Abstract
Objectives
To assess the knowledge of dentists regarding medication-related osteonecrosis of the jaw (MRONJ).
Methods
In this cross-sectional study, 74 dentists from governmental hospitals in Riyadh (Dental University Hospital in King Saud University, Military Hospital, National Guard Hospital), Jeddah (King Abdulaziz University Hospital, Ministry of Health Hospital), and the Eastern region of Saudi Arabia (Ministry of Health Hospitals in Dammam and Al-Ahsa) completed a two-part questionnaire. The first part gathered demographic data, such as sex and specialty. The second part included questions about bisphosphonate drugs and their indications; the identification of patients at risk of MRONJ; other medications associated with jaw necrosis; as well as the definition of MRONJ and its clinical features, risk factors, and preventive methods.
Results
Of the participating dentists, 60.8% knew about MRONJ, but only 35.1% were able to define it correctly. Most (79.7%) had never encountered MRONJ patients. Only 18.9% knew of the relationship between the risk of MRONJ in osteoporotic patients and long-term (>4 years) use of oral bisphosphonates or intravenous zoledronate, while 68.9% were unaware, and others answered incorrectly. Most participants did not know of MRONJ-predisposing medications, and 59.5% cited radiotherapy as the cause. Most participants identified dentoalveolar surgery as a major local factor, and the mandible as a common anatomic location.
Conclusion
Dentists at the surveyed institutions had poor knowledge of MRONJ, although their knowledge of preventive measures was good. There is an urgent need for the optimization of educational programs pertaining to MRONJ, and its related dental management considerations.
Clinical significance
Dentists in the surveyed institutions in Kingdom of Saudi Arabia have poor knowledge of MRONJ management; thus, greater effort should be taken to educate undergraduate and postgraduate students regarding this pathology.
Keywords: Biological sciences, Health sciences, Surgery, Dental surgery, Pharmacology, Dentistry, Antiresorptive agent, Bisphosphonate, Dentist, Knowledge, Medication-related osteonecrosis of the jaws
Biological sciences; Health sciences; Surgery; Dental surgery; Pharmacology; Dentistry; Antiresorptive agent, Bisphosphonate, Dentist, Knowledge, Medication-related osteonecrosis of the jaws.
1. Introduction
Bisphosphonates (BPs) are pyrophosphate-like molecules that have been used since the 1960s to prevent and treat osteoporosis. The new and more effective amino-substituted BPs are generally used to treat Paget's disease, bone metastases, and multiple myeloma and the associated malignant hypercalcemia. The incidence of complications related to the use of these drugs has gradually increased [1].
The first side-effects of BP drugs were described in 1996 by de Groen et al. [2], and consisted of common ulceration of the oesophagus upon the administration of alendronate. The most frequent side-effect of these drugs is BP-related osteonecrosis of the jaw (BRONJ), which affects the mandible more commonly than the maxilla. This is presumably due to the poorer vascularization of the mandible. BRONJ was first described by Marx et al. [3] in the early 2000s, and is currently diagnosed on the basis of necrotic bone exposed in the oral cavity for at least 8 weeks in patients with no history of head and neck radiotherapy. In 2003, the first cases of BRONJ were detected, and all of the initial observations were related to the potential role of intravenously administered BPs. In addition, BRONJ has been reported in few patients who had received oral non-nitrogen or oral nitrogen-containing BPs, for both cancerous and non-cancerous conditions [4]. BRONJ was described as an extremely therapy-resistant osteomyelitis-like disease, solely involving the jawbones of patients under treatment with BPs. In 2014, the American Association of Oral and Maxillofacial Surgeons (AAOMS) agreed to change the terminology from BRONJ to medication-related osteonecrosis of the jaw (MRONJ), to take into account the increasing number of cases of osteonecrosis of the jaws (ONJs) linked to other antiresorptive (denosumab) and antiangiogenic therapies [5].
By definition, MRONJ is an intense negative drug response, consisting of aggravating bone destruction in the maxillofacial area of patients [6]. The working definition has been modified from the 2009 AAOMS Position Paper [7]. Currently, if all features below are present, the patient is considered to have MRONJ:
-
1.
Treatment with antiangiogenic or antiresorptive agents, currently or previously.
-
2.
Bone probed through an intraoral or extra-oral fistula, or bone exposed in the maxillofacial area for more than 8 weeks.
-
3.
No previous radiation therapy or clear metastatic disease to the jaws.
The mechanisms underlying MRONJ are not yet fully understood, and many hypotheses have been postulated in an attempt to explain the unique localization of MRONJ exclusively to the jaws. These hypotheses include over-suppression of bone resorption, altered bone remodelling, persistent micro trauma, inhibition of angiogenesis, deficiency of vitamin D, suppression of acquired or innate immunity, infection or inflammation, and soft tissue BP toxicity [5].
In MRONJ, there is reduced bone resorption and remodelling due to inhibition of osteoclast differentiation and function, and increased apoptosis. Osteoclasts play an important role in bone remodelling and healing in all skeletal bones, while ONJ occurs primarily within the alveolar bone of the maxilla and mandible. This could be attributed to the increased remodelling rate in the jaws compared to other skeletal bones [5]. Many clinical studies have demonstrated that infection and inflammation can stimulate ONJ. Some studies have found bacteria, particularly Actinomyces spp., in biopsy specimens of necrotic bone from patients with ONJ [5].
