Abstract
Background
Adults spend a majority of their time outside the workplace being sedentary. Large amounts of sedentary behaviour increase the risk of type 2 diabetes, cardiovascular disease, and both all‐cause and cardiovascular disease mortality.
Objectives
Primary
• To assess effects on sedentary time of non‐occupational interventions for reducing sedentary behaviour in adults under 60 years of age
Secondary
• To describe other health effects and adverse events or unintended consequences of these interventions
• To determine whether specific components of interventions are associated with changes in sedentary behaviour
• To identify if there are any differential effects of interventions based on health inequalities (e.g. age, sex, income, employment)
Search methods
We searched CENTRAL, MEDLINE, Embase, Cochrane Database of Systematic Reviews, CINAHL, PsycINFO, SportDiscus, and ClinicalTrials.gov on 14 April 2020. We checked references of included studies, conducted forward citation searching, and contacted authors in the field to identify additional studies.
Selection criteria
We included randomised controlled trials (RCTs) and cluster RCTs of interventions outside the workplace for community‐dwelling adults aged 18 to 59 years. We included studies only when the intervention had a specific aim or component to change sedentary behaviour.
Data collection and analysis
Two review authors independently screened titles/abstracts and full‐text articles for study eligibility. Two review authors independently extracted data and assessed risk of bias. We contacted trial authors for additional information or data when required. We examined the following primary outcomes: device‐measured sedentary time, self‐report sitting time, self‐report TV viewing time, and breaks in sedentary time.
Main results
We included 13 trials involving 1770 participants, all undertaken in high‐income countries. Ten were RCTs and three were cluster RCTs. The mean age of study participants ranged from 20 to 41 years. A majority of participants were female. All interventions were delivered at the individual level. Intervention components included personal monitoring devices, information or education, counselling, and prompts to reduce sedentary behaviour. We judged no study to be at low risk of bias across all domains. Seven studies were at high risk of bias for blinding of outcome assessment due to use of self‐report outcomes measures.
Primary outcomes
Interventions outside the workplace probably show little or no difference in device‐measured sedentary time in the short term (mean difference (MD) ‐8.36 min/d, 95% confidence interval (CI) ‐27.12 to 10.40; 4 studies; I² = 0%; moderate‐certainty evidence). We are uncertain whether interventions reduce device‐measured sedentary time in the medium term (MD ‐51.37 min/d, 95% CI ‐126.34 to 23.59; 3 studies; I² = 84%; very low‐certainty evidence)
We are uncertain whether interventions outside the workplace reduce self‐report sitting time in the short term (MD ‐64.12 min/d, 95% CI ‐260.91 to 132.67; I² = 86%; very low‐certainty evidence).
Interventions outside the workplace may show little or no difference in self‐report TV viewing time in the medium term (MD ‐12.45 min/d, 95% CI ‐50.40 to 25.49; 2 studies; I² = 86%; low‐certainty evidence) or in the long term (MD 0.30 min/d, 95% CI ‐0.63 to 1.23; 2 studies; I² = 0%; low‐certainty evidence).
It was not possible to pool the five studies that reported breaks in sedentary time given the variation in definitions used.
Secondary outcomes
Interventions outside the workplace probably have little or no difference on body mass index in the medium term (MD ‐0.25 kg/m², 95% CI ‐0.48 to ‐0.01; 3 studies; I² = 0%; moderate‐certainty evidence). Interventions may have little or no difference in waist circumference in the medium term (MD ‐2.04 cm, 95% CI ‐9.06 to 4.98; 2 studies; I² = 65%; low‐certainty evidence).
Interventions probably have little or no difference on glucose in the short term (MD ‐0.18 mmol/L, 95% CI ‐0.30 to ‐0.06; 2 studies; I² = 0%; moderate‐certainty evidence) and medium term (MD ‐0.08 mmol/L, 95% CI ‐0.21 to 0.05; 2 studies, I² = 0%; moderate‐certainty evidence)
Interventions outside the workplace may have little or no difference in device‐measured MVPA in the short term (MD 1.99 min/d, 95% CI ‐4.27 to 8.25; 4 studies; I² = 23%; low‐certainty evidence). We are uncertain whether interventions improve device‐measured MVPA in the medium term (MD 6.59 min/d, 95% CI ‐7.35 to 20.53; 3 studies; I² = 70%; very low‐certainty evidence).
We are uncertain whether interventions outside the workplace improve self‐reported light‐intensity PA in the short‐term (MD 156.32 min/d, 95% CI 34.34 to 278.31; 2 studies; I² = 79%; very low‐certainty evidence).
Interventions may have little or no difference on step count in the short‐term (MD 226.90 steps/day, 95% CI ‐519.78 to 973.59; 3 studies; I² = 0%; low‐certainty evidence)
No data on adverse events or symptoms were reported in the included studies.
Authors' conclusions
Interventions outside the workplace to reduce sedentary behaviour probably lead to little or no difference in device‐measured sedentary time in the short term, and we are uncertain if they reduce device‐measured sedentary time in the medium term. We are uncertain whether interventions outside the workplace reduce self‐reported sitting time in the short term. Interventions outside the workplace may result in little or no difference in self‐report TV viewing time in the medium or long term. The certainty of evidence is moderate to very low, mainly due to concerns about risk of bias, inconsistent findings, and imprecise results. Future studies should be of longer duration; should recruit participants from varying age, socioeconomic, or ethnic groups; and should gather quality of life, cost‐effectiveness, and adverse event data. We strongly recommend that standard methods of data preparation and analysis are adopted to allow comparison of the effects of interventions to reduce sedentary behaviour.
Plain language summary
Interventions outside the workplace to reduce sedentary behaviour
Background
Adults spend most of their time outside of their workplace being sedentary, for example, sitting while watching TV or using a computer, or travelling to and from work in a car. Prolonged sedentary behaviour has been linked with increased risk of several diseases and premature death. We do not yet know if interventions to reduce sedentary behaviour outside the workplace are effective. This review will tell us whether there is evidence that these interventions reduce sedentary behaviour.
Main findings
We searched for studies up to 14 April 2020. We found 13 relevant studies involving a total of 1770 participants. All were conducted in high‐income countries, at universities, in home/community, online, and in primary care. The average age of participants in these studies was between 20 and 41 years. Most participants were female. All interventions were targeted at the individual: none were environmental or policy. Intervention components included personal monitoring devices, information or education, counselling, and prompts to reduce sedentary behaviour.
We examined the following primary outcomes: device‐measured sedentary time, self‐report sitting time, self‐report TV viewing time, and breaks in sedentary time. The certainty of evidence was moderate to very low, mainly due to concerns about risk of bias, inconsistent findings, and imprecise results. "Moderate" indicates that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. "Very low" indicates that any estimate of effect is very uncertain. Overall there is not enough evidence to support conclusions about whether interventions are effective in reducing sedentary behaviour. Collectively, studies did not provide evidence of an effect on device‐measured total sedentary time, nor on the subsets of self‐report sitting time, TV viewing time, or breaks in sedentary time.
We examined the following secondary outcomes: body composition, markers of insulin resistance, device measured moderate‐to‐vigorous physical activity (MVPA), self‐report light physical activity (PA), and step count. The certainty of evidence was moderate for body mass index and glucose, therefore interventions outside the workplace probably have little or no different on these outcomes. Interventions may have little or no difference on MPVA in the short term, steps and waist circumference (low‐certainty evidence). We are uncertain whether interventions improve MVPA in the medium term and light PA (very low‐certainty evidence). The included studies did not report any data on adverse events or symptoms.
Conclusions
Interventions outside the workplace to reduce sedentary behaviour probably lead to little or no difference in sedentary time. We are uncertain whether interventions outside the workplace reduce sitting time. Interventions may produce little or no difference in self‐report TV viewing time. More research is needed to assess the effectiveness of interventions, and studies should include participants from varying age, socioeconomic, and ethnic groups.
Summary of findings
Summary of findings 1. Intervention compared to Control for reducing sedentary behaviour in adults under 60.
| Intervention compared to control for reducing sedentary behaviour in adults under 60 | |||||
| Patient or population: community‐dwelling adults under 60 years of age Setting: outside the workplace Intervention: individual‐level interventions aiming to reduce sedentary behaviour Comparison: no intervention or attention control | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with Control | Risk with Intervention | ||||
| Device‐measured sedentary time | Short‐term follow‐up (up to 4 months) | ||||
| Control group mean was 574.44 min/d | MD 8.36 lower (‐27.12 lower to 10.40 higher | 262 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| Medium‐term follow‐up (> 4 months to 12 months) | |||||
| Control group mean was 590.67 min/day | MD 51.37 lower (126.34 lower to 23.59 higher | 188 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | ||
| Self‐report TV viewing time | Medium follow‐up (> 4 months to 12 months) | ||||
| Control group mean was 99.30 min/day | MD 12.45 lower (50.40 lower to 25.49 higher) |
459 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 4 | ||
| Long‐term follow‐up (> 12 months) | |||||
| Control group mean was 111.22 | MD 0.30 higher (0.63 lower to 1.23 higher) |
709 (2 RCTs) | ⊕⊕⊝⊝ LOW 5 6 | ||
| Device‐measured MVPA | Short‐term (up to 4 months) | ||||
| Control group mean was 48.76 min/day | MD 1.99 higher (4.27 lower to 8.25 higher) | 296 (4 RCTs) | ⊕⊕⊝⊝ LOW 1 7 | ||
| Medium‐term follow‐up (> 4 months to 12 months) | |||||
| Control group mean was 62.97 min/day | MD 6.59 higher (7.35 lower to 20.53 higher) | 214 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 8 | ||
| Self‐report light PA | Short‐term follow‐up (up to 4 months) | ||||
| Control group mean was 232.86 min/day | MD 156.32 higher (34.34 higher to 278.31 higher) | 115 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 5 9 10 | ||
| Adverse events and symptoms | None reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI:Confidence interval; MD: mean difference; RCT: randomised controlled trial; min/day: minutes per day | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1 Concerns about imprecision due to wide confidence intervals and small sample sizes
2 Low risk of bias for outcome assessment, however 2 studies have high risk for several domains
3 Large variation in effect, I2 = 87%
4 High risk of bias for outcome assessment for this outcome, unclear risk of bias for several other domains.
5 High risk of bias for outcomes assessment, unclear or high risk of bias for several other domains
6 Large sample size however large confidence intervals lead to uncertainty
7 Low risk of bias for outcome assessment, however majority of studies have unclear or high risk of bias for several domains
8 Large variation in effect, I2 = 71%
9 Large variation in effect, CI's slightly overlap, Chi2 P < 0.05, I2 = 79%
10 Very serious concerns about precision due to large confidence internals and small sample size
Background
Description of the condition
Research into sedentary behaviour is an emerging and rapidly growing field. Sedentary behaviour is defined as waking activity characterised by an energy expenditure of 1.5 or fewer metabolic equivalents and a sitting or reclining posture (Sedentary Behaviour Research Network 2012). A recent overview of systematic reviews of observational studies concluded that there is strong evidence of a positive relationship between sedentary behaviour and all‐cause mortality, fatal and non‐fatal cardiovascular disease, and type 2 diabetes and metabolic syndrome, along with moderate evidence of increased incidence of ovarian, colon, and endometrial cancers (De Rezende 2014). Conversely, interrupting sedentary time and/or replacing it with light‐intensity activity has been shown to improve several markers of cardiovascular disease risk (Dunstan 2012; Peddie 2013; Thorp 2014). Some research suggests that sedentary behaviour may be a distinct risk factor, independent of physical activity, for multiple adverse health outcomes (Chomistek 2013; Stamatakis 2011; Thorp 2011). Indeed, even people who are physically active at or above recommended levels experience the adverse effects of sedentary behaviour (Katzmarzyk 2009). Researchers estimate that people need approximately 60 to 75 minutes per day of moderate‐intensity physical activity to eliminate the increased risk of death associated with high sitting time; however, this high activity level reduces but does not eliminate the increased risk associated with high TV‐viewing time (Ekelund 2016).
The mechanisms through which sedentary behaviours lead to cardiovascular morbidity and mortality are under‐explored in the literature, but hypotheses point to defects in lipoprotein metabolism, early atherosclerosis, insulin resistance, and development of the metabolic syndrome (Same 2016). Obesity may act as a mediator between sedentary behaviours and negative health outcomes (Same 2016). Research from the genetics field has identified a genotype that is particularly susceptible to the adverse effects of excessive sedentary periods on glycaemic regulation (Alibegovic 2010), thus suggesting a potential gene–environment interplay that determines who is most susceptible to developing diabetes when exposed to excess sedentary time (Wilmot 2012).
Sedentary behaviour in adults is characterised as TV viewing and other screen‐focused behaviours in domestic environments, prolonged sitting in the workplace, and time spent sitting in automobiles (Owen 2011). Accelerometer data from a representative sample of US adults show that over 50% of waking hours are spent sedentary (Healy 2011). Weekday self‐reported sitting time varies considerably across European countries, with adults in northwestern European countries sitting the most (means 5.6 to 6.8 hours/d) (Bennie 2013). Accelerometer data suggest that UK men and women actually spend approximately 7.5 and 7 hours per day, respectively, being sedentary (Ekelund 2009). Many interventions to reduce sitting time in adults have focused on the workplace setting (Shrestha 2016); however, workplace sitting represents only one domain of sedentary behaviour, as adults spend approximately 70% of their non‐work time being sedentary as well (Parry 2013). TV viewing is a major contributor to sedentary behaviour in the USA, with the average adult watching five hours of TV per day (Pettee 2009; The Nielsen Company 2009). In addition, inactive travel modes and other non‐occupational behaviours such as leisure‐time computer use are increasing (Brownson 2005; Chau 2012). Serial cross‐sectional US data show that from 2001 to 2016, the estimated prevalence of computer use outside school or work for at least one hour per day increased from 29% to 50% for adults (Yang 2019). There are several known individual correlates of sedentary behaviour, such as age, physical activity level, body mass index, and socioeconomic status, and evidence related to social and environmental factors is emerging (O'Donoghue 2016). A taxonomy of sedentary behaviours is currently under development to provide a structure for current and future knowledge of sedentary behavior and a basis for distinguishing different behaviours (Chastin 2013).
Although no global (e.g. World Health Organization (WHO)) guidelines on sedentary behaviour exist, several countries have made population‐based recommendations. Much of the focus thus far is related to screen time for children. For example, since 2001, the American Academy of Pediatrics has recommended that parents limit children's total entertainment media time to no more than one to two hours of quality programming per day (American Academy of Pediatrics 2001). This two‐hour limit for children is consistent with the 2004 Australian guidelines (Australian Government 2004). Canada addressed general sedentary behaviour in its 2011 guidelines by recommending that children should minimise the time that they spend being sedentary each day (Tremblay 2011). More recently, the WHO included a screen time guideline for children younger than five years of age (WHO 2019). In 2011 the UK Chief Medical Officers joined Australia (among others) in providing public health guidelines aimed specifically at highlighting the potential health risks associated with sedentary behaviour for adults (BHFNC Physical Activity and Health 2012). The UK guidelines recommend that all adults minimise the amount of time spent being sedentary (sitting) for extended periods (Department of Health 2011), without specifying a duration of time. The Australian guidelines recommend that adults minimise the amount of time spent in prolonged sitting and break up long periods of sitting as often as possible (Australian Government 2014). A recent paper led by UK researchers suggested that for predominantly desk‐based occupations, workers should aim to initially progress towards accumulating two hours per day of standing and light activity during working hours, eventually progressing to a total accumulation of four hours per day (Buckley 2015); however, this is not an official guideline from the UK Chief Medical Officers.
Public health agencies have yet to present a quantified time limit on daily or weekly volumes of sedentary behaviour. Indeed several researchers suggest that the development of quantitative public health guidelines is premature, as little is known about the independent detrimental health effects of sitting, and there are many inconsistencies in how the evidence based was developed and interpreted (Stamatakis 2019). Some evidence suggests that a reduction of one to two hours of sedentary time per day could equate to substantial reductions in cardiovascular disease risk (Healy 2011). One study estimated that beneficial effects on cardiovascular disease risk biomarkers were associated with the reallocation of 30 minutes per day of sedentary time with an equal amount of sleep, light‐intensity physical activity, or moderate to vigorous physical activity (Buman 2013). A recent review of experimental studies concluded that breaking up sitting time and replacing it with light‐intensity ambulatory physical activity and standing may be a sufficient stimulus to induce acute favourable changes in postprandial (the period after eating a meal) metabolic parameters such as glucose and insulin response in people who are physically inactive and have type 2 diabetes, whereas a higher intensity or volume seems to be more effective in rendering such positive outcomes in young, regularly active people (Benatti 2015). However Stamatkais and colleagues noted the absence of long‐term prospective epidemiological evidence from studies that use objective measures of actual sitting, as opposed to absence of ambulatory movement (Stamatakis 2019). Of note is that the Second Edition of the Physical Activity Guidelines for Americans concludes that the existing evidence base does not allow a specific healthy target for total sedentary behaviour time to be determined (PA Guidelines Advisory Committee 2018). Similarly, the UK Expert Working Group for Sedentary Behaviour (tasked with examining evidence to decide if changes to current physical activity recommendations are warranted) did not support any significant changes to existing guidance nor suggest that a time limit or minimum threshold for sedentary behaviour should be added (Cooper 2018). The Expert Group supports a recommendation to interrupt prolonged periods of sedentary behaviour with light‐intensity physical activity but does not suggest that prolonged sedentary time should be interrupted by standing (Cooper 2018).
Description of the intervention
Our review assessed effects of interventions that aim to reduce sedentary behaviour among adults in non‐occupational settings. This will include studies that incorporate any component intending to reduce sedentary time, including if this is part of a larger intervention. We define a component as any strategy that explicitly targets a reduction in sedentary behaviour and is reported as a component of the intervention. This approach allows our review to include not only studies that focus exclusively on sedentary behaviour but also those that take a combined approach to reduce sedentary behaviour and increase physical activity. We note from the literature that some studies target a specific sedentary behaviour, such as TV viewing, or a collection of behaviours like overall use of screen time.
Interventions may be delivered at the individual, environmental, or policy level and include interventions within domestic environments, transport, and the wider community. Interventions include education and counselling sessions, wherein participants develop an implementation plan for behaviour change (De Greef 2010); self‐monitoring of behaviour alongside goal‐setting, where participants are encouraged to track their sitting time and set goals to increase breaks from sitting (Adams 2013); and multi‐component lifestyle interventions. Interventions targeting the environmental level may include point‐of‐decision prompts to encourage adults to stand (Lang 2015), or they could consist of controls placed on use of screen time, for example, limiting TV viewing by installing an electronic lockout system (Otten 2009). Those delivering the interventions will include counsellors, researchers, exercise physiologists, psychologists, general practitioners (GPs), and other public health professionals. Delivery modes are likely to involve face‐to‐face individual and/or group sessions, telephone support, provision of written leaflets, and use of online platforms. Many studies incorporate specific behaviour change strategies in the design, with self‐monitoring behaviour, problem‐solving, modifying social and physical environments, and giving information on the health impact of sitting most closely associated with promising interventions (Gardner 2016).
How the intervention might work
Several frameworks have emerged from recent research for understanding sedentary behaviour and informing intervention development (Owen 2014; Prapavessis 2015). An ecological model of sedentary behaviours highlights a behaviour‐ and context‐specific approach to understand the multiple determinants (Owen 2011). The behaviours and contexts of primary concern are TV viewing and other screen‐focused behaviours in domestic environments, prolonged sitting in the workplace, and time spent sitting in automobiles (Owen 2011). Trial authors suggest that change to sedentary behaviour in these domains may be altered by focusing on a specific setting with due consideration of the correlates of sedentary behaviour for that setting along with understanding factors related to high levels of overall sedentary time. A recent review of behaviour change strategies used in interventions for sedentary behaviour concluded that the most promising interventions were based on environmental restructuring, persuasion, or education (Gardner 2016). In addition, the following behaviour change techniques were particularly promising: self‐monitoring, problem‐solving, and restructuring of the social or physical environment.
We developed a logic model based on Baker 2015 to illustrate how the interventions might work and to describe the interactions between intervention activities and outcomes (Figure 1). We envisage several ways that interventions in non‐occupational settings may reduce sedentary behaviour in adults under 60 years of age.
1.

Logic Model for interventions targeted outside of workplace settings for reducing sedentary behaviour (adapted from Baker 2015).
Individual, including education/information/counselling: adults may be willing to alter behaviour after learning about the health risks of a sedentary lifestyle. To support efforts to change behaviour, counsellors could encourage adults to track their sitting time and set goals to increase breaks. Similarly, they may receive suggestions to reduce sitting time.
Environmental: for example, removing seats from certain carriages on a train would force commuters to stand for the journey. Similarly, studies could limit recreational TV viewing by installing a lockout system that engages after a specific usage period per day, thus encouraging adults to change their usual behaviour. Placing computers at standing height would also prompt standing.
Policy, including challenges to socials norms: for example, by providing prompts and invitations to encourage standing at events, participants may be more likely to stand for some or all of the duration.
Why it is important to do this review
The evidence base reporting the health implications of sedentary behaviour and interventions to address this problem is rapidly expanding. Although studies first identified an increase in cardiovascular disease (CVD) risk experienced by people in highly sedentary jobs in the 1950s, only in recent years have the potential CVD risks from sedentary behaviour, as distinct from physical activity, come to be appreciated (Ford 2012). Recent observational and experimental evidence makes a compelling case for reducing and breaking up prolonged sitting time in both primary prevention and disease management contexts (Dempsey 2014). The scale of the problem is evidenced by the fact that the adverse health effects of sedentary behaviour are present even among those who are physically active at or above recommended levels (Katzmarzyk 2009). An estimated 5.9% of deaths may be attributable to daily total sitting time, suggesting that its reduction in the population could produce comparable benefits to those achieved by reducing smoking, inactivity, and overweight and obesity (Chau 2013). In this comparison, physical inactivity is defined as "doing no or very little physical activity at work, at home, for transport, or in discretionary time" (Bull 2004; WHO 2009). See Published notes.
Although several reviews have examined interventions to reduce sedentary time in children and young people, a paucity of systematic reviews in adults have been published. The reviews to date have often included interventions designed to increase physical activity but have also reported changes in sedentary time as unintended or secondary outcomes, rather than solely focusing on interventions that purposely aimed to reduce sedentary behaviour (Martin 2015; Prince 2014). A recent review found that the most promising interventions targeted sedentary behaviour instead of physical activity (Gardner 2016). The key difference between our review and these previous reviews is that we will examine only the effects of interventions to reduce sedentary behaviour on sedentary time and health outcomes in non‐occupational settings (Martin 2015; Prince 2014; Shrestha 2016). A recent Cochrane Review examined interventions to reduce sitting time in the workplace setting (Shrestha 2016), another Cochrane Review is examining interventions for reducing sedentary behaviour in community‐dwelling older adults (Chastin 2017), and two further Cochrane Reviews have examined workplace interventions for increasing standing or walking for preventing and decreasing musculoskeletal symptoms among sedentary workers (Parry 2017a; Parry 2017b). However, to our knowledge, there is only one published synthesis of evidence in non‐occupational settings (Thraen‐Borowski 2017), and a meta‐analysis was not conducted in that review. As adults spend approximately 60% to 70% of their non‐work time being sedentary (Clemes 2014; Parry 2013), there is great scope for intervention, and a synthesis of evidence on existing interventions will help guide this task. We believe that non‐occupational settings may offer greater scope for changing sedentary behaviour than occupational settings, where individuals may have less control over their working environments and practices.
The need that policymakers and practitioners have for this Cochrane Review is evident in the focus on sedentary behaviour at the governmental level worldwide. This is also reflected in much being written in the media about the dangers of sitting. Countries are expanding their public health guidelines to include recommendations on limiting sedentary time (e.g. see Healthy Ireland 2016 and Sedentary Behaviour and Obesity Working Group 2010). This review will also provide key evidence for countries that seek to update existing sedentary behaviour guidelines in future years (e.g. Australian Government 2014). The findings of the review will therefore aid evidence‐based decision‐making by policymakers and practitioners working to address sedentary behaviour worldwide. This rapidly growing field will inform the development of public health policy over the coming decade, and a regularly updated, robust, comprehensive review of the evidence is required to support this task.
