Abstract
Pathogens originating from wildlife (zoonoses) pose a significant public health burden, comprising the majority of emerging infectious diseases. Efforts to control and prevent zoonotic disease have traditionally focused on animal-to-human transmission, or “spillover.” However, in the modern era, increasing international mobility and commerce facilitate the spread of infected humans, nonhuman animals (hereafter animals), and their products worldwide, thereby increasing the risk that zoonoses will be introduced to new geographic areas. Imported zoonoses can potentially “spill back” to infect local wildlife—a danger magnified by urbanization and other anthropogenic pressures that increase contacts between human and wildlife populations. In this way, humans can function as vectors, dispersing zoonoses from their ancestral enzootic systems to establish reservoirs elsewhere in novel animal host populations. Once established, these enzootic cycles are largely unassailable by standard control measures and have the potential to feed human epidemics. Understanding when and why translocated zoonoses establish novel enzootic cycles requires disentangling ecologically complex and stochastic interactions between the zoonosis, the human population, and the natural ecosystem. In this Review, we address this challenge by delineating potential ecological mechanisms affecting each stage of enzootic establishment—wildlife exposure, enzootic infection, and persistence—applying existing ecological concepts from epidemiology, invasion biology, and population ecology. We ground our discussion in the neotropics, where four arthropod-borne viruses (arboviruses) of zoonotic origin—yellow fever, dengue, chikungunya, and Zika viruses—have separately been introduced into the human population. This paper is a step towards developing a framework for predicting and preventing novel enzootic cycles in the face of zoonotic translocations.
Introduction
Humans have frequently enabled pathogens to overcome physical barriers to dispersal [1]. The European conquest of the Americas brought Old World diseases to the New World, movement of troops during World War II propagated dengue viruses (DENVs) across the Asia-Pacific region [2], and air travel has provided an international transmission network for emerging infectious diseases (EIDs), such as the 2019 (ongoing) severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic [3], the 2002 to 2003 SARS-CoV-1 outbreak [4], and pandemic influenza [5]. Today, the majority of pathogens that infect humans are broadly distributed across geographic regions—globalized by human movement and population expansion, particularly during the past century [1]. Animal pathogens have likewise spread globally through anthropogenic channels. The globalization of agriculture has expanded the geographic range of many livestock diseases with major economic repercussions, which continue to disproportionately affect the developing world [6]. Domestic and wild animals translocated by humans have introduced their pathogens to new ecosystems, threatening biodiversity conservation—an anthropogenic impact termed “pathogen pollution” [7]. In some cases, these invasive animal infections have maintained transmission postemergence in local wildlife, establishing persistent reservoirs that subsequently reseed transmission and thwart control efforts in the original animal host population. Examples include African swine fever virus in Eastern Europe, where a novel enzootic cycle of the invasive livestock pathogen in wild boars has prevented disease eradication [8,9], and rabies virus in Africa, where human-mediated dispersal of domestic dogs established wild carnivore reservoirs that now contribute to rabies persistence in both wildlife and human communities [10].
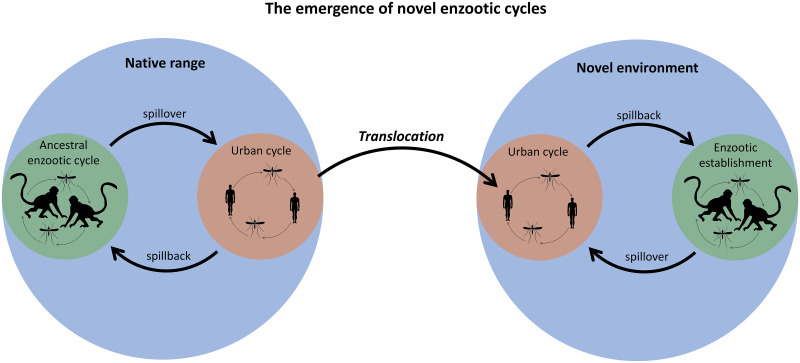
Clearly, the global spread of zoonoses poses a unique and critical threat to human health. Novel enzootic cycles occur when zoonoses are introduced to new regions, infect local wildlife (spillback), and persist in local animal host populations (enzootic establishment). Fig 1 provides a diagram of these processes, and Table 1 provides definitions of all terms in this paper. Now, more than ever, global conditions are ideal for the generation of novel enzootic cycles. In an increasingly connected world, international trade and travel provide pathways for pathogen introductions, while the recent surge in the emergence and reemergence of animal pathogens has increased the number of zoonoses poised to exploit those pathways [11]. Human population expansion into natural habitats is intensifying contact between humans and animals, creating more opportunities for imported zoonoses to spill back into naïve wildlife populations [12]. The probability that these introduced infections persist in animal populations is increasing as human development pushes wildlife into crowded habitat patches and climate change alters transmission conditions [7].
Fig 1. A diagram of the processes by which novel enzootic cycles emerge.
Table 1. Definitions of terms used in this paper.
| Term | Definition |
|---|---|
| Zoonosis | An animal pathogen that can also infect humans |
| Spillover | Animal-to-human transmission |
| Spillback | Human-to-animal transmission |
| Propagule pressure | The number, and temporal and spatial distribution of wildlife exposures to a translocated zoonosis |
| Permeability | The likelihood that humans and potential wildlife hosts, along with the translocated zoonosis, enter the boundary region at the human–wildlife interface |
| Realized niche | The set of hosts, vectors, and ecophysiological requirements that characterize existing transmission cycles of a translocated zoonosis |
In this era of globalization, zoonoses are increasingly being recognized as global threats. The emergence of SARS-CoV-2 in Wuhan, China, has since affected 210 countries and territories, causing nearly 5 million cases and 325,000 deaths worldwide as of May 21, 2020 [13]. The pandemic has prompted an extraordinary global response—many countries have imposed nationwide lockdowns and closed their borders, nonessential international travel has largely been suspended [14], warring countries have declared cease-fire [15], and the World Health Organization (WHO) and United Nations have led international health and humanitarian organizations in mobilizing unprecedented funds for mitigating the spread and impact of the virus [16]. Previously, the 2002 to 2003 SARS-CoV-1 epidemic prompted efforts to build infrastructure for global health security [17], and WHO has declared recent outbreaks of Ebola, H1N1, and Zika virus (ZIKV) as public health emergencies of international concern (PHEICs) [18]. Nevertheless, this dialogue on the globalization of infectious disease continues to conflate zoonoses and human-specific pathogens, often overlooking what makes the spread of zoonoses so uniquely dangerous—the potential for enzootic reservoirs to establish in previously naïve regions. Some zoonoses such as Ebola virus and SARS-CoV-1 have remained within the human population, never spilling back to infect wildlife, after introductions to new regions. Conversely, introductions of yellow fever virus (YFV) in South America, Yersinia pestis (plague) in the Americas [19], rabies virus in parts of Africa, and West Nile virus in North America infected and persisted in local wildlife, inhibiting control and eradication efforts [10,20,21]. The enzootic establishment of YFV in South America is a particularly noteworthy case because three additional Old World arboviruses—DENV, chikungunya virus (CHIKV), and ZIKV—have since been introduced to the New World human population. All three arboviruses now circulate in the same urban transmission cycle as YFV in the South American human population, raising the question: Will their transmission remain within the human population, or will novel enzootic cycles emerge [22–25]? Identifying mechanisms that shape the outcome of zoonotic translocations is critical for developing strategies to mitigate the public health consequences of global transmission networks.
An emerging body of literature is beginning to discuss the risk that human-to-animal transmission will seed persistent enzootic reservoirs [22–25], but, overall, disease emergence and spillover from wildlife continues to dominate the conversation on zoonotic transmission. Our understanding of enzootic establishment is limited by the difficulty in quantifying a process that is both highly stochastic and the product of interactions between multiple systems. In this Review, we provide a conceptual framework to begin disentangling this ecological complexity, applying concepts from disease ecology, invasion biology, and population ecology. Cross-species pathogen emergence has previously been compared to species invasions [26] and population ecology used to understand postintroduction persistence [27] in the context of zoonotic spillover in human populations and host shifts within wildlife communities. Adapting this interdisciplinary theory on pathogen emergence to enzootic establishment, we review potential ecological mechanisms affecting the probability that translocated zoonoses emerge in novel enzootic cycles. We discuss the impact of each mechanism on the process of enzootic establishment: (1) Local wildlife becomes exposed, (2) the zoonosis successfully infects the novel hosts, and (3) transmission persists indefinitely [28,29] (Fig 2). We ground our discussion in the neotropics, where four arboviruses of zoonotic origin—YFV, DENV, CHIKV, and ZIKV—have separately been introduced into the human population. We additionally discuss the utility of modeling approaches, which we illustrate by building a simulation model for our neotropics case study. Our aim is to delineate the ecological processes that shape the outcome of zoonotic translocations as a first step towards developing a framework for predicting and preventing novel enzootic cycles, and, therefore, we do not discuss other key factors such as immunity, phylogeny, and evolution.
