Abstract
Objectives
This study aimed to systematically evaluate the effects of constraint-induced aphasia therapy (CIAT) for aphasic patients reported by randomized controlled trials.
Methods
Relevant randomized controlled trials were retrieved from 11 electronic databases. A methodological quality assessment was conducted in accordance with the Cochrane Handbook, and meta-analyses were performed by using RevMan 5.2. A descriptive analysis was conducted when the included trials were not suitable for a meta-analysis.
Results
A total of 12 trials were included. A statistically significant group difference was shown from the meta-analysis in the results measured by the Western Aphasia Battery (random-effects model, MD = 1.23, 95% CI = 0.31 to 2.14, P < 0.01). However, there were no statistically significant differences shown in the results of the Boston Naming Test (fixed-effects model, MD = −1.79, 95% CI = −11.19 to 7.62, P > 0.05) and Aachen Aphasia Test (fixed-effects model, MD = −1.11, 95% CI = −4.49 to 2.27, P > 0.05). The descriptive analysis showed positive results in language performances of naming, repetition, and comprehension.
Conclusion
This systematic review indicated that CIAT was efficient for improving language performance with regard to naming, comprehension, repetition, written language, and oral language based on the current evidence. And this review provides some meaningful guides for clinical practice: expand the therapy duration to 2 or 3 h per day, focus on naming, and choose the best assessment tool. It also indicates a need for more rigorous, large-scale, and high-quality trials in the future.
Keywords: Aphasia, Constraint-induced aphasia therapy, Descriptive analysis, Language tests
What is known?
-
•
Constraint-induced aphasia therapy (CIAT), a noninvasive treatment approach for aphasia, has attracted great interests in therapists since it was developed in 2001, but there is a lack of systematic review in recent years to explore its efficiency on the patients with aphasia.
What is new?
-
•
We included studies that reported the CIAT in the intervention group compared with conventional therapy and other speech and language therapy in both English and Chinese electronic databases.
-
•
Our finding verified that CIAT was efficient for improving language performance with regard to naming, comprehension, repetition, written language, and oral language based on the current evidence.
-
•
This review provided some meaningful guides for clinical practice: expand the therapy duration to 2 or 3 h per day, focus on naming, and choose the best assessment tool.
1. Introduction
Aphasia is an acquired language disorder characterized by the inability to formulate or comprehend language, including verbal expressions, auditory comprehension, reading and writing, and functional communication [[1], [2], [3]]. Aphasia is usually caused by brain injuries [4] and progressive neurological disorders [5], which damage specific brain regions and affect the speech of patients on semantic, phonological, morphological, and syntactic components. The influence range depends on injured brain locations and severity but is not related to the intelligence of patients with aphasia [6]. However, aphasia may result in impaired reasoning and the inability to problem-solve [7]. Aphasia seems to deprive patients of the basic capacity of “freedom of expression”, which destroys their abilities to be involved in normal life as before. It thus makes patients disconnect with their social networks and hinders them from returning back to work, which increases their social support needs [8,9]. A recent comprehensive national audit data in the United Kingdom reported that approximately 33% of the patients who suffered from stroke were diagnosed with aphasia [10].
There is a huge amount of rehabilitation treatment approaches for aphasia in which speech and language therapy (SLT) is the most frequently used therapy, including intensive therapy [11], melodic intonation therapy [12], and constraint-induced aphasia therapy (CIAT) [13]. CIAT, as a noninvasive treatment approach, has attracted great interests in therapists [14,15] since it was first developed by Pulvermüller et al. [16] in 2001. CIAT primarily concentrates on two principles of constraints (force patients to use verbal language) and intensity (massed practice) due to patients with aphasia often making the least effort in communication and even solely using drawings or gestures instead of speaking out. Meanwhile, it is of importance for CIAT to induce patients with aphasia to employ words that they often neglect in order to enhance the treatment effect [16]. Studies showed that high-intensity speech training can stimulate the corresponding brain language regions of patients and thus enable them to be gradually accustomed to normal language communication [17,18]. Neuroimaging-related studies exploring the change of brain areas concerning language and speech function after the training of CIAT showed that the activated areas primarily included the left hemisphere, such as left inferior frontal gyrus [19] and left middle frontal gyrus [20], which are considered language performance control regions.
However, the effects of CIAT on patients with aphasia are still uncertain due to some inconsistent study results, especially for the subtests of language performance. CIAT has been compared with conventional therapy in two studies [16,21], in which conventional therapy included repeating and recalling targeted words, naming some pictures on paper, and answering some simple questions. The results showed that patients receiving CIAT had significant improvements compared with patients receiving conventional therapy in terms of naming, comprehension, and token test, but not in repetition [16]. In the other study [21], there were no significant improvements in all outcomes for patients in the CIAT group. In the study by Wilssens et al. [22], researchers indicated that CIAT could significantly improve verbal communication in terms of token test and naming compared with the intensive semantic treatment (BOX), but in the study by Kurland et al. [23], no significant difference was shown in terms of naming when comparing CIAT with Promoting Aphasia Communication Effectiveness (PACE). In Berthier’s study [24], participants with severe aphasia achieved great improvements by combining CIAT training with Memantine. Moreover, researchers focused not only on the effectiveness of CIAT after stroke in the chronic phase, but also in the acute phase. The results of the study of Woldag et al. [25] showed that CIAT in the acute phase could work very well for patients with aphasia solely in Communication Activity Log-quality, but no significant improvements were identified for the Aachen Aphasia Test (AAT).
A recent systematic review showed that CIAT may be useful for improving patients with aphasia, but evidence was limited [26]. Therefore, it is necessary to include more high-quality studies in order to identify the rehabilitation effects of CIAT among patients with aphasia. We expanded the retrieved number of databases and the ranges of language and time in order to obtain richer evidence. The purpose of this review was thus to systematically evaluate the effects of CIAT for aphasic patients reported by randomized controlled trials.
2. Material and methods
This systematic review was performed according to the PRISMA guidelines [27]. We wondered whether CIAT was more efficient than conventional therapy and other speech and language therapies such as BOX and PACE for patients with aphasia.
2.1. Inclusion and exclusion criteria
The inclusion criteria for studies to be included in this review were: (1) Study: RCTs with or without blinding designs, (2) Participants: participants were male and/or female adults aged 18 years old or above and were diagnosed with aphasia [28], (3) Intervention and Control: CIAT with clear intervention time and duration was applied in the intervention group and compared with the control group, (4) the included trials were evaluated at least one of the primary outcomes including the Western Aphasia Battery (WAB) assessing the severity of aphasia, the Aachen Aphasia Test (AAT), the Boston Naming Test (BNT) and China Rehabilitation Research Center Aphasia (CRRCAE) assessing language performance; the secondary outcomes including Communication Activity Log (CAL) and Communication Ability of Daily Living (CADL) assessing language performance, (5) Language: articles written in English or Chinese.