Objectives
Primary
To assess effects on sedentary time of non‐occupational interventions for reducing sedentary behaviour in adults under 60 years of age
Secondary
To describe other health effects and adverse events or unintended consequences of these interventions
To determine whether specific components of interventions are associated with changes in sedentary behaviour
To identify if there are any differential effects of interventions based on health inequalities (e.g. age, sex, income, employment)
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and cluster randomised controlled trials (cluster RCTs) aimed at changing sedentary behaviour. Given the growing volume of research on interventions targeting sedentary behaviour, particularly RCTs, we believe that solely including RCTs and cluster RCTs will allow us to draw conclusions from the best available evidence.
Types of participants
We included studies involving community‐dwelling adults aged 18 to 59 years who are free from pre‐existing medical conditions that may limit participation in the intervention.
Types of interventions
We included interventions targeted outside of workplace settings. Hypothetically, these may include interventions within domestic environments, transport, and the wider community. The following are examples of interventions that may be included in the review.
Counselling/education to reduce and self‐monitor sedentary behaviour.
Limits/controls placed on screen time.
Environmental change interventions, for example, point‐of‐decision prompts to encourage standing.
Multi‐component lifestyle interventions that include a sedentary behaviour element.
Community‐level interventions that specifically aim to address sedentary behaviour.
Interventions may be delivered at the individual, environmental, or policy level. We excluded interventions provided in workplace settings, as they fall under the scope of a separate Cochrane Review (Shrestha 2016). In addition, we excluded studies with participants 60 years of age and older, as another Cochrane Review is focusing on that age group (Chastin 2017). We also excluded studies that aim to improve physical activity levels but happen to report sedentary time, as they do not specifically target sedentary behaviour in their design.
Comparison was between those receiving the intervention and those receiving no intervention or attention controls.
Types of outcome measures
We included studies that report sedentary behaviour as a primary or secondary outcome.
Primary outcomes
The primary outcome is sedentary behaviour, assessed at baseline and post intervention. There is no international consensus on a gold standard measure of sedentary behaviour. With this in mind, we included studies that utilised device‐based (e.g. accelerometer, inclinometer) or self‐report (e.g. diary, questionnaire) measures of sedentary time. We included studies that report sedentary behaviour in one domain only, for example, sitting during transport or TV viewing at home, as well as those reporting total daily sedentary behaviour. We considered both total duration of sedentary behaviour reported and breaks in sedentary behaviour as primary outcome measures.
We included the following primary outcomes.
Device‐measured sedentary time.
Self‐report sitting time.
Self‐report TV viewing.
Breaks in sedentary time.
Secondary outcomes
We included the following secondary outcome measures.
Energy expenditure.
Body composition (e.g. body mass index, waist and hip circumference, body fat percentage, body weight).
Cholesterol (e.g. total cholesterol, low‐density lipoprotein (LDL) cholesterol, high‐density lipoprotein (HDL) cholesterol).
Markers of insulin resistance (e.g. fasting blood glucose, liver transaminases, insulin levels or insulin resistance/impaired insulin sensitivity).
Inflammatory markers (e.g. C‐reactive protein (CRP), interleukin (IL)‐6, tumour necrosis factor (TNF)‐α).
Measures of carotid intima media thickness (e.g. ultrasound).
Measures of endothelial function (e.g. peripheral arterial tonometry).
-
Measures of mental health (e.g. stress symptoms, anxiety, depression, self‐image).
Mood
Wellness
Adverse events and symptoms (e.g. musculoskeletal injuries/pain, cardiovascular events).
-
Unintended outcomes (e.g. social approval/disapproval by others, change in overall physical activity behaviour).
Device‐measured moderate to vigorous physical activity (MVPA)
Self‐report MVPA
Self‐report light, moderate, vigorous, and total physical activity (PA)
Step count
Search methods for identification of studies
Electronic searches
We searched the following electronic databases up to 14 April 2020, using a search strategy developed by NR and EM in liaison with the Cochrane Public Health Group (CPHG) Trials Search Co‐ordinator (see Appendix 1).
CPHG Specialised Register.
Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library, Wiley.
MEDLINE (Ovid MEDLINE Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE) (OvidSP) (1946 to present).
Embase (OvidSP) (1974 to present).
Cochrane Database of Systematic Reviews, in the Cochrane Library, Wiley.
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOHost) (1982 to present).
PsycINFO (OvidSP) (1806 to present).
SportDiscus (EBSCOHost).
We did not impose any language, publication status, or date restrictions. We contacted trial authors and research groups for information about unpublished or ongoing studies.
Searching other resources
We handsearched reference lists of included studies and key systematic reviews. We searched the Clinicaltrials.gov trial register (http://clinicaltrials.gov) on 14 April 2020. We contacted authors of included studies and relevant systematic reviews to identify additional studies. In addition, we contacted experts in the field and asked them to identify further articles. We also searched the websites of organisations involved in addressing and reporting research on sedentary behaviour.
Sedentary Behaviour Research Network (http://www.sedentarybehaviour.org).
World Health Organization (http://www.who.int).
US Centers for Disease Control and Prevention (http://www.cdc.gov).
International Society for Physical Activity and Health (http://www.ispah.org).
National Physical Activity Plan (http://www.physicalactivityplan.org).
The Community Guide (http://www.thecommunityguide.org).
European Commission, Public Health (https://ec.europa.eu/health/home_en).
NR and EM carried out the searches.
Data collection and analysis
Selection of studies
We downloaded the references retrieved through electronic searches and handsearching to the reference management software Endnote, removing duplicates (Endnote 2015). Two review authors (EM and MM) independently undertook an initial screening of titles and abstracts to exclude records outside the scope of the review. A third review author (CF) reviewed any items of disagreement to reach a consensus. We obtained full‐text papers when we deemed titles to be relevant, or when eligibility was unclear. Inclusion decisions were based on the full texts of potentially eligible studies. Two review authors, working independently, determined whether each study met the eligibility criteria (EM and MM). When any disagreements occurred, a third review author (CF) examined the paper and the three review authors reached a consensus. We kept a record of reasons for excluding studies. If we identified papers detailing study design, study protocols, or process evaluations, we contacted the study authors to locate published or unpublished findings from the study. We collated multiple reports of the same study and treated each study as the unit of interest. We did not find any potentially relevant title of a paper in a language other than English, so we did not require translation services.
We used the online software Covidence to manage the study selection process (Covidence 2016).
Data extraction and management
Two review authors (EM and KM) independently extracted study characteristics and outcome data using a modified version of the Public Health Group Data Extraction and Assessment Form. We consulted a third review author (CF) when disagreements occurred and we reached consensus among the three authors. All participating review authors piloted the Data Extraction and Assessment Form, modifying it where necessary to ensure comprehensiveness and comparability between results. We completed data extraction online using Covidence software and exported data directly to Review Manager 5 (Covidence 2016; RevMan 2014). When information was missing or when we needed clarification, we contacted the authors of included studies. We report relevant information in the Characteristics of included studies table. When we found multiple articles from the same study, we compared them for completeness and possible contradictions.
We extracted the following data.
Study objectives: for example, to decrease sedentary time or to decrease sedentary time and increase physical activity.
Study design: RCTs and cluster RCTs.
Methods: study location, study setting, dates of study, duration of intervention, and duration of follow‐up. We recorded how investigators measured sedentary behaviour, for example, by questionnaire/accelerometer.
Participants: number randomised to each group, age, withdrawals. We extracted sociodemographic characteristics at baseline and at endpoint using the PROGRESS framework (Place, Race, Occupation, Gender, Religion, Education, Socioeconomic status, Social status).
Intervention: content of intervention, description of comparison. We noted whether or not interventions included particular strategies to address diversity or disadvantage. We also noted the theoretical basis for the intervention when reported.
Outcomes: outcome measures post intervention and at follow‐up when available. We noted whether clustering was taken into account in cluster RCTs. When data on multiple measures of the same or similar outcomes were available, for example, body composition measures of body mass index (BMI) and body fat percentage, we recorded both.
Notes: funding received and conflicts of interest as declared by study authors.
In addition to study characteristics and outcomes data, we collected from included studies any available information about context, implementation factors, equity, cost, and sustainability and reported it in the Characteristics of included studies table (CPHG 2011). We view sustainability of the interventions as a combination of intervention components (dose) and magnitude of effect over time. We collected any available data related to sustainability (e.g. follow‐up measures) and assessed the data using an adapted version of the approach adopted by Müller‐Riemenschneider 2008. We included potential moderators and confounders of study outcomes, such as age, race, and gender, on the Data Extraction and Assessment Form.
For several studies, it was necessary to process data in preparation for analysis. For example, in four studies, sedentary time was converted from hours per day to minutes per day (Barwais 2013; Biddle 2015; French 2011; Laska 2016). To calculate the mean device‐measured MVPA in Ellingson 2016, we summed the mean values reported for moderate PA and vigorous PA. For Arrogi 2017, we calculated the mean value for device‐measured sedentary time by obtaining the average of weekday and weekend day results reported in the paper. We utilised the same methods to calculate mean device‐measured MVPA in Jago 2013.
In Finni 2011, three of the time points for data collection (6, 9, and 12 months) would all be considered as medium‐term follow‐up in the present review (i.e. > 4 months to 12 months). We used the data collected at 12 months as the medium‐term value for subgroup analysis. Similarly, Williams 2019 reported data at 17 weeks and 6 months; we used the data collected at 6 months in our analysis.
Assessment of risk of bias in included studies
Two review authors (EM and KM) independently assessed risk of bias using the Cochrane 'Risk of bias' tool (Higgins 2011a). When disagreements occurred, a third review author (MM) reviewed the studies, and review authors together reached consensus by discussion. This tool assesses:
selection bias (sequence generation and allocation concealment);
performance bias (blinding of participants and personnel);
detection bias (blinding of outcome assessment);
attrition bias (incomplete outcome data); and
reporting bias (selective reporting).
We graded each domain as being at 'low', 'high', or 'unclear' risk of bias.
We considered blinding separately for different key outcomes when necessary, for example, the risk of bias for sitting measured by means of an inclinometer may be very different from that for a self‐reported reduction in sitting time (Shrestha 2016). We did not consider blinding of participants and personnel for risk of bias assessment, as it is not possible to blind these individuals in studies examining attempts to modify activity behaviour (Shrestha 2014). We considered the following additional criteria for cluster RCTs, as recommended in Section 16.3.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b): recruitment bias; baseline imbalance; loss of clusters; incorrect analysis; and comparability with individually randomised trials.
We summarised risk of bias at the outcome level and judged each outcome as being at 'low', 'medium', or 'high' overall risk, given the study design and the potential impact of identified risks noted in the table for each study that contributed results for that outcome (CPHG 2011).
Measures of treatment effect
For studies with continuous outcome measures, we reported mean scores and standard deviations. We used the mean difference between post‐intervention values of intervention and control groups to analyse the size of the effects of interventions. For cluster RCTs we used the adjusted MD between groups.
Unit of analysis issues
We identified one study with multiple intervention groups (Kitagawa 2020). We pooled the intervention arms into one group to create a single pair‐wise comparison, as recommended in Section 16.5.4 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). This method avoids including a group of participants twice in the same meta‐analysis. All of the included cluster RCTs made allowance for the design effect of clustering; therefore it was not necessary to re‐analyse data.
Dealing with missing data
We contacted study authors via email when data were missing or unclear (to request e.g. missing information on methods, missing participants due to dropout, and missing statistics). We retrieved email addresses from author information provided in the study publication and, when necessary, accessed contact directories from the authors' documented affiliated organisations. We noted missing data on the data extraction form and reported this in the 'Risk of bias' table. If numerical outcome data such as standard deviations or correlation coefficients were missing, and we could not obtain them from the study authors, we calculated these values from other available statistics such as P values, according to the methods described in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b; Shrestha 2014). We used the RevMan calculator to determine standard deviation (SD) from standard error (SE) for several studies (Biddle 2015; Laska 2016; Williams 2019). Similarly, for French 2011, we used the SE of the mean difference to calculate the SD in intervention and control groups post intervention. For outcomes that are reported narratively, we used the RevMan calculator to determine MD for several studies (Barwais 2013; Cotten 2016; Ellingson 2016; French 2011; Sui 2018).
Assessment of heterogeneity
We considered methodological heterogeneity by assessing differences between included studies in terms of study design. We considered clinical heterogeneity by assessing variability among participants, interventions, and outcomes, as recorded in the Characteristics of included studies table. We visually inspected forest plots to assess statistical heterogeneity and used the I² statistic to quantify the level of heterogeneity present (P < 0.10). This describes the percentage of variability in effect estimates due to heterogeneity rather than to sampling error (chance) (Deeks 2011). We planned to perform sensitivity analyses to investigate heterogeneous results; however due to the number of included studies, we did not conduct these analyses.
Assessment of reporting biases
As we included fewer than 10 studies per outcome, we could not use funnel plots to assess reporting bias, as the power of these tests would be too low to distinguish chance from real asymmetry (Sterne 2011).
Data synthesis
Given that participants, interventions, and comparisons were sufficiently similar, we conducted a meta‐analysis using RevMan 5. We used the random‐effects model, as it allows for a greater level of natural heterogeneity between studies. The appropriate method of meta‐analysis depends on the nature of the data, and we followed the guidelines presented in Chapter 9 ("Analysing data and undertaking meta‐analyses") of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). We included data from cluster randomised trials in meta‐analyses, as trial authors had taken clustering into account. We were unable to examine the effects of interventions according to types of intervention, as all were provided at the individual level.
When it was not possible to conduct a meta‐analysis, we reported results narratively. We grouped the data by outcome, as this makes the most sense for the reader. We presented data in tables and summarised results narratively.
We created Summary of findings table 1 for the main comparisons. Summary of findings table 1 includes the numbers of participants and studies for the primary outcomes (device‐based and self‐report measures of sedentary behaviour), summarises the intervention effects, and includes a measure of the certainty of evidence (see Quality of the evidence section below). We also reported the following secondary outcomes as they were deemed most relevant: device‐measured MVPA, self‐report light PA, steps.
We identified the theoretical frameworks and models identified in the primary studies. We considered costs and sustainability of studies in preparing the synthesis.
Subgroup analysis and investigation of heterogeneity
Given the small number of common outcomes across studies, we were unable to conduct the planned range of subgroup analyses for our primary outcome to see if there was any evidence of differential responses to the intervention. We included subgroup analysis for length of follow‐up. When studies reported several follow‐up points, we included data from each relevant time point. In addition, we assessed subgroup heterogeneity by examining forest plots and quantification by using the I² statistic.
Had sufficient data been available, we planned to carry out the following subgroup analyses for our primary outcome to see if there was any evidence of differential responses to interventions.
Intervention type: e.g. personal monitoring device, information/education, counselling, text messages or combinations of these categories.
Gender: given the unique sedentary behaviour profiles of men and women (Bennie 2013; Matthews 2008), and the fact that interventions to reduce sedentary behaviour seem to have limited effects when targeting women only (Martin 2015), outcomes by gender should be examined (men, women, men and women).
Socioeconomic group (education or income): because variations in response to public health interventions according to socioeconomic status are frequent (White 2009), outcomes by socioeconomic group should be compared. It has been noted that high levels of education are associated with higher levels of sitting (Bennie 2013).
Age: subgroup analysis to consider the influence of the age of participants.
Intensity of the intervention: using an adapted version of the approach used by Baker 2015.
Category of study setting: as interventions may be setting‐specific, the influence of study setting should be considred (e.g. schools/universities, transport, home).
BMIor another measure of overweight/obesity: to consider the influence of body composition given the evidence that associations between prolonged sitting and risk of CVD are stronger in overweight than in normal weight adults (Chomistek 2013).
Study aim: as previous reviews have demonstrated differential effects between interventions that solely aim to reduce sedentary behaviour or that take a combined approach to reducing sedentary behaviour and increasing physical activity (Gardner 2016; Martin 2015), subgroup analysis to compare outcomes by study intention are warranted.
Baseline sedentary status: as daily sedentary time for adults varies across studies (Bennie 2013), whether baseline sedentary level has an influence on outcomes should be investigated.
Baseline physical activity: influence of baseline physical activity level should be considered.
Sensitivity analysis
Given the small number of studies included in the review, we did not undertake sensitivity analysis. Had sufficient data been available, we planned to use sensitivity analysis for primary outcomes to explore the impact of risk of bias on study findings, while excluding studies at high or unclear risk of bias.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE system to assess the certainty of the body of evidence for each outcome, and to draw conclusions about this within the text of the review. The certainty of a body of evidence as assessed by GRADE is understood as the extent to which one can be confident in the estimate of effect (Guyatt 2008). We summarised the assessment in a 'Summary of findings' table created with GRADEpro software (GRADEpro GDT). Two review authors independently assessed outcomes across studies (EM and KM). We resolved disagreements by consensus.
We rated evidence as very low, low, moderate, or high certainty by considering the GRADE domains. Table 2 presents definitions for these ratings (Balshem 2011). The GRADE approach to rating the quality of evidence begins with the study design (randomised trials start as high quality) and then addresses five reasons to possibly downgrade the quality of evidence (Balshem 2011). The five factors that may lead to downgrading the certainty of evidence are:
1. Definitions for quality ratings in GRADE.
| Quality level | Definition |
| High | Further research is very unlikely to change our confidence in the estimate of effect |
| Moderate | Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate |
| Low | Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate |
| Very low | Any estimate of effect is very uncertain |
study limitations ‐ risk of bias;
publication bias ‐ available evidence derived from a number of small studies;
imprecision ‐ random error;
inconsistency ‐ inconsistency in the magnitude of effect in studies of alternative management strategies (Guyatt 2011a); and
indirectness ‐ indirect participants, interventions, outcomes, or comparisons.
If one of these factors is found to exist, it is classified either as serious (rating down by one level) or as very serious (rating down by two levels). We followed guidance from Ryan 2016 when incorporating the GRADE ratings into the results of the review, so that the certainty of evidence is clear.
Results
Description of studies
See Characteristics of included studies, Characteristics of excluded studies, Characteristics of ongoing studies.
Results of the search
Our searches to 14 April 2020 yielded 21,100 hits from electronic databases and 79 from other studies. This resulted in 10,976 hits following removal of duplicates (Figure 2). The full search strategies and the number of hits for the eight electronic databases and the clinical trials registry can be found in the Appendices. After reading titles and abstracts, we excluded 10,799 records and selected 177 reports for full‐text review. Of these, we excluded 144 reports. We collated multiple reports of the same study, with the paper that reported the outcomes of particular note to this review chosen as the main source of study results. We identified 24 reports, representing 13 unique studies, for inclusion in this review (Arrogi 2017; Barwais 2013; Biddle 2015; Cotten 2016; Ellingson 2016; Finni 2011; French 2011; Jago 2013; Kitagawa 2020Laska 2016; Lioret 2012; Sui 2018; Williams 2019). In addition, we identified eight studies that are classified as ongoing (NCT02909725; ISRCTN58484767; NCT03698903; Latomme; Martin Borras 2014; NCT04257539; Pinto 2017; Schroe 2019). For one study, we could not locate a full‐text version (Marcinkevage 2012), and we categorised this as a study awaiting classification (see Characteristics of studies awaiting classification).
2.
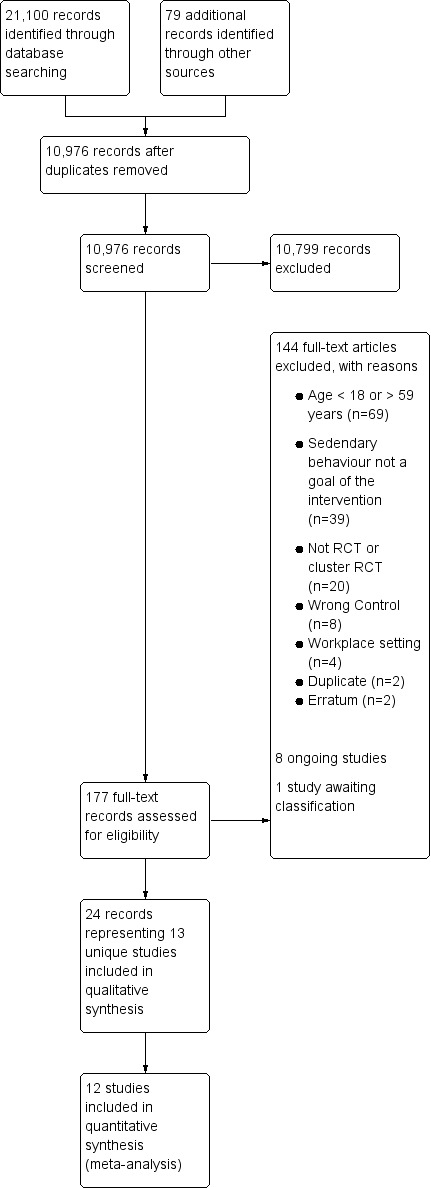
Study flow diagram.
We sent requests to the authors of several studies to obtain additional data or to clarify data (Biddle 2015; Finni 2011; French 2011; Marcinkevage 2012; Martin Borras 2014). We received unpublished data from the authors of two studies (Biddle 2015; Finni 2011).
Included studies
Design
Ten studies are RCTs (Arrogi 2017; Barwais 2013; Biddle 2015; Cotten 2016; Ellingson 2016; Jago 2013; Kitagawa 2020; Laska 2016; Sui 2018; Williams 2019), and three are cluster RCTs (Finni 2011; French 2011; Lioret 2012). See the Characteristics of included studies table for further information. All of the cluster RCTs reported adjusted results; therefore re‐analysis of data was not required. One study included multiple intervention groups (Kitagawa 2020).
Setting
Settings for all studies were outside the workplace and included home/community (Arrogi 2017; Finni 2011; Jago 2013; Kitagawa 2020; Lioret 2012), online (Barwais 2013), primary care (Biddle 2015; Williams 2019), university (Cotten 2016; Ellingson 2016; French 2011; Sui 2018), and community college (Laska 2016).
Three studies were undertaken in the United States (Ellingson 2016; French 2011; Laska 2016), three in the United Kingdom (Biddle 2015; Jago 2013; Williams 2019), two in Australia (Barwais 2013; Lioret 2012), and two in Canada (Cotten 2016; Sui 2018). Finally, one study each was undertaken in Belgium, Finland and Japan (Arrogi 2017; Finni 2011, Kitagawa 2020 respectively),
Participants
The included studies involved 1770 participants. Sample sizes ranged from 30 participants in Ellingson 2016 to 542 participants in Lioret 2012. In nine studies, a majority of participants were female (Arrogi 2017; Biddle 2015; Cotten 2016; Finni 2011; French 2011; Jago 2013; Laska 2016; Lioret 2012; Sui 2018). One study reported that there was not a considerable difference in the proportions of males and females (Ellingson 2016). Another two studies included only females (Kitagawa 2020; Lioret 2012). The mean age of study participants ranged from 20 years in Ellingson 2016 to 41 years in French 2011. Five of the studies involved participants in their 20's (Barwais 2013; Cotten 2016; Ellingson 2016; Laska 2016; Sui 2018). Several studies targeted the family (Finni 2011; Jago 2013; Lioret 2012).
Few studies provided sociodemographic characteristics, apart from gender, using the PROGRESS framework (Place, Race, Occupation, Gender, Religion, Education, Socioeconomic status, Social status). Six studies noted the occupation of participants (97% officer workers in Arrogi 2017; 63% officer workers in Barwais 2013; 100% housewives in Kitagawa 2020; 100% university students in Cotten 2016, Ellingson 2016, and Sui 2018). Six studies reported race/ethnicity (Biddle 2015; Ellingson 2016; French 2011; Jago 2013; Laska 2016; Williams 2019). Biddle 2015 reported that participants were recruited from areas with a diverse ethnic and socioeconomic makeup. Two studies reported income data of participants (French 2011; Laska 2016). Education level was reported in one study (Lioret 2012).One study purposively recruited adults with a diagnosis of a serious mental illness (Williams 2019)
Interventions
Nine studies aimed to reduce sedentary behaviour (Arrogi 2017; Biddle 2015; Cotten 2016; Ellingson 2016; Finni 2011; French 2011; Jago 2013; Kitagawa 2020; Sui 2018), and four sought to both reduce sedentary behaviour and increase physical activity levels (Barwais 2013; Laska 2016; Lioret 2012; Williams 2019). All interventions were delivered at the individual level (i.e. none were considered environmental or policy activities) (see Figure 1). Table 3 provides a summary of the interventions. Three studies used a personal monitoring device (Arrogi 2017; Barwais 2013; Kitagawa 2020). Several studies included some form of information or education (French 2011; Laska 2016; Lioret 2012; Jago 2013), or some type of counselling (Finni 2011; Sui 2018). Two studies included both information/education and a personal monitoring device (Biddle 2015; Ellingson 2016). One study incorporated information/education, a personal monitoring device and counselling (Williams 2019). One study sent daily text messages to participants (Cotten 2016).
