Abstract
What is known and objective
The HbA1C marker used in assessing diabetes control quality is not sufficient in diabetes patients with thalassaemia.
Case description
A male diabetic patient with thalassaemia was hospitalized due to distal neuropathic pain, right toe trophic ulcer, unacceptable five‐point glycaemic profile and recommended HbA1C value. After simultaneously initiated insulin therapy and management of ulcer by hyperbaric oxygen, the patient showed improved glycaemic control and ulcer healing, which led to the patient's discharge.
What is new and conclusion
In thalassaemia and haemoglobinopathies, due to discrepancies in the five‐point glycaemic profile and HbA1C values, it is necessary to measure HbA1C with a different method or to determine HbA1C and fructosamine simultaneously.
Keywords: diabetes, fructosamine, glycaemic control, glycaemic profile, HbA1C, thalassaemia
The HbA1C marker used in assessing diabetes control quality is not sufficient in diabetes patients with thalassaemia. In thalassaemia and haemoglobinopathies, due to discrepancies in the five‐point glycaemic profile and HbA1C values, it is necessary to measure HbA1C with a different method or to determine HbA1C and fructosamine simultaneously.
1. WHAT IS KNOWN
The major functions of haemoglobin are the transport oxygen from the lungs to peripheral tissues, and the transport of carbon dioxide in the opposite direction. The flexible haemoglobin structure enables such fine‐tuned processes.1 A haemoglobin molecule is composed of four polypeptide globin chains that contain haem. Haem has a protoporphyrin ring made up of four pyrrole rings and a central iron ion in the reduced, ferrous state (Fe2+). Contrary to its relatively unstable, ferric state, ferrous state of iron ion enables the binding of oxygen.1, 2 Haemoglobin A constitutes about 97% of the total haemoglobin, thus being the most common form of haemoglobin in humans. It is composed of two α (141 amino acids) and two β (146 amino acids) chains. HbA2 is composed of two α and two δ chains and comprises 2.2%‐3.5% of an adult's haemoglobin.3, 4 Inherited diseases that affect any part of haemoglobin components syntheses alter haemoglobin structure and biochemical properties with different physiological and clinical significance.1, 3, 4
Thalassaemia is a group of inherited diseases, characterized by abnormal production of one or more α or β globin chains with subsequent imbalance in haemoglobin (Hb) production. Red blood cells (RBC) in thalassaemia syndromes are prone to medullary or extramedullary haemolysis due to membrane damage induced by non‐matched globin chains.5, 6 α‐thalassaemia occurs when one or more of the genes that produce α‐globin chains is absent or mutated. The α‐thalassaemia deletions remove either one or two α‐globin genes on each chromosome,7 and in cases where the foetus lacks all four α‐globin genes, Bart's hydrops in utero occurs. In the cases where three genes deletion are present, haemoglobin H (HbH) disease occurred. The carriers with localized deletions on two or one α globin gene are asymptomatic with mild or with no anaemia. 8
β‐thalassaemia minor (β0/β+ or β/β+) is a heterozygous type of usually asymptomatic anaemia, with observed mild to moderate anaemia and a slight increase in HbA2 and HbF levels. More severe forms with enlarged liver and spleen, β‐thalassaemia intermedia (ie β+/β+) and β‐thalassaemia major (ie β0/β0) present as anaemia (that does not require blood transfusion) and severe anaemia (infants fail to thrive), respectively. The inability to produce β‐globin chains causes the excessive production of α‐globin chains, which eventually precipitates.9, 10 The result is the production of fragile RBCs and their precursors that causes further medullary and extramedullary haemolysis. As medullary haematopoiesis is ineffective, extramedullary haematopoiesis becomes expansive and clinically apparent (skull bossing and hair‐on‐end signs, hepatosplenomegaly, and osteopenia). The reduced lifespan of RBCs results in increased iron turnover through increased iron absorption, haemolysis and numerous blood transfusions. The increased iron turnover leads to excessive deposits of iron in different organs, such as the endocrine glands, liver and heart. β‐thalassaemia is confirmed by complete blood count, haematological indices and film, measurement of iron, HbA2 and HbF, and Hb electrophoresis. Asymptomatic thalassaemia patients routinely have scheduled follow‐ups with a haematologist. Folates, iron‐chelators, large doses of vitamin C (favour urinary iron excretion), hormone replacement therapy (to compensate for the insufficient hormones secreted by the endocrine glands) and bone marrow transplantation are used to manage β‐thalassaemia major patients, as well as splenectomy in the cases of hypersplenism. The antenatal diagnosis using foetal blood or DNA is of extreme importance.6, 8, 11, 12
HbA1C is a valuable parameter that determines the quality of glycaemic control in diabetes mellitus over the 2 months preceding the RBC half‐life of 80‐120 days. Blood glucose glycates the ε‐amino group of lysine residues and the amino terminals of Hb in RBC. About 5% of Hb is usually glycated normally, and glycaemia determined this proportion.13
2. OBJECTIVE
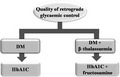
In conditions that affect Hb status or rate of RBC turnovers, such as in thalassaemia and haemoglobinopathies, HbA1C could be inappropriate as a retrograde glycaemic regulation marker. In such cases, fructosamine may be very beneficial.13, 14 Fructosamine is a ketoamine created by glycosylation of total serum proteins, primarily albumin.15 It reflects average glycaemia over the previous 1‐4 weeks.16
With this case study, we analyse the pitfalls in the assessment of retrograde diabetes control quality in a patient with thalassaemia.
