Abstract
Background
Identification of patients at risk for malnutrition is important for timely nutrition intervention to reduce morbidity and mortality. Objective: The objective of this study was to compare the sensitivity and specificity of the Nutrition Risk Screen (NRS) 2002 and the ThedaCare NRS to identify patients at risk for malnutrition.
Methods
The NRS 2002 and ThedaCare NRS were administered to 594 patients, aged 63 ± 16 years (mean ± SD), in the non–intensive care unit hospital setting. Risk for malnutrition and malnutrition diagnosis were confirmed with the 6 malnutrition clinical characteristics defined by the Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition and using the nutrition assessment that included the Nutrition Focused Physical Exam. Sensitivity, specificity, and κ coefficient were calculated.
Results
When compared with the NRS 2002, the ThedaCare NRS had higher sensitivity (98.8% vs 63.5%), indicating improved identification of patients at risk for malnutrition, but lower specificity (74.0% vs 93.4%), indicating that more patients at low risk for malnutrition were misclassified. ThedaCare NRS missed fewer patients at risk for malnutrition when compared with the NRS 2002. ThedaCare NRS had a higher κ coefficient when compared with the NRS 2002, indicating better agreement of results regardless of who administered the screen. The ThedaCare NRS required less time to complete when compared with the NRS 2002 (mean ± SE: ThedaCare, 17 ± 1 seconds; NRS 2002, 9 ± 1 minutes; P < .0001).
Conclusion
The ThedaCare NRS improves the identification of patients at risk for malnutrition in the non–intensive care unit hospital setting. This trial was registered at www.clinicaltrials.gov as NCT02585245.
Keywords: length of hospital stay, malnutrition, Nutrition Focused Physical Assessment, Nutrition Focused Physical Exam, sensitivity, specificity
Clinical Relevancy Statement
Malnutrition in the hospital setting can raise healthcare costs, increase 30‐day readmissions, and reduce quality of life. We developed the ThedaCare Nutrition Risk Screen, which improved the accuracy of identification of patients, especially elderly patients, at moderate and high risk for malnutrition in less time when compared with the Nutrition Risk Screen 2002, a validated screening tool. This new screening tool provides a time‐effective and cost‐effective approach to improve the identification of malnutrition and allows for earlier nutrition assessment and intervention in the non–intensive care unit hospital setting.
Introduction
Malnutrition in hospitalized patients is a common problem that increases length of stay, healthcare costs, and mortality.1, 2 The reported prevalence of malnutrition ranges from 15%–80% of hospitalized patients, yet only 3% of patients with malnutrition are diagnosed.3, 4, 5, 6, 7, 8 For patients with malnutrition, costs are >45% higher and length of stay is >17% longer.2, 9, 10, 11 Early nutrition intervention of patients with malnutrition can reduce length of stay and healthcare costs2, 12; however, nutrition intervention is often delayed due to the accuracy of various nutrition risk screens used to identify patients at nutrition risk.7 Thus, the improvement of nutrition risk screening tools is necessary to enhance identification of patients at risk for malnutrition to allow for prompt nutrition assessment, diagnosis, and intervention.11, 13
The Joint Commission on Accreditation of Healthcare Organizations requires that patients are screened for risk of malnutrition within 24 hours of hospital admission. The American Society for Parenteral and Enteral Nutrition (ASPEN) has defined nutrition risk screening as the process by which individuals at risk for malnutrition are identified to determine if a nutrition assessment is needed.3, 11 Ideally, a nutrition risk screen is a tool that can quickly identify patients at risk for malnutrition with high sensitivity and specificity and can easily be administered by any healthcare professional, including a nutrition and dietetics technician, registered (NDTR).14, 15, 16
Several nutrition risk screens with a range of complexity have been validated, such as the Nutrition Risk Screen 2002 (NRS 2002), Malnutrition Universal Screening Tool, and the Nutrition Risk Index. The NRS 2002, developed by Kondrup et al and the European Society for Parenteral and Enteral Nutrition, was validated based on a meta‐analysis of 128 trials.17, 18 However, subsequent studies have reported that the ability or sensitivity of the NRS 2002 to identify patients at risk for malnutrition is highly variable among disease populations and age groups. In particular, the NRS 2002 demonstrates reduced sensitivity in the elderly and a high false negative rate where patients at risk for malnutrition are missed.4, 19, 20
When a patient is identified at nutrition risk, the patient is assessed for malnutrition using the ASPEN and Academy of Nutrition and Dietetics (AND) guidelines as part of the nutrition care process.11, 14, 16 Nutrition assessment is a complex process by which a trained clinician (registered dietitian nutritionist [RDN], physician, or nurse) obtains detailed patient information to formulate a diagnosis to plan an intervention.11 To guide best practice for the diagnosis of malnutrition, AND and ASPEN have provided the following 6 malnutrition clinical characteristics: (1) inadequate energy intake, (2) interpretation of weight loss, (3) loss of fat mass, (4) loss of muscle mass, (5) fluid accumulation, (6) reduced grip strength.8, 16 The Nutrition Focused Physical Exam (NFPE) is used to enhance the detection of fat and muscle loss and presence of fluid accumulation in specific areas of the body.21 However, these malnutrition clinical characteristics are still being validated.3, 8, 16, 22
To improve the detection of patients at risk for malnutrition, the RDNs at ThedaCare Regional Medical Center developed a nutrition risk screening tool, known as the ThedaCare Nutrition Risk Screen (ThedaCare NRS), which is easy to use and time effective. The primary objective of this study was to compare the sensitivity and specificity of the ThedaCare NRS with the NRS 2002 in their ability to identify patients at risk for malnutrition who warrant further nutrition assessment. The results of the nutrition risk screens that indicated a patient was at risk for malnutrition were confirmed by the RDN, who completed a nutrition assessment that included the 6 malnutrition clinical characteristics defined by AND/ASPEN.21 This approach is consistent with best clinical practice for the diagnosis of malnutrition.21
Methods
Participants
Patients admitted to the ThedaCare Regional Hospitals, Neenah and Appleton, WI, were recruited from October 2015 to July 2016 (n = 607). All patients admitted during this time frame were enrolled. A total of 16 patients were excluded from the final analysis due to voluntary participation withdrawal (n = 3) and data collection errors (n = 13); therefore, 594 patients were included in the final statistical analysis. Inclusion criteria for study enrollment were the following: ≥18 years old and received non–intensive care unit (ICU) inpatient hospitalization for medical or surgical reasons. Exclusion criteria were pregnancy or concerns that would interfere with ability to give informed consent. The Western Institutional Review Board approved this study, and all patients provided written informed consent. This trial was registered at www.clinicaltrials.gov as NCT02585245.