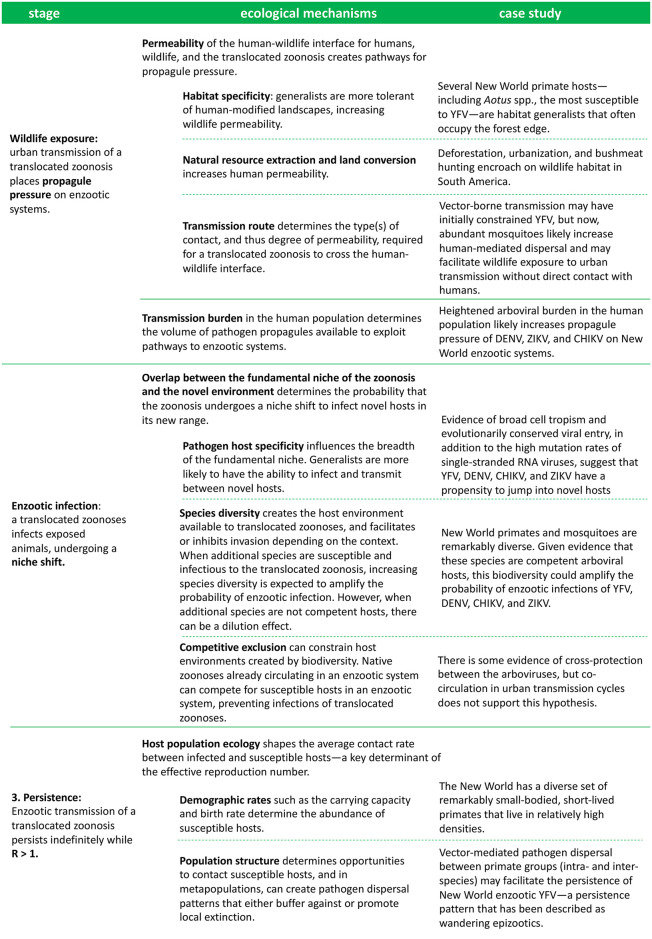
Fig 2. An outline of the ecological mechanisms affecting each stage of enzootic establishment, and their influence on the enzootic potential of translocated arboviruses in the neotropics.
The case study
YFV, DENV, CHIKV, and ZIKV all originated in sylvatic cycles involving nonhuman primates and primatophilic Aedes spp. mosquitoes in either Africa or Southeast Asia. As a result of human introductions, all four now circulate in human urban cycles in the Americas vectored by the anthropophilic mosquitoes Aedes aegypti and A. albopictus [30]. YFV eventually spilled back to infect New World mosquitoes and primates, establishing a novel enzootic cycle that is broadly similar to the sylvatic transmission cycle in which it originated, albeit the taxonomic separation between Old World and New World hosts and vectors [31]. To date, only YFV has successfully established sustained sylvatic transmission in New World primate and mosquito populations [31]. However, given the similar histories of DENV, CHIKV, and ZIKV to that of YFV, there seems a high risk that neotropical mosquitoes and primates will also provide a suitable ecological niche for novel enzootic reservoirs of DENV, CHIKV, and ZIKV. DENV and ZIKV belong to the same genus, Flavivirus, as YFV, and CHIKV (family Togaviridae, genus Alphavirus) belongs to the same phylogenetic group as Mayaro virus (MAYV), an endemic South American zoonosis that circulates in primates and Haemagogus spp. [32]. DENV additionally has spilled back at least once into a novel enzootic system—the virus established a persistent enzootic cycle in Africa after being introduced from Asia [33]—which offers a formidable warning of enzootic establishment in the American tropics.
ZIKV infections have recently been detected in New World primates, suggesting that a persistent enzootic cycle could emerge. Carcasses of free-living Callithrix spp. (marmosets) and Sapajus spp. (capuchins) were found to be infected with ZIKV strains of the ZIKV lineage currently circulating in the South American human population [34], and several monkeys have tested PCR-positive [35,36]. Mosquito surveillance in Brazil additionally detected an amplicon of DENV in a pool of primatophilic Haemagogus leucocelaenus [37]. Sylvatic YFV now feeds recurring human epidemics in South America, allowing urban YFV transmission to continue despite vaccination campaigns. Thus, preventing the other three arboviruses as well as any new introductions from also establishing persistent enzootic reservoirs will be critical for forestalling further human morbidity and mortality from zoonotic transmission in the American tropics. However, the majority of the work on these imported arboviruses has focused on retrospective analysis of the conditions that enabled their introductions—particularly the global invasion of mosquito vectors A. aegypti and A. albopictus—and the transmission burden in the human population [38–41]. Only a few recent papers have begun to discuss the threat of enzootic establishment [22–25,42]. We add to this discussion by considering how each ecological mechanism identified in our Review may affect the trajectory of DENV, CHIKV, and ZIKV in South America, using YFV as a frame of reference.
Wildlife exposure
Once a translocated zoonosis has established in a new human system, there is an immediate risk that the pathogen spills back into local wildlife populations. The probability of spillback first depends on the rate at which wildlife is exposed, which can be captured by propagule pressure—a concept from invasion biology that represents the number and temporal and spatial distribution of nonnative individuals introduced to a new system—and is a key determinant of invasion success [43,44].
Propagule pressure hinges on introduction pathways between a source and recipient population. The propagule pressure of a translocated zoonosis on local wildlife will vary based on the availability of transmission pathways between the human (source) and wildlife (recipient) populations. Borrowing from landscape and movement ecology, Borremans and colleagues [45] identified permeability—the likelihood that source and recipient hosts, along with the pathogen, enter an ecosystem boundary region—as the ecological basis of pathways available for cross-species pathogen emergence across ecosystem boundaries. With respect to the human–wildlife boundary, permeability for translocated zoonoses will increase with wildlife tolerance of (or preference for) anthropogenically modified landscapes and human communities’ proximity to the edge of a species’ habitat and incursions into natural habitat for resource extraction.
Host boundary permeability creates opportunities for contacts between infected source and recipient hosts, increasing propagule pressure on the recipient host population. Transmission route determines the type(s) of contact, and thus degree of permeability, required for the translocated zoonosis to cross the human–wildlife interface [45,46]. Zoonotic introductions can occur via direct contacts such as bushmeat hunting or the wildlife trade—common in the developing world—or via indirect mechanisms such as environmental contamination—e.g., if infected bats leave saliva on forest fruits consumed by humans or shed excreta in the human environment [47]. For directly transmitted zoonoses, propagule pressure on local enzootic systems will require sufficient permeability for humans and wildlife to come into close contact. Conversely, zoonoses that can survive outside their hosts will be less constrained by host boundary permeability. Domestic animals often intersect with both humans and wildlife and, thus, have the potential to bridge transmission between the two populations. Vectors can likewise function as bridge hosts; as long as a competent vector is present, vector-borne zoonoses only require some degree of spatial and temporal overlap to transmit between humans and wildlife.
Transmission burden in the human population inhabiting the new region—a combination of time since introduction and the number of subsequent human cases—will determine the volume of pathogen propagules available to exploit transmission pathways to local wildlife [48]. Consistent circulation and a high number of cases in the human population may result in more opportunities to spill back into enzootic transmission cycles, producing greater propagule pressure. The precise propagule pressure that led YFV to invade New World nonhuman primate populations is unknown, but phylogenetic analyses suggest multiple spillback introductions [49,50]. Evidence that YFV reached its current widespread distribution in South America through long-distance, human-mediated dispersal implies that many spillback introductions occurred across a broad spatiotemporal landscape.
Vector-borne transmission may limit opportunity for spillback introductions to wildlife populations during periods of robust vector control efforts. Notably, in the 20th century, A. aegypti eradication campaigns significantly reduced the YFV burden, to the point where health officials erroneously considered the arbovirus to be eradicated from the New World [21]. Following relaxation of eradication efforts, A. aegypti populations rebounded and A. albopictus invaded [38]. These vectors increase arboviral boundary permeability, allowing zoonotic exchange to evade physical barriers (i.e., animals and humans do not need to interact directly or even occupy the same habitat for effective contacts to occur) [51]. A. albopictus populations are often peridomestic, which may further bridge urban and sylvatic systems [42]. It has been hypothesized that human-mediated movement of infected vectors played a significant role in the spread of enzootic YFV [50]. Human-mediated vector dispersal and vector capacity to transmit between species without direct contacts have the potential to similarly facilitate enzootic invasion of DENV, CHIKV, and ZIKV.
Several New World primates are considered habitat generalists, with high permeability of human-modified landscapes, likely increasing opportunities for human-to-animal pathogen introductions. In particular, Aotus spp. (howler monkeys)—the New World primate most susceptible to YFV—often occupy the forest edge and have been hypothesized to bridge urban and enzootic transmission of YFV [52]. At the same time, deforestation, urbanization, and bushmeat hunting are pushing humans into wildlife habitats [53,54].
Inconsistent circulation in the human population likely limited YFV propagule pressure on New World nonhuman primates. A virulent pathogen, YFV historically emerged intermittently in large, deadly outbreaks in human cities, relying on reintroductions along shipping routes [21]. However, in recent decades, unprecedented population growth, combined with climate change and the reinvasion of A. aegypti, has fueled an increase in the frequency and magnitude of arboviral epidemics in the neotropics [55]. Between 1980 and 2007, the number of reported DENV cases in the Americas increased 4.6-fold [56,57] and, in 2019, exceeded 3 million, surpassing a previous record of 2.4 million [58]; the 2013 introduction of CHIKV resulted in 2.9 million cases within the following three years [59], and the 2015–2016 ZIKV pandemic reached 48 countries and territories [60]. Furthermore (unlike YFV), DENV, ZIKV, and CHIKV lack available, safe vaccines [61]. This heightened arboviral burden has the potential to increase propagule pressure of DENV, ZIKV, and CHIKV on New World wildlife populations, accelerating the timeline between translocation and enzootic establishment.
Enzootic infection
Not all wildlife exposures result in enzootic infections. To progress to the second step of enzootic establishment, the translocated zoonosis must be able to infect the exposed animals. Infecting novel host species in a novel environment can be described as a niche shift. The concept of an ecological niche has many nuanced definitions in ecology, but generally represents the set of abiotic and biotic conditions that allow a species to occupy a particular space within an ecosystem [62]. A pathogen niche is defined by its hosts, vectors, ecophysiological requirements and the many ways in which these parts interact [63,64]. Like other species, a translocated zoonosis will have a realized niche—existing transmission cycles—and a fundamental niche—the range of systems the zoonosis could theoretically invade if given the opportunity [63]. The probability that the zoonosis undergoes a niche shift to infect novel hosts in its new range depends on the degree of overlap between its fundamental niche and novel environment [62].