3. CASE DESCRIPTION
We performed blood analyses using the DxC 800 and DXI‐600 devices, Beckman Coulter Inc, USA. An abdominal ultrasound was performed by Toshiba Xario, Japan. A chest X‐ray and abdominal X‐ray were performed using the Agfa DX‐D100+, Belgium.
We hospitalized a 67‐year‐old male due to chronic distal neuropathic pain, trophic right toe ulcer and distal sensorimotor polyneuropathy verified by EMG. In his medical history, we found that he had thalassaemia not requiring blood transfusions. It was also noted that his daughter suffered from the β‐thalassaemia‐heterozygous state. The patient's five‐point glycaemic profile showed moderate postprandial hyperglycaemic episodes, with no hypoglycaemia (Table 1), but we observed irregularities with the retrograde glycaemic control, as the levels of HbA1C were repeatedly optimal, despite electromyography confirmation of distal polyneuropathy (Table 1). Because a record about β‐thalassaemia was noticed later, fructosamine measurements were not performed at this point.
Table 1.
Laboratory analyses on admission and at discharge
| Analysis | On admission | After six months | Reference values |
|---|---|---|---|
| Peak postprandial glycaemia (mmol/L) | 15 | 13 | 3.9‐6.1 |
| HbA1C (%) | 6.5 | 6.5 | ≤6.5 |
| C peptide (ng/mL) | 4.36 | / | 0.9‐4.0 |
| Fructosamine (µmol/L) | / | 267 | 205‐285 |
Abbreviation: HbA1C, haemoglobin A1C.
During the examination of the obese and normotensive patient (BMI 32.7 kg/m2, BP 130/80 mmHg), we identified a small trophic ulcer of the right toe with palpable pulses on distal arteries. We observed no other physical abnormalities and did not detect any chronic micro‐ or macrovascular diabetes complication on proper imaging.
Laboratory analyses revealed microcytic anaemia and enzyme syndrome of liver necrosis and remodelling (Table 2). An abdominal ultrasound further revealed mild enlargement of liver and spleen (liver 160 mm, spleen 142 × 70 mm). The findings of immunochemistry, thyroid function tests, proteinuria and estimated glomerular filtration rate were at standard levels. Chest X‐ray and Doppler scan of distal peripheral arteries did not show any pathology.
Table 2.
The results of biochemical analyses
| Analysis | On admission | Reference values |
|---|---|---|
| Red blood cells (×1012/L) | 6.1 | 4.5‐6.3 |
| Haemoglobin (g/dL) | 127 | 140‐175 |
| Haematocrit (L/L) | 0.40 | 0.40‐0.52 |
| MCV (fL) | 69 | 80‐96 |
| MCH (pg) | 21.8 | 27.0‐33.0 |
| MCHC (g/L) | 325 | 330‐360 |
| AST (U/L) | 41 | <37 |
| ALT (U/L) | 69 | <43 |
| γGT (U/L) | 177 | <50 |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; MCHC, mean corpuscular haemoglobin concentration; MCH, mean corpuscular haemoglobin; γGT, gamma‐glutamyl transferase; MCV, mean corpuscular volume.
Despite the preserved pancreatic insulin reserve estimated by basal C peptide measurement (Table 1), conventional insulin treatment was introduced, along with insulin sensitizer. After hyperbaric oxygen treatment, the patient was discharged with improved glycaemic profile and right toe trophic ulcer healing, as well as with the mild improvement of polyneuropathy‐associated complaints after the introduction of treatment for peripheral neuropathic pain control (alpha‐lipoic acid, amitriptyline and pregabalin). Six months later, the five‐point glycaemic profile was suboptimal, but HbA1C and fructosamine levels pointed out to optimal retrograde glycaemic control (Table 1).
