Abstract
The immune system enables organisms to combat infections and to eliminate endogenous challenges. Immune responses can be evoked through diverse inducible pathways. However, various constitutive mechanisms are also required for immunocompetence. The inducible responses of pattern recognition receptors of the innate immune system and antigen-specific receptors of the adaptive immune system are highly effective, but they also have the potential to cause extensive immunopathology and tissue damage, as seen in many infectious and autoinflammatory diseases. By contrast, constitutive innate immune mechanisms, including restriction factors, basal autophagy and proteasomal degradation, tend to limit immune responses, with loss-of-function mutations in these pathways leading to inflammation. Although they function through a broad and heterogeneous set of mechanisms, the constitutive immune responses all function as early barriers to infection and aim to minimize any disruption of homeostasis. Supported by recent human and mouse data, in this Review we compare and contrast the inducible and constitutive mechanisms of immunosurveillance.
Subject terms: Infectious diseases, Infection, Innate immunity
Constitutive innate immune mechanisms, such as restriction factors, RNA interference, antimicrobial peptides, basal autophagy and proteasomal degradation, exert early host defence activities that also aim to minimize tissue damage and homeostatic disruption by limiting the activation of inducible innate immunity.
Introduction
A major challenge for living organisms is to maintain homeostasis in response to changes in external and internal environments. These include alterations in nutrient and water supplies, physical stress, temperature changes, physiological stress, infections and malignancies1. Through billions of years of evolution, the forms of life and biological processes that cope with these challenges in the most successful way have been selected. One challenge that all organisms have to deal with is the elimination of microorganisms and of abnormal or damaged cellular material. The ideal immune response would eliminate the potential threat and re-establish homeostasis without causing excessive damage to healthy cells and tissues. However, immune responses to infections are often disruptive and can cause marked tissue damage2,3. Such responses are evolutionarily advantageous when the benefit of eliminating the challenge outweighs the risk of associated tissue damage and the requirement for regeneration. However, for potential challenges that occur frequently but rarely develop into serious homeostasis-altering threats, it is not desirable to mount systemic or potentially disruptive immune responses. In addition, vigorous immune responses are not desirable in organs and tissues that are particularly sensitive to immune-mediated damage, such as the brain. Therefore, the ideal immune response has checks and balances, which allow the organism to modulate the magnitude and duration of the response according to the nature of the threat caused by the challenge.
The mammalian immune system, as we understand it today, is induced mainly by two types of receptor systems, the germline-encoded pattern recognition receptors (PRRs), which initiate innate immune responses, and the antigen-specific receptors generated through gene rearrangement after antigen encounter, which initiate adaptive immune responses4–6. The immune responses induced by PRRs, such as Toll-like receptors (TLRs), interact with those induced by antigen-specific receptors; this interaction is notably represented by dendritic cells, which rely on PRR-driven cues to initiate dendritic cell maturation for the stimulation of lymphocytes through antigen-specific receptors5. However, the research literature contains numerous reports of host defence activities that occur independently of both PRR-based immunity and antigen-specific receptors7–10, and emerging evidence suggests that several of these mechanisms have non-redundant roles in host defence in humans11,12. Here we review the literature on this topic by focusing on constitutive immune mechanisms. On the basis of this analysis, and by integrating concepts previously reviewed13, we propose that this constitutive layer of innate immunity exerts early host defence activities through specific molecular mechanisms and at the same time limits PRR activation as a specific feature.
Constitutive and inducible mechanisms
The innate immune system uses both constitutive and inducible mechanisms to eliminate infections and damaged self to maintain homeostasis (Fig. 1). Although the constitutive mechanisms have the advantage of providing an immediate response to a danger signal, they lack the potential to amplify the response. In addition, constitutive mechanisms consume energy to remain operative, and there are hence limits to how many of these can be maintained in any one organism. By contrast, inducible mechanisms such as those mediated through PRRs, as well as antigen-specific receptors, are activated only in response to stimuli and have the ability to amplify signals many times. Hence, inducible mechanisms can give rise to very strong and efficient immune responses, but can also lead to excess inflammation and immunopathology. Given their amplification potential, inducible immune mechanisms require tight control and negative regulatory systems.
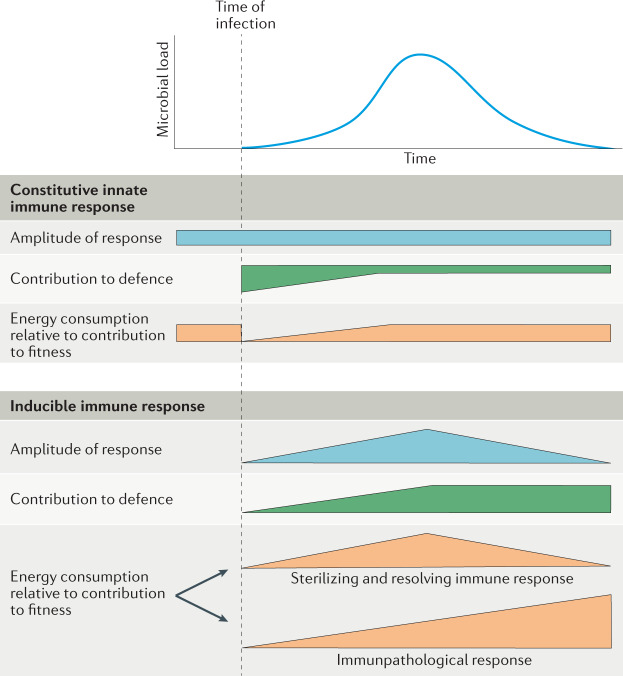
Fig. 1. Constitutive innate immune responses versus inducible immune responses.
Illustration of how constitutive and inducible immune responses vary over time during the course of a generalized infection, and their impact on host defence, energy consumption and host fitness. In the case of a sterilizing and resolving immune response, the additional energy consumption required by the inducible immune response is balanced by the re-establishment of homeostasis. By contrast, in the case of an immunopathological response, the energy that is consumed to mount an inducible response does not benefit the host and instead leads to tissue damage and disruption of homeostasis.
The constitutive immune mechanisms can be divided into the chemical and physical barriers of the body, such as skin, saliva, stomach acid and urine flow, which are not the focus of this Review, and various molecularly defined mechanisms that control microbial infection and/or replication1. Although these mechanisms have been known for many years, they have generally been considered to have only minor roles in the immune system, and evidence has been lacking as to their specific, non-redundant functions in host defence. Consequently, they have not received much attention in front-line immunology research. Here we discuss the constitutive innate immune responses in comparison with the better-described inducible innate responses triggered by PRRs. In addition, we present evidence suggesting that efficient action of constitutive innate immune mechanisms leads to both antimicrobial activity and mitigation of PRR-driven activities (Fig. 2).
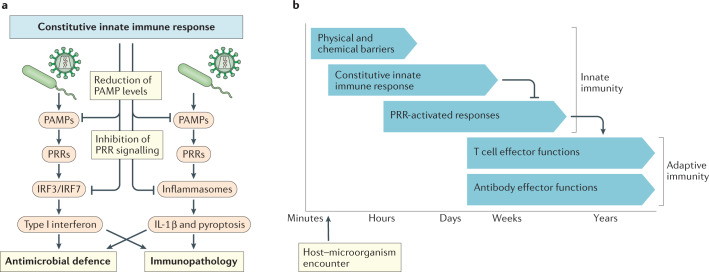
Fig. 2. Constitutive innate immune responses negatively regulate inducible immune responses.
a | Constitutive innate immune mechanisms eliminate pathogens during the initial stages of an infection, which prevents the accumulation of pathogen-associated molecular patterns (PAMPs) that would otherwise activate an inducible immune response through pattern recognition receptors (PRRs). In addition, many of the constitutive mechanisms are known to directly downregulate PAMP signalling through PRRs. Both of these effects limit PRR-induced expression of type I interferon and IL-1β. b | The relationship between the different proposed layers of the immune response. A first layer of defence is exerted by physical and chemical barriers. Constitutive innate immune mechanisms function as soon as a danger signal is detected and eliminate harmful microorganisms and host molecules by specific non-inflammatory mechanisms that operate independently of PRRs. This prevents establishment of the infection and accumulation of PAMPs, thus limiting the activation of PRR-based inducible innate immune responses. If PRR-based immunity is activated, owing to the level of PAMPs exceeding a certain threshold, this leads to inflammation and promotes activation of the adaptive immune response mediated by T cells and antibodies. IRF, interferon regulatory factor.
PRR-activated inducible innate immune responses
PRRs detect pathogen-associated molecular patterns (PAMPs), microorganism-associated molecular patterns14, host-derived danger-associated molecular patterns15 and molecular signatures associated with homeostasis-altering molecular processes16. These molecular patterns activate PRR signalling, which ultimately leads to the transcription of antimicrobial and proinflammatory genes. Downstream activities of PRR signalling include the production of type I interferon (interferon-α (IFNα) and IFNβ), IL-1β and tumour necrosis factor (TNF). These cytokines, in turn, activate antimicrobial and proinflammatory activities, as well as the maturation of antigen-specific adaptive immune responses17,18. PRR-based immune responses can be highly potent, and numerous inflammatory diseases are driven by excessive PRR signalling pathways2,19,20 (Box 1). However, the nature of PRR-based immunity is influenced by many factors, and it is worth mentioning that the gut microbiota and chronic viral infections can induce PRR-based, host-beneficial responses that tend towards tolerance rather than inflammation21,22. Nevertheless, given the potency of PRR-based immunity, full activation of PRR-driven immune responses each time a microorganism is encountered may not be beneficial for an organism in the longer term. Moreover, it is essential to control the activation and duration of PRR signalling-induced activities. This is achieved through multiple mechanisms, including two-step procedures for full PRR activation23,24, the requirement for a threshold PAMP concentration to achieve PRR activation25–28, amplification loops from initial low responses29 and numerous negative-feedback mechanisms30. One way in which the activation of PRR signalling in response to very low levels of PAMPs is avoided at the molecular level is through supramolecular organizing centres. These are higher-order signalling complexes at specific subcellular locations that rely on amplification mechanisms to achieve full activation, thus preventing signalling by subthreshold levels of PAMPs but amplifying signalling by superthreshold levels of PAMPs29. The double-edged sword-like nature of PRR-induced immune responses in terms of their roles in both protection and disease is also supported by evolutionary evidence. This includes the recurring loss of 2′-5′-oligoadenylate synthase 1 (OAS1) in primates31. OAS1 is an interferon-inducible protein that is associated with both antiviral and pathological activities32,33.
Box 1 Diseases induced by excessive production of IL-1 and type I interferon.
Excessive or prolonged activation of pattern recognition receptor (PRR) signalling is associated with a range of human diseases. Several cytokines are involved in PRR-driven diseases, including tumour necrosis factor (TNF), IL-1β, IL-6 and type I interferon169,170. Among these, IL-1β and type I interferon are induced exclusively by PRR signalling. Thus, the existence of human diseases that are mediated by these two classes of cytokines provides strong evidence for the pathological potential of PRR-based immune responses. Here we describe some examples of sterile inflammation involving IL-1β and type I interferon. We now know that diseases such as familial Mediterranean fever, TNF receptor-associated periodic syndrome, hyper-IgD syndrome and cryopyrin-associated periodic syndrome are characterized by increased expression of IL-1β; furthermore, blocking IL-1-induced signalling in these disease can relieve clinical symptoms and improve disease outcome171. Similarly, diseases such as Aicardi–Goutières syndrome, stimulator of interferon gene (STING)-associated vasculopathy with onset in infancy, Sjögren syndrome, proteasome-associated autoinflammatory syndromes and systemic lupus erythematosus are associated with high levels of expression of interferon-stimulated genes (known as an ‘interferon signature’) and are termed ‘interferonopathies’, although the precise contribution of the interferon signature to disease pathogenesis is not completely understood170. For several of these diseases, inhibition of Janus kinase 1 (JAK1) and JAK3, which are involved in interferon-induced signalling, significantly reduces disease activity172. There are marked differences in the pathogenesis of IL-1-driven diseases and interferon-driven diseases. Diseases that depend on IL-1 are generally neutrophilic and associated with fever and increased levels of acute phase reactants, whereas interferon-driven diseases are characterized mainly by lymphopenia, vasculitis, central nervous system manifestations in some diseases, skin manifestations and varying levels of autoantibodies171,173.