Host specificity influences the breadth of the pathogen’s fundamental niche. Generalists are defined by broad fundamental host ranges [65], which, intuitively, will intersect with a wider range of enzootic systems, facilitating shifts to novel hosts [66–68]. Alternatively, zoonoses can evolve to invade environments outside of their original fundamental niches [62]. Some pathogen types inherently have higher potential for fundamental niche shifts than others. In particular, YFV, DENV, CHIKV, and ZIKV are all single-stranded RNA viruses—a group of pathogens previously shown to be the most likely to shift host species, predisposed to cross-species emergence by high mutation rates [28]. Species diversity creates the host environment available to a translocated zoonosis. Disease ecologists have described a complex relationship between biodiversity and pathogen transmission within a given focal host species, where increasing diversity can have either an amplification or dilution effect on transmission, largely contingent on changes in community capacity to support infection (community competence) [69,70]. Similarly, biodiversity in enzootic systems may either facilitate or inhibit the invasion of a translocated zoonosis depending on the abundance and distribution of competent hosts and vector species—susceptible to the zoonosis and infectious enough to transmit to the next susceptible individual. When increasing biodiversity adds competent host and vector species, we expect an amplified probability that wildlife exposures result in enzootic infections. However, adding low-competence species may cause a dilution effect, in which wildlife exposures are increasingly “wasted” on hosts that cannot support infection. Additionally, competition among infectious agents can constrain host environments created by biodiversity. Native zoonoses already circulating in an enzootic system can compete for susceptible hosts, driving the competitive exclusion of a translocated zoonosis [71–73].
The “complete” host ranges of YFV, DENV, ZIKV, and CHIKV are not known, as it is practically infeasible to detect every enzootic infection. However, evidence of broad cell tropism and evolutionarily conserved viral entry strategies [74,75] suggest wide fundamental host ranges which are more likely to launch into novel systems [76]. Phylogenetic analysis has demonstrated the relative ease with which YFV can shift between human and nonhuman primate host types, with multiple sylvatic strains circulating in the human population but no evidence of major genetic adaptations between urban and enzootic transmission cycles [77].
A remarkably diverse assemblage of nonhuman primates and mosquitoes inhabit the neotropics. This biodiversity could amplify the probability of novel enzootic infections because New World primates and mosquitoes are competent hosts of a broad range of arboviruses [24,78]. Previous meta-analyses suggest that the probability of cross-species emergence increases as the phylogenetic distance between novel and original host species decreases (i.e., as hosts become more closely related) [67,68,79–82]. Thus, YFV, DENV, ZIKV, and CHIKV may be predisposed to shift to New World monkeys and arboreal mosquito vectors, which are phylogenetically related to the Old World monkeys and Aedes spp. that maintain sylvatic YFV, DENV, ZIKV, and CHIKV in Africa and Asia [31]. That being said, New and Old World monkeys and mosquitoes could be divergent in critical immune factors and/or cell-surface receptors involved in viral infection. Nevertheless, experimental infection has demonstrated that neotropical primates are competent hosts for ZIKV and DENV [83–86], neotropical H. leucocelaenus and A. terrens are competent vectors for CHIKV [25], and Sabethes cyaneus is a competent vector for ZIKV, although significantly less competent than A. aegypti [87]. However, even if neotropical primatophilic mosquito species have limited capacity to vector DENV, ZIKV, or CHIKV, as humans encroach on forest habitat, anthropophilic vectors A. aegypti and A. albopictus could play an increasingly important role in sustaining enzootic cycles in peridomestic urban forests [42].
Evidence of cross-protective effects that could drive competitive exclusion of DENV, CHIKV, and ZIKV from New World enzootic systems is inconclusive. Speculation that hyperendemic DENV has conferred widespread cross-immunity against YFV in Asia—where YFV has remained absent despite the presence of suitable vectors and an entirely susceptible human population—has since been challenged [31,88]. Additionally, there is no evidence of reciprocal crossprotective effects that would allow YFV to exclude DENV from New World enzootic systems [89]. It has been hypothesized that ZIKV crossprotective immunity against DENV underlies the decline in DENV incidence following the first ZIKV outbreaks observed in Brazil [90] and Colombia [91]; however, neutralization assays have not supported this hypothesis [92]. A recent experimental infection study in mice suggests strong cross-protection of CHIKV against MAYV—the endemic alphavirus that circulates in South American primates and Haemagogus spp. [93]. However, there is no evidence of reciprocal crossprotective effects that would allow MAYV to exclude CHIKV from New World enzootic systems [89].
Persistence
The outcome of spillback events depends on the potential for transmission between individuals in the novel animal host population. If animal transmission is limited, spillback might result in an isolated wildlife case or, alternatively, trigger an outbreak that threatens conservation efforts but eventually dies out [94,95]. However, above a critical transmission threshold, the translocated zoonosis will persist indefinitely—the final step of successful enzootic establishment. In disease ecology and epidemiology, that critical transmission threshold is represented by the effective reproduction number (R)—the average number of secondary cases generated by a single infected individual in a population of susceptible and nonsusceptible hosts. While R is greater than 1, each infected individual will, on average, produce at least one secondary infection, allowing the pathogen to persist. The effective reproduction number is a function of pathogen attributes, such as transmissibility and duration of infectiousness, as well as the average rate of contact between infected and susceptible individuals (and vectors if vector-borne) in a given population.
The average contact rate between infected and susceptible hosts is largely shaped by population ecology [96]. Dynamic demographic rates and structuring of host populations determine the abundance, distribution, and movement of hosts available to translocated zoonoses in enzootic systems. Wildlife populations with high carrying capacities will have larger baseline populations of susceptible hosts. High birth rates replenish the supply of susceptible hosts, inhibiting mortality and conferred immunity from depleting the susceptible population and driving the effective reproduction below the threshold of persistence [97]. Spatial structuring of susceptible hosts can either limit or enhance the potential for pathogen persistence. Pathogen dispersal between patches can promote persistence across a metapopulation by buffering against local depletion of susceptible individuals. On the other hand, spatial structure can limit contacts between patches, lowering the effective reproduction number and driving an epidemic to extinction [96,98].
While some New World monkeys are large species with low birth rates, one of the clade’s defining features is its diverse set of remarkably small-bodied, short-lived primates. For example, the pygmy marmoset (Callithrix pygmaea) is a small-bodied New World primate with bimodal annual birth peaks, high twin birth rates, and a natural life span of about 10 years [99]. These smaller-bodied primates also tend to require smaller home ranges and live in higher densities, allowing for greater sympatric species richness. A meta-analysis of New World primate assemblages found that, on average, forest sites contained six sympatric species but this number could reach as high as 14 species, peaking near the equator [100]. New World enzootic mosquito species occupy the canopy, preying primarily on primates. These vectors do not appear to demonstrate strong host preferences and, thus, likely bridge transmission between sympatric groups of primate species. This spatial structure—vector-mediated pathogen dispersal between primate groups (intra- and interspecies)—may have facilitated the enzootic establishment of YFV. It has been hypothesized that enzootic YFV persists within primate metapopulations occupying continuous forest in wandering epizootics, in which transmission continually shifts between subpopulations. We suspect that the demographic rates and structuring of primate host and mosquito vector populations in the New World would, as with YFV, facilitate the persistence of DENV, CHIKV, and ZIKV should they spill back successfully.
The ecology of enzootic establishment in the Anthropocene
Anthropogenic impacts are affecting ecological processes at every stage of enzootic establishment. Wildlife exposure to urban transmission of translocated zoonoses will likely increase as humans continue to encroach on wildlife habitats [2,12,22,23,101]. Land conversion and extraction of natural resources drive humans, mosquito vectors, and primates to coincide in human-modified landscapes, potentially increasing the boundary permeability of the translocated arboviruses. Climate change will alter the epidemiology of zoonoses, particularly vector-borne zoonoses, substantially reducing transmission at temperature extremes, but increasing transmission in moderate warming scenarios [102]. Rapid population growth and the global expansion of mosquito vectors contribute to heightened zoonotic transmission burden in the human population, which subsequently places greater propagule pressure on enzootic systems. Species composition is changing in many ecosystems, which can facilitate or inhibit pathogen invasions depending on whether lost species are competent hosts [70]. However, habitat specialists are highly sensitive to anthropogenic impacts, whereas habitat generalists—which often bridge transmission between urban and enzootic systems—often persist [103]. By increasing the concentration of competent hosts, anthropogenic change can have an amplification effect on enzootic infection. Habitat loss is additionally pushing animals into dense populations ripe for disease persistence [7].
Recent trends in enzootic YFV reflect the changing ecology of enzootic establishment in the Anthropocene. The past decade has seen a surge in the frequency and magnitude of YFV epizootics in South America. The discovery of cocirculating sylvatic transmission cycles during the 2016 to 2017 YFV epidemic in Brazil implies multiple spillback introductions on a local scale across a short timespan [77]. Additionally, enzootic YFV has invaded previously nonendemic regions, significantly expanding its range in the New World.
A case for modeling
It is challenging to approach the ecological complexity of enzootic establishment through field and experimental studies alone. Mathematical models can however be a useful tool that allows us to integrate existing data and ecological theory to elucidate system dynamics, particularly when data are sparse, as is often the case with enzootic systems [22,104,105]. Many modeling approaches can be applied to a range of questions that allow us to better understand the risk that translocated zoonoses will emerge in novel enzootic cycles. For example, species distribution models, or ecological niche models—statistical approaches that leverage associations between presence-absence information and environmental variables to infer habitat suitability—can be used to identify at-risk systems where high permeability of humans, vectors, and translocated zoonoses create ideal conditions for enzootic establishment [46,106–108]. Metapopulation modeling is often an important tool to demonstrate conditions of pathogen persistence in wildlife populations, given that they are typically fragmented [96]. Next-generation matrix methods are a useful tool to quantify the effective reproduction number of translocated zoonoses in novel enzootic systems to understand the probability of successful invasion [109]. Explicit simulations that capture significant amounts of the complexity of systems have been effectively used to compare the impact of interventions in the human and wildlife population [110]. We would also argue that simple models can be very useful in helping us understand the system-specific dynamics that influence the ecological processes underlying enzootic establishment. For example, Althouse and colleagues [22] developed the only previous model of vector-borne transmission in nonhuman primate hosts [22,104,105] and showed that whether ZIKV persists enzootically in South America is highly dependent on primate birth rates and mosquito population sizes. Based on model outcomes for the range of parameter values estimated to apply to the neotropics, they concluded that ZIKV has a high potential for enzootic establishment in the New World.