Studies were excluded in this review if 1) they were clinical case reports, quasi-RCTs, reviews, or conference proceedings papers and/or 2) CIAT was combined with other therapies in the intervention group and/or 3) studies which explored that specific features of ILAT/CIAT are (not) essential or that this method can be (further) improved. Any disagreements about the excluded studies were resolved by discussion between reviewers and further assessments.
2.2. Data sources and search strategies
A computerized database search was performed by two reviewers in 11 electronic databases: PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), Allied and Alternative Medicine (AMED), Cumulative Index of Nursing and Allied Health Literature (CINAHL), PsycINFO, Web of Science, China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database (CBMdisc), WanFang Data, and Chinese Scientific Journal Database (VIP) from each database’s inception to October 2019. Meanwhile, a manual search was also conducted to search for eligible studies from the reference lists of the included studies. The keywords and MeSH terms used for identifying “CIAT” involved “constraint-induced aphasia therapy”, “constraint-induced language therapy”, “constraint-induced speech therapy”, “intensive language action therapy”, “CIAT”, and “ILAT”. The keywords used for identifying “aphasia” included “aphasi∗”, “dysphasi∗”, “language disorders”, and “speech disorders”. Appendix A lists the search strategy for PubMed in this systematic review.
2.3. Data extraction and quality assessment
Data extraction and quality assessment were conducted independently by two reviewers. The characteristics of each included trial were extracted using a data extraction form, which included: 1) author(s) and publication year, 2) sample sizes of the intervention and control groups; 3) the ages of the participants; 4) the intervention protocols of each group, including therapy types and intervention time and durations, and 5) outcome measures. A methodological quality assessment of the included studies was based on the Cochrane Handbook [29], which included: 1) random sequence generation, 2) allocation concealment, 3) blinding of the participants and personnel, 4) blinding of the outcome assessments, 5) incomplete outcome data, 6) selective outcome reporting, and 7) other bias. Each item was rated as “unclear risk”, “high risk”, or “low risk”. Moreover, studies would be rated as the grade of A when they fully met the quality standard; studies would be rated as the grade of B when they partially met the quality standard; studies would be rated as the grade of C when they did not meet the quality standard and had a high risk for bias in at least one item. Studies with the grade of A and B would be included after the critical appraisal [29]. Disagreements between the reviewers were solved through discussion with the corresponding author.
2.4. Data analysis
The meta-analysis was conducted by using the Review Manager 5.2. Means and standard deviations of each outcome were extracted and pooled in order to obtain the mean differences (MD) and 95% confidence intervals (CI). Heterogeneity among studies was assessed using I2. I2 was considered low heterogeneity when I2 was less than 50.0%, moderate heterogeneity when I2 was between 50.0% and 75.0%, and high heterogeneity when I2 was more than 75.0%. The fixed-effect model was used to combine studies when heterogeneity was not significant (P > 0.01). Otherwise, the random-effect model was used to combine the studies. When heterogeneity was high, the subgroup or sensitivity analysis would be performed to investigate the potential sources of clinical heterogeneity and to test the reliability of the results. If a meta-analysis was not appropriate, a descriptive analysis was employed to summarize the studies.
3. Results
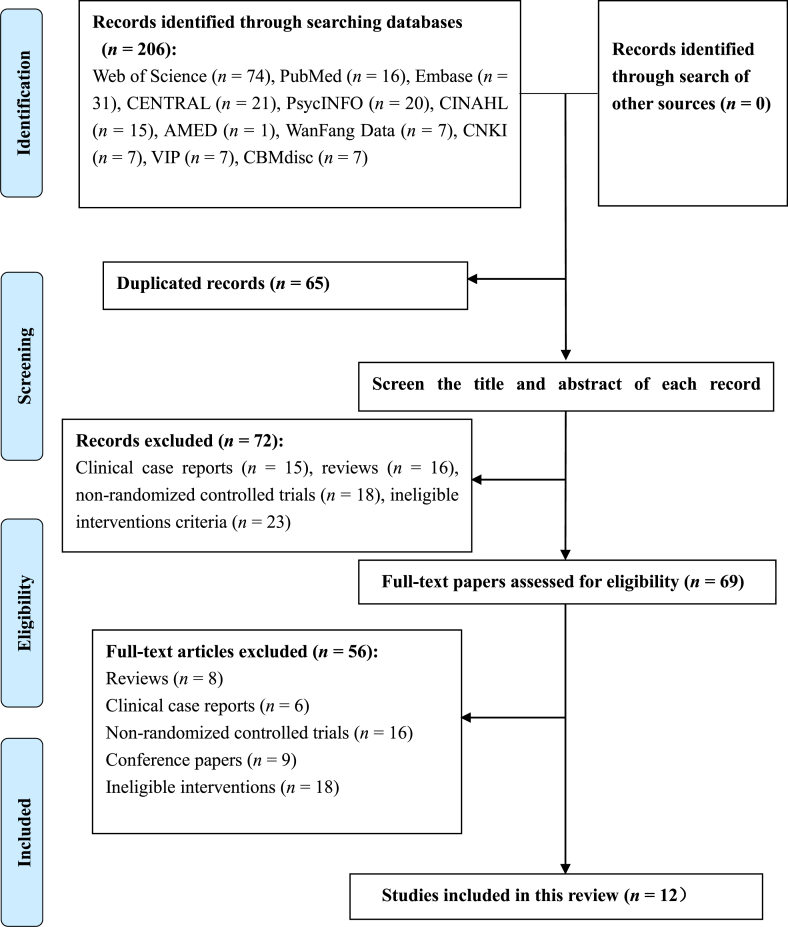
A total of 206 records were identified from the database and manual search. A total of 65 duplicated papers were first removed, then 72 papers were further excluded through reading the titles and abstracts, including clinical case reports (n = 15), reviews (n = 16), nonrandomized controlled trials (n = 18), and ineligible interventions (n = 23). Among the remaining 69 records, full-texts were retrieved to assess the eligibility, of which 56 papers were finally removed because they were either clinical case reports (n = 6), reviews (n = 8), conference proceedings papers (n = 9), nonrandomized controlled trials (n = 16), or ineligible interventions (n = 18). Hence, 12 studies were identified for analysis [16,[21], [22], [23],25,[30], [31], [32], [33], [34], [35], [36]]. The process is shown as a flow chart in Fig. 1.
Fig. 1.
Flow chart of the studies selected for the systematic review.
