Abstract
Study objective:
An increasing number of overweight and obese patients are presenting for ambulatory surgical procedures and may be at risk of complications including longer surgeries, longer length of stay (LOS), and possible increase in unanticipated return visits or hospital admissions.
Design:
Observational study using prospectively-collected data.
Setting:
Freestanding and hospital-based ambulatory surgery facilities.
Patients and Interventions:
13,957 patients underwent ambulatory cancer surgery procedures at the Josie Robertson Surgery Center (JRSC) since opening in 2016, and 4591 patients eligible for ambulatory surgery at JRSC underwent surgery at the main hospital during the same timeframe.
Measurements:
We assessed whether BMI was associated with increased operative time, post-operative LOS, hospital transfer after surgery, or hospital readmission or urgent care center visits within 30 days. Using multivariable logistic regression, we assessed whether BMI was associated with decision to do surgery at JRSC controlling for age, ASA score and surgical service.
Main results:
While higher BMI was associated with a higher rate of transfer out of JRSC (p=0.014), the difference in rate was small (mean risk 0.8% for BMI 25 vs 1.3% for BMI 40, difference in risk 0.52%, 95% CI 0.05%, 1.0%). We found no evidence that higher BMI increased the risk of urgent care visits or readmissions within 30 days or outpatient LOS (p=0.7 for all). There was a statistically but not clinically significant difference in operative time for outpatient procedures (p = <0.0001), with a mean operative time of 59 vs 63 min for BMI 25 vs 40. Ambulatory extended recovery patients with higher BMI had shorter operative times (p < 0.0001). Patients with higher BMI were not significantly less likely to undergo surgery at JRSC (84% vs 83% vs 82% probability of treatment at JRSC for BMI 25, BMI 40 or BMI 50, respectively, p=0.089).
Conclusions:
Ambulatory cancer surgeries can be performed safely among clinically eligible patients. Patients with BMI up to 50 or more can be treated safely in an ambulatory setting if they otherwise meet eligibility criteria.
Keywords: Ambulatory surgery, Ambulatory anesthesia, Obesity, Morbidly obese, BMI
1. Introduction
The prevalence of obesity (BMI≥30), including class 3 (severe or extreme obesity, BMI≥40), has increased in recent years. In 1980, an estimated 15% of adults in developed countries had a BMI > 25 [1]. As of 2016, it has been estimated that the proportion of obese adults has risen to nearly 40% in the United States [1,2]. The prevalence of morbid obesity has grown even faster, with a relative increase of 70% in the United States between 2000 and 2010 [3]. Obesity and its coexisting diseases are associated with elevated morbidity and mortality during surgery. Specifically, obesity has been linked to cardiovascular [4,5], pulmonary, [6] renal, and thromboembolic complications [7] during anesthesia and surgery, as well as difficulty with glucose control and other endocrine and metabolic issues [8]. While some of these issues may be related to comorbidities rather than increased BMI alone, obesity itself can also pose challenges. For anesthesiologists, these challenges can include difficulty in monitoring of hemodynamic and respiratory parameters or obtaining intravenous access, higher incidence of difficult airway [9] and complications associated with airway management, [10,11] as well as increased risk of position-related nerve injuries and compartment syndrome. [12] From a surgical perspective, technical difficulties during surgery and increased blood loss, duration of surgery [13], need for reoperation, and risk for infection have been demonstrated. [13]
While previous studies have investigated the question of the safety of ambulatory surgery for obese patients, many of these studies do not completely address this research question. For example, some prior studies on obese patients have been conducted in inpatient or hospital-based ambulatory surgery centers or are limited in the types of patients or procedures included, for example, only bariatric surgery patients. [14] A recent systematic review of the literature identified gaps in existing data that do not adequately assess clinically significant outcomes such as unplanned admission rate and readmission rate in addition to discharge time (or discharge readiness) [15].
