Abstract
Background
Electronic cigarettes (e‐cigarettes) have been proposed as a potential harm reduction tool for combustible cigarette smokers. The majority of adult e‐cigarette users continue to smoke combustible cigarettes and are considered dual users. The vascular impact of e‐cigarettes remains incompletely defined.
Methods and Results
We examined the association of e‐cigarette use with measures of vascular function and tonometry, preclinical measures of cardiovascular injury. As part of the CITU (Cardiovascular Injury due to Tobacco Use) study, we performed noninvasive vascular function testing in individuals without known cardiovascular disease or cardiovascular disease risk factors who were nonsmokers (n=94), users of combustible cigarettes (n=285), users of e‐cigarettes (n=36), or dual users (n=52). In unadjusted analyses, measures of arterial stiffness including carotid‐femoral pulse wave velocity, augmentation index, carotid‐radial pulse wave velocity, and central blood pressures differed across the use groups. In multivariable models adjusted for age, sex, race, and study site, combustible cigarette smokers had higher augmentation index compared with nonusers (129.8±1.5 versus 118.8±2.7, P=0.003). The augmentation index was similar between combustible cigarette smokers compared with sole e‐cigarette users (129.8±1.5 versus 126.2±5.9, P=1.0) and dual users (129.8±1.5 versus 134.9±4.0, P=1.0). Endothelial cells from combustible cigarette smokers and sole e‐cigarette users produced less nitric oxide in response to A23187 stimulation compared with nonsmokers, suggestive of impaired endothelial nitric oxide synthase signaling.
Conclusions
Our findings suggest that e‐cigarette use is not associated with a more favorable vascular profile. Future longitudinal studies are needed to evaluate the long‐term risks of sustained e‐cigarette use.
Keywords: e‐cigarettes, electronic cigarettes, smoking, vascular function
Subject Categories: Vascular Biology, Hemodynamics, Endothelium/Vascular Type/Nitric Oxide
Clinical Persepctive
What Is New
Augmentation index, a measure of vascular stiffness, was similar between sole combustible cigarette users compared with sole e‐cigarette users and compared with dual users, suggesting that e‐cigarette use is not associated with a more limited arterial stiffening impact than combustible cigarette smoking.
In endothelial cells freshly collected from study participants, stimulated nitric oxide production was diminished in both combustible and e‐cigarette users, suggesting the presence of endothelial cell dysfunction.
What Are the Clinical Implications?
Our study suggests that e‐cigarette use is associated with a similar vascular profile compared with combustible cigarette use.
Nonstandard Abbreviations and Acronyms.
AIx augmentation index
BP blood pressure
CVD cardiovascular disease
DAF‐2 DA 4,5‐diaminofluorescein diacetate
EC endothelial cell
eNOS endothelial nitric oxide synthase
NO nitric oxide
PWV pulse wave velocity
Introduction
E‐cigarettes have gained popularity among adult smokers seeking to reduce their consumption of or quit combustible cigarettes.1, 2, 3 Many users and public health activists view e‐cigarettes as safer alternatives to combustible cigarettes because these products contain a limited number of ingredients (nicotine, propylene glycol/glycerin, and in many cases flavoring additives) compared with combustible tobacco products. The perception that e‐cigarettes are safer than combustible cigarettes is widespread, with the majority of adult e‐cigarette users reporting that the primary reason for use is the perception that e‐cigarettes pose less of a health risk than combustible cigarette smoking.1 Consequently, e‐cigarettes have drawn significant attention as a potential way to reduce harm. However, it is unclear whether e‐cigarettes are a safer alternative to combustible cigarettes.
Cardiovascular disease (CVD) is the primary cause of morbidity and mortality among combustible cigarette smokers.4, 5 Smoking combustible cigarettes exposes the cardiovascular system to inhaled toxins and leads to widespread changes in vascular function that are associated with adverse cardiovascular outcomes.6, 7, 8, 9 Vascular dysfunction, associated with smoking combustible cigarettes, is characterized by impaired endothelial function and increased vascular stiffness, both of which are predictive of adverse cardiovascular outcomes and mortality.10, 11, 12 Although smoke generated from combustible cigarettes generates a wide range of harmful or potentially harmful substances, the increased cardiovascular risk associated with smoking has largely been attributed to reactive aldehydes such as acrolein, formaldehyde, and acetaldehyde.13 Importantly, such aldehydes have also been found in e‐cigarette–generated aerosol,13, 14, 15, 16 although their contribution to the cardiovascular effects of e‐cigarette use remains unknown.
To gain early evidence of the cardiovascular effects of e‐cigarettes, we performed a cross‐sectional study (the CITU [Cardiovascular Injury due to Tobacco Use] study) of nonsmokers, combustible cigarette users, e‐cigarette users, and dual combustible and e‐cigarette users. The objective of this study was to compare vascular function between combustible cigarette users and users of e‐cigarettes, alone or with contemporaneous use of combustible cigarettes.
Methods
Primary de‐identified data supporting the findings of this study are available through the American Heart Association Tobacco Regulation and Addiction Center upon request.
