Abstract
Obesity is a multifactorial condition arising from the interaction between genetic and lifestyle factors. We aimed to assess the impact of lifestyle and genetic factors on obesity-related traits in 302 healthy Ghanaian adults. Dietary intake and physical activity were assessed using a 3 day repeated 24 h dietary recall and global physical activity questionnaire, respectively. Twelve single nucleotide polymorphisms (SNPs) were used to construct 4-SNP, 8-SNP and 12-SNP genetic risk scores (GRSs). The 4-SNP GRS showed significant interactions with dietary fat intakes on waist circumference (WC) (Total fat, Pinteraction = 0.01; saturated fatty acids (SFA), Pinteraction = 0.02; polyunsaturated fatty acids (PUFA), Pinteraction = 0.01 and monounsaturated fatty acids (MUFA), Pinteraction = 0.01). Among individuals with higher intakes of total fat (>47 g/d), SFA (>14 g/d), PUFA (>16 g/d) and MUFA (>16 g/d), individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles. This is the first study of its kind in this population, suggesting that a higher consumption of dietary fatty acid may have the potential to increase the genetic susceptibility of becoming centrally obese. These results support the general dietary recommendations to decrease the intakes of total fat and SFA, to reduce the risk of obesity, particularly in individuals with a higher genetic predisposition to central obesity.
Keywords: genetic risk score, obesity, Ghana, GONG, fat intake, gene–diet interaction
1. Introduction
Obesity is a known risk factor for several health conditions, including type 2 diabetes, cardiovascular diseases, hypertension and cancer, and hence it is considered as an increasing public health problem worldwide, including in Africa [1,2]. Obesity prevalence varies widely between African countries with a range of 5.3% in Uganda to 30% in Nigeria and 45.7% in South Africa [2]. A recent systematic review has reported that nearly 43% of Ghanaian adults are either overweight or obese and that the prevalence of overweight and obesity was higher in women and urban dwellers [3]. While obesity is strongly affected by changes in environmental factors (such as dietary intake, sedentary lifestyle, and urbanization), the composition of the gut microbiome, the disruption of circadian rhythms, exposure to endocrine-disrupting chemicals and epigenetic modifications [4,5,6,7,8,9], it also has strong genetic determinants with a heritability rate from 40 to 70% [10,11]. Genome-wide association studies (GWAS) in European populations have revealed more than 100 loci to be associated with the body mass index (BMI) [12,13,14,15,16,17,18]. However, these genetic associations have not been consistently replicated in African populations [19,20,21,22,23], which could be attributed to differences in lifestyle and genetic architecture [24].
Given that single nucleotide polymorphisms (SNPs) have relatively small effect sizes on obesity, several studies have aggregated information from multiple-risk variants into a polygenic genetic risk score (GRS) [13,15,25,26,27,28,29]. Employing a combined risk allele score is an efficient and effective approach in maximising statistical power, decreasing the drawback of multiple testing, and widening the generalisable nature of genetic associations [25,27]. A study among a rural population of Gambia demonstrated a positive association between a GRS of 28 SNPs and BMI and adult weight, whereas no association was found with the single SNP analysis [30,31]. Although genetic research in Africans is increasing in numbers [22], only a few studies have examined the association of GRS with obesity in Africa [30,32,33], which highlights the need for further research in African populations.
Current evidence has shown that heritability estimates for obesity-related traits can be modified by lifestyle factors such as diet and physical activity. Several studies have reported significant GRS–diet interactions on obesity-related traits. Studies in European populations have shown that the genetic association with BMI was stronger with higher intakes of sugar-sweetened beverages (SSBs) and fried foods than among those with lower intakes [34,35]. Studies have also shown that genetic associations with BMI in Europeans can be modified by the levels of physical activity, television watching, and changes in sleep pattern [36,37]. In addition, higher adherence to healthy eating patterns have shown to reduce BMI in Europeans despite having increased genetic susceptibility to obesity [38]. Gene–lifestyle interaction studies have largely been conducted in populations of European ancestry, and the replication of these studies in African populations remains unknown [36,39]. Therefore, our study aimed to investigate the association of GRS with obesity-related traits and to examine whether lifestyle factors such as dietary intake and physical activity modified these associations in the Ghanaian population.
2. Methods
2.1. Study Population
The Genetics of Obesity and Nutrition in Ghana (GONG) study is a cross-sectional study that was conducted in the Oforikrom Municipality in Kumasi, Ashanti region, Ghana. The GONG study was conducted as part of the ongoing GeNuIne (Gene–Nutrient Interactions) Collaboration, the main objective of which is to investigate the effect of gene–nutrient interactions (nutrigenetics) on metabolic disease outcomes using population-based studies from various ethnic groups [40,41]. The Oforikrom Municipal Assembly is one of the five Municipal Assemblies carved out of the Kumasi Metropolitan Assembly. There are seventeen recognized communities in this Municipal Assembly, with an estimated total population of 360,254. Five communities (Ayeduase, Bomso, Ayigya, Oforikrom and Kotei) were randomly selected from the list of communities in the Oforikrom Municipal Assembly. In each community, a central point was located (a vehicle station, marketplace or other landmarks). A fieldworker entered the first house that faced either North, South, East or West of that central point, and randomly recruited one respondent from each household. Upon exiting a house, the fieldworker entered the next house, and the house-level selection process was repeated.
Three hundred and two free-living and healthy (with no physical complaints or prior diagnosis of cardiometabolic disease) adult volunteers, both men and women, were screened and recruited for the study by trained researchers. The inclusion criteria included the following: healthy individuals aged 25 to 60 years old and being Asante (both parents must be Asante). The exclusion criteria included the following: participants less than 25 years old or older than 60 years, those with existing cardiovascular complications or disease, those with a previous history of hypertension, type 2 diabetes or cardiovascular diseases, participants with any communicable or non-communicable chronic diseases, pregnant women and participants on lipid-lowering drugs, anti-diabetic drugs or anti-hypertensive drugs. A medical screening questionnaire was developed to screen participants for inclusion or exclusion from the study.
This study was approved by the Council for Scientific and Industrial Research (CSIR) Institutional Review Board (IRB) (Ref: RPN 003/CSIR-IRB/2018). In addition, this study was approved by the Metro Director of Health Services, Kumasi (KMHD/MPHs/13). All participants signed informed consent prior to their participation.
2.2. Data Collection
Structured questionnaires were used to elicit information about the participants’ demographic characteristics, dietary intakes, physical activity levels, sleep and sunshine exposure patterns and medical history. Fieldworkers were trained before the start of data collection. Survey instruments were also pre-tested on the 10 July 2018 to enhance the field workers’ understanding of questionnaires, ensure clearness and avoid ambiguity. Data collection took place from July to September 2018.
2.3. Anthropometric Measurements
Height, weight, percentage of body fat and visceral fat, waist circumference (WC) and hip circumference (HC) were measured. The measurements were taken with respondents wearing light clothing. Height was measured with a stadiometer (Seca 213 mobile stadiometer, Hamburg, Germany) to the nearest 0.1 cm with participants standing upright without shoes. Weight was measured using an OMRON Body Composition Analyzer to the nearest 0.1 kg. The same equipment provided values for BMI, percentage of body fat and visceral fat. WC and HC measurements were taken using a non-extensible measuring tape with participants in light clothing. The WC was measured just above the naval to the nearest 0.1 cm whereas the HC was measured at the level of the greater trochanter to the nearest 0.1 cm. The waist-to-hip ratio (WHR) was calculated by dividing WC by HC.
2.4. Physical Activity and Dietary Assessments
The health-related physical activity level of participants was measured using the interviewer-administered Global Physical Activity Questionnaire (GPAQ) version 2 developed by the World Health Organization (WHO) for physical activity surveillance [42]. This questionnaire contains 16 questions (P1–P16) which gather information on the respondent’s engagement in physical activities under three domains or settings (work-related activity, transportation and recreational activities) as well as sedentary behaviours. The total physical activity per week was calculated in Metabolic Equivalents (MET- minutes) and the respondents who had total physical activity ≥ 600 MET- minutes/week were classified as active while those who had < 600 MET- minutes/week were classified as inactive [42].
A three-day repeated (two weekdays and one weekend) 24 h dietary recall method was used to elicit the information concerning the participants’ dietary intake. Participants were requested to recollect all the meals taken as well as the times of the meal consumption in the previous day. Common household measures were used to estimate the actual quantities of foods and drinks consumed by the participants. The nutritional composition of the foods eaten was then analysed using the Nutrient Analysis Template (Food Science and Nutrition Department, University of Ghana, Accra, Ghana, 2010).