Study Design
Using Lean methodology, a collection of tools and concepts used to improve quality, safety, and efficiency of care delivery in the healthcare setting, the RDNs at ThedaCare Regional Medical Center identified that the validated NRS 2002 was missing patients at risk for malnutrition. To address this issue, the ThedaCare NRS was developed.23 The primary objective of this crossover intervention trial was to compare the sensitivity and specificity of the ThedaCare NRS when compared with the NRS 2002. To diagnose malnutrition, RDNs performed a nutrition assessment and an NFPE that used the 6 malnutrition clinical characteristics established by AND/ASPEN.8 The abbreviation RDNA is used throughout this article to indicate the administration of the nutrition assessments, which included the NFPE, performed by the RDN in the context of this study. The study protocol is shown in Figure 1.
Figure 1.
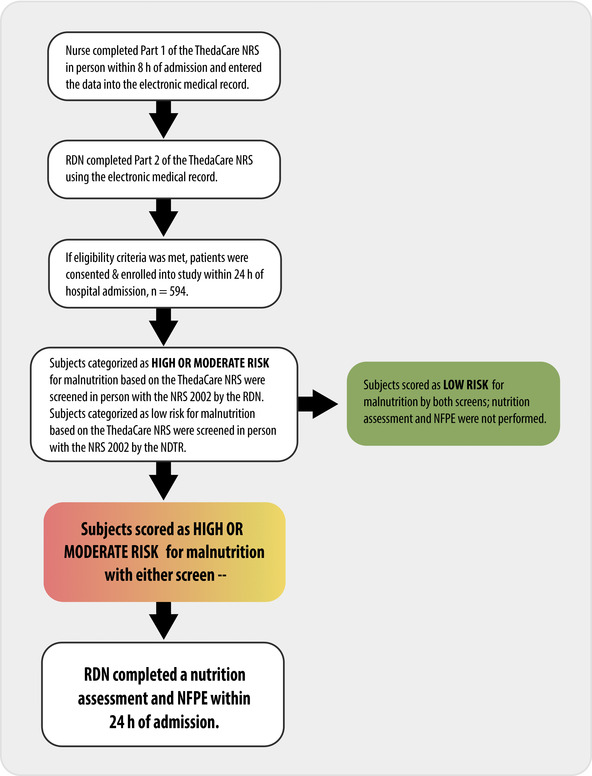
Flow chart of study design and protocol. NDTR, nutrition and dietetics technician, registered; NFPE, Nutrition Focused Physical Exam; NRS 2002, Nutrition Risk Screen 2002; RDN, registered dietitian nutritionist; ThedaCare NRS, ThedaCare Nutrition Risk Screen.
Study Protocol
Within 24 hours of hospital admission, each patient was screened for malnutrition using the ThedaCare NRS and the NRS 2002 (Figure 2 and Table 1). First, part 1 of the ThedaCare NRS was completed in person by a nurse within 8 hours of hospital admission, and part 2 was completed using the electronic medical record by the RDN within 24 hours of hospital admission. If the ThedaCare NRS indicated that a patient was at high or moderate risk for malnutrition, the RDNA was administered within 24 hours of hospital admission. If the ThedaCare NRS indicated that a patient was at moderate or high risk for malnutrition, the NRS 2002 and the RDNA were administered by the RDN. In general clinical practice, when patients are categorized as high or moderate risk for malnutrition based on the ThedaCare NRS, the RDNA is administered within 24–48 hours and 72 hours, respectively.
Figure 2.
