Abstract
BACKGROUND AND OBJECTIVE:
To characterize the burden of eye disease and the utility of teleophthalmology in nursing home patients, a population with ophthalmic needs not commensurate with care received.
PATIENTS AND METHODS:
Informed consent was obtained from 78 California Bay Area skilled nursing facility patients. Near visual acuity (VA) and anterior/posterior segment photographs were taken with a smartphone-based VA app and ophthalmic camera system. The Nursing Home Vision-Targeted Health-Related Quality of Life questionnaire was also administered. Risk factors for visual impairment were assessed. Institutional review board approval was obtained from Stanford University.
RESULTS:
Cataracts (51%), diabetic retinopathy (DR) (12%), optic neuropathy (12%), and age-related macular degeneration (AMD) (10%) were common findings; 11.7% had other referral-warranted findings. AMD and DR correlated with a higher risk of poor VA, with adjusted odds ratios of 22 (P = .01) and 43 (P = .004).
CONCLUSIONS:
This study demonstrated a high prevalence of poor VA and ophthalmic disease in the nursing home population impacting quality of life. Smartphone-based teleophthalmology platforms have the potential to increase access to eye care for nursing home patients.
INTRODUCTION
According to the World Health Organization, adults older than 50 years of age are at higher risk for vision impairment.1 Prevalence of vision impairment is even higher in nursing homes, where a significant number of these adults reside. Compared to their noninstitutionalized peers, nursing home residents have a three- to 15-fold increase in incidence of visual impairment, depending on the geographical population and study setting.2-6 Rates of ophthalmic disease are also high in this population, with one study finding incidences in nursing home residents of cataract, macular degeneration, and glaucoma to be 37% to 54%, 7% to 29%, and 4% to 10%, respectively.7,8
Decreased visual function has been found to diminish quality of life through decreased functional ability as measured by the Barthel index, decreased activities of daily living independence, decreased mobility, increased fall risk, higher rates of depression, and negative self-reported impact on mental and physical wellbeing.9-13
Current American Academy of Ophthalmology guidelines recommend that adults 55 to 64 years have a comprehensive eye evaluation every 1 to 3 years, whereas individuals 65 years and older should be examined every 1 to 2 years, even if asymptomatic.14 Despite these guidelines and the high prevalence of visual impairment and eye disease in this vulnerable population, a study conducted in Alabama nursing homes demonstrated that 66% of patients had no documented eye exam, though 90% had insurance coverage. Another study found that only 46% of nursing home patients had seen an eye care professional in the last 2 years.15 Possible barriers to care include limited transportation resources, delay of specialty care until problems become significant, shortage of eye care professionals, and patients’ diminished sense of importance regarding regular eye exams.2,4,16
A telehealth study conducted in long-term care facilities in Brisbane, Australia, demonstrated that 5% of external specialty consults were to ophthalmology, and all 40 of them required transport to an ophthalmologist.17 Teleophthalmology is a potential method for addressing accessibility barriers and supporting the increased need for ophthalmic care in the nursing home setting. Smartphone-based platforms have emerged as promising modalities to expand accessibility to teleophthalmology due to their portability. The Paxos ophthalmic camera and visual acuity testing app originally developed at Stanford University and later Verana Health (former Digisight Technologies) are examples of such a platform, one that has been previously validated with 91% sensitivity and 99% specificity to detect gradations of diabetic retinopathy (DR) through measurements of visual acuity (VA) and acquisition of anterior and posterior segment photographs remotely graded by an ophthalmologist.18
The aim of this study was to characterize the prevalence of ophthalmic disease and visual impairment in the ethnically and socioeconomically diverse geriatric nursing home population of the California Bay Area that, to our knowledge, has not previously been studied. The use of smartphone-based screening tools in this study serves as a proof-of-concept for teleophthalmology to address the ophthalmic needs of this population.
PATIENTS AND METHODS
Population
From three skilled nursing facilities (SNFs) in the San Francisco Bay Area, specifically Santa Clara and San Mateo counties, 78 patients were recruited. Of current residents invited to participate, those who provided informed consent were deemed eligible if they (1) were 55 years or older and (2) scored 13 or higher on a Mini-Mental State Exam.19 Patient medical records at the SNFs were reviewed for age, sex, race, past ocular history, and other medical diagnoses. Institutional review board approval was granted by Stanford University, and the study was conducted in compliance with the principles of the Declaration of Helsinki.
