This cross-sectional study of pediatric emergency department visits evaluates changes over time and hospital variation in advanced imaging use.
Key Points
Question
How has the use of advanced imaging changed during the past 10 years across pediatric emergency departments in the US?
Findings
This cross-sectional study of 26 million pediatric emergency department visits revealed that, overall, the rate of advanced imaging increased from 6.4% of encounters in 2009 to 8.7% in 2018; specifically, the rate of computed tomography decreased from 3.9% to 2.9%, the rate of ultrasonography increased from 2.5% to 5.8%, and the rate of magnetic resonance imaging increased from 0.3% to 0.6%.
Meaning
Overall use of advanced imaging has increased during the past decade, driven by the use of nonradiating modalities replacing the use of computed tomography.
Abstract
Importance
There is increased awareness of radiation risks from computed tomography (CT) in pediatric patients. In emergency departments (EDs), evidence-based guidelines, improvements in imaging technology, and availability of nonradiating modalities have potentially reduced CT use.
Objective
To evaluate changes over time and hospital variation in advanced imaging use.
Design, Setting, and Participants
This cross-sectional study assessed 26 082 062 ED visits by children younger than 18 years from the Pediatric Health Information System administrative database from January 1, 2009, through December 31, 2018.
Exposures
Imaging.
Main Outcomes and Measures
The primary outcome was the change in CT, ultrasonography, and magnetic resonance imaging (MRI) rates from January 1, 2009, to December 31, 2018. Imaging for specific diagnoses was examined using all patient-refined diagnosis related groups. Secondary outcomes were hospital admission and 3-day ED revisit rates and ED length of stay.
Results
There were a total of 26 082 062 visits by 9 868 406 children (mean [SD] age, 5.59 [5.15] years; 13 842 567 [53.1%] male; 9 273 181 [35.6%] non-Hispanic white) to 32 US pediatric EDs during the 10-year study period, with 1 or more advanced imaging studies used in 1 919 283 encounters (7.4%). The proportion of ED encounters with any advanced imaging increased from 6.4% (95% CI, 6.2%-6.2%) in 2009 to 8.7% (95% CI, 8.7%-8.8%) in 2018. The proportion of ED encounters with CT decreased from 3.9% (95% CI, 3.9%-3.9%) to 2.9% (95% CI, 2.9%-3.0%) (P < .001 for trend), with ultrasonography increased from 2.5% (95% CI, 2.5%-2.6%) to 5.8% (95% CI, 5.8%-5.9%) (P < .001 for trend), and with MRI increased from 0.3% (95% CI, 0.3%-0.4%) to 0.6% (95% CI, 0.6%-0.6%) (P < .001 for trend). The largest decreases in CT rates were for concussion (−23.0%), appendectomy (−14.9%), ventricular shunt procedures (−13.3%), and headaches (−12.4%). Factors associated with increased use of nonradiating imaging modalities included ultrasonography for abdominal pain (20.3%) and appendectomy (42.5%) and MRI for ventricular shunt procedures (17.9%) (P < .001 for trend). Across the study period, EDs varied widely in the use of ultrasonography for appendectomy (median, 57.5%; interquartile range [IQR], 40.4%-69.8%) and MRI (median, 15.8%; IQR, 8.3%-35.1%) and CT (median, 69.5%; IQR, 54.5%-76.4%) for ventricular shunt procedures. Overall, ED length of stay did not change, and hospitalization and 3-day ED revisit rates decreased during the study period.
Conclusions and Relevance
This study found that use of advanced imaging increased from 2009 to 2018. Although CT use decreased, this decrease was accompanied by a greater increase in the use of ultrasonography and MRI. There appears to be substantial variation in practice and a need to standardize imaging practices.
Introduction
Computed tomography (CT), ultrasonography, and magnetic resonance imaging (MRI) are important diagnostic tools in the evaluation of children seeking emergency department (ED) care. Historically, CT has been the most commonly used advanced imaging modality in the ED setting1 because it is fast, accurate, and accessible. However, scientific consensus is that radiation from CT is associated with increased risk of cancer, particularly with exposure in childhood.2 Advocacy campaigns, such as Image Gently2 and Choosing Wisely,3 and media reports,4,5,6,7 have raised awareness in the medical community and the public about these risks. Consequently, health care professionals, patients, and families may seek alternative, nonradiating modalities, such as ultrasonography and MRI, when they are considered effective and it is feasible. The benefits of ultrasonography and MRI are balanced by the often limited availability, operator dependence, cost, and, in some cases for MRI, the need for sedation.
Prior studies8,9,10,11,12,13 evaluating ED imaging use have focused on specific diagnoses or local patterns of use or have only examined use of CT without considering alternative imaging options. Ultrasonography has increasingly been used as a replacement for the evaluation of several conditions that traditionally have relied on CT.14,15,16 Advances in MRI technology, including the development of so-called fast or rapid protocols,17,18,19 and increased availability have led to greater feasibility of MRI for children in the ED. In addition, clinical decision rules20,21 and objective scoring tools22,23,24 have provided opportunities to safely minimize unnecessary imaging altogether. It is for these reasons that emergency imaging patterns have likely continued to change. A comprehensive, up-to-date assessment of pediatric ED-specific imaging practices and patterns can provide benchmarks for practitioners, hospitals, and insurers. Thus, the primary objective of this study was to evaluate the changes in the use of advanced imaging, including diagnosis-specific patterns, in US-based pediatric EDs between 2009 and 2018. We hypothesized that CT use decreased with a concomitant increase in ultrasonography and MRI. Our secondary objectives were to assess variation in these imaging patterns across pediatric EDs and to examine changes in hospitalization and 3-day revisit rates and ED length of stay (LOS).
Methods
Data Source and Design
We conducted a multicenter cross-sectional study using the Pediatric Health Information System (PHIS), an administrative database that includes ED and inpatient data from 52 tertiary care children’s hospitals in the US and is housed by the Children’s Hospital Association. Data quality is assured through a joint effort between the Children’s Hospital Association and participating hospitals. Data are deidentified and subject to multiple validity and reliability checks before inclusion in the database. For this study, we included 32 EDs in the final cohort after excluding 20 hospitals that did not contribute comprehensive ED-specific data during the study period. We included visits by patients younger than 18 years with an ED encounter from January 1, 2009, through December 31, 2018. The University of Pittsburgh Human Research Protection Office determined the study was not human subjects research and was therefore exempt from review and informed consent.
Outcome Measures and Variables
The primary outcome was the proportion of ED encounters with at least 1 advanced imaging study, identified through billing codes, and defined as CT, ultrasonography, MRI, or a combination of these. The database permits identification of the date the imaging was performed; however, it does not distinguish between ED and inpatient testing for patients admitted from the ED. Therefore, for patients admitted to the hospital from the ED, we defined ED imaging based on time of arrival. Specifically, we attributed imaging to the ED visit when the ED arrival time was before 6 pm and on the initial or second hospital day for an admitted patient with an ED arrival after 6 pm.25 For children who were discharged from the ED, we examined their entire ED encounter.