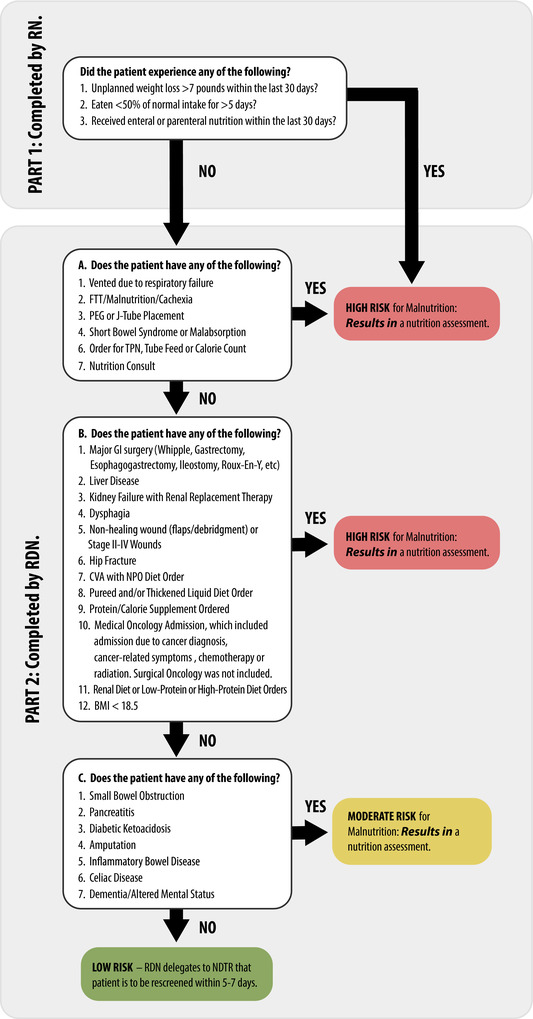
Flowchart of the ThedaCare Nutrition Risk Screen. This screen was completed using the electronic medical record. BMI, body mass index; CVA, cerebrovascular accident; FTT, failure to thrive; GI, gastrointestinal; J‐tube, jejunostomy tube; NDTR, nutrition and dietetics technician, registered; NPO, nothing by mouth; PEG, percutaneous endoscopic gastrostromy; RDN, registered dietitian nutritionist; RN, registered nurse; TPN, total parenteral nutrition.
Table 1.
Method Used to Evaluate Risk for Malnutrition Using the Nutrition Risk Screen 2002
| Impaired Nutrition Status | Severity of Disease | ||
|---|---|---|---|
| Mild |
|
Mild | Hip fracture, chronic disease, in particular with acute complications: cirrhosis, chronic obstructive pulmonary disease, chronic hemodialysis, diabetes, malignant oncology. |
| Score 1 | Score 1 | ||
| Moderate |
|
Moderate | Major abdominal, stroke, severe pneumonia, malignant hematology. |
| Score 2 | Score 2 | ||
| Severe |
|
Severe | Head injury, bone marrow transplantation, intensive care patients with an APACHE II score > 10. |
| Score 3 | Score 3 | ||
| Add 1 point to the score if the patient is ≥70 years of age. | |||
|
Severity of Disease Score: | ||
| Total Score = Impaired Nutrition Status and Severity of Disease Scores | |||
This screen was completed in person. Nutrition care plans were initiated for patients who were categorized with high risk for malnutrition (scores ≥ 5) and moderate risk for malnutrition (scores = 3–4). Patients that were categorized with low risk for malnutrition (scores = 0–2) were rescreened weekly. APACHE, Acute Physiology and Chronic Health Evaluation; BMI, body mass index.
If the ThedaCare NRS indicated that a patient was at low risk for malnutrition, the NDTR, rather than the RDN, met in person with each patient to administer the NRS 2002 and to verify that parts 1 and 2 of the ThedaCare NRS were answered correctly. Screening patients for nutrition risk is within the NDTR scope of practice.14 If the NDTR found that the patient might be at risk for malnutrition based on the NRS 2002 or verification of ThedaCare NRS, the patient was transferred back to the RDN for a nutrition assessment. Patients that were categorized as low risk for malnutrition were rescreened within 5–7 days. The nutrition risk screen methodology for the NRS 2002 is detailed in Table 1 and for the ThedaCare NRS in Figure 2.
Nutrition Assessment and the NFPE
As previously stated, the abbreviation RDNA is used throughout the article to indicate the administration of a nutrition assessment, which included the NFPE, by the RDN. Each nutrition assessment incorporated the clinical diagnosis, surgical history, clinical and anthropometric data, laboratory/inflammation markers, dietary history, functional status, and NFPE. The NFPE is a physical exam systematically carried out using a head‐to‐toe approach. Both visualization and palpation are used to identify muscle and fat stores and edema. The NFPE included inspection and rating of muscle groups in the following areas: temporal, clavicle, shoulders, scapula, interosseous, thigh, knee, and calf. Loss of subcutaneous fat was assessed and rated in the following 3 main areas: orbital, triceps, and ribs. The ThedaCare RDNs completed a comprehensive competency to assure standard, repeatable methodology to complete the NPFE. The competency consisted of 4 parts that assess both knowledge and hands on demonstrations of accurately diagnosing malnutrition.
