Abstract
Background and Objective
Recent systematic reviews show promising effects for multidisciplinary biopsychosocial (BPS) interventions in patients with chronic low back pain (CLBP). Nowadays, BPS interventions have also been developed for primary care physiotherapy settings. Our aim was to systematically review the evidence on the effectiveness of primary care BPS interventions in improving functional disability, pain, and work status for patients with CLBP. Secondly, we aimed to provide an elaborated overview of BPS intervention designs, physiotherapist training programs, and process‐related factors (practical implementation).
Methods
We searched in scientific databases and reference lists. Randomized controlled trials (RCTs) evaluating primary care physiotherapist‐led BPS interventions in adults (≥18 years) with nonspecific CLBP (≥12 weeks) were included.
Results
Our search resulted in 943 references; 7 RCTs were included (1,426 participants). Results show moderate‐quality evidence (3 trials; 991 participants) that a BPS intervention is more effective than education/advice for reducing disability and pain in the short, medium, and long term. Low‐quality evidence (4 trials; 435 participants) was found for no difference with physical activity treatments.
Conclusions
BPS interventions seem more effective than education/advice and were found to be as effective as physical activity interventions in patients with CLBP. BPS interventions with a clear focus on psychosocial factors (understanding pain, unhelpful thoughts, coping styles, and goal setting) seem most promising. Sufficient delivery of BPS elements is expected when physiotherapists participate in training programs with extensive support prior and during delivery (manual, supervision, and informative resources).
Keywords: low back pain, chronic pain, biopsychosocial intervention, primary health care, physiotherapy, systematic review
Introduction
Chronic low back pain (CLBP) is defined as a health condition in which low back pain (LBP) persists for ≥12 weeks.1 CLBP can be very disabling at an individual's functional, psychological, and social level. Moreover, it has a large impact on society due to the related high healthcare consumption and work absenteeism.2 The recognition that many of these factors can influence a patient's LBP problem led to the development of the biopsychosocial (BPS) model.3 Subsequently, multiple interventions with a BPS approach have been developed to target influencing factors, aiming to improve the level of a patient's daily life functioning.4
Within BPS treatment, cognitive‐behavioral approaches are often used, such as graded activity,5 exposure in vivo,6 or acceptance and commitment therapy.7, 8 BPS interventions are frequently provided by multidisciplinary teams in rehabilitation centers or specialized pain clinics for patients with moderate to high levels of disability. Multidisciplinary BPS interventions are more effective in reducing pain and disability as compared to usual care (eg, provided by a general practitioner [GP]) or physical treatment (eg, passive or active therapy provided by a physiotherapist).4 Due to the promising effects of such BPS interventions, similar interventions have also been developed for primary care (physiotherapy) settings.
Physiotherapy treatments in general are easily accessible, less expensive, and often have shorter waiting lists in a primary care physiotherapy setting than in a multidisciplinary care setting. A BPS intervention is not regularly implemented by physiotherapists in primary care, however, and the evidence for BPS interventions for patients with CLBP is lacking. Few systematic reviews have investigated the evidence from existing BPS primary care interventions but focused instead only on BPS interventions in patients with LBP in general (ie, acute, subacute, and chronic)9 or (sub)acute LBP specifically.10, 11 No systematic review has been performed in patients with CLBP until now. Since patients with CLBP may respond differently from patients with acute or subacute LBP due to the persistence of pain and disability,12 it is essential to perform a systematic review to investigate the evidence of BPS interventions provided by physiotherapists working in primary care for patients with CLBP specifically.
Furthermore, many systematic reviews focus mainly on methodological factors that influence the quality of evidence. Less attention is paid to factors other than methodological ones that could influence the outcome of an intervention. Examples are the education of physiotherapists or the adherence of patients and physiotherapists to the treatment protocol. As these practical factors can influence outcomes, it is important to review not only methodological but also these factors.
The aim of the current systematic review is therefore (1) to provide an overview of the evidence of randomized controlled trials (RCTs) for the effectiveness of primary care BPS interventions compared with waiting list controls or other primary care treatments in improving functional disability, pain, and work status of patients with CLBP; and (2) to provide an overview of the design of each BPS intervention, of the profiles of physiotherapists, of the BPS training programs for therapists, as well as of other factors such as protocol adherence and therapy compliance.
Methods
The systematic review was performed following the Cochrane Collaboration guidelines13, 14 and reported using the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement.15 The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO; available from http://www.crd.york.ac.uk/PROSPERO/; registration number: CRD42015029878; 08.12.2015).
Eligibility Criteria
Types of Studies
English‐, Dutch‐, and German‐language full‐text and peer‐reviewed RCTs studying the effectiveness of BPS primary care treatment in patients with CLBP were included. No publication date or publication status restrictions were imposed.
Types of Participants
Studies with adult participants (≥18 years) experiencing nonspecific CLBP were included. Nonspecific CLBP was defined as pain between the 12th rib and gluteal region, with or without radiation towards 1 or both legs, present for at least 12 weeks.3 Studies evaluating patients with acute and subacute LBP were excluded unless these subjects comprised 10% or less of the total study population (≥90% should be CLBP), or results of patients with CLBP were presented separately.
Types of Interventions
We defined a BPS intervention as a multicomponent intervention including at least (1) a biological component (eg, to improve [knowledge of] physical components, pain physiology, pain sensitization, or differences between acute and chronic pain) and (2) a psychological or social component (eg, to improve [knowledge about the influence of] cognitions, attitude, [pain] behavior, coping styles, [self‐] management strategies, and/or coping styles of family, friends, and colleagues). The literature and a recently conducted systematic review were used to formulate the definition of a BPS intervention.3, 4 Interventions had to be provided individually or in a group and delivered by a physiotherapist working in primary care (ie, a local primary care practice or a primary care practice of a hospital physiotherapy department). Studies evaluating multidisciplinary interventions delivered by different healthcare professionals were excluded. Primary care treatments without a BPS approach (eg, usual care, physical treatment), no treatment, or waiting list were considered as control interventions.
Types of Outcome Measures
In accordance with recently conducted reviews on multidisciplinary rehabilitation treatments4, 16 (and as recommended by the Cochrane Back Review Group13), primary outcomes included patient‐centered measures such as functional disability, pain, and work status. Secondary outcomes included generic functional status or well‐being, overall improvement or satisfaction, emotional functioning and cognitions (depression, anxiety, catastrophizing, fear‐avoidance), and adverse events (AEs). Outcomes were categorized as short term (up to 3 months), medium term (>3 to 12 months), and long term (>12 months).
Search Methods for Identification of Studies
A search strategy was developed by review authors (R.V.E., I.H., J.K., R.S.). The search strategy included indexed keywords (eg, medical subject headings) and text terms for title and/or abstract of database records. An information specialist (S.D.) finalized the search strategy, adapted keywords according to the configuration of each database, and performed the computer‐aided search (Appendix S1, 30.11.15 to 01.12.2015). The following databases were used:
MEDLINE (Ovid)
MEDLINE In‐Process Citations & Daily Update (Ovid)
PubMed (NLM) (Internet) http://www.ncbi.nlm.nih.gov/pubmed
Embase (Ovid)
PsycINFO (Ovid)
Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO)
Cochrane Database of Systematic Reviews (CDSR; Cochrane Library: Wiley)
Cochrane Central Register of Controlled Trials (CENTRAL; Cochrane Library: Wiley)
Database of Abstracts of Reviews of Effects (DARE; Cochrane Library: Wiley)
Health Technology Assessment (HTA) database (Cochrane Library: Wiley)
PEDro (Internet) http://www.pedro.org.au/
Reference lists of review articles and included articles were checked on relevant studies. Identified references were downloaded and collected using EndNote bibliographic software (Clarivate Analytics, Philadelphia, PA, U.S.A.).
Study Selection
Two review authors (R.V.E. and M.J.) independently screened and selected search results by title and abstract based on previously formulated eligibility criteria. A third review author (I.H.) was consulted to resolve disagreement. Subsequently, selected searches were independently screened as full text by 2 review authors (R.V.E. and M.J.) and if necessary by a third review author (I.H.) to gain consensus.
Risk for Bias Assessment
Two review authors (R.V.E. and M.J.) independently performed the risk for bias assessment, and a third review author (I.H.) was involved in case of disagreement. The Cochrane Back Review Group “risk of bias” tool was used.13 Twelve items were scored as yes (= low risk), no (= high risk), or unclear. Review authors were not blinded for author names, institutions, or journals. If additional information was needed, corresponding authors were contacted.
