Abstract
Background:
Brain health diplomacy aims to influence the global policy environment for brain health (i.e. dementia, depression, and other mind/brain disorders) and bridges the disciplines of global brain health, international affairs, management, law, and economics. Determinants of brain health include educational attainment, diet, access to health care, physical activity, social support, and environmental exposures, as well as chronic brain disorders and treatment. Global challenges associated with these determinants include large-scale conflicts and consequent mass migration, chemical contaminants, air quality, socioeconomic status, climate change, and global population aging. Given the rapidly advancing technological innovations impacting brain health, it is paramount to optimize the benefits and mitigate the drawbacks of such technologies.
Objective:
We propose a working model of Brain health INnovation Diplomacy (BIND).
Methods:
We prepared a selective review using literature searches of studies pertaining to brain health technological innovation and diplomacy.
Results:
BIND aims to improve global brain health outcomes by leveraging technological innovation, entrepreneurship, and innovation diplomacy. It acknowledges the key role that technology, entrepreneurship, and digitization play and will increasingly play in the future of brain health for individuals and societies alike. It strengthens the positive role of novel solutions, recognizes and works to manage both real and potential risks of digital platforms. It is recognition of the political, ethical, cultural, and economic influences that brain health technological innovation and entrepreneurship can have.
Conclusions:
By creating a framework for BIND, we can use this to ensure a systematic model for the use of technology to optimize brain health.
Keywords: Brain health, dementia, Alzheimer’s, technology, depression, innovation, diplomacy, entrepreneurship
Introduction
Health diplomacy focuses on negotiations that aim to influence and affect the global policy environment for human health and it leverages the disciplines of global health, international affairs, management, law, and economics (Kennedy et al., 2017; Turekian et al., 2014; WHO, 2018). Health diplomacy uses conventional approaches to optimizing global health such as strengthening the health system and leveraging the public and not-for-profit sectors. It is an important means of exercising large-scale reforms because it can have cultural and economic impact on many nations. There have been numerous examples of health diplomacy making important contributions to solving global health care crises (e.g. the President’s Emergency Plan for AIDS Relief [PEPFAR]; projects addressing Ebola and Zika viruses, the “bird flu” and “swine flu” epidemics, the rise of antimicrobial resistance; and the Sustainable Development Goals aiming to impact chronic disease deaths (Colglazier, 2018; Gomez-Olive and Thorogood, 2018; Reid et al., 2019)).
The population of people with illnesses affecting brain health (i.e. dementia, depression, and other mind/brain disorders) is increasing rapidly around the world (ADI, 2018; Cantarero-Prieto et al., 2019). The global societal and economic cost of dementia is approximately USD $1 trillion per year (ADI, 2018). Rates of dementia and their associated economic burden are both growing (ADI, 2015; 2018; Cantarero-Prieto et al., 2019). While dementia is not a normal part of the aging process, advanced age remains a primary risk factor. In the coming decades, expansion of aging populations will occur most rapidly in low- and middle-income countries (LMICs [Parra et al., 2018]). Therefore, the burden of dementia will be disproportionately experienced in these regions (ADI, 2013; GBHI, 2019; UN, 2015). Dementia incidence is driven largely by the same determinants that drive other major health conditions that are rooted in socioeconomic inequities such as lower educational attainment, poor diet, smoking, less access to health care, and inadequate treatment of hypertension and other medical diseases (GBHI, 2019; Livingston et al., 2017; Sukumaran, 2019). Alarmingly, few countries have developed a national dementia plan, dementia still is often assumed to be a normal part of aging and is often underrecognized (GBHI, 2019; Livingston et al., 2017; Valcour et al., 2000). The World Health Organization (WHO) has set a target of 75% of all member states (or 146 countries) to have a national plan on dementia in place by 2025 (WHO, 2017). As of 2019, only 32 countries had implemented a plan (ADI, 2019). These 32 adopters tend to be high-income countries (HICs) such as Australia, Japan, Norway, and the U.S., although Mexico, Cuba, and Indonesia all have national plans for dementia. Another 30 countries have plans under development, which would result in a much broader global reach once implemented (Barbarino et al., 2019).
Epidemiological modeling demonstrates that a population-level dementia risk reduction approach of 10–20% could prevent up to 8–15% of dementia cases projected around the world, respectively, in the next 20 years (Norton et al., 2014). Additionally, individual-level factors such as access to medicine and information, neuroimaging, diagnostics, specialist care, and personal beliefs associated with brain health can have a significant impact on personal well-being. Further, higher-level determinants – e.g. air pollution and conflict-driven mass migration – may impact disease course by hastening disease onset (Peters et al., 2019) or preventing access to care (Ledoux et al., 2018), respectively. Current global challenges that may be exacerbating population brain health disorders include climate change, air pollution, large-scale conflicts and associated mass migration, food insecurity, and lost productivity due to communicable and noncommunicable health conditions (for reviews, see Carey et al., 2018; Chen et al., 2017; Jung et al., 2015; Killin et al., 2016; Ledoux et al., 2018; Livingston et al., 2017; Wei et al., 2019). Given the breadth of factors that affect brain health, large-scale diplomatic activity is necessary to improve such societal conditions. These activities will help to coordinate and enhance projects in research, advocacy, clinical care, and public health across the globe HICs and LMICs.
We propose these traditional health diplomacy approaches to brain health should be referred to as “brain health diplomacy.” We hereby propose that brain health diplomacy will influence the global policy environment for brain health by leveraging the disciplines of global brain health, international affairs, management, law, and economics. Key examples of brain health diplomacy approaches include the WHO Guidelines titled “Risk Reduction of Cognitive Decline and Dementia” (WHO, 2019a), The Lancet’s Commission on Dementia Prevention, Intervention and Care (Livingston et al., 2017), and The Lancet-World Psychiatric Association Commission on Depression (Herrman et al., 2019). Such approaches aim to provide equity care and outcomes for dementia risk reduction and care in LMICs and HICs, as well as to save costs.
The current field of brain health diplomacy is valuable but, as it is, will not likely make a big enough impact on global brain health outcomes. It does not adequately consider the growing importance of technological innovation and entrepreneurship. Technological innovation and entrepreneurship may augment the impact of conventional brain health diplomacy mechanisms. With increasing rates of technological ubiquity, decreasing costs, and rapidity of innovation, the impact of technology on society is more visible than ever. The World Economic Forum (WEF) has conceptualized a Fourth Industrial Revolution as a model for articulating the disintegration of boundaries among the physical, digital, and biological worlds (WEF, 2019). It signifies the merging of infotech, biotech, robotics, 3D printing, artificial intelligence (AI), the Internet of Things (IoT), genetic engineering, omics, quantum computing, and other deep technologies.
In the domain of brain health, technological innovation is the application of technologies to brain health services and solutions using, for example, biomarkers and genomics, personal computing devices such as smartphones and tablets, computerized neurocognitive assessment systems, wearable monitors, web-based psychosocial and self-help resources, telehealth, multimodal neuroimaging, AI, virtual reality, and augmented reality (Abbott et al., 2018; Eyre et al., 2015a, 2017, 2018; Knapp et al., 2015; NSTC, 2019).
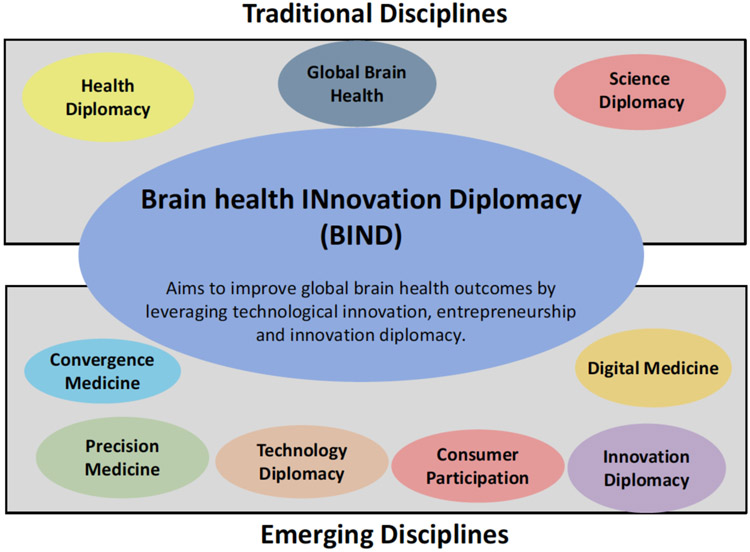
The model on Brain health INnovation Diplomacy (BIND) proposed is adapted from the previously proposed model of Mental Health Innovation Diplomacy (Eyre et al., 2019). BIND aims to improve global brain health outcomes by leveraging technological innovation, entrepreneurship, and innovation diplomacy. Improving outcomes may arise from optimization of access to care, prevention, screening, diagnosis, treatment, and treatment outcome tracking. BIND broadens the scope of health diplomacy by bringing together (or bind aka “BIND”) the disciplines of brain health, health diplomacy, and science diplomacy with the emerging disciplines of precision medicine, digital health, convergence science, innovation diplomacy, technology diplomacy, implementation science, and consumer participation. Each of these disciplines provides critical input to the field of BIND, but none alone are sufficient. Here, we offer current examples of BIND in action and provide further recommendations to develop the field.
In this paper, mental health and brain health are distinctly different fields. Mental health focuses on mental health disorders (e.g. depression, schizophrenia, attention deficit hyperactivity disorder), and brain health focuses on neurodegenerative disorders such as dementia and other cognitive disorders. There is ever greater convergence of these areas as the biological basis of mental disorders is increasingly defined.
Review of the role of technology and innovation in global health, brain health, and aging
If the model of BIND proposes to manage the promise and perils of technological in brain health, it is important to first review the role technology in this context. In the sections below, we explore the role of technology in global health, brain health, and aging contexts. We explore the role of technologies such as social media, internet use, remote monitoring sensors, and conclude by considering ethics.
Prototypes of innovations and innovation ecosystems influencing global health
There are a number of examples of specific innovations and innovation ecosystems serving to address neglected global disease and health conditions with new health technologies (Juma, 2018; Staruch et al., 2018). These examples are illustrative and could be adapted or leveraged for brain health innovation. One example is the provision and use of low-cost tablet computers like “Aakash” which was developed by Datawind and the Government of India and sold to Indian university students for USD $35 with the intention of reaching rural communities via e-learning (Staruch et al., 2018). Such low-cost computers have the potential to optimize the completion and sharing of medical records to better coordinate care for displaced peoples who are migrating across countries. They are also platforms for digital health resources, among other uses.
