Abstract
This case illustrates a rare, underdiagnosed disease, with a high mortality rate that is frequently misdiagnosed as acute bacterial endocarditis. Clinicians should include non-bacterial thrombotic endocarditis (NBTE) as a differential diagnosis in patients with culture-negative endocarditis, so that its underlying etiology can be further investigated.
Keywords: non-bacterial thrombotic endocarditis, pancreatic cancer, infectious endocarditis, echocardiogram
Introduction
Non-bacterial thrombotic endocarditis (NBTE) is a rare syndrome, with a similar presentation to infective endocarditis (IE) [1-3]. The cause of NBTE is the presence of a hypercoagulable state due to an underlying malignancy, or an autoimmune disease, predisposing to thrombus formation on cardiac valves (most commonly involving the aortic and mitral valves) [1]. An antemortem diagnosis of NBTE is exceedingly rare [4].
Case presentation
A 67-year-old male presented to the emergency department for loss of vision, slurred speech, and altered mental status for one day. He experienced symptoms two months prior to admission, including night sweats, a 15-pound weight loss, but denied fever. He is an active smoker and cocaine user. His past medical history includes hypertension, type II diabetes mellitus, chronic kidney disease, and bilateral lower extremity deep venous thrombosis. Upon admission, he presented with the following vital signs: temperature: 101.1˚F; blood pressure: 118/65 mmHg; heart rate: 72 beats/minute; respiratory rate: 15 breaths/minute. On examination, he was confused with anisocoria, and non-reactive pupils. The remainder of his cardiopulmonary examination was normal. His initial laboratory results were significant for leukocytosis of 19.3 K/μL, with an 82% neutrophil count, and a C-reactive protein level of 105 mg/dL. An MRI study of the head indicated bilateral thalamic, left midbrain, pons, and bilateral cerebellar infarcts with a mass effect. A transesophageal echocardiogram (TEE) revealed multiple echogenic densities that were approximately 0.6 cm in size, involving both the anterior, and posterior mitral leaflets (Figures 1, 2). He was started on empiric broad-spectrum antibiotics for suspected IE. Due to a combination of multiple negative blood cultures, persistent fever while on antibiotics, and weight loss, there was a suspicion for NBTE.
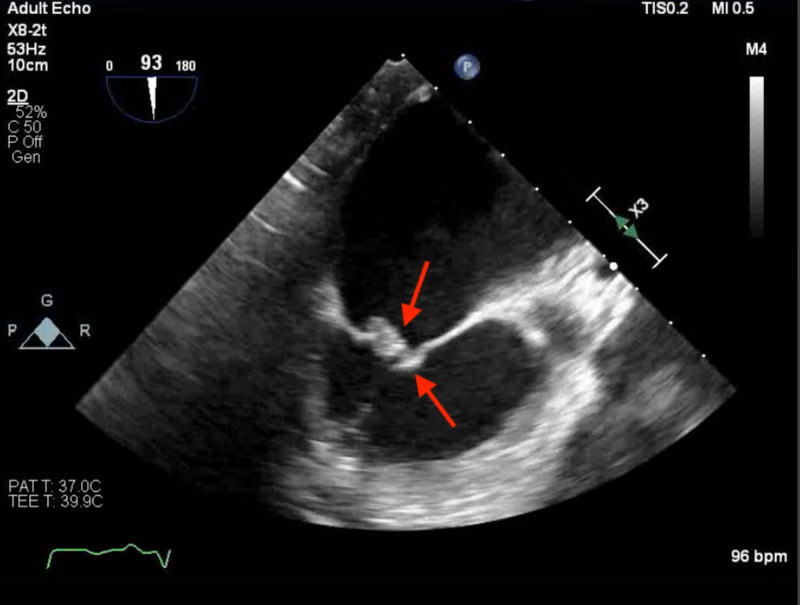
Figure 1. Transesophageal echocardiogram (TEE).