The Josie Robertson Surgery Center (JRSC) is an ambulatory surgery facility at Memorial Sloan Kettering Cancer Center (MSKCC) that opened in January 2016 and performs both standard outpatient and advanced ambulatory surgery procedures. Five main surgical services (breast, plastics, gynecology, head and neck, and urology) operate at JRSC, performing with approximately 65% standard outpatient and 35% ambulatory extended recovery (AXR) cases. AXR cases are defined as surgeries which traditionally required traditional two to three day inpatient admissions that are performed in the ambulatory setting with a single overnight stay. Potential AXR procedures were identified by teams of surgeons and anesthesiologists at the MSKCC hospital during the 5 years prior to JRSC opening. Over 9000 procedures were performed in a pilot AXR program during which clinical pathways were developed and comorbidities associated with failure to be discharged after one night were used to identify exclusion criteria for performing surgery at JRSC. These initial exclusion criteria included patients with end-stage renal disease, ASA score 4, AICD (automatic implanted cardioverter-defibrillator), and procedures likely requiring transfusions. While initially patients with BMI≥45 were considered for exclusion, a review of the pilot experience showed that pathway drop-off was not higher in these patients. Instead, BMI≥45 was considered as a screening trigger to closely evaluate an individual patient’s comorbidities, and patients with high BMIs were not automatically excluded. In addition, surgeons generally have scheduled block time at both the main hospital and JRSC and may schedule a given patient’s surgery at the main hospital or JRSC based on the anticipated surgical complexity, patient comorbidities, or, most frequently, patient convenience or other scheduling considerations.
Due to the possibility of adverse outcomes in obese and morbidly obese patients, it is necessary to carefully assess these patients for their fitness for ambulatory surgery, as available resources may make it safer for some obese patients to undergo surgery in a hospital-based rather than a freestanding ambulatory surgery facility. Our experience with a large cohort of high BMI patients undergoing both standard and advanced cancer surgeries at our free-standing ambulatory surgery center allows us to track clinically significant outcomes and examine the safety of performing these surgeries in the ambulatory setting. We aimed to assess whether patients who met all other criteria for treatment at JRSC should instead be treated at the main hospital based on BMI alone. We also compared patients treated at JRSC to those patients who were treated at the main hospital, despite meeting selection criteria for treatment at JRSC, to establish whether BMI played a role in the choice of surgery location and potentially confounded our results through selection bias.
2. Materials and methods
After obtaining approval for this observational study from the Memorial Sloan Kettering Cancer Center Institutional Review Board (IRB) and an IRB waiver for consent (#16–227), we analyzed prospectively-collected data on all patients that underwent surgical procedures from January 1, 2016 to July 1, 2018 at the Josie Robertson Surgery Center. A total of 17,229 procedures were performed at JRSC during this time period. As most patients with>1 surgery had multiple procedures as part of a planned breast reconstruction, we excluded any procedures after the patient’s first procedure (n=3269). Procedures were also excluded if the procedure was not performed under MAC or general anesthesia (n=3), leaving a total of 13,957 JRSC patients in the analysis.
Patients undergoing ambulatory procedures, outpatient or AXR, were eligible for treatment at JRSC. AXR procedures are more complex than typical outpatient surgeries, are managed on defined care pathways, and are scheduled to have a one night overnight stay. The most common AXR procedures include mastectomy with or without immediate tissue expander reconstruction, thyroidectomy, and minimally invasive hysterectomy, prostatectomy, and nephrectomy. A list of AXR and outpatient procedures performed at JRSC is available in Supplementary Table 1.
For patients undergoing traditional outpatient procedures with same day discharge, post-operative length of stay in hours was defined as time from entry into the PACU to discharge home from the PACU. Patients were excluded from the length of stay analysis if they were transferred to the main hospital or underwent re-operation on the same day. For patients undergoing AXR procedures, we assessed the time of discharge on the day after surgery rather than total post-operative length of stay, as total length of stay in these overnight patients is influenced by the time the surgery was performed [16]. Patients were excluded from the discharge time analysis if they were transferred out of JRSC, underwent re-operation on the same day, or did not stay overnight. While “meets discharge criteria” time is sometimes used to separate out logistic issues from clinical ones that delay physical discharge [16], nonclinical issues prolonging LOS or discharge time are actually uncommon in our model.
Our primary goal was to determine whether patients with high BMIs can be safely treated at JRSC. We assessed whether there was an association between BMI and the risk of any transfer out of JRSC after surgery using Wilcoxon rank sum tests. If a significant association was found, we investigated the association between BMI and the most common reasons for transfer, again using Wilcoxon rank sum tests. We also assessed the association between BMI and risk of urgent care center (UCC) visit or hospital readmission at an MSK facility within 30 days after surgery using Wilcoxon rank sum tests. Results were visualized using locally-weighted scatterplot smoothing. We also assessed the association between BMI and post-operative length of stay for outpatient procedures and discharge time for AXR procedures using multivariable linear regression models adjusted for surgery start time. The association between BMI and operative time was tested using linear regression adjusted for procedure class (outpatient or AXR). We did not adjust for OSA in these analyses given the risk of multicollinearity due to the strong association between BMI and OSA. Restricted cubic splines with knots at the tertiles were used to test for non-linearity. Results were visualized using local polynomial smoothing.
