Abstract
Surgical site infection (SSI) rates in low- and middle-income countries (LMICs) range from 8 to 30% of procedures, making them the most frequent healthcare-acquired infection (HAI) with substantial morbidity, mortality, and economic impacts. Presented here is an approach to surgical site infection prevention based on surveillance and focused on five critical areas identified by international experts. These five areas include
1. Collecting valid, high-quality data;
2. Linking HAIs to economic incapacity, underscoring the need to prioritize infection prevention activities;
3. Implementing SSI surveillance within infection prevention and control (IPC) programs to enact structural changes, develop procedural skills, and alter healthcare worker behaviors;
4. Prioritizing IPC training for healthcare workers in LMICs to conduct broad-based surveillance and to develop and implement locally applicable IPC programs; and
5. Developing a highly accurate and objective international system for defining SSIs, which can be translated globally in a straightforward manner.
Finally, we present a clear, unambiguous framework for successful SSI guideline implementation that supports developing sustainable IPC programs in LMICs. This entails
1. Identifying index operations for targeted surveillance;
2. Identifying IPC “champions” and empowering healthcare workers;
3. Using multimodal improvement measures;
4. Positioning hand hygiene programs as the basis for IPC initiatives;
5. Use of telecommunication devices for surveillance and healthcare outcome follow-ups.
Additionally, special considerations for pediatric SSIs, antimicrobial resistance development, and antibiotic stewardship programs are addressed.
Introduction
Increased awareness of infection prevention and control as a critical patient safety issue in low- and middle-income countries
The last decade has seen increased attention to the creation and improvement of hospital- and community-based infection prevention and control programs (Allegranzi et al., 2019, Allegranzi et al., 2017, Storr et al., 2017, World Health Organization, 2011). The publication of quantitative information detailing the extent of the problem in low- and middle-income countries (LMICs) coupled with the emergence of public health crises has highlighted the need for trained infection prevention and control (IPC) personnel. Outbreaks of HIV, SARS-CoV, MERS-CoV, Ebola virus disease, Zika virus, and COVID-19 have renewed focus on appropriate IPC measures to protect healthcare providers and improve patient health (Reperant and Osterhaus, 2017). In healthcare-associated infections (HAI) and community-based epidemics, trained IPC specialists are critical for successful responses.
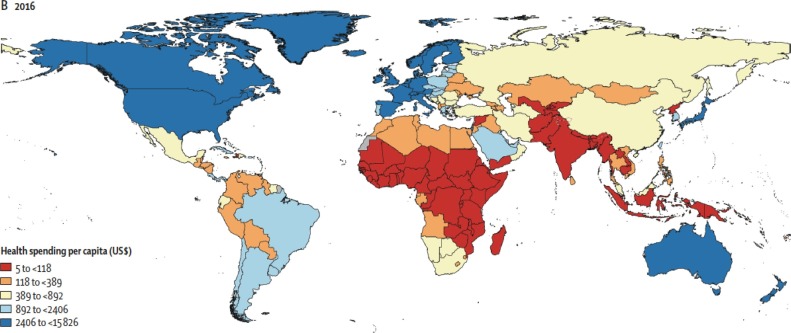
Two major obstacles to IPC implementation in LMICs include a lack of adequate funding and insufficient human resources (Figure 1) ( Global Burden of Disease Health Financing Collaborator Network, 2019). Some acute care settings in LMICs may lack IPC programs altogether, and the trained personnel required to conduct broad-based surveillance and follow-up infection prevention activities may not be available.
Figure 1.
The Health Care Economics in GDP/Capita in 2016. Between 1995 and 2016, health spending grew at a rate of 4.00% in 22 of 195 countries. The highest annual growth rates in per capita health spending were observed in upper-middle-income countries (5.55%), mainly due to growth in government health spending, and in lower-middle-income countries (3.71%), mainly from Development Assistance for Health. Health spending globally reached $8.0 trillion in 2016, comprising 8.6% of the global economy.
Why surgical site infections? A high-value focus for IPC in healthcare settings
Surgical site infections (SSIs) in LMICs are an example of HAIs that can be prevented by established techniques. SSI rates are declining in high-income countries with clean operations, with rates approximating 1–4% (Gaynes et al., 2001, Edwards et al., 2009). This reduction in SSI rates is not reflected in LMICs. SSI rates in LMICs range from 8 to 30% (Allegranzi et al., 2011, Biccard et al., 2018, Sobhy et al., 2019, Horan et al., 2008). In these environments, SSIs are the most common HAI, often with substantial morbidity, mortality, and economic impacts. Thus, SSIs are an important target for quality improvement and patient safety initiatives (Allegranzi et al., 2011, Bagheri Nejad et al., 2011).
There is considerable variability of SSI rates between hospitals, across regions within one country, and also in continental groupings. To date, this variability remains unexplained. There are significant concerns regarding the validity of published data and the challenges this creates when defining IPC priorities within health care systems. Importantly, the precision of studies examining SSI rates is not increased by more copious amounts of data. Only when there is an improved understanding of SSIs via surveyor training, experience, and the standardization of metrics allowing interrater reliability, can data accuracy be improved. Concerning standardized SSI metrics, the current Centers for Disease Control/National Health Care Safety Network (CDC/NHSN) scheme is based on a complex system that prevents data clarity (Horan et al., 2008). Further, variations in SSI rates between healthcare facilities may not be random, and therefore, pooling is not an accurate measure of risk across all hospitals. The aggregation of data does not itself ensure a generalizable statement.
These problems are also present in systematic reviews. Individual reports in LMIC settings are skewed towards bigger, higher-level hospitals with functioning microbiology laboratories. Institutions of this size are more likely to have IPC activity and personnel awareness of IPC programs. Conversely, most patient care occurs in smaller hospitals, described broadly as first-level hospitals with approximately 50–200 beds serving populations between 50,000–200,000 people (Mock et al., 2015). Many of these hospitals have neither microbiology laboratories nor effective IPC activity, such as hand hygiene programs and SSI surveillance. Therefore, we believe the accumulation of valid, high-quality data that accurately captures SSI rates in individual healthcare settings is a critical need in LMIC healthcare settings.
The economic and human costs of SSIs in LMICs
SSIs impact many aspects of the patient journey. These include increased pain and reduction in mobility, delayed wound healing, increased use of antibiotics, a common need for additional surgery, increased length of hospital stay, and increased mortality (Harrop et al., 2012). The consequences of such infections have been explored in various modeling studies with researchers pinpointing patient fees and out-of-pocket expenses as impediments to healthcare-seeking behaviors among the most vulnerable (McIntyre et al., 2006). A more extended hospital stay represents a direct cost to the hospital system and the payer and has patient and societal economic implications. Some of these include the cost of medical supplies, nursing care, and the extended loss of work/productivity. In low-resource settings, where many live on less than $2 USD per day, even minor SSIs may have a significant social and economic burden. Framing the impact of SSIs to include morbidity, mortality, and economic data can further highlight this challenge's urgency and focus attention on the benefits derived from successful interventions.