2.5. SNP Selection
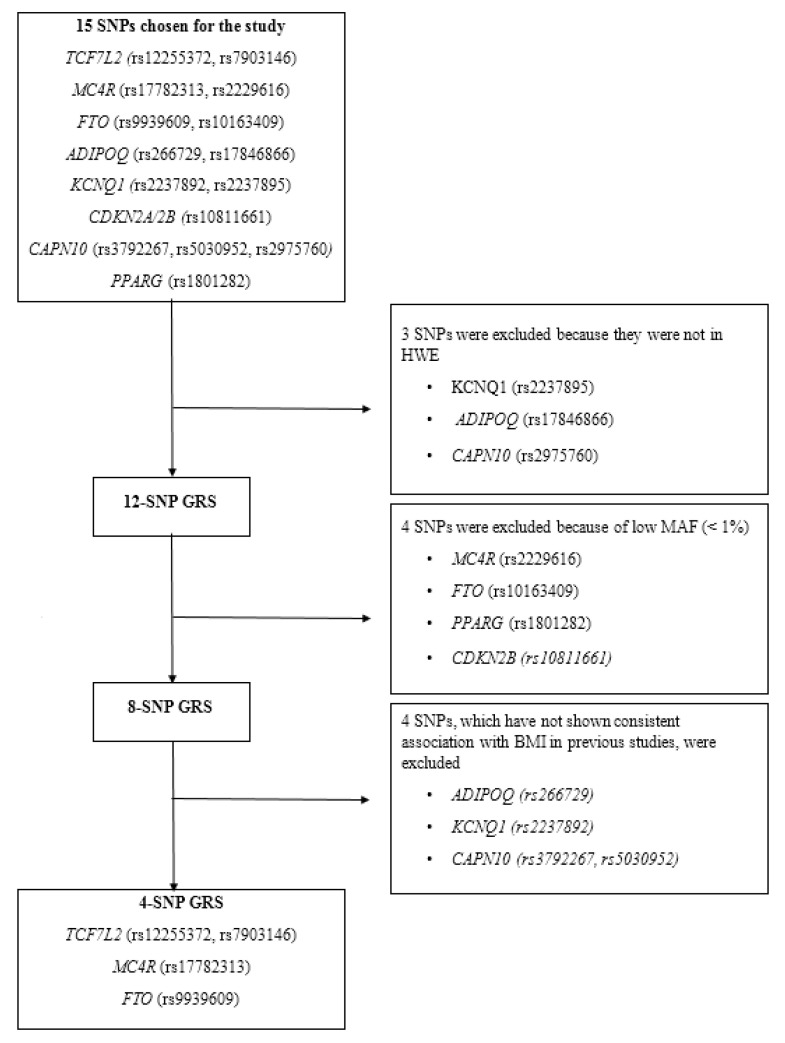
Fifteen SNPs near or in 8 obesity-susceptibility loci were chosen for the study based on the previous GWAS for metabolic traits [12,13,14,15,16,17,18]. These include Transcription factor 7-like 2 (TCF7L2) (rs12255372, rs7903146), melanocortin 4 Receptor (MC4R) (rs17782313, rs2229616), fat mass and obesity-associated (FTO) (rs9939609, rs10163409), adiponectin (ADIPOQ) (rs266729, rs17846866), Potassium voltage-gated channel subfamily Q member 1(KCNQ1) (rs2237892, rs2237895), Cyclin dependent kinase inhibitor 2A/2B (CDKN2A/2B) (rs10811661), Calpain 10 (CAPN10) (rs3792267, rs5030952, rs2975760) and Peroxisome proliferator-activated receptor gamma (PPARG) (rs1801282). Three of these SNPs, KCNQ1 (rs2237895), ADIPOQ (rs17846866) and CAPN10 (rs2975760), reported significant deviations from Hardy–Weinberg Equilibrium (HWE) (p < 0.05) and were excluded from the current analysis. The detailed information of the 15 SNPs is shown in Supplementary Table S1.
2.6. Genotyping
Blood samples for the measurement of DNA were transported in dry ice to the United Kingdom (UK). Genomic DNA was extracted from a 5 mL whole blood sample from each participant and genotyping was performed at the LGC Genomics (http://www.lgcgroup.com/services/genotyping), which employs the competitive allele-specific PCR-KASP® assay.
2.7. Construction of the Metabolic GRSs
To evaluate the combined effects of the 12 SNPs on obesity-related traits, an additive model was used to construct the unweighted metabolic GRSs (Figure 1). We did not weigh the risk alleles based on their individual effect sizes, because no previously reported effect sizes were available for these SNPs for the Ghanaian population, and it has been shown that the weighting of risk alleles may only have limited effects [43]. The unweighted metabolic GRSs were calculated by the summation of the number of risk alleles across the 12 variants. The risk alleles were defined as alleles previously associated with an increased risk of obesity in the literature. To reduce the bias caused by the missing data, only those participants without any missing data were included in our metabolic GRS analysis. Different metabolic GRSs were constructed including the 12-, 8- and the 4-SNP GRSs. The 12-SNP GRS included the following SNPs: TCF7L2 (rs12255372, rs7903146), MC4R (rs17782313, rs2229616), FTO (rs9939609, rs10163409), ADIPOQ (rs266729), KCNQ1 (rs2237892), CDKN2A/2B (rs10811661), CAPN10 (rs3792267, rs5030952) and PPARG (rs1801282), and the score ranged from 0 to 9 risk alleles. In the 12-SNP GRS analysis, no significant results were identified which might be because four of the SNPs had a minor allele frequency (MAF) of less than 5%. Therefore, we excluded the four SNPs: MC4R (rs2229616), FTO (rs10163409), CDKN2B (rs10811661) and PPAR (rs1801282) and created an 8-SNP GRS. No significant findings were observed using the 8-SNP GRS; this might be because four of the eight SNPs (ADIPOQ (rs266729), KCNQ1 (rs2237892) and CAPN10 (rs3792267, rs5030952)) have not shown consistent associations with obesity-related traits in other populations [44,45,46,47,48,49]. Hence, these four SNPs were removed and a 4-SNP GRS including the SNPs (TCF7L2 (rs12255372, rs7903146), MC4R (rs17782313), FTO (rs9939609)) that have shown consistent associations with obesity across several populations was constructed. The 4-SNP GRS ranged from 0 to 6 risk alleles and significant results were observed. Based on the median number of each GRS, the individuals were separated into two groups.
Figure 1.
Steps involved in the construction of the metabolic GRS. Fifteen SNPs were genotyped in our study; however, the GRS analysis was based only on 12 SNPs as 3 SNPs were not in the HWE. Three different GRSs, including the 12-SNP GRS, 8-SNP GRS and the 4-SNP GRS were constructed. In the 12-SNP GRS analysis, no significant results were identified, which could be because 4 of the SNPs had MAF of less than 5%. Therefore, the 4 SNPs were excluded, and an 8-SNP GRS was created. No significant findings were observed using the 8-SNP GRS; this could be because four of the eight SNPs have not shown a consistent association with obesity-related traits in other populations. Hence, these four SNPs were removed and a 4-SNP GRS including those SNPs that have shown consistent associations with obesity across several populations was constructed. Abbreviations: SNP: single nucleotide polymorphisms; GRS: genetic risk score; HWE: Hardy–Weinberg equilibrium; MAF: minor allele frequency.
Given that there were no previously reported effect sizes available for these SNPs for the Ghanaian population, we were unable to perform sample size calculation.
Data analyses were performed using Statistical Package for the Social Sciences (SPSS) software (version 24; SPSS Inc., Chicago, IL, USA). A natural log transformation was used for the non-normally distributed variables. Unadjusted differences of descriptive characteristics between the overweight/obese and non-obese participants were calculated using an independent samples t-test for continuous variables. General linear models were used to examine the association between the metabolic GRSs and obesity traits. GRS–lifestyle interactions were analysed by including the interaction terms in these models. Models were adjusted for covariates including sex, age and BMI (when BMI is not an outcome). Nutrient–GRS interaction analysis was additionally adjusted for total energy intake. All GRS–lifestyle interactions reaching a nominal level of significance (p < 0.05) were investigated further using binary analysis. Based on the median intake of total fat—saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and polyunsaturated fatty acids (PUFA)—the individuals were separated into two groups: ‘’below the median group’’ and ‘’above the median group”. Within each group, the association between the GRS and the outcome was examined. We also tested for GRS–sex interactions to test if sex influenced the genetic associations with obesity traits. The lifestyle factors investigated in our study included physical activity and the total dietary intake of fat, protein, carbohydrate and fibre. Significant interactions between the GRS and the total fat intake were further investigated to examine the influence of fat subtypes including saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and polyunsaturated fatty acids (PUFA). Two-tailed value of p < 0.05 was considered statistically significant.
