Summary
Background
Discerning the determinants of weight loss maintenance is important in the planning of future interventions and policies regarding overweight and obesity. We have therefore systematically synthesized recent literature on determinants of weight loss maintenance for individuals with overweight and obesity.
Methods
With the use of the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement, prospective studies were identified from searches in PubMed and PsycINFO from 2006 to 2016. We included articles investigating adults with overweight and obesity undergoing weight loss without surgery or medication. Included articles were scored on their methodological quality, and a best‐evidence synthesis was applied to summarize the results.
Results
Our search resulted in 8,222 articles of which 67 articles were selected. In total, 124 determinants were identified of which 5 were demographic, 59 were behavioural, 51 were psychological/cognitive and 9 were social and physical environmental determinants. We found consistent evidence that demographic determinants were not predictive of weight loss maintenance. Behavioural and cognitive determinants that promote a reduction in energy intake, an increase in energy expenditure and monitoring of this balance are predictive determinants.
Conclusion
This review identifies key determinants in weight loss maintenance. However, more research regarding cognitive and environmental determinants of weight loss maintenance is needed to advance our knowledge on determinants of weight loss maintenance.
Keywords: Obesity, overweight, predictors, weight loss maintenance, weight management, weight regain
Introduction
In an effort to prevent further increase in overweight and obesity, many studies have investigated ideal weight loss and weight loss strategies. A 5% weight loss has shown to improve health outcomes and is currently a standard goal in weight loss interventions 1, 2. However, diet, exercise, behaviour and pharmacologic weight loss strategies have indicated that maximal weight loss is achieved at 6 months with most individuals regaining weight thereafter 3. Wing and Phelan notably reported that roughly 20% of individuals who are overweight are successful in long‐term weight loss 4. Moreover, a systematic review by Dombrowski et al. in 2014 promisingly demonstrated that weight loss maintenance interventions using strategies of behaviour/lifestyle modification were moderately effective at maintaining weight loss up to 24 months 5. These studies illustrate that long‐term weight loss can be achieved and the importance of interventions to increase the rate of success.
In order to improve weight loss maintenance strategies, successes and failures can be studied. Comparing individuals who are able to maintain their weight loss with those who regain weight in studies such as the National Weight Control Registry has identified several characteristics associated with successful weight loss maintenance. A systematic review conducted by Elfhag and Rössner in 2005 identified and summarized factors in successful weight loss maintenance and characterized successful individuals as those who had substantial weight loss during initial treatment, those who reach a self‐determined weight loss goal, those who lead an active lifestyle and those who engage in leisure time activities 6. They further define those successful in weight loss maintenance as those who continue to monitor their weight and eating behaviour. Further, these individuals ate healthy and low‐fat diets, ate at regular intervals and did not skip breakfast. Individuals who were successful in weight loss maintenance were also able to correct weight regain quickly, were self‐sufficient and autonomous and suffered less from psychological and emotional instability, binge eating and weight cycling. Lastly, Elfhag and Rössner report that individuals successful in weight loss maintenance used support from a social context 6.
Since 2005, many studies that have measured determinants of weight loss maintenance have been published. Obesity remains a multifactorial process involving not only behaviour but also psychology and the environment. Investigating weight loss maintenance, therefore, requires a synthesis of all determinants influencing an individual 7. Synthesizing the newest insights with an updated search of current literature will help to determine the level of evidence for known determinants and will identify new determinants in weight loss maintenance. Additionally, previous reviews have yet to systematically evaluate the quality of evidence for individual determinants. It is therefore our aim to systematically review the current evidence on prospectively assessed demographic, behavioural, psychological/cognitive and environmental (social and physical) determinants of weight loss maintenance in adults who recently lost weight, while taking the methodological quality of the studies into account.
Methods
This review adheres to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines. The review protocol is registered in the PROSPERO International Prospective Register of Systematic Reviews (registration number CRD42017058033) 8.
Search strategy
A systematic literature search of studies published between January 2006 and October 2016 in peer‐reviewed journals was conducted in the medical database PubMed and the psychological database PsycINFO with the eligibility criteria presented in Table 1. The full search strategy was created by JK, RV and MS. The full search strategy is published elsewhere 8 and includes the following search terms: Obesity and overweight AND Weight loss AND Weight maintenance AND observational studies, randomized controlled trials, systematic reviews AND Determinant AND Physical Activity and Eating Behaviour NOT (<18 years old OR Animal Studies OR Pharmacological Studies OR Bariatric Surgery OR Pregnancy, lactation OR Publication types that are not journal articles OR Cancer OR Mental Disorders OR Diabetes mellitus type 1).
Table 1.
Eligibility criteria
| Inclusion | Exclusion | |
|---|---|---|
| Population |
Studies with a mean age of 18 to 65. BMI before weight loss > 25 kg m−2. Studies using WHO definition of overweight and obesity. Weight loss of 5% before initiation of maintenance phase. |
Participants with acute or chronic disease unable to undergo a weight loss trial. Participants who are using medication to lose weight. Participants who are pregnant or lactating. |
| Intervention |
Experimental study where long‐term weight loss is followed by ≥1‐year post‐intervention. Experimental study where weight loss maintenance is conducted for ≥1 year from baseline. Observational study where participants have been followed up ≥1 year. |
Cross‐sectional study. Qualitative study. |
| Outcome | Determinant analysed for effect on weight. | |
| Long‐term weight loss: | ||
| Weight change (kg), percent weight change (%), BMI change (kg m−2) from end of study to follow‐up. | ||
| Weight loss maintenance study: | ||
| Weight change (kg), percent weight change (%), BMI change (kg m−2) from baseline to follow‐up. | ||
| Observational study: | ||
| Maintenance vs. regain, where maintenance is defined as 5% weight loss for >1 year. | ||
| Demographic, behavioural, psychological/cognitive, environmental (social and physical) determinants. | ||
| Study |
Language: English. Year: Publication year 2006–2016. Publication type: peer‐reviewed journals. |
BMI, body mass index; WHO, World Health Organization.
Study inclusion criteria
Study design
We included longitudinal studies, both experimental and observational. Experimental studies included randomized controlled and non‐controlled trials and were long‐term weight loss interventions or weight loss maintenance interventions. Long‐term weight loss interventions consisted of an initial weight loss programme with a follow‐up for a minimum of a year after weight loss. Weight loss maintenance interventions included participants who had already lost weight and were observed for a minimum of a year. Observational studies included prospective cohort studies and follow‐up studies on randomized and non‐randomized controlled trials.
Participation
We included studies with participants between the ages of 18 and 65. Studies where participants had overweight or obesity, or had overweight and obesity prior to a weight loss maintenance phase, were included. Overweight and obesity are defined by the World Health Organization classification body mass index (BMI) 25–29.9 kg m−2 and BMI > 30 kg m−2, respectively. We selected the age range, 18–65, as evidence suggests that the current World Health Organization cut‐offs for overweight and obesity are not appropriate for those above the age of 65 9.
As our population of interest are those who have overweight and obesity, we chose to exclude studies that had a sole focus on acute or chronic diseases. However, if studies had a focus on participants with overweight and obesity, and these individuals had acute or chronic diseases without contraindication to active weight loss or participation in weight loss trials, these were included. Therefore, studies including participants with type 2 diabetes, hypertension and hypercholesterolaemia were included. Furthermore, studies that included pregnant or lactating participants or individuals who had undergone bariatric or pharmacological weight loss were excluded.
We further specified our inclusion criteria for studies that define weight loss maintenance as weight loss of at least 5% of initial body weight and remaining below 5% for the minimum duration of a year. We chose 5% as a cut‐off as current guidelines on weight loss practices indicate that 5% to 10% weight loss leads to health benefits 10, 11. Although a greater reduction of ≥10% may be preferred for maximal health benefits, studies have shown that a minimum of 5% has positive effects on blood glucose level, hypertension, cholesterol and mental health 10, 11, 12.
This review was further limited to articles published within the last decade (2006–2016). We are interested in the newest insights in the determinants of weight loss maintenance and build upon a previous narrative review by Elfhag and Rössner entitled ‘Who succeeds in maintaining weight loss?’ published in 2005 6.
Outcomes
The primary outcome is the determinant predictive of weight loss maintenance. The determinant was included if it was analysed between individuals who were able to maintain weight loss or suffered regain, or if the determinant was analysed for change in weight (kg) from baseline, percent weight change or BMI change (Table 1). Determinants measured were required to have been specifically analysed as determinant of weight loss maintenance. Studies with demographic, behavioural, psychological/cognitive and environmental (social and physical) determinants as outcomes were included. We chose to include these determinants as these may help detect target groups and inform intervention content.
Study selection
One reviewer (RV) screened all titles (n = 8,229), and two reviewers (RV and MS) independently screened abstracts (n = 3,858) to assess inclusion. Two reviewers (RV and MS) conducted the full‐text screening independently (n = 380). Disagreements during abstract screening and full‐text screening were resolved through consensus discussion. When disagreements could not be resolved, the third and fourth reviewers (IS and WK) were called on to make a final decision.
Data extraction
Study characteristics including authors, year of publication, country of origin, study design and duration, analytic sample, mean age, mean BMI and weight measure were collected by RV. Determinants were collected by two reviewers (RV and MS). As study designs vary greatly, we categorized the studies as cohort studies, follow‐up studies on randomized controlled trials or non‐controlled trials. When determinants were reported with univariate and multivariate analyses, the result under multivariate analysis was taken.
Quality assessment
Quality assessment was conducted using a modified quality assessment tool formerly used by Uijtdewilligen et al. 13. A maximum of one point could be awarded per category (Table 2), and a total score of six points could be awarded per article. The categories, as previously described by Uijtdewilligen et al., in which studies could score points, were as follows 13:
The representativeness of the exposed cohort. A point was given if the participation rate at baseline was at least 80% or if the non‐response was not selective.
Non‐selective non‐response during follow‐up measurements. A point is given if the response rate at follow‐up was greater than or equal to 80% or if the non‐selective dropout on key characteristics (age, gender, determinants or weight) is reported.
Determinants were measured with a valid and reliable tool. If the determinant measure showed test–retest correlations of ≥0.80 or κ/ICC ≥ 0.70, one point is given 13. If the article investigates multiple determinants, this criterion is scored on a scale of 0–1. For example, if a study assessed four determinants, of which one was measured with a reliable tool, a score of 0.25 is given.
Weight was measured with a valid and reliable tool. A point is given only if weight was assessed with an objective measurement instrument, or questionnaire with test–retest correlations of ≥0.80 or κ/ICC ≥ 0.70.
Sample size ≥ 10 times the number of independent variables.
Appropriate statistical model adjusted for relevant confounders. In experimental studies, the findings of a determinant analysis were included (i.e. b‐path of mediation analysis).
Table 2.
Quality assessment tool 13
| Representativeness of the exposed cohort |
1 point is awarded if the participation rate is ≥80%. 1 point is awarded if the participation rate is <80% and the non‐response was not selective. 0 points are awarded if the participation rate is <80% and the non‐response is selective or not described. |
| Non‐selective non‐response |
1 point is awarded if attrition rate ≥ 80%. 1 point is awarded if attrition rate < 80% and dropout was not selective on key study characteristics (age, gender, determinant or weight). 0 points are awarded if attrition rate < 80% and dropout was selective on key study characteristics or not described. |
| Determinants are measured with valid and reliable tools | Each determinant measured in the outcome is assessed and scored. Each determinant can score either 1 (valid and reliable) or 0 (not valid nor reliable). The average of all determinants is taken as the total score. |
| Weight is measured with a valid and reliable tool |
1 point is awarded if weight is measured with a valid and reliable tool. 0 points are awarded if weight is not measured with a valid and reliable tool. |
| Sample size |
1 point is awarded if n is 10 times the number of measured determinants. 0 points are awarded if n is less than 10 times the number of measured determinants. |
| Appropriate statistical model |
1 point is awarded if appropriate statistical analysis is conducted. 0 points are awarded if the statistical analysis is not appropriate or not clearly reported. |
This was converted to a percentage by calculating the mean and multiplying 100. A score ≥ 75% was considered high quality and <75% low quality.
Data synthesis
Categorization of determinants
The determinants and their predictive nature were extracted. The quality of the determinant was determined by the quality assessment of the study in which it was measured. These determinants were then first categorized into four main categories:
demographic, personal determinants;
behavioural determinants;
cognitive/psychological determinants; and
social and physical environmental determinants.
After determinants and their quality were extracted, each determinant was placed under conceptual categories 14. Figure 1 illustrates how the determinants were placed into these conceptual categories, and finally under the four main determinant groups. Determinants were first listed as shown in Fig. 1. In this figure, we give the following examples of determinants: fruit and vegetable consumption increase, fish consumption increase, portion control, healthy eating increase, protein intake increase, fat intake (baseline) and binge eating. These determinants could be categorized under similar concepts. In Fig. 1, the conceptual categories were created as follows: dietary intake product level, eating behaviour, dietary intake nutrient level and problematic eating. These concepts were then categorized under a general concept of dietary intake, which falls under the main determinant category, behavioural determinants. The placement of the determinants under concept categories was conducted by RV and MS. Reviewers WK and IS were consulted when there were disagreements in the creation of concepts or placement of determinants within these concepts.
Figure 1.
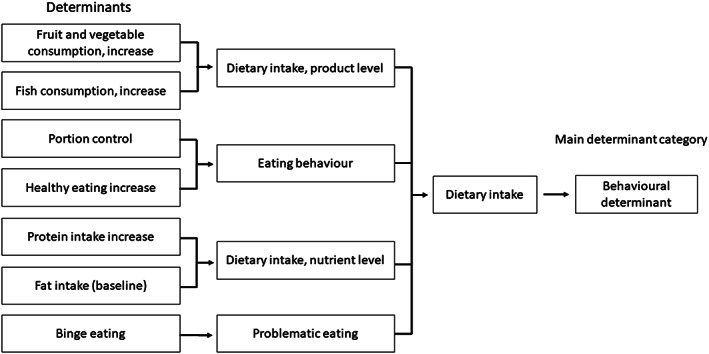
Categorization of determinants
Best‐evidence synthesis
In order to determine the level of the evidence for each determinant, we combined the quality of the studies the determinant was measured in with the consistency of the direction of the association of each determinant. This was performed using similar methods as Uijtdewilligen et al. 13.
Determinants of weight loss were categorized as significantly positively predictive, significantly negatively predictive or not significant in either direction of weight loss maintenance. Dividing the number of times a determinant is reported in a certain direction by the total number of times the determinant is measured multiplied by a hundred gave a percentage of consistency. If the determinant was reported more than 75%, we considered this a consistent finding in a certain direction. As previously used in Uijtdewilligen et al., the quality of evidence was identified as follows 13:
Strong evidence: consistent findings in multiple (≥2) high‐quality studies.
Moderate evidence: consistent findings in one high‐quality study and one or more low‐quality studies, or in multiple (≥2) low‐quality studies.
Insufficient evidence: only one study available or inconsistent findings in multiple (≥2) studies.
A determinant that was reported in a certain direction greater than 75% with two or more of these studies being high quality would result in the conclusion that there is strong evidence that the determinant is positively, negatively or not predictive of weight loss maintenance.
Results
As shown in Fig. 2, this search yielded 8,222 articles. Title screening led to the selection of 3,851 articles. Articles excluded at this stage were animal studies or paediatric studies. Further screening of the abstracts led to the selection of 373 articles for full‐text screening. Through cross referencing, seven more articles were included in the full‐text screening. Full‐text manuscripts were retrieved for 380 articles and screened on the basis of the eligibility criteria found in Table 1. A total of 49 studies, reported in 67 articles, fulfilled all inclusion criteria and are analysed in this review.
Figure 2.
