Abstract
Cardiovascular diseases (CVDs) are the leading cause of disease burden globally, disproportionately affecting low and middle-income countries. The continued scarcity of literature on CVDs burden in Nepal has thwarted efforts to develop population-specific prevention and management strategies. This article reports the burden of CVDs in Nepal including, prevalence, incidence, and disability basis as well as trends over the past two decades by age and gender. We used the Institute of Health Metrics and Evaluation’s Global Burden of Diseases database on cardiovascular disease from Nepal to describe the most recent data available (2017) and trends by age, gender and year from 1990 to 2017. Data are presented as percentages or as rates per 100,000 population. In 2017, CVDs contributed to 26·9% of total deaths and 12·8% of total DALYs in Nepal. Ischemic heart disease was the predominant CVDs, contributing 16·4% to total deaths and 7·5% to total DALYs. Cardiovascular disease incidence and mortality rates have increased from 1990 to 2017, with the burden greater among males and among older age groups. The leading risk factors for CVDs were determined to be high systolic blood pressure, high low density lipoprotein cholesterol, smoking, air pollution, a diet low in whole grains, and a diet low in fruit. CVDs are a major public health problem in Nepal contributing to the high DALYs with unacceptable numbers of premature deaths. There is an urgent need to address the increasing burden of CVDs and their associated risk factors, particularly high blood pressure, body mass index and unhealthy diet.
Keywords: Prevalence, Health system, Mortality, Cardiovascular disease, Incidence, Nepal
1. Background
Cardiovascular diseases (CVDs) are the leading cause of premature death and disease burden globally [1] disproportionately affecting low and middle-income countries (LMICs) [2]. Overall it accounted for 43% of deaths in low income countries (LIC) vs 41% in middle income countries (MIC) and 23% in high income countries (HIC) [3]. The CVD incidence in LIC (7.1 per 1000 person years), and MIC (6.8 per 1000 person years) is double compared to the incidence in high income countries (4.1per 1000 person years) [3], [4]. The South East Asia Region (SEAR) (including India, Pakistan, Bhutan, Bangladesh, Sri Lanka, and Nepal) is home to 20% of the world’s population and has one of the highest burdens of CVDs in the world [5]. Eliminating CVDs would produce gains in both quality and longevity of life [6], [7]. The estimated economic loss due to CVDs in LMICs was 3.7 trillion US dollars in 2010, approximately 2% of the Gross Domestic Product of all LMICs [8].
Non Communicable Diseases (NCD) burden is fueled by the interplay of demographic and lifestyle factors, urbanization [9], [10], [11] and economic stagnation [12] in LMICs, resulting in a higher demand for health services [13], [14], [15], [16]. However, despite higher CVD burden and subsequent demands, LICs have lower first hospitalization rates and CVD medication use reflecting poor access to health care [3], [4]. Lack of appropriately designed health financing arrangements hinder scaling up of the cost effective NCD interventions [17], [18]. The limited government health budgets and low coverage of health insurance to deal with increasing NCD burden has led to growing out of pocket health expenditure deepening the socioeconomic inequalities in LMICs [19], [20], [21].
Like many other LMICs, Nepal’s existing national health system is not well prepared to address the growing burden of CVD [22]. The rural health facilities in Nepal do not provide NCD related preventive and clinical services. These services are concentrated in cities, increasing disparities in access to health services [23]. In 2013, nearly 26% of the population had elevated blood pressure, 4% had elevated blood sugar, 21% were overweight or obese, and 23% had high cholesterol [24]. The prevalence of smoking was 19% [24], chewing tobacco was more common among the poor [25], and almost everyone (99%) consumed less than five servings of fruits and vegetables on an average day [24]. Further, Nepal lacks access to the technological advances in early detection and management of CVD that contributed to the reduction of mortality in high income countries (HICs) [26]. The continued poor access to CVD care and management services [9] and the high prevalence of CVD risk factors is expected to substantially increase the CVD burden in the coming years if appropriate action is not taken [24]. To address the increasing burden of NCDs, Nepal has endorsed a multisector action plan for prevention and control of NCDs [27], and also introduced a package to prevent and treat NCDs, but implementation of the plan has remained challenging and the health promotional activities have remained inadequate [28].
Few studies have assessed the CVD burden in Nepal. CVDs is the seventh most frequently occurring condition, accounting for forty percent of NCD cases admitted in non-specialty tertiary hospitals [29]. Hypertension (47%) and rheumatic heart disease (22%) were the most common CVDs in non-specialty and specialty hospitals [29]. The prevalence of coronary artery disease was reported to be 5% in a study conducted in six hospitals of Kathmandu in 2003 [30], and 5.7% in a population-based study in eastern Nepal in 2009 [31]. The prevalence of rheumatic heart disease was 0.9 per thousand among 5–15 years old children in Kathmandu in 2013 [32]. National level data on CVDs, including incidence of myocardial infarction and stroke, are not available. The continued dearth of literature on the burden of CVD in Nepal has thwarted efforts to develop population-specific prevention and management strategies. A comprehensive analysis of the types of CVDs most common in the population, their major risk factors, trends, age and gender distribution has been overdue. In this article, we report the burden of CVD in Nepal including prevalence, incidence, and several estimates of disability over time, by age and gender. The findings from this analysis of CVD mortality and morbidity data could provide a base for setting public health priorities and creating evidence-informed policies.