Constitutive innate immune mechanisms
Constitutive innate immune mechanisms respond to microbial activities, cellular stress and metabolic alterations by inducing antimicrobial effector functions. As there is most evidence for constitutive innate immune mechanisms that exert antiviral and antibacterial activities, these are the focus of this Review (Fig. 3). A large range of constitutive mechanisms of innate immunity have been identified, including restriction factors, antimicrobial peptides, basal autophagy and proteasomal degradation (Box 2; Table 1). Here we divide these mechanisms into two classes: those that target specific steps in microbial replication cycles, such as restriction factors34,35, and those that lead to degenerative processes, such as autophagy9,36. The constitutive mechanisms that target specific steps in microbial replication function by blocking molecularly defined events that are essential for the replication of specific microorganisms but are dispensable for cellular fitness. By contrast, those mechanisms that operate through degenerative programmes target microbial or altered host molecules for recycling or degradation. The modes of action of representative examples from each of these mechanistic classes are described in the following sections.
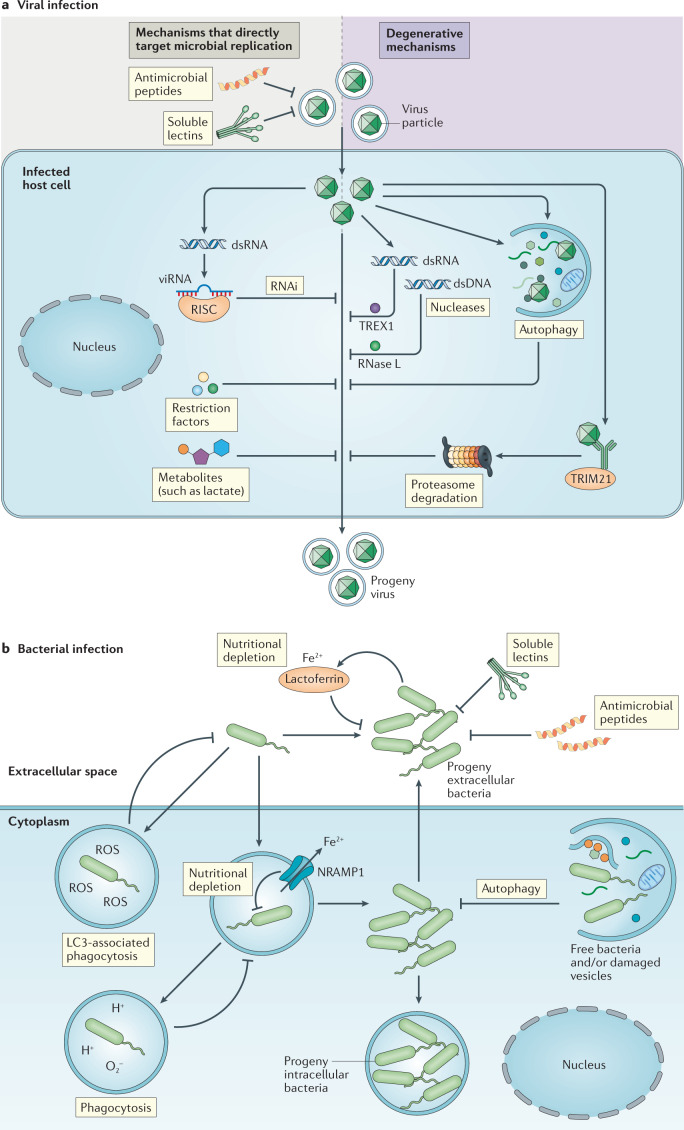
Fig. 3. Overview of the regulation of microbial replication by constitutive innate immune mechanisms.
a | Constitutive innate immune mechanisms and viral infection. The accumulation of specific viral molecular structures (such as double-stranded RNA (dsRNA) or capsids) and cellular stress responses (such as autophagy) activate constitutive–latent mechanisms with direct antiviral activity, independently of pattern recognition receptors. Some of the antiviral effector functions target microbial replication by blocking specific steps in the replication cycles of viruses; these effectors include soluble lectins, antimicrobial peptides, restriction factors, RNA interference (RNAi) and metabolites. Other antiviral effectors of the constitutive response function through the degradation of virus particles; these include nucleases such as TREX1, which degrades viral DNA in the cytoplasm, and RNase L, which degrades viral RNA, as well as autophagy and proteasomal degradation. Viruses can be targeted for proteasomal degradation by the ubiquitin E3 ligase TRIM21, which binds to antibody-attached viral capsids. b | Constitutive innate immune mechanisms and bacterial infection. The presence of bacteria changes the local microenvironment, for example through the accumulation of hydrophobic and charged bacterial surfaces or alteration of cellular metabolism. This activates antibacterial activities independently of pattern recognition receptors, including inactivation by soluble lectins and antimicrobial peptides, nutritional depletion by natural resistance-associated macrophage protein 1 (NRAMP1) and lactoferrin, and bacterial degradation by phagocytosis and basal autophagy. dsDNA, double-stranded DNA; RISC, RNA-induced silencing complex; ROS, reactive oxygen species; viRNA, virus-derived small interfering RNA.
Table 1.
Constitutive immune mechanisms in host defence
| Type of effector | Examples | Trigger | Target microorganisms | Evidence for control of inflammatory responses | Refs |
|---|---|---|---|---|---|
| Targeting microbial replication | |||||
| Restriction factors | BST2, YBX1, IFITMs | Specific viral replication events | HIV-1, HCV, HSV-1, VSV, RSV | Increased IL-6 and IL-1β expression in the lungs of RSV-infected Ifitm1–/– mice; increased constitutive infiltration of monocytes and macrophages in the kidney in Ybx1–/– mice | 40,44,154–156 |
| SAMHD1, APOBEC3 | Modulation of nucleic acid availability and/or function | HIV-1, vaccinia virus, HSV-1, murine herpesvirus 68, parvovirus | Increased spontaneous and lentivirus-induced interferon and ISG expression in Samhd1–/– mice; increased IFNβ expression in Apobec3–/– mice infected with murine leukaemia virus | 39,41,120,121,157,158 | |
| RNAi | RISC | dsRNA | Cucumovirus (plants), Flock House virus (worms), cricket paralysis virus (flies) | Introduction of Drosophila Dicer-2 in mammalian cells reduced dsRNA-induced IFNβ expression | 50–52,159 |
| Antimicrobial peptides | β-Defensins, cathelicidin | Negatively charged surfaces | Salmonella enterica subsp. enterica serovar Typhimurium, Escherichia coli, Shigella spp., HIV-1 | LL37 inhibits DNA-sensing inflammasomes in psoriatic skin; an engineered antimicrobial peptide inhibits TLR4 signalling through the TRIF pathway | 58–60,65,129,160 |
| Soluble lectins | Collectins, ficolins, galectins, pentraxins | Glycans | HIV-1, influenza A virus, Streptococcus pneumoniae | SP-A inhibits LPS-induced TLR4 activation by preventing the interaction with LPS-binding protein; SP-D-deficient mice have increased levels of proinflammatory cytokines after influenza virus infection | 68–72,161 |
| Metabolites | Lactate, palmitic acid | Metabolic alterations | HIV-1, HSV-1, Zika virus, VSV | Ldha–/– mice express increased levels of type I interferon on infection with RNA viruses | 73,74,77,162,163 |
| NRAMP1, lactoferrin | Iron depletion | Mycobacterium tuberculosis, S. Typhimurium, Leishmania donovani, Streptococcus mutans | Lactoferrin binds CpG DNA and impedes stimulation through TLR9 | 80,81,84,123 | |
| Degenerative mechanisms | |||||
| Autophagy | – | Viral proteins, organelle dysfunction, protein aggregates | M. tuberculosis, S. Typhimurium, Sindbis virus | Increased interferon expression and inflammasome activation in autophagy-defective cells; excess IL-1β production and lung inflammation in autophagy-deficient mice after infection and sterile challenge | 9,89,96,126,164 |
| Phagocytosis | – | Opsonization | Staphylococcus aureus, Salmonella spp., Mycobacteria spp., Aspergillus spp. | Patients with CGD have increased inflammasome activity and IL-1β production | 165,166 |
| LC3-associated phagocytosis | – | Not known | S. Typhimurium, Listeria monocytogenes, Burkholderia pseudomallei | LC3-deficient mice fail to clear dead cells and develop lupus-like inflammatory disease | 102,123,167,168 |
| Proteasomal degradation | – | Cytosolic capsids and capsid–IgG complexes | Adenovirus, turnip yellow mosaic virus | Patients with PRAAS-associated mutations in proteasome genes have strong interferon signatures | 105–107,111,148,149 |
| Nucleic acid degradation | – | Cytosolic RNA and DNA | Endogenous retroviruses, murine coronaviruses | Patients with defective TREX1 have increased interferon expression and develop Aicardi–Goutières syndrome | 117,118,137 |
APOBEC3, apolipoprotein B mRNA-editing complex 3; BST2, bone marrow stromal antigen 2 (also known as tetherin); CGD, chronic granulomatous disease; dsRNA, double-stranded RNA; HCV, hepatitis C virus; HSV-1, herpes simplex virus type 1; IFITMs, interferon-induced transmembrane proteins; ISG, interferon-stimulated gene; Ldha, lactate dehydrogenase A; LPS, lipopolysaccharide; NRAMP1, natural resistance-associated macrophage protein 1; PRAAS, proteasome-associated autoinflammatory syndromes; RISC, RNA-induced silencing complex; RNAi, RNA interference; RSV, respiratory syncytial virus; SAMHD1, SAM domain and HD domain-containing protein 1; SP, surfactant protein; TLR, Toll-like receptor; VSV, vesicular stomatitis virus; YBX1, Y-box binding protein 1.
Given the ability of constitutive immune mechanisms to exert antimicrobial activity, one consequence of their successful action is decreased levels of PAMPs (Fig. 2a). This, in turn, limits PRR activation and the downstream inflammatory response (Fig. 2b). Thus, constitutive immune mechanisms equip cells and tissues with a layer of defence that can fight infections immediately and hence potentially limit the requirement for inducible immune responses, such as type I interferon, IL-1β and other proinflammatory cytokines.
Box 2 Overlap between constitutive and inducible immune responses.
In most respects, constitutive and inducible immune responses operate through different principles; however, in certain cases, their downstream effector activities may overlap. This is to be expected given that all of these responses use mechanisms from the same ‘evolutionary toolbox’ to achieve optimal protection of the host. For example, autophagy can be activated during infection and upon sterile danger9,174. Similarly, phagocytosis can be activated by both Toll-like receptor (TLR)-dependent and TLR-independent mechanisms175–177. Moreover, many restriction factors are expressed at basal levels to exert immediate antiviral activity, but are also induced transcriptionally in response to stimulation with type I interferon35,40,178. Nevertheless, despite these minor areas of overlap between constitutive immune mechanisms and the pattern recognition receptor (PRR)-induced immune responses, the differences are more pronounced. The key difference between constitutive immune mechanisms and PRR-induced immunity is that the former mechanisms are all activated through pre-existing molecules to directly eliminate danger, whereas the latter system functions mainly through inducible transcription-dependent proinflammatory programmes. In addition, inducible innate responses can amplify adaptive responses, whereas constitutive innate responses do not amplify inducible innate responses.
