Abstract
Background
Neonatal resuscitation is a life-saving intervention for birth asphyxia, a leading cause of neonatal mortality. Worldwide, four million neonate deaths happen annually, and birth asphyxia accounts for one million deaths. Improving providers’ neonatal resuscitation skills is critical for delivering quality care and for morbidity and mortality reduction. However, retention of these skills has been challenging in developing countries, including Ethiopia. Hence, this study aimed to assess neonatal resuscitation skills retention and associated factors among midwives and nurses in Eastern Ethiopia.
Methods
An institution-based cross-sectional study was conducted using a pre-tested, structured, observational checklist. A total of 427 midwives and nurses were included from 28 public health facilities by cluster sampling and simple random sampling methods. Data were collected on facility type, availability of essential resuscitation equipment, socio-demographic characteristics of participants, current working unit, years of professional experience, whether a nurse or midwife received refresher training, and skills and knowledge related to neonatal resuscitation. Binary logistic regression was used to analyse the association between neonatal resuscitation skill retention and independent variables.
Results
About 11.2% of nurses and midwives were found to have retention of neonatal resuscitation skills. Being a midwife (AOR, 7.39 [95% CI: 2.25, 24.24]), ever performing neonatal resuscitation (AOR, 3.33 [95% CI: 1.09, 10.15]), bachelor sciences degree or above (AOR, 4.21 [95% CI: 1.60, 11.00]), and good knowledge of neonatal resuscitation (AOR, 3.31 [95% CI: 1.41, 7.73]) were significantly associated with skill retention of midwives and nurses.
Conclusion
Basic neonatal resuscitation skills of midwives and nurses in Eastern Ethiopia are not well retained. This could increase the death of neonates due to asphyxia. Being a midwife, Bachelor Sciences degree or above educational status, ever performing neonatal resuscitation, and good knowledge were associated with skill retention. Providers should be encouraged to upgrade their educational level to build their skill retention and expose themselves to NR. Further, understanding factors affecting how midwives and nurses gain and retain skills using high-level methodology are essential.
Introduction
Worldwide, 136 million babies are born annually. Ten million require some stimulation at birth to breathe, while six million require basic resuscitation with a bag and mask [1,2]. Evidence shows that one million neonatal deaths occur on the day of birth per year. Close to two million babies die in the first week of life and four million dies in the neonatal period [3–5], which accounts for 46% of under-five mortality [6–8]. This mortality is estimated to increase to 52% in 2030 [9,10], unless strategic interventions are implemented. Surprisingly, about 99% of neonatal deaths occur in low-income and middle-income countries [1]. Unfortunately, four million neonates experience birth asphyxia and one million deaths are caused by birth asphyxia annually [11–18], while resuscitation at birth can prevent a large proportion of mortality [11,19].
Neonatal resuscitation (NR) is a crucial intervention for birth asphyxia [20]. In low- income and middle-income countries, facility-based NR may avert 30% of intrapartum-related neonatal deaths [3,21]. NR training for health workers potentially prevents many neonatal deaths currently misclassified as still births [22]. NR with a bag and mask is a high-impact intervention that can reduce neonatal deaths in resource-limited countries [23].
The burden of neonatal death is particularly severe in sub-Saharan Africa, including Ethiopia, which suffers from a current neonatal mortality rate of 29 deaths per 1000 live births annually [1,2,24,25]. To provide effective resuscitation, care providers should apply detailed information and employ their technical skills competently. Therefore, those who perform resuscitation, nurses and midwives are expected to be competent and have the required knowledge and skills. These skills should be learned through training during their academic courses. Despite the time, resources, and expenses allocated to such training, little is known about the outcomes of these educational programs and whether students’ educational needs are met.
Simulation-based assessment of NR skills to identify providers' strengths and weaknesses is a less costly and more practical alternative to direct observation of actual NR [23]. The delivery of effective, safe, and good quality health services is essential interventions to improving maternal, newborn, and child health. Skill retention has paramount importance to improving quality service delivery [26].
Moreover, to achieve sustainable development goals (SDG) in 2030, all countries should reduce neonatal mortality to 12 per 1,000 live births and under 5 mortality to at least as low as 25 per 1,000 live births [27]. Retention of NR skills is of crucial importance, along with access to basic equipment to save the life of millions of newborns [23,28,29]. However, maintaining NR skills presents a different set of challenges, particularly in settings where providers attend few deliveries, infrequently resuscitate newborns, and have limited access to refresher training in resource-scarce settings, including Ethiopia. Available evidence indicates that the rapid loss of NR skills occurs after an initial training [21,28,30–33].