Assessment
Near VA and contrast sensitivity were measured with Paxos Checkup, a smartphone-based near visual acuity testing application.20 Personnel trained on Paxos Checkup conducted all assessments with patients’ own corrective lenses or a +2.5 diopter lens held in front of the eye as needed. Anterior and posterior segment photographs were taken with the Paxos Scope ophthalmic camera system coupled to an iPhone (Apple, Cupertino, CA).18,21,22 Anterior and posterior photographs were reviewed and graded remotely by an ophthalmologist masked to patient identifiers. Smartphone-acquired data were uploaded to a secure HIPAA-compliant server.
To measure quality of life, the Nursing Home Vision-Targeted Health-Related Quality of Life (NHVQoL) questionnaire was administered. The questionnaire consists of nine subcategories: general vision; reading; ocular symptoms; mobility; psychological distress; activities of daily living, social activities, and hobbies; adaptation; and coping. Results were scored according to the provided scoring algorithm, with values ranging from 0 (lowest level of function) to 100 (highest level of function.23
Statistical Analysis
Descriptive statistics were calculated for prevalence of ophthalmic disease and vision impairment, range of visual function, quality of life, and demographic factors. Univariate and multivariate logistic regression analyses were performed to assess structure-function correlations between diagnoses ascertained by history and photography and level of visual function (VA, contrast sensitivity, and NHVQoL score).
RESULTS
Of the 78 patients who participated in this study, the mean age was 77 years ± 11 years. Males (51%) and females (49%) were approximately equally represented in an ethnically diverse sample that had Caucasian (65%), Latino (17%), Asian (10%), and African American (6%) representation.
Functional vision measurements including VA and contrast sensitivity are summarized in Table 1. Mean scores for the nine subscales of the NHVQoL questionnaire can be found in Table 2.
TABLE 1.
Visual Acuity and Contrast Sensitivity Measurements
| Near VA | ||
|---|---|---|
| ETDRS letters, mean ± SD | Better eye | 53 ± 17 |
| Worse eye | 41 ± 17 | |
| Number of patients, % | < 20/40 | 57 (73%) |
| ≤ 20/200 | 23 (29%) | |
| Contrast Sensitivity | ||
| LogCS, mean ± SD | Better eye | 1.1 ± 0.4 |
| Worse eye | 0.7 ± 0.5 | |
| Number of patients, % | < 1.5 | 62 (79%) |
| < 0.9 | 24 (31%) | |
ETDRS letters were presented to the patients using forced multiple-choice, single-letter discriminations at 14 inches. Mean number of letters identified in the better and worse eye and standard deviation were reported and converted to equivalent Snellen scores. A 5-letter difference was equivalent to one Snellen line.
VA = visual acuity; ETDRS = Early Treatment Diabetic Retinopathy Study; SD = standard deviation
TABLE 2.
Mean Quality of Life Scores and Standard Deviations for Each of the Nine Subcategories in the NHVQoL Questionnaire
| Quality of Life Scale (0-100) | |
|---|---|
| Mean ± SD | Overall |
| General vision | 70 ± 25 |
| Reading | 83 ± 22 |
| Ocular symptoms | 84 ± 19 |
| ADLs | 97 ± 9 |
| Mobility | 92 ± 12 |
| Activities | 89 ± 16 |
| Psychological | 81 ± 25 |
| Adapting | 85 ± 26 |
| Social | 91 ± 16 |
NHVQoL = Nursing Home Vision-Targeted Health-Related Quality of Life; ADLs = activities of daily living; SD = standard deviation
Anterior and posterior segment photographs were available for 77 of the 78 patients with findings summarized in Table 3 and example images shown in Figures 3 and 4. Nine patients (11.7%) had referral-warranted findings in their anterior or posterior segment photography that were not previously documented in their medical records. “Referral-warranted” was defined as any abnormal finding for a disease that may need future treatment. These included visually significant cataract (2), referral-warranted DR (3), wet age-related macular degeneration (AMD) conversion (1), hypertensive retinopathy (2), and epiretinal membrane (1).
TABLE 3.
