Abstract
BACKGROUND CONTEXT:
Past studies have focused on the association of high body mass index (BMI) on spine surgery outcomes. These investigations have reported mixed conclusions, possible due to insufficient power, poor controlling of confounding variables, and inconsistent definitions of BMI categories (e.g. underweight, overweight, and obese). Few studies have considered outcomes of patients with low BMI.
PURPOSE:
To analyze how anterior cervical spine surgery outcomes track with World Health Organization categories of BMI to better assess where along the BMI spectrum patients are at risk for adverse perioperative outcomes.
DESIGN/SETTING:
Retrospective cohort study.
PATIENT SAMPLE:
Patients undergoing elective anterior cervical spine surgery were abstracted from the 2005 to 2016 American College of Surgeons National Surgical Quality Improvement Program database.
OUTCOME MEASURES:
Thirty-day adverse events, hospital readmissions, postoperative infections, and mortality.
METHODS:
Patients undergoing anterior cervical spine procedures (anterior cervical discectomy and fusion, anterior cervical corpectomy, cervical arthroplasty) were identified in the 2005 to 2016 National Surgical Quality Improvement Program database. Patients were then aggregated into modified World Health Organization categories of BMI. Odds ratios of adverse outcomes, normalized to average risk of normal weight subjects (BMI 18.5–24.9 kg/m2), were calculated. Multivariate analyses were then performed on aggregated adverse outcome categories controlling for demographics (age, sex, functional status) and overall health as measured by the American Society of Anesthesiologists classification.
RESULTS:
In total, 51,149 anterior cervical surgery patients met inclusion criteria. Multivariate analyses revealed the odds of any adverse event to be significantly elevated for underweight and super morbidly obese patients (Odds Ratios [OR] of 1.62 and 1.55, respectively). Additionally, underweight patients had elevated odds of serious adverse events (OR=1.74) and postoperative infections (OR=1.75) and super morbidly obese patients had elevated odds of minor adverse events (OR=1.72). Relative to normal BMI patients, there was no significant elevation for any adverse outcomes for any of the other overweight/obese categories, in fact some had reduced odds of various adverse outcomes.
CONCLUSIONS:
Underweight and super morbidly obese patients have the greatest odds of adverse outcomes after anterior cervical spine surgery. The current study identifies underweight patients as an at-risk population that has previously not received significant focus. Physicians and healthcare systems should give additional consideration to this population, as they often already do for those at the other end of the BMI spectrum.
Keywords: American College of Surgeons National Surgical Quality Improvement Program (NSQIP), Anterior cervical spine, Body mass index (BMI), Mortality, Perioperative adverse events, Readmission, Risk factors, Underweight
Introduction
Anterior cervical surgery is one of the most common types of surgery performed on the spine each year, and the number of procedures continues to increase due to the aging population in the United States [1,2]. Identifying factors that place patients at risk for adverse outcomes after such interventions has thus been identified as an important step to better conduct patient counseling, surgical planning, and target quality improvement initiatives.
Body mass index (BMI) has been evaluated as a potential risk factor for adverse outcomes after a number of surgical interventions, including anterior cervical spine surgery [3–8]. However, the majority of studies investigating BMI as a risk factor have focused on the upper end of the BMI spectrum. This has largely been due to the number of individuals that are classified as obese continues to increase in most developed countries [9].
Although a number of studies have investigated the effect of BMI on adverse outcomes following anterior cervical surgeries, the results have been inconsistent; some studies have shown higher complication rates associated with obesity [10] and others have shown no significant difference. [5,11] A limitation to these and other studies, is that many are often performed at single institutions, have limited sample size, and/or draw data only from administrative inpatient databases [5,10–13].
A potentially important explanation of the variation seen for the effect of BMI on outcomes is that different studies use varying cutoff values for the BMI categories and do not separate increasing BMI into granular categories. For example, studies may label any patient with a BMI over 35 kg/m2 as obese and not consider the variation within the spectrum above this cutoff. [14] Aggregating large ranges of BMI like this, have the potential to mask the effect of BMI on outcomes. Patients with a BMI of 36 kg/m2 clearly may be different than patients with a BMI of 46 kg/m2 or even 56 kg/m2, yet all these patients would be considered in the same “obese” category if using the aforementioned categorization. In order to truly understand the effect of high BMI on outcomes, a more granular separation of overweight populations would be necessary.
In addition to ambiguity pertaining to differentiation of different overweight categories, studies often overlook the other end of the BMI spectrum, namely underweight patients [4,15–17]. To that end, studies often include underweight patients with those of the normal BMI which does not allow for examination of underweight as a specific BMI group and has the potential to skew the results of normal weight patient outcomes if underweight patients were to represent a group with distinct outcomes [14].
To address the above-noted questions, the current study was designed to utilize incremental BMI categories, as defined by the World Health Organization, to investigate perioperative outcomes after anterior cervical spine surgery for patients across the BMI spectrum. Perioperative outcomes were assessed using these BMI categories in the large, nationally representative sample of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database.
Methods
Patient cohort
The NSQIP database records and aggregates more than 150 variables on individual surgical cases from over 500 participating institutions. These variables, which include demographics, perioperative variables, and 30-day postoperative morbidity and mortality [18], are collected by trained reviewers from medical records, operative reports, and patient interviews [19]. Inter-rater reliability disagreement rates have been reported to be less than 2% [18].
Anterior cervical discectomy and fusion, anterior cervical corpectomy, and cervical arthroplasty cases were extracted from the 2005 to 2016 NSQIP datasets using Current Procedural Terminology (CPT) codes. The following CPT codes were used to identify anterior cervical discectomy and fusion cases: 22551, 22552, 22554, 63075; anterior cervical corpectomy cases: 63081, 63082; and cervical arthroplasty cases: 22856, 22857. Additional levels were measured through CPT codes 22552, 63082, and 22858.
Patients undergoing nonemergent surgery were identified based on NSQIP coding and were included in the study population. Fracture, trauma, infection, and tumor cases were excluded. Further, cases involving more than three levels were excluded from the study population.
Patient/surgical characteristics
BMI, defined as weight/height2, was calculated from recorded height (m) and weight (kg) and then cases were then binned into six different BMI group categories (Fig. 1). These were: underweight (BMI<18.5 kg/m2), normal weight (BMI of 18.5–24.9 kg/m2), overweight (BMI 25.0–29.9 kg/m2), obese (BMI of greater than 30.0–39.9 kg/m2), morbidly obese (BMI of greater than 40.0–49.9 kg/m2), and super morbidly obese (BMI greater than 50.0 kg/m2).
Fig. 1.
Projected variance of body shape based on body mass index of World Health Organization categories.
Age, sex, functional status prior to surgery, American Society of Anesthesiologists (ASA) classification, smoking status (current and/or within 1 year), and presence of noninsulin-dependent or insulin-dependent diabetes were also directly extracted from the dataset. The ASA score was used to approximate the overall health of patients, as supported by past literature [20–23,32–34].