The most complete work on SSIs' societal costs has focused on maternal morbidity and mortality (Kes et al., 2015). The unexpected occurrence of maternal morbidity triggers a series of consequences that are often amplified by women's central economic and social roles in LMIC households. The loss of a woman’s contributions, combined with healthcare bills' spending shock, can force a household into poverty. Other consequences include negative impacts on nutrition, reduced access to healthcare for surviving children, and lost educational opportunities as older children may withdraw from school to fulfill roles previously occupied by the mother (Molla et al., 2015). Connecting HAIs to financial incapacity further underscores the need for priority investments in specific HAI prevention activities.
Role of surgical site infections as the initial target of HAI surveillance
The WHO and CDC have developed and published SSI prevention guidelines based on systematic reviews, meta-analyses, and GRADE methodologies (Allegranzi et al., 2016a, Allegranzi et al., 2016b, Berrios-Torres et al., 2017). These were the first major SSI guidelines to pivot from expert opinion-based guidance to a systematic, transparent, and evidence-based approach. Further strengthening these guides is the WHO’s commitment to implement strategies sensitive to local cultural practices. Collectively, this evidence-based, culturally-considerate approach to healthcare intervention provides the best chance for successful IPC program implementation. Additionally, the use of multimodal improvement strategies that include communication plans, emphasizes the desire to increase utilization of existing tools and recommendations (Allegranzi et al., 2018, Allegranzi et al., 2019, Allegranzi et al., 2017, Ariyo et al., 2019, Tartari et al., 2019). These recommendations and associated implementation approaches provide the framework for hospital-level programs targeting a reduction in SSIs.
Establishing IPC programs with SSI components is an ideal focus for introducing critical structural changes, procedural alterations, and behavioral skills for all healthcare workers. The identification of SSIs is perhaps less difficult than other HAIs and includes teams across the health system who are responsible for surgical patient care. Identifying an SSI does not solely depend on microbiology, radiology, or other laboratory services for diagnosis. SSIs may be addressed by the surgeon and a range of other healthcare providers. Surveillance is crucial to reducing SSI rates, and to achieve this, a trained team is necessary to examine at-risk wounds and support the dissemination of results.
Initial scope and design of IPC programs
The WHO has stated that “an IPC program with a dedicated, trained team should be in place in each acute healthcare facility for the purpose of preventing HAIs and combating antimicrobial resistance through IPC good practices” (Storr et al., 2017; Table 1). The number of trained professionals necessary to implement such recommendations is not defined but generally considered to be one IPC practitioner per 200–250 beds. Without dedicated IPC programs, some IPC activities might still exist, but the likelihood of their success, sustainability, and appropriate resource allocation is limited. To fulfill the requirements of a successful SSI improvement program, consideration must be given to both the broader IPC program recommendations and any existing safe surgery programs. More recently, the WHO has outlined the minimum requirements for IPC programs in a comprehensive document to assist countries with IPC implementation ( World Health Organization, 2016b).
Table 1.
The components of a full infection prevention and control program.
| The WHO recommendation states that a program consists of (Storr, 2017 #223): |
|
|
|
|
|
|
|
Is this achievable as a start-up model for infection prevention and control services?
Addressing the lack of certified/professionally recognized IPC training
Providing IPC training to healthcare workers is vital for patient safety and to reduce the measurables of HAIs and antimicrobial resistance (AMR). This is well known, and various training programs have been created to train broad-based IPC personnel. Most IPC strategies are developed following North American and/or European standards, with little input from practitioners working in LMICs. In LMICs with national IPC strategies, there may be a lack of resources to fully implement these programs (Sastry et al., 2017). Most training curricula for health professionals at all degree levels lack IPC components that sensitize and cultivate an interest in IPC by healthcare professionals. IPC is not recognized in many countries as a specialty, which hinders structured career paths. In countries such as South Africa, Zimbabwe, and Egypt, where IPC is offered as a graduate-level concentration, there has been progress in IPC implementation.
Failing to recognize IPC specialists and their role in overseeing the implementation of IPC programs is an obstacle to program growth and sustainability. This challenge persists in settings where national programs have developed policies, guidelines, strategic plans, and short course IPC training (online and in-person) for frontline healthcare workers (Pruckner et al., 2019). The reality in many LMICs is that there are insufficient, trained personnel to conduct broad-based surveillance or develop and implement a formal IPC program. Therefore, it is necessary to determine aspects of the recommended IPC structure that are indispensable for a specific healthcare facility through discussions with facility leadership, staff, regional experts, and global authorities.
The details of surgical site infection surveillance
Accurate risk assessment tools
Certain patient characteristics are related to higher infection rates, and when risk-adjusting is not applied to observed infection rates, this may lead to false conclusions. The current infection rating system–referred to as the National Nosocomial Infection Survey–evolved from data collected as part of the US CDC Study of the Efficacy of Nosocomial Infection Control (SENIC study) (Haley et al., 1985). The index was developed based on 58,498 patients undergoing operations in 1970. Analyzing ten risk-factors with stepwise multiple logistic regression techniques, the authors found that a model combining information on three of the risk factors predicted a patient's probability of developing an SSI. These three risk factors were wound class, operation time, and the American Society of Anesthesia (ASA) score. The index as a predictor of SSI infection risk was then validated against a separate sample of 59,352 surgical patients admitted in 1975−1976. By measuring risk with patient susceptibility and the level of wound contamination, the simplified index predicted surgical wound infection risk about twice as well as the traditional classification of wound contamination alone. Forty-five years later, this same tool is still routinely used to determine the risk for SSIs across a broad range of procedures (Allegranzi et al., 2018, Andiman et al., 2018, Culver et al., 1991, Mathias, 2015).
While the NHSN is one of the most commonly referenced in published system descriptions and studies globally, its utility remains uncertain. The NHSN was intended for use as a domestic HAI surveillance and reporting mechanism in the United States. There have been frequent calls to add procedure-specific variables to the existing risk assessment tool; however, these variables add complexity for the surveyors assigned to capture data (Haridas and Malangoni, 2008). In some cases, relatively complex laboratory procedures are mentioned apparently in an attempt to develop a patient-specific, vs. facility-specific risk score. The risk assessment system is intended only for healthcare systems, not for patient-level analysis.
The generalizability of this system across the LMIC healthcare spectrum is not known. Debates generally center upon the subjectivity of the classifications–particularly the ASA classification. When viewed in the context of cesarean sections, morbid obesity is a significant risk factor for SSIs and moves these patients to ASA 3 (Wang et al., 2018). ASA 3 is the cutoff for additional points in the risk assessment equation. This classification is not well characterized in LMIC healthcare settings as the 75% cutoff for cesarean section procedure duration is based on the US experience. Similarly, wound class related to cesarean sections has not been evaluated as a predictor of SSIs. These wounds can be classified as clean-contaminated if a prolonged rupture of membranes results in chorioamnionitis.