3.1. Characteristic of the included studies
The 12 studies, including seven in English and five in Chinese, were published between 2001 and 2019. A total of 493 participants ranging in age from 32 to 86 years were identified from the included studies. Studies originated from the United Kingdom [16], Australia [21], Belgium [22], Germany [25,30], the United States [23,31], and China [[32], [33], [34], [35], [36]]. The intervention groups in all included trials employed CIAT, while the control groups used three types of therapies: conventional therapy [16,21,25,30,[32], [33], [34], [35], [36]], intensive semantic treatment [22], Promoting Aphasia Communicative Effectiveness [23], or no intervention [31]. The intervention duration ranged from 1 h to 4 h per day, of which two or 3 h per day was adopted by the majority of studies. The included trials used various outcome measurement tools to evaluate language performance, and the most frequent objective tools were the BNT, the AAT, and the WAB. More detailed information is shown in Table 1.
Table 1.
Characteristics of the included trials.
| Study | Sample size (I/C) | Aphasia cause | Age (I/C) | Intervention (time and duration) | Outcome measures |
|---|---|---|---|---|---|
| Pulvermüller et al 2001 [16] |
10/7 | Chronic aphasia after Stroke | 55.40 ± 10.86/54.29 ± 8.10 | I: CIAT (3 h/d for 10 days) C: CT (3 h/d for 4 weeks) |
1.AAT 2.CAL |
| Ciccone et al 2015 [21] |
12/8 | Acute aphasia after Stroke | 69.40 ± 15.00/72.60 ± 14.10 | I: CIAT (45–60 min/d, 5 d/week for 5 weeks) C: CT (45–60 min/d, 5 d/week for 5 weeks) |
1.WAB-AQ 2.DA 3.SAQoL |
| Wilssens et al 2015 [22] |
5/4 | Acute aphasia after Stroke | 63.20 ± 8.44/71.25 ± 9.22 | I: CIAT (3 h/d for 10 days) C: BOX (2–3 h/d for 10 days) |
1.AAT 2.BNT 3.PALPA 4.ANELT 5.CETI 6.SAT |
| Kurland et al 2016 [23] |
12/12 | Chronic aphasia after Stroke | 68.60(55–78)/65.00(47–81) | I: ILAT (3 h/d for 10 days) C: PACE (3 h/d for 10 days) |
1.BNT 2.BDAE 3.CTPD 4.PICA |
| Woldag et al 2016 [25] |
20/20/20 | Acute aphasia after Stroke | 71.30 ± 7.20/63.00 ± 14.30/70.30 ± 11.20 | I: CIAT (3 h/d for 10 days) C: CT (3 h/d for 10 days) Individual and group therapy (14 h/2weeks) |
1.AAT 2.CAL |
| Sickert et al 2013 [30] |
50/50 | Subacute aphasia after Stroke | 60.70(41–81)/60.20(34–84) | I: CIAT (2 h/d for 15 days) C: CT (2 h/d for 15 days) |
1.AAT 2.CAL |
| Szaflarski et al 2015 [31] |
12/10 | Chronic aphasia after Stroke | 57.00 ± 11.00/51.00 ± 13.00 | I: CIAT (4 h/d for 10 days) C: no intervention |
1. BNT 2. CAL 3.BDAE 4.COWA 5.SFT 6.PPVT |
| Shi et al 2006 [32] |
10/10 | Chronic aphasia after Stroke | 51.70 ± 19.80 | I: CIAT (30–35 h/2weeks) C: CT (30–35 h/4weeks) |
1. WAB 2. CAL |
| Lin et al 2007 [33] |
15/15 | Chronic aphasia after Stroke | Unclear | I: CIAT (2–3 h/d, 20 d/month for 2 months) C: CT (2–3 h/d, 20 d/month for 2 months) |
1.CRRCAE 2.CFCP |
| Lin 2017 [34] |
51/51 | Chronic aphasia after Stroke | 53.30 ± 10.30/52.60 ± 11.20 | I: CIAT (2 h/d) C: CT (unclear) |
1.WAB 2.CADL |
| Xie et al 2014 [35] |
15/15 | Chronic aphasia after Stroke | 63.13 ± 5.66/57.17 ± 6.04 | I: CIAT (3 h/d, 5 d/week for 2 weeks) C: CT (30 h/4weeks) |
1. WAB 2. CAL |
| Zhao et al 2014 [36] |
29/30 | Subacute aphasia after Stroke | 51.40 ± 12.57/52.90 ± 9.60 | I: CIAT (3h/d for 10 days) C: CT (30 min/d, 5 d/week for 10 days) |
1. CRRCAE 2. CADL |
Notes:CIAT=Constraint-induced Aphasia Therapy; ILAT=Intensive Language Aphasia Therapy; CILT=Constraint-induced Language Therapy: ILAT and CILT are different names for CIAT. AAT = Aachen Aphasia Test; ANELT = Amsterdam Nijmegen Everyday Language Test; AQ = Aphasia Quotient; BNT=Boston Naming Test; BOX=Intensive semantic treatment; BDAE=Boston Diagnostic Aphasia Examination; C=Control Group; CAL=Communication Activity Log; CADL=Communicative Ability of Daily Living; CETI=Communicative Effectiveness Index; CFCP=Chinese Functional Communication Profile; COWA=Controlled Oral Word Association Test; CRRCAE=China Rehabilitation Research Center Aphasia Examination; CT=Conventional Therapy; CTPD=Cookie Theft Picture Description; DA = Discourse Analysis; d=day; h=hour; I=Intervention Group; Min=minute; PACE=Promoting Aphasia Communicative Effectiveness; PALPA=Psycholinguistic Assessment of Language Processing in Aphasia; PICA=Porch Index of Communicative Ability; PPVT=Peabody Picture Vocabulary Test; SAQoL = The Stroke and Aphasia Quality of Life Scale; SAT=Semantic Association Test; SFT=Semantic Fluency Test; WAB=Western Aphasia Battery.