Our secondary goal was to assess the process used for selecting patients to have their surgery at JRSC. We compared patient characteristics of the cohort of patients treated at JRSC (N = 13,957) to a separate cohort of patients undergoing the same ambulatory surgery procedures at MSKCC main hospital, by the same surgeons, during the same time frame. This cohort included 5655 JRSC-eligible procedures performed at the MSKCC main hospital between January 1, 2016 and July 1, 2018, with 4594 patients having their first eligible procedure at the main hospital during this time frame. Again, we excluded procedures after the patient’s first procedure (n = 1061) or procedures where patients did not receive MAC or general anesthesia (n = 3), for a total of 4591 patients eligible for analysis. JRSC-eligible surgeries may be performed at the main hospital for both clinical reasons, such as patient comorbidities or surgical complexity, and non-clinical reasons, including scheduling considerations or surgeon or patient preference. To assess whether BMI (treated as a continuous variable) was independently associated with surgery location after controlling for other factors which could affect a patient’s referral to JRSC, we created a multivariable logistic regression model which was adjusted for age, ASA score, and surgical service, as these are strong predictors of surgical risk. The use of surgical service also accounts for type of anesthesia and procedure class. Univariate analyses were two-tailed and an alpha level of 0.05 was used. All analyses were performed using Stata 15 (Stata Corp, College Station, TX). This manuscript adheres to the applicable Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
3. Results
A total of 13,957 surgical procedures performed at JRSC were included in the primary analysis. In this cohort, 4142 patients (30%) were obese (BMI≥30), with 520 patients (3.7%) having a BMI > 40 and 46 (0.3%) patients having a BMI > 50. The maximum BMI of a patient treated in this cohort was 68. Other patient characteristics are presented in Table 1.
Table 1.
Patient characteristics by treatment facility. Data are presented as median (quartiles) or frequency (%).
| Characteristic | JRSC (N=13,957) | Main hospital (N=4591) | p value |
|---|---|---|---|
| Male | 2513 (18%) | 1681 (37%) | <0.0001 |
| Age at surgery | 56 (46, 65) | 59 (47, 68) | <0.0001 |
| Age 65 and older | 3427 (25%) | 1481 (32%) | |
| Age 75 and older | 736 (5.3%) | 421 (9.2%) | |
| BMI category | <0.0001 | ||
| Underweight (< 18.5) | 197 (1.4%) | 58 (1.3%) | |
| Normal (18.5–25) | 5095 (37%) | 1371 (30%) | |
| Overweight (25–30) | 4523 (32%) | 1546 (34%) | |
| Obese | |||
| 30–35 | 2589 (19%) | 903 (20%) | |
| 35–40 | 1018 (7.3%) | 424 (9.2%) | |
| 40–45 | 368 (2.6%) | 173 (3.8%) | |
| 45–50 | 121 (0.9%) | 61 (1.3%) | |
| > 50 | 46 (0.3%) | 55 (1.2%) | |
| ASA score | <0.0001 | ||
| 1 | 447 (3.2%) | 106 (2.3%) | |
| 2 | 8117 (58%) | 1777 (39%) | |
| 3 | 5393 (39%) | 2708 (59%) | |
| Type of anesthesia | <0.0001 | ||
| General | 9115 (65%) | 3934 (86%) | |
| MAC | 4842 (35%) | 657 (14%) | |
| Robotic-assisted procedure | <0.0001 | ||
| No | 11,595 (83%) | 3686 (80%) | |
| Yes | 2362 (17%) | 905 (20%) | |
| Surgical service | <0.0001 | ||
| Breast | 7531 (54%) | 282 (6.1%) | |
| Dental | 8 (< 0.1%) | 11 (0.2%) | |
| Gastric mixed tumor | 252 (1.8%) | 231 (5.0%) | |
| Gynecology | 2002 (14%) | 1253 (27%) | |
| Head and neck | 995 (7.1%) | 1350 (29%) | |
| Plastics | 1225 (8.8%) | 449 (10%) | |
| Urology | 1944 (14%) | 1015 (22%) | |
There were 122 (0.9%) patients transferred to the main hospital or other nearby acute care facility after surgery at JRSC. The most common reasons for transfer were surgical bleeding (35%), cardiac issues (12%), and abnormal lab results (11%). Five patients (4.1%) were transferred for pulmonary events and all five had BMI > 30. The median length of stay for transferred patients was 2 days, with 75% of patients discharged within 3 days. A total of 626 patients (4.5%) visited the UCC within 30 days of surgery, and 287 (2.1%) patients were readmitted to the hospital within 30 days of surgery. One patient treated at JRSC died within 30 days of surgery; this patient had a BMI of 25.8, was not transferred to the main hospital, did not have any UCC visits or readmissions prior to death, and had undergone a palliative procedure for their end-stage cancer. There were no hospital transfers and no readmissions within 30 days among patients with a BMI of 50 or higher. One patient with a BMI > 50 had a UCC visit within 30 days.