Data Extraction and Data Synthesis
Data from the selected studies were extracted by one review author (R.V.E.) and checked by a second review author (I.H.). Extracted data included relevant reported information about the study population (age, gender, duration of symptoms, baseline score of outcomes), type of intervention (using an adapted version of the National Institutes of Health Behavior Change Consortium checklist, Appendix S2), type of comparison intervention, type of methodology and analysis, and outcomes (baseline and follow‐up). In case multiple publications existed regarding 1 RCT, all available publications were checked and relevant data extracted. After data extraction from the included studies, it became evident that the studies were too heterogeneous to justify meta‐analysis. Therefore, narrative analyses were conducted. The overall quality of the evidence was assessed using the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) approach. Evidence was defined as high‐quality evidence, moderate‐quality evidence, low‐quality evidence, or very low‐quality evidence.17
Results
The computer‐aided database search identified 1,633 records (Figure 1). One additional record was identified through reference checking. After removing duplicates, 943 records remained and were screened on title and abstract. This resulted in 42 records to be assessed as full text for eligibility. Eventually, 7 RCTs (12 articles) met predefined eligibility criteria and were included in the systematic review.18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29
Figure 1.
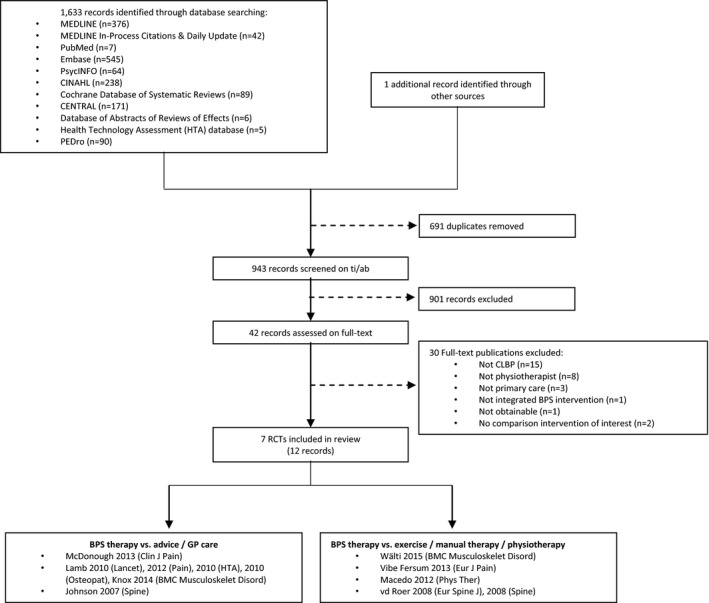
Study flow diagram. BPS, biopsychosocial; CLBP, chronic low back pain; RCT, randomized controlled trial; ti/ab, Title/Abstract.
Characteristics of Included Studies
The studies included in the systematic review were all RCTs, written in English. Studies were conducted in Switzerland,29 Norway,28 Australia,24 the Netherlands,26 and the United Kingdom.18, 21, 25
Participants
Participants were recruited via GPs, medical specialists working in hospitals, primary care physiotherapists, retrospective searches (patient records), and advertisements. Sample sizes of the included studies ranged from 28 (pilot RCT)29 to 701 patients,21 resulting in an overall included sample size of 1,426 patients (Table 1). Mean baseline levels of disability and pain intensity were on average mild to moderate (Roland Morris Disability Questionnaire [RMDQ] scores ranging from 9.0 to 12.1, Oswestry Disability Index [ODI] scores ranging from 21.3 to 31.9, pain intensity numeric rating scale [NRS] scores ranging from 4.6 to 6.2, and pain intensity VAS scores ranging from 45 to 59). Most studies reported an employment percentage between 47% and 72%, except for Vibe Fersum et al.28 (88% and 79% in the BPS and control groups, respectively). One study reported a relatively low fear‐avoidance beliefs score (Fear‐Avoidance Beliefs Questionnaire [FABQ] physical activity score < 14),28 while 3 studies reported increased fear‐avoidance beliefs (FABQ physical activity score > 14) or kinesiophobia (Tampa Scale for Kinesiophobia [TSK] score ≥ 3730).21, 25, 26 Wälti et al.29 did not report on subscales specifically but reported an FABQ total score for which no cut‐off values are available. Total scores included 23.93 ± 11.58 (BPS intervention) and 25.92 ± 12.28 (control group).
Table 1.
Characteristics of Included Randomized Controlled Trials (RCTs)
| Study | Study Design | Participants | BPS Intervention | Comparison | Outcome Measures | Time Points |
|---|---|---|---|---|---|---|
| McDonough et al. (2013)25 | Feasibility RCT |
Education/advice + pedometer‐driven walking program (EWP) N = 39 Age: 48 y (range 43–53) Gender: 46% female Duration of LBP: 10.3 y (range 6.5–14.0) Baseline ODI: 31.9% (range 26.6–37.2) Baseline FABQ (physical): 16.0 (range 13.9–18.0) Education/advice (E) N = 17 Age: 51 y (range 42–60) Gender: 76% female Duration of LBP: 11.1 y (range 7.7–14.5) Baseline ODI: 27.7% (range 23.3–32.2) Baseline FABQ (physical): 15.1 (range 11.8–18.4) |
Education/advice + pedometer‐driven walking program (EWP) 1× individual session (60 min): physical examination and standardized education The Back Book Pedometer‐driven walking program: 1× face‐to‐face (week 1) 1× face‐to‐face (week 2) Phone contacts (weeks 3–8) Structured around 5 components of the 5 A's (ask, advice, agree, assist, arrange) |
Education/advice (E) 1× individual session (60 min): physical examination and standardized education The Back Book |
Functional disability: ODI Pain: NRS Quality of life: EQ‐5D Overall improvement: Satisfaction: Baseline and Exit Questionnaires Psychological/cognitive function: FABQ, BBQ, PASES AE: Yes |
Baseline, 9 wk, 6 mo (post randomization) |
| Lamb et al. (2010)21 | RCT |
Education/advice (E) + CBT N = 468 Age: 53.0 ± 14.6 y Gender: 59% female Duration of LBP: 13.0 ± 13.2 y Baseline RMDQ: 9.0 ± 5.0 Baseline FABQ (physical): 14 ± 6.3 Education/advice (E) N = 233 Age: 54.0 ± 14.9 y Gender: 61% female Duration of LBP: 13.0 ± 12.7 y Baseline RMDQ: 9.0 ± 5.0 Baseline FABQ (physical): 14 ± 6.2 |
Education/advice (E) + CBT 1× active management advice (15 min) The Back Book 1× individual assessment (90 min) 1×/wk group therapy (90 min, for 6 wk) The Back Skills Training (BeST) program; aiming to target behaviors and beliefs about physical activity and avoidance of activity |
Education/advice (E) 1× active management advice (15 min) The Back Book Free to seek further care |
Functional disability: RMDQ, modified Von Korff scale Pain: Modified Von Korff scale Quality of life: SF‐12, EQ‐5D Overall improvement: Self‐rated benefit from treatment Satisfaction: Satisfaction with treatment Psychological/cognitive function: FABQ, PSES AE: Yes |
Baseline, 3 mo, 6 mo, 12 mo >12 mo (post randomization) |
| Johnson et al. (2007)18 | RCT |
Education/advice (E) + community‐based program N = 116 Age: 47.3 ± 10.9 y Gender: 61% female Duration of LBP: ≥3 mo Baseline RMDQ: 10.6 ± 3.9 Baseline FABQ (physical): Education/advice (E) N = 118 Age: 48.5 ± 11.4 y Gender: 58% female Duration of LBP: ≥3 mo Baseline RMDQ: 10.9 ± 4.0 Baseline FABQ (physical): |