2. Methods
We used the Institute for Health Metrics and Evaluation (IHME)’s Global Burden of Diseases (GBD) database [33] to download cardiovascular disease mortality rates, prevalence, incidence, disability adjusted life years (DALYs), years of life lost (YLLs) and years lived with disability (YLDs) data from Nepal and other comparator countries including India, Bangladesh, Pakistan, Bhutan, Maldives, Sri Lanka and the USA by age, gender and year from 1990 to 2017. We downloaded the data in excel format and used descriptive statistics (rates and proportions) to compare patterns and trends in mortality, incidence and prevalence rates, DALYs, YLDs, and YLLs for CVDs in Nepal by age and gender using tables, graphs and histograms. The source data i.e. GBD study uses a standardized analytical approach for estimating incidence, prevalence, and YLDs by age, sex, cause, year, and location. The description of metrics, data collection procedures, and analytical approaches used for GBD 2017 are reported elsewhere [34]. The GBD 2017 used several input sources from surveillance and survey data, published, and unpublished papers, vital registration, hospital data to generate the data for 354 causes from 195 countries [34], including Nepal. We direct interested readers to the Data Input Sources Tool, which lists all the publications and papers used for Nepal GBD 2017 [35]. Here, we present the prevalence, and mortality rates, and DALYs due to CVD from 1990 to 2017. We also report the contribution of major risk factors to CVD DALYs in 2017.
3. Results
In 2017, CVDs contributed to 26·9% (UI 29·5–24·4) of total deaths and 12·8% (UI 14·6–11·0) of total DALYs in Nepal (Table 1). Ischemic heart disease and stroke were the predominant CVDs, contributing 16·4% (UI 18·2–14·6) and 7·5% (UI 8·6–6·7) to total deaths and 7·5% (UI 8·7–6·3) and 3·5% (UI 4·0–3·0) of total DALYs, respectively. The proportion of death and DALYs from Ischemic heart disease and stroke was higher in men than in women. Hypertensive heart disease and rheumatic heart disease each contributed to about 0.8% of total deaths.
Table 1.
Percentage of total deaths and DALYs due to CVDs by gender in Nepal (all ages, 2017).
|
Percentage of total deaths (95% UI) |
Percentage of total DALYs (95% UI) |
|||||
|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | |
| Ischemic heart disease | 16.4 (18.2–14.6) | 20.5 (22.7–18.03) | 11.1 (13.0–9.4) | 7.6 (8.7–6.2) | 10.3 (11.9–8.3) | 4.5 (5.5–3.7) |
| Stroke | 7.5 (8.6–6.7) | 8.6 (9.8–7.4) | 6.2 (7.7–4.9) | 3.5 (4.0–2.9) | 4.2 (5.0–3.5) | 2.6 (3.3–2.2) |
| Hypertensive heart disease | 0.8 (1.0–0.6) | 0.7 (0.9–0.5) | 0.9 (1.4–0.6) | 0.4 (0.4–0.3) | 0.3 (0.4–0.3) | 0.3 (0.5–0.2) |
| Rheumatic heart disease | 0.8 (1.0–0.5) | 0.6 (1.0–0.5) | 0.9 (1.2–0.6) | 0.6 (0.7–0.4) | 0.5 (0.7–0.4) | 0.6 (0.8–0.4) |
| Non-rheumatic valvular heart disease | 0.1 (0.1–0.1) | 0.1 (0.2–0.1) | 0.1 (0.1–0.1) | 0.1 (0.1–0.0) | 0.1 (0.1–0.0) | 0.0 (0.1–0.0) |
| Atrial Fibrillation and flutter | 0.2 (0.2–0.1) | 0.2 (0.3–0.1) | 0.2 (0.3–0.2) | 0.1 (0.2–0.1) | 0.1 (0.2–0.1) | 0.1 (0.1–0.1) |
| Aortic aneurysm | 0.2 (0.2–0.1) | 0.2 (0.3–0.2) | 0.1 (0.1–0.1) | 0.1 (0.1–0.1) | 0.1 (0.1–0.1) | 0.0 (0.0–0.0) |
| Peripheral artery disease | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0(0.0–0.1) | 0.0 (0.0–0.0) |
| Endocarditis | 0.0 (0.1–0.0) | 0.0 (0.1–0.0) | 0.0 (0.01–0.0) | 0.0 (0.0–0.0) | 0.0 (0.1–0.0) | 0.0 (0.0–0.0) |
| Cardiomyopathy and myocarditis | 0.2 (0.4–0.2) | 0.4 (0.5–0.2) | 0.2 (0.2–0.1) | 0.2 (0.2–0.1) | 0.2 (0.3–0.1) | 0.1 (0.1–0.1) |
| Other cardiovascular and circulatory diseases | 0.5 (0.8–0.4) | 0.6 (1.1–0.4) | 0.5 (0.7–0.3) | 0.4 (0.5–0.3) | 0.5 (0.7–0.4) | 0.3 (0.4–0.2) |
| Total Cardiovascular diseases | 26.9 (29.5–24.4) | 32.1 (34.8–29.2) | 20.3 (24.8–16.2) | 12.8 (14.5–10.9) | 16.4 (18.7–13.8) | 8.9 (10.5–7.3) |
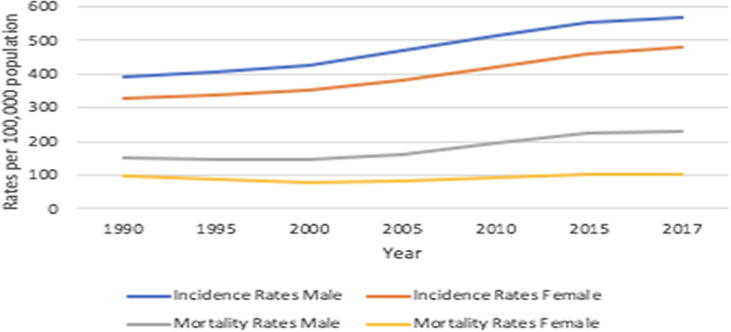
The trends in CVD mortality and incidence by gender from 1990 to 2017 in Nepal is shown in Fig. 1. The incidence rates have increased between 1990 and 2017. In 2017, the CVD incidence among males was 569.5 per 100,000 population (UI 594.0–546.5) and females was 479.1 per 100,000 population (UI 501.1–459.1). The CVD mortality rate in Nepal increased from 124.1 per 100,000 population (UI 142.8–108.1) in 1990 to 164.7 per 100,000 population (UI 185.5–142.7) in 2017. In 2017, the CVD mortality rates among males was estimated to be 230.7 (UI 260.1–188.7) and among females it was 104.3 (UI 127.0–84.7).
