Abstract
Objectives
Low back pain (LBP) has a major impact on health workers, and its prevalence and risk factors among them in Saudi Arabia have been investigated previously. However, the results have never been comprehensively reviewed. Therefore, the aim of this study was to perform a systematic review and meta‐analysis of the available literature to identify the prevalence and risk factors of LBP among health workers in Saudi Arabia.
Methods
MEDLINE/PubMed, Web of Science, Scopus, CINAHL, and Saudi peer‐reviewed journals were searched for relevant literature. After quality assessment of the eligible articles, 18 studies targeting seven occupational categories, with a total number of 5345 health workers, were analyzed.
Results
Pooled prevalence rates of 40.8% (n = 7 studies), 65.0% (n = 13 studies), and 81.4% (n = 2 studies) were obtained for week, year, and career, respectively, across all professional groups. Nurses and physical therapists were more susceptible to LBP, in that order, than the other categories considering week and career periods. Age, body mass index, and female gender were the most commonly reported individual risk factors. Occupational risk factors mainly included work‐related activities requiring back bending and twisting, lifting and pulling objects, and manual patient‐handling.
Conclusions
The results of this review indicate that LBP is highly prevalent among health workers in Saudi Arabia when compared with international rates. Proper prophylactic measures are necessary to reduce LBP and minimize its consequences. Further high‐quality research is needed in different Saudi regions to achieve a broader understanding of LBP prevalence and causes.
Keywords: health personnel, low back pain, prevalence, risk factors, Saudi Arabia
1. INTRODUCTION
Low back pain (LBP) is highly prevalent around the world. 1 In Saudi Arabia, its prevalence is estimated to range from 18.8% 2 to 53.5%. 3 At the same time, LBP is considered one of the leading reasons for loss of productive work time and missed workdays. 4 In fact, 24.1% of workers in Saudi Arabia reported reduced working hours, 29.2% reported limited working activities, and 15.3% reported absence from work due to LBP. 3
LBP is a common cause of absenteeism among health workers in Saudi Arabia. 5 , 6 , 7 , 8 Previous studies showed that 10.9%‐54.4% of health workers who had LBP reported taking sick days because of it. 8 , 9 For 71% of them, their sick leave may extend from 2 to 30 days. 6 Around 70%‐85% believed that their LBP was caused by work‐related activities. 10 , 11 , 12 In fact, 15%‐17% of health workers had to change their work setting because of LBP. 7 , 8 Other consequences of LBP reported by health workers in Saudi Arabia range from limited social, leisure, and daily activities 6 , 7 , 8 to seeking medical help, hospital admission, and even surgery. 5 , 6 , 9 , 13 , 14
In recent years, there has been a rapid increase in the number of published papers investigating the prevalence and risk factors of LBP across different categories of health workers in different parts of Saudi Arabia, with studies reporting a wide range of LBP prevalence rates. For instance, the annual prevalence of LBP across health workers in Saudi Arabia was estimated to range from 46.5% 15 to 92.6%. 16 These rates were attributed to various individual risk factors, such as age and gender. Work‐related factors were also reported, such as high workload, manual patient‐handling, and workplace. To the best of the author's knowledge, these studies have never been systematically analyzed.
1.1. Objectives and research questions
To achieve an overall understanding of the development of LBP and its associated risk factors in the healthcare sector in Saudi Arabia, the primary objectives of this review were (a) to estimate the prevalence of LBP among health workers in Saudi Arabia and (b) to identify the associated risk factors of LBP. The secondary objectives were to identify, when possible, the characteristics of LBP episodes in terms of duration and intensity, and compare the risk of developing LBP between the different occupational categories. Accordingly, the main research questions of this review were as follows: (a) What is the estimated prevalence of LBP among health workers in Saudi Arabia? and (b) What are the risk factors of LBP in this population?
2. MATERIALS AND METHODS
2.1. Search strategy
A search of the literature was conducted in the following electronic databases: MEDLINE/PubMed, Web of Science, Scopus, and CINAHL. The key terms used for performing the search were (“Saudi”) AND (“hospital” OR “physicians” OR “surgeons” OR “nurses” OR “dentists” OR “physical therapists” OR “clinicians" OR “health professionals” OR “health associate professionals” OR “healthcare workers” OR “healthcare professionals” OR “medical practitioners” OR “health personnel”) AND (“low back pain” OR “lower backache” OR “spinal pain” OR “spinal disorders” OR “musculoskeletal disorders” OR “musculoskeletal pain”) AND (“prevalence” OR “frequency” OR “incidence” OR “risk factors”). Furthermore, electronic Saudi peer‐reviewed journals were searched for relevant articles. Duplicate records were manually removed by the author. The abstracts of the obtained titles were examined for inclusion. If inclusion or exclusion could not be decided based on the abstract, the full text was retrieved to determine the eligibility of the study. The references of the retrieved articles were also inspected to identify additional potential publications. The author performed the literature search that extended until March 2020.
2.2. Inclusion and exclusion criteria
The obtained articles were screened by the author based on the following inclusion criteria: cross‐sectional full‐text articles published in a peer‐reviewed journal, conducted in Saudi Arabia, written in English, and investigating the prevalence and/or risk factors of LBP and/or musculoskeletal pain including LBP among health professionals and/or health associate professionals (according to the international classification of health workers of the World Health Organization), 17 regardless of age or gender. Both classifications of LBP (specific and nonspecific) were considered. Excluded were review articles, letters to the editor, case reports, and editorials. Studies with an undefined prevalence period or including the general population or health students, interns, or cohorts other than health professionals and/or health associate professionals were also excluded.
2.3. Risk of bias and quality assessment
All articles that fulfilled the eligibility criteria were assessed using the risk‐of‐bias tool developed by Hoy et al. 18 This tool was designed mainly for prevalence studies and consists of 10 items addressing internal and external validity. Each item is scored as having either low or high risk of bias. If there was not sufficient information in the article to permit scoring a specific item, that item was scored as high risk of bias. The overall risk‐of‐bias score for each individual study was the total number of high‐risk items (considering a score of 0‐2 as low, 3‐4 as moderate, and 5‐10 as high risk of bias). Two independent raters performed the assessment of risk of bias, and the differences between the raters were resolved by discussion. To improve the quality of the results, studies with a high risk of bias were eventually excluded from the final analysis (Figure 1). A sensitivity analysis was performed to explore whether including studies with a high risk of bias affected the prevalence rates extracted only from studies with low and moderate risk of bias.
FIGURE 1.
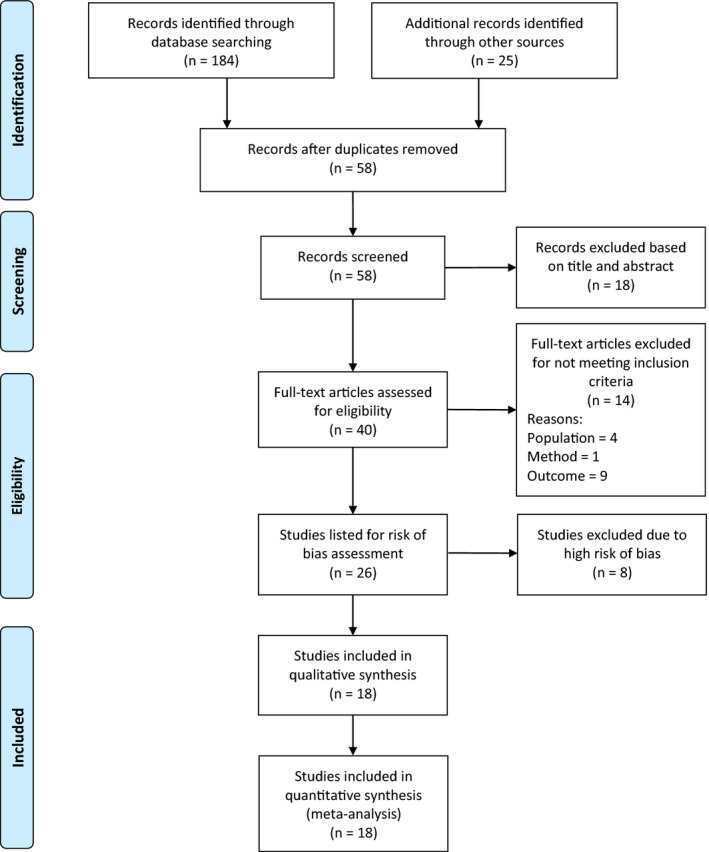
Flow diagram of the screening and selection process used in the review
2.4. Data extraction
A data extraction form for prevalence and risk factor studies 19 was adapted and modified to meet the purpose of this review. The form was used to extract the characteristics of the eligible studies, including study design, method, location, setting, occupational category, sample description, inclusion and exclusion criteria, outcome measure, prevalence rate, duration and intensity of LBP, and significant risk factors along with odds ratios (ORs) and 95% confidence intervals (95% CIs). For studies that reported risk factors for musculoskeletal disease in general, only the prevalence rates of LBP were extracted, as the risk factors were not specific for LBP. For the studies that did not report the number of cases, this was calculated based on the prevalence rate reported. Whenever essential data were missing from the article, or conflicts were noticed in the results, the authors were contacted for clarification or to obtain the missing information.
2.5. Statistical analysis and data synthesis
Separate meta‐analyses were conducted, and forest plots were generated, to obtain pooled prevalence rates and 95% CIs for each identified prevalence period and occupational category using a Microsoft Excel spreadsheet published by Neyeloff et al. 20 The heterogeneity of the analyzed studies was examined using Cochran's Q and I2 statistics. The I2 values were interpreted as follows: <25%, low heterogeneity; 25%‐75%, moderate heterogeneity; and >75%, high heterogeneity. 21 To calculate the pooled prevalence rates, either fixed‐effect or random‐effects models were used if heterogeneity was low or moderate to high, respectively. 20
Furthermore, the risk of developing LBP for the identified occupational categories was estimated by calculating the ORs and 95% CIs. Chi‐square tests were used to examine the significance of the obtained ratios with an alpha level set at 0.05. All statistical tests were performed using IBM SPSS Statistics for Windows version 25.0 (Armonk, NY).