Supporting global health technology development is the newly established Global Health Technologies Coalition (GHTC) (GHTC, 2019). The GHTC is an advocacy organization, funded by the Bill and Melinda Gates Foundation, focused on global health, research, and development for new tools and technologies. The coalition of more than 25 nonprofit organizations, academic institutions, and aligned businesses advances policies to accelerate the creation of new drugs, vaccines, diagnostics, and other tools. The GHTC educates policymakers and stakeholders and convenes members and partners to facilitate innovation and advocacy for policy solutions and investment to spur innovation. This may be a useful platform for brain health innovation.
A recent review explored the role of health diplomacy through health entrepreneurship and using hackathons to address Palestinian-Israeli health concerns (Ramadi et al., 2019). Specifically, a hackathon was organized in Nazareth, Israel, supported in partnership by MIT’s Hacking Medicine and Hasoub, a local nonprofit. The authors noted “Bringing together Arab-Israeli and Jewish stakeholders, key academic and industry figures along with governmental agencies, the event bridged cultural lines and created an open forum to allow participants to network with large organisations, which could help move their ideas forward. Importantly, participants were exposed to health innovation methodologies and received the opportunity to learn, build diverse teams and create solutions to health problems” (page 6). This may be a useful predicate for approaches to optimizing brain health outcomes and cross-cultural understandings via hackathons.
Clinical brain health innovation in action
There are several areas of demonstrated clinical value for brain health technologies (Lund et al., 2018). A recent review was published by members of the U.S. Alzheimer’s Association Technology Professional Interest Area (Astell, 2019). There are three broad categories:
Dementia risk reduction technologies: Technology can be used to address lifestyle-based dementia risk reduction factors (Hartin et al., 2016). For example, a recent meta-analysis of web-based multidomain lifestyle programs for brain health (targeting physical and cognitive activities) demonstrated that these programs can positively influence brain health outcomes (Wesselman et al., 2019).
In-home remote monitoring and care for individuals diagnosed with dementia: The provision of technologies such as apps, wearables, and smart home systems could allow clinicians to remotely monitor patients, hence reducing unnecessary outpatient and inpatient visits. Such technologies can also provide prompts to support maintenance of cognitive, social, and physical functioning as well as tracking completion of daily activities.
Technological solutions for dementia caregivers: An illustrative example is the Supporting Family Caregivers with Technology for Dementia Home Care (FamTechCare) intervention (Williams et al., 2018). As stated, this intervention provides individualized dementia-care strategies to in-home caregivers based on video recordings that the caregiver creates of complex and challenging care situations (Williams et al., 2018). A team of dementia care experts review videos submitted by caregivers and provide interventions to improve care weekly for the experimental group.
A recent British dementia technology report with additional health economic analysis revealed dementia technology would be cost effective from a health and social care perspective in two core scenarios: postponing care home admission by at least 3 months and reducing unpaid care hours by about 8% or improved carer quality of life by 0.06 to 0.08 Quality Adjusted Life Years (QALYs) per year (Knapp et al., 2015).
Investment into the brain health innovation industry appears to be increasing (SharpBrains, 2013), yet some technology may be advancing without clear theoretical frameworks, awareness of ethical and privacy considerations, and without proof of concept. This is not to say that technology should not be part of the solution, but rather development and scaling should proceed with caution.
Clinical aging innovation in action
A report from the Task Force on Research and Development for Technology to Support Aging Adults, White House National Science and Technology Council (NSTC, 2019) was recently released seeking to convene U.S. federal government experts to identify emerging technologies to meet the needs of older adults. The report identified “a range of emerging technologies that have significant potential to assist older adults with successfully aging in place, each categorized by their role in supporting a set of primary capabilities” (page 2). These emerging technology areas included nutrition, hygiene, medication management, cognition, financial security, hearing, and telehealth. The report then provided recommendations as a guide for research and development.
The risk of adverse drug reactions and events is correlated to old age, complex comorbidities, dementia, and frailty, with the major contributor being polypharmacy (Mangin et al., 2018). Each characteristic alters the risk–benefit balance of medications, typically reducing anticipated benefits and amplifying risk (Mangin et al., 2018). Pharmacogenetic-based clinical decision support tools (DSTs) may offer value for polypharmacy reduction in old age, hence decreases hospitalizations and emergency department attendances (Abbott et al., 2018; Chang et al., 2018).
Effects of computer and internet use on brain health
Internet access has been designated a human right by the United Nations (United Nations General Assembly, 2016). Access to the internet, particularly broadband internet, has significant potential impacts on health outcomes for persons living with dementia and the brain health of aging adults. However, with the rising number of older adults using the internet has come increasing rates of cybercrime and digital exploitation (Iyengar et al., 2019).
The myriad ways that new health technologies can promote better outcomes and innovative care require this platform in order to reach people. While internet utilization among older adults may be driven by education, income level, and other social determinants, internet access is also greatly impacted by these same variables (PRC, 2014). Geography also plays a role in access. Older populations with high disease burdens living in rural areas are particularly at-risk of lacking reliable internet access. The U.S. Federal Communications Commission (FCC) tracks broadband access and prevalence of chronic health conditions such as diabetes and obesity – the so-called “double burden” (FCC, 2017). Their geomapping of these overlapping characteristics demonstrates the stark inequality that exists. A lack of internet access – particularly broadband internet – undermines the very platform needed to run and access new technological innovations, which in turn limits the opportunity to receive care, support, and education that technological innovations offer. Ensuring internet access is widely accessible to all persons as they age is a key step in promoting health innovation and health equity.
Internet use has a number of recognized brain health benefits, including reducing depression, increased health literacy, and increased social engagement, particularly in advanced age (Choi and Dinitto, 2013; Shim et al., 2018). In the past, older adults who used computers regularly were often white, better educated, and wealthier. However, those demographics are changing. A recent study examining the effects of computer use in older adults in and out of the home (e.g. libraries, friend’s homes) found that those who access computers from social resources were more likely to report higher self-efficacy and better self-reported health (Shim et al., 2018). Compared to occasional or never users, regular computer users reported higher self-efficacy, indicating that computer and internet access are associated with more positive views of self by older adults (Cacioppo and Hawkley, 2009). A large study has suggested that self-reported craft activities in late life, and social activities, game playing, and computer use in combined late-life and midlife stages were all linked to a decreased incidence of mild cognitive impairment (MCI) (Krell-Roesch et al., 2019). In late life, a decreased risk of MCI was tied to reading books, playing games, or engaging in craft or social activities at least 2–3 times a month, or using a computer at least 5–6 times a week (Krell-Roesch et al., 2019). Interestingly, only computer use was associated with a significantly decreased risk of developing MCI regardless of when in life computer use was reported (late-life, midlife, or both) (Krell-Roesch et al., 2019).
Internet assessment of brain health and cognitive assessment are growing. The Brain Health Registry (Weiner et al., 2018) uses online strategies to assess cognitive function and refer potential participants to clinical trials. The Alzheimer Prevention Trial (APT) web study uses similar approaches to online assessment with the goal of referring cognitively normal persons to clinical trials for the prevention of AD. The Cleveland Clinic’s healthybrains.org website provides a Brain Heath Index (BHI) based on six pillars of brain health to guide users to more brain-healthy lifestyles (Zhong and Cummings, 2016).
The negative implications of internet usage by older adults is discussed later in this paper.
Social media use and brain health
Social media platforms may have a positive effect by promoting interpersonal connectedness (Boll and Brune, 2016). Numerous studies show that loneliness and social isolation can negatively impact overall health in older adults (Landeiro et al., 2017). Social media platforms such as Facebook and Twitter are known to enhance social connectedness, and a recent Pew Research report showed that about one-third of all adults over age 65 reported using them (Anderson and Perrin, 2017). Given the established relationship between the frequency of supportive interactions with others and the delayed onset of cognitive decline, there are hypotheses that social media may be protective against some forms of dementia (Seeman et al., 2001), although reverse causation may be occurring. A 2018, 34-person, waitlist control trial demonstrated that teaching older adults to use social media improved their executive functioning significantly as measured by their inhibitory control and improved their overall cognition as measured by the Mini-Mental State Examination (MMSE) compared to controls. These data suggested that social media may have impacts on brain health beyond those of social and emotional connection (Quinn, 2018). However, it should be noted that these study findings are limited by a small sample size, a nonstatistically significant improvement in MMSE between baseline and 4 weeks, and a short follow-up period. The study did demonstrate that older adults are capable of effectively learning how to operate these newer technologies given the opportunity to do so, a finding echoed in a 2015 randomized controlled trial assessing the feasibility of using direct to home daily video chats to evaluate for an increase in social engagement in older adults without dementia (Dodge et al., 2015). Not only did the intervention group show greater improvement in tests of language-based executive functions, but adherence in the intervention group was remarkably high: there were no dropouts and the mean percentage of days completed in the 6-week trial was 89% (Dodge et al., 2015). It is an impressive statistic considering the average age of participants was 80.5 years. The chat software used did not require prior knowledge of how to operate a computer (Dodge et al., 2015).
Alternatively, however, social media may have adverse effects for older adults. Loneliness and social isolation can dramatically alter cognitive performance, decision making, and emotional regulation (Cacioppo and Hawkley, 2009). Lonely adults have more difficulty maintaining vigilance and self-regulating and demonstrate a heightened awareness of social threats, as well as paying greater attention to negative social stimuli (Cacioppo and Hawkley, 2009; Hawkley and Cacioppo, 2010). This broad constellation of behaviors likely predisposes older, lonely adults to gravitate toward information on social media that mirrors their own worldview, a trend amplified further by the algorithms of social media platforms that are constructed to keep users on the platforms as long as possible, by showing users content they are most likely to agree with and enjoy. These ideas could explain recent reports showing that individuals over age 65 are seven times more likely to share and disseminate fake news domains on social media than their younger counterparts (Guess et al., 2019). These results are particularly concerning given the increased numbers of aging adults on social media and the fact that political and policy decisions are now often shaped by information publicly available on these platforms. Furthermore, other findings from Guess et al. (2019) suggest that “memory and other cognitive domains deteriorate in some elders in a way that particularly undermines resistance to ‘illusions of truth’ and other effects related to belief persistence and the availability heuristic, especially in relation to source cues (Glisky et al., 2001; Swire et al., 2017)” (page 5). The severity of these issues would hypothetically increase with the prevalence of misinformation and the complexity of the information. This wealth of data demonstrates the overwhelming interest in social media as an influential technological tool of our society and its potential for both therapeutic and negative effects. More research and monitoring are needed to strike an optimal balance. The difficulty of balancing protected free speech and protection from negative effects of social media is an ongoing debate.