Fig. 1.
Trend in CVD Mortality and Incidence Rates by Gender (all ages, 1990–2017).
Table 2 shows CVD mortality rates in Nepal by age group and gender in 2017. In 2017, the overall CVD mortality rate was 260.8 per 100,000 population with the rates being higher among older age groups. In all age groups, the CVD mortality rate was higher among males compared to females, with the greatest difference in the 60–64 years age group (953.1 per 100,000 for male vs 374.0 per 100,000 for female). Compared to other age groups the death rate from CVD was highest among 80 years and above (4274.7 UI 4807.6–3777.9); however, the proportion of total deaths from CVD was highest among those in age groups 65–69 years (36.2 UI 40.2–32.5).
Table 2.
Deaths from CVDs in Nepal by age groups and gender in 2017.
| Age groups (yrs) | Death per 100,000 (95% UI) |
Percentage of total deaths (95% UI) |
||||
|---|---|---|---|---|---|---|
| Both | Male | Female | Both | Male | Female | |
| 1–4 | 0.4 (0.7–0.2) | 0.6 (1.0–0.3) | 0.3 (0.5–0.1) | 0.4 (0.7–0.2) | 0.6 (0.9–0.3) | 0.3 (0.5–0.1) |
| 5–9 | 0.3 (0.5–0.2) | 0.4 (0.6–0.2) | 0.3 (0.5–0.2) | 0.7 (1.0–0.4) | 0.7 (1.0–0.4) | 0.7 (1.0–0.4) |
| 10–14 | 0.7 (0.9–0.4) | 0.8 (1.2–0.5) | 0.5 (0.8–0.3) | 1.6 (2.2–1.1) | 1.7 (2.5–1.1) | 1.4 (2.1–0.8) |
| 15–19 | 3.9 (5.1–2.7) | 5.8 (8.2–3.9) | 2.0 (2.8–1.3) | 4.8 (6.2–3.4) | 5.7 (7.9–3.9) | 3.2 (4.5–2.2) |
| 20–24 | 7.2 (9.8–4.9) | 11.7 (17.2–7.4) | 3.2 (4.6–2.2) | 6.6 (8.8–4.6) | 8.2 (11.3–5.3) | 4.1 (5.7–2.9) |
| 25–29 | 9.6 (13.5–5.1) | 15.4 (23.4–7.0) | 5.1 (7.2–2.8) | 8.4 (11.2–4.4) | 10.9 (7.5–3.0) | 5.4 (7.5–3.0) |
| 30–34 | 15.8 (22.9–4.7) | 23.0 (37.2–3.0) | 10.3 (14.7–4.8) | 10.8 (14.8–3.3) | 13.8 (20.9–1.9) | 7.9 (10.9–3.7) |
| 35–39 | 28.3 (39.6–10.3) | 38.4 (59.7–5.0) | 20.4 (29.0–12.3) | 13.7 (18.5–5.0) | 16.9 (25.1–2.1) | 10.8 (14.3–7) |
| 40–44 | 63.0 (82.6–34.4) | 83.6 (121.4–26.9) | 46.1 (63.1–34.4) | 20.4 (25.2–11.3) | 24.2 (31.9–8.7) | 16.4 (20.5–12.3) |
| 45–49 | 124.1 (156.8–86.1) | 168.9 (234.5–102.2) | 84.2 (110.8–60.5) | 25.9 (30.6–19.4) | 30.7 (37.6–20.3) | 20.3 (24.7–16.2) |
| 50–54 | 237.0 (287.3–187.9) | 338.2 (432.2–244.1) | 140.7 (186.1–104.4) | 31.0 (35.1–26.1) | 37.3 (42.9–30.0) | 22.3 (27.1–18.0) |
| 55–59 | 405.1 (475.8–328.6) | 578.4 (703.4–440.2) | 238.7 (312.6–178.0) | 34.1 (37.8–30.2) | 39.3 (44.0–34.1) | 26.1 (30.8–20.9) |
| 60–64 | 653.7 (756.1–539.5) | 953.1 (1131.4–738.4) | 374.0 (476.8–284.5) | 34.9 (38.7–30.9) | 40.4 (45.1–35.5) | 26.5 (31.5–21.3) |
| 65–69 | 1038.6 (1190.2–878.5) | 1503.6 (1742.5–1199.7) | 617.0 (797.6–474.5) | 36.2 (40.3–32.5) | 41.6 (46.2–37.0) | 28.2 (33.8–22.8) |
| 70–74 | 1557.5 (1782.2–1323.2) | 2254.4 (2570.3–1822.2) | 892.7 (1148.4–661.9) | 34.6 (38.3–30.7) | 40.7 (45.1–36.0) | 25.4 (31.5–19.4) |
| 75–79 | 2442.9 (2771.2–2118.6) | 3407.0 (3854.0–2807.5) | 1537.0 (1964.4–1135.3) | 35.0 (38.8–31.4) | 40.5 (45.0–36.0) | 27.2 (33.5–20.8) |
| 80 above | 4274.7 (4807.6–3777.9) | 5938.5 (6636.2–5075.9) | 2994.7 (3760.7–2345.3) | 30.6 (34.2–27.7) | 37.3 (41.0–33.4) | 24.0 (29.4–19.6) |
| Total | 260.8 (292.3–227.6) | 372.0 (414.6–309.7) | 165.4 (200.8–134.6) | 27.0 (29.5–24.4) | 32.1 (34.8–29.2) | 20.3 (23.4–17.4) |
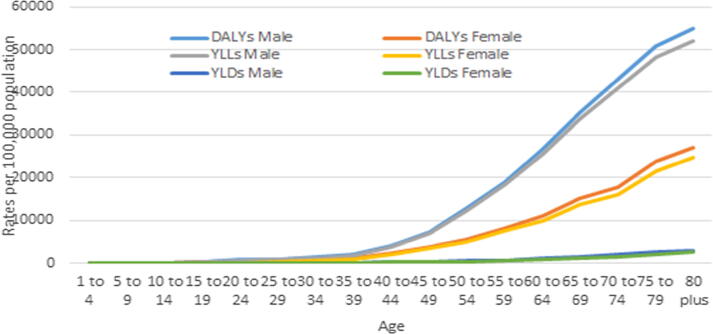
The burden of CVD in terms of DALYs, YLDs and YLLs in 2017 was higher among older age groups and higher in males compared to females (Fig. 2).
