009000-00005 [DOI] [PubMed] [Google Scholar]
- 12.Shea MT, Zlotnick C, Weisberg RB. Commonality and specificity of personality disorder profiles in subjects with trauma histories. J Pers Disord. 1999;13(3):199-210. doi: 10.1521/pedi.1999.13.3.199 [DOI] [PubMed] [Google Scholar]
- 13.Zanarini MC, Frankenburg FR, Dubo ED, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155(12):1733-1739. doi: 10.1176/ajp.155.12.1733 [DOI] [PubMed] [Google Scholar]
- 14.McLean LM, Gallop R. Implications of childhood sexual abuse for adult borderline personality disorder and complex posttraumatic stress disorder. Am J Psychiatry. 2003;160(2):369-371. doi: 10.1176/appi.ajp.160.2.369 [DOI] [PubMed] [Google Scholar]
- 15.Karatzias T, Murphy P, Cloitre M, et al. Psychological interventions for ICD-11 complex PTSD symptoms: systematic review and meta-analysis. Psychol Med. 2019;49(11):1761-1775. doi: 10.1017/S0033291719000436 [DOI] [PubMed] [Google Scholar]
- 16.Herzog JI, Thome J, Demirakca T, et al. Influence of severity of type and timing of retrospectively reported childhood maltreatment on female amygdala and hippocampal volume. Sci Rep. 2020;10(1):1903. doi: 10.1038/s41598-020-57490-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teicher MH, Khan A. Childhood maltreatment, cortical and amygdala morphometry, functional connectivity, laterality, and psychopathology. Child Maltreat. 2019;24(4):458-465. doi: 10.1177/1077559519870845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lyssenko L, Schmahl C, Bockhacker L, Vonderlin R, Bohus M, Kleindienst N. Dissociation in psychiatric disorders: a meta-analysis of studies using the dissociative experiences scale. Am J Psychiatry. 2018;175(1):37-46. doi: 10.1176/appi.ajp.2017.17010025 [DOI] [PubMed] [Google Scholar]
- 19.Naismith I, Zarate Guerrero S, Feigenbaum J. Abuse, invalidation, and lack of early warmth show distinct relationships with self-criticism, self-compassion, and fear of self-compassion in personality disorder. Clin Psychol Psychother. 2019;26(3):350-361. doi: 10.1002/cpp.2357 [DOI] [PubMed] [Google Scholar]
- 20.McDonagh-Coyle A, Friedman MJ, McHugo GJ, et al. Randomized trial of cognitive behavioral therapy for chronic PTSD in adult female childhood sexual abuse survivors. J Consult Clin Psychol. 2005;73(3):515-524. doi: 10.1037/0022-006X.73.3.515 [DOI] [PubMed] [Google Scholar]
- 21.Clarke SB, Rizvi SL, Resick PA. Borderline personality characteristics and treatment outcome in cognitive-behavioral treatments for PTSD in female rape victims. Behav Ther. 2008;39(1):72-78. doi: 10.1016/j.beth.2007.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feeny NC, Zoellner LA, Foa EB. Treatment outcome for chronic PTSD among female assault victims with borderline personality characteristics: a preliminary examination. J Pers Disord. 2002;16(1):30-40. doi: 10.1521/pedi.16.1.30.22555 [DOI] [PubMed] [Google Scholar]
- 23.Hembree EA, Cahill SP, Foa EB. Impact of personality disorders on treatment outcome for female assault survivors with chronic posttraumatic stress disorder. J Pers Disord. 2004;18(1):117-127. doi: 10.1521/pedi.18.1.117.32767 [DOI] [PubMed] [Google Scholar]
- 24.Holder N, Holliday R, Pai A, Surís A. Role of borderline personality disorder in the treatment of military sexual trauma-related posttraumatic stress disorder with cognitive processing therapy. Behav Med. 2017;43(3):184-190. doi: 10.1080/08964289.2016.1276430 [DOI] [PubMed] [Google Scholar]
- 25.Kredlow MA, Szuhany KL, Lo S, et al. Cognitive behavioral therapy for posttraumatic stress disorder in individuals with severe mental illness and borderline personality disorder. Psychiatry Res. 2017;249:86-93. doi: 10.1016/j.psychres.2016.12.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162(2):214-227. doi: 10.1176/appi.ajp.162.2.214 [DOI] [PubMed] [Google Scholar]
- 27.Ronconi JM, Shiner B, Watts BV. Inclusion and exclusion criteria in randomized controlled trials of psychotherapy for PTSD. J Psychiatr Pract. 2014;20(1):25-37. doi: 10.1097/01.pra.0000442936.23457.5b [DOI] [PubMed] [Google Scholar]
- 28.Harned MS, Chapman AL, Dexter-Mazza ET, Murray A, Comtois KA, Linehan MM. Treating co-occurring Axis I disorders in recurrently suicidal women with borderline personality disorder: a 2-year randomized trial of dialectical behavior therapy versus community treatment by experts. J Consult Clin Psychol. 2008;76(6):1068-1075. doi: 10.1037/a0014044 [DOI] [PubMed] [Google Scholar]