Perioperative outcomes and readmission
NSQIP captures the occurrence of individual postoperative adverse outcome for every case through the 30th postoperative day, regardless of discharge status. Thus, occurrences of adverse events were extracted from NSQIP and investigated individually as well as in aggregated groups of any adverse, major adverse, and minor event and used for analyses.
Any adverse event (AAE) was defined as the occurrence of a minor adverse event (MAE) or serious adverse event (SAE). A MAE was defined as the occurrence of any of the following: superficial surgical site infection, wound dehiscence, pneumonia, urinary tract infection, and postoperative renal insufficiency. A SAE was defined as the occurrence of any of the following: deep infection, sepsis, failure to wean, unplanned intubation, postoperative renal failure, thromboembolic event, cardiac arrest, myocardial infarction, and stroke/cerebrovascular event.
In addition to being included in the above aggregated variables, postoperative infections (occurrence of superficial infection, deep infection, urinary tract infection, or sepsis) were separately assessed. Occurrence of death and readmission within 30 days of operation was also abstracted and assessed (noted that the readmissions data element was only available for cases that occurred in 2011–2016). Further, operative time (in minutes) and length of stay (in days) were collected. Incidence of all variables were investigated for each of the six BMI categories.
Data analysis
Univariate logistic regression models of BMI groups were calculated for surgical outcomes to estimate the relative risks of BMI on adverse events that occurred anytime during the 30-day postoperative period. Distribution of the patient population’s BMI was then charted on a histogram which was overlaid with adverse event frequency and binomial outcomes data as a function BMI shown in Figs. 2 and 3 respectively.
Fig. 2.
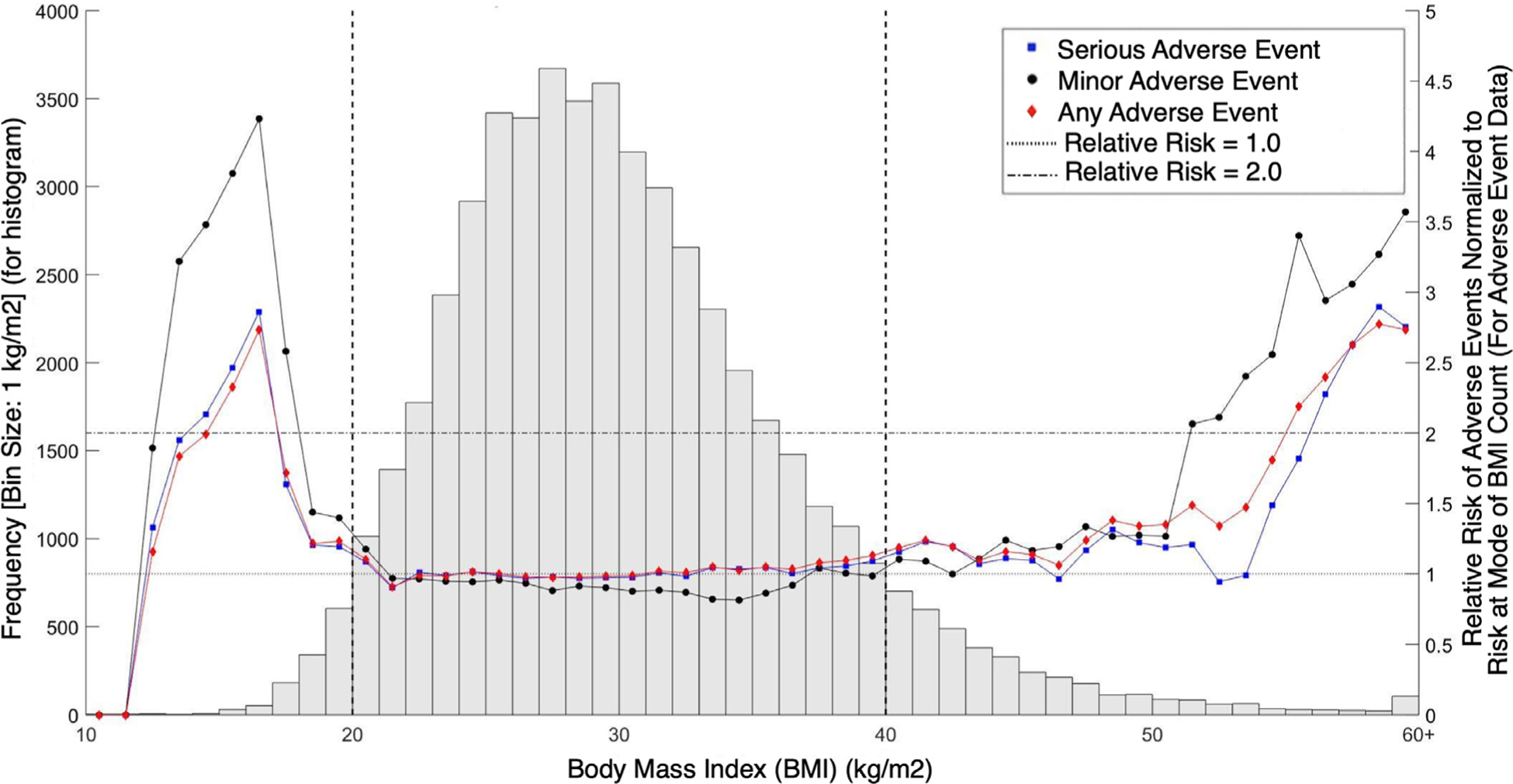
Adverse event data as a function of BMI and BMI histogram for patients undergoing anterior cervical procedures. Note: Left y-axis refers to the grey histogram in the figure. Right y-axis refers to the line and scatter plot of adverse event data. Horizontal lines denote relative risks of 1.0 and 2.0 as reference lines. Vertical lines bookend the stable BMI ranges. Blue squares represent major adverse events, black circles represent minor adverse events, red diamond represent any adverse events.
Fig. 3.