Midwives and nurses are healthcare providers who are able to provide promotive, preventive, curative, and rehabilitative services at all levels of the health care system. Midwifery and nursing training in Ethiopia offered in both public and private per the ministry of science and higher education requirement: the diploma, post-basic, direct Bachelor of Sciences (BSc) degree, MSc degree, and PhD level in both qualifications. Since nursing professionals are assigned to all units of the health facility, their education focuses on all medical care. Even if midwives take all medical care education, lastly they focus on maternal and neonatal care. In addition to these, some midwives and nurses take in-service training that can help them to give quality care at where they are assigned. Therefore, both midwives and nurses have access to managing critically ill newborns, midwives in the labor and delivery ward and nurses in delivery, neonatology, and pediatric ward.
NR skills are a key component of efforts to reduce neonatal morbidity and mortality. Although appropriate neonatal care programs are a current issue in Ethiopia, evidence on NR skill retention among midwives and nurses is scarce. Therefore, this study aimed to assess the magnitude of NR skills retention and associated factors among midwives and nurses in Eastern Ethiopia.
Materials and methods
Study setting and period
The study was conducted in Eastern Ethiopia, specifically in health care facilities from the Harari regional state, the Dire Dawa administration, and the Eastern and Western Harerghe zones from the Oromia regional states. In the included locations, there were an estimated 6,565,406 total population and 14 hospitals and 221 health centers with a total of 521 midwives and 2735 nurses working in all public health facilities in Eastern Ethiopia in November 2018.
Study design and participants
A facility-based cross-sectional study was conducted among midwives and nurses who were working in public health facilities and were employed for at least one year anywhere in the study area were included. A total of 437 midwives and nurses were expected to be included in the assessment. Of these, 10 midwives and nurses were not included because of different reasons (four participants refused the invitation and the remaining six participants were inaccessible because they were in annual leave at the time of the assessment. Therefore, the assessment was limited to 427 (97.7%) of midwives and nurses those completely addressed by the assessment team. The assessment team visited each facility for one to three days to collect data if the study participants were unavailable.
Sample size determination and sampling procedures
The sample size was determined using a single population proportion formula ( by considering the proportion of NR skill retention of healthcare providers (76.3%) [34], 95% confidence level z values of 1.96, a margin of error of 5%, and adding a 5% allowance for non-response. Since the study had two stages, we used a design effect of 1.5. The final sample size resulted in 437 study participants. We used a cluster-sampling method first, based on their geographic location and administration into the Dire Dawa Administration (desert/hot climate and urban), Harari regional state (urban and middle climate region), and East Hararghe and West Hararghe (rural with different geographic locations and administrations). Then, we selected a total of 10 hospitals and 18 health centers from those clusters using a simple random sampling method from the list of public health facilities. In addition, a simple random sampling (lottery) method and proportional allocation to size were used to enroll midwives and nurses from the selected facilities.
Data collection techniques
A structured questionnaire was adapted and modified from similar literatures. The knowledge questionnaire was based on model assessment forms in the Needs Assessment Toolkit (the Averting Maternal Death and Disability Program’s Needs Assessment toolkit) regarding steps providers should take during newborn resuscitation [23, 35–38]. Each knowledge question was designed to elicit multiple responses (25 expected responses). The tool was pre-tested and modified to suit the local context. The data collection procedure was undertaken using the pre-tested face-to-face interview administered questionnaire using paper-printed English version language. First, we interviewed facility directors and the study subjects about facility characteristics like the type of facility (hospital or health center), availability of essential NR equipment, current participants working unit, years of professional experience, refresher training status, and knowledge questions. Then, experts observed participants performing NR on an anatomical model and used an observational checklist (38-item skills tools) to rate their skill level [23, 39, 40].
Measurement of knowledge and skills
Knowledge of midwives and nurses on neonatal resuscitation was determined using a set of 25 objective questions. Each correct answer was valued at one point, and incorrect answer scored zero points. Questions not answered were considered incorrect answers. Eventually, participants were then grouped into two categories based on their total score on the knowledge scale: good knowledge (score 80% or higher) and poor knowledge (score less than 80%), which have been used in different studies after the overall cumulative mean score and the cumulative mean percentage score were calculated [37, 41–44].
Similar to knowledge measurement, the skill of midwives and nurses on neonatal resuscitation was determined using a set of 38 steps of the objective observational checklist. Each complete performed step was valued at one point, and an incomplete performed step/not performed steps was valued zero point. Eventually, participants were then grouped into two categories based on their total score on the skill scale, good retention of skill (score 80% or higher), and poor retention of skill (score less than 80%), after the overall cumulative mean score and the cumulative mean percentage score were calculated [41].