2. Summary of the interventions.
| Study | Target group | SB/PA‐related aim | Intervention components | Last follow‐up | Theory |
| Personal monitoring device | |||||
| Arrogi 2017 | Adults aged 18 to 55 years with sedentary jobs and/or predominantly sedentary leisure time | SB | Motion sensor and smartphone app to provide feedback in relation to targets, including a warning signal to modify behaviour | 2 weeks | BCT principles |
| Barwais 2013 | People who reported high total sitting time | SB + PA | Online personal activity monitor to provide feedback on progress towards their daily goal | 4 weeks | NR |
| Kitagawa 2020 | Housewives | SB | Motion sensor and smartphone application to provide feedback on sitting time. The tailored feedback group also received individual suggestions to shorten sitting time. | 2 weeks | NR |
| Information/Education | |||||
| French 2011 | At least one child aged at least 5 years and two household members aged at least 12 years, with weekly average household TV viewing of at least 10 hours per person | SB | 6 monthly face‐to‐face group sessions, monthly newsletters, 12 home‐based activities, a TV‐limiting device, and monthly telephone support calls |
12 months | NR |
| Laska 2016 | Adults aged 18 to 35 years, with BMI of 20 to 34.9 kg/m² | SB + PA | 1 credit course at university plus social networking and a support website | 24 months | Ecological theories of health behaviour, social‐cognitive theory, and social network theory |
| Lioret 2012 | First‐time mothers | SB + PA | 6 quarterly 2‐hour sessions at parent group and a newsletter | 18 months | Theory of anticipatory guidance |
| Jago 2013 | Parents with at least one child aged 6 to 8 years | SB | 8 weekly 2‐hour education sessions | 16 weeks | Self‐determination theory |
| Information/Education plus personal monitoring device | |||||
| Biddle 2015 | Overweight or obese adults aged 18 to 40 years with one or more additional risk factors for diabetes | SB | 1 × 3‐hour group workshop and a self‐monitoring device to view and track progress against personal goals and provide feedback via vibration notifications | 12 months | Bandura’s social‐cognitive theory, Gollwitzer’s implementation intentions concept, Behavioural Choice Theory, and Leventhal’s Common Sense Model |
| Ellingson 2016 | Full‐time students aged 18 to 26 years, reporting more than 3 hours of daily leisure‐time sedentary behaviour | SB | 10 to 15‐minute information session and personal monitor with vibration feedback to modify behaviour towards a set target | 5 weeks | Habit theory |
| Counselling | |||||
| Finni 2011 | Healthy men and women with children aged 3 to 8 years and an occupation where they sit for more than 50% of their work time | SB | Tailored counselling, 2 telephone calls at 1 and 5 months, and motivational emails | 12 months | Theory of planned behaviour |
| Sui 2018 | Full‐time university students aged 18+ years with good physical and mental health |
SB | Counselling sessions with an action plan | 6 weeks | Health action process approach |
| Information/Education plus personal monitoring device plus counselling | |||||
| Williams 2019 | Community dwelling adults with serious mental illness | SB + PA | Initial education session, fortnightly one‐to‐one health coaching, provision of pedometers and access to a weekly walking group |
17 weeks | COM‐B model of behaviour change |
| Daily text messages | |||||
| Cotten 2016 | Adults aged 18 to 65 years | SB | Daily text messages | 6 weeks | NR |
BCT: behaviour change technique.
BMI: body mass index.
NR: not reported.
PA: physical activity.
SB: sedentary behaviour.
In terms of sustainability of the interventions, five included a follow‐up measure of at least 12 months (Biddle 2015; Finni 2011; French 2011; Laska 2016; Lioret 2012).
Control group
The comparison group in five studies was a no intervention control (Arrogi 2017; Barwais 2013; Finni 2011; French 2011; Jago 2013), with one of these specifically instructing participants to follow their normal daily lifestyle patterns (Barwais 2013). Other studies provided information leaflets to the control group regarding sedentary behaviour (Biddle 2015; Kitagawa 2020), or consisting of basic health promotion information (Laska 2016; Lioret 2012; Williams 2019). Three studies used attention control. In one study, participants received daily text messages about random health facts (Cotten 2016), and in another study, participants were given an accelerometer to wear without feedback (Ellingson 2016). Finally in one study, the control group was given strategies to achieve Canada's Food Guide weekly food group servings (Sui 2018).
Outcomes
Primary outcomes
We found 13 studies that reported using two principal forms of continuous outcomes ‐ device‐derived and self‐reported. These were categorised into three groups: device‐measured sedentary time, self‐reported TV viewing, and self‐reported sitting time.
Self‐report measures of sedentary behaviour were utilised in nine studies, device‐based measures were used in four studies, and a further two studies used both. Seven studies used a questionnaire (Biddle 2015; Ellingson 2016; French 2011; Jago 2013; Laska 2016; Lioret 2012; Sui 2018). Two studies used the 7‐Day Sedentary and Light Intensity Physical Activity Log (7‐Day SLIPA Log) (Barwais 2013; Cotten 2016); however in the study by Cotten and colleagues, participants were asked to fill out the items based on a typical weekday and a typical weekend day, rather than on a daily basis. Six studies used a device‐based measure of sedentary time (Arrogi 2017; Biddle 2015; Ellingson 2016; Finni 2011; Kitagawa 2020; Williams 2019). Three of these studies used a thigh‐worn device that measured posture (Arrogi 2017; Biddle 2015; Ellingson 2016) and two studies used a waist‐worn accelerometer (Biddle 2015; Finni 2011), with both using < 100 counts per minute (cpm) as the definition of sedentary. Two further studies used a wrist‐worn accelerometer (Kitagawa 2020; Williams 2019). Note that two of the aforementioned studies included both a device‐based and a self‐report measure of sedentary behaviour (Biddle 2015; Ellingson 2016).
Six studies reported total sedentary time (Arrogi 2017; Barwais 2013; Biddle 2015; Ellingson 2016; Finni 2011; Williams 2019). Several other studies reported sedentary behaviour in one domain only: TV viewing (French 2011; Jago 2013; Laska 2016), or TV, video, and DVD viewing (Lioret 2012). Biddle 2015 reported sedentary behaviour separately for multiple domains: daily sitting time, sitting while travelling, sitting at work, sitting while watching TV, sitting while using a computer at home, and sitting in leisure time. One study reported longest prolonged sitting time (Kitagawa 2020). Five studies presented findings in relation to breaks in sedentary time. Two of these studies reported frequency of breaks in sedentary time (i.e. breaks every X minutes) (Cotten 2016; Sui 2018), and three studies reported number of breaks per hour or day in sedentary time (Arrogi 2017; Biddle 2015; Finni 2011). Arrogi 2017 defined breaks as the number of sit‐to‐stand transitions. Biddle 2015 reported bouts of light to vigorous physical activity as breaks in sedentary time. Finni 2011 defined a break as "an interruption in sedentary time when accelerometer counts rose up to or above 100 counts/min for a minimum of one minute".
Secondary outcomes
We found one study that reported energy expenditure; this was reported specifically in relation to leisure‐time physical activity and was assessed using the Paffenbarger Questionnaire (Laska 2016).
Several studies reported measures of body composition. Two of these reported body fat data; one used total fat mass percentage measured using dual‐energy X‐ray absorptiometry (Finni 2011), and the other reported body fat percentage measured used bioelectrical impedance analysis (Biddle 2015). Three studies reported BMI (Biddle 2015; Finni 2011; French 2011), two studies provided data on weight (Biddle 2015; Finni 2011) and two studies reported waist circumference (Biddle 2015; Williams 2019).
Only one study reported cholesterol as an outcome measure (Biddle 2015). Two studies provided data on glucose control and insulin sensitivity (Biddle 2015; Finni 2011). Both reported fasting glucose and fasting insulin. In addition, Biddle 2015 reported two‐hour post‐challenge glucose and glycosylated haemoglobin (HbA1c). Finni 2011 included homeostatic model assessment of insulin resistance (HOMA‐IR) and homeostatic model assessment of β‐cell function (HOMA‐%B).
One study included mood state as an outcome variable and used a Profle of Mood State (POMS) to assess mood over the course of the previous week (Ellingson 2016). Another study assessed wellness using an online version of the Wellness Evaluation of Lifestyle (WEL) inventory (Barwais 2013).
Five studies reported MVPA as measured by an accelerometer (Biddle 2015; Ellingson 2016; Finni 2011; Jago 2013; Williams 2019). Different methods of classifying moderate and vigorous physical activity were used across studies. Two studies used widely known cut‐points developed by Freedson and Troiano and colleagues (Biddle 2015; Freedson 1998; Jago 2013; Troiano 2008). Finni 2011 used cut‐points calibrated from Troiano 2008. Ellingson 2016 employed the sojourn method (Lyden 2014) and Williams used the thresholds developed by Esliger 2011.
Self‐report physical activity was measured in several studies using a variety of assessment tools including the 7‐Day Sedentary and Light‐Intensity Physical Activity (SLIPA) Log (Barwais 2013; Cotten 2016), the seven‐day physical activity recall questionnaire (Cotten 2016), an unspecified physical activity questionnaire (Lioret 2012), the short form of the International Physical Activity Questionnaire (IPAQ) (Barwais 2013; Biddle 2015), and a modified version of the long‐form IPAQ (French 2011). Ellingson 2016 did not report which version of IPAQ was used. Note that some studies used several self‐report instruments, with each assessing activities of different intensity.
Three studies reported step counts per day. One of these studies measured steps using a thigh‐worn ActivPAL accelerometer (Arrogi 2017), another measured steps using the waist‐worn Actigraph GT3X accelerometer (Biddle 2015) and the third measured steps using a wrist‐worn UP24 accelerometer Kitagawa 2020.
Duration of follow‐up varied across studies. In seven studies, the duration of longest follow‐up was four months or less (Arrogi 2017; Barwais 2013; Cotten 2016; Ellingson 2016; Jago 2013; Kitagawa 2020; Sui 2018); these were defined as providing short‐term follow‐up. Four studies conducted a follow‐up measure between 4 and 12 months (Biddle 2015; Finni 2011; French 2011; Williams 2019); these were considered to provide medium‐term follow‐up. We categorised studies with a follow‐up measure longer than 12 months as providing long‐term follow‐up. Only two studies met this criteria (Laska 2016; Lioret 2012). If studies reported multiple follow‐up time points, the data for each time point were pooled as appropriate with short‐, medium‐ or long‐term studies.
Excluded studies
Risk of bias in included studies
Risk of bias varied across studies (Figure 3). No study was judged to be at low risk of bias across all domains (Figure 4). Only one study was assessed as having low risk of bias in six of the seven domains (Biddle 2015).
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Most studies described a random component in the sequence generation process (Barwais 2013; Biddle 2015; Cotten 2016; Ellingson 2016; Finni 2011Jago 2013; Kitagawa 2020; Laska 2016; Lioret 2012; Sui 2018; Williams 2019); we therefore judged them to be at low risk of bias. Methods included utilising a random number generator (Barwais 2013; Cotten 2016; Ellingson 2016; Lioret 2012), a computer‐generated list or sequence (Biddle 2015; Jago 2013; Kitagawa 2020; Laska 2016), a web service (Sui 2018; Williams 2019), and coin flipping (Finni 2011).
The remaining two studies did not provide sufficient information to permit a judgement (Arrogi 2017; French 2011).
Selection bias due to inadequate concealment of allocations before group assignment was judged as having unclear risk in nine studies due to failure to provide sufficient information to assign a judgement of low or high risk (Arrogi 2017; Barwais 2013; Cotten 2016; Ellingson 2016; Finni 2011; French 2011; Kitagawa 2020; Laska 2016; Sui 2018). Four studies reported appropriate methods used to conceal allocation to intervention or control and were therefore judged as having low risk of bias (Biddle 2015; Jago 2013; Lioret 2012; Williams 2019). Allocation was determined by an independent statistician (Biddle 2015; Jago 2013; Lioret 2012) or researcher (Williams 2019).
Blinding
Due to the nature of the intervention, performance bias was not considered for this review. For detection bias, we considered outcome assessment and outcome assessors separately.
For outcome assessment, six studies included a device‐based measure of sedentary behaviour (Arrogi 2017; Biddle 2015; Ellingson 2016; Finni 2011; Kitagawa 2020; Williams 2019); these were judged to be at low risk of bias. Seven studies used only self‐report measures of sedentary behaviour, and we judged these to have high risk of bias for outcome assessment (Barwais 2013; Cotten 2016; French 2011; Jago 2013; Laska 2016Lioret 2012; Sui 2018).
Regarding blinding of outcome assessors, three studies reported any level of blinding to group assignment among those responsible for data entry or analysis. We therefore judged Ellingson 2016, Kitagawa 2020 and Williams 2019 to be at low risk of bias. Sui 2018 stated that assessors were not blinded to group allocation, and we judged this study to be at high risk of bias. As the remaining studies did not report on blinding, we judged them to have unclear risk of bias (Arrogi 2017; Barwais 2013; Biddle 2015; Cotten 2016; Finni 2011; French 2011; Jago 2013; Laska 2016; Lioret 2012).
Incomplete outcome data
Ten studies were judged to be at low risk for attrition bias. Missing data were similar across groups in seven of these studies (Arrogi 2017; Biddle 2015; Cotten 2016; Finni 2011; French 2011; Lioret 2012; Sui 2018). In Barwais 2013 and Kitagawa 2020 there did not appear to be any missing data. In Ellingson 2016, the reasons provided for missing data were unlikely to be related to the outcome.
Two studies were judged to have high risk of attrition bias, as dropout was not balanced across intervention and control groups (Jago 2013; Williams 2019).
Laska 2016 was considered to be at unclear risk of bias, as reporting of attrition was insufficient to permit a judgement.
Selective reporting
We judged the majority of studies to be at unclear risk for reporting bias as information was insufficient to permit a judgement of high or low risk (Barwais 2013; Ellingson 2016; French 2011; Jago 2013; Kitagawa 2020; Laska 2016; Sui 2018). Three studies were deemed to be at high risk of bias (Cotten 2016; Lioret 2012; Williams 2019). In the case of Lioret 2012 and Williams 2019, some variables outlined in the protocol were not reported. Another study reported that the self‐reported sitting measure was not included in the analysis, and this decision was made after data collection (Cotten 2016).
Other potential sources of bias
We judged the majority of studies to have low risk of other potential sources of bias (Arrogi 2017; Barwais 2013; Biddle 2015; Ellingson 2016; Finni 2011; French 2011; Jago 2013; Laska 2016; Lioret 2012; Williams 2019). Cotten 2016 was deemed to be at high risk of bias as not all instruments used were established validated tools of sedentary behaviour. The remaining two studies were deemed as having unclear risk of bias due to insufficient information to assess whether an important risk of bias exists (Kitagawa 2020; Sui 2018).
Additional risk of bias domains for cluster RCTs
Five additional items were considered for cluster RCTs: recruitment bias; baseline imbalance; loss of clusters; incorrect analysis; and comparability with individually randomised trials.
We judged two studies to be at low risk of recruitment bias (French 2011; Lioret 2012). In Finni 2011, recruitment occurred after randomisation of clusters, and this study was considered to be at high risk of bias.
For baseline imbalance, information was insufficient to permit a judgement of high or low risk; therefore all studies were deemed to be at unclear risk of bias.
French 2011 reported similar dropout across groups; we judged this study to have low risk of bias in relation to loss of clusters. For Finni 2011 and Lioret 2012, information was insufficient to permit a judgement of high or low risk; we therefore judged these studies as having unclear risk of bias.
We judged all three cluster RCTs to have low risk of bias for incorrect analysis (Finni 2011; French 2011; Lioret 2012), as all reported adjusted results.
Regarding the risk of bias associated with comparability with individually randomised trials, one study was considered as having low risk of bias because clustering took place at the level of parent groups, and therefore contamination between groups was unlikely (Lioret 2012). In French 2011, households were recruited from various sites in the community; therefore the possibility of contamination existed. We judged this study as having high risk of bias. Finally, for Finni 2011, information was insufficient to permit a judgement of high or low risk, and this study was therefore deemed to be at unclear risk of bias.
Effects of interventions
See: Table 1
See Table 1 for the main comparison. We present results using only outcomes for which data were available. We were unable to address all of the secondary objectives set for this review due to lack of available data.
Primary outcomes
We pooled studies according to outcome measures.
Device‐measured sedentary time
We pooled four studies that compared effects of the intervention versus control on device‐measured sedentary time with short‐term follow‐up (up to four months) (Arrogi 2017; Biddle 2015; Ellingson 2016; Finni 2011). The interventions probably made little or no difference in device‐measured sedentary time in adults under 60 years of age (mean difference (MD) ‐8.36 min/d, 95% confidence interval (CI) ‐27.12 to 0.40; I² = 0%; Analysis 1.1; Figure 5). Results were imprecise due to wide confidence intervals and small sample sizes. Overall the certainty of evidence was moderate; therefore further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
1.1. Analysis.

Comparison 1: Intervention vs control, Outcome 1: Device‐measured sedentary time
5.

Forest plot of comparison: 1 Intervention vs control, outcome: 1.1 Device‐measured sedentary time (min/day)
Three studies provided data for medium‐term follow‐up (longer than 4 to 12 months) (Biddle 2015; Finni 2011; Williams 2019). We are uncertain whether interventions reduce device‐measured sedentary time in the medium term (MD ‐51.37 min/d, 95% CI ‐126.34 to 23.59; I² = 84%; Analysis 1.1; Figure 5). Results were imprecise due to wide confidence intervals and small sample sizes. In addition we had concerns about risk of bias, with two studies having high risk of bias for several domains. There was also a large variation in effect. The certainty of evidence was very low; therefore any estimate of effect is very uncertain.
Self‐report sitting time
We are uncertain whether interventions outside the workplace reduces self‐reported sitting time in the short term. Evidence was drawn from two studies with 61 participants (Barwais 2013; Ellingson 2016) (MD ‐64.12 min/d, 95% CI ‐260.91 to 132.67; I² = 86%; Analysis 1.2; Figure 6). We had concerns about risk of bias, as several domains were judged to be unclear and outcomes assessment was at high risk of bias. Results were inconsistent due to large variation in effect and high levels of heterogeneity. Both studies recruited participants who reported high levels of sedentary behaviour and employed interventions of similar duration using personal activity monitors. It is unclear why the direct effect was different. In addition, imprecision was evident due to the wide confidence intervals and small sample sizes. Overall the certainty of evidence was very low; therefore any estimate of effect is very uncertain.
1.2. Analysis.

Comparison 1: Intervention vs control, Outcome 2: Self‐report sitting time
6.

Forest plot of comparison: 1 Intervention vs control, outcome: 1.2 Self‐report sitting time (min/d).
Self‐report TV viewing time
Interventions outside the workplace may make little or no difference in self‐reported TV viewing in the medium term (MD ‐12.45 min/d, 95% CI ‐50.40 to 25.49; I² = 86%; Analysis 1.3; Figure 7). We pooled two studies with 459 participants that recorded data at medium‐term follow‐up (French 2011; Laska 2016). The width of confidence intervals raises concerns about imprecision. We determined that studies were at high risk of bias for outcome assessment, and we judged several other domains to be unclear.
1.3. Analysis.

Comparison 1: Intervention vs control, Outcome 3: Self‐report TV viewing time
7.

Forest plot of comparison: 1 Intervention vs control, outcome: 1.3 Self‐report TV viewing time (min/day)
We pooled two studies that provided data for the comparison at long‐term follow‐up (> 12 months) (Laska 2016; Lioret 2012). Interventions may make little or no difference in self‐report TV viewing in the long term (MD 0.30 min/d, 95% CI ‐0.63 to 1.23; I² = 0%; Analysis 1.7; Figure 7). Sample sizes were large, but the large confidence intervals led to uncertainty. There was high risk of bias for outcome assessment, and we judged several other domains to be at unclear risk.
Overall the certainty of evidence for self‐report TV viewing time was low; therefore further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Breaks in sedentary time
It was not possible to pool all studies that reported breaks in sedentary time given the variation in the definition used for a "break" (Arrogi 2017; Biddle 2015; Cotten 2016; Finni 2011; Sui 2018). Table 4 provides a summary of data collection methods, break definitions, and study findings.
3. Summary of studies reporting breaks in sedentary time.
| Study | Definition of break in sedentary time | Measure | Findings |
| Arrogi 2017 | Number of sit‐to‐stand transitions per day | ActivPAL Monitor | Short‐term follow‐up: MD 5.7 per day (94% CI 1.0 to 10.4) |
| Biddle 2015 | Bouts of light to vigorous physical activity per day | Actigraph Accelerometer | Short‐term follow‐up: MD ‐29.6 (95% CI ‐97.0 to 37.9) Medium‐term follow‐up: MD ‐2.96 (95% CI ‐73.0 to 67.0) |
| Cotten 2016 | Frequency of breaks to "get up and move around every day" (break every X minutes). Options were provided every 30 minutes or less, 45 minutes, 60 minutes, 75 minutes, 90 minutes, 120 minutes, 180 minutes, or 240 minutes or longer | Questionnaire | Short‐term follow‐up: MD ‐10.25 (‐25.58 to 5.08) |
| Finni 2011 | An interruption in sedentary time when accelerometer counts rose up to or above 100 counts/min for a minimum of 1 minute. Breaks per sedentary hour | Alive Technologies Accelerometer | Short‐term follow‐up: MD 1.0 (95% CI ‐0.2 to 2.2) Medium‐term follow‐up: MD 0.6 (95% CI ‐0.6 to 1.8) |
| Sui 2018 | Frequency of interrupting sitting time (break every X minutes). Options included less than every 30 min, every 30 to 45 min, every 45 minutes to 1 hour, every 1 to 1.5 hours, every 1.5 to 2 hours, every 2 to 3 hours, every 3 to 4 hours, every 4 to 5 hours, over every 5 hours, no interruption | Questionnaire | Short‐term follow‐up: MD ‐53.12 (‐96.98 to ‐9.28) |
CI: confidence interval.
MD: mean difference.
In Arrogi 2017 a mean difference in sit‐to‐stand transitions of 5.7 per day (95% CI 1.0 to 10.4 ) was reported at short‐term follow‐up. Biddle 2015 reported the number of breaks in sedentary behaviour per day (i.e. light to vigorous PA bouts) at short‐term (MD ‐29.6, 95% 95% CI ‐97.0 to 37.9) and medium‐term follow‐up (MD ‐2.96, 95% CI ‐73.0 to 67.0). Cotten 2016 reported self‐reported frequency of breaks at short‐term follow‐up (MD ‐10.25, 95% CI ‐25.58 to 5.08). Finni 2011 reported device‐determined breaks per sedentary hour during leisure time at short‐term (MD 1.0, 95% CI ‐0.2 to 2.2) and medium‐term follow‐up (MD 0.6, 95% CI ‐0.6 to 1.8). In Sui 2018, a MD of ‐53.12 (‐96.98 to ‐9.28) in self‐reported break frequency was found at short‐term.
Secondary outcomes
Energy expenditure
Laska 2016 reported that the intervention did not change energy expenditure in leisure‐time physical activity at 24 months (MD ‐66.5 weekly kcal).
Body composition
We pooled three studies that reported medium‐term follow‐up points for body mass index (Biddle 2015; Finni 2011; French 2011) (MD ‐0.25 kg/m², 95% CI ‐0.48 to ‐0.01; I² = 0%; moderate‐certainty evidence; Analysis 1.4). Most studies had high risk of bias for two domains. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Biddle 2015 also reported data for short‐term follow‐up (MD ‐13.3 kg/m², 95% CI ‐15.0 to 41.6).
