Abstract
Introduction
The majority (99%) of the children who die during the first 4 weeks of life do so in the poorer parts of the world, especially in sub-Saharan Africa and South Asia. In 2018, sub-Saharan Africa had a neonatal mortality rate of 28 deaths per 1000 live births. The purpose of the review was to explore and describe the trends of neonatal mortality within the two sub-Saharan countries.
Methods
We did a literature search in biomedical databases of data published, in English, between Jan 1, 1975, and November 30, 2019. The databases included Scopus, Web of Science, Science Direct, Cochrane Library, PUBMED, OVID and Google scholar. The keywords used in the search: “Neonatal Survival”, “Sub-Sahara”, “Kenya” and “South Africa”.
Results
The search generated 2209 articles of which only 27 met the inclusion criteria. The present study qualitatively analysed data. Data were presented and organized under two thematic domains: 1) trends of national neonatal mortality rates in South Africa and Kenya and 2) causes of neonatal mortality.
Conclusion
The current review results noted that in 2018, the neonatal mortality rate for Kenya was 19.6 deaths per 1000 live births. The neonatal mortality rate has fallen gradually from 35.4 deaths per 1000 live births in 1975. On the other hand, South Africa has had its neonatal mortality rate fall from 27.9 deaths per 1000 live births in 1975 to 10.7 deaths per 1000 live births in 2018. Most neonatal deaths resulted in preterm birth complications followed by intrapartum-related events for the two countries. Within the sub-Saharan region, disparities exist as neonates born in South Africa are more likely to survive during the neonatal period compared to Kenya.
Keywords: Africa, infant, Kenya, newborn, mortality, South Africa
What is known?
The majority (99%) of the children who die during the first 4 weeks of life do so in the poorer parts of the world, especially in sub-Saharan Africa and South Asia.
In 2018, the Neonatal Mortality Rate (NMR) for Kenya was 19.6 deaths per 1000 live births.
In 2018, the NMR for South Africa was 10.7 deaths per 1000 live births.
What is new?
The most neonatal deaths resulted from preterm birth complications followed by intrapartum-related events for the two countries.
Within the sub-Saharan region, disparities exist as neonates born in South Africa are more likely to survive during the neonatal period compared to Kenya.
Introduction
A newborn infant, or neonate, is a child under 28 days of age.1 During these first 28 days of life, the child is at the highest risk of dying.1 Globally 2.5 million children died in the first month of life in 2018, an estimate that may be significantly higher considering the likelihood of under-reporting, especially in low-income and middle-income countries.2,3 There are approximately 7000 newborn deaths every day.2 On current trends, neonatal mortality declined more slowly than mortality among children aged 1–59 months.2 As a result, the share of neonatal deaths among all under-five deaths increased from 40% in 1990 to 47% in 2018.2 Reducing neonatal mortality is increasingly important not only because the proportions of under-five deaths that occur during the neonatal period are increasing as under-five mortality declines but also because the health interventions needed to address the major causes of neonatal deaths generally differ from those needed to address other under-five deaths.4
Every year, 135 million newborns enter the world, each arriving naked and apparently equal.5 Yet, their chances of surviving and thriving vary dramatically depending on which world these babies are born into—ranging from high-income countries with universal neonatal intensive care to the world of home births without midwives, medical supplies, or health system support.5 Skilled health care during pregnancy, childbirth and in the postnatal (immediately following birth) period prevents complications for mother and newborn, and allows for early detection and management of problems.1 In addition, WHO and UNICEF now recommend home visits by a skilled health worker during a baby’s first week of life to improve newborn survival.1
Among the Sustainable Development Goal (SDG) regions, sub-Saharan Africa had the highest neonatal mortality rate in 2018 at 28 deaths per 1000 live births, followed by Central and Southern Asia with 25 deaths per 1000 live births.6 A child born in sub-Saharan Africa is 10 times more likely to die in the first month than a child born in a high-income country.6
With modest trends in reducing neonatal mortality in sub-Saharan Africa and high levels of neonatal mortality, many countries in the region are at risk of missing the SDG target on neonatal mortality.6 Estimates by UNICEF show that 42 of 48 countries in the region are projected to miss the SDG neonatal mortality target by 2030.6 About half are projected to meet the SDG target sometime after 2050 if progress is not accelerated.6
In the African Region, 1.12 million newborn deaths occur annually.1 The main causes include prematurity and low-birth-weight, infections, lack of oxygen at birth, and birth trauma.1 These causes account for nearly 80% of the deaths in this age group.1,7 Neonates, especially in sub-Saharan Africa (SSA), are challenged with a diversity of lethal clinical conditions, especially infectious diseases, which demand urgent interventions.8 When these clinical conditions, such as birth asphyxia, septicemia, jaundice, meningitis and tetanus are not appropriately diagnosed and attended to in time, they worsen the statistics of neonatal mortality in SSA.8 The purpose of the current review was to explore and describe the trends of neonatal mortality within the two sub-Saharan countries that is Kenya and South Africa.