It is difficult to construct an alternative system, as some have urged, because the NHSN system is widely used and has been validated. Recently, a new risk assessment tool–The African Surgical Outcome Study (ASOS) Risk Calculator–was developed using patient data from 8799 patients across 168 African hospitals in 25 countries (Kluyts et al., 2018). The risk calculator included patient age, ASA status, indication for surgery, urgency, severity, and surgery type in the multivariable logistic regression model. When the tool was applied to preoperative assessment, it showed good discrimination and calibration to predict postoperative morbidity and mortality. The ASOS Risk Calculator was validated by a separate study that applied the tool to assess surgical outcomes in 1425 patients across 79 hospitals in Nigeria (Osinaike et al., 2019). While the new ASOS Risk Calculator is a promising advancement, roll-out to facilities in LMCIs would require a significant amount of retraining of surveyors and re-analysis of performance across broad patient samples in countries that use it. Further, for regional or national purposes, the NHSN risk assessment system creates a standardized metric not offered by the ASOS Risk Calculator. If new assessment tools are implemented, such as the ASOS Risk Calculator, it will be difficult to compare these tools against NHSN outcomes.
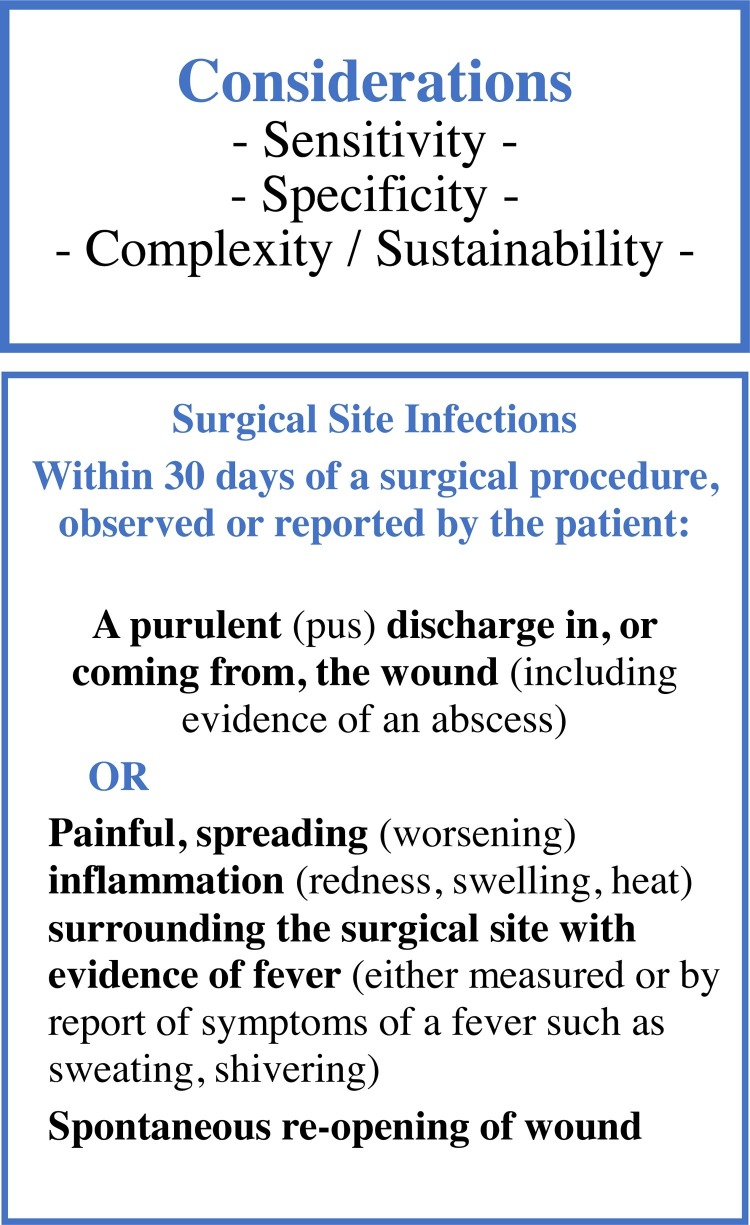
Finding the ‘best’ definition of surgical site infection
SSI definitions vary, ranging from simple subjective definitions (e.g., surgeon diagnosis) to complex multifactorial definitions, such as the ASEPSIS score (Bruce et al., 2001, Wilson et al., 1990; CDC surgical site definitions are shown in Table 2 ). The evolution of SSI definitions highlights the lack of an immediately obvious system. Nonetheless, a highly accurate and objective international system or one that can be translated globally in a straightforward manner is needed. Current subjective case definitions generally preclude comparability and limit the goal of tracking changes in HAI rates.
Table 2.
The evolution of CDC wound infection definitions.
| First Author citation | Definition |
|---|---|
| Berard and Gandon (1964) |
|
| Hart et al. (1968) | “As in the NRC Cooperative Study these data do not include stitch abscesses or erythema around sutures, these being considered as reactions about a foreign body in the skin. Included are all operations where pus, even in small amounts, had to be evacuated from the subcutaneous tissue.” |
| Pollock (1979) | Wound sepsis is the discharge of pus. It is subdivided into primary (when the first discharge is pus) and secondary (when the first discharge is not pus, but the discharging wound becomes colonized by bacteria from endogenous or exogenous sources). Both primary and secondary sepsis can be classified as minor (when constitutional disturbances are absent) and major (which makes the patient ill) |
| Polk et al. (1983) | Wound infection has been defined as the emergence of pus from a wound, irrespective of the results of subsequent cultures. Indeed, any incision that must be opened for local care probably should be considered infected. |
| Garner et al. (1988) | SURGICAL WOUND INFECTIONSurgical wound infection includes incisional surgical wound infection and deep surgical wound infection.Incisional surgical wound infection must meet the following criteria: Infection occurs at incision site within 30 days after surgery AND involves skin, subcutaneous tissue, or muscle located above the fascial layer AND any of the following:
|
| Consensus paper on the surveillance of surgical wound infections (1992); Garner et al. (1988); Horan et al. (1992); Mangram et al. (1999) | In the 1988 definitions, it was not clear that for deep surgical wound infections, specifying the anatomic location of the deep infection was necessary. For example, NNIS System hospitals would report osteomyelitis as the specific site of a deep surgical wound infection if it followed an orthopedic operative procedure. Hospitals unfamiliar with this two-level designation might not have gleaned this information from the 1988 definitions. In this revision, we have included a Table listing specific sites. Second, we have removed the term "wound," because in surgical terminology, "wound" connotes only the incision from the skin. For infections involving the incision, we (now) use the term "incisional SSI." The previous definitions of incisional surgical wound infection and deep soft tissue surgical wound infection' are replaced by superficial incisional SSI and deep incisional SSI. Infections that involve the organ/space component of the surgical site were previously called deep surgical wound infections at specific sites other than soft tissue. These are now termed organ/space SSI and use the same specific sites as soft tissues. We introduce the term "organ/space" to define any part of the anatomy (e.g., organs or spaces), other than the incision, opened or manipulated during the operative procedure. |
The assessment criteria we consider most important are the depth of the infection, the extent of a systemic reaction, and the qualitative values, including objectivity and simplicity. Concerning wound descriptions or syndromic approaches, the CDC system is less accurate than one would desire, particularly with superficial infections (definitions in Table 2). In many surveys, a large percentage, or even the majority of infections are classified as superficial. When this objective criteria system was evaluated in scientific studies, classification agreement was reached in approximately one-half of the wounds. The most common wound class and the one carrying no significant risk or cost to the patient or healthcare system ends up determining the outcomes of even well-performed randomized and controlled studies (Anderson et al., 2008).
