Abstract
Background
Fear of falling is common in older people and associated with serious physical and psychosocial consequences. Exercise (planned, structured, repetitive and purposive physical activity aimed at improving physical fitness) may reduce fear of falling by improving strength, gait, balance and mood, and reducing the occurrence of falls.
Objectives
To assess the effects (benefits, harms and costs) of exercise interventions for reducing fear of falling in older people living in the community.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (July 2013), the Central Register of Controlled Trials (CENTRAL 2013, Issue 7), MEDLINE (1946 to July Week 3 2013), EMBASE (1980 to 2013 Week 30), CINAHL (1982 to July 2013), PsycINFO (1967 to August 2013), AMED (1985 to August 2013), the World Health Organization International Clinical Trials Registry Platform (accessed 7 August 2013) and Current Controlled Trials (accessed 7 August 2013). We applied no language restrictions. We handsearched reference lists and consulted experts.
Selection criteria
We included randomised and quasi‐randomised trials that recruited community‐dwelling people (where the majority were aged 65 and over) and were not restricted to specific medical conditions (e.g. stroke, hip fracture). We included trials that evaluated exercise interventions compared with no intervention or a non‐exercise intervention (e.g. social visits), and that measured fear of falling. Exercise interventions were varied; for example, they could be 'prescriptions' or recommendations, group‐based or individual, supervised or unsupervised.
Data collection and analysis
Pairs of review authors independently assessed studies for inclusion, assessed the risk of bias in the studies and extracted data. We combined effect sizes across studies using the fixed‐effect model, with the random‐effect model used where significant statistical heterogeneity was present. We estimated risk ratios (RR) for dichotomous outcomes and incidence rate ratios (IRR) for rate outcomes. We estimated mean differences (MD) where studies used the same continuous measures and standardised mean differences (SMD) where different measures or different formats of the same measure were used. Where possible, we performed various, usually prespecified, sensitivity and subgroup analyses.
Main results
We included 30 studies, which evaluated 3D exercise (Tai Chi and yoga), balance training or strength and resistance training. Two of these were cluster‐randomised trials, two were cross‐over trials and one was quasi‐randomised. The studies included a total of 2878 participants with a mean age ranging from 68 to 85 years. Most studies included more women than men, with four studies recruiting women only. Twelve studies recruited participants at increased risk of falls; three of these recruited participants who also had fear of falling.
Poor reporting of the allocation methods in the trials made it difficult to assess the risk of selection bias in most studies. All of the studies were at high risk of performance and detection biases as there was no blinding of participants and outcome assessors and the outcomes were self reported. Twelve studies were at high risk of attrition bias. Using GRADE criteria, we judged the quality of evidence to be 'low' for fear of falling immediately post intervention and 'very low' for fear of falling at short or long‐term follow‐up and all other outcomes.
Exercise interventions were associated with a small to moderate reduction in fear of falling immediately post intervention (SMD 0.37 favouring exercise, 95% confidence interval (CI) 0.18 to 0.56; 24 studies; 1692 participants, low quality evidence). Pooled effect sizes did not differ significantly between the different scales used to measure fear of falling. Although none of the sensitivity analyses changed the direction of effect, the greatest reduction in the size of the effect was on removal of an extreme outlier study with 73 participants (SMD 0.24 favouring exercise, 95% CI 0.12 to 0.36). None of our subgroup analyses provided robust evidence of differences in effect in terms of either the study primary aim (reduction of fear of falling or other aim), the study population (recruitment on the basis of increased falls risk or not), the characteristics of the study exercise intervention or the study control intervention (no treatment or alternative intervention). However, there was some weak evidence of a smaller effect, which included no reduction, of exercise when compared with an alternative control.
There was very low quality evidence that exercise interventions may be associated with a small reduction in fear of falling up to six months post intervention (SMD 0.17, 95% CI ‐0.05 to 0.38; four studies, 356 participants) and more than six months post intervention (SMD 0.20, 95% CI ‐0.01 to 0.41; three studies, 386 participants).
Very low quality evidence suggests exercise interventions in these studies that also reported on fear of falling reduced the risk of falling measured either as participants incurring at least one fall during follow‐up or the number of falls during follow‐up. Very low quality evidence from four studies indicated that exercise interventions did not appear to reduce symptoms of depression or increase physical activity. The only study reporting the effects of exercise interventions on anxiety found no difference between groups. No studies reported the effects of exercise interventions on activity avoidance or costs. It is important to remember that our included studies do not represent the totality of the evidence of the effect of exercise interventions on falls, depression, anxiety or physical activity as our review only includes studies that reported fear of falling.
Authors' conclusions
Exercise interventions in community‐dwelling older people probably reduce fear of falling to a limited extent immediately after the intervention, without increasing the risk or frequency of falls. There is insufficient evidence to determine whether exercise interventions reduce fear of falling beyond the end of the intervention or their effect on other outcomes. Although further evidence from well‐designed randomised trials is required, priority should be given to establishing a core set of outcomes that includes fear of falling for all trials examining the effects of exercise interventions in older people living in the community.
Keywords: Aged; Aged, 80 and over; Female; Humans; Male; Exercise; Independent Living; Accidental Falls; Accidental Falls/prevention & control; Fear; Fear/psychology; Postural Balance; Randomized Controlled Trials as Topic; Resistance Training; Tai Ji; Yoga
Plain language summary
Exercise for reducing fear of falling in older people living in the community
Many older people are afraid of falling, more so after experiencing a fall. Fear of falling can have a serious impact on an older person's health and life as it often reduces their physical and social activities.
We wanted to find out whether exercise, in the form of a planned, structured, repetitive physical activity aimed at improving physical fitness, helps to reduce fear of falling. Types of exercise interventions include balance training, strength and resistance training and three‐dimensional (3D) exercises, such as dance or Tai Chi. Exercise can be provided in various ways. It can involve group sessions where participants are taught in a class by an instructor or individuals may be provided with exercise instruction booklets, DVDs or tapes to enable them to exercise on their own without supervision.
We searched the medical literature up to July 2013 for studies that tested the effects of exercise and reported fear of falling in community‐dwelling people (i.e. who live either at home or in places of residence that do not provide nursing care or rehabilitation) aged 65 years and older. The studies compared exercise with no treatment or an alternative intervention, such as education.
Summary of the evidence
We included 30 studies in the review, with a total of 2878 participants whose average age ranged from 68 to 85 years. Most studies recruited mainly women. Twelve studies recruited participants at increased risk of falls and three of these recruited people who also had fear of falling. All of the studies were at some risk of bias mainly because the participants were aware what group they were in. This lack of blinding may have influenced the study results.
We found low quality evidence from 24 studies that exercise interventions result in a small to moderate reduction in fear of falling immediately after the intervention. Some exploratory analyses did not enable us to determine whether this effect differed in different groups of people, such as those at high risk of falling, or with different exercise interventions, such as group or individual exercise. We are very unsure that the effect of exercise on fear of falling is maintained in the next few months after the end of the intervention.
We only included studies that reported fear of falling, therefore the evidence on our other outcomes (occurrence of falls, depression, anxiety and physical activity) is only a small part of the total evidence of the effects of exercise on these outcomes. However, the evidence from nine studies included in our review showing that exercise reduced the risk and number of falls is consistent with the results of another Cochrane review testing the effects of exercise on preventing falls. The evidence on the other outcomes was far less and none of the included studies reported the effects of exercise interventions on activity avoidance or costs.
Conclusion
We concluded that exercise interventions in community‐dwelling older people probably reduce fear of falling to a limited extent immediately after the intervention, without increasing the risk or frequency of falls. We also concluded that there is not enough evidence to determine whether exercise interventions reduce fear of falling beyond the end of the intervention or their effect on other outcomes. We encourage further research on this topic.
Summary of findings
Summary of findings for the main comparison. Exercise for reducing fear of falling in older people living in the community.
| Exercise for reducing fear of falling in older people living in the community | ||||||
|
Population: older people living in the community
Setting: community
Intervention: exercise (planned, structured, repetitive and purposive physical activity aimed at improving physical fitness)1 Control: no intervention or alternative non‐exercise intervention2 | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Exercise | |||||
|
Fear of falling3 Immediately post intervention |
The mean fear of falling score4 in the intervention groups was 0.37 standard deviations higher (0.18 to 0.56 higher) (a higher score indicates less fear of falling) | SMD 0.37 (0.18 to 0.56) | 1692 (24 studies) | ⊕⊕⊝⊝ low5 | 0.2 SD represents a small difference, 0.5 SD a moderate difference and 0.8 SD a large difference We are unaware of any definitions of minimal clinically important difference for any fear of falling measure1 There was significant heterogeneity of effect sizes, which was attributable mainly to 1 study, Nguyen 2012, having a much larger effect size than other studies. Upon removal of this study, the effect size reduced to SMD 0.24, 95% CI 0.12 to 0.36; 23 studies; 1619 participants None of the subgroup analyses6 provided robust evidence of a difference in effect between different subgroups. The possible exception was evidence of a smaller effect, which included no reduction, of exercise when compared with an alternative control2 |
|
|
Fear of falling < 6 months follow‐up |
The mean fear of falling score in the intervention groups was 0.17 standard deviations higher (0.05 lower to 0.38 higher) (a higher score indicates less fear of falling) | SMD 0.17 (‐0.05 to 0.38) | 356 (4 studies) |
⊕⊝⊝⊝ very low7 | Very low quality evidence7 was also available from 3 studies (386 participants) at long‐term follow‐up (6 or more months post end of the intervention period): SMD 0.20, 95% CI ‐0.01 to 0.41 | |
|
Occurrence of at least 1 fall Follow‐up: 2 to 12 months |
500/10008 | 425/1000 (370 to 490) |
RR 0.85 (0.74 to 0.98) | 1113 (9 studies) | ⊕⊝⊝⊝ very low9 | Some studies measured falls using prospective falls diaries, some measured falls retrospectively and in some studies it was unclear whether falls were measured prospectively or retrospectively Note: Studies included in the analysis represent only a subset of studies evaluating the effect of exercise interventions on falls risk Very low quality evidence9 suggests exercise interventions were associated with a significant reduction in the rate of falls (rate ratio 0.68, 95% CI 0.53 to 0.87; 9 studies; 1121 participants) |
| Depressive symptoms10 | The mean depression score in the intervention groups was 0.08 standard deviations lower (0.28 lower to 0.13 higher) where a lower score indicates fewer symptoms of depression |
SMD ‐0.08 (‐0.28 to 0.13) |
406 (4 studies) | ⊕⊝⊝⊝ very low9 | 0.2 SD represents a small difference, 0.5 a moderate difference and 0.8 a large difference Note: Studies included in the analysis represent only a very small subset of studies evaluating the effect of exercise interventions on symptoms of depression |
|
| Anxiety | Mean HADS11 anxiety score = 4.3 (SD 3.4) | Mean HADS anxiety score = 4.3 (SD 3.9) | Difference between means = 0. No 95% CI reported | 77 participants (1 study) | ⊕⊝⊝⊝ very low9 | Anxiety was reported by the subscale of HADS, which ranged from 0 to 21 with a higher score indicating higher symptoms of anxiety Note: This study represents only a subset of studies evaluating the effect of exercise interventions on anxiety |
| Physical activity | The mean physical activity score in the intervention groups was 3.44 (1.65 lower to 8.54 higher) where a higher score indicates greater physical activity | MD 3.44 (‐1.65 to 8.54) | 547 (4 studies) | ⊕⊝⊝⊝ very low9 | All studies used the Physical Activity Scale for the Elderly (PASE) scale, which ranged from 0 to 400, with a higher score indicating greater physical activity Note: Studies included in the analysis represent only a subset of studies evaluating the effect of exercise interventions on physical activity |
|
| Activity avoidance or restriction | See comment | See comment | No studies reported this outcome | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; HADS: Hospital Anxiety and Depression Scale; MD: mean difference; RR: Risk ratio; SD: Standard deviation; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1The exercises interventions in the included trials fell into three categories: 3D (Tai Chi, Yoga); gait, balance, co‐ordination, functional tasks; and strength and resistance based interventions. They were either supervised or unsupervised activities, delivered in group settings or individually; and varied in duration from up to 12 weeks to over 26 weeks. The majority of exercise interventions were to be performed between one to three times per week. 2Twenty of the 30 included studies compared an exercise intervention with no intervention. Five studies used education as the control intervention; two studies used social home visits; one used individualised crafts/games; one used home safety assessment; and one used discussion groups. 3Measurement tools for fear of falling included:
FES: 10 questions rated 1 (very confident) to 10 (not confident at all). A higher score indicates a lower perceived self efficacy at avoiding falls. FES‐I: 16 questions rated 1 (not at all concerned) to 4 (very concerned). A higher score indicates a higher concern about falling. Short FES‐I: 7 questions rated 1 (not at all concerned) to 4 (very concerned). A higher score indicates a higher concern about falling. K‐FES: 10 questions rated on a scale from 1 (no confidence) to 10 (extremely confident). A higher score indicates a higher perceived self efficacy at avoiding falls. MFES: 14 questions rated 0 (not confident at all) to 10 (completely confident). A higher score indicates more confidence at avoiding falls. ABC: 16 questions. Some studies rated from 0 (no confidence) to 100 (complete confidence), whilst others rated from 0 (no confidence) to 10 (very confident). A higher score indicates higher balance confidence. Balance Self‐Perceptions Test: 12 questions rated 1 (no confidence) to 5 (complete confidence) in performing 12 activities of daily living without fear of loss of balance. VAS: Participants asked to rate their fear of falling on a scale of 0 to 100 (0 = low, 100 = high fear of falling).
Single item questions: (a) Participants asked to rate their fear of falling on a scale of 0 to 4 (0 = low, 4= high fear of falling). (b) Participants asked to rate their worry about falling on a scale of 1 to 5 (1 = not at all worried, 5 = extremely worried).
4Pooled effect sizes did not differ significantly between the different scales used to measure fear of falling (test for subgroup differences: Chi² = 5.21, df = 3, P value = 0.16). 5Downgraded by one level because of study limitations, primarily a likelihood of high risk of bias from lack of blinding, and one level because the funnel plot indicated possible publication bias. 6We carried out the following subgroup analyses: type of exercise intervention; frequency of exercise; duration of the exercise intervention; group exercises rather than individual exercises; studies which did and did not recruit participants on the basis of increased falls risk; studies whose primary aim was to reduce fear of falling and those with an alternative primary aim; no treatment versus an alternative intervention (e.g. education, social visits, craft activities, discussion groups) control group. 7Downgraded by one level because of study limitations, primarily a high likelihood of risk of bias from lack of blinding, one level because of possible publication bias, and one level because of the small number of studies contributing data to this outcome. 8Assumed control risk based on median control group risk across studies. 9Downgraded by one level because of study limitations, primarily likelihood of high risk of bias from lack of blinding, and two levels for indirectness of evidence. Our review includes only a subset of studies reporting the effect of exercise interventions on this outcome, as studies had to report fear of falling and this outcome to be included in our review. 10Measurement tools included for depression:
GDS Scale: 30 questions, range 0 to 30 with higher scores indicating greater symptoms of depression. GDS 5‐item: 5 questions, range 1 to 5 with higher scores indicating greater symptoms of depression. GDS‐20: 20 questions, range 0 to 20 with higher scores indicating greater symptoms of depression. HADS Depression subscale, range from 0 to 21 with higher scores indicating higher symptoms of depression.
11HADS = Hospital Anxiety and Depression Scale.
Background
Description of the condition
Falls are an important cause of morbidity and premature mortality among community‐dwelling adults aged 65 years and older. The consequences of falls can be severe, resulting in long‐term disability and substantial reduction in quality of life. Approximately one in three community‐dwelling older adults experience at least one fall (including medically attended falls and self reported falls not receiving any medical attention) each year (Fletcher 2004; Gillespie 2012b). This figure increases to two in three for those adults who have a history of a fall or who are afraid of falling (Andresen 2006).
Fear of falling is common in older people. A recent systematic review found that the prevalence of fear of falling in 19 studies of community‐dwelling older adults ranged from 21% to 85% (Scheffer 2008). An earlier review found the prevalence varied by falls history, ranging from 12% to 65% in community‐dwelling older adults who had not fallen and from 29% to 92% in those who had fallen (Legters 2002). A number of risk factors for fear of falling have been identified including old age (Scheffer 2008), female gender (Howland 1993; Scheffer 2008), previous falls (Cumming 2000), the presence of environmental hazards that increase the risk of falls (Legters 2002), dizziness (Howland 1993), visual problems (Wang 2012), poor self rated health (Cumming 2000), symptoms of depression and generalised anxiety (Legters 2002), poor balance and gait abnormalities (Tinetti 1990), cognitive impairment (Vellas 1997), functional dependence in activities of daily living (Scheffer 2008), living alone and lower levels of economic resources (Kempen 2009; Scheffer 2008). The consequences of fear of falling include falling, restriction or avoidance of daily activities, loss of independence, reduction in social activity, depression and a reduction in quality of life (Delbaere 2010; Legters 2002).
Tinetti and Powell defined fear of falling in 1993 as "a lasting concern about falling that leads to an individual avoiding activities that he/she remains capable of performing" (Tinetti 1993). Fear of falling has been conceptualised in different ways and measured using different tools and this, along with differences in characteristics of study populations and study settings, might explain some of the variability in the estimates of this condition (Jung 2008; Zijlstra 2007). While single‐item questions have been used to measure fear of falling, they are limited by their inability to measure variability in degrees of fear (Jorstad 2005). The most commonly used measures can be broadly divided into the following conceptualisations: those measuring fear of falling using single‐item questions; those measuring 'falls efficacy' (a person's belief in their ability to avoid falling during activity); those measuring confidence in maintaining balance; and those measuring concern or worry about falling during activities.
Examples of tools commonly used to measure falls efficacy include the Falls Efficacy Scale (FES) (Tinetti 1990) and adaptations to the scale (MFES (Hill 1996), rFES (Tinetti 1994)). The most commonly used measure of balance confidence is the Activities‐specific Balance Confidence scale (ABC) (Powell 1995). Commonly used measures for concern about falling include the international version of the FES in its long (FES‐I) (Yardley 2005) and short forms (Short FES‐I) (Kempen 2008), and the Modified Efficacy Scale (Hill 1996). The Survey of Activities and Fear of Falling in the Elderly (SAFFE) measures worry about falling, as well as activity restriction (based on the concept that activity avoidance may be an early sign of fear of falling) (Lachman 1998). In their systematic review of psychological outcome measures of falling, Jorstad 2005 highlighted inconsistency and confusion in the application of the various tools that have been used in this area. Contributing to this problem, there are often several variants of tools in use and the names of the scales may not match the construct they measure: e.g. FES‐I assesses concerns about falling instead of falls efficacy as its name may suggest (Kempen 2008; Yardley 2005). The large number of different tools highlights the importance of clearly identifying the construct being measured by each tool (Jorstad 2005).
Description of the intervention
This review is focused on exercise interventions. Exercise is defined as physical activity that is "planned, structured, repetitive, and purposive in the sense that the improvement or maintenance of one or more components of physical fitness is the objective" (CDC 2011) and includes gait, balance, functional, strength, resistance, flexibility, three‐dimensional (3D), such as dance or Tai Chi, and endurance training. Exercise interventions may be exercise 'prescriptions' or recommendations, done in groups or individually and may be supervised or unsupervised. Exercise prescriptions (e.g. the UK exercise referral scheme, the New Zealand "Green Prescription" or the US "Exercise is Medicine" programme) typically involve a healthcare professional assessment of current physical activity level, a referral to a physical activity specialist or service and an assessment by a physical activity specialist or service to determine a recommended exercise programme. Other exercise interventions include exercise supervised by direct contact with a professional, a trained non‐professional or volunteer, or exercise interventions without supervision: e.g. providing exercise instruction booklets, DVDs or tapes for people to use to exercise on their own. We included exercise interventions whether they were primarily aimed at reducing fear of falling or not.
How the intervention might work
Many factors may contribute to fear of falling, including gait and balance impairment, age‐related loss of muscle mass (sarcopenia), activity avoidance, anxiety, risk factors for falling (e.g. visual impairment) and previous falls. There is a complex relationship between fear of falling and falls (Hadjistravropoulos 2007), and exercise may impact directly on fear of falling or indirectly on factors associated with fear of falling and the risk of falling.
Exercise has been shown to be the single most effective strategy to reduce the number of falls in older adults (Sherrington 2008b). Exercise may reduce muscle loss, improve muscle strength, increase endurance, improve gait and balance and improve mood (Bula 2011b; Jung 2008). It may increase the increase the ability to get up following a fall, and may therefore, through these mechanisms, reduce fear of falling (Sherrington 2008b). Exercise may also enable individuals to perform more daily activities without falling, leading to a more positive appraisal of their ability to maintain balance during these activities (Howe 2011).
Why it is important to do this review
Fear of falling is associated with a range of negative health consequences, including an increased risk of falls (Delbaere 2010). Delbaere 2010 suggested that fear of falling can lead to falls independent of any objective balance impairment. Exercise interventions have been proposed as a promising means for the prevention of falls (Gillespie 2012b), and are recommended in evidence‐based guidelines for fall prevention across the world. Several recent reviews have been published on similar topics (Bula 2011b; Gillespie 2012b; Howe 2011; Liu 2009b; McClure 2005; Zijlstra 2007), but few have specifically focused on exercise and its potential effect on fear of falling. A narrative systematic review by Zijlstra and colleagues found that Tai Chi delivered in a group format, home‐based exercise interventions and multi‐component falls‐related programmes (some of which included exercise) reduced fear of falling in community‐dwelling older people (Zijlstra 2007). This review also found that only three included studies explicitly aimed to reduce fear of falling. A review by Bula 2011b found exercise interventions targeted at balance confidence risk factors and which decreased activity avoidance to be effective in improving balance confidence. Three Cochrane reviews of exercise interventions in older people do not report the effect of interventions on fear of falling, but do demonstrate that exercise interventions can improve balance (Howe 2011), reduce the risk and rate of falls (Gillespie 2012b) and that progressive resistance strength training improves muscle strength and activities of daily living such as walking and bathing (Liu 2009b). One further review of co‐ordinated community‐wide multi‐strategy initiatives, some of which included the promotion of physical activity or community walking programmes, found that the population‐based approach was effective in preventing fall‐related injury, but again the review did not report on fear of falling (McClure 2005). This stresses the importance of our review, which aimed to appraise the existing literature for evidence, or the lack of evidence, that exercise reduces fear of falling.
Objectives
To assess the effects (benefits, harms and costs) of exercise interventions for reducing fear of falling in older people living in the community.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomised and quasi‐randomised (method of allocating participants to a treatment that is not strictly random, e.g. by date of birth, hospital record number, alternation) controlled trials. We included studies with cluster allocation, but excluded those with only one or two clusters in each intervention group because randomisation was unlikely to achieve balance in the important prognostic factors between intervention groups.
Types of participants
We included trials where the majority of the study population comprised people aged 65 years and over who were 'community‐dwelling', i.e. living either at home or in places of residence that do not provide nursing care or rehabilitation. We excluded trials including combined populations (i.e. community‐dwelling older people and those receiving nursing or rehabilitation care) if they did not report separate results for community‐dwelling adults. We also excluded trials whose populations were restricted to individuals with a specific condition (e.g. stroke or hip fracture). We included trials irrespective of whether the participants were people who had recorded fear of falling or had a history of falling.
Types of interventions
We included studies reporting on the effect of exercise interventions, whether an exercise 'prescription' or a recommendation, done in a group or individually and supervised or not. The content of the exercises varied: for example, gait, balance and functional training; strength or resistance training; flexibility training; 3D training such as Tai Chi, Qigong and dance; and endurance training, which comprised aerobic exercise aimed at cardiovascular fitness. We excluded multi‐component interventions that combined exercises with other intervention components (such as medication reviews, home hazard assessments, screening for and managing visual impairment, cognitive behavioural interventions and other interventions that aim to address risk factors for falling) due to the difficulty of attributing observed effects to the exercise.
The comparators of interest included no intervention (usual care) and alternative non‐exercise intervention, e.g. education. We excluded studies where the comparator treatment might have increased exercise, e.g. provision of lifestyle advice including advice about exercise.
Types of outcome measures
We included trials that measured fear of falling as a primary or secondary outcome.
Primary outcomes
The primary outcome was fear of falling, which included measurement using single‐item measures and measures of falls efficacy, balance confidence, and concern or worry about falling.
Measurement tools for these primary outcomes were ascertained from a systematic review measuring psychological outcomes of fear of falling (Jorstad 2005), and tools developed since that review (Kempen 2008; Yardley 2005). Where reported by the included studies, we used the following:
Fear of falling as measured by a single‐item question.
Falls efficacy as measured by the Falls Efficacy Scale (FES; Tinetti 1990) and its associated versions, FmES (Hill 1996), rFES (Tinetti 1994), and FES‐UK (Parry 2001).
Balance confidence as measured by the Activities‐specific Balance Confidence scale for older adults (ABC) (Powell 1995) (and its UK version ABC‐UK (Parry 2001)).
Concern about falling as measured by the international version of the FES in its long (FES‐I) (Yardley 2005) and short forms (Short FES‐I) (Kempen 2008), Mobility Efficacy Scale (MES) (Lusardi 1997), aFES (Lusardi 1997), and amFES (Lusardi 1997), and worry about falling measured using the Survey of Activities and Fear of Falling in the Elderly (SAFFE) (Yardley 2002).
Secondary outcomes
Occurrence of falls: number or rate of falls, or participants experiencing at least one fall (fallers). Falls were included as a secondary outcome as there may be beneficial effects on falls from exercise but they may also occur as adverse events during exercise.
Activity avoidance or restriction: the modified SAFFE (Yardley 2002), or single questions asking about activity avoidance (Jorstad 2005).
Depression: the depression subscale of the Hospital Anxiety and Depression Scale (HADS), the Geriatric Depression Scale (GDS; Yesavage 1983), GDS‐5 (Hoyl 1999), GDS‐20 (Gottfries 1997), or the Cornell Scale for Depression in Dementia (CSDD) (Rodda 2011).
Anxiety: Beck Anxiety Inventory, the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS), Penn State Worry Questionnaire and Geriatric Mental State Examination (Therrien 2011). These scales have been validated for use in older adults.
Compliance with or adherence to exercise interventions, including measures of physical activity.
Cost.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (July 2013), the Central Register of Controlled Trials (CENTRAL 2013, Issue 7), MEDLINE (1946 to July Week 3 2013), EMBASE (1980 to 2013 Week 30), CINAHL (1982 to July 2013), PsycINFO (1967 to August 2013) and Allied and Complementary Medicine (AMED) (1985 to August 2013). We did not apply any restrictions based on language or publication status.
In MEDLINE, we combined the subject‐specific terms with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2011). Search strategies for CENTRAL, MEDLINE, EMBASE, CINAHL, PsycINFO and AMED are shown in Appendix 1.
We searched the WHO International Clinical Trials Registry Platform (accessed 7 August 2013) and Current Controlled Trials (accessed 7 August 2013) for ongoing and recently completed trials.
Searching other resources
We searched reference lists of existing reviews on fear of falling as well as falls prevention (Bula 2011b; Gillespie 2012b; Sherrington 2008b; Zijlstra 2007), and the reference lists of studies included in the review (see Included studies). We contacted experts in the field and relevant trial authors to identify appropriate unidentified studies (published or unpublished). We contacted the Falls and Bone Section of the British Geriatrics Society for information on unpublished or ongoing studies. We searched conference abstracts from the 55th, 56th and 57th Gerontological Society of America Scientific Meetings (2002 to 2004) and the 2004 Annual Scientific Meeting of the American Geriatrics Society.
Data collection and analysis
Review authors worked in pairs to independently assess studies for eligibility, to extract data and to assess each study's risk of bias.
Selection of studies
Pairs of review authors (from DK, AK, HC, RZ, DS, JC, ZS, CB, DH, SG, HG, TM, AB, MP, SI, KD) independently checked all titles and abstracts retrieved to assess eligibility against inclusion criteria. We obtained full‐text copies of all papers considered to be potentially eligible. Disagreements were resolved by discussion between the pairs of authors and, where necessary, a third review author (DK, DS or SI). We contacted authors of primary studies for clarification where necessary. We used a hierarchy of reasons for exclusion, based in turn on the consideration of study design, participants, interventions and outcomes. Usually only the first encountered reason for exclusion is given in the table of Characteristics of excluded studies, except where supplementary reasons were also informative. For clarity, we provide more details of interventions, namely multi‐component interventions and comparator treatments that may have increased exercise.
Data extraction and management
Pairs of members of the review team (as listed above) completed data extraction independently using a standard data extraction form. Disagreements were resolved by discussion between the pairs of review authors and where necessary, a third review author (DK, DS or SI).
Assessment of risk of bias in included studies
Pairs of members of the review team (as listed above) assessed risk of bias using the tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We reported the following seven domains: random sequence generation; allocation concealment; blinding (participants and personnel); blinding (outcome assessment); incomplete outcome data; selective outcome reporting; and 'other bias' (comparability of treatment and control group at entry, and post‐randomisation recruitment bias in studies with cluster allocation). Where necessary, we contacted study authors for clarification. Disagreements were resolved by discussion between the pairs of review authors and where necessary, a third review author (DK, DS or SI).
Measures of treatment effect
We estimated risk ratios with 95% confidence intervals (CI) for dichotomous data. For continuous data, we estimated mean differences (and 95% CI) where studies reported the same measure in the same format and standardised mean differences (and 95% CI) where different measures were used or where the same measure was presented in different formats. Where cluster‐randomised controlled trials are included in the meta‐analyses, we adjusted the standard errors of effect sizes for clustering, and entered these into meta‐analyses estimating standardised mean differences. Where means and standard deviations are reported for change from baseline scores, we entered these into meta‐analyses estimating mean differences not standardised mean differences. One study reported a standard deviation of zero for the FES score at follow‐up (Yoo 2010): we used a standard deviation of 0.00001 to allow data from this study to be included in the meta‐analysis. We estimated pooled incidence rate ratios (and 95% CI) for falls rates using an inverse variance meta‐analysis.
We entered raw data as presented in the articles, or as obtained from authors, into the meta‐analyses. For falls rates, because most studies did not report the number of falls and person time at risk, we calculated log incidence rate ratios and standard errors from published rate ratios and entered these into the meta‐analysis. For two studies (Weerdesteyn 2006; Wolf 1996), we used data on the number of falls and person time at risk and estimated the log incidence rate ratio and its standard error using Poisson regression in Stata v11.0. Weerdesteyn 2006 provided unpublished data for this analysis; these excluded those from a non‐randomised group that were included in analyses in the published paper. For Wolf 1996, we calculated the number of falls and person years at risk for the combined intervention groups from published data. For studies that employed a cross‐over design, we used outcome measurement scores prior to the cross‐over to ensure the control group still met the review inclusion criteria. For the majority of scales used in the studies, a higher score represents less fear of falling. However, some studies used a scale where a higher score means a higher fear of falling. Therefore, to correct for differences in the direction of the scale, the mean scale score in studies using a higher score to indicate a higher fear of falling was multiplied by ‐1 to ensure that all scales pointed in the same direction. The standard deviation was not modified in these studies.
Unit of analysis issues
We adjusted the standard errors for effect sizes of continuous outcome measures to take account of clustering in cluster‐randomised trials. For fear of falling measures, we used the intra cluster correlation coefficient (ICC) and its 95% CI calculated from the data of an ongoing UK trial evaluating an exercise intervention for community‐dwelling older people, which allocated participants to treatment arm by general practice (Iliffe 2010b). The standard error of the effect size was inflated by the square root of the design effect, i.e. [1+ (m‐1)*ICC], where m = average cluster size. For depression measures, we used the ICC from a UK trial of exercise for depression in older care home residents (Underwood 2013). Where studies were adjusted for clustering, it was not possible to present means and standard deviations for outcome measures in the forest plots because the adjustment for clustering required data on the adjusted standard error of the difference between the means to be entered into the meta‐analysis. We have therefore reported means and standard deviations for fear of falling scales in Table 2 and for depression scales in Table 3.