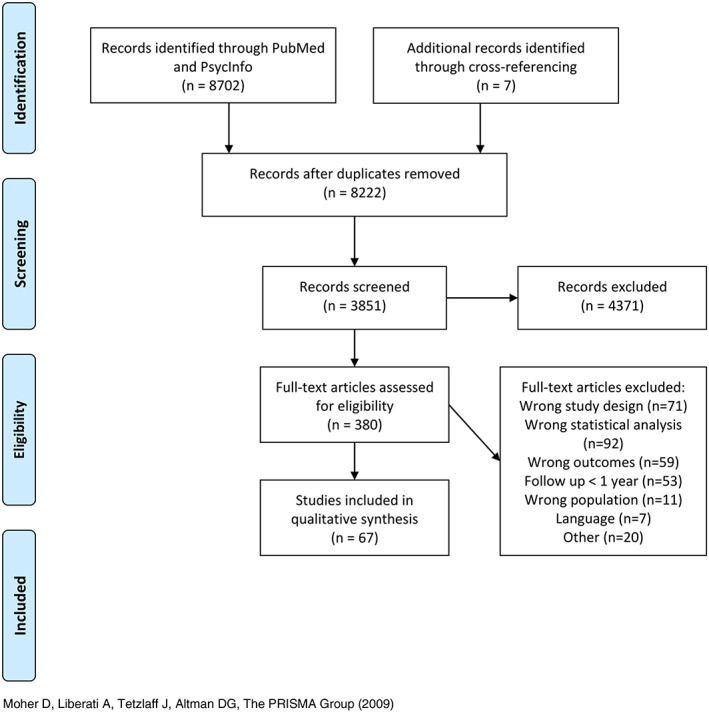
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses flow diagram [Colour figure can be viewed at wileyonlinelibrary.com]
Study characteristics are found in Table 3. Thirty of the 49 studies were conducted in the USA 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60. Studies were further conducted in Germany (4) 61, 62, 63, 64, Finland (4) 65, 66, 67, 68, Japan (3) 69, 70, 71, Australia (2) 72, 73, Portugal (1) 74, 75, Switzerland 76, Denmark 77, Israel 78, France 79, Canada 80 and the Netherlands 81. Twenty‐nine studies were follow‐up studies on randomized controlled trials, 13 were follow‐up studies on non‐controlled trials and 7 were observational cohort studies. In total 31,741 participants were included, and the average duration of studies was 30 months, with a range from 12 months 45 to 10 years 32. There was a great heterogeneity in the included studies with ages ranging from an average of 28.9 77 to an average age of 61.2 80 and baseline BMIs ranging from 27.3 77 to 42 71. The average age of participants was 47.2 years with a baseline BMI of 35.5 kg m−2, and 72% was female.
Table 3.
Study characteristics of the 67 articles included in this review
| Analytic sample | Weight measure | Study duration including follow‐up | Determinants | Outcome measures | Quality | |
|---|---|---|---|---|---|---|
| Look Action for Health in Diabetes (AHEAD) | ||||||
| Look AHEAD Research Group, 2014 15 |
Country: USA Population: 825 overweight adults aged 45–76 with type 2 diabetes participating in the Look AHEAD intervention who lost ≥10% of weight at year 1. Study design: follow‐up on RCT Mean age: 58.7 ± 6.8 Mean BMI or weight: 36.0 ± 5.9 kg m−2 % Female: 59.3 |
Weight change (kg) | 8 years | Individuals compared at year 8 who maintained the ≥10% loss versus gained above baseline weight revealed that those who are successful at maintaining weight loss (at year 8) had a higher activity‐related energy expenditure (1,471.9 ± 121.1 vs. 799.9 ± 100.9 kcal week−1, p < 0.001) and a greater number of weeks (in the prior year) reducing their calorie and fat intake (both p values < 0.001). Individuals who were able to maintain weight loss were also more likely than those who suffer full regain to weigh themselves daily or more often (47.8% vs. 28.4%), as well as weekly or more (82.4% vs. 69.8%) (both p < 0.001).The odds of achieving a ≥10% weight loss at year 8 were 2.3 (95% CI: 1.83, 2.97) times greater for participants who at year 1 lost ≥10%, than for those who lost 5 to <10%, and 3.9 (95% CI: 2.99, 5.15) times greater than for those who lost <5% at year 1. |
Energy expenditure: Paffenbarger Activity Questionnaire. Calorie and fat intake reduction: questionnaire developed by authors Self‐weighing: questionnaire developed by authors Initial weight loss: digital scale (model BWB‐800; Tanitas, Willowbrook, IL) |
High |
| Neiberg RH et al., 2012 16 |
Country: USA Population: 2,438 overweight adults aged 45–76 with type 2 diabetes participating in the Look AHEAD study. Study design: follow‐up on RCT Mean age: — Mean BMI or weight: — % Female: 59.5 |
Weight change (kg) | 4 years | Both individuals who had larger month‐to‐month weight losses (vs. smallest monthly losses) in year 1 and whose weight loss was more sustained (vs. early but not sustained) during the first year had better maintenance of weight loss over 4 years, independent of characteristics traditionally linked to weight loss success (p < 0.001). | Gradual and sustained weight loss: digital scale (model BWB‐800; Tanitas, Willowbrook, IL) | High |
| Unick JL et al., 2015 17 |
Country: USA Population: 2,290 overweight adults aged 45–76 with type 2 diabetes participating in the Look AHEAD study Study design: follow‐up on RCT Mean age: 58.69 ± 6.82 Mean BMI or weight: 35.65 ± 5.93 % Female: 59.2 |
Weight change (%) | 8 years | Greater weight loss at months 1 and 2 was associated with greater weight loss at any given year over the 8‐year period (p's < 0.001). Participants achieving the greatest weight loss at month 1 (>4%) and month 2 (>6%) had the highest odds (OR = 1.99; 95% CI: 1.54, 2.55; and OR = 2.78; 95% CI: 2.15, 3.57, respectively) of achieving ≥5% weight loss at years 4 and 8. | Initial weight loss: digital scale (model BWB‐800; Tanitas, Willowbrook, IL) | High |
| Wadden TA et al., 2011 18 |
Country: USA Population: 887 overweight adults aged 45–76 with type 2 diabetes participating in the Look AHEAD intervention. Study design: follow‐up on RCT Mean age: 58.6 ± 6.8 Mean BMI or weight: 35.3–36.3 kg m−1 % Female: 59.3 |
Weight maintenance | 4 years | Participants who maintained a 10% loss from the end of year 1 to the end of year 4, compared with those who did not, reported more favourable physical activity (p < 0.005) and reported eating fewer calories (p < 0.001) at year 4. |
Physical activity: Paffenbarger Activity Questionnaire Calorie intake reduction: questionnaire developed by author |
High |
| PESO Study | ||||||
| Santos I et al., 2015 74 |
Country: Portugal Population: 154 overweight women participating in a weight loss and management trial PESO Study design: follow‐up on RCT Mean age: 37.6 ± 7.0 Mean BMI or weight: 31.6 ± 4.1 kg m−2 % Female: 100 |
Weight maintenance of weight change (%) | 3 years | Correlation analysis: participants with high exercise intrinsic motivation, high intrinsic exercise goals, high exercise self‐efficacy, low perceived barriers, low self‐ideal body size discrepancy, high physical self‐worth, low impact of weight on quality of life and high, moderate to vigorous physical activity were more likely to have lost weight at 3 years. No association with weight change at 3 years was found for awareness of self, perceived choice, exercise controlled motivation, exercise autonomous motivation, extrinsic exercise goals, body shape concerns, self‐esteem, body attractiveness, exercise social support, depressive symptoms, physical health‐related quality of life, mental health‐related quality of life, flexible restraint, rigid restrained, disinhibition, hunger, energy intake, fat intake, fibre intake. |
General and exercise motivation: Self‐Determination Scale, Exercise Self‐Regulation Questionnaire, Intrinsic Motivation Inventory, the Exercise Motivations Inventory, self‐efficacy for exercise barriers scale and exercise perceived barriers scale. Psychological well‐being and quality of life: Figure Rating Scale, Body Shape Questionnaire, Rosenberg Self‐Concept/Self‐Esteem Scale, Physical Self‐Perception Profile Questionnaire, Social Support for Exercise Survey, Beck Depression Inventory, Short Form Health Survey and Weight on Quality of Life‐Lite. Eating behaviour and eating habits: the Three‐Factor Eating Questionnaire and semi‐quantitative Food‐Frequency Questionnaire. Physical activity: 7‐Day Physical Activity Recall Scale and lifestyle physical activity index. Body weight: electronic scale (SECA, Hamburg, Germany). |
Low |
| Silva MN et al., 2011 75 |
Country: Portugal Population: 156 overweight women participating in a weight loss and management trial PESO Study design: follow‐up on RCT Mean age: 37.6 ± 7.0 Mean BMI or weight: 31.6 ± 4.1 kg m−2% Female: 100 |
Weight change (%) | 3 years | Weight change at 3 years was significantly associated with perceived need support at year 1 (b = −0.04; SE = 0.01), autonomous self‐regulation at year 1 (b = 0.08; SE = 0.03) and at year 2 (b = −0.11; SE = 0.04) and moderate to vigorous physical activity at year 2 (b = −0.32). No association was found with external self‐regulation or introjected self‐regulation. |
Perceived need support: Health Care Climate Questionnaire. Behavioural regulations of exercise: 7‐Day Physical Activity Recall Scale Body weight: electronic scale (SECA, Hamburg, Germany). |
Low |
| Treatment of Obesity in Underserved Rural Settings (TOURS) study | ||||||
| Laitner MH et al., 2016 19 |
Country: USA Population: 152 obese women living in medically underserved rural counties participating in the TOURS trial Study design: follow‐up on RCT Mean age: 59.9 ± 6.2 Mean BMI or weight: 37 ± 5.1 % Female: 100 |
Weight maintenance | 18 months | Participants who were in the weight loss maintenance cluster significantly completed more dietary self‐monitoring records than did participants who were in the ‘weight loss and regain’ cluster (p < 0.001) or ‘low weight loss success’ cluster (p < 0.001). |
Dietary self‐monitoring: standardized self‐monitoring logs. Height and weight: calibrated and certified beam scale. |
Low |
| Nackers LM et al., 2010 20 |
Country: USA Population: 298 obese women living in medically underserved rural counties participating in the TOURS trial Study design: follow‐up on RCT Mean age: 59.3 ± 6.2 Mean BMI or weight: 36.8 ± 5.0 kg m−2 % Female: 100 |
Weight change (kg) | 18 months | No significant differences were found in weight maintenance between 6 and 18 months between participants who lost weight at a fast, moderate or slow rate within the first months of behavioural treatment. | Height and weight: certified balance beam and scale. | Low |
| Perri MG et al., 2008 21 |
Country: USA Population: 298 obese women living in medically underserved rural counties participating in the TOURS trial Study design: follow‐up on RCT Mean age: 59.4 ± 6.1 Mean BMI or weight: 36.8 ± 4.9 % Female: 100 |
Weight change (kg) | 18 months | A significant relationship between adherence to weight management strategies and weight changes during months 6 to 18 was observed, with poorer adherence resulting in greater weight gain. |
Adherence to weight management strategies: Number of self‐monitoring records completed. Height and weight: certified balance beam and scale. |
High |
| Peterson ND et al., 2014 22 |
Country: USA Population: 220 women living in medically underserved rural counties who took part in the TOURS trial Study design: follow‐up on RCT Mean age: 59.3 ± 6.1 Mean BMI or weight: 36.8 ± 4.9 % Female: 100 |
Weight change (%) | 18 months | High‐frequency and high‐consistency self‐monitoring of diet produced beneficial effect on weight change. Meeting daily caloric intake goals was associated with weight change. |
Dietary self‐monitoring records: Self‐monitoring forms. Height and weight: certified balance beam and scale. |
High |
| Weight Loss Maintenance trial (WLMT) | ||||||
| Brantley PJ et al., 2014 23 |
Country: USA Population: 1,025 overweight/obese adults who were taking medication for either hypertension or hyperlipidaemia and participated in the Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 55.6 ± 8.7 Mean BMI or weight: — % Female: 63 |
Weight change (kg) | 12 and 30 months | At 12 months, higher SF‐36 mental health composite score (b = −0.05; SE = 0.02) were associated with less weight regain, family discouragement on healthy eating was related to more weight regain (b = 0.25; SE = 0.11), friends' discouragement on healthy eating was associated with less weight regain (b = −0.24; SE = 0.11) and higher exercise encouragement was related to more weight regain (only Black participants). At 30 months, friends' encouragement for healthy eating was associated with more weight regain, higher SF‐36 mental health composite scores were related to less weight regain (b = −0.15; SE = 0.05), lower perceived physical functioning was related to more weight regain for non‐Black and higher vitality scores were associated with less weight regain among Blacks. |
Social Support and Exercise Survey, Social Support and Eating Habits Survey and SF‐36. Height and weight: calibrated height and weight scale. |
High |
| Champagne CM et al., 2011 24 |
Country: USA Population: 1,032 overweight/obese adults who were taking medication for either hypertension or hyperlipidaemia and participated in the Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 55.6 Mean BMI or weight: 34.0 ± 5.0 kg m−2 % Female: 63 |
Weight change (kg) | 3 years | Participants who substituted protein for fat (b = −0.07; 95% CI: −0.10, −0.05), substituted fat for carbohydrates (b = −0.03; 95% CI: −0.04, −0.02), substituted protein for carbohydrates (b = −0.05; 95% CI: −0.07, −0.02), increased fruit and vegetable intake (b = −0.04; 95% CI: −0.07, −0.01) or increased dairy intake (b = −0.17; 95% CI: −0.26, −0.08) lost more weight at follow‐up. Dietary fibre intake was not associated with weight change 25. |
Height and weight: calibrated height and weight scale. Dietary intake: block food frequency questionnaire. |
High |
| Coughlin JW et al. 2013 25 |
Country: USA Population: 880 overweight/obese adults who were taking medication for either hypertension or hyperlipidaemia and participated in the Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 55.9 ± 8.7 Mean BMI or weight: 30.9 ± 4.7 % Female: 62 |
Weight change (kg) | 30 months | Increased physical activity (b = −1.25; SE = 0.51), increased intake of fruit and vegetables (b = −2.39; SE = 0.63), more frequent weighing (p < 0.0001), decreases in number of times eating fast food (p < 0.05), decreases in portion sizes (p < 0.01), decreases in amount of desserts (p < 0.0001) and decreased consumption of sugared beverages (p < 0.10), as well as increase in intake of water or diet beverages (p < 0.10) predicted less weight regain at follow‐up. |
Height and weight: calibrated digital scale. Weight management strategies questionnaire. Physical activity: RT3 accelerometers. Dietary intake: Block food frequency questionnaire. |
High |
| Svetkey LP et al., 2012 26 |
Country: USA Population: 1,032 overweight/obese adults who were taking medication for either hypertension or hyperlipidaemia and participated in the Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 53–58 Mean BMI or weight: 33.4–35.3 kg m−2 % Female: 63 |
Weight change (%) | 3 years | Older age, male sex, less social support for diet and physical activity at entry of study, higher healthy eating at entry and increase in healthy eating and increase in moderate to vigorous physical activity were associated with more weight loss from end of phase 1 to end of study. Educational level, income, smoking status, quality of life, perceived stress, depression, weight loss history, perceived discrepancy between current weight and desired weight were not associated with weight loss. |
Height and weight: calibrated scale dietary intake: Block food frequency questionnaire. Physical activity: RT3 accelerometers. Questionnaire of demographic characteristics. Health‐related quality of life: SF‐36. Patient Health Questionnaire depression scale PHQ‐8. Perceived Stress Scale. |
High |
| Weight‐to‐Be Study (WTB) | ||||||
| Linde JA et al., 2006 27 |
Country: USA Population: 1,801 adults with a self‐reported BMI of >27.0 participating in the Weight‐to‐Be Study Study design: follow‐up on RCT Mean age: 50.7 ± 12.4 Mean BMI or weight: 34.2 kg m−2 % Female: 28.2 |
Weight change (kg) | 2 years | Decreased fat intake (men: b = 0.04; SE = 0.01; p < 0.01; women: b = 0.03; SE = 0.01; p < 0.01), and increased fruit/vegetable/fibre intake over the course of the study were associated with reductions in BMI at 24 months (men: b = −0.02; SE = 0.01; p < 0.01; women: b = −0.02; SE = 0.00 p < 0.01). Among individual food items, for men, increased hamburger, beef, hot dog, salad dressing, margarine, cheese, French fry, chip ice cream, pastry and total fat intake was associated with increased BMI; and increased fruit, green salad, vegetable, high‐fibre cereal, dark bread and total fibre intake was associated with decreases in BMI. For women, increased hamburger, beef, hot dog, salad dressing, margarine, bacon, cheese, French fry, ice cream, pastry and total fat intake over the course of the study was associated with increases in BMI; and increased fruit, green salad, vegetable, high‐fibre cereal and total fibre intake was associated with decreases in BMI. |
