Abstract
The bile acid receptor, TGR5, is a key regulator of glucose homeostasis, but the mechanisms by which TGR5 signaling improves glucose regulation are incompletely defined. In particular, TGR5 has an increasingly appreciated role in liver physiology and pathobiology; however, whether TGR5 signaling within the liver contributes to its glucoregulatory effects is unknown. Therefore, we investigated the role of hepatocyte TGR5 signaling on glucose regulation using a hepatocyte-specific TGR5 knockout mouse model. Hepatocyte-specific Tgr5Hep+/+ and Tgr5Hep−/− mice were fed a high fat diet (HFD) for 7 weeks and then orally gavaged with three doses of a highly potent, TGR5-specific agonist, Compound 18 (10 mg/kg), or vehicle, over 72 h and underwent an oral glucose tolerance test (OGTT) after the last dose. Herein, we report that TGR5 mRNA and protein is present in mouse hepatocytes. Cumulative food intake, body weight, and adiposity do not differ between Tgr5Hep+/+ and Tgr5Hep−/− mice with or without treatment with Compound 18. However, administration of Compound 18 improves glucose tolerance in Tgr5HEP+/+ mice, but not in Tgr5Hep−/− mice. Further, this effect occurred independent of body weight and GLP-1 secretion. Together, these data demonstrate that TGR5 is expressed in hepatocytes, where it functions as a key regulator of whole-body glucose homeostasis.
Keywords: hepatocyte, TGR5, glucose regulation
1. Introduction
Bile acids are amphipathic steroid molecules that activate the nuclear receptor, farnesoid X receptor (FXR), and the transmembrane G-protein coupled receptor, TGR5, to integrate lipid, glucose, and energy metabolism and maintain metabolic homeostasis [1,2,3]. Dysregulated bile acid signaling is associated with the pathogenesis of various diseases including cholestatic liver diseases, dyslipidemia, fatty liver diseases, and type 2 diabetes [4,5,6,7]. As such, TGR5 is a key regulator of metabolic homeostasis; however, the mechanisms remain incompletely defined.
TGR5 is expressed in many tissues including endocrine glands, adipocytes, muscle, liver, brain, and the gastrointestinal tract [8,9,10,11,12]. TGR5 signaling in many of these tissue types has been shown to contribute to glucose regulation [3,13]. For example, in gastrointestinal enteroendocrine L cells, TGR5 signaling promotes glucagon-like peptide-1 (GLP-1) secretion [3,14,15]. Furthermore, in mice fed a high fat diet (HFD), TGR5 agonists have been shown to increase in GLP-1 secretion from L cells, which was associated with an improvement in insulin sensitivity and measures of hepatic steatosis [16]. TGR5 is also found on pancreatic beta-cells where its activation increases glucose-stimulated insulin secretion [17]. It has also been demonstrated that TGR5 signaling increases energy expenditure by increasing the activity of the cyclic-AMP-dependent thyroid hormone activating enzyme type 2 iodothyronine deiodinase, mitochondrial thermogenesis, and fat mass oxidation to enhance basal metabolic rate [13,18,19]. TGR5 signaling in adipocytes promotes beiging of white adipose tissue in mice [19] and enhances energy expenditure to improve glucose regulation [13,20]. Finally, TGR5 signaling in immune cells decreases inflammatory cytokine secretion [11,21,22], which likely decreases systemic inflammation to improve insulin sensitivity [23].
TGR5 is also robustly expressed in the liver, but the role of hepatic TGR5 signaling in glucose regulation remains poorly understood. Various studies have identified anti-inflammatory, anti-apoptotic, choleretic, and proliferative effects of TGR5 signaling in nonparenchymal cell types of the liver. Within the liver, TGR5 is highly expressed on Kupffer cells [9], sinusoidal endothelial cells [10], and cholangiocytes [24,25]. In Kupffer cells and resident macrophages, bile acid signaling through TGR5 activates a cAMP-dependent pathway that attenuates LPS-induced cytokine expression and reduces the NF-kB-dependent inflammatory response, thereby dampening hepatic inflammation and promoting tissue remodeling [9,21]. Further, activation of TGR5 on sinusoidal endothelial cells functions to modulate liver microcirculation through increased production of nitric oxide [10,26]. This serves to both mitigate portal hypertension and enable adaptation of hepatic blood flow to nutrient uptake [26,27]. TGR5 activation of biliary epithelial cells results in CFTR-dependent chloride and bicarbonate secretion into bile, which reduces bile acid protonation to protect the liver parenchyma from bile acid toxicity [25,28,29,30]. Additionally, TGR5 stimulates relaxation of gallbladder smooth muscle cells to induce gallbladder filling [31,32]. TGR5 has also been shown to induce cholangiocyte proliferation [33] and promote barrier function by reinforcing cholangiocyte tight junctions [30].
Previous studies highlight a role for TGR5 in liver biology and pathobiology. For example, the genetic ablation of TGR5 or the inactivation of TGR5 signaling has been shown to make mice more susceptible of cholestatic liver injuries [30,33,34,35]. This is thought to be due to a role for TGR5 in maintaining a healthy bile acid profile. Specifically, mice with homozygous deficiency of TGR5 exhibit decreased total bile acid pool size [8,24,32], an excessively hydrophobic bile acid pool [32,36], as well as protection from gallstone formation when fed a lithogenic diet [24]. In addition, treatment of HFD-fed mice with a TGR5-specific agonist, INT-777, decreased liver steatosis [3,24], suggesting that TGR5 signaling in the liver attenuates triglyceride accumulation. Furthermore, HFD-fed whole body Tgr5−/− mice are more susceptible to liver injury than littermate controls as evidenced by an elevation of serum liver enzymes due to increased cytokine mRNA levels, more pronounced inflammatory infiltrates, and increased liver necrosis [34,37], highlighting the hepatoprotective role of TGR5 signaling. Together, these data demonstrate that TGR5 exerts important effects on various aspects of liver health. As the liver is a key organ involved in whole body glucose regulation, this suggests that liver TGR5 signaling may be a critical contributor to the overall metabolic benefits of TGR5 agonists.
Despite the growing body of literature regarding the role of TGR5 in liver health, it is unknown if TGR5 signaling within the liver contributes to TGR5′s role in glucose regulation, largely due to a lack of cell-type specific in vivo studies of liver TGR5 function. As the hepatocyte is the predominant cell type in the liver, here, we tested the hypothesis that TGR5 signaling in the hepatocyte improves glucose regulation. It is thought that TGR5 is, at most, lowly expressed on hepatocytes; however, this has not been extensively studied. TGR5 expression has been identified in a human hepatocellular carcinoma cell line [38], in canine hepatocytes [39], and here, in mouse hepatocytes. In this study, we employed a highly potent and specific non-bile acid TGR5 agonist, Compound 18 [40], as well as hepatocyte-specific TGR5 knockout mice to investigate the role of hepatocyte TGR5 on glucose regulation. Our results demonstrate that Compound 18 enhances glucose regulation in a hepatocyte TGR5-dependent manner.