3. RESULTS
A total of 209 articles were obtained by searching the databases and references of the retrieved publications. After removing duplicates, 58 studies were screened, and 18 were excluded based on the title and abstract. The remaining 40 articles were identified as potentially relevant publications, and their full texts were retrieved and assessed for eligibility. A total of 14 studies were excluded for not meeting the inclusion criteria as follows: two studies included health students/interns; two included administration staff; four did not define the prevalence period; one was not fully conducted in Saudi Arabia; and five grouped LBP with upper back pain, defined as “back pain”. Finally, 26 articles 6 , 7 , 8 , 9 , 10 , 13 , 14 , 15 , 16 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 fulfilled the inclusion criteria and underwent a risk‐of‐bias assessment. Figure 1shows the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses 39 flow diagram illustrating the screening and selection process followed in the present review.
3.1. Risk of bias and quality assessment
For the assessment of risk of bias of the 26 articles, low risk of bias was found for 5 (19.2%) studies, 16 , 24 , 30 , 32 , 34 moderate risk for 13 (50%), 6 , 7 , 9 , 10 , 13 , 15 , 23 , 27 , 28 , 33 , 35 , 36 , 37 and high risk for 8 (30.8%). 8 , 14 , 22 , 25 , 26 , 29 , 31 , 38 The risk‐of‐bias assessment for the studies is shown in detail in Table 1. The sensitivity analysis revealed that excluding prevalence estimates of high risk‐of‐bias studies from the meta‐analyses did not substantially affect the prevalence rates, as will be shown later in this section.
TABLE 1.
Risk‐of‐bias scores for included and excluded articles
| Study | External validity | Internal validity | Overall | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Representation | Sampling | Random selection | Non‐response bias | Data collection | Case definition | Validity of instrument | Consistency of data collection | Prevalence period | Numerators and denominators | ||
| Included articles (n = 18) | |||||||||||
| Al‐Eisa and Al‐Abbad, 2013 6 | High | High | High | Low | Low | Low | Low | Low | Low | Low | Moderate |
| Alghadir et al, 2017 7 | High | High | High | Low | Low | Low | High | Low | Low | Low | Moderate |
| Abbas et al, 2010 9 | High | Low | Low | High | Low | Low | High | Low | Low | Low | Moderate |
| Alsiddiky et al, 2015 10 | High | Low | Low | Low | Low | High | Low | Low | High | Low | Moderate |
| Alzidani et al, 2018 13 | High | High | High | Low | Low | Low | High | Low | Low | Low | Moderate |
| Muaidi and Shanb, 2016 15 | Low | High | High | High | Low | High | Low | Low | Low | Low | Moderate |
| Alnaami et al, 2019 16 | High | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low |
| Abu Tariah et al, 2020 23 | High | High | High | High | Low | Low | Low | Low | Low | Low | Moderate |
| Al Shammari et al, 2019 24 | High | Low | High | Low | Low | Low | Low | Low | Low | Low | Low |
| Aljanakh et al, 2015 27 | High | High | High | Low | Low | Low | Low | Low | Low | High | Moderate |
| Aljerian et al, 2018 28 | High | High | High | Low | Low | Low | Low | Low | Low | High | Moderate |
| Al‐Mohrej et al, 2016 30 | High | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low |
| Al‐Ruwaili and Khalil, 2019 32 | High | Low | Low | Low | Low | High | Low | Low | Low | Low | Low |
| Alsultan et al, 2018 33 | High | High | High | Low | Low | Low | Low | Low | Low | Low | Moderate |
| Attar, 2014 34 | High | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low |
| Bin Homaid et al, 2016 35 | High | Low | High | Low | Low | Low | Low | Low | High | Low | Moderate |
| Keriri, 2013 36 | High | High | Low | High | Low | Low | High | Low | Low | Low | Moderate |
| Mohamed and Al Amer, 2019 37 | High | High | High | Low | Low | Low | Low | Low | Low | High | Moderate |
| Excluded articles (n = 8) | |||||||||||
| Al Dajah and Al Daghdi, 2013 8 | High | High | High | Low | Low | High | High | Low | Low | Low | High |
| Aseri et al, 2019 14 | High | Low | High | High | Low | High | Low | Low | High | Low | High |
| Abduljabbar, 2008 22 | High | High | Low | High | Low | High | High | Low | Low | High | High |
| Alamri et al, 2018 25 | High | Low | Low | High | Low | High | High | Low | Low | High | High |
| Alghadir et al, 2015 26 | High | High | High | High | Low | High | High | Low | High | High | High |
| Almalki et al, 2016 29 | High | Low | High | Low | Low | High | High | Low | High | Low | High |
| AlNekhilan et al, 2020 31 | High | High | High | High | Low | Low | Low | Low | Low | High | High |
| Gaowgzeh, 2019 38 | High | High | Low | Low | Low | High | High | Low | High | Low | High |
3.2. Study characteristics
A total of 18 articles were included in the final analysis. All of them were cross‐sectional, and their characteristics are listed in Table 2. The study sample sizes ranged from 68 27 to 937, 9 with a total number of 5345 health workers. Out of the 18 studies included, 5 targeted physicians, 10 , 13 , 24 , 32 , 33 2 focused on dentists, 27 , 30 5 studied nurses, 6 , 9 , 23 , 34 , 36 2 targeted physical therapists, 7 , 15 1 studied emergency medical service (EMS) staff, 28 and 3 included more than one category of health workers. 16 , 36 , 37 Other health workers were anesthesia technicians (AT) and operation room technicians (ORT). 35
TABLE 2.
Characteristics of the studies included in the review
| Study | Design | City | Setting | Period | Occupation | Sample size | Age (y) | Inclusion/exclusion criteria | Outcome measure | Definition of low back pain |
|---|---|---|---|---|---|---|---|---|---|---|
| Al‐Eisa and Al‐Abbad, 2013 6 | Cross‐sectional | Riyadh | 1 hospital | Not reported | Nurses |
155 M = 29 F = 126 |
39.8 ± 8.2 |
Inclusion: work full time in the rehabilitation hospital and responsible for patient handling activities Exclusion: pregnancy and health‐related problems prohibiting from handling patients |
Self‐designed, four‐part questionnaire; part 4 is the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Alghadir et al, 2017 7 | Cross‐sectional | Riyadh | NA; online survey | Not reported | PTs |
502 M = 307 F = 195 |
<30 to >40 | Inclusion: in direct patient contact for at least 1 h each day | Self‐designed questionnaire | Unpleasant sensation in the lower back region below the scapulae and above the hip region, that may or may not radiate to the thighs and legs |
| Abbas et al, 2010 9 | Cross‐sectional | Riyadh | 4 hospitals | Not reported | Nurses |
937 M = 114 F = 823 |
<30 to >50 | Exclusion: history of musculoskeletal or bone disorders | Self‐designed questionnaire and the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Musculoskeletal Nordic Questionnaire |
| Alsiddiky et al, 2015 10 | Cross‐sectional | Riyadh | 1 hospital | May 2013 to August 2013 | Physicians |
411 M = 248 F = 163 |
20‐50 | Not reported | Self‐designed questionnaire | No definition reported |
| Alzidani et al, 2018 13 | Cross‐sectional | Taif | 3 hospitals | January to March 2018 | Physicians |
138 M = 107 F = 31 |
≤ 30 to >50 | Exclusion: history of back or spinal surgery, any fracture or disorder in the pelvic region, spinal deformities, osteoporosis, back or spinal tumor, or any other malignancies | Self‐designed questionnaire | Pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain |
| Muaidi and Shanb, 2016 15 | Cross‐sectional | Nationwide | NA | Not reported | PTs |
690 M = 408 F = 282 |
Not reported | Exclusion: less than 1 y in their current work settings or reported musculoskeletal pain as a result of previous trauma | Self‐designed questionnaire | No definition reported |
| Alnaami et al, 2019 16 | Cross‐sectional | Aseer | Hospitals and primary healthcare centers | Not reported |
Physicians Dentists Nurses |
594 | 20 to >50 | Exclusion: retired or not practicing clinical work | Self‐designed questionnaire | Pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain (sciatica) |
| Abu Tariah et al, 2020 23 | Cross‐sectional | Riyadh | 1 hospital | Not reported | Nurses |
94 M = 2 F = 92 |
<25 to ≥50 |
Inclusion: at least 1 y of work experience with direct patients' care Exclusion: not involved in direct patients' care such as nurse administrators and students |
The Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Al Shammari et al, 2019 24 | Cross‐sectional | Eastern Province | 12 health institutions | April, 2019 | Physicians |
198 M = 111 F = 87 |
<30 to ≥50 | Not reported | Self‐designed, four‐part questionnaire and the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Aljanakh et al, 2015 27 | Cross‐sectional | Ha'il | Governmental hospitals and clinics | January 2014 to January 2015 | Dentists |
68 M = 43 F = 25 |
38.5 ± 7.4 | Inclusion: at least 1 y of work experience in the current position | Self‐designed questionnaire based on the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Aljerian et al, 2018 28 | Cross‐sectional | Riyadh | SRCA and hospitals | Not reported | EMS |
360 all males |
Not reported | Exclusion: dispatchers and non‐shift EMS personnel | Self‐designed, two‐part questionnaire; part 2 is the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Al‐Mohrej et al, 2016 30 | Cross‐sectional | Riyadh | 150 hospitals and private clinics | Not reported | Dentists |
204 M = 103 F = 101 |
38.0 ± 10.6 |
Inclusion: worked as a dentist for at least 1 y Exclusion: history of orthopedic trauma or congenital deformities (of the neck, back and upper extremities) |
Self‐designed questionnaire based on the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Al‐Ruwaili and Khalil, 2019 32 | Cross‐sectional | Tabuk | 1 hospital | 2019 | Physicians |
254 M = 170 F = 84 |
36.0 ± 9.3 |
Inclusion: physicians, from both genders, all specialties and qualifications working during 2019 Exclusion: chronic or recurrent back pain, trauma in the back, osteoporosis, infection, or neoplasm |
Self‐designed questionnaire | No definition reported |
| Alsultan et al, 2018 33 | Cross‐sectional | Riyadh | 1 hospital | Not reported | Physicians |
140 M = 110 F = 30 |
27 | Not reported | Self‐designed, two‐part questionnaire; part 2 is the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire |
| Attar, 2014 34 | Cross‐sectional | Jeddah | 1 hospital | September, 2011 to February, 2012 | Nurses |
200 M = 9 F = 191 |
34.6 ± 8.1 | Exclusion: employees other than nurses | Self‐designed, three‐part questionnaire; part 3 is the Standardized Nordic Musculoskeletal Questionnaire | Defined by the Standardized Nordic Musculoskeletal Questionnaire: Symptoms (pain, numbness, tingling, aching, stiffness, and burning) that resulted from a work‐related event, excluding other injuries experienced over the past year that lasted 1 wk or more or occurred at least monthly with at least moderate pain on average |
| Bin Homaid et al, 2016 35 | Cross‐sectional | Makkah | 1 hospital | June, 2014 |
Physicians Nurses AT ORT |
114 | 33.9 ± 7.6 | Not reported | Self‐designed questionnaire | Pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain (sciatica) |
| Keriri, 2013 36 | Cross‐sectional | Taif | 4 hospitals | January to June 2011 | Nurses |
126 M = 27 F = 99 |
34.0 ± 8.0 |
Inclusion: nurses from both genders, belonging to any ethnic group, age less than 60 y, and working in operating rooms Exclusion: nurses with specific causes of back pain as a result of trauma, osteoporotic fractures, infections, and neoplasms |
Self‐designed questionnaire | Experiencing pain, ache, or discomfort in the lower back |
| Mohamed and Al Amer, 2019 37 | Cross‐sectional | Tabuk | 6 hospitals and 4 clinics | Not reported |
Physicians Nurses PTs |
160 M = 66 F = 94 |
35.5 ± 12.4 |
Inclusion: in direct contact with patients, work in both government and private hospitals or polyclinics Exclusion: work as a part timer, pregnant or on leave from their duties |
Cornell Musculoskeletal Discomfort Questionnaire for Male and Female and Self‐designed questionnaire | Defined by Cornell Musculoskeletal Discomfort Questionnaire |
Abbreviations: AT, anesthesia technicians; EMS, emergency medical service personnel; F, female; M, male; NA, not applicable; ORT, operation room technicians; PTs, physical therapists; SRCA, Saudi Red Crescent Authority.