Height and weight: calibrated electronic scale and a wall‐mounted ruler. Dietary intake: block screening questionnaire for fat and block screening questionnaire for fruit/vegetable/fibre intake. |
Low |
| Linde JA et al., 2006 28 |
Country: USA Population: 1,801 adults with a self‐reported BMI of >27.0 participating in the Weight‐to‐Be Study Study design: follow‐up on RCT Mean age: 50.7 ± 12.4 Mean BMI or weight: 34.2 kg m−2 % Female: 28.2 |
Weight change (kg) | 2 years | Reducing calories (p < 0.0001), increasing fruits and vegetables (p < 0.01), decreasing fat intake (p < 0.001), cutting sweets/junk food (p < 0.0001) and reducing amount of food (p < 0.0001) were associated with associated with weight loss at 24 months. Increasing exercise was not associated with 24‐month weight change, although the duration of increasing exercise was associated with weight change (b = −0.10; SE = 0.01; p < 0.0001). Increased use of these weight loss strategies was significantly associated with greater 24 months weight loss. |
Height and weight: calibrated electronic scale and a wall‐mounted ruler. Weight loss strategies (reducing calories, increasing fruit and vegetables, increasing exercise etc.). |
High |
| National Weight Control Registry (NWCR) | ||||||
| Butryn ML et al., 2007 29 |
Country: USA Population: 3,003 adults who enrolled in the NWCR and have maintained a weight loss of at least 30 lb for at least a year Study design: cohort study Mean age: 48.0 ± 12.6 Mean BMI or weight: 37.1 ± 8.8 kg m−2 % Female: 75.1 |
Weight loss maintainers | 1‐year follow‐up | Weight regain at 1‐year follow‐up was significantly greater for participants whose self‐weighing frequency decrease between baseline and 1 year than for those whose frequency increased or remained the same. |
Height and weight: self‐report. Self‐weighing frequency. |
High |
| Lillis J et al., 2016 30 |
Country: USA Population: 5,320 who enrolled in the NWCR and have maintained a weight loss of at least 30 lb for at least a year without bariatric surgery and who have reached 5‐year follow‐up Study design: cohort study Mean age: 47 ± 12.2 Mean BMI or weight: 25.07 ± 4.5 % Female: 75 |
Weight change (%) | 5‐year follow‐up | Percent weight loss across the 5‐year follow‐up period was lower in the presence of higher baseline scores on both internal disinhibition (ID) and external disinhibition (ED), but only baseline ID was significantly related to more rapid deterioration in percent weight loss. Baseline ED was not significantly associated with the rate of change in percent weight loss over 5 years. Higher scores on ID were significantly associated with lower percent weight loss at the following year's assessment. Scores on ED were not predictive of weight change. |
Height and weight: self‐report. Disinhibition: Three‐Factor Eating Questionnaire. |
Low |
| Raynor HA et al., 2006 31 |
Country: USA Population: 1,884 Study design: cohort study Mean age: 47.9 ± 12.7 Mean BMI or weight: 36.4 ± 8.9 % Female: 77 |
Weight change (kg) | 1‐year follow‐up | Baseline TV viewing (β = 0.081; p < 0.05), increases in TV viewing over 1 year (β = 0.123; p < 0.001), decrease in physical activity over 1 year (β = −0.074; p < 0.05) and increase in % calories from sweets (β = 0.088; p < 0.005) were significant predictors of 1‐year weight regain. Baseline physical activity and baseline % calories from sweets were not associated with weight change. |
Height and weight: self‐report. TV viewing: questionnaire by author. Physical activity: Physical Activity Questionnaire. Dietary intake: Block food frequency questionnaire. |
Low |
| Thomas JG et al., 2014 32 |
Country: USA Population: 2,886 participants who lost ≥30 lb and maintained that for ≥1 year Study design: cohort Mean age: 47.8 ± 12.4 Mean BMI or weight: 24.8 ± 4.5 % Female: 77.5 |
Weight change (kg and %) | 10 years | Participants with larger initial weight losses and longer duration of maintenance of weight upon enrolment were associated with better weight loss maintenance. Being female and having less than a college degree were associated with short‐term weight loss maintenance but not with long‐term weight loss maintenance. Ethnic and racial background was not associated with weight change. Baseline levels of dietary intake, percent of calories from fat, restraint, disinhibition, self‐weighing frequency and leisure time caloric expenditure were not associated with 10‐year weight change. However, decreases in leisure time caloric expenditure, restraint, and self‐weighing frequency and increases in % of intake from fat and disinhibition from baseline to 1 year were independently associated with increased weight regain across 10 years. |
Demographics and weight history: questionnaire by author. Height and weight: self‐report. Weight‐related behaviours: established questionnaires. Physical activity: Physical Activity Questionnaire. Dietary intake: block food frequency questionnaire. Dietary restraint: Three‐Factor Eating Questionnaire. Self‐weighing: questionnaire by author. |
Low |
| PREMIER Trial | ||||||
| Bartfield JK et al., 2011 33 |
Country: USA Population: 507 overweight/obese adults with either pre‐hypertension or stage 1 hypertension not on anti‐hypertensive medication Study design: follow‐up on RCT Mean age: 49.8 ± 8.7 Mean BMI or weight: 33.7 ± 5.6 kg m−2 % Female: 60.9 |
Measured weight loss maintenance | 18 months | Participants who maintained their lost weight kept (=less decline) a higher number of food records and recorded days of physical activity at 18 compared with 6 months than did people who relapsed in lost weight. |
Food and physical activity records: Food & Fitness Diary. Weight and height: calibrated scale and a wall‐mounted stadiometer. |
Low |
| Chen L et al., 2009 34 |
Country: USA Population: 810 adults with pre‐hypertension or stage 1 hypertension Study design: follow‐up on RCT Mean age: 50.0 ± 8.9 Mean BMI or weight: 33.1 ± 5.8 kg m−2 % Female: 62 |
Weight change (kg) | 18 months | Reduction in liquid calorie intake (b = 0.24; 95% CI: 0.06, 0.41), reduction in solid calorie intake (b = 0.09; 95% CI: 0.005, 0.16), reduction in sugar‐sweetened beverage consumption (b = 0.65; 95% CI: 22, 1.09) were associated with long‐term weight loss. Changes in diet drinks, milk, juice, coffee and tea with sugar, coffee and tea without sugar and alcoholic beverages were not associated with weight change. |
Dietary intake: 24‐h dietary recall. Weight and height: calibrated scale and a wall‐mounted stadiometer. |
High |
| Wingo BC et al., 2013 35 |
Country: USA Population: 537 adults with pre‐hypertension/stage 1 hypertension not receiving medication, participating in the intervention arm of the PREMIER trial Study design: follow‐up on RCT Mean age: 50 ± 8.9 Mean BMI or weight: 33.2 ± 5.9 % Female: 6 |
Weight change (kg) | 18 months | At 18 months, the group with the greatest decrease in dietary self‐efficacy lost 6.0 ± 1.6 lb less than did the group with no significant changes in dietary self‐efficacy and 6.0 ± 1.5 lb less that the group with the greatest increase in dietary self‐efficacy (p < 0.001). The group with the greatest increase in exercise self‐efficacy lost 7.7 ± 1.5 lb more than did the group with the greatest decrease in exercise self‐efficacy score (p < 0.001). Changes in minutes of physical activity were not significantly associated with changes in weight. Change in cardiorespiratory fitness was significantly associated with change in weight (β = −0.31; p < 0.001) |
Self‐efficacy: eating habits confidence questionnaire and exercise confidence questionnaire. Physical activity: 7‐day physical recall. Weight and height: calibrated scale and a wall‐mounted stadiometer. |
Low |
| Healthy Weight for Life (HW4L) | ||||||
| Cussler EC et al., 2008 36 |
Country: USA Population: 161 peri‐menopausal women participating in the Healthy Weight for Life programme Study design: follow‐up on RCT Mean age: 48.0 ± 4.4 Mean BMI or weight: 31.1 ± 3.8 % Female: 100 |
Weight change (%) | 16 months | Internet diet‐log entries were correlated with follow‐up weight change (r = −0.29; p < 0.05). Follow‐up weight change was not correlated with change in dietary intake. |
Internet log entries. Dietary intake: diet record entries. Weight and height: electronic scale (SECA model 770, Hamburg, Germany). |
Low |
| Teixeira PJ et al., 2006 37 |
Country: USA Population: 136 overweight and obese middle‐aged women who lost weight in a 4‐month behavioural weight loss intervention participating in a 12‐month Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 48.1 ± 4.4 Mean BMI or weight: 30.6 ± 5.6 kg m−2 % Female: 100 |
Weight change (kg) | 16 months | Weight loss during initial 4 months, high (intrinsic) exercise motivation, less exercise perceived barriers, higher exercise self‐efficacy and higher physical self‐worth were associated with more weight loss during the maintenance period. Eating restraint, disinhibition, binge eating and body image were not associated with weight change. |
Weight and height: electronic scale (SECA model 770, Hamburg, Germany). Eating related variables: Three‐Factor Eating Questionnaire and the Binge Eating Scale. Exercise related variables: self‐efficacy for exercise behaviour scale, exercise perceived barriers scale and Intrinsic Motivation Inventory. Body image variables: Body Shape Questionnaire and Physical Self‐Perception Profile Questionnaire. |
High |
| Buscemi and Raynor | ||||||
| Buscemi J et al., 2014 38 |
Country: USA Population: 202 overweight/obese adults Study design: follow‐up on RCT Mean age: 51.3 Mean BMI or weight: 34.9 kg m−2 % Female: 58 |
Weight change | 6 to 18 months | Gender, race, baseline reinforcement ratio, change in reinforcement ratio and baseline BMI were not associated with BMI change from 6 to 18 months. |
Demographics: questionnaire by authors. Weight and height: calibrated digital scale and stadiometer. Reinforcement: activity level‐questionnaire eating version. |
Low |
| Raynor HA et al., 2012 39 |
Country: USA Population: 202 overweight adults participating in a behavioural weight loss programme Study design: follow‐up on RCT Mean age: 51.3 ± 9.5 Mean BMI or weight: 34.9 ± 4.3 kg m−2 % Female: — |
Weight change (%) | 18 months | No significant association was found between energy intake and weight loss at 18 months. |
Dietary intake: 24‐h dietary recall. Weight and height: calibrated digital scale and stadiometer. |
Low |
| Annesi JJ et al., 2016 40 |
Country: USA Population: 51 obese adult women who were physically inactive participating in a weight loss trial who were classified as emotional eaters Study design: follow‐up on RCT Mean age: 49.3 Mean BMI or weight: 35.5 % Female: 100 |
Weight change (kg) | 2 years | Increase in weight from baseline to 24 months was significantly predicted by 24‐month decrease in fruit and vegetable (β = −0.31; SE = 0.49; p = 0.01), increase in sweets (β = 0.37; SE = 0.62; p = 0.003) and decrease in physical activity (β = −0.24; SE = 0.08; p = 0.04) |
Dietary intake: self‐report survey. Physical activity: Godin–Shephard Leisure Time Physical Activity Questionnaire. Weight and height: calibrated digital scale and stadiometer. |
Low |
| Annesi JJ et al., 2016 41 |
Country: USA Population: 110 obese women Study design: follow‐up on RCT Mean age: 48.2 ± 7.8 Mean BMI or weight: 35.3 ± 3.2 kg m−2 % Female: 100 |
Measured weight change during weight loss maintenance phase (kg) | 2 years | Changes in physical activity (−0.45; SE = 0.11) and changes in fruit and vegetable consumption (−0.25; SE = 0.87) significantly predicted weight change during the weight loss maintenance phase (6 and 24 months). Changes in self‐regulation (b = −5.91; SE = 1.52) predicted weight change during the weight maintenance phase. Changes in self‐efficacy and mood were not predictors. |
Physical activity: Godin–Shephard Leisure Time Physical Activity Questionnaire. Dietary intake: self‐report survey. Self‐regulation: validated scale. Self‐efficacy: Exercise Self‐Efficacy Scale. Overall negative mood: Profile of Mood States Short Form. Self‐efficacy for controlled eating: weight efficacy lifestyle scale. Weight and height: calibrated digital scale and stadiometer. |
High |
| Barone Gibbs B et al., 2012 42, WOMAN study |
Country: USA Population: 419 Overweight and obese post‐menopausal women Study design: follow‐up RCT Mean age: 57.0 ± 2.9 Mean BMI or weight: 30.8 ± 3.8 % Female: 100 |
Measured long‐term weight loss (kg) | 4 years | Decreased desserts (b = 1.2; p < 0.01), decreased sugar‐sweetened beverages (b = 1.25; p < 0.05), decreased meats/cheeses (b = 0.82; p < 0.05) and increased fruit and vegetable (b = −1.48; p < 0.001) consumption were associated with weight loss from baseline to 48 months. No association was found for changes in eating at restaurants, changes in fried foods and changes in fish consumption. |
Height and weight: not reported. Eating behaviour: Connor Diet Habit Survey. Leisure time physical activity: modifiable activity questionnaire. |
High |
| Befort CA et al., 2008 43 |
Country: USA Population: 179 Study design: follow‐up on RCT Mean age: 48.7 ± 9.0 Mean BMI or weight: 37.6 ± 6.5 kg m−2 % Female: 65.9 |
Weight maintenance | 6–21 months | Initial weight loss (OR = 0.85; 95% CI: 0.78, 0.93); exercise 30–60 min d−1 (OR = 5.09; 95% CI: 1.69, 15.36) and perceived difficulty of managing weight as easy compared with impossible (OR = 24.08; 95% CI: 2.24, 259.4) were more likely to successfully maintain lost weight. Fruit and vegetable consumption, using pre‐packaged meals, planning ahead for meals, portion control, counting carbs, counting fats, keeping dietary food logs, keeping exercise logs, making specific plans for exercise, using a pedometer, self‐monitoring weight, reading diet books and participating in commercial weight loss programmes were not associated with successful weight loss maintenance. |
Height and weight: self‐report. Frequency of weight control behaviour and barriers: questionnaire by author. |
High |
| Brock DW et al., 2010 44 |
Country: USA Population: 113 formerly overweight pre‐menopausal women who had previously completed a weight loss programme to achieve a normal body weight Study design: follow‐up on NCT Mean age: 34.6 ± 6.2 Mean BMI or weight: 28.2 ± 1.3 kg m−2 % Female: 100 |
Weight change (kg) | 13 months | More days to weight loss goal (b = 0.026; p < 0.001) and perceived exertion during exercise (b = 0.44; p = 0.015) were associated with weight regain. No association was found for age and pre‐weight loss BMI. |
Physical activity: 7‐Day Physical Activity Recall Scale. Perceived effort: measured during submaximal aerobic exercise. |
Low |
| Buclin‐Thiébaud S et al., 2010 76 |
Country: Switzerland Population: 39 obese patients Study design: follow‐up on NCT Mean age: 57 Mean BMI or weight: 35−42 ± kg m−2 % Female: 70 |
Weight change | 5 years | Dietary habits (daily caloric intake, fat, carbohydrates and alcohol consumption) (p < 0.01), physical activity (p = 0.006), weight management and psychosocial difficulties (p = 0.0007), motivation, difficulties in dietary adherence and modification of the attitude of the entourage (p < 0.001) had a significant relationship to body weight after the 5 years' follow‐up. No information on other included variables was provided. |