Targeting microbial replication
Direct inhibition of microbial replication is executed by molecules that interfere with specific steps in the replication cycle of a given microorganism. There are at least six mechanisms of action in this category: restriction factors that directly block a specific replication step; restriction factors that deplete molecules essential for replication; RNA interference (RNAi); antimicrobial peptides; soluble lectins; and metabolite-mediated inhibition of microbial replication (Table 1).
Restrictions factors
Restriction factors are antiviral proteins that target viral replication. Extensive studies, particularly of HIV-1 and herpesviruses37,38, have led to the identification of numerous restriction factors that together target nearly all steps in the viral replication cycle (Fig. 4a). For example, APOBEC3 proteins belong to the family of cytidine deaminases, which catalyse the deamination of cytidine to uridine in single-stranded DNA, thus introducing potentially deleterious mutations into the HIV-1 genome39. Likewise, tetherin is a membrane-bound protein that prevents the release of progeny HIV-1 particles from the cell surface40. These two mechanisms provide examples of direct blockade of specific steps in the replication cycle. By contrast, SAM domain and HD domain-containing protein 1 (SAMHD1) blocks HIV-1 replication indirectly, by converting deoxynucleoside triphosphates into inorganic phosphate and 2′-deoxynucleoside, thus depleting essential building blocks for HIV-1 reverse transcription34,41. The aforementioned restriction factors work in the plasma membrane or in the cytoplasm. However, many DNA viruses, including herpesviruses, replicate in the nucleus, where they are also targeted by numerous restriction factors. These include nuclear domain 10 bodies (ND10 bodies) and IFNγ-inducible protein 16 (IFI16), which operate by different mechanisms to epigenetically silence viral genomes35,42. The herpesvirus DNA rapidly associates with ND10 bodies, which restrict viral gene expression by promoting processes that lead to the formation of nucleosome-like structures42. IFI16 restricts viral replication in the nucleus mainly by interfering directly with transcription35. New evidence suggests that this involves the ability of IFI16 to form DNA filaments, which reduces recruitment of RNA polymerase II (ref.43), but also leads to recruitment of ND10 bodies, thus indicating that these two restriction systems might interact. The restriction factors discussed here are all constitutively expressed, although the expression of many of them is further increased by interferons35,44,45. Tonic type I interferon signalling or constitutive activity of interferon regulatory factor 1 (IRF1) drives the basal expression of many constitutive restriction factors8,46,47.
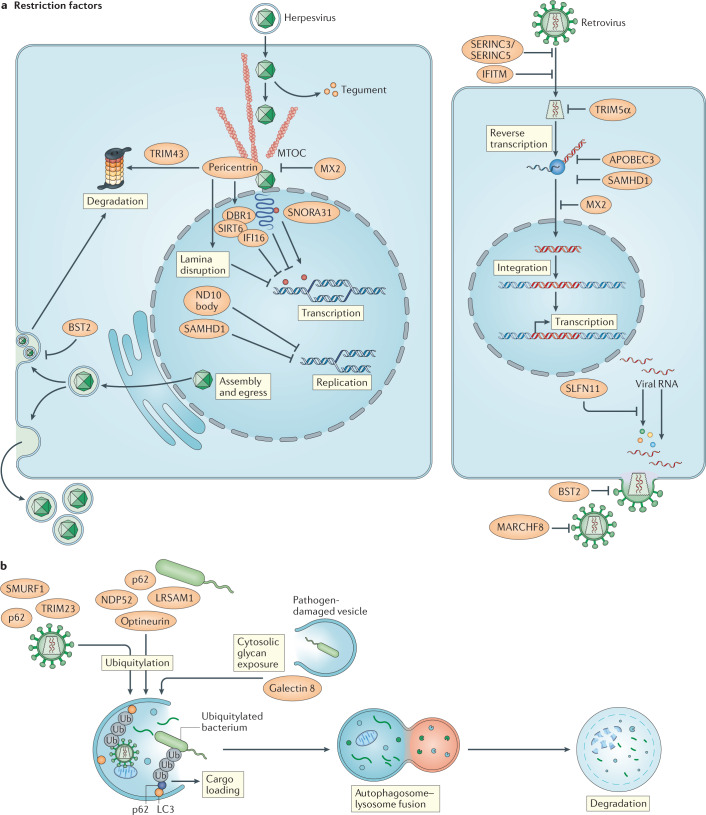
Fig. 4. Constitutive control of microbial replication by restriction factors and autophagy.
a | Restriction factors that control herpesvirus and retrovirus infections, including their targets in the viral replication cycle. Restriction factors interfere with viral replication by either blocking a specific and essential step in the viral replication cycle (for example, viral gene transcription or release of progeny virus) or depletion of factors that are essential for replication (such as deoxynucleoside triphosphates). b | Blockade of viral and bacterial replication by autophagy. Various ubiquitin E3 ligases (such as SMURF1, LRSAM1 and TRIM23) and ubiquitin-binding proteins (such as p62, optineurin and NDP52) have been identified to conjugate ubiquitin to microbial surfaces, which targets them for loading into autophagosomes. Also, cytosolic exposure of glycans by pathogen-damaged vesicles can be recognized by galectin 8 for targeting to autophagosomes. APOBEC3, apolipoprotein B mRNA-editing complex 3; BST2, bone marrow stromal antigen 2 (also known as tetherin); DBR1, RNA lariat debranching enzyme 1; IFI16, interferon-γ-inducible protein 16; IFITM, interferon-induced transmembrane protein; MTOC, microtubule-organizing centre; ND10, nuclear domain 10; SAMHD1, SAM domain and HD domain-containing protein 1; SIRT6, sirtuin 6; SNORA31, small nucleolar RNA, H/ACA box 31.
RNA interference
RNAi is another constitutive immune mechanism that directly controls viral replication. RNAi involves the processing of double-stranded RNA molecules by members of the Dicer nuclease family to 20–25-bp fragments, thus leading to the formation of the RNA-induced silencing complex (RISC), which blocks gene expression or translation through binding to target mRNAs48. The ability of RNAi to directly block viral replication was first shown in plants49 and was later also shown in insects and worms50–52. For example, Caenorhabditis elegans and Drosophila melanogaster infected with Flock House virus activate antiviral defence mechanisms that depend on Dicer51,53. This constitutive immune mechanism might have a more important role in lower organisms, but as some mammalian viruses do target the RNAi system, there may be a subdominant role for this primordial antiviral system in host defence in more evolved organisms54. For example, Ebola virus VP35 and VP30 proteins interact with Dicer cofactors, and the hepatitis C virus core protein directly associates with Dicer55,56.
Antimicrobial peptides
Antimicrobial peptides, including defensins and cathelicidins, contribute to the first line of defence against bacteria in the skin and at mucosal surfaces. They work by binding directly to bacterial membranes, thus perturbing membrane integrity and inhibiting microbial growth57–60. These peptides are rich in both cationic and hydrophobic amino acids, and generally form amphiphilic helical structures, although this may not be the case for all antimicrobial peptides61. This enables the peptides to interact with negatively charged bacterial surfaces through electrostatic interactions, thus triggering disruption of the bacterial membranes by pore-forming or non-pore-forming mechanisms62. Many antimicrobial peptides, such as β-defensin 1, are constitutively expressed on epithelial surfaces, thus providing immediate antimicrobial action on infection63. This is illustrated by the increased susceptibility to a broad range of bacterial infections in mice lacking cathelicidin antimicrobial peptide (CAMP)59,64. Beyond their role in antibacterial defence, there is also evidence that antimicrobial peptides can disrupt viral particles, thus exerting antiviral activity65,66. Similarly to the restriction factors, many antimicrobial peptides are expressed in both constitutive and inducible manners. This illustrates the general principle that different branches of the immune system can use overlapping effector functions (Box 2).
Soluble lectins
Many microorganisms have extensive and more complex glycan patterns than mammalian cells, and these sugars can therefore be used as a means to distinguish self from non-self. There are four classes of soluble lectins carrying out this function, namely collectins, ficolins, galectins and pentraxins67. On recognition of non-self glycans, soluble lectins can exert host defence activities indirectly through complement activation and opsonization, as discussed later, or directly through aggregation and neutralization. For example, the collectin surfactant protein D (SP-D) has been reported to bind directly to highly glycosylated viruses such as HIV-1 and influenza A virus and neutralize their infectivity68,69. Similarly, pentraxin 3 directly binds influenza A virus particles and neutralizes virus infectivity70. Importantly, SP-D-deficient mice have impaired clearance of influenza A virus and increased production of proinflammatory cytokines in response to viral challenge71. In addition to viruses, SP-D also binds and agglutinates Streptococcus pneumoniae72, thus suggesting that soluble lectins might also have a role in the immediate inactivation of bacteria.
Metabolite-mediated inhibition
A final example of constitutive immune mechanisms that directly interfere with microbial growth is provided by metabolites that block pathogen replication, and perhaps the best example of which is lactate73,74. Many viral infections are characterized by a shift of host cellular metabolism to aerobic glycolysis, which leads to the production of lactate75,76. Viral infections also induce fatty acid synthesis and intermediate molecules in these pathways. These include palmitic acid and oleic acid, which have been shown to have antiviral activity77,78. The mechanisms by which lactate and other metabolites block viral replication remain to be determined, but the antiviral activity of lactate illustrates a general principle that select molecules accumulating during alterations of cellular homeostasis can interfere with microbial replication.
A second form of metabolite-dependent constitutive host defence is mediated through nutritional depletion and starvation of pathogens. For example, natural resistance-associated macrophage protein 1 (NRAMP1; also known as SLC11A1) is a metal ion transporter that transports divalent cations from vacuoles into the cytoplasm, hence depleting factors from vacuoles that are essential for the growth of intracellular pathogens79. The gene encoding NRAMP1 was shown to contribute to defence against, for example, Mycobacterium tuberculosis, Salmonella enterica subsp. enterica serovar Typhimurium and Leishmania donovani80,81, which was later shown to be mediated by the reduction of metal ion concentrations inside microorganism-containing vacuoles82. A second example of nutritional depletion is provided by lactoferrin, which is present in various secretory fluids. Lactoferrin is a highly cationic molecule that shows antimicrobial activity, in part, by binding and sequestering iron from pathogenic microorganisms83. Lactoferrin contributes to host defence in a non-redundant manner, as lactoferrin-deficient mice have increased susceptibility to Streptococcus mutans-induced dental caries, for example84.
Degenerative mechanisms
The second class of constitutive innate immune mechanisms functions through the degradation of danger molecules and elimination of unwanted cells. This class of mechanisms includes autophagy, phagocytosis, proteasomal degradation and nucleases (Table 1). Collectively, degenerative programmes function to continually limit danger signals, allowing for the rapid elimination of unwanted molecules without the activation of energy-consuming amplificative induced immune responses.
Autophagy and phagocytosis
Autophagy and phagocytosis execute the digestion of intracellular and extracellular microorganisms, respectively, through membrane encapsulation followed by chemical and enzymatic degradation85,86. Pathogens are shunted into these pathways through the recognition of polyubiquitin chains or glycans inside damaged vacuoles in the case of autophagy9,87, and through complement coating of microorganisms in the case of phagocytosis88. In the case of autophagy, a large number of ubiquitin E3 ligases have been identified that coat viral and bacterial surfaces with ubiquitin9,89–92, thus targeting microorganisms for loading into autophagosomes through interaction with the autophagosome-associated protein LC3 (also known as MAP1ALC3)85 (Fig. 4b). This targeting mechanism involves E3 ligases, including SMURF1 and LRSAM1 (refs91,92), as well as the ubiquitin-binding selective autophagy receptors p62 (also known as SQSTM1), optineurin and NDP52 (also known as CALCOCO2)9,89,93. An alternative mechanism for sensing of vesicle-damaging pathogens has been identified that involves damaged vesicles exposing glycans in the cytoplasm for sensing by galactin 8, which links to autophagy via NDP52 (ref.87). This triggers phagophore formation in the vicinity of cytosolic bacteria94. Autophagy has important roles in the control of infection. For example, defective autophagy leads to increased susceptibility to infection with Sindbis virus in mice89. In addition, stimulation of autophagy in primary human macrophages mediated protection against M. tuberculosis infection95,96. However, mice defective in autophagy do not have impaired antimycobacterial defence in vivo, which indicates that the precise role of autophagy requires further investigation97. Third, herpes simplex virus type 1 specifically interferes with autophagy, which is essential for neuropathogenicity of the virus36.