Study Participants
We recruited male and female participants between the ages of 21 and 45 years from Boston University Medical School and the University of Louisville who were without established CVD or CVD risk factors (dyslipidemia, hypertension, diabetes mellitus), as previously described.17 Participants were classified as nonsmokers if they were not current smokers or users of other tobacco products, smoked fewer than 100 cigarettes in their lifetime, and had a urinary cotinine level <10 ng/mL. Combustible cigarette smokers were defined based on current smoking of at least 5 days per week, having smoked ≥100 cigarettes in their lifetime, and no current e‐cigarette use. E‐cigarette users were defined as participants who currently use e‐cigarettes at least 5 days per week and do not currently use combustible cigarettes. Dual combustible and e‐cigarette users were defined as participants who reported current use of both combustible and e‐cigarettes, at least 5 days per week, with a lifetime usage of ≥100 cigarettes. All inclusion and exclusion criteria can be found in Table S1. All participants gave written informed consent and all study protocols were approved by the Boston Medical Center and University of Louisville institutional review boards.
Vascular Function Testing
Noninvasive vascular function was measured as previously described to calculate 5 measures: baseline brachial artery diameter, baseline flow velocity, hyperemic flow velocity, flow‐mediated dilation, and hyperemic shear stress.9, 17, 18 Participants were asked to fast from food and tobacco products overnight, 8 to 12 hours before the study visit. Brachial artery diameter was measured at baseline and after a 5‐minute occlusion (blood pressure [BP] cuff attached to the lower arm inflated to 200 or 50 mm Hg higher than the systolic pressure) to determine flow‐mediated dilation, a noninvasive measure of conduit artery endothelial‐dependent vasodilation. Resting and hyperemic flow velocities and shear stress were measured in the brachial artery using Doppler ultrasound. Shear stress (dynes/cm2) was calculated as 8 μV/diameter, where μ was blood viscosity (assumed to be 0.035 dyne‐s/cm2) and V was brachial velocity (cm/s) at baseline.19 All vascular images were analyzed at Boston University using Vascular Research Tools Brachial Analyzer for Research V.6.8.5 (Medical Imaging Applications, LLC) by a technician blinded to tobacco product use group.
Tonometry Measurements
Arterial tonometry and waveform analysis were used to determine carotid‐femoral pulse wave velocity (PWV), carotid‐radial PWV, augmentation index (AIx), central systolic BP, central diastolic BP, and heart rate using (SphygmoCor, Atcor).20, 21 Participants rested supine for at least 5 minutes before measurement. A tonometer was used over 3 locations (radial, carotid, femoral arteries) sequentially and the R wave from the ECG was used to measure transit time with a caliper used to measure distance between locations. Pulse waveform analysis was performed from the radial artery recordings with a validated transfer function along with brachial BP readings used to determine central BPs. AIx was assessed from the radial artery waveform by comparing the augmentation pressure divided by the pulse pressure and is expressed as a percentage.21
EC Collection
Venous endothelial cells (ECs) were collected as previously described.2 In brief, a 0.018 inch J‐wire (Arrow International) was inserted into a forearm vein through a 20 or 22 gauge intravenous catheter and used to gently rub the endothelial surface. ECs were recovered from the wire in red blood cell lysis/dissociation buffer, centrifuged, and applied to poly‐L‐lysine–coated slides (Sigma). Nitric oxide (NO) bioavailability was assessed immediately after isolation as described below. All other cells were fixed onto the slides using 4% paraformaldehyde, dried, and frozen at −80°C before staining and immunofluorescence imaging to quantify protein expression as described below.
Fluorescence Imaging and Quantification
To evaluate NO production, freshly isolated ECs were incubated with 3 μmol/L 4,5‐diaminofluorescein diacetate (DAF‐2DA; Calbiochem) for 30 minutes. After 2 washes with Hanks balanced salt solution, cells were stimulated with 1 μmol/L A23187 (Sigma) for 15 minutes and fixed with 2% paraformaldehyde. Mean fluorescence intensity at an excitation of 498 nm was measured on a fluorescence microscope (Nikon Eclipse TE2000), quantified for 20 cells, and averaged for each condition. Data are expressed as percent increase in DAF‐2DA fluorescence stimulated by A23187 compared with unstimulated cells.
Protein levels of endothelial NO synthase (eNOS) were quantified using immunofluorescence microscopy. Cells were permeabilized with 0.1% triton‐X in 50 mmol/L glycine for 10 minutes, washed 3 times with 50 mmol/L glycine in 1X PBS, and blocked for 10 minutes with 0.5% bovine serum albumin in 50 mmol/L glycine/1X PBS. Slides were stained with primary antibody against eNOS (1:100 dilution, BD Transduction, catalog #610296) for 3 hours at 37°C. Following 3 washes with 50 mmol/L glycine/1X PBS, the cells were incubated with secondary antibody for 45 minutes at 37°C. The fluorescence intensity was quantified in 20 ECs and averaged for each condition. To control for batch‐to‐batch variability, fluorescence intensity was normalized to the intensity in human aortic ECs, which were stained simultaneously. Final intensity was calculated by dividing the average fluorescence intensity for the patient sample by the average fluorescence intensity of the human aortic EC sample and multiplying by 100. The intensity is expressed in arbitrary units. All quantification for all measures was performed blinded to participant identity and tobacco product status.