- 29.Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav Res Ther. 2014;55:7-17. doi: 10.1016/j.brat.2014.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Psychological Association Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Published 2017. Accessed August 9, 2019. https://www.apa.org/ptsd-guideline/ptsd.pdf
- 31.International Society for Traumatic Stress Studies Posttraumatic stress disorder prevention and treatment guidelines: methodology and recommendations. Published 2019. Accessed September 2, 2019. https://istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- 32.US Department of Veteran Affairs VA/DOD Clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Published 2017. Accessed August 15, 2019. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf
- 33.Berliner L, Bisson J, Cloitre M, et al. New ISTSS prevention and treatment guidelines. Published 2019. Accessed August 9, 2019. http://istss.org/treating-trauma/new-istss-prevention-and-treatment-guidelines
- 34.De Jongh A, Resick PA, Zoellner LA, et al. Critical analysis of the current treatment guidelines for complex PTSD in adults. Depress Anxiety. 2016;33(5):359-369. doi: 10.1002/da.22469 [DOI] [PubMed] [Google Scholar]
- 35.Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. Treatment of complex PTSD: results of the ISTSS expert clinician survey on best practices. J Trauma Stress. 2011;24(6):615-627. doi: 10.1002/jts.20697 [DOI] [PubMed] [Google Scholar]
- 36.Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. J Consult Clin Psychol. 2002;70(5):1067-1074. doi: 10.1037/0022-006X.70.5.1067 [DOI] [PubMed] [Google Scholar]
- 37.Cloitre M, Stovall-McClough KC, Nooner K, et al. Treatment for PTSD related to childhood abuse: a randomized controlled trial. Am J Psychiatry. 2010;167(8):915-924. doi: 10.1176/appi.ajp.2010.09081247 [DOI] [PubMed] [Google Scholar]
- 38.Harned MS, Gallop RJ, Valenstein-Mah HR. What changes when? the course of improvement during a stage-based treatment for suicidal and self-injuring women with borderline personality disorder and PTSD. Psychother Res. 2018;28(5):761-775. doi: 10.1080/10503307.2016.1252865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosner R, Rimane E, Frick U, et al. Effect of developmentally adapted cognitive processing therapy for youth with symptoms of posttraumatic stress disorder after childhood sexual and physical abuse: a randomized clinical trial. JAMA Psychiatry. 2019;76(5):484-491. doi: 10.1001/jamapsychiatry.2018.4349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences. Oxford University Press; 2007. [Google Scholar]
- 41.Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. J Consult Clin Psychol. 2008;76(2):243-258. doi: 10.1037/0022-006X.76.2.243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bohus M, Dyer AS, Priebe K, et al. Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: a randomised controlled trial. Psychother Psychosom. 2013;82(4):221-233. doi: 10.1159/000348451 [DOI] [PubMed] [Google Scholar]
- 43.Steil R, Dyer A, Priebe K, Kleindienst N, Bohus M. Dialectical behavior therapy for posttraumatic stress disorder related to childhood sexual abuse: a pilot study of an intensive residential treatment program. J Trauma Stress. 2011;24(1):102-106. doi: 10.1002/jts.20617 [DOI] [PubMed] [Google Scholar]
- 44.Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. J Consult Clin Psychol. 2005;73(5):965-971. doi: 10.1037/0022-006X.73.5.965 [DOI] [PubMed] [Google Scholar]
- 45.Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J Consult Clin Psychol. 2002;70(4):867-879. doi: 10.1037/0022-006X.70.4.867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Resick PA, Wachen JS, Dondanville KA, et al. ; and the STRONG STAR Consortium . Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2017;74(1):28-36. doi: 10.1001/jamapsychiatry.2016.2729 [DOI] [PubMed] [Google Scholar]
- 47.Bohus M, Schmahl C, Fydrich T, et al. A research programme to evaluate DBT-PTSD, a modular treatment approach for complex PTSD after childhood abuse. Borderline Personal Disord Emot Dysregul. 2019;6:7. doi: 10.1186/s40479-019-0099-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Resick PA, Monson CM, Chard KM. Cognitive Processing Therapy for PTSD: A Comprehensive Manual. Guilford Press; 2016. [Google Scholar]
- 49.Linehan MM. DBT Skills Training Manual. Guilford Press; 2014. [Google Scholar]
- 50.Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behav Res Ther. 2005;43(4):413-431. doi: 10.1016/j.brat.2004.03.006 [DOI] [PubMed] [Google Scholar]
- 51.Gilbert P. Compassion-Focused Therapy: Distinctive Features (CBT Distinctive Features). Routledge; 2010. doi: 10.4324/9780203851197 [DOI] [Google Scholar]