1. Means and SDs for fear of falling scales entered as SMD and SE into the meta‐analysis.
| Study | Time point | Scale | Scale direction | Intervention group mean | Intervention group SD | Intervention group number of participants | Control group mean | Control group SD | Control group number of participants |
| Clemson 2010 | Post intervention | MFES | High score = low FOF | 49.4 | 6.1 | 17 | 42.6 | 9.4 | 12 |
| Clemson 2010 | Post intervention | ABC | High score = low FOF | 995.3 | 377.9 | 17 | 805.0 | 297.1 | 12 |
| Freiberger 2012 | Post intervention | ABC | High score = low FOF | 148.6 | 16.8 | 57 | 150.3 | 12.4 | 64 |
| Haines 2009 | Post intervention | ABC | High score = low FOF | 5.3 | 2.0 | 19 | 5.6 | 2.0 | 28 |
| Halvarsson 2011 | Post intervention | FES‐I | High score = high FOF | ‐22.6 | 6.1 | 34 | ‐28.9 | 9.3 | 21 |
| Hinman 2002 | Post intervention | MFES | High score = low FOF | 134.6 | 10.9 | 58 | 135.4 | 14.1 | 30 |
| Karinkanta 2012 | Post intervention | 100 mm VAS | High score = high FOF | ‐10.7 | 15.7 | 106 | ‐16.9 | 21.2 | 34 |
| Lai 2013 | Post intervention | MFES | High score = low FOF | 136.0 | 6.1 | 15 | 116.4 | 27.9 | 15 |
| Lajoie 2004 | Post intervention | ABC | High score = low FOF | 92.0 | 8.0 | 12 | 82.5 | 26.0 | 12 |
| Logghe 2009 | Post intervention | FES | High score = high FOF | ‐4.9 | 4.4 | 73 | ‐5.8 | 5.3 | 89 |
| McCormack 2004 | Post intervention | MFES | High score = low FOF | 9.1 | 1.5 | 27 | 8.1 | 2.4 | 7 |
| Nguyen 2012 | Post intervention | FES | High score = high FOF | ‐35.2 | 5.9 | 39 | ‐51.4 | 8.1 | 34 |
| Resnick 2008 | Post intervention | Participants asked to rate fear of falling on a scale of 0 to 4 (0 = low, 4 = high) | High score = high FOF | ‐1.6 | 1.8 | 64 | ‐1.8 | 1.8 | 39 |
| Reinsch 1992 | Post intervention | Participants asked to rate worry about falling on a scale of 1 to 5 (1 = not at all worried, 5 = extremely worried) | High score = high FOF | ‐1.5 | 0.8 | 44 | ‐1.7 | 1.3 | 42 |
| Tiedemann 2012 | Post intervention | FES‐I | High score = high FOF | ‐9.8 | 4.5 | 27 | ‐10.6 | 3.2 | 25 |
| Ullmann 2010 | Post intervention | FES | High score = low FOF | 9.3 | 1.4 | 19 | 9.0 | 1.7 | 22 |
| Ullmann 2010 | Post intervention | ABC | High score = low FOF | 83.5 | 13.5 | 19 | 86.4 | 10.6 | 22 |
| Vogler 2009 | Post intervention | MFES | High score = low FOF | 8.6 | 1.8 | 114 | 8.5 | 1.8 | 57 |
| Vrantsidis 2009 | Post intervention | MFES | High score = low FOF | 8.6 | 1.6 | 26 | 7.7 | 1.9 | 29 |
| Wallsten 2006 | Post intervention | ABC | High score = low FOF | 76.2 | 20.3 | 25 | 70.5 | 12.3 | 28 |
| Weerdesteyn 2006 | Post intervention | ABC | High score = low FOF | 76.3 | 13.4 | 29 | 69.7 | 17.8 | 23 |
| Westlake 2007 | Post intervention | ABC | High score = low FOF | 85.7 | 9.5 | 17 | 79.1 | 24.2 | 19 |
| Wolf 2001 | Post intervention | 100 mm VAS | High score = high FOF | ‐38.6 | 29.7 | 37 | ‐44.7 | 29.9 | 40 |
| Yang 2012 | Post intervention | MFES | High score = low FOF | 9.2 | 1.2 | 59 | 9.1 | 1.4 | 62 |
| Yoo 2010 | Post intervention | K‐FES | High score = low FOF | 100.0 | 0.0 | 11 | 95.4 | 6.8 | 10 |
| Zhang 2006 | Post intervention | FES | High score = low FOF | 78.3 | 4.0 | 24 | 75.3 | 5.9 | 23 |
ABC: Activities‐specific Balance Confidence scale FES: Falls Efficacy Scale FES‐I: FES‐International FOF: fear of falling K‐FES: Korean version of the FES MFES: Modified Falls‐Efficacy Scale VAS: visual analogue scale
2. Means and SDs for depression scales entered into meta‐analyses as SMD and SE.
| Study | Time point | Scale | Scale direction | Intervention group mean | Intervention group SD | Intervention group number of participants | Control group mean | Control group SD | Control group number of participants |
| Halvarsson 2011 | Post intervention | GDS‐20 | Higher score = greater symptoms of depression | 2.7 | 2.4 | 34 | 3 | 2 | 21 |
| Resnick 2008 | Post intervention | GDS 5‐item | Higher score = greater symptoms of depression | 0.41 | 0.79 | 64 | 0.79 | 1.1 | 39 |
| Vogler 2009 | Post intervention | GDS | Higher score = greater symptoms of depression | 7.2 | 4.49 | 114 | 6.4 | 4.3 | 57 |
| Wolf 2001 | Post intervention | HADS‐Depression | Higher score = greater symptoms of depression | 4.8 | 3.85 | 37 | 5.6 | 4.01 | 40 |
GDS: Geriatric Depression Scale HADS: Hospital Anxiety and Depression Scale
Where studies included more than one intervention arm that met our inclusion criteria, we combined results from intervention arms in the meta‐analyses. Where appropriate for subgroup analyses, we made comparisons separately for each intervention arm. For cross‐over trials, we incorporated only data from the first period prior to cross‐over. Some studies reported outcomes (fear of falling and depression) at multiple time points. We therefore undertook meta‐analyses at several times points including immediately post intervention, short‐term follow‐up (less than six months post intervention) and long‐term follow‐up (six months or more post intervention).
Dealing with missing data
We contacted study authors for missing data. Where standard deviations were not reported, but 95% CI were reported, we divided the CI width by 3.92, and multiplied by the square root of the sample size (Higgins 2011b). We used only the available data and did not impute missing values.
Assessment of heterogeneity
We assessed heterogeneity between effect sizes of included studies by visual inspection of forest plots and by using the Chi² test for heterogeneity (with a P value of < 0.1) and described inconsistency between trials using the percentage of the variability in effect estimates that is due to heterogeneity rather than chance (I² statistic).
Assessment of reporting biases
Where an individual meta‐analysis contained at least 10 studies, we assessed publication bias using funnel plots and Egger's test.
Data synthesis
We combined effect sizes across studies using the fixed‐effect model where there was no statistical heterogeneity. Where there was statistically significant heterogeneity that could not readily be explained, we used a random‐effects meta‐analysis to incorporate heterogeneity among studies. We pooled data across intervention arms for trials that had more than one intervention arm of interest. However, where appropriate for the subgroup analysis, we made comparisons separately for each intervention arm.
Subgroup analysis and investigation of heterogeneity
Where a minimum of two studies existed, we undertook the following a priori defined subgroup analyses, exploring the effect of exercise interventions on fear of falling immediately post intervention by:
type of exercise classified using the ProFaNE taxonomy of interventions (ProFaNE 2011);
type of control group (alternative intervention versus no intervention);
baseline falls risk (studies recruiting participants at increased risk of falls, e.g. history of falls or other risk factors for falls versus those not recruiting participants on this basis);
type (individual versus group), frequency (one to three times per week, four or more times per week) and duration (0 to 12 weeks, 13 to 26 weeks, more than 26 weeks) of exercise;
primary aim of the study (to reduce fear of falling versus other primary aim).
We investigated whether effect sizes in subgroups were significantly different by inspecting the overlap of confidence intervals and by using the test for subgroup differences available in Review Manager software (RevMan 2014).
We did not undertake two a priori defined subgroup analyses for reasons explained in Differences between protocol and review.
Sensitivity analysis
We had planned to undertake sensitivity analyses to explore the robustness of our findings by restricting analyses to studies at low risk of selection bias (those with adequate allocation concealment) and those at low risk of detection bias. We did undertake a sensitivity analysis based on attrition bias (restricting to studies with follow‐up on more than 80% of participants). We also undertook three other sensitivity analyses: (a) assessing the effect of removing one study that had a much larger effect size than other studies, (b) assessing the effect of using ABC scores instead of FES scores for two studies that used both scales and (c) assessing the effect of varying the ICC used to adjust standard errors of effect sizes in cluster‐randomised controlled trials.
'Summary of findings' tables
We have produced a 'Summary of findings' table for fear of falling post intervention. We used the GRADE approach (Chapter 12.2, Higgins 2011a) to assess the quality of evidence related to key outcomes: fear of falling, falls rate, occurrence of at least one fall, depressive symptoms, anxiety and physical activity.
Results
Description of studies
Results of the search
The search strategies identified 916 citations from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (24 records); Cochrane Central Register of Controlled Trials (84 records), MEDLINE (186 records), EMBASE (169 records), CINAHL (290 records), PsycINFO (36 records), AMED (23 records), the WHO International Clinical Trials Registry Platform (20 records) and Current Controlled Trials (84 records). We identified a further 130 potentially eligible citations from handsearching reference lists of relevant systematic reviews and included studies and consulting with experts in the field.
After examination of the title and abstract from the search results, we identified a total of 209 articles for potential inclusion, for which we obtained the full texts for more detailed evaluation. From the 209 articles, we included 30 studies (published in 53 articles), excluded 134 studies (published in 144 articles) and two studies (published in three articles) were ongoing. Seven studies (published in nine articles) await classification. A flow diagram summarising the study selection process is shown in Figure 1.
1.
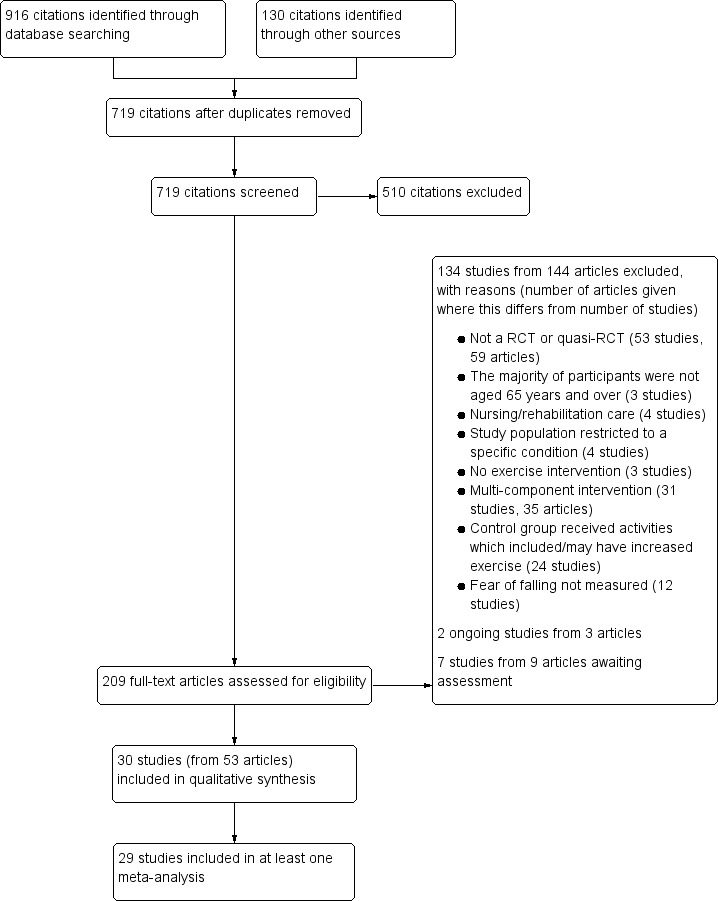
Study flow diagram
Included studies
Design
Thirty studies have been included in this review (see Characteristics of included studies for details of these). The majority of the studies were randomised controlled trials (n = 29), including two cluster‐randomised controlled trials (Reinsch 1992; Resnick 2008), and two cross‐over trials (Lai 2013; Wallsten 2006). One study was a quasi‐randomised trial (Lajoie 2004).
Aim
The primary aim of seven studies was to reduce fear of falling (Freiberger 2012; Halvarsson 2011; Karinkanta 2012; McCormack 2004; Wallsten 2006; Yoo 2010; Zhang 2006). The primary aim of the majority (n = 22) of the included studies was to improve balance, physical performance and/or prevent falls (Barnett 2003; Campbell 1997; Clemson 2010; Haines 2009; Hinman 2002; Lai 2013; Lajoie 2004; Lin 2007; Logghe 2009; Nguyen 2012; Reinsch 1992; Rendon 2012; Sihvonen 2004; Tiedemann 2012;Ullmann 2010; Vogler 2009; Vrantsidis 2009; Weerdesteyn 2006; Westlake 2007; Wolf 1996; Wolf 2001; Yang 2012). One study was aimed at improving self efficacy for exercise, exercise outcome expectations, exercise and overall physical activity (Resnick 2008).
Sample sizes
A total of 2878 community‐dwelling older adults participated in the 30 included studies. Sample sizes in included studies ranged from 21 participants (Yoo 2010) to 269 (Logghe 2009).
Setting
The included studies were based in 12 countries. Eight studies were conducted in Australia (Barnett 2003; Clemson 2010; Haines 2009; McCormack 2004; Tiedemann 2012;Vogler 2009; Vrantsidis 2009; Yang 2012), seven in the USA (Hinman 2002; Reinsch 1992; Rendon 2012; Resnick 2008; Ullmann 2010; Wallsten 2006; Wolf 1996), three in the Netherlands (Logghe 2009; Weerdesteyn 2006; Wolf 2001), two in Canada (Lajoie 2004; Westlake 2007), two in Finland (Karinkanta 2012; Sihvonen 2004), two in Taiwan (Lai 2013; Lin 2007), one in China (Zhang 2006), one in Germany (Freiberger 2012), one in New Zealand (Campbell 1997), one in South Korea (Yoo 2010), one in Sweden (Halvarsson 2011), and one in Vietnam (Nguyen 2012).
Participants
Four studies recruited only women (Campbell 1997; Karinkanta 2012; Sihvonen 2004; Yoo 2010). Of the 26 studies that recruited both sexes, 25 reported the sex of participants, with most of these including a majority of women (ranging from 51% to 89%). The mean age of participants ranged from 68 years to 85 years. In 12 studies the mean age was less than 75 years (Barnett 2003; Hinman 2002; Karinkanta 2012; Lai 2013; Lajoie 2004; Nguyen 2012; Resnick 2008; Tiedemann 2012; Vrantsidis 2009; Weerdesteyn 2006; Yoo 2010; Zhang 2006); in all other studies the mean age was 75 years or older. Two studies specifically recruited people aged over 75 (Wolf 2001) and over 80 (Campbell 1997).
Twelve studies recruited participants who were at increased risk of falls (either because they had previously fallen or because they had other risk factors for falls) (Barnett 2003; Clemson 2010; Freiberger 2012; Haines 2009; Halvarsson 2011; Lin 2007; Logghe 2009; Vogler 2009; Vrantsidis 2009; Weerdesteyn 2006; Yang 2012; Zhang 2006). Three of these studies recruited participants who had fear of falling in addition to being at increased risk of falls (Freiberger 2012; Halvarsson 2011; Yang 2012). The inclusion and exclusion criteria for each study are presented in the Characteristics of included studies table.
Interventions
Five studies had more than one intervention arm that met the inclusion criteria (Hinman 2002; Karinkanta 2012; McCormack 2004; Vogler 2009; Wolf 1996). As a result, 36 interventions were reported from the 30 included studies. We classified these interventions according to the fall prevention classification taxonomy developed by ProFaNE (ProFaNE 2011), with nine (25%) classified as 3D (Tai Chi, Yoga); 19 (53%) classified as gait, balance, co‐ordination, functional tasks; and eight (22%) classified as strength and resistance based interventions. Interventions were also categorised according to whether they were supervised activities (n = 27; 75%) or unsupervised activities (n = 9; 25%), see Table 4. Additionally, we categorised interventions by whether they were delivered in group settings (n = 20; 56%) or individually (n = 16; 44%), and according to the duration of the intervention (i.e. up to 12 weeks (n = 22; 61%), 13 to 26 weeks (n = 7; 19%) and more than 26 weeks (n = 7; 19%). The majority (n = 32; 89%) of the exercise interventions were to be performed between one to three times per week. Four (11%) exercise interventions were to be carried out four or more times a week. Details are provided in the Characteristics of included studies table.
3. Exercise type classified using the ProFaNE taxonomy of interventions (ProFaNE 2011).
| Study | Exercise type classified using the ProFaNE taxonomy of interventions (ProFaNE 2011) | Control Type |
Supervised activity? |
Group setting? |
| Barnett 2003 | Gait, balance, co‐ordination, functional tasks | Education (falls prevention) | Supervised | Group |
| Campbell 1997 | Strength/resistance | Social visits | Unsupervised | Individual |
| Clemson 2010 | Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual |
| Freiberger 2012 | Strength/resistance | No intervention | Supervised | Group |
| Haines 2009 | Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual |
| Halvarsson 2011 | Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group |
| Hinman 2002 | Home exercise programme: gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual |
| Hinman 2002 | Computerised balance training: gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual |
| Karinkanta 2012 | Resistance training: strength/resistance | No intervention | Supervised | Group |
| Karinkanta 2012 | Balance jumping: gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group |
| Karinkanta 2012 | Combined resistance and balance jumping: gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group |
| Lai 2013 | Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual |
| Lajoie 2004 | Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual |
| Lin 2007 | Gait, balance, co‐ordination, functional tasks | Home safety assessment | Supervised | Individual |
| Logghe 2009 | 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
| McCormack 2004 | Holistic exercise: 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
| McCormack 2004 | Conventional exercise: strength/resistance | No intervention | Supervised | Group |
| Nguyen 2012 | 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
| Reinsch 1992 | Gait, balance, co‐ordination, functional tasks | Discussion group | Unsupervised | Individual |
| Rendon 2012 | Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Individual |
| Resnick 2008 | Strength/resistance | Education (nutrition) | Supervised | Group |
| Sihvonen 2004 | Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual |
| Tiedemann 2012 | 3D (Tai Chi, Qi Gong, dance, yoga) | Education (falls prevention) | Supervised | Group |
| Ullmann 2010 | 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
| Vogler 2009 | Seated exercise: strength/resistance | Social visits | Unsupervised | Individual |
| Vogler 2009 | Weight‐bearing exercise: strength/resistance | Social visits | Unsupervised | Individual |
| Vrantsidis 2009 | 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
| Wallsten 2006 | 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
| Weerdesteyn 2006 | Gait, balance, co‐ordination, functional tasks | No intervention | Supervised | Group |
| Westlake 2007 | Gait, balance, co‐ordination, functional tasks | Education (falls prevention) | Supervised | Group |
| Wolf 1996 | Tai chi: 3D (Tai Chi, Qi Gong, dance, yoga) | Education (gerontology) | Supervised | Group |
| Wolf 1996 | Computerised balance training: gait, balance, co‐ordination, functional tasks | Education (gerontology) | Supervised | Individual |
| Wolf 2001 | Gait, balance, co‐ordination, functional tasks | Crafts/games | Supervised | Individual |
| Yang 2012 | Gait, balance, co‐ordination, functional tasks | No intervention | Unsupervised | Individual |
| Yoo 2010 | Strength/resistance | No intervention | Supervised | Group |
| Zhang 2006 | 3D (Tai Chi, Qi Gong, dance, yoga) | No intervention | Supervised | Group |
Five studies had two or more arms with exercise interventions. Each intervention arm is described separately in the table.
Controls
Twenty of the studies compared an exercise intervention with no intervention (see Table 4). Five studies used education as the control intervention: three on falls prevention (Barnett 2003; Tiedemann 2012; Westlake 2007), one on nutrition (Resnick 2008), and one on a range of topics including medicines, sleep, cognitive impairment and bereavement (Wolf 1996). Two studies used social home visits (Campbell 1997; Vogler 2009), one used individualised crafts/games (Wolf 2001), one used home safety assessment (Lin 2007), and one used discussion groups (Reinsch 1992).
Outcomes
Seven studies used single‐item questions for participants to measure fear of falling. Four of these studies asked participants to rate their fear of falling on a numerical scale: Resnick 2008 used a numerical scale of 0 to 4 (0 = low, 4 = high); Karinkanta 2012 and Wolf 2001 used a visual analogue scale (VAS) from 0 (no fear of falling) to 100 mm (very afraid of falling); and Lin 2007 used a VAS from 0 (no fear) to 10 cm (extremely fearful). One study measured worry about falling on a scale of 1 to 5 (1 = not at all worried, 5 = extremely worried) (Reinsch 1992). Two studies employed a single question with binary or ordinal response for fear of falling: in Barnett 2003 participants were asked if they were afraid of falling (yes/no) and in Sihvonen 2004 participants were asked "Generally speaking are you afraid of falling?" with the response options of "No", "Yes, some" or "Yes, a lot". Falls efficacy was measured by FES in six studies (Campbell 1997; Logghe 2009; Nguyen 2012; Ullmann 2010; Wolf 1996; Zhang 2006), MFES in seven studies (Clemson 2010; Hinman 2002; Lai 2013; McCormack 2004; Vogler 2009; Vrantsidis 2009; Yang 2012), and K‐FES in one study (Yoo 2010). Nine studies measured balance confidence using ABC (Clemson 2010; Freiberger 2012; Haines 2009; Lajoie 2004; Rendon 2012; Ullmann 2010; Wallsten 2006; Weerdesteyn 2006; Westlake 2007). Two studies used both FES and ABC (Clemson 2010; Ullmann 2010). Concerns about falling were measured by FES‐I in one study (Halvarsson 2011) and short FES‐I in one study (Tiedemann 2012).
All studies reported fear of falling immediately at the end of the intervention period, apart from Barnett 2003, which reported fear of falling halfway through the one‐year intervention period, and Lin 2007, which reported fear of falling at two and four months after the end of the intervention period. Six studies reported fear of falling in the short term (less than six months) post intervention (Clemson 2010; Lin 2007; Vogler 2009; Westlake 2007; Wolf 1996; Wolf 2001). Clemson 2010 reported data at three and six months. We included the three‐month data from Clemson 2010 and the two‐month data from Lin 2007 in our short‐term follow‐up (less than six months) analyses. These were most similar to the other studies in the same analyses, which reported data at one or three months. Three studies reported fear of falling in the long term (six months or more post intervention) (Freiberger 2012; Karinkanta 2012; Logghe 2009). Freiberger 2012 reported fear of falling at two time points in the long term (six months and 18 months post intervention), and we used the six‐month scores in the meta‐analysis as the other studies in the meta‐analysis reported data at nine or 12 months.
Eight studies either did not present data for outcome measures in the format required for meta‐analysis (i.e. mean, SDs) or did not report data for their measures of fear of falling (Clemson 2010; Halvarsson 2011; Lajoie 2004; Rendon 2012; Ullmann 2010; Vogler 2009; Wallsten 2006; Weerdesteyn 2006). We were able to obtain the data from study authors for seven of these studies (Clemson 2010; Halvarsson 2011; Lajoie 2004; Ullmann 2010; Vogler 2009; Wallsten 2006; Weerdesteyn 2006), enabling their inclusion in the meta‐analyses. Clemson 2010 provided means and SDs for M‐FES and ABC scores at baseline, post intervention and three months post intervention. Halvarsson 2011 provided means and SDs for FES‐I and GDS‐20 scores at baseline and post intervention. Lajoie 2004 provided means and SDs for the ABC score at baseline and post intervention. Ullmann 2010 provided means and SDs for the ABC and FES at baseline and prior to six participants form the control group crossing over into the intervention group. Vogler 2009 provided means and SDs for the MFES and GDS post intervention and at 24 weeks. Wallsten 2006 provided means and SDs for the ABC post intervention. Weerdesteyn 2006 provided means and SDs for ABC post intervention and number of falls and number of participants experiencing at least one fall at seven‐month follow‐up for the randomised exercise group. We were not able to obtain data in a format suitable for inclusion in the meta‐analyses for fear of falling from Rendon 2012, which presented medians and ranges (not SDs) for the ABC and GDS scores at baseline and post intervention.
Excluded studies
We excluded a total of 134 studies (144 articles) for the following main reasons: they were not RCTs or quasi‐RCTs (n = 53); the majority of participants were not aged 65 years and over (n = 3), participants were in nursing or rehabilitation care (n = 4) or the study population was restricted to a specific condition (n = 4); they did not contain an exercise intervention (n = 3), they involved multi‐component interventions (n = 31) or it was plausible that the comparator group might have increased exercise (n = 24); or fear of falling was not measured (n = 12). More details are provided in the Characteristics of excluded studies table.
Ongoing studies
Two ongoing studies (published in three articles) met the review criteria (see Characteristics of ongoing studies). The first study is a multicentre cluster‐randomised controlled trial of two exercise intervention groups compared with a no intervention control group in community‐dwelling older people aged 65 years and older in the UK (Iliffe 2010b). Fear of falling will be measured by the Short FES‐I. The other ongoing study is a multicentre cluster‐randomised controlled trial of a 16‐week exercise programme with a focus on falls prevention compared with a no intervention control group in community‐dwelling older people in Germany (NCT01032252). Fear of falling will be measured with the German version of the FES‐I.
Studies awaiting classification
Seven studies are awaiting classification (see Characteristics of studies awaiting classification). It is plausible but unclear whether the comparator group treatment in these studies may have increased exercise and further details are required to enable a decision regarding their inclusion or exclusion. Four studies used awareness or education programmes that included advice about exercise (Arai 2007; Brouwer 2003; Morris 2008; Wolf 2003); one study provided social activities that included walking (Kim 2009b); one study invited all participants (including the control group) to practice exercise techniques before randomisation (Henwood 2008), and one study provided the control group with ethylene vinyl acetate copolymer shoe insoles and explicitly stated that these would improve postural balance (Jorgensen 2013).
Risk of bias in included studies
We assessed studies for risk of bias and the findings are reported in the tables of Characteristics of included studies. See Figure 2 for the 'Risk of bias' summary and Figure 3 for the 'Risk of bias' graph.
2.
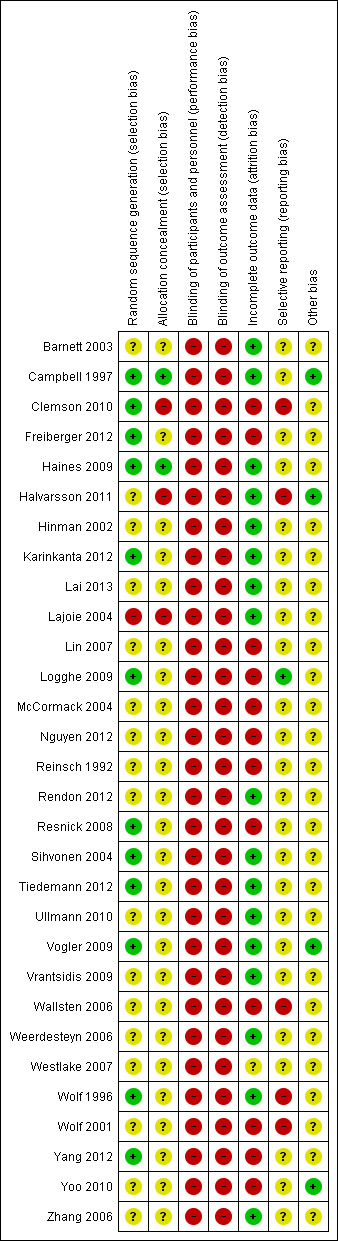
'Risk of bias' summary: authors' judgements about each risk of bias item for each included study
3.
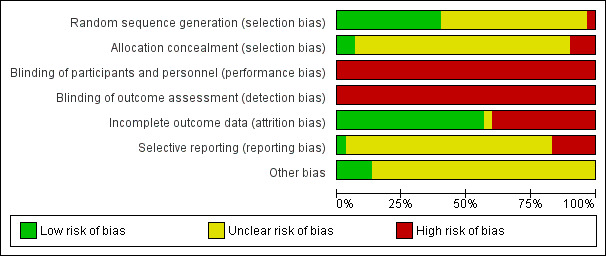
'Risk of bias' graph: authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
Apart from the one quasi‐randomised trial, all other studies reported that they allocated participants to the intervention and control groups randomly. We judged the risk of bias in random sequence generation to be 'low' if a random component in the sequence generation process was used (e.g. random number table, computer random number generator, coin tossing, shuffling cards or envelopes, throwing dice) and 'high' if a systematic non‐random component was used in the sequence generation process (e.g. allocation by odd or even date of birth, by some algorithm based on date (or day) of admission, by alternation). We judged the risk of bias in random sequence generation to be low in 40% (12/30) of studies (Campbell 1997; Clemson 2010; Freiberger 2012; Haines 2009; Karinkanta 2012; Logghe 2009; Resnick 2008; Sihvonen 2004; Tiedemann 2012; Vogler 2009; Wolf 1996; Yang 2012), high in 3% (1/30) of studies (Lajoie 2004), and unclear in the remaining 57% (17/30) of studies (Barnett 2003; Halvarsson 2011; Hinman 2002; Lai 2013; Lin 2007; McCormack 2004; Nguyen 2012; Reinsch 1992; Rendon 2012; Ullmann 2010; Vrantsidis 2009; Wallsten 2006; Weerdesteyn 2006; Westlake 2007; Wolf 2001; Yoo 2010; Zhang 2006).
We judged the risk of bias in allocation concealment to be low if participants and investigators enrolling participants could not foresee assignment (e.g. sequentially numbered, opaque, sealed envelopes) and high if participants or investigators enrolling participants could possibly foresee assignments (e.g. use of an open random allocation schedule). We judged the risk of bias in allocation concealment to be low in 7% (2/30) of studies (Campbell 1997; Haines 2009), high in 10% (3/30) of studies (Clemson 2010; Halvarsson 2011; Lajoie 2004), and unclear in 83% (25/30) of included studies (Barnett 2003; Freiberger 2012; Hinman 2002; Karinkanta 2012; Lai 2013; Lin 2007; Logghe 2009; McCormack 2004; Nguyen 2012; Reinsch 1992; Rendon 2012; Resnick 2008; Sihvonen 2004; Tiedemann 2012; Ullmann 2010; Vogler 2009; Vrantsidis 2009; Wallsten 2006; Weerdesteyn 2006; Westlake 2007; Wolf 1996; Wolf 2001; Yang 2012; Yoo 2010; Zhang 2006). We judged only two studies to be at low risk of bias for both random sequence generation and allocation concealment (Campbell 1997; Haines 2009). We judged the single quasi‐randomised controlled trial to be at high risk of bias for both random sequence generation and allocation concealment (Lajoie 2004).
Blinding
Participants were not blinded to the treatment group allocation (as the intervention was exercise), hence we judged all studies as being at high risk of performance bias. Outcome measurements were self reported so participants completed these knowing their allocation and we therefore judged all studies to be at high risk of detection bias.
Incomplete outcome data
We judged the risk of attrition bias to be low in 57% (17/30) of studies (Barnett 2003; Campbell 1997; Haines 2009; Halvarsson 2011; Hinman 2002; Karinkanta 2012; Lai 2013; Lajoie 2004; Rendon 2012; Sihvonen 2004; Tiedemann 2012; Ullmann 2010; Vogler 2009; Vrantsidis 2009; Weerdesteyn 2006; Wolf 1996; Zhang 2006), with outcome data in these studies reported for 80% or more of the original sample in each arm of the trial. We judged the risk of attrition bias to be high in 40% (12/30) of studies (Clemson 2010; Freiberger 2012; Lin 2007; Logghe 2009; McCormack 2004; Nguyen 2012; Reinsch 1992; Resnick 2008; Wallsten 2006; Wolf 2001; Yang 2012; Yoo 2010), and unclear in 3% (1/30) of included studies (Westlake 2007).
Selective reporting
We judged the majority of studies (80%; 24/30) to be at unclear risk of reporting bias because it was not possible to tell from the article if all prespecified outcomes had been reported. We judged 17% (5/30) of studies to be at high risk because data were not reported on all prespecified outcomes (Clemson 2010; Halvarsson 2011; Wallsten 2006; Wolf 1996; Wolf 2001), and we judged the remaining 3% (1/30) to be at low risk because the protocol was available and data were reported for all prespecified outcomes (Logghe 2009).
Other potential sources of bias
We judged the risk of other bias to be low in 13% (4/30) of studies (Campbell 1997; Halvarsson 2011; Vogler 2009; Yoo 2010), where the study appeared to be free any other source of bias, and unclear in the remaining 87% (26/30) of included studies.
Effects of interventions
See: Table 1
Exercise versus control (no intervention or alternative non‐exercise intervention)
Primary outcome: fear of falling
Effect of exercise interventions immediately post intervention
We pooled data from 24 studies in a meta‐analysis for fear of falling. The means and standard deviations (SDs) for each study are shown in Table 2. Combining effect sizes for all fear of falling scales (Falls Efficacy Scale (FES) (all versions), Activities‐specific Balance Confidence (ABC) scale, plus other numerical scales) showed that exercise interventions were associated with a small to moderate and statistically significant reduction in fear of falling (standardised mean difference (SMD) 0.37, 95% confidence interval (CI) 0.18 to 0.56; 24 studies, 1692 participants; Analysis 1.1; Figure 4). There was significant heterogeneity between effect sizes (Chi² = 75.01, df = 23, P value < 0.00001, I² = 69%). Pooled effect sizes did not differ significantly between the different scales used to measure fear of falling (test for subgroup differences: Chi² = 5.21, df = 3, P value = 0.16).
1.1. Analysis.
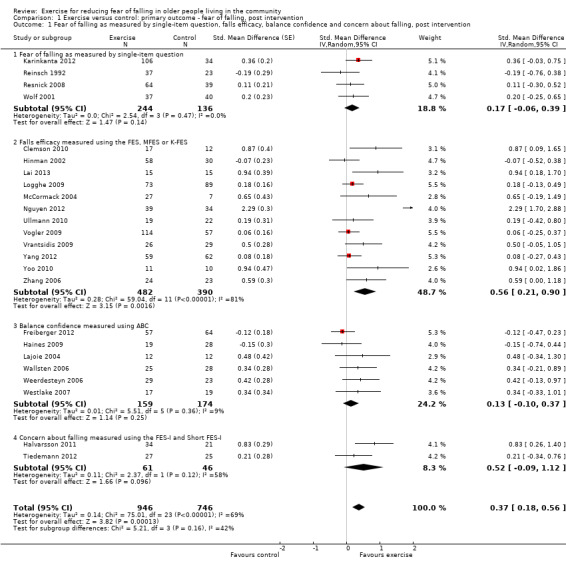
Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 1 Fear of falling as measured by single‐item question, falls efficacy, balance confidence and concern about falling, post intervention.
4.