In addition to evaluating overall use of advanced imaging, as a subanalysis, we focused on conditions that were associated with the overall decreases in CT; specifically, we evaluated conditions associated with CT changes above the mean decrease, comparing 2018 with 2009. Encounter diagnoses were categorized using the all patient-refined diagnosis related groups (APR-DRGs), a standardized method of classifying patients into 1 of 311 clinically relevant groups, according to International Classification of Diseases (ICD) diagnosis codes, severity of illness, and mortality risk.26 To avoid including APR-DRGs with low absolute frequencies of imaging, for this analysis, we excluded diagnoses with a mean of fewer than 30 CT scans performed per hospital annually.27
To examine potential unintended consequences associated with changes in advanced imaging, for these conditions, we assessed 3 secondary outcome measures: (1) ED LOS for discharged patients, (2) hospitalization rates, and (3) 3-day ED revisit rates. For measuring LOS, we examined only patients discharged from the ED, excluding hospitalized patients because it is not possible in the database to isolate ED-specific LOS for admitted patients. We also assessed patient characteristics across the study period, including age, sex, race/ethnicity, presence of a complex chronic condition28 during the encounter, primary insurance, ED disposition, and geographic region.
Statistical Analysis
We evaluated overall and APR-DRG–specific annual trends of each advanced imaging modality as a proportion of ED visits. We summarized categorical variables using frequencies and percentages and continuous variables with medians and interquartile ranges (IQRs). We used χ2 tests to compare categorical data. For the analysis of CT trends, we used nonlinear modeling optimization to identify the year in which there was a change in slope. We used generalized estimating equations, which accounted for hospital clustering, to analyze trends over time. We constructed groups of generalized linear models with a random effect for hospital, evaluating the independent association of relevant covariates with our primary outcomes of modes of advanced imaging (first group) and with secondary outcome measures of ED LOS, hospitalization, and revisit rates (second group). Significance was set at 2-sided P < .05. All analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
Results
Patient and Characteristics
There were a total of 26 082 062 visits to 32 US pediatric EDs during the 10-year study period, with 1 or more advanced imaging studies used in 1 919 283 encounters (7.4%). A total of 9 273 181 patients (35.6%; mean [SD] age, 5.59 [5.15] years; 13 842 567 [53.1%] male) were non-Hispanic white, 7 136 412 (27.4%) were non-Hispanic black, and 7 543 194 (28.9%) were Hispanic (Table). A total of 16 511 436 (64.4%) had public insurance, and most 22 455 390 (86.1%) were discharged from the ED. No substantive changes in patient demographics were found across the study period.
Table. Characteristics in Patient Encounters to Emergency Departments of 32 US Children’s Hospitals Across the Study Period.
| Characteristic | Patients, No. (%) | P valuea | ||||
|---|---|---|---|---|---|---|
| Overall | 2009 | 2012 | 2015 | 2018 | ||
| Encounters | 26 082 062 | 2 300 773 | 2 590 346 | 2 743 284 | 2 819 384 | NA |
| Age group, y | ||||||
| <1 | 4 351 048 (16.7) | 406 365 (17.7) | 435 603 (16.8) | 451 833 (16.5) | 451 214 (16.0) | <.001 |
| 1-4 | 9 432 406 (36.2) | 862 153 (37.5) | 959 644 (37.0) | 970 525 (35.4) | 985 230 (34.9) | |
| 5-12 | 8 488 882 (32.5) | 720 738 (31.3) | 831 429 (32.1) | 909 941 (33.2) | 942 260 (33.4) | |
| 13-17 | 3 809 698 (14.6) | 311 504 (13.5) | 363 668 (14.0) | 410 985 (15.0) | 440 680 (15.6) | |
| Male sex | 13 842 567 (53.1) | 1 234 541 (53.7) | 1 380 175 (53.3) | 1 449 885 (52.9) | 1 484 373 (52.7) | <.001 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 9 273 181 (35.6) | 802 446 (34.9) | 960 403 (37.1) | 934 474 (34.1) | 971 489 (34.5) | .01 |
| Non-Hispanic black | 7 136 412 (27.4) | 690 558 (30.0) | 664 834 (25.7) | 742 264 (27.1) | 736 418 (26.1) | |
| Hispanic | 7 543 194 (28.9) | 633 256 (27.5) | 663 572 (25.6) | 854 808 (31.2) | 890 190 (31.6) | |
| Other | 2 129 275 (8.2) | 174 513 (7.6) | 301 537 (11.6) | 211 738 (7.7) | 221 287 (7.8) | |
| Complex chronic condition(s) | 1 565 472 (6.0) | 124 739 (5.4) | 146 078 (5.6) | 168 971 (6.2) | 188 496 (6.7) | <.001 |
| Insurance | ||||||
| Public | 16 511 436 (64.4) | 6 519 739 (63.8) | 1 329 523 (59.3) | 1 676 181 (65.1) | 1817359 (66.4) | .19 |
| Private | 7 504 040 (29.3) | 3 062 916 (30.0) | 720 402 (32.1) | 764 819 (29.7) | 770482 (28.2) | |
| Otherb | 1 606 001 (6.3) | 634 538 (6.2) | 191 445 (8.5) | 133 442 (5.2) | 147402 (5.4) | |
| Disposition | ||||||
| Discharged | 22 455 390 (86.1) | 1 973 612 (85.8) | 2 198 937 (84.9) | 2 381 230 (86.8) | 2 459 165 (87.2) | .003 |
| Inpatient admission | 2 845 465 (10.9) | 250 795 (10.9) | 275 318 (10.6) | 300 903 (11.0) | 313 896 (11.1) | |
| ICU admission | 272 060 (1.0) | 20 770 (0.9) | 25 659 (1.0) | 30 341 (1.1) | 33 937 (1.2) | |
| Transferred | 162 777 (0.6) | 8896 (0.4) | 14 951 (0.6) | 19 437 (0.7) | 18 885 (0.7) | |
| Died | 4402 (0) | 455 (0) | 478 (0) | 406 (0) | 428 (0) | |
| Other | 614 028 (2.4) | 67 015 (2.9) | 100 662 (3.9) | 41 308 (1.5) | 27 010 (1.0) | |
| Census region | ||||||
| Midwest | 7 562 417 (29.0) | 744 817 (32.4) | 742 418 (28.7) | 773 932 (28.2) | 806 368 (28.6) | <.001 |
| Northeast | 2 095 794 (8.0) | 178 722 (7.8) | 216 352 (8.4) | 211 764 (7.7) | 222 281 (7.9) | |
| South | 10 322 420 (39.6) | 925 648 (40.2) | 1 061 249 (41.0) | 1 061 693 (38.7) | 1 096 150 (38.9) | |
| West | 6 101 431 (23.4) | 451 586 (19.6) | 570 327 (22.0) | 695 895 (25.4) | 694 585 (24.6) | |
Abbreviations: ICU, intensive care unit; NA, not applicable.
The χ2 test P values comparing all years are given for each variable.
Other includes American Indian, Asian, multiracial, Native Hawaiian, other race, and missing race.