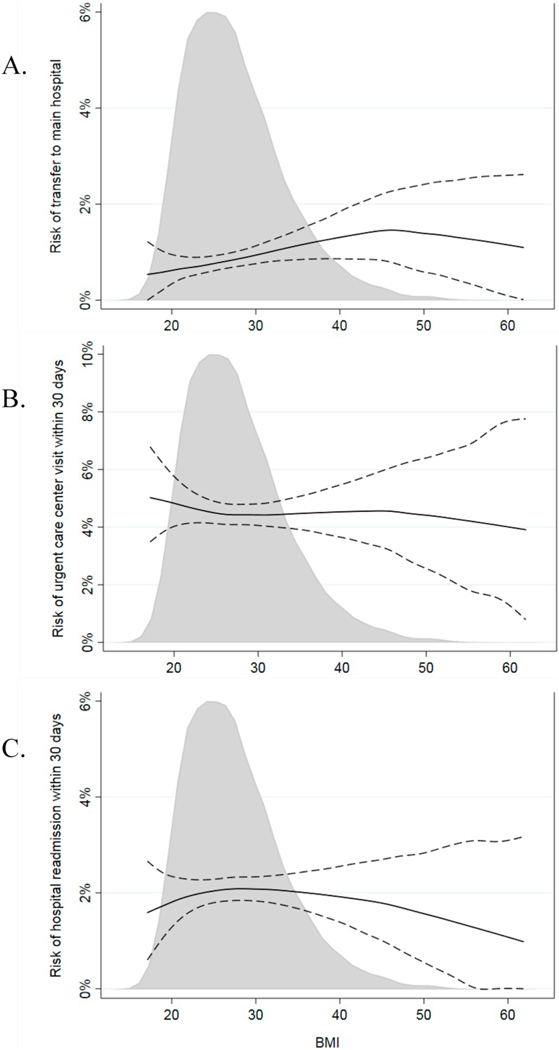
Higher BMI was associated with a higher risk of transfer from JRSC to the main hospital or other acute care facility (p=0.014, Fig. 1A). However, the 95% CI excludes the sort of increase in risk that would make us reconsider the safety of surgery at JRSC for an obese patient: based on univariate logistic regression, the risk of transfer for a patient with BMI 25 is 0.8% and the upper bound of the 95% CI for a patient with BMI 40 is 1.7%, with this 0.9% difference in risk indicating that at least 111 patients with BMI 40 would need to be treated at the main hospital instead of JRSC to prevent one transfer. We then investigated the top two reasons for transfer, which were surgical bleeding and cardiac issues. Among the 43 patients transferred for surgical bleeding, 7 had a BMI > 35. Fifteen patients were transferred for cardiac issues, with 3 of these patients having BMI > 35. Ten of these cardiac transfers were due to arrhythmias, 4 to hypotension, dyspnea or risk of ischemia, and one for uncontrolled hypertension. While there was a significant association between BMI and cardiac-related transfers (p=0.001), the overall rate of cardiac-related transfer was very low (N=15 (0.11%)) and we did not consider the 0.2% difference in risk (0.07% risk for BMI 25 vs 0.28% risk for BMI 40) to be clinically relevant. We found no evidence of a significant association between BMI and bleeding-related transfers (p=0.7), UCC visits within 30 days (p=0.7, Fig. 1B), or hospital readmissions within 30 days (p=0.7, Fig. 1C).
Fig. 1.
Risk of A) transfer out of JRSC; B) urgent care center visit within 30 days; or C) readmission within 30 days, estimated using locally-weighted scatterplot smoothing with 95% confidence interval (dashed lines) and density plot of BMI values.
ap=0.014; bp=0.7; cp=0.7 (p-values from Wilcoxon rank-sum tests).