Finally, the role of social media in optimizing sociability is nuanced. A recent review (Waytz and Gray, 2018) suggests social media can influence sociability in 3 core ways and these depend on whether it allows a deeper understanding of peoples’ thoughts and feelings. The suggestion is that social media “(a) benefits sociability when it complements already deep offline engagement with others, (b) impairs sociability when it supplants deeper offline engagement for superficial online engagement and (c) enhanced sociability when deep offline engagement is otherwise difficult to attain”. Clearly further exploration of this issue is needed.
Ethical considerations in brain health technological innovation
New and potentially valuable technologies that are targeted toward improving the lives of either patients or caregivers include memory and communication aids, global positioning satellites (GPS) tracking devices, “smart home” technologies, and even companion robots (Landau and Werner, 2012; Majumder et al., 2017; Shibata and Wada, 2011). Although the goals of these technologies have been positive, such as aiming to delay entry into institutionalized care and reduce caregiver burden, the ethical implications of such technologies are only beginning to be studied. Little consideration has been given to how these technologies should be regulated in order to be compliant with human rights obligations or how they should be incorporated into advance care planning while an individual may still have decision-making capacity (Bennett et al., 2017). Although many assistive technologies were developed as a response to the traditionally restrictive means of dementia care (i.e. restraints, medication), these technologies may provide new and unprecedented levels of surveillance, privacy limitation, and movement restriction (Bennett et al., 2017). Even the use of care or companion robots has ethical considerations beyond the obvious benefits of caregiver unburdening, some have argued these robots may eventually devalue care and reduce person-to-person contact with older adults, which would restrict rather than enhance social interaction (Elder, 2015). Furthermore, there are philosophical, ethical, and policy considerations that deserve thoughtful attention when developing assistive technologies for those with dementia (Sharkey and Sharkey, 2012) – how can we balance the need for safety and monitoring against the potential feelings of objectification and lack of control? Is there an element of deception and infantilization created in addition to the potential loss of privacy and personal liberties when technology is responsible for caring and monitoring a human? Are there circumstances under which a person living with dementia should be able to control their own devices?
With middle aged and older adults being among the fastest growing demographics creating social media profiles, ethical issues will undoubtedly arise in concurrence with the pending dementia epidemic (Batchelor et al., 2012). Although the older adults may be registering for profiles while they still have capacity to accept the terms and conditions of a social media account, what happens when they develop dementia and no longer understand the far-reaching implications of their digital footprint (Batchelor et al., 2012)? How can we support digital autonomy while also protecting privacy? Clearly, there is a need to develop and integrate emerging ethicolegal frameworks into new technologies and innovation diplomacy in order to protect and promote brain health in the most vulnerable populations.
Introducing the BIND model
BIND aims to improve global brain health outcomes by leveraging technological innovation, entrepreneurship, and innovation diplomacy. Improving outcomes may arise from optimization of access to care, prevention, screening, diagnosis, treatment, and treatment outcome tracking. It acknowledges the key role that technology, entrepreneurship, and digitization will play now and in the future of brain health for individuals and societies alike. It strengthens the positive role of novel solutions (e.g. “omics,” neuroimaging, digital tools, sensors, internet-based platforms, virtual reality, and augmented reality) and recognizes and works to manage the potential and real risks of digital platforms. It also recognizes the political, cultural, and economic influences that brain health technological innovation and entrepreneurship has in the 21st century.
Economic influence is derived from direct investment into brain health-related technologies. It is also derived from the recognition of the economic and productivity impact of brain health disorders. Cultural influences may emerge and develop as BIND advocates for enhanced brain health care equity, destigmatization, and socioeconomic inclusion for people with brain health issues. In addition, human rights violations, e.g. force restraints, physical and sexual violence, and torture (in community or institutional settings in LMICs or HICs), may be reduced with greater awareness and education around brain health. With a greater engagement of the private sector and trade and investment linkages for global brain health innovation, avenues for cross-cultural understanding and improvement of brain health care will be scaled up. Figure 1 provides a graphical representation of the model.
Figure 1.
Foundational Disciplines of Brain health INnovation Diplomacy. BIND aims to improve global brain health outcomes by leveraging technological innovation, entrepreneurship, and innovation diplomacy. BIND incorporates insights from traditional as well as emerging disciplines.
Traditional disciplines of brain health diplomacy
Brain health diplomacy draws insights from the disciplines of global brain health, health diplomacy and science diplomacy. Below we provide a summary of these disciplines and describe frameworks for developing practitioners in these fields.
Science diplomacy
Science diplomacy is a field which uses science as an instrument to achieve foreign policy objectives that serve to promote peace, sustainable development and ethical research. It leverages “science” as a process and way of communicating, as well as the research outcomes (UNESCO, 2018).
A major source of capacity building for science diplomacy was established in 2008, when the American Association for the Advancement of Science established the Center for Science Diplomacy (AAAS, 2020). The Center is a leader in positioning science diplomacy as a key aspect of 21st century science and international affairs. The Center has strengthened engagements between the scientific and diplomatic communities and developed the framework and training to support the practice of science diplomacy. Importantly, it has shown how science can work to strengthen relationships between countries when geopolitical strains are apparent. A range of education and capacitybuilding programs for early career academic innovators are outlined by Holford and Nichols (2018).
Health diplomacy
Health diplomacy is a field that merges the disciplines of public health, management, international affairs, economics, and law, with a focus on negotiations that impact the global public health policy (WHO, 2018).
There are three levels of health diplomacy that have been formally postulated, as “core”, “multi-stakeholder”, and “informal” (Brown et al., 2014; Katz et al., 2011). Each level has varying actors, tools, roles, and levels of accreditation.
“Core” health diplomacy practitioners are officially accredited “Health Attachés” charged with connecting public health organizations in one government to public health and related organizations in another government (e.g. departments of innovation, science, industry, aging, trade and investment, and social services). “Health Attachés” require formal credentialing which involves obtaining agreements between two state Foreign Affairs Ministries.
“Multi-stakeholder” health diplomacy practitioners include government employees and multilateral representatives.
“Informal” health diplomacy includes host country officials as well as a wide array of other stakeholders including universities, non-governmental organizations, private enterprises, and the general public.
Global brain health
Global brain health aims to protect the global aging populations from risks and threats to brain health (e.g. dementia and stroke) (AARP, 2019; GBHI, 2019). The field aims to collaborate in developing and expanding preventions and interventions, share knowledge and engage in advocacy for all of the major neurodegenerative disorders of late life.
In 2019, the AARP (formerly known as the American Association of Retired Persons) established the Global Council on Brain Health (GCBH). The GCBH is an independent collaborative, created to provide trusted information on how individuals can maintain and improve their brain health (AARP, 2019). The GCBH states a primary goal of supporting consumers to apply the latest scientific advances to boost their brain health and optimize their quality of life.
Emerging disciplines informing BIND
With the growth of technological innovation and entrepreneurship in brain health there is a need to incorporate emerging disciplines into standard working models that are adapted to address the likely brain health challenges in the 21st century. An overview of these emerging disciplines is presented below.
Precision medicine
The clinical neurosciences have been transformed by embracing precision medicine and systems biology. Leveraging such models has helped to facilitate novel care solutions for proteinopathies, neurodegenerative disease (such as AD), protein misfolding disorders, and other dementias (Hampel et al., 2018). Development of treatments targeted to the needs of specific individuals are conceived on the basis of technologies using “multi-omics” inputs from genomics, epigenomics, connectomics, lipidomics, proteomics, metabolomics, digitomics, and phenomics. These new treatments may include novel drug compounds, pharmacogenomic strategies, or other companion diagnostics (such as neuroimaging biomarkers) (Hampel et al., 2018). Such strategies also help to illuminate novel pathophysiological mechanisms and help refine staging and classification of disease. (Hampel et al., 2018). This discipline is of course most relevant in HICs, as opposed to LMICs.
Digital health
Digital health describes a field that leverages digital technologies (e.g. hardware and software) as tools for optimizing screening, diagnostics, treatment, and prevention of health disorders (DMS, 2019). Digital technologies may assist in driving efficiencies within the health care ecosystem (e.g. in various settings including inpatient, outpatient, home, and community) (Coravos et al., 2019).
Digital health solutions can be used stand alone or in “companion” with pharmaceuticals, biologics, devices, or other products. Digital health facilitates patient and health care provider empowerment with data and can be used in public health/epidemiological projects. Digital biomarkers aka “digitomics” can be examined in parallel with other biological, environmental, and lifestyle factors to deliver previously unavailable insights into disease states, their development, and treatment.
Convergence medicine
Convergence science in medicine, ala convergence medicine, involves leveraging convergence or transdisciplinary science in order to achieve improved outcomes for patients and health care systems. This means robust integration of scientists, clinicians, bioinformaticists, global health experts, engineers, technology entrepreneurs, medical educators, caregivers, and patients (Eyre et al., 2015b; Eyre et al., 2017). Convergence medicine will be realized when there is an abundance of clinical tools in use leveraging convergence science.
Innovation diplomacy
Innovation diplomacy involves the use of diplomacy to further innovation for a country, as well as leveraging innovation to improve the relations among countries in bi-, multi-, or transnational settings (Miremadi, 2016). Innovation diplomacy includes supporting partnerships with industry, academic, and nongovernmental organizations; supporting open innovation and collaboration; shaping intellectual property rights, ethical regulation, and use of technology; structuring global value chains; as well as developing, deploying, and scaling innovative solutions to global problems (Leijten, 2017). These practices sit somewhere between science diplomacy (mentioned previously) and economic diplomacy, which focus on trade, investment, and international regulations (Leijten, 2017).
Technology diplomacy
Technology diplomacy acknowledges “the key role that technology and digitalization will play now and in the future for individuals and societies alike and notes the tech industry’s political and global influence” (Udenrigsministeriet, 2019). The “TechPlomacy Initiative,” launched by the Danish government in 2017, suggests “technology will contribute to solving some of the most acute global challenges and bring about a positive transformation with enormous potential for people around the world” (Udenrigsministeriet, 2019).
The Danish government established a “Tech Ambassador” Office between Silicon Valley (California, USA), Copenhagen (Denmark), and Beijing (China) (Udenrigsministeriet, 2019). With a global mandate to rethink traditional diplomatic representation, the Tech Ambassador functions to develop strategic partnerships with entrepreneurs and executives, tech ecosystems and hubs, biotechnology organizations, governments, international organizations, civil society, cities, regions, and universities. Relevant initiatives include security, cyber, biotechnology, development, export, and investment promotion. Opportunities and challenges arising with this technology agenda are then also addressed in relevant and complementary bi-, multi-, and transnational fora.