Angiogenesis is the process of forming new blood vessels, and it requires the attachment of signalling molecules (e.g., vascular endothelial growth factor) to receptors on endothelial cells, which in turn stimulates new blood-vessel growth. Osteonecrosis is considered to involve an interruption in vascular supply, and therefore inhibits angiogenesis. This is one of the main hypotheses regarding ONJ pathophysiology [5].
Globally, a number of studies and various scientific societies have reported guidelines regarding MRONJ [5, 6, 7, 8, 9, 10]. In contrast, only two studies [11, 12] have measured the knowledge and degree of awareness of dental students about BRONJ, while no study to date has reported on the knowledge regarding drugs related to MRONJ. The aim of the present study was therefore to investigate the knowledge about MRONJ and its management among dentists.
2. Methods
The study was approved by the College of Medicine Institutional Review Board of King Saud University and the study complies with all regulations and the informed consent was obtained for each participant in the questionnaire. This cross-sectional questionnaire-based study was conducted among 100 dentists from several governmental hospitals in Riyadh (Dental University Hospital in King Saud University, Military Hospital, National Guard Hospital), Jeddah (King Abdulaziz University Hospital, Ministry of Health Hospital in Jeddah), and the Eastern region of Saudi Arabia (Ministry of Health Hospitals in Dammam and Al-Ahsa).
At a statistical significance level of alpha = 0.05, with 95% confidence level and a statistical power of 90%, the sample size was estimated as 36 participants. Adding 10% overestimation for any dropout from the survey making the minimum required is 40 participants. The final attained sample size was 74 dentists.
2.1. Questionnaire
The questionnaire was designed by the principal investigator and written in English language in the form of multiple-choice, closed-ended questions. It was composed of two main parts: the first consisted of demographic data related to age, sex, specialty, and city, while the second part consisted of questions pertaining to (1) BP drugs and their indications; (2) the identification of patients at risk of MRONJ; (3) other medications associated with jaw necrosis; as well as (4) the definition of MRONJ and its clinical features, risk factors, preventive methods, and dental management guidelines. The questionnaire forms were distributed in soft copies using Google forms. A probability sampling method have been used in distribution of the questionnaire through random sampling using email address-based sampling. The participants were made aware of our aim, the significance of the study, and the principal investigator's name. To maintain confidentiality, the participants were informed that their names were not required on the questionnaire.
2.2. Data management and statistical analysis
Data from this cross-sectional study was presented descriptively. All categorical variables were presented as percentages, while continuous variables were presented as mean and standard deviation. Student's t-test was used for comparison in cases of quantitative variables, and the chi-square or Fisher's exact test was used in cases of categorical variables. The null hypothesis was tested with p < 0.05 being considered statistically significant. All statistical tests were performed with SPSS for Windows version 15.0 (SPSS Inc., Chicago, IL).
3. Results
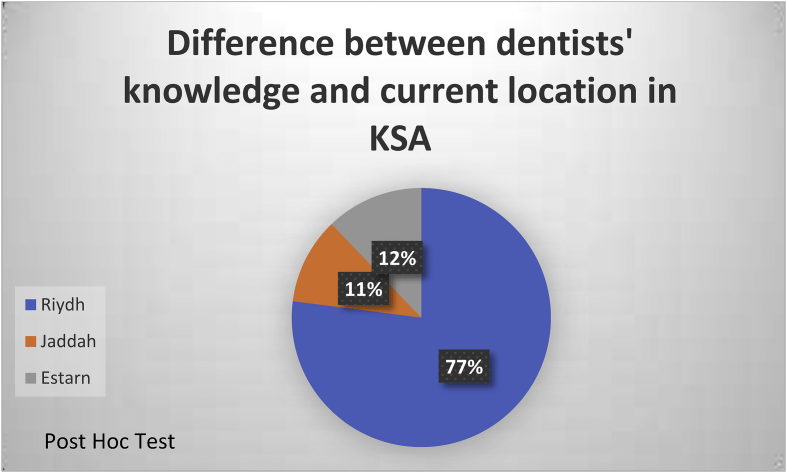
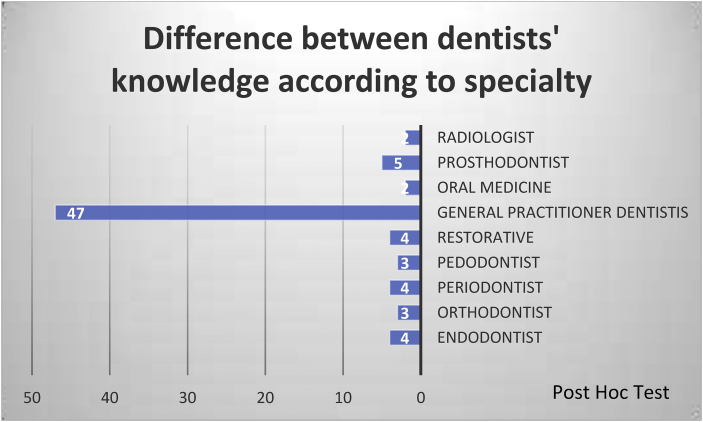
Seventy-four dentists completed the questionnaire after agreeing to participate. Regarding part 1 of the questionnaire, 77% of the respondents worked in Riyadh, 12.2% in the Eastern region, and 10.8% in Jeddah. Moreover, 71.6% of the participants worked in a clinical position, while 28.4% reported working in an academic position. In terms of experience, most (54.1%) had only some months of experience, while less than half (45.9%) had some years of experience. Respondents were working in different specialties (endodontics, pedodontics, prosthodontics, periodontics, operative dentistry, etc.). The dentists' area of specialty is summarized in Table 1. In terms of the relationship of dentists' knowledge of MRONJ and their region of work or specialty, we found that there was no significant difference between the knowledge about MRONJ and the location of participants or their field of specialty (Figures 1 and 2, respectively).