Statistical Analyses
Clinical characteristics and vascular function measures were compared across the 4 groups (nonsmokers, combustible cigarette users, e‐cigarette users, and dual combustible and e‐cigarette users) using 1‐way ANOVA or chi‐square testing for continuous or categorical data, respectively. Using a generalized linear model, we compared means while adjusting for age, sex, race, and study site. We performed post hoc analyses comparing combustible cigarette use with nonuse and with e‐cigarette use alone or dual use with Bonferroni correction for multiple testing. Data are reported as mean±SD. Two‐sided P˂0.05 was considered statistically significant. All statistical analyses were peformed using SAS 9.4 (TS1M3; SAS Institute).
Results
Clinical Characteristics
Combustible cigarette and dual users were older than nonsmokers and e‐cigarette users (Table 1). E‐cigarette users were more likely to be younger, men, and white. The number of pack‐years or average number of cigarettes smoked per day were similar for both combustible cigarette smokers and dual users (15±13 versus 13±10, respectively; P=1.0). All e‐cigarette users were former smokers.
Table 1.
Clinical Characteristics and Vascular Measures of the CITU Study Cohort
| Nonsmokers (n=94) | Combustible Cigarette Users (n=285) | E‐Cigarette Users (n=36) | Dual Users (n=52) | P Value | |
|---|---|---|---|---|---|
| Clinical characteristics | |||||
| Age, y | 29±6 | 32±7 | 29±6 | 33±7 | <0.0001 |
| Women, % | 56 | 42 | 28 | 47 | 0.01 |
| Black race, % | 65 | 61 | 28 | 54 | <0.01 |
| Average number of cigarettes per d, % | |||||
| <5 | 100 | 10 | 100 | 16 | <0.0001 |
| ≥5 | 90 | 84 | |||
| Urinary cotinine, mg/dL | 3±2 | 917±879 | 856±959 | 775±740 | <0.0001 |
| Vascular function and tonometry measures | |||||
| Baseline brachial diameter, mm | 3.8±0.8 | 4.0±0.7 | 3.8±0.7 | 3.9±0.6 | 0.28 |
| Baseline mean flow velocity, cm/s | 12.7±5.6 | 15.3±8.9 | 15.1±9.2 | 14.9±10.0 | 0.61 |
| Hyperemic mean flow velocity, cm/s | 77.6±19.1 | 72.8±19.0 | 70.3±17.5 | 73.9±20.2 | 0.21 |
| Flow‐mediated dilation, % | 7.0±4.1 | 6.2±3.9 | 7.5±4.9 | 5.9±5.2 | 0.16 |
| Shear stress, dyne/cm2 | 60.3±19.6 | 53.8±18.3 | 53.6±14.2 | 54.7±20.1 | 0.14 |
| Carotid‐femoral PWV, m/s | 5.6±1.1 | 6.0±1.2 | 5.8±0.6 | 6.4±1.2 | 0.004 |
| Carotid‐radial PWV, m/s | 6.7±1.8 | 7.4±1.8 | 5.9±1.0 | 7.4±1.8 | 0.0001 |
| AIx | 116.7±17.5 | 130.9±25.8 | 113.3±9.0 | 137.2±29.3 | <0.0001 |
| Central systolic BP, mm Hg | 119±12 | 122±13 | 118±10 | 127±15 | 0.003 |
| Central diastolic BP, mm Hg | 72±9 | 76±10 | 71±6 | 79±13 | <0.001 |
| Heart rate, beats per min | 69±10 | 66±11 | 64±8 | 69±13 | 0.12 |
Values are expressed as mean±SD or percentage. AIx indicates augmentation index; BP, blood pressure; CITU, Cardiovascular Injury due to Tobacco Use; and PWV, pulse wave velocity.
E‐Cigarette Product Characteristics
All e‐cigarette users reported using second‐ or third‐generation devices (Table 2). Among dual users, 9 participants reported using first‐generation devices and 40 reported use of second‐ or third‐generation devices. Only 2 e‐cigarette users and 6 dual users reported never using e‐liquids containing nicotine. Most e‐cigarette and dual users reported using flavored e‐liquids (Table 2). The majority of e‐cigarette and dual users reported using fruit‐flavored e‐liquids. Use of menthol or mint flavored e‐liquids were frequently reported among dual users. Among the e‐cigarette users, 93% reported quitting smoking combustible cigarettes for months or years at the time of the study visit, with only 2 participants reporting quitting combustible cigarettes for weeks.
Table 2.
