Abstract
Overweight and obesity in childhood are associated with early cardiovascular dysfunction and promote heightened risk of cardiovascular morbidity and mortality in adulthood. Waist circumference (WC) correlates with visceral obesity, which is why obese children with elevated WC need to be carefully monitored to prevent long-term cardio-metabolic complications. The purpose of our study was to establish if WC could be a predictor of cardiovascular complications in children.
The authors conducted a retrospective study that included 160 overweight and obese children and adolescents, aged 6 to 18 years. Patients were evaluated completely anthropometrically, biologically, and imagistic. The anthropometric data tracked were height, weight, WC, and body mass index. Echocardiography evaluated the following parameters: the interventricular septum, left ventricular mass, the relative thickness of the ventricular wall, the pathological epicardial fat.
Our results confirm that the presence of visceral obesity was significantly associated (χ2 = 11.72, P = .0006) with pathological epicardial fat. In children, visceral obesity is not a risk factor for vascular or cardiac impairment, but in adolescents, the results showed that visceral obesity is an important predictive factor for the occurrence of vascular (AUC = 0.669, P = .021) and cardiac (AUC = 0.697, P = .037) impairment. Concentric left ventricular (LV) hypertrophy is significantly influenced by the presence of visceral obesity (AUC = 0.664, P = .013 children; AUC = 0.716, P = .026 adolescents).
WC above the 90th percentile is a predictive factor for increased LVM index and concentric hypertrophy in both children and adolescents.
Keywords: adolescents, cardio-vascular complications, children, obesity, visceral obesity, waist circumference
1. Introduction
In recent years, the prevalence of obesity has increased in developed and developing countries, both in children and adults.[1,2]
In children, we are witnessing an upward trend in the prevalence of obesity globally, from 0.7% in 1975 to 5.6% in 2016 in girls and from 0.9% to 7.8% in boys.[3] With the increasing prevalence of obesity in pediatric age, the number of complications associated with obesity has also increased: dyslipidemias, type 2 diabetes mellitus, fatty liver disease, sleep apnea, microalbuminuria, elevated triglycerides (TG), total and low density lipoprotein cholesterol (LDL-C), and insulin levels, as well as a reduced high density lipoprotein cholesterol (HDL-C) levels. All of them represent risk factors for the occurrence of cardiovascular diseases.[4,5]
Overweight and obesity in childhood are associated with early cardiovascular dysfunction and promote heightened risk of cardiovascular morbidity and mortality in adulthood. The signs of cardiovascular dysfunction in the obese child are: significantly higher arterial blood pressure, changes in the structure and function of the myocardium (left ventricular hypertrophy, left ventricular diastolic dysfunction, and myocardial dysfunction), and the occurrence of long-term epicardial fat.[4–8] Cardiovascular disorders in childhood are serious because they cause heart failure, acute coronary syndrome, and sudden premature death in adult life.[9–11]
Screening for early metabolic complications is considered very important, but it is still unclear which parameter would be better to focus on: assessing body mass index or waist circumference as a cardio-metabolic risk factor.[12] The waist circumference (WC) is an easy-to-determine clinical parameter for assessing the nutritional status of the child, independent of body mass index (BMI).[13] Studies in adults have shown that individuals with central obesity are more susceptible to cardio-metabolic risk factors. WC is one of the criteria for defining the metabolic syndrome and a cardiovascular risk factor.[14–16] WC correlates with visceral obesity, which is why obese children with elevated WC need to be carefully monitored to prevent long-term cardio-metabolic complications.[17–19] Studies have proven that central obesity is an independent risk factor for coronary artery disease, arterial hypertension, dyslipidemia.[20,21] Moreover, WC at the ages of 5 to 17 years was shown to be associated with abnormal concentrations of TG, LDL-C, HDL-C, and insulin.[22]
However, the association of abdominal obesity in children and adolescents with cardio-metabolic risk factors remains controversial. The purpose of our paper was to establish if WC could be a predictor of cardiovascular complications in children.