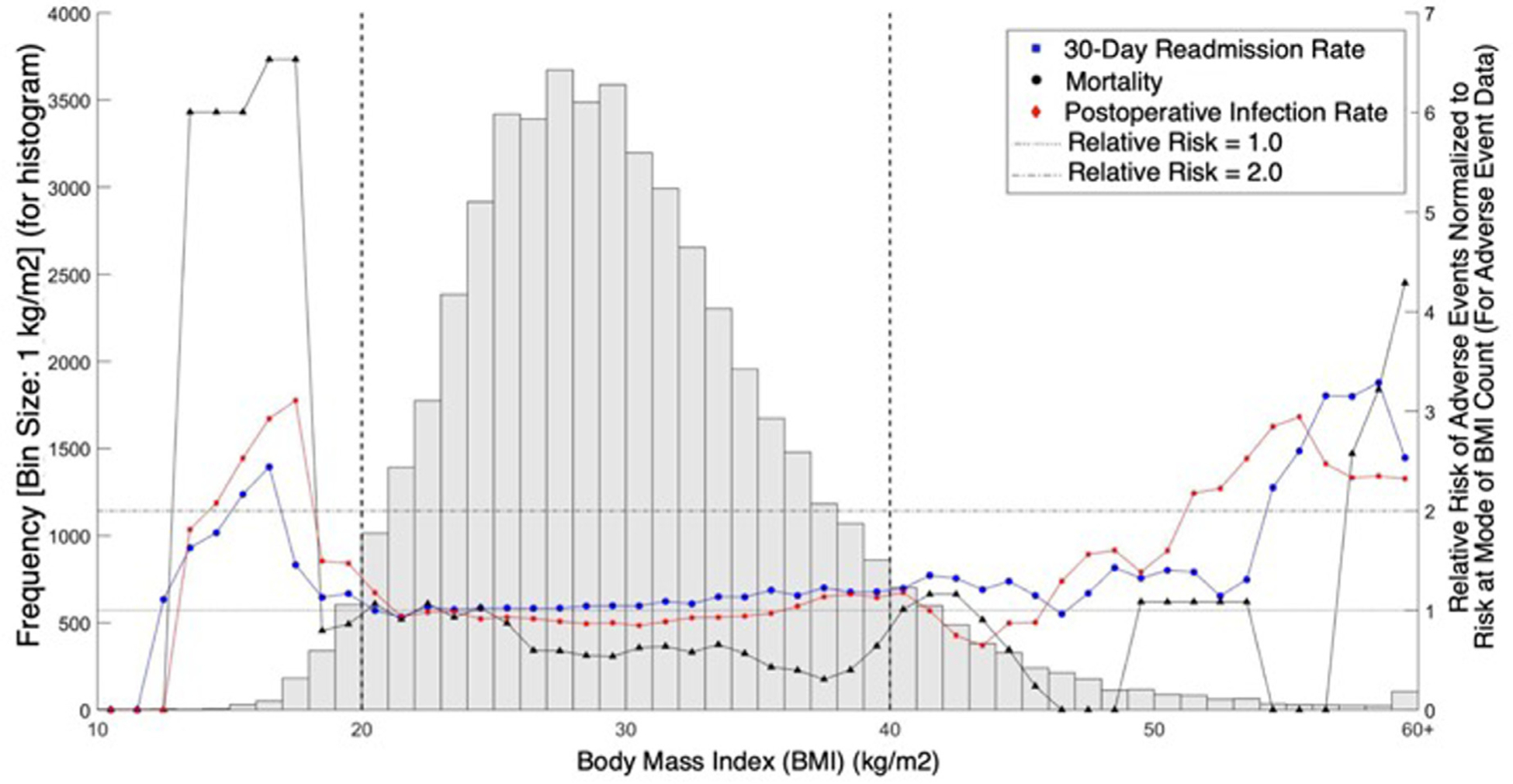
Binomial outcomes data as a function of BMI and BMI histogram for patients undergoing anterior cervical procedures. Just as in Fig. 2, left y-axis refers to the grey histogram in the figure. Right y-axis refers to the line and scatter plot of adverse event data. Horizontal lines denote relative risks of 1.0 and 2.0 as reference lines. Vertical lines bookend the stable BMI ranges. In this figure, blue circles represent 30-day readmission rates, black triangles represent mortality, and red stars represent infection rates.
To better control for potential demographic and health status differences between BMI categories, robust multivariate logistic regression models of BMI groups were fitted on the major surgical outcomes (AAEs, SAEs, MAEs, postoperative infections, readmissions, and mortality).
All statistical analyses were performed using STATA version 13 (StataCorp LP, College Station, TX). Our institutional review board granted an exemption for studies using the NSQIP dataset.
Results
Population characteristics and perioperative outcomes
A total of 51,149 patients met inclusion criteria. Of these, 9.94% (n=10,199) were “normal weight” with a BMI of 18.5 to 24.9 kg/m2. An additional 34.07% (n=17,425) were “overweight” with a BMI of 25.0 to 29.9 kg/m2, 37.60% (n=19,233) were “obese” (BMI: 30.0–39.9 kg/m2), 6.52% (n=3,333) were “morbidly obese” (BMI: 40.0–50.0 kg/m2), 1.05% (n=538) were “super morbidly obese” (BMI: >50 kg/m2), and 0.82% (n=421) were “underweight” (BMI: <18.5 kg/m2). The demographics and comorbidities for these in the different BMI categories are shown in Table 1.
Table 1.
Demographic and comorbid characteristics of patients undergoing anterior cervical procedures with varying body mass index (BMI)
| BMI<18.5 kg/m2 | BMI 18.5–24.9 kg/m2 | BMI 25.0–29.9 kg/m2 | BMI 30.0–39.9 kg/m2 | BMI 40.0–49.9 kg/m2 | BMI ≥ 50.0 kg/m2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight | Normal weight | Overweight | Obese | Morbidly obese | Super morbidly obese | |||||||
| Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | |
| Total number of patients (n=51,149) | 421 | 0.82% | 10,199 | 19.94% | 17,425 | 34.07% | 19,233 | 37.60% | 3,333 | 6.52% | 538 | 1.05% |
| Age | Median: 54 | IQR: 46–63 | Median: 53 | IQR: 45–61 | Median: 53 | IQR: 46–62 | Median: 53 | IQR: 46–61 | Median: 52 | IQR: 45–60 | Median: 51 | IQR: 43–57 |
| ≤ 40 | 57 | 13.54% | 1,364 | 13.37% | 1,939 | 11.13% | 1,931 | 10.04% | 351 | 10.53% | 74 | 13.75% |
| 41–50 | 90 | 21.38% | 2,608 | 25.57% | 4,376 | 25.11% | 5,076 | 26.39% | 963 | 28.89% | 166 | 30.86% |
| 51–60 | 137 | 32.54% | 3,238 | 31.75% | 5,655 | 32.45% | 6,378 | 33.16% | 1,150 | 34.50% | 207 | 38.48% |
| 61–70 | 74 | 17.58% | 1,943 | 19.05% | 3,634 | 20.86% | 4,183 | 21.75% | 96 | 2.88% | 73 | 13.57% |
| 71–80 | 48 | 11.40% | 869 | 8.52% | 1,516 | 8.70% | 1,492 | 7.76% | 160 | 4.80% | 16 | 2.97% |
| > 80 | 15 | 3.56% | 177 | 1.74% | 305 | 1.75% | 173 | 0.90% | 13 | 0.39% | 2 | 0.37% |
| Sex | ||||||||||||
| Male | 111 | 26.37% | 3,961 | 38.84% | 9,895 | 56.79% | 10,012 | 52.06% | 1,167 | 35.01% | 171 | 31.78% |
| Female | 310 | 73.63% | 6,238 | 61.16% | 7,530 | 43.21% | 9,221 | 47.94% | 2,166 | 64.99% | 367 | 68.22% |
| Functional status prior to surgery | ||||||||||||
| Independent | 395 | 93.82% | 10,015 | 98.20% | 17,205 | 98.74% | 18,956 | 98.56% | 3,252 | 97.57% | 517 | 96.10% |
| Partially/Totally Dependent | 26 | 6.18% | 184 | 1.80% | 220 | 1.26% | 277 | 1.44% | 81 | 2.43% | 21 | 3.90% |
| ASA | Median: 2 | IQR: 2–3 | Median: 2 | IQR: 2–3 | Median: 2 | IQR: 2–3 | Median: 2 | IQR: 2–3 | Median: 3 | IQR: 2–3 | Median: 3 | IQR: 3–3 |
| 1 | 16 | 3.80% | 727 | 7.13% | 1,045 | 6.00% | 489 | 2.54% | 15 | 0.45% | 2 | 0.37% |
| 2 | 223 | 52.97% | 6,429 | 63.04% | 10,850 | 62.27% | 10,055 | 52.28% | 886 | 26.58% | 103 | 19.14% |
| 3 | 175 | 41.57% | 2,920 | 28.63% | 5,311 | 30.48% | 8,377 | 43.56% | 2,317 | 69.52% | 366 | 68.03% |
| 4+ | 7 | 1.66% | 123 | 1.21% | 219 | 1.26% | 312 | 1.62% | 115 | 3.45% | 67 | 12.45% |
| Smoker | ||||||||||||
| No | 222 | 52.73% | 6,468 | 63.42% | 12,448 | 71.44% | 14,463 | 75.20% | 2,677 | 80.32% | 434 | 80.67% |
| Yes | 199 | 47.27% | 3,731 | 36.58% | 4,977 | 28.56% | 4,770 | 24.80% | 656 | 19.68% | 104 | 19.33% |
| Diabetes mellitus | ||||||||||||
| No diabetes mellitus | 404 | 95.96% | 9,606 | 94.19% | 15,490 | 88.90% | 15,440 | 80.28% | 2,318 | 69.55% | 337 | 62.64% |
| Noninsulin-dependent diabetes mellitus | 8 | 1.90% | 355 | 3.48% | 1,247 | 7.16% | 2,438 | 12.68% | 591 | 17.73% | 117 | 21.75% |