1.4. Analysis.

Comparison 1: Intervention vs control, Outcome 4: Body mass index
Biddle 2015 reported no changes in waist circumference at 3 months (MD 13.4 cm, 95% CI ‐14.7 to 41.5). We pooled two studies that report waist circumference at medium‐term follow‐up (Biddle 2015; Williams 2019) (MD ‐2.04 cm 95% CI ‐9.06 to 4.98, I² = 65%; low‐certainty evidence; Analysis 1.5). There were concerns about imprecision due to small sample size. In addition, one study had high risk of bias for two domains. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
1.5. Analysis.

Comparison 1: Intervention vs control, Outcome 5: Waist circumference
Biddle 2015 reported no change in body fat percentage at 3 months (MD 0.54, 95% CI ‐38.4 to 39.5) or at 6 months (MD ‐0.25, 95% CI ‐2.72 to 2.22). In Finni 2011, there was no change in total fat mass percentage at 6 months (MD ‐0.54, 95% CI ‐1.2 to 0.11) or at 12 months (MD ‐0.60, 95% CI ‐1.26 to 0.07); however percentage leg lean mass changed between groups at 12 months (MD 0.48, 95% CI 0.18 to 0.77), and a decrease within the control group was observed.
Biddle 2015 reported no changes in body weight at 3 months (MD 14.3 kg, 95% CI ‐16.1 to 44.6) or at 6 months (MD 0.46 kg, 95% CI ‐5.06 to 5.97), whereas Finni 2011 reported changes at 6 months (MD ‐0.83 kg, 95% CI ‐1.64 to ‐0.02) and at 12 months (MD ‐0.95 kg, 95% CI ‐1.76 to ‐0.13).
Cholesterol
Only one study reported the effects of the intervention on cholesterol (Biddle 2015). No changes were noted for serum total cholesterol (MD 0.21 mmol/L, 95% CI ‐0.15 to 0.40), HDL cholesterol (MD 0.06 mmol/L, 95% CI ‐0.02 to 0.14; P= 0.122), triglycerides (MD ‐0.17 mmol/L, 95% CI, ‐0.42 to 0.08), or LDL cholesterol (MD 0.13 mmol/L, 95% CI ‐0.10 to 0.36) at 3 months and at 12 months (findings for 12 months are shown).
Markers of insulin resistance
We pooled two studies (Biddle 2015; Finni 2011 that reported glucose (Biddle 2015; Finni 2011) at short‐term follow‐up (MD ‐0.18 mmol/L, 95% CI ‐0.30 to ‐0.06, I² = 0%; moderate‐certainty evidence; Analysis 1.6) and medium‐term follow‐up (MD ‐0.08 mmol/L, 95% CI ‐0.21 to 0.05, I² = 0%; moderate‐certainty evidence; Analysis 1.6). There were concerns in relation to risk of bias as unclear or high for several domains. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
1.6. Analysis.

Comparison 1: Intervention vs control, Outcome 6: Glucose
Finni 2011 noted no change in insulin at 3 months (MD ‐0.55 pM, 95% CI ‐9.15 to 8.05) or at 6, 9, or 12 months (MD ‐1.47 pM, 95% CI ‐10.3 to 7.37).
Biddle 2015 reported two‐hour glucose challenge at 3 months (MD ‐0.08 mmol/L, 95% CI ‐0.63 to 0.46) and 12 months (MD 0.10 mmol/L, 95% CI ‐0.65 to 0.84). No changes were seen in HbA1c at 3 months (MD 0.01%, 95% CI ‐0.08 to 0.11) or at 12 months (MD 0.06%, 95% CI ‐0.04 to 0.16).
Finni 2011 reported HOMA‐%B at 3 months (MD 12.62, 95% CI ‐6.81 to 32.05) and 12 months (MD 7.93, 95% CI ‐12.1 to 27.96).
Inflammatory markers
No data were reported.
Meaures of carotid intima media thickness
No data were reported.
Measures of endothelial function
No data were reported.
Meaures of mental health
Mood
Ellingson 2016 reported a group by time interaction for mood state, favouring the intervention group (F1,27 = 4.17; P = 0.05).
Wellness
Barwais 2013 revealed a time by treatment effect on total wellness (F1,31 = 9.5; P < 0.001), with increases in wellness scores seen in the intervention group (t17 = ‐6.5; P < 0.001).
Adverse events and symptoms
No data were reported.
Unintended outcomes
Device‐measured moderate to vigorous physical activity
Interventions outside the workplace may make little or no difference in device‐measured MVPA in the short term (MD 1.99 min/d, 95% CI ‐4.27 to 8.25; I² = 23%; low‐certainty evidence; Analysis 1.7; Figure 8). Four studies with 296 participants provided data for this outcome (Biddle 2015; Ellingson 2016; Finni 2011; Jago 2013). Most studies had unclear or high risk of bias in several domains. Small sample sizes and wide confidence intervals raised concerns about imprecision. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
1.7. Analysis.

Comparison 1: Intervention vs control, Outcome 7: Device‐measured MVPA
8.

Forest plot of comparison: 1 Intervention vs control, outcome: 1.6 Device‐measured MVPA (min/day)
We are uncertain whether interventions improve device‐measured MVPA in the medium term (MD 6.59 min/d, 95% CI ‐7.35 to 20.53; I² = 70%; very low‐certainty evidence; Analysis 1.7). Three studies with 214 participants were pooled (Biddle 2015; Finni 2011;Williams 2019). Results were imprecise due to wide confidence intervals and small sample sizes. Two studies had unclear or high risk of bias for several domains. In addition there was a large variation in effect. The certainty of evidence was very‐low and any estimate of effect is very uncertain.
Self‐report moderate to vigorous physical activity
French 2011 reported self‐report MPVA at medium‐term follow‐up (MD 29.6331 min/d; 95%CI 4.60 ‐ 54.66).
Self‐report light‐intensity physical activity
Two studies with 115 participants reported data on light‐intensity PA, assessed using the 7‐Day SLIPA Log (Barwais 2013; Cotten 2016). We are uncertain whether interventions outside the workplace improve light‐intensity PA in the short‐term (MD 156.32 min/d, 95% CI 34.34 to 278.31; I² = 79%; Analysis 1.8). Results were inconsistent due to large variation in effect and high levels of heterogeneity. We had very serious concerns about precision due to the very large confidence intervals. In addition, risk of bias was high for outcome assessment and unclear for several domains. The certainty of evidence was very low, meaning that any estimate of effect is very uncertain.
1.8. Analysis.

Comparison 1: Intervention vs control, Outcome 8: Self‐report light PA
Self‐report moderate‐intensity physical activity
Three studies reported self‐report moderate‐intensity PA with short‐term follow‐up. Cotten 2016 reported moderate‐intensity activity as minutes per week with a MD of 50.39 (95% CI ‐76.27 to 177.05). Barwais 2013 found a MD of 457.0 MET/min per week (95%CI 202.43 to 711.58).The third study found a MD of ‐22.10 min/d (95%CI ‐87.59 to 43.39) (Ellingson 2016).
Self‐report vigorous‐intensity physical activity
Barwais 2013 reported vigorous‐intensity physical activity in MET‐minutes per week and found a MD of 540.00 (95% CI 129.53 to 950.47) at short‐term follow‐up. Ellingson 2016 reported minutes per day of vigorous activity at short‐term (MD ‐15.60, 95% CI ‐33.37 to 2.17). Biddle 2015 found a MD of ‐2.5 vigorous METs at short‐term (95% CI ‐536.9 to 531.8) and ‐242.0 (95% CI ‐849.9 to 365.8) at long‐term follow‐up.
Self‐report total physical activity
Lioret 2012 found no change in self‐report total physical activity at long‐term follow‐up (MD 0.75 min/week, 95% CI ‐0.90 to 2.40).
Steps
We pooled three studies that reported step count at short‐term follow‐up (Arrogi 2017; Biddle 2015; Kitagawa 2020) (MD 226.90 steps/day, 95% CI ‐519.78 to 973.59, I² = 0%; low‐certainty evidence; Analysis 1.9). There were concerns about imprecision due to large confidence internals and small sample sizes. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
1.9. Analysis.

Comparison 1: Intervention vs control, Outcome 9: Steps
Biddle 2015 also reported data for medium‐term follow‐up and found no change in average steps per day (MD 402.7, 95% CI ‐807.9 to 1613.4).
Discussion
Summary of main results
We included 13 studies in this review. A synopsis of findings for the primary outcomes of device‐measured sedentary time, self‐report sitting time, and self‐report TV viewing time can be seen in Summary of findings table 1. Interventions outside the workplace to reduce sedentary behaviour probably make little or no difference in device‐measured sedentary time in adults under 60 years of age in the short term (moderate‐certainty evidence). We are uncertain whether such interventions reduce device‐measured sedentary time in the medium term (very low‐certainty evidence). We are uncertain whether interventions outside the workplace reduce self‐reported sitting time in the short term (very low‐certainty evidence). Interventions may make little or no difference in self‐reported TV viewing time (low‐certainty evidence). We were unable to pool studies that reported breaks in sedentary time due to the multiple ways that studies defined a break.
We were able to complete meta‐analyses for only five of the secondary outcomes: body mass index, waist circumference, device‐measured moderate to vigorous physical activity (MVPA), self‐report light‐intensity physical activity (PA) and step count. Interventions outside the workplace to reduce sedentary behaviour probably make little or no difference in BMI among adults under 60 years of age in the medium term (moderate‐certainty evidence). Interventions outside the workplace may make little or no difference in device‐measured MVPA in the short term (low‐certainty evidence). We are uncertain whether interventions increase device‐measured MVPA in the medium term (very low‐certainty evidence) . We are uncertain whether interventions outside the workplace improve self‐report light‐intensity PA (very low‐certainty evidence). Interventions outside the workplace may make little or no difference in daily step count in the short term (low‐certainty evidence)
A majority of study participants were female and were aged 20 to 41 years. Two studies reported follow‐up measures undertaken more than 12 months post baseline. Despite six studies assessing outcomes using device‐based measures, the overall certainty of evidence was determined as moderate to very low.
All interventions were delivered at the individual level, and none were considered environmental or policy activities. Interventions at an individual level included information/education, counselling, wearable technology, apps, SMS prompts, web‐based interventions and phone calls. Interventions were delivered in home or community settings, within primary care or educational settings. Details of the frequency and intensity of these different elements and their fidelity were missing. No interventions yielded data on cost‐effectiveness, quality of life, or adverse events.
Overall completeness and applicability of evidence
A majority of studies recruited female participants and younger participants (aged 20 to 41) in high‐income countries. Therefore it is not clear to what extent these types of interventions might be effective among other population groups.
The identified studies were insufficient to address all of the objectives of the review. We could not investigate most of the secondary outcomes (related to health effects) due to absence of eligible studies reporting these outcomes. BMI status was reported in only three studies. No studies reported data on adverse events or cost‐effectiveness.
We were unable to determine whether specific components of interventions are associated with changes in sedentary behaviour. In addition, we could not examine if there were any differential effects of interventions based on health inequalities. Very few studies reported sociodemographic characteristics at baseline and endpoint using the PROGRESS framework (Place, Race, Occupation, Gender, Religion, Education, Socioeconomic status, Social status). No studies were conducted in low‐ or middle‐income countries, and we found a dearth of quality research in marginalised and poorer populations.
This review was limited to trials involving a randomised controlled trial (RCT) or cluster RCT study design. It is possible that other evidence is available from other, less robust, studies.
Overall the evidence presented may not hold true for middle‐aged adults and those from low‐middle‐income countries (for which trials were not available) or for adults over 60 years of age (outside the scope of the review).
Quality of the evidence
The body of evidence identified does not allow a robust conclusion regarding the objectives of this review. We included data from 13 studies and 1770 participants. We found certainty of evidence, according to GRADE, to range from very low to moderate. Uncertainty was mainly due to concerns about imprecision, risk of bias, and inconsistency. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Available studies demonstrate that it is possible to conduct RCTs of non‐workplace interventions to reduce sedentary behaviour; however no studies were considered to have low risk of bias. In addition to the limitations of self‐report tools, a common challenge to undertaking high‐quality trials relates to blinding of outcome assessments. Blinding was possible in studies that used device‐based measures. Most studies used self‐report measures of sedentary behaviour. These measures are subject to recall bias and may lack precision; however any misclassification is non‐differential (as both intervention and control groups complete the measure) and attenuates the effects of the intervention (Richards 2013). We also note that the use of self‐report measures and the wide ranges of values for sedentary behaviours could contribute to uncertainty around intervention effects. Although none of our studies blinded participants to their group allocation, we believe that this criterion was not appropriate because it is very difficult to do this for any intervention that requires movement.
Potential biases in the review process
Assessing risk of bias and certainty of the body of evidence (GRADE) involves personal judgement and the potential for some degree of subjectivity (Hombali 2019). We tried to minimise the potential for bias by ensuring that two review authors conducted these assessments independently. To avoid language bias, we did not impose any language restrictions in our searches. To increase the likelihood that all relevant studies were identified, we (1) emailed trial authors and research groups for information about unpublished or ongoing studies, (2) contacted experts in the field and asked them to identify further articles, (3) handsearched reference lists of included studies and key systematic reviews, and (4) searched a clinical trial registry and the websites of organisations involved in addressing and reporting research on sedentary behaviour.
One limitation of this review is the potential for publication bias. Unpublished studies may exist but have not been submitted or accepted for publication, or only those with positive results may have been published. However we were unable to examine a funnel plot due to the small numbers of studies with common outcome measures. One principal investigator declared receiving in‐kind support through provision of a sit‐to‐stand desk by Ergotron from 2012‐2014. This study reported no intervention effects (Biddle 2015).
Agreements and disagreements with other studies or reviews
This is the first review of interventions intended to change sedentary behaviour delivered in contexts outside of workplaces. This review is relevant, as adults spend approximately 70% of their non‐work time being sedentary, plus not all adults work.
A recent systematic review reported that 10 of the 13 studies observed a reduction in objectively measured sitting time (Thraen‐Borowski 2017). However this review included non‐randomised and uncontrolled studies. Another review ‐ including only RCTs ‐ noted that effects reported between 7 and 12 months were not sustained beyond 12 months, with high heterogeneity between studies (Martin 2015). However only eight non‐workplace studies were identified for the review. In addition, in the subgroup analysis by study setting (workplace vs home/community), no attempt was made to discriminate between interventions that were designed to increase physical activity and those that purposely aimed to reduce sedentary behaviour. This is important, as the same review and another demonstrated differential effects between interventions that solely aim to reduce sedentary behaviour or take a combined approach of reducing sedentary behaviour and increasing physical activity (Gardner 2016).
We were concerned that most of our studies recruited younger adults outside of workplace settings; this has the potential to increase health inequalities (i.e. differential responses in recruitment and focus on effects on the younger and potentially more active). We support the conclusions of these reviews that it remains a priority to identify what is a clinically meaningful change in sedentary behaviour.
Authors' conclusions
Implications for practice.
It is currently unclear what interventions outside of the workplace, if any, might be effective for reducing sedentary behaviour. Interventions outside the workplace probably has little or no difference on device‐measured sedentary time in the short term and we are uncertain whether they reduce sedentary time in the medium term. Evidence is uncertain about the effects of non‐workplace interventions on self‐reported sitting time in the short term. Interventions may result in little or no difference in self‐report TV viewing time in the medium or long term.
We were not able to draw conclusions about the effectiveness of individual components of the interventions, and we are unable to demonstrate what the most effective strategies were within the interventions. We cannot comment on the balance of benefits or harms, as no studies provided data for adverse events, quality of life, or cost‐effectiveness. The decision for policymakers or practitioners to recommend interventions outside the workplace for adults under 60 years should consider the certainty of this evidence base.
Many of the interventions used some type of feedback mechanism to encourage participants to reduce their sedentary behaviour time. This feedback about current behaviour is a common strategy used in physical activity interventions. Feedback was generated by devices and/or self‐monitoring. Encouragement to take the opportunity to stand (in non‐workplace settings) was included in a few studies, but this may prove still to be a difficult behaviour to undertake in an unsupportive environment (e.g. modified desks or tables). Unless the environment can support the behaviour, future attempts to change sedentary behaviour will prove difficult to start and maintain.
We note that, particularly in high‐income countries, there is much media attention on the use of home equipment or furniture to reduce sedentary behaviour. Recent estimates of the market value of the standing desk industry suggest that the global market will grow to US$ 2.80 billion by 2025 (Credence Research 2017). However, the unit cost of such equipment or furniture may mean that they are available only for those who can afford them, and practitioners may wish to consider (if proved effective) whether this intervention is an equitable option.
Implications for research.
Future RCTs are clearly needed to build and improve this evidence base by assessing the impact of interventions outside the workplace for reducing sedentary behaviour in adults under 60 years of age for at least 6 to 12 months and ideally beyond 12 months. Methods of measurement need careful consideration in future research on sedentary behaviour outcomes. Blinding of the outcome assessment was possible in studies that used device‐based measures; therefore a transition towards greater use of device‐based measures in future studies would help to overcome some of the limitations of the current evidence base. However, until standard methods of data collection, preparation, and analysis are adopted, it will prove difficult to compare effects of studies. This is a research priority. For most studies, it is unclear whether outcome assessors were blinded; therefore better executed and reported studies are needed.
To address concerns about imprecision, studies with larger sample sizes in experimental and control groups are needed. Future studies must recruit participants from varying age, socioeconomic, and ethnic groups to examine differential effects in relevant subgroups. In addition, study authors should gather quality of life, cost‐effectiveness, and adverse event data. We suggest that studies adopt the use of PAT plots (graphical representations of interventions) to show intervention components and intensity (Perera 2007). Studies conducted to examine environmental or policy level interventions are needed. It may be particularly prudent for future trials to evaluate the effectiveness of interventions that are potentially scalable at the population level.
History
Protocol first published: Issue 2, 2017 Review first published: Issue 7, 2020
Notes
'Physical inactivity' and 'insufficient physical activity' are sometimes used to refer to failing to meet physical activity guidelines. In both cases, this is distinct from 'sedentary behaviour', for which a definition already exists (see Sedentary Behaviour Research Network 2012).
Acknowledgements
We acknowledge feedback from the CPHG Editorial Team, Philip Baker (Contact Editor), and the CPHG Search Trials Co‐ordinator.
We thank Sharon Lewis (Lancaster Patient Safety Research Unit, Royal Lancaster Infirmary) for her advice on using Covidence.
