Abstract
Objectives
The purpose of this study was to evaluate the potential impact of the coronavirus disease-2019 (COVID-19) pandemic on out-of-hospital cardiac arrest (OHCA) responses and outcomes in 2 U.S. communities with relatively low infection rates.
Background
Studies in areas with high COVID-19 infection rates indicate that the pandemic has had direct and indirect effects on community responses to OHCA and negative impacts on survival. Data from areas with lower infection rates are lacking.
Methods
Cases of OHCA in Multnomah County, Oregon, and Ventura County, California, with attempted resuscitation by emergency medical services (EMS) from March 1 to May 31, 2020, and from March 1 to May 31, 2019, were evaluated.
Results
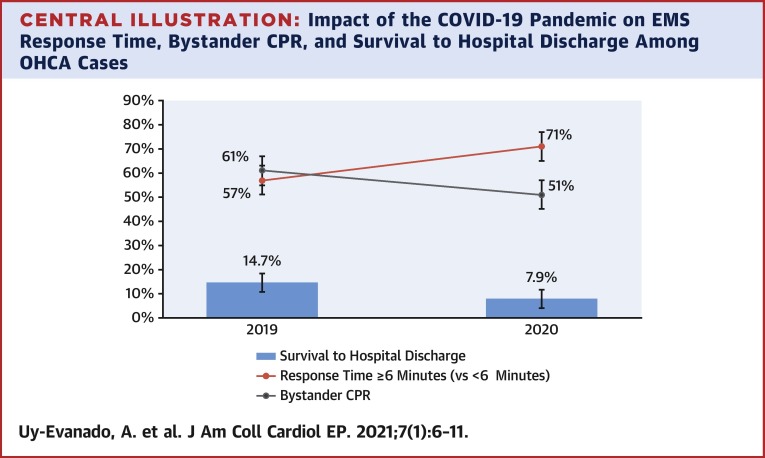
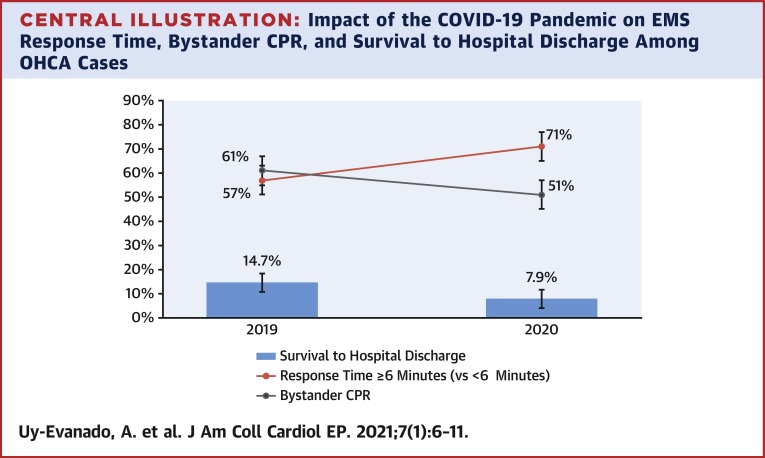
In a comparison of 231 OHCA in 2019 to 278 in 2020, the proportion of cases receiving bystander cardiopulmonary resuscitation (CPR) was lower in 2020 (61% to 51%, respectively; p = 0.02), and bystander use of automated external defibrillators (AEDs) declined (5% to 1%, respectively; p = 0.02). EMS response time increased (6.6 ± 2.0 min to 7.6 ± 3.0 min, respectively; p < 0.001), and fewer OHCA cases survived to hospital discharge (14.7% to 7.9%, respectively; p = 0.02). Incidence rates did not change significantly (p > 0.07), and coronavirus infection rates were low (Multnomah County, 143/100,000; Ventura County, 127/100,000 as of May 31) compared to rates of ∼1,600 to 3,000/100,000 in the New York City region at that time.
Conclusions
The community response to OHCA was altered from March to May 2020, with less bystander CPR, delays in EMS response time, and reduced survival from OHCA. These results highlight the pandemic’s indirect negative impact on OHCA, even in communities with relatively low incidence of COVID-19 infection, and point to potential opportunities for countering the impact.
Key Words: COVID-19, out-of-hospital cardiac arrest, resuscitation
Abbreviations and Acronyms: AED, automated external defibrillator; COVID-19, coronavirus disease-2019; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; OHCA, out-of-hospital cardiac arrest
Central Illustration
Out-of-hospital cardiac arrest (OHCA) results from a sudden circulatory collapse. It is fatal without rapid cardiopulmonary resuscitation (CPR) and/or defibrillation and is responsible for >350,000 deaths per year in the United States (1). Emergency medical service (EMS) first responders play a vital role in survival from OHCA. Rapid EMS response and high-quality CPR improve survival rates (2,3), and provision of bystander CPR can double survival from OHCA (4).