3. Results
3.1. Characteristics of the Study Participants
The anthropometric and dietary characteristics of the study participants are presented in Table 1. The mean age and BMI of the total sample were 38.17 ± 9.64 years and 26.63 ± 4.99 kg/m2, respectively. Overweight/obese individuals were older than the non-obese (p < 0.05). Moreover, the dietary intakes were significantly different between the two groups. Overweight/obese individuals reported significantly lower intakes of total calories, protein, carbohydrate, total fat, fibre, SFA, MUFA and PUFA compared to the non-obese (p < 0.05). Women had significantly higher levels of BMI, body fat percentage and WHR compared to men, despite the men consuming significantly higher levels of carbohydrate, protein and fat (p < 0.05) (Supplementary Table S2).
Table 1.
Characteristics of the study participants.
| Total (N = 302) |
Non-Obese * (N = 126) |
Overweight/Obese ** (N = 176) |
p Value *** | |
|---|---|---|---|---|
| Age (years) | 38.17 ± 9.64 | 35.96 ± 9.55 | 39.75 ± 9.42 | 0.001 |
| BMI (kg/m2) | 26.63 ± 4.99 | 22.01 ± 1.79 | 29.95 ± 3.75 | <0.001 |
| WC (cm) | 88.48 ± 12.41 | 77.99 ± 7.13 | 96.00 ± 9.61 | <0.001 |
| WHR | 1.45 ± 6.96 | 1.55 ± 7.76 | 1.38 ± 6.34 | 0.84 |
| Visceral fat (%) | 8.02 ± 7.39 | 6.49 ± 10.97 | 9.12 ± 2.26 | 0.01 |
| Body fat (%) | 33.12 ± 13.90 | 22.05 ± 12.47 | 41.05 ± 8.36 | <0.001 |
| Total energy intake (%) | 1647.93 ± 685.83 | 1772.17 ± 723.85 | 1558.99 ± 644.75 | 0.008 |
| Protein intake (g/day) | 53.24 ± 23.73 | 57.38 ± 24.52 | 50.28 ± 22.76 | 0.01 |
| Total fat intake (g/day) | 51.17 ± 26.94 | 55.00 ± 29.29 | 48.42 ± 24.85 | 0.04 |
| Carbohydrates intake (g/day) | 239.03 ± 95.84 | 259.44 ± 104.01 | 224.42 ± 86.94 | 0.002 |
| Fibre intake (g/day) | 21.31 ± 10.84 | 23.19 ± 11.44 | 19.96 ± 10.21 | 0.01 |
| Total SFA intake (g/day) | 16.23 ± 10.36 | 17.41 ± 11.29 | 15.39 ± 9.58 | 0.10 |
| Total MUFA intake (g/day) | 18.08 ± 10.49 | 19.63 ± 11.30 | 16.96 ± 9.74 | 0.03 |
| Total PUFA intake (g/day) | 9.12 ± 5.03 | 10.20 ± 5.56 | 8.35 ± 4.47 | 0.002 |
Data presented as the means ± standard deviations. * Non-obese individuals refer to the individuals with a BMI < 25 Kg/m2, according to the WHO classification of BMI. ** Overweight/obese cases refer to individuals with BMI ≥ 25 Kg/m2, according to the WHO classification of BMI. *** p values for the differences in the means between the two groups were calculated using the independent samples t-test. Abbreviations: BMI: body mass index; WC: waist circumference; WHR: waist–hip ratio; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids; WHO: World Health Organisation.
3.2. Effect of Metabolic GRSs on Obesity-Related Traits
We first investigated the combined effect of 12 common SNPs on obesity-related traits and no significant associations were observed (Supplementary Table S3). Similar results were found using an 8-SNP GRS (Supplementary Table S4) and a 4-SNP GRS (Table 2).
Table 2.
Associations of the 4-SNP GRS on obesity-related traits.
| GRS < 3 Risk Alleles (N = 123) |
GRS ≥ 3 Risk Allele (N = 172) |
* p Value | |
|---|---|---|---|
| BMI (kg/m2) | 26.13 ± 0.45 | 26.85 ± 0.37 | 0.24 |
| WC (cm) | 87.13 ± 1.15 | 89.14 ± 0.92 | 0.19 |
| WHR | 2.27 ± 0.98 | 0.88 ± 0.01 | 0.18 |
| Visceral fat (%) | 7.89 ± 0.71 | 8.08 ± 0.55 | 0.43 |
| Body fat (%) | 31.75 ± 1.32 | 33.87 ± 1.02 | 0.15 |
* p Values obtained from the linear regression analysis adjusted for age, sex and additionally for BMI when BMI is not an outcome. The analysis was performed on log-transformed variables. Abbreviations: SNP: single nucleotide polymorphism; GRS: genetic risk score; BMI: body mass index; WC: waist circumference; WHR: waist–hip ratio.
3.3. GRS–Lifestyle Interactions on Obesity-Related Traits
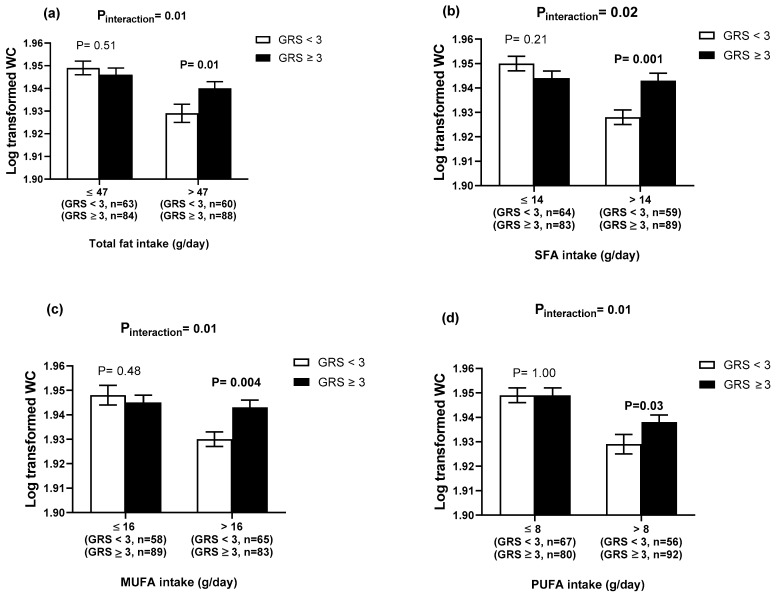
There was a significant interaction of the 4-SNP GRS with dietary fat intake (g/day) on WC (Total fat, Pinteraction = 0.01; SFA, Pinteraction = 0.02; PUFA, Pinteraction = 0.01 and MUFA, Pinteraction = 0.01, Table 3). Individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles, among individuals with higher intakes of total fat (>47 g/day), SFA (>14 g/day), PUFA (>16 g/day) and MUFA (>16 g/day), (Figure 2a–d). There was also a significant interaction between 4-SNP GRS and dietary fibre intake (g/day) on body fat percentage (Pinteraction = 0.04). Individuals with <3 risk alleles had a significantly lower body fat percentage compared to those with ≥3 risk alleles (p = 0.02), among individuals with a higher intake of fibre (>19 g/day). In addition, there was a significant interaction between the 4-SNP GRS and physical activity on WHR (Pinteraction = 0.002). However, the finding was not significant after stratifying them by physical activity levels. Some significant interactions were observed between the 12- and the 8-SNP GRSs and lifestyle factors on obesity-related traits (Supplementary Tables S5 and S6), however, none of these interactions were significant after binary analysis. Given the significant differences in the dietary intakes and obesity-related outcomes between men and women, interactions between the 4-SNP GRS and sex were tested but no significant results were found (Supplementary Table S7).
Table 3.