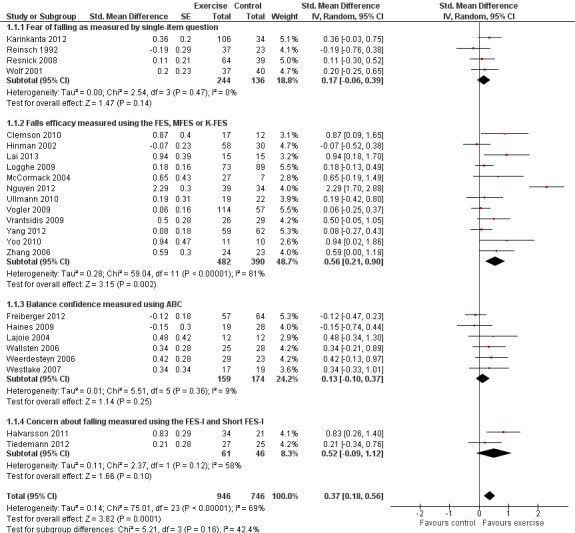
Forest plot: Exercise versus control: primary outcome ‐ fear of falling, post intervention
Two studies measured fear of falling using both the FES and ABC (Clemson 2010; Ullmann 2010). We used FES scores in the main analysis and undertook a sensitivity analysis replacing FES scores with ABC scores for these two studies, with similar findings (SMD 0.34, 95% CI 0.15 to 0.53; 24 studies, 1692 participants; analysis not shown).
Two studies were cluster‐RCTs (Reinsch 1992; Resnick 2008), for which the standard error of the SMD was inflated as described above using an intracluster correlation coefficient (ICC) (ICC 0.02, 95% CI 0.00 to 0.05) calculated from a cluster‐RCT investigating community‐based exercise interventions in older people with randomisation by General Practitioner practice (average cluster size 25) (Iliffe 2010b). A sensitivity analysis showed that using the lower or upper 95% CI for the ICC did not change the results compared with using an ICC of 0.02: the same result (SMD 0.37, 95% CI 0.18 to 0.56) applied with either an ICC of 0 or analysis with an ICC of 0.05.
One study, Nguyen 2012 (73 participants), had a much larger effect size than other studies in the meta‐analysis. We undertook a sensitivity analysis excluding this outlier study. Without Nguyen 2012, exercise interventions were still associated with a small to moderate, and statistically significant, improvement in fear of falling immediately post intervention (SMD 0.24, 95% CI 0.12 to 0.36; 23 studies, 1619 participants). There was no significant heterogeneity between effect sizes after removing Nguyen 2012 from the meta‐analysis (Chi² = 28.67, df = 22, P value = 0.15; I² = 23%).
Six studies with a total of 666 participants were not included in the meta‐analysis. One study was not included because it did not report fear of falling immediately post intervention (Lin 2007; results for 85 participants). Two studies used single‐question measures with binary or ordinal responses for measuring fear of falling (Barnett 2003; Sihvonen 2004). Barnett 2003 (results for 137 participants) reported that the percentage of participants reporting fear of falling did not differ significantly between treatment groups (intervention group = 7.5%, control group = 8.6%, P value not reported). However, Sihvonen 2004 (results for 27 participants), found a significant reduction from baseline in the intervention group (10% reporting high fear of falling post intervention versus 25% at baseline, P value = 0.02) but no difference in the control arm (14% at both baseline and post intervention, P value not reported). Wolf 1996 (results for 165 participants) was not included in the meta‐analysis because FES scores were reported grouped into four categories (from 'not at all afraid' to 'very afraid'). This three‐arm study found a significant difference in change from baseline between the three groups in an analysis that included data at both post intervention and four months post intervention. In the Tai Chi group, the percentage not at all afraid of falling increased from 43% at baseline to 53% post intervention and reduced to 47% at four‐month follow‐up; in the balance training group, the percentages at baseline, post intervention and four‐month follow‐up were 29%, 27% and 33%; and in the control group, these were 44%, 35% and 41%, respectively (reported P value = 0.046). Campbell 1997 (results for 212 participants) was not included in the meta‐analysis as standard deviations (SDs) for the FES were reported only for change from baseline scores. This study reported a significant increase in fear of falling post intervention for the control group compared with the intervention group (difference in mean change from baseline 3.6, 95% CI 0.4 to 6.8, P value not reported). Rendon 2012 (results for 40 participants) was not included in the meta‐analysis as only medians and ranges were reported for the ABC. The study reported significantly improved balance confidence in the intervention group compared with the control group (post intervention median (range) intervention group = 78.8 (55.0 to 96.9), control group = 76.9 (45.0 to 100.0), reported P value = 0.04).
Effect of exercise interventions on fear of falling up to and beyond six months post intervention
Seven of the studies that reported fear of falling at follow‐up times beyond post intervention provided data that could be included in a meta‐analysis. Exercise interventions were associated with a small but statistically non‐significant reduction in fear of falling at short‐term follow‐up (less than six months post end of the intervention period) (SMD 0.17, 95% CI ‐0.05 to 0.38; P value = 0.12; four studies; 356 participants; Analysis 1.2). Two studies could not be included in the meta‐analysis. Westlake 2007 reported data at two‐month follow‐up only for the intervention group. The data from Wolf 1996 at four‐month follow‐up is reported under the post intervention results above as the analyses combines both time points. At long‐term follow‐up (six or more months post end of the intervention period), exercise interventions were associated with a small reduction in fear of falling of borderline statistical significance (SMD 0.20, 95% CI ‐0.01 to 0.41; P value = 0.06, three studies; 386 participants; Analysis 1.3). There was no significant heterogeneity between effect sizes at short‐term follow‐up (Chi² = 2.86, df = 3, P value = 0.41; I² = 0%) or long‐term follow‐up (Chi² = 0.78, df = 2, P value = 0.68; I² = 0%).
1.2. Analysis.
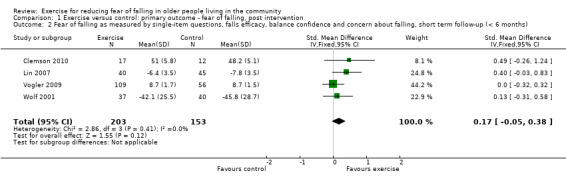
Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 2 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, short term follow‐up (< 6 months).
1.3. Analysis.
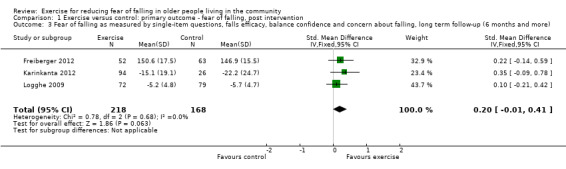
Comparison 1 Exercise versus control: primary outcome ‐ fear of falling, post intervention, Outcome 3 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, long term follow‐up (6 months and more).
Sensitivity analyses: effect of exercise interventions immediately post intervention
We did not undertake a sensitivity analysis restricting to studies at low risk of bias from allocation concealment as this applied to only one study that was included in the meta‐analysis (Haines 2009). We were also unable to undertake sensitivity analyses restricting to studies at low risk of detection bias as we judged no studies to be at low risk. Restricting analyses to the 12 studies (802 participants) judged to be at low risk of attrition bias produced similar results (SMD 0.31, 95% CI 0.13 to 0.49; 12 studies, 802 participants; analysis not shown) to the analysis including all studies (SMD 0.37, 95% CI 0.18 to 0.56; 24 studies, 1692 participants; Analysis 1.1).
Subgroup analyses: effect of exercise interventions immediately post intervention
We performed seven subgroup analyses. We also examined the effect of removing the extreme outlier trial, Nguyen 2012, and illustrate below instances where its removal demonstrated the lack of robustness of findings of potential subgroup differences.
The available evidence did not show that the effect of exercise interventions on fear of falling varied by type of exercise intervention (3D (Tai Chi); gait, balance, co‐ordination, functional task exercises; strength and resistance exercises); test for subgroup differences: Chi² = 3.46, df = 2, P value = 0.18; Analysis 2.1). Two studies were excluded from this subgroup analysis as we used combined data from more than one intervention group in our analysis and the intervention groups provided different types of exercise (Karinkanta 2012; McCormack 2004).
2.1. Analysis.
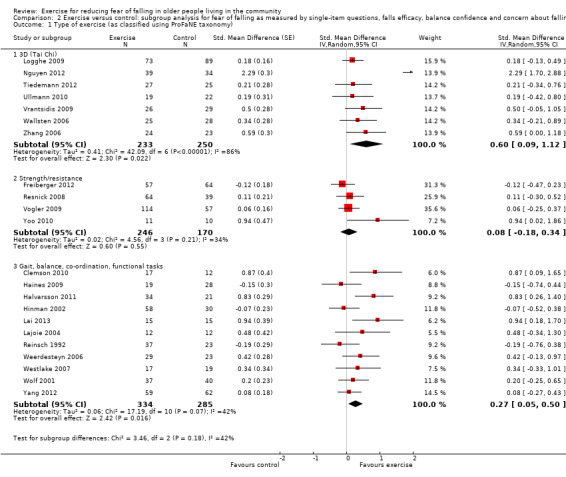
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 1 Type of exercise (as classified using ProFaNE taxonomy).
The effect of exercise interventions on fear of falling may be smaller in studies where the control group received an alternative intervention (e.g. education, social visits, craft activities, discussion groups; SMD 0.11, 95% CI ‐0.08 to 0.29; six studies, 499 participants) compared with those where the control group received no intervention (SMD 0.48, 95% CI 0.22 to 0.73; 18 studies, 1199 participants) as shown by the test for subgroup differences: Chi² = 5.45, df = 1, P value = 0.02; Analysis 2.2). Although plausible, these subgroup results should be interpreted with caution as the 95% CI for the subgroup effect sizes overlap and removal of Nguyen 2012 markedly reduces the difference: Chi² = 2.83, df = 1, P value = 0.09 (analysis not shown).
2.2. Analysis.
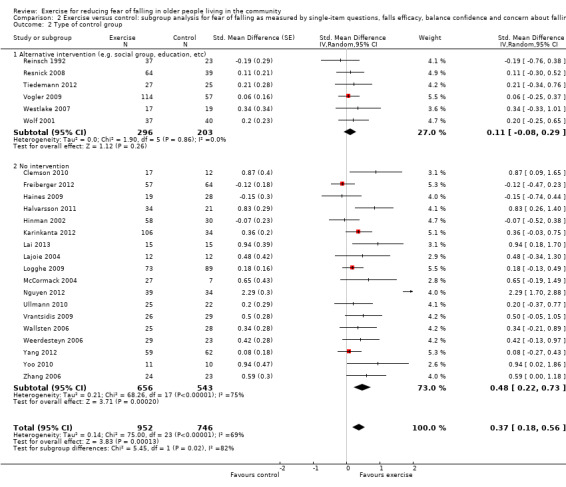
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 2 Type of control group.
The available evidence did not show that the effect of exercise interventions on fear of falling differed between studies that did not recruit participants on the basis of increased falls risk (14 studies, 926 participants) and those which did recruit participants at increased risk of falls (10 studies, 772 participants); test for subgroup differences: Chi² = 1.18, df = 1, P value = 0.28; Analysis 2.3).
2.3. Analysis.
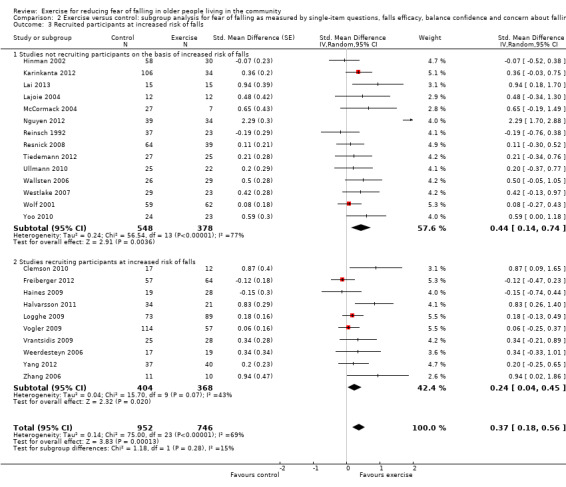
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 3 Recruited participants at increased risk of falls.
The effect of exercise interventions on fear of falling may be greater where exercise interventions are delivered in groups (SMD 0.49, 95% CI 0.22 to 0.76; 15 studies, 1051 participants) than those delivered to individuals (SMD 0.14, 95% CI ‐0.06, 0.35; nine studies, 647 participants); test for subgroup differences: Chi² = 3.99, df = 1, P value = 0.05; Analysis 2.4). However, these subgroup results should be interpreted with caution as the 95% CI for the subgroup effect sizes overlap, the effect is marginal and removal of Nguyen 2012 markedly reduces the difference: Chi² = 1.46, df = 1, P value = 0.23 (analysis not shown).
2.4. Analysis.
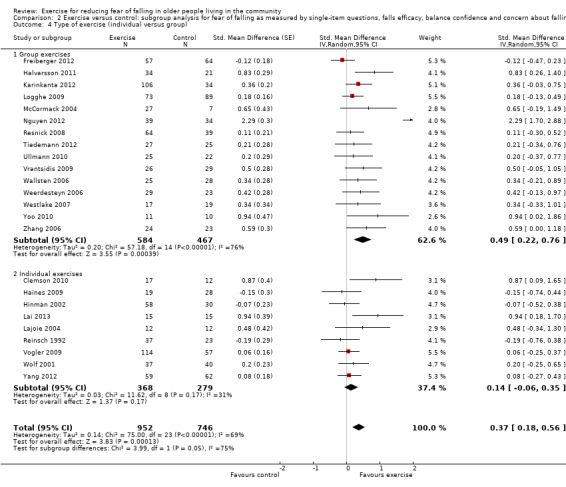
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 4 Type of exercise (individual versus group).
The available evidence did not show that the effect of exercise interventions on fear of falling varied according to exercise frequency (one to three times per week; four or more times per week); test for subgroup differences: Chi² = 0.20, df = 1, P value = 0.66; Analysis 2.5). The same lack of difference between subgroups was observed when subgrouping by duration of interventions (up to 12 weeks; 13 to 26 weeks; more than 26 weeks); test for subgroup differences: Chi² = 0.88, df = 2, P value = 0.64; Analysis 2.6; and when subgrouping by primary aim of study (to reduce fear of falling; other primary aim); test for subgroup differences: Chi² = 0.17, df = 2, P value = 0.68; Analysis 2.7.
2.5. Analysis.
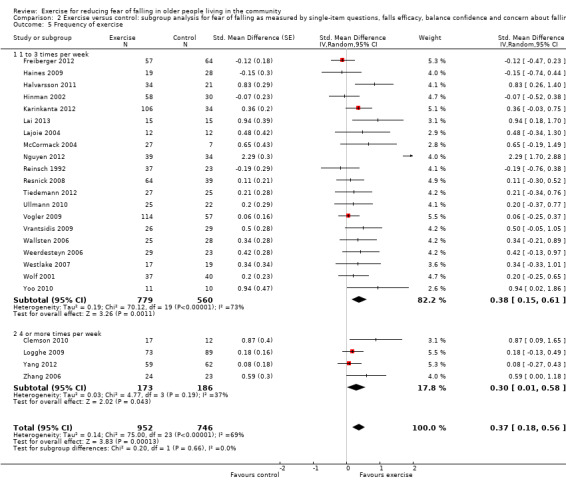
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 5 Frequency of exercise.
2.6. Analysis.
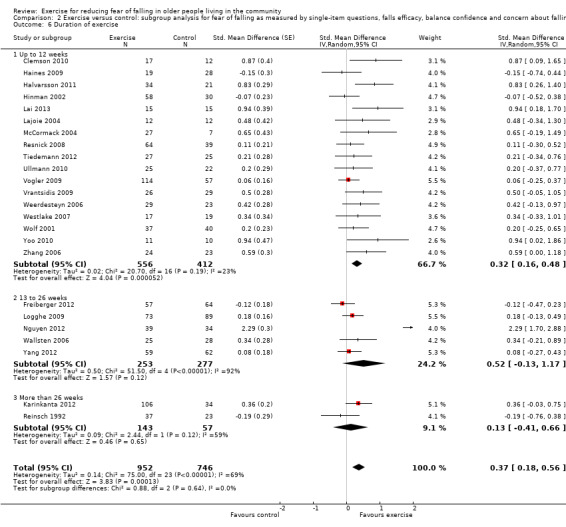
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 6 Duration of exercise.
2.7. Analysis.
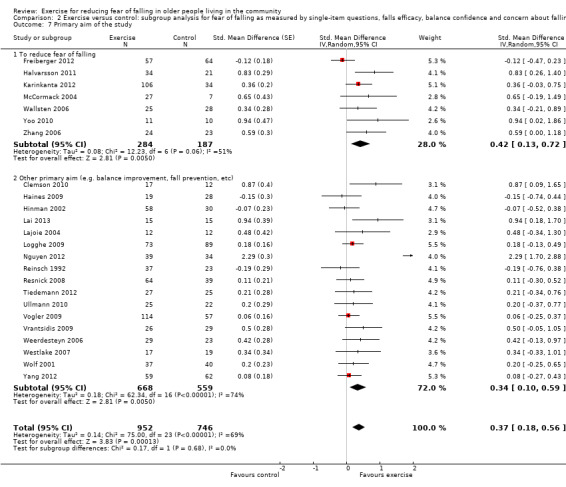
Comparison 2 Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention, Outcome 7 Primary aim of the study.
Publication bias: effect of exercise interventions immediately post intervention
The funnel plot for fear of falling post intervention and the Egger's test (bias coefficient 2.98, 95% CI 0.68 to 5.28; P value = 0.01) indicates funnel plot asymmetry suggesting publication bias due to small studies with negative findings that we failed to identify in our review (see Figure 5). Also of note is that the most extreme data point on the right is that of Nguyen 2012.
5.
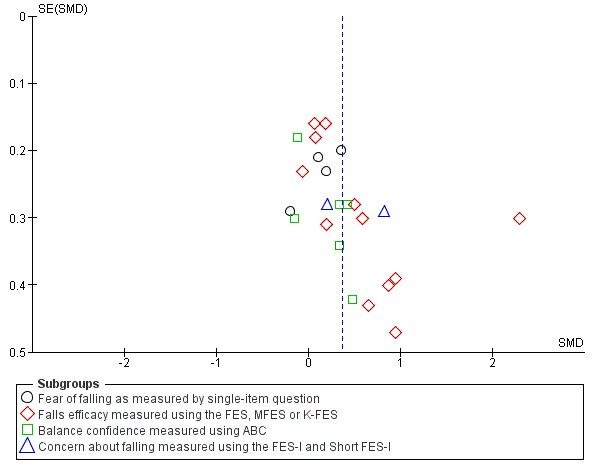
Exercise versus control: primary outcome ‐ fear of falling, post intervention (see Figure 4 for forest plot)
Secondary outcomes
For all outcomes described below (occurrence of falls, activity avoidance or restriction, depression, anxiety, exercise compliance or adherence and physical activity) it is important to remember that our included studies do not represent the totality of the evidence of the effect of exercise interventions on these outcomes, as our review only includes studies that measured fear of falling as an outcome. These outcomes have been included in our review because they may help explain why exercise interventions were or were not effective in reducing fear of falling.
Occurrence of falls
Occurrence of at least one fall was reported in nine studies (Barnett 2003; Campbell 1997; Clemson 2010; Haines 2009; Logghe 2009; Sihvonen 2004; Vogler 2009; Weerdesteyn 2006; Yang 2012). Exercise interventions were associated with a significant reduction in the proportion of participants having at least one fall (risk ratio (RR) 0.85, 95% CI 0.74 to 0.98; nine studies; 1113 participants; Analysis 3.1). There was no significant heterogeneity between effect sizes (Chi² = 2.50, df = 8, P value = 0.96; I² = 0%). The follow‐up periods in these studies varied from immediately post intervention to 11 months post intervention. Reinsch 1992 (107 participants at baseline) was not included in the meta‐analysis because the number of participants for whom falls data were available at follow‐up was not reported. This study reported the results of a survival analysis of time to first fall, stating only that there was no significant difference between study groups (P value = 0.53).
3.1. Analysis.
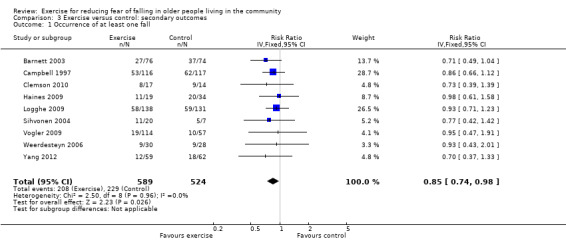
Comparison 3 Exercise versus control: secondary outcomes, Outcome 1 Occurrence of at least one fall.
Nine studies reporting data on falls rates were included in the meta‐analysis (Barnett 2003; Campbell 1997; Clemson 2010; Freiberger 2012; Haines 2009; Logghe 2009; Sihvonen 2004; Weerdesteyn 2006; Wolf 1996). Exercise interventions were associated with a significantly lower falls rate (IRR 0.68, 95% CI 0.53 to 0.87; nine studies; 1121 participants; Analysis 3.2), but there was significant heterogeneity between effect sizes (Chi² = 18.72, df = 8, P value = 0.02; I² = 57%). The follow‐up periods in these studies varied from immediately post intervention to 20 months post intervention. One study (Lin 2007; 85 participants) was not included in the meta‐analysis as it did not report rate ratios or data from which we could calculate falls rates. This study reported falls rates of 1.6/1000 person years in the intervention group and 1.1/1000 person years in the control group (home safety assessment and modification group). No further figures or P values are reported.
3.2. Analysis.
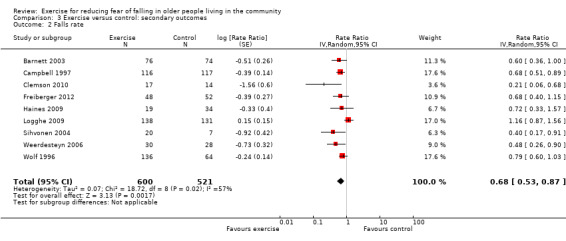
Comparison 3 Exercise versus control: secondary outcomes, Outcome 2 Falls rate.
Activity avoidance or restriction
No information was provided on activity avoidance or restriction using the modified Survey of Activities and Fear of Falling in the Elderly (SAFFE) or single questions asking about activity avoidance in any of the studies.
Depression
Depressive symptoms were measured in seven studies, using the Geriatric Depression Scale (GDS) (Rendon 2012; Vogler 2009), GDS‐5 (Resnick 2008), GDS‐15 (Lin 2007), GDS‐20 (Halvarsson 2011), the depression subscale of the Hospital Anxiety and Depression Scale (HADS) (Wolf 2001), and the Center for Epidemiologic Studies ‐ Depression (CES‐D) scale (Wolf 1996). Notably, five of these studies had 'active' control interventions. This was education on nutrition in Resnick 2008; education on a range of topics including medicines, sleep, cognitive impairment and bereavement in Wolf 1996; social home visits in Vogler 2009; individualised crafts/games in Wolf 2001; and home safety assessment in Lin 2007.
Four studies reported depression scores immediately post intervention (Halvarsson 2011; Resnick 2008; Vogler 2009; Wolf 2001), as shown in Table 3. Exercise interventions did not appear to reduce depression scores (SMD ‐0.08, 95% CI ‐0.28 to 0.13; four studies; 406 participants; Analysis 3.3) and there was no significant heterogeneity between effect sizes (Chi² = 5.19, df = 3, P value = 0.16; I² = 42%).
3.3. Analysis.
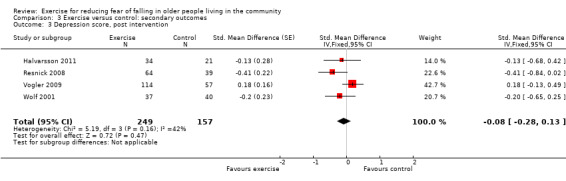
Comparison 3 Exercise versus control: secondary outcomes, Outcome 3 Depression score, post intervention.
One study was a cluster‐RCT (Resnick 2008); the standard error was inflated to account for clustering as described above using the ICC of 0.03 from a cluster‐RCT investigating exercise for depression in older care home residents with the GD‐15 (Underwood 2013). This trial reported two ICCs, both without 95% CI (an ICC of 0.00 at 12 months and an ICC of 0.03 at six months in participants who were depressed at baseline). We used the ICC of 0.03 in the analysis and undertook a sensitivity analysis using an ICC of zero. Findings were very similar using ICCs of 0.03 (SMD ‐0.08, 95% CI ‐0.28 to 0.13; four studies; 186 participants) and zero (SMD ‐0.09, 95% CI ‐0.29 to 0.11; four studies; 186 participants); analyses not shown.
Rendon 2012 could not be included in the meta‐analysis because the published data were reported as medians and ranges. This study reported no significant difference post intervention between the GDS scores of the exercise and control groups (GDS median (range) in the exercise group was 4.0 (0.0 to 13.0) and in the control group 5.0 (1.0 to 14.0); 40 participants, P value = 0.09).
Three studies (Lin 2007; Vogler 2009; Wolf 2001), all with 'active' control groups, reported results at short‐term follow‐up (less than six months post intervention). Exercise interventions did not appear to reduce depression scores; these results favoured the no exercise, 'active' control, group (SMD 0.20, 95% CI ‐0.02 to 0.43; three studies; 327 participants; Analysis 3.4). There was no significant heterogeneity between effect sizes (Chi² = 2.55, df = 2, P value = 0.28; I² = 22%).
3.4. Analysis.
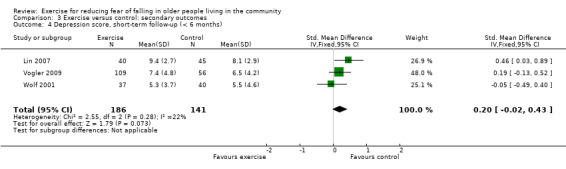
Comparison 3 Exercise versus control: secondary outcomes, Outcome 4 Depression score, short‐term follow‐up (< 6 months).
One study was not included in the meta‐analyses immediately post intervention or at short‐term follow‐up (Wolf 1996). This study (185 participants) measured depression using the CES‐D scale and reported no significant difference between treatment groups (CES‐D scores and P values not reported).
Anxiety
Anxiety was reported by the subscale of the HADS by Wolf 2001 and no significant differences were observed between mean scores in the intervention group and control group immediately post intervention (mean (SD): intervention group:4.3 (3.9); control group 4.3 (3.4), 77 participants, P value > 0.05).
Compliance with or adherence to exercise interventions
Twenty‐one studies reported adherence rates. The definitions of adherence, which varied between studies, are given in the table of Characteristics of included studies. Seventeen studies reported adherence rates over 50% (Barnett 2003; Freiberger 2012; Hinman 2002; Karinkanta 2012; McCormack 2004; Reinsch 1992; Rendon 2012; Resnick 2008; Sihvonen 2004; Tiedemann 2012; Ullmann 2010; Vogler 2009; Vrantsidis 2009; Weerdesteyn 2006; Westlake 2007; Wolf 1996; Zhang 2006). Six studies reported adherence rates of 90% or higher (Barnett 2003; Hinman 2002; Sihvonen 2004; Ullmann 2010; Wolf 1996; Zhang 2006). Hinman 2002 partly attributed this high adherence to participants being offered a cash incentive for taking part in the trial. Of those studies reporting adherence rates above 50%, 41% (7/17) were classified as gait, balance, co‐ordination or functional task exercises, 18% (3/17) as strength and resistance exercises, 24% as 3D exercises (4/17) and 18% (3/17) had more than one intervention group each with a different type of exercise. This suggests higher adherence rates were not confined to studies evaluating particular types of exercise. Four studies reported adherence rates less than 50% (Campbell 1997; Haines 2009; Logghe 2009; Yang 2012). Nine studies did not report adherence rates (Clemson 2010; Halvarsson 2011; Lai 2013; Lajoie 2004; Lin 2007; Nguyen 2012; Wallsten 2006; Wolf 2001; Yoo 2010).
As physical activity can be regarded as a measure of compliance or adherence to exercise interventions, we also report on this. Eight studies measured physical activity in participants using a variety of scales (Barnett 2003; Campbell 1997; Logghe 2009; Resnick 2008; Sihvonen 2004; Westlake 2007; Yang 2012; Yoo 2010). The Physical Activity Scale for the Elderly (PASE) (Washburn 1993) was used in four studies (Barnett 2003; Campbell 1997; Logghe 2009; Westlake 2007), the Yale Physical Activity Survey (YPAS) in two studies (Resnick 2008; Yoo 2010), and a four‐category graded physical activity scale (only activities of daily living, less than three hours per week, three to four hours per week, more than four hours per week) (Sihvonen 2004) and Human Activity Profile ‐ Adjusted Activity Score (HAP‐AAS) (Yang 2012) were used in the remaining two studies.
Meta‐analysis of four studies using the PASE score (Barnett 2003; Campbell 1997; Logghe 2009; Westlake 2007) showed exercise interventions did not appear to increase physical activity (MD 3.44, 95% CI ‐1.65 to 8.54; four studies; 547 participants; Analysis 3.5) and no significant heterogeneity between effect sizes (Chi² = 2.04, df = 3, P value = 0.57; I² = 0%). Barnett 2003 reported physical activity at six months into a 12‐month intervention. The remaining three studies reported physical activity immediately post intervention.
3.5. Analysis.
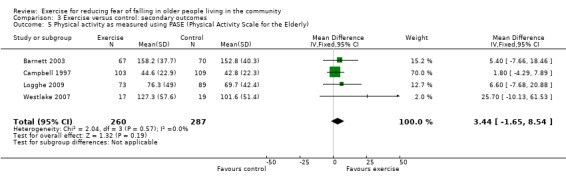
Comparison 3 Exercise versus control: secondary outcomes, Outcome 5 Physical activity as measured using PASE (Physical Activity Scale for the Elderly).
Three studies not included in the meta‐analysis reported physical activity significantly increased in the intervention group compared with the control group post intervention (Resnick 2008; Sihvonen 2004; Yang 2012). Resnick 2008 (103 participants) reported an intervention group mean of 281 (SD 320) minutes and a control group mean of 199 (SD 257) minutes per week spent in moderate intensity physical activity post intervention (P value = 0.04), Sihvonen 2004 (27 participants) reported a significant increase in physical activity from baseline in the intervention group but not in the control group (20% more than four hours per week to 45% in intervention group versus 0% doing more than four hours per week in control group at both time points, P value = 0.004). Yang 2012 (121 participants) reported a significantly higher HAP‐AAS score in the intervention group than the control group post intervention (difference between means comparing intervention to control group: 4.57, 95% CI 1.84 to 7.29, P value = 0.001). Yoo 2010 (21 participants) reported no significant difference in energy expenditure per week between the exercise and control groups (mean (SD) kcal/week 9806 (4062) versus 6068 (2216) respectively, P value only reported as non‐significant).
Cost
No information was provided on the cost of the interventions in any of the studies.
Discussion
Summary of main results
The 30 included studies, which included a total of 1692 participants, investigated a wide variety of interventions using different types of exercise, of varied intensity and duration, in a range of different settings. A summary of the evidence is shown in Table 1.
Low quality evidence suggests that exercise interventions are associated with a small to moderate reduction in fear of falling amongst community‐dwelling older adults immediately at the end of the intervention period (standardised mean difference (SMD) 0.37, 95% confidence interval (CI) 0.18, 0.56; 24 studies, 1692 participants). Pooled effect sizes did not differ significantly between the different scales used to measure fear of falling. Although none of the sensitivity analyses changed the direction of effect, the greatest reduction in the size of the effect was on removal of an extreme outlier study with 73 participants (SMD 0.24, 95% CI 0.12 to 0.36; 23 studies, 1619 participants).
Subgroup analyses did not provide evidence that the effect of exercise interventions on fear of falling differed by type of exercise intervention, the frequency of exercise or the duration of the exercise intervention. Similarly, subgroup analyses did not provide evidence that the effect of exercise interventions on fear of falling differed between studies which did and did not recruit participants on the basis of increased falls risk, or between those where the primary aim was to reduce fear of falling and those with an alternative primary aim. It is possible that the small number of studies in some of the subgroups may have resulted in a lack of power to detect differential effects.
Subgroup analysis provided some weak evidence that the effect of exercise interventions on fear of falling was less, including no effect or a small increase, where the control group received an alternative intervention (e.g. education, social visits, craft activities, discussion groups) than where the control group received no intervention. There was also some weak evidence that the effect of exercise interventions on fear of falling is larger where the intervention involved group exercises rather than individual exercises. However, these subgroup results should be interpreted with caution as the 95% CIs for the subgroup effect sizes overlap and there was substantial reduction of the effect upon removal of the above‐mentioned outlier study.
There was very low quality evidence from four studies of exercise resulting in either little effect or a small reduction in fear of falling in the short term (less than six months from the end of the intervention) during follow‐up. A similar conclusion resulted from long‐term data provided by three studies.
Very low quality evidence suggests exercise interventions in these studies that also reported on fear of falling reduced the risk of falling measured either as participants incurring at least one fall during follow‐up or number of falls during follow‐up. These provide reassurance that reduced fear of falling was not associated with an increased risk of falling. Very low quality evidence from four studies indicated that exercise interventions did not appear to reduce symptoms of depression or increase physical activity. Only one study reported effects of exercise interventions on anxiety, finding no difference between groups. No studies reported the effects of exercise interventions on activity avoidance or costs. It is important to remember that our included studies do not represent the totality of the evidence of the effect of exercise interventions on falls, depression, anxiety or physical activity as our review only includes studies that reported fear of falling.
Overall completeness and applicability of evidence
This is the largest review of the effect of exercise interventions on fear of falling in community‐dwelling older people. Where data were not presented in the required format or were missing, the review team attempted to obtain data from trial authors and, as a result, we were able to include unpublished data from seven studies (Clemson 2010; Halvarsson 2011; Lajoie 2004; Ullmann 2010; Vogler 2009; Wallsten 2006; Weerdesteyn 2006). We pooled data from 24 of the 30 included studies (1692 participants) for our primary outcome: fear of falling measured immediately post intervention. Very few studies reported on fear of falling subsequently. As stressed repeatedly, the evidence for our secondary outcomes, such as falls, does not represent the totality of the evidence of the effect of exercise interventions on these outcomes.