Table 1.
Dentists' area of specialty.
| Specialty | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| General Practitioner dentist | 47 | 63.5 | 63.5 |
| Endodontist | 4 | 5.4 | 68.9 |
| Oral Medicine | 2 | 2.7 | 71.6 |
| Radiologist | 2 | 2.7 | 74.3 |
| Orthodontist | 3 | 4.1 | 78.4 |
| Pedodontist | 3 | 4.1 | 82.4 |
| Periodontist | 4 | 5.4 | 87.8 |
| Prosthodontist | 5 | 6.8 | 94.6 |
| Restorative | 4 | 5.4 | 100.0 |
| Total | 74 | 100.0 |
Figure 1.
Difference between dentists' knowledge and current location in the Kingdom of Saudi Arabia.
Figure 2.
Difference between dentists' knowledge according to specialty.
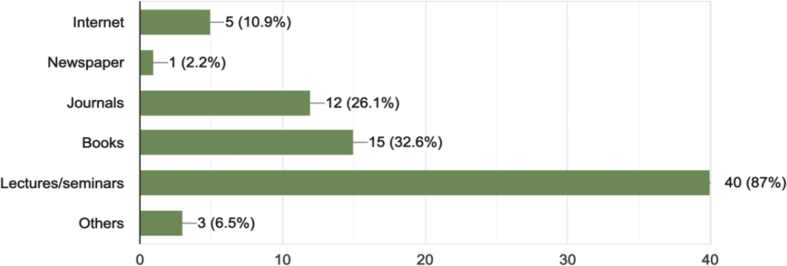
Results from part 2 of the questionnaire indicated that 60.8% of participants knew about MRONJ from various sources (Figure 3). While 39.2% said that they had not heard about MRONJ before, 2.7% of the dentists considered themselves as having a good understanding of MRONJ, to a large extent, 9.5% to a moderate extent, 33.8% to some extent, 37.8% to a small extent, and 16.2% not at all. Just under a tenth (9.5%) of the dentists had previously encountered a patient with MRONJ, while the majority (79.7%) never had such an experience. Over a third (35.1%) of respondents were able to recognize the correct definition of MRONJ.
Figure 3.
Percentage of dentists' answer to the question “How did you hear about MRONJ?”
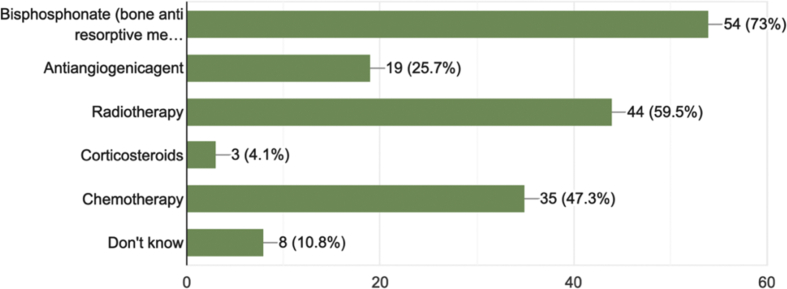
With respect to the MRONJ risk factors, most of the participants did not know the medications that predispose to MRONJ, and most of them selected incorrect answers, with the majority (59.5%) selecting radiotherapy (Figure 4).
Figure 4.
Percentage of dentists' answer to the question “MRONJ can occur with which medication?”
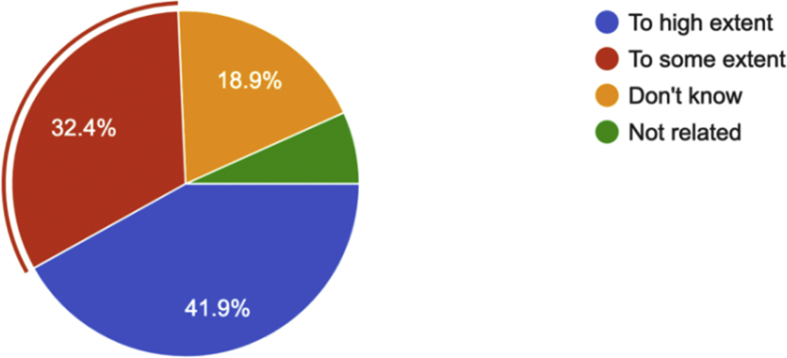
Regarding the risk of long-term therapy with intravenous BPs, only 18.9% of participants were able to identify osteoporotic patients receiving long-term (>4 years) oral BPs or IV zoledronate treatment, as a risk. The majority (68.9%) were unaware of the risk, and the rest provided incorrect answers (Table 2).
Table 2.