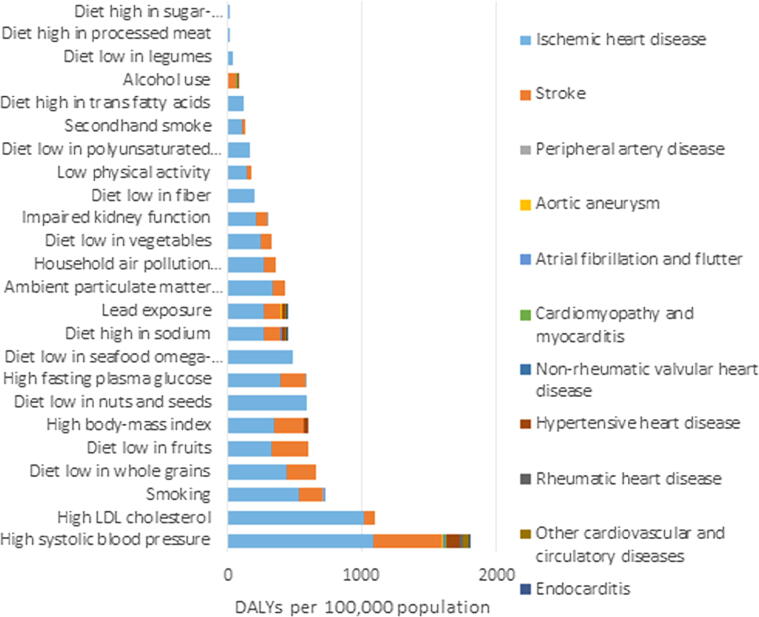
Fig. 3.
Shows the risk Fig. 3: CVD risk factors contributing to DALYs for specific CVD diseases (all ages, 2017).
Fig. 2.
CVD related DALYs, YLLs and YLDs by age and gender in 2017.
Factors that contributed to DALYs due to CVDs in Nepal in 2017. The leading risk factors associated with the highest DALYs were high systolic blood pressure 2624.0 (UI 2867.7–2373.1), high low density lipoprotein (LDL) cholesterol 1242.4 (UI 1472.0–1031.5), high body mass index 1058.2 (UI 1452.1–694.1), a diet low in whole grains 920.2 (UI 1217.6–641.7), high fasting plasma glucose 877.3 (UI 1196.6–663.4), smoking 872.9 (UI 915.9–835.9), a diet low in fruits 682.4 (UI 995.0–408.7), and a diet low in nuts and seeds 557.8 (UI 767.9–357.3). High systolic blood pressure, lead exposure, and a diet high in sodium were common risk factors across all the CVDs.
Table 3 compares incidence, prevalence, death rates and DALYs in Nepal to global, regional, and country-specific rates in South Asia. Although Nepal’s prevalence of CVD was lower than global estimates, the burden of CVDs measured by DALYs was higher than the global rates while slightly lower than South Asia. The incidence of CVD for Nepal was lower than the global rate but higher than rates in South Asia, while the death rate was higher than the global rate, yet lower than South Asia. In comparison to other countries in the region, Nepal burden of CVD was lower than Bangladesh, Pakistan and India and higher than Bhutan, Sri Lanka and Maldives. The prevalence and incidence rates of the United States were higher than of Nepal, global, South Asia and other countries in the region but the death rates and DALYs were lower.
Table 3.
Comparing CVD-related incidence, prevalence, death and DALYs between countries and region.