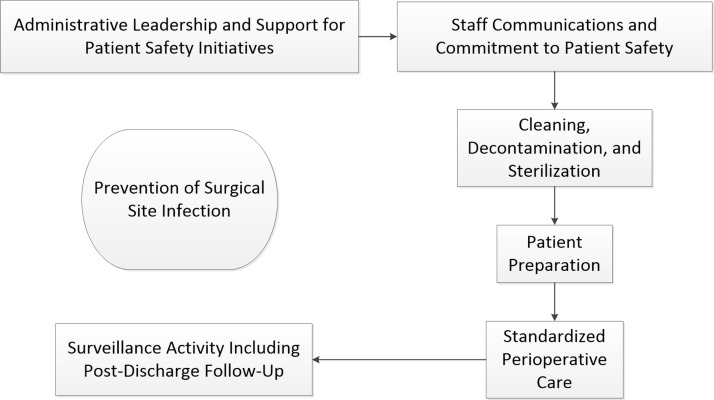
The infection depth is a primary variable for determining the necessity of hospitalization and the intervention needed to cure the infection. No intervention is needed in most superficial infections, and an operating room environment is not commonly required. For deep infections, exploration in the operating room and debridement of infected skin, subcutaneous tissue, fascia, and muscle is routine with a preference for general anesthesia, the need for lighting, and the need for clean instruments. Organ space infections are common following bowel surgery but may occur following any surgical procedure that opens a cavity Figure 2 .
Figure 2.
The Flow of an ‘Organized Surgical Infection Control Program.’ We specifically note that cleaning, decontamination, and sterilization is the only point in this cycle where the drapes and instruments placed into the field are decontaminated and then sterilized. This point, along with a detailed guideline, has been emphasized by the systems engineers.
A more suitable definition for use in limited-resource settings would forgo the CDC definition system and focus on the accompaniments of objectivity, specificity, and simplicity. This definition is reproduced in Figure 3 .
Figure 3.
Proposed definitions for SSIs in LMICs. Figured adapted from Westercamp, MJ: Association of Professionals in Infection Control, 2019 annual meeting, Philadelphia PA USA, June 4, 2019.
What implementation methods have been tried?
Safe Surgery Checklist
The need for a locally designed IPC program with SSI considerations is best illustrated with the Safe Surgery Checklist (World Health Organization, 2009a). This tool provides a standardized framework designed to improve patient safety while reducing morbidity and mortality associated with potential deviations from best practices (Russ et al., 2015). In studies of utilization, two themes were identified that reflected organizational barriers. The first theme, reported by 24% of participants, was related to the style in which the checklist was initially implemented within their healthcare setting. When there was no planned approach to implementation (e.g., a lack of education or training, a perceived lack of support from executives and physicians, and no customization to the local context), or an imposed approach, staff buy-in to adopt the usage of the tool was jeopardized due to a lack of initiative ownership and failure to communicate the local relevance of the tool. The second theme, reported by the same proportion of the sample (but not the same individual staff members), concerned the healthcare setting's culture. This information is directly relevant to any intervention designed to reduce SSIs, including WHO guidelines.
Comprehensive unit-based safety program
Additional work has focused on implementing a comprehensive, clinical unit-based safety program (CUSP). CUSPs are used in select US hospitals and African countries (Allegranzi et al., 2018, Ariyo et al., 2019). The utility of CUSPs has been questioned as studies were conducted in larger African hospitals, which may already implement measures to reduce HAIs and operate with significant staffing resources. Thus, its utility in district hospitals has not been tested and remains unproven. Despite the lack of evidence from smaller healthcare facilities, the available research has informed the WHO’s SSI prevention improvement tools (World Health Organization, 2016a).
The way forward: specific steps for successful SSI guideline implementation and building sustainable IPC programs in LMICs
Identify index operations for targeted surveillance
Cesarean section (CS) delivery is one of the most common operative procedures performed in sub-Saharan Africa (SSA), accounting for as much as 80% of the surgical workload (Bjerring et al., 2015). In contrast to CSs performed in high-income countries, CSs performed in SSA are primarily emergency operations and accompanied by high morbidity and mortality rates (Sway et al., 2019). This operation is the most important known variable associated with an increased probability of postpartum bacterial infection compared to vaginal birth. Reported infection rates following CSs are between 1% and 25% in LMICs - about five to 20 times higher than postpartum bacterial infection rates in vaginal delivery (Reperant and Osterhaus, 2017). In addition to the physical consequences of postpartum bacterial infection, such as maternal infirmity, sepsis, and neonatal mortality, these infections often share a common pathophysiological pathway with fetal and neonatal infections, thereby contributing to the significant societal costs stemming from maternal illness.
Identify champions and empower healthcare workers
The lack of IPC programs in LMICs coupled with insufficient personnel to conduct broad-based surveillance and follow-up activities results in significant task shifting among healthcare providers. Medical or clinical officers who are rarely trained in IPC are left to provide most of the operative care and may lack the bandwidth to perform SSI surveillance (Bergstrom et al., 2015). A broadly supported approach creating or expanding an IPC program is the identification and creation of “champions”—healthcare workers who are devoted to IPC and empower the continuous adoption of IPC activities. For SSIs, surgeons are the obvious choice as they serve as gatekeepers for programs impacting surgical patients. This team requires leadership authority and should engage perioperative care workers as champions to support clinical care practices that are well known and strongly supported by recommended GRADE-based guidelines (Allegranzi et al., 2016a, Allegranzi et al., 2016b; Berrios-Torres et al., 2017; Bratzler et al., 2013). We recognize that in many settings, surgical practice is conducted by non-specialist medical officers.
Within IPC teams, a ‘surveyor’ position should be designated. This position is best filled by surgical care nurses given their daily contact with postoperative patients and their review of wounds at each dressing change. This also represents an ideal opportunity to introduce/reinforce safe hand hygiene measures before handling wounds, dressing changes, and applying disinfectants. Therefore, substantial efforts should be made to engage facility staff at all levels and sectors because SSI prevention and control programs in LMICs are unlikely to succeed without the involvement of surgical providers.
Global interest in surgery has been renewed due to a 2015 declaration by the World Health Assembly. In response to this interest, LMICs are both creating and implementing national surgical, obstetrics, and anesthesia plans (NSOAPs). These NSOAPs scale up access to surgical care – particularly at district level hospitals – and expand capacity by training new surgeons. These activities will increase the volume of surgical cases and, in turn, complications such as SSIs. An associated expansion of IPC programs with SSI prevention and surveillance activities is needed to avoid an upsurge in the burden of this complication in LMICs.