Interactions between the 4-SNP GRS and the lifestyle factors on obesity-related traits.
| Protein (g/day) | Carbohydrate (g/day) | Fibre (g/day) | Fat (g/day) | SFA (g/day) | MUFA (g/day) | PUFA (g/day) | Physical Activity | |
|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | 0.45 | 0.22 | 0.12 | 0.15 | - | - | - | 0.76 |
| WC (cm) | 0.08 | 0.21 | 0.41 | 0.01 | 0.02 | 0.01 | 0.01 | 0.24 |
| WHR | 0.82 | 0.88 | 0.49 | 0.80 | - | - | - | 0.002 |
| Visceral fat (%) | 0.50 | 0.35 | 0.32 | 0.38 | - | - | - | 0.93 |
| Body fat (%) | 0.46 | 0.11 | 0.04 | 0.75 | - | - | - | 0.60 |
Data are p values obtained from the linear regression analysis adjusted for age, sex, total energy intake and additionally for BMI when BMI is not an outcome. The analysis was performed on log-transformed variables. Abbreviations: SNP: single nucleotide polymorphism; GRS: genetic risk score; BMI: body mass index; WC: waist circumference; WHR: waist–hip ratio; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids.
Figure 2.
Interaction between the 4-SNP GRS and fat intake (g/day) on the log transformed WC. (a) Interaction between the 4-SNP GRS and the log transformed total fat intake (g/day) on WC. White bars indicate individuals with a GRS < 3 risk alleles; the black bars indicate individuals with GRS ≥ 3 risk alleles. Individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles, among individuals with a higher total fat intake (above median group > 47 g/day): 71.28 ± 23.68 g/day (34.99 ± 5.54 % TEI); (b) the interaction between the 4-SNP GRS and the log transformed SFA intake (g/day) on the log transformed WC. White bars indicate individuals with a GRS < 3 risk alleles; the black bars indicate individuals with GRS ≥ 3 risk alleles. Individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles, among individuals with a higher SFA intake: 23.50 ± 10.08 g/day (12.19 ± 3.21% TEI); (c) the interaction between the 4-SNP GRS and the log transformed MUFA intake (g/day) on the log transformed WC. White bars indicate individuals with a GRS < 3 risk alleles; the black bars indicate individuals with GRS ≥ 3 risk alleles. Individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles, among individuals with a higher MUFA intake: 25.72 ± 9.58 g/day (12.79 ± 2.53% TEI); (d) the interaction between the 4-SNP GRS and the log transformed PUFA intake (g/day) on the log transformed WC. White bars indicate individuals with a GRS < 3 risk alleles; the black bars indicate individuals with GRS ≥ 3 risk alleles. Individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles, among individuals with a higher PUFA intake: 12.74 ± 4.7 g/day (6.28 ± 1.08% TEI). Abbreviations: SNP: single nucleotide polymorphisms; GRS: genetic risk score; WC: waist circumference; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids; TEI: total energy intake. Error bars indicate the standard error of the mean.
4. Discussion
To our knowledge, this is the first nutrigenetic study investigating the interaction between metabolic GRSs and lifestyle factors on obesity-related traits in a Ghanaian population. Our study provides evidence for an interaction between the 4-SNP GRS and fat intake on WC, where individuals with ≥3 risk alleles had a significantly higher WC compared to those with <3 risk alleles among those who consumed a diet high in total fat, SFA, MUFA and PUFA. These results are in accordance with the general dietary recommendations, which suggest that the population decrease their intakes of total fat and SFA, to reduce the risk of obesity, and this will be more applicable in individuals with a higher genetic predisposition to obesity. Our findings are of importance to public health, considering the high consumption of foods that are rich in SFA and MUFA in the Ghanaian population [50].
Our study is the first study of its kind, investigating the effect of different metabolic GRSs (the 12-, 8- and the 4-SNP GRS) on obesity-related traits in a Ghanaian population. We found that none of the metabolic GRSs were significantly associated with obesity-related traits in the Ghanaian population, which contradicts the findings of the previous GRS-related studies in European and African populations [15,25,26,27,28,29,30,32,33]. Efforts to replicate previously reported genetic associations of individual SNPs with obesity measures in non-African populations have shown limited success among Africans [23,31,51,52], which is also in line with the findings from the present study. Several factors are likely to be involved in such discrepancies between our findings and genetic association studies in Europeans. First, the metabolic GRS in the present study was constructed based on variants strongly associated with BMI in European populations, which raises the question of the usefulness, applicability and accuracy of using this metabolic GRS in our African population. Analysing the genetic associations of such variants with obesity-related traits in African population may not be ideal because of differences in risk allele frequency and effect size across populations [53,54]. Second, the ‘lead’ SNPs identified in Europeans might tag smaller regions in Africans [19,20,55] and the ‘true’ causal polymorphisms might be at different loci [56]. A systematic review of genetic research in African samples has reported that more than 300 SNPs in 42 loci analysed in relation to obesity, but only a few positive associations were replicable in Africans [57]. Of the 36 variants previously established by GWAS in non-African populations, only the SNPs located at the FTO and MC4R loci were significantly associated with obesity in Nigerians, Ghanaians and black South Africans [58,59]. Furthermore, in a large-scale GWAS meta-analysis consisting of 71,412 individuals of African ancestry, of the 36 previously identified BMI-associated SNPs in Europeans, only five variants reached a genome-wide significant level in Africans [60]. Such inconsistencies in results are likely due, in part, to the variation in the genetic architecture between populations of different ancestry [61]. African populations are characterised by greater genetic variation, reduced patterns of linkage disequilibrium (LD) and more haplotype diversity in comparison with populations of another ancestry, which may cause difficulties in replicating previously reported genetic associations [61]. Hence, future studies with a larger sample size are needed to investigate the combined effect of a larger number of genetic variants on obesity-related traits in the Ghanaian population.
Our study has identified significant interactions between the 4-SNP GRS and intakes of total fat, SFA, PUFA and MUFA on WC, an indicator of central obesity that has been associated with the increased risk of morbidity and mortality [62,63]. Our findings suggest that dietary fatty acid consumption and composition may have the potential to influence the genetic susceptibility of becoming centrally obese. Evidence is limited concerning the GRS–diet interactions on obesity and its related traits, and most of the research has focused on the influence of a single locus [64,65,66], despite the genetic effects on obesity being polygenic [13]. Our results are consistent with previous findings generated from single-locus gene–diet interactions on obesity, in which fat intake is considered as an important lifestyle modulator of genetic associations with obesity-related traits. Two previous studies in 2163 participants from two independent United States (US) populations and in 28,449 individuals living in Malmö have shown significant interactions of the FTO SNP rs9939609 with total dietary fat on BMI [64,67], however, a large-scale meta-analysis of 177,330 individuals (154,439 Whites, 5776 African Americans and 17,115 Asians) failed to identify this interaction [68]. In addition, studies in 2163 participants from two US populations, 1754 French individuals and 354 Spanish children and adolescents have demonstrated a significant interaction of FTO SNP rs9939609 with SFAs [64,65,66] and MUFAs [64] on BMI. Furthermore, a study in 305 obese individuals in Finland reported that the high intake of MUFA was associated with weight loss among carriers of the risk allele (A) FTO rs9939609 [69]. Additionally, a study in 1680 South Asians has shown a significant interaction of the risk allele ‘T’ of the TCF7L2 SNP rs12255372 with fat intake on high-density lipoprotein cholesterol (HDL-C) [70]. Studies on GRS–diet interactions on obesity traits have mainly focused on European populations [71,72,73]. In agreement with our study, data from UK Biobank [72] and two studies from the US [71] have reported significant interactions between the GRS and dietary intakes of total fat and SFA on WC; the GRS was associated with a higher WC among individuals with high intakes of total fat and SFA. However, the interactions on BMI were not identified in the present study, which contradicts the previously reported findings [71,72]. Hence, larger studies are required to replicate our GRS–fat intake interactions on WC in the Ghanaian population.