Overall Advanced Imaging Trends
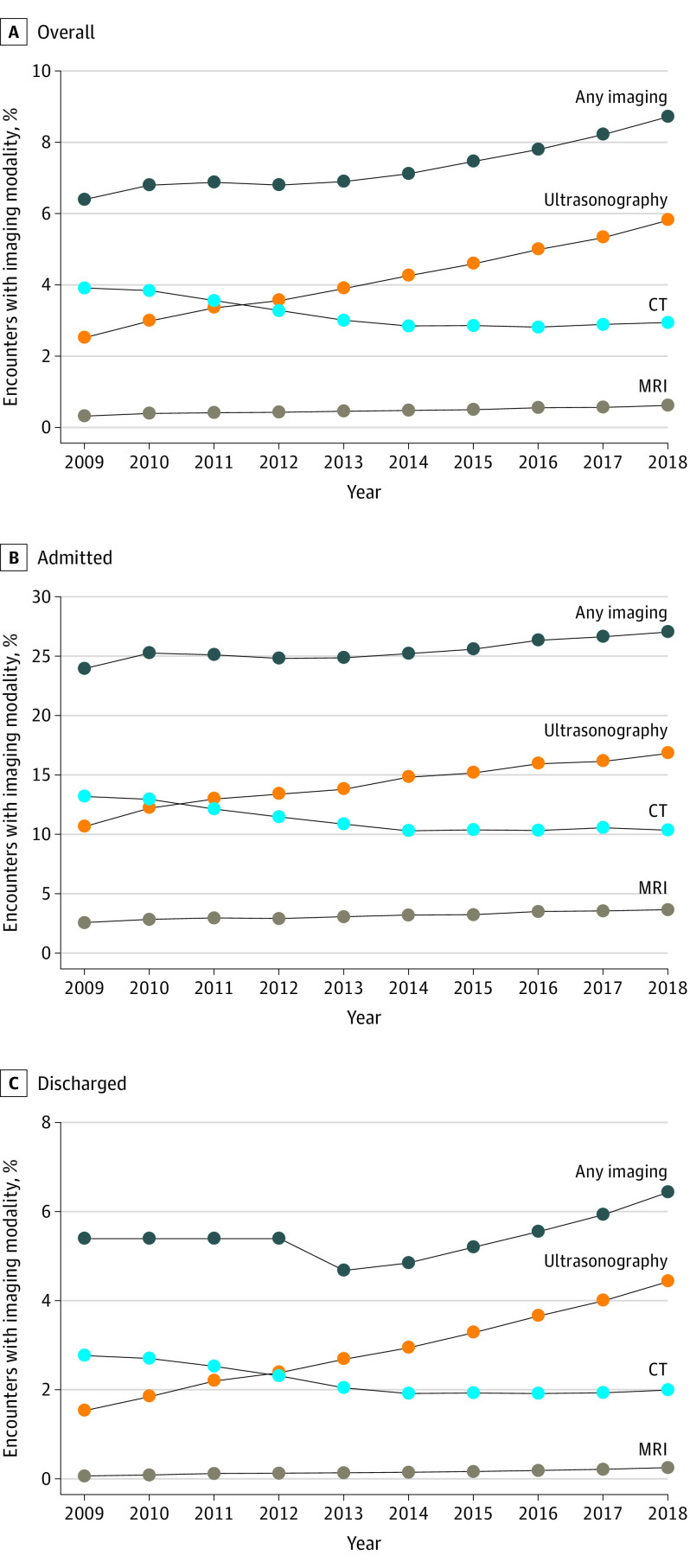
The percentage of ED encounters associated with any advanced imaging increased from 6.4% (95% CI, 6.4%-6.4%) in 2009 to 8.7% (95% CI, 8.7%-8.8%) in 2018 (P < .001 for trend) (Figure 1), resulting in 65 613 more encounters with advanced imaging in 2018. Computed tomography use decreased from 3.9% (95% CI, 3.9%-3.9%) in 2009 to 2.9% (95% CI, 2.9%-3.0%) in 2018 (P = .001 for trend), resulting in 27 487 fewer encounters with CT in 2018. Despite this decrease during the 10-year period, there was a plateau from 2014 to 2018. Specifically, CT use decreased from 3.9% (95% CI, 3.9%-3.9%) to 2.9% (95% CI, 2.8%-2.9%) from 2009 to 2014 (P < .001) but did not change from 2014 (2.9%; 95% CI, 2.8%-2.9%) to 2018 (2.9%; 95% CI, 2.7%-2.9%) (P = .32). Ultrasonography use increased from 2.5% (95% CI, 2.5%-2.6%) in 2009 to 5.8% (95% CI, 5.8%-5.9%) in 2018 (P < .001 for trend), resulting in 92 852 more encounters with ultrasonography in 2018, and MRI use increased from 0.3% (95% CI, 0.3%-0.4%) in 2009 to 0.6% (95% CI, 0.6%-0.6%) in 2018 (P < .001 for trend), resulting in 8116 more encounters with MRI in 2018. There were similar patterns of increases in use of MRI and ultrasonography and decreases in use of CT when stratifying encounters by ED disposition (Figure 1 and eTable 1 in the Supplement). Of the 1 919 283 ED encounters with advanced imaging, 133 862 (7.0%) included more than 1 advanced imaging modality, and 92 232 (68.9%) of these encounters included both ultrasonography and CT. Children 5 years and older, white patients, those with complex chronic conditions, those with private insurance, and those who were admitted had higher odds of undergoing CT, MRI, and ultrasonography (eTable 2 in the Supplement).
Figure 1. Trends in Use of Computed Tomography (CT), Ultrasonography, and Magnetic Resonance Imaging (MRI) for Pediatric Emergency Department Encounters Overall and for Encounters Resulting in Admission and Discharge, 2009-2018.
P < .001 for trend for all comparisons.
Diagnosis-Specific Patterns
There were 19 APR-DRGs associated with at least 30 CT encounters per hospital per year. The percentage change (median, −2.1%) in CT across the study period ranged from −23.0% to 0.9% across these 19 APR-DRGs. Among these conditions, there were 8 APR-DRGs with decreases in use of CT that were greater than the mean (−5.2%; 95% CI, −8.1% to −2.3%) decrease, which were the focus of this subanalysis: concussion, closed skull fracture, uncomplicated intracranial, coma of less than 1 hour, or no coma (−23.0% change; 95% CI, −24.1% to −21.9%); appendectomy (−14.9% change; 95% CI, −16.0% to −13.8%); ventricular shunt procedures (−13.3% change; 95% CI, −16.7% to −10.0%); migraine and other headaches (−12.4% change; 95% CI, −13.0% to −11.7%); other disorders of the nervous system (−10.1% change; 95% CI, −11.3% to −8.9%); abdominal pain (−6.1% change; 95% CI, −6.4% to −5.8%); other ear, nose, mouth, throat, and cranial or facial diagnoses (−5.9% change; 95% CI, −6.2% to −5.7%); and seizure (−5.3% change; 95% CI, −5.8% to −4.8%) (P < .001 for trend). These APR-DRGs were associated with 51.1% of CT imaging and 31.5% of advanced imaging performed during the study period. APR-DRG–specific patterns of CT, ultrasonography, and MRI use over time are shown in Figure 2, Figure 3, and eTable 3 in the Supplement. These APR-DRGs were associated with more than 1 advanced imaging modality in 14.7% (ventricular shunt procedures), 8.6% (appendectomy), 3.4% (abdominal pain), 3.1% (other disorders of the nervous system), 1.2% (seizure), 0.9% (migraine), 0.8% (concussion), and 0.1% (other ear, nose, mouth, throat, and cranial or facial diagnoses) of encounters. The most common principal ICD-9 or ICD-10 diagnosis codes for each of these 8 APR-DRGs are listed in eTable 4 in the Supplement.
Figure 2. Trends Over Time in Advanced Imaging for 4 All Patient-Refined Diagnosis Related Groups With the Largest Decreases in Computed Tomography (CT) Use, 2009-2018.