| Insulin-dependent diabetes mellitus | 8 | 1.90% | 221 | 2.17% | 642 | 3.68% | 1,254 | 6.52% | 403 | 12.09% | 81 | 15.06% |
| Number of spine levels involved | ||||||||||||
| 1 | 305 | 72.45% | 7,096 | 69.58% | 11,795 | 67.69% | 12,933 | 67.24% | 2,247 | 67.42% | 372 | 69.14% |
| 2 | 99 | 23.52% | 2,733 | 26.80% | 4,919 | 28.23% | 5,560 | 28.91% | 964 | 28.92% | 48 | 8.92% |
| 3 | 17 | 4.04% | 370 | 3.63% | 711 | 4.08% | 740 | 3.85% | 122 | 3.66% | 18 | 3.35% |
= Chi-square statistically significant at p<.05.
IQR, interquartile range.
Notably, partial/total functional dependency was more common at both extremes of the BMI range (underweight: 6.2%, morbidly obese: 2.4%, super morbidly obese: 3.9%) and smoking prevalence declined as BMI increased, dropping from 47.3% among underweight patients to 19.3% among the super morbidly obese. In contrast, the risk of diabetes, showed a stepwise increase, rising from 1.9% of underweight patients with both insulin-dependent and noninsulin-dependent diabetes mellitus to 15.1% of super morbidly obese patients with insulin-dependent diabetes and 21.8% of super morbidly obese patients with noninsulin-dependent diabetes.
Thirty-day postoperative adverse outcome data is shown in Table 2. Overall, 2.65% (n=1,353) of patients experienced ≥1 adverse event (AAE), 1.63% (n=833) experienced a serious adverse event, and 1.44% (n=736) experienced a minor adverse event. In addition, 1.42% (n=728) experienced postoperative infections, 2.49% (n=1,274) were readmitted, and 0.16% (n=83) died within 30 days of operation.
Table 2.
Number of adverse events, infection, readmissions and mortality for patients of varying body mass index (BMI)
| BMI<18.5 kg/m2 | BMI 18.5–24.9 kg/m2 | BMI 25.0–29.9 kg/m2 | BMI 30.0–39.9 kg/m2 | BMI 40.0–49.9 kg/m2 | BMI ≥ 50.0 kg/m2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight | Normal weight | Overweight | Obese | Morbidly obese | Super morbidly obese | |||||||
| Total number of patients (n=51,149) | n=421 | n=10,199 | n=17,425 | n=19,233 | n=3,333 | n=538 | ||||||
| Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | |
| Any adverse event (AAE) | 23 | 5.46% | 277 | 2.72% | 429 | 2.46% | 497 | 2.58% | 97 | 2.91% | 30 | 5.58% |
| Serious adverse event (SAE) | 16 | 3.80% | 176 | 1.73% | 272 | 1.56% | 289 | 1.50% | 62 | 1.86% | 18 | 3.35% |
| Deep infection | 3 | 0.71% | 36 | 0.35% | 58 | 0.33% | 61 | 0.32% | 12 | 0.36% | 3 | 0.56% |
| Sepsis | 3 | 0.71% | 37 | 0.36% | 51 | 0.29% | 40 | 0.21% | 7 | 0.21% | 3 | 0.56% |
| Failure to wean | 3 | 0.71% | 54 | 0.53% | 63 | 0.36% | 61 | 0.32% | 13 | 0.39% | 5 | 0.93% |
| Reintubation | 11 | 2.61% | 64 | 0.63% | 78 | 0.45% | 84 | 0.44% | 17 | 0.51% | 2 | 0.37% |
| Renal failure | 0 | 0.00% | 6 | 0.06% | 2 | 0.01% | 6 | 0.03% | 2 | 0.06% | 1 | 0.19% |
| Thromboembolic events | 1 | 0.24% | 32 | 0.31% | 61 | 0.35% | 80 | 0.42% | 16 | 0.48% | 4 | 0.74% |
| Cardiac arrest | 2 | 0.48% | 12 | 0.12% | 27 | 0.15% | 15 | 0.08% | 5 | 0.15% | 2 | 0.37% |
| MI | 1 | 0.24% | 11 | 0.11% | 21 | 0.12% | 23 | 0.12% | 4 | 0.12% | 2 | 0.37% |
| Stroke | 1 | 0.24% | 14 | 0.14% | 17 | 0.10% | 13 | 0.07% | 2 | 0.06% | 1 | 0.19% |
| Minor adverse event (MAE) | 12 | 2.85% | 158 | 1.55% | 230 | 1.32% | 267 | 1.39% | 50 | 1.50% | 19 | 3.53% |
| Superficial infection | 1 | 0.24% | 34 | 0.33% | 44 | 0.25% | 77 | 0.40% | 15 | 0.45% | 4 | 0.74% |
| Dehiscence | 0 | 0.00% | 9 | 0.09% | 10 | 0.06% | 12 | 0.06% | 4 | 0.12% | 1 | 0.19% |
| Pneumonia | 8 | 1.90% | 72 | 0.71% | 102 | 0.59% | 102 | 0.53% | 22 | 0.66% | 5 | 0.93% |
| UTI | 5 | 1.19% | 48 | 0.47% | 80 | 0.46% | 82 | 0.43% | 12 | 0.36% | 10 | 1.86% |
| Post renal insufficiency | 0 | 0.00% | 3 | 0.03% | 5 | 0.03% | 6 | 0.03% | 1 | 0.03% | 0 | 0.00% |
| Postoperative infections | 12 | 2.85% | 151 | 1.48% | 229 | 1.31% | 273 | 1.42% | 47 | 1.41% | 16 | 2.97% |
| Readmission within 30 d of operation ‡ | 15 | 3.56% | 241 | 2.36% | 407 | 2.34% | 496 | 2.58% | 95 | 2.85% | 20 | 3.72% |
| Mortality within 30 d of operation | 3 | 0.71% | 24 | 0.24% | 23 | 0.13% | 22 | 0.11% | 7 | 0.21% | 4 | 0.74% |
| Median | ±SD | Median | ±SD | Median | ±SD | Median | ±SD | Median | ±SD | Median | ±SD | |
| Length of stay (d) | 1 | 1–2 | 1 | 1–2 | 1 | 1–2 | 1 | 1–2 | 1 | 1–2 | 1 | 1–2 |
| Operative time (min) | 112 | 77–167 | 109 | 79–153 | 112 | 81–156 | 114 | 82–160 | 115 | 85–162 | 121 | 86–171 |
IQR, inter quartile range.