We found exercise interventions were associated with a small to moderate reduction in fear of falling. To our knowledge there are no definitions of minimal clinically important differences in fear of falling for the measures used in studies in our review. A minimal clinically important difference is the smallest change in an outcome measure that a patient would find important. Defining this for measures of fear of falling would be difficult. Items in the scales may require different weightings for different individuals and populations as fear, concern or worry about falling may vary in importance across the items included in the scales. For example, fear about falling whilst having a bath or shower or whilst walking around the neighbourhood may have very different impacts on the life of an older person. Consequently it is not possible to consider our findings in terms of a minimal clinically important difference.
Although all studies tested exercise in older people living in the community and reported on fear of falling, there was considerable variation in study characteristics. Where there were sufficient data available for discrete subgroups, none of our subgroup analyses provided robust evidence of differences in effect in terms of either the study primary aim (reduction of fear of falling or other aim), the study population (recruitment on the basis of increased falls risk or not), the characteristics of the study exercise intervention, the study control intervention (no treatment or alternative intervention), or the method of outcome measurement. The potential for differences of effect in different populations or from different exercise interventions cannot be ruled out but the currently available evidence is insufficient to provide these insights.
We were also unable to explore the effect of exercise adherence on fear of falling, either during the intervention period or beyond the end of the intervention period due to some studies not measuring adherence and the use of varying definitions by other studies. It is possible that participants in the trials included in our review may have been more physically active and more interested or motivated to participate in an exercise programme than the general population of older people. If this is the case, our findings may overestimate the effect of exercise interventions if they were implemented in a wider population of community‐dwelling older people. The majority of the studies in our review come from high‐income countries, so our findings may not be generalisable to low‐ and middle‐income countries.
The relationship between fear of falling and falls occurrence is important, because one potential unintended consequence of reducing fear of falling may be increased exposure to activities associated with a higher risk of falls. Our review therefore reported on falls outcomes as well as on fear of falling. While the studies included in our review are only a subset of studies examining the effect of exercise on preventing falls, the results of our analyses are consistent with those of reviews focusing on the prevention of falls (Gillespie 2012b; Sherrington 2008b).
Quality of the evidence
Due to the nature of the intervention and outcome measures, blinding of participants and outcome assessors was not possible and therefore we judged all studies to be at high risk of performance and detection biases. Most studies were not reported in sufficient detail to judge the risk of other biases, particularly in terms of selection bias and reporting bias. We judged 12 studies to be at high risk of attrition bias. However, a sensitivity analysis including only the 17 studies at low risk of attrition bias showed similar results for the primary analysis. We downgraded the quality of evidence for all outcomes by one level for study limitations reflecting the high risk of bias from lack of blinding.
The funnel plot and Egger's test for data from our primary outcome of fear of falling immediately post intervention indicated the potential that we had failed to identify and include some small studies with negative findings. This suggests that the findings of our review may overestimate the effect of exercise interventions on reducing fear of falling. We thus downgraded the quality of evidence for fear of falling by a further level for publication bias. We downgraded fear of falling measured at short and long term follow‐up after the end of the intervention by one further level because of the small number of studies contributing these data.
We did not downgrade the quality of the evidence for fear of falling immediately post intervention for heterogeneity, including that relating to wide variety of exercise interventions tested in the included studies. As well as drawing on the findings of the subgroup analyses, this decision reflected that the significant heterogeneity between effect sizes in the meta‐analysis for our primary outcome measure was mainly due to one outlier study (Nguyen 2012). This evaluated group‐based Tai Chi classes lasting for one hour, twice weekly for six months in adults aged 60 to 79 years. There is no obvious explanation for the much larger effect on fear of falling favouring the intervention group than other studies included in our meta‐analysis.
We downgraded the quality of evidence for all secondary outcomes by two further levels for indirectness. This is because our review includes only a subset of studies reporting the effect of exercise interventions on these outcomes, as studies had to report fear of falling and these outcomes to be included in our review. Thus these results cannot be considered representative of the effects of the interventions under test.
In consequence, we judged the quality of the evidence for the outcome 'fear of falling immediately post intervention' to be 'low', and the quality of evidence for all other outcomes including fear of falling at short and long‐term follow‐ups to be 'very low'. Where the quality of evidence is 'low' this suggests further research is very likely to change the estimate of, and confidence in the estimate of, the effect of exercise on those outcomes. Where the quality of evidence is 'very low', there is considerable uncertainty about the effect of exercise on those outcomes.
Potential biases in the review process
Since many studies included in our review did not measure fear of falling as a primary outcome, it is likely that our searches failed to identify some studies that measured but did not report fear of falling. To reduce potential bias, we contacted authors of studies that met our criteria for study design, participants and interventions but did not report fear of falling as an outcome measure although they reported on fear of falling at baseline or mentioned it in their methods. We tried also to minimise reporting bias by contacting authors of included studies to obtain unpublished data and were successful in obtaining data for seven studies, enabling their inclusion in the meta‐analyses. We tried to minimise publication bias by searches of a range of databases, by examining reference lists of included studies and relevant reviews and by contacting authors and experts in the field of fear of falling and exercise. However, the funnel plot (Figure 5) and the Egger's test (P value = 0.01) indicate funnel plot asymmetry suggesting publication bias from the non‐availability of small studies with negative findings.
Upon reconsideration of our study selection judgements subsequent to editorial feedback on our review, we identified seven studies (695 participants) where it was unclear whether the treatment in the comparator group may have increased exercise. These are currently awaiting assessment as more details are required on the content of the comparator treatment to decide on inclusion of these studies and to consider the implications of the current decision not to include these studies in terms of introducing bias into the review.
As stipulated in our protocol, we performed sensitivity analyses to check on various decisions that we had made in presenting the data. These suggested that our findings for fear of falling were very similar when we used the Activities‐specific Balance Confidence (ABC) scores instead of the Falls Efficacy Scale (FES) scores for two studies that reported both scores and when we varied the intracluster correlation coefficient (ICC) used to adjust the results from cluster‐randomised controlled trials. Restricting analyses to studies at low risk of attrition bias also produced similar results to the analysis containing all studies.
Agreements and disagreements with other studies or reviews
Notably, the narrative and dated (search date January 2006) systematic review by Zijlstra 2007 provided separate conclusions for different types of exercise interventions. Zijlstra 2007 concluded that community‐based Tai Chi and home‐based exercise interventions reduced fear of falling in community‐dwelling older people, but that community‐based group exercise and computerised balance training did not. While we categorised our interventions in various ways (Table 4), our primary analysis included all exercise interventions. Our subgroup analyses did not provide evidence that different types of exercise interventions differed in their effect on fear of falling.
Our review included only a limited subset of the studies included in other reviews evaluating the effect of exercise interventions on the risk and rate of falls. In consequence, our review does not comprise the totality of evidence in this area. However, our findings on exercise interventions are consistent with those of the Cochrane review on preventing falls in older people living in the community (Gillespie 2012b). This found group and home‐based exercise programmes containing strength and balance training exercises, including Tai Chi, are effective in preventing falls. A review by Bula 2011b, examining interventions aimed at improving balance confidence in older adults, found the majority of effective interventions included some component of exercise, with no superiority of one type of exercise. Whilst our review did not find evidence of a significant effect of exercise interventions on symptoms of depression, a review by Bridle 2012 found exercise to reduce the severity of symptoms in older people suffering from depression. A Cochrane review including 35 trials (1356 participants) also found exercise had a significant effect, of moderate size, in improving symptoms of depression (Cooney 2013). As well as only a small number of studies included in our review reporting measures of depression, the populations included in studies in the reviews by Bridle 2012 and Cooney 2013 comprised people with pre‐existing depression, whereas none of the studies reporting depression as an outcome in our review specifically recruited people with depression.
Authors' conclusions
Implications for practice.
Exercise interventions in community‐dwelling older people probably reduce fear of falling to a limited extent immediately after the intervention, without increasing the risk or frequency of falls. There is insufficient evidence from the included studies to determine whether exercise interventions reduce fear of falling beyond the end of the intervention or their effect on other outcomes.
Implications for research.
Further well‐designed randomised trials are required to assess the effect of exercise interventions on fear of falling amongst community‐dwelling older people. However, priority should be given to establishing a core set of outcomes that includes fear of falling, and other related outcomes, for all trials examining the effects of exercise interventions in older people living in the community. The variety of the tools used to measure fear of falling is likely to continue to be a problem, but a pragmatic approach is that all trials should be explicit about the tools they use to measure fear of falling and the constructs measured by the tools. Consideration is needed regarding the time of outcome measurement; in particular, outcome should be measured at suitable time points beyond the end of the intervention period. Trials should also measure and clearly define exercise adherence. Discussion in the research community, with consumer and other stakeholder input, is required to identify priorities for future research and trials. This includes informing the decisions on the target population and the exercise interventions to be tested in trials whose primary aim is to reduce fear of falling.
What's new
| Date | Event | Description |
|---|---|---|
| 14 October 2015 | Amended | Correction to a subgroup analysis (Analysis 2.3) involving the removal of an incorrectly included study (Lin 2007). Minimal change to test for subgroup differences results. |
Acknowledgements
We would like to thank Caragh Flannery for her assistance to Heather Gage in screening of papers, extracting data from papers and undertaking quality assurance. We would like to thank Joanne Elliott for undertaking searches and Lindsey Elstub and Laura MacDonald for providing editorial support. We would also like to thank Catherine Sherrington, Jacqueline Close and Diane Horsley for their feedback. We especially acknowledge Helen Handoll for her substantial contribution to this review.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley Online Library)
#1 MeSH descriptor: [Aged] this term only (208) #2 ((old* or aged or elder* or geriatric* or senior*) near/5 (people or person* or adult*)):kw,ti,ab (171550) #3 #1 or #2 (171638) #4 MeSH descriptor: [Exercise] this term only (8610) #5 MeSH descriptor: [Exercise Therapy] this term only (4820) #6 MeSH descriptor: [Exercise Movement Techniques] this term only (87) #7 MeSH descriptor: [Physical Education and Training] this term only (1238) #8 MeSH descriptor: [Walking] explode all trees (2175) #9 MeSH descriptor: [Postural Balance] this term only (1141) #10 MeSH descriptor: [Resistance Training] this term only (782) #11 MeSH descriptor: [Tai Ji] this term only (178) #12 MeSH descriptor: [Breathing Exercises] this term only (477) #13 MeSH descriptor: [Dance Therapy] this term only (28) #14 (exercis* or training):kw,ti,ab (51483) #15 balance near/3 (reeducation or re‐education or retraining or re‐training):ti,ab,kw (14) #16 (aerobic near/1 exercis*):ti,ab,kw (1385) #17 #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 (52890) #18 MeSH descriptor: [Accidental Falls] this term only and with qualifiers: [Prevention & control ‐ PC] (610) #19 MeSH descriptor: [Fear] this term only (763) #20 (fright* or fear* or afraid):ti,ab,kw (2563) #21 #19 or #20 (2563) #22 #18 and #21 (70) #23 (fear* or fright* or afraid) near/5 fall*:ti,ab,kw (145) #24 "fear of falling":ti,ab,kw (121) #25 ("Falls Efficacy Scale" or "Mobility Efficacy Scale" or "Survey of Activities and Fear of Falling in the Elderly"):ti,ab,kw 31 #26 "University of Illinois at Chicago Fear of Falling Measure" or "SAFFE" or "UICFM":ti,ab,kw (Word variations have been searched)0 #27 "Activities Specific Balance Confidence Scale" or "Confidence in Maintaining Balance Scale" or "CON‐Fbal":ti,ab,kw (Word variations have been searched) (15) #28 #22 or #23 or #24 or #25 or #26 or #27 (177) #29 #3 and #17 and #28 (84)
MEDLINE (Ovid Online)
1 Aged/ (2296985) 2 ((old$ or aged or elder$ or geriatric$ or senior$) adj5 (people or adult$ or person$1)).tw. (122481) 3 1 or 2 (2336369) 4 Exercise/ (66495) 5 Exercise therapy/ (25373) 6 Exercise Movement Techniques/ (353) 7 "Physical Education and Training"/ (11702) 8 Walking/ (19465) 9 Postural Balance/ (14173) 10 Resistance Training/ (2878) 11 Tai Ji/ (579) 12 Breathing Exercises/ (2697) 13 Dance Therapy/ (206) 14 (exercis$ or training).tw. (377131) 15 (balance adj3 (retraining or re‐training or reeducation or re‐education)).tw. (41) 16 (aerobic adj exercise$).tw. (4523) 17 or/4‐16 (438843) 18 *Accidental Falls/pc [Prevention & Control] (3335) 19 *Fear/ (12030) 20 (fright$ or fear$ or afraid).tw. (49908) 21 19 or 20 (52676) 22 18 and 21 (189) 23 ((fear$ or fright$ or afraid) adj5 fall$).tw. (780) 24 "fear of falling".tw. (667) 25 ("Falls Efficacy Scale" or "Mobility Efficacy Scale" or "Survey of Activities and Fear of Falling in the Elderly" or "University of Illinois at Chicago Fear of Falling Measure" or "SAFFE" or "UICFFM" or "Activities Specific Balance Confidence Scale" or "Confidence in Maintaining Balance Scale" or "CON‐Fbal").tw. (267) 26 or/22‐25 (951) 27 3 and 17 and 26 (415) 28 Randomized controlled trial.pt. (379376) 29 Controlled clinical trial.pt. (88638) 30 randomized.ab. (276583) 31 placebo.ab. (149709) 32 Drug therapy.fs. (1726877) 33 randomly.ab. (193902) 34 trial.ab. (288497) 35 groups.ab. (1243213) 36 or/28‐35 (3217356) 37 exp Animals/ not Humans/ (4002688) 38 36 not 37 (2738483) 39 38 and 27 (186)
EMBASE (Ovid Online)
1 aged/ (2174749) 2 ((old$ or aged or elder$ or geriatric$ or senior$) adj5 (people or adult$ or person$1)).tw. (149531) 3 1 or 2 (2237738) 4 exercise/ (168031) 5 Kinesiotherapy/ (22205) 6 Physical Education/ (9724) 7 Walking/ (34132) 8 Body equilibrium/ (10805) 9 Resistance training/ (4218) 10 Tai Chi/ (1199) 11 Breathing exercise/ (4199) 12 Music therapy/ (3992) 13 (exercis$ or training).tw. (475514) 14 (balance adj3 (retraining or re‐training or reeducation or re‐education)).tw. (61) 15 (aerobic adj exercise$).tw. (6108) 16 or/4‐15 (584260) 17 Falling/pc [Prevention] (2860) 18 Fear/ (33833) 19 (fright$ or fear$ or afraid).tw. (63252) 20 18 or 19 (71927) 21 17 and 20 (118) 22 ((fear$ or fright$ or afraid) adj5 fall$).tw. (1050) 23 "fear of falling".tw. (891) 24 ("Falls Efficacy Scale" or "Mobility Efficacy Scale" or "Survey of Activities and Fear of Falling in the Elderly").tw. (226) 25 ("University of Illinois at Chicago Fear of Falling Measure" or "SAFFE" or "UICFFM").tw. (17) 26 ("Activities Specific Balance Confidence Scale" or "Confidence in Maintaining Balance Scale" or "CON‐Fbal").tw. (151) 27 21 or 22 or 23 or 24 or 25 or 26 (1278) 28 3 and 16 and 27 (454) 29 Randomized controlled trial/ (351774) 30 Clinical trial/ (886237) 31 Controlled clinical trial/ (402939) 32 Randomization/ (62859) 33 Single blind procedure/ (17953) 34 Double blind procedure/ (116581) 35 Crossover procedure/ (37887) 36 Placebo/ (222408) 37 Prospective study/ (244222) 38 ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. (709691) 39 (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. (173367) 40 ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. (156631) 41 (cross?over$ or (cross adj1 over$)).tw. (67196) 42 ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. (220755) 43 RCT.tw. (12160) 44 or/29‐43 (1841794) 45 Case Study/ or Abstract Report/ or Letter/ (899731) 46 44 not 45 (1804535) 47 28 and 46 (169)
CINAHL (EBSCO)
S1 MH Aged (422,300) S2 TX (old$ or aged or elder$ or geriatric$ or senior$) N5 (people or person$) (4,243) S3 S1 or S2 (424,084) S4 MH Exercise (26,588) S5 MH Therapeutic Exercise (12,810) S6 (MH "Physical Education and Training") (1,651) S7 MH Walking (11,671) S8 MH Balance, Postural (7,728) S9 MH Tai chi (1,095) S10 MH Breathing Exercises (1,242) S11 MH Dance Therapy (259) S12 TX (exercis$ or training) 112,307 S13 TX (balance N5 (retraining or re‐training or reeducation or re‐education)) (43) S14 TX "aerobic exercise$" 1,661 S15 S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 (163,166) S16 (MH "Accidental Falls/PC") (5,413) S17 MH Fear (6,436) S18 TX (fright$ or fear$ or afraid) (17,271) S19 S17 or S18 (17,271) S20 S16 and S19 (204) S21 TX “fear of falling” 537 S22 TX ("Falls Efficacy Scale" or "Mobility Efficacy Scale" or "Survey of Activities and Fear of Falling in the Elderly") 344 S23 TX ("University of Illinois at Chicago Fear of Falling Measure" or "SAFFE" or "UICFFM") (19) S24 TX ("Activities Specific Balance Confidence Scale" or "Confidence in Maintaining Balance Scale" or "CON‐Fbal") 183 S25 S20 or S21 or S22 or S23 or S24 (930) S26 S3 and S15 and S25 (410) S27 (MH "Clinical Trials+") (164,114) S28 (MH "Evaluation Research+") (19,640) S29 (MH "Comparative Studies") (72,606) S30 (MH "Crossover Design") (10,719) S31 PT Clinical Trial (74,252) S32 (MH "Random Assignment") (35,304) S33 S27 or S28 or S29 or S30 or S31 or S32 (260,433) S34 TX ((clinical or controlled or comparative or placebo or prospective or randomi?ed) and (trial or study)) (451,035) S35 TX (random* and (allocat* or allot* or assign* or basis* or divid* or order*)) (62,517) S36 TX ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) (685,831) S37 TX ( crossover* or 'cross over' ) or TX cross n1 over (13,447) S38 TX ((allocat* or allot* or assign* or divid*) and (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)) (78,624) S39 S34 or S35 or S36 or S37 or S38 (1,051,116) S40 S33 or S39 (1,114,460) S41 S26 and S40 (290)
PsycINFO (Ovid Online)
1 "fear of falling".mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (377) 2 ("Falls Efficacy Scale" or "Mobility Efficacy Scale" or "Survey of Activities and Fear of Falling in the Elderly" or "University of Illinois at Chicago Fear of Falling Measure" or "SAFFE" or "UICFFM" or "Activities Specific Balance Confidence Scale" or "Confidence in Maintaining Balance Scale" or "CONFbal").mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (285) 3 48 or 49 or 50 (4556) 4 randomised controlled trial.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (7473) 5 controlled clinical trial.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (913) 6 Clinical trial.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (8051) 7 exp Clinical trials/ or exp Experimental Design/ (46361) 8 randomiz*.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (40199) 9 single blind procedure.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (4) 10 double blind procedure.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (137) 11 crossover procedure.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (10) 12 placebo.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (29770) 13 prospective study.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (7750) 14 trial.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (66178) 15 or/52‐62 (150453) 16 23 and 39 and 51 and 63 (36)
AMED (Ovid Online)
1 aged.mp. [mp=abstract, heading words, title] (15703) 2 exp Aged/ or exp Aged 80/ or exp Frail Elderly/ (10876) 3 1 or 2 (15919) 4 exercis$.mp. (20198) 5 exp Exercise/ or exp Weight Training/ or exp Leisure Activities/ or exp Recreation/ or exp Dancing/ or exp Gardening/ or exp "Play and Playthings"/ or exp Physical Fitness/ or exp Retirement/ or exp Sports/ or exp Athletics/ or exp Baseball/ or exp Bicycling/ or exp Boxing/ or exp Football/ or exp Golf/ or exp Gymnastics/ or exp Jogging/ or exp Martial Arts/ or exp Feng Shui/ or exp Tai Chi/ or exp Tai Ji/ or exp Riding/ or exp Skiing/ or exp Soccer/ or exp Swimming/ or exp Tennis/ (13323) 6 exercise therapy.mp. [mp=abstract, heading words, title] (5673) 7 exercise movement techniques.mp. [mp=abstract, heading words, title] (15) 8 exp Physical education/ or exp Resistance training/ or exp Physical training/ (1280) 9 Physical fitness/ (1791) 10 exp Kinematics/ or exp Balance/ (21995) 11 exp Tai chi/ or exp Exercise therapy/ or Muscle strength/ or tai chi.mp. (10592) 12 exp Muscle strength/ or exp Breathing exercises/ or breathing exercises.mp. (6022) 13 Dance therapy/ (111) 14 kinesiotherapy.mp. (23) 15 or/4‐14 (45641) 16 fall$.mp. [mp=abstract, heading words, title] (3295) 17 exp Accidental falls/ (1435) 18 16 or 17 (3295) 19 fear.mp. [mp=abstract, heading words, title] (1285) 20 exp Fear/ (325) 21 afraid.mp. (62) 22 fright.mp. (12) 23 19 or 20 or 21 or 22 (1394) 24 18 and 23 (204) 25 ("Falls Efficacy Scale" or "Mobility Efficacy Scale" or "Survey of Activities and Fear of Falling in the Elderly").mp. [mp=abstract, heading words, title] (53) 26 ("University of Illinois at Chicago Fear of Falling Measure" or "SAFFE" or "UICFFM").mp. [mp=abstract, heading words, title] (3) 27 ("Activities Specific Balance Confidence Scale" or "Confidence in Maintaining Balance Scale" or "CONFbal").mp. [mp=abstract, heading words, title] (51) 28 fear of falling.mp. [mp=abstract, heading words, title] (184) 29 24 or 25 or 26 or 27 or 28 (271) 30 randomised controlled trial.mp. [mp=abstract, heading words, title] (1909) 31 controlled clinical trial.mp. [mp=abstract, heading words, title] (309) 32 Clinical trial.mp. [mp=abstract, heading words, title] (1645) 33 randomiz*.mp. [mp=abstract, heading words, title] (7694) 34 single blind procedure.mp. [mp=abstract, heading words, title] (0 Advanced) 35 double blind procedure.mp. [mp=abstract, heading words, title] (4) 36 crossover procedure.mp. [mp=abstract, heading words, title] (0 Advanced) 37 placebo.mp. [mp=abstract, heading words, title] (2419) 38 prospective study.mp. [mp=abstract, heading words, title] (1337) 39 trial.mp. [mp=abstract, heading words, title] (7754) 40 exp clinical trials/ or exp randomised controlled trials/ (3318) 41 or/30‐40 (14476) 42 3 and 15 and 29 and 41 (23)
Data and analyses
Comparison 1. Exercise versus control: primary outcome ‐ fear of falling, post intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fear of falling as measured by single‐item question, falls efficacy, balance confidence and concern about falling, post intervention | 24 | 1692 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 1.1 Fear of falling as measured by single‐item question | 4 | 380 | Std. Mean Difference (Random, 95% CI) | 0.17 [‐0.06, 0.39] |
| 1.2 Falls efficacy measured using the FES, MFES or K‐FES | 12 | 872 | Std. Mean Difference (Random, 95% CI) | 0.56 [0.21, 0.90] |
| 1.3 Balance confidence measured using ABC | 6 | 333 | Std. Mean Difference (Random, 95% CI) | 0.13 [‐0.10, 0.37] |
| 1.4 Concern about falling measured using the FES‐I and Short FES‐I | 2 | 107 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.09, 1.12] |
| 2 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, short term follow‐up (< 6 months) | 4 | 356 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.05, 0.38] |
| 3 Fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, long term follow‐up (6 months and more) | 3 | 386 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.01, 0.41] |
Comparison 2. Exercise versus control: subgroup analysis for fear of falling as measured by single‐item questions, falls efficacy, balance confidence and concern about falling, post intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Type of exercise (as classified using ProFaNE taxonomy) | 22 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 3D (Tai Chi) | 7 | 483 | Std. Mean Difference (Random, 95% CI) | 0.60 [0.09, 1.12] |
| 1.2 Strength/resistance | 4 | 416 | Std. Mean Difference (Random, 95% CI) | 0.08 [‐0.18, 0.34] |
| 1.3 Gait, balance, co‐ordination, functional tasks | 11 | 619 | Std. Mean Difference (Random, 95% CI) | 0.27 [0.05, 0.50] |
| 2 Type of control group | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 2.1 Alternative intervention (e.g. social group, education, etc) | 6 | 499 | Std. Mean Difference (Random, 95% CI) | 0.11 [‐0.08, 0.29] |
| 2.2 No intervention | 18 | 1199 | Std. Mean Difference (Random, 95% CI) | 0.48 [0.22, 0.73] |
| 3 Recruited participants at increased risk of falls | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 3.1 Studies not recruiting participants on the basis of increased risk of falls | 14 | 926 | Std. Mean Difference (Random, 95% CI) | 0.44 [0.14, 0.74] |
| 3.2 Studies recruiting participants at increased risk of falls | 10 | 772 | Std. Mean Difference (Random, 95% CI) | 0.24 [0.04, 0.45] |
| 4 Type of exercise (individual versus group) | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 4.1 Group exercises | 15 | 1051 | Std. Mean Difference (Random, 95% CI) | 0.49 [0.22, 0.76] |
| 4.2 Individual exercises | 9 | 647 | Std. Mean Difference (Random, 95% CI) | 0.14 [‐0.06, 0.35] |
| 5 Frequency of exercise | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 5.1 1 to 3 times per week | 20 | 1339 | Std. Mean Difference (Random, 95% CI) | 0.38 [0.15, 0.61] |
| 5.2 4 or more times per week | 4 | 359 | Std. Mean Difference (Random, 95% CI) | 0.30 [0.01, 0.58] |
| 6 Duration of exercise | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 6.1 Up to 12 weeks | 17 | 968 | Std. Mean Difference (Random, 95% CI) | 0.32 [0.16, 0.48] |
| 6.2 13 to 26 weeks | 5 | 530 | Std. Mean Difference (Random, 95% CI) | 0.52 [‐0.13, 1.17] |
| 6.3 More than 26 weeks | 2 | 200 | Std. Mean Difference (Random, 95% CI) | 0.13 [‐0.41, 0.66] |
| 7 Primary aim of the study | 24 | 1698 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.18, 0.56] |
| 7.1 To reduce fear of falling | 7 | 471 | Std. Mean Difference (Random, 95% CI) | 0.42 [0.13, 0.72] |
| 7.2 Other primary aim (e.g. balance improvement, fall prevention, etc) | 17 | 1227 | Std. Mean Difference (Random, 95% CI) | 0.34 [0.10, 0.59] |
Comparison 3. Exercise versus control: secondary outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Occurrence of at least one fall | 9 | 1113 | Risk Ratio (IV, Fixed, 95% CI) | 0.85 [0.74, 0.98] |
| 2 Falls rate | 9 | 1121 | Rate Ratio (Random, 95% CI) | 0.68 [0.53, 0.87] |
| 3 Depression score, post intervention | 4 | 406 | Std. Mean Difference (Fixed, 95% CI) | ‐0.08 [‐0.28, 0.13] |
| 4 Depression score, short‐term follow‐up (< 6 months) | 3 | 327 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.02, 0.43] |
| 5 Physical activity as measured using PASE (Physical Activity Scale for the Elderly) | 4 | 547 | Mean Difference (IV, Fixed, 95% CI) | 3.44 [‐1.65, 8.54] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barnett 2003.
| Methods | RCT | |
| Participants | Country: Australia n = 163 67% female Mean age in years (SD) = 75 (5.5) Study population: recruited from general practice clinics or 2 acute physiotherapy departments Inclusion criteria: participants were aged 65 years and older recruited from general practice clinics with 1 or more physical performance impairments known to be important risk factors for falls (i.e. lower limb weakness, poor balance and slow reaction time) Exclusion criteria: cognitive impairments, degenerative conditions or medical condition involving neuromuscular, skeletal or cardiovascular system which could prevent them from taking part in an exercise programme |
|
| Interventions | 1. Exercise group (n = 83). Weekly structured exercise group in a community setting, combined with a home exercise programme and written information on practical strategies for avoiding falls. Classes ran for 1 hour, over 4 terms for 1 year (37 classes) and steadily increased in speed and complexity. Class content was designed by a physiotherapist to specifically address physical falls risk factors and was delivered in groups of 6 to 18. Content included stretching, balance, co‐ordination, aerobic capacity and muscle strengthening exercises. The home exercise programme was based on the class content with diaries to record participation. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 80). Provided with the same information about falls prevention, but no alternative 'non‐exercise' activity |
|
| Outcomes | Number of falls (recorded by retrospective monthly fall calendars); fear of falling (single‐item measure ‐ recorded as % of participants who are afraid of falling); physical activity (Physical Activity Scale for the Elderly (PASE)). Outcomes were measured at baseline and 6 months post baseline. Falls were measured over the 12‐month intervention period | |
| Notes | The outcomes for the study were measured at 6 months into the 12‐month trial as this was deemed a sufficient period to achieve the beneficial results of the exercise programme. Adherence: 91% were still attending exercise classes at the end of the trial and performing home exercises at least once a week | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No further information provided on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | "Subjects were randomised in matched blocks (n = 6) after the baseline assessment using consecutively numbered opaque envelopes". Paper does not say if envelopes were sealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Fear of falling, number of falls and PASE were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Falls data collected retrospectively by postal survey at the end of each month |
Campbell 1997.
| Methods | RCT | |
| Participants | Country: New Zealand n = 233 100% female Mean age in years (SD) = 84 (3.3) Study population: recruited from general practice registers Inclusion criteria: women aged 80 and over who lived in the community recruited from general practice, able to move around within their own home and not receiving physiotherapy Exclusion criteria: score < 7 from 10 on the Mental Status Questionnaire (MSQ) |
|
| Interventions | 1. Exercise group (n = 116). 1‐year home‐based exercise programme prescribed by a physiotherapist. Exercises took approximately 30 minutes to complete and participants were to complete them at least 3 times a week, and walk outside the home at least 3 times per week. The programme included moderate intensity strengthening exercises with ankle cuff weights (0.5 kg and 1 kg), strength, balance and "active range of movement" exercises. The physiotherapist visited participants 4 times over 2 months prescribing a selection of exercise at appropriate and increasing levels of difficulty, and a walking plan. Participants were telephoned regularly to maintain motivation. ProFaNE taxonomy classification: strength/resistance 2. Control group (n = 117). Participants received a social visit from the research nurse 4 times during the first 2 months and telephoned them regularly during the year of follow‐up |
|
| Outcomes | Number of falls (recorded by monthly fall calendars); falls efficacy (Falls Efficacy Scale (FES)); physical activity (PASE). Outcomes were measured at baseline and post intervention. FES and PASE only presented as % change from baseline | |
| Notes | Adherence: after 1 year 42% were still completing the exercise programme 3 or more times a week | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The group allocation schedule was developed by a statistician using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Central allocation (telephone) after all baseline questionnaires and assessments were completed. List held off site by an independent person |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls, FES and PASE were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Low risk | Appears to be free of other sources of bias |
Clemson 2010.
| Methods | RCT | |
| Participants | Country: Australia n = 34 47% female Mean age in years (SD) = 82 (6.0) Study population: recruited from the Department of Veterans Affairs Home Front Database and a list from a general medical practice Inclusion criteria: community‐dwelling older adults aged 70 years and above who had 2 or more falls or an injurious fall in the past year Exclusion criteria: moderate to severe cognitive problems (> 2 errors on the Short Portable Mental Status Questionnaire); non‐conversational English; unable to walk around independently; resident in nursing home or hostel; unstable or terminal medical illness that would preclude planned exercises; neurological conditions that would result in motor performance difficulties (e.g. Parkinson's disease) |
|
| Interventions | 1. Lifestyle approach to reducing Falls through Exercise (LiFE) (n = 18). Home‐based lifestyle‐integrated balance and strengthening exercise programme specifically developed for fall prevention. LiFE was taught in 5 home visits with 2 booster visits over a 3‐month period and 2 follow‐up phone calls. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 16). No intervention |
|
| Outcomes | Number of falls (recorded by monthly fall calendars); falls efficacy (Modified Falls‐Efficacy Scale (MFES)); balance confidence (Activities Specific Balance Confidence Scale (ABC)). Measured at baseline, post intervention and 3 months follow‐up | |
| Notes | Adherence rates not reported MFES and ABC means and SDs obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using a random numbers table and stratifying by age and fall history (1 to 2 falls; ≥ 3 falls), but no further information provided |
| Allocation concealment (selection bias) | High risk | Open random allocation schedule. Participants were allocated in order of completion from random number list by an investigator not involved in assessment or intervention |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls, MFES and ABC were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on > 80% of participants in intervention group, but < 80% for the control group |
| Selective reporting (reporting bias) | High risk | Stated that adherence was monitored for the exercise group but data are not presented. Protocol not available |
| Other bias | Unclear risk | The intervention group were able to stand for longer on the tandem stand eyes open test (median 15 seconds) than the control group (median 1.65 seconds) at baseline. This baseline difference was adjusted for in the falls analysis and the results remained significant. The LiFE intervention was developed collaboratively by 4 of the authors |
Freiberger 2012.