Data quality control and management
Three experts (midwifery department lecturers, one Master in neonatology and pediatrics, and two Master in maternity and neonatology) were trained for observation. Three interviewers (BSc degree in midwifery) and two Master of public health (MPH) supervisors received intensive training for three days about the purpose of the study, the sampling procedure, and observational skills. All were experienced service providers and had data collection experience in a maternal and neonatal related study. Before data collection, the principal investigators shared ethical issues and ways of addressing contingency management. The questionnaire was pre-tested on 5% (22 participants) of the sample size on a similar population other than the included facility (in one hospital and two health centers). Then, all completed questionnaires were checked for completeness and cleaned manually.
Data processing and analysis
The questionnaires were coded and entered into the EPI data version 3.1 statistical software and then exported to SPSS version 21 statistical software for analysis. Data were summarized and presented using descriptive statistics. The outcome variables were coded as “1” for having good retention whereas “0” for not having good retention. The association between the outcome variables (i.e., NR skill retention) and independent variables were analyzed using a binary logistic regression model. Covariates with a p-value<0.25 were retained and entered into the multivariable logistic regression analysis using a forward stepwise approach. The Hosmer and Lemeshow goodness-of-fit test was used to assess whether the necessary assumptions were fulfilled. The results are presented as odds ratios OR with 95% confidence intervals. An association with a p-value<0.05 was considered significant.
Ethical considerations
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee of Haramaya University in Ethiopia. Following the approval, an official letter of cooperation was given to the Region and City administration Health Bureaus, zonal and Woreda health offices, hospitals, and health center officials. Permission was obtained from each facility’s director prior to the study. The purpose and importance of the study were explained to the study participants and directors of the facilities. Overall, data were collected only after fully written informed consent was obtained from each participant. All findings were kept confidential. The names and addresses of the participants were not recorded in the questionnaire. Furthermore, all the basic principles of human research ethics (respect for persons, beneficence, voluntary participation, confidentiality, and justice) were respected.
Results
Sociodemographic characteristics of participants
A total of 427 study subjects participated, yielding a response rate of 97.7%. The mean (SD) age of participants was 28.4 (± 7.05). Two hundred fifty-eight (60.4%) were female and 245 (57.4%) were married. Two hundred (46.8%) were Orthodox Christian, 285 (66.7%) were nurses, and 292 (68.4%) had a bachelor sciences degree or above. Two hundred sixty-three (61.6) of them had 1–5 years of professional experience (Table 1).
Table 1. Sociodemographic characteristics of study participants among midwives and nurses working in public health facilities in Eastern Ethiopia, November 2018 (n = 427).
| Variables | Frequency (N) | Percent (%) |
|---|---|---|
| Age | ||
| 15–24 | 116 | 27.2 |
| 25–34 | 253 | 59.3 |
| 35–49 | 42 | 9.8 |
| 50–61 | 16 | 3.7 |
| Sex | ||
| Female | 258 | 60.4 |
| Male | 169 | 39.6 |
| Marital status | ||
| Never married | 171 | 40.0 |
| Married | 245 | 57.4 |
| Divorced/Separated | 11 | 2.6 |
| Religion | ||
| Orthodox Christian | 200 | 46.8 |
| Muslim | 179 | 42.0 |
| Protestant | 48 | 11.2 |
| Profession | ||
| Midwifery | 142 | 33.3 |
| Nurse | 285 | 66.7 |
| Professional education levels | ||
| Level IV diploma | 135 | 31.6 |
| BSc degree and above | 292 | 68.4 |
| Professional experience in years | ||
| 1–5 | 263 | 61.6 |
| 6–10 | 114 | 26.7 |
| ≥11 | 50 | 11.7 |
| Current working unit | ||
| Obstetrics & gynecology | 290 | 67.9 |
| Pediatrics & neonatal | 137 | 32.1 |
Training and work-related exposure
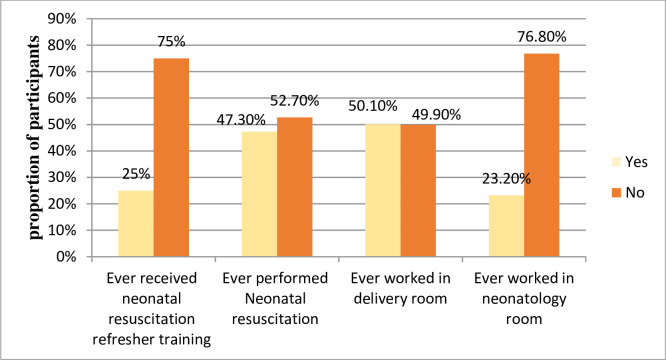
One hundred seven (25.1%) participants had ever taken NR refresher training and 202 (47.3%) had ever performed NR. About half (50.1%) of study subjects ever worked in the delivery room (Fig 1).