2. Materials and Methods
2.1. Animals and Diet
All experiments were performed in accordance with the Guide for the Care and Use of Laboratory Animals and approved by the Institutional Animal Care and Use Committee of Cornell University (approved animal protocol number: 2013-0065). Study mice were individually housed and maintained in a temperature and humidity-controlled room, with a 14:10 h light-dark cycle. Whole body TGR5 knockout mice (B6.Gpbar1 tm1(KOMP)Vlcg) (KOMP Repository, The Knockout Mouse Project; University of California, Davis, CA, USA) were used for immunofluorescence analysis of hepatocyte TGR5 expression. Hepatocyte-specific TGR5 knockout mice were generated by crossing a TGR5 floxed mouse line (B6.Gpbar1 < tm1.1Auw/J) [23] with hepatocyte-specific albumin-Cre mouse line (B6N.Cg-Tg (Alb-cre)21Mgn/J). To validate this model, hepatocytes were isolated from Tgr5HEP+/+ and Tgr5HEP−/− mice and analyzed by RT-PCR to confirm the presence of Tgr5 mRNA in Tgr5HEP+/+ mice and loss of Tgr5 mRNA in the hepatocytes of Tgr5HEP−/− mice (Figure S1). Starting at 8 weeks of age, male and female Tgr5HEP+/+ and Tgr5HEP−/− littermates were fed a HFD consisting of ground chow (5012 LabDiets; St. Louis, MO, USA) supplemented with 3.4% butter fat, 8.5% tallow, 13.1% soybean oil, 3.5% mineral mix, and 1% vitamin mix (Dyets; Bethlehem, PA, USA) by weight for 7 weeks to produce an obese, insulin resistant phenotype. Mice were matched for baseline body weight at the start of the HFD. Food intake and body weight were measured once per week (Tgr5HEP+/+ n = 16, 8 males, 8 females; Tgr5HEP−/−; n = 12; 7 males, 5 females). In a separate cohort of mice, following 7 weeks of the HFD, mice received 3 consecutive, daily doses of either vehicle (20% Captisol w/v with water, CyDex Pharmaceuticals) or Compound 18 (10 mg/kg/day, Eli Lilly & Company-molecular weight = 508.62) by oral gavage. Compound 18 was formulated in 20% Captisol w/v with water, as previously described [40]. An oral glucose tolerance test (OGTT, 2 g/kg body weight oral gavage with dextrose), following an overnight (12 h) fast, was performed as previously described [41]. To minimize the contribution of TGR5-stimulated GLP-1 release, the OGTT was performed 1 h after the last dose of Compound 18 [40]. Blood glucose measurements were made using a glucometer (One-Touch Ultra, Lifescan; Milpitas, CA, USA). Serum insulin concentrations were measured by ELISA (Millipore; Burlington, MA, USA) and serum total GLP-1 concentrations were measured by sandwich electrochemiluminescence immunoassay (Meso Scale Discovery; Gaithersburg, MA, USA). Immediately following the OGTT, mice were euthanized by an overdose of pentobarbital (200 mg/kg i.p.) and tissues were weighed and collected. The following groups were studied: Vehicle Tgr5HEP+/+ (VEH Tgr5HEP+/+; n = 9; 4 males, 5 females), Compound 18 Tgr5HEP+/+ (C18 Tgr5HEP+/+; n = 8; 4 males, 4 females), Vehicle Tgr5HEP−/− (VEH Tgr5HEP−/−; n = 9; 4 males, 5 females), and Compound 18 Tgr5HEP−/− (C18 Tgr5HEP−/−; n = 9; 4 males, 5 females).
2.2. HOMA-IR Calculation
The HOMA-IR (homeostasis model assessment of insulin resistance) index was calculated as (fasting serum glucose × fasting serum insulin/22.5) to assess insulin resistance [42]. Log (HOMA-IR) was used as a surrogate index of insulin resistance, which has been validated for use in rodents, as previously described [43].
2.3. Immunofluorescence
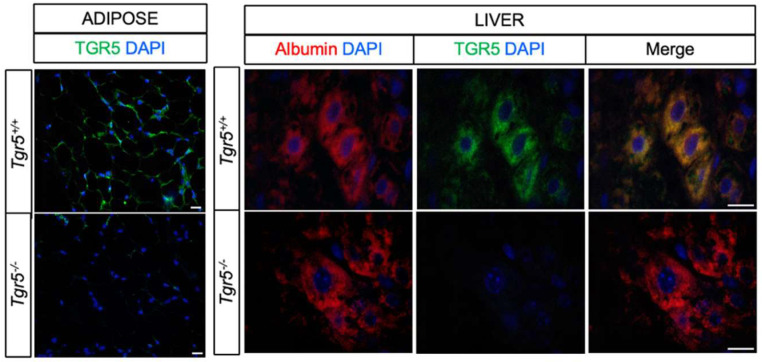
Liver samples from whole body TGR5 wildtype (Tgr5+/+) and knockout (Tgr5−/−) mice were used for immunofluorescence analysis, as previously described [41]. Briefly, samples were collected, fixed in 4% paraformaldehyde, and paraffin embedded. Sections were deparafinized in a xylene ethanol series, placed in Tris-EDTA buffer for antigen retrieval (10 mM Tris, 1 mM EDTA, 0.05% Tween, pH = 9.0), and then blocked in 5% bovine serum albumin. Sections were immunostained for TGR5 using a polyclonal anti-rabbit antibody (LSBio; Seattle, WA, USA; 1:500) and for albumin using a monoclonal anti-mouse antibody (Santa Cruz Biotechnology; Dallas, TX, USA; 1:500). The antibody against TGR5 was validated on adipose samples from whole-body TGR5 wildtype (Tgr5+/+) and knockout (Tgr5−/−) (Figure 1). Detection of the primary antibodies was performed using Alexa Flour 488 anti-rabbit and Alexa Fluor 633 anti-mouse secondary antibodies (1:500) (Invitrogen; Foster City, CA, USA). Nuclei were detected using 4′,6′-diamino-2-phenyl inodole (DAPI), which was included in the mounting solution (Invitrogen; Foster City, CA, USA). Images were captured using Nikon Eclipse E400 fluorescent microscope with Olympus DP73 color camera (final magnification 20× for adipose and 100× for liver).
Figure 1.
TGR5 is expressed in hepatocytes. Representative images of whole body TGR5 wild-type (Tgr5+/+) and knockout (Tgr5−/−) mouse adipose and liver sections immunostained for TGR5 (green), albumin (red), and DAPI. Scale bar = 20 um.