Complement-mediated phagocytosis involves specific recognition of complement components bound to the surface of microorganisms by the corresponding complement receptors on phagocytes. Activation of the complement system, for example after sensing of glycans by the lectin pathway, leads to the formation of C3 convertase, eventually generating C3b, which binds to complement receptors, thus inducing phagocytosis98. Mice devoid of the lectin-based complement pathway have increased susceptibility to Staphylococcus aureus infection and impaired bacterial phagocytosis99. Furthermore, several bacteria, including Streptococcus pyogenes, inhibit complement-mediated phagocytosis100.
A third degenerative mechanism for the degradation of membrane-encapsulated extracellular material is LC3-associated phagocytosis (LAP), which uses components from both the phagocytosis and autophagy pathways101. LAP is involved in the clearance of extracellular pathogens and dead cells102, and LAP-deficient mice fail to clear Aspergillus fumigatus infection103. Thus, autophagy, phagocytosis and LAP are important systems for immediate host defence.
Proteasomal degradation
The proteasome is a cytoplasmic protein complex that degrades proteins by proteolysis104. Proteins to be degraded are tagged by K48-linked polyubiquitylation, attracted to the proteasome, unfolded into polypeptides and then degraded104. The proteasomal degradation pathway also contributes to immediate defence against infecting pathogens. For example, viruses can be detected by the ubiquitin E3 ligase TRIM21 through binding to antibody-bound viral capsids, which links to downstream proteasomal degradation105. This process is involved in the elimination of infecting viral capsids from the cytoplasm and contributes to antiviral defence105–107. Other studies have shown that the viral RNA-dependent RNA polymerase of turnip yellow mosaic virus is degraded by the ubiquitin–proteasome pathway to control infection108. Proteasome activity also contributes to defence against many bacterial infections, including Yersinia spp. infections109, and the ubiquitin–proteasome pathway is targeted by many viruses and bacteria to promote replication110–114. For example, the human cytomegalovirus protein pUL25 inhibits proteasomal degradation of another viral protein, pUL26, to sustain the activity of a pUL26-mediated immune evasion mechanism114. Collectively, these examples show that the conserved proteasome pathway is part of the constitutive immune defence repertoire.
Nucleases
The cytoplasm contains RNAses and DNAses that eliminate unwanted nucleic acid species, including viral nucleic acids, and these enzymes can thereby contribute to sterilization of the cytoplasm. RNase L is a latent cytoplasmic exoribonuclease that is activated by 2′-5′ oligoadenylates produced by OASs115. Although OASs are highly interferon inducible, they are also expressed at a basal level and hence induce basal RNase L activity116. Importantly, this activity has been suggested to contribute to basal restriction of coronaviruses in myeloid cells, and hence to protect other cell types from infection117. TREX1 is a cytoplasmic exodeoxyribonuclease that eliminates DNA from the cytoplasm. Very few microorganisms have free DNA as part of their productive replication cycle, but exogenous and endogenous retroviruses have a cytoplasmic DNA step that is sensitive to degradation by TREX1. Consequently, Trex1–/– mice have increased levels of endogenous retroviral DNA in the cytoplasm118, which indicates that TREX1 has a role in limiting retroviral infection and hence maintaining genome integrity.
Limiting inflammatory responses
Immune responses induced by PRRs and by antigen-specific receptors are often highly potent and sterilizing. However, they may also be relatively disruptive and can be associated with tissue damage and the requirement for significant tissue repair and energy consumption119. Many of the constitutive immune mechanisms discussed here not only interfere with microbial replication but also have negative effects on PRR activity (Table 1). This raises the possibility that an overarching function of the constitutive immune mechanisms is to both eliminate danger and limit the use of PRR-driven activities. At the mechanistic level, this immunoregulatory function of the constitutive mechanisms can be exerted in two qualitatively different ways. The first is through the direct effect of their antimicrobial activity on decreasing levels of PAMPs. The second is through specific inhibition of PRR signalling.
Reduction of PAMP levels
Many studies have shown that PRR activation requires PAMP levels to be above a certain threshold25–28. Above this threshold, PRRs are activated in a concentration-dependent manner until saturation is reached. Therefore, constitutive immune mechanisms that reduce PAMP levels will limit or even prevent PRR activation (Fig. 2a). For example, mice deficient in the restriction factor APOBEC3, which has antiretroviral activity, have higher viral loads after infection with murine leukaemia virus and corresponding higher levels of reverse viral transcripts and downstream interferon induction through the cGAS–STING pathway (cyclic GMP–AMP synthase–stimulator of interferon genes pathway)120. Similarly, SAMHD1 activity in vivo controls lentivirus load and limits virus-induced production of interferons in myeloid cells121. In addition, SAMHD1 deficiency leads to increased expression of costimulatory molecules and T cell activation on lentiviral infection, which suggests that the constitutive reduction of PRR activation by SAMHD1 limits not only the expression of innate immune cytokines but also downstream adaptive immune responses121. A third example is provided by the observation that expression of Drosophila Dicer in mammalian cells leads to decreased induction of IFNβ by double-stranded RNA, most likely owing to the digestion of immunostimulatory RNA into shorter 20–25-bp RNA species that activate PRRs only inefficiently122. Finally, constitutive innate immune mechanisms can also reduce PRR activity by lowering the concentration of PAMPs that have immunostimulatory activity. For example, lactoferrin binds CpG DNAs and inhibits their ability to activate TLR9 (ref.123).
Inhibition of PRR signalling
In addition to reducing the levels of PAMPs, some constitutive mechanisms have been reported to target PRR activity at the signalling level (Fig. 2a). For example, autophagy negatively regulates signalling by the RIG-I–MAVS pathway (retinoic acid-inducible gene I protein–mitochondrial antiviral signalling protein pathway) and by the cGAS–STING pathway; in the former case by limiting reactive oxygen species-mediated amplification of signalling and by LC3-dependent MAVS inactivation124,125, and in the latter case through degradation of STING126. In line with this, defective autophagy as a result of ATG16L deficiency predisposes to STING-dependent intestinal pathology in mice127, and ATG5 deficiency selectively in neutrophils exacerbates M. tuberculosis immunopathology without affecting bacterial load97. As a second example, lactate, which is produced during aerobic glycolysis and has virus-restricting activity73,74, also directly inhibits MAVS activity; thus lactate both reduces levels of viral PAMPs and has a negative regulatory function to inhibit PAMP-driven signalling and interferon expression128. Third, an engineered amphipathic-helical antimicrobial peptide was found to block TLR4 signalling through the TRIF pathway129. This occurs by the inhibition of TLR4 endocytosis, which is an essential step for the engagement of TRIF from endosomal compartments.
Collectively, the current literature suggests that constitutive immune mechanisms reduce PRR activation through a range of mechanisms and, therefore, that these constitutive mechanisms impose a threshold and negative regulatory activity on the amplificative innate and adaptive immune responses (Fig. 2b). We propose that rapid, molecularly specific and non-amplificative responses to challenges provided by constitutive immune mechanisms are beneficial for achieving optimal host defence with minimal immunopathology.
Constitutive immunity beyond infection
Our main focus here has been on infections. However, constitutive immune mechanisms are also involved in the elimination of sterile danger. For example, DNA damage in the nucleus and the accumulation of DNA in extranuclear compartments are eliminated by the DNA damage response and specific DNases130, respectively; the accumulation of misfolded proteins leads to the formation of aggresomes, which are cleared by selective autophagy131,132; excessive accumulation of reactive oxygen species leads to death of the oxygen-stressed cells133; and free cholesterol is converted into an ester derivative by lecithin–cholesterol acyltransferase, thus enabling transport to the liver by high-density lipoprotein and eventual degradation134. Defects in these constitutive and latent danger-eliminating mechanisms lead to the accumulation of danger-associated molecular patterns and activation of PRR-based immunity. For example, in cells with defects in either the DNA damage response or extranuclear DNases, the accumulation of DNA induces type I interferon production through the cGAS–STING pathway135–138. Similarly, defective elimination of protein aggregates or cholesterol leads to the induction of IL-1β production through activation of the NLRP3 inflammasome139,140. Common to all of the examples given above is that the accumulated abnormal endogenous molecules are detected and eliminated through molecularly specific mechanisms independently of PRRs. This elimination limits PRR activation and hence inflammatory reactions. Therefore, in addition to eliminating microorganisms and PAMPs, constitutive immune mechanisms also eliminate sterile danger signals in a damage-limiting manner that prevents the activation of excessive inflammation.
Constitutive immunity in human health
We propose that constitutive immune mechanisms enable cells and organisms to fight infections and eliminate endogenous abnormalities in a non-inflammatory manner. Therefore, an important benefit of these mechanisms may be to increase the threshold for development of clinically overt signs of disease on exposure to infections or endogenous danger. Studies of the associations between single-nucleotide polymorphisms and infections have shown that restriction factors, antimicrobial peptides and autophagy have important roles in antimicrobial defence141–144. Constitutive immune mechanisms may be particularly active in the protection of tissues that are frequently exposed to pathogens, such as epithelial cells in the airways and the gut, or tissues that are particularly vulnerable to immunopathology, such as the brain. In favour of this idea, RNA lariat debranching enzyme 1 (DBR1) and small nucleolar RNA, H/ACA box 31 (SNORA31) were recently shown to have non-redundant, interferon-independent roles in the prevention of viral brainstem encephalitis and herpes simplex encephalitis, respectively11,12. The mechanisms through which they exert their antiviral activity remain to be determined. Reports have shown that autophagy is an antiviral mechanism in the brain in mice36,89,145. In addition, some cell populations, including stem cells, seem to use constitutive immune mechanisms to eliminate danger without losing key functions, such as self-renewal and differentiation capacity, that are known to be impaired by PRR-based immunity146,147.
An important question related to human immunology is how individuals with a loss-of-function mutation in a constitutive immune mechanism may present clinically. Deficiency of a mechanism that is expressed in specific organs or cell types might lead to a higher frequency of clinical infections by a subset of microorganisms that are normally controlled by the defective mechanism. This seems to be the case for defects in DBR1, which confer susceptibility to disease caused by infections with herpes simplex virus type 1, influenza virus or norovirus in the brainstem11. The impact of deficiencies in constitutive immune mechanisms might not be limited to acute infections and could also include chronic and latent infections. In support of a link between such defects and increased inflammation, patients with inborn defects in DNA repair, elimination of extranuclear DNA or degradation of misfolded proteins develop autoinflammatory diseases, including Aicardi–Goutières syndrome and proteasome-associated autoinflammatory syndromes, which are characterized by type I interferon-dependent autoinflammation and are termed ‘interferonopathies’137,148–150. Therefore, a loss of function in constitutive immune mechanisms can lead to selective susceptibility to specific infections or to infections in specific organs. Likewise, such deficiency might lead to the accumulation of PAMPs, microorganism-associated molecular patterns, danger-associated molecular patterns and/or homeostasis-altering molecular processes and associated pathological inflammation (Box 1).