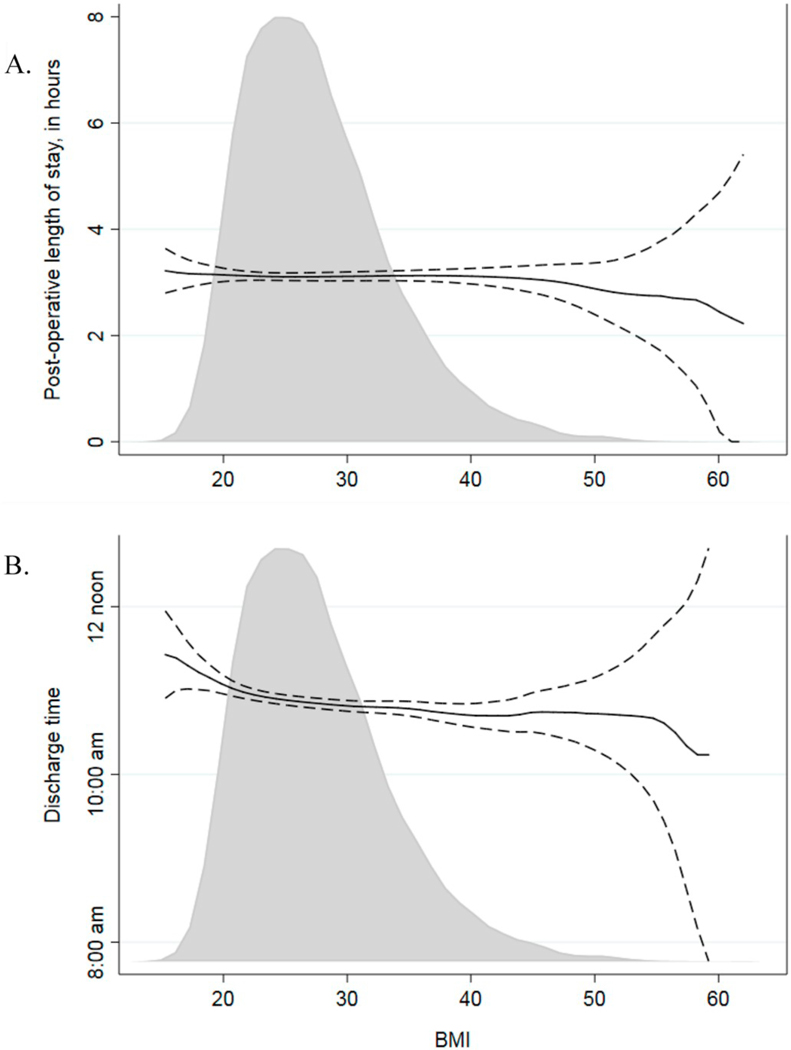
Median length of stay for patients undergoing outpatient procedures was 2.5 h (Quartile 1 2.0, Quartile 3 3.3), and we found no evidence of an effect of BMI on post-operative length of stay among outpatient procedures (p=0.7, Fig. 2A). Median discharge time for patients undergoing AXR procedures was 10:40 am (quartiles 9:48 am, 11:40 am). While we did find a significant decrease in discharge time associated with higher BMIs in patients undergoing AXR procedures, this was consistent with only a 0.74 min earlier discharge time associated with each one point increase in BMI (95% CI 0.27 min, 1.2 min, p=0.002, Fig. 2B).
Fig. 2.
A) Post-operative length of stay for outpatient procedures and B) discharge time for AXR procedures, estimated using an Epanechnikov kernel-weighted local polynomial regression with 95% CI (dashed lines) and density plot of BMI values.
ap=0.7; bp=0.002 (p-values from linear regression models adjusted for surgery start time).
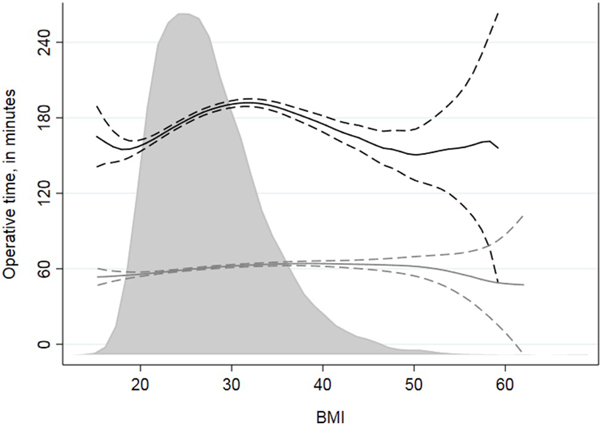
Median operative time was 52 min (quartiles 34, 76) for outpatient procedures and 172 min (quartiles 120, 229) for AXR procedures. For the outcome of operative time, we found a significant interaction between BMI and procedure class (OP vs AXR) (p < 0.0001), indicating that the effect of BMI on operative time was different for patients undergoing outpatient and AXR procedures. Despite a statistically significant effect (p < 0.0001), there was little change in operative time by BMI for outpatient procedures (Fig. 3). For example, based on our logistic regression model, the average outpatient operative time for a patient with BMI 25 was 59 min versus 63 min for a patient with BMI 40. For AXR procedures, operative time increased slightly as BMI increased up to 35 and then decreased in patients with BMI over 40 (p < 0.0001). This decrease could be due to a conservative selection process for these procedures, which would mean that patients with higher BMIs who had comorbidities or more complex procedures were less likely to undergo treatment at JRSC.