3.2. Quality assessment
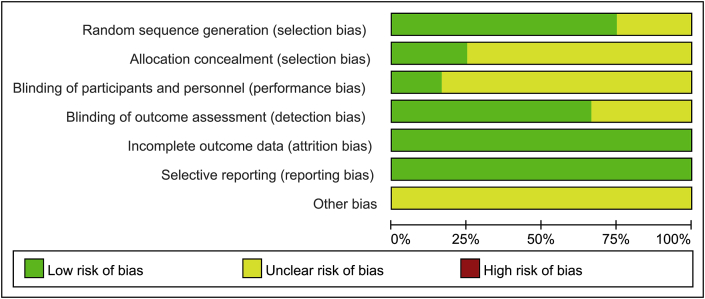
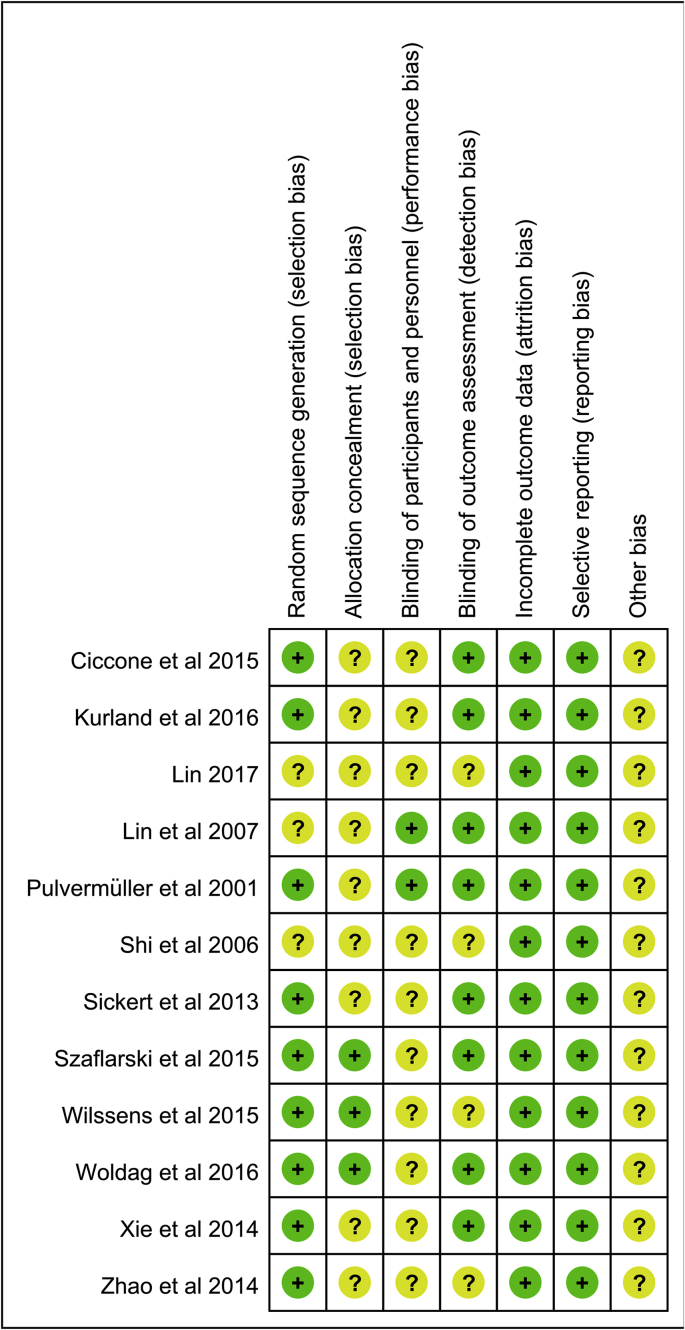
Randomization was applied in all studies, whereas the generation methods of random sequences were described in nine studies [16,[21], [22], [23],25,30,31,35,36]. Three studies [22,25,31] described the allocation concealment and the rest of studies did not describe it. Two studies [16,33] presented the blinding of the participants and personnel, while eight studies [16,21,23,25,30,31,33,35] showed the blinding of outcome assessments. All included studies described dropout and exclusion cases, of which four studies [21,23,25,31] reported their dropout rates. All included studies had no selective reporting. Moreover, all included trials could not be judged whether they had other bias. All the included studies were rated as the grade of B based on the methodological quality assessment from the Cochrane Handbook. Fig. 2 and Fig. 3 show the details of the methodological assessments of the included trials.
Fig. 2.
Methodological quality of all included studies.
Fig. 3.
Risk of bias assessment of all included studies.
3.3. Therapeutic effects of CIAT for aphasia from the meta-analysis
Of the 12 included clinical trials, three studies [22,23,31] were meta-analyzed with the BNT, two studies [22,30] were meta-analyzed with the AAT, two studies [32,35] were meta-analyzed with the WAB, and six studies [16,21,25,33,34,36] performed descriptive analyses.
3.3.1. Evaluation of therapeutic effectiveness with the BNT
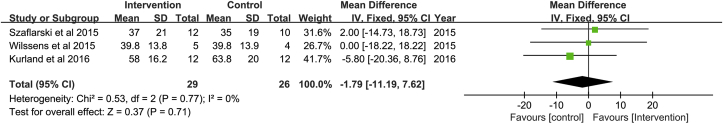
A total of 55 participants in three studies [22,23,31] were measured using the BNT. The results of the meta-analysis indicated that the BNT scores in the intervention group were not statistically significant compared with those in the control group (fixed-effects model, MD = −1.79, 95% CI = −11.19 to 7.62, P > 0.05) (see Fig. 4).
Fig. 4.
Meta-analysis of the results measured by the Boston Naming Test.
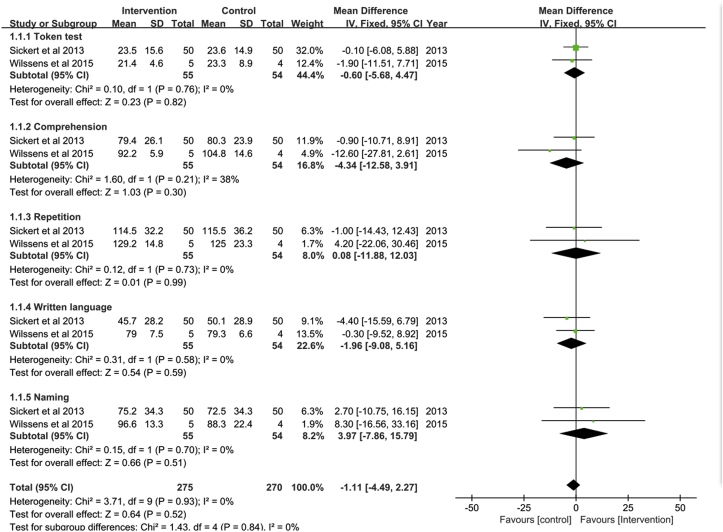
3.3.2. Evaluation of therapeutic effectiveness with the AAT
A total of 109 participants in two studies [22,30] were measured using the AAT. The pooled results from the two studies showed that the AAT scores in the intervention group were not significantly higher than those in the control group (fixed-effects model, MD = −1.11, 95% CI = −4.49 to 2.27, P > 0.05). Moreover, since the AAT was divided into five dimensions (token test, comprehension, repetition, written language, and naming), five subgroup analyses were respectively performed. The results of the subgroup analyses indicated that the scores of token test (fixed-effects model, MD = −0.60, 95% CI = −5.68 to 4.47, P > 0.05), comprehension (fixed-effects model, MD = −4.34, 95% CI = −12.58 to 3.91, P > 0.05), repetition (fixed-effects model, MD = 0.08, 95% CI = −11.88 to 12.03, P > 0.05), written language (fixed-effects model, MD = −1.96, 95% CI = −9.08 to 5.16, P > 0.05), and naming (fixed-effects model, MD = 3.97, 95% CI = −7.86 to 15.79, P > 0.05) in the intervention group were not significantly higher compared with those in the control group (see Fig. 5).