Relative to normal weight patients, the incidence of AAE was elevated in underweight patients (5.46% versus 2.72%). Similarly, super morbidly obese patients also exhibited higher incidence of AAE (5.58% versus 2.72%) while morbidly obese patients had a milder increase of AAE (2.91% vs 2.72%). Overweight, obese, in contrast, had a lower incidence relative to normal weight patients suggestive of fewer adverse events (2.46% and 2.58%, respectively). Further, underweight and super morbidly obese patients exhibited elevated incidence of over half of all variables investigated relative to normal weight patients. Of note, length of stay and operative time was similar across the six categories.
Univariate analyses
Univariate analyses (Table 3) found underweight patients being 2.07 times more likely to experience AAE (p=.001), 2.25 times more likely to experience SAE (p=.002), 1.86 times more likely to experience MAE (p=.040), and 1.95 times more likely to develop postoperative infections (p=.028). This underweight population was not statistically more likely to be readmitted to the hospital within 30 days of the operation (p=.118) or experience mortality within 30 days of the operation (p=.070). Statistically significant increases in odds ratios of adverse outcomes were also found for the super morbidly obese patients including being 2.12 times more likely to experience AAE (p<.001), 1.97 times more likely to experience SAE (p=.007), 2.33 times more likely to experience MAE (p=.001), and 1.60 times more likely to be readmitted within 30 postoperative days (p=.049).
Table 3.
Univariable odds ratio for adverse events, infection, readmissions and mortality for patients of varying body mass index (BMI)
| BMI 25.0–29.9 kg/m2 | BMI 30.0–39.9 kg/m2 | BMI 40.0–49.9 kg/m2 | BMI ≥ 50.0 kg/m2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight | Normal weight | Overweight | Obese | Morbidly obese | Super morbidly obese | |||||||
| Total number of patients (n=51,149) | n=421 | n=10,199 | n=17,425 | n=19,233 | n=3,333 | n=538 | ||||||
| Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | |
| Any adverse event (AAE) | 2.07 | .001 | 1 | – | 0.90 | .197 | 0.95 | .501 | 1.07 | .552 | 2.12 | <.001 |
| Serious adverse event (SAE) | 2.25 | .002 | 1 | – | 0.90 | .296 | 0.87 | .145 | 1.08 | .608 | 1.97 | .007 |
| Minor adverse event (MAE) | 1.86 | .040 | 1 | – | 0.85 | .119 | 0.90 | .271 | 0.97 | .842 | 2.33 | .001 |
| Postoperative infections | 1.95 | .028 | 1 | – | 0.89 | .252 | 0.96 | .676 | 0.95 | .769 | 2.04 | .008 |
| Readmission within 30 d of operation | 1.53 | .118 | 1 | – | 0.99 | .885 | 1.09 | .259 | 1.21 | .117 | 1.60 | .049 |
| Mortality within 30 d of operation | 3.04 | .070 | 1 | – | 0.56 | .047 | 0.49 | .014 | 0.89 | .791 | 3.18 | .033 |
Bolding indicates statistical significance at p<.05.
Further univariate analyses found in obese patients had reduced odds of mortality within 30-postoperative days when compared with normal weight patients (OR-0.49, p=.014). These findings suggest an increased risk of adverse outcomes among patients at the extremes of BMI (underweight and super morbidly obese) relative to patients who are overweight or obese.
Figs. 2 and 3 display histograms of patient BMI which were then overlaid with adverse event data. This data was normalized to the risk of both adverse events (Fig. 2) and binomial outcomes (Fig. 3) of normal weight patients (BMI 18.5–24.9 kg/m2). The data was converted to a moving average using 1 BMI group increments to reduce granularity and noise of the data.
Multivariate analyses
Given preoperative differences in patient characteristics across the BMI spectrum, multivariable logistic regression analyses controlling for age, sex, BMI, preoperative functional status, and ASA class were performed. The results of these analyses are shown in Table 4 and Fig. 4. After controlling for these preoperative factors, underweight patients were still 1.62 times more likely to experience AAE (p=.036), 1.74 times more like to experience SAE (p=.044), and 1.75 times more likely to develop postoperative infections (p<.019). Super morbidly obese patients were 1.55 times more likely experience AAE (p=.032) and 1.72 times more like to experience MAE (p=.034). Conversely, obese patients continued to show reduced odds of AAE, SAE, postoperative infections and mortality within 30 days. Overweight patients were also significantly less likely to die within 30 days of the operation (OR=0.49, p=.017) and morbidly obese patients were significantly less likely to have postoperative infections (OR=0.67, p=.009). Overall, these data again suggest an increased risk of adverse outcomes among patients at the extremes of the BMI range relative to overweight to obese patients.