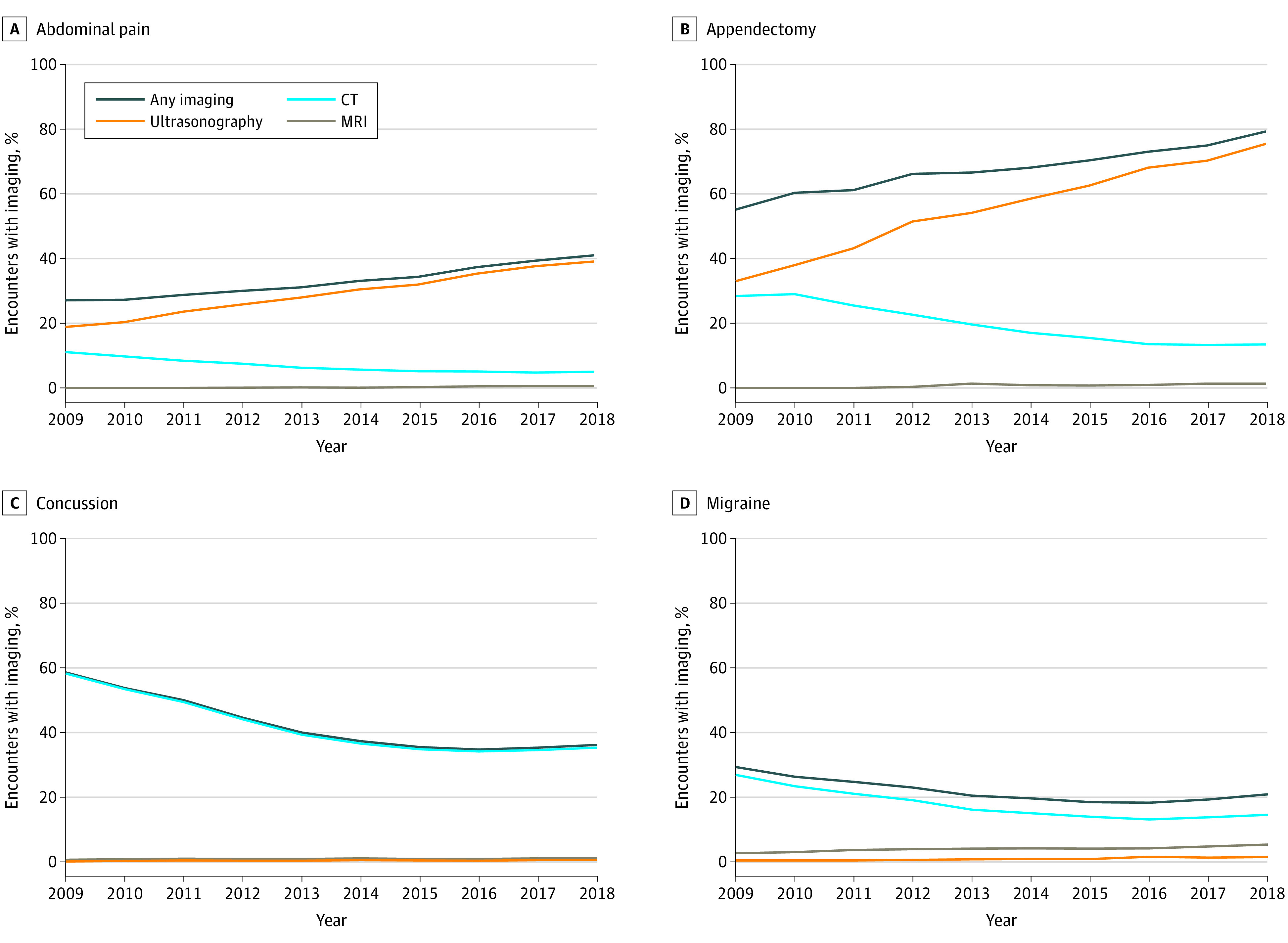
Concussion includes concussion, closed skull fracture, uncomplicated intracranial injury, coma of less than 1 hour, or no coma. Migraine includes migraines and other headache. P < .01 for trend for all comparisons. MRI indicates magnetic resonance imaging.
Figure 3. Trends Over Time in Advanced Imaging for the Remaining 4 All Patient-Refined Diagnosis Related Groups With the Largest Decreases in Computed Tomography (CT) Use, 2009-2018.
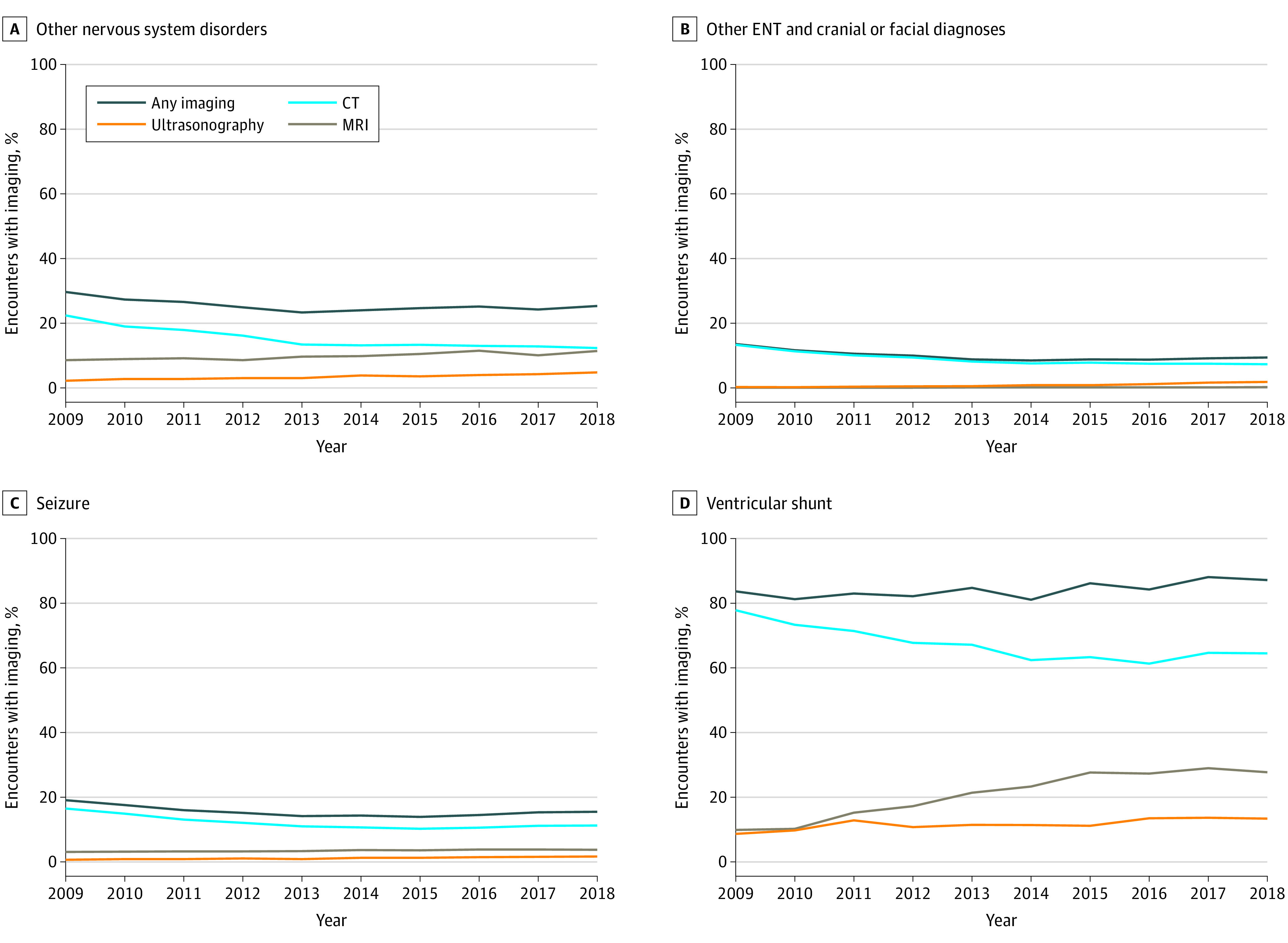
P < .001 for trend for all comparisons except for magnetic resonance imaging (MRI) seizure (P = .005), ultrasonographic ventricular shunt (P = .007), and any imaging ventricular shunt (P = .001). ENT indicates ear, nose, and throat.