Fig. 5.
Meta-analysis of the results measured by the Aachen Aphasia Test.
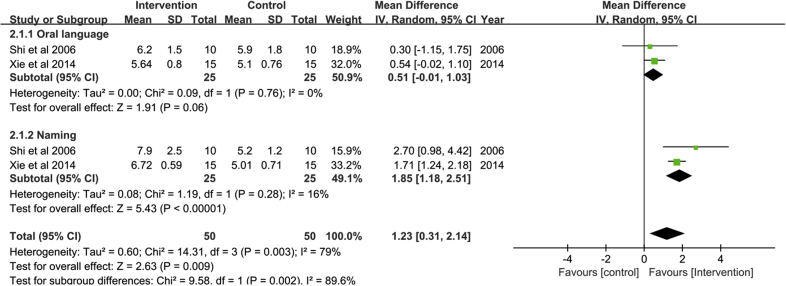
3.3.3. Evaluation of therapeutic effectiveness with the WAB
The severity of aphasia among 50 participants in two studies [32,35] was measured by the WAB. The results of the meta-analysis showed that the scores of the WAB (random-effects model, MD = 1.23, 95% CI = 0.31 to 2.14, P < 0.01) in the intervention group were significantly higher compared with those in the control group. Considering that the two different dimensions of the WAB comprised naming and oral language, two subgroup analyses were conducted. The naming scores (random-effects model, MD = 1.85, 95% CI = 1.18 to 2.51, P < 0.01) showed that these were statistically higher in the intervention group than those in the control group, whereas the scores of oral language (random-effects model, MD = 0.51, 95% CI = −0.01 to 1.03, P > 0.05) in the intervention group were not significantly higher compared with those in the control group (see Fig. 6).
Fig. 6.
Meta-analysis of the results measured by the Western Aphasia Battery.
3.4. Therapeutic effects of CIAT for aphasia from the descriptive analysis
Six studies [16,21,25,33,34,36] were inappropriate to conduct a meta-analysis due to the different outcome measures and scales used. Hence, a descriptive analysis was performed, which was respectively divided into subgroup analyses according to the subtests of language performance (naming, comprehension, and repetition) and intervention durations (1-h intervention, 2-h intervention, and 3-h intervention).
3.4.1. Evaluation of therapeutic effectiveness with subtests of language performance
In terms of naming, comprehension, and repetition, Pulvermüller et al. [16] and Woldag et al. [25] used the AAT to examine the subtests of language performance. Pulvermüller et al. [16] has shown that the CIAT groups scored significantly higher than the control groups in terms of naming and comprehension, but not in repetition. Woldag et al. [25] has shown that no significant difference was found in naming, comprehension, and repetition.
Lin et al. [33] and Zhao et al. [36] examined naming, comprehension, and repetition by using the CRRCAE, and both studies found that patients receiving CIAT gained greater improvements compared with those in the control group in terms of naming, comprehension, and repetition.
3.4.2. Evaluation of therapeutic effectiveness with various durations of intervention
Ciccone et al. [21] conducted a 1-h intervention every day for each patient over a period of five weeks and used the WAB to examine language performance, and it showed that the CIAT group had no significant improvements for language performance compared with the control group.
Lin [34] conducted CIAT on patients with aphasia for 2 h per day, but Lin did not report the total duration. In the study by Lin [34], there was a significant difference between the two groups using the WAB after one month of hospital discharge.
Lin et al. [33] and Zhao et al. [36] provided 3 h per day training over a span of two months and ten days, respectively, and used the CRRCAE to examine language performance. Both studies found that patients receiving CIAT gained greater improvements compared with those in the control group in terms of comprehension, repetition, speaking, and oral reading. Pulvermüller et al. [16] and Woldag et al. [25] performed 3-h interventions every day for each patient over a period of ten days and used the AAT to examine the subtests of language performance. Pulvermüller et al. [16] showed that the CIAT groups scored significantly higher than the control groups in terms of naming, comprehension, and token test. Woldag et al. [25] showed that no significant differences were found in all the subtests of the AAT.
4. Discussion
In this systematic review, 12 clinical trials reporting the effects of CIAT on patients with aphasia involving 493 participants were identified. The meta-analysis showed that there was a significant difference in the severity of aphasia as measured by the WAB in two studies [32,35]. There was no statistically significance between the CIAT groups and the control groups in terms of language performance measured by the BNT in three studies [22,23,31] and the AAT in two studies [22,30]. The descriptive analysis showed positive results in language performance. Two studies [33,36] indicated significant differences concerning naming, comprehension, and repetition. One study [16] indicated significant differences concerning naming and comprehension, but not in repetition. Only one study [25] indicated insignificant differences concerning naming, comprehension, and repetition. Moreover, interventions that were carried out for two or 3 h per day seemed to be the most commonly used dosage in the current literature.
The quality of the included studies was appraised to be moderate based on the Cochrane Handbook [29]. All the included studies were rated as the grade of B because they partially met the quality standard and no any item of the methodological quality assessment was considered as “high risk”. In terms of detection bias, attrition bias and reporting bias, most of studies were rated as having low risk. Eight studies reported the blinding of outcome assessment, all included studies showed the complete outcome data and did not have selective reporting. However, two quality assessments including selection bias and performance bias were appraised to be poor. The assessment for selection bias included random sequence generation and allocation concealment. In our review, nine studies reported the random sequence generation but only three studies described the allocation concealment, which might generate an overestimate of the therapy efficiency [37]. In terms of the performance bias, the blinding of participants and personnel was hard to be conducted when performing the CIAT. In accordance with the Cochrane Handbook, there is no empirical evidence that the bias was generated due to lack of blinding of participants and personnel [29].
A recent systematic review by Zhang et al. [26] concluded that CIAT may be useful for improving language performance on patients with chronic post-stroke. The conclusion was consistent with ours as the effects of CIAT on naming, comprehension, repetition, written language, and oral language for aphasia patients were positive. However there remained the difference between Zhang et al.’s review and ours. In Zhang et al.’s review, nine included studies focused on patients with aphasia after strokes or cerebrovascular accidents [26], of which CIAT in six studies seemed to be useful for improving aphasic, while we included 12 studies in which recruited patients with aphasia were without pathological limitations, of which CIAT in six studies was significantly different between the CIAT groups and the control groups. For the inclusion criteria, we expanded the electronic databases to Chinese so that five Chinese studies were finally included in our review, which indicated that the CIAT groups gained greater improvements than the control groups. And there were consistent results from the meta-analysis in the review [26] and our review in terms of language performance as measured by the BNT and the AAT, whereby there was no significant difference between the CIAT group and the control group.