Education/advice (E) + community‐based program Educational pack: booklet + audio cassette (by e‐mail) 8× 120 min group sessions (6 wk) Community‐based group program using CBT approach |
Education/advice (E) Educational pack: booklet + audio cassette (by email) Usual GP care: Mean number of sessions was not reported. |
Functional disability: RMDQ Pain: VAS Quality of life: EQ‐5D |
Baseline, 3 mo, 9 mo, 15 mo (post randomization) |
| Wälti et al. (2015)29 |
Pilot RCT |
Multimodal treatment (MMT) N = 14 Age: 41.57 ± 9.77 y Gender: 64.3% female Duration of LBP: ≥3 mo Baseline RMDQ: 10.21 ± 4.44 Baseline FABQ (total): 23.93 ± 11.58 Usual physiotherapy treatment (UPT) N = 14 Age: 41.71 ± 12.21 y Gender: 42.9% female Duration of LBP: ≥3 mo Baseline RMDQ: 11.21 ± 3.95 Baseline FABQ (total): 25.92 ± 12.28 |
Multimodal treatment (MMT) 1 or 2×/wk physiotherapy (30 min) + 5×/wk homework (30 min) (max. 12 wk) Intervention including 3 components: (1) education pain‐neurophysiology; (2) sensory retraining; (3) motor retraining |
Usual physiotherapy treatment (UPT) First session: basic education Other sessions: 2/3 active treatment, 1/3 passive applications |
Functional disability: RMDQ, PSFS Pain: NRS Work status: Sick leave Satisfaction: Treatment satisfaction Psychological/cognitive function: FABQ, PCS |
Baseline, 12 wk (post randomization) |
| Vibe Fersum et al. (2013)28 | RCT |
Classification‐Based Cognitive‐Functional Therapy (CB‐CFT) N = 62 Age: 41.0 ± 10.3 y Gender: 53% female Duration of LBP: 3–12 mo (12%), 1–5 y (28%), >5 y (61%) Baseline ODI: 21.3 ± 7.5 Baseline FABQ (physical): 11.1 ± 3.9 Manual Therapy and Exercise (MT‐EX) N = 59 Age: 42.9 ± 12.5 y Gender: 49% female Duration of LBP: 3–12 mo (14%), 1–5 y (31%), >5 y (55%) Baseline ODI: 24.0 ± 8.0 Baseline FABQ (physical): 11.8 ± 5.0 |
Classification‐Based Cognitive‐Functional Therapy (CB‐CFT) 1× initial session (60 min) 1×/wk individual sessions (30–45 min) After 2–3 wk: 1× individual session every 2–3 wk (12 wk) Structured around 4 components: (1) cognitive component; (2) specific movement exercises; (3) targeted functional integration of activities; (4) physical activity program tailored to the movement classification |
Manual Therapy and Exercise (MT‐EX) 1× initial sessions (60 min) Follow‐up sessions (30 min) Follow‐up sessions included joint mobilization/manipulation techniques + (home) exercise program |
Functional disability: ODI Pain: NRS Work status: Sick leave Satisfaction: Patient satisfaction Psychological/cognitive function: HSCL‐25, FABQ |
Baseline, 3 mo, 15 mo (post randomization) |
| Macedo et al. (2012)24 | RCT |
Graded activity (GA) N = 86 Age: 49.6 ± 16.3 y (range 18–80) Gender: 52% female Duration of LBP: 100.7 ± 109.2 mo Baseline RMDQ: 11.2 ± 5.3 Baseline FABQ (physical): Motor control exercises (MC) N = 86 Age: 48.7 ± 13.7 y (range 20–75) Gender: 66% female Duration of LBP: 74.0 ± 94.8 mo Baseline RMDQ: 11.4 ± 4.8 Baseline FABQ (physical): |
Graded activity (GA) 2×/wk individual sessions (60 min) + 30 min/wk homework (first 4 wk) 1×/wk individual sessions (60 min) + 60 min/wk homework (next 4 wk) 2 booster sessions (at 4 and 10 mo post randomization) Graded activity program; using time‐contingent and cognitive‐behavioral principles to help natural anxiety associated with pain and activities |
Motor control exercises (MC) 2×/wk individual sessions (60 min) + 30 min/wk homework (first 4 wk) 1×/wk individual sessions (60 min) + 60 min/wk homework (next 4 wk) 2 booster sessions (at 4 and 10 mo post randomization) Motor control exercise program; aiming to regain control and coordination of the spine and pelvis using principles of motor learning such as segmentation and simplification |
Functional disability: PSFS, RMDQ Pain: NRS Quality of life: SF‐36 Overall improvement: GPE, pain recovery Satisfaction: Credibility of treatment, therapists’ helpfulness, understanding, friendliness AE: Yes |
Baseline, 2 mo, 6 mo, 12 mo (post randomization) Pain was measured each month (for 12 mo) |
| Van der Roer et al. (2008)26 | RCT |
Protocol group (graded activity [GA]) N = 60 Age: 41.5 ± 8.8 y Gender: 55% female Duration current LBP episode: 53.9 ± 70.6 wk Baseline RMDQ: 11.6 Baseline TSK: 37.9 Guideline group N = 54 Age: 42.0 ± 9.9 y Gender: 48% female Duration current LBP episode: 47.2 ± 64.3 wk Baseline RMDQ: 12.1 Baseline TSK: 39.6 |
Protocol group (graded activity [GA]) 6× individual sessions (30 min, distributed over 3 wk) 2×/wk group sessions (90 min, for 8 wk) 1×/wk group sessions (90 min, for 4 wk) 2× individual sessions (30 min, during 12‐wk training period) 1× individual sessions (30 min, at 3 wk post‐training) 1× individual sessions (30 min, at 3 mo post‐training) Combination of exercise therapy, back school, and behavioral therapy (graded activity and operant conditioning) |
Guideline group Individual therapy (number of sessions was at discretion of physiotherapist). Mean number of sessions was 13. The Low Back Pain Guideline of the Royal Dutch College for Physiotherapy for low back pain |
Functional disability: RMDQ Pain: NRS Quality of life: QALY (EQ‐5D) Overall improvement: GPE Psychological/cognitive function: TSK, PCI, PSES AE: Yes |
Baseline, 6 wk, 13 wk, 26 wk, 52 wk (post randomization) |
AE, adverse event; BBQ, Back Beliefs Questionnaire; BPS, biopsychosocial; CBT, cognitive‐behavioral therapy; EQ‐5D, EuroQol 5D; FABQ, Fear‐Avoidance Beliefs Questionnaire; GP, general practitioner; GPE, Global Perceived Effect Scale; HSCL‐25, Hopkins Symptoms Checklist; LBP, low back pain; NRS, numeric rating scale; ODI, Oswestry Disability Index; PASES, Physical Activity Self‐Efficacy Scale; PCI, Pain Coping Inventory; PCS, Pain Catastrophizing Scale; PSES, Pain Self‐Efficacy Scale; PSFS, Patient‐Specific Functional Scale; QALY, Quality‐Adjusted Life Year; RMDQ, Roland‐Morris Disability Questionnaire; SF‐12, 12‐item short‐form health survey; SF‐36, 36‐item short‐form health survey; TSK, Tampa Scale for Kinesiophobia.
Interventions
Three studies compared a BPS intervention with education and advice.18, 21, 25 Four studies compared a BPS intervention with physical activity therapy. Physical activity therapy included usual or guideline physiotherapy,26, 29 motor control therapy,24 and manual therapy plus exercise28 (Table 2).
Table 2.