One study 16 evaluated the LBP prevalence in paramedics, and another study 35 examined the prevalence among central sterile supply department staff. The prevalence rates for those two categories were not extracted, as the former study did not provide a clear description of health workers under the paramedics category, and central sterile supply department staff in the latter study do not fall under either health professionals or health associate professionals. 17 Furthermore, these two studies reported risk factors for more than one occupational category without segregation. One reported the risk factors for operation room staff including physicians, nurses, AT, ORT, and central sterile supply department staff combined. 35 The other study reported risk factors for physicians, dentists, nurses, and paramedics. 16 A decision was made to include the risk factors reported in the latter study, as the authors examined job title as a risk factor of LBP, and it was found not significant. Therefore, it is reasonable to assume that the reported risk factors can be correlated with the occupational categories included in the study, since there was no significant difference in LBP prevalence between them.
Intensity and/or duration of LBP episodes were reported in 9 out of the 18 studies (see Table 3). Duration was reported by two studies with nurses, 6 , 36 and one study each with physicians, 32 dentists, 30 and physical therapists. 7 Intensity of LBP episodes was reported by seven studies using different methods. Four studies surveyed the intensity among physicians, 10 , 13 dentists, 30 and physical therapists 7 on an ordinal scale of mild, moderate, or severe pain. Another study 35 used the same method to measure LBP intensity among more than one occupational category; however, it added “very severe” to the scale. Three studies measured intensity in physicians, 32 nurses, 36 and among different occupational categories 37 using numerical rating scales.
TABLE 3.
Duration and intensity of low back pain episodes
| Occupation | Study | Duration | Intensity |
|---|---|---|---|
| Physicians | Alsiddiky et al, 2015 10 | Not reported |
Mild = 83 (34) Moderate = 68 (28) Severe = 93 (38) |
| Alzidani et al, 2018 13 | Not reported |
Mild = 34 (33.7) Moderate = 60 (59.4) Severe = 7 (6.9) |
|
| Al‐Ruwaili and Khalil, 2019 32 |
Duration of last episode: 0‐<1 wk = 109 (56.5) 1‐2 wks = 32 (16.6) 3‐4 wks = 26 (13.5) 4‐5 wks = 13 (6.7) >5 wks = 13 (6.7) |
Intensity during the past 3 mo on a scale of 0‐5: 0 = 12 (6.2) 1 = 25 (13.0) 2 = 62 (32.1) 3 = 70 (36.3) 4 = 18 (9.3) 5 = 6 (3.1) |
|
| Dentists | Al‐Mohrej et al, 2016 30 |
<4 wks = 112 (80.6) 2‐3 mo = 19 (13.7) 3‐6 mo = 6 (4.3) >6 mo = 2 (1.4) |
Mild = 14 (10.1) Moderate = 92 (66.2) Severe = 33 (23.8) |
| Nurses | Al‐Eisa and Al‐Abbad, 2013 6 |
1‐7 d = 65 (56.0) 8‐30 d = 30 (25.9) >30 d = 9 (7.8) Every day = 12 (10.3) |
Not reported |
| Keriri, 2013 36 |
<2 y = 31 (50.8) >2 y = 30 (49.2) |
Intensity during the past 3 mo on a scale of 1‐5: 1 = 9 (14.8) 2 = 23 (37.7) 3 = 20 (32.8) 4 = 6 (9.8) 5 = 3 (4.9) |
|
| PTs | Alghadir et al, 2017 7 |
<1 wk = 250 (55) 2‐4 wks = 135 (30) >4 wks = 65 (14) |
Mild = 216 (43) Moderate = 126 (25) Severe = 108 (22) |
|
Physicians Nurses AT ORT |
Bin Homaid et al, 2016 35 | Not reported |
Mild = 32 (36) Moderate = 48 (53.9) Severe = 7 (7.9) Very severe = 2 (2.2) |
|
Physicians Nurses PTs |
Mohamed and Al Amer, 2019 37 | Not reported |
Average of intensity during the past wk on a scale of 0‐10: Physicians: 3.31 Nurses: 4.55 PTs: 3.75 Overall: 4.01 |
Values of duration and intensity are given as number (percentage) unless otherwise indicated.
Abbreviations: AT, anesthesia technicians; ORT, operation room technicians; PTs, physical therapists.
The 18 studies were conducted in different cities in Saudi Arabia, with the majority (8 studies) in Riyadh, 6 , 7 , 9 , 10 , 23 , 28 , 30 , 33 2 each in Taif 13 , 36 and Tabuk, 32 , 37 and 1 each in Eastern Province, 24 Jeddah, 34 Asser, 16 Makkah, 35 and Ha'il. 27 One study was conducted nationwide. 15
3.3. Outcome measures
All the 18 studies used self‐developed questionnaires to measure the prevalence and associated risk factors of LBP in their samples. However, nine studies 6 , 9 , 23 , 24 , 27 , 28 , 30 , 33 , 34 incorporated the Standardized Nordic Musculoskeletal Questionnaire 40 in their tools, while one study 37 integrated the Cornell Musculoskeletal Discomfort Questionnaire. 41
3.4. Prevalence of LBP
Six different prevalence periods were identified, namely point, week, month, year, career (defined as the incidence of LBP at some point during the professional career), 7 , 35 and lifetime prevalence, with some studies reporting more than one prevalence period. The most commonly reported prevalence period was year prevalence (13 studies), followed by week prevalence (4 studies), point and lifetime prevalence (3 studies each), career prevalence (2 studies), and month prevalence (1 study). In this review, episodes occurring in the past 7 days or less (ie, week and point prevalence) were pooled together as week prevalence. 42
It should be noted that one study 9 calculated the lifetime prevalence exclusive of point and previous year episodes, unlike the other studies included. To ensure consistency across the studies reporting lifetime prevalence, only point and year prevalence rates were extracted from this study, and the lifetime prevalence was excluded. Additionally, one study 35 calculated the prevalence for two medicine specialties separately (surgery and anesthesiology). Since the aim of this review was to study the prevalence among health workers regardless of the specialty within their field, the prevalence rates of the two specialties were combined under physicians.
3.4.1. Prevalence and odds ratios of LBP by period
Pooled rates of 40.8% (95% CI = 28.4%‐53.2%; n = 7 studies), 65.0% (95% CI = 59.4%‐70.5%; n = 13 studies), and 81.4% (95% CI = 69.3%‐93.5%; n = 2 studies) were obtained for week, year, and career, respectively, across all professional groups (Table 4; Figures S1‐S3). Month and lifetime prevalence rates were identified only for physicians and were therefore described in the following section.
TABLE 4.