Type 2 diabetes mellitus (T2DM) is a common complication of thalassaemia major patients, with incidence rates ranging from 14%‐24%.17 The onset of T2DM in thalassaemia patients is often very deceptive.18 The exact mechanism of T2DM in thalassaemia patients is still unclear. However, the contribution of iron overload, insulin resistance, and α‐ and β‐cells destruction induced by iron deposition and associated inflammation is unequivocal.18, 19, 20
Thalassaemia can interfere with the markers of glycaemic regulation in T2DM patients through several mechanisms, such as reduction of RBC lifespan and the presence of some Hb variants (ie HbS, HbA2 and HbF). Hb variants can affect HbA1C measurement in multiple ways, such as through the change of 1/ Hb net charge, 2/ glycation rate and 3/ RBC lifespan.21 This interference can be the reason for false lower or higher measurement results, which can cause patients to be over‐ or under‐treated.22, 23 Such false results can even impact T2DM diagnosis.20 Thus, determining appropriate measures that can deal with the validation of results suspected of the presence of Hb variants is of interest.24 Developing more appropriate measures requires an understanding of the HbA1C measurement methods, as well as the information on the presence of Hb variants.20, 21, 25 Even more factors that could interfere with HbA1C measurement are being identified.26, 27 Thus, there is a need for the development of new methods for HbA1C measurement.28
Besides that, iron‐deficiency anaemia, haemorrhage, haemolysis, blood transfusions or uremia can also impact the RBC lifespan. In the conditions followed by the reduced RBC life span, fructosamine correlated better with the actual glycaemic level than HbA1C.25, 29 It is noteworthy that heterozygous subjects with any of the worldwide most common Hb variants (eg S, C, E, D) are usually asymptomatic and have regular RBC lifespan.25
In the cases of discrepancy between profile or average glycaemia values and markers of retrograde glycaemic control, such as HbA1C, the clinician should be cautious about the presence of some disease or condition that interferes with HbA1C measurement. Such consideration is especially important in the case where T2DM patients have existing micro‐ or macrovascular complications and preserved renal function. Also, biochemists and clinicians should collaborate more closely on proper diagnosis. This way, biochemist will better understand the value of identifying a parameter that interferes with HbA1C measurement (such as Hb variants or determined chemical compound, eg carbamylated Hb), as it may suggest a more reliable marker for the assessment of retrograde glycaemic regulation, such as fructosamine.30
The non‐enzymatic addition of glucose to the N‐terminal valine of the Hg β‐chains irreversibly modifies HbA1C.31 It is well‐known that glycation of Hb can be affected by genetics, ethnicity or even race.32 The false results of HbA1C measurement can be observed as increased or decreased, depending on already mentioned RBC lifespan and administered blood transfusions, but also the assay used.33 Additionally, the premature destruction of RBCs shortens the time for Hb glycation and hence lowers levels of measured HbA1C.30
4. WHAT IS NEW AND CONCLUSION
Here, we present the case report of a male thalassaemia patient with co‐existing T2DM complicated with distal polyneuropathy and vasculopathy. Shortly after insulin introduction, the five‐point glycaemic profile was improved on patient hospital discharged. Because of poor compliance with non‐pharmacological diabetes management, the problems with daily glycaemic regulation persisted. Despite that, the patient displayed some improvement in postprandial glycaemic values that were evident after the six months follow‐up, even though the initial postprandial glycaemic peaks were suboptimal (peak postprandial glycaemia on admission and six months later were 15.0 and 13.0mmol/L, respectively). We observed a discrepancy between the actual five‐point glycaemic profile (suboptimal) and retrograde glycaemic control (optimal). This discrepancy led us to identify fructosamine as a preferable and more reliable marker of retrograde glycaemic control for cases that involve haemoglobinopathies and thalassaemia syndromes. After conventional insulinization of the patient improved five‐point glycaemic profile was registered (suboptimal but within the reasonable bounds) and optimal values of HbA1C and fructosamine. It seems that in the cases with a suboptimal glycaemic profile, both HbA1C and fructosamine are equally reliable markers of retrograde glycaemic control. It appears that fructosamine is a more reliable and competent marker of retrograde glycaemic control than HbA1C in cases of poor daily glycaemic control. Also, clinicians should be familiar with the commonly used HbA1C measurement methods, as well as measurement methods used alternatively.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
AUTHOR CONTRIBUTIONS
ZG, ML, VS, and JTJ contributed to the conception and design of the study, acquisition, and analysis of data, and drafting the article. MO, ME, VBB, and ERI contributed to drafting the article, revising article critically for relevant intellectual content and final approval of the version to be published.