2. Material and methods
The authors conducted a retrospective study that included 160 children with overweight and obesity, hospitalized between January 1, 2016 and December 31, 2018 in the “Saint Mary” Emergency Children Hospital, Iasi, Romania. The inclusion criteria were overweight and obesity diagnosis without associated pathologies. Only children and adolescents with an informed consent (paternalistic consent) for data processing in the medical record were included in the study. Obese patients with associated medical illness (genetic syndromes, diabetes, congenital heart or dyslipidemic diseases, renal, or neurological diseases), eating disorders, chronic medications were excluded.
According to their age, patients were included in 2 groups: group A: children between 6 and 11 years old; group B: adolescents between 12 and 18 years old.
We collected the data from the patient's observation sheets. During the hospitalization, patients were evaluated completely anthropometrically, biologically, and imagistic. The anthropometric data tracked were height, weight, WC, and the BMI. Interpretation of BMI values was based on BMI Z score and BMI percentile, applicable for age and sex, according to WHO standards, using WHO AnthroPlus software.[23] Depending on the BMI Z score, the patients were classified into overweight (BMI Z score >+1SD or BMI percentiles between 85 and 97th), obese (BMI Z score >+2SD or BMI percentiles between 97 and 99.9th), and severe obesity (BMI Z score >+3 SD or BMI percentiles>99.9th).[24,25]
WC was measured using a centimeter, halfway between the coastal rim and the iliac crest, at the end of the expiration. For WC interpretation, we used tables with specific percentiles for age and sex, developed based on National Health and Nutrition Examination Survey (NHANES) III data.[26] Because WC provides an indication of visceral adipose tissue, visceral obesity was defined by values over the 90th percentile of WC.[13,15]
Fasting blood profile included: total cholesterol (TC), low-density lipoprotein cholesterol (LDLc) and high-density lipoprotein cholesterol (HDLc), triglycerides (TG), glucose levels, alanine aminotransferase values, urea and creatinine values. The reference standards were used to interpret the values of biological parameters.
The blood pressure (BP) value was interpreted according to the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. Children hypertension was defined as systolic BP and/or diastolic BP >95th percentile, adjusted for height, age, and sex, at least 3 separate determination. Normally, high blood pressure was considered for values between the 90 and 95 percentile values (National Institute for Health, 2004). In our study, BP values ≥90th percentile were defined as ”elevated BP” or vascular impairment.[27]
Echocardiography was performed in all patients, the following parameters being thickness of the interventricular septum (IVS), diastolic diameters of the left ventricle (DdLV), left ventricular mass (LVM), the relative thickness of the ventricular wall (RWT), the presence of epicardial fat. Diastolic dysfunction was evaluated through the E/A ratio and the pulmonary venous flow through the S/D ratio.
The interpretation of the LVM was made according to LVM index or LVM-for-height Z score (LVM divided by height raised to a power of 2.7).[28] Left ventricular hypertrophy (LVH) was defined as LVM index >95th percentile for normal children and adolescents.[29] Relative wall thickness (RWT) was measured to assess the LV geometric pattern.[30] The RWT value above >0.41 is considered pathological. Patients with increased LVM index and elevated RWT (>0.41) had concentric LVH; those with increased LVM index and normal RWT (<0.41) had eccentric LVH. Concentric remodeling was defined as elevated RWT, but with normal LVM index. Pathological epicardial fat quantified by echocardiography was considered over 4.1 mm.[31]
Patients who had concentric or eccentric LVM hypertrophy, concentric remodeling, and/or epicardial fat with pathological values were considered to have cardiac impairment.
Statistical analyzes of the variables were performed using SPSS software v.20 (IBM Corporation, North Castle Drive, Armonk, NY 10504-1785, U.S.A.) type variables were reported as mean with standard deviation. Comparisons between the analyzed groups were performed using Student t test or Mann–Whitney U test for continuous variables. The qualitative variables were presented as absolute (n) and relative (%) frequencies, and the comparisons between groups were made based on the results of McNemar, Yates Chi-square, or Fisher exact test. Univariate and multivariate analysis of prognostic factors regarding cardiovascular complications was performed using the Logistic regression model. The significance level calculated in the used tests (P-value) was considered significant for P values <.05.