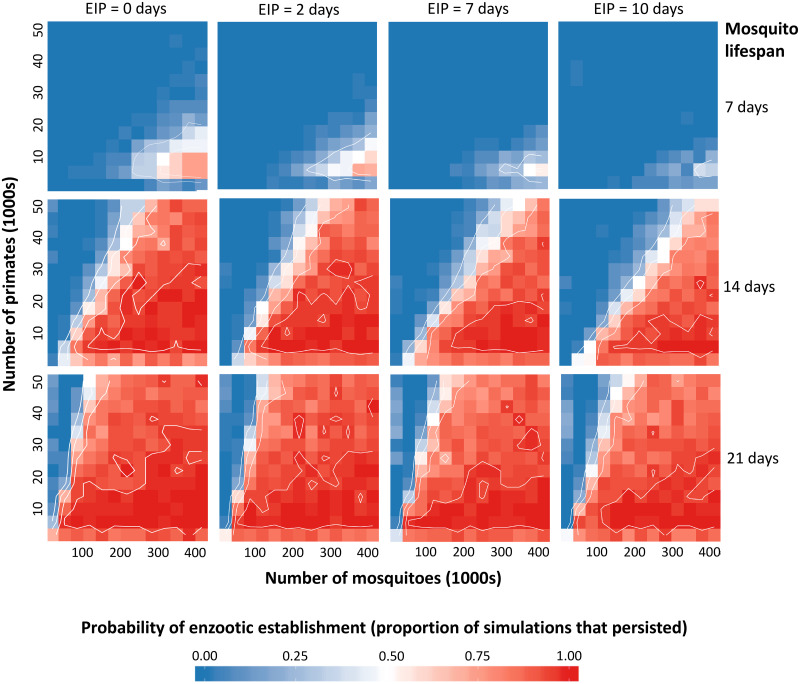
The modeling approach of Althouse and colleagues [22] can be applied to all four translocated arboviruses circulating in the neotropics. In particular, we can examine how key differences between the different viruses may impact their relative risk of enzootic establishment. Specifically, the extrinsic incubation period (EIP)—the delay from initial infection until transmission is possible—varies between YFV, DENV, CHIKV, and ZIKV [111–114]. The EIP helps determine the length of the mosquito infectious period, defining onward transmission [115] and, therefore, has the potential to impact the risk of spillback. However, a model is needed to explore whether these differences are likely to be relevant, particularly in the context of the long lifespans of New World sylvatic mosquitoes in South American enzootic systems. To examine this question, we built on the model of Althouse and colleagues [22] and simulated the introduction of a single infected primate within a multihost metapopulation model to explore how a spillback event might play out for all four translocated arboviruses given New World mosquito lifespans (see the Supplementary Information for a more detailed description of the model methods). Except for the primate birth rate (which we hold constant), we reproduce their range of parameter values, additionally varying the length of the EIP to reflect differences between the arboviruses and the mosquito life span to reflect differences between species and environmental conditions. Given that EIP and mosquito life span are highly variable across conditions, the values selected for our simulations were not meant to perfectly describe the four arboviruses or particular mosquito species; instead, we aimed to capture the range of values that have been observed across arboviruses and environmental conditions to understand general trends in the effect of EIP and life span on the probability of enzootic establishment. For EIP, we selected values between 2 (reflecting the lower bound for CHIKV [111]) and 10 days (approximating the longer EIP of ZIKV [87]). For the mosquito life span, we used 7 days—taken from the previous model of enzootic vector-borne transmission in primates [22]—as our starting value and selected two additional values at 7 day intervals: 14 days approximately represents mean values from mark–release–recapture studies in South America for A. albopictus in field conditions [116], and 21 days approximately represents conservative mean values for Haemogogus spp. and Sabethes spp. at warmer temperatures [117]. For each set of values, we ran 50 simulations, calculating the probability of persistence as the proportion of simulations in which infected primates remained at the end of the three-year period.
At shorter mosquito lifespans, EIP length affected the probability of persistence; increasing the EIP to 10 days, as we might observe with ZIKV, decreased the probability of persistence, whereas shortening EIP to 2 days, as we might observe with CHIKV or at warm temperatures, increased the probability of persistence (Fig 3). However, extending the mosquito life span negated this effect; when the mosquito life span reflects New World sylvatic species and warm temperatures at 21 days, there is a relatively high probability of sylvatic establishment across all EIP values. Long-lived sylvatic mosquitoes are hypothesized to play a substantial role in YFV maintenance in the neotropics [118], which may be part of the reason why YFV has established and maintained enzootic transmission despite an EIP of 7 days. These results also suggest that despite differences in EIP, there may be a particularly high risk of enzootic establishment for DENV, CHIKV, and ZIKV in the New World due to naturally longer-lived sylvatic species and warmer temperatures, which both shorten EIP and extend mosquito lifespans. This work is important in highlighting the need for surveillance efforts to be equally vigilant of DENV, CHIKV, and ZIKV spillback in the New World. The results give a good example of how models can be useful in our understanding of complex ecological interactions. In this case we may have expected that difference in EIP may have been important in determining relative risk of enzootic establishment; however, due to longer mosquito lifespans, our model suggests that these differences are unlikely to be relevant.
Fig 3. Model results predicting the probability of establishment across mosquito birthrates and EIPs.
Mosquito birthrate is equivalent to the inverse of life span (1/life span) and increases from the top to bottom panels, while the EIP increases left to right. Within each panel, the total population size of mosquitoes (in two populations) and primates (in two populations) changes horizontally and vertically, respectively. For each parameter set, we simulated the introduction of a single infected primate and subsequent transmission for a three-year period. Blue indicates no simulations establishing, whereas red indicates all simulations establishing. Contour lines show 0.25, 0.5, 0.75, and 0.95 probability of establishment. EIP, extrinsic incubation period.
Discussion
The goal of this study is to stimulate research on the emergence of novel enzootic cycles and begin to disentangle the underlying ecology complexity. We have argued here that the establishment of novel enzootic cycles is a pressing threat with the capacity to dramatically alter disease dynamics. The International Task Force for Disease Eradication identifies the existence of an animal reservoir as a barrier to eradicating a disease because enzootic transmission often feeds human epidemics [119]. In some cases, enzootic cycles have even contributed to the evolution of pandemic pathogens; for example, pigs have functioned as “mixing vessels” for the evolution of pandemic swine influenza [120]. We delineated potential ecological mechanisms at each stage of enzootic establishment, grounding our discussion in the neotropics, where the danger of enzootic establishment is evident in the history of YFV and an ongoing threat given the endemic circulation of DENV, CHIKV, and ZIKV in the human population. Enzootic YFV, which has triggered devastating human epidemics across the neotropics, has expanded its geographic range since its initial establishment [121]. There is a real danger that DENV, CHIKV, and ZIKV will also establish persistent enzootic reservoirs in the New World, similarly inhibiting efforts to prevent future human epidemics. Given that enzootic cycles are nearly impossible to control or eradicate, avoiding enzootic establishment will be critical to mitigate the current arbovirus public health emergency in the New World. Moreover, enzootic cycles can thwart efforts to eradicate pathogens in the human population, as has occurred with the carriage of Guinea worm by dogs [122]. In particular, the recent discovery of natural ZIKV [34–36] infection in nonhuman primates in Brazil calls for renewed urgency to understand the potential for enzootic persistence.
Now, there is significant concern that SARS-CoV-2 could spill back into susceptible wildlife within its expanded geographic range and establish novel enzootic reservoirs, becoming endemic outside of China. The high burden and global distribution of human SARS-CoV-2 transmission places propagule pressure on a wide range of enzootic systems. Bats—the putative reservoir of SARS-CoV-2 [123]—are the second most diverse mammalian group, inhabit every continent except Antarctica, and harbor a large diversity of coronaviruses [124]. Analysis of angiotensin converting enzyme 2 (ACE2)—the cell-surface receptor implicated in SARS-CoV-2 invasion of host cells—across a subset of bat species has predicted that some bats are highly susceptible to human-adapted SARS-CoV-2 [125], and crossmammal analyses suggest that the virus may have the potential to establish in a broad range of other mammalian species [126–128]. There is also a possibility that human-adapted SARS-CoV-2 could infect initially unsuitable host species through mutation events [129]. To mitigate the risk that SARS-CoV-2 establishes novel enzootic reservoirs, it is critical to identify susceptible wildlife species and populations and implement policies that limit their exposure to the virus. In response to the pandemic, the US government has, at present, suspended all bat research to prevent humans from infecting and seeding an enzootic reservoir of SARS-CoV-2 in North American bats [130], and many countries have banned bat bushmeat [131]. Additional policies may be needed to minimize human contact with other potentially susceptible wildlife, particularly populations bordering affected human communities and characterized by demographic rates and structuring predicted to facilitate sustained epidemics and enzootic persistence. Surveillance should monitor whether such populations become exposed and begin to demonstrate capacity for between-host transmission. In particular, researchers should monitor domestic animals predicted to be potential hosts—notably cats [127,132] and cattle [133]—which can bridge transmission between human and wildlife populations [45].
Spillback events in which humans introduce pathogens into wildlife populations may become common occurrences, as urbanization and anthropogenic pressure on wildlife populations increase opportunities for human–wildlife contact. As a result, understanding the risk that translocated zoonoses will persist in sylvatic cycles after spillback events should be established as a research priority. The risk of enzootic persistence depends on a multitude of factors, many of which are unknown or poorly characterized, such as infectivity, number of spillback events, and the transmission conditions needed for persistence. Here we provide a conceptual framework of ecological factors to begin addressing the challenge of predicting this risk. Considering ecological mechanisms is a first step towards developing targeted intervention strategies. We additionally argue for the utility of modeling in detangling ecological complexity, providing a simulation model of arboviral transmission in New World primates and mosquitoes as an example. Our results indicate that although long EIPs can reduce the probability of enzootic persistence, the long mosquito lifespans that are characteristic of tropical New World sylvatic species may negate this effect—suggesting that differences in EIP that we may have expected to be important in determining the translocated arboviruses’ relative risk of enzootic establishment are unlikely to be relevant. Overall, our work is important in highlighting the need to be vigilant of imported zoonoses and emphasizing the importance of robust programs to mitigate the risk of spillback events that lead to enzootic persistence.