Several studies have investigated the impact of dietary fat on obesity measures; however, the findings have been inconsistent [74]. For instance, prospective studies have examined the relationship between the intake of long-chain omega-3 (LC n−3)-PUFAs and adiposity, but results have been inconsistent. A study in 124 adults living in the UK found that the plasma levels of n-3 PUFA were negatively associated with anthropometric measures of obesity [75], whereas positive associations were reported in a study of 79,839 women living in the US [76]. However, no effect of n-3 LC-PUFA consumption on BMI was found in a 12 year follow-up US cohort of 43,671 men [77]. In a randomised controlled trial (RCT) of 27 women, the intake of a 3 g/d of fish oil (1.8 g n−3 PUFAs) for 2 months was associated with adiposity reduction [78]. Similar findings were reported in an RCT of 324 men and women from Iceland, Spain and Ireland, in which the intake of either lean fish (3 × 150 g portions of cod/week) or fatty fish (3 × 150 g portions of salmon/week), or fish oil (docosahexaenoic acid/eicosapentaenoic acid capsules) for 8 weeks were associated with weight loss in men [79]. However, a 6 week RCT in 195 UK adults found no differences in the anthropometric measures between three intervention diets of specific fatty acid compositions of total energy intake (TEI) (%TEI SFA:%TEI MUFA:%TEI omega-6 PUFA): SFA-rich diet (17:11:4), MUFA-rich diet (9:19:4) or omega-6 PUFA-rich diet (9:13:10) [80]. A meta-analysis of 534,906 European individuals revealed that the higher adherence to the Mediterranean diet, which is rich in MUFA, was associated with a beneficial effect on WC [81]. However, a recent 4 week intervention found no significant effect of the intake of 50 g/day of olive oil, which is rich in MUFA, on BMI or central obesity in 91 UK adults [82]. Conflicting evidence exists regarding the effects of dietary fat on obesity-related traits; this could be because of the genetic heterogeneity and the gene–diet interactions that vary across multiple ethnic groups [83]; hence, the influence of both genetic and lifestyle factors should be considered in understanding the pathophysiology of obesity.
In 2018, the WHO recommended that the intake of total fat and SFA should not exceed 30% and 10% of TEI, respectively, to avoid weight gain [84]. According to the WHO, the recommended range for PUFA for the general population is 6–11% of TEI [85]. It has been identified that the average consumption of SFA in Africa is between 8.9% and 12.5% TEI (North: 9.1%, Central: 12.2, Eastern: 10.7%, Southern: 8.9% and Western Africa: 12.5%; which is slightly higher than the ≤10% TEI recommended by the WHO). The intake of PUFA is low in many sub-Saharan African countries, suggesting the infrequent use of vegetable oils for cooking or preparing foods [86]. The extremely low intake of n-3 long chain PUFA was also identified in Africa, which is explained by the low availability of fish in sub-Saharan Africa countries [86]. In the present study, the average consumption of total fat intake was 23.04 ± 9.13% of TEI and the average consumption of SFA, MUFA and PUFA were 8.95 ± 4.10, 9.86 ± 3.65 and 4.99 ± 1.61% of TEI, respectively, which are in accordance with general dietary recommendations. However, nearly one third of the study population had a high consumption of total fat (mean intake: 34.99 ± 5.54 g/day), the group in which the GRS showed a significant association with a higher WC. Hence, our study suggests that following the general dietary recommendations might be an effective way to overcome the genetic susceptibility to central obesity.
The strengths of our study include the analysis of gene–lifestyle interactions in a well characterized Ghanaian population and the use of different metabolic GRSs to maximise statistical power and to reduce multiple testing [25,27]. Nevertheless, some limitations need to be acknowledged. First, our analysis included an only Ghanaian population, which limits the generalisability of our results to other population groups within Africa. Second, our metabolic GRSs were constructed based on BMI-associated loci predominantly identified in Europeans, which might not truly reflect the genetic associations with BMI among Africans. Third, the food intakes were assessed using repeated 24 h dietary recall method, which is prone to reporting bias and this might have contributed to the discrepancy in the caloric consumption between overweight/obese and non-obese groups [87]. Fourth, as with any cross-sectional study design, residual confounding might exist, despite adjustments for several confounding factors. Fifth, our sample size was small; however, our study had sufficient statistical power to detect significant gene–diet interactions.
5. Conclusions
In conclusion, our study has shown that higher intakes of total fat, SFA, MUFA and PUFA can increase the genetic risk on WC in Ghanaian adults. We found that the effect of metabolic risk alleles on WC is stronger among individuals with higher intakes of total fat, SFA, MUFA, PUFA. These results give important insights into the complex interactions between dietary intake and the genetic predisposition to central obesity and highlight the importance of personalising dietary advice according to each ethnic group. Our GRS approach provides insights into cumulative genetic susceptibility; however, studies with a large sample size will be needed to confirm the findings before public health recommendations and personalized nutrition advice can be developed for the Ghanaian population.
Acknowledgments
We thank all the participants from the GONG study for their cooperation. Karani S Vimaleswaran acknowledges support from the Ministry of Higher Education of Saudi Arabia for the scholarship given to Sooad Alsulami.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/12/7/1906/s1. Table S1: Genotype distribution of the fifteen SNPs that were included in the metabolic GRS; Table S2: Characteristics of the study participants stratified based on sex; Table S3: Associations of the 12-SNP GRS with obesity-related traits; Table S4: Associations of the 8-SNP GRS with obesity-related traits; Table S5: Interactions between the 12-SNP GRS and lifestyle factors on obesity-related traits’ Table S6: Interactions between the 8-SNP GRS and lifestyle factors on obesity-related traits; Table S7: Interactions between the 4-SNP GRS and sex on obesity-related traits.
Author Contributions
Conceptualization, K.S.V.; methodology, K.S.V. and S.A.; software, S.A., D.A.N. and A.-M.B.; validation, D.A.N. and A.-M.B.; formal analysis, S.A. and K.D.; investigation, S.A., R.A.A.; resources, K.S.V., R.A.A. and B.E.; data curation, K.S.V., S.A. and R.A.A.; writing—original draft preparation, S.A. and K.S.V.; writing—review and editing, K.S.V., S.A., D.A.N., J.A.L., R.A.A., and B.E.; supervision, K.S.V.; project training and administration, K.S.V., R.A.A., and B.E.; funding acquisition, K.S.V. and B.E. All authors have read, edited and approved the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Research England Global Challenge Research Fund Institutional allocation (University of Reading and University of Chester).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Kelly T., Yang W., Chen C.S., Reynolds K., He J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. (Lond.) 2008;32:1431–1437. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 2.Ng M., Fleming T., Robinson M., Thomson B., Graetz N., Margono C., Mullany E.C., Biryukov S., Abbafati C., Abera S.F., et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ofori-Asenso R., Agyeman A.A., Laar A., Boateng D. Overweight and obesity epidemic in Ghana-a systematic review and meta-analysis. BMC Public Health. 2016;16:1239. doi: 10.1186/s12889-016-3901-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicolaidis S. Environment and obesity. Metabolism. 2019;100s:153942. doi: 10.1016/j.metabol.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Tilg H., Kaser A. Gut microbiome, obesity, and metabolic dysfunction. J. Clin. Investig. 2011;121:2126–2132. doi: 10.1172/JCI58109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Froy O. Metabolism and circadian rhythms--implications for obesity. Endocr. Rev. 2010;31:1–24. doi: 10.1210/er.2009-0014. [DOI] [PubMed] [Google Scholar]