The BNT is a widely used neuropsychological assessment tool to measure confrontational word retrieval among individuals with aphasia or other language disturbances. There are some criticisms about the BNT, which appears to have poor psychometric properties and inadequate norms [38]. Moreover, the BNT relied on word frequency at its first published time, i.e. 1983, and its items were not listed in order from least to most frequent [39]. Furthermore, monolinguals or bilinguals may respond differently to the BNT [40], but these trials did not report whether the enrolled participants were bilingual speakers or not. Thus, there might be assessment bias when using the BNT.
The results in our review from the meta-analysis of language performance assessed by the AAT in two studies [22,30] showed that there was no significant difference between the intervention and control groups in terms of token test, comprehension, repetition, written language, and naming. An included study [25] also showed insignificant group differences in their AAT results. However, the meta-analysis showed that the naming subtest in the WAB indicated significant group differences. The naming subtest in both the BNT and the AAT was designed for patients to name pictures painted on paper [41]. However, patients are required to name some real objects on the table for the naming subtest in the Chinese version of the WAB. It is much easier for patients with aphasia to name real objects than objects in pictures [42]. Therefore, choosing a good suitable measurement tool and approach is important for measuring the intervention effects of CIAT.
Six trials were not suitable for us to perform a meta-analysis on; thus, a descriptive analysis was conducted to summarize the effects of CIAT on naming, comprehension, and repetition. The AAT was mainly employed in two studies [16,25] to evaluate language performance, but the post-treatment statistical data were not reported. The CRRCAE was used in two studies [33,36] to measure the language performance outcomes of naming, comprehension, and repetition, but one study [33] used the short version and another study [36] used the full version. The rest of two studies [21,34] showed different clinical tools and scales were used to evaluate language performance, which also made them impossible to perform a meta-analysis on. Even though the measurement tools for measuring the language performance were different in these studies, the AAT and the CRRCAE have the same subtests including naming, repetition, and comprehension. The results from summarizing the AAT and the CRRCAE in the descriptive analysis indicated positive results. In terms of naming and comprehension subtests, three studies [16,33,36] reported greater improvements among patients receiving CIAT than those in the control group, while only one study [25] did not find any significant group differences.
The intensity of the interventions (e.g. duration) has been considered as an essential factor that affects the outcomes of rehabilitation for patients with aphasia [43]. From the descriptive analysis, CIAT interventions that went on for two and 3 h per day seemed to be the most commonly used dosage in the current literature. The pioneer study of CIAT [16], enrolling participants who were 55.40 (±10.86) years old, suggested that durations of practice should be 3 h per day over a period of ten days. The post-treatment AAT scores in the CIAT group showed a significant improvement in terms of naming, comprehension, and token test compared with those in the pre-treatment results. From the latest study published by Lancet [44], the results showed that CIAT training with 2 h per day for three weeks significantly improved verbal communication among patients with chronic aphasia after strokes. In our descriptive analysis, one study [34] that employed 2 h of training per day showed that patients in the CIAT group gained better improvements in comprehension, repetition, naming, and reading than in the control group, while four studies [16,25,33,36] that employed 3 h of training per day indicated a significant improvement in language performance in the intervention group compared to the control group. In our meta-analysis, one study [35] showed significant impacts in CIAT on oral expression, naming, and repetition among patients with aphasia after 3 h of training per day, two studies [22,23] that employed 3 h of training per day indicated no significant differences between the two groups, and one study [30] that employed 2 h of training per day also indicated no significant difference between the two groups. One study [31] expanded their treatment to 4 h per day, but it yielded insignificant differences between the two groups. In conclusion, interventions of two or 3 h per day seemed to be the most commonly used dosage in the current literature, though our meta-analysis did not show any group differences on the outcomes of patients using different durations of CIAT.
In our systematic review, the conventional therapy that nine studies [16,21,25,30,[32], [33], [34], [35], [36]] employed for patients with aphasia in the control groups was proved to be efficient [45]; the intensive semantic treatment that Wilssens et al. [22] used in the control group had a beneficial effect on patients with aphasia [46]; and the Promoting Aphasia Communicative Effectiveness that Kurland et al. [23] employed in the control group was considered as being efficient for patients with aphasia [47]. In our meta-analysis and descriptive analysis, it showed that either the patients in the CIAT groups had great improvements than the control groups or there was no significant difference between the groups. Therefore, CIAT was efficient for improving language performance with regard to naming, comprehension, repetition, written language, and oral language based on the current evidence.
5. Limitations and future research
This review had some limitations. Firstly, there were methodological flaws among the included studies in this review. Only nine trials reported random sequence generation and three trials reported allocation concealment, which may result in selection bias. Only two studies and eight studies reported the blinding of their participants and personnel and the blinding of outcome assessments, respectively, which may cause performance bias and detection bias, respectively. Secondly, most of the included studies had small sample sizes, which might contribute to insufficient power [48]. Thirdly, we only searched studies from 11 electronic databases, and studies that were not in these 11 databases were not considered. Fourthly, this systematic review only included both English and Chinese literature, which may lead to language bias [49].
Based on the limitations and our review results, future studies should pay more attention to: 1) improving methodological quality, including study design, correct random sequence generation, allocation concealment, and effective blinding of the participants and personnel, and 2) performing sample size calculation, effectively explaining drop-outs, and performing an intention-to-treat analysis.
6. Conclusions
This systematic review indicated that CIAT was efficient for improving language performance with regard to naming, comprehension, repetition, written language, and oral language based on the current evidence. And this review provided some meaningful guides for nurse practitioners in the department of rehabilitation: expand therapy durations to two or 3 h per day, focus much on naming, and choose the best assessment tool. The evidence strength of CIAT for patients with aphasia is currently limited due to the poor methodological quality of the included trials. Hence, more rigorous, large-scale, high-quality trials should be performed on CIAT in the future.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Guandong Wang: Conceptualization, Methodology, Software, Formal analysis, Writing - original draft. Li Ge: Conceptualization, Validation, Data curation, Writing - review & editing, Supervision. Qingxiang Zheng: Methodology, Validation, Resources. Pingping Huang: Software, Formal analysis. Jing Xiang: Formal analysis, Visualization.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
We appreciate the Medical Publications Support Unit of the National University Health System, Singapore, for assistance in language editing of this manuscript. We appreciate the support from Associate Professor Hong-Gu He for the preparation of this manuscript.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.05.005.