|
Age standardized Rates per 100,000 populations |
||||
|---|---|---|---|---|
| Incidence | Deaths | Prevalence | DALYs | |
| Nepal | 717.8 (748.6–689.7) | 260.8 (292.3–227.6) | 5679.8 (5954.0–5437.6) | 5242.2 (5901.8–4512.9) |
| Global | 922.3 (954.3–893.1) | 233.1 (236.4–229.7) | 6081.6 (6320.8–5860.8) | 4597.9 (4734.2–4463.7) |
| South Asia | 698.7 (724.8–674.4) | 294.6 (305.4–279.1) | 5432.7 (5674.0–5213.3) | 6006.7 (6222.4–5746.4) |
| Bangladesh | 729.1 (757.1–703.8) | 298.0 (326.2–269.6) | 6296.3 (6576.5–6037.1) | 5975.2 (6534.7–5415.7) |
| India | 679.2 (705.5–655.3) | 282.3 (293.3–265.0) | 5214.2 (5447.6–5000.4) | 5804.3 (6015.2–5532.3) |
| Pakistan | 858.4 (888.4–829.7) | 423.0 (483.8–364.8) | 6566.2 (6877.5–6285.0) | 8222.9 (9506.4–7003.7) |
| Bhutan | 644.6 (670.4–621.3) | 217.1 (255.0–182.5) | 5506.8 (5760.8–5261.6) | 4285.0 (5000.9–3544.3) |
| Sri Lanka | 720.2 (750–690.9) | 197.1 (220.2–171.6) | 5600.3 (5904.0–5326.7) | 3717.4 (4204.1–3246.3) |
| Maldives | 689.4 (719.7–662.8) | 164.9 (175.6–154.3) | 5615.6 (5873.0–5366.5) | 3162.2 (3371.4–2924.0) |
| USA | 1588.2 (1637.0–1537.7) | 151.1 (153.9–148.1) | 7275.8 (7565.4–7012.2) | 3029.7 (3168.0–2900.9) |
4. Discussion
The GBD data we extracted and described here show that the total deaths from CVDs has almost doubled from 1990 to 2017, making CVDs the most significant cause of death and DALYs lost in Nepal. Cardiovascular diseases contributed to 27% of total deaths and 13% of total DALYs in 2017. Ischemic heart disease and stroke were the predominant CVDs followed by hypertensive heart disease and rheumatic heart disease. The CVD incidence, prevalence and mortality rates and DALYs increased in Nepal from 1990 to 2017. Males and older age groups were more affected compared with female and younger age groups. In South Asia, Nepal ranked third in prevalence, and the CVD related DALY rates were higher in Nepal than the global average.
Nearly half of all CVD deaths in Nepal in 2017 occurred among those 70 years and younger. Similarly, high numbers of deaths from CVDs were observed in those under 70 years in SEAR (25% of total deaths) [36]. Fifty two percent of CVD deaths in LMICs occur below the age of 70 years compared to only 23% in high income countries [37]. The high incidence and declining mortality rates due to CVD in the U.S. and other industrialized countries are a result of rapid progress in prevention and treatment of CVDs and better management of risk factors such as hypertension and cholesterol [38], [39], [40].
In the past two decades, Nepal’s health system has been focused primarily on combating communicable diseases, maternal child health and nutritional deficiencies [22]. Non communicable diseases were overshadowed by millennium development goals (MDGs) as in most LMICs and further dampened by inadequate trained health workers and non-existent public private partnership [22]. Therefore, there is inadequate attention to quality care, screening, and diagnostics to prevent and manage CVDs. The CVD management in Nepal has focused on treatment, concentrated in the cities out of reach of the majority of the rural population, and lacked preventive health care and education [22]. The high rates of premature death from CVDs can also be attributed to the health system’s inability to provide effective interventions [20] that include longitudinal and continuous systems of care for CVDs at the community level [10].
The incidence, prevalence and DALYs due to CVD have substantially increased in Nepal since 1990. The percent of total DALYs contributed by CVDs was higher among men than in women, a trend similarly observed in India, with higher rates of DALYs among males (15.8% vs 12.2%) [41]. After the age of 35 years, the gap between men and women in DALYs increased significantly. This rising CVD burden can be attributed to the country’s epidemiological and demographic transitions [42]. The life expectancy in Nepal has increased from 54 years in 1990 to 70 years in 2015 [26], [27], thus leading to an increase in the proportion of the aging population that corresponds to increases in incidence, prevalence and mortality associated with CVD since 1990 in Nepal. However, even with increasing elderly population HICs reduced risk factors through universal health coverage and effective health policies [43], [44], [45], [46]. When comparing life expectancy from 1970 to 2012, [47] on average there was a 20 years and 34 years gap in life expectancy for countries that achieved and those yet to achieve universal health coverage, respectively [48]. Urbanization and lifestyle changes also have given rise to metabolic (high blood pressure, blood sugar and cholesterol), behavioral (tobacco, physical inactivity and unhealthy diet) and psychosocial (anxiety, depression and lack of social support) risk factors for CVDs [28], [29].
Dietary risks, including diets low in whole grains, fruits, nuts, seeds, and seafoods containing omega-3 fatty acid, high systolic blood pressure and high LDL cholesterol were the leading risk factors contributing to DALYs from CVDs in Nepal. Dietary habits influence a wide range of cardiometabolic risk factors through multiple pathways, including energy intake and expenditure, body fat composition, blood pressure, lipoprotein concentration and cardiac function [49]. The traditional Nepali diet remains high in refined grains and low in fruits, vegetables, nuts, and seeds [50]. High systolic blood pressure, and high total cholesterol often remain underdiagnosed and access to medication for these conditions is limited in Nepal [33], [51], [52]. General population have inadequate knowledge on causes of CVD in Nepal, and people do not consider themselves at risk for CVD posing a barrier for behavior change [53]. There is ethnic, rural urban [22] and educational [53] differences in prevalence of risk factors and behavioral change [22]. Educated people were more likely to be physically inactive, hypertensive, and consume more fruits and less likely to use tobacco and alcohol [53]. Similarly, physical inactivity is more of an urban problem and tobacco and alcohol consumption are prevalent in both urban and rural setting - this demand diverse and contextual control measures [22].
The tide of NCDs will increase demand for medical imaging, laboratory, outpatients and rehabilitation services [13], [14], [15], [16]. Therefore, health promotional activities to promote active lifestyle and healthy diet, improving access to preventive services, [54] and enacting and monitoring policies (tobacco control) [55] must go hand in hand with increased investment in modern medical technologies and education and training of health workers [56]. The LMICs share of the total health expenditure (THE) increased from 10.7% in 1995 to 14.6% in 2013, during the same period, the medical spending out of total THE increased from 26.1% to 39.7%, indicating health systems in LMICs to experience fiscal challenges to meet the demand for medical services [57].