Table 4.
Multivariable *odds ratio for adverse events, infection, readmissions and mortality for patients of varying body mass index (BMI)
| BMI 25.0–29.9 kg/m2 | BMI 30.0–39.9 kg/m2 | BMI 40.0–49.9 kg/m2 | BMI ≥ 50.0 kg/m2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Underweight | Normal weight | Overweight | Obese | Morbidly obese | Super morbidly obese | |||||||
| Total number of patients (n=51,149) | n=421 | n=10,199 | n=17,425 | n=19,233 | n=3,333 | n=538 | ||||||
| Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | Odds ratio | *p Value | |
| Any adverse event (AAE) | 1.62 | .036 | 1.00 | – | 0.87 | .089 | 0.85 | .038 | 0.84 | .152 | 1.55 | .032 |
| Serious adverse event (SAE) | 1.74 | .044 | 1.00 | – | 0.84 | .087 | 0.76 | .005 | 0.86 | .312 | 1.45 | .157 |
| Minor adverse event (MAE) | 1.37 | .305 | 1.00 | – | 0.85 | .128 | 0.82 | .058 | 0.74 | .079 | 1.72 | .034 |
| Postoperative infections | 1.75 | .019 | 1.00 | – | 0.88 | .159 | 0.79 | .020 | 0.67 | .009 | 0.97 | .907 |
| Readmission within 30 d of operation | 1.32 | .308 | 1.00 | – | 0.94 | .431 | 0.94 | .432 | 0.91 | .450 | 1.17 | .513 |
| Mortality within 30 d of operation | 2.05 | .257 | 1.00 | – | 0.49 | .017 | 0.42 | .005 | 0.80 | .609 | 2.39 | .134 |
Regression controlled for all patient demographics including age, gender, functional status, number of levels involved, and ASA class.Bolding indicates statistical significance at p<.05.
Fig. 4.
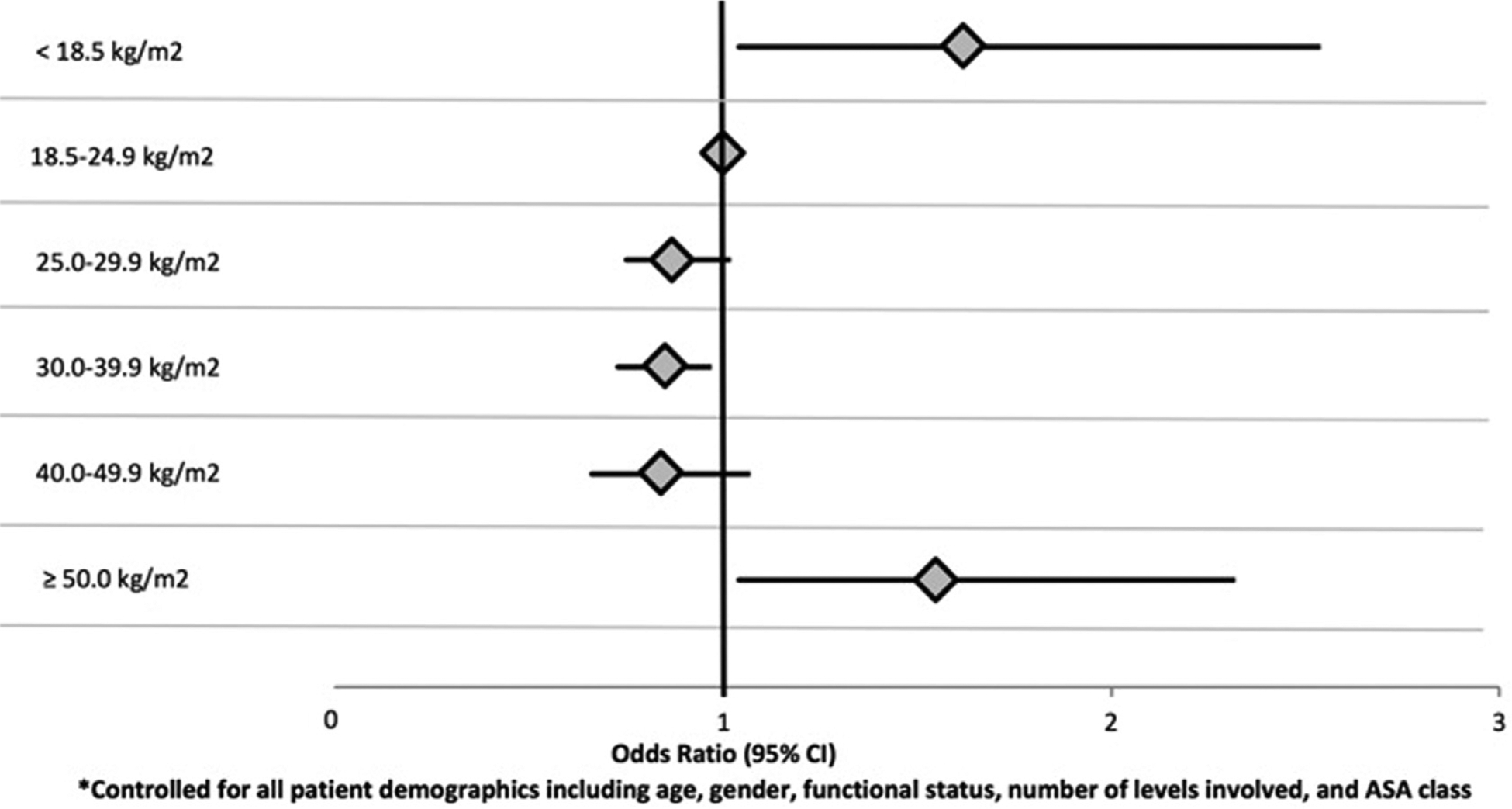
Multivariate odds ratio of experiencing any adverse event for patients of varying body mass index (BMI) following an anterior cervical procedure.
Discussion
Although the effect of obesity on surgical outcomes following anterior cervical spine surgery has been studied, there is a paucity of literature assessing the postoperative outcomes across the entire BMI spectrum. The current study thus evaluated the association of all World Health Organization BMI categories for patients undergoing such surgery with postoperative adverse outcomes. Relative to normal weight patients, underweight patients were identified as an at-risk group for AAE, serious adverse event and postoperative infections, even more than any other BMI category including super morbidly obese patients. Conversely, obese and morbidly obese patients had a lower risk of certain defined adverse postoperative outcomes.