Outlook
In this article, we have described the role and mode of action of a large panel of constitutive mechanisms used by the immune system to exert immediate control of infections and endogenous dangers independently of the inducible mechanisms that are activated through PRRs and antigen-specific receptors. Although many such constitutive responses have been known for years, greater understanding of the mechanisms involved and renewed interest in fields such as restriction factor biology and immunometabolism are spurring further work in the area. With the identification of constitutive mechanisms that have non-redundant roles in host defence, we now know that these immune mechanisms are not just redundant, non-specific players in immunology11,12. This should stimulate interest in understanding the roles played by constitutive immune mechanisms in host defence in vivo, which might include the identification of new primary immune disorders. Improved knowledge of the host cell type and tissue specificities of constitutive immune mechanisms in relation to susceptibility to infections could greatly improve our understanding of human immunology. Such work will start to provide answers to the fundamental question of how the immune system determines the degree of threat caused by an infection and balances that with the appropriate strength of the immune reaction.
Finally, as we gain further insights into the various host responses that are activated during immunological challenge, it will be interesting to explore the idea that the immune system has a defensive layer of activities that have been selected to eliminate danger without engaging the PRR system (Box 3). In this respect, it is interesting to note that in addition to the constitutive mechanisms described in this Review, there are various sensing systems that use transcriptional programmes to induce host defence independently of PRRs and with the ability to control inflammation. They include the NRF2–KEAP1, hypoxia-inducible factor 1α and bone morphogenetic protein–SMAD pathways10,151–153. In addition, the constitutive host defence exerted by commensal bacteria through several mechanisms, including niche competition, warrants more attention. With more and more data emerging on the importance of constitutive mechanisms in immunology, there is a need to understand this phenomenon in more detail. Such work may advance our understanding of one of the most interesting questions in immunology, namely how to eliminate danger in a rapid, efficient and specific manner without causing excess damage to the host.
Box 3 A new concept of damage-limiting immune mechanisms?
In addition to the constitutive immune mechanisms described in this Review, several pathways are activated in response to infections and sterile challenge that function independently of pattern recognition receptors (PRRs) and antigen-specific receptors to control infection. These include the NRF2–KEAP1, hypoxia-inducible factor 1α and bone morphogenetic protein–SMAD pathways10,151–153. These pathways differ from the constitutive immune mechanisms by engaging transcriptional programmes to execute their activities10,151–153. Some of these pathways have also been reported to exert negative control of PRR signalling151,152,179,180, which shows that they share both antimicrobial and immunoregulatory functions with the constitutive immune mechanisms. For example, NRF2-deficient mice have increased susceptibility to certain viral infections152, and NRF2 also negatively regulates cyclic GMP–AMP synthase (cGAS)–stimulator of interferon gene (STING) signalling180. As we gain more information about the actions of constitutive immune mechanisms and PRR-independent transcriptional pathways in early host defence, we believe that the immunological community should consider whether these diverse mechanisms share features that distinguish them from other immune pathways. It is possible that the constitutive immune mechanisms described in this Review are part of a larger group of damage-limiting immune mechanisms that can be defined by fulfilling all of the following criteria:
Function independently of PRRs and antigen-specific receptors
Respond to the presence of specific microbial or host stress-related molecules
Eliminate danger in a non-inflammatory manner, and limit PRR activation by removing PRR ligands and/or inhibiting PRR signalling
Eliminate danger through specific effector functions that target defined host or microbial structures and activities
Whereas the physical and chemical barrier functions of the immune system fulfil criteria 1 and 3, they do not satisfy criteria 2 and 4. Similarly, PRRs and antigen-specific receptors fulfil criteria 2 and 4, but do not fulfil criteria 1 and 3. Although it is speculative at present, we think that the idea of damage-limiting immune mechanisms may serve as a useful guide for future experimental and clinical research.
Acknowledgements
S.R.P. is funded by the European Research Council (ERC-AdG ENVISION; 786602), the Novo Nordisk Foundation (NNF18OC0030274) and the Lundbeck Foundation (R198-2015-171 and R268-2016-3927). T.P. is funded by the European Research Council (ERC-StG IDEM; 637647). S.L.M. acknowledges funding from a Howard Hughes Medical Institute–Wellcome International Research Scholarship and the Sylvia and Charles Viertel Foundation. T.H.M. received funding from Aarhus University Research Foundation (AUFF-E-215-FLS-8-66), the Danish Council for Independent Research-Medical Sciences (4004-00047B) and the Lundbeck Foundation (R268-2016-3927). The authors thank D. Olagnier for critical reading of the manuscript and comments and suggestions.
Glossary
- Pattern recognition receptors
(PRRs). A family of germline-encoded immune receptors, including the Toll-like receptors, that detect immunostimulatory molecules to activate signal transduction and gene expression, which induces antimicrobial and inflammatory responses.
- Constitutive immune mechanisms
Host mechanisms that are constitutively present in an active or latent form and thus can exert host defence activities immediately, independently of inducible processes.
- Inducible mechanisms
Biological processes that depend on the activation of transcriptional programmes and hence require intermediate steps between the trigger stimulus and effector function.
- Supramolecular organizing centres
Location-specific higher-order signalling complexes, such as the myddosome in Toll-like receptor signalling, that amplify pattern recognition receptor signalling when pathogen-associated molecular pattern levels exceed specific threshold concentrations.
- RNA interference
(RNAi). The use of double-stranded RNA molecules containing sequences that match a given gene to knock down the expression of that gene by inhibiting translation of the targeted mRNA or by directing RNA-degrading enzymes to destroy the encoded mRNA transcript.
- Nuclear domain 10 bodies
(ND10 bodies). Membraneless, interchromatin structures in the nucleus of eukaryotic cells. ND10 bodies are made up mainly of proteins and have been described to be involved in a broad range of processes, including gene regulation, cell cycle, apoptosis, DNA repair and antiviral defence.
- Aerobic glycolysis
The process by which glucose is converted to lactate in the presence of oxygen to produce energy in the form of ATP.
- cGAS–STING pathway
(Cyclic GMP–AMP synthase–stimulator of interferon genes pathway). cGAS is a cytosolic DNA-sensing pattern recognition receptor that signals via STING to induce the expression of type I interferon and inflammatory cytokines.
- RIG-I–MAVS pathway
(Retinoic acid-inducible gene I protein–mitochondrial antiviral signalling protein pathway). RIG-I is a cytosolic RNA-sensing pattern recognition receptor that signals via MAVS to induce the expression of type I interferon and inflammatory cytokines.
- DNA damage response
Cellular response to DNA damage, including the re-establishment of genome integrity and cell death responses.
- NLRP3 inflammasome
The NLRP3 inflammasome is activated by danger-associated molecular patterns and molecular signatures associated with homeostasis-altering molecular processes to execute caspase 1-mediated cleavage of molecules such as pro-IL-1β and gasdermin D.
- NRF2–KEAP1
Nuclear factor erythroid 2-related factor 2 (NRF2) senses oxidative stress, whereupon it is released from Kelch-like ECH-associated protein 1 (KEAP1) to translocate to the nucleus and induce gene expression.
- Hypoxia-inducible factor 1α
A transcription factor that is activated by hypoxia to induce the expression of genes with hypoxia-responsive elements in their promoters.
- Bone morphogenetic protein–SMAD
Bone morphogenetic proteins are growth factors that signal through SMAD proteins to induce gene transcription.
Author contributions
S.R.P. conceived the idea and wrote the first version of the manuscript together with T.H.M. All authors together fully developed the work, and drafted, finalized and revised the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information
Nature Reviews Immunology thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- 2.van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat. Rev. Immunol. 2017;17:407–420. doi: 10.1038/nri.2017.36. [DOI] [PubMed] [Google Scholar]
- 3.Coban C, Lee MSJ, Ishii KJ. Tissue-specific immunopathology during malaria infection. Nat. Rev. Immunol. 2018;18:266–278. doi: 10.1038/nri.2017.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 5.Iwasaki A, Medzhitov R. Control of adaptive immunity by the innate immune system. Nat. Immunol. 2015;16:343–353. doi: 10.1038/ni.3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flajnik MF, Kasahara M. Origin and evolution of the adaptive immune system: genetic events and selective pressures. Nat. Rev. Genet. 2010;11:47–59. doi: 10.1038/nrg2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iversen MB, et al. An innate antiviral pathway acting before interferons at epithelial surfaces. Nat. Immunol. 2016;17:150–158. doi: 10.1038/ni.3319. [DOI] [PubMed] [Google Scholar]
- 8.Yamane D, et al. Basal expression of interferon regulatory factor 1 drives intrinsic hepatocyte resistance to multiple RNA viruses. Nat. Microbiol. 2019;4:1096–1104. doi: 10.1038/s41564-019-0425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thurston TL, Ryzhakov G, Bloor S, von Muhlinen N, Randow F. The TBK1 adaptor and autophagy receptor NDP52 restricts the proliferation of ubiquitin-coated bacteria. Nat. Immunol. 2009;10:1215–1221. doi: 10.1038/ni.1800. [DOI] [PubMed] [Google Scholar]
- 10.Eddowes LA, et al. Antiviral activity of bone morphogenetic proteins and activins. Nat. Microbiol. 2019;4:339–351. doi: 10.1038/s41564-018-0301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang SY, et al. Inborn errors of RNA lariat metabolism in humans with brainstem viral infection. Cell. 2018;172:952–965. doi: 10.1016/j.cell.2018.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lafaille FG, et al. Human SNORA31 variations impair cortical neuron-intrinsic immunity to HSV-1 and underlie herpes simplex encephalitis. Nat. Med. 2019;25:1873–1884. doi: 10.1038/s41591-019-0672-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nish S, Medzhitov R. Host defense pathways: role of redundancy and compensation in infectious disease phenotypes. Immunity. 2011;34:629–636. doi: 10.1016/j.immuni.2011.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ausubel FM. Are innate immune signaling pathways in plants and animals conserved? Nat. Immunol. 2005;6:973–979. doi: 10.1038/ni1253. [DOI] [PubMed] [Google Scholar]
- 15.Matzinger P. Tolerance, danger, and the extended family. Annu. Rev. Immunol. 1994;12:991–1045. doi: 10.1146/annurev.iy.12.040194.005015. [DOI] [PubMed] [Google Scholar]
- 16.Liston A, Masters SL. Homeostasis-altering molecular processes as mechanisms of inflammasome activation. Nat. Rev. Immunol. 2017;17:208–214. doi: 10.1038/nri.2016.151. [DOI] [PubMed] [Google Scholar]
- 17.Lemaitre B, Nicolas E, Michaut L, Reichhart JM, Hoffmann JA. The dorsoventral regulatory gene cassette spätzle/Toll/cactus controls the potent antifungal response in Drosophila adults. Cell. 1996;86:973–983. doi: 10.1016/s0092-8674(00)80172-5. [DOI] [PubMed] [Google Scholar]