Methods
Inclusion and Exclusion Criteria
All descriptive or cross-sectional or observational, retrospective, national, regional studies reporting on the present research problem were included. An article was included if it met the following criteria: 1) Conducted in Kenya, South Africa, or within the sub-Saharan Region and published between Jan 1, 1975, and November 30, 2019, 2) had study participants as deceased neonates and 3) published in English. Conference abstracts, letters to editors, review, and commentary articles were excluded.
Data Sources and Search Strategies
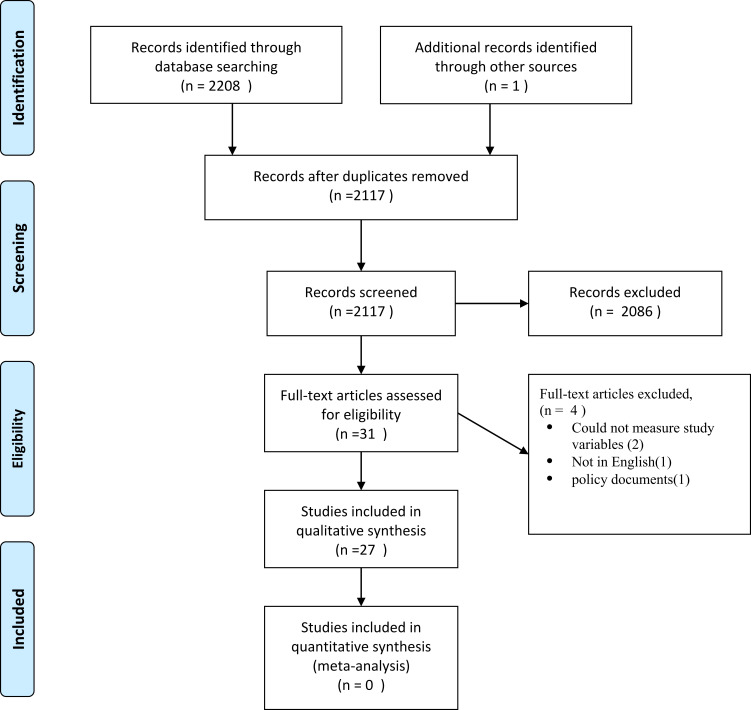
A systematic search of articles was from the following databases; Scopus, Web of Science, Science Direct, Cochrane Library, PUBMED, OVID and Google scholar (Figure 1). The search comprised both Medical Subject Headings (MeSH) and free text words (title and abstract word searches). The following were the keywords used in the search: “Neonatal Survival”, “Sub-Sahara”, “Kenya” and “South Africa”. Additionally, researchers searched grey literature resources such as a database/website of dissertations and theses and WHO websites. The reference list of included studies was manually searched for possible additional eligible articles. The searches were conducted from February 2019 to January 2020. In particular, the researchers used the following search terms in PUBMED database; “Neonatal Mortality” “causes of neonatal deaths” AND “Kenya” AND “South Africa” “Sub-Sahara”
Figure 1.
PRISMA flow diagram.
Note: Adapted from Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):65–94.9
Selection of Studies for Inclusion in the Review
Titles and abstracts of studies retrieved from each database search were stored in Mendeley Research Manager. Duplicates were removed before the screening process was initiated. Two review authors (BBM and RM) independently reviewed the titles and abstracts of all studies and disagreements were solved by discussion. The same steps were taken for full-text screening of the results.
Data Extraction and Management
Using a standardized data extraction form, two review authors (BBM and RM) independently extracted data from eligible studies including the first author’s last name, year of publication, study location, participant characteristics, study design utilized, major findings of the study.
Quality Assessment
Two review authors (BBM & RM) independently assessed the quality of all included studies using the Critical Appraisal skills programme. BBM assessed the quality of the included studies while RM checked the assessed studies. Disagreements were resolved by discussion between the four review authors. No study was excluded at this point after the quality assessment.