| Methods | RCT | |
| Participants | Country: Germany n = 144 (groups 2 and 4 below) 47% female Mean age in years (SD) = 76 (4.1) Study population: recruited from a health insurance database Inclusion criteria: community‐dwelling older adults aged 70 to 90 who had fallen in the past 6 months or reported a fear of falling Exclusion criteria: those who were unable to walk around independently or had cognitive impairment (as noted by a score < 25 on the Digit Symbol Substitution Test (DSST)) |
|
| Interventions | 1. Strength and Balance Group (SBG) (n = 63). Weight‐bearing exercises with dumbbells and balance challenging exercises, stretching, plus sensory training including standing and walking with eyes closed or on unstable surfaces and training in the perception of centre of gravity in relation to the base of support 2. Fitness Group (FG) (n = 64). Strength and balance exercise with endurance training (walking with change of pace and direction and Nordic walking). ProFaNE taxonomy classification: strength/resistance 3. Multifaceted Group (MG) (n = 73). Strength and balance training with fall risk education to address fall‐related psychological aspects and cognitive training 4. Control Group (n = 80). No intervention All active interventions included progressive exercises for upper and lower body strength, standing weight‐bearing exercises with dumbbells and balance exercises. Interventions were provided by 2 fall prevention instructors for a period of 16 weeks with 2 1‐hour group sessions per week The intervention group used in the meta‐analysis comprised only the FG |
|
| Outcomes | Number of falls (recorded by monthly fall calendars); balance confidence (ABC); measured at post intervention, 6 months and 18 months follow‐up. ABC score at 6 months follow‐up used in the analysis of fear of falling at 6 months or more post intervention | |
| Notes | Adherence rates: majority of participants (> 80%) attended at least 24 of the 32 sessions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A third party not involved in the study applied a computerised random‐number generator |
| Allocation concealment (selection bias) | Unclear risk | A third party not involved in the study applied a computerised random number generator |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls and ABC were self reported by unblinded participants |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | No baseline scores for ABC presented. The control group had a greater proportion reporting fear of falling and higher education levels than the intervention group (fitness group) at baseline. Analyses were adjusted for these variables. The majority of falls occurred during sports activities (including cycling and skiing) |
Haines 2009.
| Methods | RCT | |
| Participants | Country: Australia n = 53 60% female Mean age in years (SD) = 81 (7.7) Study population: patients of a publicly funded, metropolitan, tertiary hospital Inclusion criteria: aged 65 years and over, treated on the geriatric rehabilitation medical or surgical units of a local hospital being planned for discharge to the community, gait instability as determined by physiotherapists or walked with a mobility aid Exclusion criteria: severe cardiac disease, cognitive impairment (determined by Abbreviated Mental Test Score less than 6 out of 10), aggressive behaviour, restricted lower limb weight‐bearing status or had been referred for post discharge community rehabilitation services |
|
| Interventions | 1. Exercise Group (n = 19). A DVD and workbook describing a progressive 2‐month home exercise programme based on the Kitchen Table exercise programme containing lower limb strength and balance exercises with 6 types of exercises each with 6 different levels of difficulty. A physiotherapist visited participants at home to help engagement with the DVD and workbook, ensure a safe environment and set appropriate starting level.The physiotherapist also made weekly phone calls for 8 weeks after the first home visit to measure participation in the exercise programme and to give advice on any problems the participants had encountered in attempting the exercise programme. Participants were encouraged to continue the exercise after the 8 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 34). No intervention |
|
| Outcomes | Number of falls (recorded by monthly fall calendars); balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence: less than 50% were still completing the exercise programme at the end of the trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random number generator |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, sealed, opaque envelopes (with participant numbers) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls and ABC scales were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Control group had longer length of hospital stay and higher median number of falls than intervention group at baseline |
Halvarsson 2011.
| Methods | RCT | |
| Participants | Country: Sweden n = 59 71% female Mean age in years (range) = 77 (67 to 93) Study population: recruited from advertisements in local newspapers Inclusion criteria: community‐dwelling older people aged 65 years or older, with a fear of falling and/or an experience of a fall during the previous 12 months. An ability to walk unaided indoors and a mini mental state examination score equal or greater than 24. Recruited by advertisements in local newspapers Exclusion criteria: severely impaired vision or hearing, severe cancer, severe pain, neurological disease or damage with symptoms, dizziness requiring medical care, or heart and respiratory symptoms that might affect participation |
|
| Interventions | 1. Balance group training (n = 38). Individually adjusted progressive and specific balance training, provided by physiotherapists for 45 minutes 3 times per week for 3 months. The programme was performed at 5 levels, each reflecting different demands on the postural control system. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 21). No intervention |
|
| Outcomes | Concern about falling (FES‐International (FES‐I); depressive symptoms (Geriatric Depression Scale‐20 (GDS‐20)). Measured at baseline and post intervention | |
| Notes | Adherence rates not reported FES‐I and GDS‐20 means and SDs obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Subjects drew an allocation slip from an envelope filled with 20 slips in a 2:1 ratio. No further information given on sequence generation |
| Allocation concealment (selection bias) | High risk | Participants could possibly see their allocation as they drew the allocation slip themselves from the envelope. No further information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | FES‐I and GDS‐20 were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | High risk | GDS scores not presented. Protocol not available |
| Other bias | Low risk | Appears to be free of other sources of bias |
Hinman 2002.
| Methods | RCT | |
| Participants | Country: USA n = 97 63% female Mean age in years (range) = 72 (63 to 87) Study population: recruited from local community. No further details given Inclusion criteria: able to walk around independently (unassisted or with a walking aid) and be able to follow a structured exercise programme Exclusion criteria: acute neurological or orthopaedic conditions, history of dementia |
|
| Interventions | 1. Home Exercise (HE) Programme (n = 32). Participants expected to perform a set of 20‐minute balance exercises and activities on an independent basis 3 times a week for 4 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Computer Balance (CB) Training (n = 34). Biodex balance system which provides an unstable platform that moves in response to changes in the user's centre of mass and tilts up to 20 degrees in every direction. 4‐week programme with 8 stability levels, supervised by a research assistant. First 2 weeks consisted of a 10‐minute warm‐up and then 10 minutes training. Final 2 weeks consisted of a 15 minute warm‐up and then 15 minutes training. In the final week, participants were given goggles to obscure their vision during the warm‐up exercises. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 3. Control group (n = 31). No training programme for 4 weeks and advised not to engage in any new exercise or training programmes for the duration of the trial The intervention group used in the analysis comprised the combined HE and CB groups |
|
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention | |
| Notes | Adherence: over 90% adhered to the exercise programme. Cash incentive offered | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | MFES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Participants received a monetary compensation for their participation in the study, with intervention groups compensated at a higher rate than the control group |
Karinkanta 2012.
| Methods | RCT | |
| Participants | Country: Finland n = 149 100% female Mean age in years = 73 (2.3) Study population: random population sample invited to express interest in study by post Inclusion criteria: 70 to 79‐year old women living in the city of Tampere, Finland; willingness to participate, full understanding of the study procedures, no history of any illness contraindicating exercise or limiting participation in the exercise programme or of illness affecting balance or bone, no uncorrected vision problems, and taking no medications known to affect balance or bone metabolism (within 12 months before the enrolment) Exclusion criteria: participants were excluded if they did high‐intensity exercises more than twice a week or if there femoral‐neck T score was lower than –2.5 (i.e. indicating osteoporosis and requiring medical attention) |
|
| Interventions | 1. A resistance‐training (RT) group (n = 37). The resistance training consisted of exercises for large muscle groups with increasing intensity from 50% to 60% of 1‐repetition maximum (1RM) to 75% to 80% of 1RM. ProFaNE taxonomy classification: strength/resistance 2. A balance‐jumping (BJ) group (n = 37). The balance‐jumping training comprised modified aerobics and step aerobics including a variety of balance, agility and impact exercises The degree of difficulty of movements, steps, impacts, and jumps was gradually increased. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 3. A combination (CG) group doing resistance and balance‐jumping training (n = 38). The combination training programme consisted of resistance and balance‐jumping training in alternating weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 4. No intervention (n = 37). Participants in the control group were asked to maintain their pre‐study level of physical activity during the 12‐month trial The intervention lasted for 3 weekly sessions of 45 minutes for 12 months The intervention group used in the analysis comprised the combined RT, BJ and CG groups |
|
| Outcomes | Fear of falling (visual analogue scale ‐ no fear at all (0) to very great fear (100)). Measured at baseline, post intervention and 12 months | |
| Notes | Adherence: 67% adhered to the exercise programmes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | VAS was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Self rated general health slightly better in the intervention group than control group at baseline |
Lai 2013.
| Methods | RCT ‐ cross‐over design | |
| Participants | Country: Taiwan n = 30 57% female Mean age in years (SD) = 72 (4.6) Study population: recruitment not described Inclusion criteria: community‐dwelling older adults aged 65 years and above Exclusion criteria: participants were excluded if they had a neurological condition such as Parkinson's disease, dementia and stroke, or if they had arthritis, vision impairment and cardiovascular disease that impaired walking, or if they were unable to walk without assistance |
|
| Interventions | 1. Xavix Measured Step System (XMSS) (n = 15) console with 1 step mat and connectors to TV. The XMSS exercise was conducted for 30 minutes, 3 times a week for 6 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 15). No intervention for the first 6 weeks, then given XMSS exercises for 6 weeks. The first 6 weeks served as the control |
|
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention, and 6 weeks post intervention (after cross‐over) | |
| Notes | Adherence rates not reported Data were used from the first period prior to cross‐over |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | MFES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Intervention group had higher MFES and Berg Balance Scale scores and lower Timed Up and Go times at baseline than control group |
Lajoie 2004.
| Methods | Quasi‐randomised trial | |
| Participants | Country: Canada n = 24 83% female Mean age in years (SD) = 71 (not reported) Study population: recruited from the community and from residential care facilities Inclusion criteria: aged 65 or older, able to stand and walk without an aid Exclusion criteria: participants with diabetes, neurological or sensory disorders, recurrent dizziness or unsteadiness, use of medications that may affect balance, joint replacement and medical conditions interfering with daily activities |
|
| Interventions | 1. Computerised balance training group (n = 12). 1‐hour computerised balance training sessions completed twice per week over an 8‐week period. Participants stood on a Kistler force platform and were asked to complete 15 computerised balance tests lasting 1 minute each, with resting periods given after each trial. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 12). No intervention |
|
| Outcomes | Balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence rates not reported ABC means and SDs obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequence generated by alternation. The author stated in a personal communication that this was achieved by "First subject was in group 1, second in group 2, third in group 1 etc." |
| Allocation concealment (selection bias) | High risk | Allocation not concealed. Quasi‐randomised study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ABC was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Paper describes only minimal baseline characteristics, so unclear if groups well balanced at baseline |
Lin 2007.
| Methods | RCT | |
| Participants | Country: Taiwan n = 100 (groups 1 and 2 only) 51% female Mean age in years (SD) = 77 (not reported) Study population: recruited from clinics and hospitals in rural agricultural area Inclusion criteria: community‐dwelling older adults aged 65 and older who had required medical attention due to sustaining a fall in the previous 4 weeks Exclusion criteria: none specified |
|
| Interventions | Intervention details: 1. Home‐based exercise group (n = 50). The intervention consisted of stretching, muscle strengthening and balance training. Participants exercised at home once every 2 weeks under supervision and were instructed to practice these exercises at least 3 times a week during the 4‐month intervention period. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Home safety assessment and modification group (n = 50). Participants were visited by a public health worker to perform a safety assessment on their home environment and given a list of specifically recommended modifications 3. Education group (n = 50). Participants received 1 social visit of 30 to 40 minutes every 2 weeks over the study period, plus pamphlets on falls prevention, including stretching and strengthening exercises to encourage initiation and persistence in activities The intervention group used for this review comprised the home‐based exercise group and the control group comprised the home safety assessment and modification group |
|
| Outcomes | Fear of falling (visual analogue scale); 15‐item Geriatric Depression Scale (GDS); number of falls (self reported). Measured at baseline, and 2 and 4 months post intervention | |
| Notes | Fear of falling was assessed using a 10 cm visual analogue scale, marked with the labels "No fear" and "Extremely fearful" where participants were asked to place a mark on the line at the point representing the extent of their fear Adherence rates not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomised, but no information provided about randomisation sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | VAS and GDS‐15 self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on ≥ 80% of participants in control group, but < 80% in intervention group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all prespecified outcomes have been reported |
| Other bias | Unclear risk | Most baseline characteristics not presented by treatment group so unclear if groups well balanced at baseline |
Logghe 2009.
| Methods | RCT | |
| Participants | Country: Netherlands n = 269 71% female Mean age in years (SD) = 77 (4.7) Study population: recruited from general practices Inclusion criteria: aged 70 years and older living at home and having a high falls risk (defined as 1 or more self reported fall incidents in the year preceding the study or at least 2 self reported risk factors for falling (disturbed balance, mobility problems, dizziness, and the use of benzodiazepines or diuretics)) Exclusion criteria: none specified |
|
| Interventions | 1. Tai Chi Chuan group (n = 138). Participants received 1 hour of Tai Chi Chuan training twice a week for 13 weeks. Classes were provided by 4 professional Tai Chi Chuan instructors using a predefined protocol. Participants were encouraged to practice at home at least twice a week for 15 minutes. Also received a brochure explaining how to prevent fall incidents in and around the house. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 131). No intervention |
|
| Outcomes | Number of falls (recorded by monthly fall calendars); falls efficacy (FES); physical activity (PASE). Measured at baseline, post intervention and 9 months follow‐up | |
| Notes | Adherence: 47% attended at least 80% of the Tai Chi lessons | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment. An independent research assistant performed a pre‐stratified block randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls, FES and PASE were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in each group at all follow‐up time points |
| Selective reporting (reporting bias) | Low risk | Protocol available. All pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Inconsistency between the number of participants with missing data in flow chart and the denominators reported in the text for falls outcomes |
McCormack 2004.
| Methods | RCT | |
| Participants | Country: Australia n = 43 70% female Mean age in years (SD) = 79 (5.9) Study population: recruited from the community by postal invitation Inclusion criteria: community‐dwelling older adults aged 65 years and over Exclusion criteria: participants were excluded if they reported uncontrolled hypertension, heart attack in the previous year, irregular heart beat and if they already belonged to a formal exercise class |
|
| Interventions | 1. Conventional Exercise (CE) group (n = 17). Low intensity stretching and conditioning exercises using body weight and light dumbbells as resistance. Performed 2 days per week for 10 weeks with each session approximately lasting 30 to 45 minutes. ProFaNE taxonomy classification: strength/resistance 2. Holistic exercise (HE) group (n = 18). Participants used a Range of Motion (RoM) dance method using the principles of Tai Chi. Performed 2 days per week for 10 weeks with each session approximately lasting 30 to 45 minutes. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 3. Control group (n = 8). No intervention The intervention group used in the analysis comprised the combined CE and HE groups |
|
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention | |
| Notes | Adherence: adherence did not differ between groups. Combined adherence over 80% in each group Data on the number of females obtained from personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | MFES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in Holistic and Conventional exercise groups, and > 80% of participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Very minimal baseline data presented so unclear if groups well balanced at baseline |
Nguyen 2012.
| Methods | RCT | |
| Participants | Country: Vietnam n = 96 50% female Mean age in years (SD) = 69 (5.1) Study population: recruitment not described Inclusion criteria: community‐dwelling older adults aged 60 to 79 years old. Being able to finish the Mini Mental State Examination (MMSE) with a score greater than 25 and having no experience in Tai Chi Exclusion criteria: serious diseases, such as symptomatic coronary insufficiency, angina, arrhythmia, orthostatic hypotension, and dementia |
|
| Interventions | 1. Tai Chi (n =48). Participants in the Tai Chi group attended a 60‐minute Tai Chi practice session twice a week for 6 months. The session consisted of a 15‐minute warm‐up and a 15‐minute cool‐down period. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. No intervention (n = 48) |
|
| Outcomes | Falls efficacy (FES). Measured at baseline, interim and post intervention | |
| Notes | Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | FES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on > 80% of participants in intervention group but < 80% of participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Time periods for interim data not reported. Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | FES slightly higher in control group than intervention group at baseline |
Reinsch 1992.
| Methods | Cluster‐RCT with randomisation by senior centre | |
| Participants | Country: USA n = 107 (groups 1 and 4 only) and 8 senior centres 89% female Mean age in years (SD) = 75 (7.5) Study population: recruited from 16 senior centres located in low socioeconomic areas Inclusion criteria: aged over 60 living in a senior centre Exclusion criteria: none given |
|
| Interventions | Intervention details: 1. Exercise intervention (n = 57). Participants performed the low intensity "stand‐up/step‐up" exercises, designed to improve strength and balance for 1 hour 3 times per week for 1 year. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Cognitive‐behavioural intervention (n = 51). Participants received health and safety advice to prevent falls, relaxation training and video game playing to improve reaction time 1 hour per week for 1 year 3. Exercise‐cognitive intervention (n = 72). 1 meeting per week as per cognitive behavioural intervention group and 2 meetings per week focusing on exercise, relaxation training and discussion of safety topics for 1 year 4. Discussion control group (n = 50). Participants discussed health and discussion topics of interest to older people 1 hour per week for 1 year The intervention group used for this review comprised the exercise group and the control group comprised the discussion group |
|
| Outcomes | Fear of falling (measured by 5‐point scale (1 = not at all worried to 5 = extremely worried)) | |
| Notes | Adherence: 77% of the exercise group attended at least 67% of the exercise classes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | Senior centres were randomised but no information given on concealment of allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Fear of falling and number of falls self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in the intervention group but > 80% of participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Analyses do not appear to be adjusted for clustering |
Rendon 2012.
| Methods | RCT | |
| Participants | Country: USA n = 40 65% female Mean age in years (SD) = 85 (5.4) Study population: recruited from retirement communities Inclusion criteria: community‐dwelling adults between 60 and 95 years of age, able to participate in physical activity for 45 to 60 minutes and who verbally reported having normal vision Exclusion criteria: participants with known orthopaedic, neurological or circulatory disorders that would prevent them from participating in the study |
|
| Interventions | 1. Virtual reality group (n = 20). Participants used 3 different balance games from the Nintendo® Wii Fit Software package. Participants alternated the exercise game sequence week‐to‐week during the 18‐session intervention (3 times a week for 6 weeks). Each session lasted approximately 35 to 45 minutes. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. No intervention (n = 20) |
|
| Outcomes | Balance confidence (ABC); depressive symptoms (Geriatric Depression Scale). Measured at baseline and post intervention | |
| Notes | Adherence: 80% met the 15 sessions minimum | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned but no further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ABC and GDS were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Little baseline data presented. ABC score was higher at baseline in the control group than the intervention group. GDS score was higher at baseline in the intervention group than the control group |
Resnick 2008.
| Methods | Cluster‐RCT with randomisation by senior centre | |
| Participants | Country: USA n = 166 participants and 13 senior centres 81% female Mean age in years (SD) = 73 (8.2) Study population: recruited from senior centres Inclusion criteria: community‐dwelling urban minority older adults aged 60 years and older, having a blood pressure recording less than 200/100, heart rate between 60 to 120, no known recent (within past 6 months) history of heart attack, stroke or new irregular heartbeat Exclusion criteria: not obtaining consent from their primary health care provider |
|
| Interventions | 1. Senior Exercise Self‐efficacy Project (SESEP) group (n = 100). 12 weeks of twice weekly exercise sessions, each lasting between 60 and 90 minutes, and including stretching, resistance and aerobic activities; plus 30 minutes per week of group efficacy‐enhancing programme. ProFaNE taxonomy classification: strength/resistance 2. Control (n = 66). Participants provided with twice weekly 60 to 90‐minute sessions of nutrition education for 12 weeks |
|
| Outcomes | Fear of falling (self rated on a scale of 0 to 4); depressive symptoms (GDS); overall activity (Yale Physical Activity Survey (YPAS)). Measured at baseline and post intervention | |
| Notes | Adherence: mean adherence rate was 77% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generated by coin toss |
| Allocation concealment (selection bias) | Unclear risk | Senior centres were randomised by geographic area using coin toss. No information given on concealment of allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Fear of falling, GDS and YPAS self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Analyses do not appear to be adjusted for clustering |
Sihvonen 2004.
| Methods | RCT | |
| Participants | Country: Finland n = 28 100% female Mean age in years (SD) = 82 (5.2) Study population: recruited from residential care homes Inclusion criteria: female, aged 70 years or over, living in residential care Exclusion criteria: unable to stand without a walking aid, unable to see visual feedback from a computer screen and unable to follow instructions |
|
| Interventions | 1. Exercise (n = 20) group. Participants attended 20‐ to 30‐minute long individualised specific balance exercise sessions using a computerised force platform with visual feedback 3 times a week for 4 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 8) group. No intervention |
|
| Outcomes | Number of falls (self reported monthly fall calendar); Fear of falling (single‐item measure ("No", "Yes, some", "Yes, a lot"); physical activity (the Senior Fitness Test). Measured at baseline, post intervention and 12‐month follow‐up | |
| Notes | Adherence: over 90% adhered to the exercise programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done in blocks by drawing lots |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls and fear of falling were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Intervention group undertook more physical activity and more reported high fear of falling at baseline than control group |
Tiedemann 2012.
| Methods | RCT | |
| Participants | Country: Australia n = 54 80% female Mean age in years (SD) = 68 (7.1) Study population: recruited from advertisements in local newspapers, newsletters and websites Inclusion criteria: participants were eligible if they were community‐dwelling, aged 59 years or older, were cognitively intact (defined as a score of ≥ 7 on the Short Portable Mental Status Questionnaire) and were willing and able to attend 12 weeks of group‐based yoga classes Exclusion criteria: having a medical condition that precludes exercise (e.g. unstable cardiac disease, uncontrolled hypertension, uncontrolled metabolic diseases, and large abdominal aortic aneurysm), minimal English language skills, hostel or nursing home resident, and/or current participation in yoga or Tai Chi |
|
| Interventions | 1. Yoga (n = 27). Participants attended a 1‐hour, twice‐weekly, group‐based yoga class for 12 weeks. Participants were also instructed to practise the poses at home for 10 to 20 minutes on at least 2 days per week. The balance challenge increased over time by gradually increasing the difficulty of the postures performed. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control (n = 27) group. Provided with information about falls prevention |
|
| Outcomes | Concern about falling (FES‐I). Measured at baseline and post intervention | |
| Notes | Adherence: 70% attended at least 20 out of 24 classes, 30% attended all classes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number schedule |
| Allocation concealment (selection bias) | Unclear risk | An investigator not involved in recruitment performed a pre‐stratified block randomisation using a computer‐generated random number schedule. No further information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | FES‐I was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Higher proportion of control group reported balance as fair or poor than the intervention group at baseline |
Ullmann 2010.
| Methods | RCT | |
| Participants | Country: USA n = 47 70% female Mean age in years (SD) = 76 (7.3) Study population: recruited from senior centres, churches and retirement communities Inclusion criteria: older adults aged 65 years or older Exclusion criteria: participants were screened on the Mini‐Mental State Examination and their performance on the Timed Up and Go (TUG). No further information provided |
|
| Interventions | 1. Feldenkrais intervention (FG) (n = 25). 1‐hour Feldenkrais sessions were held 3 times per week for 5 weeks. Feldenkrais is a mind‐body exercise that involves gentle movements carried out in a quiet, non‐competitive environment focused on improving balance and mobility. Classes were taught by a certified Feldenkrais teacher. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 22). Waiting list control |
|
| Outcomes | Falls efficacy (FES); balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence: over 90% adhered to the exercise programme. 6 of the control group crossed over to the FG at the end of the intervention period. Their data are only included prior to cross‐over FES and ABC means and SDs obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The screening TUG score and age were used to complete the stratified randomisation of participants. No further information provided |
| Allocation concealment (selection bias) | Unclear risk | No information given on allocation concealment. Persons who expressed a desire to attend the same class (couples, friends and carpool) were allowed to do so in order to facilitate participation. Members of these units were assigned to the same treatment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | FES and ABC were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | The control group had a lower BMI and had experienced a higher number of falls in the 3 months prior to randomisation than the intervention group |
Vogler 2009.
| Methods | RCT | |
| Participants | Country: Australia n = 180 79% female Mean age in years (SD) = 80 (7.0) Study population: inpatients from aged care and rehabilitation services were approached to participate after leaving hospital Inclusion criteria: older people aged 65 years or older recently discharged from an Aged Care and Rehabilitation hospital, who were medically fit to exercise and had completed hospital‐related rehabilitation Exclusion criteria: participants were excluded if they had medical contraindications to exercise, if they were cognitively impaired (Mini‐Mental State Examination score < 24 out of 30), or if they were discharged to a high‐care residential facility |
|
| Interventions | 1. Seated exercises (SE) (n = 60). Prescribed exercises to be performed while sitting on a standard dining chair with cuff weights and exercise bands. Exercises were to be done 3 times a week for 12 weeks, with the physiotherapist visiting 8 times in the 12 weeks to ensure the exercises were being performed correctly and to progress exercise intensity. ProFaNE taxonomy classification: strength/resistance 2. Weight‐bearing exercises (WBE) (n = 60). Prescribed strengthening and resistance exercises to be performed while standing with a chair or bench for support if required. Resistance was provided with weight‐loaded waist belts. Exercises were to be done 3 times a week for 12 weeks, with the physiotherapist visiting 8 times in the 12 weeks to ensure the exercises were being performed correctly and to progress exercise intensity. ProFaNE taxonomy classification: strength/resistance 3. Control group (n = 60). Received a 1‐hour social visit by a research assistant each week for 12 weeks The intervention group used in the analysis comprised the combined SE and WBE groups |
|
| Outcomes | Number of falls (self reported weekly fall calendar); falls efficacy (MFES); depressive symptoms (GDS). Measured at baseline, post intervention and 3 months follow‐up | |
| Notes | Adherence: mean adherence rate was 70% in the seated exercise group, and 62% in the weight‐bearing group MFES means and SDs obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed in blocks of 15 participants by computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Allocations for each participant were concealed in opaque envelopes. Unclear if envelopes were sealed or not |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls, MFES and GDS were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Vrantsidis 2009.
| Methods | RCT | |
| Participants | Country: Australia n = 62 76% female Mean age in years (SD) = 75 (8.2) Study population: recruited from advertisements in newspapers, promotion at local community groups and retirement villages and from volunteers in a research database Inclusion criteria: adults aged 55 years or over living at home, in a retirement village or a low‐care residential aged‐care facility, and who have at least 1 functional impairment (based on the Frenchay Activity Index) or have a history of 1 or more falls in the previous 6 months Exclusion criteria: cognitive impairment (< 7 on the Abbreviated Mental Test Score), inability to understand English, and unable to stand unsupported for at least 1 minute or walk a short distance indoors (minimum 5 metres) without a walking aid |
|
| Interventions | 1. Exercise group (n = 29). Participants participated in the Getting Grounded Gracefully programme based on the Feldenkrais method to specifically target dynamic balance, postural and turning stability, and weight‐shift transfers, which involved 2 40‐ to 60‐minute sessions per week over an 8‐week period. Classes were conducted at a community‐library meeting group and provided by the programme designer, an experienced Feldenkrais practitioner. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 33). No intervention |
|
| Outcomes | Falls efficacy (MFES). Measured at baseline and post intervention | |
| Notes | Participants included those living in low‐care residential homes where they were provided with help with dressing, eating, bathing and other support services such as cleaning, laundry and meals. No nursing care provided Adherence: mean adherence rate was 88% Personal communication with author to confirm participants were not receiving nursing care at the low‐care residential facility |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly ordered opaque envelopes used, but no information provided on how random sequence generated |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomised to the intervention group or control group by the use of randomly ordered opaque envelopes by a research officer not involved in the assessments. Unclear if envelopes were sealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | FES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | A conflict of interest might have been present in that the designer (and supplier) of the Getting Grounded Gracefully programme was the Feldenkrais practitioner in this study and that CDs of the programme were purchased by interested participants at the end of the study |
Wallsten 2006.
| Methods | RCT ‐ cross‐over design | |
| Participants | Country: USA n = 77 74% female Mean age in years (range) = 81 (61 to 92) Study population: recruited from posted flyers and flyers on bulletin boards in residential facilities Inclusion criteria: older adults (age range 61 to 92 years) living independently in a continuing care retirement community Exclusion criteria: history of hip fracture or replacement, currently enrolled in a balance study, knee replacement, Parkinson's disease, neurological condition which interfered with balance or walking, leukaemia or cancer, using an assistive device to walk 25 feet or further, Mini‐Mental State Exam score < 24 |
|
| Interventions | 1. Tai Chi Chuan (TC) group (n = 41). 1‐hour twice weekly Tai Chi classes conducted for 20 weeks focusing on gait, balance and strength. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 36). No intervention for the first 20 weeks, then given Tai Chi classes for 20 weeks. The first 20 weeks served as the control |
|
| Outcomes | Balance confidence (ABC). Measured at baseline, 10 weeks post baseline, post intervention and 5 months follow‐up | |
| Notes | Adherence rates not reported Data were used from the first period prior to cross‐over ABC means and SDs obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were "randomised" to a group, but no information provided on how randomisation sequence generated |
| Allocation concealment (selection bias) | Unclear risk | "After all eligible patients completed the baseline assessments, they were randomised to the early or late groups." No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ABC was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in each group. Only 46% of participants remained in trial at 40 weeks. Those remaining had significantly higher baseline functional assessment scores than those lost to follow‐up |
| Selective reporting (reporting bias) | High risk | No baseline or follow‐up data reported for ABC. Protocol not available |
| Other bias | Unclear risk | Most baseline data only presented for those with outcome data at specific time points. Unclear if groups well balanced at baseline |
Weerdesteyn 2006.
| Methods | Randomised trial with additional non‐randomised group | |
| Participants | Country: The Netherlands n = 58 (groups 1 and 2 only) 72% female Mean age in years (SD) = 74 (5.7) Study population: recruited from advertisements in newspapers Inclusion criteria: community‐dwelling older adults aged 65 and over, with at least 1 fall prior to participation and able to walk 15 minutes without the use of a walking aid Exclusion criteria: severe cardiac, pulmonary or musculoskeletal disorders, pathologies associated with increased fall risk (i.e. stroke or Parkinson's disease), osteoporosis and the use of psychotropic drugs |
|
| Interventions | 1. Exercise group (n = 30). Twice weekly 1.5‐hour exercise sessions for 5 weeks comprised of balance, gait and co‐ordination training in an obstacle course, walking exercises that stimulated walking in a crowded environment with changes in speed and direction, the practice of fall techniques derived from marital arts. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 28). No intervention 3. Non‐randomised group (n = 49). Assigned same exercise as Exercise group above. Non‐randomised group participants have been excluded from analyses in this review |
|
| Outcomes | Number of falls (recorded by monthly fall calendars) measured at baseline, 6 months and 7 months follow‐up after intervention. Balance confidence (ABC). Measured at baseline and post intervention | |
| Notes | Adherence: mean attendance rate was 87% for the combined exercise group and non‐randomised group ABC means and SDs (excluding non‐randomised group) obtained through personal communication with author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The following information was obtained from Gillespie 2012. Quote: "Block randomisation (3 blocks of 20) with gender stratification with equal probability for either exercise or control group assignment." |
| Allocation concealment (selection bias) | Unclear risk | The following information was obtained from Gillespie 2012. Quote:"The group allocation sequence was concealed (to both researchers and participants) until assignment of interventions. We had participants draw a sealed envelope with group allocation ticket from a box containing all remaining envelopes in the block" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Falls incidence and ABC were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | The intervention group had a significantly higher proportion of fallers at baseline than the control group |
Westlake 2007.
| Methods | RCT | |
| Participants | Country: Canada n = 36 % female not reported Mean age in years (SD) = not reported Study population: recruited from advertisements in newspapers and flyers Inclusion criteria: community‐dwelling older adults aged 65 years and older Exclusion criteria: pre‐existing major lower extremity pathology neurological disorders or balance difficulties, and health conditions that would prevent participation in the exercise programme |
|
| Interventions | 1. Exercise group (n = 17). 1‐hour sensory specific balance classes were held 3 times per week over an 8‐week period, following the FallProof programme which focuses on static and dynamic balance exercises with transitions between different sensory conditions. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 19). 1‐hour falls prevention education group, held once a week for 8 weeks. The education group received information about 'non‐exercise' related potential fall risk factors, such as nutrition, environmental hazards and the importance of sleep |
|
| Outcomes | Balance confidence (ABC); physical activity (PASE). Measured at baseline and post intervention. Additionally the exercise group were re‐assessed at 2 months follow‐up | |
| Notes | Adherence: mean adherence rate was 66% Personal communication with author confirmed no exercise information was provided to the control group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised into the exercise or education group. No information given on generation of randomisation schedule |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | ABC and PASE were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 44 participants randomised into the exercise or control group. The number per group at baseline is not reported. Outcomes assessed on 17 exercise group and 19 control group participants |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Limited baseline data reported so unable to assess if groups were well balanced at baseline |
Wolf 1996.
| Methods | RCT | |
| Participants | Country: USA n = 200 81% female Mean age in years (SD) = 76 (4.7) Study population: recruited by advertisements in newspapers and from an independent living facility Inclusion criteria: aged 70 years and older, living in unsupervised environments, ambulatory and agreeing to participate weekly for 15 weeks with 4‐month follow‐up Exclusion criteria: the presence of debilitating conditions such as cognitive impairments, metastatic cancer, crippling arthritis, Parkinson's disease or major stroke, or profound visual defects that could compromise balance or ambulation |
|
| Interventions | 1. Computerised Balance Training (BT) group (n = 64). Individual balance training on a computerised force platform. Participants had 1 hour of instruction per week (with approximately 45 minutes individual contact time with an instructor) for 15 weeks. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Tai Chi Quan (TC) group (n = 72). Classes of Tai Chi Quan focusing on all components of movement that typically becomes limited with ageing. Participants had 2 hours of instruction per week (2 separate sessions) with a total of approximately 45 minutes contact time with an instructor. Participants were encouraged to practice at least 15 minutes twice a day at home. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 3. Education group (n = 64). Weekly 1‐hour meetings for 15 weeks were held with a gerontological nurse/researcher to discuss a variety of topics such as pharmacological management, sleep disorders, cognitive deficits, coping with bereavement and other issues important to each group The intervention group used in the analysis comprised the combined BT and TC groups |
|
| Outcomes | Number of falls (recorded by weekly fall calendars); falls efficacy (FES) and Center for Epidemiologic Studies ‐ Depression (CES‐D) scale. Falls were defined using the FICSIT definition ("unintentionally coming to rest on the ground, floor or lower level") and the Atlanta site definition ("falls resulting in fractures, dislocation, sprains, bruises, lacerations, scrapes and other medical problems"). Mean and SD for FES presented at baseline and categories of fear of falling (not at all afraid, somewhat afraid, fairly afraid, very afraid of falling) presented at follow‐up. Measured at baseline, post intervention and at 4‐month follow‐up | |
| Notes | We used falls defined using the FICSIT definition in the meta‐analysis. A subset of participants (n = 72) who "tended to be reclusive" were reported on in Wolf 1997. Adherence: over 90% adhered to the exercise programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Individuals were assigned to an intervention using a computer‐generated, fixed randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls and fear of falling were self reported by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on ≥ 80% of participants in each group |
| Selective reporting (reporting bias) | High risk | Protocol not available. Data only presented for outcomes that differed significantly between groups post intervention or at follow‐up |
| Other bias | Unclear risk | The Tai Chi group had a higher proportion of participants in paid work than the balance training or control group, a higher proportion volunteering than the balance training group and a higher proportion with cataracts than the control group at baseline. The Tai Chi group had a lower mean BMI than the balance training or control group at baseline |
Wolf 2001.