3. Results
We analyzed the clinical, biological, and imaging characteristics of the 160 patients included in the study group. Group A (children) included 97 patients aged 6 to 11 years old (mean age 9.82 ± 2.2 years) and group B (adolescents) included 63 patients aged 12 to 18 years old (mean age 14.7 ± 1.6).
Between the 2 groups of patients, the sex distribution showed predominance of the male sex in both groups (59.8% in group A compared with 60.3% in group B).
In both groups, obesity was more prevalent than overweight (53.61% in children vs 49.21% in adolescents). In the study group A, 32.99% of children had severe obesity while in the group B, 44.44% of adolescents had overweight (Table 1). These results are concordant with the classification of the study groups according to the nutritional status, with significant differences regarding the classification of children and adolescents in overweight, respectively morbid obesity. Thus, overweight is far more common in adolescents, while obesity and severe obesity are significantly more common in children. Obesity and severe obesity are significantly associated (P < .001) with the age of <12 years old. Therefore, the BMI percentile indicated higher mean values for children compared with adolescents (P < .0001) (Table 1).
Table 1.
Baseline characteristics.

Comparing the average values of the systolic BP and diastolic BP does not objectively reflect the presence of vascular impairment due to the different criteria for age group specific classification. Considering also the age criterion and the classification of hypertension properly, it is clearly shown that in obese adolescents (8.3% vs 30.2%; P = .0003) pre-hypertension and hypertension are significantly more frequent (20.6% vs 14.4%; P = .0003) (Table 1).
We compared several biological parameters between children and adolescents. The assessment of total cholesterol values showed that there are no statistically significant differences between the 2 age groups. Regarding triglycerides, it is observed that there are statistically significant differences between children and adolescents (P = .0142) (Table 1).
We evaluated the correlation between epicardial fat and visceral obesity in children and adolescents (Table 2).
Table 2.
Evaluation of the association of epicardial fat versus visceral obesity.

The presence of visceral obesity was unquestionably associated (χ2 = 11.72, P = .0006) with the presence of pathological epicardial fat: from the 46 cases without visceral obesity only 2.17% had pathological epicardial fat, whereas of the 92 cases with visceral obesity, 21.74% presented pathological epicardial fat. Area under the curve (AUC) showed an increased predictive power of the presence of pathological epicardial fat (AUC = 0.668, 95% confidence interval [CI]: 0.562–0.775, P = .014) in the presence of visceral obesity (Fig. 1).
Figure 1.

AUC: Epicardial fat versus visceral obesity. AUC = area under the curve.
The evaluation of the AUC regarding the predictability of the clinical and biological parameters on the vascular and cardiac impairments is presented in Table 3. The analysis revealed that BMI is not a significant predictor for vascular impairment for either children or adolescents (AUC = 0.57, P = .327 vs AUC = 0.54, P = .53). However, BMI is an important predictive factor for the occurrence of cardiac impairment in children (AUC = 0.62, P = .041) and adolescent (AUC = 0.66, P = .036) (Table 3).
Table 3.
The estimated parameters in the evaluation of the predictability of the clinical and biological parameters on the vascular and cardiac impairments.

In the age group 6 to 11 years, among the factors analyzed (BMI, visceral obesity, TC, TG, LDLc, HDLc), none of them are important predictive factors for vascular impairment (P > .05), but BMI is a significant predictive factor for cardiac impairment. Visceral obesity is not a risk factor for vascular or cardiac impairment in this age group (Table 4).
Table 4.
Estimated parameters in evaluating the predictability of visceral obesity on cardiac impairment.