Dietary intake, eating behaviour, dietary structure, and weight management strategies: questionnaire by author, diaries, dietician interviews. Physical activity: validated questionnaire. Psychosocial difficulties: Holmes's scale. |
Low |
| Chandler‐Laney PC et al., 2009 45 |
Country: USA Population: 120 moderately overweight pre‐menopausal women and of European American or African–American ancestry Study design: cohort Mean age: EA, 34.47 ± 0.84; AA, 35.03 ± 0.79 Mean BMI or weight: EA, 28.2 ± 0.17; AA, 28.19 ± 0.15 % Female: 100 |
Weight change (% fat) | 12 months | For European Americans, women who perceived others' body size as overweight gained more % body fat 1 year after weight loss than did those who perceived others as less overweight. This association was not apparent in African–American women. Cognitive restraint, age and perceived body size were not associated with percent body fat change. |
Demographic and race: self‐report. Body perception: Stunkard body rating scale. Restraint: Three‐Factor Eating Questionnaire. |
Low |
| Clifton PM et al., 2008 72 |
Country: Australia Population: 79 healthy women Study design: follow‐up on RCT Mean age: 49 ± 9 Mean BMI or weight: 32.8 ± 3.5 % Female: 100 |
Weight change (%) | 1 year | Protein in grams (r = 0.39; p = 0.001), the percentage of energy as protein (r = 0.36; p = 0.002) and the percentage of energy as carbohydrate (r = −0.24; p − 0.04) were associated with weight change. |
Dietary intake: 3‐d weighed food record. Weight and height: digital scale (model AMZ14; mercury digital scales, Tokyo, Japan) and stadiometer (Seca, Hamburg, Germany). |
Low |
| Cox TL et al., 2007 46 |
Country: USA Population: 89 former participates of weight loss programme Study design: follow‐up on NCT Mean age: 52.5 ± 13.3 Mean BMI or weight: weight: 91.9 ± 30.6 % Female: 80.9 |
Weight maintenance | >1 year (mean: 764.1 d; SD: 409.5) | Compared with individuals who suffered regain, those who were able to maintain weight loss were older (p = 0.01), consumed less total energy (p = 0.01) and had a significant lower energy density patterns (p < 0.01). No differences in level of physical activity were found. |
Physical activity: Centers for Disease Control and Prevention Behavioural Risk Factor Surveillance System Survey questionnaire. Dietary intake: 4‐d food record. Weight and height: Tanita digital scale (model no. BWB500A; Tanita Corp., Arlington Heights, IL) and a wall‐mounted stadiometer. |
Low |
| Del Corral P et al., 2011 47 |
Country: USA Population: 116 healthy pre‐menopausal women who recently lost weight to bring their BMI < 25 on a low‐calorie diet Study design: follow‐up on NCT Mean age: 33.4–35.0 Mean BMI or weight: 64.5–66.8 kg % Female: — |
Weight change (%) | 2 years | Percent weight regained (30.9 ± 6.7% vs. 66.7 ± 9.4%; p < 0.05) was significantly lower in participants with high dietary adherence to a low‐calorie diet than in participants with low adherence. |
Adherence to diet and dietary intake: calculated by authors. Weight and height: dual‐energy X‐ray absorptiometry (GE‐Lunar‐Prodigy, Madison, WI). |
Low |
| Due A et al., 2015 77 |
Country: Denmark Population: 20 participants who achieved 8% weight loss in previous trial randomized to a monounsaturated fatty acid intervention Study design: follow‐up on RCT Mean age: 28.9 (26.6–31.1) Mean BMI or weight: 27.3 (26.4–28.6) % Female: 65 |
Weight change (kg) | 18 months | A negative correlation was seen in body‐weight regain and self‐reported adherence to intake of monounsaturated fat (r = −0.703; p < 0.001), low intake of sugar (r = −0.479; p < 0.033) and high intake of legumes (r = −0.479; p < 0.033). Intake of whole grains, dairy products, red meat, fish and poultry was not associated with body‐weight regain. |
Weight and height: calibrated scale. Dietary intake and compliance: questionnaire by author. |
Low |
| Flood A et al., 2009 48, LIFE study |
Country: USA Population: 155 obese adults (BMI between 30 and 39 kg m−2) without chronic illness Study design: follow‐up on RCT Mean age: 49.4–50.6 Mean BMI or weight: 33.8–35.4 kg m−2 % Female: 37.5–59.0 |
BMI change (kg m−2) | 18 months | Changes in energy density were not associated with changes in BMI between 12 and 18 months (b = −0.31; p – 0.15) |
Weight and height: calibrated scale and wall‐mounted stadiometer. Dietary assessment: block food frequency questionnaire. |
High |
| Giel KE et al., 2008 61 |
Country: Germany Population: 79 overweight and obese patients in ambulatory weight loss programme Study design: follow‐up on NCT Mean age: 45.5 ± 12.2 Mean BMI or weight: 36.7 ± 5.6 kg m−2 % Female: 80 |
Weight change (kg) | 2 years | Age, gender, amount of initial weight loss and BMI at baseline were not correlated with weight loss maintenance. | Weight and height: self‐report. | Low |
| Greenberg I et al., 2009 78, DIRECT trial |
Country: Israel Population: 322 moderately obese participants of DIRECT trial Study design: follow‐up on RCT Mean age: 52.0 ± 7.0 Mean BMI or weight: 31.0 ± 3.6 kg m−2 % Female: — |
Weight change (%) | 2 years | Individuals who lost 5% or more of their initial weight were characterized by a higher initial BMI (31.3 ± 3.8) and a greater weight loss in the first 6 months of the intervention (9.3 ± 6.0 kg). Age, sex, smoking status, physical activity level, educational level, intake of energy (kcal), protein, fat, carbohydrate, cholesterol and dietary fibres at baseline were not associated with weight change. |
Dietary intake: food frequency questionnaire. Physical activity: validated questionnaire. Weight and height: scale and stadiometer. |
Low |
| Greene LF et al., 2006 49, EatRight study |
Country: USA Population: 74 former participants of the physician directed EatRight Weight Management programme through qualitative dietary changes Study design: follow‐up on NCT Mean age: 51.5 ± 12.9 Mean BMI or weight: 94.1 ± 25 kg % Female: — |
Weight maintainers | 2 years | Compared with those who gained weight (gained 5% or more of their body weight at follow‐up), those who maintained weight loss had significantly lower energy density intake at follow‐up (adjusted for age, gender, body‐weight post‐intervention and length of follow‐up time). No significant associations were found for total calorie intake, percent of calories from carbohydrates, protein, fat, or saturated fat, dietary fibre intake and food weight at follow‐up. Those who gained weight had larger portions of food items from several groups including meat/dairy, fats/nuts, fruits and beverages. No associations were found for vegetables and grains. |
Weight and height: Tanita digital scale (Model BWB500A; Tanita, Tokyo, Japan) and a wall‐mounted stadiometer. Dietary intake: 4‐d food recall. |
Low |
| Hübner C et al., 2016 62, German Weight Control Registry |
Country: Germany Population: 381 adults whose lifetime maximum weight was in the range of overweight and who intentionally lost at least 10% of weight that was maintained for at least 1 year Study design: cohort study Mean age: 40.6 ± 12.45 Mean BMI or weight: 33.02 ± 6.09 kg m−2 % Female: — |
BMI change (kg m−2) | 5.61 ± 5.78 years | Greater effect of retrospective weight‐related teasing during childhood and adolescence predicted less successful adult weight loss maintenance over 2 years (β = 0.12; p < 0.05). Greater emotional eating predicted a greater increase or a lower decrease in BMI between baseline and follow‐up (β = 0.14; p < 0.05). Restrained and external eating were not associated with change in BMI. |
Weight‐related teasing: Perception of Teasing Scale. Dutch Eating Behaviour Questionnaire. Weight and height: self‐report. |
Low |
| Keränen AM et al., 2009 65 |
Country: Finland Population: 49 obese adults participating in weight loss counselling intervention Study design: follow‐up on RCT Mean age: 49 ± 9 Mean BMI or weight: 35 ± 5 % Female: 72 |
Weight maintainers | 18 months | Success in weight loss maintenance was associated with high scores of cognitive restraint (p < 0.01) and low scores of uncontrolled eating, emotional eating (p < 0.05) and binge eating symptoms at follow‐up (p < 0.001). |
Eating behaviour: Three‐Factor Eating Questionnaire. Binge eating: Binge Eating Scale. Weight and height: calibrated scale. |
Low |
| Lenoir L et al., 2015 79 |
Country: France Population: 14,280 overweight/obese patients managed for weight loss by a primary care physician practicing behavioural nutrition Study design: retrospective cohort study Mean age: 44.97 ± 11.71 Mean BMI or weight: 31.15 ± 4.99 % Female: 84.6 |
Weight maintainers | ≥12 months after weight loss (mean 35.4 ± 19.3) | Initial weight and baseline BMI of patients were significantly higher in the successful maintenance (SM) group than in the unsuccessful maintenance (UM) group (p < 0.001). The achievement of the 10% initial weight loss required a shorter period in the SM group than in the UM group. |
Weight, height and body composition: digital scale and bioelectric impedance (Tanita TBF 300, Tanita BC 1000.1 or Tanita BC 420). |
High |
| Lindstrom J et al., 2006 66, Finnish Diabetes Prevention Study |
Country: Finland Population: 522 overweight, middle‐aged adults with impaired glucose tolerance participating in the Finnish Diabetes Prevention Study Study design: follow‐up on NCT Mean age: 55.0 ± 7.0 Mean BMI or weight: 31.0 ± 4.0 kg m−2 % Female: 33.2 |
Weight change (kg) | 3 years | Individuals with a diet low in fat, low in saturated fat, high in fibre (OR = 2.67; 95% CI: 1.26, 5.65) and/or low in energy density lost more weight and had a higher odd of achieving >5% weight reduction at year 3 than those consuming a diet high in fat (OR = 0.45; 95% CI: 0.23, 0.88), high in saturated fat (OR = 0.36 95% CI: 0.18, 0.74), low in fibre and low in energy density (OR = 0.19; 95% CI: 0.08, 0.41). |
Dietary intake: 3‐d food record. |
Low |
| Mason AE et al., 2016 50, SHINE trial |
Country: USA Population: 194 adults with obesity participating in the SHINE trial Study design: follow‐up on RCT Mean age: 47.0 ± 12.7 Mean BMI or weight: 35.5 ± 3.6 kg m−2 % Female: 82 |
Weight change (kg) | 18 months | Neither reward‐based eating (β = 0.06; p – 0.350) or psychological stress (β = 0.03; p = 0.556) were associated with weight loss at 18 months. |
Reward‐based eating: reward‐based eating scale. Psychological stress: Perceived Stress Scale. Weight: calibrated digital scale (Wheelchair Scale 6002, Scale‐Tronix, Carol Stream, IL). |
High |
| Nakade M et al., 2012 69, SCOP study |
Country: Japan Population: 116 participants who participated in a 1‐year weight loss programme Study design: follow‐up on NCT Mean age: USWM, 54.9 ± 6.0; SWM, 54.8 ± 6.8 Mean BMI or weight: USWM, 30.3 ± 3.1; SWM, 31.6 ± 4.8 % Female: USWM, 77; SWM, 79 |
Weight change (kg and %) | 1 year | No significant differences in the proportion of men, baseline age, height, weight and BMI between successful and unsuccessful weight maintenance. Significantly more participants successful in weight maintenance answered yes to the questions about self‐efficacy for practicing dietary objectives, measuring weight, and assessing practice and keeping records than did the participants unsuccessful in weight loss maintenance both without adjustment and after adjusting for age, sex and baseline weight. The frequency of weighing was higher in those successful in weight loss maintenance after adjusting for age, sex and baseline weight. Successful participants felt significantly less stress about measuring weight. They also felt less stress regarding assessing their practice and keeping records every day, but significance was not seen after adjusting for age, sex and the values at the end of the programme. Walking steps were significantly greater for the participants successful in weight loss maintenance after adjusting for age, sex and baseline values. |
Weight: bioelectric impedance analysis (TB‐220, Tanita Co., Japan). Weight management strategies, self‐efficacy and stress: questionnaire by author. Daily steps: uniaxial accelerometer (Suzuken Co., Japan). |
High |
| Nakata Y et al., 2014 70 |
Country: Japan Population: 188 overweight adults aged 40–65 participating in weight loss intervention Study design: follow‐up on RCT Mean age: 50.7–51.7 Mean BMI or weight: 29.0–29.2 kg m−2 % Female: 66–81 |
Weight change (kg) | 30 months | Participants in the highest quartile of percent weight lost significantly increased their step counts by 2,607, which was higher than observed in other groups (p < 0.05) and increased their moderate to vigorous physical activity by 21 min d−1, which was higher than in the lowest quartile (p < 0.054). No significant differences were observed in energy intake (kcal d−1), age or gender between the weight loss groups. |
Weight and height: calibrated digital scale (WB‐150; Tanita) and a wall‐mounted stadiometer. Energy intake: 3‐d food record. Physical activity: Active Style Pro three‐axis accelerometer (HJA‐350IT; Omron Healthcare, Kyoto, Japan). |
Low |
| Neve M et al., 2012 73 |
Country: Australia Population: 614 overweight adults subscribed for a commercial web‐based weight loss programme Study design: follow‐up on NCT Mean age: — Mean BMI or weight: — % Female: 88 |
Weight change (kg) | 15 months | Compared with participants who reported weighing themselves infrequently (never to less than once monthly), those who weighed themselves more frequently were more likely to be successful in weight loss maintenance (p < 0.001). Participants who reported they ate takeaway foods less than once weekly, particularly those who never consumed takeaway foods, were more likely to be successful (OR = 4.56; 95% CI: 1.72, 12.08). Participants who did not skip meals (OR = 2.18; 95% CI: 1.39, 3.41) or do not keep snack foods in the house (OR = 1.97; 95% CI: 1.28, 3.02), as well as those with higher dietary restraint scores (OR = 1.18; 95% CI: 1.06, 1.31) were also significantly more likely to be successful. The higher a participant's emotional eating score, the less likely the participant was to be successful (OR = 0.84; 95% CI: 77, 91). Self‐monitoring of exercise, fruit and vegetable intake, fry food intake, use butter in cooking, drink tea or coffee with milk, use low‐fat products, drink water, breakfast consumption frequency, soft drink consumption, alcohol intake, physical activity level and time spent sitting were unrelated in the multiple logistic model. |
Weight and height: self‐report. Dietary questions: validated questionnaire. Dietary restraint, emotional eating and uncontrolled eating: Three‐Factor Eating Questionnaire. Physical activity: International Physical Activity Questionnaire short format. |
Low |
| Niemeier HM et al., 2007 51 TRIM trial and NWCR |
Country: USA Population: 202 overweight participants in the TRIM behavioural weight loss trial and 3,345 weight loss maintainers registered in the NWCR Study design: cohort/follow‐up study Mean age: TRIM, 40.7 ± 6.6; NWCR, 47.2 ± 12.5 Mean BMI or weight: TRIM, 31.3 ± 3.0; NWCR, 25.2 ± 4.9 % Female: TRIM, 63.6%; NWCR: 76.1% |
Weight change (kg) |
TRIM: 18 months NWCR: 12 months |
In TRIM, internal disinhibition marginally significantly predicted weight loss at 18 months (b = 0.62; SE = 0.33; p = 0.06) with higher levels of internal disinhibition at baseline predicting less weight loss. External disinhibition did not predict weight loss. In NWCR, internal disinhibition significantly predicted 1‐year weight change (b = 0.26; SE = 0.08; p = 0.01) while external disinhibition did not. Higher levels of internal disinhibition on entry into the registry predicted more weight regain in the first year of membership. |