Key learning points
The globalization of zoonoses—capable of both infecting humans and establishing persistent enzootic reservoirs of transmission in new regions—poses a unique and critical threat to human health. Understanding the risk that translocated zoonoses spill back and establish reservoirs in novel wildlife hosts should be established as a research priority, particularly in the era of SARS-CoV-2.
Novel enzootic cycles occur when zoonoses are introduced to new regions (translocation), infect local wildlife (spillback), and persist in local animal host populations (enzootic establishment).
Understanding when and why translocated zoonoses establish novel enzootic cycles requires disentangling ecologically complex and stochastic interactions between the zoonosis, the human population, and the natural ecosystem.
Mathematical modeling can inform risk assessments by leveraging existing empirical data. For example, simulation modeling indicates that long EIPs in the mosquito can reduce the probability of enzootic persistence, but the long mosquito lifespans that are characteristic of tropical New World sylvatic species may negate this effect. These model predictions suggest that while we may have expected differences in EIP to significantly affect the risk that translocated arboviruses establish novel enzootic cycles in the neotropics, these differences are unlikely to be relevant.
Top five papers
Althouse BM, Vasilakis N, Sall AA, Diallo M, Weaver SC, Hanley KA. Potential for Zika Virus to Establish a Sylvatic Transmission Cycle in the Americas. PLoS Negl Trop Dis. 2016 Dec 15;10(12):e0005055.
Weaver SC. Urbanization and geographic expansion of zoonotic arboviral diseases: mechanisms and potential strategies for prevention. Trends in Microbiology. 2013 Aug;21(8):360–3.
Han BA, Majumdar S, Calmon FP, Glicksberg BS, Horesh R, Kumar A, et al. Confronting data sparsity to identify potential sources of Zika virus spillover infection among primates. Epidemics. 2019 Jun;27:59–65.
Lourenço-de-Oliveira R, Failloux A-B. High risk for chikungunya virus to initiate an enzootic sylvatic cycle in the tropical Americas. Vasilakis N, editor. PLoS Negl Trop Dis. 2017 Jun 29;11(6):e0005698.
Hanley KA, Monath TP, Weaver SC, Rossi SL, Richman RL, Vasilakis N. Fever versus fever: The role of host and vector susceptibility and interspecific competition in shaping the current and future distributions of the sylvatic cycles of dengue virus and yellow fever virus. Infection, Genetics and Evolution. 2013 Oct;19:292–311.
Supporting information
(DOCX)
In the case of EIP, this assumption is unrealistic because individuals have an equal probability of leaving the incubation compartment regardless of the time since infection. In reality, the probability of progressing should be very low immediately after infection and highest around the EIP mean—a trajectory better represented by a gamma distribution (in green and purple). A gamma distributed EIP can be constructed in a compartmental model via a boxcar configuration of the latent period (i.e., splitting the latent period up into a series of separate compartments, or boxes). Note how, as the number of latent boxes increases (green versus purple), the gamma distribution becomes less dispersed and more closely centered around the EIP mean. EIP, extrinsic incubation period.
(PDF)
Mosquito birthrate = 1/life span and increases from the top to bottom panels, while EIP increases left to right. Here, we constructed an Erlang-distributed EIP by splitting the exposed compartment into 10 separate boxes. Within each panel, the total population size of mosquitoes (in two populations) and primates (in two populations) changes horizontally and vertically, respectively. For each parameter set, we simulated the introduction of a single infected primate and subsequent transmission for a three-year period. Blue indicates no simulations establishing, whereas red indicates all simulations establishing. Contour lines show 0.25, 0.5, 0.75, and 0.95 probability of establishment. EIP, extrinsic incubation period.
(PPTX)
Mosquito birthrate = 1/life span and increases from the top to bottom panels, while EIP increases left to right. Here, we constructed an Erlang-distributed EIP by splitting the exposed compartment into 50 separate boxes. Within each panel, the total population size of mosquitoes (in two populations) and primates (in two populations) changes horizontally and vertically, respectively. For each parameter set, we simulated the introduction of a single infected primate and subsequent transmission for a three-year period. Blue indicates no simulations establishing, whereas red indicates all simulations establishing. Contour lines show 0.25, 0.5, 0.75, and 0.95 probability of establishment. EIP, extrinsic incubation period.
(PPTX)
Funding Statement
S.G. is supported by the National Science Foundation Graduate Research Fellowship (https://www.nsf.gov) and the RCN-IDEAS Research Exchange Program (https://ideas.princeton.edu/research-exchanges/); M.B. is supported by the National Institutes of Health (GM122061; https://www.nih.gov) and Bioscience for the Future (BB/L010879/1; https://bbsrc.ukri.org); K.A.H. is supported by the National Institutes of Health International Collaborations in Infectious Disease Research (1U01AI115577-01; https://www.nih.gov); and B.M.A. is funded by the National Institutes of Health International Collaborations in Infectious Disease Research (1U01AI115577-01; https://www.nih.gov) and Bill & Melinda Gates through the Global Good Fund (https://www.globalgoodfund.org). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Smith KF, Sax DF, Gaines SD, Guernier V, Guégan J-F. Globalization of human infectious disease. Ecology. 2007;88: 1903–1910. 10.1890/06-1052.1 [DOI] [PubMed] [Google Scholar]
- 2.Gubler DJ. Dengue, Urbanization and Globalization: The Unholy Trinity of the 21st Century. Tropical Medicine and Health. 2011;39: S3–S11. 10.2149/tmh.2011-S05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses. 2020;12: 372 10.3390/v12040372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilder-Smith A, Freedman DO. Confronting the New Challenge in Travel Medicine: SARS. Journal of Travel Medicine. 2006;10: 257–258. 10.2310/7060.2003.2669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan K, Arino J, Hu W, Raposo P, Sears J, Calderon F, et al. Spread of a Novel Influenza A (H1N1) Virus via Global Airline Transportation. New England Journal of Medicine. 2009;361: 212–214. 10.1056/NEJMc0904559 [DOI] [PubMed] [Google Scholar]
- 6.Perry BD, Grace D, Sones K. Current drivers and future directions of global livestock disease dynamics. Proceedings of the National Academy of Sciences. 2013;110: 20871–20877. 10.1073/pnas.1012953108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tompkins DM, Carver S, Jones ME, Krkošek M, Skerratt LF. Emerging infectious diseases of wildlife: a critical perspective. Trends in Parasitology. 2015;31: 149–159. 10.1016/j.pt.2015.01.007 [DOI] [PubMed] [Google Scholar]
- 8.Gogin A, Gerasimov V, Malogolovkin A, Kolbasov D. African swine fever in the North Caucasus region and the Russian Federation in years 2007–2012. Virus Research. 2013;173: 198–203. 10.1016/j.virusres.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 9.Cwynar P, Stojkov J, Wlazlak K. African Swine Fever Status in Europe. Viruses. 2019;11: 310 10.3390/v11040310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lembo T, Hampson K, Kaare MT, Ernest E, Knobel D, Kazwala RR, et al. The Feasibility of Canine Rabies Elimination in Africa: Dispelling Doubts with Data. PLoS Negl Trop Dis. 2010;4: e626 10.1371/journal.pntd.0000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibbs EPJ. Emerging zoonotic epidemics in the interconnected global community. Veterinary Record. 2005;157: 673–679. 10.1136/vr.157.22.673 [DOI] [PubMed] [Google Scholar]
- 12.Hassell JM, Begon M, Ward MJ, Fèvre EM. Urbanization and Disease Emergence: Dynamics at the Wildlife–Livestock–Human Interface. Trends in Ecology & Evolution. 2017;32: 55–67. 10.1016/j.tree.2016.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. Coronavirus Disease 2019 (COVID-19) Situation Report—122. World Health Organization; 2020.
- 14.Salcedo A, Yar S, Cherelus G. Coronavirus Travel Restrictions, Across the Globe. New York Times. 15 Apr 2020.
- 15.Hubbard B, Al-Batati S. Saudi Arabia Declares Cease-Fire in Yemen, Citing Fears of Coronavirus. New York Times. 8 Apr 2020.
- 16.WHO. WHO and UNICEF to partner on pandemic response through COVID-19 Solidarity Response Fund. WHO News Release. 3 Apr 2020.