2.4. Statistics and Data Analysis
Data are presented as mean ± SEM. The main effect of sex was not significant so the data for males and females were combined. All statistical analyses were performed using GraphPad Prism 8.00 for Mac (GraphPad Software, San Diego, CA, USA). Data were analyzed by two-factor ANOVA with Bonferroni’s post-test or Student’s t-test, as indicated. Differences were considered significant at p < 0.05.
3. Results
3.1. TGR5 Is Expressed in Hepatocytes
TGR5 is highly expressed in the liver [9,10,24,25]; however, whether TGR5 is expressed in mouse hepatocytes has not been previously reported. Therefore, we assessed TGR5 expression in mouse liver sections. Adipose tissue sections from a whole body TGR5 knockout mouse model were used for antibody validation (Figure 1). As previously reported [11,44], TGR5 was highly expressed in adipocytes. TGR5 was not detected in adipocytes from Tgr5−/− mice, confirming antibody specificity. TGR5 expression was also detected in some, but not all, hepatocytes in Tgr5+/+, but not Tgr5−/− mice (Figure 1). These data are the first to demonstrate that while lowly expressed, TGR5 is present in mouse hepatocytes. Given that hepatocytes comprise the majority of the liver parenchyma and are a key determinant of whole body glucose homeostasis, we used a hepatocyte-specific TGR5 knockout mouse model to determine the role of hepatocyte TGR5 signaling in metabolic health.
3.2. Hepatocyte TGR5 Does Not Contribute to Regulation of Food Intake, Body Weight, or Adiposity
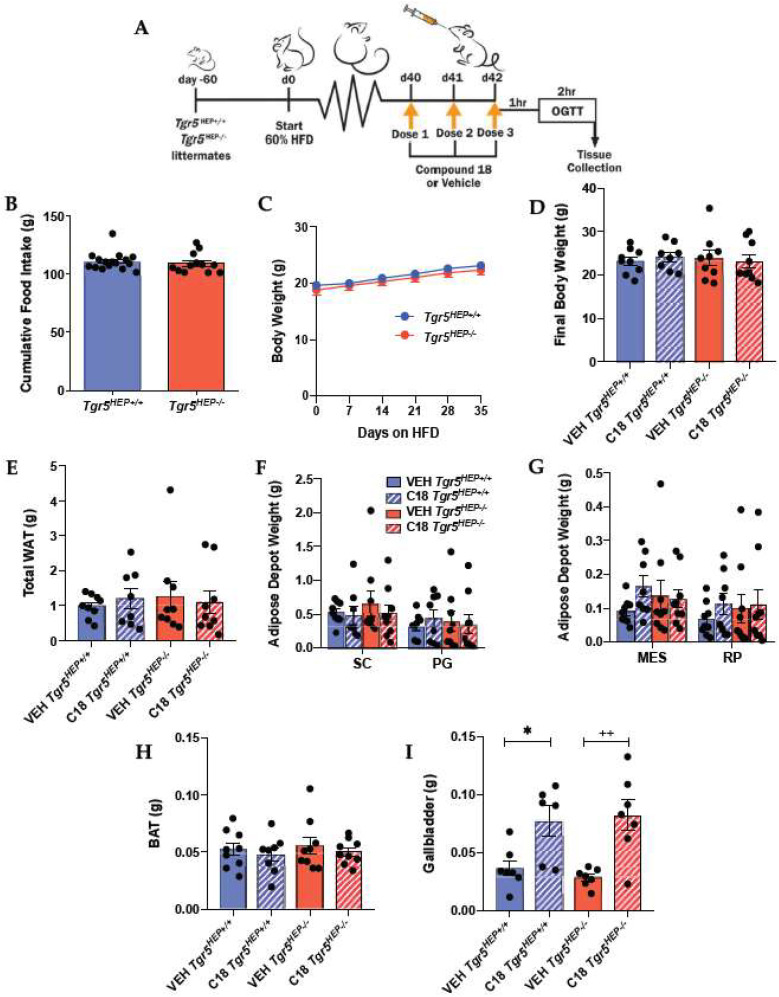
To assess the role of hepatocyte TGR5 on the regulation of body weight, we measured body weight and food intake in Tgr5HEP+/+ and Tgr5HEP−/− mice over the course of 7 weeks of HFD (Figure 2A). Similar to previous work in whole body TGR5 knockout mouse models [24,41,45], cumulative food intake and body weight did not differ between Tgr5HEP+/+ and Tgr5HEP−/− mice (Figure 2B,C), which allowed us to assess the body weight-independent effects of hepatocyte TGR5 signaling on glucose regulation. In addition, final body weight and adiposity, measured after 3 consecutive daily doses of Compound 18 or vehicle, did not differ between genotype or treatment (Figure 2D–H). These data demonstrate that hepatocyte TGR5 does not regulate food intake, body weight, or adiposity under basal conditions or following stimulation by Compound 18.
Figure 2.
Hepatocyte TGR5 does not contribute to regulation of food intake, body weight, or adiposity. (A) Study design. (B) Cumulative food intake and (C) body weight over 7 weeks of high fat diet (HFD) feeding in Tgr5HEP+/+ and Tgr5HEP−/− mice. n = 12–16. (D) Body weight at the time of euthanasia; (E) total white adipose tissue (WAT) weight; (F) subcutaneous (SC) and perigonadal (PG); (G) mesenteric (MES) and retroperitoneal (RP) adipose tissue weights; (H) brown adipose tissue (BAT) weights; and (I) gallbladder weight in Tgr5HEP+/+ and Tgr5HEP−/− mice treated with Compound 18 (C18) or vehicle (VEH). n = 6–9. * p < 0.05 compared with VEH Tgr5HEP+/+; ++ p < 0.01 compared with VEH Tgr5HEP−/− by two-factor ANOVA.
TGR5 is highly enriched in the biliary tract [24,25] and its absence has been shown to slow bile flow and reduce gallbladder volume [31,32]. Consistent with this, Compound 18 and other synthetic TGR5 agonists have been reported to increase gallbladder filling [40,46,47]. Therefore, we assessed gallbladder weight at the time of euthanasia in a sub-set of mice to determine the impact of Compound 18 treatment on this negative side-effect. Treatment with Compound 18 increased gallbladder weight in both Tgr5HEP+/+ and Tgr5HEP−/− mice (Figure 2I, p < 0.05). These data demonstrate that Compound 18 promotes gallbladder filling independently of hepatocyte TGR5 signaling.