Synthesis of Results
The qualitative analysis was approved by the technical task team who got expert experience in biomedical systematic review. This was a secondary analysis and all identifiers of the individual participants were removed or presented using unique codes. This study adopted PRISMA (Figure 1) reporting as demonstrated previously by Liberati et al.9 Data was presented and organized under two thematic domains: 1) trends of national neonatal mortality rates in South Africa and Kenya and 2) causes of neonatal mortality.
Results and Discussion
The search generated 2209 articles of which 92 duplicate articles were removed. After the screening process of their titles and abstracts, only 31 articles were identified and were thereafter included in the full-text review. The identified articles were further assessed using the adopted inclusion criteria. Among 31 articles only 27 met the inclusion criteria (Figure 1). According to Table 1, the specific study settings of the articles utilised were as follows: 10 studies covered Sub-Sahara, 9 were conducted in Kenya and 8 were carried out in South Africa. The study participants were deceased neonates. Table 1 gives a further description of the articles utilised. The present study aimed to systematically explore and describe the trends of neonatal mortality within the two sub-Saharan countries. The findings were presented and discussed under two thematic domains: 1) trends of national neonatal mortality rates in South Africa and Kenya and 2) causes of neonatal mortality
Table 1.
A Description of the Articles Utilised
| Article | Year | Design | Setting | Results |
|---|---|---|---|---|
| Masaba and Mmusi-phetoe, 201910 | 2019 | Cross-sectional | Kenya | A multifaceted approach is needed to reduce neonatal mortalities in Kenya |
| Tank, Omar, and Musoke, 201911 | 2019 | Prospective audit | Kenya | Mortality was high among preterm neonates |
| Shikuku, Milimo, Ayebare, Gisore, and Nalwadda, 201812 | 2018 | Observational | Kenya | Effective resuscitation for birth asphyxia |
| Gitobu, Gichangi, and Mwanda, 201813 | 2018 | Survey | Kenya | Free maternal services increased hospital deliveries |
| Ayodo, Samba, Amimo, and Asweto, 201814 | 2018 | Survey design | Kenya | Preterm birth is one of the main causes of neonatal death |
| Wagura, Wasunna, Laving, Wamalwa, and Ng, 2018.15 | 2018 | Cross-sectional | Kenya | At-risk mothers should receive intensified antenatal care to mitigate preterm birth |
| Okube and Sambu, 201716 | 2017 | Cross-sectional | Kenya | Prevalence rate of preterm birth was 20.2% |
| Ministry-of-Health-[MOH], 201517 | 2015 | National surveys | Kenya | 1.5 million babies are born in Kenya annually |
| Yego et al, 201318 | 2013 | Retrospective | Kenya | Pre-term birth and asphyxia are the leading causes of neonatal deaths |
| Velaphi et al, 201919 | 2019 | Prospective study | South Africa | Using a combination of blood culture and a PCR-based test the common pathogens isolated in neonates with sepsis were Ureaplasma spp. and GBS |
| Rhoda, Velaphi, Gebhardt, Kauchali, and Barron, 2018.20 | 2018 | South Africa Demographic Health Survey | South Africa | South Africa has a double burden of disease driving neonatal mortality; term babies are dying owing to intrapartum-related events, and preterm deaths are linked to related complications. |
| Brits et al, 2015.21 | 2015 | Case control | South Africa | Co-morbidity as a risk to preterm birth |
| Rhoda and Velaphi, 201522 | 2015 | National survey | South Africa | Preterm infants are at high risk of developing hypothermia |
| Bruckmann and Velaphi, 2015.23 | 2015 | Medical record analysis | South Africa | The incidence of asphyxia ranged from 8.7 to 15.2/1000 live births |