E‐cigarette Product Characteristics
| E‐Cigarette Users | Dual Users | |
|---|---|---|
| Type of e‐cigarette device used | ||
| First‐generation | 0 | 9 |
| Second‐ or third‐generation | 24 | 40 |
| Types of flavored e‐liquids used | ||
| Unflavored | 0 | 6 |
| Tobacco | 0 | 2 |
| Fruit | 12 | 17 |
| Candy or other dessert | 6 | 5 |
| Vanilla | 2 | 3 |
| Mint or menthol | 2 | 15 |
| Other | 2 | 1 |
Vascular Function and Tonometry
In unadjusted analyses, baseline brachial diameter and flow velocity, flow‐mediated dilation, shear stress, reactive hyperemia, and heart rate were similar across the tobacco product users and the nonsmokers (Table 1). Carotid‐femoral PWV, carotid‐radial PWV, and AIx were different across the groups suggestive of alterations in vascular stiffness. Both central systolic and diastolic BPs were different across the groups (P=0.003 and P<0.001, respectively). Heart rate was similar across all groups.
In multivariable models adjusting for age, sex, race, and study site, the association of AIx persisted with tobacco product use (overall P=0.0008) (Table 3). In post hoc analyses, combustible cigarette users had higher AIx values compared with nonsmokers (129.8±1.5 versus 118.8±2.7, respectively; P=0.003). Dual users had AIx values similar to combustible cigarette users (134.9±4.0 versus 129.8±1.5, respectively; P=1.0) as did sole e‐cigarette users (126.2±5.9 versus 129.8±1.5, respectively; P=1.0) in post hoc analyses (Figure 1). Collectively, these data suggest that e‐cigarette use is associated with measures of vascular stiffness, which has direct relevance to CVD.
Table 3.
Vascular Function and Tonometry Measures Adjusted for Age, Sex, Race, and Study Site
| Nonsmokers | Combustible Cigarette Users | E‐Cigarette Users | Dual Users | P Value | |
|---|---|---|---|---|---|
| Baseline brachial diameter, mm | 3.8±0.08 | 3.9±0.04 | 3.8±0.1 | 3.9±0.1 | 0.63 |
| Baseline mean flow velocity, cm/s | 13.0±1.2 | 16.1±0.6 | 13.5±1.9 | 15.5±1.5 | 0.1 |
| Hyperemic mean flow velocity, cm/s | 73.8±2.7 | 72.2±1.4 | 68.9±4.1 | 73.0±3.3 | 0.79 |
| Flow‐mediated dilation, % | 6.6±0.6 | 6.3±0.3 | 7.3±0.8 | 6.1±0.7 | 0.68 |
| Shear stress, dyne/cm2 | 57.0±2.4 | 54.1±1.3 | 54.4±3.7 | 54.8±3.0 | 0.73 |
| Carotid‐femoral PWV, m/s | 5.7±0.1 | 6.0±0.08 | 6.1±0.3 | 6.3±0.2 | 0.12 |
| Carotid‐radial PWV, m/s | 6.8±0.2 | 7.2±0.1 | 6.8±0.4 | 7.3±0.2 | 0.2 |
| AIx | 118.4±2.6 | 129.8±1.5 | 126.2±5.9 | 134.9±4.0 | 0.0008 |
| Central systolic BP, mm Hg | 105±2 | 110±1 | 106±4 | 114±2 | 0.007 |
| Central diastolic BP, mm Hg | 74±1 | 76±1 | 72±3 | 78±2 | 0.14 |
| Heart rate, beats per min | 69.6±1.2 | 66.6±0.7 | 66.5±2.0 | 68.8±1.6 | 0.1 |
Values are expressed as least square mean±SEM. AIx indicates augmentation index; BP, blood pressure; and PWV, pulse wave velocity.
Figure 1.
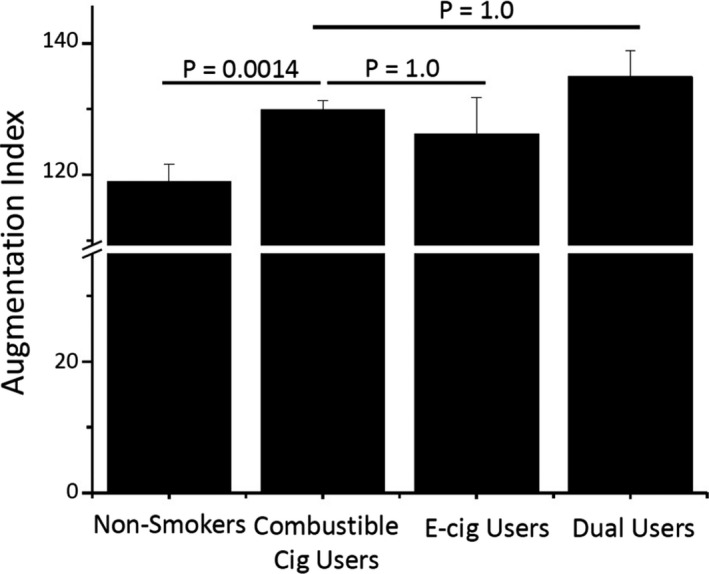
Augmentation index (AIx) is associated with tobacco product use.
AIx for nonsmokers, combustible cigarette users, e‐cigarette users, and dual users following adjustment for age, sex, race, and study site. Data are expressed as least square mean±standard error.