Prevalence rates and odds ratios of low back pain by period and by occupational category
| Prevalence period | Occupation | Study | No. of cases | Sample size | Prevalence | Online supporting information (related forest plot) | Risk of LBP | |||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | OR | 95% CI | P value | ||||||
| Week | Physicians | Alzidani et al, 2018 13 | 28 | 138 | 20.3 | 12.8‐27.8 | ||||
| Al Shammari et al, 2019 24 | 84 | 198 | 42.4 | 33.4‐51.5 | ||||||
| Mohamed and Al Amer, 2019 37 | 26 | 52 | 50.0 | 30.8‐69.2 | ||||||
| Pooled prevalence | 36.4 | 18.0‐54.7 | Figure S4 | Reference group | ||||||
| Nurses | Abbas et al, 2010 9 | 576 | 937 | 61.5 | 56.5‐66.5 | |||||
| Abu Tariah et al, 2020 23 | 16 | 94 | 17 | 8.7‐25.4 | ||||||
| Keriri, 2013 36 | 61 | 126 | 48.4 | 36.3‐60.6 | ||||||
| Mohamed and Al Amer, 2019 37 | 46 | 80 | 57.5 | 40.9‐74.1 | ||||||
| Pooled prevalence | 45.9 | 21.9‐69.9 | Figure S8 | 2.35 a | 1.86‐3.00 | <.0005 | ||||
| PTs | Mohamed and Al Amer, 2019 37 | 10 | 28 | 35.7 | 13.6‐57.9 | 1.01 | 0.45‐2.24 | .987 | ||
| EMS | Aljerian et al, 2018 28 | 134 | 360 | 37.2 | 30.9‐43.5 | 1.07 | 0.79‐1.44 | .638 | ||
| Pooled prevalence | 40.8 | 28.4‐53.2 | Figure S1 | |||||||
| Month | Physicians | Alzidani et al, 2018 13 | 67 | 138 | 48.6 | 41.0‐56.1 | ||||
| Year | Physicians | Alzidani et al, 2018 13 | 91 | 138 | 65.9 | 52.4‐79.5 | ||||
| Al Shammari et al, 2019 24 | 137 | 198 | 69.2 | 57.6‐80.8 | ||||||
| Alnaami et al, 2019 16 | 259 | 353 | 73.4 | 64.4‐82.3 | ||||||
| Al‐Ruwaili and Khalil, 2019 32 | 177 | 254 | 69.6 | 59.4‐80.0 | ||||||
| Alsultan et al, 2018 33 | 74 | 140 | 52.9 | 40.8‐64.9 | ||||||
| Pooled prevalence | 66.8 | 59.9‐73.7 | Figure S5 | Reference group | ||||||
| Dentists | Aljanakh et al, 2015 27 | 39 | 68 | 57.4 | 39.4‐75.4 | |||||
| Al‐Mohrej et al, 2016 30 | 139 | 204 | 68.1 | 56.8‐79.5 | ||||||
| Alnaami et al, 2019 16 | 25 | 27 | 92.6 | 56.3‐128.3 | ||||||
| Pooled prevalence | 67.3 | 54.1‐80.5 | Figure S7 | 0.98 | 0.75‐1.30 | .934 | ||||
| Nurses | Al‐Eisa and Al‐Abbad, 2013 6 | 116 | 155 | 74.8 | 61.2‐88.5 | |||||
| Abbas et al, 2010 9 | 611 | 937 | 65.2 | 60.0‐70.4 | ||||||
| Abu Tariah et al, 2020 23 | 60 | 94 | 63.8 | 47.7‐80.0 | ||||||
| Alnaami et al, 2019 16 | 156 | 214 | 72.9 | 61.5‐84.3 | ||||||
| Attar, 2014 34 | 130 | 200 | 65.0 | 53.8‐76.2 | ||||||
| Pooled prevalence | 66.9 | 62.9‐70.9 | Figure S9 | 0.95 | 0.80‐1.12 | .557 | ||||
| PTs | Muaidi and Shanb, 2016 15 | 321 | 690 | 46.5 | 41.4‐51.6 | 0.40 a | 0.33‐0.49 | <.0005 | ||
| EMS | Aljerian et al, 2018 28 | 217 | 360 | 60.3 | 52.3‐68.3 | 0.71 a | 0.55‐0.91 | .006 | ||
| Pooled prevalence | 65.0 | 59.4‐70.5 | Figure S2 | |||||||
| Career | Physicians | Bin Homaid et al, 2016 35 | 45 | 61 | 73.8 | 52.2‐95.3 | Reference group | |||
| Nurses | Bin Homaid et al, 2016 35 | 26 | 34 | 76.5 | 47.1‐105.9 | 1.15 | 0.43‐3.06 | .772 | ||
| PTs | Alghadir et al, 2017 7 | 450 | 502 | 89.6 | 81.4‐97.9 | 3.01 a | 1.62‐5.82 | <.0005 | ||
| AT | Bin Homaid et al, 2016 35 | 10 | 12 | 83.3 | 31.7‐135.0 | 1.78 | 0.35‐9.00 | .482 | ||
| ORT | Bin Homaid et al, 2016 35 | 3 | 7 | 42.9 | −5.6 to 91.4 | 0.27 | 0.05‐1.32 | .089 | ||
| Pooled prevalence | 81.4 | 69.3‐93.5 | Figure S3 | |||||||
| Lifetime | Physicians | Alsiddiky et al, 2015 10 | 244 | 411 | 59.4 | 51.9‐66.8 | ||||
| Alzidani et al, 2018 13 | 101 | 138 | 73.2 | 58.9‐87.5 | ||||||
| Al‐Ruwaili and Khalil, 2019 32 | 193 | 254 | 76.0 | 65.3‐86.7 | ||||||
| Pooled prevalence | 68.7 | 57.0‐80.4 | Figure S6 | |||||||
Abbreviations: AT, anesthesia technicians; CI, confidence interval; EMS, emergency medical service personnel; LBP, low back pain; OR, odds ratio; PTs, physical therapists; RT, operation room technicians.
Significant at α = 0.05.
Taking physicians as the reference group, Table 4 shows the ORs of developing LBP for each of the identified category for week, year, and career prevalence periods. For week prevalence, nurses were more likely to develop LBP with a significant OR of 2.35 (95% CI = 1.86‐3.00). For year prevalence, the risk was similar for dentists and nurses with no significant difference. Physical therapists and EMS personnel, however, had a significantly lower risk of LBP than physicians, with ORs of 0.40 (95% CI = 0.33‐0.49) and 0.71 (95% CI = 0.55‐0.91), respectively. For career prevalence, physical therapists had the highest risk of developing LBP, with a significant OR of 3.01 (95% CI = 1.62‐5.82).
3.4.2. Prevalence of LBP by occupational category
Detailed prevalence rates for each occupational category are listed in Table 4 and described below.
Physicians
The week prevalence of LBP among physicians was reported in three studies, 13 , 24 , 37 with a pooled prevalence of 36.4% (Figure S4). Only one study reported month prevalence, and another study reported career prevalence, which were 48.6% 13 and 73.8%, 35 respectively. Year prevalence was reported in five studies, 13 , 16 , 24 , 32 , 33 ranging from 52.9% 33 to 73.4%, 16 with a pooled prevalence of 66.8% (Figure S5). Finally, three studies 10 , 13 , 32 reported lifetime prevalence, with a pooled prevalence of 68.7% (Figure S6).
Dentists
For dentists, only the year prevalence of LBP was identified in the analysis and was reported in three studies, 16 , 27 , 30 ranging between 57.4% 27 and 92.6%, 16 with a pooled prevalence of 67.3% (Figure S7).
Nurses
The week prevalence of LBP among nurses was reported in four studies, 9 , 23 , 36 , 37 ranging from 17.0% 23 to 61.5%, 9 with a pooled prevalence of 45.9% (Figure S8). The year prevalence was reported in five studies 6 , 9 , 16 , 23 , 34 and ranged between 63.8% 23 and 74.8%, 6 with a pooled prevalence of 66.9% (Figure S9). The career prevalence of LBP was reported in one study only (76.5%). 35
Physical therapists
Week, year, and career prevalence rates among physical therapists were reported in one study each, and were 35.7%, 37 46.5%, 15 and 89.6%, 7 respectively.
EMS, AT, and ORT
Only one study 28 reported the prevalence of LBP for EMS, estimating the week and year prevalence to be 37.2% and 60.3%, respectively. For AT and ORT, only their career prevalence was reported in one study (83.3% and 42.9%, respectively). 35
3.5. Duration and intensity of LBP episodes
Table 3 summarizes the information about the duration and/or intensity of LBP episodes that were reported in the studies included in the final analysis. The majority of physicians (86.6%), 32 dentists (80.6%), 30 and physical therapists (85%) 7 described their LBP as acute (less than 4 weeks). For nurses, one study 6 reported that 81.9% of their episodes had lasted for 30 days or less, while another study 36 stated that approximately half of the sample had LBP for more than 2 years and the other half for less than 2 years.
Regarding the intensity of LBP episodes, one study 13 stated that the majority of physicians (59.4%) described their LBP episodes as moderate; while another study 10 reported that around 38% had severe LBP, slightly higher than those who described their pain as mild (34%). One study 32 reported that 68.4% of the physicians rated their episodes as 2 or 3 on a scale of 0‐5. As for dentists, around 66.2% reported moderate levels of LBP. 30 Similarly, most physical therapists (43%) rated their LBP as moderate. 7 On a scale of 1‐5, approximately 70.5% of nurses selected either 2 or 3 to describe their LBP intensity. 36 One study 35 recorded LBP intensity among samples of physicians, nurses, AT, and ORT, and reported that 53.9% described their pain as moderate. Another study 37 found that the overall average of pain, on a scale of 0‐10, among a group of physicians, nurses, and physical therapist was 4.01.
3.6. Risk factors for LBP
Several statistically significant risk factors for LBP among health workers across different prevalence periods were identified in the included studies. The risk factors along with ORs and 95% CIs for each occupational category are shown in Table 5, and were classified under two categories: individual and occupational risk factors. Overall, the most frequently reported individual factors were age, 10 , 16 , 30 body mass index (BMI), 9 , 16 , 33 and gender. 9 , 10 , 15 , 30 , 36 As for occupational risk factors, type of work activities, 6 , 9 , 10 , 30 work setting, 13 , 16 , 34 and specialty 10 , 13 , 30 , 32 were the factors most commonly found to be significant.
TABLE 5.