Fig 1. Refresher training and work-related exposure of midwives and nurses working in public health facilities in Eastern Ethiopia, November 2018 [n = 427].
Health facilities characteristics
According to the study, 127 (29.7%), 107 (25.1%), 99 (23.2%) and 94 (22%) study participants were from Dire Dawa city administration, Harari regional state, and Eastern and Western Hararghe zone respectively. Furthermore, 97.4%, 63% and 85% of health facilities had neonatal resuscitation corners (NR area), adequate newborn resuscitation guidelines, and essential equipment for newborn resuscitation, respectively. Regarding health care provision facilities, 333 (78%) midwives and nurses were from hospitals and the remaining 94 (22%) were from health centers.
The magnitude of neonatal resuscitation skill retention
Among participants in this study, only 48 (11.2%) 95% CI (8–14%) had good skill retention.
Factors associated with the neonatal resuscitation skill retention
In multivariate logistic analyses, being a midwife, having a BSc degree or above, ever performing NR, and having good knowledge of NR were independently associated with skill retention. Midwives were seven times more likely to retain NR skills (AOR, 7.39 [95% CI: 2.25, 24.25]) as compared to nurses. Those with a BSc degree and above were four times more likely to retain skills (AOR, 4.21 [95% CI: 1.60, 11.00]). Furthermore, participants who ever performed NR were three times more likely to retain NR skill (AOR, 3.33 [95% CI: 1.09, 10.15]), and those with good knowledge in NR (AOR, 3.31 [95% CI: 1.41, 7.73]) were three times more likely to retain their NR skill when compared with those with poor knowledge (Table 2).
Table 2. Factors associated with neonatal resuscitation skill retention among midwives and nurses working in public health facilities in Eastern Ethiopia, November 2018 (n = 427).
| Variables | NR skill retention | COR | AOR | p-value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Religion | |||||
| Orthodox Christian | 27(13.5) | 173(86.5) | 1 | ||
| Muslim | 18(10.1) | 161(89.9) | 0.72(0.38, 1.35) | 0.64(0.30, 1.34) | 0.23 |
| Protestant | 3(6.2) | 45(93.8) | 0.43(0.12, 1.47) | 0.44(0.11, 1.74) | 0.24 |
| Profession | |||||
| Nurse | 10(3.5) | 275(96.5) | 1 | ||
| Midwifery | 38(26.8) | 104(73.2) | 10.05(4.82, 20.89) | 7.39(2.25, 24.24) | 0.001* |
| Level of education | |||||
| Diploma | 6(4.4) | 129(95.6) | 1 | ||
| Degree and above | 42(14.4) | 250(85.6) | 3.61(1.49, 8.72) | 4.21(1.60, 11.00) | 0.003* |
| Ever received refresher NR training | |||||
| No | 23(7.2) | 297(92.8) | 1 | ||
| Yes | 25(23.4) | 82(76.6) | 3.94(2.12, 7.29) | 2.72(0.81, 3.63) | 0.15 |
| Ever performed NR | |||||
| No | 6(2.7) | 219(97.3) | 1 | ||
| Yes | 42(20.8) | 160(79.2) | 9.58(3.97, 23.08) | 3.33(1.09, 10.15) | 0.03* |
| Ever worked in a delivery unit | |||||
| No | 9(4.2) | 204(95.8) | 1 | ||
| Yes | 39(18.2) | 175(81.8) | 5.05(2.38, 10.72) | 0.52(0.15, 1.79) | 0.30 |
| Ever worked in a pediatrics unit | |||||
| No | 42(12.8) | 286(87.2) | 1 | ||
| Yes | 6(6.0) | 93(94.0) | 0.44(0.09, 0.77) | 0.80(0.22, 2.76) | 0.71 |
| Level of knowledge about NR | |||||
| Poor knowledge | 31(8.1) | 354(91.9) | 1 | ||
| Good knowledge | 17(40.5) | 25(59.5) | 7.77(3.79, 15.90) | 3.31(1.41, 7.73) | 0.006* |
*Statistically significant at p-value <0.05 in multivariate logistic regression analysis.
