“Can we just do it on the phone? I don’t have internet.” The voice was familiar, but the fear and uncertainty tinged with a hint of frustration in what otherwise should have been a routine follow-up visit were new. Telemedicine in the time of pandemic novel coronavirus disease 2019 (COVID-19) had arrived, and neither patient nor doctor knew what to make of it.
The COVID-19 pandemic has served as a stress test for a multitude of sectors of our society. The fault lines that marginalized its most vulnerable members in the best of times now have the potential to expand into chasms. As our healthcare delivery systems pivot to adapt to a challenge, the scope of which it has not seen in more than a century, we increasingly look to technological solutions to help span these divides.
Once thought of as a science fiction fantasy, telemedicine has evolved over the decades into a seemingly always on-the-horizon solution for healthcare access challenges in rural communities; never gaining much widespread traction beyond its use in neurology for remote stroke assessment. Healthcare providers faced with the need to maintain continuity of and access to care have struggled to remain financially solvent in the setting of physical distancing guidelines. As a result, telemedicine has been thrust into center stage as a potential solution to current challenges.
Telemedicine solutions come in 2 forms: audio-only encounters typically conducted via mobile phone or traditional landline telephone, or synchronous 2-way audio–video conferencing. Although very few comparative effectiveness studies between modalities have been conducted, synchronous video conferencing adds the capability to perform visual medication reconciliation, review test results via screenshare capabilities, and perform limited elements of the physical examination such as jugular vein and lower extremity edema assessment. Videoconferencing can give providers new context to the realities of a patient’s living conditions and offer the beginnings of a home safety assessment.
A successful transition to telemedicine requires the intersection of at least 3 key factors: access to broadband internet, an internet-capable device, and sufficient technology literacy to take advantage of the first 2 factors.
Under the most favorable of estimates, the Federal Communications Commission estimated in the Eighth Broadband Progress Report, published in 2019, that 19 million Americans lack access to fixed broadband service. This disparity is disproportionately experienced in rural communities where 1 in 4 people do not have access. The quality of these data have come under heavy scrutiny by Commissioner Jessica Rosenworcel, who notes that this report deserves a “failing grade” and that we should “stop relying on data [that] we know [are] wrong.”1 An independent advocacy group, Broadband Now, estimates that the true number may be closer to 42 million Americans.2 These national data rely on self-reporting from internet service providers. Real-world testing in Pennsylvania revealed that median speeds for most of the state did not meet the federal definition for broadband defined by the Federal Communications Commission as download speeds of at least 25 Mbps and upload speeds of at least 3 Mbps.3
Access by no means indicates subscription, of which a key component is affordability. On closer examination of broadband access, a stark landscape emerges. Urban centers are not immune to shortfalls in access. In 2018 New York City released Truth in Broadband: Access and Connectivity, which noted that 31% of households in New York City lack a home broadband subscription. The rates of absence of connectivity are higher for black and Hispanic residents (32% and 33%, respectively) than among white residents (21%) of the city. The city’s poorest experience a similar fate with 56% lacking a broadband connection.
Our collective failure to treat widespread access to high-speed internet as the public utility that it has become sets the stage for reliance on expensive mobile data plans to fill the connectivity void. In 2018, the United States was the 5th most expensive mobile data market by median gigabyte price among European Union and Organization for Economic Co-operation and Development countries.4,5
On the unsteady foundation of the preexisting digital divide, a new tower of inequity in access to care will be built in the era of postpandemic recovery unless decisive action is taken. As a first step, the Centers for Medicare and Medicaid Services have ensured that patients and healthcare providers are not penalized for lack of broadband connectivity by ensuring, in many cases, telephone and video-based telemedical activities are viewed and reimbursed similarly. This will help to mitigate unintended barriers to accessing care resulting from unequal access to high-speed internet required for optimal video interactions; however, these changes are currently only temporary and must be made permanent.