Disinhibition: disinhibition scale, Three‐Factor Eating Questionnaire. Weight and height: TRIM, calibrated scale and stadiometer. NWCR, self‐report. |
High |
| Nurkkala M et al., 2015 67 |
Country: Finland Population: 120 obese adults participating in a behavioural weight loss trial Study design: follow‐up on RCT Mean age: 45.0 ± 11.0 Mean BMI or weight: 35.6 (33.2–30.1) % Female: 94 |
Weight maintenance | 3 years | Participants successful in weight loss maintenance (weight loss maintenance ≥ 5%) had a higher increase in cognitive restraint (p = 0.015) and had less uncontrolled eating from 9 to 36 months (p < 0.05) and less emotional eating from 24 to 36 months (p < 0.05). |
Weight and height: calibrated digital scale (SOEHNLE S20, Soehnle waagen, Germany), and a right‐angle ruler anda tape measure. Eating behaviour: Three‐Factor Eating Questionnaire. |
Low |
| Ochner CN and Lowe MR, 2007 52 |
Country: USA Population: 103 overweight or obese women participating in a dietary weight loss trial Study design: follow‐up on RCT Mean age: 43.87 ± 10.49 Mean BMI or weight: 31.85 ± 2.61 % Female: 100 |
Weight change (kg) | 33 months | Increases dietary calcium intake at between 6 and 18‐months follow‐up inversely predicted weight regain (β = −0.380; p < 0.05), whereas increased energy intake positively predicted weight regain (β = .511; p < 0.01). |
Weight and height: digital scale (Tanita BWB‐800P) and standardized stadiometer. Dietary intake: 110‐item block and 5‐d food records. |
High |
| Pekkarinen T et al., 2015 68 |
Country: Finland Population: 201 obese patients participating in a Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 47 Mean BMI or weight: 40 % Female: 71 |
Weight change (%) | 69 weeks (post‐maintenance programme) and 121 weeks (1‐year post‐maintenance programme) | Partial correlation, which controlled for treatment, baseline weight and therapist, showed that weight loss percent at week 17 correlated with weight loss percent at week 69 (r = 0.63, p < 0.0001) and at week 121 (r = 0.46, p < 0.0001). There was no interaction with treatment and sex, age of the onset on obesity (child/adult), previously lost weight > 10 kg (no, once, twice or more), basic education and employed (yes/no) on weight loss at week 69 or 121. |
Weight: digital scale (Soehnle model 7307, Soehnle‐Waagen GmbH & Co., Murrhardt, Germany). Demographic and other anthropometric data: self‐report. |
High |
| Phelan S et al., 2010 53, CARDIA study |
Country: USA Population: 536 overweight/obese African–American and White young adults who had ≥5% weight loss. Study design: cohort study Mean age: 40.1 ± 3.7 Mean BMI or weight: 34.0–35.4 kg m−2 % Female: 47 |
Weight maintainers | 5 years | Higher odds of successful weight loss maintenance were related to African–American race (OR = 1.7; p = 0.03), smoking (OR = 3.4; p ≤ 0.001); increases in moderate physical activity (OR = 1.4; p < 0.001); increases in emotional support (OR = 1.6; p = 0.001) and less sugar‐sweetened soft drink consumption at follow‐up (OR = 0.08; p < 0.01). Gender, marital status, initial weight loss and dieting history were not associated with weight change. |
Weight and height: calibrated equipment. Leisure time activity: CARDIA Physical Activity Questionnaire. Dietary intake: diet history intake and fast food habits questionnaire. Psychosocial measures: social support. |
Low |
| Postrach E et al., 2013 63, KiloCoach |
Country: Germany Population: 479 overweight users of the commercial weight loss KiloCoach platform Study design: cohort study Mean age: 44.2 ± 11.8 Mean BMI or weight: 31.3 ± 3.1 kg m−2 % Female: 61.3 |
Weight maintainers | ~18 months | A significant positive correlation between early weight loss in weeks 1–2 and weight maintenance up to 2 years (r = 0.278; p < 0.01). No gender differences were found. |
Weight and height: self‐report. |
Low |
| Senechal M et al., 2011 80 |
Country: Canada Population: 19 obese women who participated in a 15‐week weight loss programme Study design: follow‐up on NCT Mean age: 61.2 ± 6.0 Mean BMI or weight: 31.8 ± 4.0 kg m−2 % Female: 100 |
Weight change (kg) | 15.5 months | Body‐weight gain since menopause (r = 0.65; p < 0.01), baseline body weight (r = 0.48; p < 0.01) and BMI (r = 0.58; p < 0.01) were associated with body‐weight regain. Age was not associated with regain. |
Weight and height: calibrated balance (Seca 707; Seca, Hamburg, Germany) and a standard stadiometer (Takei Scientific Instruments Co. Ltd, Tokyo, Japan). Weight gain since menopause: self‐report. |
Low |
| Szabo‐Reed AN et al., 2016 57 |
Country: USA Population: 359 overweight/obese adults participating in a behavioural weight loss programme Study design: follow‐up on NCT Mean age: 44.4 ± 0.5 Mean BMI or weight: 34.7 ± 0.3 kg m−2 % Female: 66.6 |
Weight change (%) | 18 months | During maintenance, participants at 18 months with ~14% weight loss performed more physical activity (p < 0.001), had higher self‐efficacy for weight management (p < 0.0001) and had higher self‐efficacy for exercise barriers (p < 0.0001) than did participants who had <1% weight loss at 18 months. Participants with greater weight loss had higher fruit and vegetable consumption (p < 0.0001). No differences were found between weight loss groups in entrées and shakes consumption, gender, ethnicity, income level and weight at baseline. |
Weight and height: digital scale (Befour Inc Model #PS6600, Saukville, WI) and stadiometer (model PE‐WM‐60‐84, Perspective Enterprises, Portage, MI). Barriers to exercise: 5‐item questionnaire by Marcus and Owen 1992. Weight management and self‐efficacy: Weight Efficacy Lifestyle Questionnaire. Estimated income: self‐report and zip code. |
Low |
| Tate DF et al., 2007 58 |
Country: USA Population: 202 overweight adults participating in a behavioural weight loss programme Study design: follow‐up on RCT Mean age: 42.4 ± 6.4 Mean BMI or weight: 31.7 ± 2.6 kg m−2 % Female: 58 |
Weight change (kg) | 30 months | Participants sustaining higher exercise levels for 30 months had significantly (p < 0.001) greater 30‐month weight loss than had those exercising less. Weight loss from baseline to 30 months was greater in men than in women. |
Weight and height: calibrated digital scale (Detecto, Webb City, MS) and wall‐mounted stadiometer (Perspective, Portage, MI). Physical activity: Paffenbarger activity questionnaire. |
High |
| Vogels N and Westerterp‐Plantenga MS, 2007 81 |
Country: The Netherlands Population: 133 overweight and obese participants following a very‐low‐calorie diet Study design: follow‐up on NCT Mean age: 49.6 ± 9.7 Mean BMI or weight: 30.9 ± 3.8 kg m−2 % Female: — |
Weight maintainers | 25.5 months | After 2 years, participants successful in long‐term weight loss maintenance (<10% body‐weight regain) had higher baseline BMI and significantly increased their dietary restraint over 2 years than had those who suffered regain (>10% body‐weight regain). No associations were found with level physical activity, disinhibition and hunger. |
Weight and height: digital balance (model 707; Seca, Hamburg, Germany) and a stadiometer (model 220; Seca). Attitudes towards eating: Three‐Factor Eating Questionnaire. Physical activity: validated Baecke questionnaire. |
Low |
| Volger S et al., 2013 59, POWER UP study |
Country: USA Population: 390 obese adults aged ≥ 21 years living in the Philadelphia region participating in the weight loss intervention POWER‐UP Study design: follow‐up on RCT Mean age: 51.5 ± 11.5 Mean BMI or weight: 38.5 ± 4.7 % Female: — |
2 years | There were no associations between 24‐month weight loss and any of the baseline measures of diet, physical activity, eating behaviour, gender and age. Change in hunger (partial R 2; p = 0.038) and race (p < 0.0001) were significantly associated with 24‐month weight loss. Changes in restraint and disinhibition at 6 months did not increase the explained variance in 24‐month weight loss. The odds of losing 5% or more weight at 24 months were 4.7 times greater (95% CI: 2.83, 7.77) for participants who lost ≥5% of their weight at month 6 than for those who did not achieve a 5% weight loss at this time. |
Weight and height: digital scale (Tanita BWB 800, Tanita Corp, Tokyo, Japan) and stadiometer (Seca Stadiometer 202, Seca, Hamburg, Germany). Eating behaviour: eating inventory). Dietary assessment: fruit and vegetable screener and percentage from fat screener. Physical activity: Paffenbarger activity questionnaire. |
Low | |
| Wang J et al., 2015 60 |
Country: USA Population: 210 overweight (BMI 27–43) adults (aged 21–59) without major medical conditions participating in behavioural weight loss interventions Study design: follow‐up on RCT Mean age: 46.8 ± 9.0 Mean BMI or weight: 34 ± 4.5 % Female: 84.8 |
Weight change (kg) | 2 years | The barriers to healthy eating (β = 0.11; p < 0.001) as well as the scores on the emotions subscale (β = 0.19; p < 0.001), the daily mechanics subscale (β = 0.19; p < 0.001) and the social support subscale (β = 0.16; p = 0.01) were significantly associated with weight over the 24 months. |
Weight: digital scale (TBF‐300A, Tanita Corp., Arlington Heights, IL). Barriers to heath eating: Barriers to Healthy Eating Scale. |
Low |
| Wang X et al., 2008 54 |
Country: USA Population: 34 overweight/obese post‐menopausal women participating in a weight loss intervention Study design: follow‐up on RCT Mean age: 58.6 ± 5.2 Mean BMI or weight: 90.1 ± 10.2 kg % Female: 100 |
Weight change (kg) | 16.5 months | The amount of weight regained 12 months post‐intervention was inversely associated with decreases in physical activity energy expenditure during the initial weight loss period (r = −0.404; p < 0.05). |
Weight and height: measured Physical activity energy expenditure: RT3 (StayHealthy, Inc., Monrovia, CA). |
Low |
| West DS et al., 2011 55 |
Country: USA Population: 226 overweight women with urinary incontinence who participated in a behavioural weight loss intervention and randomized to a Weight Loss Maintenance trial Study design: follow‐up on RCT Mean age: 53.0 ± 10 Mean BMI or weight: 36 ± 6 kg m−2 % Female: 100 |
Weight change (kg) | 18 months | Within the skill‐based programme, successful weight maintenance self‐concept (b = 0.56; p < 0.01) predicted weight change during maintenance phase. In the motivation‐focused programme, focus on progress (b = 2; p < 0.001) and self‐concept as an exerciser (b = 0.28; p = 0.02) predicted weight change during maintenance phase. Autonomous self‐regulation, controlled self‐regulation and reinforcing activities were not associated with weight change. |
Weight and height: digital scale (Tanita BWB 800) and a wall‐mounted stadiometer. Motivational self‐measures: Treatment Self‐Regulation Questionnaire. Measures of self‐identity: adapted Exercise Identity Scale. |
High |
| Weygandt M et al., 2015 64 |
Country: Germany Population: 23 subjects who achieved reduction in their body weight by 8% during an earlier 12‐week diet Study design: follow‐up on RCT Mean age: — Mean BMI or weight: — % Female: — |
Weight change (BMI) | 12 months | Impulse control (measured with activity in the dorsolateral prefrontal cortex) at baseline was coupled to the degree of success in weight maintenance (p < 0.05). No association was found between changes in impulse control and success in weight maintenance. Higher behavioural impulsivity at baseline was associated with poorer weight maintenance (r = −0.36; p = 0.047). Changes in impulsivity were not associated with changes in weight loss maintenance. | Impulse control: fMRI activity in the dorsolateral prefrontal cortex. | Low |
| Wing RR et al., 2006 56 |
Country: USA Population: 314 participants who lost 10% of their body weight in the previous 2 years Study design: follow‐up on RCT Mean age: C = 52.0 ± 10.8; I1 = 50.9 ± 9.3; I2 = 51.0 ± 10.3 Mean BMI or weight: C = 29.1 ± 5.0; I1 = 28.1 ± 4.6; I2 = 28.7 ± 4.7 % Female: 81 |
Weight change (kg) | 18 months | Increases in daily self‐weighing were associated with a decreased risk of regaining 2.3 kg or more. |
Weight and height: calibrated scale and a stadiometer. Self‐weighing: frequency of self‐weighing self‐report. |
Low |
| Yamada T et al., 2015 71 |
Country: Japan Population: 120 consecutive hospital patients with severe obesity participating in an in‐patient programme targeting 5% weight loss. Study design: follow‐up on NCT Mean age: 48.0 ± 14 Mean BMI or weight: 42.0 ± 9.0 % Female: 57 |
Weight maintenance | 2 years | Greater than 5% weight loss was associated with lower risk of regaining weight compared with ≤5% weight loss (HR = 0.37; 95% CI: 0.15, 0.89). Rapid weight loss (>3% within 7 d after admission) did not significantly increase the risk of subsequently regaining weight than in patients who showed slower weight loss (≤3% within 7 d: HR = 1.26; 95% CI: 0.64, 2.48) | Weight and height: AD 6107NW scales (A and D Co. Ltd, Tokyo, Japan). | Low |
BMI, body mass index; CI, confidence interval; HR, hazard ratio; NCT, non‐controlled trial; OR, odds ratio; RCT, randomized controlled trial; SE, standard error.
Quality
Table 4 shows the percentage of articles fulfilling each quality criterion assessed. On average, the quality of the articles was low with 42 (63%) of the 67 articles scoring low on the quality assessment and 25 articles (37%) scoring high. A large percent of the articles used valid and reliable tools for measuring weight and included an appropriate sample size, where most articles lost points were in the representativeness of the exposed cohort, mainly due to unclear reporting and baseline participation below 80% without reporting the non‐selective non‐response. While assessing the validity and reliability of the determinants, we found that many articles reported the validity and reliability of their determinant tools. Lastly, the statistical models used for the determinants of weight loss maintenance were often not adjusted for relevant confounders or were associative and not longitudinal analyses.
Table 4.
Percentage of articles fulfilling each quality assessment criterion
| Criteria assessing quality of studies | Percent of articles fulfilling the criteria |
|---|---|
| Representativeness of the exposed cohort | 25.4 |
| Non‐selective non‐response | 47.0 |
| Determinants were measured with a valid and reliable tool | 64.1 |
| Weight was measured with a valid and reliable tool | 89.6 |
| Sample size ≥ 10 times number of independent variables | 91.0 |
| Appropriate statistical model adjusted for relevant confounders | 56.7 |
In total, 124 determinants were identified, and 28 conceptual categories were created. The measured determinants, their predictive nature on weight loss maintenance and level of evidence can be found in Tables 5, 6, 7, 8. The results are summarized per main determinant category: demographic, behavioural, cognitive/psychological, and social and physical determinants.
Table 5.
Demographic determinants, percentage of directional consistency and level of evidence
| Conceptual category of determinant | Determinant | % Positively predictive of weight loss maintenance | % Not significantly predictive of weight loss maintenance | % Negatively predictive of weight loss maintenance | Level of evidence | Number of studies |
|---|---|---|---|---|---|---|
| Age (older) | 18.2 | 81.8 | 0 | Strong | n = 11 | |
| Gender (female) | 0 | 78.5 | 21.4 | Strong | n = 154 | |
| Ethnicity/race | 28.6 | 71.4 | 0 | Strong | n = 5 | |
| Socioeconomic status (high) | Education level, income, occupational status | 0 | 100 | 0 | Strong | n = 5 |
| Marital status (married/living together) | 0 | 100 | 0 | Insufficient | n = 1 |
Table 6.