Low BMI patients have been studied previously in non-spine surgery populations. For example, Benjamin et al. evaluated patients undergoing emergency abdominal operations and found that underweight patients had increased morbidity and mortality when compared with those of normal BMI [24]. Additionally, a systematic review of complications following vascular surgery by Galyfos et al. found underweight patients had higher mortality rates and respiratory morbidity rates compared with normal BMI patients [8]. Regarding spine studies, one prior lumbar study performed by Bono et al. included a low BMI group, but did not find low BMI patients to be at greater risk of adverse outcomes [25]. In another spine study, Tarrant et al. showed low BMI patients undergoing surgery for adolescent idiopathic scoliosis had increased risk postoperative ileus [26]. However, identification of patients undergoing anterior cervical procedures with low BMI as an at-risk category has not been previously evaluated in the cervical spine literature to our knowledge.
For overweight and obese patients, the prior orthopedic literature has been mixed, as noted in the introduction. For example, Auffinger et al. found those with BMI>30 kg/m2 had worse clinical outcomes 6 months postoperatively when undergoing elective anterior or posterior cervical spine surgery for degenerative pathology [12]. Conversely, Narain et al. found that those with class I and II obesity (BMI>35.0 kg/m2) undergoing anterior cervical discectomy and fusion had equivalent surgical outcomes, narcotic consumption and hospital costs relative to nonobese patients [14].
The current study found no increased risks for the overweight and mildly to morbidly obese patients, and in fact a protective effect against some of the adverse outcomes. This has been shown in literature of other surgical fields. Studies in emergency abdominal operations, [24] drug-eluting stents [27], and vascular surgery patients [8], all exhibited lower rates of various complications in this population. Although it is poorly understood why some degree of increased BMI may be associated with some protective effect, the “obesity paradox” has been suggested due to the effect of increased stress and release of cytokines exerted on the body from extra weight [28]. This may cause changes in the immune system not seen in patients without this. The addended inherent stress this places the body may put it into a state of defense, which persistently stimulates the immune system enabling the patient to be better prepared to cope with the physical insult of surgical intervention and various adverse events [29–31].
While overweight, obesity, and morbidly obese showed no effect or a protective effect, super morbidly obese patients were found to be associated with increased risk of AAEs and minor adverse events. Similar to underweight patients, super morbidly obese patients have also received less attention in the spine literature and have rarely been studied as a group. However, when considering the effect of BMI on outcomes, it is important to consider such categories of BMI as health status and the effect of elevated weight on patient outcomes cannot be assumed to be the same for a patient with BMI of 30.0 kg/m2 and a patient with a BMI of 50.0 kg/m2. Variation in conclusions of past studies may be due to these differences in BMI category definitions (such as aggregating all obese patients as BMI>30.0 kg/m2 without differentiating).
There are limitations to the current study. The NSQIP database only provides data on 30-day postoperative outcomes, so complications that occur after this time point would not be reflected the analysis. Additionally, the dataset lacks spine specific outcome variables such as dysphagia, patient reported outcomes, and fusion rate. Lastly, due to the nature of the NSQIP database, we were unable to directly investigate specific disease patterns and thus chose procedures based on CPT code to fulfill that role. While we know this is not a perfect comparison, we have done our best to control for all other comorbidities and health status and stove to be true to the data. We acknowledge this approach may impact findings, however, the outcomes of radiculopathy or myopathy could be due to stenosis or disc disease in origin, thus it is not feasible to separate based on only one listed code. As a result, we chose to focus on CPT guided procedures but acknowledge the potential impact diagnosis may have on complications independent of procedure. Despite these limitations there are many strengths to the presented data. The large number of patients with abstracted data provides substantial power to analyze groups that have not previously received attention.
Overall, the current study evaluated 51,149 patients undergoing anterior cervical spine patients and identified those at the extremes of the BMI spectrum (underweight with BMI<18.5 kg/m2 and super morbidly obese with BMI>50 kg/m2) to be at the greatest risk for postoperative adverse outcomes. While it has become relatively accepted that there are risks associated with being particularly obese, the underweight category has previously received less attention. Such underweight patients could suffer from a variety of underlying medical and nutritional problems, vitamin deficiencies / alcoholism, etc. which place them at risk. Additional attention should be given to this patient population through preoperative medical and laboratory workup to identify and potentially treat reversible nutritional and metabolic problems. Meanwhile, for obese patients, the presented data allows surgeons to provide specific preoperative counseling depending on the severity of obesity.
Acknowledgment
No conflicts of interest or external sources of funding for this study are reported.
Footnotes
Author disclosures: TDO: Nothing to disclose. RM: Nothing to disclose. ARG: Nothing to disclose. CKZ: Nothing to disclose. AGV: Nothing to disclose. JNG: Consulting, Bioventus; TIDI Products (B); Stryker (B). Board of Directors: North American Spine Society (B).
References
- [1].Marawar S, Girardi FP, Sama AA, Ma Y, Gaber-Baylis LK, Besculides MC, et al. National trends in anterior cervical fusion procedures. Spine (Phila Pa 1976) 2010;35(15):1454–9. [DOI] [PubMed] [Google Scholar]
- [2].McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus 2015;39(6):E9. [DOI] [PubMed] [Google Scholar]
- [3].Flippin M, Harris J, Paxton EW, Prentice HA, Fithian DC, Ward SR, et al. Effect of body mass index on patient outcomes of surgical intervention for the lumbar spine. J Spine Surg 2017;3(3):349–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine 2007;6(4):291–7. [DOI] [PubMed] [Google Scholar]
- [5].Buerba RA, Fu MC, Grauer JN. Anterior and posterior cervical fusion in patients with high body mass index are not associated with greater complications. Spine J 2014;14(8):1643–53. [DOI] [PubMed] [Google Scholar]