Gluvic Z, Obradovic M, Lackovic M, et al. HbA1C as a marker of retrograde glycaemic control in diabetes patient with co‐existed beta‐thalassaemia: A case report and a literature review. J Clin Pharm Ther. 2020;45:379–383. 10.1111/jcpt.13073
Funding information
This work is part of the collaboration between the Laboratory of Radiobiology and Molecular Genetics, Vinca Institute of Nuclear Sciences, University of Belgrade, Belgrade, Serbia, Department of Endocrinology and Diabetes, Zemun Clinical Hospital, School of Medicine, University of Belgrade, Belgrade, Serbia, and King Abdullah University of Science and Technology (KAUST), Computational Bioscience Research Center (CBRC), Thuwal, Saudi Arabia. This work has been supported by grants No. 173033 (ERI) from the Ministry of Education, Science and Technological Development, Republic of Serbia and by the KAUST grant OSR#4129 (to ERI and VBB), which also supported ERI, MO; VBB by the KAUST Base Research Fund (BAS/1/1606‐01‐01), and VBB and ME by KAUST Office of Sponsored Research (OSR) grant no. FCC/1/1976‐17‐01.
Contributor Information
Zoran Gluvic, Email: zorangluvic@yahoo.com.
Milan Obradovic, Email: obradovicmilan@hotmail.com.
REFERENCES
- 1. Thomas C, Lumb AB. Physiology of haemoglobin. Cont Educ Anaesth Crit Care Pain. 2012;12(5):251‐256. [Google Scholar]
- 2. Khoshouei M, Danev R, Plitzko JM, Baumeister W. Revisiting the Structure of hemoglobin and myoglobin with cryo‐electron microscopy. J Mol Biol. 2017;429(17):2611‐2618. [DOI] [PubMed] [Google Scholar]
- 3. Thom CS, Dickson CF, Gell DA, Weiss MJ. Hemoglobin variants: biochemical properties and clinical correlates. Cold Spring Harb Perspect Med. 2013;3(3):a011858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barrera‐Reyes PK, Tejero ME. Genetic variation influencing hemoglobin levels and risk for anemia across populations. Ann N Y Acad Sci. 2019;1450(1):32‐46. [DOI] [PubMed] [Google Scholar]
- 5. Musallam KM, Taher AT, Rachmilewitz EA. Beta‐thalassemia intermedia: a clinical perspective. Cold Spring Harb Perspect Med. 2012;2(7):a013482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Quek L, Thein SL. Molecular therapies in beta‐thalassaemia. Br J Haematol. 2007;136(3):353‐365. [DOI] [PubMed] [Google Scholar]
- 7. Farashi S, Harteveld CL. Molecular basis of alpha‐thalassemia. Blood Cells Mol Dis. 2018;70:43‐53. [DOI] [PubMed] [Google Scholar]
- 8. Ian BW, Tim R, Kate W, Anna G, Catriona H, Harriet ON. Oxford Handbook of Clinical Medicine. Oxford, UK: Oxford University Press; 2017. [Google Scholar]
- 9. Borgna‐Pignatti C, Rigon F, Merlo L, et al. Thalassemia minor, the Gilbert mutation, and the risk of gallstones. Haematologica. 2003;88(10):1106‐1109. [PubMed] [Google Scholar]
- 10. Graffeo L, Vitrano A, Giambona A, et al. The heterozygote state for beta‐thalassemia detrimentally affects health outcomes. Am J Hematol. 2017;92(3):E23‐e25. [DOI] [PubMed] [Google Scholar]
- 11. Alaithan MA, Abdulazeez S, Borgio JF. A comprehensive review of the prevalence of beta globin gene variations and the co‐inheritance of related gene variants in Saudi Arabians with beta‐thalassemia. Saudi Med J. 2018;39(4):329‐335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kırım S, Keşkek ŞÖ, Turhan A, Saler T. Is β‐thalassaemia minor associated with metabolic disorder? Med Princ Pract. 2014;23(5):421‐425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dorcely B, Katz K, Jagannathan R, et al. Novel biomarkers for prediabetes, diabetes, and associated complications. Diabetes Metab Syndr Obes. 2017;10:345‐361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wu WC, Ma WY, Wei JN, et al. Serum glycated albumin to guide the diagnosis of diabetes mellitus. PLoS ONE. 2016;11(1):e0146780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ribeiro RT, Macedo MP, Raposo JF. HbA1c, Fructosamine, and Glycated Albumin in the Detection of Dysglycaemic Conditions. Curr Diabetes Rev. 2016;12(1):14‐19. [DOI] [PubMed] [Google Scholar]