Across the 8 APR-DRGs, 4 conditions were associated with an overall increase in advanced imaging use despite the decrease in CT use. Specifically, this increase from 2009 to 2018 was greatest in ultrasonography for appendectomy (42.5%; 95% CI, 41.3%-43.8%) and abdominal pain (20.3%; 95% CI, 19.8%-20.8%) and MRI for ventricular shunt procedures (17.9%; 95% CI, 15.0%-20.8%) (P < .001 for trend). For other conditions, most notably concussion, the decrease in CT use was not associated with a compensatory increase in other modalities.
Variation in Imaging Across Hospitals by APR-DRG
Variability of advanced imaging across EDs for the 8 APR-DRGs is shown in Figure 4. We observed the widest variation across the 32 EDs in the use of ultrasonography for appendectomy (median, 57.5%; IQR, 40.4%-69.8%) and MRI (median, 15.8%; IQR, 8.3%-35.1%) and CT (median, 69.5%; IQR, 54.5%-76.4%) for ventricular shunt procedures. Emergency department–specific changes in CT use, comparing the years before and after the plateau in CT in 2014, are shown in eFigure 1 in the Supplement. For encounters among the 8 APR-DRGs, the median baseline CT use across EDs was 15.0% (range, 8.3%-27.6%), with rates changing across the 2 periods by −10.7% before 2014 to 1.4% after 2014. The EDs with baseline CT rates in the lowest quartile did not have large changes in their overall rates of CT. Four hospitals consistently had reduced CT use greater than the median decrease for all conditions, whereas others did so only for certain conditions.
Figure 4. Hospital Variation in Advanced Imaging by All Patient-Refined Diagnosis Related Groups, 2009-2018.
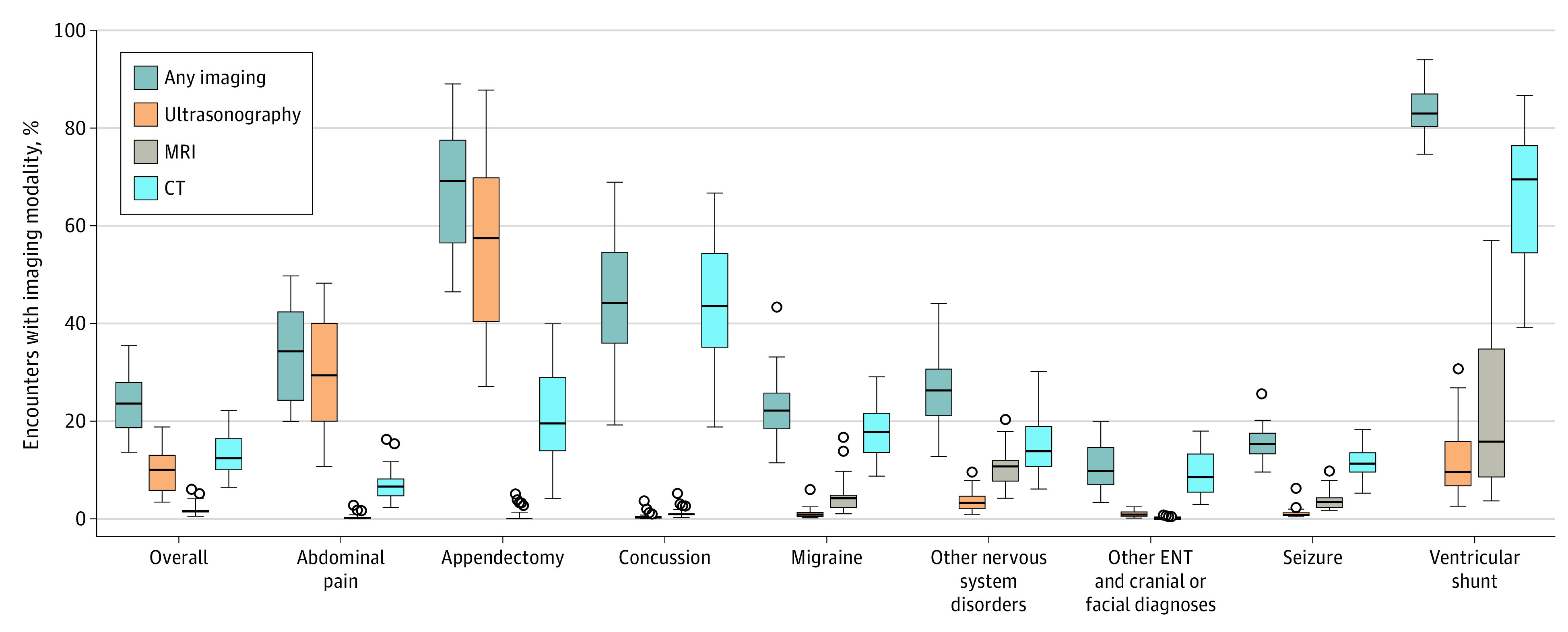
Distribution of the proportion of emergency department encounters with imaging. For each box, the horizontal line represents the median proportion, and the upper and lower edges of the box represent the upper and lower quartiles. The whiskers indicate the range, excluding outliers. Outliers (circles) are values greater than 1.5 times the interquartile range above the median. Concussion includes concussion, closed skull fracture, uncomplicated intracranial injury, coma of less than 1 hour, or no coma. Migraine includes migraine and other headaches. ENT indicates ear, nose, and throat; MRI, magnetic resonance imaging.
Secondary Outcomes
Across the 8 APR-DRGs, advanced imaging was independently associated with an increase in ED LOS and odds of admission and 3-day revisits (eTable 5 in the Supplement). However, despite these encounter-level increases and an increase in advanced imaging across the study period, overall ED LOS remained stable across the study period, with decreasing rates of admission and 3-day revisits (eFigure 2 in the Supplement).
Discussion
We observed an overall increase in the use of advanced imaging across US pediatric EDs during the past decade. The use of CT decreased, with most of this decrease associated with 8 APR-DRGs. For certain APR-DRGs, this decrease was associated with increases in other radiation-sparing advanced imaging modalities, such as ultrasonography for abdominal conditions and MRI for patients with ventricular shunts. The magnitude of the decrease in CT use for these conditions varied by hospital but was not associated with increases in hospitalizations, ED revisits, or ED LOS.
Reasons for these changing imaging patterns are likely multifactorial. Epidemiologic studies29,30,31 have provided more insight for the scientific community into the association between radiation exposure from CT and cancer risk. There have been several high-profile media publications7,32 that have likely provoked concerns regarding CT from patients and families.33 Campaigns that target health care professionals and the public, such as Image Gently in 20072 and Choosing Wisely in 2012,34 have raised awareness regarding optimizing pediatric imaging practices. Efforts such as these may, in part, explain the trends toward nonradiating imaging modalities.