| Bamford, 2015.24 | 2015 | National DHS analysis | South Africa | South Africa continues to face a high burden of disease and high maternal and child mortality rates. |
| Mabaso, Ndaba, and Mkhize-kwitshana, 2014.25 | 2014 | Analysis of National Department of Health | South Africa | Re-engineering of the Primary Health Care (PHC) services to reduce neonatal mortality |
| Save the Children Fund [SCF], 2013.26 | 2013 | National analysis | South Africa | 84,000 preterm births occur in South Africa annually |
| WHO, 20191 | 2019 | Regional estimates | Sub-Sahara | 15 million babies are born too early every year |
| Chawanpaiboon et al, 2019.27 | 2019 | Multi-regional analysis | Sub-Sahara | 12·0 million (81.1%) of these preterm births occurred in Asia and sub-Saharan Africa. |
| Amare, Mela, and Dessie, 2019.28 | 2019 | Review | Developing countries | Neonatal sepsis was found to be high which accounted for a third of the neonates. |
| Ranjeva, Warf, and Schiff, 2018.29 | 2018 | Global health agencies data analysis | Africa | Neonatal sepsis presents a $10–$469 billion financial burden that could be alleviated through successful treatment and prevention |
| Mongella, Songane, and Akande, 201030 | 2010 | Regional estimates | Africa | Each year at least 1.16 million newborns die in Sub-Saharan Africa |
| UNICEF, 2019.6 | 2019 | Global survey | United Nation regions | In 2018, the NMR for Kenya was 19.6 deaths per 1000 live births |
| Lawn et al, 2013.5 | 2013 | Systematic estimates | 12 countries | Investing in care of every woman and every newborn will reduce both deaths and disabilities |
| UNICEF, 2013.31 | 2013 | Regional estimates | Global analysis | Globally, an estimated 10 million babies have breathing difficulties at birth. |
| Gillam-Krakauer and Gowen, 2018.32 | 2018 | Regional estimates | – | 15–20% of babies diagnosed with birth asphyxia die during the neonatal period |
| Lawn, Mongi, and Cousens, 201033 | 2010 | Regional estimates | Africa | Birth asphyxia also accounts for 280,000 deaths a year in sub-Saharan Africa |
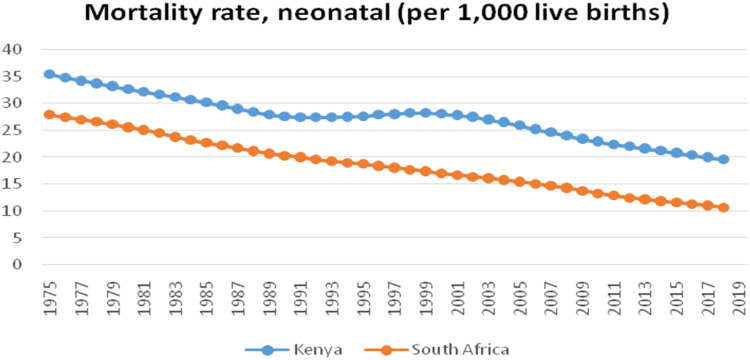
Kenya and South Africa National Neonatal Mortality Rate
In 2018, the NMR for Kenya was 19.6 deaths per 1000 live births (Figure 2). The NMR has fallen gradually from 35.4 deaths per 1000 live births in 1975, but the country is yet to achieve the SDG3 target 2 of reducing neonatal mortality to 12 deaths per 1000 live births.6 South Africa compared to Kenya has been having lower neonatal mortality rates for the past three decades. Its NMR has fallen gradually from 27.9 deaths per 1000 live births in 1975 to 10.7 deaths per 1000 live births in 2018. Of note also is that South Africa has achieved the set goal of SDG 3.2.6
Figure 2.
Kenya and South Africa National Neonatal Mortality rate, (per 1000 live births).
Causes of Neonatal Deaths in 2018: South Africa and Kenya
Table 2 shows that most neonatal deaths resulted from preterm birth complications followed by intrapartum-related events for South Africa, while in Kenya intrapartum-related complications were the leading cause. Neonatal sepsis, congenital abnormalities and pneumonia ranked 3rd, 4th, and 5th in both countries as diarrhoea was insignificant as a cause of neonatal death. South Africa has been able to manage intrapartum-related complications better than Kenya. However, South Africa continues to struggle with preterm births. Because South Africa’s economy is more developed than Kenya’s, their increased death rate from more preterm birth was unexpected. More developed income countries tend to have better universal neonatal intensive care to care for the preterm births than their counterparts.5
Table 2.