The novel coronavirus disease-2019 (COVID-19) pandemic, with nearly 2 million U.S. cases and more than 112,000 deaths as of June 11, 2020 (5), may directly impact the burden of cardiovascular disease and deaths, including OHCA, due to its effects on the heart (6). The pandemic may also indirectly affect OHCA by altering the capacity of the community and EMS agencies to respond to OHCA. There is also evidence that patients are avoiding calling 911 or going to the hospital for chest discomfort or shortness of breath. Hospital visits for acute myocardial infarction have been significantly reduced during the pandemic (7). Fear of contagion may discourage bystanders from participating in the community response to OHCA. Furthermore, EMS agencies have implemented additional screening of all 911 calls for potential COVID-19 symptoms or known infection, and new processes have been instituted for provision of personal protective equipment to maximize the safety of first responders (8).
We hypothesized that, during the pandemic, community response to OHCA and EMS processes for responding to OHCA would be altered, with negative effects on survival outcomes. To test this hypothesis, cases of OHCA were evaluated during from March to May 2020 and March to May 2019 in Multnomah County, Oregon, and Ventura County, California, 2 communities with an established infrastructure for investigation of OHCA (9, 10, 11).
Methods
Study population
Consecutive cases of OHCA were identified from 2 communities with ongoing population-based studies: the Oregon SUDS (Sudden Unexpected Death Study) (Multnomah County, Oregon, population 812,855) and the Ventura PRESTO (Prediction of Sudden Death in Multi-Ethnic Communities) study (Ventura County, California, population 846,006). Incident OHCA cases were identified through collaboration with each county’s 2-tiered EMS system (both ambulance and fire first response); cases with resuscitation attempted by EMS were included. These studies were approved by the Institutional Review Boards of Cedars-Sinai Medical Center, Oregon Health and Science University, and all participating hospitals and health systems. All survivors of cardiac arrest provided informed consent; for nonsurvivors, this requirement was waived.
Comparison of COVID-19 pandemic and pre-pandemic periods
The pandemic followed a similar course in the 2 counties (Table 1 ). The first cases in each community were diagnosed in early March, and total cases, deaths, and COVID-19 incidence rates were similar as of May 31, 2020 (143 per 100,000 and 127 per 100,000 in Multnomah and Ventura counties, respectively). OHCA cases occurring during the pandemic period (March 1 to May 31, 2020) were compared to OHCA cases during the same time period in the previous year (March 1 to May 31, 2019). COVID-19-positive cases with EMS response and their overlap with OHCA cases were evaluated in Multnomah County from March 1 to May 13, 2020.
Table 1.
Source Populations for the Oregon SUDS and Ventura PRESTO Studies (Multnomah County, Oregon, and Ventura County, California)
| Multnomah County | Ventura County |
|
|---|---|---|
| Total population, July 1, 2019∗ | 812,855 | 846,006 |
| Race/ethnicity (%) | ||
| White non-Hispanic | 69.3 | 45.0 |
| Hispanic | 11.7 | 43.0 |
| Asian | 8.1 | 7.9 |
| Black | 6.1 | 2.4 |
| Other† | 4.8 | 1.7 |
| Date of first COVID-19 case diagnosed | March 10 | March 4 |
| Statewide stay-at-home order enacted | March 23 | March 19 |
| Number of COVID-19 cases (as of 5/31/2020)‡ | 1,165 | 1,078 |
| Number of COVID-19 deaths (as of 5/31/2020)‡ | 59 | 33 |
| Incidence of COVID-19 per 100,000 (as of 5/31/2020)‡ | 143/100,000 | 127/100,000 |
COVID-19 = coronavirus disease-2019; PRESTO = Prediction of Sudden Death in Multi-Ethnic Communities study; SUDS = Sudden Unexpected Death Study.
Quick Facts, U.S. Census Bureau, Washington, DC (Multnomah County, Oregon, and Ventura County, California).
American Indian and Alaska Native alone, Native Hawaiian and Other Pacific Islander alone, or Two or More Races.
U.S. Centers for Disease Control and Prevention, county maps.