Consumer participation
Consumer participation is a contemporary approach and may take place through research, policy, ethics discussions, clinical care, or novel solution development. Indeed, consumers are already involved in managing their own health through the use of smart devices, the internet as a source of information, and social networks to share ideas and organize (Sagner et al., 2017).
A key outcome for the brain health field is novel solution development that appropriately focuses on end user needs by incorporating consumer contributions to both product design as well as testing. Validation of new technologies prior to their implementation can be difficult through current research practices; however, consumers can help expand research practices by identifying the highest-priority questions to answer, advocating for necessary resources, and influencing the design of models for joint clinical decision making. As both research subjects and the ultimate beneficiaries or users of new technologies, consumers also have a critical perspective on ethical issues unique to brain health.
A useful example of consumer participation comes from the field of bipolar disorders. Community-based participatory research (CBPR) leverages the lived experience of bipolar disorder, inviting consumers to act as coinvestigators rather than merely test subjects. Research priorities are dictated by the needs of the community, resulting in relevant, timely, and applicable findings that reciprocally benefit the community by improving mental health literacy, treatment planning, treatment adherence, and stigma reduction (Michalak et al., 2016).
Forums such as PatientsLikeMe are a repository of health data shared by patients, enabling learning from shared experiences, unlike generalized and nonspecific information available on traditional health information websites (PatientsLikeMe., 2017). Online patient communities can facilitate screening and recruitment of patients into studies, transcending the conventional method that relies on treating clinicians. Not only is there a dataset that can be readily accessed, this method may also offer greater study exposure and more diverse sample populations. The overarching message is that consumers can and do contribute to research and that existing platforms can be utilized to support the process.
Introducing a working model for the roles of BIND practitioners
In this rapidly emerging field, it is important to conceptualize the toolkit for BIND practitioners. Table 1 outlines roles relevant to BIND practitioners. These roles are developed from the real-world experiences of the authors, understandings of the foundational disciplines of BIND, and use of the adapted UK-based innovation foundation, NESTA’s Innovation Toolkit for iDiplomats (Bound and Saunders, 2018).
Table 1.
Roles relevant to Brain health INnovation Diplomacy practitioners
| EXPLORING AND ASSESSING | INFLUENCING AND PROMOTING |
CULTIVATING AND CONNECTING |
ADVOCATING AND SUPPORTING |
ACTIVATING AND SCALING |
|---|---|---|---|---|
|
|
|
|
|
Adapted from the UK-based innovation foundation, NESTA’s Innovation Toolkit for iDiplomats (Bound and Saunders, 2018). This adaptation involved modification to frame relevant to brain health, as well as the inclusion of “Advocating and Supporting” as a new category.
Examples of BIND projects
There is a range of existing projects that further the goals of BIND and could be seen as useful models to develop new programs in the future. These projects are outlined in Table 2.
Table 2.
Examples of Brain health INnovation Diplomacy projects
| BRAIN HEALTH INNOVATION DIPLOMACY PROJECT | POTENTIAL MEASURABLE OUTCOMES |
|---|---|
World Young Leaders in Dementia (www.wyldementia.org): The World Young Leaders in Dementia (WYLD) is a network of passionate, young clinicians, researchers, advocates, artists, and entrepreneurs working across disciplines and borders to develop innovative dementia solutions. Membership represents over 300 engaged individuals under the age of 40, covering 30 countries across six continents. WYLD emerged from a series of legacy meetings following the 2013 G8 Dementia summit. The UK Science & Innovation Network invited emerging leaders working in diverse fields of dementia to meet at events held in Ottawa, Tokyo, Washington DC, and London. In March 2015, a draft a set of proposals was presented at WHO’s First Ministerial Conference on Global Action Against Dementia. This process sparked a number of new research collaborations and creation of the WYLD network. Together, WYLD will create a better world for those living with dementia, their families, and their communities. WYLD aims to do this by: Bringing creative brainstorming, fresh perspectives, and novel solutions to the dementia field.
|
|
| Centre for Aging and Brain Health Innovation (https://www.cabhi.com/): CABHI is a unique collaboration of health care, science, industry, not-for-profit and government partners whose aim is to help improve quality of life for the world’s aging population, allowing older adults to age safely in the setting of their choice while maintaining their cognitive, emotional, and physical well-being. The mission is to accelerate: development, validation, commercialization, dissemination and adoption of innovative products, services and best practices to support brain health and aging. |
|
| US Against Alzheimer’s (https://www.usagainstalzheimers.org/): UsAgainstAlzheimer’s is an innovative nonprofit organization demanding – and delivering – a solution to Alzheimer’s. Driven by the suffering of millions of families, UsAgainstAlzheimer’s presses for greater urgency from government, industry, and the scientific community in the quest for an Alzheimer’s cure—accomplishing this through effective leadership, collaborative advocacy, and strategic investments. |
|
| Aging 2.0 (www.aging2.com): Aims to accelerate innovation to address the biggest challenges and opportunities in aging. Aging 2.0’s international, interdisciplinary and intergenerational community has grown to 40 k + innovators across 20 + countries. The volunteer-run chapter network, which spans 80 + cities, has hosted more than 550 events around the world. Aging 2.0 is run by a team out of San Francisco, California and Chapter Ambassadors in more than 80 cities around the globe. |
|
iSupport is the World Health Organization’s E-Programme for Carers of People Living with Dementia (WHO, 2019b):It is an online knowledge and skills training program for carers of people with dementia. iSupport aims to prevent and/or decrease mental and physical health problems associated with caregiving and to improve the quality of life of those caring for people with dementia. iSupport covers the following topics:
|
|
| International Genomics of Alzheimer’s Project (IGAP) (https://consortiapedia.fastercures.org/consortia/igap/): The aim of the IGAP consortium is to discover and map the genes that contribute to Alzheimer’s disease (AD). The effort spans several consortia focused on AD and includes universities from Europe and the U.S. The goal is to create a shared resource database that includes genetic data for the more than 40,000 individuals with AD. Launched in 2011, initiating organizations include European Alzheimer Disease Initiative, Alzheimer’s Disease Genetics Consortium, Genetic and Environmental Risk in Alzheimer’s Disease, and Cohorts for Heart and Aging Research in Genomic Epidemiology |
|
Mayo Clinic Neuroscience Convergence Course, November 7–9, 2019 (https://ce.mayo.edu/neurology-and-neurologic-surgery/content/neuroscience-convergence-2019). This course has a number of core aims:
|
|
Global Brain Health Institute (GBHI) (www.gbhi.org): Funded by Atlantic Philanthropies and based between the University of California, San Francisco and Trinity College Dublin, the GBHI works to reduce the scale and impact of dementia around the world by training and supporting a new generation of leaders to translate research evidence into effective policy and practice. Atlantic Fellows hail from all over the world and comprise a diverse array of professions including medicine, law, business, social science, journalism, and the arts. Examples of current and former Atlantic Fellows’ projects are as follows:
|
|
| World Wide Fingers (http://wwfingers.com/): An interdisciplinary network to share experiences, harmonize data, and plan joint international initiatives for the prevention of cognitive impairment/dementia. Its main goal is to generate robust evidence to define effective preventive approaches for various at-risk groups and settings. World Wide FINGERS will facilitate synergistic use of data from several countries, creating a unique opportunity for rapid knowledge dissemination and implementation. |
|
| Neuroscape (https://neuroscape.ucsf.edu/): A translational neuroscience center at University of California, San Francisco involved in research and development of cutting-edge technologies to optimize brain assessment and optimization. The center provides state-of-the-art development studios and research facilities to transform neuroscience research into real-world solutions. Their mission is to use modern technology and a wide range of industry partners to harness the brain’s plasticity to ultimately enhance cognition and improve brain function. Neuroscape believes that partnerships with private companies serve as bridges between academia and industry, with the goal of more rapidly accelerating advances in science, education, and medicine. |
|
Center for the Future of Aging, Milken Institute (https://www.milkeninstitute.org/centers/center-for-the-future-of-aging): The mission is to improve lives and strengthen societies through the promotion of health purposeful aging and by:
|
|
| The Global Council on Brain Health (GCBH), AARP and Age UK, (https://www.aarp.org/health/brain-health/global-council-on-brain-health/about-us/): An independent collaborative of scientists, health professionals, scholars, and policy experts from around the world working in areas of brain health related to human cognition. GCBH will operate as a hub-and-spoke collaborative to address the many factors that can impact brain health. Debate the latest advancements in brain health scientific research to reach consensus on what works. Seek to translate critical scientific information on brain health into simple actions people can take. |
|
| Dementia Discovery Fund (https://theddfund.com/): The world’s largest venture capitalist fund focused entirely on developing and discovering new therapies for dementia. Over the 15-year life of the fund, there is a mandate to validate novel hypotheses and expand the breadth of target mechanisms in dementia development. The DDF has raised over £250 million while investing in diverse technologies targeted toward new disease-modifying drugs and also attempting to meet other clinical needs such as relieving symptomatic burdens of illness and improving quality of life. |
|
| BrainMind (https://www.brain-mind.org/): BrainMind is a platform and private community of brain scientists, entrepreneurs, philanthropists, investors, and academic institutions dedicated to impactful innovation of brain science. It seeks to coordinate talent from the entrepreneurial community with capital from the philanthropic community to deliver stewardship of neuroscience to impact focused stakeholders. By using the principles of “gather, curate, cultivate,” it brings together a powerful community of diverse and motivated leaders interested in changing brain science to establish a roadmap for an effective way forward. The platform recognizes areas in brain science research that are under supported relative to their impact and provides high consciousness capital and leadership to grow and scale these innovations to ultimately benefit society. |
|
KAER Toolkit from the Gerontological Society of America (http://www.geron.org/kaer): Focused on the KAER model developed by the GSA Workgroup on Cognitive Impairment Detection and Earlier Diagnosis. The workgroup identified valuable tools and resources to implement the four steps in the KAER model. The resulting toolkit provides options for each of the steps so that primary care providers (PCPS), health plans, and health care systems can select the approaches and tools that fit best with their existing primary care structure, organization, and procedures. The toolkit is broken down by each section of the KAER model to allow quick and easy access:
|
|
| The McLean Technology and Aging Lab (http://www.geropsychtech.org): The Technology and Aging Lab at McLean Hospital in Belmont, MA, is research and clinical unit focused exclusively on studying how newer technologies can impact care for older adults with dementia and psychiatric illness. The lab studies both digital diagnostics and therapeutics and its work spans multiple technological domains including artificial intelligence, passive sensing, wearable devices, virtual reality, and wearable devices. The lab lays special focus on the process of integrating technology into patient care and developing outcomes that can capture how digital tools impact clinical decision making. In addition to its intramural activities, the lab conducts collaborative research and consultation with companies and academic institutions around the world, including projects in India, Norway, and Ecuador. |
|
| The Oregon Center for Aging and Technology (ORCATECH; https://www.ohsu.edu/oregon-center-for-aging-and-technology): Is a multidisciplinary organization that is transforming clinical research by developing and implementing leading-edge technologies that measure life’s data in real time. ORCATECH specializes in: Medical technology consultation, design, and development; Technology-based medical trial consultation and coordination, from focus groups to field-testing; high-resolution data handling and analysis. |
|
The below table contents are derived from project-related websites and referenced accordingly.