- 17.Hoffman SJ. The evolution, etiology and eventualities of the global health security regime. Health Policy and Planning. 2010;25: 510–522. 10.1093/heapol/czq037 [DOI] [PubMed] [Google Scholar]
- 18.Hoffman SJ, Silverberg SL. Delays in Global Disease Outbreak Responses: Lessons from H1N1, Ebola, and Zika. American Journal of Public Health. 2018;108: 329–333. 10.2105/AJPH.2017.304245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kugeler KJ, Staples JE, Hinckley AF, Gage KL, Mead PS. Epidemiology of Human Plague in the United States, 1900–2012. Emerging Infectious Diseases. 2015;21: 16–22. 10.3201/eid2101.140564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kilpatrick AM. Globalization, Land Use, and the Invasion of West Nile Virus. Science. 2011;334: 323–327. 10.1126/science.1201010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bryan CS, Moss SW, Kahn RJ. Yellow fever in the Americas. Infectious Disease Clinics of North America. 2004;18: 275–292. 10.1016/j.idc.2004.01.007 [DOI] [PubMed] [Google Scholar]
- 22.Althouse BM, Vasilakis N, Sall AA, Diallo M, Weaver SC, Hanley KA. Potential for Zika Virus to Establish a Sylvatic Transmission Cycle in the Americas. PLoS Negl Trop Dis. 2016;10: e0005055 10.1371/journal.pntd.0005055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weaver SC. Urbanization and geographic expansion of zoonotic arboviral diseases: mechanisms and potential strategies for prevention. Trends in Microbiology. 2013;21: 360–363. 10.1016/j.tim.2013.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han BA, Majumdar S, Calmon FP, Glicksberg BS, Horesh R, Kumar A, et al. Confronting data sparsity to identify potential sources of Zika virus spillover infection among primates. Epidemics. 2019;27: 59–65. 10.1016/j.epidem.2019.01.005 [DOI] [PubMed] [Google Scholar]
- 25.Lourenço-de-Oliveira R, Failloux A-B. High risk for chikungunya virus to initiate an enzootic sylvatic cycle in the tropical Americas. PLoS Negl Trop Dis. 2017;11: e0005698 10.1371/journal.pntd.0005698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunn AM, Hatcher MJ. Parasites and biological invasions: parallels, interactions, and control. Trends in Parasitology. 2015;31: 189–199. 10.1016/j.pt.2014.12.003 [DOI] [PubMed] [Google Scholar]
- 27.Dobson A. Population Dynamics of Pathogens with Multiple Host Species. The American Naturalist. 2004;164: S64–S78. 10.1086/424681 [DOI] [PubMed] [Google Scholar]
- 28.Woolhouse MEJ, Haydon DT, Antia R. Emerging pathogens: the epidemiology and evolution of species jumps. Trends Ecol Evol (Amst). 2005;20: 238–244. 10.1016/j.tree.2005.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Fine Licht HH. Does pathogen plasticity facilitate host shifts? PLoS Pathog. 2018;14: e1006961 10.1371/journal.ppat.1006961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weaver SC, Charlier C, Vasilakis N, Lecuit M. Zika, Chikungunya, and Other Emerging Vector-Borne Viral Diseases. Annual Review of Medicine. 2018;69: 395–408. 10.1146/annurev-med-050715-105122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hanley KA, Monath TP, Weaver SC, Rossi SL, Richman RL, Vasilakis N. Fever versus fever: The role of host and vector susceptibility and interspecific competition in shaping the current and future distributions of the sylvatic cycles of dengue virus and yellow fever virus. Infection, Genetics and Evolution. 2013;19: 292–311. 10.1016/j.meegid.2013.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Thoisy B, Gardon J, Salas RA, Morvan J, Kazanji M. Mayaro Virus in Wild Mammals, French Guiana. Emerging Infectious Diseases. 2003;9: 1326–1329. 10.3201/eid0910.030161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vasilakis N, Cardosa J, Hanley KA, Holmes EC, Weaver SC. Fever from the forest: prospects for the continued emergence of sylvatic dengue virus and its impact on public health. Nature Reviews Microbiology. 2011;9: 532–541. 10.1038/nrmicro2595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Terzian ACB, Zini N, Sacchetto L, Rocha RF, Parra MCP, Del Sarto JL, et al. Evidence of natural Zika virus infection in neotropical non-human primates in Brazil. Scientific Reports. 2018. 10.1038/s41598-018-34423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Favoretto SR, Araujo DB, Duarte NFH, Oliveira DBL, da Crus NG, Mesquita F, et al. Zika Virus in Peridomestic Neotropical Primates, Northeast Brazil. EcoHealth. 2019;16: 61–69. 10.1007/s10393-019-01394-7 [DOI] [PubMed] [Google Scholar]
- 36.Favoretto S, Araújo D, Oliveira D, Duarte N, Mesquita F, Zanotto P, et al. First detection of Zika virus in neotropical primates in Brazil: a possible new reservoir. bioRxiv. 2016. 10.1101/049395 [DOI] [Google Scholar]
- 37.de Figueiredo ML, de C Gomes A, Amarilla AA, de S Leandro A, de S Orrico A, de Araujo RF, et al. Mosquitoes infected with dengue viruses in Brazil. Virology Journal. 2010;7 10.1186/1743-422X-7-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kraemer MUG, Reiner RC, Brady OJ, Messina JP, Gilbert M, Pigott DM, et al. Past and future spread of the arbovirus vectors Aedes aegypti and Aedes albopictus. Nature Microbiology. 2019;4: 854–863. 10.1038/s41564-019-0376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodriguez-Morales AJ, Villamil-Gómez WE, Franco-Paredes C. The arboviral burden of disease caused by co-circulation and co-infection of dengue, chikungunya and Zika in the Americas. Travel Medicine and Infectious Disease. 2016;14: 177–179. 10.1016/j.tmaid.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 40.Campbell LP, Luther C, Moo-Llanes D, Ramsey JM, Danis-Lozano R, Peterson AT. Climate change influences on global distributions of dengue and chikungunya virus vectors. Philosophical Transactions of the Royal Society B: Biological Sciences. 2015;370: 20140135–20140135. 10.1098/rstb.2014.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fauci AS, Morens DM. Zika Virus in the Americas—Yet Another Arbovirus Threat. New England Journal of Medicine. 2016;374: 601–604. 10.1056/NEJMp1600297 [DOI] [PubMed] [Google Scholar]
- 42.Hendy A, Hernandez-Acosta E, Chaves BA, Fé NF, Valério D, Mendonça C, et al. Into the woods: Changes in mosquito community composition and presence of key vectors at increasing distances from the urban edge in urban forest parks in Manaus, Brazil. Acta Tropica. 2020;206: 105441 10.1016/j.actatropica.2020.105441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Levine JM. Species Diversity and Biological Invasions: Relating Local Process to Community Pattern. Science. 2000;288: 852–854. 10.1126/science.288.5467.852 [DOI] [PubMed] [Google Scholar]
- 44.Simberloff D. The Role of Propagule Pressure in Biological Invasions. Annual Review of Ecology, Evolution, and Systematics. 2009;40: 81–102. 10.1146/annurev.ecolsys.110308.120304 [DOI] [Google Scholar]
- 45.Borremans B, Faust C, Manlove KR, Sokolow SH, Lloyd-Smith JO. Cross-species pathogen spillover across ecosystem boundaries: mechanisms and theory. Philosophical Transactions of the Royal Society B: Biological Sciences. 2019;374: 20180344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Plowright RK, Parrish CR, McCallum H, Hudson PJ, Ko AI, Graham AL, et al. Pathways to zoonotic spillover. Nature Reviews Microbiology. 2017;15: 502–510. 10.1038/nrmicro.2017.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Plowright RK, Eby P, Hudson PJ, Smith IL, Westcott D, Bryden WL, et al. Ecological dynamics of emerging bat virus spillover. Proceedings of the Royal Society B: Biological Sciences. 2015;282: 20142124. 10.1098/rspb.2014.2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cassey P, Delean S, Lockwood JL, Sadowski JS, Blackburn TM. Dissecting the null model for biological invasions: A meta-analysis of the propagule pressure effect. Jordano P, editor. PLoS Biol. 2018;16: e2005987 10.1371/journal.pbio.2005987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bryant JE, Holmes EC, Barrett ADT. Out of Africa: A Molecular Perspective on the Introduction of Yellow Fever Virus into the Americas. PLoS Pathog. 2007;3: e75 10.1371/journal.ppat.0030075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mir D, Delatorre E, Bonaldo M, Lourenço-de-Oliveira R, Vicente AC, Bello G. Phylodynamics of Yellow Fever Virus in the Americas: new insights into the origin of the 2017 Brazilian outbreak. Scientific Reports. 2017;7 10.1038/s41598-017-07873-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kilpatrick AM, Randolph SE. Drivers, dynamics, and control of emerging vector-borne zoonotic diseases. The Lancet. 2012;380: 1946–1955. 10.1016/S0140-6736(12)61151-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Warner MD. Assessing habitat utilization by neotropical primates: A new approach. Primates. 2002;43: 59–71. 10.1007/BF02629577 [DOI] [PubMed] [Google Scholar]
- 53.Robinson JG, Bennett EL. Having your wildlife and eating it too: an analysis of hunting sustainability across tropical ecosystems. Animal Conservation. 2004;7: 397–408. 10.1017/S1367943004001532 [DOI] [Google Scholar]
- 54.Barreto P, World Resources Institute, Global Forest Watch (Organization), Instituto do Homem e Meio Ambiente da Amazônia, editors. Human pressure on the Brazilian Amazon forests. Washington, D.C.: World Resources Institute; 2006.
- 55.Gubler DJ. The Global Emergence/Resurgence of Arboviral Diseases As Public Health Problems. Archives of Medical Research. 2002;33: 330–342. 10.1016/s0188-4409(02)00378-8 [DOI] [PubMed] [Google Scholar]
- 56.San Martín JL, Brathwaite Dick O, del Diego J, Montoya RH, Dayan GH, Zambrano B. The History of Dengue Outbreaks in the Americas. The American Journal of Tropical Medicine and Hygiene. 2012;87: 584–593. 10.4269/ajtmh.2012.11-0770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Solórzano JO, Guzmán MG, Brathwaite O, Bouckenooghe A, Zambrano B, Dayan GH, et al. The Epidemiology of Dengue in the Americas Over the Last Three Decades: A Worrisome Reality. The American Journal of Tropical Medicine and Hygiene. 2010;82: 128–135. 10.4269/ajtmh.2010.09-0346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.PAHO Epidemiological Update: Dengue, February 2020. Pan American Health Organization (PAHO), World Health Organization (WHO); 2020.
- 59.Yactayo S, Staples JE, Millot V, Cibrelus L, Ramon-Pardo P. Epidemiology of Chikungunya in the Americas. Journal of Infectious Diseases. 2016;214: S441–S445. 10.1093/infdis/jiw390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pan American Health Organization. Zika Epidemiological Update. 2017.