Sensitivity and Specificity Calculations
To assess how well the ThedaCare NRS and NRS 2002 identify patients at moderate or high risk for malnutrition vs patients at low risk for malnutrition, sensitivity and specificity were calculated. The definitions and calculations used to determine sensitivity, specificity, negative predictive value, and positive predictive value are described in Supplemental Table 1.24
Statistical Analysis
Statistical analyses used to compare patient characteristics were completed in SAS 9.4 (SAS Institute, Cary, NC). The ratio to compare sex, mortality, rates of 30‐day hospital readmissions, transitions to palliative or hospice care, number of misclassified patients, false negatives, and true positives were compared using the Fisher's exact test. Age and length of stay comparisons were analyzed using 2‐sample t‐tests. When data were skewed, the Kruskal‐Wallis test was used. Statistical significance to compare patient characteristics was set at P < .05. The statistical analyses to compare nutrition risk screening and assessment tools and the odd ratio estimation were completed in R version 3.3.3 with RStudio version 1.0.136.25, 26 The results are expressed a mean ± SD and, where appropriate, 95% confidence intervals are indicated. To determine correlations between nutrition assessment parameters and the NRS 2002 and ThedaCare NRS screening tools, nutrition risk was categorized as low risk = 0, moderate risk = 1, and high risk (defined as high risk or nutrition assessment diagnosed severe or moderate malnutrition) = 2. The χ2 test was used to compare the differences in the prevalence of nutrition risk. In addition, agreement between a screening tool vs the nutrition assessment was tested through analysis of the κ statistic. κ statistic values as a measure of agreement were interpreted as follows: <0.2 = poor, 0.2–0.4 = fair, 0.4–0.6 = moderate, 0.6–0.8 = substantial, and >0.8 near‐perfect agreement. Odds ratio estimations to measure association between screening tools and length of stay were computed using multiple logistic regression adjusted for the age of the patient. Odds ratios with 95% confidence intervals report a measure of significance of the effects of low, moderate, or high risk for malnutrition as assessed by the screening tool in comparison with reference categories of length of stay = 1–5 days and length of stay >5 days. Significance of the κ statistic, odds ratios, and χ2 statistical tests are reported as observed or in comparison with P = .001.
Results
Patient Characteristics
Characteristics among patients with vs without malnutrition and characteristics among patients diagnosed with moderate vs severe malnutrition are described in Table 2. Sex distribution among patients with and without malnutrition did not differ. Patients diagnosed with moderate or severe malnutrition were significantly older, had a longer length of stay, and had more 30‐day hospital readmissions, transitions to palliative or hospice care, and deaths by the conclusion of the study when compared with patients without malnutrition (Table 2). Patients with moderate and severe malnutrition had similar ages, length of stay, and similar rates of 30‐day hospital readmissions and transitions to palliative or hospice care. However, 36% of patients with severe malnutrition were deceased by the conclusion of the study, which was significantly higher when compared with the 25% of patients with moderate malnutrition who were deceased by the conclusion of the study (Table 2). Of the 184 patients diagnosed with moderate or severe malnutrition, 9 patients did not receive a nutrition intervention due to hospital discharge or comfort of care or declined the intervention.
Table 2.
Patient Characteristics at Hospital Admission Based on Malnutrition Diagnosis
| Malnutrition Diagnosis (n = 594) | Negative (n = 410) | Positivea (n = 184) | P |
|---|---|---|---|
| Male/female, n | 189/221 | 87/97 | .79c |
| Male/female, % | 46/54 | 47/53 | – |
| Age, yearsb | 61 ± 15 | 66 ± 15 | .0005d |
| Length of stay, days2 | 3.5 ± 4.0 | 4.8 ± 3.8 | <.0001d |
| 30‐day hospital readmission, yes/no | 25/385 (6%) | 26/158 (14%) | .0023c |
| Palliative care, yes/no, n | 7/403 (2%) | 13/171 (7%) | .002c |
| Hospice, yes/no, n | 11/399 (3%) | 16/168 (9%) | .002c |
| Life ratio, deceased/lived, n | 46/364 (11%) | 67/117 (36%) | <.0001c |
| Positive Malnutrition Diagnosis (n = 184) | Moderate Malnutrition | Severe Malnutrition | P |
|---|---|---|---|
| Male/female, n | 29/30 | 58/67 | .75c |
| Male/female, % | 49/51 | 46/54 | – |
| Age, years | 67 ± 16 | 66 ± 15 | .63e |
| Length of stay, days | 4.5 ± 3.4 | 5.0 ± 4.0 | .54d |
| 30‐day hospital readmission, yes/no | 8/51 (4%) | 18/107 (14%) | 1.00c |
| Palliative Care, yes/no, n | 5/54 (8%) | 8/117 (6%) | .76c |
| Hospice, yes/no, n | 3/56 (5%) | 13/112 (10%) | .28c |
| Life ratio, deceased/lived, n | 15/44 (25%) | 52/73 (36%) | .03c |
A positive malnutrition diagnosis refers to the patients that were diagnosed with moderate or severe malnutrition per the nutrition assessment.
Age and length of stay values are means ± SD.
Fishers’ exact test.
Kruskal‐Wallis test.
Two‐sample t‐test.
ThedaCare NRS Was More Sensitive, But Less Specific, When Compared With the NRS 2002
The nutrition risk screen performance comparisons are summarized in Table 3. All differences among the proportions of the ThedaCare NRS and NRS 2002 that categorized patients with low, moderate, and high risk for malnutrition were significant, which suggests that the quality of these proportions was adequate (χ2, P < .0001). The ThedaCare NRS demonstrated higher sensitivity (98.8%) when compared with the NRS 2002 (63.5%), which indicates that the ThedaCare NRS was able to identify more patients at moderate or high risk for malnutrition when compared with the NRS 2002. However, the ThedaCare NRS had lower specificity (74.0%) when compared with the NRS 2002 (94.3%), which suggests that the NRS 2002 correctly identified more patients with low risk for malnutrition than the ThedaCare NRS.
Table 3.