Behavioural determinants, percentage of directional consistency and level of evidence
| Conceptual category of determinant | Determinant | % Positively predictive of weight loss maintenance | % Not significantly predictive of weight loss maintenance | % Negatively predictive of weight loss maintenance | Level of evidence | Number of studies |
|---|---|---|---|---|---|---|
| Weight‐related determinants | ||||||
| Weight | Pre‐weight loss BMI/weight/fat mass at baseline. | 33.3 | 55.6 | 11.1 | Insufficient | n = 9 |
| Weight loss patterns | Initial weight loss (kg) | 71.4 | 28.6 | 0 | Insufficient | n = 14 |
| Duration to weight loss goal, and gradual and sustained weight loss vs. early but not sustained | 40 | 40 | 20 | Insufficient | n = 5 | |
| Duration of weight loss maintenance | 100 | 0 | 0 | Insufficient | n = 1 | |
| Weight history (weight cycling and history of weight loss) | 0 | 100 | 0 | Strong | n = 3 | |
| Weight gain since menopause | 0 | 0 | 100 | Insufficient | n = 1 | |
| Monitoring determinants | ||||||
| Monitoring weight | Weekly data reports completed, being frequently weighed in trial, frequent self‐weighing/monitoring body weight | 80 | 20 | 0 | Strong | n = 10 |
| Weight management | 100 | 0 | 0 | Insufficient | n = 1 | |
| Self‐monitoring exercise | Self‐monitoring exercise, use of a pedometer | 75 | 25 | 0 | Moderate | n = 4 |
| Self‐monitoring diet | Counting carbohydrates and counting fats | 0 | 100 | 0 | Insufficient | n = 1 |
| Self‐monitoring eating | 75 | 25 | 0 | Strong | n = 4 | |
| Physical activity determinants | ||||||
| Energy expenditure | Physical activity level at baseline††† | 0 | 100 | 0 | Moderate | n = 3 |
| Increase in physical activity level, energy expenditure, leisure time activity at follow‐up‡‡‡ | 76.2 | 23.8 | 0 | Strong | n = 21 | |
| Change in cardiovascular fitness from baseline to follow‐up‡ | 100 | 0 | 0 | Insufficient | n = 1 | |
| Baseline TV viewing†† | 0 | 0 | 100 | Insufficient | n = 1 | |
| Increase in TV viewing‡‡ | 0 | 0 | 100 | Insufficient | n = 1 | |
| Time sitting | 0 | 100 | 0 | Insufficient | n = 1 | |
| Dietary intake | ||||||
| Eating behaviour | Restrained eating; cognitive restraint eating at baseline††† | 44.4 | 55.6 | 0 | Insufficient | n = 9 |
| Increase in restrained eating‡‡‡ | 50 | 50 | 0 | Insufficient | n = 2 | |
| Flexible restraint post‐weight loss | 0 | 0 | 100 | Insufficient | n = 1 | |
| Meal replacement usage during weight loss and maintenance (as weight management technique) | 20 | 80 | 0 | Strong | n = 4 | |
| Portion control and reducing the amount of food during weight loss and maintenance | 75 | 25 | 0 | Strong | n = 4 | |
| Following a diet (book) or adherence to a diet during weight loss and maintenance. | 66.7 | 33.3 | 0 | Insufficient | n = 3 | |
| Healthy eating at baseline†† | 100 | 0 | 0 | Insufficient | n = 1 | |
| Increase in healthy eating‡‡ | 100 | 0 | 0 | Insufficient | n = 1 | |
| Cut unhealthy food (cut sweet/junk food, decreased fried food consumption, decrease fast food consumption, decrease dessert consumption) during weight loss and maintenance | 87.5 | 12.5 | 0 | Strong | n = 7 | |
| Low fat product use during weight loss maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Not skipping meals and eating breakfast during weight loss maintenance | 50 | 50 | 0 | Insufficient | n = 2 | |
| Energy intake, baseline energy/calorie intake, energy intake level, energy density. | 33.3 | 66.7 | 0 | Insufficient | n = 6 | |
| Decrease or reduction in energy intake, energy density, calories (liquid or solid)‡‡‡ | 80 | 20 | 0 | Strong | n = 10 | |
| Eating out or eating at restaurants during weight loss maintenance | 0 | 100 | 0 | Strong | n = 2 | |
| Eating packaged meals during maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Dietary intake, product level | Change in meat and cheese consumption, decrease‡‡‡ | 50 | 50 | 0 | Insufficient | n = 2 |
| Change in fish consumption, increase‡‡‡ | 0 | 100 | 0 | Moderate | n = 2 | |
| Change in whole grain consumption, increase‡‡‡ | 0 | 100 | 0 | Moderate | n = 2 | |
| Fruit and vegetable intake at baseline††† | 40 | 60 | 0 | Insufficient | n = 5 | |
| Change in fruit and vegetable consumption, increase‡‡‡ | 83.3 | 16.7 | 0 | Strong | n = 6 | |
| Eating takeaway, fast food and sweets at baseline††† | 0 | 50 | 50 | Insufficient | n = 2 | |
| Eating fried food and using unhealthy cooking practices (i.e. cooking with butter) during maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Sugar‐sweetened beverages intake during maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Change in consumption of sugar‐sweetened beverages, coffee and tea with sugar, and juice, decrease‡‡‡ | 80 | 20 | 0 | Strong | n = 5 | |
| Change in consumption of coffee and tea without sugar, without milk and diet drinks, increase‡‡‡ | 33.3 | 66.7 | 0 | Insufficient | n = 3 | |
| Diet drinks intake and water during maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Dietary intake, nutrient level | Change in dietary calcium intake, dairy intake and milk intake, increase‡‡‡ | 50 | 50 | 0 | Insufficient | n = 4 |
| Protein intake | 0 | 100 | 0 | Moderate | n = 2 | |
| Increase in protein intake, substituting protein for fat, substituting protein for carbohydrates during weight loss maintenance | 100 | 0 | 0 | Moderate | n = 2 | |
| (Dietary) fibre intake at baseline††† | 40 | 60 | 0 | Insufficient | n = 5 | |
| Change in (dietary) fibre intake, increase‡‡ | 0 | 100 | 0 | Insufficient | n = 1 | |
| Carbohydrate intake during weight loss and maintenance | 40 | 40 | 20 | Insufficient | n = 5 | |
| Change in carbohydrates, substitute fat for carbs, decrease‡‡ | 100 | 0 | 0 | Insufficient | n = 1 | |
| Fat intake at baseline††† | 37.5 | 50 | 12.5 | Insufficient | n = 8 | |
| Change in fat intake, decrease‡‡‡ | 75 | 25 | 0 | Strong | n = 4 | |
| Cholesterol intake at baseline† | 0 | 100 | 0 | Insufficient | n = 1 | |
| Problematic eating | Binge eating, uncontrolled eating, emotional eating during weight loss and maintenance | 0 | 20 | 80 | Moderate | n = 5 |
| External eating during weight loss maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Reward‐based eating during weight loss and maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Other behaviours | ||||||
| Smoking | 33.3 | 66.7 | 0 | Insufficient | n = 3 | |
| Alcohol intake at baseline‡‡‡ | 33.3 | 66.7 | 0 | Insufficient | n = 3 | |
| Change in alcohol consumption, increase‡ | 0 | 100 | 0 | Insufficient | n = 1 | |
Baseline measurement at the beginning of a weight loss intervention.
Baseline measurement at the beginning of a weight maintenance cohort.
Baseline measurements at the beginning of a long‐term weight loss intervention or at baseline entry in a weight maintenance intervention/cohort.
Increase in measurement from baseline of a weight loss intervention to the end of the follow‐up period.
Increase in measurement from baseline of a weight maintenance intervention/cohort to the end of the follow‐up period.
Increase in measurement from baseline of a weight loss intervention or weight maintenance intervention/cohort to the end of the follow‐up period.
Table 7.
Psychological/cognitive determinants, percentage of directional consistency and level of evidence
| Conceptual category of determinant | Determinant | % Positively predictive of weight loss maintenance | % Not significantly predictive of weight loss maintenance | % Negatively predictive of weight loss maintenance | Level of evidence | Number of studies |
|---|---|---|---|---|---|---|
| Stress | Psychological stress during weight loss and maintenance | 0 | 100 | 0 | Strong | n = 2 |
| Stress about self‐weighing (low) | 100 | 0 | 0 | Insufficient | n = 1 | |
| Stress about self‐monitoring | 0 | 100 | 0 | Insufficient | n = 1 | |
| Depression, mood and psychiatric diagnoses | Depressive symptoms, negative mood | 0 | 66.7 | 33.3 | Insufficient | n = 3 |
| Change in negative mood, increase‡ | 0 | 100 | 0 | Insufficient | n = 1 | |
| Psychosocial difficulties | 0 | 0 | 100 | Insufficient | n = 1 | |
| Emotions | 100 | 0 | 0 | Insufficient | n = 1 | |
| Quality of life | Quality of life – physical | 0 | 100 | 0 | Insufficient | n = 1 |
| Quality of life – mental | 50 | 50 | 0 | Insufficient | n = 2 | |
| Quality of life | 0 | 100 | 0 | Insufficient | n = 1 | |
| Impact of weight loss on quality of life, low | 100 | 0 | 0 | Insufficient | n = 1 | |
| Motivation | Exercise autonomous motivation (high) and intrinsic motivation (high) during weight loss and maintenance | 66.7 | 33.3 | 0 | Insufficient | n = 3 |
| Exercise controlled motivation during weight loss and maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| Motivation during weight loss and maintenance | 100 | 0 | 0 | Insufficient | n = 1 | |
| Self‐efficacy/barriers | Change in self‐efficacy, increase‡ | 0 | 100 | 0 | Insufficient | n = 1 |
| Self‐efficacy for exercise and exercise barriers (high) during weight loss and maintenance | 80 | 20 | 0 | Strong | n = 5 | |
| Change in self‐efficacy for exercise, increase‡ | 100 | 0 | 0 | Insufficient | n = 1 | |
| Self‐efficacy for diet during weight loss maintenance | 100 | 0 | 0 | Moderate | n = 2 | |
| Change in self‐efficacy for diet, increase‡ | 100 | 0 | 0 | Insufficient | n = 1 | |
| Self‐efficacy for weight management and perceived difficulty weight management during weight loss maintenance | 100 | 0 | 0 | Strong | n = 3 | |
| Barriers to Healthy Eating, daily mechanics | 100 | 0 | 0 | Insufficient | n = 1 | |
| Perceived choice | 0 | 100 | 0 | Insufficient | n = 1 | |
| Perceived low physical functioning | 0 | 0 | 100 | Insufficient | n = 1 | |
| Perceived exertion during exercise | 0 | 0 | 100 | Insufficient | n = 1 | |
| Body image | Self‐ideal body size discrepancy (high = negative body image) | 0 | 0 | 100 | Insufficient | n = 1 |
| Self‐awareness | 0 | 100 | 0 | Insufficient | n = 1 | |
| Body shape concerns | 0 | 100 | 0 | Insufficient | n = 2 | |
| Body satisfaction, body attractiveness and body image | 0 | 100 | 0 | Insufficient | n = 2 | |
| Physical self‐worth (high) | 100 | 0 | 0 | Moderate | n = 2 | |
| Perceived self‐body size | 0 | 100 | 0 | Insufficient | n = 1 | |
| Perceived discrepancy between current weight and desired weight | 0 | 100 | 0 | Insufficient | n = 1 | |
| Perceiving others as overweight | 0 | 0 | 100 | Insufficient | n = 1 | |
| Self‐concept | Self‐concept as successful weight maintainer | 100 | 0 | 0 | Insufficient | n = 1 |
| Self‐concept as exerciser | 100 | 0 | 0 | Insufficient | n = 1 | |
| Self‐esteem | 0 | 100 | 0 | Insufficient | n = 1 | |
| Self‐regulation | Change in autonomous self‐regulation, increase‡ | 66.7 | 33.3 | 0 | Insufficient | n = 3 |
| Controlled self‐regulation during weight loss maintenance | 0 | 100 | 0 | Insufficient | n = 1 | |
| External self‐regulation and introjected self‐regulation | 0 | 100 | 0 | Moderate | n = 2 | |
| Focus on progress to sustain engagement in weight control behaviours | 100 | 0 | 0 | Insufficient | n = 1 | |
| Intrinsic exercise goals (high) | 100 | 0 | 0 | Insufficient | n = 1 | |
| Extrinsic exercise goals | 0 | 100 | 0 | Insufficient | n = 1 | |
| Planning exercise | 100 | 0 | 0 | Insufficient | n = 1 | |
| Planning meals and snacks | 0 | 100 | 0 | Insufficient | n = 1 | |
| Disinhibition/impulse control | Disinhibition, low impulse control and impulsivity | 0 | 80 | 20 | Moderate | n = 5 |
| Change in disinhibition, impulse control change‡‡‡ | 33.3 | 66.7 | 0 | Insufficient | n = 3 | |
| Change in internal disinhibition, increase‡‡ | 0 | 0 | 100 | Insufficient | n = 1 | |
| Internal disinhibition (high) | 0 | 0 | 100 | Strong | n = 2 | |
| Change in external disinhibition, decrease‡‡ | 0 | 100 | 0 | Insufficient | n = 1 | |
| External disinhibition | 0 | 50 | 50 | Insufficient | n = 2 | |
| Reinforcement | Baseline reinforcement ratio | 0 | 100 | 0 | Insufficient | n = 1 |
| Change in reinforcement ratio/reinforcement | 0 | 100 | 0 | Moderate | n = 2 |
Baseline measurement at the beginning of a weight loss intervention.
Baseline measurement at the beginning of a weight maintenance cohort.
Baseline measurements at the beginning of a long‐term weight loss intervention or at baseline entry in a weight maintenance intervention/cohort.
Increase in measurement from baseline of a weight loss intervention to the end of the follow‐up period.
Increase in measurement from baseline of a weight maintenance intervention/cohort to the end of the follow‐up period.
Increase in measurement from baseline of a weight loss intervention or weight maintenance intervention/cohort to the end of the follow‐up period.
Table 8.
Social and physical environmental determinants, percentage of directional consistency and level of evidence
| Conceptual category of determinant | Determinant | % Positively predictive of weight loss maintenance | % Not significantly predictive of weight loss maintenance | % Negatively predictive of weight loss maintenance | Level of evidence | Number of studies |
|---|---|---|---|---|---|---|
| Social environmental determinants | ||||||
| Social support | Change in emotional support, increase‡ | 100 | 0 | 0 | Insufficient | n = 1 |
| Social support for behaviour, social support exercise, and social support exercise and diet during weight loss and maintenance | 33.3 | 33.3 | 33.3 | Insufficient | n = 3 | |
| Family discouragement of healthy eating during weight loss and maintenance | 0 | 0 | 100 | Insufficient | n = 1 | |
| Friends' discouragement of healthy eating during weight loss and maintenance | 100 | 0 | 0 | Insufficient | n = 1 | |
| Exercise encouragement during weight loss and maintenance | 0 | 0 | 100 | Insufficient | n = 1 | |
| Perceived need of support | 100 | 0 | 0 | Insufficient | n = 1 | |
| Modification of the attitude of the entourage | 100 | 0 | 0 | Insufficient | n = 1 | |
| Weight‐related teasing | History of weight‐related teasing | 0 | 0 | 100 | Insufficient | n = 1 |
| Physical environmental determinants | ||||||
| Availability of unhealthy food | Keep snack food in house | 0 | 0 | 100 | Insufficient | n = 1 |
Baseline measurement at the beginning of a weight loss intervention.
Baseline measurement at the beginning of a weight maintenance cohort.
Baseline measurements at the beginning of a long‐term weight loss intervention or at baseline entry in a weight maintenance intervention/cohort.
Increase in measurement from baseline of a weight loss intervention to the end of the follow‐up period.
Increase in measurement from baseline of a weight maintenance intervention/cohort to the end of the follow‐up period.
Increase in measurement from baseline of a weight loss intervention or weight maintenance intervention/cohort to the end of the follow‐up period.
Demographic determinants
The five demographic determinants of, age, gender, ethnicity, socioeconomic status and marital status were identified, and the quality and strength of evidence were synthesized for the predictive effect on weight loss maintenance. Consistent evidence was found that age, gender and socioeconomic status were not significantly predictive of weight loss maintenance (Table 5). Insufficient evidence was found to make a conclusion for marital status and ethnicity.
Behavioural determinants
Table 6 shows the 59 behavioural determinants identified in the articles included in this review. These behavioural determinants were grouped into four concepts – weight‐related determinants, monitoring determinants, determinants related to energy expenditure and determinants related to energy/nutritional intake – and a miscellaneous group including determinants such as smoking or alcohol intake.
Of the weight‐related determinants, weight history had strong evidence of being non‐significant in predicting weight loss maintenance. Other determinants showed insufficient evidence.