3.3. Compound 18 Improves Glucose Regulation in a Hepatocyte TGR5-dependent Manner
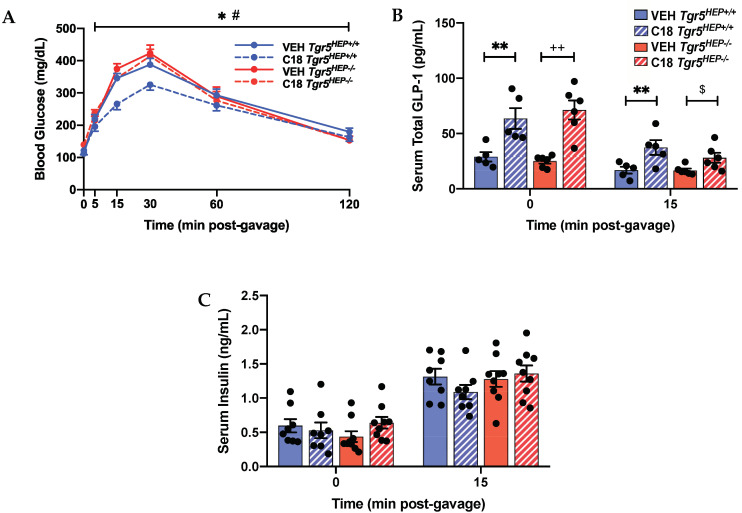
To assess the role of hepatocyte TGR5 on glucose regulation, we performed an OGTT in HFD-fed Tgr5HEP+/+ and Tgr5HEP−/− mice with and without Compound 18 treatment. Compound 18 improved glucose tolerance compared with vehicle-treated controls in Tgr5HEP+/+ mice, but not Tgr5HEP−/− mice (Figure 3A, p < 0.05). Furthermore, Compound 18-treated Tgr5HEP+/+ mice exhibited lower blood glucose excursions compared with Compound 18-treated Tgr5HEP−/− mice (Figure 3A, p < 0.05).
Figure 3.
Compound 18 improves glucose regulation in a hepatocyte TGR5-dependent manner. (A) Blood glucose, (B) serum total GLP-1, and (C) serum insulin concentrations during an OGTT in Tgr5HEP+/+ and Tgr5HEP−/− mice after 3 doses of Compound 18 (C18) or vehicle (VEH). n = 5–9. * p < 0.05, ** p < 0.01 C18 Tgr5HEP+/+ vs. VEH Tgr5HEP+/+; ++ p < 0.01 C18 Tgr5HEP−/− vs. VEH Tgr5HEP−/−; # p < 0.05 C18 Tgr5HEP−/− vs. C18 Tgr5HEP+/+ by two-factor ANOVA; $ p < 0.05 compared with VEH Tgr5HEP−/− by Student’s t-test.
A key mechanism by which TGR5 agonists improve glucose tolerance is through induction of GLP-1 secretion and subsequent enhancement of glucose-stimulated insulin secretion [3]. Previous work finds that while Compound 18 potently promotes GLP-1 secretion, GLP-1 levels return to baseline within approximately 1 h of Compound 18 administration in mice [40]. Therefore, to control for the effect of GLP-1, we performed the OGTT 1 h following the last dose of Compound 18 or vehicle. As baseline fasting blood samples were collected approximately 45 min after the last Compound 18 dose, fasting total serum GLP-1 levels were still elevated in Compound 18-treated Tgr5HEP+/+ and Tgr5HEP−/− mice compared to vehicle controls (Figure 3B, p < 0.05). While this Compound 18-induced increase in serum GLP-1 levels was diminished by 15 min post-glucose gavage, there remained an elevation of serum GLP-1 levels in Compound 18-treated mice compared with control (p < 0.05 by 2-factor ANOVA in the Tgr5HEP+/+ mice and p < 0.05 by Student’s t-test in the Tgr5HEP−/− mice). Nevertheless, fasting serum insulin concentrations and serum insulin concentrations at 15 min after the glucose gavage did not differ between the genotype or treatment condition (Figure 3C). As expected, serum insulin levels at 15 min post-glucose gavage were elevated compared with fasting serum insulin concentrations in all groups. Of note, the lack of a difference in fasting serum insulin concentrations despite marked elevations in fasting serum GLP-1 concentrations points to the glucose-dependent actions of GLP-1 to promote insulin secretion. Together, these data demonstrate that hepatocyte TGR5 signaling contributes to the effect of Compound 18 to improve glucose tolerance, independently of insulin and GLP-1 secretion.
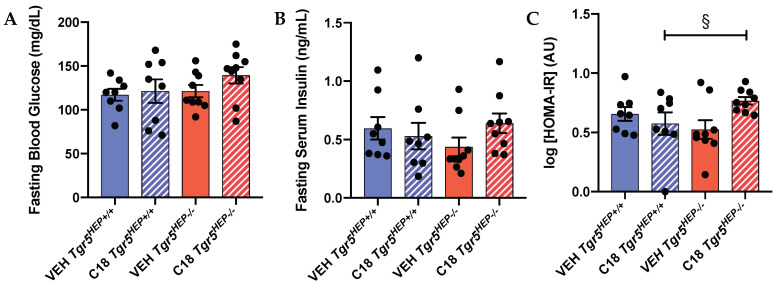
3.4. An Index of Insulin Sensitivity Is Impaired in Compound 18-treated Mice Lacking Hepatocyte TGR5
As expected, we did not observe alterations in insulin secretion during the OGTT between genotype or between treatment. It has been previously shown that enhanced TGR5 signaling improves insulin resistance in various tissues by decreasing inflammation [23] and lipotoxicity [16] and increasing energy expenditure [13,20], but the hepatocyte-specific effect of TGR5 signaling on insulin resistance has not been investigated. Therefore, we evaluated an index of insulin resistance in Tgr5HEP+/+ and Tgr5HEP−/− mice with and without Compound 18 treatment. We chose the log(HOMA-IR) as a surrogate index of insulin sensitivity as it has been shown to have improved predictive accuracy compared with other indices [43].
There was no significant difference in fasting blood glucose (Figure 4A) or fasting serum insulin concentrations (Figure 4B) between genotype or treatment. However, Compound 18-treated Tgr5HEP+/+ mice exhibited a lower log(HOMA-IR) compared to Compound 18-treated Tgr5HEP−/− mice (Figure 4C, p < 0.05 by Student’s t-test). Together, with a lack of a difference in glucose-stimulated insulin secretion, these data suggest that hepatocyte TGR5 signaling may improve glucose homeostasis, in part, through an improvement in insulin sensitivity. Nevertheless, further work is needed to define the impact of hepatocyte TGR5 signaling on insulin sensitivity.
Figure 4.
Compound 18 improves insulin sensitivity in a hepatocyte TGR5-dependent manner. (A) Fasting blood glucose, (B) fasting serum insulin concentrations, and (C) log(HOMA-IR) in Tgr5HEP+/+ and Tgr5HEP−/− mice after 3 doses of Compound 18 (C18) or vehicle (VEH). n = 8–9. § p < 0.05 compared with Compound 18 Tgr5HEP+/+ by one-tailed Student’s t-test.