Nutrition Risk Screen Performance Comparison Between the NRS 2002 and ThedaCare NRS, Confirmed Using the Nutrition Assessment
| Malnutrition Characteristics, n | ||||||
|---|---|---|---|---|---|---|
| NRS 2002 | ThedaCare NRS | |||||
| Low Risk, n | Moderate or High Risk, n | Total, n | Low Risk, n | Moderate or High Risk, n | Total, n | |
| RDNA | ||||||
| Low risk, n | 250 | 15 | 265 | 196 | 69 | 265 |
| Moderate or high risk; moderate or severe malnutrition, n | 120 | 209 | 329 | 4 | 325 | 329 |
| Total, n | 370 | 224 | 594 | 200 | 394 | 594 |
| Statistical Measures of Nutrition Risk Screen Performance | ||||
|---|---|---|---|---|
| NRS 2002 | ThedaCare NRS | |||
| % | 95% CI | % | 95% CI | |
| Sensitivity | 63.5 | 58.3–68.7 | 98.8 | 97.6–99.9 |
| Specificity | 94.3 | 91.5–97.1 | 74.0 | 68.7–79.2 |
| PPV | 93.3 | 90.0–96.6 | 82.5 | 78.7–86.2 |
| NPV | 67.6 | 62.8–72.3 | 98.0 | 96.1–99.9 |
| κ coefficient | 0.56 (z = 14.5, P < .001) | 0.75 (z = 18.6, P < .001) | ||
NPV, negative predictive value; NRS 2002, Nutrition Risk Screen 2002; PPV, positive predictive value; RDNA, administration of the nutrition assessment, which included the Nutrition Focused Physical Exam, by the registered dietitian nutritionist; ThedaCare NRS, ThedaCare Nutrition Risk Screen.
Overall, the ThedaCare NRS misclassified fewer patients (147/594 or 24.7%) when compared with the NRS 2002 (263/594 or 44.3%; P < .0001). Furthermore, the ThedaCare NRS yielded significantly fewer false negatives (4/325 or 1%) when compared with the NRS 2002 (120/209 or 36%, P < .0001), indicating that the ThedaCare NRS missed fewer patients at risk for malnutrition. Of the 120 patients misclassified as low risk for malnutrition by the NRS 2002, 56 patients were determined to be at moderate risk for malnutrition and 64 patients were determined to be at high risk for malnutrition or moderate or severe malnutrition per the nutrition assessment. Of the 4 patients misclassified as low risk for malnutrition by the ThedaCare NRS, all 4 patients were determined to be at moderate risk for malnutrition per the nutrition assessment. Thus, no patients with high risk for malnutrition or moderate/severe malnutrition were misclassified by the ThedaCare NRS.
ThedaCare NRS Had Better Agreement and Took Less Time to Administer Than the NRS 2002
To evaluate the inter‐rater agreement between a nutrition risk screen and the RDNA, we used the κ statistic for the following comparisons: (1) the ThedaCare NRS and the RDNA and (2) the NRS 2002 and the RDNA. The ThedaCare NRS had a higher κ coefficient when compared with the NRS 2002 (κ coefficient: ThedaCare NRS, 0.75, P < .001; NRS 2002, 0.56, P < .001). This suggests that regardless of who administered the nutrition risk screen and the RDNA, the results generated by the ThedaCare NRS will more likely agree than when compared with the NRS 2002. Furthermore, the ThedaCare NRS required less time to complete (in part because it used the electronic medical record) when compared with the in person NRS 2002 (mean ± SE: ThedaCare, 17 ± 1 seconds; NRS 2002, 9 ± 1 minutes; P < .0001).
ThedaCare NRS and NRS 2002 as Predictors of Length of Stay
Multiple logistic regressions adjusted for age were used to estimate the odds ratios between the nutrition risk screens and length of stay. The results are summarized in Table 4. The analysis was run for length of stay 1–5 days and >5 days. The average length of stay was 4.8 days for the patients categorized with moderate or severe malnutrition (n = 184). Patients categorized at high risk for malnutrition using the ThedaCare NRS or based on the RDNA had a significant association with a length of stay (age‐adjusted odds ratio [95% CI]: ThedaCare NRS, 4.26 [2.52–7.60], P < .001; nutrition assessment, 3.07 [1.97–4.88], P < .001). This association with length of stay did not maintain significance when patients were categorized with moderate or low risk for malnutrition using the ThedaCare NRS or RDNA. The patients categorized with moderate and high risk for malnutrition had a significant association with length of stay based on the NRS 2002 (age‐adjusted odds ratio [95% CI]: moderate risk, 3.04 [1.94–4.76], P < .001; high risk, 4.08 [2.17–7.59], P < .001). In summary, the patients who were categorized as high risk for malnutrition by the RDNA, ThedaCare NRS, or NRS 2002 were significant predictors of length of stay >5 days. In addition, the patients categorized with moderate‐risk malnutrition by the NRS 2002 were found to have a significant association with length of stay >5 days.
Table 4.
Age‐Adjusted ORs Among LOS and the Nutrition Assessment or the Nutrition Risk Screens
| LOS, 1–5 days | LOS, > 5 days | |||||
|---|---|---|---|---|---|---|
| % | n | % | n | OR (95% CI) | P‐Value | |
| RDNA | ||||||
| Low risk | 81 | 231 | 13 | 34 | 1 | |
| Moderate risk | 82 | 68 | 18 | 15 | 1.49 (0.74–2.86) | .24 |
| High risk | 68 | 168 | 32 | 78 | 3.07 (1.97–4.88) | <.001 |
| ThedaCare NRS | ||||||
| Low risk | 92 | 183 | 9 | 17 | 1 | |
| Moderate risk | 81 | 26 | 19 | 6 | 2.49 (0.83–6.62) | .08 |
| High risk | 71 | 258 | 29 | 104 | 4.26 (2.52–7.60) | <.001 |
| NRS 2002 | ||||||
| Low risk | 87 | 320 | 16 | 50 | 1 | |
| Moderate risk | 68 | 112 | 33 | 54 | 3.04 (1.94–4.76) | <.001 |
| High risk | 60 | 35 | 40 | 23 | 4.08 (2.17–7.59) | <.001 |
LOS, length of stay; NRS 2002, Nutrition Risk Screen 2002; OR, odds ratio; RDNA, administration of the nutrition assessment, which included the Nutrition Focused Physical Exam, by the registered dietitian nutritionist; ThedaCare NRS, ThedaCare Nutrition Risk Screen.