Self‐monitoring weight and self‐monitoring eating had strong evidence to suggest they were predictive of weight loss maintenance. Self‐monitoring of exercise, on the other hand, had moderate evidence of predicting weight loss maintenance.
Strong evidence was found for physical activity increase being positively predictive of weight loss maintenance, whereas moderate evidence was found for physical activity level at baseline being non‐significant in predicting weight loss maintenance.
Eating behaviours such as portion control, cutting unhealthy foods and reducing energy intake were found to be positively predictive of weight loss maintenance supported by strong evidence. Furthermore, eating out and use of meal replacements were supported by strong evidence to be non‐significant in predicting weight loss maintenance.
At the product level, an increase in fruit and vegetable consumption and a reduction in sugar‐sweetened beverages were positively predictive of weight loss maintenance. The evidence supporting these results were strong. Moderate evidence was found for fish consumption increase and whole grain consumption as non‐significant in predicting weight loss maintenance. At the nutrient level, fat intake decrease was found to be positively predictive of weight loss maintenance.
Problematic eating was found to be negatively predictive of weight loss maintenance with moderate evidence. Other behaviours such as smoking and alcohol consumption had insufficient evidence to draw conclusions.
Psychological/cognitive determinants
Fifty‐one psychological or cognitive determinants were found. These determinants were sorted in the concepts: stress, mood/depression, quality of life, motivation, self‐efficacy and perceived barriers, body image, self‐concept, disinhibition/impulse control and reinforcement (Table 7).
Strong evidence found that psychological stress was non‐significant in predicting weight loss maintenance. Differently, self‐efficacy for exercise and self‐efficacy for weight management were strongly supported to be positively predictive of weight loss maintenance. Moderate evidence was found for self‐efficacy of diet being predictive of weight loss maintenance. Having high physical self‐worth was found to be positively predictive of weight loss maintenance with moderate evidence. Disinhibition or low impulse control was found to not be predictive of weight loss maintenance with moderate evidence, whereas strong evidence supported having high internal disinhibition as negatively predictive of weight loss maintenance. A change in reinforcement was moderately supported to be not predictive of weight loss maintenance. None of the determinants measured in the concept groups of depression and mood, quality of life, motivation and self‐concept had sufficient evidence to draw conclusions.
Social and physical environmental determinants
Table 8 shows the ten social and physical environmental determinants identified in the articles included in this review. The three concepts were social support, weight‐related teasing and availability of unhealthy foods. None of the determinants in this main determinant group had sufficient evidence to draw conclusions for weight loss maintenance. However, family discouragement of healthy eating and exercise encouragement were measured in a high‐quality paper and were reported to be negatively predictive of weight loss maintenance. Additionally, the use of a commercial weight loss programme was not found to be significantly predictive of weight loss maintenance in one high‐quality study.
Discussion
With the findings from this review, the model in Fig. 3 was created, illustrating the influence of the determinants on energy balance. The determinants included in this figure were those with moderate or strong levels of evidence and represent their influence on weight loss maintenance. Arrows indicate the direct and indirect influences of the determinants on weight loss maintenance.
Figure 3.

Determinants of weight loss maintenance. Determinants in bold have a strong level evidence; those not bolded have moderate level of evidence. The green arrows indicate positive factors for weight loss maintenance. The red arrow indicates negative determinants in weight loss maintenance. Determinants that are not significant for weight loss maintenance are represented in the dotted box [Colour figure can be viewed at wileyonlinelibrary.com]
This review identified several energy intake‐reducing behaviours and energy expenditure‐increasing behaviours previously identified in the Elfhag and Rössner review 6. These determinants were the most studied and reported in this review. However self‐evident, these determinants remain key elements in weight loss maintenance.
In Fig. 3, we emphasize the indirect influence that determinants can have on weight loss maintenance. Specifically, self‐monitoring determinants were found to be positively predictive in weight loss maintenance. Previously, Michie et al. 82 and Samdal et al. 83 reported self‐monitoring as one of the five main techniques of self‐regulation, and an effective tool in engaging healthy eating and physical activity. Monitoring determinants are important as they influence behaviours regarding energy intake and expenditure.
In addition to self‐monitoring determinants, several cognitive/psychological determinants also indirectly influence weight loss maintenance, i.e. high self‐efficacy for exercise and self‐efficacy for weight management. A review by Teixeira and colleagues found similar trends in social/cognitive determinants considered to be important for weight loss maintenance 84. Unfortunately, research on the psychological determinants of weight loss maintenance remains limited. Considering the critical influence of self‐efficacy on self‐regulation techniques through its effects on goal setting, preparation for action 85, 86 and consequently behaviour, it may be meaningful to conduct further research in self‐efficacy in promoting weight loss maintenance. Specifically, a systematic review and meta‐analyses on changing physical activity self‐efficacy and behaviour by Olander et al. found four behaviour change techniques that enabled a positive change in self‐efficacy. These techniques are action planning, time management, prompting of self‐monitoring behaviour outcomes and planning of social support change 87. Similarly, a meta‐analysis by Prestwich et al. reports on the increase of self‐efficacy in dietary interventions that stress management and several behaviour change techniques including self‐monitoring, providing feedback and prompting review of behavioural goals 88. We hypothesize that interventions that increase self‐efficacy will enable longer maintenance of weight loss.
When reviewing the existing literature, it is equally important to establish the determinants that do not of influence weight loss maintenance. Interestingly, no demographic determinants had a predictive effect on weight loss maintenance or, rather, lacked evidence to be conclusive (Fig. 3). Fascinatingly, consistent evidence shows that age, gender and socioeconomic status are not significant in predicting weight loss maintenance. This may indicate that target groups are better selected using non‐demographic‐related factors.
In addition to demographic determinants, baseline measures seem to be insignificant or inconclusive in predicting weight loss maintenance. Measures such as baseline physical activity, energy/calorie intake, protein, fat, carbohydrate and dietary intake do not predict weight loss maintenance (Fig. 3). The results of this systematic review propose that individuals can achieve weight loss maintenance despite their baseline dietary intake and baseline physical activity level. The most important determinants appear to be those that involve change in behaviour.
A few articles in this review examined determinants of weight loss maintenance at the nutrient level. With the exception of fat intake decrease, intake of nutrients such as calcium, protein, fibre and carbohydrates failed to show conclusive evidence for achieving weight loss maintenance. It has been previously suggested by Sacks et al. 89 and Katan 90 that macronutrient composition plays a lesser role in weight loss than previously believed. Despite our findings being inconclusive, we hypothesize that determinants at the nutrient level are less important in weight loss maintenance than are other eating behaviours such as overall energy reduction.
Recommendations
On the basis of this systematic review, we recommend that future weight loss maintenance programmes focus on changing behaviour to reduce energy intake through cutting unhealthy foods, decreasing sugar‐sweetened beverage consumption and fat intake, portion control, increasing fruit and vegetable intake, and adhering to a diet. Additionally, energy expenditure should be promoted through increasing physical activity. Greater focus on behaviour change techniques such as self‐monitoring should be regarded as central to future interventions. Furthermore, it is the hypothesis of the reviewers that behaviour change can be predominantly stimulated by helping individuals to develop self‐efficacy for diet, exercise and weight management.
We suggest future research focus on two determinant groups with limited evidence. Firstly, despite cognitive and psychological determinants being reported more frequently in the last decade, there remains a limited amount of evidence for several determinants. One issue we encountered was that studies often use varying theoretical models and different questionnaires, leading to many new determinants being reported but with little replication (Table 3). We hypothesize that cognitive/psychological determinants influence weight loss maintenance through their effect on behaviour. Therefore, we suggest further research to identify psychological and cognitive determinants on weight loss maintenance.
Secondly, environmental determinants were the least measured group of determinants with insufficient evidence to draw any conclusions. Elfhag and Rössner previously suggest that the environment influences opportunities and barriers for engaging in healthy eating and regular physical activity, and thereby weight loss maintenance 6. The most frequently reported environmental determinants were those pertaining to the social environment. Moreover, Elfhag and Rössner 6 and Wing and Hill 91 have mentioned the use of social support by individuals with successful weight loss maintenance in their respective publications. Yet in contrast, Brantley et al. report that friends' encouragement of healthy eating is negatively predictive of weight loss maintenance 23. Evidently, more research needs to be conducted to draw any conclusions. In addition, physical and macro‐environmental determinants for weight loss maintenance were scarcely reported. A singular study by Neve et al. reported not keeping unhealthy food in the house as positively predictive for weight loss maintenance 73. Previously, studies have shown the impact of physical environment on obesity 92. Our hypothesis is that an obesogenic environment would create barriers for weight loss maintenance and may be an intriguing area to investigate. Lastly, the macro‐environment and factors such as gross domestic product per capita 93 and pricing policies 94, 95 have been reported to be associated with weight and weight control behaviours but were not identified in this review on weight loss maintenance.
Limitations
This is the first systematic review summarizing evidence of the determinants of weight loss maintenance while taking methodological quality of studies into account. Moreover, it is the first systematic review to determine the level of evidence for determinants of weight loss maintenance.
Through our inclusion/exclusion criteria and quality assessment, we have aimed to draw conclusions with the best level of evidence. Consequently, our strict criteria may account for the differences to previous reviews. Elfhag and Rössner report achieving greater initial weight loss as a characteristic of an individual successful in weight loss maintenance 6. In our review, we found insufficient evidence to draw the same conclusions. We found initial weight loss to be predictive of weight loss maintenance in 71.4% of the included studies. As our criteria require ≥75% to draw conclusions, the level of evidence for this determinant is insufficient. These cut‐offs remain arbitrary and can explain the differences we find to previous literature. Furthermore, as with any systematic review, the inclusion and exclusion are based on the reviewers and are subject to the researchers' interpretation. We attempt to reduce this subjectivity by having two independent reviewers to include and exclude studies and the third and fourth reviewers to be included if necessary.
We further limited studies to those published in English and those published after 2006. This cut‐off may have led to certain determinants being underreported in this review. Meal rhythm, meal frequency and breakfast consumption, locus of control, personality and attitude are a few determinants discussed in other reviews that either were not reported in the studies we included or were reported less frequently than was previous literature 6, 91.
A further limitation is the great heterogeneity in the studies included in this review. This remains an issue when comparing behavioural determinants as study designs vary greatly. Previous studies attempting to compare behavioural studies have faced similar issues 82. Furthermore, there was a general lack of detail in regard to methodology of interventions. Many included studies have scored low on areas regarding participation selection and validity/reliability of determinant measurement, largely owing to a lack of reporting. Additionally, a range of terminology and methods are used when measuring determinants of weight loss maintenance, making comparability difficult. However, reviews are necessary in order to develop hypotheses for more effective and innovative interventions.
Furthermore, the validity of memory‐based measurements of nutrition has increasingly been questioned in the nutrition field. This may have consequences for studies that may have scored highly in the quality assessment.
Another crucial limitation in this review is the comparison of long‐term weight loss studies to studies differentiating those who are successful in maintenance to those who regain. In long‐term weight loss, the initiation of weight loss is included, whereas studying the maintenance phase or comparing weight maintenance and regain purely observes the maintenance phase. The determinants in these two phases may therefore differ. Such an example is the determinant initial weight loss. In long‐term weight loss trials, the initial weight loss phase is observed in which it may give the appearance that an individual is successful in weight loss maintenance owing to a greater initial weight loss; however, this says little about the actual maintenance of weight loss itself. In essence, the maintenance phase is observing whether an individual can maintain their new weight. This information is lost when observing long‐term weight loss. In the study by Nackers et al., they found that initial weight loss was predictive of long‐term weight loss maintenance, although this was not the case for weight regain 20. Such differences in outcome illustrate the importance of separating the weight loss phase from the maintenance phase in long‐term weight loss maintenance. This may further explain the inconclusive evidence found for some determinants such as initial weight loss. Future studies in determinants of weight loss maintenance need to make clear distinctions between the weight loss phase and maintenance phase.
Conclusion
The overweight and obesity epidemic remains a growing public health issue. With this systematic review, we conclude with a high level of evidence that weight loss maintenance is not entirely reliant on the individual's demographic background but on the behavioural determinants engaging in energy balance and determinants promoting it. The current literature in regard to psychological/cognitive, social, physical and macro‐environmental determinants remain scarce or ambiguous at best. Future solutions in weight loss maintenance likely require a greater focus on self‐efficacy to engage in behaviour change and to maintain it.
Conflict of interest statement
We declare to have no conflict of interest.
Acknowledgement
The contribution of MS is supported by the Innovational Research Incentives Scheme Veni from Nederlandse Organisatie voor Wetenschappelijk Onderzoek (Netherlands Organization for Scientific Research – Division for the Social Sciences) project number 451‐16‐018.
Varkevisser, R. D. M. , van Stralen, M. M. , Kroeze, W. , Ket, J. C. F. , and Steenhuis, I. H. M. (2019) Determinants of weight loss maintenance: a systematic review. Obesity Reviews, 20: 171–211. 10.1111/obr.12772.