Characteristics of Biopsychosocial Interventions, Therapists, and Training Programs
| Study | McDonough et al. (2013)25 | Lamb et al. (2010)21 | Johnson et al. (2007)18 | Wälti et al. (2015)29 | Vibe Fersum et al. (2013)28 | Macedo et al. (2012)24 | van der Roer et al. (2008)26 |
|---|---|---|---|---|---|---|---|
| BPS intervention | Education/advice + pedometer‐driven walking program (EWP) | Education/advice + cognitive‐behavioral intervention (CBI) | Education/advice + community‐based program (CBP) | Multimodal treatment (MMT) | Classification‐Based Cognitive‐Functional Therapy (CB‐CFT) | Graded activity (GA) | Protocol group (GA) |
| Control | Education/advice (E) | Education/advice (E) | Education/advice (E) | Usual physiotherapy treatment (UPT) | Manual Therapy and Exercise (MT‐EX) | Motor control exercises (MC) | Guideline group |
| Design BPS intervention |
Session 1 (week 1): Step‐test Familiarize wearing pedometer Recording daily steps Session 2 (week 2): Setting step target for next week Phone contact (weeks 3–8): Discuss progress Document mean daily step count Setting new daily step target |
Session 1: Understanding Pain Benefits of exercise Session 2: Pain fluctuations Working out starting point for exercise/activity How to set goals Session 3: Unhelpful thoughts and feelings Session 4: Restarting activities or hobbies Session 5: When pain worries us Session 6: Coping with flare‐ups |
Session 1: Explanation of pain Develop exercise program Session 2: Activity management and pacing Exercise circuits Session 3: Goal setting Emotions and pain Session 4: Relaxation Meaning of diagnosis Session 5: Posture and manual handling Sleep hygiene Session 6: Posture and manual handling Sleep hygiene Session 7: Flare‐up management Healthcare usage Session 8: Review of course Planning for the future |
Sessions 2–4: Neurophysiological education of pain + book Explain Pain Other sessions: ‐ Sensory retraining: Two‐point discrimination ‐ Motor retraining: Photos of rotated or side bended human trunk + physically or mentally performing motor imagery exercises |
1. Cognitive component Pain education Goal setting 2. Functional movement exercises Diaphragm breathing Graded exposure model but relaxed/controlled 3. Functional integration Exercise program for functional goals 4. Physical activity levels Homework: 3 to 5×/wk physical exercise increased to 20–40 min duration. |
Goal setting Time contingent Quotas/pacing Reinforce wellness behavior and ignore illness behavior Education pain system and reassurance Education ergonomic factors and body awareness Generalized (whole body) exercises without consideration of specific muscle activity Strength training Cardiovascular/fitness training Muscle stretching Progression to functional activities Home exercises |
Starting phase (weeks 1–3): 6 individual sessions: patient history, physical examination, providing information on the treatment, determining baseline level of functional capacity, setting treatment goals, signing a treatment contract and evaluating treatment goals Treatment phase: 20 group sessions: patients trained according to operant‐conditioning behavioral principles based on the baseline level of functional capacity Generalization phase: 4 individual |
| Individual/group | Individual |
Individual + group (mean 8 ± 1.6, range 4–12) |
Group (4–10 patients) | Individual | Individual | Individual | Individual + group |
| Duration | 8 wk | 6 wk | 6 wk | 8 wk (max 12) | 12 wk |
8 wk 10 mo (including booster) |
12 wk 3 mo (including booster) |
| No. of therapists | 2 | 19 therapists | Team (number N/R) | 1 | 3 | 10 | 25 |
| Expertise | PT | PTs (n = 14), nurses (n = 1), psychologists (n = 2), and occupational therapists (n = 2) | PT | PT | PT | PT | PT |
| Years of experience in BPS interventions | N/R | Little/no experience | N/R | N/R | N/R | N/R | N/R (no criteria) |
| Training duration | 2.5 days (over 2 mo) | 2 days | 4 days | N/R | 106 h CB‐CFT (on average) + half a day | Series of evening interactive seminars | 2× 6 h |
| Training ingredients | 5 A's model, background brief Motivational Interviewing, main messages The Back Book, managing patient behavior, recording AEs, motivation, self‐efficacy for PA, using a pedometer, setting tailored goals and graded activity | Understanding LBP, risk factors associated with chronicity, CB model. Developing basic CB skills (eg, questioning techniques, group facilitation skills and topics of each session, including pain management techniques) | Principles of CBT for LBP, reflective practice | N/R | Workshops, patient examinations, pilot study, the concepts of best‐practice cognitive approach to managing back pain | N/R | Protocol training, behavioral principles |
| Additional support | Supervision on site | Supervision on site, via phone or e‐mail, website, DVD, manual (PT), workbook (patients) | Teaching notes per session | N/R | Clinical manual | Protocol, audits to encourage compliance | Protocol |
AE, adverse event; BPS, biopsychosocial; CB, cognitive‐behavioral; CBT, cognitive‐behavioral therapy; LBP, low back pain; N/R, not reported; PA, physical activity; PT, physiotherapist.
The BPS interventions in all selected studies contained cognitive‐behavioral principles. However, the applied approach varied. Two studies used operant conditioning and graded activity principles,24, 26 and another study used the 5 A's model of health behavior advice (ask/assess, advice, agree, assist, arrange).25 These 3 BPS interventions focused on specific exercise programs to improve activity levels, and cognitive‐behavioral approaches were used additionally to encourage active behavior. Another study used neurophysiological education about pain, disability, and perceptions in addition to sensory and motor retraining.29 The remaining studies used cognitive‐behavioral therapy (CBT)18, 21 or cognitive‐functional therapy.28 Although the latter 2 BPS interventions did include exercises, the main focus was on targeting beliefs and behavior (eg, to reduce fear avoidance and catastrophizing, and to improve coping style). By doing so, they aimed to improve the level of functional activities. Four studies reported providing a booklet with education about LBP and coping strategies such as The Back Book, 31 Explain Pain, 32 or a general booklet on self‐management strategies.18
All interventions were of low intensity (≤16 hours), except for the BPS intervention of van der Roer et al.,26 which consisted of 35 hours of contact time. The total duration of included BPS interventions ranged between 6 and 12 weeks. Two studies also provided booster sessions for the BPS interventions in the longer term (ie, at 3 months,26 and at 4 and at 10 months24). Four BPS interventions consisted of individual sessions,24, 25, 28, 29 2 interventions of individual and group sessions combined,21, 26 and 1 intervention of group sessions only.18
Physiotherapists
The number of physiotherapists providing the BPS interventions varied from 129 or 225 to 2526 (see Table 2). Physiotherapists mostly participated in a short training program with a duration ranging from 2 days21 to a maximum of 4 days.18 One exception was the study of Vibe Fersum et al.,28 in which physiotherapists had on average 106 hours of cognitive‐behavioral training. Training programs generally included protocol training and understanding of cognitive‐behavioral approaches. As additional support, most therapists received a manual. The studies of Lamb et al.21 and Vibe Fersum et al.28 were the only ones that provided (or at least reported on) support via other sources (see Table 2).
Outcomes
All studies measured functional disability (RMDQ or ODI) and pain (NRS, Modified Von Korff Scale [MVKS], or VAS). Only 4 studies measured sick leave.21, 26, 28, 29 Studies differed in the number and type of additional primary and secondary outcome measures (eg, generic functional status, overall improvement, satisfaction, psychological and cognitive function, AEs). All studies provided data at short term (≤3 months follow‐up), 5 studies at medium term (>3 to 12 months follow‐up), and 5 studies at long term (≥12 months follow‐up; all follow‐up outcomes were measured postrandomization). Data at medium term were not available for Vibe Fersum et al.28 and Wälti et al.29 (pilot RCT), and not at long‐term for Wälti et al.29 (pilot RCT) and McDonough at al.25 (feasibility RCT).
Risk for Bias Assessment
All studies reported an adequate method of randomization (criterion 1), and 6 studies described treatment allocation as concealed (criterion 2; Table 3). The corresponding author of Johnson et al.18 replied that allocation in the study was not concealed for patients and therapists.
Table 3.
Risk for Bias Assessment
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Random Sequence Generation | Allocation Concealment | Blinding of Participants | Blinding of Care Providers | Blinding of Outcome Assessor | Incomplete Outcome Data | Selective Reporting | Group Similarity at Baseline | Co‐interventions | Compliance | Intention‐to‐Treat Analysis | Timing of Outcome Assessment | |
| McDonough et al. (2013)25 | Y | Y | N | N | N | Y | Y | Y | U | Y | Y | Y |
| Lamb et al. (2010)21 | Y | Y | N | N | N | Y | Y | Y | U | Y | Y | Y |
| Johnson et al. (2007)18 | Y | N | N | N | N | Y | Y | Y | U | N | Y | Y |
| Walti et al. (2015) | Y | Y | U | N | N | Y | Y | N | N | N | N | Y |
| Vibe Fersum et al. (2013)28 | Y | Y | N | N | N | N | Y | N | N | Y | N | Y |
| Macedo et al. (2012)24 | Y | Y | N | N | N | Y | Y | Y | U | Y | Y | Y |
| van der Roer et al. (2008)26 | Y | Y | N | N | N | Y | Y | Y | Y | U | Y | Y |
Y, yes, criteria fulfilled; N, no, criteria not fulfilled, U, unclear.
Six studies were not able to blind patients (criterion 3), and 1 study did not report on patient blinding.29 All studies blinded neither therapists (criterion 4) nor outcome assessors (criterion 5), as therapists provided the treatments and therefore could not be blinded, and all studies used self‐reported outcomes.