In LMICs, both the direct cost of annual care and the cost for seeking care for an acute episode of CVD exceeded the per capita health expenditure [58]. The costs per episode for CVDs were estimated as between $500 and $1500; and about $5000 for a stroke episode [58]. The monthly cost for hypertension treatment are estimated to be around $22 [58]. The majority of the Nepali population cannot afford the exorbitant cost of managing CVDs when 52% of total health care expenditure is out-of-pocket [59]. Only 8.9% of the total health care expenditures, both government and private is spent on CVDs management [59].
Socioeconomic vulnerabilities seriously affect the poor members of the community [60]. The rural poor are further marginalized when diagnostic, treatment, and rehabilitative services and health professionals are concentrated in large urban hospitals [56]. Households in Nepal incur catastrophic expenditures on health. For 2% of households, 25% of their total household expenditures were on health, and for the next 11% of households, 10% of their total household expenditure were on health, pushing an additional 2% of people below the poverty line of $1.9 per day in 2015/16 [59]. Thus families face a huge financial barrier to the prevention and management of CVDs in Nepal. In India, 10% of families who have a member with CVD are driven into poverty and the total income loss due to CVDs was about two billion dollars per year [61]. Other major barriers to CVD management in Nepal are unequal distribution of health workers, untrained health care workers and lack of essential drugs at the primary care level for providing CVD services [61]. Upgrading and decentralizing laboratories, training and equitable distribution of health workers, monitoring and evaluation of clinical protocol implementation and a working referral system from community to tertiary level facilities are important to halt CVD in Nepal [22].
Several comprehensive programs focused on CVD management in both high, low- and middle-income countries have demonstrated success, including those aimed at modes of community empowerment, creating enabling environments through policy change and health promotion efforts [38], [62], [63]. Effective strategies help to minimize the development of increased risk [54], [64] as well as to detect and prevent progression of CVD throughout the life course [65], [66]. Such efforts should include population-wide approaches implemented throughout all tiers of the health system, including community settings to address tobacco use and hypertension, promoting physical activity and advocacy for healthy diets (e.g., adequate whole grains, fruits and vegetables and less salt and unhealthy fat). Health systems working in synergy with individual approaches have the potential to detect early and effectively control the risk among high risk groups and those already diagnosed with CVDs [29], [39].
This is the first study to report on trends and distribution of the CVD burden at a national level in Nepal. We extracted data from the GBD database, which uses standardized methods to estimate metrics creating comparable data within South Asian countries and globally. The main limitation of these data is the lack of primary data sources from Nepal. Nepal does not have a cause of death surveillance system or other national, validated forms of verbal or social autopsy to document CVD. Thus, data were imputed using statistical models. However, in a resource-constrained setting such as Nepal, where reliable health statistics on CVDs are limited, findings from the GBD data provide a basis for setting public health priorities and creating evidence-informed policies. Other limitations of CVD estimates of GBD 2017 include misclassification and bias due to miscoding of death certificates [67], [68], [69].
5. Conclusion
Cardiovascular diseases is the topmost cause of disability adjusted life years in Nepal. It contributes to about a third of total deaths; with half of the CVD deaths occurring among 70 years or younger in Nepal. Ischemic heart disease and stroke were the most predominant CVDs. The cardiovascular disease burden in Nepal is particularly attributable to high blood pressure and unhealthy diet.
Funding
Research reported in this publication was supported in part by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number U24HL136789.
The views expressed in this paper are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the U.S. Department of Health and Human Services.
Contributor Information
David Citrin, Email: david@possiblehealth.org.
Helen Cox, Email: helen.cox@nih.gov.
Annette Fitzpatrick, Email: fitzpal@uw.edu.
Biraj Man Karmacharya, Email: birajmk@kusms.edu.np.
Rashmi Maharjan, Email: rashmimaharjan@kusms.edu.np.
Donna Spiegelman, Email: donna.spiegelman@yale.edu.
Archana Shrestha, Email: archana@kusms.edu.np.
References
- 1.GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016, Lancet 390 (2017) 1151–1210. [DOI] [PMC free article] [PubMed]
- 2.World Health Organization. Cardiovascular Disease Programme, World Health Organization & World Health Organization. Noncommunicable Disease and Mental Health Cluster, Integrated Management of Cardiovascular Risk. (World Health Organization, 2002).
- 3.Dagenais G.R. Variations in common diseases, hospital admissions, and deaths in middle-aged adults in 21 countries from five continents (PURE): a prospective cohort study. The Lancet. 2020;395:785–794. doi: 10.1016/S0140-6736(19)32007-0. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. The Lancet. 2020;395:795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roth G.A. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu X. Potential gains in health-adjusted life expectancy from reducing four main non-communicable diseases among Chinese elderly. BMC Geriatr. 2019;19:16. doi: 10.1186/s12877-019-1032-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klenk J., Rapp K., Buchele G., Keil U., Weiland S.K. Increasing life expectancy in Germany: quantitative contributions from changes in age- and disease-specific mortality. Eur. J. Public Health. 2007;17:587–592. doi: 10.1093/eurpub/ckm024. [DOI] [PubMed] [Google Scholar]
- 8.D.E. Bloom, et al., From burden to ‘best buys’: reducing the economic impact of non-communicable diseases (2011).
- 9.Popkin B.M., Adair L.S., Ng S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.N. Sudharsanan, D.E. Bloom, N. Sudharsanan, et al., The demography of aging in low-and middle-income countries: chronological versus functional perspectives, in: Future directions for the demography of aging: Proceedings of a workshop, National Academies Press, 2018, pp. 309–338.
- 11.R.A. Riana, Middle-class composition and growth in middle-income countries, https://www.econstor.eu/handle/10419/179209, 2017.