Percentage Distribution of Causes of Neonatal Deaths in 2018: South Africa and Kenya
| Causes | South Africa | Kenya |
|---|---|---|
| Preterm birth complications | 36% | 28% |
| Intrapartum related events | 20% | 29% |
| Sepsis/tetanus | 14% | 16% |
| Congenital abnormalities | 10% | 13% |
| Diarrhoea | 0% | 0% |
| Pneumonia | 5% | 7% |
| Other conditions | 15% | 8% |
Preterm Birth Complications
Findings from this review reveal that preterm birth complications were the top cause of neonatal mortalities in South Africa while in Kenya it ranked second.6,17,21 This finding implies that preterm births dying in South Africa were higher than in Kenya. Preterm birth (PTB) refers to babies born alive before 37 weeks of pregnancy are completed.14 Estimated 15 million babies are born too early every year.1 That is more than 1 in 10 babies.1 Approximately 1 million children die each year due to complications of preterm birth.1
Comparing with developed countries, preterm babies born from developing countries face higher morbidity and mortality rates.1 In low-income settings, half of the babies born as a preterm die due to a lack of feasible, cost-effective care, like provision of basic warmth, supporting breathing difficulties and taking preventive and control measures of infection.1 In high-income countries, almost all of these babies survive.16 The risk of neonatal death due to complications of preterm birth is at least 12 times higher for an African baby than for a European baby.15
Out of the 1.5 million babies born in Kenya annually, around 134,000 come too soon, according to the Ministry of Health’s Division of Family Health.17 Moreover, a hospital-based study by Yego et al18 found that pre-term birth and asphyxia are the leading causes of early neonatal deaths in a teaching and referral hospital in Kenya.18 In South Africa, more than 1.2 million babies are born annually, of whom 14% are born prematurely.21 Sadly, about 10% of these babies do not survive despite most births occurring at health-care facilities.26
Common complications of preterm birth are high rates of respiratory distress syndrome, bronchopulmonary dysplasia, necrotising enterocolitis, sepsis, periventricular leucomalacia, seizures, intraventricular haemorrhage, cerebral palsy, infections, feeding difficulties, hypoxic ischaemic encephalopathy, and visual and hearing problems.27 Preterm infants are at high risk of developing hypothermia because they do not have enough energy stores and brown fat to produce heat.22 Hypothermia is an independent risk factor for mortality – the more severe the hypothermia, the greater the mortality.22 Prematurity is a major cause of neonatal mortality and morbidity as well as a significant contributor to long-term adverse health outcomes.15,27
Intrapartum-Related Events
The study revealed that intrapartum-related complications accounted for the highest neonatal mortalities in Kenya while it ranked second in South Africa (Table 2). This implies South Africa is better prepared to handle newborn complications immediately after birth compared to Kenya.
Birth asphyxia, defined as the failure to initiate and sustain breathing at birth by WHO, causes about a quarter of all the neonatal deaths.12 Effective resuscitation at birth can prevent a large proportion – approximately 30% – of these deaths.12 Clinically, the need for bag-and-mask ventilation (BMV) at birth and/or an Apgar score <7 have been used to define intrapartum asphyxia.23
A report titled “Birth Asphyxia Complications” estimated 10 million babies have breathing difficulties at birth, mainly resulting in brain injury.31 This is caused by obstructed labour or acute haemorrhage during birth.31 Globally, more than 700,000 newborns died of birth complications and among survivors, 233,000 had a moderate or severe disability and another 181,000 had learning problems.31
According to Gillam-Krakauer and Gowen, the incidence of birth asphyxia is 2 per 1000 live births in developed countries, but the rate is up to 10 times higher in developing countries where there may be limited access to maternal and neonatal care.32 Gillam-Krakauer and Gowen further noted that of those babies affected 15–20% dies during the neonatal period and up to 25% of the survivors are left with permanent neurologic deficits.32
Birth asphyxia also accounts for 280,000 deaths a year in sub-Saharan Africa.33 Babies born in sub-Saharan Africa have a very high risk of birth asphyxia and intrapartum stillbirth.33 The best intervention is prevention through improved Antenatal Care (ANC) and, particularly, skilled attendance and emergency obstetric care.33