Only Vibe Fersum et al.28 showed incomplete outcome data (>20%; criterion 6).13 In this study, 16 of 59 patients (27.1%) assigned to the control intervention and 11 of 62 patients (17.7%) assigned to the BPS intervention were excluded from the analysis (due to not starting or not completing the interventions; total excluded 22.3%). All studies had a low risk for selective outcome reporting (criterion 7). Furthermore, similar baseline characteristics (criterion 8) were reported in all except 2 studies.28, 29 In the study of Wälti et al.,29 the percentage of females was higher in the BPS group than in the control group (64.3% vs. 42.9%), and the pain catastrophizing score (on the Pain Catastrophizing Scale [PCS]) was higher in the control group than in the BPS group (mean ± standard deviation [SD] 14.43 ± 7.62 vs. 20.08 ± 8.24). In the study of Vibe Fersum et al.,28 anxiety and depression (Hopkins Symptoms Checklist [HSCL]) and fear‐avoidance of work (FABQ) scores were both higher in the control group than in the BPS group (mean ± SD, respectively, 1.57 ± 0.39 vs. 1.40 ± 0.33, and 19.3 ± 11.1 vs. 14.1 ± 9.6). Studies did not report controlling for these variables.
Co‐interventions were mostly neither reported nor clear (eg, most studies did report trying to avoid co‐interventions but did not report the number or type of co‐intervention, or whether they were similar between groups). Compliance with interventions (criterion 10) was acceptable in 4 studies,21, 24, 25, 28 unclear in 1 study,26 and not acceptable in 2 studies.18, 29 Wälti et al.29 reported good compliance in both interventions (>80%, n = 22) but did not take into account the 5 patients who discontinued the intervention after 4 or more weeks of training, and the 1 patient who was lost to follow‐up. Johnson et al.18 reported that noncompliance was modest (63% attended at least half of the sessions) but that this influenced treatment effects.
Intention‐to‐treat analysis (criterion 11) was performed in all except 2 studies.28, 29 Vibe Fersum et al.28 performed analysis on an “available case basis” and Wälti et al.29 analyzed 13 patients in the control group where 14 patients were originally included. All studies reported similar timing of outcome assessment between intervention and control groups (criterion 12).
All included studies were RCTs, although those of Wälti et al.29 and McDonough et al.25 were a pilot and feasibility RCT, respectively. Wälti et al.29 aimed to evaluate the (short‐term) effects and feasibility of a multimodal intervention in order to calculate appropriate sample size for a larger RCT. The sample size was not calculated but predefined and small (n = 28). In addition, the study of McDonough et al.25 was a feasibility RCT of a pedometer‐driven walking program (assessing recruitment, adherence, incidence of AEs, and effect sizes). For this study, no sample size (calculation) was reported and no significance tests were performed. The GRADE assessment of the quality of the evidence is presented in Tables 4 and 5.
Table 4.
GRADE Evidence Profile: Biopsychosocial Interventions Compared to Education and Advice for Patients With Chronic Low Back Pain
| Quality Assessment | ||||||
|---|---|---|---|---|---|---|
| No. of Studies | Risk for Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Quality of Evidence |
| Functional disability level (follow‐up: mean 12 mo; assessed with: RMDQ/ODI) | ||||||
| 3 RCTs | Seriousa | Not serious | Not serious | Not serious | None |
⨁⨁⨁◯ Moderate |
| Pain intensity (follow‐up: mean 12 mo; assessed with: VAS/NRS) | ||||||
| 3 RCTs | Seriousa | Not serious | Not serious | Not serious | None |
⨁⨁⨁◯ Moderate |
No blinding.
GRADE, Grades of Recommendation, Assessment, Development, and Evaluation; ODI, Oswestry Disability Index; NRS, numeric rating scale; RCT, randomized controlled trial; RMDQ, Roland‐Morris Disability Questionnaire; ⨁◯◯◯ = very low; ⨁⨁◯◯ = low; ⨁⨁⨁◯ = moderate; ⨁⨁⨁⨁ = high.
Table 5.
GRADE Evidence Profile: Biopsychosocial Interventions Compared to Physical activity Interventions for Patients With Chronic Low Back Pain
| Quality Assessment | ||||||
|---|---|---|---|---|---|---|
| No. of Studies | Risk for Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Quality of Evidence |
| Functional disability level (follow‐up: mean 12 mo; assessed with: RMDQ/ODI) | ||||||
| 4 RCTs | Seriousa | Seriousb | Not serious | Not serious | None |
⨁⨁◯◯ LOW |
| Pain intensity (follow‐up: mean 12 mo; assessed with: VAS/NRS) | ||||||
| 4 RCTs | Seriousa | Seriousb | Not serious | Not serious | None |
⨁⨁◯◯ LOW |
No blinding.
No consistent direction of effects.
GRADE, Grades of Recommendation, Assessment, Development, and Evaluation; ODI, Oswestry Disability Index; NRS, numeric rating scale; RCT, randomized controlled trial; RMDQ, Roland‐Morris Disability Questionnaire; ⨁◯◯◯ = very low; ⨁⨁◯◯ = low; ⨁⨁⨁◯ = moderate; ⨁⨁⨁⨁ = high.
BPS Intervention vs. Education/Advice
Primary Outcomes (Functional Disability, Pain, Work Status)
All studies reported that patients in both groups (BPS intervention and education/advice) improved the level of functional disability and pain over time. Between groups, the high‐quality RCT of Lamb et al.21 showed significant differences at short term for functional disability and pain in favor of the BPS intervention (mean RMDQ score 1.1 (95% confidence interval [CI] 0.38 to 1.17); mean MVKS score 4.2%, (95% CI 0.40 to 8.10), mean MVKS pain score 6.8% (95% CI 3.31 to 10.20), Appendix S3). McDonough et al.25 in their feasibility study also reported small but positive effects in favor of the BPS intervention but reported effect sizes only (functional disability, Cohen's d = −0.39; pain, Cohen's d = −0.10) at short term. Johnson et al.18 did not find significant differences between the 2 interventions at short term. At medium and long term, improvements in functional disability and pain were comparable to those at short term for each study.18, 21, 25 McDonough et al.25 additionally reported at 6 months (medium term) a higher percentage of patients achieving a minimal clinically important difference of >10% in functional disability in the BPS group than in the control group (56% vs. 44%). For pain, no difference in clinically important improvements was visible between groups. For outcomes related to work status, only Lamb et al.21 measured sick leave and reported no differences between groups at all time points.
Secondary Outcomes (Quality of Life, Health Status, Psychological Factors, AEs)
All 3 studies measured quality of life using the EuroQol‐5D (EQ‐5D) at all time points.18, 21, 25 At short term, mixed results were visible. Lamb et al.21 showed a significant mean between‐group difference of 0.07 (95% CI 0.02 to 0.12) in favor of the BPS intervention, while McDonough et al.25 and Johnson et al.18 reported no effects and no significant between‐group differences. At medium‐ and long‐term follow‐up, no studies found significant differences between the intervention groups.18, 21, 25 Lamb et al.21 also used the 12‐item short‐form health survey (SF‐12) for quality of life. They found significant mean between‐group differences for the physical functioning scale at short, medium, and long term (eg, long term −4.1 [95% CI −5.62 to −2.63]). The SF‐12 was not used by McDonough et al.25 or Johnson et al.18
Lamb et al.21 also showed significant larger mean improvements in fear‐avoidance beliefs (FABQ) in the BPS intervention compared with the control intervention at all time points (short term 2.7 [95% CI 1.68 to 3.67]; medium term 3.1 [95% CI 2.13 to 4.15]; long term 2.9 [95% CI 1.83 to 4.03]). McDonough et al.25 also measured the FABQ at short‐ and medium‐term follow‐up but found no effect (Cohen's d = −0.02 and Cohen's d = −0.06, respectively). Johnson et al.18 did not measure fear‐avoidance beliefs.
Only 1 AE (acute spinal cord compression with pulmonary embolus) was reported in the control group of Lamb et al.,21 which was not associated with the control intervention. McDonough et al.25 reported 20 AEs in the BPS group, of which 8 were related to the BPS intervention (increased pain in lower limb [n = 4] and back [n = 2], and allergic reaction to metal clip of the pedometer, which led to stopping the BPS intervention [n = 2]). Johnson et al.18 did not report on AEs.
BPS Intervention vs. Physical Activity Therapy
Primary Outcomes (Functional Disability, Pain, Work Status)
All studies reported that patients in both groups (BPS intervention and physical activity therapy) improved the level of functional disability and pain over time. Between groups, 1 study with low methodological quality showed short‐term statistically and clinically important differences for functional disability in favor of the BPS intervention (mean ODI score −9.7 [95% CI −12.7 to −6.7], Table 6).28 The differences remained significant at long‐term follow‐up (mean ODI score −8.2 [95% CI −12.6 to −3.8]). The other 3 studies did not find significant differences in functional disability between intervention groups and control groups at short‐,24, 26, 29 medium‐,24, 26 or long‐term follow‐up.24, 26
Table 6.