Data sources and definitions
The occurrence of OHCA was adjudicated based on detailed review of the EMS prehospital care report and was defined as a sudden, circulatory collapse of likely cardiac cause requiring CPR and/or defibrillation and not due to trauma or overdose. OHCA circumstances were obtained based on Utstein definitions (12). Bystander CPR was defined as CPR performed by a person who was not part of the organized EMS system response. Response time was defined as the time elapsed between receipt of the 911 call and arrival at the patient’s side by fire department or ambulance service, whichever arrived first.
Statistical analysis
We used the chi-square test for categorical variables and independent sample Student's t-test or Mann-Whitney U test for continuous variables as appropriate. Data were analyzed using SAS version 9.4 software (SAS Institute, Cary, North Carolina), and 2-sided statistical tests with a p value <0.05 were considered significant. Three-month incidence rates and 95% confidence intervals (CIs) were calculated for each county for each year using cases from Mar 1 to May 31 in the numerator and the U.S. Census county population estimate for July 1, 2019, in the denominator.
Results
OHCA incidence
In the 2 communities during both periods in 2019 and 2020, a total of 657 potential OHCA cases were identified. A total of 148 were excluded after adjudication, and 509 cases of OHCA met inclusion criteria. During the pre-pandemic period (March 1 to May 31, 2019), 231 OHCA cases were included (110 in Oregon and 121 in Ventura). During the COVID-19 pandemic period (March 1 to May 31, 2020), 278 OHCA cases were included (126 in Multnomah County, and 152 in Ventura County). Three-month incidence rates of OHCA in the 2 counties increased by 23% and 25%, respectively, from the pre-pandemic to the pandemic period. Multnomah County saw 12.2 to 15.0 per 100,000 cases (95% CI: 9.8 to 14.6 and 95% CI: 12.3 to 17.7, respectively); p = 0.12) and Ventura County saw 14.2 to 17.7 per 100,000 cases (95% CI: 11.6 to 16.7; and 95% CI: 14.9 to 20.6, respectively; p = 0.07).
Among the 126 OHCA cases in Multnomah County 1 (0.8%) had confirmed COVID-19 infection based on records of COVID-19 test-positive individuals with EMS response.
Characteristics of OHCA
Compared to the pre-pandemic period, OHCA cases during the pandemic period were younger (69.1 ± 17.4 vs. 64.9 ± 18.3 years of age, respectively; p = 0.01) (Table 2 ). An increased proportion of OHCA occurred in the home (63% vs. 76%, respectively; p = 0.009). OHCA cases were less likely to receive bystander CPR during the pandemic (61% vs. 51%, respectively; p = 0.02) (Central Illustration ), and bystander use of automated external defibrillators (AEDs) declined (5% vs. 1%, respectively; p = 0.02). EMS response time increased from 6.6 ± 2.0 min to 7.6 ± 3.0 min during the pandemic (p < 0.001), although time to defibrillation was not significantly prolonged (11.4 ± 8.4 min vs. 14.3 ± 9.7 min, respectively; p = 0.08). Survival to hospital discharge was significantly lower in the pandemic period (14.7% vs. 7.9%, respectively; p = 0.02) (Central Illustration).
Table 2.
OHCA Pre-Pandemic Versus COVID-19 Pandemic‡
| Pre-Pandemic March-May 2019 (n = 231) |
Pandemic March-May 2020 (n = 278) |
p Value | |
|---|---|---|---|
| Age, yrs | 69.1 ± 17.4 | 64.9 ± 18.3 | 0.01 |
| Age categories, yrs (%) | 0.04 | ||
| <35 | 9 (4) | 15 (5) | |
| 35-64 | 76 (33) | 122 (44) | |
| 65-84 | 108 (47) | 99 (36) | |
| ≥85 | 38 (16) | 42 (15) | |
| Males | 137 (60) | 174 (63) | 0.49 |
| Arrest location† | 0.009 | ||
| Home | 145 (63) | 210 (76) | |
| Nursing home/care facility | 43 (19) | 31 (11) | |
| Public | 41 (18) | 37 (13) | |
| Witnessed arrest | 122 (53) | 140 (50) | 0.58 |
| Shockable rhythm (VF/VT) | 64 (28) | 64 (23) | 0.24 |
| Bystander CPR | 142 (61) | 141 (51) | 0.02 |
| Bystander use of AED | 12 (5.2) | 4 (1.4) | 0.02 |
| Total response time, min∗ | <0.001 | ||
| 911 call to at patient’s side | |||
| Mean ± SD | 6.6 ± 2.0 | 7.6 ± 3.0 | |
| Median (min, max) | 6.4 (1.6, 13.7) | 7.0 (0.7, 22.8) | |
| Total response time, min∗ | |||
| ≥6 min vs. <6 min | 132 (57) | 196 (71) | 0.002 |
| Total response time, min∗ | 0.01 | ||
| <4 | 15 (7) | 13 (5) | |
| 4-5 | 36 (16) | 26 (9) | |
| 5-6 | 48 (21) | 43 (15) | |
| 6-7 | 52 (23) | 57 (21) | |
| 7-8 | 33 (14) | 44 (16) | |
| ≥8 | 47 (20) | 95 (34) | |
| Time to defibrillation, min∗† | 0.08 | ||
| Mean ± SD | 11.4 ± 8.4 | 14.3 ± 9.7 | |
| Median (min, max) | 9.3 (−3.5, 45.6) | 11.0 (1.8, 55.3) | |
| Return of spontaneous circulation | 95 (41) | 95 (34) | 0.11 |
| Admitted alive to hospital† | 74 (32) | 65 (24) | 0.03 |
| Survival to hospital discharge† | 34 (14.7) | 22 (7.9) | 0.02 |
COVID-19 = coronavirus disease-2019; OHCA = out-of-hospital cardiac arrest; PRESTO = Prediction of Sudden Death in Multi-Ethnic Communities Study; SUDS = Sudden Unexpected Death Study; VF = ventricular fibrillation; VT = ventricular tachycardia.