- 18.Poltorak A, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1999;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 19.Crow YJ, Manel N. Aicardi-Goutieres syndrome and the type I interferonopathies. Nat. Rev. Immunol. 2015;15:429–440. doi: 10.1038/nri3850. [DOI] [PubMed] [Google Scholar]
- 20.Dinarello CA, Simon A, van der Meer JW. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat. Rev. Drug Discov. 2012;11:633–652. doi: 10.1038/nrd3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rakoff-Nahoum S, Paglino J, Eslami-Varzaneh F, Edberg S, Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Barton ES, et al. Herpesvirus latency confers symbiotic protection from bacterial infection. Nature. 2007;447:326–329. doi: 10.1038/nature05762. [DOI] [PubMed] [Google Scholar]
- 23.Marie I, Durbin JE, Levy DE. Differential viral induction of distinct interferon-alpha genes by positive feedback through interferon regulatory factor-7. EMBO J. 1998;17:6660–6669. doi: 10.1093/emboj/17.22.6660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bauernfeind FG, et al. Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J. Immunol. 2009;183:787–791. doi: 10.4049/jimmunol.0901363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yan N, Regalado-Magdos AD, Stiggelbout B, Lee-Kirsch MA, Lieberman J. The cytosolic exonuclease TREX1 inhibits the innate immune response to human immunodeficiency virus type 1. Nat. Immunol. 2010;11:1005–1013. doi: 10.1038/ni.1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luecke S, et al. cGAS is activated by DNA in a length-dependent manner. EMBO Rep. 2017;18:1707–1715. doi: 10.15252/embr.201744017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gehrig S, et al. Identification of modifications in microbial, native tRNA that suppress immunostimulatory activity. J. Exp. Med. 2012;209:225–233. doi: 10.1084/jem.20111044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rice GI, et al. Gain-of-function mutations in IFIH1 cause a spectrum of human disease phenotypes associated with upregulated type I interferon signaling. Nat. Genet. 2014;46:503–509. doi: 10.1038/ng.2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kagan JC, Magupalli VG, Wu H. SMOCs: supramolecular organizing centres that control innate immunity. Nat. Rev. Immunol. 2014;14:821–826. doi: 10.1038/nri3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamerman JA, et al. Negative regulation of TLR signaling in myeloid cells–implications for autoimmune diseases. Immunol. Rev. 2016;269:212–227. doi: 10.1111/imr.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carey CM, et al. Recurrent loss-of-function mutations reveal costs to OAS1 antiviral activity in primates. Cell Host Microbe. 2019;25:336–343. doi: 10.1016/j.chom.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim JK, et al. Genetic variation in OAS1 is a risk factor for initial infection with West Nile virus in man. PLoS Pathog. 2009;5:e1000321. doi: 10.1371/journal.ppat.1000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li H, et al. Identification of a Sjogren’s syndrome susceptibility locus at OAS1 that influences isoform switching, protein expression, and responsiveness to type I interferons. PLoS Genet. 2017;13:e1006820. doi: 10.1371/journal.pgen.1006820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laguette N, et al. SAMHD1 is the dendritic- and myeloid-cell-specific HIV-1 restriction factor counteracted by Vpx. Nature. 2011;474:654–657. doi: 10.1038/nature10117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gariano GR, et al. The intracellular DNA sensor IFI16 gene acts as restriction factor for human cytomegalovirus replication. PLoS Pathog. 2012;8:e1002498. doi: 10.1371/journal.ppat.1002498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Orvedahl A, et al. HSV-1 ICP34.5 confers neurovirulence by targeting the Beclin 1 autophagy protein. Cell Host. Microbe. 2007;1:23–35. doi: 10.1016/j.chom.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 37.Harris RS, Hultquist JF, Evans DT. The restriction factors of human immunodeficiency virus. J. Biol. Chem. 2012;287:40875–40883. doi: 10.1074/jbc.R112.416925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duggal NK, Emerman M. Evolutionary conflicts between viruses and restriction factors shape immunity. Nat. Rev. Immunol. 2012;12:687–695. doi: 10.1038/nri3295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bishop KN, Holmes RK, Sheehy AM, Malim MH. APOBEC-mediated editing of viral RNA. Science. 2004;305:645. doi: 10.1126/science.1100658. [DOI] [PubMed] [Google Scholar]
- 40.Neil SJ, Zang T, Bieniasz PD. Tetherin inhibits retrovirus release and is antagonized by HIV-1 Vpu. Nature. 2008;451:425–430. doi: 10.1038/nature06553. [DOI] [PubMed] [Google Scholar]
- 41.Goldstone DC, et al. HIV-1 restriction factor SAMHD1 is a deoxynucleoside triphosphate triphosphohydrolase. Nature. 2011;480:379–382. doi: 10.1038/nature10623. [DOI] [PubMed] [Google Scholar]
- 42.Glass M, Everett RD. Components of promyelocytic leukemia nuclear bodies (ND10) act cooperatively to repress herpesvirus infection. J. Virol. 2013;87:2174–2185. doi: 10.1128/JVI.02950-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Merkl PE, Knipe DM. Role for a filamentous nuclear assembly of IFI16, DNA, and host factors in restriction of herpesviral infection. mBio. 2019;10:e02621. doi: 10.1128/mBio.02621-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pichlmair A, et al. IFIT1 is an antiviral protein that recognizes 5’-triphosphate RNA. Nat. Immunol. 2011;12:624–630. doi: 10.1038/ni.2048. [DOI] [PubMed] [Google Scholar]
- 45.Full F, et al. Centrosomal protein TRIM43 restricts herpesvirus infection by regulating nuclear lamina integrity. Nat. Microbiol. 2019;4:164–176. doi: 10.1038/s41564-018-0285-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schoggins JW, et al. Pan-viral specificity of IFN-induced genes reveals new roles for cGAS in innate immunity. Nature. 2013;505:691–695. doi: 10.1038/nature12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brien JD, et al. Interferon regulatory factor-1 (IRF-1) shapes both innate and CD8+ T cell immune responses against West Nile virus infection. PLoS Pathog. 2011;7:e1002230. doi: 10.1371/journal.ppat.1002230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou R, Rana TM. RNA-based mechanisms regulating host-virus interactions. Immunol. Rev. 2013;253:97–111. doi: 10.1111/imr.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hamilton AJ, Baulcombe DC. A species of small antisense RNA in posttranscriptional gene silencing in plants. Science. 1999;286:950–952. doi: 10.1126/science.286.5441.950. [DOI] [PubMed] [Google Scholar]
- 50.Mourrain P, et al. Arabidopsis SGS2 and SGS3 genes are required for posttranscriptional gene silencing and natural virus resistance. Cell. 2000;101:533–542. doi: 10.1016/s0092-8674(00)80863-6. [DOI] [PubMed] [Google Scholar]
- 51.Lu R, et al. Animal virus replication and RNAi-mediated antiviral silencing in Caenorhabditis elegans. Nature. 2005;436:1040–1043. doi: 10.1038/nature03870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang XH, et al. RNA interference directs innate immunity against viruses in adult Drosophila. Science. 2006;312:452–454. doi: 10.1126/science.1125694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galiana-Arnoux D, Dostert C, Schneemann A, Hoffmann JA, Imler JL. Essential function in vivo for Dicer-2 in host defense against RNA viruses in drosophila. Nat. Immunol. 2006;7:590–597. doi: 10.1038/ni1335. [DOI] [PubMed] [Google Scholar]
- 54.Maillard PV, van der Veen AG, Poirier EZ, Reis ESC. Slicing and dicing viruses: antiviral RNA interference in mammals. EMBO J. 2019;38:e100941. doi: 10.15252/embj.2018100941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang Y, et al. Hepatitis C virus core protein is a potent inhibitor of RNA silencing-based antiviral response. Gastroenterology. 2006;130:883–892. doi: 10.1053/j.gastro.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 56.Fabozzi G, Nabel CS, Dolan MA, Sullivan NJ. Ebolavirus proteins suppress the effects of small interfering RNA by direct interaction with the mammalian RNA interference pathway. J. Virol. 2011;85:2512–2523. doi: 10.1128/JVI.01160-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yeaman MR, Yount NY. Mechanisms of antimicrobial peptide action and resistance. Pharmacol. Rev. 2003;55:27–55. doi: 10.1124/pr.55.1.2. [DOI] [PubMed] [Google Scholar]
- 58.Wilson CL, et al. Regulation of intestinal alpha-defensin activation by the metalloproteinase matrilysin in innate host defense. Science. 1999;286:113–117. doi: 10.1126/science.286.5437.113. [DOI] [PubMed] [Google Scholar]
- 59.Chromek M, et al. The antimicrobial peptide cathelicidin protects the urinary tract against invasive bacterial infection. Nat. Med. 2006;12:636–641. doi: 10.1038/nm1407. [DOI] [PubMed] [Google Scholar]
- 60.Ganz T, Metcalf JA, Gallin JI, Boxer LA, Lehrer RI. Microbicidal/cytotoxic proteins of neutrophils are deficient in two disorders: Chediak-Higashi syndrome and “specific” granule deficiency. J. Clin. Invest. 1988;82:552–556. doi: 10.1172/JCI113631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kumar P, Kizhakkedathu JN, Straus SK. Antimicrobial peptides: diversity, mechanism of action and strategies to improve the activity and biocompatibility in vivo. Biomolecules. 2018;8:4. doi: 10.3390/biom8010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jenssen H, Hamill P, Hancock RE. Peptide antimicrobial agents. Clin. Microbiol. Rev. 2006;19:491–511. doi: 10.1128/CMR.00056-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Valore EV, et al. Human beta-defensin-1: an antimicrobial peptide of urogenital tissues. J. Clin. Invest. 1998;101:1633–1642. doi: 10.1172/JCI1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nizet V, et al. Innate antimicrobial peptide protects the skin from invasive bacterial infection. Nature. 2001;414:454–457. doi: 10.1038/35106587. [DOI] [PubMed] [Google Scholar]
- 65.Quinones-Mateu ME, et al. Human epithelial beta-defensins 2 and 3 inhibit HIV-1 replication. AIDS. 2003;17:F39–F48. doi: 10.1097/00002030-200311070-00001. [DOI] [PubMed] [Google Scholar]
- 66.Ahmed A, Siman-Tov G, Hall G, Bhalla N, Narayanan A. Human antimicrobial peptides as therapeutics for viral infections. Viruses. 2019;11:704. doi: 10.3390/v11080704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Casals C, Garcia-Fojeda B, Minutti CM. Soluble defense collagens: sweeping up immune threats. Mol. Immunol. 2019;112:291–304. doi: 10.1016/j.molimm.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 68.Meschi J, et al. Surfactant protein D binds to human immunodeficiency virus (HIV) envelope protein gp120 and inhibits HIV replication. J. Gen. Virol. 2005;86:3097–3107. doi: 10.1099/vir.0.80764-0. [DOI] [PubMed] [Google Scholar]
- 69.Hartshorn KL, et al. Reduced influenza viral neutralizing activity of natural human trimers of surfactant protein D. Respir. Res. 2007;8:9. doi: 10.1186/1465-9921-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reading PC, et al. Antiviral activity of the long chain pentraxin PTX3 against influenza viruses. J. Immunol. 2008;180:3391–3398. doi: 10.4049/jimmunol.180.5.3391. [DOI] [PubMed] [Google Scholar]
- 71.LeVine AM, Whitsett JA, Hartshorn KL, Crouch EC, Korfhagen TR. Surfactant protein D enhances clearance of influenza A virus from the lung in vivo. J. Immunol. 2001;167:5868–5873. doi: 10.4049/jimmunol.167.10.5868. [DOI] [PubMed] [Google Scholar]
- 72.Jounblat R, et al. Binding and agglutination of Streptococcus pneumoniae by human surfactant protein D (SP-D) vary between strains, but SP-D fails to enhance killing by neutrophils. Infect. Immun. 2004;72:709–716. doi: 10.1128/IAI.72.2.709-716.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Isaacs CE, Xu W. Theaflavin-3,3’-digallate and lactic acid combinations reduce herpes simplex virus infectivity. Antimicrob. Agents. Chemother. 2013;57:3806–3814. doi: 10.1128/AAC.00659-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tyssen D, et al. Anti-HIV-1 activity of lactic acid in human cervicovaginal fluid. mSphere. 2018;3:e00055. doi: 10.1128/mSphere.00055-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sanchez EL, Lagunoff M. Viral activation of cellular metabolism. Virology. 2015;479-480:609–618. doi: 10.1016/j.virol.2015.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Munger J, Bajad SU, Coller HA, Shenk T, Rabinowitz JD. Dynamics of the cellular metabolome during human cytomegalovirus infection. PLoS Pathog. 2006;2:e132. doi: 10.1371/journal.ppat.0020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Libran-Perez M, Pereiro P, Figueras A, Novoa B. Antiviral activity of palmitic acid via autophagic flux inhibition in zebrafish (Danio rerio) Fish Shellfish Immunol. 2019;95:595–605. doi: 10.1016/j.fsi.2019.10.055. [DOI] [PubMed] [Google Scholar]