Dentists' answer to the question “MRONJ risk among osteoporosis patients is related to…”.
| Dentist's answer | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| Oral alendronate (Fosamax®) for 1 year | 3 | 4.1 | 4.1 |
| Oral sorafenib (Nexavar®) for 2 months | 3 | 4.1 | 8.1 |
| Long term oral bisphosphonate greater than 4 years or IV zoledronate | 14 | 18.9 | 27.0 |
| Oral ibandronate (Boniva®) | 3 | 4.1 | 31.1 |
| Not aware | 51 | 68.9 | 100.0 |
| Total | 74 | 100.0 |
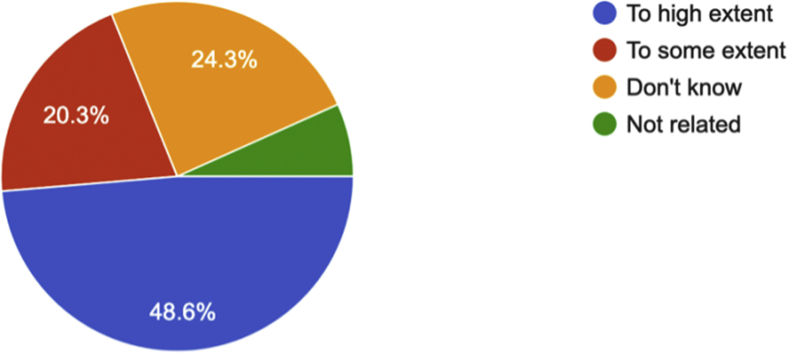
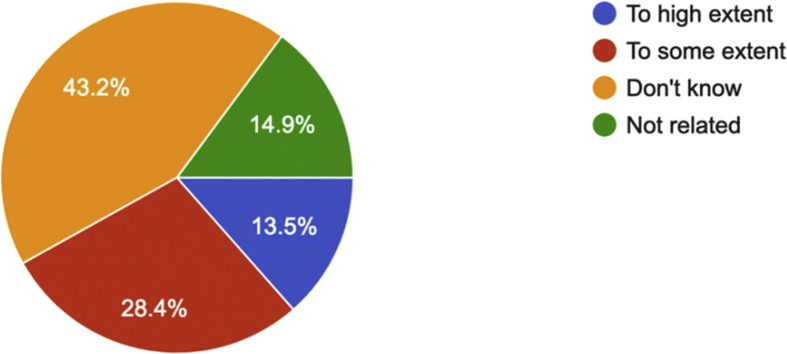
In terms of the knowledge of the duration of medication use as a general risk factor, only 32.4% of the participants were able to recognize that, regardless of indications for therapy, the duration of BPs or antiresorptive therapy continues to be a risk factor for developing MRONJ (Table 3). Regarding MRONJ risk in cancer patients and osteoporotic patients, only 14.9% of the participating dentists knew that the risk was 100 times smaller in osteoporotic patients (Table 4).
Table 3.
Dentists' answer to the question “Regardless of indications for therapy, the duration of BP or antiresorptive therapy continues to be a risk factor for developing MRONJ”.
| Dentist's answer | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| Yes | 24 | 32.4 | 32.4 |
| No | 3 | 4.1 | 36.5 |
| Don't Know | 47 | 63.5 | 100.0 |
| Total | 74 | 100.0 |
Table 4.
Dentists' answer to the question “When compared to cancer patients receiving antiresorptive treatment, the risk of MRONJ for patients with osteoporosis exposed to antiresorptive medications is about 100 times smaller”.
| Dentist's answer | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| Yes | 11 | 14.9 | 14.9 |
| No | 7 | 9.5 | 24.3 |
| Don't Know | 56 | 75.7 | 100.0 |
| Total | 74 | 100.0 |
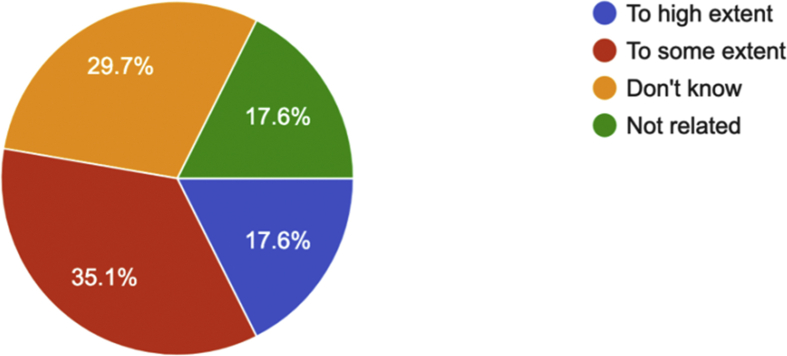
Most participants identified dentoalveolar surgery as a major local risk factor, and the mandible as a common anatomic location for MRONJ. Other predisposing local factors, including concomitant oral diseases, corticosteroid therapy, co-morbid conditions, type of cancer, and tobacco use, were singled out by up to a third (13.5–35.1%) of participants. Only 14.9% of participants identified genetic susceptibility to MRONJ as one of the risk factors for its development. Figures 5, 6, 7, 8, 9, 10, 11, and 12 show the responses of the participants regarding the influence of local factors on the incidence of MRONJ.
Figure 5.
Percentage of dentists' answers regarding dentoalveolar surgery as a local factor related to the incidence of MRONJ.
Figure 6.
Percentage of dentists' answers regarding the anatomic location as a local factor related to the incidence of MRONJ.
Figure 7.
Percentage of dentists' answers regarding concomitant oral disease as a local factor related to the incidence of MRONJ.
Figure 8.
Percentage of dentists' answers regarding corticosteroid therapy as a local factor related to the incidence of MRONJ.