Study Results (95% Confidence Intervals and P Values) of Included Randomized Controlled Trials (RCTs)
| McDonough et al. (2013)25 | Lamb et al. (2010)21 | Johnson et al. (2007)18 | Wälti et al. (2015)29 | Vibe Fersum et al. (2013)28 | Macedo et al. (2012)24 | van der Roer et al. (2008)26 | |
|---|---|---|---|---|---|---|---|
| BPS Intervention vs. Education/Advice | BPS Intervention vs. Education/Advice | BPS Intervention vs. Education/Advice | BPS Intervention vs. Physical Activity Treatment | BPS Intervention vs. Physical Activity Treatment | BPS Intervention vs. Physical Activity treatment | BPS Intervention vs. Physical Activity treatment | |
| ODIb | RMDQ | RMDQ | RMDQ | ODI | RMDQ | RMDQ | |
| Short term | −0.39 | −1.1 (−1.71 to −0.38)a | −0.31 (−1.50 to 0.88) | −2.02 (−5.6 to 1.5)a | −9.7 (−12.7 to −6.7)a | −0.8 (−2.2 to 0.7) |
0.35 (−1.29 to 1.98) 0.85 (−1.36 to 3.06) |
| Medium term | −0.44 | −1.5 (−2.22 to −0.70)a | −1.09 (−2.28 to 0.09) | — | — | −0.8 (−2.3 to 0.6) | 0.13 (−2.24 to 2.50) |
| Long term | − | −1.3 (−2.06 to −0.56)a | −0.93 (−2.30 to 0.45) | — | −8.2 (−12.6 to −3.8)a | −0.6 (−2.0 to 0.9) | 0.06 (−2.22 to 2.34) |
| NRSb | VAS | VAS | NRS | NRS | NRS | NRS | |
|---|---|---|---|---|---|---|---|
| Short‐term | −0.10 | −6.8% (−10.20 to −3.31)a | −2.44 (−8.43 to 3.56) | −1.45 (−4.0 to 0.0) | −2.1 (−2.7 to −1.4)a | 0.0 (−0.7 to 0.8) |
−0.42 (−1.29 to 0.46) −0.76 (−1.74 to 0.23) |
| Medium‐term | −0.40 | −8.0% (−11.80 to −4.28)a | −4.60 (−11.07 to 1.88) | — | — | 0.0 (−0.8 to 0.8) | −0.97 (−1.88 to −0.06)a |
| Long‐term | – | −7.0% (−10.81 to −3.12)a | −5.49 (−12.43 to 1.44) | — | −1.3 (−2.1 to −0.5)a | 0.1 (−0.7 to 0.9) | −1.02 (−2.14 to 0.09) |
A negative score indicates improvements in favor of the BPS intervention.
P < 0.05.
P < 0.01.
P < 0.001.
The numbers represent effect sizes.
BPS, biopsychosocial; NRS, numeric rating scale; ODI, Oswestry Disability Index; RMDQ, Roland‐Morris Disability Questionnaire.
For pain relief, mixed results were reported. At short term, the pilot study of Wälti et al.29 (mean NRS score −1.45 [95% CI −4.0 to 0.0]) and Vibe Fersum et al.28 (mean NRS score −2.1 [95% CI −2.7 to −1.4]) did find significant between‐group differences in favor of the BPS intervention. The other 2 studies did not find significant between‐group differences.24, 26 At medium term, 2 studies provided data: Macedo et al.24 did not find significant or clinically important differences, while van der Roer et al.26 found significant between‐group differences in favor of the BPS interventions (mean NRS score −0.97 [95% CI −1.88 to −0.06]). At long‐term follow‐up, 3 studies provided data for pain relief for which mixed results were found.24, 26, 29 Only Vibe Fersum et al.28 showed significant and clinically important improvements in favor of the BPS intervention (mean NRS score −8.2 [95% CI −12.6 to −3.8]).
For outcomes related to work status, 1 study reported that sick leave did not occur during the study.29 Another study reported that patients in the BPS intervention had a 2.95‐times lower likelihood of taking sick.28 The other 2 studies either did not report24 or did not analyze sick leave.26
Secondary Outcomes (Quality of Life, Health Status, Psychological Factors, AEs)
Only Macedo et al.24 measured quality of life and showed no between‐group differences at short‐, medium‐, and long‐term follow‐up (36‐item short‐form health survey [SF‐36], physical and mental component). Van der Roer et al.26 performed an additional economic evaluation using the EQ‐5D at long‐term follow‐up and reported no significant between‐group differences (mean EQ‐5D score 0.03 [95% CI −0.06 to 0.12]).
Psychological factors were measured in 3 of the 4 studies.26, 28, 29 The FABQ was used in 2 studies, of which 1 reported no differences in effects between groups (only measured at short term)29 and the other reported significant between‐group differences in favor of the BPS intervention at short term (mean FABQ physical score −3.6 [95% CI −5.3 to −1.9]; mean FABQ work score −5.7 [95% CI −7.8 to −3.6]) and long term (mean FABQ physical score −4.7 [95% CI −6.5 to −3.0]; mean FABQ work score −5.6 [95% CI −8.7 to −2.5]).28 Van der Roer et al.26 used other psychological functioning questionnaires (TSK; Pain Coping Inventory [PCI]; Pain Self‐Efficacy Scale [PSES]) but could not identify significant differences between interventions, except for the mean PCI‐P (items passive coping) at short term, which was in favor of the BPS intervention (mean score −0.61 [95% CI −1.10 to −0.12]).
Only 1 out of 4 studies reported AEs.24 They mentioned pain exacerbation (n = 35) and development of musculoskeletal complaints (n = 2) as similar in both intervention and control groups. Van der Roer et al.26 did not specifically report AEs but said there were no serious AEs.
Outcomes Related to Treatment Delivery
Only 1 study reported most participating therapists having little or no experience in providing a BPS intervention.21 Three studies evaluated treatment delivery by physiotherapists.18, 21, 26 Lamb et al.21 and Johnson et al.18 used audiotapes, and Van der Roer et al.26 used registration forms completed by physiotherapists (regarding therapy goals, content and evaluation of different therapy sessions) and regular therapy visits. Overall, Lamb et al.21 reported that therapists had satisfactorily delivered most of the predefined therapy items and satisfactorily demonstrated therapist skills (eg, 100% of the therapists listened appropriately, 63% elicited beliefs or thoughts, and 77% referred to the cognitive‐behavioral model). Johnson et al.18 reported that physiotherapists also delivered most cognitive‐behavioral components, but discovered that physiotherapists found it difficult to apply cognitive‐behavioral communication styles and to identify, for example, patients’ anxieties and fears (73% did not achieve this element). Van der Roer et al.26 noticed that therapists did not significantly increase their behavioral orientation after training, measured with the Pain Attitudes and Beliefs Scale for Physiotherapists (PABS‐PT). This study reported that the protocol was adequately provided to 82% of the patients (ie, treatment goals set, information provided, exercise scheme prepared). However, the extent to which cognitive‐behavioral skills were applied was not specifically assessed. The quality of the delivered cognitive‐behavioral components therefore remains unknown.
Outcomes Related to the Receipt of Treatment
The percentage of patients who discontinued the BPS intervention when allocated and after treatment was started was low (≤5%) in 3 studies,21, 24, 25 moderate (≤21%) in 3 studies,26, 28, 29 and not reported in 1 study.18 Reasons for discontinuing the BPS interventions included allergic reaction to pedometer (7%),25 not able or willing to attend group sessions (< 1%),21 losing person to support home exercises (7%) or problems with online home training program (14%),29 time constraints (2%),28 and not improving (1% and 5%, respectively, Macedo et al.24 and van der Roer et al.26). At the end, compliance was assessed differently in each study. As McDonough et al.25 evaluated a pedometer‐driven walking program, they assessed adherence to the step target. In total, 73% of the patients adhered to the weekly step target during the 8‐week program. Lamb et al.21 and Johnson et al.18 both reported that 63% attended at least half of the group sessions. Wälti et al.29 assessed to what degree patients answered questions correctly and performed exercises. They reported that ≥81% reached the predefined adherence level. However, they did not take into account the data of 6 patients who dropped out.