Individual and occupational risk factors identified for each occupational category
| Occupation | Prevalence period | Risk factor | Reference group | OR | 95% CI | P value | Reference number | |
|---|---|---|---|---|---|---|---|---|
| Physicians | Week | No risk factors identified | ||||||
| Month | No risk factors identified | |||||||
| Year | Individual | Age: 30 to <40 y | 20 to <30 | 1.87 | 1.26‐2.75 | <.05 | 16 | |
| History of back trauma | No history of back trauma |
10.44 11.52 a |
3.79‐28.78 4.14‐32.08 a |
<.05 <.05 a |
16 | |||
| BMI: obesity | Normal weight |
1.72 1.10 a |
1.04‐2.83 1.01‐3.65 a |
<.05 <.05 a |
16 | |||
| BMI: obesity | Not reported | .04 | 33 | |||||
| Occupational | Workplace: secondary and tertiary hospitals | Primary |
1.80 1.32 a |
1.25‐2.59 1.01‐1.76 a |
<.05 <.05 a |
16 | ||
| Prolonged standing working conditions | Prolonged sitting | 1.61 | 1.01‐2.56 | <.05 | 16 | |||
| Specialty: ophthalmology, emergency, anesthesia and intensive care | Not reported | .014 | 32 | |||||
| Career | No risk factors identified | |||||||
| Lifetime | Individual | Age: 31‐40 y | <30 | 2.2 | 1.1‐4.6 | .004 | 10 | |
| Age: 41 to >50 y | <30 | 3.0 | 1.4‐2.2 | .004 | 10 | |||
| Smoking | Not reported | .033 | 13 | |||||
| Nationality: non‐Saudi | Not reported | .02 | 13 | |||||
| Male gender | Females | 1.7 a | 1.1‐2.8 a | .033 a | 10 | |||
| Occupational | Job position: consultant | Resident |
2.5 4.1 a |
1.5‐4.2 2.1‐8.3 a |
.002 <.001 a |
10 | ||
| Job position: registrar | Resident | 2.2 a | 1.2‐4.2 a | .013 a | 10 | |||
| Specialty: surgery | Medicine | 2.0 | 1.3‐3.0 | .001 | 10 | |||
| Specialty: pediatrics | Medicine | 2.4 | 1.3‐4.3 | .001 | 10 | |||
| Specialty: orthopedic | Not reported | .012 | 13 | |||||
| Specialty: gynecology | Not reported | .012 | 13 | |||||
| Specialty: general surgery | Not reported | .012 | 13 | |||||
| Workplace: general hospitals | Not reported | .003 | 13 | |||||
| Working more than 10 h per week in clinic | 1‐10 h | 1.8 | 1.2‐2.7 | <.001 | 10 | |||
| Working more than 10 h per week on bedside | 1‐10 h | 1.8 a | 1.1‐3.0 a | .032 a | 10 | |||
| Stand more than 75% of the workday | Not reported | .024 | 13 | |||||
| Back bending at work | No |
8.2 8.3 a |
5.3‐12.9 5.1‐13.4 a |
<.001 <.0001 a |
10 | |||
| Pulling objects often at work | No |
4.1 3.1 a |
2.4‐7.1 1.7‐5.6 a |
<.001 <.0001 a |
10 | |||
| Severe stress level at work | Not reported | .015 | 13 | |||||
| Dentists | Year | Individual | Female gender | Male | 2.17 a | 1.12‐4.20 a | .021 a | 30 |
| Increasing age | Continuous |
1.068 1.07 a |
1.03‐1.11 1.03‐1.11 a |
<.001 <.001 a |
30 | |||
| Lack of exercise | Exercising | 2.34 | 1.25‐4.36 | .008 | 30 | |||
| Being married | Not reported | <.001 | 30 | |||||
| BMI: obesity | Normal weight |
1.72 1.10 a |
1.04‐2.83 1.01‐3.65 a |
<.05 <.05 a |
16 | |||
| History of back trauma | No history of back trauma |
10.44 11.52 a |
3.79‐28.78 4.14‐32.08 a |
<.05 <.05 a |
16 | |||
| Occupational | Specialty: restorative dentists | General practitioner/maxillofacial dentistry | 2.82 | 1.28‐6.21 | .019 | 30 | ||
| Specialty: Pediatrics/orthodontics | General practitioner/maxillofacial dentistry | 5.21 | 1.71‐15.83 | .019 | 30 | |||
| Specialty: endodontics | General practitioner/maxillofacial dentistry | 2.83 | 1.01‐7.93 | .019 | 30 | |||
| Workplace: secondary and tertiary hospitals | Primary |
1.80 1.32 a |
1.25‐2.59 1.01‐1.76 a |
<.05 <.05 a |
16 | |||
| Experience | Continuous | 1.06 | 1.03‐1.10 | .001 | 30 | |||
| Prolonged standing working conditions | Prolonged sitting | 1.61 | 1.01‐2.56 | <.05 | 16 | |||
| Increasing time spent per patient | Continuous | 1.2 | 1.00‐1.44 | .039 | 30 | |||
| Excessive bending and twisting | Not reported | <.001 | 30 | |||||
| Nurses | Week | Individual | Nationality: Asian | Western | 1.96 | 1.01‐3.83 | .032 | 9 |
| BMI: <25 | ≥30 | 1.67 | 1.02‐2.74 | .029 | 9 | |||
| Female gender | Not reported | .002 | 36 | |||||
| Occupational | Job type: inpatient nurses | Administrative nurses | 1.82 | 1.21‐2.75 | .002 | 9 | ||
| Job type: outpatient nurses | Administrative nurses | 1.79 | 1.15‐2.79 | .006 | 9 | |||
| Use of patients lifting device | No | 1.65 | 1.21‐2.25 | .0008 | 9 | |||
| Carrying patients | No | 2.07 | 1.53‐2.79 | <.0005 | 9 | |||
| Supporting patients during movement | No | 2.5 | 1.67‐3.74 | <.0005 | 9 | |||
| Pushing wheelchair | No | 3.52 | 2.23‐5.58 | <.0005 | 9 | |||
| Year | Individual | Male gender | Females | 2.05 | 1.26‐3.36 | .002 | 9 | |
| Nationality: Middle eastern | Western | 2.43 | 1.02‐5.82 | .027 | 9 | |||
| Nationality: Asian | Western | 2.24 | 1.14‐4.38 | .011 | 9 | |||
| Age: 30 to <40 y | 20 to <30 | 1.87 | 1.26‐2.75 | <.05 | 16 | |||
| History of back trauma | No history of back trauma |
10.44 11.52 a |
3.79‐28.78 4.14‐32.08 a |
<.05 <.05 a |
16 | |||
| BMI: obesity | Normal weight |
1.72 1.10 a |
1.04‐2.83 1.01‐3.65 a |
<.05 <.05 a |
16 | |||
| Occupational | Workplace: secondary and tertiary hospitals | Primary |
1.80 1.32 a |
1.25‐2.59 1.01‐1.76 a |
<.05 <.05 a |
16 | ||
| Working in surgery department | Not reported | 2.2 | 1‐4.8 | <.05 | 34 | |||
| Working in obstetrics & gynecology department | Not reported | 1.5 | 1‐2.1 | <.01 | 34 | |||
| Prolonged standing working conditions | Prolonged sitting | 1.61 | 1.01‐2.56 | <.05 | 16 | |||
| Handling more than five patients per day | 1‐5 patients | 1.9 a | 1.15‐3.56 a | <.05 a | 6 | |||
| Increasing time spent in patient handling | Continuous | 1.4 a | 1.05‐1.70 a | <.05 a | 6 | |||
| Lack of a workplace patient handling policy | Yes | 1.4 a | 1.18‐1.97 a | <.05 a | 6 | |||
| Career | No risk factors identified | |||||||
| Lifetime | Individual | Age: <30 y | ≥50 | 4.74 | 3.06‐7.35 | <.0005 | 9 | |
| PTs | Week | No risk factors identified | ||||||
| Year | Individual | Female gender | Not reported | .024 | 15 | |||
| Career | No risk factors identified | |||||||
| EMS | Week | No risk factors identified | ||||||
| Year | Individual | Smoking | Not reported | .002 | 28 | |||
| Increasing BMI | Not reported | .009 | 28 | |||||
| AT | Career | No risk factors identified | ||||||
| ORT | Career | No risk factors identified | ||||||
Abbreviations: AT, anesthesia technicians; BMI, body mass index; CI, confidence interval; EMS, emergency medical service personnel; OR, odds ratio; ORT, operation room technicians; PTs, physical therapists.
Results are related to adjusted odds ratio.
3.7. Sensitivity analysis
High risk of bias was found for eight of the eligible studies. For this reason, they were excluded from the final analysis. A sensitivity analysis was thus performed to explore whether the pooled prevalence rates would change if high risk‐of‐bias studies were included. Based on the prevalence periods identified in this review, the following periods were extracted from the excluded articles as shown in Table S1: week prevalence for nurses (one study), 8 year prevalence for dentists and medical laboratory technologists (one study each), 22 , 31 career prevalence for physicians and nurses (one study each), 14 , 38 and lifetime prevalence for physicians (three studies). 14 , 25 , 29 One additional study 26 reported the career prevalence for dentists, dental assistants, dental hygienists, and dental technicians combined. Therefore, the prevalence estimate reported in this study was not included in the sensitivity analysis.
The sensitivity analysis revealed that recalculating the lifetime prevalence for physicians after including the high risk‐of‐bias studies was comparable to the results when only the studies with acceptable methodology were included; pooled prevalence = 71.0% (95% CI = 59.4%‐82.6%). For career prevalence across all professional groups, the overall career prevalence was 75.1% (95% CI = 64.5%‐86.1%) when the high risk‐of‐bias studies were included in the analysis, which is slightly lower than the prevalence rate calculated with the lower‐of‐bias studies only. Similarly, no considerable differences were noticed in week nor year prevalence rates across all professional groups when estimates from the high risk‐of‐bias studies were included in the meta‐analysis; pooled prevalence = 42.9% (95% CI = 31.2%‐54.6%) and 63.8% (95% CI = 58.9%‐68.8%), respectively. Therefore, excluding the high risk‐of‐bias studies from the meta‐analyses did not have a substantial effect on the LBP prevalence rates calculated based on methodologically superior studies.