Figure 9.
Percentage of dentists' answers regarding co-morbid conditions as local factors related to the incidence of MRONJ.
Figure 10.
Percentage of dentists' answers regarding cancer type as a local factor related to the incidence of MRONJ.
Figure 11.
Percentage of dentists' answers regarding tobacco as a local factor related to the incidence of MRONJ.
Figure 12.
Percentage of dentists' answers regarding genetic susceptibility as a local factor related to the incidence of MRONJ.
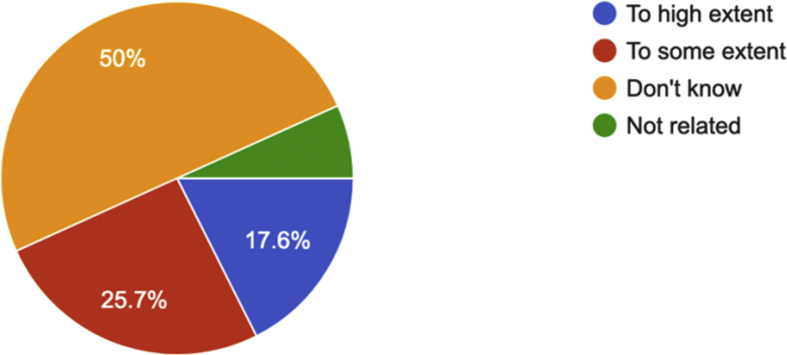
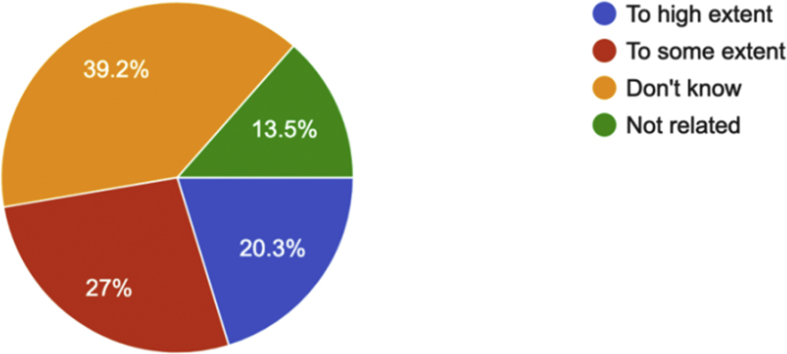
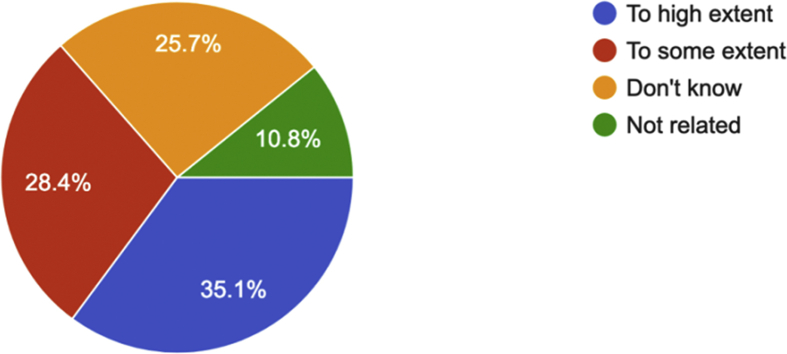
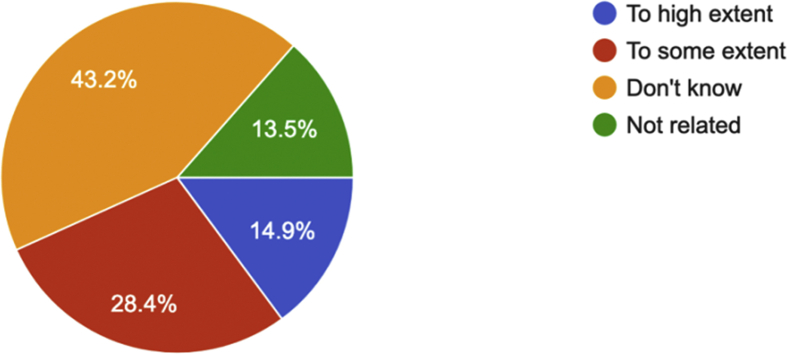
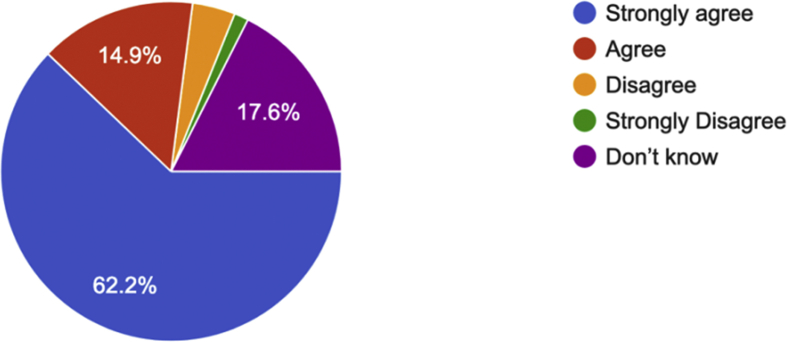
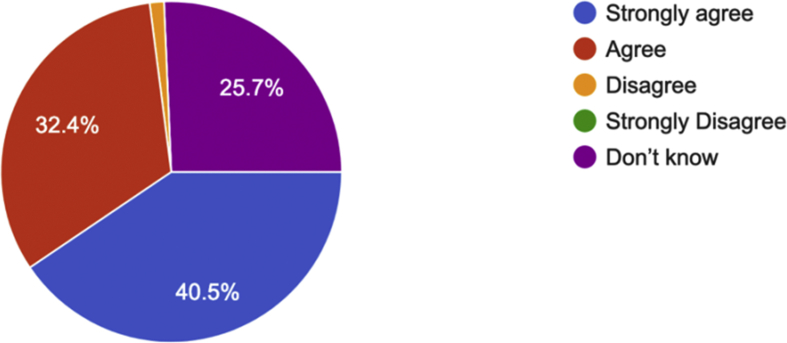
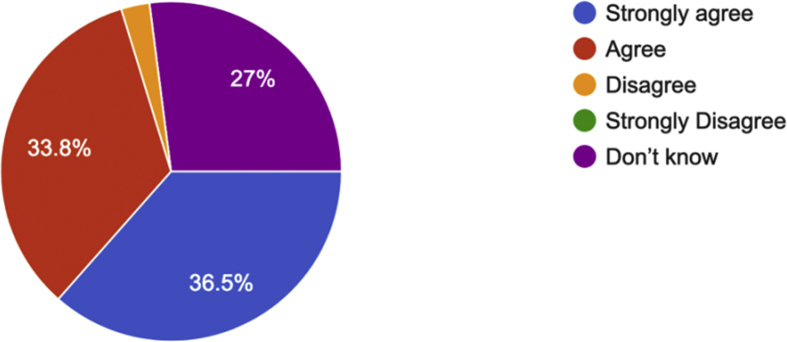
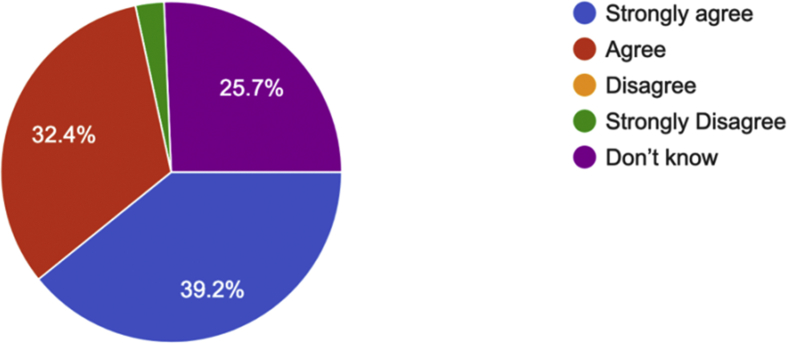
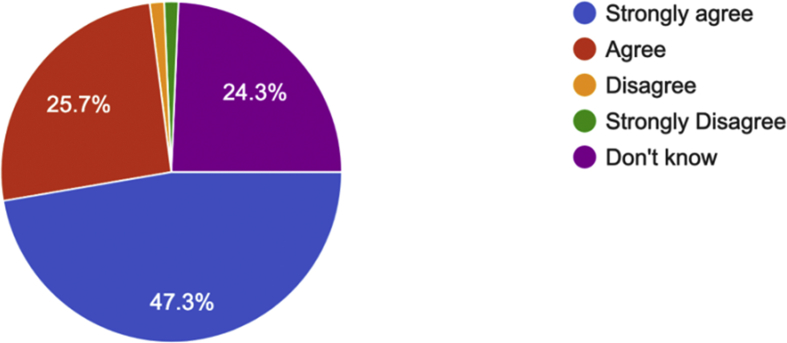
The final section of the questionnaire assessed knowledge pertaining to MRONJ management strategies and prevention. Over half (62.2%) of the dentists strongly agreed with early dental screening, and 40.5% strongly agreed with appropriate dental measures before initiating antiresorptive therapy. Over a third strongly agreed with a multi-disciplinary approach in managing MRONJ (36.5%), and an early identification of both acute infection and sites of potential infection before the start of drug therapy (39.2%). Just under a half (47.3%) strongly agreed with the patient being informed of the risks associated with these drug therapies before consenting to treatment (Figures 13, 14, 15, 16, and 17). Furthermore, just under a fifth (17.6%) of the dentists recognized that, with antiresorptive therapy in osteoporosis/osteopenia cases with extended exposure histories (>4 years), cessation of the at-risk medication therapy (i.e., a drug holiday) prior to tooth extraction or other procedures that involve osseous injury (e.g., dental implant placement, or periodontal, or apical endodontic treatment) is recommended (Table 5).
Figure 13.
Percentage of dentists' answers regarding agreement about early dental screening.
Figure 14.
Percentage of dentists' answers regarding agreement about appropriate dental measures before initiating antiresorptive therapy.
Figure 15.
Percentage of dentists' answers regarding agreement on a multidisciplinary approach.
Figure 16.
Percentage of dentists' answers regarding agreement about the identification of acute infection and sites of potential infection.
Figure 17.
Percentage of dentists' answers regarding agreement about a patient being informed of the risk.
Table 5.