- 16. Malmstrom H, Walldius G, Grill V, Jungner I, Gudbjornsdottir S, Hammar N. Fructosamine is a useful indicator of hyperglycaemia and glucose control in clinical and epidemiological studies–cross‐sectional and longitudinal experience from the AMORIS cohort. PLoS ONE. 2014;9(10):e111463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vogiatzi MG, Macklin EA, Trachtenberg FL, et al. Differences in the prevalence of growth, endocrine and vitamin D abnormalities among the various thalassaemia syndromes in North America. Br J Haematol. 2009;146(5):546‐556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cooksey RC, Jouihan HA, Ajioka RS, et al. Oxidative stress, beta‐cell apoptosis, and decreased insulin secretory capacity in mouse models of hemochromatosis. Endocrinology. 2004;145(11):5305‐5312. [DOI] [PubMed] [Google Scholar]
- 19. De Sanctis V, Gamberini MR, Borgatti L, Atti G, Vullo C, Bagni B. Alpha and beta cell evaluation in patients with thalassaemia intermedia and iron overload. Postgrad Med J. 1985;61(721):963‐967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rohlfing C, Hanson S, Weykamp C, et al. Effects of hemoglobin C, D, E and S traits on measurements of hemoglobin A1c by twelve methods. Clin Chim Acta. 2016;455(80–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bry L, Chen PC, Sacks DB. Effects of hemoglobin variants and chemically modified derivatives on assays for glycohemoglobin. Clin Chem. 2001;47(2):153‐163. [PubMed] [Google Scholar]
- 22. Lee SC, Wang LH, Tsai SM, Fang HY, Tsai LY. Effects of the Hb E, Hb H and Hb G‐Taichung variants on HbA1c values by the Bio‐Rad variant II turbo analyzer. Clin Biochem. 2011;44(16):1338‐1342. [DOI] [PubMed] [Google Scholar]
- 23. Pravatmuang P, Sae‐Ngow B, Whanpuch T, Leowattana W. Effect of HbE and HbH on HbA1C level by ionic exchange HPLC comparing to immunoturbidimetry. Clin Chim Acta. 2001;313(1–2):171‐178. [DOI] [PubMed] [Google Scholar]
- 24. Little RR, La'ulu SL, Hanson SE, Rohlfing CL, Schmidt RL. Effects of 49 different rare Hb variants on HbA1c measurement in eight methods. J Diabetes Sci Technol. 2015;9(4):849‐856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lin C‐N, Emery TJ, Little RR, et al. Effects of hemoglobin C, D, E, and S traits on measurements of HbA1c by six methods. Clin Chim Acta. 2012;413(7–8):819‐821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Xu A, Chen W, Xia Y, Zhou Y, Ji L. Effects of common hemoglobin variants on HbA1c measurements in China: results for alpha‐ and beta‐globin variants measured by six methods. Clin Chem Lab Med. 2018;56(8):1353‐1361. [DOI] [PubMed] [Google Scholar]
- 27. Jaisson S, Leroy N, Desroches C, Tonye‐Libyh M, Guillard E, Gillery P. Interference of the most frequent haemoglobin variants on quantification of HbA1c: comparison between the LC‐MS (IFCC reference method) and three routinely used methods. Diabetes Metab. 2013;39(4):363‐369. [DOI] [PubMed] [Google Scholar]
- 28. Agilli M, Yaman H, Aydin F, et al. Hb H interference on measurement of HbA1c with ion‐exchange HPLC. Acta Inform Med. 2013;21(3):216‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mitani N, Taguchi A, Sakuragi S, et al. Undetectable glycosylated hemoglobin in autoimmune hemolytic anemia. Bull Yamaguchi Med School. 2005;52(21–3. [Google Scholar]
- 30. Liew CF, Cheah JS. Hereditary spherocytosis, a pitfall in the assessment of glycaemic control. Singapore Med J. 2003;44(2):94‐97. [PubMed] [Google Scholar]
- 31. WHO Guidelines Approved by the Guidelines Review Committee , in Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation: World Health Organization 2011. [PubMed]
- 32. Herman WH, Cohen RM. Racial and ethnic differences in the relationship between HbA1c and blood glucose: implications for the diagnosis of diabetes. J Clin Endocrinol Metab. 2012;97(4):1067‐1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Spencer DH, Grossman BJ, Scott MG. Red cell transfusion decreases hemoglobin A1c in patients with diabetes. Clin Chem. 2011;57(2):344‐346. [DOI] [PubMed] [Google Scholar]