Appendices
Appendix 1. Search Strategies
Medline (OvidSP) [1946‐present]
| # ▲ | Searches | Results |
| 1 | Sedentary Lifestyle/ | 8983 |
| 2 | (sedentary or sitting or seated).ti. | 10110 |
| 3 | ((sedentary or sitting or seated) adj5 (behavio* or lifestyle or life‐style)).ti,ab. | 10341 |
| 4 | (sedentary adj3 (adult? or men or women or males or females or individuals or people or population?)).ti,ab. | 5931 |
| 5 | ((sedentary or sitting or seated) adj5 time).ti,ab. | 5596 |
| 6 | ((sedentary or sitting or seated or inactiv* or underactiv* or under activ*) and (computer* or television or tv or video game? or videogame? or gaming)).ti,ab. | 4882 |
| 7 | (time adj5 (computer* or television or tv or video game? or videogame? or gaming or screen or media)).ti,ab. | 11932 |
| 8 | ((watch* or view*) adj5 (television or tv)).ti,ab. | 5139 |
| 9 | (play* adj5 (video game? or videogame? or computer game?)).ti,ab. | 1825 |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 | 43650 |
| 11 | adult/ or middle aged/ or young adult/ | 6462178 |
| 12 | (adult* or men or women or males or females).ti,ab. | 2645941 |
| 13 | 11 or 12 | 7719230 |
| 14 | 10 and 13 | 22453 |
| 15 | (occupational or workplace or work place).ti. | 61004 |
| 16 | 14 not 15 | 22173 |
| 17 | randomized controlled trial.pt. | 503795 |
| 18 | controlled clinical trial.pt. | 93619 |
| 19 | randomized.ab. | 476077 |
| 20 | placebo.ab. | 206825 |
| 21 | clinical trials as topic.sh. | 190741 |
| 22 | randomly.ab. | 331110 |
| 23 | trial.ti. | 216504 |
| 24 | 17 or 18 or 19 or 20 or 21 or 22 or 23 | 1281334 |
| 25 | exp animals/ not humans.sh. | 4689936 |
| 26 | 24 not 25 | 1178813 |
| 27 | 16 and 26 | 3891 |
Embase (OvidSP) [1974‐present]
| # ▲ | Searches | Results |
| 1 | sedentary lifestyle/ or physical inactivity/ | 18698 |
| 2 | (sedentary or sitting or seated).ti. | 11582 |
| 3 | ((sedentary or sitting or seated) adj5 (behavio* or lifestyle or life‐style)).ti,ab. | 13720 |
| 4 | (sedentary adj3 (adult? or men or women or males or females or individuals or people or population?)).ti,ab. | 7470 |
| 5 | ((sedentary or sitting or seated) adj5 time).ti,ab. | 7151 |
| 6 | ((sedentary or sitting or seated or inactiv* or underactiv* or under activ*) and (computer* or television or tv or video game? or videogame? or gaming)).ti,ab. | 6446 |
| 7 | (time adj5 (computer* or television or tv or video game? or videogame? or gaming or screen or media)).ti,ab. | 15746 |
| 8 | ((watch* or view*) adj5 (television or tv)).ti,ab. | 6693 |
| 9 | (play* adj5 (video game? or videogame? or computer game?)).ti,ab. | 2230 |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 | 62334 |
| 11 | adult/ or middle aged/ or young adult/ | 7312914 |
| 12 | (adult* or men or women or males or females).ti,ab. | 3611863 |
| 13 | 11 or 12 | 8976075 |
| 14 | 10 and 13 | 32131 |
| 15 | (occupational or workplace or work place).ti. | 68227 |
| 16 | 14 not 15 | 31796 |
| 17 | randomized controlled trial/ or single blind procedure/ or double blind procedure/ or crossover procedure/ | 668799 |
| 18 | (random or ((singl* or doubl*) adj (blind* or mask*)) or crossover or cross over or factorial* or latin square or assign* or allocat* or volunteer*).ti,ab. | 1342908 |
| 19 | 17 or 18 | 1692983 |
| 20 | (exp animals/ or nonhuman/) not human/ | 6489517 |
| 21 | 19 not 20 | 1510668 |
| 22 | 16 and 21 | 5556 |
PsycINFO (OvidSP)[1967‐present]
| # ▲ | Searches | Results |
| 1 | SEDENTARY BEHAVIOR/ | 1444 |
| 2 | (sedentary or sitting or seated).ti. | 2211 |
| 3 | ((sedentary or sitting or seated) adj5 (behavio* or lifestyle or life‐style)).ti,ab. | 3088 |
| 4 | (sedentary adj3 (adult? or men or women or males or females or individuals or people or population?)).ti,ab. | 1188 |
| 5 | ((sedentary or sitting or seated) adj5 time).ti,ab. | 1659 |
| 6 | ((sedentary or sitting or seated or inactiv* or underactiv* or under activ*) and (computer* or television or tv or video game? or videogame? or gaming)).ti,ab. | 1395 |
| 7 | (time adj5 (computer* or television or tv or video game? or videogame? or gaming or screen or media)).ti,ab. | 5255 |
| 8 | ((watch* or view*) adj5 (television or tv)).ti,ab. | 5562 |
| 9 | (play* adj5 (video game? or videogame? or computer game?)).ti,ab. | 2794 |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 | 17366 |
| 11 | (adulthood 18 yrs older or middle age 40 64 yrs or thirties 30 39 yrs or young adulthood 18 29 yrs).ag. | 2E+06 |
| 12 | (adult* or men or women or males or females).ti,ab. | 824589 |
| 13 | 11 or 12 | 2E+06 |
| 14 | 10 and 13 | 10089 |
| 15 | (occupational or workplace or work place).ti. | 23524 |
| 16 | 14 not 15 | 9982 |
| 17 | (random* or trial* or controlled stud* or placebo* or ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) or cross over or crossover or factorial* or latin square or assign* or allocat* or volunteer*).ti,ab,hw,id. | 461035 |
| 18 | clinical trial.md. | 26139 |
| 19 | 17 or 18 | 465051 |
| 20 | 16 and 19 | 2010 |
CINAHL (EBSCOHost)[1982‐present]
| S10 | S7 NOT S8 Limiters ‐ Clinical Queries: Therapy ‐ Best Balance | 1,843 |
| S9 | S7 NOT S8 | 12,705 |
| S8 | TI occupational or workplace or work place | 39,495 |
| S7 | S3 AND S6 | 12,875 |
| S6 | S4 OR S5 | 2,137,408 |
| S5 | TI ( adult* or men or women or males or females ) OR AB ( adult* or men or women or males or females ) | 1,076,441 |
| S4 | (MH "Adult") OR (MH "Middle Age") OR (MH "Young Adult") | 1,626,645 |
| S3 | S1 OR S2 | 23,165 |
| S2 | TI ( sedentary or sitting or seated ) OR AB ( ((sedentary or sitting or seated) N5 (behavio* or lifestyle or life‐style)) ) OR AB ( (sedentary N3 (adult? or men or women or males or females or individuals or people or population?)) ) OR AB ( ((sedentary or sitting or seated) N5 time) ) OR AB ( ((sedentary or sitting or seated or inactiv* or underactiv* or under activ*) and (computer* or television or tv or video game? or videogame? or gaming)) ) OR AB ( (time N5 (computer* or television or tv or video game? or videogame? or gaming or screen or media)) ) OR AB ( ((watch* or view*) N5 (television or tv)) ) OR AB ( (play* N5 (video game? or videogame? or computer game?)) ) | 19,374 |
| S1 | (MH "Life Style, Sedentary") | 8,588 |
Cochrane Central Register of Controlled Trials (CENTRAL) [Issue 5 of 12, May 2018] and Cochrane Database of Systematic Reviews (CDSR) [Issue 6 of 12, June 2018]Database of Abstracts of Reviews of Effects (DARE) [Issue 2 of 4, April 2015) – all on Cochrane Library via Wiley
| Search | Terms |
| #1 | MeSH descriptor: [Sedentary Lifestyle] explode all trees |
| #2 | sedentary or sitting or seated:ti (Word variations have been searched) |
| #3 | ((sedentary or sitting or seated) near (behavio* or lifestyle or life‐style)):ti,ab,kw (Word variations have been searched) |
| #4 | (sedentary near/3 (adult? or men or women or males or females or individuals or people or population?)):ti,ab,kw (Word variations have been searched) |
| #5 | ((sedentary or sitting or seated) near time):ti,ab,kw (Word variations have been searched) |
| #6 | ((sedentary or sitting or seated or inactiv* or underactiv* or "under activ*") and (computer* or television or tv or "video game?" or videogame? or gaming)):ti,ab,kw (Word variations have been searched) |
| #7 | (time near (computer* or television or tv or "video game?" or videogame? or gaming or screen or media)):ti,ab,kw (Word variations have been searched) |
| #8 | ((watch* or view*) near (television or tv)):ti,ab,kw (Word variations have been searched) |
| #9 | (play* near ("video game?" or videogame? or "computer game?")):ti,ab,kw (Word variations have been searched) |
| #10 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 |
| #11 | MeSH descriptor: [Adult] this term only |
| #12 | MeSH descriptor: [Middle Aged] explode all trees |
| #13 | MeSH descriptor: [Young Adult] explode all trees |
| #14 | adult* or men or women or males or females:ti,ab,kw (Word variations have been searched) |
| #15 | #11 or #12 or #13 or #14 |
| #16 | #10 and #15 |
| #17 | occupational or workplace or work place:ti (Word variations have been searched) |
| #18 | #16 not #17 |
SPORTDiscus (EBSCOHost)
| S9 | S7 AND S8 | 1,362 |
| S8 | (random* or trial* or controlled stud* or placebo* or ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) or cross over or crossover or factorial* or latin square or assign* or allocat* or volunteer*) | 121,463 |
| S7 | S5 NOT S6 | 5,346 |
| S6 | TI occupational or workplace or work place | 4,573 |
| S5 | S3 AND S4 | 5,373 |
| S4 | TI ( adult* or men or women or males or females ) OR AB ( adult* or men or women or males or females ) | 304,975 |
| S3 | S1 OR S2 | 12,649 |
| S2 | TI ( sedentary or sitting or seated ) OR AB ( ((sedentary or sitting or seated) N5 (behavio* or lifestyle or life‐style)) ) OR AB ( (sedentary N3 (adult? or men or women or males or females or individuals or people or population?)) ) OR AB ( ((sedentary or sitting or seated) N5 time) ) OR AB ( ((sedentary or sitting or seated or inactiv* or underactiv* or under activ*) and (computer* or television or tv or video game? or videogame? or gaming)) ) OR AB ( (time N5 (computer* or television or tv or video game? or videogame? or gaming or screen or media)) ) OR AB ( ((watch* or view*) N5 (television or tv)) ) OR AB ( (play* N5 (video game? or videogame? or computer game?)) ) | 11,843 |
| S1 | (DE "SEDENTARY behavior" OR DE "SEDENTARY lifestyles") OR (DE "SEDENTARY people" OR DE "SEDENTARY women") | 2,885 |
ClinicalTrials.govhttp://clinicaltrials.gov
| Search terms | Limits: | Hits: |
| Title=sedentary | Adult: 18‐65 | 462 |
| Condition=sedentary | Adult: 18‐65 | 736 |
| Title=inactive OR inactivity | Adult: 18‐65 | 523 |
| Condition=inactive OR inactivity | Adult: 18‐65 | 819 |
| Total: | 2440 | |
| Duplicates: | 1674 | |
| Final total: | 766 |
Data and analyses
Comparison 1. Intervention vs control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Device‐measured sedentary time | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 Short‐term follow‐up (up to 4 months) | 4 | 262 | Mean Difference (IV, Random, 95% CI) | ‐8.36 [‐27.12, 10.40] |
| 1.1.2 Medium‐term follow‐up (> 4 months to 12 months) | 3 | 188 | Mean Difference (IV, Random, 95% CI) | ‐51.37 [‐126.34, 23.59] |
| 1.2 Self‐report sitting time | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.2.1 Short‐term follow‐up (up to 4 months) | 2 | 61 | Mean Difference (IV, Random, 95% CI) | ‐64.12 [‐260.91, 132.67] |
| 1.3 Self‐report TV viewing time | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.3.1 Medium‐term follow‐up (> 4 months to 12 months) | 2 | 459 | Mean Difference (IV, Random, 95% CI) | ‐12.45 [‐50.40, 25.49] |
| 1.3.2 Long‐term follow‐up (> 12 months) | 2 | 709 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.63, 1.23] |
| 1.4 Body mass index | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4.1 Medium‐term follow‐up (> 4 months to 12 months) | 3 | 326 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.48, ‐0.01] |
| 1.5 Waist circumference | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.5.1 Medium‐term follow‐up (> 4 months to 12 months) | 2 | 160 | Mean Difference (IV, Random, 95% CI) | ‐2.04 [‐9.06, 4.98] |
| 1.6 Glucose | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 Short‐term follow‐up (up to 4 months) | 2 | 263 | Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.30, ‐0.06] |
| 1.6.2 Medium‐term follow‐up (> 4 months to 12 months) | 2 | 238 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.21, 0.05] |
| 1.7 Device‐measured MVPA | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.7.1 Short‐term follow‐up (up to 4 months) | 4 | 296 | Mean Difference (IV, Random, 95% CI) | 1.99 [‐4.27, 8.25] |
| 1.7.2 Medium‐term follow‐up (> 4 months to 12 months) | 3 | 214 | Mean Difference (IV, Random, 95% CI) | 6.59 [‐7.35, 20.53] |
| 1.8 Self‐report light PA | 2 | 115 | Mean Difference (IV, Random, 95% CI) | 156.32 [34.34, 278.31] |
| 1.8.1 Short‐term follow‐up (up to 4 months) | 2 | 115 | Mean Difference (IV, Random, 95% CI) | 156.32 [34.34, 278.31] |
| 1.9 Steps | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.9.1 Short‐term follow‐up (up to 4 months) | 3 | 204 | Mean Difference (IV, Random, 95% CI) | 226.90 [‐519.78, 973.59] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arrogi 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: flyer and email in the local area Study SB/PA objective/aim: short‐term effectiveness of the stAPP smartphone‐based intervention on prolonged sitting behavior in healthy adults. It was hypothesised that use of stAPP would result in more interruptions in prolonged sitting. More specifically, we expected (1) a decrease in total prolonged sitting time and (2) a decrease in the number and duration of prolonged sitting bouts Country: Belgium Setting: home/community Study dates: recruitment between November 2013 and March 2014; study duration: 2 weeks |
|
| Participants |
Included criteria: convenience sample, 18 to 55 years. Desk‐bound job and/or predominantly sedentary leisure time. Able to work a smartphone Excluded criteria: none stated Baseline characteristics Intervention
Control
Overall
Pretreatment: sociodemographic variables and work characteristics did not differ between groups except for age. Specifically, the control group was found to be older than the intervention group: 39.2 (11.5) years vs 33.6 (8.3) years. No significant baseline differences emerged in any of the activPAL parameters between intervention and control groups (P > 0.05) |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: Department of Welfare, Public Health and Family of the Flemish Government Author's name: An Bogaerts Institution: KU Leuven Email: an.bogaerts@kuleuven.be Address: Faculty of Kinesiology and Rehabilitation Sciences, KU Leuven, Leuven, Belgium Conflicts of interest declared: not stated Publication type: journal article |
|
| Notes | Clinical trial number NCT01975870 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Unclear risk | No information reported to allow judgement |
| Allocation concealment | Unclear risk | No information reported |
| Blinding of outcome assessors | Unclear risk | Not reported |
| Blinding of outcome assessment (sedentary time) Sedentary time | Low risk | Device‐based measure |
| Incomplete outcome data | Low risk | Missing data similar across groups |
| Selective reporting | Low risk | Study protocol available on clinical trials registry. The study’s prespecified outcomes have been reported |
| Other sources of bias | Low risk | None |
Barwais 2013.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: advertisements in local newsletters, flyers, and emails at a metropolitan university in Brisbane, Australia, during October/November 2012 Study SB/PA objective/aim: to reduce sedentary behaviour and increase physical activity levels in daily living Country: Australia Setting: university recruitment/online delivery Study dates: recruitment during October/November 2012; study duration: 4 weeks (data collection at baseline and at 4 weeks) |
|
| Participants |
Included criteria: only those who reported a high total sitting time, defined as spending > 7 hours per day, were invited to participate in the study Excluded criteria: NR Baseline characteristics Intervention
Control
Overall
|
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: NR Author's name: Faisal A Barwais Institution: Queensland University of Technology and Umm Al‐Qura University Email: faisal.barwais@student.qut.edu.au Address: School of Exercise and Nutrition Sciences, Institute of Health and Biomedical Innovation, Queensland University of Technology, Brisbane, Australia Publication type: journal article and PhD thesis Conflicts of interest declared: "The author declares that they have no competing interests" |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | Computer random number generator was used |
| Allocation concealment | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessors | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | "7‐Day Sedentary and Light‐Intensity Physical Activity Log (7‐Day SLIPA Log)" |
| Incomplete outcome data | Low risk | No data appear to be missing |
| Selective reporting | Unclear risk | Insufficient information to permit judgement. No protocol published |
| Other sources of bias | Low risk | No comments |
Biddle 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: recruited from primary care in Leicestershire and Northamptonshire. Invitations were sent from the general practitioner to potential participants Study SB/PA objective/aim: to reduce sitting time Country: England Setting: primary care Study dates: 9 March 2011 to 23 October 2012; study duration: 12 months (data collected at baseline and at 3 and 12 months after baseline) |
|
| Participants |
Included criteria: (1) age 18 to 40 years inclusive; (2) BMI in the obese range (> 30 kg/m² with > 27.5 kg/m² for South Asians) or BMI in the overweight range (> 25 kg/m² with > 23 kg/m² for South Asians) and with 1 or more additional risk factors for diabetes from (a) family history of diabetes or cardiovascular disease in a first‐degree relative; (b) previous gestational diabetes; (c) polycystic ovarian syndrome; (d) HbA1c > 5.8%; (e) impaired glucose tolerance; and/or (f) impaired fasting glucose Excluded criteria: NR Baseline characteristics Intervention
Control
Overall
Pretreatment: random assignment led to the control group being slightly older and having fewer females than the intervention group, but these differences were small |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: the STAND study was funded by a grant from the Medical Research Council (UK) under the National Prevention Research Initiative (Project #91409). The research was also supported by the National Institute for Health Research (NIHR) Diet, Lifestyle, Physical Activity Biomedical Research Unit based at University Hospitals of Leicester and Loughborough University, the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care–East Midlands (NIHR CLAHRC–EM), and the Leicester Clinical Trials Unit Author's name: Stuart Biddle Institution: Institute of Sport, Exercise Active Living, Victoria University Email: stuart.biddle@vu.edu.au Address: Melbourne, Australia Conflicts of interest declared Stuart Biddle: funding has been received since 2013 for consultancy work from Fitness First, Nuffield Health, and Unilever. None of these are currently active. Funding was received in 2016 for consultancy work for Halpern PR Limited. In‐kind support through provision of a sit‐to‐stand desk was provided by Ergotron from 2012 to 2014. Unpaid advice has been requested by and offered to Bluearth, Active Working, and Get Britain Standing Charlotte L Edwardson: no conflicts of interest to disclose Trish Gorely: no conflicts of interest to disclose Emma G Wilmot: no conflicts of interest to disclose Thomas Yates: no conflicts of interest to disclose Myra A Nimmo: discloses that funding has been received from Technogym during this trial Kamlesh Khunti: no conflicts of interest to disclose Melanie J Davies: no conflicts of interest to disclose. Publication type: journal article × 3 (protocol, main results, process evaluation), conference abstract, additional data received from study authors |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | Randomisation (stratified by age, sex, and ethnicity) was set up by an independent statistician using a computer‐generated list and was conducted remotely |
| Allocation concealment | Low risk | Determined in advance, remotely, by an independent statistician |
| Blinding of outcome assessors | Unclear risk | No information on who conducted the outcomes assessments |
| Blinding of outcome assessment (sedentary time) Sedentary time | Low risk | "The primary outcome was a reduction in sedentary behaviour at 12 months, measured using the Actigraph GT3X accelerometer" Comment: device‐based measure |
| Incomplete outcome data | Low risk | Similar number/proportion lost to follow‐up across groups. "In total, 30 (32%) in the intervention group and 25 (27%) in the control group were lost to follow‐up at 12 months" |
| Selective reporting | Low risk | Protocol available. All outcomes reported (see Supplementary Table 4 for secondary outcomes by randomisation group) |
| Other sources of bias | Low risk | No comment |
Cotten 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: study was advertised through emails sent out to various faculties at Western University, and students who were interested in the study emailed the researcher to sign up. The study was also advertised through an article in the university newspaper due to the interest of a reporter Study SB/PA objective/aim: increasing non‐sedentary behaviours in university students Country: Canada Setting: University Study dates: January to March 2015; study duration: measures taken at baseline and at 2, 4, and 6 weeks |
|
| Participants |
Included criteria: participants had to be between the ages of 18 and 65, had to be able to read and write in English, had to own a mobile phone with free unlimited incoming text messages, and had to be a student at Western University Excluded criteria: none reported Baseline characteristics Intervention
Control
Overall
Pretreatment: groups were equivalent at baseline for all measures (all P values > 0.05) |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: none declared Authors name: Emma Cotten Institution: Western University Email: ecotten@uwo.ca Address: Exercise and Health Psychology LaboratorySchool of KinesiologyWestern UniversityRoom 408, Arthur and Sonia Labatt Health Sciences BuildingLondon, ON, N6A 5B9 Canada Conflicts of interest declared: "none declared" Publication type: journal article and MA thesis |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | Computer‐generated randomised stratification |
| Allocation concealment | Unclear risk | "randomised by the researcher" |
| Blinding of outcome assessors | Unclear risk | No mention of who conducted assessments. Surveys were sent via email. Intervention and control groups received the same emails and surveys. Surveys were administered through a third party website called SoSCI |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | "sedentary and light‐intensity physical activity (SLIPA) questionnaire" |
| Incomplete outcome data | Low risk | "Taken together, all missing data were considered random" Similar dropout across groups |
| Selective reporting | High risk | "Although the SLIPA provides a measure of sedentary behavior, the goal of this text intervention was to directly target and positively change standing and light‐intensity physical activity. After careful examination of the sedentary behavior items (items 1, 5, 6, 15, 16, 17, and 18), it became evident that some items were not relevant to the text intervention (e.g. driving a car) or overlapped each other (e.g. sitting‐studying, writing, desk work, typing vs sitting‐using a computer) causing many overestimated data points. For these reasons, this sitting measure was not calculated and used in subsequent analyses" |
| Other sources of bias | Low risk | No comment |
Ellingson 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: recruited from a large midwestern university using posted flyers and word of mouth. To improve generalisability to the broader university population, participants were recruited using stratified sampling to enrol equal numbers of males and females and no more than 2 students from a single major Study SB/PA objective/aim: using wearable technology to reduce sedentary time in daily life Country: USA Setting: university Comments: study dates: NR Study duration: 9 weeks (5‐week intervention, follow‐up 4 weeks after end of intervention) |
|
| Participants |
Included criteria: (1) being full‐time students, (2) between the ages of 18 and 26 years, (3) absence of mobility limitations, (4) self‐reporting of more than 3 hours of daily leisure‐time sedentary behaviour Excluded criteria: NR Baseline characteristics Intervention
Control
Overall
Pretreatment: there were no significant differences in physical activity between groups at baseline |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: this work was funded by the American College of Sports Medicine's Paffenbarger–Blair Fund for Epidemiological Research on Physical Activity. Jacob Meyer was supported by a National Research Service Award from the Health Resources and Services Administration T32HP10010 to the University of Wisconsin Department of Family Medicine and Community Health Author's name: Laura D Ellingson Institution: Iowa State University Email: ellingl@iastate.edu Address: Department of Kinesiology, Iowa State University, 239 Forker, Ames, IA 50011 Conflicts of interest declared: "The authors have no conflicts of interest" Publication type: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "they were randomly assigned (using a random number generator) to one of two groups" |
| Allocation concealment | Unclear risk | Method of concealment not described |
| Blinding of outcome assessors | Low risk | "data entry and quality checking of accelerometer data at the single‐subject level were conducted by study personnel who were blind to the group assignment" |
| Blinding of outcome assessment (sedentary time) Sedentary time | Low risk | "...received a set of monitors to objectively measure sedentary (activPAL3™ VT (AP)) and physical activity behaviours (ActiGraph GT3X+ (AG)) over the subsequent 7 d under free‐living conditions" Comment: device‐based measure |
| Incomplete outcome data | Low risk | "One participant in the MEC group did not complete the study because of scheduling difficulties, and one participant (also in MEC) had AP malfunctions during baseline testing; both of these individuals were in the fall cohort" Comment: reasons provided for missing data |
| Selective reporting | Unclear risk | No protocol published |
| Other sources of bias | Low risk | No comment |
Finni 2011.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Methods of recruitment: by delivering advertisements to parents via kindergartens and primary schools that have been pre‐randomised to control and intervention groups after balancing different environmental and socioeconomic regions within the city Study SB/PA objective/aim: reduce sedentary time Country: Finland Setting: community Study dates: recruitment started in April 2011; study duration: 12 months (data collected at baseline and at 3, 6, 9, and 12 months) |
|
| Participants |
Included criteria: healthy men and women with children 3 to 8 years old, having an occupation where they self‐reportedly sit more than 50% of their work time Excluded criteria: self‐reported chronic, long‐term musculoskeletal disease or progressive neurological disease, diagnosed cardiovascular or metabolic disease with regular medication, families with pregnant mother at baseline and BMI > 35 Baseline characteristics Intervention
Control
Overall
Pretreatment: significant difference in age between groups at baseline |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: Ministry of Education and Culture, Finland (DNRO 42/627/2010) Author's name: Taija Finni Institution: University of Jyväskylä Email: taija.finni@jyu.fi Address: Neuromuscular Research Center, Department of Biology of Physical Activity, University of Jyväskylä, Jyväskylä, Finland Conflicts of interest declared: "the authors declare that they have no competing interests" Publication type: 3 journal articles (including protocol) and PhD thesis |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "The 14 regions were randomised by flipping a coin to select intervention (n = 7) and control (n = 7) regions within each cluster" |
| Allocation concealment | Unclear risk | No information provided |
| Blinding of outcome assessors | Unclear risk | It does not state who the assessor was and whether the assessor was blinded |
| Blinding of outcome assessment (sedentary time) Sedentary time | Low risk | Device‐based measure |
| Incomplete outcome data | Low risk | "Between the baseline and 12 month follow‐up, seven participants dropped out from the control group (11%) and nine from the intervention group (13%), from which two (3%) withdrew before the allocated intervention" Similar dropout across groups |
| Selective reporting | High risk | Not all data are reported (e.g. occupational stress, quality of life, family influence questionnaire) |
| Other sources of bias | Low risk | NR |
| Recruitment bias (cluster RCT only) | High risk | "The recruitment is performed in the city of Jyväskylä, Finland, by delivering advertisements to parents via kindergartens and primary schools which have been pre‐randomised to control and intervention groups" Recruitment after randomisation of clusters |
| Baseline imbalance (Cluster RCT only) | Unclear risk | NR |
| Loss of clusters (Cluster RCT only) | Unclear risk | Not stated |
| Incorrect analysis (Cluster RCT only) | Low risk | "Intervention effectiveness was tested with linear mixed‐effects model fit by REML in statistical programming language R (R 3.0.1, NLME package, the R foundation for Statistical Computing). The analysis was based on a three level hierarchy, where the random grouping variables participants (n=133) where nested within families (n=89), and families were nested within the clusters (n=7)" |
| Comparability with individually randomized trials (Cluster RCT only) | Unclear risk | "In the randomization, the areas within the city centre and in different types of suburbs were balanced. Regarding socioeconomic regions, information from city registry was used to balance the areas. Thus, in each type of environment and socioeconomic region, there were to be two or more kindergartens and/or primary schools that were then randomized into control and intervention groups" Comment: possibility of herd effect due to diffusion of information within clusters, and contamination of control clusters if they knew of the intervention |
French 2011.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel groups Study SB/PA objective/aim: reduce TV viewing Methods of recruitment: households (HHs) were recruited from the community over an 8‐month period. Recruitment sources included community libraries, worksites, schools, daycare centres, health clinics, religious institutions, park and recreation centres, grocery stores, and food co‐ops Country: USA Setting: university Comments: study dates:study duration: 12 months |
|
| Participants |
Included criteria: (1) at least 1 child ≥ 5 years of age and 2 HH members ≥ 12 years of age; (2) residence in a private house or apartment within 20 miles of the university; (3) HH TV viewing weekly average ≥ 10 hours per person; (4) no HH members with dietary, medical, psychological, or physical limitations that would prevent their participation in intervention activities; and (5) willingness to be randomised to active intervention or control group Excluded criteria: NR Baseline characteristics Intervention
Control
Overall
Pretreatment: not reported |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: this study was supported by grants #1U54CA116849 and #R21CA137240 from the National Institutes of Health/National Cancer Institute Author's name: Simone French Institution: University of Minnesota Email: frenc001@umn.edu Address: Division of Epidemiology Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota, USA Publication type: journal article Conflicts of interest declared: study authors declared no conflict of interest |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Unclear risk | No information provided |
| Allocation concealment | Unclear risk | No information provided |
| Blinding of outcome assessors | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | "TV viewing and computer use hours per day were self‐reported using a standard set of questions" |
| Incomplete outcome data | Low risk | Similar number lost to follow‐up in each group |
| Selective reporting | Unclear risk | No protocol available |
| Other sources of bias | Low risk | No comment |
| Recruitment bias (cluster RCT only) | Low risk | Recruitment took place before randomisation |
| Baseline imbalance (Cluster RCT only) | Unclear risk | Insufficient information to permit judgement |
| Loss of clusters (Cluster RCT only) | Low risk | Similar dropout across groups |
| Incorrect analysis (Cluster RCT only) | Low risk | "The study is a cluster randomized trial in which households (HHs) are randomized to intervention or control condition. In such a situation, it is imperative that HH be included in the statistical model as a random effect nested within randomization condition. Data are presented individually to the calculation of the maximum likelihood but are modeled as correlated within HH. The analysis essentially estimates an HH mean outcome, adjusted for individual characteristics, and analyses these means" |
| Comparability with individually randomized trials (Cluster RCT only) | High risk | "HHs were recruited from the community over an 8‐month period. Recruitment sources included community libraries, worksites, schools, daycare centres, health clinics, religious institutions, park and recreation centres, grocery stores, and food co‐ops" Comment: possibility of contamination |
Jago 2013.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Methods of recruitment: participants were recruited via leaflets and advertisements that were distributed across the community in coffee shops, children’s centres, play groups, school playgrounds, and community centres and face‐to‐face in schools and community centres. Parents were invited to meet the study team at an informal coffee morning at their child’s school or local community venue or to contact the study team by telephone Study SB/PA objective/aim: to reduce parents' TV viewing Country: UK Setting: community Study dates: not reported; study duration: 16 weeks |
|
| Participants |
Included criteria: participants were parents with at least 1 child 6 to 8 years of age recruited from 2 neighbouring wards in Bristol (UK) Excluded criteria: NR Baseline characteristics Intervention
Control
Overall
Pretreatment: control and intervention groups appear balanced on all variables at baseline except for parents’ weekend MVPA, where intervention parents engaged in fewer minutes of MVPA than control parents (36.4 vs 53.0 minutes per day) |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
|
|
| Identification |
Sponsorship source: this project was funded by a project grant from the British Heart Foundation (PG/10/025/28302) Author's name: Russ Jago Institution: University of Bristol Email: Russ.Jago@bristol.ac.uk Address: Centre for Exercise, Nutrition Health Sciences, School for Policy Studies, University of Bristol, Bristol, UK Publication type: journal article Conflicts of interest declared: Professor Stewart‐Brown is Vice‐Chair of Parenting UK (http://www.parentinguk.org/) |
|
| Notes | . | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | Computer‐generated random sequences |
| Allocation concealment | Low risk | "Participants who consented to take part were randomised, within their chosen course preference to the intervention or control arm by an independent statistician with no other involvement in the study" |
| Blinding of outcome assessors | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | "Using a validated scale, parents were also asked to report the average number of hours per day that both they and the target child spent watching television" Comment: self‐reported measure |
| Incomplete outcome data | High risk | "As a result, 25 participants allocated to the intervention group and 23 allocated to the control group provided baseline data. Some data were provided by 23 intervention and 15 control group participants at first follow up, and by 22 intervention and 11 control group participants at the second follow‐up. Three intervention and 12 control group participants dropped out of the study during follow‐up stages; 9 because of lost contact, 3 because they no longer wanted to take part" Comment: dropout not balanced across groups (see Figure SA in additional file) |
| Selective reporting | Unclear risk | No protocol available |
| Other sources of bias | Low risk | No comment |
Kitagawa 2020.