Appendices. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Watila M.M., Balarabe S.A. Factors predicting post-stroke aphasia recovery. J Neurol Sci. 2015;352(1–2):12–18. doi: 10.1016/j.jns.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 2.Tippett D.C. Update in aphasia research. Curr Neurol Neurosci Rep. 2015;15(8):49. doi: 10.1007/s11910-015-0573-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spinelli E.G., Mandelli M.L., Miller Z.A., Santos-Santos M.A., Wilson S.M., Agosta F. Typical and atypical pathology in primary progressive aphasia variants. Ann Neurol. 2017;81(3):430–443. doi: 10.1002/ana.24885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Des Roches C.A., Kiran S. Technology-based rehabilitation to improve communication after acquired brain injury. Front Neurosci. 2017;11:382. doi: 10.3389/fnins.2017.00382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matias-Guiu J.A., Cabrera-Martín M.N., Moreno-Ramos T., García-Ramos R., Porta-Etessam J., Carreras J.L. Clinical course of primary progressive aphasia: clinical and FDG-PET patterns. J Neurol. 2015;262(3):570–577. doi: 10.1007/s00415-014-7608-0. [DOI] [PubMed] [Google Scholar]
- 6.Gialanella B., Prometti P., Vanoglio F., Comini L., Santoro R. Aphasia and activities of daily living in stroke patients. Eur J Phys Rehabil Med. 2016;52(6):782–790. [PubMed] [Google Scholar]
- 7.Baldo J.V., Paulraj S.R., Curran B.C., Dronkers N.F. Impaired reasoning and problem-solving in individuals with language impairment due to aphasia or language delay. Front Psychol. 2015;6:1523. doi: 10.3389/fpsyg.2015.01523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tuuli N., Ulla J. The lived experience of engaging in everyday occupations in persons with mild to moderate aphasia. Disabil Rehabil. 2013;35(21):1828–1834. doi: 10.3109/09638288.2012.759628. [DOI] [PubMed] [Google Scholar]
- 9.Wray F., Clarke D. Longer-term needs of stroke survivors with communication difficulties living in the community: a systematic review and thematic synthesis of qualitative studies. BMJ Open. 2017;7(10) doi: 10.1136/bmjopen-2017-017944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell C., Bowen A., Gittins M., Vail A., Conroy P., Paley L. Prevalence of aphasia and co-occurrence of dysarthria: the UK sentinel stroke national audit programme. Aphasiology. 2018;32(sup1):145–146. doi: 10.1080/02687038.2018.1485863. [DOI] [Google Scholar]
- 11.Sage K., Snell C., Lambon Ralph M.A. How intensive does anomia therapy for people with aphasia need to be? Neuropsychol Rehabil. 2011;21(1):26–41. doi: 10.1080/09602011.2010.528966. [DOI] [PubMed] [Google Scholar]
- 12.Haro-Martínez A.M., Lubrini G., Madero-Jarabo R., Díez-Tejedor E., Fuentes B. Melodic intonation therapy in post-stroke nonfluent aphasia: a randomized pilot trial. Clin Rehabil. 2019;33(1):44–53. doi: 10.1177/0269215518791004. [DOI] [PubMed] [Google Scholar]
- 13.Kristensen L.F., Steensig I., Pedersen A.D., Pedersen A.R., Nielsen J.F. Constraint-induced aphasia therapy in subacute neurorehabilitation. Aphasiology. 2015;29(10):1152–1163. doi: 10.1080/02687038.2015.1028328. [DOI] [Google Scholar]
- 14.Nickels L., Osborne A. Constraint Induced Aphasia Therapy: volunteer-led, unconstrained and less intense delivery can be effective. NeuroRehabilitation. 2016;39(1):97–109. doi: 10.3233/NRE-161341. [DOI] [PubMed] [Google Scholar]
- 15.Pierce J.E., Menahemi-Falkov M., O’Halloran R., Togher L., Rose M.L. Constraint and multimodal approaches to therapy for chronic aphasia: a systematic review and meta-analysis. Neuropsychol Rehabil. 2019;29(7):1005–1041. doi: 10.1080/09602011.2017.1365730. [DOI] [PubMed] [Google Scholar]
- 16.Pulvermüller F., Neininger B., Elbert T., Mohr B., Rockstroh B., Koebbel P. Constraint-induced therapy of chronic aphasia after stroke. Stroke. 2001;32(7):1621–1626. doi: 10.1161/01.STR.32.7.1621. [DOI] [PubMed] [Google Scholar]
- 17.Bang D.H., Shin W.S., Choi H.S. Effects of modified constraint-induced movement therapy combined with trunk restraint in chronic stroke: a double-blinded randomized controlled pilot trial. NeuroRehabilitation. 2015;37(1):131–137. doi: 10.3233/NRE-151245. [DOI] [PubMed] [Google Scholar]
- 18.Stahl B., Mohr B., Büscher V., Dreyer F.R., Lucchese G., Pulvermüller F. Efficacy of intensive aphasia therapy in patients with chronic stroke: a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2018;89(6):586–592. doi: 10.1136/jnnp-2017-315962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Szaflarski J.P., Griffis J., Vannest J., Allendorfer J.B., Nenert R., Amara A.W. A feasibility study of combined intermittent theta burst stimulation and modified constraint-induced aphasia therapy in chronic post-stroke aphasia. Restor Neurol Neurosci. 2018;36(4):503–518. doi: 10.3233/RNN-180812. [DOI] [PubMed] [Google Scholar]
- 20.Nenert R., Allendorfer J.B., Martin A.M., Banks C., Ball A., Vannest J. Neuroimaging correlates of post-stroke aphasia rehabilitation in a pilot randomized trial of constraint-induced aphasia therapy. Med Sci Monit Int Med J Exp Clin Res. 2017;23:3489–3507. doi: 10.12659/MSM.902301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciccone N., West D., Cream A., Cartwright J., Rai T., Granger A. Constraint-induced aphasia therapy (CIAT): a randomised controlled trial in very early stroke rehabilitation. Aphasiology. 2015;30(5):566–584. doi: 10.1080/02687038.2015.1071480. [DOI] [Google Scholar]
- 22.Wilssens I., Vandenborre D., Van D.K., Verhoeven J., Visch-Brink E., Mariën P. Constraint-induced aphasia therapy versus intensive semantic treatment in fluent aphasia. Am J Speech Lang Pathol. 2015;24(2):281–294. doi: 10.1044/2015_AJSLP-14-0018. [DOI] [PubMed] [Google Scholar]
- 23.Kurland J., Stanek E.J., Stokes P., Li M., Andrianopoulos M. Intensive language action therapy in chronic aphasia: a randomized clinical trial examining guidance by constraint. Am J Speech Lang Pathol. 2016;25(4S):798–812. doi: 10.1044/2016_AJSLP-15-0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berthier M.L., Green C., Lara J.P., Higueras C., Barbancho M.A., Dávila G. Memantine and constraint-induced aphasia therapy in chronic poststroke aphasia. Ann Neurol. 2009;65(6):577–585. doi: 10.1002/ana.21597. [DOI] [PubMed] [Google Scholar]