Discussion
This systematic review is, as far as we know, the first in comparing BPS primary care interventions delivered by physiotherapists with other primary care interventions for patients with CLBP. In addition, it provides an overview of practical characteristics of the BPS interventions and is therefore useful for both researchers and clinicians. Our systematic review was based on 7 studies, including 1 feasibility RCT and 1 pilot RCT, leaving 5 full‐scale RCTs. Since the included studies suffered from methodological and/or practical limitations, new, higher quality studies would add valuable information to the findings of this systematic review.
In summary, this systematic review provides moderate‐quality evidence that a BPS intervention is more effective than education and advice in improving functional disability and pain at short, medium, and long term. For work status, no differences in effect were visible between the interventions. When a BPS intervention is compared to physical activity therapy, there is low‐quality evidence that no differences in improving functional disability, pain, and work status exist between interventions at short, medium, and long term. Based on these findings, it can be suggested that a BPS intervention is recommended over education and advice, but not specifically over physical activity therapy.
The beneficial effects of BPS interventions over education and advice could be explained by the fact that patients may need to experience that the learned information is applicable to their personal context. It is conceivable that they need to apply learned information into practice, while undergoing treatment, and need support from a physiotherapist on how to implement it in their daily lives. Regarding the BPS intervention protocols, nearly all BPS interventions included such practical components.
The comparable effects with a physical activity intervention could be explained by the fact that primary care physiotherapy has for many years promoted a BPS approach. This might have lessened the contrast between a BPS intervention and physical activity therapy. Indeed, BPS interventions with a clear focus on psychosocial factors, presumably having more contrast with the control condition, seemed more promising than interventions with less or no focus on psychosocial factors.28, 29 Psychosocial factors on which promising interventions focused included understanding pain, defining unhelpful thoughts or beliefs, avoidance behavior, coping styles, and goal setting.
The extent to which physiotherapists were educated in providing such BPS elements furthermore differed, which could have led to less contrast between interventions as well. While physiotherapists in the study of Vibe Fersum et al.28 were extensively trained, most studies offered short training programs ranging from 2 to 4 days only. Van der Roer et al.26 additionally reported that physiotherapists did not significantly increase their behavioral orientation after a 2‐day program. Also, physiotherapists in the study of Johnson et al.18 experienced difficulties when applying BPS principles in practice and discussing patients’ beliefs and fears after a 4‐day program. Only the study of Lamb et al.21 reported adequate delivery after a short training program. Physiotherapists had no or little experience prior to the start and participated in a 2‐day training program. These physiotherapists, however, also received a treatment protocol with a detailed description of each treatment session, supervision, and a DVD with examples of the first sessions, and they had access to a website with supporting materials. The extensive support in addition to the training program could have positively influenced the delivery of the therapy.
The findings of the current systematic review are in part comparable to those of other systematic reviews. Kamper et al.,4 for example, reviewed the evidence for a multidisciplinary BPS intervention and also found moderate‐quality evidence for more effectiveness in pain relief and disability compared to usual care (GP). In line with the current systematic review, Kamper et al.4 found in their systematic review small differences in effects between intervention groups. The magnitude of change (ie, between‐group differences) required to meet the definition of clinical meaningfulness is debatable. It is mainly determined by the pros and cons of the therapy, or factors such as costs, effects on secondary outcomes, and convenience.33, 34 In our systematic review, the BPS intervention was more favorable than education and advice when considering costs and psychological factors (eg, fear‐avoidance beliefs and self‐efficacy21). No serious AEs were reported, and 1 study25 additionally reported a slightly higher number of patients achieving a minimal clinically important difference in the BPS intervention group (ie, defined as a minimal improvement of 10% on the ODI over time). Based on these findings, one might consider effects clinically meaningful and therefore consider a BPS intervention more promising than just education and advice.
Compared with physical treatments, Kamper et al.4 found low‐quality evidence for greater effectiveness of behavioral treatments, and Henschke et al.16 moderate‐quality evidence. Hall et al.9 even reported high‐quality evidence for greater effectiveness of BPS interventions compared with exercise interventions. Our systematic review did not detect a difference between a BPS intervention and physical activity therapy. The differences in findings between the systematic reviews are likely due to different therapy settings and participant populations included in previously mentioned systematic reviews. These systematic reviews focused on interventions delivered in both primary and secondary (multidisciplinary) care settings, and not in primary care settings specifically. Hall et al.9 furthermore did not focus on patients with CLBP in specific but rather on patients with acute, subacute, and chronic pain. Patients with CLBP might have different beliefs and behavior, and might have received several treatments already. It is therefore possible that patients with a longer duration of LBP respond differently to treatments than patients with acute or subacute LBP.
The strengths of this systematic review are the fact that the search was conducted by an experienced information specialist and the use of guidelines for optimal reporting. Furthermore, this systematic review included studies with RCT designs only. In general, RCTs represent the highest level of evidence since the risk for bias is lowest compared to other designs (eg, observational designs). The main source of bias in the included studies was the inability to blind patients, therapists, and outcome assessors. However, since patients may recognize the therapy to which they are allocated and therapists will know the intervention they are delivering, bias with respect to blinding is unavoidable.
This systematic review aimed at primary care interventions. It should be mentioned, however, that the included studies used a mixed nature of patient selection strategies, such as GPs, advertisements, and/or secondary care specialists. Therefore, part of the study population was composed of patients initially referred to secondary care. In addition, a requirement of the systematic review was to only include studies evaluating a BPS intervention of interest in patients with nonspecific CLBP. Although no strict inclusion and exclusion criteria for nonspecific CLBP were formulated for this systematic review, we believe that, on the basis of exclusion criteria used by all included studies (see Appendix S3), the significant proportion of patients of the studies included in this review do fulfil the definition of nonspecific CLBP. We furthermore defined a BPS intervention as a multicomponent intervention, focusing on biological (eg, pain physiology, physical components), psychological (eg, beliefs, behavior, coping style), or social aspects (eg, family, work, etc.). This definition was based on descriptions in the current literature, self‐defined criteria, and a previously conducted systematic review.3, 4 As can be seen from this definition, the psychological and social components are interchangeable. This is because the social component is frequently not addressed in depth during a BPS intervention or studies do not provide in‐depth information about to what extent it was explicitly addressed during treatment. It is then hard to define whether the BPS intervention actually comprises all 3 components. The included studies in our review included at least a psychosocial and to some extent a social component, and therefore met our inclusion criteria. For future BPS interventions, however, it may still be recommended to explicitly address the social component35 and furthermore to publish a protocol of the BPS intervention to inform readers. In addition, it might be recommended to perform a process evaluation for a better interpretation of the study results. This will be helpful for replication or development of a BPS intervention and its implementation.
Limitations of the included studies were the heterogeneity in study and treatment designs and the use, or not, of measurement instruments, especially psychosocial ones. Two studies did not measure psychosocial factors at all.18, 24 Since BPS interventions initially aim to target psychosocial factors, psychosocial measurements are of high value and should be used in future trials.
Future clinical trials should develop and evaluate BPS primary care interventions that are specifically focused on functional goals (valuable for the patient) and psychosocial needs. It is important to select therapists based on their BPS skills or to adequately educate and support them in providing BPS elements. The essential role of sufficient training and resources (eg, treatment protocols and support) in complex behavioral interventions can be confirmed by the current literature.9, 36 Both studies suggest that if physiotherapists receive appropriate training and resources, and possess sufficient competencies, physiotherapists will be able to effectively provide a cognitive‐behavioral intervention. Trained physiotherapists might furthermore be able to identify patients with LBP at risk for developing chronic complaints and treat them at an early stage without the need of referral. This might be more convenient for patients than being treated in expensive, secondary care settings, which frequently have a medicalizing focus instead of a de‐medicalizing focus, and for which referral to a specialist is necessary.
When reporting outcomes of trials, it is necessary to provide a detailed description of the treatment design (BPS elements), its practical implementation (process information), and information on the selection, training, and supervision of physiotherapists. Such information is necessary for adequate interpretation of findings and for appropriate replication of BPS interventions in clinical practice.
Conclusions
This systematic review shows beneficial effects for primary care BPS interventions over education and advice in patients with CLBP. Furthermore, primary care BPS interventions and physical activity interventions provide equally promising effects. However, some included studies suffered from methodological and practical limitations. In combination with the rather low number of studies evaluating primary care BPS interventions, it is recommended that additional studies of high methodological as well as practical quality be performed. This is of particular importance for comparison with physical activity treatments. High‐quality studies are expected to add valuable information to the findings of this systematic review and will be important for future directions of primary care interventions for patients with CLBP.