- 61.Silva JVJ, Lopes TRR, de Oliveira-Filho EF, Oliveira RAS, Durães-Carvalho R, Gil LHVG. Current status, challenges and perspectives in the development of vaccines against yellow fever, dengue, Zika and chikungunya viruses. Acta Tropica. 2018;182: 257–263. 10.1016/j.actatropica.2018.03.009 [DOI] [PubMed] [Google Scholar]
- 62.Guisan A, Petitpierre B, Broennimann O, Daehler C, Kueffer C. Unifying niche shift studies: insights from biological invasions. Trends in Ecology & Evolution. 2014;29: 260–269. 10.1016/j.tree.2014.02.009 [DOI] [PubMed] [Google Scholar]
- 63.Roche B, Broutin H, Choisy M, Godreuil S, de Magny GC, Chevaleyre Y, et al. The niche reduction approach: an opportunity for optimal control of infectious diseases in low-income countries? BMC Public Health. 2014;14 10.1186/1471-2458-14-753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lloyd-Smith JO. Vacated niches, competitive release and the community ecology of pathogen eradication. Philosophical Transactions of the Royal Society B: Biological Sciences. 2013;368: 20120150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carroll GR. Concentration and Specialization: Dynamics of Niche Width in Populations of Organizations. American Journal of Sociology. 1985;90: 1262–1283. 10.1086/228210 [DOI] [Google Scholar]
- 66.Turner PE, Morales NM, Alto BW, Remold SK. Role of evolved host breadth in the initial emergence of an RNA virus: predicting virus emergence. Evolution. 2010;64: 3273–3286. 10.1111/j.1558-5646.2010.01051.x [DOI] [PubMed] [Google Scholar]
- 67.Gilbert GS, Webb CO. Phylogenetic signal in plant pathogen–host range. PNAS. 2007;104: 4979–4983. 10.1073/pnas.0607968104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Olival KJ, Hosseini PR, Zambrana-Torrelio C, Ross N, Bogich TL, Daszak P. Host and viral traits predict zoonotic spillover from mammals. Nature. 2017;546: 646–650. 10.1038/nature22975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Johnson PTJ, Preston DL, Hoverman JT, Richgels KLD. Biodiversity decreases disease through predictable changes in host community competence. Nature. 2013;494: 230–233. 10.1038/nature11883 [DOI] [PubMed] [Google Scholar]
- 70.Johnson PTJ, Ostfeld RS, Keesing F. Frontiers in research on biodiversity and disease. Seabloom E, editor. Ecology Letters. 2015;18: 1119–1133. 10.1111/ele.12479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pepin KM, Lambeth K, Hanley KA. Asymmetric competitive suppression between strains of dengue virus. BMC Microbiology. 2008;8: 28 10.1186/1471-2180-8-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Durbin AP, Mayer SV, Rossi SL, Amaya-Larios IY, Ramos-Castaneda J, Eong Ooi E, et al. Emergence potential of sylvatic dengue virus type 4 in the urban transmission cycle is restrained by vaccination and homotypic immunity. Virology. 2013;439: 34–41. 10.1016/j.virol.2013.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bremermann HJ, Thieme HR. A competitive exclusion principle for pathogen virulence. Journal of Mathematical Biology. 1989;27: 179–190. 10.1007/BF00276102 [DOI] [PubMed] [Google Scholar]
- 74.Laureti M, Narayanan D, Rodriguez-Andres J, Fazakerley JK, Kedzierski L. Flavivirus Receptors: Diversity, Identity, and Cell Entry. Frontiers in Immunology. 2018;9 10.3389/fimmu.2018.02180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schnierle BS. Cellular Attachment and Entry Factors for Chikungunya Virus. Viruses. 2019;11: 1078 10.3390/v11111078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Woolhouse MEJ. Population biology of emerging and re-emerging pathogens. Trends in Microbiology. 2002;10: s3–s7. 10.1016/s0966-842x(02)02428-9 [DOI] [PubMed] [Google Scholar]
- 77.Moreira-Soto A, Torres MC, Lima de Mendonça MC, Mares-Guia MA, Dos Santos Rodrigues CD, Fabri AA, et al. Evidence for multiple sylvatic transmission cycles during the 2016–2017 yellow fever virus outbreak, Brazil. Clin Microbiol Infect. 2018;24: 1019.e1–1019.e4. 10.1016/j.cmi.2018.01.026 [DOI] [PubMed] [Google Scholar]
- 78.Althouse BM, Durbin AP, Hanley KA, Halstead SB, Weaver SC, Cummings DAT. Viral kinetics of primary dengue virus infection in non-human primates: A systematic review and individual pooled analysis. Virology. 2014;452–453: 237–246. 10.1016/j.virol.2014.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Parker IM, Saunders M, Bontrager M, Weitz AP, Hendricks R, Magarey R, et al. Phylogenetic structure and host abundance drive disease pressure in communities. Nature. 2015;520: 542–544. 10.1038/nature14372 [DOI] [PubMed] [Google Scholar]
- 80.Cooper N, Griffin R, Franz M, Omotayo M, Nunn CL. Phylogenetic host specificity and understanding parasite sharing in primates. Fryxell J, editor. Ecology Letters. 2012;15: 1370–1377. 10.1111/j.1461-0248.2012.01858.x [DOI] [PubMed] [Google Scholar]
- 81.Gomez JM, Nunn CL, Verdu M. Centrality in primate-parasite networks reveals the potential for the transmission of emerging infectious diseases to humans. Proceedings of the National Academy of Sciences. 2013;110: 7738–7741. 10.1073/pnas.1220716110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Guth S, Visher E, Boots M, Brook CE. Host phylogenetic distance drives trends in virus virulence and transmissibility across the animal–human interface.: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vanchiere JA, Nehete PN, Abee CR, Wilkerson GK, Weaver SC, Brady AG, et al. Experimental Zika Virus Infection of Neotropical Primates. The American Journal of Tropical Medicine and Hygiene. 2018;98: 173–177. 10.4269/ajtmh.17-0322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chiu CY, Sánchez-San Martín C, Bouquet J, Li T, Yagi S, Tamhankar M, et al. Experimental Zika Virus Inoculation in a New World Monkey Model Reproduces Key Features of the Human Infection. Scientific Reports. 2017;7 10.1038/s41598-017-17067-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Althouse BM, Durbin AP, Hanley KA, Halstead SB, Weaver SC, Cummings DAT. Viral kinetics of primary dengue virus infection in non-human primates: A systematic review and individual pooled analysis. Virology. 2014;452–453: 237–246. 10.1016/j.virol.2014.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carrion R, Patterson JL. An animal model that reflects human disease: the common marmoset (Callithrix jacchus). Current Opinion in Virology. 2012;2: 357–362. 10.1016/j.coviro.2012.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Karna AK, Azar SR, Plante JA, Yun R, Vasilakis N, Weaver SC, et al. Colonized Sabethes cyaneus, a Sylvatic New World Mosquito Species, Shows a Low Vector Competence for Zika Virus Relative to Aedes aegypti. Viruses. 2018;10: 434 10.3390/v10080434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wasserman S, Tambyah PA, Lim PL. Yellow fever cases in Asia: primed for an epidemic. International Journal of Infectious Diseases. 2016;48: 98–103. 10.1016/j.ijid.2016.04.025 [DOI] [PubMed] [Google Scholar]
- 89.e Souza NCS, Félix AC, de Paula AV, Levi JE, Pannuti CS, Romano CM. Evaluation of serological cross-reactivity between yellow fever and other flaviviruses. International Journal of Infectious Diseases. 2019;81: 4–5. 10.1016/j.ijid.2019.01.023 [DOI] [PubMed] [Google Scholar]
- 90.Ribeiro GS, Kikuti M, Tauro LB, Nascimento LCJ, Cardoso CW, Campos GS, et al. Does immunity after Zika virus infection cross-protect against dengue? The Lancet Global Health. 2018;6: e140–e141. 10.1016/S2214-109X(17)30496-5 [DOI] [PubMed] [Google Scholar]
- 91.Rico-Mendoza A, Porras-Ramírez A, Chang A, Encinales L, Lynch R. Co-circulation of dengue, chikungunya, and Zika viruses in Colombia from 2008 to 2018. Revista Panamericana de Salud Pública. 2019;43: 1 10.26633/RPSP.2019.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ariën KK, Michiels J, Foqué N, Heyndrickx L, Van Esbroeck M. Can Zika virus antibodies cross-protect against dengue virus? The Lancet Global Health. 2018;6: e494 10.1016/S2214-109X(18)30122-0 [DOI] [PubMed] [Google Scholar]
- 93.Webb EM, Azar SR, Haller SL, Langsjoen RM, Cuthbert CE, Ramjag AT, et al. Effects of Chikungunya virus immunity on Mayaro virus disease and epidemic potential. Scientific Reports. 2019;9 10.1038/s41598-019-56551-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.MacArthur JA, Mann PG, Oreffo V, Scott GBD. Measles in monkeys: an epidemiological study. Journal of Hygiene. 1979;83: 207–211. 10.1017/s0022172400025985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Langwig KE, Voyles J, Wilber MQ, Frick WF, Murray KA, Bolker BM, et al. Context-dependent conservation responses to emerging wildlife diseases. Frontiers in Ecology and the Environment. 2015;13: 195–202. 10.1890/140241 [DOI] [Google Scholar]
- 96.Keeling MJ. Metapopulation moments: coupling, stochasticity and persistence. Journal of Animal Ecology 2000, 69, 725±736. 2000; 12 10.1046/j.1365-2656.2000.00430.x [DOI] [PubMed] [Google Scholar]
- 97.Anderson RM, May RM. The invasion, persistence and spread of infectious diseases within animal and plant communities. Philosophical Transactions of the Royal Society B: Biological Sciences. 1986; 533–570. [DOI] [PubMed] [Google Scholar]
- 98.Keeling MJ, Gilligan CA. Metapopulation dynamics of bubonic plague. Nature. 2000;407: 903–906. 10.1038/35038073 [DOI] [PubMed] [Google Scholar]
- 99.Harris RA, Tardif SD, Vinar T, Wildman DE, Rutherford JN, Rogers J, et al. Evolutionary genetics and implications of small size and twinning in callitrichine primates. Proceedings of the National Academy of Sciences. 2014;111: 1467–1472. 10.1073/pnas.1316037111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Peres CA, Janson CH. Species coexistence, distribution, and environmental determinants of neotropical primate richness: A community-level zoogeographic analysis. In: Primate Communities. 1999. 10.1017/CBO9780511542381.004 [DOI] [Google Scholar]