Sepsis | Tetanus
Systemic infections of the newborn such as septicaemia refer to generalised bacterial infection documented by a positive blood culture in the first 28 days of life.19 It encompasses various systemic infections of the newborn such as septicaemia, meningitis, pneumonia, arthritis, osteomyelitis and urinary tract infections.19
Sepsis accounts for around one-third of deaths in neonates worldwide.11 Neonatal sepsis usually has nonspecific presentation; hence, delay in treatment, and especially initiation of effective antibiotic therapy results in serious consequences ranging from neuro-developmental deficits to death.11 Sepsis was attributed to cause approximately 400,000 neonatal deaths in 2015 globally, half of which occurred in sub-Saharan Africa where 34.6% to 66.0% of neonatal deaths reportedly occur within the first 24 hours of life.19 Bacteria are the leading cause of neonatal sepsis.28 Early empirical antimicrobial treatment is associated with better outcomes in neonatal sepsis, but antimicrobials must be discontinued timeously to prevent the emergence of further antimicrobial resistance.34
Despite its disproportionate burden on childhood mortality, neonatal sepsis receives vastly less investment internationally as a public health priority compared with other major conditions.29 Studies by Save the Children Fund corroborate this by noting that neonatal tetanus is one of the most cost-effective conditions to prevent – yet it still kills tens of thousands of African babies each year.30
Conclusion
This systematic review noted that, although South Africa has achieved the WHO target of 12 neonatal deaths per every 1000 live births by 2030, it still has to work towards the challenges managing the preterm births. Additionally, review results noted that in 2018, the neonatal mortality rate for Kenya was 19.6 deaths per 1000 live births. The neonatal mortality rate has fallen gradually from 35.4 deaths per 1000 live births in 1975. On the other hand, South Africa has had its neonatal mortality rate fall from 27.9 deaths per 1000 live births in 1975 to 10.7 deaths per 1000 live births in 2018. Most neonatal deaths resulted from, preterm birth complications followed by intrapartum-related events for the two countries. Within the sub-Saharan region, disparities exist as neonates born in South Africa are more likely to survive during the neonatal period compared to Kenya.
Acknowledgments
The authors would like to thank the University of South Africa for their support to the study.
Author Contributions
All authors contributed towards data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors have declared that no conflicts of interest exist.
References
- 1.WHO. Newborn for Africa. Geneva: WHO; 2019. [Google Scholar]
- 2.WHO. Newborns Reducing Mortality. Geneva: World Health Organization; 2020. [Google Scholar]
- 3.Kayode GA, Grobbee DE, Amoakoh-coleman M, Ansah E, Uthman OA, Klipstein-grobusch K. Variation in neonatal mortality and its relation to country characteristics in sub-Saharan Africa: an ecological study. BMJ Glob Health. 2017;3(1–9):e000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Neonatal Mortality. Geneva: World Health Organization; 2016. [Google Scholar]
- 5.Lawn JE, Blencowe H, Darmstadt GL, Bhutta ZA. Beyond newborn survival: the world you are born into determines your risk of disability-free survival. Pediatr Res. 2013;74:4–6. doi: 10.1038/pr.2013.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNICEF. Child Mortality 2019. New York: United Nations Children’s Fund; 2019. [Google Scholar]
- 7.The-African-Academy-of-Sciences. From minding the gap to closing the gap. Acad Med Sci. 2018;9:1–28. [Google Scholar]
- 8.Afolabi BM. Sub-Sahara African neonates – ghosts to statistics. J Neonatal Biol. 2017;6(1):1–3. doi: 10.4172/2167-0897.1000246 [DOI] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):65–94. doi: 10.7326/0003-4819-151-4-200908180-00136 [DOI] [PubMed] [Google Scholar]
- 10.Masaba BB, Mmusi-phetoe R. Determinants of high neonatal mortality rates in Migori county referral hospital in Kenya. Int J Nurs Educ. 2019;11(4):181–185. doi: 10.5958/0974-9357.2019.00115.6 [DOI] [Google Scholar]