4. DISCUSSION
The literature search in the present review identified 26 eligible studies examining the prevalence of LBP or musculoskeletal disorders including LBP and the associated risk factors among different groups of health workers in Saudi Arabia. Nearly all of these studies were conducted in the last 10 years. This dramatic increase in the number of studies on that topic in recent years indicates the gravity of the problem and the current interest in investigating the main issues of health workers in relation to the development of LBP. This review provides a comprehensive summary of such attempts in the literature. The information provided in this review is expected to increase awareness in the healthcare sector in about the issue of LBP among health workers in Saudi Arabia.
4.1. Prevalence
The meta‐analysis revealed a LBP year prevalence rate of 65.0% for health workers in Saudi Arabia. This is to some degree higher than the rates reported in other cross‐sectional and review studies conducted in the Middle East and internationally. For example, a meta‐analysis conducted in Iran 43 estimated the year prevalence of LBP among health workers to be 58%. Similarly, other cross‐sectional studies reported an annual prevalence of 39%‐61.3% in Turkey, 44 , 45 51.1% in Tunisia, 46 46% in Nigeria, 47 56.9% in Malaysia, 48 and 30% in Ireland. 49 The week prevalence estimated in the current review was also found to be higher than that estimated for their Turkish counterparts (29.5%). 44
Nurses are at higher risk of developing LBP than other health workers in Saudi Arabia considering a week period, with an estimated prevalence of 45.9%. In addition, the estimates computed for nurses in the current review were higher than those reported in other reviews. A meta‐analysis of 22 studies in Iran 50 reported a year prevalence rate among Iranian nurses of 61.2%, which is slightly lower than the rate reported for nurses in this review (66.9%). The worldwide 7‐day and year LBP prevalence rates among nurses were 35% and 55%, respectively, 42 which are also lower than the pooled week and annual prevalence rates for nurses reported in this review.
For physicians, on the other hand, the prevalence rates calculated in this review are somehow comparable with those reported in another systematic review that included studies from the United States, Ireland, Turkey, Spain, and China. 51 That review reported a year prevalence ranging from 33% to 68%, and a lifetime prevalence of 67%. The current review found that the pooled year prevalence of LBP among physicians in Saudi Arabia was 66.8%, and the lifetime prevalence was 68.7%. This might indicate a worldwide similarity among physicians in terms of predisposing factors.
The highest year prevalence of LBP was found among dentists, with a pooled rate of 67.3%, which is also higher than the year prevalence of 56.4% reported in Western countries. 52 Physical therapists, among other health workers in Saudi Arabia, showed the highest risk of developing LBP over their career, with a prevalence rate of 89.6%. This might not be surprising, since physical therapists routinely perform manual therapy techniques and repetitive tasks that sometimes involve heavy physical demands. 53 A previous study found that physical therapists were more vulnerable to work‐related musculoskeletal disorders during their career than other health workers. 54 The results of this review confirm this finding.
It should be mentioned that the lifetime prevalence described in this review must be inferred with caution, as it represents physicians only. This might also explain the higher rate reported for career prevalence, as this rate was computed based on data taken from different categories (physicians, nurses, physical therapists, ORT, and AT).
In some instances, the prevalence rates for the same occupational category showed some variability between the studies. This was mainly evident in the year prevalence for dentists. Perhaps the lack of a uniform case definition of LBP might explain this variability. Although half of the studies standardized the definition of LBP utilizing the Standardized Nordic Musculoskeletal Questionnaire, and one study utilized the Cornell Musculoskeletal Discomfort Questionnaire, the remaining studies recorded and defined LBP incidents using self‐designed questionnaires. However, this high variability in prevalence rates was not found in the year prevalence among nurses, which was reported in five studies and ranged between 63.8% 23 and 74.8%, 6 regardless of the LBP definition choice. This indicates that other factors might lead to this variability as well, such as the setting where the study was conducted. Two studies in the current analysis concluded that the prevalence of LBP differed based on type of healthcare facility. 13 , 16 Another factor could be the specialty, as some studies found significant differences in LBP prevalence among physicians and dentists based on their specialty. 10 , 13 , 30 , 32
Another observed variability between the 18 studies that were included in the analyses (due to having low or medium risk of bias) was in the eligibility criteria for LBP type (specific vs nonspecific). Although four studies 13 , 15 , 32 , 36 were clear about only including cases with nonspecific LBP by excluding those with LBP secondary to other pathology or abnormality, the rest did not state precise eligibility criteria related to the type of LBP. At the same time, all 18 studies defined LBP as “work‐related LBP” and/or attributed it to work‐related factors, and none was linked to disease. This inconsistency made it difficult to classify cases into specific and nonspecific, and may have contributed to the variability in prevalence rates between the studies.
4.2. Duration and intensity of LBP episodes
Estimating and comparing the duration and intensity of LBP episodes was challenging in this review for two reasons. First, only five 6 , 7 , 30 , 32 , 36 out of the 18 studies reported the duration, and eight articles 7 , 10 , 13 , 30 , 32 , 35 , 36 , 37 provided data about the intensity. This may provide insufficient estimates about the actual duration and intensity of LBP. Second, studies lacked standardized methods for reporting duration and intensity. This inconsistency makes comparisons among occupational categories difficult.
Overall, duration of LBP episodes was reported for physicians, dentists, nurses, and physical therapists, with approximately 80%‐86% describing their pain as acute (less than 4 weeks). Intensity can be described as moderate for physicians, dentists, nurses, physical therapists, AT, and ORT based on the data reported. However, these inferences must be made with caution, as further studies are needed to provide adequate estimates and comparisons of the duration and intensity of LBP episodes among health workers in Saudi Arabia.
4.3. Risk factors
4.3.1. Individual risk factors
The analysis of individual risk factors of LBP in health workers in Saudi Arabia revealed that as age and BMI increased, so did the likelihood of developing LBP. However, one study 9 reported a higher prevalence of LBP among participants with lower BMI and younger age. A similar conflict was found for gender, as three studies 15 , 30 , 36 reported that female gender was associated with higher LBP prevalence, while two studies 9 , 10 reported that male gender was a significant risk factor of LBP. Nevertheless, increasing age and weight, and female gender are well‐documented risk factors of LBP in the literature. 55 Other relatively common risk factors reported were smoking and nationality, with non‐Saudi health workers being more vulnerable to developing LBP. One study hypothesized that this might be because the Saudi participants in their study were younger than non‐Saudis. 13 Another possible explanation could be that the contracts of non‐Saudi staff are renewed every year based on their performance, 56 and job insecurity was found to be significantly associated with LBP, 57 which may also explain this finding.
4.3.2. Occupational risk factors
The majority of occupational risk factors were related to the type of activities performed at work with high physical demands, including those requiring bending and twisting, and lifting and pulling objects. Alsiddiky et al 10 reported that clinicians who often performed back bending and pulling objects at work had a risk of LBP up to eight times higher. Back flexion, especially when combined with lifting weights, has serious consequences on the lower back, as it highly increases the intradiscal pressure, 58 and may damage the discs. Similarly, work activities involving patient manual‐handling, mainly among nurses, were also identified as risk factors, such as transferring and carrying patients, supporting patients during movement, pushing wheelchairs, increased time spent handling patients, and number of patients handled. The highest risk of LBP was found among nurses who often pushed wheelchairs (three times higher). 9 These findings are in agreement with previous reviews conducted internationally. 57 , 59 , 60 Some explanations of the relationship between these types of activities and LBP in nurses were reported, such as a reduction in the ability to endure the physical load among those with weak muscle strength 61 or lack of knowledge about ergonomically safe patient‐handling techniques. 45 Organizational factors may also play a role, as Al‐Eisa and Al‐Abbad 6 concluded that the absence of a workplace patient handling policy was a significant risk factor for LBP in nurses. One study, 9 however, reported that the utilization of patient‐lifting devices does not protect nurses against LBP, as it was found to be positively correlated with LBP occurrence. Nevertheless, it was previously reported that it might take up to 4 years of follow‐up to detect the effect of those devices on reducing the LBP incidence. 60 Moreover, the beneficial effect of implementing patient‐lifting devices on LBP and musculoskeletal disorders among health workers is well documented in the literature among newly recruited staff 60 and when combined with other preventive strategies. 62
Working department and workplace were also recognized as risk factors of LBP. Those who worked in hospitals (secondary, tertiary, or general hospitals) were at higher risk of LBP than their counterparts who worked in small or primary health centers, which is consistent with a previous review. 57 This is possibly due to extended working hours and higher patient loads associated with stressful working environments. 63 Furthermore, nurses who worked in surgical departments were found to be twice more likely to suffer from LBP than those in other departments, 35 which is in agreement with an earlier report. 64 Similarly, inpatient and outpatients nurses, as compared with administrative nurses, were at a higher risk of LBP. 9 Variations in workplace equipment 11 , 60 , 65 and work systems and duties 6 , 44 , 48 , 66 could explain these findings.
Certain subspecialties among physicians and dentists were also noticed to be more susceptible to LBP. Among dentists, pediatric dentists, orthodontists, restorative dentists, and endodontic dentists were found to be at a higher risk of LBP in comparison with general dentists and maxillofacial surgeons. A greater risk was found for orthodontics and pediatrics dentist (five times higher), followed by endodontics and restorative dentists (approximately three times higher). 30 Maintaining an awkward static posture for extended periods of time is the most commonly reported explanation for such high risk of LBP among different dental specialties. 30 , 67 Similarly, among physicians, orthopedic and general surgeons, gynecologists, pediatricians, ophthalmologists, emergency and intensive care physicians, and anesthesiologists were at a greater risk of LBP development than other specialties, which can be explained by extended procedure times and high physical and mental demands in those specialties. 13 , 30
High stress level at work is a well‐documented risk factor of LBP, 57 , 63 and its negative impact on work performance among health workers has been established. 68 However, two studies included in the review examined stress, and only one found it to be significant. 13 Earlier reports found that prolonged standing induces LBP. This was explained by multiple reasons such as standing in more lumbar lordosis 69 and alteration of muscle activities around the back. 70 In this review, moreover, it was found that those who spent most of their time working in a standing position were around 1.5 time more likely to develop LBP. 16 However, it has been suggested that sitting breaks alone do not protect from the harmful effect of prolonged standing on the lower back region, and those periods of rest should include other types of activities. 71 Years of experience was also found to have a significant association with LBP. This could be a risk factor because of its direct proportionality with age, which was identified as a significant risk factor, as described earlier.