For example, the American Academy of Pediatrics35 and the American College of Radiology36 Choosing Wisely lists of “ten things physicians and patients should question” recommend that practitioners consider performing ultrasonography first before or in lieu of CT for children with abdominal pain. Although the diagnostic accuracy of CT is superior to ultrasonography for appendicitis,37 EDs have used various strategies to reduce CT use and thus radiation exposure for the evaluation of abdominal pain. Several studies38,39,40,41 highlight the association of guideline implementation and integration of clinical decision support into electronic health systems with reducing abdominal CT use without increasing adverse outcomes. Such strategies may be associated with some of the increase in ultrasonography use we observed in patients with diagnoses related to abdominal issues (ie, abdominal pain and appendectomy). Interestingly, the increase in the use of ultrasonography for these conditions was greater than the decrease in the use of CT. Therefore, a proportion of these ultrasonographic examinations likely represent overuse of a typically widely available and nonradiating imaging tool. With respect to concussion encounters, the reduction in CT use was not supplanted by increases in alternative imaging modalities. The decreases in CT use in both instances may reflect the knowledge translation of clinical decision rules,20,22,23,24,42,43 whereas the divergence in replacement may reflect alternative options: ultrasonography for appendicitis is relatively inexpensive, readily available, and safe, whereas MRI for intracranial hemorrhage is expensive and less available and, although safe, often requires sedation.
Another area of imaging growth we observed in our study was the use of MRI in patients with ventricular shunt procedures. In the past decade, studies17,44,45,46,47 have highlighted the accuracy and feasibility of so-called rapid or fast MRI in lieu of CT for the evaluation of ventricular shunt malfunction. With rapid MRI technology, there is often no requirement for sedation, even for infants and young children. As more indications for these rapid MRI studies emerge and MRI availability increases,18,19,48,49,50 MRI adoption may continue to increase and may be associated with further decreases in CT imaging for many diagnoses.51
For certain APR-DRGs, specifically concussion, the decrease in CT use was not associated with an increase in other advanced imaging modalities. Clinical decision rules for head trauma20,42,43 allow for the safe selection of low-risk patients who can be observed without neuroimaging. These decreases in CT may be associated with dissemination and implementation52 of these clinical decision rules. It is also plausible that given the increases in awareness and attention surrounding concussion in the past decade,53 the volume and recognition of patients with concussion have increased, resulting in a lower overall proportion of CT in this population.
Our findings build on other studies9,10,11,54,55 of imaging in children. Specifically, earlier work9,10,11,54 demonstrated decreases in CT use among pediatric ED patients and increases in ultrasonography and MRI use for certain conditions beginning in the mid-2000s. Our work provides additional insight into more recent trends, revealing an unexpected plateau in CT use since 2014. This finding may indicate that, at least with current efforts, a lower limit to CT use has been reached. A recent study by Smith-Bindman et al55 examined trends in advanced imaging and found increases in ultrasonography beyond the decreases in CT use, as well as a similar plateau after the more rapid decreases in CT use. That study, however, examined encounters by privately insured patients across all health care settings. Our study examined ED-specific practices and allowed for more detailed investigation into specific diagnoses associated with imaging trends over time.
We observed significant between-site variation, which may be secondary to local guidelines and protocols, equipment availability, and practice preferences among subspecialists.56 Our findings provide benchmarks for EDs that seek to understand their imaging practices in the context of peer hospitals. Further reductions in CT use at some sites remain possible but likely require a greater emphasis on knowledge translation and quality improvement initiatives.38,52,57
Limitations
Our study has several limitations. We were unable to assess the indications for imaging studies, and unmeasured confounders related to the performance of advanced imaging may exist that could have affected our findings. Similarly, we do not know if there were harms, such as incidental findings that required additional visits, more downstream testing, and direct costs to patients and the health care system. Some revisits were not captured in our database because, although the PHIS database allows for tracking individual patients longitudinally, only revisits to the same hospital are captured. If patients returned to other EDs for additional care, we would have underestimated the frequency of 3-day ED revisits. The effect of this limitation, however, is likely to be small because patients are more likely to return to the index ED.58 APR-DRGs are assigned using diagnostic algorithms that are based on discharge codes associated with individual encounters.26 In addition, severity of illness is ascribed to the encounter based on multiple factors, including the use of diagnostic imaging. Therefore, some patients may be misclassified when assigned to certain APR-DRGs (eg, a patient with a clinically insignificant intracranial hemorrhage seen on CT may be assigned a different APR-DRG than if a CT had not been performed and the patient was diagnosed with concussion). This study was conducted across children’s hospitals in the US and may not be generalizable to other hospitals or institutions in other countries. However, the trends we observed in rates of CT, ultrasonography, and MRI in children’s hospital EDs mirror those found in the more comprehensive analysis by Smith-Bindman et al.55 We may have misclassified some imaging studies as having occurred within the ED for hospitalized patients who had imaging after admission to the hospital. In addition, point-of-care ultrasonographic examinations by emergency physicians may not have been captured because PHIS data are based on procedures billed and site variation in billing exists for these examinations.59 This occurrence would have resulted in an underestimation of true ultrasonography use rates.
Conclusions
The study found that overall use of advanced imaging in pediatric EDs in the US increased between 2009 and 2018. A decrease in CT use occurred during the 10-year period, with a plateau after 2014. The magnitude of the decrease in CT use varied by site and was associated, in part, with the use of alternative advanced imaging modalities for certain diagnoses, most notably ultrasonography for abdominal conditions. Future efforts appear to be needed to standardize imaging approaches and evaluate the effect of the changing landscape of advanced imaging on patient-level outcomes.