Dentists' answer to the question “You recommend cessation of at-risk medication therapy (drug holiday) prior to tooth extraction or other procedures that involve osseous injury (e.g.: dental implant placement, periodontal or apical endodontic treatment)”.
| Dentist's' answer | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| Antiresorptive therapy for osteoporosis/osteopenia for those patients with extended exposure histories (>4 yrs) | 13 | 17.6 | 17.6 |
| Oncology patients receiving monthly antiresorptive therapy until soft tissue closure has occurred | 12 | 16.2 | 33.8 |
| Patient taking oral alendronate 70 mg once weekly for 8 months | 4 | 5.4 | 39.2 |
| Sunitinib 50 mg orally for 4 weeks | 1 | 1.4 | 40.5 |
| Not aware | 44 | 59.5 | 100.0 |
| Total | 74 | 100.0 |
4. Discussion
A high level of awareness and knowledge of MRONJ is necessary for its adequate prevention and management. In this study, we investigated the knowledge of MRONJ and its management among 74 dentists from different specialties, at various institutions in the Kingdom of Saudi Arabia. A large majority of the surveyed dentists had never encountered a MRONJ case, and had poor knowledge in terms of MRONJ management, although their knowledge about preventive measures was good.
The results of this study are a reason for concern, as 39.2% of the participants had not heard about MRONJ at all. A large proportion also lacked adequate knowledge of MRONJ diagnosis, and of issues related to the dental management of patients receiving BPs and other related drugs. The majority of dentists who had heard about MRONJ before, cited previous lectures or seminars as the source. Overall, about a third considered themselves to have a good understanding of MRONJ to some extent, while only 2.7% considered themselves to have good knowledge to a large extent. Similar findings have been reported by studies conducted in other countries. In a survey of dentists in Mexico, Vinitzky-Brener et al. [13] reported that 40.5% of respondents were familiar with the term BP-related osteonecrosis. Only 24.6% knew of at least one BP drug, and 15.9% could recognize at least one BP brand name. Another study, conducted in Korea by Yoo et al. [15], found that 56.5% of dentists were familiar with BRONJ, and 31.4% documented BP use in their patients' medical history. A more recent similar research among medical students by S. Franchi et al 2019 was showing results in agreement with our results more specifically the deficiency in knowledge about medications that predispose patients to the jaw necrosis [17].
The authors reported that most of the surveyed dentists were not aware of the guidelines of the AAOMS [15]. A study conducted by Alhussain et al. [16] among dentists in Ontario, Canada, reported that 60% had sufficient knowledge of BP-related osteonecrosis. However, half (50%) of the respondents were incompetent in treating patients using BPs, and only 23% reported that they followed published guidelines regarding surgical treatment [16].
A comparison between the present study and the results of previous similar work conducted by Rosella et al. [6] at Sapienza University of Rome, Italy, suggests that, in general, the dentists in Saudi Arabia have less knowledge about MRONJ cases. For instance, 79.6% of the surveyed dentists in Italy identified the duration of BP use and antiresorptive therapy as risk factors for MRONJ, compared to only 32.4% of the surveyed Saudi dentists. The surveyed Italian dentists also showed a greater awareness of issues related to the dental management of patients receiving medication for MRONJ. Contrastingly, in our study, 73% of Saudi dentists knew the correct definition of MRONJ, compared to 61.7% in Italy. Regarding risk factors for MRONJ development, 28.4% were able to recognize chronic corticosteroid therapy as a risk factor, compared with 24% among Italian dentists. Additionally, almost three-quarters (74.5%) of our participants recognized that the anatomic location (i.e. the mandible, as opposed to the maxilla) is the most important local factor related to the incidence of MRONJ.
BPs are divided into two main groups: non-nitrogen containing molecules (clodronate and etidronate) which are less potent, and a more potent nitrogen-moiety-containing group (zoledronic acid, pamidronate, alendronate, ibandronate, risedronate, and others) [14]. In addition to their effects on bone, BPs containing nitrogen have been used in the treatment of cancer because of their antiangiogenic and antitumor properties [13]. The specific mechanisms through which BPs and other medications increase the risk of ONJ is still unknown. Nevertheless, it is apparent that ONJ is a multifactorial condition in which local trauma, disruption of bone remodelling, concomitant cancer therapies, and pre-existing dental disease may have a role in reducing angiogenesis, and super-infection can lead to a disrupted bone microenvironment susceptible to osteonecrosis [13].
A few limitations are acknowledged in the present study. For instance, the sample size was relatively small, and restricted to selected locales in Saudi Arabia. As such, the results obtained may not be representative of all dentists across the entire country. Future studies should utilize larger sample sizes, and sample from a larger number of cities in Saudi Arabia.
5. Conclusion
Knowledge of MRONJ management among the surveyed dentists in this study was found to be poor. These results are a cause for concern, and suggest that greater efforts should be made to educate undergraduate and postgraduate students about this pathology. Additionally, we advise an increase in the number of seminars and educational programs about MRONJ which are targeted towards both dentists and physicians. This would serve to both increase the awareness of this complication, and facilitate co-operation between physicians and dental teams, ultimately leading to improved patient care.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Declarations
Author contribution statement
R. Al Eid: Conceived and designed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
M. Khuthaylah: Analyzed and interpreted the data; Wrote the paper.
T. Alduwayan: Performed the experiments; Wrote the paper.
M. Al Shemali: Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We wish to acknowledge all of the dentists who participated in the survey and contributed to the research.