Discussion
The present study showed that only 11.2% of midwives and nurses had retained the skills of NR. In multivariate logistic regression analysis, being a midwife, having a BSc degree and above educational status, ever performed NR, and having a good level of knowledge were independently associated with NR skill retention of midwives and nurses.
Eleven percent of our sample retained their NR skills. This was lower than studies conducted in India [45, 46], Afghanistan [23], Tanzania [47], and northern Ethiopia [44]. This is probably due to the fact that the other studies were conducted in a single facility and urban facilities, while this study incorporated a broad study setting that included rural facilities that had no access to many infrastructures, limited essential equipment, updated NR information and internet access. However, 11.2% reported in our study was greater than some other studies, for example, in Pune city, India (6.3%) [20]. This might be due to the impact of the current focus of neonatal care service in Ethiopia. In Ethiopia, to improve access to neonatal care, many neonatal intensive care unit were opened and midwives and nurses training were started. During this time, a quarter of the midwives and nurses in Eastern Ethiopia received refresher training.
Regarding factors associated with NR skill retention, being a midwife was significantly associated with skill retention; midwives were 7.39 times more likely to retain NR skills as compared with nurses. This might be due to the fact that midwives were frequently exposed in the delivery room and received refresher training. This finding is in agreement with a finding in Afghanistan [23]. In addition, those who ever performed NR were 3.33 times more likely to retain their skill than those not exposed in NR. This finding is in line with studies in Nepal and Italy [48–50].
Furthermore, having higher educational status was associated with better skill retention. Those with a BSc degree and above were 4.21 times more likely to retain their skill than a level IV diploma nurse or midwives. This might be due to the fact that in the curricula of degree learners, there was greater focus on maternal and child health and using evidence-based practice. Moreover, having a good knowledge was found to be significantly associated with the NR skill retention of nurses and midwives. Those with good knowledge about NR were 3.31 times more likely to retain their skill. It is clear that knowledgeable care providers can apply their knowledge to skill. Paradoxically, receiving NR refresher training was not associated with the multivariate logistic analysis of this study, but in many studies, NR training was found to be significantly associated with retention of NR skill [23,30,50–55].
A limitation of this study was the use of anatomic model simulation and observations to assess NR skill. Most providers may not consider and give attention to the anatomical model as a human being. Furthermore, the skill was scored by a single expert, and no inter-rater variation test was conducted. The stress of testing, as well as the stress of clinical situations where NR are needed, may have contributed to the low outcome of skill retention. In addition, the study was undertaken at one-time point so it is not possible to establish cause-effect relationships.
Conclusion
NR skills among midwives and nurses are not well retained in public health care facilities in the Eastern part of Ethiopia, which might increase the death rate of neonates due to asphyxia. Being a midwife, having a BSc degree or above, ever performed NR, and having good knowledge in NR were independently associated with NR skills retention in this study setting. Providers should be encouraged to upgrade their educational level to build their skill retention and expose themselves to NR. Further, understanding factors affecting how midwives and nurses gain and retain skills using high-level methodology are essential.
Supporting information
(SAV)
(DOCX)
Acknowledgments
The authors would like to thanks CIRHT-Ethiopia for their constructive comments and Haramaya University College of Health and Medical Sciences for their constructive comments and ethical review, and all respective Health Bureau for their cooperation to write permission letters to their health facilities. We also thank the data collectors, participants of the study and Pre-Publication Support Service (PREPSS) supported the development of this manuscript by providing pre-publication peer-review and copy editing.
Abbreviations
- NR
Neonatal Resuscitation
- WHO
World Health Organization 31769
Data Availability
All related data are presented fully within the paper and its Supporting Information files.
Funding Statement
CIRHT-Ethiopia provided support in the form of per diem for data collectors, supervisors and provided training for the team. No additional external funding was received for this study.