Summary of Anterior and Posterior Segment Findings
| Anterior Segment Findings | |
|---|---|
| n (%) | |
| Cataract | 39 (51%) |
| Pseudophakia | 26 (34%) |
| Iris nevus | 4 (5%) |
| Peripheral iridotomy | 2 (3%) |
| Uveitis | 1 (1%) |
| Posterior Segment Findings | |
| n (%) | |
| Other fundus abnormalities | 10 (13%) |
| Diabetic retinopathy | 9 (12%) |
| Optic neuropathy | 9 (12%) |
| AMD | 8 (10%) |
Percentages are based on the 77 patients for whom anterior and posterior segment photographs were available. Other fundus abnormalities included vascular abnormalities (tortuosity, hypertensive retinopathy), pigmentary retinopathy, choroidal nevus, and epiretinal membrane.
AMD = age-related macular degeneration
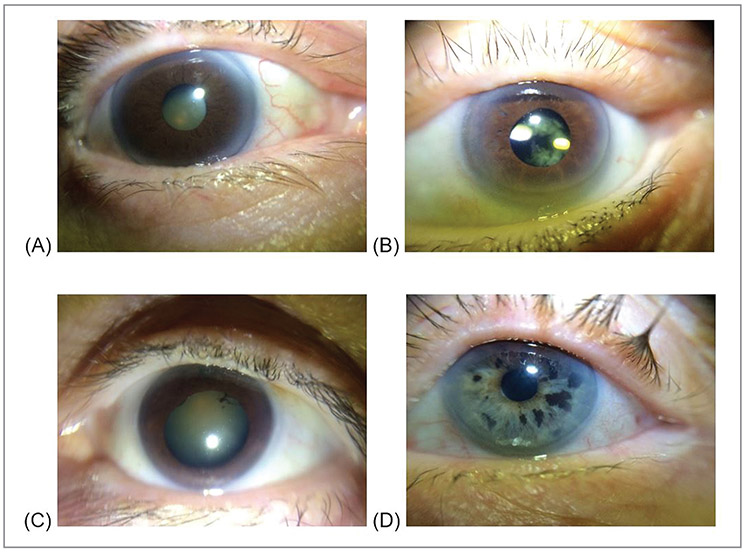
Figure 3.
Example anterior segment photographs taken with the Paxos Scope showing (A) cataract, (B) pseudophakia with posterior capsular opacification, (C) cataract with posterior synechiae, and (D) suspicious iris nevi.
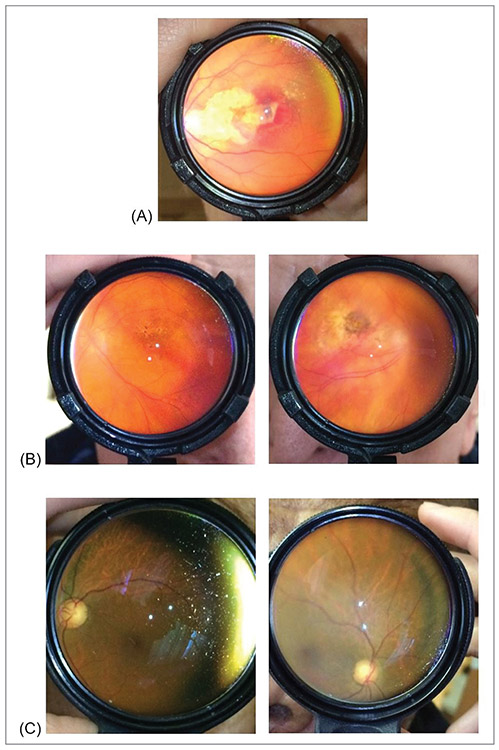
Figure 4.
Example posterior segment fundus photographs taken with Paxos Scope showing (A) neovascular age-related macular degeneration (AMD) with active choroidal neovascular membrane and hemorrhage, (B) high-risk intermediate AMD and advanced dry AMD with geographic atrophy, and (C) asymmetric disc cupping.
Univariate and multivariate logistic regression analyses were performed to evaluate the association between different factors and poor VA (≤ 20/200). Crude and adjusted odds ratios (ORs) were calculated for age, sex, race, and ophthalmic pathology. Male sex had a protective adjusted OR of 0.06 (P = .003). Patients with AMD and DR had a higher risk of poor VA, with adjusted ORs of 22 (P = .01) and 43 (P = .004), respectively (Table 4).
TABLE 4.