- 7.Egusquiza R.J., Blumberg B. Environmental Obesogens and Their Impact on Susceptibility to Obesity: New Mechanisms and Chemicals. Endocrinology. 2020;161 doi: 10.1210/endocr/bqaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herrera B.M., Keildson S., Lindgren C.M. Genetics and epigenetics of obesity. Maturitas. 2011;69:41–49. doi: 10.1016/j.maturitas.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsanathan R., Jain S.K. Glutathione deficiency induces epigenetic alterations of vitamin D metabolism genes in the livers of high-fat diet-fed obese mice. Sci. Rep. 2019;9:14784. doi: 10.1038/s41598-019-51377-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodarzi M.O. Genetics of obesity: What genetic association studies have taught us about the biology of obesity and its complications. Lancet Diabet. Endocrinol. 2018;6:223–236. doi: 10.1016/S2213-8587(17)30200-0. [DOI] [PubMed] [Google Scholar]
- 11.Owen J.B. Genetic aspects of body composition. Nutrition. 1999;15:609–613. doi: 10.1016/S0899-9007(99)00097-0. [DOI] [PubMed] [Google Scholar]
- 12.Berndt S.I., Gustafsson S., Magi R., Ganna A., Wheeler E., Feitosa M.F., Justice A.E., Monda K.L., Croteau-Chonka D.C., Day F.R., et al. Genome-wide meta-analysis identifies 11 new loci for anthropometric traits and provides insights into genetic architecture. Nat. Genet. 2013;45:501–512. doi: 10.1038/ng.2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Locke A.E., Kahali B., Berndt S.I., Justice A.E., Pers T.H., Day F.R., Powell C., Vedantam S., Buchkovich M.L., Yang J., et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okada Y., Kubo M., Ohmiya H., Takahashi A., Kumasaka N., Hosono N., Maeda S., Wen W., Dorajoo R., Go M.J., et al. Common variants at CDKAL1 and KLF9 are associated with body mass index in east Asian populations. Nat. Genet. 2012;44:302–306. doi: 10.1038/ng.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Speliotes E.K., Willer C.J., Berndt S.I., Monda K.L., Thorleifsson G., Jackson A.U., Lango Allen H., Lindgren C.M., Luan J., Magi R., et al. Association analyses of 249,796 individuals reveal 18 new loci associated with body mass index. Nat. Genet. 2010;42:937–948. doi: 10.1038/ng.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wen W., Cho Y.S., Zheng W., Dorajoo R., Kato N., Qi L., Chen C.H., Delahanty R.J., Okada Y., Tabara Y., et al. Meta-analysis identifies common variants associated with body mass index in east Asians. Nat. Genet. 2012;44:307–311. doi: 10.1038/ng.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willer C.J., Li Y., Abecasis G.R. METAL: Fast and efficient meta-analysis of genomewide association scans. Bioinformatics. 2010;26:2190–2191. doi: 10.1093/bioinformatics/btq340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winkler T.W., Justice A.E., Graff M., Barata L., Feitosa M.F., Chu S., Czajkowski J., Esko T., Fall T., Kilpelainen T.O., et al. Correction: The Influence of Age and Sex on Genetic Associations with Adult Body Size and Shape: A Large-Scale Genome-Wide Interaction Study. PLoS Genet. 2016;12:e1006166. doi: 10.1371/journal.pgen.1006166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fesinmeyer M.D., North K.E., Ritchie M.D., Lim U., Franceschini N., Wilkens L.R., Gross M.D., Buzkova P., Glenn K., Quibrera P.M., et al. Genetic risk factors for BMI and obesity in an ethnically diverse population: Results from the population architecture using genomics and epidemiology (PAGE) study. Obesity (Silver Spring) 2013;21:835–846. doi: 10.1002/oby.20268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hester J.M., Wing M.R., Li J., Palmer N.D., Xu J., Hicks P.J., Roh B.H., Norris J.M., Wagenknecht L.E., Langefeld C.D., et al. Implication of European-derived adiposity loci in African Americans. Int. J. Obes. (Lond.) 2012;36:465–473. doi: 10.1038/ijo.2011.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rotimi C., Abayomi A., Abimiku A., Adabayeri V.M., Adebamowo C., Adebiyi E., Ademola A.D., Adeyemo A., Adu D., Affolabi D., et al. Research capacity. Enabling the genomic revolution in Africa. Science. 2014;344:1346–1348. doi: 10.1126/science.1251546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rotimi C.N., Bentley A.R., Doumatey A.P., Chen G., Shriner D., Adeyemo A. The genomic landscape of African populations in health and disease. Hum. Mol. Genet. 2017;26:225–236. doi: 10.1093/hmg/ddx253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adeyemo A., Chen G., Zhou J., Shriner D., Doumatey A., Huang H., Rotimi C. FTO genetic variation and association with obesity in West Africans and African Americans. Diabetes. 2010;59:1549–1554. doi: 10.2337/db09-1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vimaleswaran K.S., Loos R.J. Progress in the genetics of common obesity and type 2 diabetes. Expert Rev. Mol. Med. 2010;12:e7. doi: 10.1017/S1462399410001389. [DOI] [PubMed] [Google Scholar]
- 25.Belsky D.W., Moffitt T.E., Sugden K., Williams B., Houts R., McCarthy J., Caspi A. Development and evaluation of a genetic risk score for obesity. Biodemogr. Soc. Biol. 2013;59:85–100. doi: 10.1080/19485565.2013.774628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hung C.F., Breen G., Czamara D., Corre T., Wolf C., Kloiber S., Bergmann S., Craddock N., Gill M., Holsboer F., et al. A genetic risk score combining 32 SNPs is associated with body mass index and improves obesity prediction in people with major depressive disorder. BMC Med. 2015;13:86. doi: 10.1186/s12916-015-0334-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li S., Zhao J.H., Luan J., Luben R.N., Rodwell S.A., Khaw K.T., Ong K.K., Wareham N.J., Loos R.J. Cumulative effects and predictive value of common obesity-susceptibility variants identified by genome-wide association studies. Am. J. Clin. Nutr. 2010;91:184–190. doi: 10.3945/ajcn.2009.28403. [DOI] [PubMed] [Google Scholar]
- 28.Peterson R.E., Maes H.H., Holmans P., Sanders A.R., Levinson D.F., Shi J., Kendler K.S., Gejman P.V., Webb B.T. Genetic risk sum score comprised of common polygenic variation is associated with body mass index. Hum. Genet. 2011;129:221–230. doi: 10.1007/s00439-010-0917-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sandholt C.H., Sparso T., Grarup N., Albrechtsen A., Almind K., Hansen L., Toft U., Jorgensen T., Hansen T., Pedersen O. Combined analyses of 20 common obesity susceptibility variants. Diabetes. 2010;59:1667–1673. doi: 10.2337/db09-1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fulford A.J., Ong K.K., Elks C.E., Prentice A.M., Hennig B.J. Progressive influence of body mass index-associated genetic markers in rural Gambians. J. Med. Genet. 2015;52:375–380. doi: 10.1136/jmedgenet-2014-102784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hennig B.J., Fulford A.J., Sirugo G., Rayco-Solon P., Hattersley A.T., Frayling T.M., Prentice A.M. FTO gene variation and measures of body mass in an African population. BMC Med. Genet. 2009;10:21. doi: 10.1186/1471-2350-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badsi M.N., Mediene-Benchekor S., Ouhaibi-Djellouli H., Lardjam-Hetraf S.A., Boulenouar H., Meroufel D.N., Hermant X., Hamani-Medjaoui I., Saidi-Mehtar N., Amouyel P., et al. Combined effect of established BMI loci on obesity-related traits in an Algerian population sample. BMC Genet. 