EC Phenotype
In a cross‐sectional cohort of nonsmokers (n=21), combustible cigarette users (n=22), and sole e‐cigarette users (n=14), we evaluated EC phenotype of freshly collected ECs. All groups were similar for sex (P=0.7), and e‐cigarette users were younger and the majority were former smokers (93%) (Table 4). Combustible cigarette smokers were more likely to be black.
Table 4.
Clinical Characteristics of Participants With EC Phenotype Data
| Nontobacco Product Users (n=21) | Combustible Cigarette Users (n=22) | E‐Cigarette Users (n=14) | P Value | |
|---|---|---|---|---|
| Clinical characteristics | ||||
| Age, y | 38±13 | 40±11 | 29±6 | <0.01 |
| Women, % | 43 | 32 | 21 | 0.65 |
| Black race, % | 62 | 91 | 36 | 0.011 |
Values are expressed as mean±SD or percentage. EC indicates endothelial cell.
In ECs, NO (DAF‐2DA fluorescence) production in response to A23187 stimulation differed across the groups (P=0.03). In post hoc analyses, combustible cigarette users had lower A23187‐induced NO production compared with nonsmokers (2.8±2.2% versus 14.1±1.5%, P=0.003) (Figure 2A) consistent with EC dysfunction. E‐cigarette users also had lower A23187‐induced NO production compared with nonsmokers (2.6±3.0% versus 14.1±1.5%, P=0.018). A23187‐stimulated NO production in ECs from combustible and e‐cigarette users was not different (P=0.828), suggesting similar impairment in NO signaling. eNOS levels quantified using immunofluorescence imaging differed across the groups (Figure 2B, P=0.033). E‐cigarette users had lower eNOS levels compared with combustible cigarette users (10.7±2.2 arbitrary units versus 22.1±3.6 arbitrary units, P=0.03) and trended to have lower levels compared with nonsmokers (Figure 2B, P=0.122). Consequently, the differences in NO production could, in part, be caused by differential expression of eNOS. Collectively, these studies suggest that ECs from combustible and e‐cigarette users have similar alterations in EC phenotype indicative of a loss of NO signaling.
Figure 2.
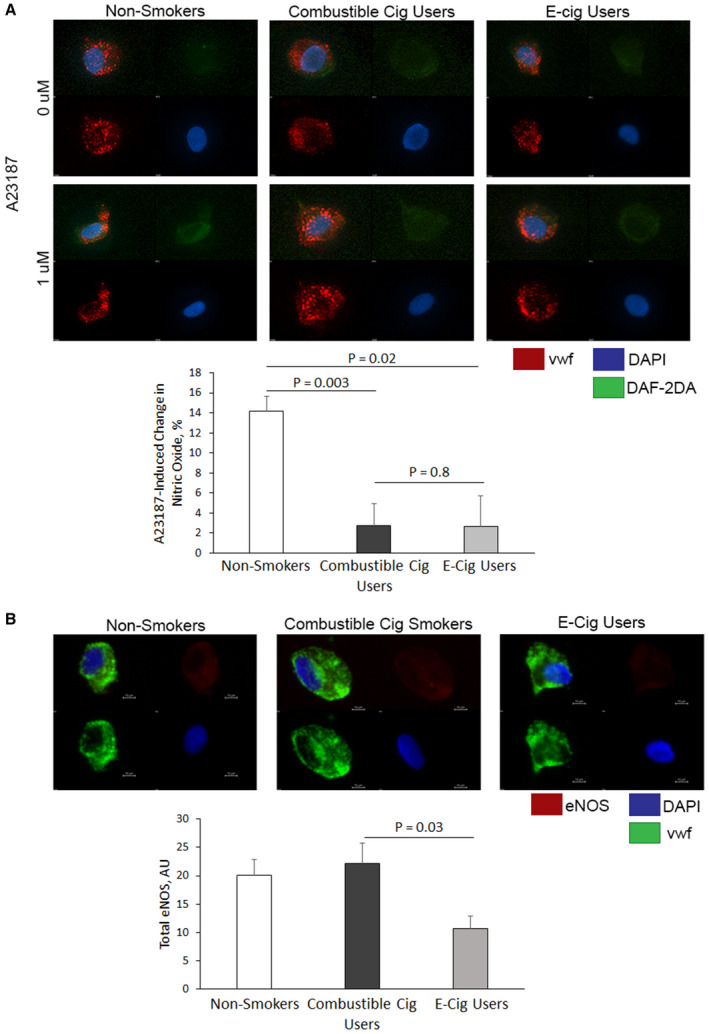
Tobacco product use is associated with impaired endothelial cell (EC) phenotype.
A, Nitric oxide (NO) production (4,5‐diaminofluorescein diacetate [DAF‐2DA] fluorescence) in response to A23187 stimulation in ECs freshly isolated from combustible cigarette users (n=11) and e‐cigarette users (n=5) was lower compared with nontobacco product users (n=10). B, Endothelial NO synthase (eNOS) levels quantified by immunofluorescence in ECs from nontobacco product users (n=11), combustible cigarette users (n=13), and e‐cigarette users (n=12) were similar. Data are expressed as mean±standard error.