As the United States transitions to a phased reopening, national guidelines released by the White House recommend that vulnerable individuals continue to shelter in place. The definition casts a wide net that includes millions of people “with serious underlying health conditions, including high blood pressure, chronic lung disease, diabetes [mellitus], obesity, asthma, and those whose immune system is compromised such as by chemotherapy for cancer and other conditions requiring such therapy.” Increasing availability of affordable access to high-speed internet and telemedicine devices will be crucial if we are to ensure that all Americans have access to the care they need in the next stage of this pandemic. As this field grows, additional research is needed to help outline best practices for telemedicine implementation with the recognition that these tools are not to be used indiscriminately.
The COVID-19 pandemic has demonstrated the power of telemedicine to complement in-person visits between clinicians and their patients and expand access to care. However, if we fail to get this right, instead of clumsy attempts at video visits and “can we do this over the phone?” we just may hear nothing at all from our forgotten Americans.
Figure.
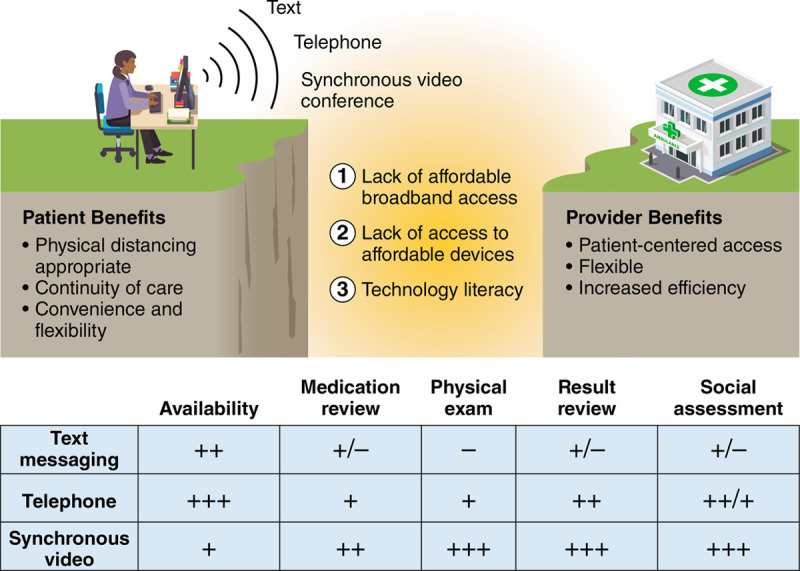
The telemedicine landscape: modalities, benefits, and barriers to implementation.
Disclosures
None.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.Federal Communications Commission. Statement of Commissioner Jessica Rosenworcel, Dissenting. Accessed 8 June 2020. https://docs.fcc.gov/public/attachments/FCC-19-44A4.pdf.
- 2.Busby J, Tanberk J. FCC Reports Broadband Unavailable to 21.3 Million Americans, BroadbandNow Study Indicates 42 Million Do Not Have Access. BroadbandNow Research; Accessed 8 June 2020. https://broadbandnow.com/research/fcc-underestimates-unserved-by-50-percent. [Google Scholar]
- 3.Meinrath SD, Bonestroo H, Bullen G, Jansen A, Mansour S, Mitchell C, Ritzo C, Thieme N. Broadband Availability and Access in Rural PennsylvaniaJune 2019The Center for Rural Pennsylvania; Accessed 8 June 2020.https://www.rural.palegislature.us/broadband/Broadband_Availability_and_Access_in_Rural_Pennsylvania_2019_Report.pdf [Google Scholar]
- 4.Pennsylvania House of Representatives Presentation on the telecommunications industryMarch 22, 2017Consumer affairs committee public hearing; Accessed 8 June 2020. https://www.legis.state.pa.us/WU01/LI/TR/Transcripts/2017_0039T.pdf [Google Scholar]
- 5.The state of 4G pricing Digital Fuel Monitor 10th releaseOctober 2018Rewheel; Accessed 8 June 2020. http://research.rewheel.fi/downloads/The_state_of_4G_pricing_DFMonitor_10th_release_2H2018_PUBLIC.pdf [Google Scholar]