Risk Factors for Poor VA (≤ 20/200)
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR | P Value | OR | P Value | |
| Age | 1.1 | .02 | 1.1 | .14 |
| Male Sex | 0.1 | .001* | 0.06 | .003* |
| Race | ||||
| Caucasian | Ref | Ref | Ref | Ref |
| African American | 0.8 | .06 | 1.9 | .65 |
| Latino | 2.0 | .28 | 3.9 | .19 |
| Asian | 1.9 | .41 | 0.8 | .84 |
| Cataract | 6 | .10 | 10.1 | .11 |
| Pseudophakia | 4.4 | .19 | 0.9 | .97 |
| AMD | 11 | .006* | 22 | .01* |
| Diabetic Retinopathy | 7.2 | .01* | 43 | .004* |
| Optic Neuropathy | 0.3 | .28 | ||
| Other Fundus | 3.2 | .09 | ||
Odds ratio calculated using univariate and multivariate logistic regression.
Indicates P values < .05
VA = visual acuity; OR = odds ratio; Ref = reference; AMD = age-related macular degeneration
DISCUSSION
This study was conducted to evaluate the prevalence of visual impairment and eye disease within a specific nursing home population in the Bay Area, specifically within Santa Clara and San Mateo counties. The final sample size ended up being representative of the ethnic diversity within these regions. According to census data, San Mateo County has a population of 60.6% Caucasian, 29.6% Asian, 24.5% Latino, and 2.8% African American, whereas Santa Clara county has a distribution of 53.8% Caucasian, 37.5% Asian, 25.6% Latino, and 2.8% African American.24,25 To our knowledge, this is the first study to evaluate the prevalence of visual impairment and eye disease in the Bay Area nursing home population. One limitation of this study was low participation rates and a smaller sample size, which could have resulted in biased estimates of prevalence rates in this population. Future studies could strengthen participation by including more nursing homes in the geographic area.
A large proportion of patients in this nursing home setting were found to have impaired or diminished VA (73%) and contrast sensitivity (79%). Prevalence of visual impairment (VA < 20/40) was higher than previously reported values found in other geographical regions in the U.S.: 18.8%,3 57%,2 70%,26 and 29.11%.27 Prevalence of eye disease is also comparable to a previous study conducted in Baltimore nursing homes, which found the following incidences: cataract (37% to 54%) and AMD (7% to 29%). The prevalence of DR (12%), however, was much higher than the 2.3% of participants with signs of DR as found in the Blue Mountains eye study.12
Vision quality of life as determined by the NHVQoL was most affected by problems with general vision (70 ± 25), psychological (81 ± 25), reading (83 ± 22), and ocular symptoms (84 ± 19). Table 5 compares previous studies utilizing the NHVQoL questionnaire in nursing home populations. Variation in the reported NHQVoL scores between studies may be affected by interdependent factors including location, mean age, sex, socio-economic status of patients within the population, and incidence of pathologies within the population. Determining the specific effects of these factors on the NHQVoL scores would require a more in-depth analysis of the previously published data, though the variations themselves underscore the benefits of evaluating survey scores and corresponding prevalence of disease within specific populations before drawing population-specific conclusions or proceeding with interventions.
TABLE 5.
Comparison of Previously Reported Quality of Life Mean Scores and Standard Deviations for the Nine Subcategories in the NVHQoL Questionnaire
| This Study | Dreer 2007 | Dev 2014 | Lamoureux 2009 | |
|---|---|---|---|---|
| Location | Bay Area, CA | Birmingham, AL | Kathmandu Valley, Nepal | Victoria, Australia |
| Mean Age | 77 ± 11 | 82 ± 7.7 | 75 ± 7.12 | 83.9 ± 9.9 |
| Male | 51% | 16% | 33.54% | 40% |
| NHQVoL Scores (Mean ± SD) | ||||
| General Vision | 70 ± 25 | 64 ± 21 | 43.39 ± 22.11 | 77.49 ± 20.13 |
| Reading | 83 ± 22 | 78 ± 28 | 62.39 ± 24.27 | 75.78 ± 32.19 |
| Ocular Symptoms | 84 ± 19 | 69 ± 29 | 41.38 ± 11.74 | 90.22 ± 13.92 |
| ADLs | 97 ± 9 | 94 ± 15 | 64.85 ± 18.18 | 94.78 ± 12.57 |
| Mobility | 92 ± 12 | 86 ± 16 | 63.00 ± 19.08 | 90.55 ± 12.97 |
| Activities | 89 ± 16 | 86 ± 22.6 | 64.10 ± 22.46 | 75.04 ± 22.93 |
| Psychological | 81 ± 25 | 67 ± 23 | 37.28 ± 23.41 | 85.78 ± 21.91 |
| Adapting | 85 ± 26 | 85 ± 24 | 40.36 ± 22.57 | 85.78 ± 21.91 |
| Social | 91 ± 16 | 89 ± 17 | 58.83 ± 17.22 | 91.63 ± 16.62 |
NVHQoL = Nursing Home Vision-Targeted Health-Related Quality of Life; ADLs = activities of daily living; SD = standard deviation
Though many of the mean scores for the nine subscales in this study were similar to or higher than other studies, any significant decrease from 100 (which indicates highest level of function) as was noted in general vision, psychological, reading, and ocular symptoms, warrants attention and potential intervention. By identifying specific domains in which quality of life is most affected, future public health initiatives and screening programs can be directed toward these areas. For example, general vision problems can potentially be attributed to treatable refractive error and cataract which can be addressed if detected through screening programs.3,16 Future work should be directed towards elucidating the underlying causes for lower scores in these subscales.