References
- 1.Viviano M., Addamo A., Cocca S. A case of bisphosphonate-related osteonecrosis of the jaw with a particularly unfavourable course: a case report. J. Korean Assoc. Oral Maxillofac. Surg. 2017;43:272–275. doi: 10.5125/jkaoms.2017.43.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Groen P.C., Lubbe D.F., Hirsch L.J., Daifotis A., Stephenson W., Freedholm D., Pryor-Tillotson S., Seleznick M.J., Pinkas H., Wang K.K. Esophagitis associated with the use of alendronate. N. Engl. J. Med. 1996;335:1016–1021. doi: 10.1056/NEJM199610033351403. [DOI] [PubMed] [Google Scholar]
- 3.Marx R.E., Sawatari Y., Fortin M., Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J. Oral Maxillofac. Surg. 2005;63:1567–1575. doi: 10.1016/j.joms.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Beninati F., Pruneti R., Ficarra G. Bisphosphonate-related osteonecrosis of the jaws (BRONJ) Med. Oral Patol. Oral Cir. Bucal. 2013;18:e752–e758. doi: 10.4317/medoral.18076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruggiero S.L., Dodson T.B., Fantasia J., Goodday R., Aghaloo T., Mehrotra B., O'Ryan F. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J. Oral Maxillofac. Surg. 2014;72:1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 6.Rosella D., Papi P., Pompa G., Capogreco M., De Angelis F., Di Carlo S. Dental students' knowledge of medication-related osteonecrosis of the jaw. Eur. J. Dermatol. 2017;11:461–468. doi: 10.4103/ejd.ejd_27_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruggiero S.L., Dodson T.B., Assael L.A., Landesberg R., Marx R.E., Mehrotra B. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws—2009 update. J. Oral Maxillofac. Surg. 2009;67:2698–2699. doi: 10.1016/j.joms.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Rosella D., Papi P., Giardino R., Cicalini E., Piccoli L., Pompa G. Medication-related osteonecrosis of the jaw: clinical and practical guidelines. J. Int. Soc. Prev. Community Dent. 2016;6:97–104. doi: 10.4103/2231-0762.178742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim K.M., Rhee Y., Kwon Y.D., Kwon T.G., Lee J.K., Kim D.Y. Medication related osteonecrosis of the jaw: 2015 position statement of the Korean society for bone and mineral research and the Korean association of oral and maxillofacial surgeons. J. Bone Metab. 2015;22:151–165. doi: 10.11005/jbm.2015.22.4.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Japanese Allied Committee on Osteonecrosis of the Jaw. Yoneda T., Hagino H., Sugimoto T., Ohta H., Takahashi S., Soen S., Taguchi A., Nagata T., Urade M., Shibahara T., Toyosawa S. Antiresorptive agent-related osteonecrosis of the jaw: position paper 2017 of the Japanese allied committee on osteonecrosis of the jaw. J. Bone Miner. Metabol. 2017;35:6–19. doi: 10.1007/s00774-016-0810-7. [DOI] [PubMed] [Google Scholar]
- 11.Lo J.C., O'Ryan F.S., Gordon N.P., Yang J., Hui R.J., Martin D., Hutchinson M., Lathon P.V., Sanchez G., Silver P., Chandra M., McCloskey C.A., Staffa J.A., Willy M., Selby J.V., Go A.S. Prevalence of osteonecrosis of the jaw in patients with oral bisphosphonate exposure. J. Oral Maxillofac. Surg. 2010;68:243–253. doi: 10.1016/j.joms.2009.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vandone A.M., Donadio M., Mozzati M., Ardine P., Polimeni M.A., Beatrice S., Ciuffreda L., Scoletta M. Impact of dental care in the prevention of bisphosphonate-associated osteonecrosis of the jaw: a single-center clinical experience. Ann. Oncol. 2012;23:193–200. doi: 10.1093/annonc/mdr039. [DOI] [PubMed] [Google Scholar]
- 13.Vinitzky-Brener I., Ibáñez-Mancera N.G., Aguilar-Rojas A.M., Álvarez-Jardón A.P. Knowledge of bisphosphonate-related osteonecrosis of the jaws among Mexican dentists. Med. Oral Patol. Oral Cir. Bucal. 2017;22:e84–e87. doi: 10.4317/medoral.21433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rogers M.J. New insights into the molecular mechanisms of action of bisphosphonates. Curr. Pharmaceut. Des. 2003;9:2643–2658. doi: 10.2174/1381612033453640. [DOI] [PubMed] [Google Scholar]
- 15.Yoo J.Y., Park Y.D., Kwon Y.D., KimY D.Y., Ohe J.Y. Survey of Korean dentists on the awareness on bisphosphonate-related osteonecrosis of the jaws. J. Investig. Clin. Dent. 2010;1:90–95. doi: 10.1111/j.2041-1626.2010.00024.x. [DOI] [PubMed] [Google Scholar]
- 16.Alhussain A., Peel S., Dempster L., Clokie C., Azarpazhooh A. Knowledge, practices, and opinions of Ontario dentists when treating patients receiving bisphosphonates. J. Oral Maxillofac. Surg. 2015;73:1095–1105. doi: 10.1016/j.joms.2014.12.040. [DOI] [PubMed] [Google Scholar]
- 17.Franchi S., Brucoli M., Boffano P., Dosio C., Benech A. Medical students’ knowledge of medication related osteonecrosis of the jaw. J. Stomatol. Oral Maxillofac. Surg. 2019 doi: 10.1016/j.jormas.2019.10.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.