Complex technological issues justifying the need for, and value of, BIND
There are a range of complex technology-related issues which we believe justify the need for, and value of, BIND. For example, a recent paper highlighted key issues slowing the pervasive use of computing technology in aging (Kaye, 2017). Core issues noted were lack of appreciation for computing technology providing therapeutic benefits in aging, lack of evidence-based technologies, and lack of sustaining investment in the field. BIND is uniquely positioned to understand and integrate these issues, their business drivers, and current regulations. Such knowledge will therefore help to optimize the effects of these platforms on brain health. In Table 3, we outline these issues and how BIND is uniquely placed to address them.
Table 3.
Complex technological issues justifying the need for and value of Brain health INnovation Diplomacy
| EXAMPLES OF BRAIN HEALTH ISSUE |
DESCRIPTION | FACTORS SUPPORTING THE DEED FOR AND VALUE OF BHIND |
|---|---|---|
| Cyber issues for older adults |
Cybercrime: The yearly cost of cybercrime theft on vulnerable older adults in the USA is approximately $40 billion (Hall et al., 2016). According to the US Federal Bureau of Investigation (FBI) (FBI, 2019), many factors contribute to vulnerable older adults being major targets of cybercriminals. These include:
|
Increased cybersecurity education for vulnerable populations is necessary to protect those who are vulnerable from cybercrimes and increase awareness of suspicious websites (Iyengar et al., 2019). Increased individual protections for victims and increased prosecution against perpetrators are also necessary. Optimized digital literacy is also key. |
| Medical data hacking: As electronic technologies in health care are increasingly prevalent around the world, there are major concerns relating to the security of health care data, biobank data, and devices. There are many examples of major hacks/breaches of large health systems and their data. To further complicate matters, there is increased connectivity to existing computer networks by medical devices, smart phones, hence creating more cyber vulnerabilities The health care industry is seen as an easier target for cybercrime given (1) it is a rich source of valuable data and (2) defences are weak compared to other industries. Breaches and hacks can reduce patient trust, disrupt health system and their services, and threaten lives (Coventry and Branley, 2018). | Cybersecurity is an integral part of patient safety and treatment. Legislation and regulations at the country and global level are critical to minimizing these risks. | |
| Issues around direct to consumer genetic testing | Many people worry about Alzheimer’s disease. Physicians often face questions about the patient’s risk to develop Alzheimer’s disease. The Memory and Aging Center of the University of California, San Francisco, has developed a report titled “Ordering Genetic Testing” (MAC, 2017). In this report they outline: “although APOE testing is clinically available, it is not advised. Direct-to-consumer APOE genotyping is also not advised (Goldman et al., 2011). APOE is a susceptibility gene, not a deterministic one. If your patient wishes to pursue APOE genotyping despite recommendations to the contrary, consider referring to a genetic counselor. Genetic counselors who are knowledgeable about dementia can provide counseling and education to your patients.” (page 2). | Education is required for clinicians and consumers alike. Furthermore, regulatory agencies must be aware of the dynamics in this market. |
| Loneliness may reinforce social media bubbles for older adults | Recently, a review (Ghosh and Iyengar, 2019) demonstrated that “‘lonelier adults exhibit declines in their ability to self-regulate, a heightened awareness of social threats in their environment, a greater attention towards negative social stimuli. and a reappraisal of negative interactions in the service of preserving one’s self esteem’. It then went on to note, “this constellation of behaviors is noted as seeking to avoid conflict and minimize disappointment, hence individuals are more likely to source information that mirrors their own worldview thereby maintaining a sense of self”” (Ghosh and Iyengar, 2019). | Clearly this is an area that requires close attention and awareness from consumers, family, social services, and regulatory agencies. |
| Lack of privacy policies for health apps focused on dementia | Little is known about how well these health care applications “apps” protect user health-related data. A recent systematic analysis of all iPhone-based apps focused on dementia revealed significant issues about the privacy policies clarity and the lack of policies offered (Rosenfeld et al., 2017). Seventy-two apps were found and only 33 (46%) had an available privacy policy. Nineteen of the 33 with policies (58%) were specific to the app in question, and 25 (76%) specified how individual user as opposed to aggregate data would be handled. Among these, authors noted there was a preponderance of missing information, the majority acknowledged collecting individual data for internal purposes, and most admitted to instances in which they would share user data with outside parties. | Increased consumer protections are necessary to protect patients using dementia apps. Legislation and regulations at the country and global level are critical to Improving privacy policies and hence facilitating more trust in these apps. |
| Emergence of cognitive training digital programs | In 2014, experts from the neurocognition community came together to develop a consensus on the brain training industry. This work was led by the Max Planck Institute for Human Development and Stanford Center on Longevity (NASA, 2018). The consensus stated “We object to the claim that brain games offer consumers a scientifically grounded avenue to reduce or reverse cognitive decline when there is no compelling scientific evidence to date that they do. The promise of a magic bullet detracts from the best evidence to date, which is that cognitive health in old age reflects the long-term effects of healthy, engaged lifestyles. In the judgment of the signatories below, exaggerated and misleading claims exploit the anxieties of older adults about impending cognitive decline. We encourage continued careful research and validation in this field.” | Increased awareness by clinicians and those of the public that brain training games are not ultimately solely protective against cognitive decline. Brain training should be implemented as part of a healthy mental and physical lifestyle. |
| Access to broadband Internet | Many people lack access to reliable internet access across the globe. This is particularly true of older adults – particularly for those of low socioeconomic status and lower education levels (PRC, 2014). This is an issue of health equity. If knowledge, care, services, and interconnections with others – all important ways of supporting brain health – are increasingly accessed and delivered through the internet (particularly broadband), but populations at a higher risk of dementia are disproportionately unable to access it, then this is major technological challenge that Brain health INnovation Diplomacy could help to mitigate. |
Legislation that supports access to broadband internet particularly for aging populations at higher risk of developing dementia is both a national and global policy imperative. |
Recommendations
To increase the value and practice of BIND, measurable outcomes, training, and education should be developed and scaled up. We provide the following recommendations to support the emergence and growth of this field.
Involve consumers in brain health innovation design, research, ethics, and advocacy
Individuals with brain disorders (and those at risk) should be involved in research, policy, advocacy, ethics discussions, clinical care, and novel solution development. This reflects Alzheimer Europe’s position on patient and public involvement (PPI) in the context of dementia research (Gove et al., 2018). Novel solution development should focus on end-user needs, and patients can make valuable contributions to product design and testing. Validating new technologies prior to implementation can be difficult through current research practices, but consumers can help expand research practices through research prioritization, resource advocacy, as well as through exploring models for joint clinical decision making. Patients also have an invaluable perspective on ethical issues unique to innovative brain health technologies as both research subjects and the ultimate beneficiaries of new technologies (Arandjelovic et al., 2019; NSTC, 2019). The definition of “patients” is evolving as the neurodynamics of dementia is increasingly shown to begin decades prior to onset of cognitive decline, implying that interventions must similarly begin earlier in life and involve advocacy by healthy at-risk individuals (Brookmeyer et al., 2018).
Construct BIND training opportunities
Education and training opportunities are critical to developing the field of BIND. These opportunities must be relevant to the various stakeholders including clinicians, scientists, policymakers, technology executives, innovators, philanthropists, and diplomats. Moreover, education and training must be relevant across the training spectrum from early to late career. Examples of education and training could include incorporating innovation into school curricula, offering fellowship opportunities in brain health innovation for post-graduate trainees, and creating certificate programs for clinicians or researchers. We propose that to optimally support BIND, brain health technological innovation and entrepreneurship engagements should occur in interdepartmental environments in universities. This should include departments of neurology, psychiatry, geriatrics, regulatory science, psychology, sociology, politics, public policy, public health schools, law schools, business schools, international studies programs, and design schools. Table 4 outlines potential methods of incorporating components of BIND into education programs.
Table 4.