2014;15:128. doi: 10.1186/s12863-014-0128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Munthali R.J., Sahibdeen V., Kagura J., Hendry L.M., Norris S.A., Ong K.K., Day F.R., Lombard Z. Genetic risk score for adult body mass index associations with childhood and adolescent weight gain in an African population. Genes Nutr. 2018;13:24. doi: 10.1186/s12263-018-0613-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qi Q., Chu A.Y., Kang J.H., Huang J., Rose L.M., Jensen M.K., Liang L., Curhan G.C., Pasquale L.R., Wiggs J.L., et al. Fried food consumption, genetic risk, and body mass index: Gene-diet interaction analysis in three US cohort studies. BMJ. 2014;348:g1610. doi: 10.1136/bmj.g1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qi Q., Chu A.Y., Kang J.H., Jensen M.K., Curhan G.C., Pasquale L.R., Ridker P.M., Hunter D.J., Willett W.C., Rimm E.B., et al. Sugar-sweetened beverages and genetic risk of obesity. N. Engl. J. Med. 2012;367:1387–1396. doi: 10.1056/NEJMoa1203039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qi Q., Li Y., Chomistek A.K., Kang J.H., Curhan G.C., Pasquale L.R., Willett W.C., Rimm E.B., Hu F.B., Qi L. Television watching, leisure time physical activity, and the genetic predisposition in relation to body mass index in women and men. Circulation. 2012;126:1821–1827. doi: 10.1161/CIRCULATIONAHA.112.098061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li S., Zhao J.H., Luan J., Ekelund U., Luben R.N., Khaw K.T., Wareham N.J., Loos R.J. Physical activity attenuates the genetic predisposition to obesity in 20,000 men and women from EPIC-Norfolk prospective population study. PLoS Med. 2010;7:e1000332. doi: 10.1371/journal.pmed.1000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang T., Heianza Y., Sun D., Huang T., Ma W., Rimm E.B., Manson J.E., Hu F.B., Willett W., Qi L. Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: Gene-diet interaction analysis in two prospective cohort studies. BMJ. 2018;360:693. doi: 10.1136/bmj.j5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kilpelainen T.O., Qi L., Brage S., Sharp S.J., Sonestedt E., Demerath E., Ahmad T., Mora S., Kaakinen M., Sandholt C.H., et al. Physical activity attenuates the influence of FTO variants on obesity risk: A meta-analysis of 218,166 adults and 19,268 children. PLoS Med. 2011;8:e1001116. doi: 10.1371/journal.pmed.1001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vimaleswaran K.S. Gene–nutrient interactions on metabolic diseases: Findings from the GeNuIne collaboration. Nutr. Bull. 2017;42:80–86. doi: 10.1111/nbu.12252. [DOI] [Google Scholar]
- 41.Vimaleswaran K.S. A nutrigenetics approach to study the impact of genetic and lifestyle factors on cardiometabolic traits in various ethnic groups: Findings from the GeNuIne Collaboration. Proc. Nutr. Soc. 2020;79:194–204. doi: 10.1017/S0029665119001186. [DOI] [PubMed] [Google Scholar]
- 42.Global Physical Activity Surveillance. [(accessed on 19 March 2020)]; Available online: https://www.who.int/ncds/surveillance/steps/GPAQ/en/
- 43.Janssens A.C., Moonesinghe R., Yang Q., Steyerberg E.W., van Duijn C.M., Khoury M.J. The impact of genotype frequencies on the clinical validity of genomic profiling for predicting common chronic diseases. Genet. Med. 2007;9:528–535. doi: 10.1097/GIM.0b013e31812eece0. [DOI] [PubMed] [Google Scholar]
- 44.Bazzi M.D., Nasr F.A., Alanazi M.S., Alamri A., Turjoman A.A., Moustafa A.S., Alfadda A.A., Pathan A.A., Parine N.R. Association between FTO, MC4R, SLC30A8, and KCNQ1 gene variants and type 2 diabetes in Saudi population. Genet. Mol. Res. 2014;13:10194–10203. doi: 10.4238/2014.December.4.14. [DOI] [PubMed] [Google Scholar]
- 45.Holmkvist J., Banasik K., Andersen G., Unoki H., Jensen T.S., Pisinger C., Borch-Johnsen K., Sandbaek A., Lauritzen T., Brunak S., et al. The type 2 diabetes associated minor allele of rs2237895 KCNQ1 associates with reduced insulin release following an oral glucose load. PLoS ONE. 2009;4:e5872. doi: 10.1371/journal.pone.0005872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hsiao T.J., Lin E. A Validation Study of Adiponectin rs266729 Gene Variant with Type 2 Diabetes, Obesity, and Metabolic Phenotypes in a Taiwanese Population. Biochem. Genet. 2016;54:830–841. doi: 10.1007/s10528-016-9760-y. [DOI] [PubMed] [Google Scholar]
- 47.Kommoju U.J., Maruda J., Kadarkarai Samy S., Irgam K., Kotla J.P., Reddy B.M. Association of IRS1, CAPN10, and PPARG gene polymorphisms with type 2 diabetes mellitus in the high-risk population of Hyderabad, India. J. Diabetes. 2014;6:564–573. doi: 10.1111/1753-0407.12142. [DOI] [PubMed] [Google Scholar]
- 48.Lu J.F., Zhou Y., Huang G.H., Jiang H.X., Hu B.L., Qin S.Y. Association of ADIPOQ polymorphisms with obesity risk: A meta-analysis. Hum. Immunol. 2014;75:1062–1068. doi: 10.1016/j.humimm.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 49.Martinez-Gomez L.E., Cruz M., Martinez-Nava G.A., Madrid-Marina V., Parra E., Garcia-Mena J., Espinoza-Rojo M., Estrada-Velasco B.I., Piza-Roman L.F., Aguilera P., et al. A replication study of the IRS1, CAPN10, TCF7L2, and PPARG gene polymorphisms associated with type 2 diabetes in two different populations of Mexico. Ann. Hum. Genet. 2011;75:612–620. doi: 10.1111/j.1469-1809.2011.00668.x. [DOI] [PubMed] [Google Scholar]
- 50.Galbete C., Nicolaou M., Meeks K.A., de-Graft Aikins A., Addo J., Amoah S.K., Smeeth L., Owusu-Dabo E., Klipstein-Grobusch K., Bahendeka S., et al. Food consumption, nutrient intake, and dietary patterns in Ghanaian migrants in Europe and their compatriots in Ghana. Food Nutr. Res. 2017;61:1341809. doi: 10.1080/16546628.2017.1341809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Logan M., Van der Merwe M.T., Dodgen T.M., Myburgh R., Eloff A., Alessandrini M., Pepper M.S. Allelic variants of the Melanocortin 4 receptor (MC4R) gene in a South African study group. Mol. Genet. Genom. Med. 2016;4:68–76. doi: 10.1002/mgg3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sahibdeen V., Crowther N.J., Soodyall H., Hendry L.M., Munthali R.J., Hazelhurst S., Choudhury A., Norris S.A., Ramsay M., Lombard Z. Genetic variants in SEC16B are associated with body composition in black South Africans. Nutr. Diabetes. 2018;8:43. doi: 10.1038/s41387-018-0050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adeyemo A.A., Tekola-Ayele F., Doumatey A.P., Bentley A.R., Chen G., Huang H., Zhou J., Shriner D., Fasanmade O., Okafor G., et al. Evaluation of Genome Wide Association Study Associated Type 2 Diabetes Susceptibility Loci in Sub Saharan Africans. Front. Genet. 2015;6:335. doi: 10.3389/fgene.2015.00335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen J., Sun M., Adeyemo A., Pirie F., Carstensen T., Pomilla C., Doumatey A.P., Chen G., Young E.H., Sandhu M., et al. Genome-wide association study of type 2 diabetes in Africa. Diabetologia. 2019;62:1204–1211. doi: 10.1007/s00125-019-4880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gong J., Schumacher F., Lim U., Hindorff L.A., Haessler J., Buyske S., Carlson C.S., Rosse S., Buzkova P., Fornage M., et al. Fine Mapping and Identification of BMI Loci in African Americans. Am. J. Hum. Genet. 2013;93:661–671. doi: 10.1016/j.ajhg.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shriner D., Adeyemo A., Gerry N.P., Herbert A., Chen G., Doumatey A., Huang H., Zhou J., Christman M.F., Rotimi C.N. Transferability and fine-mapping of genome-wide associated loci for adult height across human populations. PLoS ONE. 2009;4:e8398. doi: 10.1371/journal.pone.0008398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yako Y.Y., Echouffo-Tcheugui J.B., Balti E.V., Matsha T.E., Sobngwi E., Erasmus R.T., Kengne A.P. Genetic association studies of obesity in Africa: A systematic review. Obes. Rev. 2015;16:259–272. doi: 10.1111/obr.12260. [DOI] [PubMed] [Google Scholar]
- 58.Chen G., Doumatey A.P., Zhou J., Lei L., Bentley A.R., Tekola-Ayele F., Adebamowo S.N., Baker J.L., Fasanmade O., Okafor G., et al. Genome-wide analysis identifies an african-specific variant in SEMA4D associated with body mass index. Obesity (Silver Spring) 2017;25:794–800. doi: 10.1002/oby.21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yako Y.Y., Madubedube J.H., Kengne A.P., Erasmus R.T., Pillay T.S., Matsha T.E. Contribution of ENPP1, TCF7L2, and FTO polymorphisms to type 2 diabetes in mixed ancestry ethnic population of South Africa. Afr. Health Sci. 2015;15:1149–1160. doi: 10.4314/ahs.v15i4.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Monda K.L., Chen G.K., Taylor K.C., Palmer C., Edwards T.L., Lange L.A., Ng M.C., Adeyemo A.A., Allison M.A., Bielak L.F., et al. A meta-analysis identifies new loci associated with body mass index in individuals of African ancestry. Nat. Genet. 2013;45:690–696. doi: 10.1038/ng.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Campbell M.C., Tishkoff S.A. African genetic diversity: Implications for human demographic history, modern human origins, and complex disease mapping. Annu. Rev. Genom. Hum. Genet. 2008;9:403–433. doi: 10.1146/annurev.genom.9.081307.164258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schleinitz D., Bottcher Y., Bluher M., Kovacs P. The genetics of fat distribution. Diabetologia. 2014;57:1276–1286. doi: 10.1007/s00125-014-3214-z. [DOI] [PubMed] [Google Scholar]