4. Discussion
The TGR5 receptor is ubiquitously expressed throughout the body and has a well-defined role in many regulatory functions that affect hepatic metabolism and extrahepatic glucose homeostasis [3,9,13,21]; however, the expression of TGR5 and its functional significance in hepatocytes remained unknown to date. In this study, we performed the first targeted assessment of TGR5 expression in mouse hepatocytes. TGR5 was detected in hepatocytes of paraffin embedded liver sections by immunofluorescence staining. Our understanding of the liver-specific effects of TGR5 on glucose regulation remain limited due to a lack of cell-type specific in vivo studies of liver TGR5 function. To this end, we employed a hepatocyte-specific TGR5 knockout mouse model in order to dissect the functional significance of hepatocyte TGR5 signaling. Herein, we provide compelling data that TGR5 is expressed in hepatocytes, where it functions as a regulator of whole body glucose homeostasis.
TGR5 has been implicated in body weight regulation through its role in energy metabolism. Specifically, TGR5 regulates energy expenditure by inducing mitochondrial biogenesis and thereby increasing basal metabolism in thermogenically competent tissues, such as brown adipose tissue and skeletal muscle and through the beiging of white adipose tissue [13,18,19,48]. In this study, there was no difference in body weight or adiposity between Tgr5HEP+/+ and Tgr5HEP−/− mice with or without treatment with Compound 18, demonstrating that hepatocyte TGR5 signaling does not regulate body weight, food intake, or adiposity. While Briere et al. reported that 14 days of Compound 18 administration at 60 mg/kg reduced body weight and fat mass gain in HFD-fed mice [40], it is likely that our 3-day dosing paradigm at 10 mg/kg was not long enough or robust enough to induce Compound 18-dependent reductions in adiposity. Nevertheless, the absence of genotype-dependent and Compound 18-dependent effects on adiposity and body weight in this study enabled us to assess the body weight-independent effects of hepatocyte TGR5 signaling on glucose homeostasis.
While our data are consistent with previous work demonstrating that TGR5 ablation contributes to metabolic dysregulation in mouse models [3,19,34,37,49], our data are the first to demonstrate that TGR5 signaling specifically within the hepatocyte plays a significant role in whole body glucose regulation. Until now, the role of TGR5 in the maintenance of glucose homeostasis and insulin sensitivity has been attributed to its effects on mitochondrial function in muscle and BAT and/or insulin release from the pancreas, enhanced by enteroendocrine L cell GLP-1 secretion [3,13,14,15,17,20]. For example, various TGR5 agonists have been shown to ameliorate glucose intolerance in obese and diabetic mice [3,13,50,51]. While in some studies, this improvement in glucose tolerance was associated with increased energy expenditure and subsequent weight loss [3,50], other studies attributed body weight-independent improvements in hyperglycemia to enhanced GLP-1 secretion [40,52]. In contrast, our data show that Compound 18 improves glucose tolerance in a hepatocyte TGR5-dependent manner. Further, in contrast to the aforementioned studies, this effect can occur independently of body weight, GLP-1 secretion, and glucose-stimulated insulin secretion. Thus, we provide evidence that TGR5 agonists improve glucose homeostasis through an additional novel mechanism specific to hepatocyte TGR5 signaling.
The hepatocyte TGR5-dependent improvement in glucose tolerance occurred in the absence of a difference in insulin secretion, suggesting that hepatocyte TGR5 signaling regulates hepatic glucose metabolism and/or insulin sensitivity. Hepatic glucose metabolism is dictated predominantly by hepatic glucose output and insulin sensitivity [53]. Using an index of insulin resistance, our data suggest that hepatocyte TGR5 signaling may regulate insulin sensitivity. Recent studies have proposed that HOMA-IR measurements of insulin resistance refer mostly to the liver, rather than describing peripheral insulin sensitivity [54,55]. This is of particular interest in our model as we sought to understand how liver TGR5 regulates glucose homeostasis. Consistent with our findings, previous work has shown that administration of INT-777 reduced insulin resistance in liver and muscle in obese mice, as assessed by a hyperinsulinemic euglycemic clamp and 14C-2-deoxy-glucose tracers [3]. It is also possible that the improved hepatic insulin resistance in Tgr5HEP+/+ mice, as compared to Tgr5HEP−/− mice, following treatment with Compound 18 is mediated by reduced inflammation and decreased ectopic triglyceride deposition, characteristic of enhanced liver TGR5 signaling [3,24]. Nevertheless, further work is needed to determine the mechanisms by which hepatocyte TGR5 signaling improves glucose tolerance.
A growing body of literature has highlighted the potential value of TGR5 agonists in the treatment of various metabolic and liver diseases [3,13,20,23,40,41,52]. However, the clinical development of TGR5 agonists is complicated by the wide range of effects associated with systemic TGR5 activation. TGR5 expression in mouse and human gallbladder is estimated to be 10-fold higher than any other tissue [24,25,40]. Studies in whole body Tgr5−/− mice have documented decreased bile flow from the liver [32] and reduced gallbladder volume [31,32], which is explained by reduced TGR5-dependent biliary secretion and impaired smooth muscle relaxation of the gallbladder, respectively. In contrast, the oral administration of TGR5 agonists, including INT-777, oleanolic acid, Compound 23g, and RO552739, has been shown to induce hepatic bile flow [32,52] and increase gallbladder filling in wild type mice [32,46,47,50]. Similarly, Compound 18 has been shown to have a dose-dependent effect on gallbladder filling, an effect that is lost in whole body Tgr5−/− mice [40]. To this end, a major side effect of TGR5 agonists is the inhibition of gallbladder emptying, ultimately leading to cholestatic liver injury [24,32,40]. As expected, in this present study, we found no difference in gallbladder weight between Tgr5HEP+/+ and Tgr5HEP−/− mice in the absence of Compound 18. However, in response to Compound 18 administration, our data demonstrate a significant increase in gallbladder weight in both Tgr5HEP+/+ and Tgr5HEP−/− mice. Together, these results suggest that hepatocyte TGR5 does not contribute to the role of TGR5 in gallbladder filling under basal conditions or in the presence of a TGR5 agonist. Further, our results highlight the need to identify cell-type specific effects and downstream signaling targets of TGR5 signaling in order to develop better bile acid-based therapeutics to treat diabetes and metabolic disease.
5. Conclusions
In conclusion, TGR5 is a promising therapeutic target, but its breadth of actions, particularly in the gallbladder, complicates this task. As such, there is a growing need to identify cell-type specific effects of TGR5 signaling in order to begin to identify and target the downstream effectors of TGR5 signaling. Our findings provide additional insight into the underlying mechanisms by which TGR5 agonists improve whole body glucose homeostasis. Importantly, our data demonstrate that hepatocyte TGR5 signaling regulates whole body glucose homeostasis.
Acknowledgments
We thank Eli Lilly & Company for supplying Compound 18. We thank the Animal Health and Diagnostic Center Histopathology Core for preparation of samples for histological analysis. We would like to thank Jackie Belliveau for assistance with animal care.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/12/7/2124/s1, Figure S1: Validation of hepatocyte-specific TGR5 knockout mouse model.