Methods of incorporating components of Brain health INnovation Diplomacy into educational programs
| TARGET OF EDUCATION |
EXAMPLE OF GENERIC TRAINING PROGRAM | POTENTIAL TO TAILOR TO BRAIN HEALTH INNOVATION DIPLOMACY |
|---|---|---|
| Undergraduate college students | iDiplomats Program, Innovation Initiative, Massachusetts Institute of Technology’s (MIT) (MIT, 2019): This program involved providing undergraduate students with skills on how to represent MIT in various international ecosystems, analyze innovation ecosystems, and engage key stakeholders who can help take innovation from early stages to final products: entrepreneurs, risk capital providers, government policymakers, universities, and corporations. Participants receive a stipend for travel and expenses, as well as academic credit. Upon returning to MIT, they write reports on their regions’ innovation ecosystems. | This program could be tailored to focus on brain health-related innovations occurring in various countries. |
| Hacking for Diplomacy, Stanford University (http://web.stanford.edu/class/msande298/): Hacking for Diplomacy is an undergraduate class that allows students to address real-world foreign policy challenges by using innovative research and technology methods. Students learn how to apply “Lean Startup” principles (“Mission Model Canvas”, ”Customer Development,” “Agile Engineering”) to create and validate agency and user needs to continually build iterative prototypes to test understanding of the problem and solution. Teams of students use a hands-on approach that facilitates close engagement with officials in the U.S. State Department and other civilian agencies. | ||
| Medical students | Psyc 240: Leadership and Innovation in Mental Healthcare, Stanford University (Stanford, 2019): The country’s first university course on mental health innovation. The course included a diverse group of students from multiple faculties including Stanford’s School of Medicine, Graduate School of Business, Law School, School of Engineering, School of Education, and College. Students learn about mental health, care delivery, technology, and startups. They apply frameworks to assessing the impact of current innovations and developed their own ideas for solving mental health problems. They are paired with faculty to improve the clinical validity and marketability of the idea. | This program could be tailored to brain health and by also including international affairs students and practitioners. |
| Medical Residency | Digital Health Elective, Yale Department of Psychiatry Adult Residency Program: This course provides residents an opportunity to explore innovative digital health solutions and their role in clinical care. Topics range from telepsychiatry and text-based therapy to digital CBT and mobile applications designed to treat behavioral health diagnoses. By the end of the elective (during the 3-month research rotation for second-year residents or as a half-day 6 or 12 month course for third-year and fourth-year residents), residents will produce and submit at least one submission for a peer-reviewed publication relevant to the field of digital health. | This elective could include global digital brain health initiatives in its research to better serve Brain health INnovation Diplomacy purposes. |
| Early Career Academic Investigators | Science Diplomacy Dialogue Series, Science Diplomacy Center, The Fletcher School, Tufts University (Tufts University, 2019): The diplomacy dialogue series includes discussions on Globally Interconnected Civilization, Informed Decision Making for Sustainability, The Arctic Case Study, Capstone Project Enhancement with Holistic Integration. The series aims to educate on theory and practice of science diplomacy and participate in discussions about how to incorporate both natural and social sciences into foreign policy decision making and international negotiations. | This program could be tailored toward brain health issues |
| Innovation to Impact Program for Substance Use Researchers at Yale University (http://www.innovationtoimpact.com): Because substance use is an underserved and heavily stigmatized area of growing concern, Yale Psychiatry faculty developed a program to help researchers translate their insights into better clinical treatments for substance use. The program runs an annual innovation bootcamp to train researchers in the principles of entrepreneurship and innovation. It then provides mentorship and seed funding to innovators to help them launch substance use innovations that measurably impact patients struggling with substance use disorder. The program is funded by the National Institute of Drug Abuse (NIDA). | This program’s curriculum could further incorporate principles of BIND by addressing how to destigmatize substance use in the eyes of the general public and of investors. | |
| Psychiatrists, neurologists, psychologists and other brain health clinicians | Recommendations for Value-driven Innovation in Global Mental Health Training, Society for the Study of Psychiatry and Culture: Developed during an interdisciplinary discussion during the annual meeting (Kohrt et al., 2016). Priority values included humility, stakeholder engagement, ethical awareness of power differentials, collaborative action, and “deep accountability” when working in low-resource settings in low- and middle-income countries and high-income countries. Competencies included flexibility and tolerating ambiguity when working across diverse settings, the ability to systematically evaluate personal biases, historical and linguistic proficiency, and evaluation skills across a range of stakeholders. Training experiences included didactics, language training, self-awareness, and supervision in immersive activities related to professional or academic work. | These programs could be tailored to focus on brain health (which GBHI is) and by including extensive entrepreneurship and innovation diplomacy teachings. |
| Atlantic Fellow in Global Brain Health, Global Brain Health Institute, UCSF and Trinity College Dublin (https://www.gbhi.org/programs): The Atlantic Fellows for Equity in Brain Health program provides innovative training in brain health, leadership, and dementia risk reduction to a broad array of promising leaders from various professions, including medicine, science, business, law, journalism, social science, and the arts. Through their work, fellows are expected to emphasize local and global health inequities that need to be addressed by practitioners and policymakers, with the goal of transforming local communities around the world. Atlantic Fellows join the program for 12 months and have a base at the University of California, San Francisco or Trinity College Dublin. A core curriculum of weekly courses in economics, epidemiology, law and ethics, leadership, neuroscience, public policy, and statistics constitutes part of the experience. They also have opportunities to work with individuals with cognitive disorders. | ||
| Leadership in Mental Health Short Course, Sangath Institute, Goa, India (http://www.sangath.in): The Leadership in Mental Health (LMH) course aims to equip participants with methods to develop and scale-up interventions for mental health in resource-constrained settings. It also aims to augment leadership skills needed to scale-up mental health care programs and promote the human rights of people with mental illness. The course has been widely accepted globally, and since its inception, over 400 participants from around the world, including Nepal, Afghanistan, Sri Lanka, Vietnam, Cambodia, Germany, United States, Canada, Japan, Brazil, Peru, China, Zambia, Liberia, and Kenya have attended the course. | ||
| Corporations | Johnson & Johnson Mental Health Diplomats Program (https://www.jnj.com/tag/mental-health-diplomats): Founded in April 2017, the Mental Health Diplomats Program was initially conceived to help reduce workplace mental health stigma and creative a supportive workplace environment through personal empowerment programs and leadership trainings for employees of Johnson & Johnson. It has since become one of the fastest growing new employee resource groups with over 1000 employees in 32 countries and over 350 trained in mental health first aid. Johnson & Johnson has since gone on to cofound citiesRISE, which is a global platform dedicated to changing the state of mental health care policy and practice to better serve the needs of populations across the world. | These programs could be tailored to focus on brain health. |
| General Programs | MIT Hacking Mediicne (http://hackingmedicine.mit.edu/): The Massachusetts Institute of Technology Hacking Medicine (MIT HM) team is a student, academic, and community-led group that developed and pioneered the hackathon methodology in 2012 specifically for health, using systems-oriented design thinking to address challenges in health and medicine 30. The MIT HM methodology has employed this process toward over 100 events in over 20 countries in both low-resource and high-resource settings and continuously refined this methodology over the past 6 years. Over the past 6 years, over 40 companies have been created out of HM events, collectively raising over $150M in funding. An MIT HM hackathon comprises four stages: (1) problem identification, (2) team formation, (3) solution conception, and (4) iteration and implementation. | These programs could be tailored to focus on brain health. |
The below table contents are derived from project-related websites and referenced accordingly.
Advance global policy change through
BIND
BIND must actively engage with national and global policymakers. Building on the strengths and expertise of existing programs and partnerships, there is an opportunity to become the go-to trusted resource of knowledge and expertise on all matters related to brain health innovation to whom policymakers will turn to during the decision-making process.
A global forum where a consensus of policy ideas (such as a white paper) is agreed on would be one possible approach to help facilitate this. Policymakers as well as intragovernmental organizations (such as the WHO) must be invited to participate in this forum. The translation of these consensus recommendations to policymakers is essential to their implementation and success. Making this connection will require active engagement of the BIND community. This would include active advocacy to address the issues identified within the consensus agreements. This will help bring recommendations for brain health innovation to the forefront of national and global policy agendas. This requires consensus building and stakeholder engagement so that a coalition of relevant stakeholders will support any recommendations made. A visible role within the policymaking process – as experts, innovators, and advocates – is needed.
Develop measurable outcomes to track
In developing the BIND model, it is critical to also envisage measurable outcomes to track the value of the model. In Table 2 and Figure 2, we have outlined potential measurable outcomes for BIND projects.
Figure 2.
Potential Measurable Outcomes of Brain health INnovation Diplomacy-Related Activities.
Conclusions
BIND is a novel model that, if operationalized effectively, can bring about positive changes through its role in economic and cultural influence. The field will continue to grow in importance as advances in data analytics, “omic” analyses, and more ubiquitous and affordable use of smart devices are coupled with increasing globalization and decreasing brain health stigma in the modern world.
Acknowledgments
Conflicts of interest
HE reports ownership of shares in CNSdose LLC. HL has a research grant from Allergan. JC has provided consultation to Acadia, Actinogen, Alkahest, Allergan, Alzheon, Avanir, Axsome, BiOasis, Biogen, Bracket, Cassava, Cerecin, Cortexyme, EIP Pharma, Eisai, Foresight, Genentech, Green Valley, Grifols, Hisun, Merck, Otsuka, Resverlogix, Roche, Samumed, Samus, Takeda, Third Rock, Toyama, and United Neuroscience pharmaceutical and assessment companies. SD reports consultation for Amgen, Acumen, Biogen, Cognition Therapeutics. WD reports ownership of shares in Insights to Illuminate LLC. IV receives research funding from the Once Upon a Time Foundation. JK receives research support from the NIH (U2C AG054397, P30 AG008017, P30 AG024978, R01 AG051628, R01 AG051628, U01 AG010483) and Merck; directs centers at Oregon Health & Science University that receives research support from the NIH, CDC, National Science Foundation, the Department of Veterans Affairs, AbbVie, Novartis, Kyowa, Glovia, and Eisai; is (or has been in the last 36 months) compensated for serving on Data Safety Monitoring Committees for Eli Lilly and Suven; is compensated for serving on the Scientific Advisory Board for Sage Bionetworks; receives reimbursement through Medicare or commercial insurance plans for providing clinical assessment and care for patients; and serves on the editorial advisory board and as Associate Editor of the journal, Alzheimer’s & Dementia and as Associate Editor for the Journal of Translational Engineering in Health and Medicine. The other authors have no conflicts of interest to declare.
Source of funding
HL reported grant support by NIH grant AT009198. JC was supported by KMA and NIGMS grant P20GM109025. SD reported grant support from NIA AG047266 and the Ed and Ethel Moore Alzheimers Disease Research Program, State of Florida. AI was partially supported by grants GBHI ALZ UK-20639295, NIH/NIA R01 AG057234, CONICET, FONCYT-PICT (2017-1818, 2017-1820), CONICYT/FONDECYT Regular (1170010), FONDAP 15150012, the INECO Foundation, and the Interamerican Development Bank. JK reported grants including the following from NIH: U2C AG054397, P30 AG008017, P30 AG024978, R01 AG051628, R01 AG051628, U01 AG010483, Merck Investigator Study Program.
References
- AAAS (2020). Center for Science Diplomacy. Available at: https://www.aaas.org/programs/center-science-diplomacy.
- AARP (2019). Global Council on Brain Health. Available at: https://www.aarp.org/health/brain-health/global-council-on-brain-health/.