Use of multimodal improvement strategies
The WHO has presented a multimodal improvement strategy to address guideline implementation for SSIs and other HAI challenges. This strategy builds upon previously tested approaches to implement hand hygiene interventions. While different terminologies have been used for this approach, it is clear that a concept of applying a range of resources, reminders, evaluations, training, and culture changes do lead to improvements in SSI rates in healthcare settings (Ariyo et al., 2019). For SSI reduction, the WHO outlined a step-by-step implementation method for evidence-based recommendations. The first step requires assessing currently enacted IPC practices and determining how these align with WHO recommendations. Next, healthcare providers must identify the barriers that have prevented the adoption of the remaining recommendations. In LMIC healthcare settings, these challenges may relate to resource access to disinfectants, clean water supplies, and sterilization equipment. Other challenges may include electrical supply interruptions, sterilization failures, and a lack of appropriate educational resources. Following the identification of barriers, providers must breakdown the steps required to overcome these obstacles, including financial opportunities to address structural barriers and iteration methods that incorporate feedback from individuals responsible for carrying out the newly established activities.
Ensuring that teams can work together to improve and scale-down practices deeply rooted in healthcare settings, is critical for successful IPC. Addressing cultures and behaviors can be supported by using existing safety assessment tools that, while challenging and, at times, uncomfortable, may be the only way to address a long-standing poor practice, e.g., change from using adhesive drapes or stopping prolonged duration of surgical antibiotic prophylaxis.
Hand hygiene programs as the basis for IPC programs–focusing on ownership
The evidence for the effectiveness of hand hygiene improvement programs is undisputed (World Health Organization, 2017, Pfäfflin et al., 2017). Within the structure of an IPC program, hand hygiene activities are reported through the IPC committee. By accepting this responsibility, the executive authority sends an important message to all workers in the healthcare setting and the IPC committee. This becomes even more important where IPC personnel have not yet been established or are struggling to gain attention.
The script used to engage managers is critical when considering the ownership model. Scripts should cover key points, such as supporting a plan and establishing targets for IPC compliance. The WHO's “Five Moments of Hand Hygiene” serves as a valid basis for hand hygiene interventions in all healthcare settings (World Health Organization, 2009b). The activities described in the “Five Moments of Hand Hygiene” can track progress towards hygiene targets, and program administrators can share results via internal and external publications. Additionally, the chief executive, chief medical officer/medical superintendent, and chief nurse should all be expected to make visible commitments to demonstrate their support for hand hygiene improvement. This commitment must be demonstrated on numerous occasions on surgical rounds and at town hall meetings to engage senior surgical teams. It is a visible and rewarding area of healthcare improvement, which should not be underestimated. In LMIC healthcare settings, these are easily adoptable activities that can significantly improve patient health outcomes.
Use of telecommunication devices for patient follow-up and surveillance
Patients often travel great distances to reach the hospitals that perform necessary surgical procedures. As many SSIs occur after a patient has been discharged, it is not uncommon for a patient to seek treatment from a local practitioner instead of traveling back to the original surgical care facility. Follow-up surveys that collect information about patient health outcomes utilizing telecommunication devices have been recommended and successfully used in various countries. These communications take advantage of text messaging services and smartphone apps, thus minimizing the need for a revisit to the healthcare facility. Additional benefits to these communication platforms include counseling patients on responsible antibiotic use and providing other healthcare information. When data from telecommunication surveys are assessed in conjunction with hospital readmission rates, wound debridement procedures, and antibiotic prescribing practices, healthcare institutions can improve their monitoring of SSI rates.
Special considerations
Surgical site infections in pediatric patients
In high-income countries, pediatric SSIs may constitute one-third of all surgical complications in children (Raval et al., 2011). In LMICs, the extent of pediatric SSIs is poorly characterized as limited data exists to accurately capture infection rates and healthcare outcomes in this patient population. One systematic analysis of interventional studies on SSI prevention in SSA concluded there was “extremely limited research from sub-Saharan Africa on interventions to curb the occurrence of SSI” (Aiken et al., 2012). The same is sadly true for other LMICs and, in particular, for pediatric populations. From what research has been conducted, the results are concerning. A report on SSIs in pediatric patients from Nigeria indicated the overall SSI rate was 23.6%, while the rate in clean wounds was reported at 14.3% (Ameh et al., 2009).
Even more worrisome is the near-total silence on SSI prevention guidelines in the pediatric population. The WHO’s 2016 global SSI prevention guidelines found insufficient data on children (World Health Organization, 2016a). Current guidelines on children are based on evidence generated from adult studies (Araujo da Silva et al., 2016). Araujo da Silva et al. point out that a lack of pediatric-specific data is a hindrance to the standardization of care across different settings. Children make up >40% of the population in most LMICs, and it is crucial to create prevention and surveillance guidelines that specifically address this age group. The role of surgical wound classification, application of the NHSN risk index, and antibiotic prophylaxis administration to reduce SSIs in pediatric patients, is poorly characterized (Gonzalez et al., 2016, Kagen et al., 2007, Oyetunji et al., 2016). Thus, high-quality studies are urgently needed to fill this gap.
Antibiotic resistance prevention
A challenge for preventing and treating SSIs is the growing rate of infections with antibiotic-resistant bacteria confirmed through microbiological testing in approved laboratories. There are sparse data on the incidence of antibiotic resistance (ABR) in most LMICs, in large part due to the absence of certified laboratories at anyplace other than national referral centers, as well as a similar absence of surveillance programs (Saied et al., 2015; Talaat et al., 2014). However, overuse and misuse of antibiotics in LMICs is a probable contributing factor to ABR development (Manenzhe et al., 2015). The small amount of data available from LMICs raises a real concern about the dynamic spread of multi-drug- and extensively-drug resistant bacteria, especially Gram-negatives, in settings where the availability of appropriate treatments is absent.
Reports from several countries in Africa, Southeast Asia, and India reveal rates of extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae of >50%, often associated with prior antibiotic use (Rickard, 2019). Recent reports from Africa indicate the presence of carbapenemase-producing genes (e.g., OXA-48, VIM, NDM-1, GES) in Gram-negative bacteria (Adam and Elhag, 2018, Pedersen et al., 2018). It is important to note these are healthcare-acquired bacterial infections, not patient-specific colonizing organisms. In environments where there is a rapid turnover of patients – often two patients in one bed – and no decontamination of beds and linens, expedited ABR infection acquisition is unlikely to diminish, even with strict antibiotic stewardship. Other factors in LMICs associated with a higher prevalence of ABR infections are a lack of laboratory facilities to guide prescribing practices, mobile bacterial resistance genes, substandard drug quality, and overcrowding in healthcare facilities.
-
To mitigate ABR in LMICs from the surgical field, efforts should focus on:1
Antimicrobial stewardship to ensure the appropriate use of antimicrobials in surgical patients;
-
2
Standardized and audited protocols of perioperative antibiotic prophylaxis (addressing who is given prophylaxis, proper timing, number of doses and when to be repeated during surgery), and alternatives in the case of allergies;
-
3
And targeted IPC strategies including implementation of hand hygiene (Adam and Elhag, 2018).