To that end, this study found that female sex, AMD, and DR were risk factors associated with poor vision, defined as 20/200 or less. AMD and DR are both pathologies for which, if detected promptly, interventions can slow progression. Undetected and untreated, patients are at greater risk for developing poor vision, which in previous studies noted above can lead to decreased quality of life and poor health outcomes. These findings further support the need for improved screening and increased rates of comprehensive ophthalmic exams in the nursing home to catch these pathologies earlier and thus improve quality of life and health outcomes for this population.
The smartphone-based ophthalmic camera and visual acuity testing app that were used in this study serve as proof-of-concept for the use of universal ophthalmic telemedicine as an accessible nursing home screening tool. Using this system to capture anterior and posterior segment photographs, nine patients (11.7%) were found to have referral-warranted findings that were not noted in their medical records. These were new abnormal findings that suggested disease that may need future treatment and would benefit from a follow-up visit with an ophthalmologist.
In concordance with previous studies, this study suggests a high prevalence of poor VA and ophthalmic disease in the nursing home population. To better detect and address these findings, telemedicine options like the mobile platform evaluated in this study provide screening solutions that are low cost, allow for remote analysis of patient data, and may be useful for the detection and triage of referral-warranted eye disease.
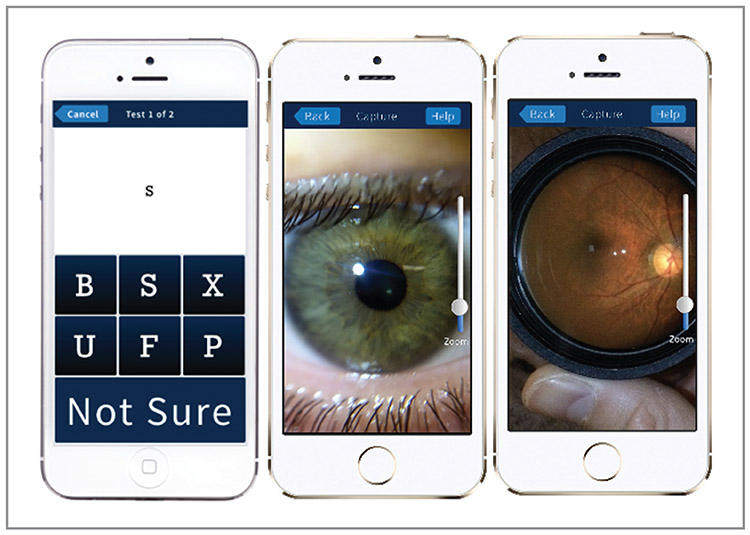
Figure 1.
Photograph of the Paxos Scope smartphone adapter. An indirect ophthalmoscopy lens was fitted to the adapter, which together were coupled and aligned to the camera lens of an iPhone.
Figure 2.
Screen shots of the visual acuity (VA) testing app used with the Paxos Scope. (Left) VA measurement using an interactive alphabet letter match. (Middle) An example of an anterior segment photograph captured with the Paxos Scope adapter. (Right) An example of a dilated fundus photograph taken with the same adapter. Photographs and data collected through the app are securely uploaded through a HIPAA-compliant telemedicine platform (Verana Health, formerly Digisight Technologies).
Acknowledgments
Supported by unrestricted grants to the Departments of Ophthalmology at both Stanford and USC from Research to Prevent Blindness (RPB), New York, New York, and a departmental P30-EY026877 core grant to Stanford from the National Eye Institute.