Author Contributions
Investigation: M.M.H., M.K.C., A.M., and B.P.C.; Conceptualization, Resources: D.A.B., K.W.S., K.S., and B.P.C.; Methodology: M.M.H., M.K.C., A.M., D.A.B., K.W.S., K.S., and B.P.C.; Formal Analysis, Validation: M.M.H. and B.P.C.; Writing—Original Draft Preparation: M.M.H.; Writing—Review & Editing: M.K.C., A.M., D.A.B., K.W.S., K.S., and B.P.C.; Supervision, Funding Acquisition: B.P.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Nutracia 2018-55 and NIH/NCI 5R21CA195002.
Conflicts of Interest
The authors have no conflicts of interest to disclose, except KWS and DAB are employees of Eli Lilly & Company. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Pathak P., Liu H., Boehme S., Xie C., Krausz K.W., Gonzalez F., Chiang J.Y.L. Farnesoid X receptor induces Takeda G-protein receptor 5 cross-talk to regulate bile acid synthesis and hepatic metabolism. J. Biol. Chem. 2017;292:11055–11069. doi: 10.1074/jbc.M117.784322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cariou B., van Harmelen K., Duran-Sandoval D., van Dijk T.H., Grefhorst A., Abdelkarim M., Caron S., Torpier G., Fruchart J.C., Gonzalez F.J., et al. The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice. J. Biol. Chem. 2006;281:11039–11049. doi: 10.1074/jbc.M510258200. [DOI] [PubMed] [Google Scholar]
- 3.Thomas C., Gioiello A., Noriega L., Strehle A., Oury J., Rizzo G., Macchiarulo A., Yamamoto H., Mataki C., Pruzanski M., et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10:167–177. doi: 10.1016/j.cmet.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li T., Chiang J.Y. Bile acid signaling in metabolic disease and drug therapy. Pharmacol. Rev. 2014;66:948–983. doi: 10.1124/pr.113.008201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erickson S.K., Lear S.R., Deane S., Dubrac S., Huling S.L., Nguyen L., Bollineni J.S., Shefer S., Hyogo H., Cohen D.E., et al. Hypercholesterolemia and changes in lipid and bile acid metabolism in male and female cyp7A1-deficient mice. J. Lipid Res. 2003;44:1001–1009. doi: 10.1194/jlr.M200489-JLR200. [DOI] [PubMed] [Google Scholar]
- 6.Ferslew B.C., Xie G., Johnston C.K., Su M., Stewart P.W., Jia W., Brouwer K.L., Barritt A.S.T. Altered Bile Acid Metabolome in Patients with Nonalcoholic Steatohepatitis. Dig. Dis. Sci. 2015;60:3318–3328. doi: 10.1007/s10620-015-3776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brufau G., Stellaard F., Prado K., Bloks V.W., Jonkers E., Boverhof R., Kuipers F., Murphy E.J. Improved glycemic control with colesevelam treatment in patients with type 2 diabetes is not directly associated with changes in bile acid metabolism. Hepatology. 2010;52:1455–1464. doi: 10.1002/hep.23831. [DOI] [PubMed] [Google Scholar]
- 8.Maruyama T., Miyamoto Y., Nakamura T., Tamai Y., Okada H., Sugiyama E., Nakamura T., Itadani H., Tanaka K. Identification of membrane-type receptor for bile acids (M-BAR) Biochem. Biophys. Res. Commun. 2002;298:714–719. doi: 10.1016/S0006-291X(02)02550-0. [DOI] [PubMed] [Google Scholar]
- 9.Keitel V., Donner M., Winandy S., Kubitz R., Haussinger D. Expression and function of the bile acid receptor TGR5 in Kupffer cells. Biochem. Biophys. Res. Commun. 2008;372:78–84. doi: 10.1016/j.bbrc.2008.04.171. [DOI] [PubMed] [Google Scholar]
- 10.Keitel V., Reinehr R., Gatsios P., Rupprecht C., Gorg B., Selbach O., Haussinger D., Kubitz R. The G-protein coupled bile salt receptor TGR5 is expressed in liver sinusoidal endothelial cells. Hepatology. 2007;45:695–704. doi: 10.1002/hep.21458. [DOI] [PubMed] [Google Scholar]
- 11.Kawamata Y., Fujii R., Hosoya M., Harada M., Yoshida H., Miwa M., Fukusumi S., Habata Y., Itoh T., Shintani Y., et al. A G protein-coupled receptor responsive to bile acids. J. Biol. Chem. 2003;278:9435–9440. doi: 10.1074/jbc.M209706200. [DOI] [PubMed] [Google Scholar]
- 12.Poole D.P., Godfrey C., Cattaruzza F., Cottrell G.S., Kirkland J.G., Pelayo J.C., Bunnett N.W., Corvera C.U. Expression and function of the bile acid receptor GpBAR1 (TGR5) in the murine enteric nervous system. Neurogastroenterol. Motil. 2010;22:814-e228. doi: 10.1111/j.1365-2982.2010.01487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watanabe M., Houten S.M., Mataki C., Christoffolete M.A., Kim B.W., Sato H., Messaddeq N., Harney J.W., Ezaki O., Kodama T., et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439:484–489. doi: 10.1038/nature04330. [DOI] [PubMed] [Google Scholar]
- 14.Katsuma S., Hirasawa A., Tsujimoto G. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem. Biophys. Res. Commun. 2005;329:386–390. doi: 10.1016/j.bbrc.2005.01.139. [DOI] [PubMed] [Google Scholar]
- 15.Li Y., Cheng K.C., Niu C.-S., Lo S.-H., Cheng J.-T., Niu H.-S. Investigation of triamterene as an inhibitor of the TGR5 receptor: Identification in cells and animals. Drug Des. Dev. Ther. 2017;11:1127–1134. doi: 10.2147/DDDT.S131892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finn P.D., Rodriguez D., Kohler J., Jiang Z., Wan S., Blanco E., King A.J., Chen T., Bell N., Dragoli D., et al. Intestinal TGR5 agonism improves hepatic steatosis and insulin sensitivity in Western diet-fed mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2019;316:G412–G424. doi: 10.1152/ajpgi.00300.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar D.P., Rajagopal S., Mahavadi S., Mirshahi F., Grider J.R., Murthy K.S., Sanyal A.J. Activation of transmembrane bile acid receptor TGR5 stimulates insulin secretion in pancreatic beta cells. Biochem. Biophys. Res. Commun. 2012;427:600–605. doi: 10.1016/j.bbrc.2012.09.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broeders E.P., Nascimento E.B., Havekes B., Brans B., Roumans K.H., Tailleux A., Schaart G., Kouach M., Charton J., Deprez B. The bile acid chenodeoxycholic acid increases human brown adipose tissue activity. Cell Metab. 