eTable 1. Proportions of Encounters With Advanced Imaging by Disposition
eTable 2. Multivariable Model of Factors Associated With Emergency Department Advanced Imaging Studies
eTable 3. Frequency of Advanced Imaging, Admission, and Proportions of Total ED Visits for the 8 APR-DRGs
eTable 4. Ten Most Frequent ICD-9 and ICD-10 Codes as Principal Diagnosis for the 8 APR-DRGs
eTable 5. Multivariable Model of Factors Associated With Secondary Outcome Measures for the 8 APR-DRGs
eFigure 1. Hospital-Specific Changes in CT Imaging Overall and for Each of the 8 APR-DRGs Comparing 2009-2013 to 2014-2018
eFigure 2. Trends in Secondary Outcome Measures 2009-2018 for the 8 DRGs
References
- 1.Larson DB, Johnson LW, Schnell BM, Goske MJ, Salisbury SR, Forman HP. Rising use of CT in child visits to the emergency department in the United States, 1995-2008. Radiology. 2011;259(3):793-801. doi: 10.1148/radiol.11101939 [DOI] [PubMed] [Google Scholar]
- 2.Goske MJ, Applegate KE, Boylan J, et al. The ‘Image Gently’ campaign: increasing CT radiation dose awareness through a national education and awareness program. Pediatr Radiol. 2008;38(3):265-269. doi: 10.1007/s00247-007-0743-3 [DOI] [PubMed] [Google Scholar]
- 3.Choosing Wisely. An initiative of the ABIM Foundation. Accessed July 21, 2014. https://www.choosingwisely.org
- 4.Dolan TG. CT in the ER. Published July 1, 2011. Accessed December 7, 2015. https://www.radiologytoday.net/archive/rt0711p16.shtml
- 5.Marchione M. CT scans pose risks, need more regulation. Published June 23, 2010. Accessed September 18, 2019. https://www.huffingtonpost.com/news/ct-scans
- 6.Wang SS. CT scans on children worry experts. Wall Street Journal. Published June 10, 2013. Accessed June 24, 2015. https://www.wsj.com/articles/SB10001424127887324904004578537564115192112
- 7.Redberg RF, Smith-Bindman R We are giving ourselves cancer. New York Times. Published January 30, 2014. Accessed September 18, 2019. http://www.nytimes.com/2014/01/31/opinion/we-are-giving-ourselves-cancer.html?hp&rref=opinion&_r=1
- 8.Bachur RG, Hennelly K, Callahan MJ, Monuteaux MC. Advanced radiologic imaging for pediatric appendicitis, 2005-2009: trends and outcomes. J Pediatr. 2012;160(6):1034-1038. doi: 10.1016/j.jpeds.2011.11.037 [DOI] [PubMed] [Google Scholar]
- 9.Otero HJ, Crowder L. Imaging utilization for the diagnosis of appendicitis in stand-alone children’s hospitals in the United States: trends and costs. J Am Coll Radiol. 2017;14(5):603-608. doi: 10.1016/j.jacr.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 10.Mannix R, Meehan WP, Monuteaux MC, Bachur RG. Computed tomography for minor head injury: variation and trends in major United States pediatric emergency departments. J Pediatr. 2012;160(1):136-139.e1. doi: 10.1016/j.jpeds.2011.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trost MJ, Robison N, Coffey D, Mamey MR, Robison RA. Changing trends in brain imaging technique for pediatric patients with ventriculoperitoneal shunts. Pediatr Neurosurg. 2018;53(2):116-120. doi: 10.1159/000485923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menoch MJA, Hirsh DA, Khan NS, Simon HK, Sturm JJ. Trends in computed tomography utilization in the pediatric emergency department. Pediatrics. 2012;129(3):e690-e697. doi: 10.1542/peds.2011-2548 [DOI] [PubMed] [Google Scholar]
- 13.Lodwick DL, Cooper JN, Kelleher KJ, Brilli R, Minneci PC, Deans KJ. Variation in utilization of computed tomography imaging at tertiary pediatric hospitals. Pediatrics. 2015;136(5):e1212-e1219. doi: 10.1542/peds.2015-1671 [DOI] [PubMed] [Google Scholar]
- 14.Koberlein GC, Trout AT, Rigsby CK, et al. ; Expert Panel on Pediatric Imaging . ACR Appropriateness Criteria®: suspected appendicitis-child. J Am Coll Radiol. 2019;16(5S):S252-S263. doi: 10.1016/j.jacr.2019.02.022 [DOI] [PubMed] [Google Scholar]
- 15.Riccabona M, Avni FE, Blickman JG, et al. Imaging recommendations in paediatric uroradiology: minutes of the ESPR uroradiology task force session on childhood obstructive uropathy, high-grade fetal hydronephrosis, childhood haematuria, and urolithiasis in childhood; ESPR Annual Congress, Edinburgh, UK, June 2008. Pediatr Radiol. 2009;39(8):891-898. doi: 10.1007/s00247-009-1233-6 [DOI] [PubMed] [Google Scholar]
- 16.Swenson DW, Ayyala RS, Sams C, Lee EY. Practical imaging strategies for acute appendicitis in children. AJR Am J Roentgenol. 2018;211(4):901-909. doi: 10.2214/AJR.18.19778 [DOI] [PubMed] [Google Scholar]
- 17.Boyle TP, Paldino MJ, Kimia AA, et al. Comparison of rapid cranial MRI to CT for ventricular shunt malfunction. Pediatrics. 2014;134(1):e47-e54. doi: 10.1542/peds.2013-3739 [DOI] [PubMed] [Google Scholar]
- 18.Flom L, Fromkin J, Panigrahy A, Tyler-Kabara E, Berger RP. Development of a screening MRI for infants at risk for abusive head trauma. Pediatr Radiol. 2016;46(4):519-526. doi: 10.1007/s00247-015-3500-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Missios S, Quebada PB, Forero JA, et al. Quick-brain magnetic resonance imaging for nonhydrocephalus indications. J Neurosurg Pediatr. 2008;2(6):438-444. doi: 10.3171/PED.2008.2.12.438 [DOI] [PubMed] [Google Scholar]
- 20.Kuppermann N, Holmes JF, Dayan PS, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009;374(9696):1160-1170. doi: 10.1016/S0140-6736(09)61558-0 [DOI] [PubMed] [Google Scholar]
- 21.Holmes JF, Lillis K, Monroe D, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013;62(2):107-116.e2. doi: 10.1016/j.annemergmed.2012.11.009 [DOI] [PubMed] [Google Scholar]
- 22.Kharbanda AB, Vazquez-Benitez G, Ballard DW, et al. Development and validation of a novel pediatric appendicitis risk calculator (pARC). Pediatrics. 2018;141(4):e20172699. doi: 10.1542/peds.2017-2699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-564. doi: 10.1016/S0196-0644(86)80993-3 [DOI] [PubMed] [Google Scholar]
- 24.Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002;37(6):877-881. doi: 10.1053/jpsu.2002.32893 [DOI] [PubMed] [Google Scholar]
- 25.Samuels-Kalow M, Neuman MI, Rodean J, et al. The care of adult patients in pediatric emergency departments. Acad Pediatr. 2019;19(8):942-947. doi: 10.1016/j.acap.2019.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Averill RF, Goldfield N, Hughes JS, et al. All patient refined diagnosis related groups (APR-DRGs), version 20.0: methodology overview. Published July 1, 2003. Accessed September 18, 2019. https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf
- 27.Ash AS, Shwartz M, Pekoz EA. Comparing outcomes across providers In: Iezzoni LI, ed. Risk Adjustment for Measuring Health Care Outcomes. Health Administration Press; 1994:1-37. [Google Scholar]
- 28.Feinstein JA, Russell S, DeWitt PE, Feudtner C, Dai D, Bennett TD. R package for pediatric complex chronic condition classification. JAMA Pediatr. 2018;172(6):596-598. doi: 10.1001/jamapediatrics.2018.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hong J-Y, Han K, Jung J-H, Kim JS. Association of exposure to diagnostic low-dose ionizing radiation with risk of cancer among youths in South Korea. JAMA Netw Open. 2019;2(9):e1910584-e11. doi: 10.1001/jamanetworkopen.2019.10584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499-505. doi: 10.1016/S0140-6736(12)60815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. doi: 10.1136/bmj.f2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.USA Today: CT scans in children linked to cancer. Published June 19, 2001. Accessed March 22, 2013. http://usatoday30.usatoday.com/news/nation/2001-01-22-scans.htm