Contributor Information
Krystal Y. Lai, Byers Eye Institute, Stanford University, Palo Alto, California.
Mythili P. Pathipati, Byers Eye Institute, Stanford University, Palo Alto, California.
Mark S. Blumenkranz, Byers Eye Institute, Stanford University, Palo Alto, California.
Loh-Shan Leung, Byers Eye Institute, Stanford University, Palo Alto, California; VA Palo Alto Health Care System, Palo Alto, California.
Darius M. Moshfeghi, Byers Eye Institute, Stanford University, Palo Alto, California.
Brian C. Toy, Roski Eye Institute, Department of Ophthalmology, University of Southern California, Los Angeles, California.
David Myung, Byers Eye Institute, Stanford University, Palo Alto, California; VA Palo Alto Health Care System, Palo Alto, California.
REFERENCES
- 1.World Health Organization. Blindness and visual impairment. World Health Organization; http://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. Updated October 11, 2018. [Google Scholar]
- 2.Owsley C, McGwin G, Scilley K, Meek GC, Dyer A, Seker D. The visual status of older persons residing in nursing homes. Arch Ophthalmol. 2007;125(7):925–930. 10.1001/archopht.125.7.925 PMID:17620572 [DOI] [PubMed] [Google Scholar]
- 3.Tielsch JM, Javitt JC, Coleman A, Katz J, Sommer A. The prevalence of blindness and visual impairment among nursing home residents in Baltimore. N Engl J Med. 1995;332(18): 1205–1209. 10.1056/NEJM199505043321806 PMID:7700315 [DOI] [PubMed] [Google Scholar]
- 4.West SK, Friedman D, Muñoz B, et al. A randomized trial of visual impairment interventions for nursing home residents: study design, baseline characteristics and visual loss. Ophthalmic Epidemiol. 2003;10(3):193–209. 10.1076/opep.10.3.193.15081 PMID:12815493 [DOI] [PubMed] [Google Scholar]
- 5.Horowitz A Vision impairment and functional disability among nursing home residents. Gerontologist. 1994;34(3):316–323. 10.1093/geront/34.3.316 PMID:8076872 [DOI] [PubMed] [Google Scholar]
- 6.Mitchell P, Hayes P, Wang JJ. Visual impairment in nursing home residents: the Blue Mountains Eye Study. Med J Aust. 1997; 166(2):73–76. 10.5694/j.1326-5377.1997.tb138724.x PMID:9033561 [DOI] [PubMed] [Google Scholar]
- 7.Friedman DS, O’Colmain BJ, Muñoz B, et al. ; Eye Diseases Prevalence Research Group. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004;122(4):564–572. 10.1001/archopht.1941.00870100042005 PMID:15078675 [DOI] [PubMed] [Google Scholar]
- 8.Friedman DS, Wolfs RC, O’Colmain BJ, et al. ; Eye Diseases Prevalence Research Group. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122(4):532–538. 10.1001/archopht.122.4.532 PMID:15078671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knudtson MD, Klein BE, Klein R, Cruickshanks KJ, Lee KE. Age-related eye disease, quality of life, and functional activity. Arch Ophthalmol. 2005;123(6):807–814. 10.1001/archopht.123.6.807 PMID:15955982 [DOI] [PubMed] [Google Scholar]
- 10.Rubin GS, Roche KB, Prasada-Rao P, Fried LP. Visual impairment and disability in older adults. Optom Vis Sci. 1994;71(12):750–760. 10.1097/00006324-199412000-00005 PMID:7898882 [DOI] [PubMed] [Google Scholar]
- 11.Rokicki W, Drozdzowska B, Czekajło A, et al. Relationship between visual status and functional status and the risk of falls in women. The RAC-OST-POL study. Arch Med Sci. 2016;12(6):1232–1238. 10.5114/aoms.2015.55146 PMID:27904513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chia EM, Wang JJ, Rochtchina E, Smith W, Cumming RR, Mitchell P. Impact of bilateral visual impairment on health-related quality of life: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 2004;45(1):71–76. 10.1167/iovs.03-0661 PMID:14691156 [DOI] [PubMed] [Google Scholar]