The results of a TEE study: echogenic densities, approximately 0.6 cm in size, involving both anterior and posterior mitral leaflets, primarily at the tips, suggestive of endocarditis.
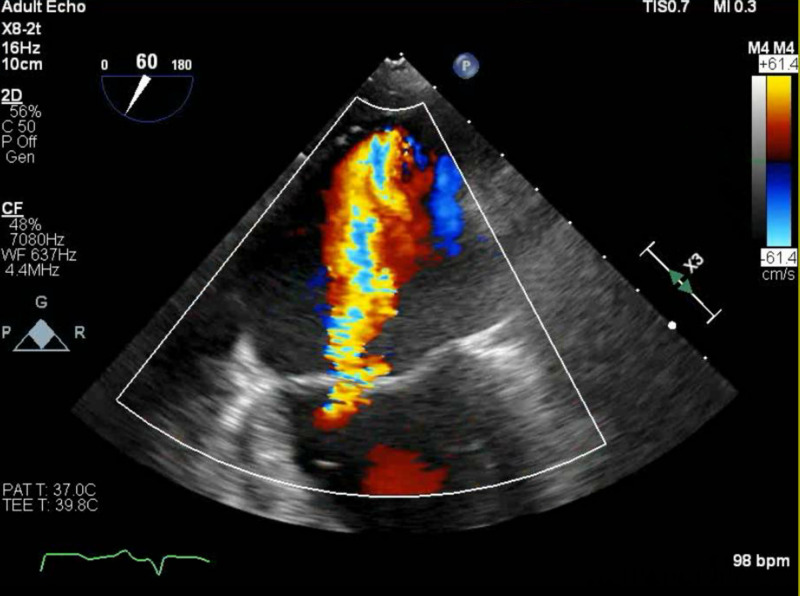
Figure 2. Transesophageal echocardiogram (TEE).
This TEE image demonstrates regurgitant flow over the mitral valve.
CT of the chest, abdomen, and pelvis revealed bilateral pulmonary emboli, with metastatic disease found throughout the liver. The study also revealed a heterogeneous mass, with areas of necrosis at the distal body/tail of the pancreas, consistent with a metastatic pancreatic carcinoma (Figure 3). Antibiotics were discontinued, and unfractionated heparin was initiated.
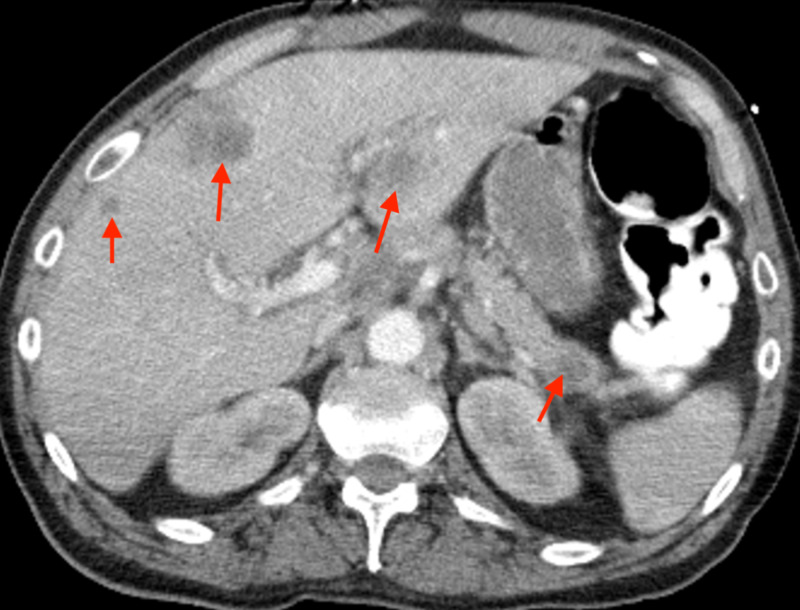
Figure 3. CT of the abdomen with contrast.