Discussion
We performed noninvasive vascular testing in a cohort of young adults without CVD risk factors or CVD, consisting of nonsmokers, combustible cigarette users, e‐cigarette users, and dual users. In agreement with national surveys, adult e‐cigarette users were predominately white and male who were current or former smokers. Many measures of vascular health did not differ between tobacco product users and nonusers including measures of large and small vessel vasodilator response. In unadjusted models, tobacco product use was associated with higher arterial stiffness by multiple measurements. Furthermore, in adjusted models, combustible cigarette use was associated with a higher AIx compared with nonusers. AIx was not different in users of e‐cigarettes alone or in conjunction with combustible cigarette use compared with combustible cigarette use alone. ECs freshly collected from combustible cigarette smokers and sole e‐cigarette users produced less NO in response to A23187 stimulation compared with nonsmokers, suggestive of impaired eNOS signaling. The lower NO production in the cells from e‐cigarette users could, in part, be explained by lower eNOS expression. These findings suggest that there was not a vascular benefit to the addition or substitution of e‐cigarettes. In addition, several measures of vascular function may be relatively insensitive to detect the vascular effects of chronic tobacco product use in healthy young individuals. Measures of vascular stiffness may be more sensitive than measures of vasodilation for detecting effects associated with chronic tobacco use, and measures of the response to acute use may be needed to enhance the detection of vascular effects of specific products.
Previous work has shown that increased vascular stiffness and sympathetic regulation of BP and heart rate are associated with the use of combustible cigarettes.10, 11, 12, 22, 23, 24 Among younger individuals, a higher AIx is associated with early alterations in vascular remodeling and is thought to be an early indicator of arterial remodeling and future central aortic stiffness.25 In a cross‐sectional study, AIx in young chronic smokers was found to be higher than that in age‐ and sex‐matched nonsmokers, and smoking a single combustible cigarette led to an acute increase in the carotid‐femoral PWV.24 It has also been reported that in smokers acute use of an e‐cigarette with nicotine or smoking a single combustible cigarette increased carotid‐femoral PWV, when compared with the use of an e‐cigarette without nicotine. These findings suggest that nicotine is a contributor to the hemodynamic effects associated with acute e‐cigarette use.23
Our study provides additional insights into the chronic effects of e‐cigarette use. We found that chronic e‐cigarette use, alone or in conjunction with combustible cigarette use, was associated with a similar impairment of selected arterial stiffness measures. There is no evidence from our study that e‐cigarettes are a harm reduction tobacco product as compared with combustible cigarettes. Our observation of the association of higher AIx and impaired eNOS signaling with e‐cigarette use could indicate adverse vascular remodeling, which, with continued tobacco product use, may lead to hypertension. The cross‐sectional nature of our study precludes direct evaluation of the effect of switching from combustable cigarette use to e‐cigarette use. However, we required a minimum of 3 months of e‐cigarette use to classify patients as e‐cigarette users; e‐cigarette use had to be exclusive for at least 3 months in the exclusive e‐cigarette use group. Prior studies have shown a reduction in AIx with smoking cessation in healthy tobacco users in as litte as 4 weeks.26 Thus, our findings are consistent with the possibility that e‐cigarette use does not confer the same benefit as complete cessation of tobacco products.
Our finding that endothelial function was similar in tobacco product users compared with nonusers is in contrast to prior reports. Several large cohort studies, including the Framingham Heart Study, have shown lower flow‐mediated dilation associated with active combustible cigarette use.18, 27 In addition, the acute use of combustible cigarettes or e‐cigarettes has been reported to impair endothelial function that may be in part attributable to nicotine exposure.28, 29 In our study we did not observe a difference in flow‐mediated dilation in tobacco product users. Many factors may account for the apparent contradiction of the prior literature. It may be, at least in part, attributable to tobacco product abstinence 8 to 12 hours before the study visit. Another reason for this lack of difference may be lower exposure (fewer pack‐years) in our cohort. Indeed, previous studies have found a consistent inverse association between flow‐mediated dilation with the number of pack‐years.22 In addition, many of the prior studies involved cohorts with a greater burden of cardiovascular risk factors and more advanced age. However, in our study, the ECs from combustible cigarette and sole e‐cigarette users had impaired NO production in response to A23187, suggestive of endothelial dysfunction. Nevertheless, further work is required to assess how the duration and the intensity of use affect vascular function, and whether there is a threshold of exposure at which the use of tobacco products significantly and chronically affect endothelial function.