| Methods | RCT | |
| Participants | Country: The Netherlands n = 94 73% female Mean age in years (SD) = 84 (5.6) Study population: recruited from 3 residential care facilities and by advertisements in newspapers Inclusion criteria: older adults aged 75 years and older, living independently or in a residential care facility Exclusion criteria: recovering from an acute illness, received physical therapy during the previous month, a Mini‐Mental State Examination score < 17, Berg Balance Scale (BBS) score < 52 and impaired balance during functional activities (as determined by a physiotherapist) |
|
| Interventions | 1. Balance training group (n = 47). Participants received 12 sessions of 30‐minute balance training provided by physical and recreational therapists 2 to 3 times per week during a 4‐ to 6‐week period at home or at a physical therapy department. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control group (n = 47). Offered individual‐orientated activities including handicraft, music, media, board games, discussion groups, memory training and car tours |
|
| Outcomes | Fear of falling (visual analogue scale (VAS)); anxiety and depression (Hospital Anxiety and Depression Scale (HADS)). Measured at baseline, post intervention and 1 month follow‐up | |
| Notes | Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Subjects were randomly assigned to the 2 treatments using sealed envelopes selected by a blindfolded person. No information provided on how randomisation sequence generated |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes selected by a blindfolded person. Unclear if envelopes were sequentially numbered |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | VAS and HADS were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on > 80% of participants in the control group, but < 80% in the intervention group |
| Selective reporting (reporting bias) | High risk | Means and SDs not presented for HADS. Protocol not available |
| Other bias | Unclear risk | Control group had slightly higher HADS depression scores at baseline than the intervention group |
Yang 2012.
| Methods | RCT | |
| Participants | Country: Australia n = 165 44% female Mean age in years (SD) = 81 (6.2) Study population: recruited from advertisements in newspapers, newsletters and presentations to community groups Inclusion criteria: community‐dwelling older adults aged 65 years and older, community ambulant, requiring no walking aid, no more than 1 fall in the previous 12 months, having concerns about balance and a mild balance dysfunction Exclusion criteria: participants were excluded if balance performance was within normal limits |
|
| Interventions | 1. Home‐based exercise programme (n = 82). Participants received a 6‐month physical therapist prescribed balance and strength home exercise programme based on the Otago Exercise Program and the Visual Health Information Balance and Vestibular Exercise Kit. The programme consisted of a warm‐up, balance and strength exercises with a tailored walking programme. All exercises were performed without upper limb support and with ankle weights if able. Participants were instructed to perform exercises taking approximately 20 minutes 5 times per week and a graduated walking programme aiming for at least 30 minutes per day. ProFaNE taxonomy classification: gait, balance, co‐ordination, functional tasks 2. Control (n = 83). No intervention |
|
| Outcomes | Number of falls (self reported); falls efficacy (MFES); Human Activity Profile ‐ Adjusted Activity Score (HAP‐AAS). Measured at baseline and post intervention | |
| Notes | Adherence: 44.1% reported full adherence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation schedule was developed by computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Group allocation was performed by a researcher who was not involved in recruiting or assessing participants. No further information on allocation concealment provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Number of falls, MFES and HAP‐AAS were self reported by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Groups appeared well balanced at baseline. Those who withdrew from the trial had significantly worse scores on the step test and limit of stability maximum excursion test than those who completed the trial |
Yoo 2010.
| Methods | RCT | |
| Participants | Country: South Korea n = 21 100% female Mean age in years (SD) = 71 (2.7) Study population: community volunteers. No further information provided Inclusion criteria: community‐dwelling older women aged 65 years and older capable of participating in moderate intensity aerobic and resistance exercises, with no more than 1 risk factor for cardiovascular disease Exclusion criteria: difficulty with activities of daily living (ADL), uncontrolled hypertension, a history of metabolic disorders, irregular menstrual cycles or amenorrhoea, hip or vertebral fracture and currently taking hormones or hormonal medication |
|
| Interventions | 1. Exercise group (n = 11). Participants were involved in a 12‐week supervised walking exercise programme 3 times a week wearing ankle weights (1 kg each) in an outdoor field in a local elementary school. The programme included a 10‐minute warm‐up without ankle weights, 45 minutes of walking with ankle weights, and a 5‐minute cool down without ankle weights. Exercise intensity was maintained at 60% of heart rate reserve (HRR) determined by a heart rate monitor. ProFaNE taxonomy classification: strength/resistance 2. Control group (n = 10). No intervention |
|
| Outcomes | Falls efficacy (K‐FES), Tideiksaar (1997) Fear of Falling questionnaire Yale Physical Activity score (YPAS). Measured at baseline and post intervention | |
| Notes | Adherence rates not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, but no information provided about randomisation sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Tideiksaar Fear of Falling questionnaire and K‐FES were self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data are based on < 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Low risk | Appears to be free of other sources of bias |
Zhang 2006.
| Methods | RCT | |
| Participants | Country: China n = 49 47% female Mean age in years (SD) = 70 (4.3) Study population: selected from a previous study investigating falls among community‐dwelling older adults Inclusion criteria: community‐dwelling older adults aged 60 and older who had a lower ability for maintaining balance (defined as a 1‐leg stand time between 5 and 20 seconds) and able to walk around independently Exclusion criteria: participants were excluded if they had a 1‐leg stance time of less than 5 seconds and were considered at risk to practice Tai Chi Chuan |
|
| Interventions | 1. Tai Chi Chuan (TC) group (n = 25). Participants attended 1‐hour group classes 7 times a week for 8 weeks and were instructed to perform 24 simplified forms of TC. Exercises were performed in a park and taught by experienced TC instructors. If participants could not attend the class, they were asked to complete a home TC programme consisting of 11 easy forms of TC taking approximately 30 minutes to complete. ProFaNE taxonomy classification: 3D (Tai Chi, Qi Gong, dance, yoga) 2. Control group (n = 24). No intervention |
|
| Outcomes | Falls efficacy (FES ‐ translated into Chinese). Measured at baseline and post intervention | |
| Notes | Adherence: over 90% adhered to the exercise programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Prior to randomisation, the 49 participants were divided into 25 pairs according to sex, experience of falling and exercise habits. Not all pairs were matched for sex or exercise habits. Pairs were then randomly assigned to either the intervention or control group by a coin toss |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded to allocation. Note: blinding not possible due to nature of intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | FES was self completed by participants who knew their allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data are based on > 80% of participants in each group |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Unclear if all pre‐specified outcomes have been reported |
| Other bias | Unclear risk | Participants were selected from a previous study by the authors (Zhang et al 2003) |
ABC: Activities‐specific Balance Confidence scale BBS: Berg Balance Scale BMI: body mass index FES: Falls Efficacy Scale FES‐I: FES‐International FICSIT: 'Frailty and Injuries: Cooperative Studies of Intervention Techniques' study GDS: Geriatric Depression Scale GDS‐20: Geriatric Depression Scale‐20 HADS: Hospital Anxiety and Depression Scale HAP‐AAS: Human Activity Profile ‐ Adjusted Activity Score K‐FES: Korean version of the FES LiFE: Lifestyle approach to reducing Falls through Exercise MFES: Modified Falls‐Efficacy Scale PASE: Physical Activity Scale for the Elderly RCT: randomised controlled trial SD: standard deviation TUG: Timed Up and Go VAS: visual analogue scale XMSS: Xavix Measured Step System YPAS: Yale Physical Activity Survey
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bainbridge 2011 | Not a RCT or quasi‐RCT |
| Ballard 2004 | Multi‐component intervention. Participants received strength and balance exercises plus 6 home safety education sessions. Comparator group invited to attend exercise programme for 6 classes |
| Banez 2008 | Not a RCT or quasi‐RCT |
| Batson 2006 | Multi‐component intervention. Participants received exercise and mental practice of motor imagery. Comparator group were provided with exercise |
| Bean 2002 | Comparator group were assigned to a walking programme |
| Beyer 2007 | Multi‐component intervention. Participants were allocated to a multidimensional training programme and behaviour counselling |
| Bishop 2007 | Not a RCT or quasi‐RCT |
| Bishop 2010 | Not a RCT or quasi‐RCT |
| Bula 2011a | Not a RCT or quasi‐RCT |
| Bunout 2005 | Fear of falling not measured |
| Chang 2007 | Community‐dwelling people and nursing home residents. Data not presented separately for community participants |
| Conroy 2010 | Multi‐component intervention. Participants invited to attend a falls prevention programme involving a medical review, physiotherapy and occupational therapy treatments |
| Davis 2011 | Not a RCT or quasi‐RCT |
| Davison 2005 | Multi‐component intervention. The intervention group received medical assessment, physiotherapy and occupational therapy |
| Delbaere 2006 | Not a RCT or quasi‐RCT |
| Devereux 2005 | Study population restricted to participants with osteopenia or osteoporosis |
| Duque 2013 | Multi‐component intervention. Participants received training on a virtual reality system, an invitation to join an exercise programme, medication review, home visit by an occupational therapist, hearing and visual assessment, nutritional supplements and educational materials on falls prevention. Comparator group participants received the same intervention but with no training on the virtual reality system |
| Elley 2003 | Majority of participants under 65 years old |
| Elley 2008 | Multi‐component intervention. Exercise group referred to optometrist, podiatrist, physical therapist and occupational therapist |
| Faber 2006 | Participants recruited from low and high‐level care nursing centres |
| Faes 2011 | Multi‐component intervention. Physical and psychological interventions provided |
| Foley 2009 | Not a RCT or quasi‐RCT |
| Gillespie 2012 | Not a RCT or quasi‐RCT |
| Gitlin 2006 | Multi‐component intervention. Participants provided with physical and occupational therapy |
| Greendale 2009 | Study population restricted to participants with adult‐onset hyperkyphosis |
| Hagedorn 2010 | Comparator group received resistance, balance and physical fitness training |
| Hakim 2003 | Not a RCT or quasi‐RCT |
| Hakim 2004 | Not a RCT or quasi‐RCT |
| Hakim 2010 | Not a RCT or quasi‐RCT |
| Harling 2008 | Not a RCT or quasi‐RCT |
| Harmer 2008 | Not a RCT or quasi‐RCT |
| Hartmann 2009 | Not a RCT or quasi‐RCT |
| Hess 2005 | Not a RCT or quasi‐RCT |
| Hinrichs 2009 | Not a RCT or quasi‐RCT |
| Huang 2011 | Multi‐component intervention. Tai Chi with cognitive behavioural strategies |
| Hugel 2000 | Not a RCT or quasi‐RCT |
| Inokuchi 2007 | Not a RCT or quasi‐RCT |
| ISRCTN05350123 | Comparator group received strength and balance exercises |
| ISRCTN05545178 | Comparator group received strength and balance exercises |
| ISRCTN21695765 | Nursing home residents |
| ISRCTN48015966 | Multi‐component intervention. Intervention group received general guidance for physical activity, guidance for adequate nutrition, individually tailored or group training of strength and balance, treatment of illnesses increasing the risk of falling, review of medications, home hazard assessment and modification |
| ISRCTN67535605 | Multi‐component intervention. Intervention group received strength and balance training, community falls prevention rehabilitation and medical and social care |
| ISRCTN75134517 | Multi‐component intervention. Intervention group received exercise training in combination with cognitive training. Comparator group received exercise training |
| ISRCTN89512790 | No exercise intervention reported. Health coaching programme using face to face and telephone coaching sessions |
| Iwamoto 2009 | Fear of falling not measured |
| Jansson 2004 | Not a RCT or quasi‐RCT |
| Juarbe 2009 | Not a RCT or quasi‐RCT |
| Jury 2009 | Not a RCT or quasi‐RCT |
| Kelsey 2010 | Not a RCT or quasi‐RCT |
| Kemmler 2010 | Comparator group received a wellness programme of low‐intensity walking and strength and balance exercises. Fear of falling not measured |
| Kerse 2010 | Multi‐component intervention. Intervention group received exercises on a Green Prescription and motivational interviewing techniques from exercise specialists. Fear of falling not measured |
| Kim 2009a | Intervention did not include exercise |
| Kim 2011 | Study population restricted to community‐dwelling women aged 70 or older with multiple symptoms of geriatric syndrome (MSGS) including functional decline, urinary incontinence and fear of falling |
| Kuo 2011 | Not a RCT or quasi‐RCT |
| Kuptniratsaikul 2011 | Not a RCT or quasi‐RCT |
| Kuramoto 2006 | Not a RCT or quasi‐RCT |
| Kwok 2011 | Multi‐component intervention. All participants given home safety and modification advice in addition to their exercise. Comparator group provided with a gym‐based rehabilitation programme and home exercise |
| Kwon 2011 | Not a RCT or quasi‐RCT |
| Lee 2010 | Not a RCT or quasi‐RCT |
| Leininger 2006 | Comparator group were provided with 4 1‐hour presentations on osteoporosis and exercise in older adults, including discussion and handouts over a 10‐week period |
| Li 2005 | Comparator group were provided with a stretching exercise programme for 1 hour, 3 times a week, for 26 weeks |
| Li 2010 | Intervention did not include exercise |
| Lin 2008 | Not a RCT or quasi‐RCT |
| Liu 2007 | Comparator group provided with seated exercises |
| Liu 2008 | Not a RCT or quasi‐RCT |
| Liu 2009a | Not a RCT or quasi‐RCT |
| Liu 2010 | Not a RCT or quasi‐RCT |
| Lord 1995 | Fear of falling not measured |
| Lord 2005 | Multi‐component interventions. The extensive intervention group received group exercises and strategies for maximising vision and sensation. The minimal intervention group received home exercise sheets and written advice about how to maximise their vision and take precautions for loss of peripheral sensation |
| Luukinen 2007 | Study population restricted to participants with ≥ 1 risk factor for falling (≥ 2 falls in previous year, loneliness, poor self rated health, poor visual acuity, poor hearing, depression, poor cognition, impaired balance, impaired chair rise and slow walking speed) |
| Maginnis 1999 | Not a RCT or quasi‐RCT |
| Mahoney 2007 | Multi‐component intervention. Intervention group provided with exercise, falls risk assessment and medication review |
| Marchetti 2005 | Not a RCT or quasi‐RCT |
| McCulloch 2002 | Fear of falling not measured |
| McKinley 2008 | Comparator group provided with walking exercises for 2 hours, 2 times per week, for 10 weeks |
| McMurdo 1997 | Multi‐component intervention. Intervention group exercised and took calcium supplements |
| Mihay 2006 | Comparator group provided with strength training exercises 3 times a week for 18 months |
| Miller 2010 | Not a RCT or quasi‐RCT |
| Morgan 2004 | Fear of falling not measured |
| Nagai 2011 | Not a RCT or quasi‐RCT |
| NCT00037167 | Fear of falling not measured |
| NCT00140322 | Multi‐component intervention. Intervention group received a comprehensive health assessment combined with tailored risk reduction strategies such as strength and balance exercises |
| NCT00217360 | Multi‐component intervention. Intervention participants received a "customised multifactorial falls prevention program" |
| NCT00323596 | Multi‐component intervention. Strength and balance training, plus falls risk factor assessment followed by a comprehensive geriatric assessment and treatment |
| NCT00483275 | Multi‐component intervention. Intervention included fall prevention programme with alfacalcidol and calcium, patient education and a mobility programme |
| NCT00805220 | Comparator group participated in a walking programme |
| NCT00986466 | Multi‐component intervention. Participants received exercise and vitamin D supplementation |
| NCT01006967 | Comparator group received a standard programme of physical therapy for gait and balance |
| NCT01313481 | Comparator group performed strength and balance exercises 3 times a week for 12 weeks |
| NCT01523600 | Comparator group received wellness education, which consisted of supervised group training done once a week with the focus on stretching and flexibility exercises |
| Nitz 2004 | Comparator group received balance training strategies |
| Obuchi 2004 | Comparator group provided with treadmill exercises. Fear of falling not measured |
| Oh 2012 | Multi‐component intervention. Before randomisation, all participants attended 3 educational classes that discussed falling, osteoporosis and bone fracture. Comparator group were provided with daily stretch exercises |
| Robertson 2001a | Fear of falling not measured |
| Robertson 2001b | Not a RCT or quasi‐RCT |
| Romero 2010 | Not a RCT or quasi‐RCT |
| Rosendahl 2006 | Multi‐component intervention. Participants provided with exercise and protein‐enriched energy supplement |
| Rosie 2007 | Comparator group performed low‐intensity knee extension exercises daily for 6 weeks |
| Rubenstein 2000 | Fear of falling not measured |
| Schwarting 2002 | Not a RCT or quasi‐RCT |
| Sherrington 2008a | Not a RCT or quasi‐RCT |
| Sherrington 2014 | Multi‐component intervention. Participants provided with home exercises and a 32‐page booklet about fall prevention. The booklet contained information about risk factors for falls, environmental modification for falls risk reduction and what to do after a fall |
| Shigematsu 2008 | Comparator group provided with strength and balance training |
| Shumway‐Cook 1997 | Not a RCT or quasi‐RCT |
| Silsupadol 2009 | Comparator group provided with balance training exercises |
| Simmons 1996 | Fear of falling not measured |
| Singh 2012 | Majority of participants under 65 years old |
| Sipe 2009 | Comparator group provided with resistance exercises 3 days a week for 12 weeks |
| Snow 1999 | Not a RCT or quasi‐RCT |
| Southard 2004 | Not a RCT or quasi‐RCT |
| Southard 2006 | Multi‐component intervention. Intervention group received balance retraining exercises and efficacy training (including discussion of group fears, introduction to home safety and an opportunity to practise any skill that is difficult or avoided secondary to fear). Comparator group provided with balance retraining exercises |
| Spink 2011 | Not a RCT or quasi‐RCT |
| Suzuki 2004 | Fear of falling not measured |
| Sze 2008 | Not a RCT or quasi‐RCT |
| Szturm 2011 | Comparator group provided with strength and balance exercises, assessment of walking aids, a gait re‐education programme and an unsupervised walking programme |
| Taggart 2002 | Not a RCT or quasi‐RCT |
| Takai 2010 | Nursing home residents |
| Talley 2008 | Not a RCT or quasi‐RCT |
| Tennstedt 1998 | Multi‐component intervention. Participants received group discussions focused on self efficacy, cognitive restructuring and exercise |
| Tousignant 2012 | Comparator group provided with strength and walking exercises |
| Underwood 2011 | Multi‐component intervention. Care home staff received depression awareness and physical activity training. Intervention participants received a twice weekly exercise group |
| Van Haastregt 2007 | Not a RCT or quasi‐RCT |
| Vind 2010 | Multi‐component intervention. Participants received personalised exercises and medical treatment |
| Voukelatos 2007 | Fear of falling not measured |
| Williams 2002 | Multi‐component intervention. Intervention participants received a 16‐week balance and mobility exercise group with a self efficacy intervention. Comparator group provided with balance and mobility exercises |
| Williams 2010 | Not a RCT or quasi‐RCT |
| Williams 2010a | Not a RCT or quasi‐RCT |
| Woo 2007 | Fear of falling not measured |
| Wrisley 2006 | Majority of participants under 65 years old |
| Wu 2010 | Comparator group provided with Tai Chi exercises |
| Yamada 2011 | Not a RCT or quasi‐RCT |
| Yamada 2011a | Comparator group provided with strength and balance training exercises each week |
| Yan 2009 | Not a RCT or quasi‐RCT |
| Zilstra 2007 | Not a RCT or quasi‐RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Arai 2007.
| Methods | RCT |
| Participants | Country: Japan n = 171 % female not reported Mean age in years (SD) = 74.1 (not reported) Study population: recruited via advertisements in publications and clubs for the elderly Inclusion criteria: community‐dwelling, aged ≥ 65, ambulatory with or without assisting devices Exclusion criteria: cerebrovascular or cardiovascular accidents reported within the past 6 months, acute liver problems or the active phase of chronic hepatitis, diabetes mellitus with a history of hypoglycaemic attack, or with fasting levels of plasma glucose concentrations of 200 mg/dl or higher, or with complications such as retinopathy or nephropathy, systolic blood pressure above 180 mm Hg or diastolic blood pressure above 110 mm Hg at rest, diagnosis of severe heart disease or an acute orthopaedic problem, diagnosis of dementia or depression made by a medical doctor, or an inability to understand and follow the instructions of the research staff; restriction of physical activities by a medical doctor |
| Interventions | 1. Exercise group (n = 86). Group‐based resistance and balance training for 1.5 hours, twice weekly, for 3 months 2. Control group (n = 85). Health education group for 1.5 hours, twice a month, for 3 months. Lectures included "Knowledge of Resistance Training" |
| Outcomes | Falls efficacy (FES ‐ translated into Japanese, with the degree of confidence in accomplishing tasks based on a scale of 1 to 4 rather than 1 to 10). Measured at baseline and post intervention |
| Notes | — |
Brouwer 2003.
| Methods | RCT |
| Participants | Country: Canada n = 38 74% female Mean age in years (SD) = 77.1 (5.1) for exercise group, 78.0 (5.5) for control Study population: recruited through newspaper and radio advertisements seeking individuals fearful of falling Inclusion criteria: seniors living independently with a lasting concern about falling causing them to avoid or curtail activities they felt they were capable of doing Exclusion criteria: coexisting conditions affecting balance (e.g. neuropathy, vestibular deficits, mobility limiting arthritis, pre‐existing neurological conditions), not being able to commit to an 8‐week intervention |
| Interventions | 1. Exercise group (n = 17). Group‐based low‐resistance exercises and weight shifting activities, and a 40‐minute, twice weekly home programme of exercises and stretches 2. Control group (n = 17). Group‐based education programme focused on identifying and reducing risk factors for falls. Topics included "the importance of good nutrition and activity" Both groups were delivered by a physiotherapist for 1 hour, weekly, for 8 weeks |
| Outcomes | Balance confidence (ABC). Measured at baseline, post intervention and 6 weeks follow‐up. Adherence to exercise intervention measured by class attendance and participant log books |
| Notes | 38 participants randomised but 4 withdrew during study. Number of participants randomised to each group before the withdrawals not reported |
Henwood 2008.
| Methods | RCT |
| Participants | Country: Australia n = 67 54% female Mean age in years (SD) = 71.2 (1.3) for high‐velocity training group, 69.6 (1.1) for strength training group, 69.3 (1.0) for control Study population: recruited by newspaper advertisement Inclusion criteria: independently living, community‐dwelling, aged 65 to 84 Exclusion criteria: acute or terminal illness, unstable or ongoing cardiovascular and/or respiratory disorder, neurological or musculoskeletal disease or impairment, resistance training experience within the previous 12 months, the inability to commit to a period of time equivalent to the duration of the study |
| Interventions | 1. High‐velocity training group (n = 23). High‐velocity varied resistance exercises 2. Strength training group (n = 22). Constant resistance exercises 3. Control group (n = 22). Non‐training group Participants in the exercise interventions trained twice weekly for 24 weeks |
| Outcomes | Balance confidence (ABC); physical activity (PASE). Measured at baseline and post intervention |
| Notes | All participants were invited to attend 2 familiarisation sessions, during which exercise techniques were demonstrated and practised, before baseline assessments and randomisation |
Jorgensen 2013.
| Methods | RCT |
| Participants | Country: Denmark n = 58 69% female Mean age in years (SD) = 75 (6) Study population: recruited through advertisements in local newspapers, senior citizens' clubs, and senior society organisations Inclusion criteria: ≥ 65, self reported balance poor to average (on a discrete scale: good, average, poor), capability of understanding verbal instructions Exclusion criteria: orthopaedic surgery within the previous 6 months, acute illness within the previous 3 weeks, physiotherapy within the previous month, poor visual acuity (not capable of seeing the visual features on the TV screen) |
| Interventions | 1. Exercise group (n = 28). Biofeedback‐based Nintendo Wii training for 35 (SD 5) minutes, twice weekly, for 10 weeks 2. Control group (n = 30). Daily use of ethylene vinyl acetate copolymer shoe insoles for 10 weeks. Participants were explicitly informed that the use of insoles was expected to increase sensory inputs from the feet to the central nervous system, resulting in an improved postural balance |
| Outcomes | Concern about falling (short FES‐I). Measured at baseline and post intervention |
| Notes | Study record reported at ‐ NCT01371253. 10 weeks of Nintendo Wii Fit balance training improved postural balance and muscle strength in elderly individuals. http://clinicaltrials.gov/show/NCT01371253 (accessed 1 August 2013) |
Kim 2009b.
| Methods | RCT |
| Participants | Country: USA n = 24 92% female Mean age in years (SD) = 72.5 (6.8) in balance training group, 72.0 (5.5) in weight training group, 76.5 (8.3) in control Study population: recruited from the local community via advertisements Inclusion criteria: older adults, no history of the formal weight and balance exercises in the past 6 months, current exercises (such as walking, running, swimming, dancing, gardening, tennis and golf) do not particularly target weight lifting and balance control, current exercises that target improved muscle strength and balance do not exceed more than 30 minutes a week in total Exclusion criteria: physical problems (i.e. hip, knee, ankle problems) |
| Interventions | 1. Balance training group (n = 6) 2. Weight training group (n = 6) 3. Control group (n = 6). Social activities (picnics, bingo, shopping and park visits). Activities that required physical performance were not included in the control group activities, except for walking The groups met for 50 to 60 minutes, 3 times weekly, for 8 weeks |
| Outcomes | Fear of falling (on a scale from 1 to 10 (10 being high)). Measured at baseline and post intervention |
| Notes | 24 participants randomised, but 5 withdrew and 1 participant's data were eliminated because his physical abilities were exceptionally superior to the other participants' physical abilities. Number of participants randomised to each group before the withdrawals and data elimination not reported |
Morris 2008.
| Methods | RCT |
| Participants | Country: USA n = 26 100% female Mean age in years (SD) = 76.1 (6.4) Study population: recruited from among the current users of any of the activities sponsored by a hospital supported senior wellness programme Inclusion criteria: willingness to participate after full understanding of the elements and risks involved, completion of a health history form and a signed informed consent form Exclusion criteria: advanced osteoporosis, hip replacement, glaucoma, Parkinson's disease, common occurrences of dizziness, any surgery within the past year |
| Interventions | 1. Group‐based yoga exercises (n = 10) 2. Group‐based balance training exercises (n = 10) 3. Control group (n = 6). Fall risk awareness group. Topics included "exercise" and "walking/healthy feet" All groups met for 1 hour, twice weekly, for 8 weeks |
| Outcomes | Falls efficacy (FES); balance confidence (ABC). Measured at baseline, every other week, post intervention and at 1 month follow‐up. Adherence to exercise interventions measured by class attendance |
| Notes | — |
Wolf 2003.
| Methods | RCT |
| Participants | Country: USA n = 311 94% female Mean age in years (SD) = 80.9 (6.6) for Tai Chi group, 80.8 (5.8) for wellness education group Study population: recruited from congregate living facilities Inclusion criteria: ≥ 70, transitioning to frailty, fallen at least once in the past year Exclusion criteria: major unstable cardiopulmonary diseases (ischaemic chest pain, unaccustomed shortness of breath, shortness of breath with mild exertion, recurrent syncopal episodes, orthopnoea, paroxysmal nocturnal dyspnoea, palpitations, tachycardia, claudication or severe pitting ankle oedema), cognitive impairment defined as a Mini‐Mental State Examination (MMSE) score of less than 24, contraindications to physical exercise, such as major orthopaedic conditions (e.g. severe lumbar spine, hip, knee, or ankle arthritis that limits exercise capability), restricted to a wheelchair; terminal cancer; or evidence of any other progressive or unstable neurological or medical condition |
| Interventions | 1. Exercise group (n = 158). Group‐based Tai Chi, for 60 to 90 minutes, twice weekly, for 48 weeks 2. Control group (n = 153). Wellness education programme for 1 hour, weekly, for 48 weeks. Topics included "exercise and balance" |
| Outcomes | Falls efficacy (FES); balance confidence (ABC); depression (CES‐D). Measured at baseline and every 4 months for 12 months during a 48‐week intervention. Number of falls (recorded by weekly forms). Adherence to exercise intervention measured by class attendance |
| Notes | Fear of falling sub‐study reported at ‐ Sattin R, Easley K, Wolf S, Chen Y, Kutner M. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. Journal of American Geriatrics Society 2005;53:1168‐78 |
ABC: Activities‐specific Balance Confidence scale CES‐D: Center for Epidemiologic Studies ‐ Depression scale FES: Falls Efficacy Scale FES‐I: FES‐International RCT: randomised controlled trial SD: standard deviation
Characteristics of ongoing studies [ordered by study ID]
Iliffe 2010b.
| Trial name or title | Multicentre cluster‐randomised trial comparing a community group exercise programme with home based exercise with usual care for over 65s in primary care |
| Methods | Cluster‐RCT |
| Participants | N = 1200 Setting: UK Inclusion criteria: community‐dwelling older adults aged 65 and over, able to walk around independently indoors and outdoors (with or without a walking aid) and not undergoing long term physiotherapy Exclusion criteria: 3 or more falls in the previous year ("frequent fallers"), resting BP > 180/100 mm Hg, uncontrolled arrhythmia, critical aortic stenosis, very severe vestibular disturbances, psychiatric conditions, significant cognitive impairment (unable to follow simple instructions), acute medical problems such as pneumonia or acute rheumatoid arthritis, hip/knee replacement in past 3 months, stroke/transient ischaemic attacks in the last 6 months or not living independently (e.g. residential or nursing care) |
| Interventions | 1. Home‐based exercise programme (n = 400). Otago Exercise Programme (OEP) consists of 30‐minute leg muscle strengthening and balance retraining exercises progressing in difficulty performed at least 3 times per week, for 24 weeks. Participants also advised to walk at least twice per week for up to 30 minutes at a moderate pace 2. Community‐based exercise programme (FaME) (n = 400). 1‐hour group exercise class in a local community centre, and 2 30‐minute home exercise sessions (based on the OEP) per week, for 24 weeks. Participants also advised to walk at least twice per week for up to 30 minutes at a moderate pace 3. Treatment as usual (TAU). No intervention |
| Outcomes | Number and type of falls (fall diary); fear of falling (FES‐I); balance confidence (ConfBal); quality of life (Older People's QOL Questionnaire (OPQOL); SF‐12); economic analysis |
| Starting date | June 2008 |
| Contact information | Prof Steve Iliffe Department of Primary Care & Population Health University College London Rowland Hill Street London NW3 2PF United Kingdom |
| Notes | Recruitment completed. Study end date May 2013 |
NCT01032252.
| Trial name or title | Prevention of falls in community‐dwelling older adults by a standardized assessment of fall risks in the general practitioner setting and through implementation of a network for effective individual reduction on fall risks |
| Methods | RCT |
| Participants | N = 378 Setting: Germany Inclusion criteria: community‐dwelling adults aged 65 years and older with an increased risk of falling, as seen by history of falls, fear of falling, chair rise > 10 seconds, TUG > 10 seconds and subjective and objective balance deficits Exclusion criteria: older people not living independently, or suffering from physical or mental restrictions that do not allow the participation in an exercise programme or the assessment of risk of falling |
| Interventions | 1. Exercise group. 16‐week exercise programme performed once a week for 60 minutes. Exercises include strength/power training, balance/gait training, behavioural aspects, perceptual and functional training 2. Control group. No intervention |
| Outcomes | Number of falls and falls rates (fall diary); fear of falling (FES‐I); quality of life (EuroQol) |
| Starting date | April 2009 |
| Contact information | Dr Monika Siegrist Department of Medicine Division of Prevention and Sports Medicine Technische Universität Munich 80809 Germany |
| Notes | Study has been completed March 2012. Data expected to be published spring or summer 2013 (as per email from Chief Investigator received January 2013) |
BP: blood pressure RCT: randomised controlled trial TUG: Timed Up and Go
Differences between protocol and review
We made substantial edits to the Background.
To improve clarity, we changed the terminology for the overall intervention to "exercise interventions" from "prescribed or provided exercise" as described in the protocol.
In the primary outcomes section, we subdivided 'falls efficacy' into two categories ('falls efficacy' and 'concern about falling') because some falls efficacy scales (e.g. FES‐I, amFES, Modified Efficacy Scale) measure "concern" or "worry" (e.g. SAFFE) about falling as opposed to falls efficacy.
Since physical activity can be regarded as a measure of compliance or adherence to exercise interventions, we reported on this.