Fig. 3.
Operative time for outpatient procedures (gray lines) and AXR procedures (black lines), estimated using an Epanechnikov kernel-weighted local polynomial regression with 95% CI (dashed lines) and density plot of BMI values.
p < 0.0001 (outpatient); p < 0.0001 (AXR) (p-values from univariable linear regression models).
We then compared the patient populations treated at JRSC to those having the same procedures at the main hospital to investigate the selection process used to identify patients for referral to JRSC. In addition to the 13,957 JRSC procedures, a total of 4591 procedures performed at the main hospital were included in this analysis. In the main hospital cohort, 35% of patients were obese (BMI≥30), with 287 (6.3%) patients having a BMI > 40 and 55 (1.2%) having a BMI > 50, with a maximum BMI of 70.
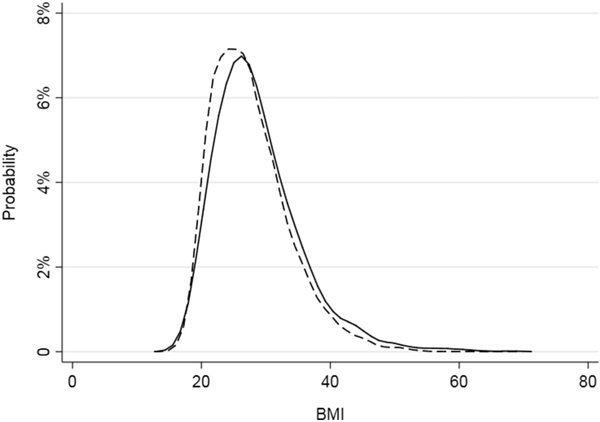
Patients treated at the main hospital were significantly more likely to be older, male, and have higher BMI and higher ASA scores (all p < 0.0001, Table 1). Compared to JRSC, where the majority of procedures were in the breast service, patients at main hospital were more likely to undergo head and neck and gynecology surgeries (p < 0.0001, Table 1). They were also more likely to undergo roboticassisted surgery and surgery under general anesthesia (p < 0.0001 for both). While significant (p < 0.0001), the difference in BMI for patients treated at JRSC and at the main hospital was not large (Fig. 4). Given that we found statistically significant differences in patient and surgical characteristics between patients treated at the main hospital and at JRSC, we then conducted a multivariable regression analysis to assess the selection process used to choose whether JRSC-eligible patients should be treated at JRSC or at the main hospital. We did not find a significant association between BMI and the choice to do surgery at JRSC after controlling for age, ASA score, and surgical service (OR 0.97, 95% CI 0.94, 1.00, p=0.089). The average patient eligible for surgery at JRSC had an 84% probability of being treated at JRSC, with little difference in probability by BMI: an average JRSC-eligible patient with BMI 25 had an 84% chance of treatment at JRSC vs. an 83% probability for a BMI of 40 and an 82% probability for a BMI of 50.
Fig. 4.
Distribution of BMI for patients treated at Josie Robertson Surgery Center (dashed line) and at the main hospital (solid line).
4. Discussion
BMI was not significantly associated with length of stay, UCC visits within 30 days, or readmissions within 30 days in this JRSC cohort of patients undergoing ambulatory surgery. While we found that BMI was associated with transfer from JRSC to the main hospital, the difference in risk of transfer based on BMI was small and not clinically significant. Operative times for patients undergoing AXR procedures did increase as BMI increased up to approximately 35; operative times decreased for BMIs higher than 35, potentially due to the conservative selection of patients with extreme values of BMI and associated comorbidities undergoing complex ambulatory surgeries at a freestanding facility. We have confirmed that using our current patient selection process allows us to select appropriate candidates for ambulatory surgery at JRSC, even those who are morbidly or super-morbidly obese and undergoing advanced ambulatory surgery procedures, and treat them safely at our facility.
While we were able to identify some statistically significant associations between BMI and post-operative outcomes in our cohort of nearly 14,000, the effect of BMI on these outcomes was small and not clinically relevant. Other studies have found similar results, showing no clinically important associations between BMI and post-operative outcomes including length of stay and unanticipated hospital admissions or readmissions. In a small study of ambulatory surgery which included 235 patients with BMI≥40, Hofer et al. found that obesity was not independently associated with unplanned admission [17]. A systematic review on the selection of obese patients for ambulatory surgery also found that, overall, there was no increased rate of hospital admissions in obese patients [15]. One study of ambulatory surgery did find an association between BMI and unplanned admissions [18]. However, in this study the risk of hospital admission was significantly higher only among patients with BMIs between 30 and 35. No significant increase in risk was seen for patients with BMI > 35, the population we are most concerned about for ambulatory surgeries. The results of this study were not consistent with our study, in which we used a larger cohort and assessed a full range of BMI values rather than BMI categories.