Despite its many strengths related to the concurrent evaluation of several vascular measures across users of tobacco products, our study has several limitations. The study groups were inherently different regarding age, race, and sex. For example, the sole e‐cigarette users were predominantly white males and former smokers, which is consistent with national surveys of tobacco use.1, 2 Consequently, residual confounding can not be fully excluded. Additionally, it remains possible that longer time periods of exclusive e‐cigarette use would be required to observe improvements in cardiovascular health metrics, although, as noted, prior studies have suggested that improvements in AIx occur in as little as 4 weeks. Further, most of the e‐cigarette users in our study reported using nicotine in their devices and it is possible that products with less or no nicotine may be associated with reduced cardiovascular harm. However, a number of studies indicate that e‐cigarette users self‐titrate in order to obtain similar levels of nicotine, regardless of the product nicotine content. Moreover, even though we measured urinary cotinine to validate self‐reported tobacco product use, we were unable to differentiate between combustible and e‐cigarette use with urinary cotinine as both products contain nicotine. Therefore, we are unable to validate that sole e‐cigarette users are completely abstaining from combustible cigarettes. Additionally, our study cohort consisted primarily of healthy, young adults, and it is likely that they may have responded differently compared with individuals with cardiovascular risk factors. We examined venous ECs rather than arterial ECs, which may be more relevant to CVD. However, previous studies have shown correlated findings in arterial and venous ECs collected using similar methodology.30, 31 Finally, e‐cigarettes represent a diverse class of tobacco products with a wide range of operating conditions, use patterns, product characteristics, and e‐liquid constituents, which often include varying levels of nicotine, several flavors, and different ratios of the vehicles—glycerin and propylene glycol. Thus, it appears likely that the use of different products may be associated with exposure to different toxicants that exert different toxicities.
Conclusions
Our study provides new insights into the effects of tobacco product use on measures of vascular function in young, healthy adult individuals without CVD risk factors. The most recent nationally representative sample shows that the majority of adult e‐cigarette users are either former (36.5%) or current (22.1%) combustable cigarette smokers emphasizing the importance of understanding cardiovascular health measures in these groups.32 Significantly, we found that e‐cigarette use either with or without combustible cigarette use was associated with a similar elevation of AIx, a measure of vascular stiffness, as compared with users of combustible cigarettes alone. Several measures of vascular function did not distinguish between tobacco product users and nonusers in young healthy adults. These data suggest that the abnormalities in vascular stiffness persist in e‐cigarette users and that, at least within the limitations of our cohort and measurement approaches, there was no evidence that the use of e‐cigarettes reduces cardiovascular injury, dysfunction, or harm associated with the use of combustible tobacco products. Further, ECs from combustible cigarette and e‐cigarette users had impaired A23187‐induced NO production, suggestive of EC dysfunction. With the diversity of tobacco products available and continuing to increase, methods to evaluate tobacco product–induced cardiovascular toxicity are needed. Our study suggests that measures of vascular stiffness, such as AIx, may be useful methods in evaluating novel tobacco product cardiovascular toxicity.
Sources of Funding
This work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award numbers 5P50HL120163 and U54HL120163, and an American Heart Association Mentored Clinical and Population Research Award 17MCPRP32650002 (Fetterman). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
None.
Supporting information
Table S1
(J Am Heart Assoc. 2020;9:e014570 DOI: 10.1161/JAHA.119.014570.)
For Sources of Funding and Disclosures, please see page 8.
References
- 1. Rodu B, Plurphanswat N. E‐cigarette use among US adults: population assessment of tobacco and Health (PATH) study. Nicotine Tob Res. 2018;20:940–948. [DOI] [PubMed] [Google Scholar]
- 2. Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C, Choi K, Anic G, Goniewicz ML, Cummings KM, et al. Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, waves 1 and 2 (2013–2015). Tob Control. 2019;28:50–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Silveira ML, Conway KP, Green VR, Kasza KA, Sargent JD, Borek N, Stanton CA, Cohn A, Hilmi N, Cummings KM, et al. Longitudinal associations between youth tobacco and substance use in waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study. Drug Alcohol Depend. 2018;191:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, et al. Heart disease and stroke statistics‐2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 5. Burns DM. Epidemiology of smoking‐induced cardiovascular disease. Prog Cardiovasc Dis. 2003;46:11–29. [DOI] [PubMed] [Google Scholar]
- 6. Gokce N, Keaney JF Jr, Hunter LM, Watkins MT, Nedeljkovic ZS, Menzoian JO, Vita JA. Predictive value of noninvasively determined endothelial dysfunction for long‐term cardiovascular events in patients with peripheral vascular disease. J Am Coll Cardiol. 2003;41:1769–1775. [DOI] [PubMed] [Google Scholar]