It is impossible for the above strategies to be defined, implemented, and evaluated without knowledge of local pathogens and their susceptibility profiles. Clinical microbiology laboratories embedded in local referral network schemes could be developed and strengthened to scale up microbiological testing. Advocates for this referral scheme are present throughout LMICs; this recommendation is not born from high-income settings. The Bacteriology in Low Resource Settings Working Group proposed solutions that prioritize harmonization, quality assurance, availability, and adaptation to the local setting of the equipment, consumables, techniques, rationalized bacterial identification, and antimicrobial testing resistance (Ombelet et al., 2018). Diagnostics should be integrated into clinical care and patient management, while clinically relevant specimens must be appropriately selected and prioritized. Training lab personnel by using open-access training materials should be developed; open-access software like WHONET can be used for interpreting and communicating results. In LMICs, political commitment and resource allocation are essential to organize and equip microbiology laboratories at all healthcare levels.
Conclusions
HAIs, and in particular SSIs, remain a high impact challenge in LMICs. While several IPC guidelines and tools are available through global organizations and national governments, the implementation and evaluation of these tools is far from ideal. We are particularly concerned with the lack of validated and accurate data on the extent of SSIs in LMICs. We recommend that short-term efforts focus on identifying and cultivating facility "champions," the creation and dissemination of simple, readily available educational resources, and implementation of strong SSI prevention measures supported by WHO evidence-based guidelines, for all patient populations (World Health Organization, 2016a). Long term measures must be holistic and include the training of IPC professionals, changes in the patient safety culture, aggregation of high-quality data, and standardization of SSI definitions.
Funding
None.
Ethical Approva
Not required.
Conflict of Interest
None.
References
- Adam M.A., Elhag W.I. Prevalence of metallo-beta-lactamase acquired genes among carbapenems susceptible and resistant Gram-negative clinical isolates using multiplex PCR, Khartoum hospitals, Khartoum Sudan. BMC Infect Dis. 2018;18(1):668. doi: 10.1186/s12879-018-3581-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken A.M., Karuri D.M., Wanyoro A.K., Macleod J. Interventional studies for preventing surgical site infections in sub-Saharan Africa–A systematic review. Int J Surgery. 2012;10(5):242–249. doi: 10.1016/j.ijsu.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allegranzi B., Bagheri Nejad S., Combescure C., Graafmans W., Attar H., Donaldson L. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377(9761):228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- Allegranzi B., Bischoff P., de Jonge S., Kubilay N., Zayed B., Gomes S. New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e276–e287. doi: 10.1016/S1473-3099(16)30398-X. [DOI] [PubMed] [Google Scholar]
- Allegranzi B., Zayed B., Bischoff P., Kubilay N., de Jonge S., de Vries F. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16(12):e288–e303. doi: 10.1016/S1473-3099(16)30402-9. [DOI] [PubMed] [Google Scholar]
- Allegranzi B., Kilpatrick C., Storr J., Kelley E., Park B.J., Donaldson L. Global infection prevention and control priorities 2018–22: a call for action. Lancet Glob Health. 2017;5(12):e1178–e1180. doi: 10.1016/S2214-109X(17)30427-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allegranzi B., Aiken A., Zeynep Kubilay N., Nthumba P., Barasa J., Okumu G. A multimodal infection control and patient safety intervention to reduce surgical site infections in Africa: a multicentre, before-after, cohort study. Lancet Infect Dis. 2018;18(5):507–515. doi: 10.1016/S1473-3099(18)30107-5. [DOI] [PubMed] [Google Scholar]
- Allegranzi B., Donaldson L.J., Kilpatrick C., Syed S., Twyman A., Kelley E. Infection prevention: laying an essential foundation for quality universal health coverage. Lancet Glob Health. 2019;7(6):e698–e700. doi: 10.1016/S2214-109X(19)30174-3. [DOI] [PubMed] [Google Scholar]
- Ameh E., Mshelbwala P., Nasir A., Lukong C., Jabo B., Anumah M. Surgical site infection in children: prospective analysis of the burden and risk factors in a Sub-Saharan African setting. Surg Infect. 2009;10(2):105–109. doi: 10.1089/sur.2007.082. [DOI] [PubMed] [Google Scholar]
- Anderson D.J., Chen L.F., Sexton D.J., Kaye K.S. Complex surgical site infections and the devilish details of risk adjustment: important implications for public reporting. Infect Control Hosp Epidemiol. 2008;29(10):941–946. doi: 10.1086/591457. [DOI] [PubMed] [Google Scholar]
- Andiman S.E., Xu X., Boyce J.M., Ludwig E.M., Rillstone H.R.W., Desai V.B. Decreased surgical site infection rate in hysterectomy: effect of a gynecology-specific bundle. Obstet Gynecol. 2018;131(6):991–999. doi: 10.1097/AOG.0000000000002594. [DOI] [PubMed] [Google Scholar]
- Araujo da Silva A.R., Zingg W., Dramowski A., Bielicki J.A., Sharland M. Most international guidelines on prevention of healthcare-associated infection lack comprehensive recommendations for neonates and children. J Hosp Infect. 2016;94(2):159–162. doi: 10.1016/j.jhin.2016.05.008. [DOI] [PubMed] [Google Scholar]
- Ariyo P., Zayed B., Riese V., Anton B., Latif A., Kilpatrick C. Implementation strategies to reduce surgical site infections: a systematic review. Infect Control Hosp Epidemiol. 2019;40(3):287–300. doi: 10.1017/ice.2018.355. [DOI] [PubMed] [Google Scholar]
- Bagheri Nejad S., Allegranzi B., Syed S.B., Ellis B., Pittet D. Health-care-associated infection in Africa: a systematic review. Bull World Health Organ. 2011;89(10):757–765. doi: 10.2471/BLT.11.088179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berard F., Gandon J. Postoperative wound infections: the influence of ultraviolet irradiation of the operating room and of various other factors. Annals Surg. 1964;160(Suppl 2):1–192. [PubMed] [Google Scholar]
- Bergstrom S., McPake B., Pereira C., Dovlo D. Workforce Innovations to Expand the Capacity for Surgical Services. In: Debas H.T., Donkor P., Gawande A., Jamison D.T., Kruk M.E., Mock C.N., editors. Essential Surgery: Disease Control Priorities. third ed. The International Bank for Reconstruction and Development/The World Bank; Washington (DC): 2015. [PubMed] [Google Scholar]
- Berrios-Torres S.I., Umscheid C.A., Bratzler D.W., Leas B., Stone E.C., Kelz R.R. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–791. doi: 10.1001/jamasurg.2017.0904. [DOI] [PubMed] [Google Scholar]