Discussion
Identification of patients at risk for or with malnutrition in the hospital setting with an effective nutrition risk screening tool is essential for early nutrition assessment and intervention to reduce morbidity and mortality. Previous studies have indicated that the NRS 2002 yields high rates of false negatives, meaning that patients with malnutrition are frequently missed, particularly in elderly populations.4, 19, 20, 27, 28 The high rates of false negatives with the NRS 2002 may be due to lack of a score to address plan of care.19 We developed a nutrition risk screening tool, known as the ThedaCare NRS, which incorporated plan of care and expanded the list for disease etiology in the decision matrix (Figure 2). With incorporation of plan of care and the expansion of disease etiology into the decision matrix, the ThedaCare NRS had higher sensitivity (ThedaCare NRS, 98.8% vs NRS 2002, 63.5%), but lower specificity when compared with the NRS 2002. In addition, the ThedaCare NRS missed fewer patients at risk for malnutrition (ie, fewer false negatives), misclassified fewer patients overall, and took less time to complete when compared with the NRS 2002. To the best of our knowledge, this is the first prospective study to evaluate NRS 2002 and confirm risk for malnutrition or malnutrition diagnosis using the nutrition assessment, which included the NFPE and employed the 6 malnutrition clinical characteristics as defined by AND/ASPEN as the reference method. In short, the ThedaCare NRS may improve the identification of adult patients in the non‐ICU hospital setting at risk for or with malnutrition in the non‐ICU hospital setting to allow for early nutrition assessment and intervention. These advantages of the ThedaCare NRS may lead to reduced complications, length of stay, and healthcare costs.
The NRS 2002 is recognized by the European Society for Parenteral and Enteral Nutrition as the preferred3, 29 nutrition risk screening tool for hospitalized patients, but its reported sensitivity and specificity varies widely at 50%–86% and 21%–93%, respectively.4, 17, 30, 31, 32 Many studies that have evaluated the NRS 2002 used the Subjective Global Assessment as the reference method.4, 17, 22, 29 However, the nutrition assessment using the 6 malnutrition clinical characteristics as outlined by AND/ASPEN has replaced the Subjective Global Assessment as part of the nutrition care process.14, 16
Kyle et al4 evaluated the sensitivity and specificity of the NRS 2002 as confirmed using the Subjective Global Assessment as the reference method in 995 adult hospitalized patients. Interestingly, Kyle et al4 found similar sensitivity, specificity, and agreement for the NRS 2002 as confirmed using the Subjective Global Assessment when compared with the results that we report for the NRS 2002.4 Current guidelines for the nutrition assessment as part of the nutrition care process use the 6 malnutrition clinical characteristics developed by AND/ASPEN.3, 16 Given these similar results, the current study contributes to the evidence base that the nutrition assessment and NFPE, which employs the 6 malnutrition clinical characteristics outlined by AND/ASPEN, produces similar results as a nutrition assessment tool when compared with the Subjective Global Assessment.
In addition, Kyle et al4 reported a high false negative rate of 38% with the NRS 2002 as confirmed using the Subjective Global Assessment, which is similar to the 36% false negative rate with the NRS 2002 that we report in this study. The high false negative rates of the NRS 2002 observed in our study and by Kyle et al4 indicate that more than one third (36%–38%) of patients at risk for malnutrition would have been missed, thereby delaying nutrition assessment and intervention and increasing the risk of prolonged length of stay, hospital readmission, and health complications.10
The ThedaCare NRS identified more patients at risk for malnutrition and in less time when compared with the NRS 2002, allowing for prompt nutrition assessment and intervention. This study confirms that the ThedaCare NRS has the sensitivity to identify elderly patients in the non‐ICU hospital setting who were at risk for malnutrition, considering that 50% of our patients were older than the age of 65 years. Consistent with previous reports, our study provides additional evidence that the NRS 2002 cannot adequately identify elderly patients in the non‐ICU hospital setting who are at risk for malnutrition. Given that the ThedaCare NRS had a high sensitivity of 98.8% and missed fewer patients at risk for malnutrition, as evidenced by a false negative rate of 2%, the ThedaCare NRS might allow for earlier malnutrition diagnosis to initiate early nutrition intervention or to create an early opportunity for patients to determine the aggressiveness of the intervention based on quality of life.
The improved sensitivity of the ThedaCare NRS when compared with the NRS 2002 may be related to the incorporation of the plan of care and expanded disease etiology into the nutrition risk screen (Figure 2). Plans of care incorporated into the ThedaCare NRS that could categorize a patient at moderate or high risk for malnutrition included special diet orders, nutrition support, and major gastrointestinal surgery. Although disease severity is addressed in the NRS 2002 (Table 1), the ThedaCare expanded on the disease etiology that could increase the risk for malnutrition, such as pancreatitis, celiac disease, and inflammatory bowel disease. Despite the improved sensitivity of the ThedaCare NRS with the incorporation of the plan of care and expanded list for disease etiology to allow for more prompt nutrition assessments and interventions, it may have reduced the specificity of the screen. Albeit reduced specificity, it is more important that the ThedaCare NRS has a high sensitivity for the identification of patients at risk for malnutrition. Early identification of malnutrition risk allows for nutrition assessment and intervention, which may reduce clinical complications, hospital stay, and cost. However, this study was not designed to test the impact of the ThedaCare NRS and subsequent nutrition interventions on clinical outcomes.