- 7. Huang AL, Silver AE, Shvenke E, Schopfer DW, Jahangir E, Titas MA, Shpilman A, Menzoian JO, Watkins MT, Raffetto JD, et al. Predictive value of reactive hyperemia for cardiovascular events in patients with peripheral arterial disease undergoing vascular surgery. Arterioscler Thromb Vasc Biol. 2007;27:2113–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ben‐Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, Boutouyrie P, Cameron J, Chen CH, Cruickshank JK, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta‐analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63:636–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation. 2010;121:505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Powell JT. Vascular damage from smoking: disease mechanisms at the arterial wall. Vasc Med. 1998;3:21–28. [DOI] [PubMed] [Google Scholar]
- 11. Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34:509–515. [DOI] [PubMed] [Google Scholar]
- 12. Benowitz NL. Cigarette smoking and cardiovascular disease: pathophysiology and implications for treatment. Prog Cardiovasc Dis. 2003;46:91–111. [DOI] [PubMed] [Google Scholar]
- 13. Haussmann HJ. Use of hazard indices for a theoretical evaluation of cigarette smoke composition. Chem Res Toxicol. 2012;25:794–810. [DOI] [PubMed] [Google Scholar]
- 14. Jensen RP, Luo W, Pankow JF, Strongin RM, Peyton DH. Hidden formaldehyde in e‐cigarette aerosols. N Engl J Med. 2015;372:392–394. [DOI] [PubMed] [Google Scholar]
- 15. Fagan P, Pokhrel P, Herzog TA, Moolchan ET, Cassel KD, Franke AA, Li X, Pagano I, Trinidad DR, Sakuma KK, et al. Sugar and aldehyde content in flavored electronic cigarette liquids. Nicotine Tob Res. 2018;20:985–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ogunwale MA, Li M, Ramakrishnam Raju MV, Chen Y, Nantz MH, Conklin DJ, Fu XA. Aldehyde detection in electronic cigarette aerosols. ACS Omega. 2017;2:1207–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Keith RJ, Fetterman JL, Riggs DW, O'Toole T, Nystoriak JL, Holbrook M, Lorkiewicz P, Bhatnagar A, DeFilippis AP, Hamburg NM. Protocol to assess the impact of tobacco‐induced volatile organic compounds on cardiovascular risk in a cross‐ sectional cohort: cardiovascular Injury due to Tobacco Use study. BMJ Open. 2018;8:e019850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr, Lehman BT, Fan S, Osypiuk E, Vita JA. Clinical correlates and heritability of flow‐mediated dilation in the community: the Framingham Heart Study. Circulation. 2004;109:613–619. [DOI] [PubMed] [Google Scholar]
- 19. Chung WB, Hamburg NM, Holbrook M, Shenouda SM, Dohadwala MM, Terry DF, Gokce N, Vita JA. The brachial artery remodels to maintain local shear stress despite the presence of cardiovascular risk factors. Arterioscler Thromb Vasc Biol. 2009;29:606–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Supiano MA, Lovato L, Ambrosius WT, Bates J, Beddhu S, Drawz P, Dwyer JP, Hamburg NM, Kitzman D, Lash J, et al. Pulse wave velocity and central aortic pressure in systolic blood pressure intervention trial participants. PLoS One. 2018;13:e0203305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Butlin M, Qasem A. Large artery stiffness assessment using sphygmocor technology. Pulse (Basel). 2017;4:180–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Celermajer DS, Sorensen KE, Georgakopoulos D, Bull C, Thomas O, Robinson J, Deanfield JE. Cigarette smoking is associated with dose‐related and potentially reversible impairment of endothelium‐dependent dilation in healthy young adults. Circulation. 1993;88:2149–2155. [DOI] [PubMed] [Google Scholar]
- 23. Franzen KF, Willig J, Talavera SC, Meusel M, Sayk F, Reppel M, Dalhoff K, Mortensen K, Droemann D. E‐Cigarettes and cigarettes worsen peripheral and central hemodynamics as well as arterial stiffness: a randomized, double‐blinded pilot study. Vasc Med. 2018;23:419–425. [DOI] [PubMed] [Google Scholar]
- 24. Mahmud A, Feely J. Effect of smoking on arterial stiffness and pulse pressure amplification. Hypertension. 2003;41:183–187. [DOI] [PubMed] [Google Scholar]
- 25. McEniery CM, Yasmin Hall IR, Qasem A, Wilkinson IB, Cockcroft JR; ACCT Investigators . Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo‐Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 2005;46:1753–1760. [DOI] [PubMed] [Google Scholar]
- 26. Rehill N, Beck CR, Yeo KR, Yeo WW. The effect of chronic tobacco smoking on arterial stiffness. Br J Clin Pharmacol. 2006;61:767–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hamburg NM, Keyes MJ, Larson MG, Vasan RS, Schnabel R, Pryde MM, Mitchell GF, Sheffy J, Vita JA, Benjamin EJ. Cross‐sectional relations of digital vascular function to cardiovascular risk factors in the Framingham Heart Study. Circulation. 2008;117:2467–2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, Peruzzi M, Marullo AG, De Falco E, Chimenti I, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150:606–612. [DOI] [PubMed] [Google Scholar]
- 29. Chaumont M, de Becker B, Zaher W, Culie A, Deprez G, Melot C, Reye F, Van Antwerpen P, Delporte C, Debbas N, et al. Differential effects of E‐cigarette on microvascular endothelial function, arterial stiffness and oxidative stress: a randomized crossover trial. Sci Rep. 2018;8:10378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Colombo PC, Ashton AW, Celaj S, Talreja A, Banchs JE, Dubois NB, Marinaccio M, Malla S, Lachmann J, Ware JA, et al. Biopsy coupled to quantitative immunofluorescence: a new method to study the human vascular endothelium. J Appl Physiol. 2002;92:1331–1338. [DOI] [PubMed] [Google Scholar]
- 31. Silver AE, Christou DD, Donato AJ, Beske SD, Moreau KL, Magerko KA, Seals DR. Protein expression in vascular endothelial cells obtained from human peripheral arteries and veins. J Vasc Res. 2010;47:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dai H, Leventhal AM. Prevalence of e‐cigarette use among adults in the United States, 2014–2018. JAMA. 2019;322:1824–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