- [6].Meller MM, Toossi N, Gonzalez MH, Son MS, Lau EC, Johanson N. Surgical risks and costs of care are greater in patients who are super obese and undergoing THA. Clin Orthop Relat Res 2016;474 (11):2472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Meller MM, Toossi N, Johanson NA, Gonzalez MH, Son MS, Lau EC. Risk and cost of 90-day complications in morbidly and superobese patients after total knee arthroplasty. J Arthroplasty 2016;31 (10):2091–8. [DOI] [PubMed] [Google Scholar]
- [8].Galyfos G, Geropapas GI, Kerasidis S, Sianou A, Sigala F, Filis K. The effect of body mass index on major outcomes after vascular surgery. J Vasc Surg 2017;65(4):1193–207. [DOI] [PubMed] [Google Scholar]
- [9].Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England) 2014;384(9945):766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine (Phila Pa 1976) 2012;37(11):982–8. [DOI] [PubMed] [Google Scholar]
- [11].Minhas SV, Chow I, Jenkins TJ, Dhingra B, Patel AA. Preoperative predictors of increased hospital costs in elective anterior cervical fusions: a single-institution analysis of 1,082 patients. Spine J 2015;15(5):841–8. [DOI] [PubMed] [Google Scholar]
- [12].Auffinger B, Lam S, Kraninger J, Shen J, Roitberg BZ. The impact of obesity on surgeon ratings and patient-reported outcome measures after degenerative cervical spine disease surgery. World Neurosurg 2014;82(1–2):e345–52. [DOI] [PubMed] [Google Scholar]
- [13].Mehta AI, Babu R, Sharma R, Karikari IO, Grunch BH, Owens TR, et al. Thickness of subcutaneous fat as a risk factor for infection in cervical spine fusion surgery. J Bone Joint SurgAm Vol 2013;95 (4):323–8. [DOI] [PubMed] [Google Scholar]
- [14].Narain AS, Hijji FY, Haws BE, Kudaravalli KT, Yom KH, Markowitz J, et al. Impact of body mass index on surgical outcomes, narcotics consumption, and hospital costs following anterior cervical discectomy and fusion. J Neurosurg Spine 2017:1–7. [DOI] [PubMed] [Google Scholar]
- [15].Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY. The effect of obesity on clinical outcomes after lumbar fusion. Spine (Phila Pa 1976) 2008;33(16):1789–92. [DOI] [PubMed] [Google Scholar]
- [16].Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976) 2009;34(5):495–500. [DOI] [PubMed] [Google Scholar]
- [17].McClendon J Jr, Smith TR, Thompson SE, Sugrue PA, O’Shaughnessy BA, Ondra SL, et al. The impact of body mass index on hospital stay and complications after spinal fusion. Neurosurgery 2014;74(1):42–50. discussion. [DOI] [PubMed] [Google Scholar]
- [18].ACS-NSQIP. User guide for the 2015 ACS NSQIP participant use data file (PUF). Chicago, IL; 20152015 [02/26/2017]; Available from:https://www.facs.org/~/media/files/quality%20programs/bariatric/mbsaqip_2015_puf_user_guide.ashx. [Google Scholar]
- [19].Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA Jr, et al. Successful implementation of the department of veterans affairs’ national surgical quality improvement program in the private sector: the patient safety in surgery study. Ann Surg 2008;248 (2):329–36. [DOI] [PubMed] [Google Scholar]
- [20].Ottesen TD, Zogg CK, Haynes MS, Malpani R, Bellamkonda KS, Grauer JN. Dialysis patients undergoing total knee arthroplasty have significantly increased odds of perioperative adverse events independent of demographic and comorbidity factors. J Arthroplasty 2018. [DOI] [PubMed] [Google Scholar]
- [21].Duchman KR, Gao Y, Pugely AJ, Martin CT, Callaghan JJ. Differences in short-term complications between unicompartmental and total knee arthroplasty: a propensity score matched analysis. J Bone Joint Surg Am 2014;96(16):1387–94. [DOI] [PubMed] [Google Scholar]
- [22].Bovonratwet P, Webb ML, Ondeck NT, Lukasiewicz AM, Cui JJ, McLynn RP, et al. Definitional differences of ‘outpatient’ versus ‘inpatient’ THA and TKA can affect study outcomes. Clin Orthop Relat Res 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ottesen TD, McLynn RP, Zogg CK, Shultz BN, Ondeck NT, Bovonratwet P, et al. Dialysis is an independent risk factor for perioperative adverse events, readmission, reoperation and mortality for patients undergoing elective spine surgery. Spine J 2018. [DOI] [PubMed] [Google Scholar]
- [24].Benjamin ER, Dilektasli E, Haltmeier T, Beale E, Inaba K, Demetriades D. The effects of body mass index on complications and mortality after emergency abdominal operations: the obesity paradox. Am J Surg 2017;214(5):899–903. [DOI] [PubMed] [Google Scholar]
- [25].Bono OJ, Poorman GW, Foster N, Jalai CM, Horn SR, Oren J, et al. Body mass index predicts risk of complications in lumbar spine surgery based on surgical invasiveness. Spine J 2017. [DOI] [PubMed] [Google Scholar]
- [26].Tarrant RC, Lynch S, Sheeran P, O’Loughlin PF, Harrington M, Moore DP, et al. Low body mass index in adolescent idiopathic scoliosis: relationship with pre- and postsurgical factors. Spine (Phila Pa 1976) 2014;39(2):140–8. [DOI] [PubMed] [Google Scholar]
- [27].Faggioni M, Baber U, Afshar AE, Giustino G, Sartori S, Sorrentino S, et al. Effects of body mass index on clinical outcomes in female patients undergoing percutaneous coronary intervention with drug-eluting stents: results from a patient-level pooled analysis of randomized controlled trials. JACC Cardiovasc Interv 2018;11(1):68–76. [DOI] [PubMed] [Google Scholar]
- [28].Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Annals Surg 2009;250(1):166–72. [DOI] [PubMed] [Google Scholar]
- [29].Iyer A, Fairlie DP, Prins JB, Hammock BD, Brown L. Inflammatory lipid mediators in adipocyte function and obesity. Nat Rev Endocrinol 2010;6(2):71–82. [DOI] [PubMed] [Google Scholar]
- [30].Mungo B, Zogg CK, Hooker CM, Yang SC, Battafarano RJ, Brock MV, et al. Does obesity affect the outcomes of pulmonary resections for lung cancer? A national surgical quality improvement program analysis. Surgery 2015;157(4):792–800. [DOI] [PubMed] [Google Scholar]
- [31].Zogg CK, Mungo B, Lidor AO, Stem M, Rios Diaz AJ, Haider AH, et al. Influence of body mass index on outcomes after major resection for cancer. Surgery 2015;158(2):472–85. [DOI] [PubMed] [Google Scholar]
- [32].Ottesen TD, McLynn RP, Galivanche AR, Bagi PS, Zogg CK, Rubin LE, et al. Increased complications in geriatric patients with a fracture of the hip whose postoperative weight-bearing is restricted: an analysis of 4918 patients. The Bone & Joint Journal 2018;100–b (10):1377–84. In press. 10.1302/0301-620x.100b10.Bjj-2018-0489.R1. [DOI] [PubMed] [Google Scholar]
- [33].Ottesen TD, Yurter A, Shultz BN, Galivanche AR, Zogg CK, Bovonratwet P, et al. Dialysis Dependence Is Associated With Significantly Increased Odds of Perioperative Adverse Events After Geriatric Hip Fracture Surgery Even After Controlling for Demographic Factors and Comorbidities. J Am Acad Orthop Surg Glob Res Rev 2019;3 (8):e086 In press. 10.5435/JAAOSGlobal-D-19-00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ottesen TD, Zogg CK, Haynes MS, Malpani R, Bellamkonda KS, Grauer JN. Dialysis Patients Undergoing Total Knee Arthroplasty Have Significantly Increased Odds of Perioperative Adverse Events Independent of Demographic and Comorbidity Factors. The Journal of Arthroplasty 2018;33(9):2827–34. In press. 10.1016/j.arth.2018.04.012. [DOI] [PubMed] [Google Scholar]