- 78.Kachroo A, et al. An oleic acid-mediated pathway induces constitutive defense signaling and enhanced resistance to multiple pathogens in soybean. Mol. Plant Microbe Interact. 2008;21:564–575. doi: 10.1094/MPMI-21-5-0564. [DOI] [PubMed] [Google Scholar]
- 79.Nevo Y, Nelson N. The NRAMP family of metal-ion transporters. Biochim. Biophys. Acta. 2006;1763:609–620. doi: 10.1016/j.bbamcr.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 80.Vidal SM, Malo D, Vogan K, Skamene E, Gros P. Natural resistance to infection with intracellular parasites: isolation of a candidate for Bcg. Cell. 1993;73:469–485. doi: 10.1016/0092-8674(93)90135-d. [DOI] [PubMed] [Google Scholar]
- 81.Plant JE, Blackwell JM, O’Brien AD, Bradley DJ, Glynn AA. Are the Lsh and Ity disease resistance genes at one locus on mouse chromosome 1? Nature. 1982;297:510–511. doi: 10.1038/297510a0. [DOI] [PubMed] [Google Scholar]
- 82.Supek F, Supekova L, Nelson H, Nelson N. A yeast manganese transporter related to the macrophage protein involved in conferring resistance to mycobacteria. Proc. Natl Acad. Sci. USA. 1996;93:5105–5110. doi: 10.1073/pnas.93.10.5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mayeur S, Spahis S, Pouliot Y, Levy E. Lactoferrin, a pleiotropic protein in health and disease. Antioxid. Redox Signal. 2016;24:813–836. doi: 10.1089/ars.2015.6458. [DOI] [PubMed] [Google Scholar]
- 84.Velusamy SK, Markowitz K, Fine DH, Velliyagounder K. Human lactoferrin protects against Streptococcus mutans-induced caries in mice. Oral Dis. 2016;22:148–154. doi: 10.1111/odi.12401. [DOI] [PubMed] [Google Scholar]
- 85.Levine B, Mizushima N, Virgin HW. Autophagy in immunity and inflammation. Nature. 2011;469:323–335. doi: 10.1038/nature09782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lim JJ, Grinstein S, Roth Z. Diversity and versatility of phagocytosis: roles in innate immunity, tissue remodeling, and homeostasis. Front. Cell. Infect. Microbiol. 2017;7:191. doi: 10.3389/fcimb.2017.00191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Thurston TLM, Wandel MP, von Muhlinen N, Foeglein A, Randow F. Galectin 8 targets damaged vesicles for autophagy to defend cells against bacterial invasion. Nature. 2012;482:414–418. doi: 10.1038/nature10744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gros P, Milder FJ, Janssen BJ. Complement driven by conformational changes. Nat. Rev. Immunol. 2008;8:48–58. doi: 10.1038/nri2231. [DOI] [PubMed] [Google Scholar]
- 89.Orvedahl A, et al. Autophagy protects against Sindbis virus infection of the central nervous system. Cell Host Microbe. 2010;7:115–127. doi: 10.1016/j.chom.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sparrer KMJ, et al. TRIM23 mediates virus-induced autophagy via activation of TBK1. Nat. Microbiol. 2017;2:1543–1557. doi: 10.1038/s41564-017-0017-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Franco LH, et al. The ubiquitin ligase Smurf1 functions in selective autophagy of Mycobacterium tuberculosis and anti-tuberculous host defense. Cell Host Microbe. 2017;21:59–72. doi: 10.1016/j.chom.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Huett A, et al. The LRR and RING domain protein LRSAM1 is an E3 ligase crucial for ubiquitin-dependent autophagy of intracellular Salmonella Typhimurium. Cell Host Microbe. 2012;12:778–790. doi: 10.1016/j.chom.2012.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wild P, et al. Phosphorylation of the autophagy receptor optineurin restricts Salmonella growth. Science. 2011;333:228–233. doi: 10.1126/science.1205405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ravenhill BJ, et al. The cargo receptor NDP52 initiates selective autophagy by recruiting the ULK complex to cytosol-invading bacteria. Mol. Cell. 2019;74:320–329. doi: 10.1016/j.molcel.2019.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gutierrez MG, et al. Autophagy is a defense mechanism inhibiting BCG and Mycobacterium tuberculosis survival in infected macrophages. Cell. 2004;119:753–766. doi: 10.1016/j.cell.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 96.Castillo EF, et al. Autophagy protects against active tuberculosis by suppressing bacterial burden and inflammation. Proc. Natl Acad. Sci. USA. 2012;109:E3168–E3176. doi: 10.1073/pnas.1210500109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kimmey JM, et al. Unique role for ATG5 in neutrophil-mediated immunopathology during M. tuberculosis infection. Nature. 2015;528:565–569. doi: 10.1038/nature16451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ricklin D, Reis ES, Lambris JD. Complement in disease: a defence system turning offensive. Nat. Rev. Nephrol. 2016;12:383–401. doi: 10.1038/nrneph.2016.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shi L, et al. Mannose-binding lectin-deficient mice are susceptible to infection with Staphylococcus aureus. J. Exp. Med. 2004;199:1379–1390. doi: 10.1084/jem.20032207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Whitnack E, Beachey EH. Inhibition of complement-mediated opsonization and phagocytosis of Streptococcus pyogenes by D fragments of fibrinogen and fibrin bound to cell surface M protein. J. Exp. Med. 1985;162:1983–1997. doi: 10.1084/jem.162.6.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Heckmann BL, Boada-Romero E, Cunha LD, Magne J, Green DR. LC3-associated phagocytosis and inflammation. J. Mol. Biol. 2017;429:3561–3576. doi: 10.1016/j.jmb.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Martinez J, et al. Noncanonical autophagy inhibits the autoinflammatory, lupus-like response to dying cells. Nature. 2016;533:115–119. doi: 10.1038/nature17950. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 103.Martinez J, et al. Molecular characterization of LC3-associated phagocytosis reveals distinct roles for Rubicon, NOX2 and autophagy proteins. Nat. Cell. Biol. 2015;17:893–906. doi: 10.1038/ncb3192. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 104.Wang Y, Le WD. Autophagy and ubiquitin-proteasome system. Adv. Exp. Med. Biol. 2019;1206:527–550. doi: 10.1007/978-981-15-0602-4_25. [DOI] [PubMed] [Google Scholar]
- 105.Hauler F, Mallery DL, McEwan WA, Bidgood SR, James LC. AAA ATPase p97/VCP is essential for TRIM21-mediated virus neutralization. Proc. Natl Acad. Sci. USA. 2012;109:19733–19738. doi: 10.1073/pnas.1210659109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tam JC, Bidgood SR, McEwan WA, James LC. Intracellular sensing of complement C3 activates cell autonomous immunity. Science. 2014;345:1256070. doi: 10.1126/science.1256070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bottermann M, et al. Complement C4 prevents viral infection through capsid inactivation. Cell Host Microbe. 2019;25:617–629 e617. doi: 10.1016/j.chom.2019.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Camborde L, et al. The ubiquitin-proteasome system regulates the accumulation of Turnip yellow mosaic virus RNA-dependent RNA polymerase during viral infection. Plant Cell. 2010;22:3142–3152. doi: 10.1105/tpc.109.072090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ruckdeschel K, et al. The proteasome pathway destabilizes Yersinia outer protein E and represses its antihost cell activities. J. Immunol. 2006;176:6093–6102. doi: 10.4049/jimmunol.176.10.6093. [DOI] [PubMed] [Google Scholar]
- 110.Sahana N, et al. Inhibition of the host proteasome facilitates papaya ringspot virus accumulation and proteosomal catalytic activity is modulated by viral factor HcPro. PLoS ONE. 2012;7:e52546. doi: 10.1371/journal.pone.0052546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xu Y, et al. Rice stripe tenuivirus nonstructural protein 3 hijacks the 26S proteasome of the small brown planthopper via direct interaction with regulatory particle non-ATPase subunit 3. J. Virol. 2015;89:4296–4310. doi: 10.1128/JVI.03055-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dudnik A, Bigler L, Dudler R. Production of proteasome inhibitor syringolin A by the endophyte Rhizobium sp. strain AP16. Appl. Environ. Microbiol. 2014;80:3741–3748. doi: 10.1128/AEM.00395-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Groll M, et al. A plant pathogen virulence factor inhibits the eukaryotic proteasome by a novel mechanism. Nature. 2008;452:755–758. doi: 10.1038/nature06782. [DOI] [PubMed] [Google Scholar]
- 114.Zimmermann C, et al. The abundant tegument protein pUL25 of human cytomegalovirus prevents proteasomal degradation of pUL26 and supports its suppression of ISGylation. J. Virol. 2018;92:e01180–e01218. doi: 10.1128/JVI.01180-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chakrabarti A, Jha BK, Silverman RH. New insights into the role of RNase L in innate immunity. J. Interferon Cytokine Res. 2011;31:49–57. doi: 10.1089/jir.2010.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Banerjee S, et al. OAS-RNase L innate immune pathway mediates the cytotoxicity of a DNA-demethylating drug. Proc. Natl Acad. Sci. USA. 2019;116:5071–5076. doi: 10.1073/pnas.1815071116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Birdwell LD, et al. Activation of RNase L by murine coronavirus in myeloid cells is dependent on basal Oas gene expression and independent of virus-induced interferon. J. Virol. 2016;90:3160–3172. doi: 10.1128/JVI.03036-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Stetson DB, Ko JS, Heidmann T, Medzhitov R. Trex1 prevents cell-intrinsic initiation of autoimmunity. Cell. 2008;134:587–598. doi: 10.1016/j.cell.2008.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin. Microbiol. Rev. 2009;22:240–273. doi: 10.1128/CMR.00046-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Stavrou S, Blouch K, Kotla S, Bass A, Ross SR. Nucleic acid recognition orchestrates the anti-viral response to retroviruses. Cell Host Microbe. 2015;17:478–488. doi: 10.1016/j.chom.2015.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Maelfait J, Bridgeman A, Benlahrech A, Cursi C, Rehwinkel J. Restriction by SAMHD1 limits cGAS/STING-dependent innate and adaptive immune responses to HIV-1. Cell Rep. 2016;16:1492–1501. doi: 10.1016/j.celrep.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Marques JT, et al. A structural basis for discriminating between self and nonself double-stranded RNAs in mammalian cells. Nat. Biotechnol. 2006;24:559–565. doi: 10.1038/nbt1205. [DOI] [PubMed] [Google Scholar]
- 123.Britigan BE, Lewis TS, Waldschmidt M, McCormick ML, Krieg AM. Lactoferrin binds CpG-containing oligonucleotides and inhibits their immunostimulatory effects on human B cells. J. Immunol. 2001;167:2921–2928. doi: 10.4049/jimmunol.167.5.2921. [DOI] [PubMed] [Google Scholar]
- 124.Cheng J, et al. Autophagy regulates MAVS signaling activation in a phosphorylation-dependent manner in microglia. Cell Death Differ. 2017;24:276–287. doi: 10.1038/cdd.2016.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Tal MC, et al. Absence of autophagy results in reactive oxygen species-dependent amplification of RLR signaling. Proc. Natl Acad. Sci. USA. 2009;106:2770–2775. doi: 10.1073/pnas.0807694106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Prabakaran T, et al. Attenuation of cGAS-STING signaling is mediated by a p62/SQSTM1-dependent autophagy pathway activated by TBK1. EMBO J. 2018;37:e97858. doi: 10.15252/embj.201797858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Aden K, et al. ATG16L1 orchestrates interleukin-22 signaling in the intestinal epithelium via cGAS-STING. J. Exp. Med. 2018;215:2868–2886. doi: 10.1084/jem.20171029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang W, et al. Lactate is a natural suppressor of RLR signaling by targeting MAVS. Cell. 2019;178:176–189.e15. doi: 10.1016/j.cell.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shim DW, et al. Anti-inflammatory action of an antimicrobial model peptide that suppresses the TRIF-dependent signaling pathway via inhibition of toll-like receptor 4 endocytosis in lipopolysaccharide-stimulated macrophages. PLoS ONE. 2015;10:e0126871. doi: 10.1371/journal.pone.0126871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Haber JE. Deciphering the DNA damage response. Cell. 2015;162:1183–1185. doi: 10.1016/j.cell.2015.08.034. [DOI] [PubMed] [Google Scholar]