The study reveals diffuse metastatic disease found throughout the liver and a heterogeneous mass with areas of necrosis at the distal body and tail of the pancreas. These findings are consistent with a metastatic pancreatic carcinoma.
Discussion
The pathophysiology of pancreatic cancer and NBTE involves the release of prothrombotic molecules from cancer cells, such as tissue factor, cancer procoagulant, and mucin, which form a hypercoagulable state [1].
NBTE and IE are difficult to distinguish. However, there are several differences between the two conditions. In NBTE, patients are less likely to have fever and leukocytosis. In addition, the vegetations are smaller than 1 cm and friable. They rarely cause significant hemodynamic instability, valvular destruction, or cardiac murmurs [2]. Recurrent emboli are considered a hallmark feature of NBTE, occurring in up to 50% of patients, which are widely distributed in the body, involving the kidneys, spleen, skin, and extremities [3,5].
Both NBTE and IE are often evaluated with echocardiography. A TEE is more sensitive than a transthoracic echocardiogram; however, a retrospective study indicated that TEE studies were able to detect vegetations in only 18% of NBTE patients [6].
Fever with leukocytosis stemming from embolic complications often makes the diagnosis of NBTE challenging, as in our patient. It is important to rule out IE in order to avoid the overuse of antibiotics and antimicrobial resistance.
Therapy of NBTE involves treating its underlying etiology, and effective systemic anticoagulation, considering 50% of patients with NBTE present with systemic emboli [5]. Unfractionated heparin remains the anticoagulant of choice, as warfarin is implicated in recurrent thromboembolic events, and the efficacy of newer anticoagulant medications remains unknown.
Conclusions
NBTE is a rare, devastating condition, which is clinically difficult to distinguish from IE. Although the two conditions are difficult to discern, clinicians should be aware of their key differences. Due to its catastrophic complications, antemortem cases of NBTE are very rare. Early diagnosis relies upon a strong clinical suspicion. NBTE should be considered by clinicians as a differential diagnosis in patients with culture negative endocarditis and multiple embolic complications, prompting further investigation of the underlying etiology.
Acknowledgments
We would like to acknowledge the contributions of Dr. Arsalan Hashmi, MBBS, and Dr. Adnan Sadiq, MD. Both were instrumental in obtaining the echocardiogram images. We thank them for their efforts.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Severe fatal systemic embolism due to non-bacterial thrombotic endocarditis as the initial manifestation of gastric adenocarcinoma: case report. Moţăţăianu A, Maier S, Gothard A, Bajkó Z, Bălaşa R. J Crit Care Med. 2018;4:68–73. doi: 10.2478/jccm-2018-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Non-bacterial thrombotic endocarditis. Asopa S, Patel A, Khan OA, Sharma R, Ohri SK. Eur J Cardiothorac Surg. 2007;32:696–701. doi: 10.1016/j.ejcts.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 3.Nonbacterial thrombotic endocarditis concomitant with repeated systemic embolization that received palliative care based on the antemortem diagnosis. Shibata N, Matsumoto K, Kitamura S, Sakashita A, Kizawa Y, Hirata KI. Intern Med. 2018;57:3559–3563. doi: 10.2169/internalmedicine.1381-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nonbacterial thrombotic endocarditis in pancreatic cancer. Piovanelli B, Rovetta R, Bonadei I, Vizzardi E, D'Aloia A, Metra M. Monaldi Arch Chest Dis. 2013;80:189–192. doi: 10.4081/monaldi.2013.5236. [DOI] [PubMed] [Google Scholar]
- 5.Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. el-Shami K, Griffiths E, Streiff M. Oncologist. 2007;12:518–523. doi: 10.1634/theoncologist.12-5-518. [DOI] [PubMed] [Google Scholar]
- 6.Yield of transesophageal echocardiography for nonbacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia. Dutta T, Karas MG, Segal AZ, Kizer JR. Am J Cardiol. 2006;97:894–898. doi: 10.1016/j.amjcard.2005.09.140. [DOI] [PubMed] [Google Scholar]