For each measurement, the minimum time was used (ambulance or fire).
Time to defibrillation was calculated for 62 cases in 2019 and 63 cases in 2020 with primary VF or VT; Data on arrest location was missing for 2 cases in 2019; Data on admitted alive to hospital was missing for 1 case in 2019 and 2 cases in 2020; Data on survival to hospital discharge was missing for 1 case in 2020 who was still in the hospital as of 6/15/2020.
Data compare OHCA cases from March to May 2019 (pre-pandemic) with March to May 2020 (COVID-19 pandemic) in the Oregon SUDS study (Multnomah Co., Oregon) and Ventura PRESTO study (Ventura Co., California).
Central Illustration.
Impact of the COVID-19 Pandemic on EMS Response Time, Bystander CPR, and Survival to Hospital Discharge Among OHCA Cases
In a comparison of the pre-pandemic (March 1 to May 31, 2019) and pandemic (March 1 to May 31, 2020) periods, the proportion of OHCA cases with EMS response ≥6 min (red line) increased from 57% in the pre-pandemic period to 71% in the pandemic period (p = 0.002). The proportion of OHCA with bystander CPR (gray line) decreased from 61% to 51% (p = 0.02). Survival to hospital discharge (blue area) decreased from 14.7% to 7.9% (p = 0.02). Error bars are 95% confidence intervals of proportions. CPR = cardiopulmonary resuscitation; EMS = emergency medical services; OHCA = out-of-hospital cardiac arrest.
Discussion
During the first 3 months of the COVID-19 pandemic in 2 communities (Multnomah County, Oregon, and Ventura County, California), EMS response times for OHCA were longer, bystander use of CPR and AED decreased, and survival to hospital discharge for OHCA declined compared to the same period the year before. The incidence of OHCA also increased, but this change did not reach statistical significance.
These findings are largely consistent with results from 2 studies in Europe (13,14) and 1 in New York City (15). The first European study, from the Lombardy region of Italy, reported a 58% increase in the incidence of OHCA (n = 362) from February 20 through March 31, 2020, compared to the same 40-day period in 2019 (n = 229), with longer EMS response times, less bystander CPR, and lower survival (13). In Paris, France, the incidence of OHCA doubled in the early weeks of the lockdown. The proportion of cases admitted alive to hospital decreased from 22.8% to 12.8%, respectively (14). The Paris study also reported longer EMS response times and declines in bystander CPR and shockable rhythm. In New York City, the incidence of nontraumatic OHCA with EMS resuscitation from March 1 to April 25, 2020, was 3-fold higher than during the same period a year before, and OHCA during the pandemic had substantially lower shockable rhythm, return of spontaneous circulation, and survival than the year before, although bystander CPR rates did not change (15). These studies were conducted in areas with a higher COVID-19 incidence than in the 2 communities in the present study. The authors estimated that individuals with suspected or diagnosed COVID-19 constituted 77% of the excess OHCA cases in the Italian study (13) and 33% in the Paris study (14). In Seattle and King Counties, Washington, which had 2 to 3 times higher COVID-19 rates (5) than Multnomah and Ventura Counties, patients with confirmed COVID-19 or COVID-like illness accounted for 5% of OHCA at home and 11% in nursing homes from February 26 to April 15, 2020 (16).