- 11.Tank PJ, Omar A, Musoke R. Audit of antibiotic prescribing practices for neonatal sepsis and measurement of outcome in new born unit at Kenyatta National Hospital. Int J Pediatr. 2019;2019:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shikuku DN, Milimo B, Ayebare E, Gisore P, Nalwadda G. Practice and outcomes of neonatal resuscitation for newborns with birth asphyxia at Kakamega County General Hospital, Kenya: a direct observation study. BMC Pediatr. 2018;18(167):1–11. doi: 10.1186/s12887-018-1127-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gitobu CM, Gichangi PB, Mwanda WO. The effect of Kenya ’ s free maternal health care policy on the utilization of health facility delivery services and maternal and neonatal mortality in public health facilities. BMC Pregnancy Childbirth. 2018;18(77):1–11. doi: 10.1186/s12884-018-1708-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayodo G, Samba BO, Amimo F, Asweto CO. Experience And perceptions on preterm births among women attending anc clinic at Kisumu County. J Public Health (Bangkok). 2018;4(3):1–17. [Google Scholar]
- 15.Wagura P, Wasunna A, Laving A, Wamalwa D, Ng P. Prevalence and factors associated with preterm birth at Kenyatta National Hospital. BMC Pregnancy Childbirth. 2018;18(107):2–9. doi: 10.1186/s12884-018-1740-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okube OT, Sambu LM. Determinants of Preterm Birth at the Postnatal Ward of Kenyatta National Hospital, Nairobi, Kenya. Open J Obstet Gynecol. 2017;7(6):973–988. doi: 10.4236/ojog.2017.79099 [DOI] [Google Scholar]
- 17.Ministry-of-Health-[MOH]. Maternal and Child Health. Nairobi: Ministry of Health; 2015. [Google Scholar]
- 18.Yego F, Williams JS, Byles J, Nyongesa P, Aruasa W, Este CD. A retrospective analysis of maternal and neonatal mortality at a teaching and referral hospital in Kenya. Reprod Health. 2013;10(1):1. doi: 10.1186/1742-4755-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Velaphi SC, Westercamp M, Moleleki M, et al. Surveillance for incidence and etiology of early-onset neonatal sepsis in Soweto, South Africa. PLoS One. 2019;14(4):1–18. doi: 10.1371/journal.pone.0214077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhoda NR, Velaphi S, Gebhardt GS, Kauchali S, Barron P. Reducing neonatal deaths in South Africa: progress and challenges. S Afr Med J. 2018;3(1):9–16. doi: 10.7196/SAMJ.2017.v108i3b.12804 [DOI] [Google Scholar]
- 21.Brits H, Adriaanse M, Rall D, Van Biljon M, Van Der Walt A, Wasserman E. Causes of prematurity in the bloemfontein academic complex causes of prematurity in the bloemfontein academic complex. S Afr Fam Pract. 2015;57(3):223–226. doi: 10.1080/20786190.2014.976960 [DOI] [Google Scholar]
- 22.Rhoda NR, Velaphi S. Reducing neonatal deaths in South Africa – are we there yet, and what can be done. S Afr Med J. 2015;6(3):67–71. [Google Scholar]
- 23.Bruckmann EK, Velaphi S. Intrapartum asphyxia and hypoxic ischaemic encephalopathy in a public hospital: incidence and predictors of poor outcome. S Afr Med J. 2015;105(4):298–303. doi: 10.7196/SAMJ.9140 [DOI] [PubMed] [Google Scholar]
- 24.Bamford L. Maternal, Newborn and Child Health. Pretoria: University of Pretoria; 2015. [Google Scholar]
- 25.Mabaso MHL, Ndaba T, Mkhize-kwitshana ZL. Overview of maternal, neonatal and child deaths in South Africa: challenges, opportunities, progress and future prospects. Int J MCH AIDS. 2014;2(2):182–189. [PMC free article] [PubMed] [Google Scholar]
- 26.SavetheChildrenFund [SCF]. Time to Focus on 84 000 Preterm Births in South Africa. South Africa: Save the Childrens; 2013. [Google Scholar]
- 27.Chawanpaiboon S, Vogel JP, Moller A, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7:37–46. doi: 10.1016/S2214-109X(18)30451-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amare D, Mela M, Dessie G. Unfinished agenda of the neonates in developing countries: magnitude of neonatal sepsis: systematic review and meta-analysis. Heliyon. 2019;5:e02519. doi: 10.1016/j.heliyon.2019.e02519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Glob Health. 2018;3(e000347):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mongella GI, Songane F, Akande EO. Opportunities for Africa’ S Newborns. Pretoria: Save the Children; 2010. [Google Scholar]
- 31.UNICEF. Baby Boys at Higher Risk of Death and Disability Due to Preterm Birth. New York: UNICEF; 2013. [Google Scholar]
- 32.Gillam-Krakauer M, Gowen CW. Birth Asphyxia. London: StatPearls; 2018. [PubMed] [Google Scholar]
- 33.Lawn J, Mongi P, Cousens S. Africa ’ s newborns – counting them and making them count. Lancet. 2010;2(5):1–12. [Google Scholar]
- 34.Coetzee M, Mbowane NT, de Witt TW. Neonatal sepsis: highlighting the principles of diagnosis and management. S Afr J Child Health. 2017;11(2):0–4. [Google Scholar]