- 101.Vasconcelos PFC, Monath TP. Yellow Fever Remains a Potential Threat to Public Health. Vector-Borne and Zoonotic Diseases. 2016;16: 566–567. 10.1089/vbz.2016.2031 [DOI] [PubMed] [Google Scholar]
- 102.Githeko AK, Lindsay SW, Confalonieri UE, Patz JA. Climate change and vector-borne diseases: a regional analysis. Bulletin of the World Health Organization. 2000; 12. [PMC free article] [PubMed] [Google Scholar]
- 103.Sverdrup-Thygeson A, Skarpaas O, Blumentrath S, Birkemoe T, Evju M. Habitat connectivity affects specialist species richness more than generalists in veteran trees. Forest Ecology and Management. 2017;403: 96–102. 10.1016/j.foreco.2017.08.003 [DOI] [Google Scholar]
- 104.Althouse Benjamin M., Hanley Kathryn A. The tortoise or the hare? Impacts of within-host dynamics on transmission success of arthropod-borne viruses. Philosophical Transactions of the Royal Society B: Biological Sciences. 2015;370: 20140299. 10.1098/rstb.2014.0299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Althouse BM, Lessler J, Sall AA, Diallo M, Hanley KA, Watts DM, et al. Synchrony of Sylvatic Dengue Isolations: A Multi-Host, Multi-Vector SIR Model of Dengue Virus Transmission in Senegal. PLoS Negl Trop Dis. 2012;6: e1928 10.1371/journal.pntd.0001928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Judson SD, Fischer R, Judson A, Munster VJ. Ecological Contexts of Index Cases and Spillover Events of Different Ebolaviruses. PLoS Pathog. 2016;12: e1005780 10.1371/journal.ppat.1005780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Walsh MG, Wiethoelter A, Haseeb MA. The impact of human population pressure on flying fox niches and the potential consequences for Hendra virus spillover. Scientific Reports. 2017;7 10.1038/s41598-017-08065-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pigott DM, Golding N, Mylne A, Huang Z, Weiss DJ, Brady OJ, et al. Mapping the zoonotic niche of Marburg virus disease in Africa. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2015;109: 366–378. 10.1093/trstmh/trv024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jesse M, Mazzucco R, Dieckmann U, Heesterbeek H, Metz JAJ. Invasion and Persistence of Infectious Agents in Fragmented Host Populations. Adler FR, editor. PLoS ONE. 2011;6: e24006 10.1371/journal.pone.0024006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sokolow SH, Nova N, Pepin KM, Peel AJ, Pulliam JRC, Manlove K, et al. Ecological interventions to prevent and manage zoonotic pathogen spillover. Philosophical Transactions of the Royal Society B: Biological Sciences. 2019;374: 20180342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Dubrulle M, Mousson L, Moutailler S, Vazeille M, Failloux A-B. Chikungunya Virus and Aedes Mosquitoes: Saliva Is Infectious as soon as Two Days after Oral Infection. PLoS ONE. 2009;4: e5895 10.1371/journal.pone.0005895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Biggerstaff BJ, Arana-Vizcarrondo N, Johansson MA, Staples JE. Incubation Periods of Yellow Fever Virus. The American Journal of Tropical Medicine and Hygiene. 2010;83: 183–188. 10.4269/ajtmh.2010.09-0782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chan M, Johansson MA. The Incubation Periods of Dengue Viruses. Vasilakis N, editor. PLoS ONE. 2012;7: e50972 10.1371/journal.pone.0050972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Krow-Lucal ER, Biggerstaff BJ, Staples JE. Estimated Incubation Period for Zika Virus Disease. Emerging Infectious Diseases. 2017;23: 841–845. 10.3201/eid2305.161715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Keeling MJ, Grenfell BT. Effect of variability in infection period on the persistence and spatial spread of infectious diseases. Mathematical Biosciences. 1998;147: 207–226. 10.1016/s0025-5564(97)00101-6 [DOI] [PubMed] [Google Scholar]
- 116.Lacroix R, Delatte H, Hue T, Reiter P. Dispersal and Survival of Male and Female Aedes albopictus (Diptera: Culicidae) on Réunion Island. J Med Entomol. 2009;46: 1117–1124. 10.1603/033.046.0519 [DOI] [PubMed] [Google Scholar]
- 117.Dégallier N, SÁ Filho GC, Monteiro HAO, Castro FC, Vaz Da Silva O, Brandão RCF, et al. Release–Recapture Experiments with Canopy Mosquitoes in the Genera Haemagogus and Sabeihes (Diptera: Culicidae) in Brazilian Amazonia. J Med Entomol. 1998;35: 931–936. 10.1093/jmedent/35.6.931 [DOI] [PubMed] [Google Scholar]
- 118.da Cardoso J C, de Almeida MAB, dos Santos E, da Fonseca DF, Sallum MAM, Noll CA, et al. Yellow Fever Virus in Haemagogus leucocelaenus and Aedes serratus Mosquitoes, Southern Brazil, 2008. Emerging Infectious Diseases. 2010;16: 1918–1924. 10.3201/eid1612.100608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Center for Disease Control. International Task Force for Disease Eradication. Morbidity and Mortality Weekly Report. 1990;39: 209 [PubMed] [Google Scholar]
- 120.Nelson MI, Vincent AL. Reverse zoonosis of influenza to swine: new perspectives on the human–animal interface. Trends in Microbiology. 2015;23: 142–153. 10.1016/j.tim.2014.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Elton NW. Progress of Sylvan Yellow Fever Wave in Central America: Nicaragua and Honduras. American Journal of Public Health and the Nations Health. 1952;42: 1527–1534. 10.2105/AJPH.42.12.1527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lancet The. Guinea worm disease eradication: a moving target. The Lancet. 2019;393: 1261 10.1016/S0140-6736(19)30738-X [DOI] [PubMed] [Google Scholar]
- 123.Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579: 270–273. 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wong A, Li X, Lau S, Woo P. Global Epidemiology of Bat Coronaviruses. Viruses. 2019;11: 174 10.3390/v11020174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hou Y, Peng C, Yu M, Li Y, Han Z, Li F, et al. Angiotensin-converting enzyme 2 (ACE2) proteins of different bat species confer variable susceptibility to SARS-CoV entry. Archives of Virology. 2010;155: 1563–1569. 10.1007/s00705-010-0729-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Melin AD, Janiak MC, Marrone F, Arora PS, Higham JP. Comparative ACE2 variation and primate COVID-19 risk. Genetics; 2020. April 10.1101/2020.04.09.034967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sun K, Gu L, Ma L, Duan Y. Atlas of ACE2 gene expression in mammals reveals novel insights in transmisson of SARS-Cov-2. Genomics; 2020. March 10.1101/2020.03.30.015644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Damas J, Hughes GM, Keough KC, Painter CA, Persky NS, Corbo M, et al. Broad Host Range of SARS-CoV-2 Predicted by Comparative and Structural Analysis of ACE2 in Vertebrates. Genomics; 2020. April 10.1101/2020.04.16.045302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhang Y-Z, Holmes EC. A Genomic Perspective on the Origin and Emergence of SARS-CoV-2. Cell. 2020;181: 223–227. 10.1016/j.cell.2020.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Michelle DZ. U.S. advises suspending bat research over concerns coronavirus could infect North American species. The Washington Post.
- 131.Mccall R. Eating bats and pangolins banned in Gabon as a result of coronavirus pandemic. Newsweek. 6 Apr 2020.
- 132.Shi J, Wen Z, Zhong G, Yang H, Wang C, Liu R, et al. Susceptibility of ferrets, cats, dogs, and different domestic animals to SARS-coronavirus-2. Microbiology; 2020. March 10.1101/2020.03.30.015347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Luan J, Jin X, Lu Y, Zhang L. SARS-CoV-2 spike protein favors ACE2 from Bovidae and Cricetidae. Journal of Medical Virology. 2020. 10.1002/jmv.25817 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
In the case of EIP, this assumption is unrealistic because individuals have an equal probability of leaving the incubation compartment regardless of the time since infection. In reality, the probability of progressing should be very low immediately after infection and highest around the EIP mean—a trajectory better represented by a gamma distribution (in green and purple). A gamma distributed EIP can be constructed in a compartmental model via a boxcar configuration of the latent period (i.e., splitting the latent period up into a series of separate compartments, or boxes). Note how, as the number of latent boxes increases (green versus purple), the gamma distribution becomes less dispersed and more closely centered around the EIP mean. EIP, extrinsic incubation period.
(PDF)
Mosquito birthrate = 1/life span and increases from the top to bottom panels, while EIP increases left to right. Here, we constructed an Erlang-distributed EIP by splitting the exposed compartment into 10 separate boxes. Within each panel, the total population size of mosquitoes (in two populations) and primates (in two populations) changes horizontally and vertically, respectively. For each parameter set, we simulated the introduction of a single infected primate and subsequent transmission for a three-year period. Blue indicates no simulations establishing, whereas red indicates all simulations establishing. Contour lines show 0.25, 0.5, 0.75, and 0.95 probability of establishment. EIP, extrinsic incubation period.
(PPTX)
Mosquito birthrate = 1/life span and increases from the top to bottom panels, while EIP increases left to right. Here, we constructed an Erlang-distributed EIP by splitting the exposed compartment into 50 separate boxes. Within each panel, the total population size of mosquitoes (in two populations) and primates (in two populations) changes horizontally and vertically, respectively. For each parameter set, we simulated the introduction of a single infected primate and subsequent transmission for a three-year period. Blue indicates no simulations establishing, whereas red indicates all simulations establishing. Contour lines show 0.25, 0.5, 0.75, and 0.95 probability of establishment. EIP, extrinsic incubation period.
(PPTX)