| Study characteristics | ||
| Methods |
Study design: Randomised controlled trial Study grouping: Parallel group Recruitment: Study SB/PA objective/aim: We examined strategies to shorten housewives’ sitting time. Country: Japan Setting: Sartphone app for use at home Study dates: 2014 ‐ 2015 Study duration: One week intervention (plus additional week for baseline data collection) |
|
| Participants |
Included criteria: aged ≧20 and <50 years, housewife (defined as being dedicated to housework without paid work, including part‐time jobs), had a child who was in lower than primary school, and did not have a disease or was undergoing treatment. Excluded criteria: NR Baseline characteristics Intervention group 1
Intervention group 2
Control
Overall
Pretreatment: No significant differences were found in the age and BMI among the three groups before the intervention. Differences in PA and SB between the groups at baseline were not looked at or not reported. |
|
| Interventions |
Intervention characteristics Intervention group 1 (self‐feedback)
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes |
|
| Identification |
Sponsorship source: NR Author's name: Tomomi Kitagawa Institution: Osaka Prefecture University Email: t‐kitagawa@reha.shijonawate‐gakuen.ac.jp Address: Graduate School of Comprehensive Rehabilitation, Osaka Prefecture University, 3‐7‐30 Habikino, Habikino city, Osaka 583‐8555, Japan Conflicts of interest declared: NR Publication type: Journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "Computer generated random numbers table" |
| Allocation concealment | Unclear risk | Not reported |
| Blinding of outcome assessors | Low risk | "The staff who performed assessments or interventions were masked as to participants group assignments." |
| Blinding of outcome assessment (sedentary time) Sedentary time | Low risk | Accelerometer used |
| Incomplete outcome data | Low risk | "None of the participants dropped out during the intervention, and all participants completed the measurements during the first and second weeks." |
| Selective reporting | Unclear risk | Insufficient information to permit judgement |
| Other sources of bias | Unclear risk | Insufficient information to assess whether an important risk of bias exists |
Laska 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Methods of recruitment: colleges were required to agree to (1) allow project staff on campus to recruit students; (2) offer the one‐credit weight management course through their college and help with logistics of making the course available to students; and (3) allow staff to conduct student measurements on campus. The university agreed to cover all costs related to conducting the research. CHOICES study staff recruited students to participate in the study with help from the administrative offices at the colleges using a variety of approaches, including email invitations, posters and table tents in the college, and information tables staffed by CHOICES staff Study SB/PA objective/aim: physical activity and sedentary behaviours Country: USA Setting: 3 Minnesota community colleges Study dates: 2011‐2014; study duration: 24 months |
|
| Participants |
Included criteria: eligibility requirements included being 18 to 35 years old; having BMI of 20 to 34.9 kg/m²; and planning to be in the geographic area for ≥2 years. Original study eligibility requirements included BMI of 20 to 29.9 kg/m²; due to challenging participant enrolment in this population and initial interest from students with BMI ≥ 30 kg/m², investigators expanded the BMI inclusion criteria to 20 to 34.9 kg/m² after enrolment began Excluded criteria: individuals with BMI ≥ 35 kg/m² were ineligible because (1) CHOICES was a weight gain prevention trial, and (2) individuals with BMI ≥ 35 kg/m² have different intervention needs for weight loss. Additional EARLY trial criteria excluded participants with significant health problems Baseline characteristics Intervention
Control
Overall
Pretreatment: the only marginally significant sociodemographic or behavioural difference between intervention and control conditions was for percentage of participants identifying as white (intervention 76.3%, control 68.7%; P = 0.07) |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: this study was 1 of 7 randomised, controlled trials funded as part of the EARLY Trials consortium (Early Adult Reduction of weight through LifestYle intervention, earlytrials.org). This research was supported through a grant from NHLBI (1 U01 L096767‐01). Additional salary support was provided by Grant Number K07CA126837 from the National Cancer Institute Author's name: Melissa N Laska Institution: School of Public Health, Division of Epidemiology and Community Health, Minneapolis, MN, USA Email: mnlaska@umn.edu Address: University of Minnesota, School of Public Health, Division of Epidemiology and Community Health, 1300 S. 2nd Street, Suite 300, Minneapolis, MN 55454, United States Conflicts of interest declared: study authors have no conflicts of interest to declare Publication type: 2 journal articles |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "Blocked randomization was determined using computer‐generated randomization" |
| Allocation concealment | Unclear risk | "The randomization sequence was generated by the study programmer" |
| Blinding of outcome assessors | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | Self‐report questionnaire used to report TV viewing |
| Incomplete outcome data | Unclear risk | Missing data not addressed in the article. Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting | Unclear risk | Protocol not published |
| Other sources of bias | Low risk | No comment |
Lioret 2012.
| Study characteristics | ||
| Methods |
Study design: cluster randomised controlled trial Study grouping: parallel group Methods of recruitment: mothers were recruited via pre‐existing first‐time parent groups. A 2‐stage random sampling design was used to select first‐time parent groups across all socioeconomic position areas Country: Australia Setting: community (parent groups) Study dates: not reported;study duration: 18 months Study SB/PA objective/aim: to improve engagement in PA and decrease TV viewing |
|
| Participants |
Included criteria: first‐time parent groups; literacy in English and a minimum of 8 parents (in fact, mothers) in the groups consenting to participate (6 in low socioeconomic indices for areas) Excluded criteria: infants with chronic health problems likely to influence height, weight, physical activity, or eating behaviours were excluded from the analyses but could participate in the study Baseline characteristics Intervention
Control
Overall
Pretreatment: no differences were observed at baseline in any sociodemographic variables between intervention and control groups |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes
|
|
| Identification |
Sponsorship source: SL is supported by a Deakin University Alfred Deakin Postdoctoral Fellowship. KJC and DC are supported by fellowships from the Victorian Health Promotion Foundation. ACS was supported by a Deakin University Postgraduate Research Scholarship. KH is supported by a National Heart Foundation of Australia Career Development Award. SAM is supported by an Australian Research Council Future Fellowship. The Melbourne Infant Feeding Activity and Nutrition Trial (InFANT) Program was funded by an Australian National Health and Medical Research Council Project Grant (number 425801) Author's name: Sandrine Lioret Institution: Deakin University Email: sandrine.lioretsuteau@deakin.edu.au Address: Centre for Physical Activity and Nutrition Research; C‐PAN, School of Exerciseand Nutrition Sciences; Deakin University, 221 Burwood Hwy, Burwood,Victoria 3125, Australia Publication type: 2 journal articles Conflicts of interest declared: study authors declare that they have no competing interests |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "Randomization was undertaken using a computer‐generated random number schedule" |
| Allocation concealment | Low risk | "Developed by a statistician who had no contact with the centers" |
| Blinding of outcome assessors | Unclear risk | Insufficient information to permit judgement |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | "Mothers also reported the usual time spent watching television or videos/DVD’s on both weekdays and weekend days" Comment: self‐report measure |
| Incomplete outcome data | Low risk | People with missing data were excluded from the analysis. Dropout was fairly even across groups |
| Selective reporting | High risk | Some variables in the protocol are not reported (e.g. BMI) |
| Other sources of bias | Low risk | No comment |
| Recruitment bias (cluster RCT only) | Low risk | "First‐time parents groups will be randomised after recruitment in order to ensure baseline equivalence and minimise selection bias" |
| Baseline imbalance (Cluster RCT only) | Unclear risk | "No differences were observed at baseline in any sociodemographic variables between intervention and control groups, or between those retained or eliminated from the analyses (data not presented)" Comment: refers to groups overall rather than possible differences in clusters |
| Loss of clusters (Cluster RCT only) | Unclear risk | Unclear if any clusters (parent groups) dropped out |
| Incorrect analysis (Cluster RCT only) | Low risk | "Clustering by first‐time parents’ group was accounted for in all models" |
| Comparability with individually randomized trials (Cluster RCT only) | Low risk | Clustering at parents' group level ‐ contamination unlikely |
Sui 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: recruitment posters distributed by the university’s poster distribution service onto specific poster boards on the university campus, emails to participants in previous studies conducted by the research group, and referrals from other participants, as well as Facebook posts in each faculty student page Country: Canada Setting: university Study dates: January to December 2016; study duration: 8 weeks Study SB/PA objective/aim: increase occupational (student) break frequency and decrease break duration |
|
| Participants |
Included criteria: (1) 18 years of age or older, (2) a student attending university full‐time, and (3) in self‐reported good mental and physical health Excluded criteria: pregnant and/or unable to read and write in English Baseline characteristics Intervention
Control
Overall
Pretreatment: there were no differences between groups for break frequency or duration at baseline |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
|
|
| Identification |
Sponsorship source: NR Author's name: Wuyou Sui Institution: University of Western Ontario Email: wsui3@uwo.ca Address: Department of Kinesiology, The University of Western Ontario, 1151 Richmond St., London, Ontario, N6A 3K7 Canada Conflicts of interest declared: NR Publication type: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "Randomisation into groups was determined using the Research Randomizer web service" |
| Allocation concealment | Unclear risk | Not stated |
| Blinding of outcome assessors | High risk | "Research staff, participants, and assessors were not blinded to group allocation" |
| Blinding of outcome assessment (sedentary time) Sedentary time | High risk | "Participants completed an SB questionnaire that assessed break frequency and duration of student SB" Comment: self‐report |
| Incomplete outcome data | Low risk | "Taken together, all missing data were considered random. Hence, an intent‐to‐treat last observation carried forward was used to handle missing data" Comment: no differences between completers and dropouts and similar level of dropout between intervention and control |
| Selective reporting | Unclear risk | Protocol not published |
| Other sources of bias | Unclear risk | Insufficient information to assess whether an important risk of bias exists |
Williams 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: care coordinators (case managers) were asked to identify and refer eligible service users. All service users referred to the study who met our criteria were sent a letter explaining the study with a follow‐up telephone call a week later. Study SB/PA objective/aim: "We developed a health coaching intervention (Walk this Way) to reduce SB and increase PA in people with serious mental illness (SMI) living in the community" Country: UK Setting: Community Mental Health Team in South London Study dates: September 2015 ‐ October 2017 Study duration: 17 week intervention |
|
| Participants |
Included criteria: a diagnosis of any SMI (ICD‐10 clinical diagnosis of a schizophrenia spectrum disorder (F20–29), bipolar affective disorder (F31) or serious depression (F32.3); meeting any one of the following criteria as determined by a care coordinator (case manager): i) overweight, ii) at risk of or have diabetes, iii) in the clinician’s view, have a sedentary lifestyle, iv) or smoke tobacco; ability to provide informed consent; ability to understand English and over 18 years of age. Excluded criteria: under the age of 18, not having a diagnosis of SMI and unable to give informed consent. Baseline characteristics Intervention
Control
Overall
Pretreatment: levels of activity did not differ significantly between the two groups at baseline. |
|
| Interventions |
Intervention characteristics Intervention
Control
|
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement)
Other outcomes |
|
| Identification |
Sponsorship source: This research was supported by the Maudsley Charity and the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London (NIHR CLAHRC South London) at King’s College Hospital NHS Foundation Trust. BS is supported by Health Education England and the National Institute for Health Research HEE/NIHR CA Programme Clinical Lectureship (ICA‐CL‐2017‐03‐001). No funding source had any role in the design and conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review or approval of the manuscript. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. Author's name: Julie Williams Institution: King’s College London Email: julie.williams@kcl.ac.uk Address: Health Service and Population Research Department, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK Conflicts of interest declared: FG has received support or honoraria for CME, advisory work and lecturesfrom Bristol‐ Myers Squibb, Janssen, Lundbeck, Otsuka, Roche, and Sunovion,and has a family member with professional links to Lilly and GSK, includingshares. TC has received honoraria and travel support from pharmacompanies Lundbeck UK, Sanofi Aventis and Otsuka. He holds researchgrants from governmental and charitable research organisations. All otherauthors declare they have no conflicts of interest. Publication type: Journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sequence generation | Low risk | "random sequence generator (https://www.random.org)" |
| Allocation concealment | Low risk | "randomisation was done by a researcher independent of the study" |
| Blinding of outcome assessors | Low risk | "The researchers conducting the baseline assessment were unaware of which arm the participant had been allocated to when completing the baseline assessment" |
| Blinding of outcome assessment (sedentary time) Sedentary time | Low risk | "All participants were asked to wear a wrist‐worn GENEActiv accelerometer" |
| Incomplete outcome data | High risk | "Two intervention participants did not have accelerometer data at follow up so accelerometer data at follow up is for 31 participants. At 6 months 21 participants had accelerometer data, with 8 in the intervention group and 13 in the control group. We therefore calculated the mean minutes for SB and each classification of PA over three consecutive days for which we had the most complete data at baseline. Follow‐up data was available for 33 participants, resulting in a retention rate of 82.5%." |
| Selective reporting | High risk | Accelerometer protocol is different between protocol ("All participants will be required to wear a wrist‐worn GENEActiv accelerometer for at least 4 days (including 1 weekend day if possible) at baseline") and results paper ("We therefore calculated the mean minutes for SB and each classification of PA over three consecutive days for which we had the most complete data at baseline.") Protocol also states that IPAQ would be used but data is not reported in the resutls paper: "(IPAQ) [25] will be used to capture self‐reported physical activity and sedentary behaviour.". Protocol also states "number of disruptions in sedentary behaviour" as a secondary outcome, but this is not reported in results paper. |
| Other sources of bias | Low risk | The study appears to be free of other sources of bias. |
apo: apolipoprotein.
BMI: body mass index.
CG: control group.
FITT: frequency, intensity, time, and type.
FMS: fundamental movement skills.
HAPA: health action process approach.
HbA1c: glycosylated haemoglobin.
HDL: high‐density lipoprotein.
HOMA‐%B: homeostatic model assessment of β‐cell function.
HOMA‐IR: homeostatic model assessment of insulin resistance.
LDL: low‐density lipoprotein.
LED: light‐emitting diode.
MET: metabolic equivalent.
MVPA: moderate to vigorous physical activity.
n/a: not applicable.
NR: not reported.
PA: physical activity.
REML: reduced maximum likelihood approach.
SB: sedentary behaviour.
SD: standard deviation.
SLIPA: Sedentary and Light Intensity Physical Activity Log.
STAND: Study of Two Doses of Crizanlizumab Versus Placebo in Adolescent and Adult Sickle Cell Disease Patients.
stAPP: Smartphone‐based intervention.
VLDL: very low‐density lipoprotein.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aadahl 2012 | Sample includes participants over 59 years or under 18 years of age |
| Aadahl 2014 | Sample includes participants over 59 years or under 18 years of age |
| Adams 2013a | Sample includes participants over 59 years or under 18 years of age |
| Adams 2015 | Sample includes participants over 59 years or under 18 years of age |
| Balducci 2019 | Sample includes participants over 59 years or under 18 years of age |
| Barone Gibbs 2018 | Workplace setting |
| Barwais 2014 | Not RCT/cluster‐RCT |
| Barwais 2015 | Not RCT/cluster‐RCT |
| Bohn 2017 | Not RCT/cluster‐RCT |
| Bond 2014 | Not RCT/cluster‐RCT |
| Carr 2013 | Workplace setting |
| Casey 2018 | Workplace setting |
| Chiang 2019 | Sample includes participants over 59 years or under 18 years of age |
| Conroy 2016 | Wrong control (more than attention control or no intervention) |
| De Cocker 2008 | Age < 18 or > 59 years of age |
| Dewa 2009 | Not RCT/cluster RCT |
| Duncan 2016 | Wrong control (more than attention control or no intervention) |
| Edwards 2016 | Does not specifically target sedentary behavior (overall or TV viewing, computer use, etc.) |
| Garcia‐Ortiz 2017 | Sample includes participants over 59 years or under 18 years of age |
| Gardner 2014 | Sample includes participants over 59 years or under 18 years of age |
| George 2018 | Sample includes participants over 59 years or under 18 years of age |
| Gine‐Garriga 2017 | Sample includes participants over 59 years or under 18 years of age |
| Hartman 2020 | Does not specifically target sedentary behavior (overall or TV viewing, computer use, etc.) |
| Helgadottir 2017 | Sample includes participants over 59 years or under 18 years of age |
| Jprn 2019 | Not RCT/ cluster RCT |
| Judice 2015 | Sample includes participants over 59 years or under 18 years of age |
| King 2016a | Wrong control (more than attention control or no intervention) |
| Kirk 2012 | Not RCT/cluster‐RCT |
| Kline 2017 | Workplace setting |
| Kozey 2014 | Not RCT/cluster‐RCT |
| Kozey‐Keadle 2014 | Not RCT/cluster‐RCT |
| Lakerveld 2013 | Does not specifically target sedentary behavior (overall or TV viewing, computer use, etc.) |
| Lynch 2019 | Sample includes participants over 59 years or under 18 years of age |
| Martin 2017 | Sample includes participants over 59 years or under 18 years of age |
| Martinez‐Perez 2018 | Sample includes participants over 59 years or under 18 years of age |
| McNeil 2018 | Sample includes participants over 59 years or under 18 years of age |
| Miyamoto 2017 | Sample includes participants over 59 years or under 18 years of age |
| Nishimura 2019 | Sample includes participants over 59 years or under 18 years of age |
| Overgaard 2017 | Not RCT/cluster‐RCT |
| Prince 2018 | Sample includes participants over 59 years or under 18 years of age |
| Raynor 2013 | Wrong control (more than attention control or no intervention) |
| Recio‐Rodriguez 2018 | Sample includes participants over 59 years or under 18 years of age |
| Rockette‐Wagner 2015 | Sample includes participants over 59 years or under 18 years of age |
| Rosenberg 2018 | Sample includes participants over 59 years or under 18 years of age |
| Siddique 2017 | Not RCT/cluster‐RCT |
| Silva 2017 | Sample includes participants over 59 years or under 18 years of age |
| Teixeira 2017 | Sample includes participants over 59 years or under 18 years of age |
| Thomsen 2019 | Sample includes participants over 59 years or under 18 years of age |
| van de Glind 2017 | Sample includes participants over 59 years or under 18 years of age |
| Wilson 2018 | Not RCT / cluster RCT |
| Wyke 2019 | Sample includes participants over 59 years or under 18 years of age |
RCT: randomised controlled trial.
Characteristics of studies awaiting classification [ordered by study ID]
Marcinkevage 2012.
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: NR Study SB/PA objective/aim: reducing sedentary behaviour and increasing levels of moderate physical activity |
| Participants |
Included criteria: overweight/obese black women Excluded criteria: NR Baseline characteristics Intervention
Control
Overall
Pretreatment: NR |
| Interventions |
Intervention characteristics Intervention
Control
|
| Outcomes |
Outcomes measured in the study: glucose, self‐report PA, self‐report sedentary behaviour (MET‐hours/week), gestational weight gain |
| Notes |
MET: metabolic equivalent.
NR: not reported.
PA: physical activity.
SB: sedentary behaviour.