The strengths of this study included a large sample size, performance of both nutrition screens (ThedaCare NRS and NRS 2002) on each patient, confirmation of nutrition risk screen outcomes using the 6 malnutrition clinical characteristics with nutrition assessment and the NFPE per AND/ASPEN 2013 revised consensus statement on malnutrition, enrollment of patients through multiple seasons, and lack of selection bias with use of continuous enrollment. Limitations of this study included the inability to administer a full‐scope nutrition assessment by the RDN to patients at low risk for malnutrition due to time and resources and a lack of a control group to investigate the efficacy of the ThedaCare NRS when compared with the NRS 2002 on 30‐day hospital readmissions and health outcomes.
Conclusions
When compared with the NRS 2002, the ThedaCare NRS improved the accuracy of the identification of patients at risk for malnutrition, particularly in elderly patients. Furthermore, the ThedaCare NRS misclassified fewer patients at risk for malnutrition and required less time to administer than the NRS 2002 due in part to a reliance on the electronic medical record. To the best of our knowledge, this is the first study that has evaluated the sensitivity and specificity of the NRS 2002 as confirmed using the 6 malnutrition clinical characteristics with the nutrition assessment and NFPE per AND/ASPEN. Improvement of nutrition risk screen practices to allow for prompt nutrition assessment and intervention for patients with malnutrition can lower healthcare costs, hospital readmission rates, and length of stay. Further study to validate the efficacy of the ThedaCare NRS in various hospitalized patient populations and age groups in addition to the impact of early nutrition intervention are needed.
Supporting information
Supplementary Table 1
Acknowledgments
The authors would like to acknowledge Angelica Gronke for her efforts in the development and conduction of the competencies and training for the Nutrition Focused Physical Exam necessary to instruct the registered dietitian nutritionists collecting the data for this study. The authors would like to thank the Sharon Weitz, the registered dietitian nutritionists and nutrition and dietetics technicians, registered, at the ThedaCare Regional Hospitals, Appleton and Neenah, Wisconsin, for their contributions in the data collection for this study.
Statement of Authorship
L. L. K. Hartz, B. M. Stroup, C. Shockey, and D. M. Ney contributed to the conception and design of the research. L. L. K. Hartz, B. M. Stroup, T. A. Bibelnieks, and C. Shockey contributed to analysis of the data. B. M. Stroup and T. A. Bibelnieks contributed to analysis and interpretation of the data. L. L. K. Hartz, B. M. Stroup, T. A. Bibelnieks, C. Shockey, and D. M. Ney drafted the manuscript. All authors critically revised the manuscript, agree to be accountable for the accuracy and integrity of the data, and read and approved the final version of this manuscript.
Financial disclosure: None declared.
Conflicts of interest: None declared.
References
- 1. Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. J Acad Nutr Diet. 2013;113(9):1219‐1237. [DOI] [PubMed] [Google Scholar]
- 2. Curtis LJ, Bernier P, Jeejeebhoy K, et al. Costs of hospital malnutrition. Clin Nutr. 2017;36(5):1391‐1396. [DOI] [PubMed] [Google Scholar]
- 3. Malone A, Hamilton C. The Academy of Nutrition and Dietetics/the American Society for Parenteral and Enteral Nutrition consensus malnutrition characteristics: application in practice. Nutr Clin Pract. 2013;28(6):639‐650. [DOI] [PubMed] [Google Scholar]
- 4. Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clin Nutr. 2006;25(3):409‐417. [DOI] [PubMed] [Google Scholar]
- 5. Corkins MR, Guenter P, DiMaria‐Ghalili RA, et al. Malnutrition diagnoses in hospitalized patients: United States, 2010. JPEN J Parenter Enteral Nutr. 2014;38(2):186‐195. [DOI] [PubMed] [Google Scholar]
- 6. Makhija S, Baker J. The Subjective Global Assessment: a review of its use in clinical practice. Nutr Clin Pract. 2008;23(4):405‐409. [DOI] [PubMed] [Google Scholar]
- 7. Jensen GL, Compher C, Sullivan DH, Mullin GE. Recognizing malnutrition in adults: definitions and characteristics, screening, assessment, and team approach. JPEN J Parenter Enteral Nutr. 2013;37(6):802‐807. [DOI] [PubMed] [Google Scholar]
- 8. White JV, Guenter P, Jensen G, et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr. 2012;36(3):275‐283. [DOI] [PubMed] [Google Scholar]
- 9. Gastalver‐Martin C, Alarcon‐Payer C, Leon‐Sanz M. Individualized measurement of disease‐related malnutrition's costs. Clin Nutr. 2015;34(5):951‐955. [DOI] [PubMed] [Google Scholar]
- 10. Fingar KR, Weiss AJ, Barrett ML, et al. All‐Cause Readmissions Following Hospital Stays for Patients With Malnutrition, 2013: Statistical Brief #218. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville; (MD: ); 2016. [Google Scholar]
- 11. Toulson Davisson Correia M. Nutrition screening vs nutrition assessment: what's the difference? Nutr Clin Pract. 2018;33(1):62‐72. [DOI] [PubMed] [Google Scholar]