2015;22:418–426. doi: 10.1016/j.cmet.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Velazquez-Villegas L.A., Perino A., Lemos V., Zietak M., Nomura M., Pols T.W.H., Schoonjans K. TGR5 signalling promotes mitochondrial fission and beige remodelling of white adipose tissue. Nat. Commun. 2018;9:1–13. doi: 10.1038/s41467-017-02068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang S., Ma S., Ning M., Yang W., Ye Y., Zhang L., Shen J., Leng Y. TGR5 agonist ameliorates insulin resistance in the skeletal muscles and improves glucose homeostasis in diabetic mice. Metabolism. 2019;99:45–56. doi: 10.1016/j.metabol.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y.D., Chen W.D., Yu D., Forman B.M., Huang W. The G-protein-coupled bile acid receptor, Gpbar1 (TGR5), negatively regulates hepatic inflammatory response through antagonizing nuclear factor kappa light-chain enhancer of activated B cells (NF-kappaB) in mice. Hepatology. 2011;54:1421–1432. doi: 10.1002/hep.24525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo C., Qi H., Yu Y., Zhang Q., Su J., Yu D., Huang W., Chen W.D., Wang Y.D. The G-Protein-Coupled Bile Acid Receptor Gpbar1 (TGR5) Inhibits Gastric Inflammation Through Antagonizing NF-kappaB Signaling Pathway. Front. Pharmacol. 2015;6:287. doi: 10.3389/fphar.2015.00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perino A., Pols T.W., Nomura M., Stein S., Pellicciari R., Schoonjans K. TGR5 reduces macrophage migration through mTOR-induced C/EBPbeta differential translation. J. Clin. Investig. 2014;124:5424–5436. doi: 10.1172/JCI76289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vassileva G., Golovko A., Markowitz L., Abbondanzo S.J., Zeng M., Yang S., Hoos L., Tetzloff G., Levitan D., Murgolo N.J., et al. Targeted deletion of Gpbar1 protects mice from cholesterol gallstone formation. Biochem. J. 2006;398:423–430. doi: 10.1042/BJ20060537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keitel V., Cupisti K., Ullmer C., Knoefel W.T., Kubitz R., Haussinger D. The membrane-bound bile acid receptor TGR5 is localized in the epithelium of human gallbladders. Hepatology. 2009;50:861–870. doi: 10.1002/hep.23032. [DOI] [PubMed] [Google Scholar]
- 26.Renga B., Cipriani S., Carino A., Simonetti M., Zampella A., Fiorucci S. Reversal of Endothelial Dysfunction by GPBAR1 Agonism in Portal Hypertension Involves a AKT/FOXOA1 Dependent Regulation of H2S Generation and Endothelin-1. PLoS ONE. 2015;10:e0141082. doi: 10.1371/journal.pone.0141082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klindt C., Reich M., Hellwig B., Stindt J., Rahnenführer J., Hengstler J.G., Köhrer K., Schoonjans K., Häussinger D., Keitel V. The G Protein-Coupled Bile Acid Receptor TGR5 (Gpbar1) Modulates Endothelin-1 Signaling in Liver. Cells. 2019;8:1467. doi: 10.3390/cells8111467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baghdasaryan A., Claudel T., Gumhold J., Silbert D., Adorini L., Roda A., Vecchiotti S., Gonzalez F.J., Schoonjans K., Strazzabosco M., et al. Dual farnesoid X receptor/TGR5 agonist INT-767 reduces liver injury in the Mdr2−/− (Abcb4−/−) mouse cholangiopathy model by promoting biliary HCO(-)(3) output. Hepatology. 2011;54:1303–1312. doi: 10.1002/hep.24537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Buy Wenniger L.J.M., Hohenester S., Maroni L., van Vliet S.J., Elferink R.P.O., Beuers U. The Cholangiocyte Glycocalyx Stabilizes the ‘Biliary HCO3-Umbrella’: An Integrated Line of Defense against Toxic Bile Acids. Dig. Dis. 2015;33:397–407. doi: 10.1159/000371864. [DOI] [PubMed] [Google Scholar]
- 30.Merlen G., Kahale N., Ursic-Bedoya J., Bidault-Jourdainne V., Simerabet H., Doignon I., Tanfin Z., Garcin I., Pean N., Gautherot J., et al. TGR5-dependent hepatoprotection through the regulation of biliary epithelium barrier function. Gut. 2020;69:146–157. doi: 10.1136/gutjnl-2018-316975. [DOI] [PubMed] [Google Scholar]
- 31.Lavoie B., Balemba O.B., Godfrey C., Watson C.A., Vassileva G., Corvera C.U., Nelson M.T., Mawe G.M. Hydrophobic bile salts inhibit gallbladder smooth muscle function via stimulation of GPBAR1 receptors and activation of KATP channels. J. Physiol. 2010;588:3295–3305. doi: 10.1113/jphysiol.2010.192146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li T., Holmstrom S.R., Kir S., Umetani M., Schmidt D.R., Kliewer S.A., Mangelsdorf D.J. The G protein-coupled bile acid receptor, TGR5, stimulates gallbladder filling. Mol. Endocrinol. 2011;25:1066–1071. doi: 10.1210/me.2010-0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reich M., Deutschmann K., Sommerfeld A., Klindt C., Kluge S., Kubitz R., Ullmer C., Knoefel W.T., Herebian D., Mayatepek E., et al. TGR5 is essential for bile acid-dependent cholangiocyte proliferation in vivo and in vitro. Gut. 2016;65:487–501. doi: 10.1136/gutjnl-2015-309458. [DOI] [PubMed] [Google Scholar]
- 34.Pean N., Doignon I., Garcin I., Besnard A., Julien B., Liu B., Branchereau S., Spraul A., Guettier C., Humbert L., et al. The receptor TGR5 protects the liver from bile acid overload during liver regeneration in mice. Hepatology. 2013;58:1451–1460. doi: 10.1002/hep.26463. [DOI] [PubMed] [Google Scholar]
- 35.Merlen G., Bidault-Jourdainne V., Kahale N., Glenisson M., Ursic-Bedoya J., Doignon I., Garcin I., Humbert L., Rainteau D., Tordjmann T. Hepatoprotective impact of the bile acid receptor TGR5. Liver Int. 2020;40:1005–1015. doi: 10.1111/liv.14427. [DOI] [PubMed] [Google Scholar]
- 36.Donepudi A.C., Boehme S., Li F., Chiang J.Y.L. G-protein-coupled bile acid receptor plays a key role in bile acid metabolism and fasting-induced hepatic steatosis in mice. Hepatology. 2017;65:813–827. doi: 10.1002/hep.28707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Keitel V., Reich M., Sommerfeld A., Kluge S., Kubitz R., Häussinger D. Role of the bile acid receptor TGR5 (Gpbar-1) in liver damage and regeneration. Eur. J. Med. Res. 2014;19:S21. doi: 10.1186/2047-783X-19-S1-S21. [DOI] [Google Scholar]