- 63.Wang Y., Rimm E.B., Stampfer M.J., Willett W.C., Hu F.B. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am. J. Clin. Nutr. 2005;81:555–563. doi: 10.1093/ajcn/81.3.555. [DOI] [PubMed] [Google Scholar]
- 64.Corella D., Arnett D.K., Tucker K.L., Kabagambe E.K., Tsai M., Parnell L.D., Lai C.Q., Lee Y.C., Warodomwichit D., Hopkins P.N., et al. A high intake of saturated fatty acids strengthens the association between the fat mass and obesity-associated gene and BMI. J. Nutr. 2011;141:2219–2225. doi: 10.3945/jn.111.143826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Phillips C.M., Kesse-Guyot E., McManus R., Hercberg S., Lairon D., Planells R., Roche H.M. High dietary saturated fat intake accentuates obesity risk associated with the fat mass and obesity-associated gene in adults. J. Nutr. 2012;142:824–831. doi: 10.3945/jn.111.153460. [DOI] [PubMed] [Google Scholar]
- 66.Moleres A., Ochoa M.C., Rendo-Urteaga T., Martinez-Gonzalez M.A., Azcona San Julian M.C., Martinez J.A., Marti A. Dietary fatty acid distribution modifies obesity risk linked to the rs9939609 polymorphism of the fat mass and obesity-associated gene in a Spanish case-control study of children. Br. J. Nutr. 2012;107:533–538. doi: 10.1017/S0007114511003424. [DOI] [PubMed] [Google Scholar]
- 67.Sonestedt E., Roos C., Gullberg B., Ericson U., Wirfalt E., Orho-Melander M. Fat and carbohydrate intake modify the association between genetic variation in the FTO genotype and obesity. Am. J. Clin. Nutr. 2009;90:1418–1425. doi: 10.3945/ajcn.2009.27958. [DOI] [PubMed] [Google Scholar]
- 68.Qi Q., Kilpelainen T.O., Downer M.K., Tanaka T., Smith C.E., Sluijs I., Sonestedt E., Chu A.Y., Renstrom F., Lin X., et al. FTO genetic variants, dietary intake and body mass index: Insights from 177,330 individuals. Hum. Mol. Genet. 2014;23:6961–6972. doi: 10.1093/hmg/ddu411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.De Luis D.A., Aller R., Izaola O., de la Fuente B., Conde R., Sagrado M.G., Primo D. Evaluation of weight loss and adipocytokines levels after two hypocaloric diets with different macronutrient distribution in obese subjects with rs9939609 gene variant. Diabetes Metab. Res. Rev. 2012;28:663–668. doi: 10.1002/dmrr.2323. [DOI] [PubMed] [Google Scholar]
- 70.Bodhini D., Gaal S., Shatwan I., Ramya K., Ellahi B., Surendran S., Sudha V., Anjana M.R., Mohan V., Lovegrove J.A., et al. Interaction between TCF7L2 polymorphism and dietary fat intake on high density lipoprotein cholesterol. PLoS ONE. 2017;12:e0188382. doi: 10.1371/journal.pone.0188382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Casas-Agustench P., Arnett D.K., Smith C.E., Lai C.Q., Parnell L.D., Borecki I.B., Frazier-Wood A.C., Allison M., Chen Y.D., Taylor K.D., et al. Saturated fat intake modulates the association between an obesity genetic risk score and body mass index in two US populations. J. Acad. Nutr. Diet. 2014;114:1954–1966. doi: 10.1016/j.jand.2014.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Celis-Morales C.A., Lyall D.M., Gray S.R., Steell L., Anderson J., Iliodromiti S., Welsh P., Guo Y., Petermann F., Mackay D.F., et al. Dietary fat and total energy intake modifies the association of genetic profile risk score on obesity: Evidence from 48 170 UK Biobank participants. Int. J. Obes. (Lond.) 2017;41:1761–1768. doi: 10.1038/ijo.2017.169. [DOI] [PubMed] [Google Scholar]
- 73.Rukh G., Sonestedt E., Melander O., Hedblad B., Wirfalt E., Ericson U., Orho-Melander M. Genetic susceptibility to obesity and diet intakes: Association and interaction analyses in the Malmo Diet and Cancer Study. Genes Nutr. 2013;8:535–547. doi: 10.1007/s12263-013-0352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bray G.A., Paeratakul S., Popkin B.M. Dietary fat and obesity: A review of animal, clinical and epidemiological studies. Physiol. Behav. 2004;83:549–555. doi: 10.1016/j.physbeh.2004.08.039. [DOI] [PubMed] [Google Scholar]
- 75.Micallef M., Munro I., Phang M., Garg M. Plasma n-3 Polyunsaturated Fatty Acids are negatively associated with obesity. Br. J. Nutr. 2009;102:1370–1374. doi: 10.1017/S0007114509382173. [DOI] [PubMed] [Google Scholar]
- 76.Iso H., Rexrode K.M., Stampfer M.J., Manson J.E., Colditz G.A., Speizer F.E., Hennekens C.H., Willett W.C. Intake of fish and omega-3 fatty acids and risk of stroke in women. JAMA. 2001;285:304–312. doi: 10.1001/jama.285.3.304. [DOI] [PubMed] [Google Scholar]
- 77.He K., Rimm E.B., Merchant A., Rosner B.A., Stampfer M.J., Willett W.C., Ascherio A. Fish consumption and risk of stroke in men. JAMA. 2002;288:3130–3136. doi: 10.1001/jama.288.24.3130. [DOI] [PubMed] [Google Scholar]
- 78.Kabir M., Skurnik G., Naour N., Pechtner V., Meugnier E., Rome S., Quignard-Boulange A., Vidal H., Slama G., Clement K., et al. Treatment for 2 mo with n 3 polyunsaturated fatty acids reduces adiposity and some atherogenic factors but does not improve insulin sensitivity in women with type 2 diabetes: A randomized controlled study. Am. J. Clin. Nutr. 2007;86:1670–1679. doi: 10.1093/ajcn/86.5.1670. [DOI] [PubMed] [Google Scholar]
- 79.Thorsdottir I., Tomasson H., Gunnarsdottir I., Gisladottir E., Kiely M., Parra M.D., Bandarra N.M., Schaafsma G., Martinez J.A. Randomized trial of weight-loss-diets for young adults varying in fish and fish oil content. Int. J. Obes. (Lond.) 2007;31:1560–1566. doi: 10.1038/sj.ijo.0803643. [DOI] [PubMed] [Google Scholar]
- 80.Weech M., Vafeiadou K., Hasaj M., Todd S., Yaqoob P., Jackson K.G., Lovegrove J.A. Development of a food-exchange model to replace saturated fat with MUFAs and n-6 PUFAs in adults at moderate cardiovascular risk. J. Nutr. 2014;144:846–855. doi: 10.3945/jn.114.190645. [DOI] [PubMed] [Google Scholar]
- 81.Kastorini C.M., Milionis H.J., Esposito K., Giugliano D., Goudevenos J.A., Panagiotakos D.B. The effect of Mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J. Am. Coll. Cardiol. 2011;57:1299–1313. doi: 10.1016/j.jacc.2010.09.073. [DOI] [PubMed] [Google Scholar]
- 82.Khaw K.T., Sharp S.J., Finikarides L., Afzal I., Lentjes M., Luben R., Forouhi N.G. Randomised trial of coconut oil, olive oil or butter on blood lipids and other cardiovascular risk factors in healthy men and women. BMJ Open. 2018;8:e020167. doi: 10.1136/bmjopen-2017-020167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Heianza Y., Qi L. Gene-Diet Interaction and Precision Nutrition in Obesity. Int. J. Mol. Sci. 2017;18:787. doi: 10.3390/ijms18040787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Healthy Diet. [(accessed on 21 January 2020)]; Available online: https://www.who.int/nutrition/publications/nutrientrequirements/healthydiet_factsheet/en/.
- 85.Interim Summary of Conclusions and Dietary Recommendations on Total Fat & Fatty Acids. [(accessed on 21 January 2020)]; Available online: https://www.who.int/nutrition/topics/FFA_summary_rec_conclusion.pdf.
- 86.Micha R., Khatibzadeh S., Shi P., Fahimi S., Lim S., Andrews K.G., Engell R.E., Powles J., Ezzati M., Mozaffarian D. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ. 2014;348:2272. doi: 10.1136/bmj.g2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mertens E., Kuijsten A., Geleijnse J.M., Boshuizen H.C., Feskens E.J.M., Van’t Veer P. FFQ versus repeated 24-h recalls for estimating diet-related environmental impact. Nutr. J. 2019;18:2. doi: 10.1186/s12937-018-0425-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.