- 12.Aizenman J., Eichengreen B., Park D. Overcoming the middle-income challenge. Emerg. Markets Finance Trade. 2018;54:1205–1207. [Google Scholar]
- 13.Ranković A. Impact of imaging diagnostics on the budget–are we spending too much? Vojnosanit. Pregl. 2013;70:709–711. [PubMed] [Google Scholar]
- 14.Jakovljevic M. Cold war legacy in public and private health spending in Europe. Front Public Health. 2018;6:215. doi: 10.3389/fpubh.2018.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jakovljevic M.B. Oncology monoclonal antibodies expenditure trends and reimbursement projections in the emerging Balkan market. Farmeconomia. Health Econ. Therap. Pathways. 2014;15:27–32. [Google Scholar]
- 16.Jakovljevic M., Zugic A., Rankovic A., Dagovic A. Radiation therapy remains the key cost driver of oncology inpatient treatment. J. Med. Econ. 2015;18:29–36. doi: 10.3111/13696998.2014.971162. [DOI] [PubMed] [Google Scholar]
- 17.A. Preker, et al., Health care financing for rural and low-income populations: the role of communities in resource mobilization and risk sharing, SSRN Electronic J. doi:10.2139/ssrn.1017214.
- 18.Jakovljevic M. Comparative financing analysis and political economy of noncommunicable diseases. J. Med. Econ. 2019;22:722–727. doi: 10.1080/13696998.2019.1600523. [DOI] [PubMed] [Google Scholar]
- 19.Ranabhat C.L., Jakovljevic M., Dhimal M., Kim C.-B. Structural factors responsible for universal health coverage in low- and middle-income countries: results from 118 countries. Front Public Health. 2019;7:414. doi: 10.3389/fpubh.2019.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McIntyre D., Thiede M., Dahlgren G., Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc. Sci. Med. 2006;62:858–865. doi: 10.1016/j.socscimed.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 21.Jakovljevic M. Commentary: Patient Cost Sharing and Medical Expenditures for the Elderly. Front. Pharmacol. 2016;7:73. doi: 10.3389/fphar.2016.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vaidya A. Tackling cardiovascular health and disease in Nepal: epidemiology, strategies and implementation. Heart Asia. 2011;3:87–91. doi: 10.1136/heartasia-2011-010000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mishra S.R., Neupane D., Bhandari P.M., Khanal V., Kallestrup P. Burgeoning burden of non-communicable diseases in Nepal: a scoping review. Global. Health. 2015;11:32. doi: 10.1186/s12992-015-0119-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aryal K.K. The Burden and determinants of non communicable diseases risk factors in Nepal: findings from a nationwide STEPS Survey. PLoS One. 2015;10 doi: 10.1371/journal.pone.0134834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sinha D.N. Smokeless tobacco use in Nepal. Indian J. Cancer. 2012;49:352. doi: 10.4103/0019-509X.107728. [DOI] [PubMed] [Google Scholar]
- 26.Beaglehole R. Cardiovascular disease in developing countries. BMJ. 1992;305:1170–1171. doi: 10.1136/bmj.305.6863.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Multisectoral Action Plan for the Prevention and Control of Non Communicable Diseases 2014–2020, http://www.searo.who.int/nepal/mediacentre/ncd_multisectoral_action_plan.pdf (accessed Oct 11, 2018).
- 28.Nepal- WHO Country Coordination Strategy 2018–2022. http://www.searo.who.int/nepal/documents (accessed Oct 12, 2018).
- 29.Bhandari G.P., Angdembe M.R., Dhimal M., Neupane S., Bhusal C. State of non-communicable diseases in Nepal. BMC Public Health. 2014;14:23. doi: 10.1186/1471-2458-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maskey A., Sayami A., Pandey M.R. Coronary artery disease: an emerging epidemic in Nepal. JNMA J. Nepal Med. Assoc. 2003;42:122–124. [Google Scholar]
- 31.Vaidya A. Prevalence of coronary heart disease in the urban adult males of eastern Nepal: a population-based analytical cross-sectional study. Indian Heart J. 2009;61:341–347. [PubMed] [Google Scholar]
- 32.Prajapati D. Epidemiological survey of Rheumatic fever. Rheumatic Heart Dis. Congenital Heart Disease among School Children in Kathmandu Valley Nepal. 2013;1(10):1–5. [Google Scholar]
- 33.GBD Results Tool | GHDx, http://ghdx.healthdata.org/gbd-results-tool (accessed Oct 11, 2019).
- 34.James S.L. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Global Burden of Disease Study 2017 (GBD 2017) Data Input Sources Tool | GHDx, http://ghdx.healthdata.org/gbd-2017/data-input-sources?locations=164&components=-1 (accessed Jan 30, 2019).
- 36.Salvage J. Global Institutions – The World Health Organization (WHO) Global Institutions – The World Health Organization (WHO) Nursing Standard. 2011;25:30. [Google Scholar]
- 37.Lim S.S. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. 2007;370:2054–2062. doi: 10.1016/S0140-6736(07)61699-7. [DOI] [PubMed] [Google Scholar]
- 38.Gouda H.N., Critchley J., Powles J., Capewell S. Why choice of metric matters in public health analyses: a case study of the attribution of credit for the decline in coronary heart disease mortality in the US and other populations. BMC Public Health. 2012;12:88. doi: 10.1186/1471-2458-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mensah G.A. Decline in cardiovascular mortality: possible causes and implications. Circ. Res. 2017;120:366–380. doi: 10.1161/CIRCRESAHA.116.309115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ford E.S. Explaining the decrease in US deaths from coronary disease, 1980–2000. N. Engl. J. Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 41.India State-Level Disease Burden Initiative CVD Collaborators, The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016, Lancet Glob Health 6 (2018) e1339–e1351. [DOI] [PMC free article] [PubMed]
- 42.C.J.L. Murray, A.D. Lopez, W.H. Organization, et al., The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: summary (1996).