Characteristics of ongoing studies [ordered by study ID]
ISRCTN58484767.
| Study name | Using "IF‐THEN" plans to increase physical activity |
| Methods |
Study design: randomized controlled trial Study grouping: parallel group Recruitment: Study SB/PA objective/aim: The two conditions that complete a volitional help sheet (standard VHS and single situation VHS) will report greater physical activity and lower sedentariness at follow up than the control condition Country: UK Setting: |
| Participants |
Included criteria: UK adults who are capable of engaging in physical activity Excluded criteria: 1. Children 2. People who are not capable of engaging in physical activity 3. People not based in the UK |
| Interventions |
Intervention characteristics Intervention:
Control:
|
| Outcomes |
SB/PA outcome name and measurement tool:
|
| Starting date | May 2019 |
| Contact information | Chris J Armitage, University of Manchester chris.armitage@manchester.ac.uk |
| Notes | ISRCTN58484767 |
Latomme.
| Study name | Feel 4 Diabetes |
| Methods | |
| Participants | |
| Interventions | European study in 7 countries aiming to promote healthy lifestyles (including sedentary behaviour) among families |
| Outcomes | |
| Starting date | Unknown |
| Contact information | Julie Latomme, Ghent University julie.latomme@ugent.be |
| Notes |
Martin Borras 2014.
| Study name | SEDESTACTIV |
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: recruitment will take place in 13 PHCs in different regions of Spain (Barcelona, Lleida, Zaragoza, and Almeria). Primary healthcare professionals, who were selected on a voluntary basis from each of the participating centres, were trained. During the recruitment period, the opportunity to participate in the study will be offered at least once a week to all patients with overweight or mild obesity. A total of 30 subjects will be recruited in each PHC Study SB/PA objective/aim: to reduce sedentary time among overweight and mildly obese adults |
| Participants |
Included criteria: (1) men and women aged 25 to 65 seen at the PHC for whatever reason; (2) diagnosis of being overweight or suffering mild obesity (BMI 25 to 34.9 kg/m²); (3) autonomous subjects who have minimum physical aptitudes to follow the recommendations (being able to walk and stand up from a chair independently); (4) ≥ 6 hours of daily sitting; (5) can assure participation in the study for a year Excluded criteria: will be based on certain medical conditions that could contraindicate fulfilment of the intervention. Patients who have had obesity surgery will also be excluded |
| Interventions |
Intervention characteristics Intervention
Control
|
| Outcomes | Outcomes measured in the study: the primary outcome is sitting time measured by using the activPAL device (PAL Technologies, UK). Sitting time will also be measured with the Marshall Questionnaire. Secondary outcomes include decreasing sitting time in the workplace among individuals involved in the intervention (occupational sitting and physical activity questionnaire), quality of life (EQ5D), attitudes towards changing behaviour (Prochaska Scale), physical activity (Brief Physical Activity Assessment Tool (CBPAAT)), anthropometric variables ‐ BMI, triceps skinfold, waist circumference, metabolic indicators ‐ triglycerides, total cholesterol, HDL, LDL, glycaemia, glycated haemoglobin in diabetic patients |
| Starting date | Unknown |
| Contact information | Carme Martín‐Borràs, Primary Healthcare Research Institution IDIAP Jordi Gol and Universitat Ramon Llull mariacarmenmb@blanquerna.url.edu |
| Notes |
NCT02909725.
| Study name | BlossomUP |
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: mass email recruitment, flyers posted at local community settings and at local OBGYN offices in Ames, IA Study SB/PA objective/aim: limit accumulation of sedentary time (achieve a goal of 250 steps/hour); walk (30 minutes, most days of the week; 150 minutes/week) Country: USA Setting: community |
| Participants |
Included criteria:
Excluded criteria:
|
| Interventions |
Intervention characteristics Intervention:
Control:
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement) Change in time spent sedentary as measured by data collected via ActivPAL analysis Other outcomes: maternal insulin resistance, maternal body weight change |
| Starting date | February 2016 |
| Contact information | clmck@iastate.edu; ccampbel@iastate.edu |
| Notes | NCT02909725 Clinicaltrials.gov |
NCT03698903.
| Study name | Take a STAND 4 Health |
| Methods |
Study design: randomized controlled trial Study grouping: Recruitment: Study SB/PA objective/aim: The purpose of this study is to determine the effect of a 4‐week sedentary behavior reduction intervention on objectively measured sedentary behavior of overweight or obese adults. Country: US Setting: |
| Participants |
Included criteria:
Excluded criteria:
|
| Interventions |
Intervention characteristics Intervention: (1) an in‐person introductory session to acquaint the individuals with all intervention elements, customize to their preferences and describe the mHealth component of the intervention; (2) a website that will provide individualized feedback over time on the participant's scheduled breaks, sedentary time reduction, and sedentary patterns; (3) texts to serve as prompts and alert the participant to stand or move, with a goal of a 60 minute reduction per day, which are customized to the individual's schedule, personal preference and sedentary profile; and (4) two coaching phone calls to trouble shoot and problem solve implementation of the intervention. Control: |
| Outcomes |
SB/PA outcome name and measurement tool:
Other outcomes:
|
| Starting date | August 2018 |
| Contact information | Chelsea Larsen, University of South Carolina calarsen@email.sc.edu |
| Notes | NCT03698903 |
NCT04257539.
| Study name | Sedentary Intervention Using Motivational Interviewing and Technology (SUMIT) |
| Methods |
Study design: randomized controlled trial Study grouping: parallel group Recruitment: Study SB/PA objective/aim: This study will test the effects of a sedentary behavior intervention on pain processing, blood bio‐markers and pain symptoms in individuals with chronic low back pain Country: US Setting: |
| Participants |
Included criteria:
Excluded criteria:
|
| Interventions |
Intervention characteristics Intervention:
Control:
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement):
Other outcomes:
|
| Starting date | February 2020 |
| Contact information | Jacob Meyer, Iowa State University |
| Notes | NCT04257539 |
Pinto 2017.
| Study name | Take a STAND for Health |
| Methods | |
| Participants |
Included criteria:
|
| Interventions | |
| Outcomes | |
| Starting date | Unknown |
| Contact information | Ann Pinto, Universidade de Sao Paulo ana.pinto@usp.br |
| Notes |
Schroe 2019.
| Study name | MyPlan 2.0 |
| Methods |
Study design: randomised controlled trial Study grouping: parallel group Recruitment: Study SB/PA objective/aim: to experimentally investigate the efficacy of three behaviour‐change techniques (i.e. action planning, coping planning and self‐monitoring) on physical activity, sedentary behaviour and related determinants among adults. Country: Belgium Setting: |
| Participants |
Included criteria: (1) being ≥ 18 years old, (2) Dutch‐speaking, (3) having Internet access and (4) being the owner of a smartphone Excluded criteria: Participants will be excluded when one item or more will be endorsed on the the ‘Physical Activity Readiness Questionnaire’ (PAR‐Q) |
| Interventions |
Intervention characteristics Intervention:
Control:
|
| Outcomes |
SB/PA outcome name and measurement tool (units of measurement):
Other outcomes:
|
| Starting date | |
| Contact information | Helene Schroé, Ghent University Helene.Schroe@ugent.be |
| Notes |
BMI: body mass index.
CBPAAT: Catalan Brief Physical Activity Assessment Tool.
EQ‐5D: EuroQoL Group Quality of Life Questionnaire based on 5 dimensions.
HDL: high‐density lipoprotein.
LDL: low‐density lipoprotein.
NR: not reported.
PHC: primary health care clinic.
STAND: Study of Two Doses of Crizanlizumab Versus Placebo in Adolescent and Adult Sickle Cell Disease Patients.
Differences between protocol and review
There are some differences between our published protocol (Murtagh 2017) and this review.
We did not check timing of measures against published protocols and protocol registration documentation to consider its potential impact on risk of bias, as we deemed it not relevant given the small RCTs identified in the review.
We did not need to express dichotomous outcomes or categorical data as risk ratios, as none were identified.
We did not need to re‐analyse data from cluster RCTs by undertaking approximately correct analyses as outlined in Chapter 16: "Special topics in statistics" of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
We did not investigate reporting bias using funnel plots, as fewer than 10 studies were available for meta‐analysis
Contributions of authors
Drafting the protocol: EM, MM, CF, KM, NR, CO'G.
Selecting studies: EM, MM (CF as arbiter).
Extracting data from studies: EM, KM (CF as arbiter).
Entering data into RevMan: EM, KM.
Carrying out the analysis: EM, CF.
Interpreting the analysis: EM, CF.
Drafting the final review: EM, MM, CF, KM, NR, CO'G.
Resolving disagreements: as noted above.
Updating the review: EM, MM, CF, KM, NR, CO'G.
Sources of support
Internal sources
-
Deprtartment of Physical Education & Sport Sciences, University of Limerick, Ireland
EM works at the University of Limerick
-
Sport & Exercise Sciences Research Institute, Ulster University, UK
MM works at Ulster University
-
Norwich Medical School, University of East Anglia, UK
KM works at the Norwich Medical School, University of East Anglia
-
Bodleian Health Care Libraries, University of Oxford, UK
NR works at the Bodleian Health Care Libraries, University of Oxford
-
Graduate Entry Medical School, University of Limerick, Ireland
COG works at the Graduate Entry Medical School, University of Limerick
-
University of Bristol, Bristol, UK
CF works at the Centre for Exercise Nutrition and Health Sciences, School for Policy Studies, University of Bristol, Bristol, UK
External sources
-
Cochrane Fellowship, Health Research Board, Ireland
EM was supported by a Cochrane Fellowship from the Health Reseach Board in Ireland (2016‐2018).
Declarations of interest
Elaine M Murtagh: none known.
Marie H Murphy: together with another Ulster University colleague, the Sport & Exercise Sciences Research Institute at UU has received 20 standing desks from Ergotron to allow us to undertake a small research project on the use of sit‐to‐stand desks in office workers. This work is at feasibility stage and will not feature in the review.
Charles Foster: none known.
Karen Milton: none known.
Nia W Roberts: none known.
Clodagh SM O'Gorman: none known.
New
References
References to studies included in this review
Arrogi 2017 {published data only}
- Arrogi A, Bogaerts A, Seghers J, Devloo K, Vanden AV, Geurts L, et al. Evaluation of stAPP: a smartphone-based intervention to reduce prolonged sitting among Belgian adults. Health Promotion International 2017;6:1-6. [DOI] [PubMed] [Google Scholar]
- NCT01975870. A stAPP to a healthier lifestyle [A stAPP to a healthier lifestyle: a randomized controlled trial]. clinicaltrials.gov/ct2/show/record/NCT01975870 (first received 5 November 2013).
Barwais 2013 {published data only}
- Barwais F, Cuddihy TF, Tomson LM. Physical activity, sedentary behavior and total wellness changes among sedentary adults: a 4-week randomized controlled trial. Health & Quality of Life Outcomes 2013;11:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barwais FA. Using technology to change adult sedentary behaviour, physical activity levels and total wellness. School of Exercise and Nutrition Sciences: Doctor of Philosophy, 2013. [Google Scholar]
Biddle 2015 {published data only}
- Biddle S, Davies M, Khunti K, Gorely T, Edwardson C, Wilmot E, et al. Reducing sedentary time in young adults at risk of diabetes: Project STAND. Journal of Science and Medicine in Sport 2012;15:S4. [Google Scholar]
- Biddle SJ, Edwardson C, Wilmot EG, Yates T, Gorely T, Bodicoat DH, et al. A randomised controlled trial to reduce sedentary time in young adults at risk of type 2 diabetes mellitus: Project STAND (Sedentary Time ANd Diabetes). PLoS ONE [Electronic Resource] 2015;10(12):e0143398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle SJH, Edwardson CL, Gorely T, Wilmot EG, Yates T, Nimmo MA, et al. Reducing sedentary time in adults at risk of type 2 diabetes: process evaluation of the STAND (Sedentary Time ANd Diabetes) RCT. BMC Public Health 2017;17(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmot EG, Davies MJ, Edwardson CL, Gorely T, Khunti K, Nimmo M, et al. Rationale and study design for a randomised controlled trial to reduce sedentary time in adults at risk of type 2 diabetes mellitus: project stANd (Sedentary Time ANd diabetes). BMC Public Health 2011;11:908. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cotten 2016 {published data only}
- Cotten E, Prapavessis H. Increasing nonsedentary behaviors in university students using text messages: randomized controlled trial. JMIR mHealth and uHealth 2016;4(3):e99. [DOI: 10.2196/mhealth.5411] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotten E. Reducing sedentary behaviour in university students using a text message-based intervention. The School of Graduate and Postdoctoral Studies, Master of Arts, 2015 2015. [Google Scholar]
Ellingson 2016 {published data only}
- Ellingson LD, Meyer JD, Cook DB. Wearable technology reduces prolonged bouts of sedentary behavior. Translational Journal of the American College of Sports Medicine 2016;1(2):10-7. [Google Scholar]
Finni 2011 {published data only}
- Finni T, Saakslahti A, Laukkanen A, Pesola A, Sipila S. A family based tailored counselling to increase non-exercise physical activity in adults with a sedentary job and physical activity in their young children: design and methods of a year-long randomized controlled trial. BMC Public Health 2011;11:944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesola A, Laukkanen A, Haakana P, Havu M, Sääkslahti A, Sipilä S, et al. Muscle inactivity and activity patterns after sedentary-time targeted randomized controlled trial. Medicine & Science in Sports & Exercise 2014;46(11):2122-31. [DOI] [PubMed] [Google Scholar]
- Pesola A. Reduced muscle inactivity, sedentary time and cardio-metabolic benefits: effectiveness of a one-year family-based cluster randomized controlled trial. Faculty of Sport and Health Sciences, PhD, 2016. [Google Scholar]
- Pesola AJ, Laukkanen A, Heikkinen R, Sipilä S, Sääkslahti A, Finni T. Accelerometer-assessed sedentary work, leisure time and cardio-metabolic biomarkers during one year: effectiveness of a cluster randomized controlled trial in parents with a sedentary occupation and young children. PLOS ONE 2017;12(8):e0183299. [DOI: 10.1371/journal.pone.0183299] [DOI] [PMC free article] [PubMed] [Google Scholar]
French 2011 {published data only}
- French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action - a group-randomized trial. Obesity 2011;19(10):2082-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jago 2013 {published data only}
- Jago R, Sebire SJ, Turner KM, Bentley GF, Goodred JK, Fox KR, et al. Feasibility trial evaluation of a physical activity and screen-viewing course for parents of 6- to 8-year-old children: Teamplay. International Journal of Behavioral Nutrition & Physical Activity 2013;10:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kitagawa 2020 {published data only}
- Kitagawa, THiguchi, YTodo, EUeda, TAndo, SMurakami, T. Tailored feedback reduced prolonged sitting time and improved the health of housewives: a single-blind randomized controlled pilot study. Women & Health 2020;60:212-223. [DOI: 10.1080/03630242.2019.1616043] [DOI] [PubMed] [Google Scholar]
Laska 2016 {published data only}
- Laska MN, Lytle LA, Nanney MS, Moe SG, Linde JA, Hannan PJ. Results of a 2-year randomized, controlled obesity prevention trial: effects on diet, activity and sleep behaviors in an at-risk young adult population. Preventive Medicine 2016;89:230-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Moe SG, Nanney MS, Laska MN, Linde JA, Petrich CA, et al. Designing a weight gain prevention trial for young adults: the CHOICES study. American Journal of Health Education 2014;45(2):67-75. [DOI: 10.1080/19325037.2013.875962] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lioret 2012 {published data only}
- Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT): an early intervention to prevent childhood obesity: cluster-randomised controlled trial. BMC Public Health 2008;8(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lioret S, Campbell KJ, Crawford D, Spence AC, Hesketh K, McNaughton SA. A parent focused child obesity prevention intervention improves some mother obesity risk behaviors: the Melbourne inFANT program. International Journal of Behavioral Nutrition & Physical Activity 2012;9:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sui 2018 {published data only}
- Sui W, Prapavessis H. Standing up for student health: an application of the health action process approach for reducing student sedentary behavior-randomised control pilot trial. Applied Psychology: Health and Well-Being 2018;10(1):87-107. [DOI] [PubMed] [Google Scholar]
Williams 2019 {published data only}
- Williams J, Stubbs B, Gaughra F, Craig T. ‘Walk This Way’ – a pilot of a health coachingintervention to reduce sedentary behaviourand increase low intensity exercise in peoplewith serious mental illness: study protocol fora randomised controlled trial. Trials 2016;17(594). [DOI: 10.1186/s13063-016-1660-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, JStubbs, BRichardson, SFlower, CBarr-Hamilton, LGrey, BHubbard, KSpaducci, GGaughran, FCraig, T. 'Walk this way': Results from a pilot randomised controlled trial of a health coaching intervention to reduce sedentary behaviour and increase physical activity in people with serious mental illness. BMC Psychiatry 2019;19(1). [DOI: 10.1186/s12888-019-2274-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Aadahl 2012 {published data only}
- Aadahl M, Linneberg A, Witte D, Jorgensen T. Reduction of sitting time in sedentary men and women. A randomized controlled trial (Sedentary Intervention Trial). Aadahl 2012;15:S302. [Google Scholar]
Aadahl 2014 {published data only}
- Aadahl M, Linneberg A, Moller T C, Rosenorn S, Dunstan D W, Witte D R, et al. Motivational counseling to reduce sitting time: a community-based randomized controlled trial in adults. American Journal of Preventive Medicine 2014;47(5):576-86. [DOI] [PubMed] [Google Scholar]
Adams 2013a {published data only}
- Adams M M, Davis P G, Gill D L. A hybrid online intervention for reducing sedentary behavior in obese women. Frontiers inpublic health 2013;1:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Adams 2015 {published data only}
- Adams Melanie M, Gill Diane L. Reducing Sedentary Behavior: Active Steps for Overweight Women. Women in Sport & PhysicalActivity Journal 2015;23(1):9-18. [Google Scholar]
Balducci 2019 {published data only}
- Balducci S, D'Errico V, Haxhi J, Sacchetti M, Orlando G, Cardelli P, et al. Effect of a Behavioral Intervention Strategy on Sustained Change in Physical Activity and Sedentary Behavior in Patients With Type 2 Diabetes: The IDES_2 Randomized Clinical Trial. Journal of the American Medical Association 2019;321(9):880-90. [DOI] [PubMed] [Google Scholar]
Barone Gibbs 2018 {published data only}
- Barone Gibbs Bethany, Hergenroeder Andrea L, Perdomo Sophy J, Kowalsky Robert J, Delitto Anthony, Jakicic John M. Reducing sedentary behaviour to decrease chronic low back pain: the stand back randomised trial. Occupational and Environmental Medicine 2018;75(5):321-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barwais 2014 {published data only}
- Barwais F, Cuddihy T. Empowering sedentary adults to reduce sedentary behaviour: Success with a technology-based physical activity monitor. Journal of Science and Medicine in Sport 2014;18:e67. [Google Scholar]
Barwais 2015 {published data only}
- Barwais F A, Cuddihy T F. Empowering sedentary adults to reduce sedentary behavior and increase physical activity levels and energy expenditure: A pilot study. International Journal ofEnvironmental Research and Public Health 2015;12(1):414-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohn 2017 {published data only}
- Bohn L, Sa-Couto P, Castro A, Ribeiro F, Oliveira J. Effects of a health education intervention on sedentary time, moderate-to-vigorous physical activity, and body mass index in individuals with moderate-to-high cardiovascular risk. Obesity Facts 2017;10 (Supplement 1):119-20. [Google Scholar]
Bond 2014 {published data only}
- Bond D S, Thomas J G, Raynor H A, Moon J, Sieling J, Trautvetter J, et al. B-MOBILE--a smartphone-based intervention to reduce sedentary time in overweight/obese individuals: a within-subjects experimental trial. PLoS One 2014;9(6):e100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carr 2013 {published data only}
- Carr L J, Karvinen K, Peavler M, Smith R, Cangelosi K. Multicomponent intervention to reduce daily sedentary time: a randomised controlled trial. BMJ Open 2013;3(10):e003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
Casey 2018 {published data only}
- Casey K, Mailey E L, Rosenkranz R R, Swank A, Ablah E, Rosenkranz S K. Does dietary intake change during an intervention to reduce sedentary behavior and cardiovascular disease risk? A randomized comparative effectiveness trial. BMC Nutrition 2018;4(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
Chiang 2019 {published data only}
- Chiang L C, Heitkemper M M, Chiang S L, Tzeng W C, Lee M S, Hung Y J, et al. Motivational Counseling to Reduce Sedentary Behaviors and Depressive Symptoms and Improve Health-Related Quality of Life Among Women With Metabolic Syndrome. The Journal of Cardiovascular Nursing 2019;34(4):327-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conroy 2016 {published data only}
- Conroy D E, Hedeker D, McFadden H G, Pellegrini C A, Pfammatter A F, Phillips S M, et al. Lifestyle Intervention Effects on the Frequency and Duration of Daily Moderate-Vigorous Physical Activity and Leisure Screen Time. Health Psychology 2016;19:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Cocker 2008 {published data only}
- De Cocker K A, De Bourdeaudhuij I M, Brown W J, Cardon G M. The effect of a pedometer-based physical activity intervention on sitting time. Preventive Medicine 2008;47(2):179-81. [DOI] [PubMed] [Google Scholar]
Dewa 2009 {published data only}
- Dewa Carolyn S, deRuiter Wayne, Chau Nancy, Karioja Kim. Walking for wellness: using pedometers to decrease sedentary behaviour and promote mental health. International Journal ofMental Health Promotion 2009;11(2):24-8. [Google Scholar]
Duncan 2016 {published data only}
- Duncan M J, Vandelanotte C, Trost S G, Rebar A L, Rogers N, Burton N W, et al. Balanced: a randomised trial examining the efficacy of two self-monitoring methods for an app-based multi-behaviour intervention to improve physical activity, sitting and sleep in adults. BMC Public Health 2016;16:670. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edwards 2016 {published data only}
- Edwards M K. The Effects of a Randomized Control Trial Sedentary Behavior Intervention on Depression in Active, Young Adults: 3211 Board #276 June 3, 2: 00. Medicine & Science inSports & Exercise 2016;48(5 Suppl 1):917. [Google Scholar]
Garcia‐Ortiz 2017 {published data only}
- Garcia-Ortiz L, Recio-Rodriguez J I, Agudo-Conde C, Repiso-Gento I, Schmolling-Guinovart Y, Gonzalez-Viejo N, et al. Effectiveness of a smartphone application in increasing physical activity and decrease sedentary lifestyle. the evident II study. Journal ofHypertension 2017;35 (Supplement 2):e298-9. [Google Scholar]
Gardner 2014 {published data only}
- Gardner B, Thuné-Boyle I, Iliffe S, Fox Kr, Jefferis Bj, Hamer M, et al. 'On Your Feet to Earn Your Seat', a habit-based intervention to reduce sedentary behaviour in older adults: study protocol for a randomized controlled trial. Trials 2014;15:368. [DOI] [PMC free article] [PubMed]
George 2018 {published data only}
- George, ES. Increasing physical activity and reducing sedentary time in middle-aged males. DissertationAbstracts International Section C: Worldwide 2018;75(1-C):No Pagination Specified-. [Google Scholar]
Gine‐Garriga 2017 {published data only}
- Gine-Garriga Maria, Coll-Planas Laura, Guerra Miriam, Domingo Alex, Roque Marta, Caserotti Paolo, et al. The SITLESS project: exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: study protocol for a randomised controlled trial. Trials 2017;18(1):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hartman 2020 {published data only}
- Hartman S J, Pekmezi D, Dunsiger S I, Marcus B H. Physical Activity Intervention Effects on Sedentary Time in Spanish-Speaking Latinas. Journal of physical activity & health 2020:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Helgadottir 2017 {published data only}
- Helgadottir Bjorg, Owen Neville, Dunstan David W, Ekblom Orjan, Hallgren Mats, Forsell Yvonne. Changes in physical activity and sedentary behavior associated with an exercise intervention in depressed adults. Psychology of Sport andExercise 2017;30:10-8. [Google Scholar]
Jprn 2019 {published data only}
- Jprn Umin. The sedentary behavior in university students and the effectiveness of intervention program to improve a sitting time. http://www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000037730 2019. [Google Scholar]
Judice 2015 {published data only}
- Judice P B, Hamilton M T, Sardinha L B, Silva A M. Randomized controlled pilot of an intervention to reduce and break-up overweight/obese adults' overall sitting-time. Trials 2015;16:490. [DOI] [PMC free article] [PubMed] [Google Scholar]
King 2016a {published data only}
- King Ac, Hekler Eb, Grieco La, Winter Sj, Sheats Jl, Buman Mp, et al. Effects of Three Motivationally Targeted Mobile Device Applications on Initial Physical Activity and Sedentary Behavior Change in Midlife and Older Adults: a Randomized Trial. PLoS One 2016;11(6):e0156370. [DOI] [PMC free article] [PubMed]
Kirk 2012 {published data only}
- Kirk A, Fitzsimons C, Murphy M, Mutrie N. Effect of a person centred consultation intervention to reduce the sedentary behaviour of working Scottish adults. Journal of Science andMedicine in Sport 2012;15:S314. [Google Scholar]
Kline 2017 {published data only}
- Kline C E, Perdomo S J, Hergenroeder A L, Barone Gibbs B. The effect of reducing sedentary behavior on sleep quality among adults with chronic low back pain: A randomized controlled pilot study. Sleep 2017;40 (Supplement 1):A387-8. [Google Scholar]
Kozey 2014 {published data only}
- Kozey Keadle S, Lyden K, Staudenmayer J, Hickey A, Viskochil R, Braun B, et al. The independent and combined effects of exercise training and reducing sedentary behavior on cardiometabolic risk factors. Applied Physiology, Nutrition,& Metabolism 2014;39(7):770-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kozey‐Keadle 2014 {published data only}
- Kozey-Keadle Sarah, Staudenmayer John, Libertine Amanda, Mavilia Marianna, Lyden Kate, Braun Barry, et al. Changes in sedentary time and physical activity in response to an exercise training and/or lifestyle intervention. Journal ofPhysical Activity & Health 2014;11(7):1324-33. [DOI] [PubMed] [Google Scholar]
Lakerveld 2013 {published data only}
- Lakerveld J, Bot S D, Ploeg H P, Nijpels G. The effects of a lifestyle intervention on leisure-time sedentary behaviors in adults at risk: the Hoorn Prevention Study, a randomized controlled trial. Preventive Medicine 2013;57(4):351-6. [DOI] [PubMed] [Google Scholar]
Lynch 2019 {published data only}
- Lynch B M, Nguyen N H, Moore M M, Reeves M M, Rosenberg D E, Boyle T, et al. A randomized controlled trial of a wearable technology-based intervention for increasing moderate to vigorous physical activity and reducing sedentary behavior in breast cancer survivors: The ACTIVATE Trial. Cancer 2019;125(16):2846-55. [DOI] [PubMed] [Google Scholar]
Martin 2017 {published data only}
- Martin Anne, Adams Jacob M, Bunn Christopher, Gill Jason M R, Gray Cindy M, Hunt Kate, et al. Feasibility of a real-time self-monitoring device for sitting less and moving more: a randomised controlled trial. BMJ Open Sport & ExerciseMedicine 2017;3(1):e000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martinez‐Perez 2018 {published data only}
- Martinez-Perez P, Gomez-Sanchez M, Gomez-Sanchez L, Agudo-Conde C, Recio-Rodriguez J, Del Rio-Garcia M, et al. The long-term effectiveness of a smartphone application to reduce sedentary time in primary care. Evident II study. Journal of Hypertension 2018;36 (Supplement 1):e66. [Google Scholar]
McNeil 2018 {published data only}
- McNeil Jessica, Farris Megan S, Ruan Yibing, Merry Heather, Lynch Brigid M, Matthews Charles E, et al. Effects of prescribed aerobic exercise volume on physical activity and sedentary time in postmenopausal women: a randomized controlled trial. International Journal of Behavioral Nutrition & Physical Activity 2018;15(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miyamoto 2017 {published data only}
- Miyamoto Toshiaki, Fukuda Kazuhito, Oshima Yoshitake, Moritani Toshio. Non-locomotive physical activity intervention using a tri-axial accelerometer reduces sedentary time in type 2 diabetes. Physician & Sportsmedicine 2017;45(3):245-51. [DOI] [PubMed] [Google Scholar]
Nishimura 2019 {published data only}
- Nishimura M, Sasai H, Nakata Y, Maeda S. Effects of Vibrotactile Feedback on Sedentary Behaviors in Adults: A Pilot Randomized Controlled Trial. International Journal of Environmental Research & Public Health 2019;16(23):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Overgaard 2017 {published data only}
Prince 2018 {published data only}
- Prince S A, Reed J L, Cotie L M, Harris J, Pipe A L, Reid R D. Results of the Sedentary Intervention Trial in Cardiac Rehabilitation (SIT-CR Study): A pilot randomized controlled trial. International Journal of Cardiology 2018;269:317-24. [DOI] [PubMed] [Google Scholar]
Raynor 2013 {published data only}
- Raynor H A, Steeves E A, Bassett D R Jr, Thompson D L, Gorin A A, Bond D S. Reducing TV watching during adult obesity treatment: two pilot randomized controlled trials. Behavior Therapy 2013;44(4):674-85. [DOI] [PubMed] [Google Scholar]
Recio‐Rodriguez 2018 {published data only}
- Recio-Rodriguez Jose I, Gomez-Marcos Manuel A, Agudo-Conde Cristina, Ramirez Ignasi, Gonzalez-Viejo Natividad, Gomez-Arranz Amparo, et al. EVIDENT 3 Study: A randomized, controlled clinical trial to reduce inactivity and caloric intake in sedentary and overweight or obese people using a smartphone application: Study protocol. Medicine 2018;97(2):e9633. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rockette‐Wagner 2015 {published data only}
- Rockette-Wagner B, Edelstein S, Venditti E M, Reddy D, Bray G A, Carrion-Petersen M L, et al. The impact of lifestyle intervention on sedentary time in individuals at high risk of diabetes. Diabetologia 2015;58(6):1198-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosenberg 2018 {published data only}
- Rosenberg Dori E, Lee Amy K, Anderson Melissa, Renz Anne, Matson Theresa E, Kerr Jacqueline, et al. Reducing Sedentary Time for Obese Older Adults: Protocol for a Randomized Controlled Trial. JMIR ResearchProtocols 2018;7(2):e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siddique 2017 {published data only}
- Siddique Juned, de Chavez Peter John, Craft Lynette L, Freedson Patty, Spring Bonnie. The Effect of Changes in Physical Activity on Sedentary Behavior: Results From a Randomized Lifestyle Intervention Trial. American Journal ofHealth Promotion 2017;31(4):287-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Silva 2017 {published data only}
- Silva, M, Teixeira, P, Gray, C, Hunt, K, Bunn, C, Roberts, G, Wyke, S, Consortium, O. The power of football: a socio-psychological approach to promoting behaviour change in overweight and sedentary men in the European fans in training project. Obesity Facts 2017;Conference: 24th Congress of the European Congress on Obesity, ECO 2017. Portugal. 10(pp 213).