- 38.Yang J.I., Yoon J.H., Myung S.J., Gwak G.Y., Kim W., Chung G.E., Lee S.H., Lee S.M., Kim C.Y., Lee H.S. Bile acid-induced TGR5-dependent c-Jun-N terminal kinase activation leads to enhanced caspase 8 activation in hepatocytes. Biochem. Biophys. Res. Commun. 2007;361:156–161. doi: 10.1016/j.bbrc.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Giaretta P.R., Suchodolski J.S., Blick A.K., Steiner J.M., Lidbury J.A., Rech R.R. Distribution of bile acid receptor TGR5 in the gastrointestinal tract of dogs. Histol. Histopathol. 2018;34:69–79. doi: 10.14670/HH-18-025. [DOI] [PubMed] [Google Scholar]
- 40.Briere D.A., Ruan X., Cheng C.C., Siesky A.M., Fitch T.E., Dominguez C., Sanfeliciano S.G., Montero C., Suen C.S., Xu Y., et al. Novel Small Molecule Agonist of TGR5 Possesses Anti-Diabetic Effects but Causes Gallbladder Filling in Mice. PLoS ONE. 2015;10:e0136873. doi: 10.1371/journal.pone.0136873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGavigan A.K., Garibay D., Henseler Z.M., Chen J., Bettaieb A., Haj F.G., Ley R.E., Chouinard M.L., Cummings B.P. TGR5 contributes to glucoregulatory improvements after vertical sleeve gastrectomy in mice. Gut. 2017;66:226–234. doi: 10.1136/gutjnl-2015-309871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matthews D.R., Hosker J.P., Rudenski A.S., Naylor B.A., Treacher D.F., Turner R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 43.Lee S., Muniyappa R., Yan X., Chen H., Yue L.Q., Hong E.G., Kim J.K., Quon M.J. Comparison between surrogate indexes of insulin sensitivity and resistance and hyperinsulinemic euglycemic clamp estimates in mice. Am. J. Physiol. Endocrinol. Metab. 2008;294:E261–E270. doi: 10.1152/ajpendo.00676.2007. [DOI] [PubMed] [Google Scholar]
- 44.Svensson P.-A., Olsson M., Andersson-Assarsson J.C., Taube M., Pereira M.J., Froguel P., Jacobson P. The TGR5 gene is expressed in human subcutaneous adipose tissue and is associated with obesity, weight loss and resting metabolic rate. Biochem. Biophys. Res. Commun. 2013;433:563–566. doi: 10.1016/j.bbrc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hao Z., Leigh Townsend R., Mumphrey M.B., Gettys T.W., Yu S., Munzberg H., Morrison C.D., Berthoud H.R. Roux-en-Y Gastric Bypass Surgery-Induced Weight Loss and Metabolic Improvements Are Similar in TGR5-Deficient and Wildtype Mice. Obes. Surg. 2018;28:3227–3236. doi: 10.1007/s11695-018-3297-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Duan H., Ning M., Chen X., Zou Q., Zhang L., Feng Y., Zhang L., Leng Y., Shen J. Design, synthesis, and antidiabetic activity of 4-phenoxynicotinamide and 4-phenoxypyrimidine-5-carboxamide derivatives as potent and orally efficacious TGR5 agonists. J. Med. Chem. 2012;55:10475–10489. doi: 10.1021/jm301071h. [DOI] [PubMed] [Google Scholar]
- 47.Ullmer C., Alvarez Sanchez R., Sprecher U., Raab S., Mattei P., Dehmlow H., Sewing S., Iglesias A., Beauchamp J., Conde-Knape K. Systemic bile acid sensing by G protein-coupled bile acid receptor 1 (GPBAR1) promotes PYY and GLP-1 release. Br. J. Pharmacol. 2013;169:671–684. doi: 10.1111/bph.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sasaki T., Kuboyama A., Mita M., Murata S., Shimizu M., Inoue J., Mori K., Sato R. The exercise-inducible bile acid receptor Tgr5 improves skeletal muscle function in mice. J. Biol. Chem. 2018;293:10322–10332. doi: 10.1074/jbc.RA118.002733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maruyama T., Tanaka K., Suzuki J., Miyoshi H., Harada N., Nakamura T., Miyamoto Y., Kanatani A., Tamai Y. Targeted disruption of G protein-coupled bile acid receptor 1 (Gpbar1/M-Bar) in mice. J. Endocrinol. 2006;191:197–205. doi: 10.1677/joe.1.06546. [DOI] [PubMed] [Google Scholar]
- 50.Sato H., Genet C., Strehle A., Thomas C., Lobstein A., Wagner A., Mioskowski C., Auwerx J., Saladin R. Anti-hyperglycemic activity of a TGR5 agonist isolated from Olea europaea. Biochem. Biophys. Res. Commun. 2007;362:793–798. doi: 10.1016/j.bbrc.2007.06.130. [DOI] [PubMed] [Google Scholar]
- 51.Pellicciari R., Gioiello A., Macchiarulo A., Thomas C., Rosatelli E., Natalini B., Sardella R., Pruzanski M., Roda A., Pastorini E., et al. Discovery of 6alpha-ethyl-23(S)-methylcholic acid (S-EMCA, INT-777) as a potent and selective agonist for the TGR5 receptor, a novel target for diabesity. J. Med. Chem. 2009;52:7958–7961. doi: 10.1021/jm901390p. [DOI] [PubMed] [Google Scholar]
- 52.Hodge R.J., Lin J., Vasist Johnson L.S., Gould E.P., Bowers G.D., Nunez D.J. Safety, Pharmacokinetics, and Pharmacodynamic Effects of a Selective TGR5 Agonist, SB-756050, in Type 2 Diabetes. Clin. Pharmacol. Drug Dev. 2013;2:213–222. doi: 10.1002/cpdd.34. [DOI] [PubMed] [Google Scholar]
- 53.Roden M., Bernroider E. Hepatic glucose metabolism in humans—Its role in health and disease. Best Pract. Res. Clin. Endocrinol. Metab. 2003;17:365–383. doi: 10.1016/S1521-690X(03)00031-9. [DOI] [PubMed] [Google Scholar]
- 54.Home P.D., Pacini G. Hepatic dysfunction and insulin insensitivity in type 2 diabetes mellitus: A critical target for insulin-sensitizing agents. Diabetes Obes. Metab. 2008;10:699–718. doi: 10.1111/j.1463-1326.2007.00761.x. [DOI] [PubMed] [Google Scholar]
- 55.Abdul-Ghani M.A., Jenkinson C.P., Richardson D.K., Tripathy D., DeFronzo R.A. Insulin secretion and action in subjects with impaired fasting glucose and impaired glucose tolerance: Results from the Veterans Administration Genetic Epidemiology Study. Diabetes. 2006;55:1430–1435. doi: 10.2337/db05-1200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.