4.4. Recommendations for occupational health
This review identified a number physical work‐related factors associated with LBP occurrence, ranging from maintenance of static posture combined with excessive back bending and twisting among dentists, to manual patient‐handling and repetitive heavy lifting among nurses. Possibly, a midpoint between the two ends of physical demands could help to minimize the risk of LBP in these two categories. For example, dentists could take more frequent breaks that include walking around and performing some stretching exercises. 30 Nurses, on the other hand, would be recommended to take a rest from heavy physical workloads on a regular basis. 6 Modifying the workplace, 30 , 33 implementing safety polices at work, 6 revising the working hours, 10 recruiting enough staff, 6 , 16 and increasing awareness about safe ergonomics at work 6 , 15 are recommended for both groups in addition to other health workers. Additionally, several studies included in this analysis documented the benefits of exercising as a protective factor against LBP. 6 , 16 , 30 Occupational health workers are recommended to spread the knowledge about the beneficial effects of regular exercise in minimizing the risk of LBP occurrence. The prophylactic measures suggested here are provided for the healthcare sector in Saudi Arabia and potentially in other countries, since there are universal similarities in the predisposing factors of LBP.
4.5. Study limitations
A potential limitation of this review is the occupational categories covered. Although the search criteria included all possible health professionals and/or health associate professionals, only seven categories were identified and included. Another limitation is that the representation of the occupations included in the analysis was not equal. This was due to a general lack of studies targeting some categories. A third limitation is that some regions of Saudi Arabia were not covered because of the lack of studies in those regions. A fourth limitation is the inconsistency of the eligibility criteria among the included studies in terms of type of LBP, which made it difficult to categorize the cases as specific and nonspecific LBP. Furthermore, the case definition of LBP in the studies included in the analysis was not consistent, and the duration and intensity of LBP episodes were not recorded by all studies. These limitations may have influenced the prevalence rate estimates reported in this review. A fifth limitation is that only one reviewer performed the selection of the studies, and only English articles were considered for eligibility in this review. Finally, as only cross‐sectional studies were included, causal relationships between LBP and the identified risk factors cannot be established.
4.6. Recommendations for future research
Based on the results of the present review and to further improve the overall understanding of LBP prevalence in the healthcare sector in Saudi Arabia, the following recommendations are provided: (a) future studies need to examine the frequency and risk factors of LBP among other common health workers such as pharmacists, medical laboratory technologists, and other allied health workers; (b) future studies need to be conducted in other regions of Saudi Arabia such as Northern Borders, Jawf, Al‐Madinah, Al‐Bahah, Jazan, Najran, and Al‐Qassim; (c) future studies need to report the duration and intensity of LBP episodes using a consistent method, and to use a uniform, standardized case definition of LBP, such as the Standardized Delphi Definitions of Low Back Pain Prevalence, 72 to facilitate the comparison of prevalence rates between different groups; and (d) future studies need to include precise criteria regarding the type of LBP (specific vs nonspecific), as such data would add important information on the type of LBP in relation to prevalence rates.
5. CONCLUSIONS
Compared with the rest of the world, LBP is highly prevalent among health workers in Saudi Arabia, with rates of 40.8%, 65.0%, and 81.4% for week, year, and career prevalence, respectively. Nurses were more susceptible to LBP over a 7‐day period, while physical therapists were more likely to develop LBP over their career. Occupational risk factors were mostly related to work‐related activities and workplace facilities. To limit LBP and minimize its consequences, working policies in the Saudi healthcare sector might need to be reviewed, and proper protective measures need to be developed. Moreover, enough staff need to be recruited to reduce the patient‐to‐staff ratio and working hours and thus decrease the workload. Work organizations need to consider adopting prophylactic strategies, including redesigning the workplace, adequately implementing lifting devices, and appropriate education and training of staff about correct patient handling techniques, safe ergonomics and body mechanics, and health benefits of exercising. Such modifications would help to reduce the incidence of LBP and associated disabilities among health workers in Saudi Arabia. This, in turn, would improve the quality of patient care by keeping health staff active and productive during their career.
DISCLOSURE
Approval of the research protocol: N/A Informed consent: N/A Registry and the registration no. of the study/trial: N/A Animal studies: N/A Conflict of Interest: Authors declare no conflict of interests for this article.
AUTHOR CONTRIBUTIONS
Hamad S. Al Amer performed the literature search, data analyses, and wrote and revised the manuscript.
Supporting information
Fig S1‐S9
Table S1
ACKNOWLEDGMENTS
The author would like to thank Dr Mohamed ELdesoky and Dr Ayman Honin for conducting the risk‐of‐bias assessment.
Al Amer HS. Low back pain prevalence and risk factors among health workers in Saudi Arabia: A systematic review and meta-analysis. J Occup Health. 2020;62:e12155 10.1002/1348-9585.12155
REFERENCES
- 1. Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205‐217. [DOI] [PubMed] [Google Scholar]
- 2. Al‐Arfaj AS, Al‐Saleh SS, Alballa SR, et al. How common is back pain in Al‐Qaseem region. Saudi Med J. 2003;24(2):170‐173. [PubMed] [Google Scholar]
- 3. Elnaggar RK, Elshazly FA, Elsayed WS, Ahmed AS. Determinants and relative risks of low back pain among the employees in Al‐Kharj area, Saudi Arabia. Eur J Sci Res. 2015;135(3):299‐308. [Google Scholar]
- 4. Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290(18):2443‐2454. [DOI] [PubMed] [Google Scholar]
- 5. Al Wassan K, Almas K, Al Shethri S, Al QM. Back & neck problems among dentists and dental auxiliaries. J Contemp Dent Pract. 2001;2(3):17‐30. [PubMed] [Google Scholar]
- 6. Al‐Eisa E, Al‐Abbad H. Occupational back pain among rehabilitation nurses in Saudi Arabia: the influence of knowledge and awareness. Workplace Health Saf. 2013;61(9):401‐407. [DOI] [PubMed] [Google Scholar]
- 7. Alghadir A, Zafar H, Iqbal ZA, Al‐Eisa E. Work‐related low back pain among physical therapists in Riyadh, Saudi Arabia. Workplace Health Saf. 2017;65(8):337‐345. [DOI] [PubMed] [Google Scholar]
- 8. Al Dajah S, Al DA. Prevalence and risk factors of low back pain among nurses in Sudayr region. Eur Sci J. 2013;9(33):198‐205. [Google Scholar]
- 9. Abbas MA, Zaid LZA, Fiala LA, Alhamdan NA. Prevalence and risk factors of low back pain among nurses in four tertiary care hospitals at King Fahad Medical City, Riyadh, KSA. The Med J Cairo Univ. 2010;78(2):219‐223. [Google Scholar]
- 10. Alsiddiky AM, Algarni N, Alluhaidan A. Prevalence and associated factors of low back pain among clinicians of a major referral hospital. Med J Malaysia. 2015;70:12‐17. [PubMed] [Google Scholar]
- 11. Meisha DE, Alsharqawi NS, Samarah AA, Al‐Ghamdi MY. Prevalence of work‐related musculoskeletal disorders and ergonomic practice among dentists in Jeddah, Saudi Arabia. Clin Cosmet Investig Dent. 2019;11:171‐179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alnefaie M, Alamri A, Hariri A, et al. Musculoskeletal symptoms among surgeons at a tertiary care center: a survey based study. Med Arch. 2019;73(1):49‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alzidani TH, Alturkistani AM, Alzahrani BS, Aljuhani AM, Alzahrani KM. Prevalence and risk factors of low back pain among Taif surgeons. Saudi J Health Sci. 2018;7(3):172‐177. [Google Scholar]
- 14. Aseri KS, Mulla AA, Alwaraq RM, Bahannan RJ. Characterizing occupational low back pain among surgeons working in ministry of health hospitals in Jeddah city: prevalence, clinical features, risk, and protective factors. KAU Med Sci. 2019;26(2):19‐34. [Google Scholar]
- 15. Muaidi QI, Shanb AA. Prevalence causes and impact of work related musculoskeletal disorders among physical therapists. J Back Musculoskelet Rehabil. 2016;29(4):763‐769. [DOI] [PubMed] [Google Scholar]
- 16. Alnaami I, Awadalla NJ, Alkhairy M, et al. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet Disord. 2019;20(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization . Mapping occupations to the international standard classification: classifying health workers. www.who.int/hrh/statistics/workforce_statistics. Published April 2010. Accessed March 2020.