- 13.Ip S, Leung YF, Mak WP Depression in institutionalized older people with impaired vision. Int J Geriatr Psychiatry. 2001;15(12):1120–1124. [DOI] [PubMed] [Google Scholar]
- 14.AAO Hoskins Center for Quality Eye Care. Frequency of ocular examinations - 2015. American Academy of Ophthalmology. https://www.aao.org/clinical-statement/frequency-of-ocular-examinations. Updated March 2015. [Google Scholar]
- 15.Keller BK, Hejkal T, Potter JF Barriers to vision care for nursing home residents. J Am Med Dir Assoc. 2001;2(1):15–21. 10.1016/S1525-8610(04)70148-6 PMID:12812600 [DOI] [PubMed] [Google Scholar]
- 16.Friedman DS, Muñoz B, Roche KB, Massof R, Broman A, West SK. Poor uptake of cataract surgery in nursing home residents: the Salisbury Eye Evaluation in Nursing Home Groups study. Arch Ophthalmol. 2005;123(11):1581–1587. 10.1001/archopht.123.11.1581 PMID:16286622 [DOI] [PubMed] [Google Scholar]
- 17.Gray LC, Edirippulige S, Smith AC, et al. Telehealth for nursing homes: the utilization of specialist services for residential care. J Telemed Telecare. 2012;18(3):142–146. 10.1258/jtt.2012.SFT105 PMID:22362837 [DOI] [PubMed] [Google Scholar]
- 18.Toy BC, Myung DJ, He L, et al. Smartphone-based dilated fundus photography and near visual acuity testing as inexpensive screening tools to detect referral warranted diabetic eye disease. Retina. 2016;36(5):1000–1008. 10.1097/IAE.0000000000000955 PMID:26807627 [DOI] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. 10.1016/0022-3956(75)90026-6 PMID:1202204 [DOI] [PubMed] [Google Scholar]
- 20.Tsui I, Drexler A, Stanton AL, Kageyama J, Ngo E, Straatsma BR. Pilot study using mobile health to coordinate the diabetic patient, diabetologist, and ophthalmologist. J Diabetes Sci Technol. 2014;8(4):845–849. 10.1177/1932296814529637 PMID:24876413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myung DJ, Jais A, He L, Blumenkranz MS, Chang RT. 3D printed smartphone indirect lens adapter for rapid, high quality retinal imaging. J Mob Technol Med. 2014;3(1):9–15. 10.7309/jmtm.3.1.3 [DOI] [Google Scholar]
- 22.Myung DJ, Jais A, He L, Chang RT. Simple, low-cost smartphone adapter for rapid, high quality ocular anterior segment imaging: A photo diary. J Mob Technol Med. 2014;3(1):2–8. 10.7309/jmtm.3.1.2 [DOI] [Google Scholar]
- 23.Dreer LE, McGwin G Jr, Scilley K, et al. Development of a nursing home vision-targeted health-related quality of life questionnaire for older adults. Aging Ment Health. 2007;11(6):722–733. 10.1080/13607860701366186 PMID:18074260 [DOI] [PubMed] [Google Scholar]
- 24.U.S. Census Bureau. QuickFacts: San Mateo county, California: U.S. Census Bureau; https://www.census.gov/quickfacts/fact/table/sanmateocounty-california/PST045217#qf-headnote-a. Updated July 1, 2018. [Google Scholar]
- 25.U.S. Census Bureau. QuickFacts: Santa Clara county, California: U.S. Census Bureau; https://www.census.gov/quickfacts/fact/table/santa-claracountycalifornia/INC110216. Updated July 1, 2018. [Google Scholar]
- 26.Elliott AF, McGwin G Jr, Owsley C. Vision impairment among older adults residing in assisted living. J Aging Health. 2013;25(2):364–378. 10.1177/0898264312472538 PMID:23338786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dev MK, Paudel N, Joshi ND, Shah DN, Subba S. Impact of visual impairment on vision-specific quality of life among older adults living in nursing home. Curr Eye Res. 2014;39(3):232–238. 10.3109/02713683.2013.838973 PMID: 24144491 [DOI] [PubMed] [Google Scholar]
- 28.Lamoureux EL, Fenwick E, Moore K, Klaic M, Borschmann K, Hill K. Impact of the severity of distance and near-vision impairment on depression and vision-specific quality of life in older people living in residential care. Invest Ophthalmol Vis Sci. 2009;50(9):4103–4109. 10.1167/iovs.08-3294 PMID:19357359 [DOI] [PubMed] [Google Scholar]