Teixeira 2017 {published data only}
- Teixeira P J, Silva M S, Gray C M, Hunt K, Ploeg H, Roberts G, et al. Promoting physical activity and reduced sedentary time in football clubs: Lessons from eurofit. Obesity Facts 2017;10 (Supplement 1):48. [Google Scholar]
Thomsen 2019 {published data only}
- Thomsen T, Aadahl M, Beyer N, Hetland M L, Loppenthin K B, Midtgaard J, et al. Sustained long-term efficacy of motivational counselling and text message reminders on daily sitting time in patients with rheumatoid arthritis? Long-term follow-up of a randomized, parallel-group trial. Arthritis Care & Research 2019;10. [DOI] [PubMed] [Google Scholar]
van de Glind 2017 {published data only}
- de Glind I, Bunn C, Gray C M, Hunt K, Andersen E, Jelsma J, et al. The intervention process in the European Fans in Training (EuroFIT) trial: a mixed method protocol for evaluation. Trials 2017;18(1):356. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2018 {published data only}
- Wilson J J, Adlakha D, Cunningham C, Best P, Cardwell C R, Stephenson A, et al. Brief Standing Desk Intervention to Reduce Sedentary Behavior at a Physical Activity Conference in 2016. American Journal of Public Health 2018;108(9):1197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wyke 2019 {published data only}
- Wyke S, Bunn C, Andersen E, Silva M N, Nassau F, McSkimming P, et al. The effect of a programme to improve men's sedentary time and physical activity: The European Fans in Training (EuroFIT) randomised controlled trial. PLoS Medicine 2019;16(2):e1002736. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Marcinkevage 2012 {published data only}
- Marcinkevage J, Correa A, Ramakrishnan U, Sharma A, Venkat Narayan KM, Umpierrez G. Reducing sedentary behavior and increasing physical activity during pregnancy: a feasibility study. Diabetes 2012;61:A344. [Google Scholar]
References to ongoing studies
ISRCTN58484767 {published data only}
- ISRCTN58484767. Using "IF-THEN" plans to increase physical activity. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN58484767 4th June 2019.
Latomme {unpublished data only}
- Feel 4 Diabetes. Ongoing study. Unknown. Contact author for more information.
Martin Borras 2014 {published data only}
- Martin-Borras C, Gine-Garriga M, Martinez E, Martin-Cantera C, Puigdomenech E, Sola M, et al. Effectiveness of a primary care-based intervention to reduce sitting time in overweight and obese patients (SEDESTACTIV): a randomized controlled trial; rationale and study design. BMC Public Health 2014;14:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02909725 {unpublished data only}
- NCT02909725. The Blossom Project: "BlossomUP" evaluating methods to decrease sedentary time in pregnancy. https://clinicaltrials.gov/ct2/show/study/NCT02909725 (first received 21 September 2016).
NCT03698903 {published data only}
- NCT03698903. Take a STAND 4 Health: A Sedentary Behavior Reduction Intervention. https://clinicaltrials.gov/ct2/show/NCT03698903 9th October 2018.
NCT04257539 {published data only}
- NCT04257539. Reducing Sedentary Time in Chronic Low Back Pain: Sedentary Intervention Using Motivational Interviewing and Technology (SUMIT). https://clinicaltrials.gov/show/NCT04257539 6th February 2020.
Pinto 2017 {unpublished data only}
- Take a STAND for Health. Ongoing study. Unknown. Contact author for more information.
Schroe 2019 {published data only}
- Schroe, HVan der Mispel, CDe Bourdeaudhuij, IVerloigne, MPoppe, LCrombez, G. A factorial randomised controlled trial to identify efficacious self-regulation techniques in an e- and m-health intervention to target an active lifestyle: study protocol. Trials 2019;20(1):340. [DOI: 10.1186/s13063-019-3456-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Alibegovic 2010
- Alibegovic AC, Sonne MP, Højbjerre L, Hansen T, Pedersen O, Hall G, et al. The T-allele of TCF7L2 rs7903146 associates with a reduced compensation of insulin secretion for insulin resistance induced by 9 days of bed rest. Diabetes 2010;59(4):836-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
American Academy of Pediatrics 2001
- American Academy of Pediatrics, Committee on Public Education. Children, adolescents, and television. Pediatrics 2001;107(2):423-6. [DOI] [PubMed] [Google Scholar]
Australian Government 2004
- Australian Government, Department of Health and Aging. Active Kids are Healthy Kids. Australia's Physical Activity Recommendations for 5-12 Year Olds. Canberra: Commonwealth of Australia, 2004. [Google Scholar]
Australian Government 2014
- Australian Government, Department of Health and Aging. Make Your Move – Sit Less. Be Active for Life! Australia's Physical Activity and Sedentary Behaviour Guidelines. Canberra: Commonwealth of Australia, 2014. [Google Scholar]
Baker 2015
- Baker PRA, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database of Systematic Reviews 2015, Issue 1. [DOI: 10.1002/14651858.CD008366.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401-6. [DOI] [PubMed] [Google Scholar]
Benatti 2015
- Benatti FB, Ried-Larsen M. The effects of breaking up prolonged sitting time: a review of experimental studies. Medicine & Science in Sports & Exercise 2015;47(100):2053-61. [DOI] [PubMed] [Google Scholar]
Bennie 2013
- Bennie JA, Chau JY, Ploeg HP, Stamatakis E, Do A, Bauman A. The prevalence and correlates of sitting in European adults - a comparison of 32 Eurobarometer-participating countries. International Journal of Behavioral Nutrition and Physical Activity 2013;10(107):1-13. [DOI: ] [DOI] [PMC free article] [PubMed]
BHFNC Physical Activity and Health 2012
- British Heart Foundation National Centre for Physical Activity and Health. Sedentary Behaviour Evidence Briefing. Loughborough: British Heart Foundation, 2012. [Google Scholar]
Brownson 2005
- Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annual Review of Public Health 2005;26:421-43. [DOI] [PubMed] [Google Scholar]
Buckley 2015
- Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. British Journal of Sports Medicine 2015;49(21):1357-62. [DOI] [PubMed] [Google Scholar]
Bull 2004
- Bull FC, Armstrong TP, Dixon TD, Ham S, Neiman A, Pratt M. Physical inactivity. In: Ezzati M, Lopez A, Rodgers A, CJL Murray, editors(s). Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Geneva: World Health Organization, 2004. [Google Scholar]
Buman 2013
- Buman MP, Winkler EAH, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. American Journal of Epidemiology 2013;179(3):323–34. [DOI] [PubMed] [Google Scholar]
Chastin 2013
- Chastin SF, Schwarz M, Skelton U, Ann D. Development of a consensus taxonomy of sedentary behaviors (SIT): report of Delphi Round 1. PloS One 2013;8(12):e82313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chastin 2017
- Chastin S, Gardiner PA, Ashe MC, Harvey JA, Leask CD, Balogun S, Helboostad JL, Skelton DA. Interventions for reducing sedentary behaviour in community-dwelling older adults. Cochrane Database of Systematic Reviews 2017, Issue 9. [DOI: 10.1002/14651858.CD012784] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chau 2012
- Chau JY, Merom D, Grunseit A, Rissel C, Bauman A, Ploeg HP, et al. Temporal trends in non-occupational sedentary behaviours from Australian Time Use Surveys 1992, 1997 and 2006. International Journal of Behavioral Nutrition and Physical Activity 2012;9(76):1-8. [DOI: 10.1186/1479-5868-9-76] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chau 2013
- Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, Matthews CE, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One 2013;8(11):e80000. [DOI: 10.1371/journal.pone.0080000] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chomistek 2013
- Chomistek AK, Manson JE, Stefanick ML, Lu B, Sands-Lincoln M, Going SB, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Women's Health Initiative. Journal of the American College of Cardiology 2013;61(23):2346-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clemes 2014
- Clemes SA, O'Connell SE, Edwardson CL. Office workers' objectively measured sedentary behavior and physical activity during and outside working hours. Journal of Occupational and Environmental Medicine 2014;56(3):298-303. [DOI] [PubMed] [Google Scholar]
Cooper 2018
- Cooper AR, Biddle S, Chastin S, Clemes S, Fenton S, Fitzsimons C, et al. UK Physical Activity Guidelines: Draft Review and Recommendations for Sedentary Behaviour. Bristol: UK Expert Committee for Physical Activity, 2019. [Google Scholar]
Covidence 2016 [Computer program]
- Covidence. Version accessed 19 March 2016. Melbourne: Covidence, 2016.
CPHG 2011
- The Cochrane Public Health Group. Guide for developing a Cochrane Protocol, 2011. Available from http://ph.cochrane.org/review-authors.
Credence Research 2017
- Credance Research. Global Standing Desk Market - Growth, Future Prospects and Competitive Analysis, 2017–2025. https://www.credenceresearch.com/report/standing-desks-market May 2017.
De Greef 2010
- De Greef K, Deforche B, Tudor-Locke C, De Bourdeaudhuij I. A cognitive-behavioural pedometer-based group intervention on physical activity and sedentary behaviour in individuals with type 2 diabetes. Health Education Research 2010;25(5):724-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Rezende 2014
- De Rezende LFM, Lopes MRS, Rey-López JP, Matsudo VKR, do Carmo LO. Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS One 2014;9(8):e105620. [DOI: 10.1371/journal.pone.0105620] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. Available from www.cochrane-handbook.org, 2011. [Google Scholar]
Dempsey 2014
- Dempsey PC, Owen N, Biddle SJH, Dunstan DW. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Current Diabetes Reports 2014;14(9):1-11. [DOI] [PubMed] [Google Scholar]
Department of Health 2011
- Department of Health. Start Active, Stay Active: A Report on Physical Activity for Health From the Four Home Countries' Chief Medical Officers. London, UK: Department of Health, 2011. [Google Scholar]
Dunstan 2012
- Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 2012;35(5):976-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekelund 2009
- Ekelund U, Brage S, Griffin SJ, Wareham NJ. Objectively measured moderate- and vigorous-intensity physical activity but not sedentary time predicts insulin resistance in high-risk individuals. Diabetes Care 2009;32(6):1081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekelund 2016
- Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al, Lancet Physical Activity Series 2 Executive Committee, Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388(10051):1302-10. [DOI] [PubMed] [Google Scholar]
Endnote 2015 [Computer program]
- EndNote X7. Version X7.4. Philadelphia: Thomson Reuters, 2015.
Esliger 2011
- Esliger DW, Rowlands AV, Hurst TL, Catt M, Murray P, Eston RG. Validation of the GENEA Accelerometer. Medicine & Science in Sports & Exercise 2011;43(6):1085-93. [DOI] [PubMed] [Google Scholar]
Ford 2012
- Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. International Journal of Epidemiology 2012;41(5):1338–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freedson 1998
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Medicine & Science in Sports & Exercise 1998;30(5):777-81. [DOI] [PubMed] [Google Scholar]
Gardner 2016
- Gardner B, Smith L, Lorencatto F, Hamer M, Biddle SJH. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychology Review 2016;10(1):89-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADE Working Group, McMaster University GRADEpro GDT. Version accessed 3 October 2016. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. British Medical Journal 2008;336(7650):924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence - inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294-302. [DOI] [PubMed] [Google Scholar]
Healthy Ireland 2016
- Healthy Ireland. Get Ireland Active! The National Physical Activity Plan for Ireland. Dublin: Department of Health and Department of Transport, Tourism and Sport, 2016. [Google Scholar]
Healy 2011
- Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. European Heart Journal 2011;32(5):590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. Available from www.cochrane-handbook.org.
Higgins 2011b
- Higgins JP, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Hombali 2019
- Hombali AS, Solon JA, Venkatesh BT, Nair NS, Peña‐Rosas JP. Fortification of staple foods with vitamin A for vitamin A deficiency. Cochrane Database of Systematic Reviews 2019, Issue 5. [DOI: 10.1002/14651858.CD010068.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Katzmarzyk 2009
- Katzmarzyk T, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Medicine & Science in Sports & Exercise 2009;41(5):998-1005. [DOI] [PubMed] [Google Scholar]
Lang 2015
- Lang JJ, McNeil J, Tremblay MS, Saunders TJ. Sit less, stand more: a randomized point-of-decision prompt intervention to reduce sedentary time. Preventive Medicine 2015;73:67-9. [DOI] [PubMed] [Google Scholar]
Lyden 2014
- Lyden K, Kozey Keadle S, Staudenmayer J, Freedson PS. A method to estimate free-living active and sedentary behavior from an accelerometer. Medicine & Science in Sports & Exercise 2014;46(2):386-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 2015
- Martin A, Fitzsimons C, Jepson R, Saunders DH, Ploeg HP, Teixeira PJ, et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta-analysis. British Journal of Sports Medicine 2015;49(16):1056-63. [DOI: 10.1136/bjsports-2014-094524] [DOI] [PubMed] [Google Scholar]
Matthews 2008
- Matthews CE, Chen Kong Y, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American Journal of Epidemiology 2008;167(7):875-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murtagh 2017
- Murtagh EM, Murphy MH, Foster C, Milton K, Roberts NW, O’Gorman CSM. Interventions outside the workplace for reducing sedentary behaviour in adults under 60. Cochrane Database of Systematic Reviews 2017, Issue 2. [DOI: 10.1002/14651858.CD012554] [DOI] [PMC free article] [PubMed] [Google Scholar]
Müller‐Riemenschneider 2008
- Müller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: a systematic review. Preventive Medicine 2008;47(4):354-68. [DOI] [PubMed] [Google Scholar]
O'Donoghue 2016
- O’Donoghue G, Perchoux C, Mensah K, Lakerveld J, Ploeg H, Bernaards C, et al. A systematic review of correlates of sedentary behaviour in adults aged 18–65 years: a socio-ecological approach. BMC Public Health 2016;16(163):1-25. [DOI: 10.1186/s12889-016-2841-3] [DOI] [PMC free article] [PubMed]
Otten 2009
- Otten JJ, Jones KE, Littenberg B, Harvey-Berino J. Effects of television viewing reduction on energy intake and expenditure in overweight and obese adults: a randomized controlled trial. Archives of Internal Medicine 2009;169(22):2109-15. [DOI] [PubMed] [Google Scholar]
Owen 2011
- Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults' sedentary behavior: determinants and interventions. American Journal of Preventive Medicine 2011;41(2):189-96. [DOI] [PubMed] [Google Scholar]
Owen 2014
- Owen N, Salmon J, Koohsari MJ, Turrell G, Giles-Corti B. Sedentary behaviour and health: mapping environmental and social contexts to underpin chronic disease prevention. British Journal of Sports Medicine 2014;48(3):174-7. [DOI] [PubMed] [Google Scholar]
PA Guidelines Advisory Committee 2018
- 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services, 2018. [Google Scholar]
Parry 2013
- Parry S, Straker L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013;13(296):1-10. [DOI: 10.1186/1471-2458-13-296] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parry 2017a
- Parry SP, Coenen P, O'Sullivan PB, Maher CG, Straker LM. Workplace interventions for increasing standing or walking for preventing musculoskeletal symptoms in sedentary workers. Cochrane Database of Systematic Reviews 2017, Issue 1. [DOI: 10.1002/14651858.CD012486] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parry 2017b
- Parry SP, Coenen P, O'Sullivan PB, Maher CG, Straker LM. Workplace interventions for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers. Cochrane Database of Systematic Reviews 2019, Issue 11. [DOI: 10.1002/14651858.CD012487] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peddie 2013
- Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. American Journal of Clinical Nutrition 2013;98(2):358-66. [DOI] [PubMed] [Google Scholar]
Perera 2007
- Perera Rl, Heneghan C, Yudkin P. Graphical method for depicting randomised trials of complex interventions. British Medical Journal 2007;334:127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pettee 2009
- Pettee KK, Ham SA, Macera CA, Ainsworth BE. The reliability of a survey question on television viewing and associations with health risk factors in US adults. Obesity 2009;17(3):487-93. [DOI] [PubMed] [Google Scholar]
Prapavessis 2015
- Prapavessis H, Gaston A, DeJesus S. The Theory of Planned Behavior as a model for understanding sedentary behavior. Psychology of Sport and Exercise 2015;19:23-32.
Prince 2014
- Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta‐analysis of controlled trials. Obesity Reviews 2014;15(11):905-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richards 2013
- Richards J, Thorogood M, Hillsdon M, Foster C. Face-to-face interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD010392.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2016
- Ryan R, Synnot A, Hill S. Describing results: CCCG. http://cccrg.cochrane.org/author-resources 1 December 2016;Version 2.0.
Same 2016
- Same RV, Feldman DI, Shah N, Martin SS, Al Rifai M, Blaha MJ, et al. Relationship between sedentary behavior and cardiovascular risk. Current Cardiology Reports 2016;18(1):1-7. [DOI] [PubMed] [Google Scholar]
Sedentary Behaviour and Obesity Working Group 2010
- The Sedentary Behaviour and Obesity Expert Working Group. Sedentary Behaviour and Obesity: Review of the Current Scientific Evidence. UK: Department of Health, 2010. [Google Scholar]
Sedentary Behaviour Research Network 2012
- Sedentary Behaviour Research Network. Letter to the Editor: Standardized use of the terms "sedentary" and "sedentary behaviours". Applied Physiology, Nutrition, and Metabolism 2012;37:540–2. [DOI] [PubMed] [Google Scholar]
Shrestha 2014
- Shrestha N, Ijaz S, Kukkonen-Harjula KT, Kumar S, Nwankwo CP. Workplace interventions for reducing sitting at work. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD010912] [DOI] [PubMed] [Google Scholar]
Shrestha 2016
- Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Bhaumik S. Workplace interventions for reducing sitting at work. Cochrane Database of Systematic Reviews 2016, Issue 3. [DOI: 10.1002/14651858.CD010912.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stamatakis 2011
- Stamatakis E, Hamer M, Dunstan DW. Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up. Journal of the American College of Cardiology 2011;57(3):292-9. [DOI] [PubMed] [Google Scholar]
Stamatakis 2019
- Stamatakis E, Ekelund U, Ding D, Hamer M, Bauman AE, Lee I. Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. British Journal of Sports Medicine 2016;53:377-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Chapter 10: Addressing reporting biases. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
The Nielsen Company 2009
- The Nielsen Company. Television, Internet and Mobile Usage in the U.S. A2/M2 Three Screen Report, 1st Quarter 2009. New York: The Nielsen Company, 2009. [Google Scholar]
Thorp 2011
- Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: a systematic review of longitudinal studies, 1996–2011. American Journal of Preventive Medicine 2011;41(2):207-15. [DOI] [PubMed] [Google Scholar]
Thorp 2014
- Thorp AA, Kingwell BA, Sethi P, Hammond L, Owen N, Dunstan DW. Alternating bouts of sitting and standing attenuate postprandial glucose responses. Medicine & Science in Sports & Exercise 2014;46(11):2053-61. [DOI] [PubMed] [Google Scholar]
Thraen‐Borowski 2017
- Thraen-Borowski KM, Ellingson LD, Meyer JD, Cadmus-Bertram CD. Nonworksite interventions to reduce sedentary behavior among adults: a systematic review. Translational Journal of the ACSM 2017;2(13):68-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tremblay 2011
- Tremblay MS, LeBlanc AG, Janssen I, Kho ME, Hicks A, Murumets K, et al. Canadian sedentary behaviour guidelines for children and youth. Applied Physiology, Nutrition, and Metabolism 2011;36(1):59-64. [DOI] [PubMed] [Google Scholar]
Troiano 2008
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise 2008;40(1):181-8. [DOI] [PubMed] [Google Scholar]
White 2009
- White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations. In: Babones SJ, editors(s). Social Inequality and Public Health. Bristol: The Policy Press, 2009:65-82. [Google Scholar]
WHO 2009
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva: WHO Press, 2009. [Google Scholar]
WHO 2019
- World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children Under 5 Years of Age. Geneva: WHO Press, 2019. [PubMed]
Wilmot 2012
- Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia 2012;55(11):2895-905. [DOI] [PubMed] [Google Scholar]
Yang 2019
- Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, et al. Trends in sedentary behavior among the US population, 2001-2016. Journal of the American Medical Association 2019;321(16):1587-97. [DOI] [PMC free article] [PubMed] [Google Scholar]