References
- 1.Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN. Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000–2013. Bull World Health Organ [Internet]. 2015;93(1):19–28. 10.2471/BLT.14.139790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agravat N. mHealth and neonatal resuscitation. A Review of Interventions, Approaches, and Applications. 2013, pp. 1–40. Available from: healthenabled.org/wordpress/wp content/ uploads. [Google Scholar]
- 3.Lee AC, Cousens S, Wall SN, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health. 2011;11(Suppl 3):S12 10.1186/1471-2458-11-S3-S12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawn JE. 4 Million Neonatal Deaths: an Analysis of Available Cause-of-Death Data and Systematic Country Estimates With a Focus on “Birth Asphyxia. Unpubl Work [Internet]. 2009;I:1–202. [Google Scholar]
- 5.You Danzhen, Hug Lucia, Ejdemyr Simon, Jan Beise PI World. Child Mortality 2015 [Internet]. UNICEF WHO World Bank Group United Nations; New York; 2015. p. 74 Available from: www.childmortality.org [Google Scholar]
- 6.UNICEF. United Nations Inter-agency Group for Child Mortality Estimation (UN IGME), ‘Levels & Trends in Child Mortality. Report 2015’, United Nations Children’s Fund, New York, 2015, available from <www.childmortality.org.
- 7.Wang H, Liddell CA, Coates MM, Mooney MD L, CE SA. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384 (9947):957–79. 10.1016/S0140-6736(14)60497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. monitoring health for the SDGs, sustainable development goals [Internet]. Geneva, Switzerland: World Health Organization; 2018. Available from: http://apps.who.int/iris [Google Scholar]
- 9.UNICEF, WHO, World Bank U-DPD. Levels and trends in child mortality [Internet]. New York:; 2015. Available from: http://www.who.int/maternal_child_adolescent/.
- 10.Bogale TN, Worku AG, Bikis GA, Kebede ZT. Why gone too soon? Examining social determinants of neonatal deaths in northwest Ethiopia using the three delay model approach. BMC Pediatr. 2017;2017(17):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO. Guidelines on Basic Newborn Resuscitation [Internet]. World Health Organization. WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland; 2012. Available from: https://www.who.int/maternal_child_adolescent/.
- 12.Aslam HM, Saleem S, Afzal R, Iqbal U, Saleem SM, Shaikh MW, et al. Risk factors of birth asphyxia. Italian journal of pediatrics. 2014. December 1;40(1):94 10.1186/s13052-014-0094-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryce J, Boschi-pinto C, Shibuya K, Black RE, Health C, Reference E. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. 10.1016/S0140-6736(05)71877-8 [DOI] [PubMed] [Google Scholar]
- 14.Stanton C, Lawn JE, Rahman H, Wilczynska-ketende K, Hill K. Stillbirth rates: delivering estimates in 190 countries. Lancet. 2006;367:1487–94. 10.1016/S0140-6736(06)68586-3 [DOI] [PubMed] [Google Scholar]
- 15.Lawn JE, Cousens S, Zupan J. Neonatal Survival 1 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. 10.1016/S0140-6736(05)71048-5 [DOI] [PubMed] [Google Scholar]
- 16.Bhutta ZA. Learn more about Perinatal Asphyxia Paediatrics in the Tropics. In: Jeremy Farrar, Peter J. Hotez… Nicholas J. White, editor. Manson’s Tropical Infectious Diseases [Internet].2014. Available from: https://www.sciencedirect.com/book/9780702051012.
- 17.Halloran DR, McClure E, Chakraborty H, Chomba E, Wright LL, Carlo WA. Birth asphyxia survivors in a developing country. Journal of Perinatology. 2009. March;29(3):243–9. 10.1038/jp.2008.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daripa M, Caldas HMG, Flores LPO, Waldvogel BC, Guinsburg R, de Almeida MFB. Perinatal asphyxia associated with early neonatal mortality: populational study of avoidable deaths. Rev Paul Pediatr [Internet]. 2013;31(1):37–45. 10.1590/s0103-05822013000100007 [DOI] [PubMed] [Google Scholar]
- 19.Antonucci R, Porcella A, Pilloni MD. Perinatal asphyxia in the term newborn. Journal of Pediatric and Neonatal Individualized Medicine (JPNIM). 2014. October 21;3(2):1–4, e030269. [Google Scholar]
- 20.Devi S. A study to assess the effectiveness of Neonatal resuscitation Programme, First Golden minute certified training Course on knowledge and skill set of Nurses working in selected Hospital of Pune city. Int J Sci Res [Internet]. 2015;4(2277):432–5. [Google Scholar]