- 33.Boutis K, Cogollo W, Fischer J, Freedman SB, Ben David G, Thomas KE. Parental knowledge of potential cancer risks from exposure to computed tomography. Pediatrics. 2013;132(2):305-311. doi: 10.1542/peds.2013-0378 [DOI] [PubMed] [Google Scholar]
- 34.Cassel CK, Guest JA. Choosing Wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802. doi: 10.1001/jama.2012.476 [DOI] [PubMed] [Google Scholar]
- 35.American Academy of Pediatrics. Choosing Wisely. Published February 21, 2013. Accessed September 22, 2019. https://www.choosingwisely.org/wp-content/uploads/2015/02/AAP-Choosing-Wisely-List.pdf
- 36.American College of Radiology, Choosing Wisely. Published April 4, 2012. Accessed September 22, 2019. https://www.choosingwisely.org/wp-content/uploads/2015/02/ACR-Choosing-Wisely-List.pdf
- 37.Mittal MK, Dayan PS, Macias CG, et al. ; Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics . Performance of ultrasound in the diagnosis of appendicitis in children in a multicenter cohort. Acad Emerg Med. 2013;20(7):697-702. doi: 10.1111/acem.12161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Russell WS, Schuh AM, Hill JG, et al. Clinical practice guidelines for pediatric appendicitis evaluation can decrease computed tomography utilization while maintaining diagnostic accuracy. Pediatr Emerg Care. 2013;29(5):568-573. doi: 10.1097/PEC.0b013e31828e5718 [DOI] [PubMed] [Google Scholar]
- 39.Shah SR, Sinclair KA, Theut SB, Johnson KM, Holcomb GW III, St Peter SD. Computed tomography utilization for the diagnosis of acute appendicitis in children decreases with a diagnostic algorithm. Ann Surg. 2016;264(3):474-481. doi: 10.1097/SLA.0000000000001867 [DOI] [PubMed] [Google Scholar]
- 40.Polites SF, Mohamed MI, Habermann EB, et al. A simple algorithm reduces computed tomography use in the diagnosis of appendicitis in children. Surgery. 2014;156(2):448-454. doi: 10.1016/j.surg.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 41.Kharbanda AB, Madhok M, Krause E, et al. Implementation of electronic clinical decision support for pediatric appendicitis. Pediatrics. 2016;137(5):e20151745. doi: 10.1542/peds.2015-1745 [DOI] [PubMed] [Google Scholar]
- 42.Dunning J, Daly JP, Lomas J-P, Lecky F, Batchelor J, Mackway-Jones K; Children’s head injury algorithm for the Prediction of Important Clinical Events Study Group . Derivation of the children’s head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Child. 2006;91(11):885-891. doi: 10.1136/adc.2005.083980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Osmond MH, Klassen TP, Wells GA, et al. ; Pediatric Emergency Research Canada (PERC) Head Injury Study Group . CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ. 2010;182(4):341-348. doi: 10.1503/cmaj.091421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iskandar BJ, Sansone JM, Medow J, Rowley HA. The use of quick-brain magnetic resonance imaging in the evaluation of shunt-treated hydrocephalus. J Neurosurg. 2004;101(2, suppl):147-151. doi: 10.3171/ped.2004.101.2.0147 [DOI] [PubMed] [Google Scholar]
- 45.DeFlorio RM, Shah CC. Techniques that decrease or eliminate ionizing radiation for evaluation of ventricular shunts in children with hydrocephalus. Semin Ultrasound CT MR. 2014;35(4):365-373. doi: 10.1053/j.sult.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 46.Miller JH, Walkiewicz T, Towbin RB, Curran JG. Improved delineation of ventricular shunt catheters using fast steady-state gradient recalled-echo sequences in a rapid brain MR imaging protocol in nonsedated pediatric patients. AJNR Am J Neuroradiol. 2010;31(3):430-435. doi: 10.3174/ajnr.A1866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yue EL, Meckler GD, Fleischman RJ, et al. Test characteristics of quick brain MRI for shunt evaluation in children: an alternative modality to avoid radiation. J Neurosurg Pediatr. 2015;15(4):420-426. doi: 10.3171/2014.9.PEDS14207 [DOI] [PubMed] [Google Scholar]
- 48.Lindberg DM, Stence NV, Grubenhoff JA, et al. Feasibility and accuracy of fast MRI versus CT for traumatic brain injury in young children. Pediatrics. 2019;144(4):1-10. doi: 10.1542/peds.2019-0419 [DOI] [PubMed] [Google Scholar]
- 49.Aspelund G, Fingeret A, Gross E, et al. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics. 2014;133(4):586-593. doi: 10.1542/peds.2013-2128 [DOI] [PubMed] [Google Scholar]
- 50.Imler D, Keller C, Sivasankar S, et al. Magnetic resonance imaging versus ultrasound as the initial imaging modality for pediatric and young adult patients with suspected appendicitis. Acad Emerg Med. 2017;24(5):569-577. doi: 10.1111/acem.13180 [DOI] [PubMed] [Google Scholar]
- 51.Ramgopal S, Karim SA, Subramanian S, Furtado AD, Marin JR. Rapid brain MRI protocols reduce head computerized tomography use in the pediatric emergency department. BMC Pediatr. 2020;20(1):14. doi: 10.1186/s12887-020-1919-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dayan PS, Ballard DW, Tham E, et al. ; Pediatric Emergency Care Applied Research Network (PECARN); Clinical Research on Emergency Services and Treatment (CREST) Network; Partners Healthcare; Traumatic Brain Injury-Knowledge Translation Study Group . Use of traumatic brain injury prediction rules with clinical decision support. Pediatrics. 2017;139(4):1-12. doi: 10.1542/peds.2016-2709 [DOI] [PubMed] [Google Scholar]
- 53.Lumba-Brown A, Yeates KO, Sarmiento K, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018;172(11):e182853-e13. doi: 10.1001/jamapediatrics.2018.2853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Otero HJ, White AM, Khwaja AB, Griffis H, Katcoff H, Bresnahan BW. Imaging intussusception in children’s hospitals in the United States: trends, outcomes, and costs. J Am Coll Radiol. 2019;16(12):1636-1644. doi: 10.1016/j.jacr.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 55.Smith-Bindman R, Kwan ML, Marlow EC, et al. Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000-2016. JAMA. 2019;322(9):843-856. doi: 10.1001/jama.2019.11456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Broder JS, Bhat R, Boyd JP, et al. Who explicitly requests the ordering of computed tomography for emergency department patients? a multicenter prospective study. Emerg Radiol. 2016;23(3):221-227. doi: 10.1007/s10140-016-1382-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ellison JS, Crowell CS, Clifton H, et al. A clinical pathway to minimize computed tomography for suspected nephrolithiasis in children. J Pediatr Urol. 2019;15(5):518.e1-518.e7. doi: 10.1016/j.jpurol.2019.06.014 [DOI] [PubMed] [Google Scholar]
- 58.Lyons TW, Olson KL, Palmer NP, Horwitz R, Mandl KD, Fine AM. Patients visiting multiple emergency departments: patterns, costs, and risk factors. Acad Emerg Med. 2017;24(11):1349-1357. doi: 10.1111/acem.13304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Marin JR, Zuckerbraun NS, Kahn JM. Use of emergency ultrasound in United States pediatric emergency medicine fellowship programs in 2011. J Ultrasound Med. 2012;31(9):1357-1363. doi: 10.7863/jum.2012.31.9.1357 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Proportions of Encounters With Advanced Imaging by Disposition
eTable 2. Multivariable Model of Factors Associated With Emergency Department Advanced Imaging Studies
eTable 3. Frequency of Advanced Imaging, Admission, and Proportions of Total ED Visits for the 8 APR-DRGs
eTable 4. Ten Most Frequent ICD-9 and ICD-10 Codes as Principal Diagnosis for the 8 APR-DRGs
eTable 5. Multivariable Model of Factors Associated With Secondary Outcome Measures for the 8 APR-DRGs
eFigure 1. Hospital-Specific Changes in CT Imaging Overall and for Each of the 8 APR-DRGs Comparing 2009-2013 to 2014-2018
eFigure 2. Trends in Secondary Outcome Measures 2009-2018 for the 8 DRGs