- Biccard B.M., Madiba T.E., Kluyts H.L., Munlemvo D.M., Madzimbamuto F.D., Basenero A. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet. 2018;391(10130):1589–1598. doi: 10.1016/S0140-6736(18)30001-1. [DOI] [PubMed] [Google Scholar]
- Bjerring A.W., Lier M.E., Rod S.M., Vestby P.F., Melf K., Endreseth B.H. Assessing cesarean section and inguinal hernia repair as proxy indicators of the total number of surgeries performed in Sierra Leone in 2012. Surgery. 2015;157(5):836–842. doi: 10.1016/j.surg.2014.12.014. [DOI] [PubMed] [Google Scholar]
- Bratzler D.W., Dellinger E.P., Olsen K.M., Perl T.M., Auwaerter P.G., Bolon M.K. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Syst Pharm. 2013;70(3):195–283. doi: 10.2146/ajhp120568. [DOI] [PubMed] [Google Scholar]
- Bruce J., Russell E.M., Mollison J., Krukowski Z.H. The quality of measurement of surgical wound infection as the basis for monitoring: a systematic review. J Hosp Infect. 2001;49(2):99–108. doi: 10.1053/jhin.2001.1045. [DOI] [PubMed] [Google Scholar]
- Consensus paper on the surveillance of surgical wound infections The Society for Hospital Epidemiology of America; The Association for Practitioners in Infection Control; The Centers for Disease Control and Surgical Infection Society. Infect Control Hosp Epidemiol. 1992;13(10):599–605. [PubMed] [Google Scholar]
- Culver D.H., Horan T.C., Gaynes R.P., Martone W.J., Jarvis W.R., Emori T.G. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med. 1991;91(3b):152s–157s. doi: 10.1016/0002-9343(91)90361-z. [DOI] [PubMed] [Google Scholar]
- Edwards J.R., Peterson K.D., Mu Y., Banerjee S., Allen-Bridson K., Morrell G. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783–805. doi: 10.1016/j.ajic.2009.10.001. [DOI] [PubMed] [Google Scholar]
- Garner J.S., Jarvis W.R., Emori T.G., Horan T.C., Hughes J.M. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128–140. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- Gaynes R.P., Culver D.H., Horan T.C., Edwards J.R., Richards C., Tolson J.S. Surgical site infection (SSI) rates in the United States, 1992-1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis. 2001;33(Suppl 2):S69–S77. doi: 10.1086/321860. [DOI] [PubMed] [Google Scholar]
- Global Burden of Disease Health Financing Collaborator Network Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet. 2019;393(10187):2233–2260. doi: 10.1016/S0140-6736(19)30841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez K.W., Dalton B.G., Kurtz B., Keirsey M.C., Oyetunji T.A., St Peter S.D. Operative wound classification: an inaccurate measure of pediatric surgical morbidity. J Ped Surg. 2016;51(11):1900–1903. doi: 10.1016/j.jpedsurg.2016.07.010. [DOI] [PubMed] [Google Scholar]
- Haley R.W., Culver D.H., Morgan W.M., White J.W., Emori T.G., Hooton T.M. Identifying patients at high risk of surgical wound infection. A simple multivariate index of patient susceptibility and wound contamination. Am J Epidemiol. 1985;121(2):206–215. doi: 10.1093/oxfordjournals.aje.a113991. [DOI] [PubMed] [Google Scholar]
- Haridas M., Malangoni M.A. Predictive factors for surgical site infection in general surgery. Surgery. 2008;144(4):496–501. doi: 10.1016/j.surg.2008.06.001. [DOI] [PubMed] [Google Scholar]
- Harrop J.S., Styliaras J.C., Ooi Y.C., Radcliff K.E., Vaccaro A.R., Wu C. Contributing factors to surgical site infections. J Am Acad Orthop Surg. 2012;20(2):94–101. doi: 10.5435/JAAOS-20-02-094. [DOI] [PubMed] [Google Scholar]
- Hart D., Postlethwait R.W., Brown I.W., Jr., Smith W.W., Johnson P.A. Postoperative wound infections: a further report on ultraviolet irradiation with comments on the recent (1964) national research council cooperative study report. Annals Surg. 1968;167(5):728–743. doi: 10.1097/00000658-196805000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan T.C., Gaynes R.P., Martone W.J., Jarvis W.R., Emori T.G. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–608. [PubMed] [Google Scholar]
- Horan T.C., Andrus M., Dudeck M.A. CDC/NHSN surveillance definition of healthcare-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Kagen J., Bilker W.B., Lautenbach E., Bell L.M., Coffin S.E., St John K.H. Risk adjustment for surgical site infection after median sternotomy in children. Infect Control Hosp Epidemiol. 2007;28(4):398–405. doi: 10.1086/513123. [DOI] [PubMed] [Google Scholar]
- Kes A., Ogwang S., Pande R., Douglas Z., Karuga R., Odhiambo F.O. The economic burden of maternal mortality on households: evidence from three sub-counties in rural western Kenya. Reprod Health. 2015;(12 Suppl 1):S3. doi: 10.1186/1742-4755-12-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluyts H., le Manach Y., Munlemvo D., Madzimbamuto F., Basenero A., Coulibaly Y. The ASOS Surgical Risk Calculator: development and Validation of a tool for identifying African surgical patients at risk of severe postoperative complications. Br J Anaesthesia. 2018;121(6):1357–1363. doi: 10.1016/j.bja.2018.08.005. [DOI] [PubMed] [Google Scholar]
- Manenzhe R.I., Zar H.J., Nicol M.P., Kaba M. The spread of carbapenemase-producing bacteria in Africa: a systematic review. J Antimicrob Chemother. 2015;70(1):23–40. doi: 10.1093/jac/dku356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangram A.J., Horan T.C., Pearson M.L., Silver L.C., Jarvis W.R. Guideline for prevention of surgical site infection, 1999. Centers for disease control and prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control. 1999;27(2):97–132. [PubMed] [Google Scholar]
- Mathias J.M. Specific care bundles successfully cut surgical site infection rates. OR Manager. 2015;31(12) 1, 10-2. [PubMed] [Google Scholar]
- McIntyre D., Thiede M., Dahlgren G., Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc Sci Med. 2006;62(4):858–865. doi: 10.1016/j.socscimed.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Mock C.N., Donkor P., Gawande A., Jamison D.T., Kruk M.E., Debas H.T. Essential surgery: key messages from Disease Control Priorities, 3rd edition. Lancet. 2015;385(9983):2209–2219. doi: 10.1016/S0140-6736(15)60091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molla M., Mitiku I., Worku A., Yamin A. Impacts of maternal mortality on living children and families: a qualitative study from Butajira, Ethiopia. Reprod Health. 2015;(12 Suppl 1):S6. doi: 10.1186/1742-4755-12-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ombelet S., Ronat J.B., Walsh T., Yansouni C.P., Cox J., Vlieghe E. Clinical bacteriology in low-resource settings: today’s solutions. Lancet Infect Dis. 2018;18(8):e248–e258. doi: 10.1016/S1473-3099(18)30093-8. [DOI] [PubMed] [Google Scholar]