- 12. Somanchi M, Tao X, Mullin GE. The facilitated early enteral and dietary management effectiveness trial in hospitalized patients with malnutrition. JPEN J Parenter Enteral Nutr. 2011;35(2):209‐216. [DOI] [PubMed] [Google Scholar]
- 13. Stratton RJ, King CL, Stroud MA, Jackson AA, Elia M. “Malnutrition Universal Screening Tool” predicts mortality and length of hospital stay in acutely ill elderly. Br J Nutr. 2006;95(2):325‐330. [DOI] [PubMed] [Google Scholar]
- 14. Academy Quality Management Committee . Academy of nutrition and dietetics: Revised 2017 standards of practice in nutrition care and standards of professional performance for registered dietitian nutritionists. J Acad Nutr Diet. 2018;118(1):132–140.e15. [DOI] [PubMed] [Google Scholar]
- 15. Academy Quality Management Committee . Academy of nutrition and dietetics: Revised 2017 standard of practice in nutrition care and standards of professional performance for nutrition and dietetics technicians, registered. J Acad Nutr Diet. 2018;118(2):317–326.e13. [DOI] [PubMed] [Google Scholar]
- 16. Hand RK, Murphy WJ, Field LB, et al. Validation of the Academy/A.S.P.E.N. malnutrition clinical characteristics. J Acad Nutr Diet. 2016;116(5):856‐864. [DOI] [PubMed] [Google Scholar]
- 17. Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Group Ad Hoc ESPEN Working. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321‐336. [DOI] [PubMed] [Google Scholar]
- 18. Anthony PS. Nutrition screening tools for hospitalized patients. Nutr Clin Pract. 2008;23(4):373‐382. [DOI] [PubMed] [Google Scholar]
- 19. van Bokhorst‐de van der Schueren MA, Guaitoli PR, Jansma EP, de Vet HC. Nutrition screening tools: does one size fit all? A systematic review of screening tools for the hospital setting. Clin Nutr. 2014;33(1):39‐58. [DOI] [PubMed] [Google Scholar]
- 20. Christner S, Ritt M, Volkert D, Wirth R, Sieber CC, Gassmann KG. Evaluation of the nutritional status of older hospitalised geriatric patients: a comparative analysis of a Mini Nutritional Assessment (MNA) version and the Nutritional Risk Screening (NRS 2002). J Hum Nutr Diet. 2016;29(6):704‐713. [DOI] [PubMed] [Google Scholar]
- 21. Academy Quality Management Committee and Scope of Practice Subcomittee of Quality Management Committee . Academy of nutrition and dietetics: Revised 2012 standards of practice in nutrition care and standards of professional performance for registered dietitians. J Acad Nutr Diet. 2013;113(6 suppl):S29–S45. [DOI] [PubMed] [Google Scholar]
- 22. Matarese LE, Charney P. Capturing the elusive diagnosis of malnutrition. Nutr Clin Pract. 2017;32(1):11‐14. [DOI] [PubMed] [Google Scholar]
- 23. Montella E, Di Cicco MV, Ferraro A, et al. The application of Lean Six Sigma methodology to reduce the risk of healthcare‐associated infections in surgery departments. J Eval Clin Pract. 2017;23(3):530‐539. [DOI] [PubMed] [Google Scholar]
- 24. Altman DG, Bland JM. Diagnostic tests. 1: sensitivity and specificity. BMJ. 1994;308(6943):1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. R Core Team (2017). R: A Language and Environment for Statistical Computing. https://www.R-project.org
- 26. RStudio Team (2017). RStudio: Integrated Development Environment for R (Version 1.0.136). RStudio Inc., Boston. https://www.rstudio.com/
- 27. Rabito EI, Marcadenti A, da Silva Fink J, Figueira L, Silva FM. Nutritional Risk Screening 2002, Short Nutritional Assessment Questionnaire, Malnutrition Screening Tool, and Malnutrition Universal Screening Tool are good predictors of nutrition risk in an emergency service. Nutr Clin Pract. 2017;32(4):526‐532. [DOI] [PubMed] [Google Scholar]
- 28. Raslan M, Gonzalez MC, Torrinhas RS, Ravacci GR, Pereira JC, Waitzberg DL. Complementarity of Subjective Global Assessment (SGA) and Nutritional Risk Screening 2002 (NRS 2002) for predicting poor clinical outcomes in hospitalized patients. Clin Nutr. 2011;30(1):49‐53. [DOI] [PubMed] [Google Scholar]
- 29. Fink JDS, Marcadenti A, Rabito EI, Silva FM. The New European Society for Clinical Nutrition and Metabolism Definition of Malnutrition: Application for nutrition assessment and prediction of morbimortality in an emergency service. JPEN J Parenter Enteral Nutr. 2018;42(3):550‐556. [DOI] [PubMed] [Google Scholar]
- 30. Poulia KA, Klek S, Doundoulakis I, et al. The two most popular malnutrition screening tools in the light of the new ESPEN consensus definition of the diagnostic criteria for malnutrition. Clin Nutr. 2017;36(4):1130‐1135. [DOI] [PubMed] [Google Scholar]
- 31. Almeida AI, Correia M, Camilo M, Ravasco P. Nutritional risk screening in surgery: valid, feasible, easy! Clin Nutr. 2012;31(2):206‐211. [DOI] [PubMed] [Google Scholar]
- 32. Velasco C, Garcia E, Rodriguez V, et al. Comparison of four nutritional screening tools to detect nutritional risk in hospitalized patients: a multicentre study. Eur J Clin Nutr. 2011;65(2):269‐274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1