We did not undertake a subgroup analysis for age group based on a cut‐off of 75 years. This was because only two studies restricted recruitment to participants aged 75 years and over and the remaining studies included participants aged 75 and over; hence it was not possible to identify distinct age groups for a subgroup analysis. We also did not undertake a subgroup analysis for baseline fear of falling. This was because only two studies specified a fear of falling as an inclusion criterion, in both cases the criterion was a history of falls or fear of falling, and baseline fear of falling scores appeared similar to studies that did not have fear of falling as an inclusion criterion. One study included concern about falling as an inclusion criterion, but the prevalence of this appeared similar to studies not specifying this as an inclusion criteria. Therefore it was not possible to identify distinct groups based on fear of falling for a subgroup analysis. In addition, the protocol stated we would use sensitivity analyses to explore the effect of the primary aim of the study (to reduce fear of falling or other primary aim). We undertook a subgroup analysis instead of a sensitivity analysis, as we considered this more appropriate for this purpose.
We undertook a sensitivity analysis for fear of falling excluding the data from Nguyen 2012, as this study had a much larger effect size than other studies included in the meta‐analysis. We also undertook sensitivity analyses using the upper and lower 95% CI for intra class correlation coefficients where we adjusted studies for clustering. Two studies measured fear of falling using both the FES and ABC. We used FES scores in the main analysis and undertook a sensitivity analysis replacing FES scores with ABC scores for these two studies.
Contributions of authors
DK had the initial idea for undertaking the review, drafted the protocol, supervised the conduct of the review, adjudicated on papers for inclusion, data extraction and 'Risk of bias' assessment, supervised analyses, interpreted data, contributed to drafting the review and is the guarantor of the review. AK supervised the review team, co‐ordinated and assisted with data extraction, database management, assessment of papers, data extraction and meta‐analyses and led the drafting of the review. HC helped draft the protocol, assisted with data extraction, assessment of papers and drafting of the review. JRC, ZS, DH, CB, SG, HG, TM, DS, AB and MP assisted with the data extraction and assessment of papers and checked reference lists for additional studies. RM contributed to drafting the protocol, provided statistical advice and interpreted data. SI contributed to drafting the protocol, adjudicated on papers for inclusion, data extraction and 'Risk of bias' assessment and interpreted data. RZ contributed to developing the search strategy, screened papers for inclusion, organised retrieval of papers, checked data extraction and 'Risk of bias' assessment of papers and interpreted data. KD assisted with organising retrieval of papers, identified potential unidentified studies as an expert consultant, undertook data extraction and assessment of papers and checked reference lists for additional studies. All authors contributed to drafting the review by critically reviewing for intellectual content.
Sources of support
Internal sources
-
University of Nottingham, UK.
Salary support for DK, BS, HC, AK and library resources
-
University College London, UK.
Salary support for SI, RM, CB, MP, SG, ZS
-
Glasgow Caledonian University, UK.
Salary support for DS
-
University of Surrey, UK.
Salary support for HG
-
St George's, University of London, UK.
Salary support for AB
-
Nottingham University Hospitals NHS Trust, UK.
Salary support for TM
External sources
No sources of support supplied
Declarations of interest
Several co‐authors of this review are involved in the NIHR HTA‐funded PROACT65+ study (Iliffe 2010a). The study is a multicentre cluster‐randomised trial comparing a community group exercise programme with home‐based exercise with usual care to increase physical activity for people aged 65 and over in primary care. The trial may be included in future versions of the review.
Denise Kendrick: coinvestigator on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Arun Kumar: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Hannah Carpenter: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) G A Rixt Zijlstra: none known Dawn A Skelton: coinvestigator on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a). Director of Later Life Training, a not‐for‐profit training organisation that provides evidence‐based training for physiotherapists and exercise instructors working with frailer older people Juliette R Cook: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Zoe Stevens: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Carolyn M Belcher: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Deborah Haworth: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Sheena J Gawler: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Heather Gage: coinvestigator on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Tahir Masud: coinvestigator on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Ann Bowling: coinvestigator on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Mirilee Pearl: researcher on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a). Teacher of Tai Chi and exercise for older people, and Director of Fitness for a Certain Age. Richard W Morris: senior statistician on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Steve Iliffe: principal investigator on NIHR HTA‐funded PROACT65+ study (Iliffe 2010a) Kim Delbaere: none known
Edited (no change to conclusions)
References
References to studies included in this review
Barnett 2003 {published data only}
- Barnett A, Smith B, Lord SR. Community‐based group exercise improves balance and reduces falls in at‐risk older people. Age and Ageing 2003;32(4):407‐14. [DOI] [PubMed] [Google Scholar]
Campbell 1997 {published data only}
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age and Ageing 1999;28:513‐8. [DOI] [PubMed] [Google Scholar]
- Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997;315:1065‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise‐based falls prevention programme. Age and Ageing 2001;30(1):77‐83. [DOI] [PubMed] [Google Scholar]
- Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta‐analysis of individual‐level data. Journal of the American Geriatrics Society 2002;50:905‐11. [DOI] [PubMed] [Google Scholar]
- Robertson MC, Devlin N, Scuffham P, Gardner MM, Buchner DM, Campbell AJ. Economic evaluation of a community based exercise programme to prevent falls. Journal of Epidemiology and Community Health 2001;55(8):600‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clemson 2010 {published and unpublished data}
- Clemson L. MFES and ABC data [personal communication]. Email to: A Kumar 21 March 2013.
- Clemson L, Singh MF, Bundy A, Cumming RG, Weissel E, Munro J, et al. LiFE Pilot Study: a randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. Australian Occupational Therapy Journal 2010;57(1):42‐50. [DOI] [PubMed] [Google Scholar]
Freiberger 2012 {published data only}
- Freiberger E, Haberle L, Spirduso WW, Rixt Zijlstra GA. Long‐term effects of three multicomponent exercise interventions on physical performance and fall‐related psychological outcomes in community‐dwelling older adults: a randomized controlled trial. Journal of the American Geriatrics Society 2012;60(3):437‐46. [DOI] [PubMed] [Google Scholar]
- Freiberger E, Menz HB, Abu‐Omar K, Rutten A. Preventing falls in physically active community‐dwelling older people: a comparison of two intervention techniques. Gerontology 2007;53(5):298‐305. [DOI] [PubMed] [Google Scholar]
Haines 2009 {published data only}
- ACTRN12607000180415. Assessment and prevention of falls, functional decline and hospital re‐admission in older adults post‐hospitalisation. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=81910 (accessed 30 September 2014).
- Haines TP, Russell T, Brauer SG, Erwin S, Lane P, Urry S, et al. Effectiveness of a video‐based exercise programme to reduce falls and improve health‐related quality of life among older adults discharged from hospital: a pilot randomized controlled trial. Clinical Rehabilitation 2009;23(11):973‐85. [DOI] [PubMed] [Google Scholar]
Halvarsson 2011 {published and unpublished data}
- Halvarsson A. FES‐I and GDS‐20 data [Personal communication]. Email to: A Kumar 31 March 2013.
- Halvarsson A, Oddsson L, Olsson E, Farén E, Pettersson A, Ståhle A. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: a randomized controlled trial. Clinical Rehabilitation 2011;25(11):1021‐31. [DOI] [PubMed] [Google Scholar]
Hinman 2002 {published data only}
- Hinman MR. Comparison of two short‐term balance training programs for community‐dwelling older adults. Journal of Geriatric Physical Therapy 2002;25(3):10‐5. [Google Scholar]
Karinkanta 2012 {published data only}
- Karinkanta S, Nupponen R, Heinonen A, Pasanen M, Sievänen H, Uusi‐Rasi K, et al. Effects of exercise on health‐related quality of life and fear of falling in home‐dwelling older women. Journal of Aging & Physical Activity 2012;20(2):198‐214. [DOI] [PubMed] [Google Scholar]
Lai 2013 {published data only}
- Lai C, Peng C, Chen Y, Huang CP, Hsiao YL, Chen SC. Effects of interactive video‐game based system exercise on the balance of the elderly. Gait and Posture 2013;37(4):511‐5. [DOI] [PubMed] [Google Scholar]
Lajoie 2004 {published and unpublished data}
- Lajoie 2004. ABC data [personal communication]. Email to: A Kumar 08 March 2013.
- Lajoie Y. Effect of computerized feedback postural training on posture and attentional demands in older adults. Aging Clinical and Experimental Research 2004;16(5):363‐8. [DOI] [PubMed] [Google Scholar]
Lin 2007 {published data only}
- Lin M, Wolf SL, Hwang H, Gong S, Chen C. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. Journal of the American Geriatrics Society 2007;55(4):499‐506. [DOI] [PubMed] [Google Scholar]
- Lin MR, Hwang H, Wang Y, Chang S, Wolf SL. Community‐based tai chi and its effect on injurious falls, balance, gait, and fear of falling in older people. Physical Therapy 2006;86(9):1189‐201. [DOI] [PubMed] [Google Scholar]
Logghe 2009 {published data only}
- ISRCTN98840266. Fall prevention in the elderly ‐ a randomized clinical trial on the effectiveness of Tai Chi Chuan. http://www.controlled‐trials.com/ISRCTN98840266 (accessed 1 August 2013).
- Logghe IH, Verhagen AP, Rademaker AC, Bierma‐Zeinstra SM, Rossum E, Faber MJ, et al. The effects of Tai Chi on fall prevention, fear of falling and balance in older people: a meta‐analysis. Preventive Medicine: An International Journal Devoted to Practice and Theory 2010;51:222‐7. [DOI] [PubMed] [Google Scholar]
- Logghe IH, Verhagen AP, Rademaker AC, Zeeuwe PE, Bierma‐Zeinstra SM, Rossum E, et al. Explaining the ineffectiveness of a Tai Chi fall prevention training for community‐living older people: a process evaluation alongside a randomized clinical trial (RCT). Archives of Gerontology & Geriatrics 2011;52(3):357‐62. [DOI] [PubMed] [Google Scholar]
- Logghe IHJ, Zeeuwe PEM, Verhagen AP, Wijnen‐Sponselee RMT, Willemsen SP, Bierma‐Zeinstra SMA, et al. Lack of effect of Tai Chi Chuan in preventing falls in elderly people living at home: a randomized clinical trial. Journal of the American Geriatrics Society 2009;57(1):70‐5. [DOI] [PubMed] [Google Scholar]
- Zeeuwe PEM, Verhagen AP, Bierma‐Zeinstra SMA, Rossum E, Faber MJ, Koes BW. The effect of Tai Chi Chuan in reducing falls among elderly people: design of a randomized clinical trial in the Netherlands [ISRCTN98840266]. BMC Geriatrics 2006;6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCormack 2004 {published and unpublished data}
- McCormack G. Data on the number of female participants [personal communication]. Email to: A Kumar 12 February 2013.
- McCormack G, Lewin G, McCormack B, Helmes E, Rose E, Naumann F. Pilot study comparing the influence of different types of exercise intervention on the fear of falling in older adults. Australasian Journal of Ageing 2004;23(3):131‐5. [Google Scholar]
Nguyen 2012 {published data only}
- Nguyen MH, Kruse A. A randomized controlled trial of Tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clinical Interventions in Aging 2012;7:185‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinsch 1992 {published data only}
- MacRae PG, Feltner ME, Reinsch S. A 1‐year exercise program for older women: effects on falls, injuries, and physical performance. Journal of Aging and Physical Activity 1994;2:127‐42. [Google Scholar]
- Reinsch S, MacRae P, Lachenbruch PA, Tobis JS. Attempts to prevent falls and injury: a prospective community study. Gerontologist 1992;32:450‐6. [DOI] [PubMed] [Google Scholar]
Rendon 2012 {published data only}
- Rendon A, Lohman E, Thorpe D, Johnson EG, Medina E, Bradley B. The effect of virtual reality gaming on dynamic balance in older adults. Age and Ageing 2012;41(4):549‐52. [DOI] [PubMed] [Google Scholar]
Resnick 2008 {published data only}
- Resnick B, Luisi D, Vogel A. Testing the Senior Exercise Self‐efficacy Project (SESEP) for use with urban dwelling minority older adults. Public Health Nursing 2008;25(3):221‐34. [DOI] [PubMed] [Google Scholar]
Sihvonen 2004 {published data only}
- Sihvonen S, Sipilä S, Taskinen S, Era P. Fall incidence in frail older women after individualized visual feedback‐based balance training. Gerontology 2004;50(6):411‐6. [DOI] [PubMed] [Google Scholar]
- Sihvonen SE, Sipilä S, Era PA. Changes in postural balance in frail elderly women during a 4‐week visual feedback training: a randomized controlled trial. Gerontology 2004;50(2):87‐95. [DOI] [PubMed] [Google Scholar]
Tiedemann 2012 {published data only}
- Tiedemann A, O'Rourke S, Sesto R, Sherrington C. A 12‐week Iyengar yoga program improved balance and mobility in older community‐dwelling people: a pilot randomized controlled trial. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2013;68(9):1068‐75. [DOI] [PubMed] [Google Scholar]
- Tiedemann A, Sherrington C, O'Rourke S. Can yoga improve balance in older people?: A randomised controlled trial. Journal of Science and Medicine in Sport 2012;15(Suppl 1):S292. [Google Scholar]
Ullmann 2010 {published and unpublished data}
- Ullman G. FES and ABC data [personal communication]. Email to: A Kumar 20 February 2013.
- Ullmann G. The Efficacy of Feldenkrais in Improving Balance, Mobility and Health Related Factors in an Older Adult Population [Thesis]. South Carolina: University of South Carolina, 2008. [Google Scholar]
- Ullmann G, Williams HG, Hussey J, Durstine JL, McClenaghan BA. Effects of Feldenkrais exercises on balance, mobility, balance confidence, and gait performance in community‐dwelling adults age 65 and older. Journal of Alternative & Complementary Medicine 2010;16(1):97‐105. [DOI] [PubMed] [Google Scholar]
Vogler 2009 {published and unpublished data}
- ACTRN12605000335695. Reducing falls risk in older people discharged from hospital: a randomised controlled trial comparing (i) seated lower limb resistance training, (ii) functional weight‐bearing training and (iii) social visits (control activity). https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12605000335695 (accessed 12 October 2014).
- Vogler C, Sherrington C, Ogle S, Lord S. Reducing risk of falling in older people discharged from hospital: a randomised controlled trial comparing seated lower limb strength training, weight‐bearing exercises and social visits [abstract]. Internal Medicine Journal 2008;38(Suppl 5):A127. [DOI] [PubMed] [Google Scholar]
- Vogler CM. MFES and GDS data [personal communication]. Email to: A Kumar 25 February 2013.
- Vogler CM, Sherrington C, Ogle SJ, Lord SR. Reducing risk of falling in older people discharged from hospital: a randomized controlled trial comparing seated exercises, weight‐bearing exercises, and social visits. Archives of Physical Medicine & Rehabilitation 2009;90(8):1317‐24. [DOI] [PubMed] [Google Scholar]
Vrantsidis 2009 {published and unpublished data}
- Vrantsidis F. Information about care provided at low‐care facility [personal communication]. Email to: A Kumar 10 February 2013.
- Vrantsidis F, Hill KD, Moore K, Webb R, Hunt S, Dowson L. Getting Grounded Gracefully: effectiveness and acceptability of Feldenkrais in improving balance. Journal of Aging and Physical Activity 2009;17(1):57‐76. [DOI] [PubMed] [Google Scholar]
Wallsten 2006 {published and unpublished data}
- Wallsten SM. ABC data [personal communication]. Email to: A Kumar 22 March 2013.
- Wallsten SM, Bintrim K, Denman DW, Parrish JM, Hughes G. The effect of Tai Chi Chuan on confidence and lower extremity strength and balance in residents living independently at a continuing care retirement community. Journal of Applied Gerontology 2006;25(1):82‐95. [Google Scholar]
Weerdesteyn 2006 {published and unpublished data}
- Weerdesteyn V. ABC data [personal communication]. Email to: A Kumar 15 March 2013.
- Weerdesteyn V, Rijken H, Geurts AC, Smits‐Engelsman BC, Mulder T, Duysens J. A five‐week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology 2006;52(3):131‐41. [DOI] [PubMed] [Google Scholar]
Westlake 2007 {published and unpublished data}
- Westlake K. Information about control group treatment [personal communication]. Email to: A Kumar 1 February 2013.
- Westlake KP, Culham EG. Sensory‐specific balance training in older adults: effect on proprioceptive reintegration and cognitive demands. Physical Therapy 2007;87(10):1274‐83. [DOI] [PubMed] [Google Scholar]
Wolf 1996 {published data only}
- Kutner NG, Barnhart H, Wolf SL, McNeely E, Xu T. Self‐report benefits of Tai Chi practice by older adults. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 1997;52(5):242‐6. [DOI] [PubMed] [Google Scholar]
- McNeely E, Clements SD, Wolf SL. A program to reduce frailty in the elderly. In: Funk SG, Tornquist EM, Champagne MT, Weise RA editor(s). Key Aspects of Eldercare: Managing Falls, Incontinence, and Cognitive Impairment. New York: Springer, 1992:89‐96. [Google Scholar]
- O'Grady M, Wolf SL, Barnhart HX, Kutner N, McNeely E. Tai Chi effect on falls in frail older adults [abstract]. Archives of Physical Medicine and Rehabilitation 1997;78:1028. [Google Scholar]
- Wolf SL, Barnhart HX, Ellison GL, Coogler CE. The effect of Tai Chi Quan and computerized balance training on postural stability in older subjects. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies on Intervention Techniques. Physical Therapy 1997;77(4):371‐81. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. Journal of the American Geriatrics Society 1996;44(5):489‐97. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Selected as the best paper in the 1990s: reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training (commentary by Lavery LL and Studenski SA. Reprinted from JAGS 1996 page 1794). Journal of the American Geriatrics Society 2003;51:1794‐805. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Kutner NG, Green RC, McNeely E. The Atlanta FICSIT study: two exercise interventions to reduce frailty in elders. Journal of the American Geriatrics Society 1993;41(3):329‐32. [DOI] [PubMed] [Google Scholar]
Wolf 2001 {published data only}
- Wolf B, Feys H, De Weerdt, van der Meer J, Noom M, Aufdemkampe G, et al. Effect of a physical therapeutic intervention for balance problems in the elderly: a single‐blind, randomized, controlled multicentre trial. Clinical Rehabilitation 2001;15(6):624‐36. [DOI] [PubMed] [Google Scholar]
Yang 2012 {published data only}
- Yang XJ, Hill K, Moore K, Williams S, Dowson L, Borschmann K, et al. Effectiveness of a targeted exercise intervention in reversing older people's mild balance dysfunction: a randomized controlled trial. Physical Therapy 2012;92(1):24‐37. [DOI] [PubMed] [Google Scholar]
Yoo 2010 {published data only}
- Yoo EJ, Jun TW, Hawkins SA. The effects of a walking exercise program on fall‐related fitness, bone metabolism, and fall‐related psychological factors in elderly women. Research in Sports Medicine 2010;18(4):236‐50. [DOI] [PubMed] [Google Scholar]
Zhang 2006 {published data only}
- Zhang JG, Ishikawa‐Takata K, Yamazaki H, Morita T, Ohta T. The effects of Tai Chi Chuan on physiological function and fear of falling in the less robust elderly: an intervention study for preventing falls. Archives of Gerontology & Geriatrics 2006;42(2):107‐16. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bainbridge 2011 {published data only}
- Bainbridge E, Bevans S, Keeley B, Oriel K. The effects of the Nintendo Wii fit on community‐dwelling older adults with perceived balance deficits: a pilot study. Physical & Occupational Therapy in Geriatrics 2011;29(2):126‐35. [Google Scholar]
Ballard 2004 {published data only}
- Ballard JE, McFarland C, Wallace LS, Holiday DB, Roberson G. The effect of 15 weeks of exercise on balance, leg strength, and reduction in falls in 40 women aged 65 to 89 years. Journal of the American Medical Women's Association 2004;59(4):255‐61. [PubMed] [Google Scholar]
Banez 2008 {published data only}
- Banez C, Tully S, Amaral L, Kwan D, Kung A, Mak K, et al. Development, implementation, and evaluation of an interprofessional falls prevention program for older adults. Journal of the American Geriatrics Society 2002;56(8):1549‐55. [DOI] [PubMed] [Google Scholar]
Batson 2006 {published data only}
- Batson G, Feltman R, McBride C, Waring J. Effect of mental practice combined with physical practice on balance in the community‐dwelling elderly. Activities, Adaptation & Aging 2006;31(2):1‐18. [Google Scholar]
Bean 2002 {published data only}
- Bean J, Herman S, Kiely DK, Callahan D, Mizer K, Frontera WR, et al. Weighted stair climbing in mobility‐limited older people: a pilot study. Journal of the American Geriatrics Society 2002;50(4):663‐70. [DOI] [PubMed] [Google Scholar]
Beyer 2007 {published data only}
- Beyer N, Simonsen L, Bulow J, Lorenzen T, Jensen DV, Larsen L, et al. Old women with a recent fall history show improved muscle strength and function sustained for six months after finishing training. Aging Clinical and Experimental Research 2007;19:300‐9. [DOI] [PubMed] [Google Scholar]
Bishop 2007 {published data only}
- Bishop MD, Meuleman J, Robinson M, Light KE. Influence of pain and depression on fear of falling, mobility, and balance in older male veterans. Journal of Rehabilitation Research & Development 2007;44(5):675‐84. [DOI] [PubMed] [Google Scholar]
Bishop 2010 {published data only}
- Bishop MD, Patterson TS, Romero S, Light KE. Improved fall‐related efficacy in older adults related to changes in dynamic gait ability. Physical Therapy 2010;90(11):1598‐606. [DOI] [PubMed] [Google Scholar]
Bula 2011a {published data only}
- Bula C, Monod S, Hoskovec C, Rochat S. Interventions aiming at balance confidence improvement in older adults: an updated review. Gerontology 2011;57(3):276‐86. [DOI] [PubMed] [Google Scholar]
Bunout 2005 {published data only}
- Bunout D, Barrera G, Avendano M, Maza P, Gattas V, Leiva L, et al. Results of a community‐based weight‐bearing resistance training programme for healthy Chilean elderly subjects. Age and Ageing 2005;34(1):80‐3. [DOI] [PubMed] [Google Scholar]
Chang 2007 {published data only}
- Chang Shuo‐Hsiu J. Improving Lateral Stability in Older Adults at Risk of Falls. North Carolina, USA: University of North Carolina, 2007. [Google Scholar]
Conroy 2010 {published data only}
- Conroy S, Kendrick D, Harwood R, Gladman J, Coupland C, Sach T, et al. A multicentre randomised controlled trial of day hospital‐based falls prevention programme for a screened population of community‐dwelling older people at high risk of falls. Age and Ageing 2010;39(6):704‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2011 {published data only}
- Davis J, Marra C, Liu‐Ambrose T. Falls‐related self‐efficacy is independently associated with quality‐adjusted life years in older women. Age and Ageing 2011;40(3):340‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davison 2005 {published data only}
- Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending accident & emergency benefit from multifactorial intervention ‐‐ a randomised controlled trial. Age and Ageing 2005;34(2):162‐8. [DOI] [PubMed] [Google Scholar]
Delbaere 2006 {published data only}
- Delbaere K, Bourgois J, Noortgate N, Vanderstraeten G, Willems T, Cambier D. A home‐based multidimensional exercise program reduced physical impairment and fear of falling. Acta Clinica Belgica 2006;61(6):340‐50. [DOI] [PubMed] [Google Scholar]
Devereux 2005 {published data only}
- Devereux K, Robertson D, Briffa NK. Effects of a water‐based program on women 65 years and over: a randomised controlled trial. Australian Journal of Physiotherapy 2005;51(2):102‐8. [DOI] [PubMed] [Google Scholar]
Duque 2013 {published data only}
- Duque G, Boersma D, Loza‐Diaz G, Hassan S, Suarez H, Geisinger D, et al. Effects of balance training using a virtual‐reality system in older fallers. Clinical Interventions in Aging 2013;8:257‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elley 2003 {published data only}
- Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 2003;326(7393):793‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elley 2008 {published data only}
- Elley C, Robertson M, Garrett S, Kerse NM, McKinlay E, Lawton B, et al. Effectiveness of a falls‐and‐fracture nurse coordinator to reduce falls: a randomized, controlled trial of at‐risk older adults. Journal of the American Geriatrics Society 56;8:1383‐9. [DOI] [PubMed] [Google Scholar]
Faber 2006 {published data only}
- Faber MJ, Bosscher RJ, Chin A Paw MJ, Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre‐frail older adults: a multicenter randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2006;87(7):885‐96. [DOI] [PubMed] [Google Scholar]
Faes 2011 {published data only}
- Faes M, Reelick M, Melis R, Borm G, Esselink RG. Multifactorial fall prevention for pairs of frail community‐dwelling older fallers and their informal caregivers: a dead end for complex interventions in the frailest fallers. Journal of the American Medical Directors Association 2011;12(6):451‐8. [DOI] [PubMed] [Google Scholar]
- NCT00512655. Trial to reduce falls incidence rate in frail elderly. http://clinicaltrials.gov/show/NCT00512655 (accessed 1 August 2013).
Foley 2009 {published data only}
- Foley A, Hillier S, Barnard R. Evaluation of a geriatric day rehabilitation centre: subjective and objective outcomes in community‐dwelling older adults. Australian Journal of Primary Health 2009;15(2):117‐22. [Google Scholar]
Gillespie 2012 {published data only}
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD007146.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gitlin 2006 {published data only}
- Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. Journal of the American Geriatrics Society 2006;54(5):809‐16. [DOI] [PubMed] [Google Scholar]
- NCT00249925. Project ABLE: Advancing Better Living for Elders. http://clinicaltrials.gov/show/NCT00249925 (accessed 1 August 2013).
Greendale 2009 {published data only}
- Greendale GA, Huang M, Karlamangla AS, Seeger L, Crawford S. Yoga decreases kyphosis in senior women and men with adult‐onset hyperkyphosis: results of a randomized controlled trial. Journal of the American Geriatrics Society 2009;57(9):1569‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hagedorn 2010 {published data only}
- Hagedorn DK, Holm E. Effects of traditional physical training and visual computer feedback training in frail elderly patients. A randomized intervention study. European Journal of Physical and Rehabilitation Medicine 2010;46(2):159‐68. [PubMed] [Google Scholar]
Hakim 2003 {published data only}
- Hakim RM, Newton RA, Segal J, DuCette JP. A group intervention to reduce fall risk factors in community‐dwelling older adults. Physical & Occupational Therapy in Geriatrics 2010;22(1):1‐20. [Google Scholar]
Hakim 2004 {published data only}
- Balzano JM, Burke JL, Hoy TW, Roberts EM, Hakim R. A comparative study of balance measures among elderly persons participating in Tai Chi or structured exercise programs. Journal of Geriatric Physical Therapy 2002;25(3):44‐5. [Google Scholar]
- Hakim RM, DiCicco J, Burke J, Hoy T, Roberts E. Differences in balance related measures among older adults participating in Tai Chi, structured exercise, or no exercise. Journal of Geriatric Physical Therapy 2004;27(1):11‐5. [Google Scholar]
Hakim 2010 {published data only}
- Cissel E, Cours J, Teel S, Hakim R. A cross‐sectional study of balance‐related measures with older adults who participate in Tai Chi, Yoga, or no exercise. Journal of Geriatric Physical Therapy 2005;28(3):119‐20. [Google Scholar]
- Hakim RM, Kotroba E, Cours J, Teel S, Leininger PM. A cross‐sectional study of balance‐related measures with older adults who participated in Tai Chi, yoga, or no exercise. Physical & Occupational Therapy in Geriatrics 2010;28(1):63‐74. [Google Scholar]
Harling 2008 {published data only}
- Harling A, Simpson JP. A systematic review to determine the effectiveness of Tai Chi in reducing falls and fear of falling in older adults. Physical Therapy Reviews 2008;13(4):237‐48. [Google Scholar]
Harmer 2008 {published data only}
- Harmer P, Li F. Tai Chi and falls prevention in older people. Medicine and Sports Science 2008;52:124‐34. [DOI] [PubMed] [Google Scholar]
Hartmann 2009 {published data only}
- Hartmann A, Murer K, Bie RA, Bruin ED. The effect of a foot gymnastic exercise programme on gait performance in older adults: a randomised controlled trial. Disability & Rehabilitation 2009;31(25):2101‐10. [DOI] [PubMed] [Google Scholar]
Hess 2005 {published data only}
- Hess JA. High Intensity Strength Training to Enhance Balance Control in Frail Older Adults [Thesis]. Oregon, USA: University of Oregon, 2004. [Google Scholar]
- Hess JA, Woollacott M. Effect of high‐intensity strength‐training on functional measures of balance ability in balance‐impaired older adults. Journal of Manipulative & Physiological Therapeutics 2005;28(8):582‐90. [DOI] [PubMed] [Google Scholar]
Hinrichs 2009 {published data only}
- Hinrichs T, Bucchi C, Brach M, Wilm S, Endres HG, Burghaus I, et al. Feasibility of a multidimensional home‐based exercise programme for the elderly with structured support given by the general practitioner's surgery: study protocol of a single arm trial preparing an RCT. BMC Geriatrics 2009;9:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 2011 {published data only}
- Huang TT, Yang LH, Liu CY. Reducing the fear of falling among community‐dwelling elderly adults through cognitive‐behavioural strategies and intense Tai Chi exercise: a randomized controlled trial. Journal of Advanced Nursing 2011;67(5):961‐71. [DOI] [PubMed] [Google Scholar]
Hugel 2000 {published data only}
- Hugel K, Sciandra T. The effects of a 12‐week Tai Chi program on thoracolumbar, hip, and knee flexion in adults 50 years and older. Issues on Aging 2000;23(3):15‐8. [Google Scholar]
Inokuchi 2007 {published data only}
- Inokuchi S, Matsusaka N, Hayashi T, Shindo H. Feasibility and effectiveness of a nurse‐led community exercise programme for prevention of falls among frail elderly people: a multi‐centre controlled trial. Journal of Rehabilitation Medicine 2007;39(6):479‐85. [DOI] [PubMed] [Google Scholar]
ISRCTN05350123 {published data only}
- ISRCTN05350123. The effects of computer game dancing on foot placement accuracy and gaze behavior in older adults: a randomized control trial. http://www.controlled‐trials.com/ISRCTN05350123 (accessed 1 August 2013).
ISRCTN05545178 {published data only}
- ISRCTN05545178. The use of a virtual reality video dance game for the training of motor control in elderly: a two‐groups pre‐test post‐test controlled experimental design. http://www.controlled‐trials.com/ISRCTN05545178 (accessed 1 August 2013).
ISRCTN21695765 {published data only}
- ISRCTN21695765. Cost‐effectiveness of a proprioceptive exercise program in institutionalised elderly with fear of falling: randomised controlled trial. http://www.controlled‐trials.com/ISRCTN21695765 (accessed 1 August 2013).
ISRCTN48015966 {published data only}
- ISRCTN48015966. The Chaos Clinic for prevention of falls and related injuries: a randomised, controlled trial. http://www.controlled‐trials.com/ISRCTN48015966 (accessed 1 August 2013).
ISRCTN67535605 {published data only}
- ISRCTN67535605. A randomised controlled trial to compare falls prevention rehabilitation for people who fall and call an emergency ambulance but who are not transported to hospital. http://www.controlled‐trials.com/ISRCTN67535605. UK, (accessed 1 August 2013).
ISRCTN75134517 {published data only}
- ISRCTN75134517. The effects of physical exercise training in combination with cognitive training on dual task costs of walking in elderly: a two‐groups pre‐test post‐test randomized controlled trial. http://www.controlled‐trials.com/ISRCTN75134517 (accessed 1 August 2013).
ISRCTN89512790 {published data only}
- ISRCTN89512790. Randomised controlled trial to test the effects of, respectively, health coaching and an integrative district nurse approach for preventing falls in elderly people living in the community. ISRCTN89512790 (accessed 1 August 2013).