- 21.Wall SN, Lee AC, Niermeyer S, English M, Keenan WJ, Carlo W, et al. Neonatal resuscitation in low-resource settings: What, who, and how to overcome challenges to scale up? Int J Gynaecol Obs. 2010;107(Suppl 1):S47–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhutta ZA, Darmstadt GL, Haws RA, Yakoob MY, Lawn JE. Delivering interventions to reduce the global burden of stillbirths: Improving service supply and community demand. BMC Pregnancy Childbirth. 2009;9(SUPPL. 1):1–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim Y, Ansari N, Kols A, Tappis H, Currie S, Zainullah P, et al. Assessing the capacity for newborn resuscitation and factors associated with providers’ knowledge and skills: a cross-sectional study in Afghanistan. BMC Pediatr [Internet]. 2013;13(1):140–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mekonnen, Biruk Tensou, Daniel S Telake TDand AB. Neonatal mortality in Ethiopia: trends and determinants. BMC Public Heal 2013,. 2013;13:471–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Central Statistical Agency (CSA)[Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF. Available: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
- 26.Cavagnero E, Daelmans B, Gupta N, Scherpbier R, Shankar a. Assessment of the health system and policy environment as critical complement to tracking interventions coverage for maternal, newborn, and child health. Lancet. 2008;371:1284–93. 10.1016/S0140-6736(08)60563-2 [DOI] [PubMed] [Google Scholar]
- 27.United Nations General Assembly. Transforming our world: The 2030 agenda for sustainable development.2015. https//sustainabledevelopment.un.org;
- 28.Maynard KR, Causey L, Kawaza K, Dube Q, Lufesi N, Maria Oden Z, et al. New technologies for essential newborn care in under-resourced areas: what is needed and how to deliver it. Paediatr Int Child Health. 2015;35(3):192–205. 10.1179/2046905515Y.0000000034 [DOI] [PubMed] [Google Scholar]
- 29.Berglund S, Norman M. Neonatal resuscitation assessment: documentation and early paging must be improved! Arch Dis Child Fetal Neonatal Ed [Internet]. 2012;97(3):F204–8. 10.1136/archdischild-2011-300295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tabangin ME, Josyula S, Taylor KK, Vasquez JC, Kamath-Rayne BD. Resuscitation skills after Helping Babies Breathe training: A comparison of varying practice frequency and impact on retention of skills in different types of providers. Int Health. 2018;10(3):163–71. 10.1093/inthealth/ihy017 [DOI] [PubMed] [Google Scholar]
- 31.Benazeera SGU. Assessment of student’s knowledge on neonatal resuscitation. J Biomed Pharm Res. 2014;3(2):67–71. [Google Scholar]
- 32.Patel J, Posencheg M, Ades A. Proficiency and Retention of Neonatal Resuscitation Skills by Pediatric Residents. Pediatrics. 2012;130(3):515–21. 10.1542/peds.2012-0149 [DOI] [PubMed] [Google Scholar]
- 33.Subbiah N, Sarin J, Jeeva S, Geetanjali. Effectiveness of educational intervention on neonatal resuscitation among nursing personnel. TT -. Heal Popul Perspect Issues [Internet]. 2012;35(1): 36–45. [Google Scholar]
- 34.Seid A. knowledge and practice of neonatal resuscitation and associated factors among health professionals at jugel and hiwot fana specialized university hospital harar, Eastern, Ethiopia. unpublished. 2015. [Google Scholar]
- 35.Averting Maternal Death and Disability Program (AMDD): Needs Assessmentof Emergency Obstetric and Newborn Care (EmONC): Facilitator’s Guide. NewYork: Averting Maternal Death and Disability; 2009. [Google Scholar]
- 36.Keyes E.B., Haile‐Mariam A., Belayneh N.T., Gobezie W.A., Pearson L., Abdullah M., et al. (2011), Ethiopia's assessment of emergency obstetric and newborn care: Setting the gold standard for national facility‐based assessments. International Journal of Gynecology & Obstetrics, 115: 94–100. 10.1016/j.ijgo.2011.07.009 [DOI] [PubMed] [Google Scholar]
- 37.Abrha MW, Asresu TT, Araya AA, Woldearegay HG. Healthcare Professionals' Knowledge of Neonatal Resuscitation in Ethiopia: Analysis from 2016 National Emergency Obstetric and Newborn Care Survey. Int J Pediatr. 2019. July 16; 2019:8571351 10.1155/2019/8571351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mirkuzie AH, Sisay MM, Reta AT, Bedane MM. Current evidence on basic emergency obstetric and newborn care services in Addis Ababa, Ethiopia; a cross sectional study. BMC pregnancy and childbirth. 2014. December;14(1):354 10.1186/1471-2393-14-354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kinzie B, Gomez P. Basic maternal and newborn care. A guide for skilled provider. 2004. Available at: http://www.healthynewbornnetwork.org/hnn-content/uploads/JHPIEGO_mnh.pdf. [Google Scholar]