- 18. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934‐939. [DOI] [PubMed] [Google Scholar]
- 19. Islam RM, Oldroyd J, Karim MN, et al. Systematic review and meta‐analysis of prevalence of, and risk factors for, pelvic floor disorders in community‐dwelling women in low and middle‐income countries: a protocol study. BMJ Open. 2017;7(6):e015626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Neyeloff JL, Fuchs SC, Moreira LB. Meta‐analyses and forest plots using a Microsoft excel spreadsheet: step‐by‐step guide focusing on descriptive data analysis. BMC Res Notes. 2012;5(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327(7414):557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Abduljabbar TA. Musculoskeletal disorders among dentists in Saudi Arabia. Pak Oral Dental J. 2008;28(1):135‐144. [Google Scholar]
- 23. Abu Tariah H, Nafaic S, Alajmia M, Almutairi F, Alanazi B. Work‐related musculoskeletal disorders in nurses working in the kingdom of Saudi Arabia. Work. 2020;65(2):421‐428. [DOI] [PubMed] [Google Scholar]
- 24. Al Shammari M, Hassan A, Al Dandan O, Al Gadeeb M, Bubshait D. Musculoskeletal symptoms among radiologists in Saudi Arabia: a multi‐center cross‐sectional study. BMC Musculoskelet Disord. 2019;20(1):541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Alamri A, Tedla JS, Ahmad I, Laftal A, Al GA. Musculoskeletal disorders among ophthalmologists in the kingdom of Saudi Arabia: a cross‐sectional study. KKU J Health Sci. 2018;3(1):7‐12. [Google Scholar]
- 26. Alghadir A, Zafar H, Iqbal ZA. Work‐related musculoskeletal disorders among dental professionals in Saudi Arabia. J Phys Ther Sci. 2015;27(4):1107‐1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aljanakh M, Shaikh S, Siddiqui AA, Al‐Mansour M, Hassan SS. Prevalence of musculoskeletal disorders among dentists in the Ha'il region of Saudi Arabia. Ann Saudi Med. 2015;35(6):456‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aljerian N, Alshehri S, Masudi E, Albawardi AM, Alzahrani F, Alanazi R. The prevalence of musculoskeletal disorders among EMS personnel in Saudi Arabia, Riyadh. Egypt J Hosp Med. 2018;73(1):5777‐5783. [Google Scholar]
- 29. Almalki M, Alkhudhayri MH, Batarfi AA, et al. Prevalence of low back pain among medical practitioners in a tertiary care hospital in Riyadh. Saudi J Sport Med. 2016;16(3):205‐209. [Google Scholar]
- 30. Al‐Mohrej OA, AlShaalan NS, Al‐Bani WM, Masuadi EM, Almodaimegh HS. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: a cross‐sectional study. BMJ Open. 2016;6(6):e011100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. AlNekhilan AF, AlTamimi AM, AlAqeel BY, AlHawery AA, AlFadhel SF, Masuadi EM. Work‐related musculoskeletal disorders among clinical laboratory workers. Avicenna J Med. 2020;10(1):29‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Al‐Ruwaili B, Khalil T. Prevalence and associated factors of low back pain among physicians working at King Salman Armed Forces Hospital, Tabuk, Saudi Arabia. Open Access Maced J Med Sci. 2019;7(17):207‐2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Alsultan A, Alahmed S, Alzahrani A, Alzahrani F, Masuadi E. Comparison of musculoskeletal pain prevalence between medical and surgical specialty residents in a major hospital in Riyadh, Saudi Arabia. J Musculoskelet Surg Res. 2018;2(4):161‐166. [Google Scholar]
- 34. Attar SM. Frequency and risk factors of musculoskeletal pain in nurses at a tertiary centre in Jeddah, Saudi Arabia: a cross sectional study. BMC Res Notes. 2014;7(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bin Homaid M, Abdelmoety D, Alshareef W, et al. Prevalence and risk factors of low back pain among operation room staff at a tertiary care center, Makkah, Saudi Arabia: a cross‐sectional study. Ann Occup Environ Med. 2016;28(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Keriri H. Prevalence and risk factors of low back pain among nurses in operating rooms, Taif, Saudi Arabia. Am J Res Commun. 2013;1(11):45‐70. [Google Scholar]
- 37. Mohamed SHP, Al Amer HS. Prevalence of work‐related low back pain among health care professionals in Tabuk, Saudi Arabia. Majmaah J Health Sci. 2019;7(1):52‐65. [Google Scholar]
- 38. Gaowgzeh RAM. Low back pain among nursing professionals in Jeddah, Saudi Arabia: prevalence and risk factors. J Back Musculoskelet Rehabil. 2019;32(4):555‐560. [DOI] [PubMed] [Google Scholar]
- 39. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264‐269. [DOI] [PubMed] [Google Scholar]
- 40. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233‐237. [DOI] [PubMed] [Google Scholar]
- 41. Hedge A, Morimoto S, Mccrobie D. Effects of keyboard tray geometry on upper body posture and comfort. Ergonomics. 1999;42(10):1333‐1349. [DOI] [PubMed] [Google Scholar]
- 42. Davis KG, Kotowski SE. Prevalence of musculoskeletal disorders for nurses in hospitals, long‐term care facilities, and home health care: a comprehensive review. Hum Factors. 2015;57(5):754‐792. [DOI] [PubMed] [Google Scholar]
- 43. Mehrdad R, Shams‐Hosseini NS, Aghdaei SM, Yousefian MM. Prevalence of low back pain in health care workers and comparison with other occupational categories in Iran: a systematic review. Iran J Med Sci. 2016;41(6):467‐478. [PMC free article] [PubMed] [Google Scholar]
- 44. Şimşek Ş, Yağcı N, Şenol H. Prevalence and risk factors of low back pain among health‐care workers in Denizli. Agri. 2017;29(2):71‐78. [DOI] [PubMed] [Google Scholar]
- 45. Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs. 2009;65(3):516‐524. [DOI] [PubMed] [Google Scholar]
- 46. Bejia I, Younes M, Jamila HB, et al. Prevalence and factors associated to low back pain among hospital staff. Joint Bone Spine. 2005;72(3):254‐259. [DOI] [PubMed] [Google Scholar]
- 47. Omokhodion F, Umar U, Ogunnowo B. Prevalence of low back pain among staff in a rural hospital in Nigeria. Occup Med. 2000;50(2):107‐110. [DOI] [PubMed] [Google Scholar]
- 48. Wong T, Teo N, Kyaw M. Prevalence and risk factors associated with low back among health care providers in a District Hospital. Malays Orthop J. 2010;4(2):23‐28. [Google Scholar]
- 49. Cunningham C, Flynn T, Blake C. Low back pain and occupation among Irish health service workers. Occup Med. 2006;56(7):447‐454. [DOI] [PubMed] [Google Scholar]
- 50. Azizpour Y, Delpisheh A, Montazeri Z, Sayehmiri K. Prevalence of low back pain in Iranian nurses: a systematic review and meta‐analysis. BMC Nurs. 2017;16(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hengel KMO, Visser B, Sluiter JK. The prevalence and incidence of musculoskeletal symptoms among hospital physicians: a systematic review. Int Arch Occup Environ Health. 2011;84(2):115‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lietz J, Kozak A, Nienhaus A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: a systematic literature review and meta‐analysis. PLoS One. 2018;13(12):e0208628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Glover W, McGregor A, Sullivan C, Hague J. Work‐related musculoskeletal disorders affecting members of the chartered society of physiotherapy. Physiotherapy. 2005;91(3):138‐147. [Google Scholar]
- 54. Wang SY, Liu LC, Lu MC, Koo M. Comparisons of musculoskeletal disorders among ten different medical professions in Taiwan: a nationwide, population‐based study. PLoS One. 2015;10(4):e0123750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769‐781. [DOI] [PubMed] [Google Scholar]
- 56. Khawaja RA, Sikander R, Khawaja AA, Jareno RJM, Halepota AT. Medically certified sickness absence among health care workers. J Pak Med Assoc. 2012;62(9):900‐904. [PubMed] [Google Scholar]
- 57. Lorusso A, Bruno S, L'abbate N. A review of low back pain and musculoskeletal disorders among Italian nursing personnel. Ind Health. 2007;45(5):637‐644. [DOI] [PubMed] [Google Scholar]
- 58. Wilke HJ, Neef P, Caimi M, Hoogland T, Claes LE. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine. 1999;24(8):755‐762. [DOI] [PubMed] [Google Scholar]
- 59. Anderson SP, Oakman J. Allied health professionals and work‐related musculoskeletal disorders: a systematic review. Saf Health Work. 2016;7(4):259‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Burdorf A, Koppelaar E, Evanoff B. Assessment of the impact of lifting device use on low back pain and musculoskeletal injury claims among nurses. Occup Environ Med. 2013;70(7):491‐497. [DOI] [PubMed] [Google Scholar]
- 61. De Looze MP, Zinzen E, Caboor D, Van Roy P, Clarijs JP. Muscle strength, task performance and low back load in nurses. Ergonomics. 1998;41(8):1095‐1104. [DOI] [PubMed] [Google Scholar]
- 62. Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup Environ Med. 2003;60(9):E6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Shieh S, Sung F, Su C, Tsai Y, Hsieh VC. Increased low back pain risk in nurses with high workload for patient care: a questionnaire survey. Taiwan J Obstet Gynecol. 2016;55(4):525‐529. [DOI] [PubMed] [Google Scholar]
- 64. Tezel A. Musculoskeletal complaints among a group of Turkish nurses. Int J Neurosci. 2005;115(6):871‐880. [DOI] [PubMed] [Google Scholar]
- 65. Klein M, Andersen LP, Alamili M, Gogenur I, Rosenberg J. Psychological and physical stress in surgeons operating in a standard or modern operating room. Surg Laparosc Endosc Percutan Tech. 2010;20(4):237‐242. [DOI] [PubMed] [Google Scholar]
- 66. Awosan KJ, Yikawe SS, Oche OM, Oboirien M. Prevalence, perception and correlates of low back pain among healthcare workers in tertiary health institutions in Sokoto, Nigeria. Ghana Med J. 2017;51(4):164‐174. [PMC free article] [PubMed] [Google Scholar]
- 67. Hayes M, Cockrell D, Smith D. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009;7(3):159‐165. [DOI] [PubMed] [Google Scholar]
- 68. Lindegård A, Larsman P, Hadzibajramovic E, Ahlborg G. The influence of perceived stress and musculoskeletal pain on work performance and work ability in Swedish health care workers. Int Arch Occup Environ Health. 2014;87(4):373‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sorensen CJ, Norton BJ, Callaghan JP, Hwang C, Van Dillen LR. Is lumbar lordosis related to low back pain development during prolonged standing? Man Ther. 2015;20(4):553‐557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Marshall PW, Patel H, Callaghan JP. Gluteus medius strength, endurance, and co‐activation in the development of low back pain during prolonged standing. Hum Mov Sci. 2011;30(1):63‐73. [DOI] [PubMed] [Google Scholar]
- 71. Gallagher KM, Campbell T, Callaghan JP. The influence of a seated break on prolonged standing induced low back pain development. Ergonomics. 2014;57(4):555‐562. [DOI] [PubMed] [Google Scholar]
- 72. Dionne CE, Dunn KM, Croft PR, et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine. 2008;33(1):95‐103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1‐S9
Table S1