- Abbott R, Chang DD, Eyre HA, Bousman CA, Merrill DA and Lavretsky H (2018). Pharmacogenetic decision support tools: a new paradigm for late-life depression? The American Journal of Geriatric Psychiatry, 26, 125–133. doi: 10.1016/j.jagp.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ADI (2013). Policy Brief for Heads of Government: The Global Impact of Dementia 2013–2050. London: Alzheimer’s Disease International. [Google Scholar]
- ADI (2015). World Alzheimer Report 2015 The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends. London: Alzheimer’s Disease International. [Google Scholar]
- ADI (2018). World Alzheimer Report 2018 The State of the Art of Dementia Research: New Frontiers. London: Alzheimer’s Disease International. [Google Scholar]
- ADI (2019). Dementia Plans. London: Alzheimer’s Disease International. [Google Scholar]
- Anderson M and Perrin A (2017). Tech adoption climbs among older adults. Pew Research Center, May 17. Available at: https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/. [Google Scholar]
- Arandjelovic K, Eyre HA, Lenze E, Singh AB, Berk M and Bousman C (2019). The role of depression pharmacogenetic decision support tools in shared decision making. J Neural Transm (Vienna), 126, 87–94. doi: 10.1007/s00702-017-1806-8. [DOI] [PubMed] [Google Scholar]
- Astell AJ (2019). Technology and dementia: the future is now. Dementia and Geriatric Cognitive Disorders, 47, 129–130. doi: 10.1159/000497800. [DOI] [PubMed] [Google Scholar]
- Barbarino P, Lynch C, Bliss A, Dabas L and ADI (Eds.). (2019). From Plan to Impact II: The Urgent Need for Action. London: Alzheimer’s Disease International. [Google Scholar]
- Batchelor R, Bobrowicz A, Mackenzie R and Milne A (2012). Challenges of ethical and legal responsibilities when technologies’ uses and users change: social networking sites, decision-making capacity and dementia. Ethics and Information Technology, 14, 99–108. doi: 10.1007/s10676-012-9286-x. [DOI] [Google Scholar]
- Bennett B et al. (2017). Assistive technologies for people with dementia: ethical considerations. Bulletin of the World Health Organization, 95, 749–755. doi: 10.2471/BLT.16.187484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boll F and Brune P (2016). Online support for the elderly – why service and social network platforms should be integrated. Procedia Computer Science, 98, 395–400. doi: 10.1016/j.procs.2016.09.060. [DOI] [Google Scholar]
- Bound K and Saunders T (2018). Innovation Policy Toolkit: Tradecraft for innovation diplomats. NESTA, London, UK. [Google Scholar]
- Brookmeyer R, Abdalla N, Kawas CH and Corrada MM (2018). Forecasting the prevalence of preclinical and clinical Alzheimer’s disease in the United States. Alzheimers Dement, 14, 121–129. doi: 10.1016/j.jalz.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown MDM, Tim K, Shapiro CN, Kolker J and Novotny TE (2014). Bridging public health and foreign affairs: the tradecraft of global health diplomacy and the role of health attachés. Science and Diplomacy, 3. [Google Scholar]
- Cacioppo JT and Hawkley LC (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13, 447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantarero-Prieto D, Leon PL, Blazquez-Fernandez C, Juan PS and Cobo CS (2019). The economic cost of dementia: a systematic review. Dementia (London). doi: 10.1177/1471301219837776. [DOI] [PubMed] [Google Scholar]
- Carey IM et al. (2018). Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ Open, 8, e022404. doi: 10.1136/bmjopen-2018-022404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang DD et al. (2018). Pharmacogenetic guidelines and decision support tools for depression treatment: application to late-life. Pharmacogenomics, 19, 1269–1284. doi: 10.2217/pgs-2018-0099. [DOI] [PubMed] [Google Scholar]
- Chen H et al. (2017). Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: a population-based cohort study. Lancet, 389, 718–726. doi: 10.1016/S0140-6736(16)32399-6. [DOI] [PubMed] [Google Scholar]
- Choi NG and Dinitto DM (2013). Internet use among older adults: association with health needs, psychological capital, and social capital. Journal of Medical Internet Research, 15, e97. doi: 10.2196/jmir.2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colglazier EW (2018). Science diplomacy and future worlds. Science & Diplomacy, 7 Available at: http://www.sciencediplomacy.org/editorial/2018/science-diplomacyand-future-worlds. [Google Scholar]
- Coravos A et al. (2019). Digital medicine: a primer on measurement. Digital Biomarkers, 3, 31–71. doi: 10.1159/000500413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coventry L and Branley D (2018). Cybersecurity in healthcare: a narrative review of trends, threats and ways forward. Maturitas, 113, 48–52. doi: 10.1016/j.maturitas.2018.04.008. [DOI] [PubMed] [Google Scholar]
- DMS (2019). The Digital Medicine Society. Available at: https://www.dimesociety.org/.
- Dodge HH et al. (2015). Web-enabled conversational interactions as a means to improve cognitive functions: results of a 6-week randomized controlled trial. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 1, 1–12. doi: 10.1016/j.trci.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder A (2015). False friends and false coinage: a tool for navigating the ethics of sociable robots. ACM SIGCAS Computers and Society, 45, 248–254. doi: 10.1145/2874239.2874274. [DOI] [Google Scholar]
- Eyre H, Baune B and Lavretsky H (2015a). Clinical advances in geriatric psychiatry: a focus on prevention of mood and cognitive disorders. Psychiatric Clinics of North America, 38, 495–514. doi: 10.1016/j.psc.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyre HA, et al. (2015b). Strengthening the role of convergence science in medicine. Convergent Science Physical Oncology, 1, 026001. doi: 10.1088/2057-1739/1/2/026001. [DOI] [Google Scholar]
- Eyre HA et al. (2017). Convergence science arrives: how does it relate to psychiatry? Academic Psychiatry, 41, 91–99. doi: 10.1007/s40596-016-0496-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyre HA, Robb A, Abbott R and Hopwood M (2019). Mental health innovation diplomacy: an under-recognised soft power. Australian and New Zealand Journal of Psychiatry, 53, 474–475. doi: 10.1177/0004867419828488. [DOI] [PubMed] [Google Scholar]
- Eyre HA, Vahabzadeh A, Abbott R, Cook IA and Berk M (2018). The future of psychiatry commission. Lancet Psychiatry, 5, 13. doi: 10.1016/S2215-0366(17)30410-8. [DOI] [PubMed] [Google Scholar]
- FBI (2019). Fraud Against Seniors. Available at: https://www.fbi.gov/scams-and-safety/common-fraud-schemes/seniors.
- FCC (2017). Mapping Broadband Health in America. Connect2Health. Available at: https://www.fcc.gov/health/maps. [Google Scholar]
- GBHI (2019). Global Brain Health Institute. Available at: https://www.gbhi.org/.
- Ghosh D and Iyengar V (2019). Older adults are especially prone to social media bubbles. Scientific American, February 21. Available at: https://blogs.scientificamerican.com/observations/older-adults-are-especially-prone-to-social-media-bubbles/. [Google Scholar]
- GHTC (2019). Global Health Technologies Coalition. Available at: https://www.ghtcoalition.org/.
- Glisky EL, Rubin SR and Davidson PS (2001). Source memory in older adults: an encoding or retrieval problem? Journal of Experimental Psychology: Learning, Memory, and Cognition, 27, 1131–1146. doi: 10.1037//0278-7393.27.5.1131. [DOI] [PubMed] [Google Scholar]
- Goldman JS et al. (2011). Genetic counseling and testing for Alzheimer disease: joint practice guidelines of the American College of Medical Genetics and the National Society of Genetic Counselors. Genetics in Medicine, 13, 597–605. doi: 10.1097/GIM.0b013e31821d69b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Olive FX and Thorogood M (2018). Sustainable development goal 3 is unlikely to be achieved without renewed effort. Lancet Glob Health, 6, e824–e825. doi: 10.1016/S2214-109X(18)30297-3. [DOI] [PubMed] [Google Scholar]
- Gove D et al. (2018). Alzheimer Europe’s position on involving people with dementia in research through PPI (patient and public involvement). Aging Ment Health, 22, 723–729. doi: 10.1080/13607863.2017.1317334. [DOI] [PubMed] [Google Scholar]
- Guess A, Nagler J and Tucker J (2019). Less than you think: prevalence and predictors of fake news dissemination on Facebook. Science Advances, 5, eaau4586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JE, Karch DL and Crosby AE (2016). Elder Abuse Surveillance: Uniform Definitions and Recommended Core Data Elements For Use In Elder Abuse Surveillance, Version 1.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Hampel H et al. (2018). Revolution of Alzheimer precision neurology. Passageway of systems biology and neurophysiology. Journal of Alzheimer’s Disease, 64, S47–S105. doi: 10.3233/JAD-179932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartin PJ et al. (2016). The empowering role of mobile apps in behavior change interventions: the gray matters randomized controlled trial. JMIR Mhealth Uhealth, 4, e93. doi: 10.2196/mhealth.4878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC and Cacioppo JT (2010). Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40, 218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrman H, Kieling C, McGorry P, Horton R, Sargent J and Patel V (2019). Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet, 393, e42–e43. doi: 10.1016/S0140-6736(18)32408-5. [DOI] [PubMed] [Google Scholar]
- Holford M and Nichols RW (2018). The challenge of building science diplomacy capabilities for early career academic investigators. Science & Diplomacy, 6 Available at: http://www.sciencediplomacy.org/perspective/2018/EACIs. [Google Scholar]
- Iyengar V, Ghosh D, Smith T and Krueger F (2019). Age-related changes in interpersonal trust behavior: can neuroscience inform public policy? NAM Perspectives. doi: 10.31478/201906c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juma C (2018). Exponential innovation and human rights: implications for science and technology diplomacy. HKS Faculty Research Working Paper Series RWP18-011, February 2018. [Google Scholar]
- Jung CR, Lin YT and Hwang BF (2015). Ozone, particulate matter, and newly diagnosed Alzheimer’s disease: a population-based cohort study in Taiwan. Journal of Alzheimer’s Disease, 44, 573–584. doi: 10.3233/JAD-140855. [DOI] [PubMed] [Google Scholar]
- Katz R, Kornblet S, Arnold G, Lief E and Fischer JE (2011). Defining health diplomacy: changing demands in the era of globalization. The Milbank Quarterly, 89, 503–523. doi: 10.1111/j.1468-0009.2011.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye J (2017). Making pervasive computing technology pervasive for health & wellness in aging. Public Policy & Aging Report, 27, 53–61. doi: 10.1093/ppar/prx005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy PJ, Manji H and Staglin G (2017). Unlocking global action on mental health. Diplomatic Courier, September. [Google Scholar]
- Killin LO, Starr JM, Shiue IJ and Russ TC (2016). Environmental risk factors for dementia: a systematic review. BMC Geriatrics, 16, 175. doi: 10.1186/s12877-016-0342-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp M, et al. (2015). The case for investment in technology to manage the global costs of dementia Working Papers 72399, Imperial College, London, Imperial College Business School. [Google Scholar]
- Kohrt BA, Marienfeld CB, Panter-Brick C, Tsai AC and Wainberg ML (2016). Global mental health: five areas for value-driven training innovation. Academic Psychiatry, 40, 650–658. doi: 10.1007/s40596-016-0504-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krell-Roesch J, et al. (2019). Quantity and quality of mental activities and the risk of incident mild cognitive impairment. Neurology, 93, e548–e558. doi: 10.1212/WNL.0000000000007897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landau R and Werner S (2012). Ethical aspects of using GPS for tracking people with dementia: recommendations for practice. International Psychogeriatrics, 24, 358–366. doi: 10.1017/S1041610211001888. [DOI] [PubMed] [Google Scholar]
- Landeiro F, Barrows P, NuttallMusson E, Gray AM and Leal J (2017). Reducing social isolation and loneliness in older people: a systematic review protocol. BMJ Open, 7, e013778. doi: 10.1136/bmjopen-2016-013778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledoux C, Pilot E, Diaz E and Krafft T (2018). Migrants’ access to healthcare services within the European Union: a content analysis of policy documents in Ireland, Portugal and Spain. Global Health, 14, 57. doi: 10.1186/s12992-018-0373-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leijten J (2017). Exploring the future of innovation diplomacy. European Journal of Futures Research, 5. doi: 10.1007/s40309-017-0122-8. [DOI] [Google Scholar]
- Livingston G et al. (2017). Dementia prevention, intervention, and care. Lancet, 390, 2673–2734. doi: 10.1016/S0140-6736(17)31363-6. [DOI] [PubMed] [Google Scholar]
- Lund C et al. (2018). Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry, 5, 357–369. doi: 10.1016/S2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- MAC (2017). Ordering Genetic Testing. Available at: https://memory.ucsf.edu/sites/memory.ucsf.edu/files/wysiwyg/UCSF_Provider_OrderingGeneticTesting_11-6-17.pdf.