- 40.Beck D, Ganges F, Goldman S, Long P. Saving Newborn Lives. Cuidados ao Recém-Nascido. Manual de Consulta Acedido a. 2004;18 [Google Scholar]
- 41.Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. : Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (Reprint). Pediatrics 2015, 136 Suppl 2:S196–218. [DOI] [PubMed] [Google Scholar]
- 42.Murila F, Obimbo MM, Musoke R. Assessment of knowledge on neonatal resuscitation amongst health care providers in Kenya. Pan African Medical Journal. 2012; 8688, pp.4–9. Available online at: http://www.panafrican-med-journal.com/content/article/11/78/full/ [PMC free article] [PubMed] [Google Scholar]
- 43.Alhassan A, Fuseini AG, Osman W, Basour Adam A. Nurs Res Pract. Knowledge and Experience of Neonatal Resuscitation among Midwives in Tamale. Nursing research and practice, 2019. January 2; 2019:3652608 10.1155/2019/3652608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gebreegziabher E, Aregawi A, Getinet H. Knowledge and skills of neonatal resuscitation of health professionals at a university teaching hospital of Northwest Ethiopia. World J Emerg Med. 2014;5(3):196‐202. 10.5847/wjem.j.issn.1920-8642.2014.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vijayan A. Effect of Structured Teaching Programmeon Knowledge and Skills on Neonatal Resuscitation. Int J Adv Res. 2015;3(7):1200–5. [Google Scholar]
- 46.Bansal SC, Nimbalkar AS, Patel D V., Sethi AR, Phatak AG, Nimbalkar SM. Current Neonatal Resuscitation Practices among Paediatricians in Gujarat, India. Int J Pediatr [Internet]. 2014;2014:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Makene CL, Plotkin M, Currie S, Bishanga D, Ugwi P, Louis H, et al. Improvements in newborn care and newborn resuscitation following a quality improvement program at scale: results from a before and after study in Tanzania. BMC Pregnancy Childbirth [Internet]. 2014;14(1):381 http://www.biomedcentral.com/1471-2393/14/38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ashish KC, Wrammert J, Nelin V, Clark RB, Ewald U, Peterson S, et al. Evaluation of Helping Babies Breathe Quality Improvement Cycle (HBB-QIC) on retention of neonatal resuscitation skills six months after training in Nepal. BMC Pediatr [Internet]. 2017;17(1):103 10.1186/s12887-017-0853-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.De Bernardo G, Sordino D, Cavallin F, Mardegan V, Doglioni N, Tataranno ML, et al. Performances of low level hospital health caregivers after a neonatal resuscitation course. Ital J Pediatr [Internet]. 2016;42(1):100 10.1186/s13052-016-0313-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ameh C a., Kerr R, Madaj B, Mdegela M, Kana T, Jones S, et al. Knowledge and Skills of Healthcare Providers in Sub-Saharan Africa and Asia before and after Competency-Based Training in Emergency Obstetric and Early Newborn Care. PLoS One. 2006;11(12): 10.1371/journal.pone.0167270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eblovi D, Kelly P, Afua G, Agyapong S, Dante S, Pellerite M. Retention and use of newborn resuscitation skills following a series of helping babies breathe trainings for midwives in rural Ghana. Glob Health Action [Internet]. 2017;10(1):0–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Das M, Chaudhary C, Bisht S, Maria A, Jain A, Kaushal S, et al. Retention of knowledge and skill of birth attendants in newborn care and resuscitation after 1 Year in clinical practice: An experience from India. J Clin Neonatol. 2018;7(2):89–95. Available from: http://www.jcnonweb.com/text.asp?2018/7/2/89/229672. [Google Scholar]
- 53.Drake M, Bishanga DR, Temu A, Njozi M, Thomas E, Mponzi V, et al. Structured on-the-job training to improve retention of newborn resuscitation skills: A national cohort Helping Babies Breathe study in Tanzania. BMC Pediatr. 2019;19(1):1–8. 10.1186/s12887-018-1376-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bookman L, Engmann C, Srofenyoh E, Enweronu-Laryea C, Owen M, Randolph G, et al. Educational impact of a hospital-based neonatal resuscitation program in Ghana. Resuscitation [Internet]. 2010;81(9):1180–2. 10.1016/j.resuscitation.2010.04.034 [DOI] [PubMed] [Google Scholar]
- 55.Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, et al. Helping Babies Breathe (HBB) training: What happens to knowledge and skills over time? BMC Pregnancy Childbirth [Internet]. 2016;16(1):364 10.1186/s12884-016-1141-3 [DOI] [PMC free article] [PubMed] [Google Scholar]