We did not address specific types of complications in our study, although we chose endpoints that would reflect whether a patient experienced a more serious complication from the patient perspective: transfer out of JRSC after surgery and visits to the urgent care center or readmission to the hospital within 30 days. Several studies have reported on complications, with findings that patients with higher BMI were at increased risk of post-operative surgical complications, such as wound complications [7], or breathing-related complications, such as hypoxemia or need for airway maneuvers [19]. However, even despite this increased risk of complications, these studies did not find a subsequent increased risk of unplanned admission or length of stay based on BMI. Among patients undergoing major surgery, Sood et al. found no increased risk of hospital readmission and reported that for several procedure types obese patients had a lower risk of prolonged length of stay, likely due to conservative selection of obese patients for surgery [7]. Our analysis of patients treated from 2016 to 2018 is consistent with the results of a study by Rosero et al., who studied a matched cohort of obese and non-obese patients from 2006 and also reported no association between BMI and either unplanned admission or post-operative length of stay [19]. Similar results for length of stay were also seen in studies focusing on inpatient cancer surgeries: both Merkow et al.’s study [20] on colectomies for cancer and Mullen et al.’s study [21] on major intra-abdominal cancer surgery found no evidence of a difference in LOS by BMI category when taking into account other patient and disease characteristics.
Several studies found significant differences in operative time by BMI, although in most studies the difference was statistically but not clinically significant. Mullen et al. found that, while statistically significant, the difference in operative times between obese and non-obese patients was on the order of only several minutes [21]. Hughes et al. reported that 42 studies in a systematic review of major abdominal surgeries for cancer found longer operative times for patients with higher BMI, but that the “relative incremental increase in operative time among most studies was small, suggesting that this factor may serve as a poor estimate of any effect of obesity on surgical complexity” [22]. These small differences in operative time are consistent with our finding that operative time for same-day procedures was not clinically significantly affected by BMI. In AXR procedures, which are usually longer and more complex, the patients with the highest BMIs had shorter operative times than others, possibly due to a conservative selection process which would exclude obese patients with more comorbidities from undergoing the most complex and extensive procedures at JRSC.
The main limitation of our study is that patient selection into this cohort was subject to some level of individual clinical judgment, introducing the risk of selection bias. Patients who undergo surgery at JRSC were chosen based on a clinical evaluation of their overall health status and comorbidities, rather than any single parameter such as BMI. As such, obesity (similar to a history of cardiac or pulmonary disease) served as a flag to trigger further assessment of the patient’s individual comorbidity-related risks. The results of this analysis therefore apply to a population of obese patients who were specifically selected into the cohort based on a careful assessment of their overall health and fitness for ambulatory surgery, and these patients likely have better health and fewer comorbidities than patients who were not selected for surgery at JRSC. We have not identified any randomized controlled trials where patients across all BMIs were randomized to a freestanding vs hospital-based ambulatory facility, and several studies specifically reported on similar selection bias issues [7,17,18]. The systematic review by Joshi et al. also concludes that consideration of comorbid conditions is important when identifying appropriate candidates for ambulatory surgery, and these considerations were also made in selecting patients for treatment at our facility [15]. Therefore, these results are generalizable to those overweight and obese patients who are candidates for ambulatory surgery based on an individualized assessment and clinical judgment, and not necessarily all overweight or obese patients. It is also probable that we are underestimating overall rates of UCC visits and readmissions, as we are only capturing those visits and readmissions in the MSKCC system, but this limitation is the same for all our patients and should not influence detecting differences between groups. Patients who were transferred out of JRSC were transferred via our contracted ambulance service to our main hospital or to a nearby tertiary care center, both located about six city blocks from our facility. Therefore, our results may not be generalizable to facilities located further from nearby inpatient hospitals. An additional limitation is that our population is limited to a few specific cancer surgeries and may not be generalizable to other types of ambulatory procedures.
Standard outpatient and advanced ambulatory cancer surgeries can be performed safely among clinically eligible patients. Obesity alone should not be a contraindication for ambulatory cancer surgery. Procedures in patients with high BMI, morbid or super-morbid obesity, can be safely performed in an ambulatory setting if the patients otherwise meet eligibility criteria.