- 25.Woldag H., Voigt N., Bley M., Hummelsheim H. Constraint-induced aphasia therapy in the acute stage: what is the key factor for efficacy? A randomized controlled study. Neurorehabilitation Neural Repair. 2017;31(1):72–80. doi: 10.1177/1545968316662707. [DOI] [PubMed] [Google Scholar]
- 26.Zhang J., Yu J., Bao Y., Xie Q., Xu Y., Zhang J. Constraint-induced aphasia therapy in post-stroke aphasia rehabilitation: a systematic review and meta-analysis of randomized controlled trials. PloS One. 2017;12(8) doi: 10.1371/journal.pone.0183349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 28.Rohde A., Worrall L., Godecke E., O’Halloran R., Farrell A., Massey M. Diagnosis of aphasia in stroke populations: a systematic review of language tests. PloS One. 2018;13(3) doi: 10.1371/journal.pone.0194143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins J.P.T., Green S. The Cochrane Collaboration; 2011. Cochrane Handbook for systematic reviews of interventions.https://www.cochrane-handbook.org [updated March 2011] [Google Scholar]
- 30.Sickert A., Anders L.C., Münte T.F., Sailer M. Constraint-induced aphasia therapy following sub-acute stroke: a single-blind, randomised clinical trial of a modified therapy schedule. J Neurol Neurosurg Psychiatry. 2014;85(1):51–55. doi: 10.1136/jnnp-2012-304297. [DOI] [PubMed] [Google Scholar]
- 31.Szaflarski J.P., Ball A.L., Vannest J., Dietz A.R., Allendorfer J.B., Martin A.N. Constraint-induced aphasia therapy for treatment of chronic post-stroke aphasia: a randomized, blinded, controlled pilot trial. Med Sci Monit Int Med J Exp Clin Res. 2015;21:2861–2869. doi: 10.12659/MSM.894291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shi S.J., Zhu H.M., Liu Z.J., Liu X. Constraint-induced aphasia threapy for patients after stroke. Chinese Journal of Rehabilitation. 2006;21(2):112. doi: 10.3870/j.issn.1001-2001.2006.02.020. [DOI] [Google Scholar]
- 33.Lin R.W., Lin M., Chen J.S., Pan S.H. A 30 cases clinical trials of constraint-induced aphasia therapy for aphasia patients after stroke. Zhejiang.Pract.Med. 2007;12(4):295–296. doi: 10.3969/j.issn.1007-3299.2007.04.034. [DOI] [Google Scholar]
- 34.Lin X.H. The practice of constraint-induced aphasia therapy for treatment of broca aphasia. Health Research. 2017;37(3):332–333. doi: 10.3969/j.issn.1674-6449.2017.03.032. [DOI] [Google Scholar]
- 35.Xie Y., Liu H.L., Wu C.W., Li X.Y., Zheng P., Chen C. Effect of constraint-induced aphasia therapy on chronic aphasia after stroke. Chin J Rehabil Theory Pract. 2014;20(11):1011–1013. doi: 10.3969/j.issn.1006-9771.2014.11.004. [DOI] [Google Scholar]
- 36.Zhao Y.J., Chen C.X., Pang H.W., Song J.P. Effect of constraint-induced language therapy on aphasia in patients with sub-acute stroke. Chin J Rehabil Theory Pract. 2014;20(7):656–658. doi: 10.3969/j.issn.1006-9771.2014.07.012. [DOI] [Google Scholar]
- 37.Zeng Z.P., Liu Y.B., Fang J.J., Liu Y., Luo J., Yang M. Effects of Baduanjin exercise for knee osteoarthritis: a systematic review and meta-analysis. Complement ther med. 2020;48 doi: 10.1016/j.ctim.2019.102279. Article 102279. [DOI] [PubMed] [Google Scholar]
- 38.Harry A., Crowe S.F. Is the Boston naming test still fit for purpose? Clin Neuropsychol. 2014;28(3):486–504. doi: 10.1080/13854046.2014.892155. [DOI] [PubMed] [Google Scholar]
- 39.Beattey R.A., Murphy H., Cornwell M., Braun T., Stein V., Goldstein M. Caution warranted in extrapolating from Boston naming test item gradation construct. Appl Neuropsychol Adult. 2016;24(1):65–72. doi: 10.1080/23279095.2015.1089505. [DOI] [PubMed] [Google Scholar]
- 40.Sheppard C., Kousaie S., Monetta L., Taler V. Performance on the Boston naming test in bilinguals. J Int Neuropsychol Soc Jins. 2016;22(3):350–363. doi: 10.1017/S135561771500123X. [DOI] [PubMed] [Google Scholar]
- 41.Jokel R., Kielar A., Anderson N.D., Black S.E., Rochon E., Graham S. Behavioral and neuroimaging changes after naming therapy for semantic variant primary progressive aphasia. Neuropsychologia. 2016;89:191–216. doi: 10.1016/j.neuropsychologia.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 42.Wang J., Song W.Q., Wu D.Y., Yuan Y. Identifying the damaged level of language processing in an optic aphasic with pure alexia using psycholin⁃guistic assessment in Chinese aphasia. Chin J Rehabil Med. 2012;27(8):708–712+723. doi: 10.3969/j.issn.1001-1242.2012.08.005. [DOI] [Google Scholar]
- 43.Stahl B., Mohr B., Dreyer F.R., Lucchese G., Pulvermüller F. Using language for social interaction: communication mechanisms promote recovery from chronic non-fluent aphasia. Cortex. 2016;85:90–99. doi: 10.1016/j.cortex.2016.09.021. [DOI] [PubMed] [Google Scholar]
- 44.Breitenstein C., Grewe T., Flöel A., Ziegler W., Springer L., Martus P. Intensive speech and language therapy in patients with chronic aphasia after stroke: a randomised, open-label, blinded-endpoint, controlled trial in a health-care setting. Lancet. 2017;389(10078):1528–1538. doi: 10.1016/S0140-6736(17)30067-3. [DOI] [PubMed] [Google Scholar]
- 45.Brady M.C., Kelly H., Godwin J., Enderby P., Campbell P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2016;6 doi: 10.1002/14651858.CD000425.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis C.H., Harrington G. Intensive semantic intervention in fluent aphasia: a pilot study with fMRI. Aphasiology. 2006;20(1):59–83. doi: 10.1080/02687030500331841. [DOI] [Google Scholar]
- 47.Meinzer M., Rodriguez A.D., Rothi L.J.G. First decade of research on constrained-induced treatment approaches for aphasia rehabilitation. Arch Phys Med Rehabil. 2012;93(1):S35–S45. doi: 10.1016/j.apmr.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Netting M., Gold M., Quinn P., El-Merhibi A., Penttila I., Makrides M. Randomised controlled trial of a baked egg intervention in young children allergic to raw egg but not baked egg. World Allergy Organ J. 2017;10(1):22. doi: 10.1186/s40413-017-0152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grzybowski A., Kanclerz P. Language bias and methodological issues in determining reliable evidence for systematic reviews. JAMA Ophthalmol. 2019;137(1):118–119. doi: 10.1001/jamaophthalmol.2018.4945. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.