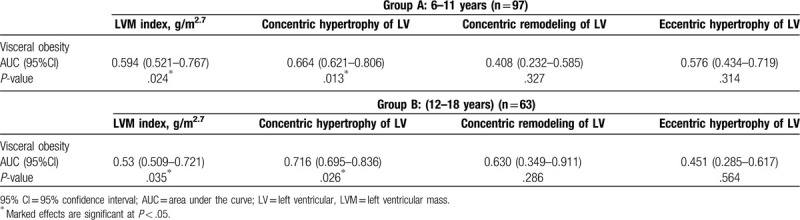
In adolescents, the results showed that visceral obesity is an important predictive factor for the occurrence of vascular (AUC = 0.669, P = .021) and cardiac (AUC = 0.697, P = .037) impairment. Also, increased levels of TG and LDLc are predictable for the occurrence of cardiac impairment in adolescents (AUC = 0.67, P = .044; AUC = 0.66, P = .038) (Table 4). Total cholesterol is not a predictive factor for cardiac manifestations.
In our study, visceral obesity was predictive for increased the LMV index values in both children (AUC = 0.594, P = .024) and adolescents (AUC = 0.53, P = .035). Moreover, concentric LV hypertrophy is significantly influenced by the presence of visceral obesity (AUC = 0.664, P = .013 children; AUC = 0.716, P = .026 adolescents) (Table 4). Concentric remodeling and the presence of eccentric hypertrophy were not significantly influenced by the presence of visceral obesity (P > .05) (Table 4). Regarding diastolic dysfunction, no changes in the E/A ratio were identified, but the S/D ratio <1 was identified in 6 patients with severe obesity who also had hypertrophic cardiomyopathy.
4. Discussions
Overweight and obesity in childhood are associated with early cardiovascular dysfunction, which increases the risk of cardiovascular morbidity and mortality in adult life.[31] Cardiac structural and functional changes in obese patients affect the myocardium and determine the so-called “obesity cardiomyopathy.”[32]
In the absence of removal of cardiovascular risk factors, childhood-onset of cardiac dysfunction will progress into adulthood, and literature studies show that in overweight and obese adults, heart failure will develop 10 years faster compared with subjects with normal BMI.[19,32] This is why it is extremely important to identify the clinical and biological parameters for predicting cardiovascular risk from childhood.
Among the clinical parameters, BMI and WC were the first cardiovascular risk factors discussed in childhood and adolescence. Janssen et al evaluated data from the Bogalusa Heart Study, which included 2597 children and adolescents aged 5 to 18 years.[35] They concluded that both BMI and WC indicate an increased cardiovascular risk in children and adolescents with visceral obesity, although there are differences in the origin environments, ethnicity.[13,33–35]
WC provides an indicator of visceral adipose tissue. Imaging techniques such as abdominal computed tomography, magnetic resonance imaging, and dual-energy x-ray absorptiometry provide accurate measurements of visceral adipose tissue, but are expensive and often unfeasible to use in the clinical setting. Studies showed that WC provides almost an identical measurement of visceral adipose tissue among adults and can be used to identify those at risk of developing cardiovascular disease and type 2 diabetes mellitus.[36,37] In obese 12 to 14-year-old children, WC correlates to a potentially atherogenic lipoprotein profile.[13,38]
The relationship between visceral adiposity and cardiovascular risk is widely acknowledged which makes the evaluation of fat distribution a compulsory procedure in obese children.[39] In evaluating overweight children, WC plays an important role in the early identification of metabolic syndrome and cardiometabolic risk.[38,40] In the study published by Bin and Li in 2011, the authors stated that increased WC was an indicator of high BP in preschool children, especially in boys. Moreover, WC was independently associated with high BP in this category of children. Thus, high BP in children has been associated with increased WC, and childhood obesity is associated with high risk of adult hypertension.[38–43] Regarding the predictive power of BMI and WC on elevated BP, literature studies have shown that increased WC is associated with elevated BP even when BMI is normal.[44,45]
In our study, we observed that WC is an important predictive factor for the occurrence of vascular impairment (pre-hypertension and hypertension) only in adolescents, not in children under 12 years. Regarding the predictive value of BMI, this is not a significant predictive factor for vascular impairment neither in children or adolescent in our study.