Iwamoto 2009 {published data only}
- Iwamoto J, Suzuki H, Tanaka K, Kumakubo T, Hirabayashi H, Miyazaki Y, et al. Preventative effect of exercise against falls in the elderly: A randomized controlled trial. Osteoporosis International 2009;20(7):1233‐40. [DOI] [PubMed] [Google Scholar]
Jansson 2004 {published data only}
- Jansson S, Sunderlund A. A new treatment programme to improve balance in elderly people ‐‐ an evaluation of an individually tailored home‐based exercise programme in five elderly women with a feeling of unsteadiness. Disability & Rehabilitation 2004;26(24):1431‐43. [DOI] [PubMed] [Google Scholar]
Juarbe 2009 {published data only}
- Juarbe A, Bondoc S. Reducing fear of falling through guided imagery. Gerontology Special Interest Section Quarterly 2009;32(4):1‐4. [Google Scholar]
Jury 2009 {published data only}
- Jung D, Juhee L, Lee S. A meta‐analysis of fear of falling treatment programs for the elderly. Western Journal of Nursing Research 2009;31(1):6‐16. [DOI] [PubMed] [Google Scholar]
Kelsey 2010 {published data only}
- Kelsey JL, Berry SD, Procter‐Gray E, Quach L, Nguyen UDT, Li W, et al. Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. Journal of the American Geriatrics Society 2010;58(11):2135‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kemmler 2010 {published data only}
- Kemmler W, Stengel S, Engelke K, Haberle L, Kalender WA. Exercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: the randomized controlled senior fitness and prevention (SEFIP) study. Archives of Internal Medicine 2010;170(2):179‐85. [DOI] [PubMed] [Google Scholar]
Kerse 2010 {published data only}
- Kerse N, Hayman KJ, Moyes SA, Peri K, Robinson E, Dowell A, et al. Home‐based activity program for older people with depressive symptoms: DeLLITE‐‐A randomized controlled trial. Annals of Family Medicine 2010;8(3):214‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2009a {published data only}
- Kim BH. The effects of guided relaxation and exercise imagery on older adults with a fear of falling. Dissertation Abstracts International: Section B: The Sciences and Engineering 2009;70(6‐B):3771. [Google Scholar]
Kim 2011 {published data only}
- Kim H, Yoshida H, Suzuki T. The effects of multidimensional exercise on functional decline, urinary incontinence, and fear of falling in community‐dwelling elderly women with multiple symptoms of geriatric syndrome: a randomized controlled and 6‐month follow‐up trial. Archives of Gerontology & Geriatrics 2011;52(1):99‐105. [DOI] [PubMed] [Google Scholar]
Kuo 2011 {published data only}
- Kuo SL, Nitz NL. Effect of exercise intervention on balance and fear of falling in elderly subjects. Hong Kong Physiotherapy Journal 2011;29(2):96‐7. [Google Scholar]
Kuptniratsaikul 2011 {published data only}
- Kuptniratsaikul V, Praditsuwan R, Assantachai P, Ploypetch T, Udompunturak S, Pooliam J. Effectiveness of simple balancing training program in elderly patients with history of frequent falls. Clinical Interventions in Aging 2011;6:111‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuramoto 2006 {published data only}
- Kuramoto M. Therapeutic benefits of Tai Chi exercise: research review. Wisconsin Medical Journal 2006;105(7):42‐6. [PubMed] [Google Scholar]
Kwok 2011 {published data only}
- Kwok BC, Mamun K, Chandran M, Wong CH. Evaluation of the Frails' Fall Efficacy by Comparing Treatments (EFFECT) on reducing fall and fear of fall in moderately frail older adults: study protocol for a randomised control trial. Trials 2011;12:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kwon 2011 {published data only}
- Kwon MS. Effects of a fall prevention program on physical fitness and psychological functions in community dwelling elders. Journal of Korean Academic Nursing 2011;41:165‐74. [DOI] [PubMed] [Google Scholar]
Lee 2010 {published data only}
- Lee Y, Tabourne CES, Harris JE. Effects of Dancing Heart Program (DHP) as therapeutic recreation intervention on risk of falling among community dwelling elders. Annual in Therapeutic Recreation 2010;18:157‐63. [Google Scholar]
Leininger 2006 {published data only}
- Leininger P. Physical and Psychological Effects of Yoga Exercise on Healthy Community‐dwelling Older Adult Women. Philadelphia: Temple University, 2006. [Google Scholar]
Li 2005 {published data only}
- Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. Journals of Gerontology Series A: Biological Sciences & Medical Sciences 2005;60(2):187‐94. [DOI] [PubMed] [Google Scholar]
Li 2010 {published data only}
- Li KZH, Roudaia E, Lussier M, Bherer L, Leroux A, McKinley PA. Benefits of cognitive dual‐task training on balance performance in healthy older adults. Journals of Gerontology Series A: Biological Sciences & Medical Sciences 2010;65A(12):1344‐52. [DOI] [PubMed] [Google Scholar]
Lin 2008 {published data only}
- Lin LJ, McClear E, Tabourne CES. The outcomes of therapeutic dance movement on physical and emotional functioning for elderly people. American Journal of Recreation Therapy 2008;Winter:25‐34. [Google Scholar]
Liu 2007 {published data only}
- Liu H, Rainey J, Zabel R, Quiben MU, Kehayov A, Boswell J. Comparison of two exercise programs using the Falls Efficacy Scale, Berg Balance Scale and ankle dorsiflexor strength in older adults. Physical & Occupational Therapy in Geriatrics 2007;26(2):23‐42. [Google Scholar]
Liu 2008 {published data only}
- Liu M, So H. Effects of Tai Chi exercise program on physical fitness, fall related perception and health status in institutionalized elders. Taehan Kanho Hakhoe Chi 2008;38(4):620‐8. [DOI] [PubMed] [Google Scholar]
Liu 2009a {published data only}
- Liu H, Grando V, Zabel R, Nolen J. Pilot study evaluating fear of falling and falls among older rolling walker users... including commentary by Hakim RM, Huang M, and Pearson B. International Journal of Therapy & Rehabilitation 2009;16:670‐7. [Google Scholar]
Liu 2010 {published data only}
- Liu H, Frank A. Tai chi as a balance improvement exercise for older adults: a systematic review. Journal of Geriatric Physical Therapy 2010;33:103‐9. [PubMed] [Google Scholar]
Lord 1995 {published data only}
- Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12‐month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. Journal of the American Geriatrics Society 1995;43:1198‐206. [DOI] [PubMed] [Google Scholar]
Lord 2005 {published data only}
- Lord SR, Tiedemann A, Chapman K, Munro B, Murray SM, Sherrington C. The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized, controlled trial. Journal of the American Geriatrics Society 2005;53:1296‐304. [DOI] [PubMed] [Google Scholar]
Luukinen 2007 {published data only}
- Luukinen H, Lehtola S, Jokelainen J, Vaananen‐Sainio R, Lotvonen S, Koistinen P. Pragmatic exercise‐oriented prevention of falls among the elderly: a population‐based, randomized, controlled trial. Preventive Medicine 2007;44(3):265‐71. [DOI] [PubMed] [Google Scholar]
Maginnis 1999 {published data only}
- Maginnis ME, Privett JL, Raskas WA, Newton RA. Balance abilities of community dwelling older adults engaged in a water exercise program. Journal of Aquatic Physical Therapy 1999;7:6‐12. [Google Scholar]
Mahoney 2007 {published data only}
- Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, Cech S, et al. Kenosha County Falls Prevention Study: a randomized, controlled trial of an intermediate‐intensity, community‐based multifactorial falls intervention. Journal of the American Geriatrics Society 2007;55:489‐98. [DOI] [PubMed] [Google Scholar]
Marchetti 2005 {published data only}
- Marchetti G, Hodges M, Brown R, Krohn K. Test‐retest reliability, external structure validity and responsiveness of gait parameters for older adult females walking at preferred and maximum velocity. Journal of Geriatric Physical Therapy 2005;28:114. [Google Scholar]
McCulloch 2002 {published data only}
- McCulloch KL, Guerra LD, Lee C, Taylor KM. Dual‐task performance on the standardized walking obstacle course: measurement of balance changes in older adults following a pilot intervention. Journal of Geriatric Physical Therapy 2002;25:37. [Google Scholar]
McKinley 2008 {published data only}
- McKinley P, Jacobson A, Leroux A, Bednarczyk V, Rossignol M, Fung J. Effect of a community‐based Argentine tango dance program on functional balance and confidence in older adults. Journal of Aging & Physical Activity 2008;16:435‐53. [DOI] [PubMed] [Google Scholar]
McMurdo 1997 {published data only}
- McMurdo ME, Mole PA, Paterson CR. Controlled trial of weight bearing exercise in older women in relation to bone density and falls. BMJ 1997;314:569. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mihay 2006 {published data only}
- Mihay LM, Boggs KM, Breck AJ, Dokken EL, NaThalang GC. The effect of Tai Chi inspired exercise compared to strength training: a pilot study. Physical & Occupational Therapy in Geriatrics 2006;24:13‐26. [Google Scholar]
Miller 2010 {published data only}
- Miller KL, Magel JR, Hayes JG. The effects of a home‐based exercise program on balance confidence, balance performance, and gait in debilitated, ambulatory community‐dwelling older adults: a pilot study. Journal of Geriatric Physical Therapy 2010;33:85‐91. [PubMed] [Google Scholar]
Morgan 2004 {published data only}
- Morgan RO, Virnig BA, Duque M, Abdel‐Moty E, Devito CA. Low‐intensity exercise and reduction of the risk for falls among at‐risk elders. Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2004;59:1062‐7. [DOI] [PubMed] [Google Scholar]
Nagai 2011 {published data only}
- Nagai K, Inoue T, Yamada Y, Tateuchi H, Ikezoe T, Ichihashi N, et al. Effects of toe and ankle training in older people: a cross‐over study. Geriatrics & Gerontology International 2011;11(3):246‐55. [DOI] [PubMed] [Google Scholar]
NCT00037167 {published data only}
- NCT00037167. Effects of exercise poles on older adults during exercise walking. http://clinicaltrials.gov/show/NCT00037167 (accessed 1 August 2013).
NCT00140322 {published data only}
- NCT00140322. Dane County Safety Assessment (SAFE) research study. http://clinicaltrials.gov/show/NCT00140322 (accessed 1 August 2013).
NCT00217360 {published data only}
- NCT00217360. RCT to reduce further falls and injuries for older fallers presenting to an emergency department. http://clinicaltrials.gov/show/NCT00217360 (accessed 1 August 2013).
NCT00323596 {published data only}
- NCT00323596. Trial of a home based strength and balance retraining program in reducing falls risk factors. http://clinicaltrials.gov/show/NCT00323596 (accessed 1 August 2013).
NCT00483275 {published data only}
- NCT00483275. Fall Prevention by Alfacalcidol and Training (SPALT). http://clinicaltrials.gov/show/NCT00483275 (accessed 1 August 2013).
NCT00805220 {published data only}
- NCT00805220. Nordic walking as gait training for frail elderly. http://clinicaltrials.gov/show/NCT00805220 (accessed 1 August 2013).
NCT00986466 {published data only}
- NCT00986466. Vitamin D and exercise in falls prevention (DEX). http://clinicaltrials.gov/show/NCT00986466 (accessed 1 August 2013).
NCT01006967 {published data only}
- NCT01006967. ActiveStep Comparative Effectiveness Trial (RACE). http://clinicaltrials.gov/show/NCT01006967 (accessed 1 August 2013).
NCT01313481 {published data only}
- NCT01313481. Effect of the Otago programme delivered as home exercise or group exercise (FALLFOR). http://clinicaltrials.gov/show/NCT01313481 (accessed 1 August 2013).
NCT01523600 {published data only}
- NCT01523600. Whole body vibration training among older people using sheltered housing. http://clinicaltrials.gov/ct2/show/NCT01523600 (accessed 1 August 2013).
Nitz 2004 {published data only}
- Nitz JC, Choy NL. The efficacy of a specific balance‐strategy training programme for preventing falls among older people: a pilot randomised controlled trial. Age and Ageing 2004;33:52‐8. [DOI] [PubMed] [Google Scholar]
Obuchi 2004 {published data only}
- Obuchi S, Kojima M, Shiba Y, Shimada H, Suzuki T. A randomized controlled trial of a treadmill training with the perturbation to improve the balance performance in the community dwelling elderly subjects [Japanese]. Nippon Ronen Igakkai Zasshi ‐ Japanese Journal of Geriatrics 2004;41:321‐7. [DOI] [PubMed] [Google Scholar]
Oh 2012 {published data only}
- Oh DH, Park JE, Lee ES, Oh SW, Cho SI, Jang SN, et al. Intensive exercise reduces the fear of additional falls in elderly people: findings from the Korea falls prevention study. Korean Journal of Internal Medicine 2012;27:417‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2001a {published data only}
- Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ 2001;322(7288):697‐701. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2001b {published data only}
- Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ 2001;322(7288):701‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Romero 2010 {published data only}
- Romero ZA. Effects of tai chi on health‐related quality of life in the elderly [Efectos del Tai Chi sobre la calidad de vida relacionada con la salud en los mayores]. Revista Española de Geriatría y Gerontología 2010;45(2):97‐102. [DOI] [PubMed] [Google Scholar]
Rosendahl 2006 {published data only}
- Rosendahl E. Fall Prediction and a High‐intensity Functional Exercise Programme to Improve Physical Functions and to Prevent Falls Among Older People Living in Residential Care Facilities [Thesis]. Sweden: Umeå University, 2006. [Google Scholar]
Rosie 2007 {published data only}
- Rosie J, Taylor D. Sit‐to‐stand as home exercise for mobility‐limited adults over 80 years of age ‐ GrandStand SystemTM may keep you standing?. Age and Ageing 2007;36:555‐62. [DOI] [PubMed] [Google Scholar]
Rubenstein 2000 {published data only}
- Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall‐prone elderly men. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2000;55(6):M317‐21. [DOI] [PubMed] [Google Scholar]
Schwarting 2002 {published data only}
- Schwarting AE, Listerman LR, Harrison AL. The effectiveness of an intervention plan in decreasing fear of falling. Journal of Geriatric Physical Therapy 2002;25:39. [Google Scholar]
Sherrington 2008a {published data only}
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta‐analysis. Journal of the American Geriatrics Society 2008;56(12):2234‐43. [DOI] [PubMed] [Google Scholar]
Sherrington 2014 {published data only}
- Sherrington C, Lord SR, Vogler CM, Close JC, Howard K, Dean CM, et al. Minimising disability and falls in older people through a post‐hospital exercise program: a protocol for a randomised controlled trial and economic evaluation. BMC Geriatrics 2009;9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherrington C, Lord SR, Vogler CM, Close JCT, Howard K, Dean CM, et al. A post‐hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PloS One 2014;9(9):e104412. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shigematsu 2008 {published data only}
- Shigematsu R, Okura T, Sakai T, Rantanen T. Square‐stepping exercise versus strength and balance training for fall risk factors. Aging Clinical & Experimental Research 2008;20:19‐24. [DOI] [PubMed] [Google Scholar]
Shumway‐Cook 1997 {published data only}
- Shumway Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercises on balance, mobility, and fall risk in community‐dwelling older adults. Physical Therapy 1997;77(1):46‐57. [DOI] [PubMed] [Google Scholar]
Silsupadol 2009 {published data only}
- Silsupadol P, Shumway‐Cook A, Lugade V, Donkelaar P, Chou L S, Mayr U, et al. Effects of single‐task versus dual‐task training on balance performance in older adults: a double‐blind, randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2009;90:381‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simmons 1996 {published data only}
- Simmons V, Hansen PD. Effectiveness of water exercise on postural mobility in the well elderly: an experimental study on balance enhancement. Journals of Gerontology Series A: Biological Sciences & Medical Sciences 1996;51:M233‐8. [DOI] [PubMed] [Google Scholar]
Singh 2012 {published data only}
- Singh DK, Rajaratnam BS, Palaniswamy V, Pearson H, Raman VP, Bong PS. Participating in a virtual reality balance exercise program can reduce risk and fear of falls. Maturitas 2012;73(3):239‐43. [DOI] [PubMed] [Google Scholar]
Sipe 2009 {published data only}
- Sipe CL. The effects of strength and power training on functional abilities in older adults. Dissertation Abstracts International: Section B: The Sciences and Engineering 2009;69:6052. [Google Scholar]
Snow 1999 {published data only}
- Snow CM. Exercise effects on falls in frail elderly: focus on strength. Journal of Applied Biomechanics 1999;15(1):84‐91. [Google Scholar]
Southard 2004 {published data only}
- Southard V, Hill J, McKenna RF. A pilot study to assess an intervention to improve falls efficacy. Journal of Geriatric Physical Therapy 2004;27:108. [Google Scholar]
Southard 2006 {published data only}
- Southard V. A randomized control trial of the application of efficacy training to balance assessment. Physical & Occupational Therapy in Geriatrics 2006;25:51‐66. [Google Scholar]
Spink 2011 {published data only}
- Spink MJ, Fotoohabadi MR, Wee E, Landorf KB, Hill KD, Lord SR, et al. Predictors of adherence to a multifaceted podiatry intervention for the prevention of falls in older people. BMC Geriatrics 2011;11:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spink MJ, Menz HB, Lord SR. Efficacy of a multifaceted podiatry intervention to improve balance and prevent falls in older people: study protocol for a randomised trial. BMC Geriatrics 2008;8:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suzuki 2004 {published data only}
- Suzuki T, Kim H, Yoshida H, Ishizaki T. Randomized controlled trial of exercise intervention for the prevention of falls in community‐dwelling elderly Japanese women. Journal of Bone and Mineral Metabolism 2004;22(6):602‐11. [DOI] [PubMed] [Google Scholar]
Sze 2008 {published data only}
- Sze P, Cheung W, Lam P, Lo HD, Leung K, Chan T. The efficacy of a multidisciplinary falls prevention clinic with an extended step‐down community program. Archives of Physical Medicine & Rehabilitation 2008;89:1329‐34. [DOI] [PubMed] [Google Scholar]
Szturm 2011 {published data only}
- Szturm T, Betker A, Moussavi Z, Desai A, Goodman V. Effects of an interactive computer game exercise regimen on balance impairment in frail community‐dwelling older adults: a randomized controlled trial. Physical Therapy 2011;91:1449‐62. [DOI] [PubMed] [Google Scholar]
Taggart 2002 {published data only}
- Taggart HM. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Applied Nursing Research 2002;15:235‐42. [DOI] [PubMed] [Google Scholar]
Takai 2010 {published data only}
- Takai I. Influence of balance exercises during an attention task on fear of falling among frail elderly fallen. Nihon Ronen Igakkai Zasshi 2010;47:220‐5. [DOI] [PubMed] [Google Scholar]
Talley 2008 {published data only}
- Talley KMC. Fear of Falling and Disability Trajectories in Community‐dwelling Older Women [Thesis]. Minnesota: University of Minnesota, 2008. [Google Scholar]
Tennstedt 1998 {published data only}
- Tennstedt S, Howland J, Lachman M, Peterson E, Kasten L, Jette A. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences 1998;53B:P384‐92. [DOI] [PubMed] [Google Scholar]
Tousignant 2012 {published data only}
- Tousignant M, Corriveau H, Roy PM, Desrosiers J, Dubuc N, Hebert R. The effect of supervised Tai Chi intervention compared to a physiotherapy program on fall‐related clinical outcomes: a randomized clinical trial. Disability & Rehabilitation 2012;34:196‐201. [DOI] [PubMed] [Google Scholar]
Underwood 2011 {published data only}
- Underwood M, Eldridge S, Lamb S, Potter R, Sheehan B, Slowther AM, et al. The OPERA trial: protocol for a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Haastregt 2007 {published data only}
- ISRCTN43792817. Reduction of fear of falling and associated increase in functional ability, activity level and quality of life in community‐living older adults who are at risk for falling: a randomised controlled trial. http://controlled‐trials.com/ISRCTN43792817 (accessed 1 August 2013).
- Haastregt JC, Zijlstra GA, Rossum E, Eijk JT, Witte LP, Kempen GI. Feasibility of a cognitive behavioural group intervention to reduce fear of falling and associated avoidance of activity in community‐living older people: a process evaluation. BMC Health Services Research 2007;7:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijlstra G, Haastregt JC, Eijk JT, Kempen GI. Evaluating an intervention to reduce fear of falling and associated activity restriction in elderly persons: design of a randomised controlled trial [ISRCTN43792817]. BMC Public Health 2005;5:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vind 2010 {published data only}
- NCT00226486. Examination and treatment of elderly after a fall. http://clinicaltrials.gov/show/NCT00226486 (accessed 1 August 2013).
- Vind AB, Andersen HE, Pedersen KD, Joergensen T, Schwarz P. Effect of a program of multifactorial fall prevention on health‐related quality of life, functional ability, fear of falling and psychological well‐being. A randomized controlled trial. Aging Clinical and Experimental Research 2010;22:249‐54. [DOI] [PubMed] [Google Scholar]
Voukelatos 2007 {published data only}
- Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. Journal of the American Geriatrics Society 2007;55:1185‐91. [DOI] [PubMed] [Google Scholar]
Williams 2002 {published data only}
- Williams K, Mustian K, Kovacs C. A home‐based intervention to improve balance, gait and self‐confidence in older adults. Activities, Adaptation & Aging 2002;27:1‐16. [Google Scholar]
Williams 2010 {published data only}
- Williams MA, Soiza RL, Jenkinson AM, Stewart A. EXercising with Computers in Later Life (EXCELL) ‐ pilot and feasibility study of the acceptability of the Nintendo WiiFit in community‐dwelling fallers. BMC Research Notes 2010; Vol. 3:238. [DOI] [PMC free article] [PubMed]
Williams 2010a {published data only}
- Williams SB, Brand CA, Hill KD, Hunt SB, Moran H. Feasibility and outcomes of a home‐based exercise program on improving balance and gait stability in women with lower‐limb osteoarthritis or rheumatoid arthritis: a pilot study. Archives of Physical Medicine & Rehabilitation 2010;91:106‐14. [DOI] [PubMed] [Google Scholar]
Woo 2007 {published data only}
- Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community‐living elderly people. Age and Ageing 2007;36(3):262‐8. [DOI] [PubMed] [Google Scholar]
Wrisley 2006 {published data only}
- Wrisley DM, Nunn D, Stephens MJ. The effects of a novel training paradigm on balance ‐‐ preliminary results... Platforms, thematic posters, and posters for CSM 2007. Journal of Neurologic Physical Therapy 2006;30:218. [Google Scholar]
Wu 2010 {published data only}
- Wu G, Keyes L, Callas P, Ren X, Bookchin B. Comparison of telecommunication, community, and home‐based Tai Chi exercise programs on compliance and effectiveness in elders at risk for falls. Archives of Physical Medicine & Rehabilitation 2010;91:849‐56. [DOI] [PubMed] [Google Scholar]
Yamada 2011 {published data only}
- Yamada M, Arai H, Uemura K, Mori S, Nagai K, Tanaka B, et al. Effect of resistance training on physical performance and fear of falling in elderly with different levels of physical well‐being. Age and Ageing 2011;40:637‐41. [DOI] [PubMed] [Google Scholar]
Yamada 2011a {published data only}
- Yamada M, Tanaka B, Nagai K, Aoyama T, Ichihashi N. Rhythmic stepping exercise under cognitive conditions improves fall risk factors in community‐dwelling older adults: Preliminary results of a cluster‐randomized controlled trial. Aging & Mental Health 2011;15:647‐53. [DOI] [PubMed] [Google Scholar]
Yan 2009 {published data only}
- Yan T, Wilber KH, Wieckowski J, Simmons WJ. Results from the Healthy Moves for Aging Well program: changes of the health outcomes. Home Health Care Services Quarterly 2009;28:100‐11. [DOI] [PubMed] [Google Scholar]
Zilstra 2007 {published data only}
- Zijlstra GAR, Haastregt JCM, Rossum E, Eijk JTM, Yardley L, Kempen GIJM. Interventions to reduce fear of falling in community‐living older people: a systematic review. Journal of the American Geriatrics Society 2007;55(4):603‐15. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Arai 2007 {published data only}
- Arai T, Obuchi S, Inaba Y, Nagasawa H, Shiba Y, Watanabe S, et al. The effects of short‐term exercise intervention on falls self‐efficacy and the relationship between changes in physical function and falls self‐efficacy in Japanese older people: a randomized controlled trial. American Journal of Physical Medicine & Rehabilitation 2007;86(2):133‐41. [DOI] [PubMed] [Google Scholar]
Brouwer 2003 {published data only}
- Brouwer BJ, Walker C, Rydahl SJ, Culham EG. Reducing fear of falling in seniors through education and activity programs: a randomized trial. Journal of the American Geriatrics Society 2003;51(6):829‐34. [DOI] [PubMed] [Google Scholar]
Henwood 2008 {published data only}
- Henwood TR, Riek S, Taaffe DR. Strength versus muscle power‐specific resistance training in community‐dwelling older adults. Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2008;63:83‐91. [DOI] [PubMed] [Google Scholar]
Jorgensen 2013 {published data only}
- Jorgensen MG, Laessoe U, Hendriksen C, Nielsen OB, Aagaard P. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community‐dwelling older adults: a randomized controlled trial. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2013;68(7):845‐52. [DOI] [PubMed] [Google Scholar]
- NCT01371253. 10 weeks of Nintendo Wii Fit balance training improved postural balance and muscle strength in elderly individuals. http://clinicaltrials.gov/show/NCT01371253. UK, (accessed 1 August 2013).
Kim 2009b {published data only}
- Kim S, Lockhart T, Roberto K. The effects of eight‐week balance training or weight training: for the elderly on fear of falling measures and social activity levels. Quality in Ageing 2009;10(4):37‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2008 {published data only}
- Morris DM. An Evaluation of Yoga for the Reduction of Fall Risk Factors in Older Adults [Thesis]. Florida: Florida State University, 2008. [Google Scholar]
Wolf 2003 {published data only}
- Sattin R, Easley K, Wolf S, Chen Y, Kutner M. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. Journal of American Geriatrics Society 2005;53:1168‐78. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Sattin RW, Kutner M, O'Grady M, Greenspan AI, Gregor RJ. Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial (commentary by Lavery L and Studenski S). Journal of the American Geriatrics Society 2003;51:1693. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Iliffe 2010b {published data only}
- Iliffe S, Kendrick D, Morris M, Skelton D, Gage H, Dinan S, et al. Multi‐centre cluster randomised trial comparing a community group exercise programme with home based exercise with usual care for people aged 65 and over in primary care: protocol of the ProAct 65+ trial. Trials 2010;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00726531. Multi‐centre cluster randomised trial comparing a community group exercise programme with home based exercise with usual care for over 65s in primary care. http://www.clinicaltrials.gov/show/NCT00726531 (accessed 25 January 2013).
NCT01032252 {published data only}
- NCT01032252. Prevention of falls in community‐dwelling older adults by a standardized assessment of fall risks in the general practitioner setting and through implementation of a network for effective individual reduction on fall risks. http://clinicaltrials.gov/show/NCT01032252 (accessed 25 January 2013).
Additional references
Andresen 2006
- Andresen EM, Wolinsky FD, Miller JP, Wilson M‐MG, Malmstrom TK, Miller DK. Cross‐sectional and longitudinal risk factors for falls, fear of falling, and falls efficacy in a cohort of middle‐aged African Americans. Gerontologist 2006;46(2):249‐57. [DOI] [PubMed] [Google Scholar]
Bridle 2012
- Bridle C, Spanjers K, Patel S, Atherton NM, Lamb SE. Effect of exercise on depression severity in older people: systematic review and meta‐analysis of randomised controlled trials. British Journal of Psychiatry 2012;201:180‐5. [DOI] [PubMed] [Google Scholar]
Bula 2011b
- Bula C, Monod S, Hoskovec C, Rochat S. Interventions aiming at balance confidence improvement in older adults: an updated review. Gerontology 2011;57(3):276‐86. [DOI] [PubMed] [Google Scholar]
CDC 2011
- Centers for Disease Control and Prevention. Physical activity for everyone: Glossary of terms. Available at http://www.cdc.gov/physicalactivity/everyone/glossary (accessed 3 August11).
Cooney 2013
- Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, et al. Exercise for depression. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD004366.pub6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cumming 2000
- Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF‐36 scores, and nursing home admission. Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2000;55:M299–305. [DOI] [PubMed] [Google Scholar]
Delbaere 2010
- Delbaere K, Close JCT, Brodaty H, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ 2010;341:c4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fletcher 2004
- Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community‐based seniors using home care services. Age and Ageing 2004;33(3):273‐9. [DOI] [PubMed] [Google Scholar]
Gillespie 2012b
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD007146.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gottfries 1997
- Gottfries C‐G, Noltorp S, Nörgaard N, Holmén A, Högstedt B. Recognition and management of depression in the elderly. International Clinical Psychopharmacology 1997;94(12):1099‐102. [Google Scholar]
Hadjistravropoulos 2007
- Hadjistavropoulos T, Martin RR, Sharpe D, Lints AC, McCreary DR, Asmundson GJG. A longitudinal investigation of fear of falling, fear of pain, and activity avoidance in community‐dwelling older adults. Journal of Aging & Health 2007;19(6):965‐84. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hill 1996
- Hill KD, Schwarz JA, Kalogeropoulos AJ, Gibson SJ. Fear of falling revisited. Archives of Physical Medicine & Rehabilitation 1996;77(10):1025‐9. [DOI] [PubMed] [Google Scholar]
Howe 2011
- Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD004963.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howland 1993
- Howland J, Peterson EW, Levin WC. Fear of falling among the community‐dwelling elderly. Journal of Aging and Health 1993;5:229–43. [DOI] [PubMed] [Google Scholar]
Hoyl 1999
- Hoyl MT, Alessi CA, Harker JO, Josephson KR, Pietruszka FM, Koelfgen M, et al. Development and testing of a five‐item version of the Geriatric Depression Scale. Journal of American Geriatric Society 1999;47(7):873‐8. [DOI] [PubMed] [Google Scholar]
Iliffe 2010a
- Iliffe S, Kendrick D, Morris M, Skelton D, Gage H, Dinan S, et al. Multi‐centre cluster randomised trial comparing a community group exercise programme with home based exercise with usual care for people aged 65 and over in primary care: protocol of the ProAct 65+ trial. Trials 2010;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jorstad 2005
- Jorstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling: a systematic review. Journal of American Geriatric Society 2005;53:505‐10. [DOI] [PubMed] [Google Scholar]
Jung 2008
- Jung D. Fear of falling in older adults: comprehensive review. Asian Nursing Research 2008;2(4):214‐22. [DOI] [PubMed] [Google Scholar]
Kempen 2008
- Kempen GIJM, Yardley L, Haastregt JCM, Zijlstra GAR, Beyer N, Hauer K, et al. The Short FES‐I: a shortened version of the falls efficacy scale‐international to assess fear of falling. Age and Ageing 2008;37(1):45‐50. [DOI] [PubMed] [Google Scholar]
Kempen 2009
- Kempen GI, Haastregt JC, McKee KJ, Delbaere K, Zijlstra GR. Socio‐demographic, health‐related and psychosocial correlates of fear of falling and avoidance of activity in community‐living older persons who avoid activity due to fear of falling. BMC Public Health 2009;9:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lachman 1998
- Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 1998;53(1):43‐50. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6.4.11: Search filters. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Legters 2002
- Legters K. Fear of falling. Physical Therapy 2002;82:264‐72. [PubMed] [Google Scholar]
Liu 2009b
- Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD002759.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lusardi 1997
- Lusardi MM, Smith EV Jr. Development of a scale to assess concern about falling and applications to treatment programs. Journal of Outcome Measurement 1997;1:34‐55. [PubMed] [Google Scholar]
McClure 2005
- McClure R, Turner C, Peel N, Spinks A, Eakin E, Highes K. Population‐based interventions for the prevention of fall‐related injuries in older people. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD004441.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parry 2001
- Parry SW, Steen N, Galloway SR . Falls and confidence related quality of life outcome measures in an older British cohort. Postgraduate Medicine 2001;77:103‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Powell 1995
- Powell L, Myers A. The activities‐specific balance confidence (ABC) scale. Journal of Gerontology 1995;50:28‐34. [DOI] [PubMed] [Google Scholar]
ProFaNE 2011
- ProFaNE. ProFaNE Taxonomy Manual. http://profane.co/2011/03/24/profane‐taxonomy‐manual/ 2011.
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rodda 2011
- Rodda J, Walker Z, Carter J. Depression in older adults. BMJ 2011;343:5219. [DOI] [PubMed] [Google Scholar]
Scheffer 2008
- Scheffer AC, Schuurmans MJ, Dijk N, Hooft T, Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing 2008;37(1):19‐24. [DOI] [PubMed] [Google Scholar]
Sherrington 2008b
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta‐analysis. Journal of the American Geriatrics Society 2008;56(12):2234‐43. [DOI] [PubMed] [Google Scholar]
Therrien 2011
- Therrien Z, Hunsley J. Assessment of anxiety in older adults: a systematic review of commonly used measures. Aging & Mental Health 2012;16(1):1‐16. [DOI] [PubMed] [Google Scholar]
Tinetti 1990
- Tinetti M, Richman D, Powell L. Falls efficacy as a measure of fear of falling. Journal of Gerontology 1990;45(6):239‐43. [DOI] [PubMed] [Google Scholar]
Tinetti 1993
- Tinetti ME, Powell L. Fear of falling and low self‐efficacy: a case of dependence in elderly persons. Journal of Gerontology 1993;48:35‐8. [DOI] [PubMed] [Google Scholar]
Tinetti 1994
- Tinetti ME, Mendes de Leon CF, Doucette JT . Fear of falling and fall‐related efficacy in relationship to functioning among community‐living elders. Journal of Gerontology 1994;49:M140–7. [DOI] [PubMed] [Google Scholar]
Underwood 2013
- Underwood M, Lamb S, Eldridge S, Sheehan B, Slowther A, Spencer A, et al. Exercise for depression in care home residents: a randomised controlled trial with cost‐effectiveness analysis (OPERA). Health Technology Assessment 2013;17(18):1‐281. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vellas 1997
- Vellas BJ, Wayne SJ, Romero LJ. Fear of falling and restriction of mobility in elderly fallers. Age and Ageing 1997;26:189–93. [DOI] [PubMed] [Google Scholar]
Wang 2012
- Wang MY, Rousseau J, Boisjoly H, Schmaltz H, Kergoat MJ, Moghadaszadeh S, et al. Activity limitation due to a fear of falling in older adults with eye disease. Investigative Ophthalmology & Visual Science 2012;53(13):7967‐72. [DOI] [PubMed] [Google Scholar]
Washburn 1993
- Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. Journal of Clinical Epidemiology 1993;46(2):153–62. [DOI] [PubMed] [Google Scholar]
Wolf 1997
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. Journal of the American Geriatrics Society 1997;44(5):489‐97. [DOI] [PubMed] [Google Scholar]
Yardley 2002
- Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community‐living older people. Gerontologist 2002;42:17‐23. [DOI] [PubMed] [Google Scholar]
Yardley 2005
- Yardley L, Beyer N, Hauer K, Kempen G, Piot‐Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale‐International (FES‐I). Age and Ageing 2005;34(6):614‐9. [DOI] [PubMed] [Google Scholar]
Yesavage 1983
- Yesavage JA, Brink TL, Rose TL. Development and validation of a geriatric depression rating scale: a preliminary report. Journal of Psychiatric Research 1983;17:27. [DOI] [PubMed] [Google Scholar]
Zijlstra 2007
- Zijlstra GAR, Haastregt JCM, Rossum E, Eijk JTM, Yardley L, Kempen GIJM. Interventions to reduce fear of falling in community‐living older people: a systematic review. Journal of the American Geriatrics Society 2007;55(4):603‐15. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Kendrick 2012
- Kendrick D, Carpenter H, Morris RW, Skelton DA, Gage H, Bowling A. Exercise for reducing fear of falling in older people living in the community. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD009848] [DOI] [PMC free article] [PubMed] [Google Scholar]