- 52.Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: The Process And Practice of Mindful Change. Guilford Press; 2011. [Google Scholar]
- 53.Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). Published 2013. Accessed January 5, 2014. http://www.ptsd.va.gov
- 54.Dittmann C, Müller-Engelmann M, Resick PA, et al. Adherence rating scale for cognitive processing therapy–cognitive only: analysis of psychometric properties. Behav Cogn Psychother. 2017;45(6):661-670. doi: 10.1017/S1352465816000679 [DOI] [PubMed] [Google Scholar]
- 55.Dittmann C, Müller-Engelmann M, Stangier U, et al. Disorder- and treatment-specific therapeutic competence scales for posttraumatic stress disorder intervention: development and psychometric properties. J Trauma Stress. 2017;30(6):614-625. doi: 10.1002/jts.22236 [DOI] [PubMed] [Google Scholar]
- 56.First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin LS. User’s Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I)—Clinical Version. American Psychiatric Press; 1997. [Google Scholar]
- 57.Loranger AW, Sartorius N, Andreoli A, et al. The international personality disorder examination: the Health Organization/Alcohol, Drug Abuse, and Mental Health Administration international pilot study of personality disorders. Arch Gen Psychiatry. 1994;51(3):215-224. doi: 10.1001/archpsyc.1994.03950030051005 [DOI] [PubMed] [Google Scholar]
- 58.Müller-Engelmann M, Schnyder U, Dittmann C, et al. Psychometric properties and factor structure of the German version of the clinician-administered PTSD scale for DSM-5. Assessment. Published May 1, 2018. doi: 10.1177/1073191118774840 [DOI] [PubMed] [Google Scholar]
- 59.Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33(6):766-771. doi: 10.1001/archpsyc.1976.01770060086012 [DOI] [PubMed] [Google Scholar]
- 60.Weathers FW, Litz BT, Keane TM, et al. The PTSD Checklist for DSM-5 (PCL-5). Published 2013. Accessed January 5, 2014. https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- 61.Bohus M, Kleindienst N, Limberger MF, et al. The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology. 2009;42(1):32-39. doi: 10.1159/000173701 [DOI] [PubMed] [Google Scholar]
- 62.Bohus M, Limberger MF, Frank U, Sender I, Gratwohl T, Stieglitz RD. Development of the Borderline Symptom List. Psychother Psychosom Med Psychol. 2001;51(5):201-211. doi: 10.1055/s-2001-13281 [DOI] [PubMed] [Google Scholar]
- 63.Beck A, Steer R, Brown G.. Beck Depression Inventory–II Manual. Psychological Corporation; 1996. [Google Scholar]
- 64.Stiglmayr C, Schimke P, Wagner T, et al. Development and psychometric characteristics of the Dissociation Tension Scale. J Pers Assess. 2010;92(3):269-277. doi: 10.1080/00223891003670232 [DOI] [PubMed] [Google Scholar]
- 65.Enders CK. A primer on the use of modern missing-data methods in psychosomatic medicine research. Psychosom Med. 2006;68(3):427-436. doi: 10.1097/01.psy.0000221275.75056.d8 [DOI] [PubMed] [Google Scholar]
- 66.Rubin DB. Multiple imputation after 18+ years. J Am Stat Assoc. 1996;91(434):473-489. doi: 10.1080/01621459.1996.10476908 [DOI] [Google Scholar]
- 67.Schafer JL. Analysis of Incomplete Multivariate Data. Chapman and Hall; 1997. doi: 10.1201/9781439821862 [DOI] [Google Scholar]
- 68.Christensen L, Mendoza JL. A method of assessing change in a single subject: an alteration of the RC index. Behav Ther. 1986;17:305-308. doi: 10.1016/S0005-7894(86)80060-0 [DOI] [Google Scholar]
- 69.Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M. Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data. Lancet. 2018;391(10121):679-686. doi: 10.1016/S0140-6736(17)32133-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Steil R, Dittmann C, Müller-Engelmann M, Dyer A, Maasch AM, Priebe K. Dialectical behaviour therapy for posttraumatic stress disorder related to childhood sexual abuse: a pilot study in an outpatient treatment setting. Eur J Psychotraumatol. 2018;9(1):1423832. doi: 10.1080/20008198.2018.1423832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schulz KF, Altman DG, Moher D; CONSORT Group . CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Description of study treatments.
eTable 1. Therapist characteristics.
eTable 2. Number of observed cases per assessment for the primary outcome (CAPS).
eTable 3. Means and standard deviations (SD) for the primary and secondary outcome data at all assessments.
eTable 4. Hospitalization during treatment.
eTable 5. Potential impact of the study site on the change scores of primary and secondary assessments of outcome.
Translated Study Protocol.
Data Sharing Statement.