Visceral obesity induces a variety of structural alterations in cardiac structure and function. Especially children with severe obesity, exhibit a tendency to develop abnormal LV geometry (LV hypertrophy or relative wall thickness) and cardiac dysfunction.[5,46] The mechanisms that lead to altered diastolic function of the LV are complex and influenced by numerous variables. Furthermore, in obese children with hypertension, the risk of left ventricular hypertrophy increases.[47]
Most studies agree that obese children have increased LVM index.[31,48,49] Also, LVM index significantly correlated with BMI in children and adolescents with essential hypertension.[50,51] In our study, WC above the 90th percentile is a predictive factor for increased LVM index and concentric hypertrophy in both children and adolescents. Moreover, concentric remodeling and the presence of eccentric hypertrophy were not significantly influenced by the presence of visceral obesity.
Greater epicardial fat deposition has been reported in children with obesity compared with sex- and age-matched children with a healthy BMI. Moreover, quantification of epicardial adipose tissue by echocardiography is reported to be associated with visceral adipose tissue deposition.[30] According to this, in our study the presence of visceral obesity was significantly associated with the presence of pathological epicardial fat.
This study has a number of limitations. Primarily, the definition of visceral obesity based on the waist circumference, in the absence of abdominal magnetic resonance imaging or dual-energy x-ray absorptiometry. In addition, the impossibility of performing the vascular ultrasound and evaluation of intima media thickness for the evaluation of subclinical atherosclerosis, a marker of morphological vascular damage.
5. Conclusions
Overweight and obesity in childhood are associated with early cardiovascular dysfunction. Visceral obesity is an important predictive factor for the occurrence of vascular impairment (pre-hypertension and hypertension) especially in adolescents compared with children. WC above the 90th percentile is a predictive factor for increased LVM index and concentric hypertrophy in both children and adolescents. Obese pediatric patients with elevated WC need to be carefully monitored to prevent long-term cardiovascular complications.
Acknowledgments
All authors contributed equally to this paper.
Author contributions
Conceptualization: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Data curation: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Formal analysis: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Investigation: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Methodology: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Writing – original draft: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Writing – review & editing: Laura Mihaela Trandafir, Georgiana Russu, Mihaela Moscalu, Ingrith Miron, Vasile Valeriu Lupu, Maria Magdalena Leon Constantin, Elena Cojocaru, Ancuta Lupu, Otilia Elena Frasinariu.
Footnotes
Abbreviations: AUC = area under the curve, BMI = body mass index, BP = blood pressure, DdLV = diastolic diameters of the left ventricle, HDLc = high-density lipoprotein cholesterol, IVS = interventricular septum, LDLc = low-density lipoprotein cholesterol, LV = left ventricular, LVM = left ventricular mass, NHANES = National Health and Nutrition Examination Survey, RWT = thickness of the ventricular wall, SD = standard deviation, TC = total cholesterol, TG = triglycerides, WC = waist circumference, WHO = World Health Organization.
How to cite this article: Trandafir LM, Russu G, Moscalu M, Miron I, Lupu VV, Leon Constantin MM, Cojocaru E, Lupu A, Frasinariu OE. Waist circumference a clinical criterion for prediction of cardio-vascular complications in children and adolescences with overweight and obesity. Medicine. 2020;99:30(e20923).
All authors contributed equally to this paper.