Funding
Adelante, Centre of Expertise in Rehabilitation and Audiology Hoensbroek, The Netherlands; the Province of Limburg (SAS‐2012‐01300) and CZ Foundation (AFVV12‐205).
Ethical Approval
Not needed.
Author Contributions
R.V.E., I.H., J.K., and R.S. contributed to the conception and design of the study. R.V.E. developed the protocol and search strategy, and I.H., J.K., and R.S. contributed with critical revision. Study selection and risk for bias assessment was performed by R.V.E., I.H., and M.J. Data extraction and analysis were done by R.V.E. and checked by I.H. R.V.E. developed the manuscript with critical revision by I.H., M.J., J.K., and R.S. All authors discussed the results and commented on the manuscript. All authors gave final approval of the version to be published.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Supporting information
Appendix S1. Search strategies.
Appendix S2. Adapted version of the National Institutes of Health Behavior Change Consortium (NIHBCC) checklist.
Appendix S3. Inclusion and exclusion criteria of the included randomized controlled trials.
Acknowledgements
We acknowledge information specialist Steven Duffy for his contribution to performing the search strategy. Furthermore, we acknowledge Les Hearn for proofreading and editing the manuscript.
Systematic review registration number: PROSPERO registration number: CRD42015029878.
References
- 1. Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. 2nd ed. Seattle, Washington: International Association for the Study of Pain; 1994; 209–214. [Google Scholar]
- 2. Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17(suppl 2):3–10. [DOI] [PubMed] [Google Scholar]
- 3. Waddell G. The Back Pain Revolution. Oxford, U.K.: Churchill Livingstone; 2004. [Google Scholar]
- 4. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2014;9:CD000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lindstrom I, Ohlund C, Eek C, et al. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant‐conditioning behavioral approach. Phys Ther. 1992;72:279–290; discussion 291–293. [DOI] [PubMed] [Google Scholar]
- 6. Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. Graded exposure in vivo in the treatment of pain‐related fear: a replicated single‐case experimental design in four patients with chronic low back pain. Behav Res Ther. 2001;39:151–166. [DOI] [PubMed] [Google Scholar]
- 7. Trompetter HR, Bohlmeijer ET, Veehof MM, Schreurs KM. Internet‐based guided self‐help intervention for chronic pain based on acceptance and commitment therapy: a randomized controlled trial. J Behav Med. 2015;38:66–80. [DOI] [PubMed] [Google Scholar]
- 8. Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies—republished article. Behav Ther. 2016;47:869–885. [DOI] [PubMed] [Google Scholar]
- 9. Hall A, Richmond H, Copsey B, et al. Physiotherapist‐delivered cognitive‐behavioural interventions are effective for low back pain, but can they be replicated in clinical practice? A systematic review Disabil Rehabil. 2016;40:1–9. [DOI] [PubMed] [Google Scholar]
- 10. Brunner E, De Herdt A, Minguet P, Baldew SS, Probst M. Can cognitive behavioural therapy based strategies be integrated into physiotherapy for the prevention of chronic low back pain? A systematic review. Disabil Rehabil. 2013;35:1–10. [DOI] [PubMed] [Google Scholar]
- 11. Ramond‐Roquin A, Bouton C, Gobin‐Tempereau AS, et al. Interventions focusing on psychosocial risk factors for patients with non‐chronic low back pain in primary care–a systematic review. Fam Pract. 2014;31:379–388. [DOI] [PubMed] [Google Scholar]
- 12. George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear‐avoidance‐based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28:2551–2560. [DOI] [PubMed] [Google Scholar]
- 13. Furlan AD, Malmivaara A, Chou R, et al. 2015 updated method guideline for systematic reviews in the cochrane back and neck group. Spine. 2015;40:1660–1673. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons Ltd; 2011. [Google Scholar]
- 15. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Henschke N, Ostelo RW, van Tulder MW, et al. Behavioural treatment for chronic low‐back pain. Cochrane Database Syst Rev. 2010;7:CD002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johnson RE, Jones GT, Wiles NJ, et al. Active exercise, education, and cognitive behavioral therapy for persistent disabling low back pain: a randomized controlled trial. Spine. 2007;32:1578–1585. [DOI] [PubMed] [Google Scholar]
- 19. Knox CR, Lall R, Hansen Z, Lamb SE. Treatment compliance and effectiveness of a cognitive behavioural intervention for low back pain: a complier average causal effect approach to the BeST data set. BMC Musculoskelet Disord. 2014;15:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lamb SE, Hansen Z, Lall R, et al. Group cognitive behavioral intervention in primary care in low back pain: a randomized, controlled study and analysis of cost‐effectiveness [German]. Osteopathische Medizin. 2010;11:24–26. [Google Scholar]
- 21. Lamb SE, Hansen Z, Lall R, et al. Group cognitive behavioural treatment for low‐back pain in primary care: a randomised controlled trial and cost‐effectiveness analysis. Lancet. 2010;375:916–923. [DOI] [PubMed] [Google Scholar]
- 22. Lamb SE, Lall R, Hansen Z, et al. A multicentred randomised controlled trial of a primary care‐based cognitive behavioural programme for low back pain. The Back Skills Training (BeST) trial. Health Technol Assess. 2010;14:1–253, iii‐iv. [DOI] [PubMed] [Google Scholar]
- 23. Lamb SE, Mistry D, Lall R, et al. Group cognitive behavioural interventions for low back pain in primary care: extended follow‐up of the Back Skills Training Trial (ISRCTN54717854). Pain. 2012;153:494–501. [DOI] [PubMed] [Google Scholar]
- 24. Macedo LG, Latimer J, Maher CG, et al. Effect of motor control exercises versus graded activity in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. 2012;92:363–377. [DOI] [PubMed] [Google Scholar]
- 25. McDonough SM, Tully MA, Boyd A, et al. Pedometer‐driven walking for chronic low back pain: a feasibility randomized controlled trial. Clin J Pain. 2013;29:972–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. van der Roer N, van Tulder M, Barendse J, Knol D, van Mechelen W, de Vet H. Intensive group training protocol versus guideline physiotherapy for patients with chronic low back pain: a randomised controlled trial. Eur Spine J. 2008;17:1193–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van der Roer N, van Tulder M, van Mechelen W, de Vet H. Economic evaluation of an intensive group training protocol compared with usual care physiotherapy in patients with chronic low back pain. Spine. 2008;33:445–451. [DOI] [PubMed] [Google Scholar]
- 28. Vibe Fersum K, O'Sullivan P, Skouen JS, Smith A, Kvale A. Efficacy of classification‐based cognitive functional therapy in patients with non‐specific chronic low back pain: a randomized controlled trial. Eur J Pain. 2013;17:916–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Walti P, Kool J, Luomajoki H. Short‐term effect on pain and function of neurophysiological education and sensorimotor retraining compared to usual physiotherapy in patients with chronic or recurrent non‐specific low back pain, a pilot randomized controlled trial. BMC Musculoskelet Disord. 2015;16:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vlaeyen JW, Kole‐Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. [DOI] [PubMed] [Google Scholar]
- 31. Roland M, Waddell G, Klaber Moffett J, et al. The Back Book: The Best Way to Deal With Back Pain—Get Back Active. Norwich, UK: The Stationary Office; 2004. [Google Scholar]
- 32. Moseley LG, Butler DS. Schmerzen Verstehen. 2nd ed. Heidelberg, Germany: Springer Verlag; 2012. [Google Scholar]
- 33. Dworkin RH, Turk DC, McDermott MP, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–244. [DOI] [PubMed] [Google Scholar]
- 34. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–121. [DOI] [PubMed] [Google Scholar]
- 35. Blyth FM, Macfarlane GJ, Nicholas MK. The contribution of psychosocial factors to the development of chronic pain: the key to better outcomes for patients? Pain. 2007;129:8–11. [DOI] [PubMed] [Google Scholar]
- 36. van der Windt D, Hay E, Jellema P, Main C. Psychosocial interventions for low back pain in primary care: lessons learned from recent trials. Spine. 2008;33:81–89. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Search strategies.
Appendix S2. Adapted version of the National Institutes of Health Behavior Change Consortium (NIHBCC) checklist.
Appendix S3. Inclusion and exclusion criteria of the included randomized controlled trials.