Supplementary Material
Acknowledgments
Disclosures
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748 and the Kimmel Center for Prostate and Urologic Cancer.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jclinane.2019.05.003.
References
- [1].Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. Jama 2018;319:1723–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the US. Int J Obes (Lond) 2013;37:889–91. (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].De Lorenzo A, Glerian L, Amaral AC, Reis TB, Lima RSL. “Metabolically healthy” obesity: prevalence, clinical features and association with myocardial ischaemia. Obes Res Clin Pract 2017;11:315–23. [DOI] [PubMed] [Google Scholar]
- [5].Kivimaki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2017;2:e277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].De Oliveira GS Jr., McCarthy RJ, Davignon K, Chen H, Panaro H, Cioffi WG. Predictors of 30-day pulmonary complications after outpatient surgery: relative importance of body mass index weight classifications in risk assessment. J Am Coll Surg 2017;225 312–23.e7. [DOI] [PubMed] [Google Scholar]
- [7].Sood A, Abdollah F, Sammon JD, Majumder K, Schmid M, Peabody JO, et al. The effect of body mass index on perioperative outcomes after major surgery: results from the National Surgical Quality Improvement Program (ACS-NSQIP) 2005–2011. World J Surg 2015;39:2376–85. [DOI] [PubMed] [Google Scholar]
- [8].Global BMIMC, Di Angelantonio E, Bhupathiraju Sh N, Wormser D, Gao P, Kaptoge S, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016;388:776–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wang T, Sun S, Huang S. The association of body mass index with difficult tracheal intubation management by direct laryngoscopy: a meta-analysis. BMC Anesthesiol 2018;18:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Moon TS, Joshi GP. Are morbidly obese patients suitable for ambulatory surgery? Curr Opin Anaesthesiol 2016;29:141–5. [DOI] [PubMed] [Google Scholar]
- [11].Moon TS, Fox PE, Somasundaram A, Minhajuddin A, Gonzales MX, Pak TJ, et al. The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth 2019;33:96–102. [DOI] [PubMed] [Google Scholar]
- [12].Passannante AN, Rock P. Anesthetic management of patients with obesity and sleep apnea. Anesthesiol Clin North America 2005;23:479–91. [vii]. [DOI] [PubMed] [Google Scholar]
- [13].Tjeertes E, Hoeks SSE, Beks S, Valentijn TTM, Hoofwijk A, Stolker R. Obesity — a risk factor for postoperative complications in general surgery? BMC Anesthesiol 2015;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Montgomery KF, Watkins BM, Ahroni JH, Michaelson R, Abrams RE, Erlitz MD, et al. Outpatient laparoscopic adjustable gastric banding in super-obese patients. Obes Surg 2007;17:711–6. [DOI] [PubMed] [Google Scholar]
- [15].Joshi GP, Ahmad S, Riad W, Eckert S, Chung F. Selection of obese patients undergoing ambulatory surgery: a systematic review of the literature. Anesth Analg 2013;117:1082–91. [DOI] [PubMed] [Google Scholar]
- [16].Assel MJ, Laudone VP, Twersky RS, Vickers AJ, Simon BA. Assessing rapidity of recovery after cancer surgeries in a single overnight short-stay setting. Anesth Analg 2019. [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hofer RE, Kai T, Decker PA, Warner DO. Obesity as a risk factor for unanticipated admissions after ambulatory surgery. Mayo Clin Proc 2008;83:908–16. [DOI] [PubMed] [Google Scholar]
- [18].Whippey A, Kostandoff G, Paul J, Ma J, Thabane L, Ma HK. Predictors of unanticipated admission following ambulatory surgery: a retrospective case-control study. Can J Anaesth 2013;60:675–83. [DOI] [PubMed] [Google Scholar]
- [19].Rosero EB, Joshi GP. Nationwide use and outcomes of ambulatory surgery in morbidly obese patients in the United States. J Clin Anesth 2014;26:191–8. [DOI] [PubMed] [Google Scholar]
- [20].Merkow RP, Bilimoria KY, McCarter MD, Bentrem DJ. Effect of body mass index on short-term outcomes after colectomy for cancer. J Am Coll Surg 2009;208:53–61. [DOI] [PubMed] [Google Scholar]
- [21].Mullen JT, Davenport DL, Hutter MM, Hosokawa PW, Henderson WG, Khuri SF, et al. Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol 2008;15:2164–72. [DOI] [PubMed] [Google Scholar]
- [22].Hughes TM, Shah K, Noria S, Pawlik T. Is BMI associated with post-operative complication risk among patients undergoing major abdominal surgery for cancer? A systematic review. J Surg Oncol 2018;117(5):1009–19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.