Funding: None.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among us children and adolescents, 1999–2010. JAMA 2012;307:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cozzolino D, Grandone A, Cittadini A, et al. Subclinical myocardial dysfunction and cardiac autonomic dysregulation are closely associated in obese children and adolescents: the potential role of insulin resistance. PLoS One 2015;10:e0123916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Alpert MA, Omran J. Bostick BP Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obes Rep 2016;5:424–34. [DOI] [PubMed] [Google Scholar]
- [6].Elshorbagy HH, Fouda ER, Kamal NM, et al. Evaluation of epicardial fat and carotid intima-media thickness in obese children. Iran J Pediatr 2016;26:e2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Russu G, Frăsinariu OE, Trandafir L. Cardiovascular suffering in childhood obesity. Rom J Pediatr 2017;56:12–7. [Google Scholar]
- [8].Gavril RS, Mitu F, Leon Constantin MM, et al. Biomarkers of inflammation patients with type 2 diabetes mellitus and hepatic steatosis. Rev Chim 2016;67:1828–31. [Google Scholar]
- [9].Attar RZ, Safdar OY, Ghoneim A, et al. Left ventricular hypertrophy in obese children. J Obes Weight Loss Ther 2016;6:309. [Google Scholar]
- [10].Wong CY, O’Moore-Sullivan T, Leano R, et al. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation 2004;110:3081–7. [DOI] [PubMed] [Google Scholar]
- [11].Zalesin KC, Franklin BA, Miller WM, et al. Impact of obesity on cardiovascular disease. Endocrinol Metab Clin North Am 2008;37:663–84. [DOI] [PubMed] [Google Scholar]
- [12].Magnussen CG, Koskinen J, Juonala M, et al. A diagnosis of the metabolic syndrome in youth that resolves by adult life is associated with a normalization of high carotid intima-media thickness and type 2 diabetes mellitus risk: the Bogalusa heart and cardiovascular risk in young Finns studies. J Am Coll Cardiol 2012;60:1631–9. [DOI] [PubMed] [Google Scholar]
- [13].Bassali R, Waller JL, Gower B, et al. Utility of waist circumference percentile for risk evaluation in obese children. Int J Pediatr Obes 2010;5:97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Janiszewski PM, Janssen I, Ross R. Does waist circumference predict diabetes and cardiovascular disease beyond commonly evaluated cardiometabolic risk factors? Diabetes Care 2007;30:3105–9. [DOI] [PubMed] [Google Scholar]
- [15].Brambilla P, Bedogni G, Moreno LA, et al. Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children. Int J Obes (Lond) 2006;30:23–30. [DOI] [PubMed] [Google Scholar]
- [16].Freedman DS, Serdula MK, Srinivasan SR, et al. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr 1999;69:308–17. [DOI] [PubMed] [Google Scholar]
- [17].Savva CS, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord 2000;24:1453–8. [DOI] [PubMed] [Google Scholar]
- [18].Romero-Velarde E, Vásquez-Garibay EM, Álvarez-Román YA. Waist circumference and its association with cardiovascular risk factors in obese children and adolescents. Bol Med Hosp Infant Mex 2013;70:357–611. [Google Scholar]
- [19].Umer A, Kelley GA, Cottrell LE, et al. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health 2017;17:683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Larsson B, Svärdsudd K, Welin L, et al. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. Br Med J (Clin Res Ed) 1984;288:1401–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ducimetiere P, Richard J, Cambien F. The pattern of subcutaneous fat distribution in middle-aged men and the risk of coronary heart disease: The Paris Prospective Study. Int J Obes 1986;10:229–40. [PubMed] [Google Scholar]
- [22].Freedman DS, Kahn HS, Mei Z, et al. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: The Bogalusa Heart Study. Am J Clin Nutr 2007;86:33–40. [DOI] [PubMed] [Google Scholar]
- [23].WHO Growth Reference for school-aged children and adolescents. Available at: http://www.who.int/growthref/en. accessed 22 April 2020. [Google Scholar]
- [24].de Onis M, Lobstein T. Defining obesity risk in childhood population: Which cut-offs should we use? Int J Pediatr Obes 2010;5:458–60. [DOI] [PubMed] [Google Scholar]
- [25].Rolland-Cachera MF. Childhood obesity: current definitions and recommendations for their use. Int J Pediatr Obes 2011;6:325–31. [DOI] [PubMed] [Google Scholar]
- [26].Fernandez JR, Redden DT, Pietrobelli A, et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr 2004;145:439–44. [DOI] [PubMed] [Google Scholar]
- [27].National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114: suppl: 555–76. [PubMed] [Google Scholar]