Our observation that more OHCA occurred at home during the pandemic is consistent with stay-at-home orders and may explain part of the decline in bystander use of CPR and AED, although bystander response declined in all locations. The longer EMS response times and declines in bystander CPR reported here have each been associated with lower survival from OHCA (4). Although this study could not evaluate whether patients in delayed calling 911, Garcia et al. (17) and others reported a steep nationwide decline in hospital-treated acute coronary syndrome during the early pandemic period, potentially indicating that fewer individuals were seeking care for cardiac symptoms (7).
We observed a modest but not statistically significant increase in the incidence of OHCA in the 2 counties, despite a relatively low incidence of COVID-19 infection (143 and 127 per 100,000 in Multnomah and Ventura Counties, respectively, as of May 31, 2020, compared to ∼1,600 to 3,000 per 100,000 in the New York City region at that time) (5). In this study’s population, COVID-19 infection among individuals with OHCA appeared to be rare (1 OHCA case in Multnomah County confirmed COVID-19 disease), in contrast to areas with higher COVID-19 incidence (13). Additionally a higher percentage of OHCA presenting at a younger age was observed in the pandemic period. Indirect and direct effects of the pandemic on the incidence and epidemiology of OHCA warrant further investigation over time.
This study used a rigorous case adjudication process and included >500 cases of OHCA from 2 separate communities; however, the study was limited to cases with resuscitation attempted by EMS.
Conclusions
The present results suggest that the pandemic may have significant effects on survival from OHCA, even in areas with relatively low COVID-19 incidence, and that optimizing community and EMS responses during the ongoing pandemic and future outbreaks may improve survival.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: This study addresses clinical competencies of medical knowledge and systems-based practice regarding the impact of the ongoing COVID-19 pandemic on the community and EMS response to OHCA. The indirect impact of the pandemic may negatively influence survival from OHCA, with implications for clinicians caring for patients at high risk for OHCA.
TRANSLATIONAL OUTLOOK: Even in geographic regions with relatively low COVID-19 incidence rates, a detrimental impact on EMS response and survival from OHCA was observed. Future research could measure the effectiveness of interventions for patients, communities, and EMS systems to improve response to and survival from OHCA during future outbreaks.
Author Disclosures
Dr. Chugh was funded by National Institutes of Health, National Heart Lung and Blood Institute (NHLBI) grants R01 HL147358 and R01 HL145675. Dr. Chugh holds the Pauline and Harold Price Chair in Cardiac Electrophysiology at Cedars-Sinai, Los Angeles. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors acknowledge significant contributions of the American Medical Response, Multnomah and Ventura Counties, the Portland/Gresham Fire Departments, the Gold Coast Ambulance, the LifeLine Medical Transport, the Ventura County Fire Protection District, the Ventura City Fire Department, and the Fillmore Fire Department.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Benjamin E.J., Muntner P., Alonso A. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Rea T.D., Cook A.J., Stiell I.G. Predicting survival after out-of-hospital cardiac arrest: role of the Utstein data elements. Ann Emerg Med. 2010;55:249–257. doi: 10.1016/j.annemergmed.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 3.Nichol G., Thomas E., Callaway C.W. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sasson C., Rogers M.A., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): Cases in the U.S. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases, Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Updated August 13, 2020. Available at:
- 6.Clerkin K.J., Fried J.A., Raikhelkar J. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 7.Solomon M.D., McNulty E.J., Rana J.S. The covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 8.Edelson D.P., Sasson C., Chan P.S., Atkins D.L., Aziz K., Becker L.B. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the Emergency Cardiovascular Care Committee and Get With the Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association in Collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: supporting organizations: American Association of Critical Care Nurses and National EMS Physicians. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chugh S.S., Jui J., Gunson K., Stecker E.C., John B.T., Thompson B. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 10.Marijon E., Uy-Evanado A., Dumas F., Karam N., Reinier K., Teodorescu C. Warning symptoms are associated with survival from sudden cardiac arrest. Ann Intern Med. 2016;164:23–29. doi: 10.7326/M14-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reinier K., Nichols G.A., Huertas-Vazquez A. Distinctive clinical profile of blacks versus whites presenting with sudden cardiac arrest. Circulation. 2015;132:380–387. doi: 10.1161/CIRCULATIONAHA.115.015673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perkins G.D., Jacobs I.G., Nadkarni V.M., Berg R.A., Bhanji F., Biarent D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for health care professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132:1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 13.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai P.H., Lancet E.A., Weiden M.D. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5:1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sayre M.R., Barnard L.M., Counts C.R. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander CPR. Circulation. 2020;142:507–509. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 17.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]