- 43.Nolte E., McKee M. Does health care save lives? Avoidable mortality revisited. The Nuffield Trust. 2004 [Google Scholar]
- 44.Ogura S., Jakovljevic M. Health financing constrained by population aging-an opportunity to learn from Japanese experience/Finansiranje Zdravstvene Zaštite U Uslovima Starenja Popualcije-Prilika Da Učimo Na Japanskom Iskustvu. Serbian J. Exp. Clin. Res. 2014;15:175–181. [Google Scholar]
- 45.Di Cesare M. The contributions of risk factor trends to cardiometabolic mortality decline in 26 industrialized countries. Int. J. Epidemiol. 2013;42:838–848. doi: 10.1093/ije/dyt063. [DOI] [PubMed] [Google Scholar]
- 46.Mathers C.D., Stevens G.A., Boerma T., White R.A., Tobias M.I. Causes of international increases in older age life expectancy. The Lancet. 2015;385:540–548. doi: 10.1016/S0140-6736(14)60569-9. [DOI] [PubMed] [Google Scholar]
- 47.Ranabhat C.L., Kim C.-B., Park M.-B., Acharaya S. Multiple disparities in adult mortality in relation to social and health care perspective: results from different data sources. Global. Health. 2017;13:57. doi: 10.1186/s12992-017-0283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ranabhat C.L., Atkinson J., Park M.-B., Kim C.-B., Jakovljevic M. The influence of universal health coverage on life expectancy at birth (LEAB) and healthy life expectancy (HALE): a multi-country cross-sectional study. Front. Pharmacol. 2018;9:960. doi: 10.3389/fphar.2018.00960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133:187–225. doi: 10.1161/CIRCULATIONAHA.115.018585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shrestha A. Food patterns measured by principal component analysis and obesity in the Nepalese adult. Heart Asia. 2016;8:46–53. doi: 10.1136/heartasia-2015-010666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Forouzanfar M.H. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA. 2017;317:165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 52.Roth G.A. High total serum cholesterol, medication coverage and therapeutic control: an analysis of national health examination survey data from eight countries. Bull. World Health Organ. 2011;89:92–101. doi: 10.2471/BLT.10.079947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vaidya A., Aryal U.R., Krettek A. Cardiovascular health knowledge, attitude and practice/behaviour in an urbanising community of Nepal: a population-based cross-sectional study from Jhaukhel-Duwakot Health Demographic Surveillance Site. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-002976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Revill P., Sculpher M. Cost effectiveness of interventions to tackle non-communicable diseases. BMJ. 2012;344 doi: 10.1136/bmj.d7883. [DOI] [PubMed] [Google Scholar]
- 55.Ranabhat C.L., Kim C.-B., Park M.B., Jakovljevic M.M. Situation, impacts, and future challenges of tobacco control policies for youth: an explorative systematic policy review. Front. Pharmacol. 2019;10:981. doi: 10.3389/fphar.2019.00981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jakovljevic M. The impact of health expenditures on public health in BRICS nations. J. Sport Health Sci. 2019;8:516–519. doi: 10.1016/j.jshs.2019.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jakovljevic M., Getzen T.E. Growth of global health spending share in low and middle income countries. Front. Pharmacol. 2016;7:21. doi: 10.3389/fphar.2016.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gheorghe A. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. 2018;18:975. doi: 10.1186/s12889-018-5806-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nepal National Health Accounts 2012/13 to 2015/16, http://www.searo.who.int/nepal/documents/nepal_nha_2012_13_2015_16_mohp_june_2018.pdf (accessed June 3, 2019).
- 60.Jakovljevic M.B., Milovanovic O. Growing burden of non-communicable diseases in the emerging health markets: the case of BRICS. Front Public Health. 2015;3:65. doi: 10.3389/fpubh.2015.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.W.H. Organization, et al., Noncommunicable diseases in the South-East Asia Region, 2011: situation and response (2012).
- 62.P. Puska, J. Tuomilehto, A. Nissinen, E. Vartiainen, The North Karelia Project: 20 year results and experiences (1995).
- 63.Dowse G.K. Changes in population cholesterol concentrations and other cardiovascular risk factor levels after five years of the non-communicable disease intervention programme in Mauritius. BMJ. 1995;311:1255–1259. doi: 10.1136/bmj.311.7015.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.UnitedHealth, National Heart, Lung, and Blood Institute Centers of Excellence et al., Global response to non-communicable disease. BMJ 342 (2011) d3823.
- 65.Reddy K.S. Cardiovascular diseases in the developing countries: dimensions, determinants, dynamics and directions for public health action. Public Health Nutr. 2002;5:231–237. doi: 10.1079/phn2001298. [DOI] [PubMed] [Google Scholar]
- 66.Institute of Medicine (US) Committee on Preventing the Global Epidemic of Cardiovascular Disease: Meeting the Challenges in Developing Countries, Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health, National Academies Press (US), 2010. [PubMed]
- 67.Khosravi A. Impact of misclassification on measures of cardiovascular disease mortality in the Islamic Republic of Iran: a cross-sectional study. Bull. World Health Organ. 2008;86:688–696. doi: 10.2471/BLT.07.046532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pattaraarchachai J. Cause-specific mortality patterns among hospital deaths in Thailand: validating routine death certification. Population Health Metrics. 2010;8 doi: 10.1186/1478-7954-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mboera L.E.G. Cause-specific mortality patterns among hospital deaths in Tanzania, 2006–2015. PLOS ONE. 2018;13 doi: 10.1371/journal.pone.0205833. [DOI] [PMC free article] [PubMed] [Google Scholar]