- [28].Foster BJ, Mackie AS, Mitsnefes M, et al. A novel method of expressing left ventricular mass relative to body size in children. Circulation 2008;117:2769–75. [DOI] [PubMed] [Google Scholar]
- [29].De Simone G, Devereux RB, Daniels SR, et al. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol 1995;25:1056–62. [DOI] [PubMed] [Google Scholar]
- [30].De Simone G, Daniels SR, Devereux RB. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 1992;20:1251–60. [DOI] [PubMed] [Google Scholar]
- [31].Fang X, Zuo J, Zhou J, et al. Childhood obesity leads to adult type 2 diabetes and coronary artery diseases. A 2-sample mendelian randomization study. Medicine (Baltimore) 2019;98:e16825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Abaci A, Tascilar ME, Saritas T, et al. Threshold value of subepicardial adipose tissue to detect insulin resistance in obese children. Int J Obes 2009;33:440–6. [DOI] [PubMed] [Google Scholar]
- [33].Csige I, Ujvárosy D, Szabó Z, et al. The impact of obesity on the cardiovascular system. J Diabetes Res 2018;2018: Article ID 3407306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Katzmarzyk PT, Srinivasan SR, Chen W, et al. Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics 2004;114:e198–205. [DOI] [PubMed] [Google Scholar]
- [35].Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Pediatrics 2005;115:1623–30. [DOI] [PubMed] [Google Scholar]
- [36].Harrington DM, Staiano AE, Broyles ST, et al. BMI percentiles for the identification of abdominal obesity and metabolic risk in children and adolescents: evidence in support of the CDC 95th percentile. Eur J Clin Nutr 2013;67:218–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Schneider HJ, Glaesmer H, Klotsche J, et al. Accuracy of anthropometric indicators of obesity to predict cardiovascular risk. J Clin Endocrinol Metab 2007;92:589–94. [DOI] [PubMed] [Google Scholar]
- [38].Flodmark CE, Sveger T, Nilsson-Ehle P. Waist measurement correlates to a potentially atherogenic lipoprotein profile in obese 12-14-year-old children. Acta Paediatr 1994;83:941–5. [DOI] [PubMed] [Google Scholar]
- [39].Roever LS, Resende E, Diniz A, et al. Abdominal obesity and association with atherosclerosis risk factors; the Uberlândia Heart Study. Medicine (Baltimore) 2016;95:e1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Maffeis CM, Banzato C, Talamini G. Waist-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr 2008;152:207–13. [DOI] [PubMed] [Google Scholar]
- [41].Chen B, Li HF. Waist circumference as an indicator of high blood pressure in preschool obese children. Asia Pac J Clin Nutr 2011;20:557–62. [PubMed] [Google Scholar]
- [42].Matsushita R, Isojima T, Takaya R, et al. Development of waist circumference percentiles for Japanese children and an examination of their screening utility for childhood metabolic syndrome: a population-based cross-sectional study. BMC Public Health 2015;13:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Mehta SK. Waist circumference to height ratio in children and adolescents. Clin Pediatr 2015;54:652–8. [DOI] [PubMed] [Google Scholar]
- [44].Finucane FM, Pittock S, Fallon M, et al. Elevated blood pressure in overweight and obese Irish children. Ir J Med Sci 2008;177:379–81. [DOI] [PubMed] [Google Scholar]
- [45].Pazin DC, Filla RC, Márcia O, et al. Waist circumference is associated with blood pressure in children with normal body mass index: a cross-sectional analysis of 3,417 school children. Arq Bras Cardiol 2017;109:509–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-heightratio are better predictors of cardiovasculardisease risk factors in children than body massindex. Int J Obes Relat Metab Disord 2000;24:1453–8. [DOI] [PubMed] [Google Scholar]
- [47].Wong CY, O’Moore-Sullivan T, Leano R, et al. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation 2004;101:3081–7. [DOI] [PubMed] [Google Scholar]
- [48].Hanevold C, Waller J, Daniels S, et al. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics 2004;113:328–33. [DOI] [PubMed] [Google Scholar]
- [49].Jing L, Binkley CM, Suever JD, et al. Cardiac remodeling and dysfunction in childhood obesity: a cardiovascular magnetic resonance study. J Cardiovasc Magn Reson 2016;18:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006;113:898–918. [DOI] [PubMed] [Google Scholar]
- [51].Lee H, Kong YH, Kim KH, et al. Left ventricular hypertrophy and diastolic function in children and adolescents with essential hypertension. Clin Hypertens 2015;21:21. [DOI] [PMC free article] [PubMed] [Google Scholar]