References
- 1. Astrup A, Pedersen S. Obesity In: Geissler C, Powers H. (eds). Human Nutrition. Elsevier: London, 2011, pp. 401–424. [Google Scholar]
- 2. Magkos F, Fraterrigo G, Yoshino J et al Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab 2016; 23: 591–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ulen CG. Weight regain prevention. Clin Diab 2008; 26: 100. [Google Scholar]
- 4. Wing RR, Phelan S. Long‐term weight loss maintenance. Am J Clin Nutr 2005; 82: 222S–225S. [DOI] [PubMed] [Google Scholar]
- 5. Dombrowski SU, Knittle K, Avenell A, Araújo‐Soares V, Sniehotta FF. Long term maintenance of weight loss with non‐surgical interventions in obese adults: systematic review and meta‐analyses of randomised controlled trials. The BMJ 2014; 348: g2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev an official journal of the International Association for the Study of Obesity 2005; 6: 67–85. [DOI] [PubMed] [Google Scholar]
- 7. Huang TT, Drewnowski A, Kumanyika SK, Glass TA. A systems‐oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis 2009; 6: A82. [PMC free article] [PubMed] [Google Scholar]
- 8. Murti RDM, Stralen MMV, Ket J, Steenhuis I. Determinants of weight loss maintenance: a systematic review. PROSPERO 2017. CRD42017058033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all‐cause mortality in older adults: a meta‐analysis. Am J Clin Nutr 2014; 99: 875–890. [DOI] [PubMed] [Google Scholar]
- 10. Montesi L, El Ghoch M, Brodosi L, Calugi S, Marchesini G, Dalle Grave R. Long‐term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes: Targets and Therapy 2016; 9: 37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stern JS, Hirsch J, Blair SN et al Weighing the options: criteria for evaluating weight‐management programs. The Committee to Develop Criteria for Evaluating the Outcomes of Approaches to Prevent and Treat Obesity. Obes Res 1995; 3: 591–604. [PubMed] [Google Scholar]
- 12. Rössner SS. Defining success in obesity management. Int J Obes Relat Metab Disord: journal of the International Association for the Study of Obesity 1997; 21: 2–4. [PubMed] [Google Scholar]
- 13. Uijtdewilligen Léonie L, Nauta J, Singh AS et al Determinants of physical activity and sedentary behaviour in young people: a review and quality synthesis of prospective studies. Br J Sports Med; 45: 896–905. [DOI] [PubMed] [Google Scholar]
- 14. Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. John Wiley & Sons, 2008. [Google Scholar]
- 15. Look AHEAD group . Eight‐year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring, Md) 2014; 22: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Neiberg RH, Wing RR, Bray GA et al Patterns of weight change associated with long‐term weight change and cardiovascular disease risk factors in the Look AHEAD Study. Obesity (Silver Spring, Md) 2012; 20: 2048–2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Unick JL, Neiberg RH, Hogan PE et al Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity 2015; 23: 1353–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wadden TA, Neiberg RH, Wing RR et al Four‐year weight losses in the Look AHEAD study: factors associated with long‐term success. Obesity (Silver Spring, Md) 2011; 19: 1987–1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Laitner MH, Minski SA, Perri MG. The role of self‐monitoring in the maintenance of weight loss success. Eat Behav 2016; 21: 193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nackers LM, Ross KM, Perri MG. The association between rate of initial weight loss and long‐term success in obesity treatment: does slow and steady win the race? Int J Behav Med 2010; 17: 161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perri MG, Limacher MC, Durning PE et al Extended‐care programs for weight management in rural communities: the Treatment of Obesity in Underserved Rural Settings (TOURS) randomized trial. Arch Intern Med 2008; 168: 2347–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peterson ND, Middleton KR, Nackers LM, Medina KE, Milsom VA, Perri MG. Dietary self‐monitoring and long‐term success with weight management. Obesity (Silver Spring, Md) 2014; 22: 1962–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brantley PJ, Stewart DW, Myers VH et al Psychosocial predictors of weight regain in the Weight Loss Maintenance trial. J Behav Med 2014; 37: 1155–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Champagne CM, Broyles ST, Moran LD et al Dietary intakes associated with successful weight loss and maintenance during the Weight Loss Maintenance trial. J Am Diet Assoc 2011; 111: 1826–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Coughlin JW, Gullion CM, Brantley PJ et al Behavioral mediators of treatment effects in the Weight Loss Maintenance trial. Ann Behav Med 2013; 46: 369–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Svetkey LP, Ard JD, Stevens VJ et al Predictors of long‐term weight loss in adults with modest initial weight loss, by sex and race. Obesity (Silver Spring, Md) 2012; 20: 1820–1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Linde JA, Utter J, Jeffery RW, Sherwood NE, Pronk NP, Boyle RG. Specific food intake, fat and fiber intake, and behavioral correlates of BMI among overweight and obese members of a managed care organization. Int J Behav Nutr Phys Act 2006; 3: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Linde JA, Erickson DJ, Jeffery RW, Pronk NP, Boyle RG. The relationship between prevalence and duration of weight loss strategies and weight loss among overweight managed care organization members enrolled in a weight loss trial. Int J Behav Nutr Phys Act 2006; 3: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self‐monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring, Md) 2007; 15: 3091–3096. [DOI] [PubMed] [Google Scholar]
- 30. Lillis J, Thomas JG, Niemeier H, Wing RR. Internal disinhibition predicts 5‐year weight regain in the National Weight Control Registry (NWCR). Obes Sci Pract 2016; 2: 83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Raynor DA, Phelan S, Hill JO, Wing RR. Television viewing and long‐term weight maintenance: results from the National Weight Control Registry . Obesity 2006; 14: 1816–1824. [DOI] [PubMed] [Google Scholar]
- 32. Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight‐loss maintenance for 10 years in the National Weight Control Registry . Am J Prev Med 2014; 46: 17–23. [DOI] [PubMed] [Google Scholar]
- 33. Bartfield JK, Stevens VJ, Jerome GJ et al Behavioral transitions and weight change patterns within the PREMIER trial. Obesity 2011; 19: 1609–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen L, Appel LJ, Loria C et al Reduction in consumption of sugar‐sweetened beverages is associated with weight loss: the PREMIER trial. Am J Clin Nutr 2009; 89: 1299–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wingo BC, Desmond RA, Brantley P et al Self‐efficacy as a predictor of weight change and behavior change in the PREMIER trial. J Nutr Educ Behav 2013; 45: 314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cussler EC, Teixeira PJ, Going SB et al Maintenance of weight loss in overweight middle‐aged women through the Internet. Obesity 2008; 16: 1052–1060. [DOI] [PubMed] [Google Scholar]
- 37. Teixeira PJ, Going SB, Houtkooper LB et al Exercise motivation, eating, and body image variables as predictors of weight control. Med Sci Sports Exerc 2006; 38: 179–188. [DOI] [PubMed] [Google Scholar]
- 38. Buscemi J, Murphy JG, Berlin KS, Raynor HA. A behavioral economic analysis of changes in food‐related and food‐free reinforcement during weight loss treatment. J Consult Clin Psychol 2014; 82: 659–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Raynor HA, Steeves EA, Hecht J, Fava JL, Wing RR. Limiting variety in non‐nutrient‐dense, energy‐dense foods during a lifestyle intervention: a randomized controlled trial. Am J Clin Nutr 2012; 95: 1305–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Annesi JJ, Mareno N, McEwen KL. Mediation of self‐regulation and mood in the relationship of changes in high emotional eating and nutritional behaviors: moderating effects of physical activity. Scand J Psychol 2016; 57(6): 523–534. [DOI] [PubMed] [Google Scholar]
- 41. Annesi JJ, Johnson PH, Tennant GA, Porter KJ, McEwen KL. Weight loss and the prevention of weight regain: evaluation of a treatment model of exercise self‐regulation generalizing to controlled eating. Perm J 2016; 20: 4–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Barone Gibbs B, Kinzel LS, Pettee Gabriel K, Chang YF, Kuller LH. Short‐ and long‐term eating habit modification predicts weight change in overweight, postmenopausal women: results from the WOMAN study. J Acad Nutr Diet 2012; 112: 1347–1355 55.e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Befort CA, Stewart EE, Smith BK, Gibson CA, Sullivan DK, Donnelly JE. Weight maintenance, behaviors and barriers among previous participants of a university‐based weight control program. Int J Obes (2005) 2008; 32: 519–526. [DOI] [PubMed] [Google Scholar]
- 44. Brock DW, Chandler‐Laney PC, Alvarez JA, Gower BA, Gaesser GA, Hunter GR. Perception of exercise difficulty predicts weight regain in formerly overweight women. Obesity (Silver Spring, Md) 2010; 18: 982–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chandler‐Laney PC, Hunter GR, Ard JD, Roy JL, Brock DW, Gower BA. Perception of others' body size influences weight loss and regain for European American but not African American women. Health Psychol 2009; 28: 414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cox TL, Malpede CZ, Desmond RA et al Physical activity patterns during weight maintenance following a low‐energy density dietary intervention. Obesity 2007; 15: 1226–1232. [DOI] [PubMed] [Google Scholar]
- 47. Del Corral P, Bryan DR, Garvey WT, Gower BA, Hunter GR. Dietary adherence during weight loss predicts weight regain. Obesity (Silver Spring, Md) 2011; 19: 1177–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Flood A, Mitchell N, Jaeb M et al Energy density and weight change in a long‐term weight‐loss trial. Int J Behav Nutr Phys Act 2009; 6: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Greene LF, Malpede CZ, Henson CS, Hubbert KA, Heimburger DC, Ard JD. Weight maintenance 2 years after participation in a weight loss program promoting low‐energy density foods. Obesity (Silver Spring, Md) 2006; 14: 1795–1801. [DOI] [PubMed] [Google Scholar]
- 50. Mason AE, Epel ES, Aschbacher K et al Reduced reward‐driven eating accounts for the impact of a mindfulness‐based diet and exercise intervention on weight loss: data from the SHINE randomized controlled trial. Appetite 2016; 100: 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity (Silver Spring, Md) 2007; 15: 2485–2494. [DOI] [PubMed] [Google Scholar]
- 52. Ochner CN, Lowe MR. Self‐reported changes in dietary calcium and energy intake predict weight regain following a weight loss diet in obese women. J Nutr 2007; 137: 2324–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Phelan S, Wing RR, Loria CM, Kim Y, Lewis CE. Prevalence and predictors of weight‐loss maintenance in a biracial cohort: results from the coronary artery risk development in young adults study. Am J Prev Med 2010; 39: 546–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wang X, Lyles MF, You T, Berry MJ, Rejeski WJ, Nicklas BJ. Weight regain is related to decreases in physical activity during weight loss. Med Sci Sports Exerc 2008; 40: 1781–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. West DS, Gorin AA, Subak LL et al A motivation‐focused weight loss maintenance program is an effective alternative to a skill‐based approach. Int J Obes (2005) 2011; 35: 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self‐regulation program for maintenance of weight loss. N Engl J Med 2006; 355: 1563–1571. [DOI] [PubMed] [Google Scholar]
- 57. Szabo‐Reed AN, Lee J, Ptomey L et al Longitudinal weight loss patterns and their behavioral and demographic associations. Ann Behav Med: a publication of the Society of Behavioral Medicine 2016; 50: 147–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Tate DF, Jeffery RW, Sherwood NE, Wing RR. Long‐term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? Am J Clin Nutr 2007; 85: 954–959. [DOI] [PubMed] [Google Scholar]
- 59. Volger S, Wadden TA, Sarwer DB et al Changes in eating, physical activity and related behaviors in a primary care‐based weight loss intervention. Int J Obes (Lond) 2013; 37: S12–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wang J, Ye L, Zheng Y, Burke LE. Impact of perceived barriers to healthy eating on diet and weight in a 24‐month behavioral weight loss trial. J Nutr Educ Behav 2015; 47: 432–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Giel KE, Binkele M, Becker S, Stubler P, Zipfel S, Enck P. Weight reduction and maintenance in a specialized outpatient health care center. Obes Res Clin Pract 2008; 2 I‐ii. [DOI] [PubMed] [Google Scholar]
- 62. Hübner C, Baldofski S, Crosby RD, Müller A, de Zwaan M, Hilbert A. Weight‐related teasing and non‐normative eating behaviors as predictors of weight loss maintenance. A longitudinal mediation analysis. Appetite 2016; 102: 25–31. [DOI] [PubMed] [Google Scholar]
- 63. Postrach E, Aspalter R, Elbelt U et al Determinants of successful weight loss after using a commercial web‐based weight reduction program for six months: cohort study. J Med Internet Res 2013; 15: e219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Weygandt M, Mai K, Dommes E et al Impulse control in the dorsolateral prefrontal cortex counteracts post‐diet weight regain in obesity. Neuroimage 2015; 109: 318–327. [DOI] [PubMed] [Google Scholar]
- 65. Keränen A‐M, Savolainen MJ, Reponen AH et al The effect of eating behavior on weight loss and maintenance during a lifestyle intervention. Prev Med: An International Journal Devoted to Practice and Theory 2009; 49: 32–38. [DOI] [PubMed] [Google Scholar]
- 66. Lindstrom J, Peltonen M, Eriksson JG et al High‐fibre, low‐fat diet predicts long‐term weight loss and decreased type 2 diabetes risk: the Finnish Diabetes Prevention Study. Diabetologia 2006; 49: 912–920. [DOI] [PubMed] [Google Scholar]
- 67. Nurkkala M, Kaikkonen K, Vanhala ML, Karhunen L, Keränen A‐M, Korpelainen R. Lifestyle intervention has a beneficial effect on eating behavior and long‐term weight loss in obese adults. Eat Behav 2015; 18: 179–185. [DOI] [PubMed] [Google Scholar]
- 68. Pekkarinen T, Kaukua J, Mustajoki P. Long‐term weight maintenance after a 17‐week weight loss intervention with or without a one‐year maintenance program: a randomized controlled trial. J Obes 2015: 651460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Nakade M, Aiba N, Morita A, Miyachi M, Sasaki S, Watanabe S. What behaviors are important for successful weight maintenance? J Obes 2012; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Nakata Y, Okada M, Hashimoto K, Harada Y, Sone H, Tanaka K. Weight loss maintenance for 2 years after a 6‐month randomised controlled trial comparing education‐only and group‐based support in Japanese adults. Obes Facts 2014; 7: 376–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Yamada T, Hara K, Svensson AK et al Successfully achieving target weight loss influences subsequent maintenance of lower weight and dropout from treatment. Obesity (Silver Spring, Md) 2015; 23: 183–191. [DOI] [PubMed] [Google Scholar]
- 72. Clifton PM, Keogh JB, Noakes M. Long‐term effects of a high‐protein weight‐loss diet. Am J Clin Nutr 2008; 87: 23–29. [DOI] [PubMed] [Google Scholar]
- 73. Neve MJ, Morgan PJ, Collins CE. Behavioural factors related with successful weight loss 15 months post‐enrolment in a commercial web‐based weight‐loss programme. Public Health Nutr 2012; 15: 1299–1309. [DOI] [PubMed] [Google Scholar]
- 74. Santos I, Mata J, Silva MN, Sardinha LB, Teixeira PJ. Predicting long‐term weight loss maintenance in previously overweight women: a signal detection approach. Obesity (Silver Spring, Md) 2015; 23: 957–964. [DOI] [PubMed] [Google Scholar]
- 75. Silva MN, Markland D, Carraca EV et al Exercise autonomous motivation predicts 3‐yr weight loss in women. Med Sci Sports Exerc 2011; 43: 728–737. [DOI] [PubMed] [Google Scholar]
- 76. Buclin‐Thiébaud S, Pataky Z, Bruchez V, Golay A. New psycho‐pedagogic approach to obesity treatment: a 5‐year follow‐up. Patient Educ Couns 2010; 79: 333–337. [DOI] [PubMed] [Google Scholar]
- 77. Due A, Larsen TM, Mu H et al The effect of three different ad libitum diets for weight loss maintenance: a randomized 18‐month trial. Eur J Nutr 2015; 56(2): 727–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Greenberg I, Stampfer MJ, Schwarzfuchs D, Shai I. Adherence and success in long‐term weight loss diets: the dietary intervention randomized controlled trial (DIRECT). J Am Coll Nutr 2009; 28: 159–168. [DOI] [PubMed] [Google Scholar]
- 79. Lenoir L, Maillot M, Guilbot A, Ritz P. Primary care weight loss maintenance with behavioral nutrition: an observational study. Obesity (Silver Spring, Md) 2015; 23: 1771–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Senechal M, Arguin H, Bouchard DR et al Weight gain since menopause and its associations with weight loss maintenance in obese postmenopausal women. Clin Interv Aging 2011; 6: 221–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Vogels N, Westerterp‐Plantenga MS. Successful long‐term weight maintenance: a 2‐year follow‐up. Obesity (Silver Spring, Md) 2007; 15: 1258–1266. [DOI] [PubMed] [Google Scholar]
- 82. Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta‐regression. Health Psychol 2009; 28: 690–701. [DOI] [PubMed] [Google Scholar]
- 83. Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta‐regression analyses. Int J Behav Nutr Phys Act 2017; 14: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Teixeira PJ, Carraca EV, Marques MM et al Successful behavior change in obesity interventions in adults: a systematic review of self‐regulation mediators. BMC Med 2015; 13: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Locke EA. New directions in goal‐setting theory. Curr Dir Psychol Sci 2006; 15: 265. [Google Scholar]
- 86. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice Hall: Englewood Cliffs, NJ, 1986. [Google Scholar]
- 87. Olander EK, Fletcher H, Williams S, Atkinson L, Turner A, French DP. What are the most effective techniques in changing obese individuals' physical activity self‐efficacy and behaviour: a systematic review and meta‐analysis. Int J Behav Nutr Phys Act 2013; 10: 29–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Prestwich A, Kellar I, Parker R et al How can self‐efficacy be increased? Meta‐analysis of dietary interventions. Health Psychol Rev 2014; 8: 270–285. [DOI] [PubMed] [Google Scholar]
- 89. Sacks FM, Bray GA, Carey VJ et al Comparison of weight‐loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009; 360: 859–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Katan MB. Weight‐loss diets for the prevention and treatment of obesity. N Engl J Med 2009; 360: 923–925. [DOI] [PubMed] [Google Scholar]
- 91. Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr 2001; 21: 323. [DOI] [PubMed] [Google Scholar]
- 92. Mackenbach JD, Rutter H, Compernolle S et al Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health 2014; 14: 233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Cameron AJ, Van Stralen MM, Kunst AE et al Macroenvironmental factors including GDP per capita and physical activity in Europe. Med Sci Sports Exerc 2013; 45: 278–285. [DOI] [PubMed] [Google Scholar]
- 94. Steenhuis IHM, Waterlander WE, de Mul A. Consumer food choices: the role of price and pricing strategies. Public Health Nutr 2011; 14: 2220–2226. [DOI] [PubMed] [Google Scholar]
- 95. Waterlander WE, Steenhuis IHM, de Boer MR, Schuit AJ, Seidell JC. Introducing taxes, subsidies or both: the effects of various food pricing strategies in a web‐based supermarket randomized trial. Prev Med 2012; 54: 323–330. [DOI] [PubMed] [Google Scholar]