- Majumder S, et al. (2017). Smart homes for elderly healthcare – recent advances and research challenges. Sensors (Basel), 17, 2496. doi: 10.3390/s17112496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangin D et al. (2018). International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): position statement and 10 recommendations for action. Drugs & Aging, 35, 575–587. doi: 10.1007/s40266-018-0554-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak EE et al. (2016). Harnessing the potential of community-based participatory research approaches in bipolar disorder. International Journal of Bipolar Disorders, 4, 4. doi: 10.1186/s40345-016-0045-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miremadi T (2016). A model for science and technology diplomacy: how to align the rationales of foreign policy and science. Available at SSRN: https://ssrn.com/abstract=2737347. [Google Scholar]
- MIT (2019). MIT Innovation Initiative: Innovation Diplomats Program. Available at: https://innovation.mit.edu/opportunity/innovation-diplomats/.
- NASA (2018). Paired sleep tracker, light therapy tools retrain circadian rhythms. NASA Spinoff; Available at: https://spinoff.nasa.gov/Spinoff2018/cg_8.html. [Google Scholar]
- Norton S, Matthews FE, Barnes DE, Yaffe K and Brayne C (2014). Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurology, 13, 788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- NSTC (2019). Emerging Technologies to Support an Aging Population. Available at: https://www.whitehouse.gov/wp-content/uploads/2019/03/Emerging-Tech-to-Support-Aging-2019.pdf.
- Parra MA et al. (2018). Dementia in Latin America: assessing the present and envisioning the future. Neurology, 90, 222–231. doi: 10.1212/WNL.0000000000004897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PatientsLikeMe. (2017). https://www.patientslikeme.com/.
- Peters R, Ee N, Peters J, Booth A, Mudway I and Anstey KJ (2019). Air pollution and dementia: a systematic review. Journal of Alzheimer’s Disease, 70, S145–S163. doi: 10.3233/JAD-180631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PRC (2014). Older adults and technology use. Pew Research Center, April 3. Available at: https://www.pewresearch.org/internet/2014/04/03/older-adults-and-technology-use/.
- Quinn K (2018). Cognitive effects of social media use: a case of older adults. Social Media and Society, 4. doi: 10.1177/2056305118787203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramadi K, Srinavasan S and Atun R (2019). Health diplomacy through health entrepreneurship: using hackathons to address Palestinian-Israeli health concerns. BMJ Global Health, 4, e001548. doi: 10.1136/bmjgh-2019-001548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid M, Goosby E and Kevany S (2019). Leveraging health diplomacy to end the tuberculosis epidemic. Lancet Global Health, 7, e561–e562. doi: 10.1016/S2214-109X(19)30058-0. [DOI] [PubMed] [Google Scholar]
- Rosenfeld L, Torous J and Vahia IV (2017). Data Security and Privacy in Apps for dementia: an analysis of existing privacy policies. The American Journal of Geriatric Psychiatry, 25, 873–877. doi: 10.1016/j.jagp.2017.04.009. [DOI] [PubMed] [Google Scholar]
- Sagner M et al. (2017). The P4 health apectrum – a predictive, preventive, personalized and participatory continuum for promoting healthspan. Progress in Cardiovascular Diseases, 59, 506–521. doi: 10.1016/j.pcad.2016.08.002. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M and Berkman L (2001). Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Journal of Health Psychology, 20, 243–255. doi: 10.1037/0278-6133.20.4.243. [DOI] [PubMed] [Google Scholar]
- Sharkey A and Sharkey N (2012). Granny and the robots: ethical issues in robot care for the elderly. Ethics and Information Technology, 14, 27–40. doi: 10.1007/s10676-010-9234-6. [DOI] [Google Scholar]
- SharpBrains (2013). The Digital Brain Health Market 2012–2020: Web-based, mobile and biometrics-based technology to assess, monitor and enhance cognition and brain functioning. San Francisco, CA: SharpBrains. [Google Scholar]
- Shibata T and Wada K (2011). Robot therapy: a new approach for mental healthcare of the elderly – a minireview. Gerontology, 57, 378–386. doi: 10.1159/000319015. [DOI] [PubMed] [Google Scholar]
- Shim H, Crimmins E and Ailshire J (2018). Internet use and social capital: findings from the national health and aging trends study. Innovations in Aging, 2, 560–561. doi: 10.1093/geroni/igy023.2074. [DOI] [Google Scholar]
- Stanford (2019). Explore Courses: PSYC 240: Leadership and Innovation in Mental Healthcare. Stanford Bulletin ExploreCourses. Available at: https://explorecourses.stanford.edu/search?view=catalog&filter-coursestatus-Active=on&q=PSYC%20240:%20Leadership%20and%20Innovation%20in%20Mental%20Healthcare&academicYear=20162017. [Google Scholar]
- Staruch RM, Beverly A, Sarfo-Annin JK and Rowbotham S (2018). Calling for the next WHO Global Health Initiative: the use of disruptive innovation to meet the health care needs of displaced populations. Journal of Global Health, 8, 010303. doi: 10.7189/jogh.08.010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukumaran P (2019). Addressing the social determinants of brain health. Salud America!, April 29 Available at: https://salud-america.org/addressing-the-social-determinants-of-brain-health/. [Google Scholar]
- Swire B, Ecker UKH and Lewandowsky S (2017). The role of familiarity in correcting inaccurate information. Journal of Experimental Psychology: Learning, Memory, and Cognition, 43, 1948–1961. doi: 10.1037/xlm0000422. [DOI] [PubMed] [Google Scholar]
- Tufts University. (2019). Science Diplomacy Dialogue Series. Available at: https://sites.tufts.edu/sciencediplomacy/2019/02/05/science-diplomacy-dialogue-series-fall-2018/.
- Turekian VC, Moore A and Rasenick MM (2014). Mental health diplomacy: building a global response. Science & Diplomacy, 3 Available at: http://www.sciencediplomacy.org/editorial/2014/mental-health-diplomacy-building-global-response. [Google Scholar]
- Udenrigsministeriet (2019). TechPlomacy. Available at: https://techamb.um.dk/en/techplomacy/.
- UN (2015). World Population Ageing (ST/ESA/SER.A/390). Available at: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf.
- UNESCO (2018). Science, Technology and Innovation Policy. Available at: http://www.unesco.org/new/en/natural-sciences/science-technology/science-policy/.
- United Nations General Assembly (2016). Human Rights Council, 32 Session. Available at: https://www.ohchr.org/EN/HRBodies/HRC/RegularSessions/Session32/Pages/ResDecStat.aspx.
- Valcour VG, Masaki KH, Curb JD and Blanchette PL (2000). The detection of dementia in the primary care setting. JAMA Internal Medicine, 160, 2964–2968. doi: 10.1001/archinte.160.19.2964. [DOI] [PubMed] [Google Scholar]
- Waytz A and Gray K (2018). Does online technology make us more or less sociable? A preliminary review and call for research. Perspectives on Psychological Science, 13, 473–491. doi: 10.1177/1745691617746509. [DOI] [PubMed] [Google Scholar]
- WEF (2019). Centre for the Fourth Industrial Revolution. In Available at: https://www.weforum.org/centre-for-the-fourth-industrial-revolution.
- Wei Y et al. (2019). Associations between seasonal temperature and dementia-associated hospitalizations in New England. Environment International, 126, 228–233. doi: 10.1016/j.envint.2018.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner MW et al. (2018). The Brain Health Registry: an internet-based platform for recruitment, assessment, and longitudinal monitoring of participants for neuroscience studies. Alzheimer’s & Dementia, 14, 1063–1076. doi: 10.1016/j.jalz.2018.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesselman LM, Hooghiemstra AM, Schoonmade LJ, de Wit MC, van der Flier WM and Sikkes SA (2019). Web-based multidomain lifestyle programs for brain health: comprehensive overview and meta-analysis. JMIR Mental Health, 6, e12104. doi: 10.2196/12104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2017). Global Action Plan on the Public Health Response to Dementia. Geneva: World Health Organization. [Google Scholar]
- WHO (2018). Global health diplomacy. Available at: https://www.who.int/trade/diplomacy/en/.
- WHO (2019a). Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines. Geneva: World Health Organization. [PubMed] [Google Scholar]
- WHO (2019b). WHO iSupport : a programme for carers of people with dementia. Available at: https://www.who.int/mental_health/neurology/dementia/isupport/en/.
- Williams K et al. (2018). A randomized trial using telehealth technology to link caregivers with dementia care experts for in-home caregiving support: FamTechCare protocol. Research in Nursing & Health, 41, 219–227. doi: 10.1002/nur.21869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong K and Cummings J (2016). Healthybrains.org: from registry to randomization. Journal of Prevention of Alzheimer’s Disease, 3, 123–126. doi: 10.14283/jpad.2016.100. [DOI] [PubMed] [Google Scholar]