- Osinaike B., Ayandipo O., Onyeka T., Alagbe-Briggs O., Mohammed A., Oyedepo O. Nigerian surgical outcomes–Report of a 7-day prospective cohort study and external validation of the African surgical outcomes study surgical risk calculator. Int J Surg. 2019;68:148–156. doi: 10.1016/j.ijsu.2019.06.003. [DOI] [PubMed] [Google Scholar]
- Oyetunji T.A., Gonzalez D.O., Gonzalez K.W., Nwomeh B.C., St Peter S.D. Wound classification in pediatric surgical procedures: measured and found wanting. J Ped Surg. 2016;51(6):1014–1016. doi: 10.1016/j.jpedsurg.2016.02.070. [DOI] [PubMed] [Google Scholar]
- Pedersen T., Sekyere J.O., Govinden U., Moodley K., Sivertsen A., Samuelsen O. Spread of Plasmid-Encoded NDM-1 and GES-5 Carbapenemases among Extensively Drug-Resistant and Pandrug-Resistant Clinical Enterobacteriaceae in Durban, South Africa. Antimicrob Agents Chemother. 2018;62(5) doi: 10.1128/AAC.02178-17. e02178-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfäfflin F., Tufa T.B., Getachew M., Nigussie T., Schönfeld A., Häussinger D. Implementation of the WHO multimodal Hand Hygiene Improvement Strategy in a University Hospital in Central Ethiopia. Antimicrob Resist Infect Control. 2017;6(1):1–10. doi: 10.1186/s13756-016-0165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polk H.C., Jr, Simpson C.J., Simmons B.P., Alexander J.W. Guidelines for Prevention of Surgical Wound Infection. JAMA Surgery. 1983;118(10):1213–1217. doi: 10.1001/archsurg.1983.01390100075019. [DOI] [PubMed] [Google Scholar]
- Pollock A.V. Surgical wound sepsis. Lancet. 1979;1(8129):1283–1286. doi: 10.1016/s0140-6736(79)92239-6. [DOI] [PubMed] [Google Scholar]
- Pruckner G.J., Schober T., Zocher K. The company you keep: health behavior among work peers. Eur J Health Econ. 2019;21(2):251–259. doi: 10.1007/s10198-019-01124-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raval M.V., Dillon P.W., Bruny J.L., Ko C.Y., Hall B.L., Moss R.L. American College of Surgeons National Surgical Quality Improvement Program Pediatric: a phase 1 report. J Am Coll Surg. 2011;212(1):1–11. doi: 10.1016/j.jamcollsurg.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Reperant L.A., Osterhaus A. AIDS, Avian flu, SARS, MERS, Ebola, Zika… what next? Vaccine. 2017;35(35 Pt A):4470–4474. doi: 10.1016/j.vaccine.2017.04.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickard J. Treating surgical infections in low- and middle-income countries: source control, then what? Surg Infect. 2019;20(3):192–196. doi: 10.1089/sur.2018.125. [DOI] [PubMed] [Google Scholar]
- Russ S.J., Sevdalis N., Moorthy K., Mayer E.K., Rout S., Caris J. A qualitative evaluation of the barriers and facilitators toward implementation of the WHO surgical safety checklist across hospitals in England: lessons from the "Surgical Checklist Implementation Project.". Ann Surg. 2015;261(1):81–91. doi: 10.1097/SLA.0000000000000793. [DOI] [PubMed] [Google Scholar]
- Saied T., Hafez S.F., Kandeel A., El-kholy A., Ismail G., Aboushady M. Antimicrobial stewardship to optimize the use of antimicrobials for surgical prophylaxis in Egypt: a multicenter pilot intervention study. Am J Infect Control. 2015;43(11):e67–71. doi: 10.1016/j.ajic.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Sastry S., Masroor N., Bearman G., Hajjeh R., Holmes A., Memish Z. The 17th International Congress on Infectious Diseases workshop on developing infection prevention and control resources for low- and middle-income countries. Int J Infect Dis. 2017;57:138–143. doi: 10.1016/j.ijid.2017.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobhy S., Arroyo-Manzano D., Murugesu N., Karthikeyan G., Kumar V., Kaur I. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis. Lancet. 2019;393(10184):1973–1982. doi: 10.1016/S0140-6736(18)32386-9. [DOI] [PubMed] [Google Scholar]
- Storr J., Twyman A., Zingg W., Damani N., Kilpatrick C., Reilly J. Core components for effective infection prevention and control programmes: new WHO evidence-based recommendations. Antimicrob Resist Infect Control. 2017;6:6. doi: 10.1186/s13756-016-0149-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sway A., Nthumba P., Solomkin J., Tarchini G., Gibbs R., Ren Y. Burden of surgical site infection following cesarean section in sub-Saharan Africa: a narrative review. Int J Womens Health. 2019;11:309–318. doi: 10.2147/IJWH.S182362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talaat M., Saied T., Kandeel A., El-Ata G.A., El-Kholy A., Hafez S. A point prevalence survey of antibiotic use in 18 hospitals in Egypt. Antibiotics. 2014;3(3):450–460. doi: 10.3390/antibiotics3030450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tartari E., Muthukumaran P., Peters A., Allegranzi B., Pittet D. Monitoring your institution: the WHO Hand Hygiene self-assessment Framework - is it worth it? Clin Microbiol Infect. 2019;25(8):925–928. doi: 10.1016/j.cmi.2019.04.009. [DOI] [PubMed] [Google Scholar]
- Wang X., Zhang X., Lai X. Exploring an optimal risk adjustment model for public reporting of cesarean section surgical site infections. J Infect Public Health. 2018;11(6):821–825. doi: 10.1016/j.jiph.2018.06.003. [DOI] [PubMed] [Google Scholar]
- Wilson A.P., Weavill C., Burridge J., Kelsey M.C. The use of the wound scoring method’ ASEPSIS’ in postoperative wound surveillance. J Hosp Infect. 1990;16(4):297–309. doi: 10.1016/0195-6701(90)90002-6. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2009. Implementation Manual WHO Surgical Safety Checklist.https://apps.who.int/iris/bitstream/handle/10665/44186/9789241598590_eng.pdf?sequence=1 Available from: [Google Scholar]
- World Health Organization . 2009. WHO Guidelines on Hand Hygiene in Health Care.https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf?sequence=1 Available from: [Google Scholar]
- World Health Organization . 2011. The Burden of Healthcare-Associated Infection Worldwide. Available from: https://www.who.int/infection-prevention/publications/burden_hcai/en/.[Accessed 8 October 2019] [Google Scholar]
- World Health Organization . 2016. Global Guidelines on the Prevention of Surgical Site Infection.https://apps.who.int/iris/bitstream/handle/10665/250680/9789241549882-eng.pdf?sequence=8 Available from: [PubMed] [Google Scholar]
- World Health Organization . 2016. Guidelines on Core Components of Infection Prevention and Control Programmes at the National and Acute Health Care Facility Level.https://apps.who.int/iris/bitstream/handle/10665/251730/9789241549929-eng.pdf;jsessionid=28FB2F1461B95BE1629F7B7F922479ED?sequence=1 Available from: [PubMed] [Google Scholar]
- World Health Organization . 2017. Evidence of Hand Hygiene as the Building Block for Infection Prevention and Control.https://www.who.int/infection-prevention/tools/core-components/evidence.pdf?ua=1 Available from: [Google Scholar]