- 131.Johnston JA, Ward CL, Kopito RR. Aggresomes: a cellular response to misfolded proteins. J. Cell. Biol. 1998;143:1883–1898. doi: 10.1083/jcb.143.7.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fortun J, Dunn WA, Jr, Joy S, Li J, Notterpek L. Emerging role for autophagy in the removal of aggresomes in Schwann cells. J. Neurosci. 2003;23:10672–10680. doi: 10.1523/JNEUROSCI.23-33-10672.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Holze C, et al. Oxeiptosis, a ROS-induced caspase-independent apoptosis-like cell-death pathway. Nat. Immunol. 2018;19:130–140. doi: 10.1038/s41590-017-0013-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Yu XH, Zhang DW, Zheng XL, Tang CK. Cholesterol transport system: an integrated cholesterol transport model involved in atherosclerosis. Prog. Lipid Res. 2019;73:65–91. doi: 10.1016/j.plipres.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 135.Mackenzie KJ, et al. cGAS surveillance of micronuclei links genome instability to innate immunity. Nature. 2017;548:461–465. doi: 10.1038/nature23449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Harding SM, et al. Mitotic progression following DNA damage enables pattern recognition within micronuclei. Nature. 2017;548:466–470. doi: 10.1038/nature23470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Crow YJ, et al. Mutations in the gene encoding the 3′-5′ DNA exonuclease TREX1 cause Aicardi-Goutieres syndrome at the AGS1 locus. Nat. Genet. 2006;38:917–920. doi: 10.1038/ng1845. [DOI] [PubMed] [Google Scholar]
- 138.Rodero MP, et al. Type I interferon-mediated autoinflammation due to DNase II deficiency. Nat. Commun. 2017;8:2176. doi: 10.1038/s41467-017-01932-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Halle A, et al. The NALP3 inflammasome is involved in the innate immune response to amyloid-beta. Nat. Immunol. 2008;9:857–865. doi: 10.1038/ni.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Duewell P, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357–1361. doi: 10.1038/nature08938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Laplana M, Caruz A, Pineda JA, Puig T, Fibla J. Association of BST-2 gene variants with HIV disease progression underscores the role of BST-2 in HIV type 1 infection. J. Infect. Dis. 2013;207:411–419. doi: 10.1093/infdis/jis685. [DOI] [PubMed] [Google Scholar]
- 142.Everitt AR, et al. IFITM3 restricts the morbidity and mortality associated with influenza. Nature. 2012;484:519–523. doi: 10.1038/nature10921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Tesse R, et al. Association of beta-defensin-1 gene polymorphisms with Pseudomonas aeruginosa airway colonization in cystic fibrosis. Genes Immun. 2008;9:57–60. doi: 10.1038/sj.gene.6364440. [DOI] [PubMed] [Google Scholar]
- 144.Shao Y, et al. Association between genetic polymorphisms in the autophagy-related 5 gene promoter and the risk of sepsis. Sci. Rep. 2017;7:9399. doi: 10.1038/s41598-017-09978-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yordy B, Iijima N, Huttner A, Leib D, Iwasaki A. A neuron-specific role for autophagy in antiviral defense against herpes simplex virus. Cell Host Microbe. 2012;12:334–345. doi: 10.1016/j.chom.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wu X, et al. Intrinsic immunity shapes viral resistance of stem cells. Cell. 2018;172:423–438 e425. doi: 10.1016/j.cell.2017.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Eggenberger J, Blanco-Melo D, Panis M, Brennand KJ, Tenoever BR. Type I interferon response impairs differentiation potential of pluripotent stem cells. Proc. Natl Acad. Sci. USA. 2019;116:1384–1393. doi: 10.1073/pnas.1812449116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Liu Y, et al. Mutations in proteasome subunit beta type 8 cause chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature with evidence of genetic and phenotypic heterogeneity. Arthritis Rheum. 2012;64:895–907. doi: 10.1002/art.33368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Brehm A, et al. Additive loss-of-function proteasome subunit mutations in CANDLE/PRAAS patients promote type I IFN production. J. Clin. Invest. 2015;125:4196–4211. doi: 10.1172/JCI81260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Massaad MJ, et al. Deficiency of base excision repair enzyme NEIL3 drives increased predisposition to autoimmunity. J. Clin. Invest. 2016;126:4219–4236. doi: 10.1172/JCI85647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Khor TO, et al. Nrf2-deficient mice have an increased susceptibility to dextran sulfate sodium-induced colitis. Cancer Res. 2006;66:11580–11584. doi: 10.1158/0008-5472.CAN-06-3562. [DOI] [PubMed] [Google Scholar]
- 152.Ivanciuc T, Sbrana E, Casola A, Garofalo RP. Protective role of nuclear factor erythroid 2-related factor 2 against respiratory syncytial virus and human metapneumovirus infections. Front. Immunol. 2018;9:854. doi: 10.3389/fimmu.2018.00854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Peyssonnaux C, et al. HIF-1alpha expression regulates the bactericidal capacity of phagocytes. J. Clin. Invest. 2005;115:1806–1815. doi: 10.1172/JCI23865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Blondeau C, et al. Tetherin restricts herpes simplex virus 1 and is antagonized by glycoprotein M. J. Virol. 2013;87:13124–13133. doi: 10.1128/JVI.02250-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Smith SE, et al. Interferon-induced transmembrane protein 1 restricts replication of viruses that enter cells via the plasma membrane. J. Virol. 2019;93:e02003. doi: 10.1128/JVI.02003-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bernhardt A, et al. Inflammatory cell infiltration and resolution of kidney inflammation is orchestrated by the cold-shock protein Y-box binding protein-1. Kidney Int. 2017;92:1157–1177. doi: 10.1016/j.kint.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 157.Hollenbaugh JA, et al. Host factor SAMHD1 restricts DNA viruses in non-dividing myeloid cells. PLoS Pathog. 2013;9:e1003481. doi: 10.1371/journal.ppat.1003481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Nakaya Y, Stavrou S, Blouch K, Tattersall P, Ross SR. In vivo examination of mouse APOBEC3- and human APOBEC3A- and APOBEC3G-mediated restriction of parvovirus and herpesvirus infection in mouse models. J. Virol. 2016;90:8005–8012. doi: 10.1128/JVI.00973-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Girardi E, et al. Cross-species comparative analysis of Dicer proteins during Sindbis virus infection. Sci. Rep. 2015;5:10693. doi: 10.1038/srep10693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Dombrowski Y, et al. Cytosolic DNA triggers inflammasome activation in keratinocytes in psoriatic lesions. Sci. Transl. Med. 2011;3:82ra38. doi: 10.1126/scitranslmed.3002001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Stamme C, Muller M, Hamann L, Gutsmann T, Seydel U. Surfactant protein a inhibits lipopolysaccharide-induced immune cell activation by preventing the interaction of lipopolysaccharide with lipopolysaccharide-binding protein. Am. J. Respir. Cell Mol. Biol. 2002;27:353–360. doi: 10.1165/rcmb.4812. [DOI] [PubMed] [Google Scholar]
- 162.Daniels BP, et al. The nucleotide sensor ZBP1 and kinase RIPK3 induce the enzyme IRG1 to promote an antiviral metabolic state in neurons. Immunity. 2019;50:64–76 e64. doi: 10.1016/j.immuni.2018.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Nair S, et al. Irg1 expression in myeloid cells prevents immunopathology during M. tuberculosis infection. J. Exp. Med. 2018;215:1035–1045. doi: 10.1084/jem.20180118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Jessop F, Hamilton RF, Rhoderick JF, Shaw PK, Holian A. Autophagy deficiency in macrophages enhances NLRP3 inflammasome activity and chronic lung disease following silica exposure. Toxicol. Appl. Pharmacol. 2016;309:101–110. doi: 10.1016/j.taap.2016.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Meissner F, et al. Inflammasome activation in NADPH oxidase defective mononuclear phagocytes from patients with chronic granulomatous disease. Blood. 2010;116:1570–1573. doi: 10.1182/blood-2010-01-264218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Segal BH, et al. NADPH oxidase limits innate immune responses in the lungs in mice. PLoS ONE. 2010;5:e9631. doi: 10.1371/journal.pone.0009631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gluschko A, et al. The beta2 integrin Mac-1 induces protective LC3-associated phagocytosis of listeria monocytogenes. Cell Host Microbe. 2018;23:324–337 e325. doi: 10.1016/j.chom.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 168.Gong L, et al. The Burkholderia pseudomallei type III secretion system and BopA are required for evasion of LC3-associated phagocytosis. PLoS ONE. 2011;6:e17852. doi: 10.1371/journal.pone.0017852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Masters SL, Simon A, Aksentijevich I, Kastner DL. Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory disease. Ann. Rev. Immunol. 2009;27:621–668. doi: 10.1146/annurev.immunol.25.022106.141627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Uggenti C, Lepelley A, Crow YJ. Self-awareness: nucleic acid-driven inflammation and the type I interferonopathies. Annu. Rev. Immunol. 2019;37:247–267. doi: 10.1146/annurev-immunol-042718-041257. [DOI] [PubMed] [Google Scholar]
- 171.Jesus AA, Goldbach-Mansky R. IL-1 blockade in autoinflammatory syndromes. Annu. Rev. Med. 2014;65:223–244. doi: 10.1146/annurev-med-061512-150641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Schwartz DM, et al. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat. Rev. Drug. Discov. 2017;17:78. doi: 10.1038/nrd.2017.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kim H, Sanchez GA, Goldbach-Mansky R. Insights from Mendelian interferonopathies: comparison of CANDLE, SAVI with AGS, monogenic lupus. J. Mol. Med. 2016;94:1111–1127. doi: 10.1007/s00109-016-1465-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sanjuan MA, et al. Toll-like receptor signalling in macrophages links the autophagy pathway to phagocytosis. Nature. 2007;450:1253–1257. doi: 10.1038/nature06421. [DOI] [PubMed] [Google Scholar]
- 175.Doyle SE, et al. Toll-like receptors induce a phagocytic gene program through p38. J. Exp. Med. 2004;199:81–90. doi: 10.1084/jem.20031237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Henneke P, et al. Cellular activation, phagocytosis, and bactericidal activity against group B streptococcus involve parallel myeloid differentiation factor 88-dependent and independent signaling pathways. J. Immunol. 2002;169:3970–3977. doi: 10.4049/jimmunol.169.7.3970. [DOI] [PubMed] [Google Scholar]
- 177.Hawley KL, et al. CD14 cooperates with complement receptor 3 to mediate MyD88-independent phagocytosis of Borrelia burgdorferi. Proc. Natl Acad. Sci. USA. 2012;109:1228–1232. doi: 10.1073/pnas.1112078109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Peng G, Lei KJ, Jin W, Greenwell-Wild T, Wahl SM. Induction of APOBEC3 family proteins, a defensive maneuver underlying interferon-induced anti-HIV-1 activity. J. Exp. Med. 2006;203:41–46. doi: 10.1084/jem.20051512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Walmsley SR, et al. Prolyl hydroxylase 3 (PHD3) is essential for hypoxic regulation of neutrophilic inflammation in humans and mice. J. Clin. Invest. 2011;121:1053–1063. doi: 10.1172/JCI43273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Olagnier D, et al. Nrf2 negatively regulates STING indicating a link between antiviral sensing and metabolic reprogramming. Nat. Commun. 2018;9:3506. doi: 10.1038/s41467-018-05861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]