Abstract
Background
COVID-19 pandemic has affected routine immunization globally. Impact will likely be higher in low and middle-income countries with limited healthcare resources and fragile health systems. We quantified the impact, spatial heterogeneity, and determinants for childhood immunizations of 48 million population affected in the Sindh province of Pakistan.
Methods
We extracted individual immunization records from real-time provincial Electronic Immunization Registry from September 23, 2019, to July 11, 2020. Comparing baseline (6 months preceding the lockdown) and the COVID-19 lockdown period, we analyzed the impact on daily immunization coverage rate for each antigen by geographical area. We used multivariable logistic regression to explore the predictors associated with immunizations during the lockdown.
Results
There was a 52.5% decline in the daily average total number of vaccinations administered during lockdown compared to baseline. The highest decline was seen for Bacille Calmette Guérin (BCG) (40.6% (958/2360) immunization at fixed sites. Around 8438 children/day were missing immunization during the lockdown. Enrollments declined furthest in rural districts, urban sub-districts with large slums, and polio-endemic super high-risk sub-districts. Pentavalent-3 (penta-3) immunization rates were higher in infants born in hospitals (RR: 1.09; 95% CI: 1.04–1.15) and those with mothers having higher education (RR: 1.19–1.50; 95% CI: 1.13–1.65). Likelihood of penta-3 immunization was reduced by 5% for each week of delayed enrollment into the immunization program.
Conclusion
One out of every two children in Sindh province has missed their routine vaccinations during the provincial COVID-19 lockdown. The pool of un-immunized children is expanding during lockdown, leaving them susceptible to vaccine-preventable diseases. There is a need for tailored interventions to promote immunization visits and safe service delivery. Higher maternal education, facility-based births, and early enrollment into the immunization program continue to show a positive association with immunization uptake, even during a challenging lockdown.
Keywords: Immunization coverage, COVID-19, Electronic Immunization Registry, Predictors of immunization, mHealth
Abbreviations: AIDS, Acquired Immunodeficiency Syndrome; AIC, Akaike’s information criterion (AIC); BCG, Bacille Calmette Guérin; CNIC, Computerized National Identity Card; COVID-19, Coronavirus Disease; EIR, Electronic Immunization Registry; DHHS, US Department of Health and Human Services; EPI, Expanded Programme on Immunization; FIC, Fully Immunized Child; GLM, Generalized linear modeling; HIV, Human Immunodeficiency Virus; IPV, Inactivated polio vaccine; IRB, Institutional Review Board; IPC, Infection Prevention Control; OHRP, Office for Human Research Protections; OPV, Oral polio vaccine; PCV, Pneumococcal Vaccine; PPE, Personal Protective Equipment; SARS, Severe Acute Respiratory Syndrome; SD, Standard deviation; SHRUCs, Super High Risk Union Councils; SIA, Supplementary Immunization Activities; SMS, Short Messaging Service; SOP, Standard Operating Procedures; TCV, Typhoid Conjugate Vaccine; UCs, Union Councils; VPDs, Vaccine-Preventable Diseases
1. Introduction
The current COVID-19 pandemic has been declared as the ‘worst public health crises in a generation' [1], with over 12 million confirmed positive cases and 556,342 reported deaths across 213 countries as of July 11, 2020 [2]. The unprecedented spread of the disease has prompted a drastic shift in global social norms and has disrupted the provision of regular health services [3]. This will have far-reaching implications for the control of other infectious diseases and preventable illnesses.
The pandemic’s impact on routine immunization is of considerable importance. It could lead to higher morbidity and mortality from vaccine-preventable diseases (VPDs) in countries with already poor coverage rates. Among the 73 Gavi-eligible countries, 69 have reported COVID-19 cases, with Indonesia, India, and Pakistan comprising the highest number of cases. Incidentally, these countries also have the highest number of zero-dose children [4] (a child who has not received any of the EPI recommended routine vaccinations). In Pakistan, the fully immunized child (FIC) coverage (a child who has received all of the required immunization doses as per the immunization schedule) stands at 66% [5], with frequent polio and measles outbreaks [6], [7]. The COVID-19 pandemic plays out against this backdrop of suboptimal immunization in the country. Pakistan reported its first COVID-19 case on February 26, 2020, a restriction on movement was put in place in Sindh province on March 23, and as of July 11, 2020, 248,856 cases were confirmed with 5197 reported deaths [8].
As regular health services continue to be disrupted, it becomes critically important to understand the impact on routine immunizations, especially as health experts warn regarding impending VPD outbreaks and resurgence of polio in countries now polio-free [9]. Shifts in health-seeking behaviors following social distancing measures and lockdowns, and fear of contagion are forcing parents to delay routine childhood vaccinations [10]. Simultaneously, as health services continue to be overstretched, governments have little choice other than taking drastic measures, including reallocating resources from immunization activities to the COVID-19 response [11]. Approximately 6260 health professionals involved in polio eradication in Pakistan have been engaged in COVID-19 surveillance, contact tracing, improving testing capacities, and health communication [12], and the national Polio helpline has also been redirected to the provision of information related to COVID-19. All Supplementary Immunization Activities (SIA), the cornerstone of the polio eradication strategy, have been suspended until further notice. The last scheduled SIA (for fractional inactivated polio vaccine (IPV) Campaign) on March 24, 2020, in Karachi, Sindh, was postponed to deal with the COVID-19 crises [13], in line with global recommendations [14], [15].
Several studies [16], [17], [18], [19], [20], [21] have shown how health emergencies have distorted existing health systems and health-seeking behaviors, precipitating secondary disease outbreaks. During the Ebola epidemic in West Africa, a secondary measles outbreak was brought about by the disruption of vaccination campaigns with a 25–75% reduction in immunization coverage rates, non-functional healthcare systems (including detection and reporting of measles cases), lack of specific treatment, and a fear of contracting Ebola virus disease leading to reluctance in seeking health assistance [16]. During the Ebola outbreak in Sierra Leone, health services were severely affected, and factors such as patients' fear of Ebola and death of healthcare staff affected health-seeking behavior and adversely impacted health service functioning [17]. The modeling studies also showed the exacerbation of mortality due to malaria, Human Immunodeficiency Virus (HIV) or Acquired Immunodeficiency Syndrome (AIDS), and Tuberculosis as a result of the Ebola epidemic in several African countries [18]. The Severe Acute Respiratory Syndrome (SARS) outbreak also demonstrated how people changed their traveling behavior, with over 70% of respondents avoiding visiting hospitals or mainland China to avoid contracting SARS [19]. With COVID-19 pandemic, there is concern for measles resurgence, because it is highly contagious and known to hit hard in the aftermath of disasters and humanitarian emergencies [20], [21], and also given the resurgence of this disease in the recent past.
UNICEF and WHO are calling for a need to maintain routine immunization activities where possible [22]. Examining the trends in routine immunization as the COVID-19 situation unfolds can reveal key insights, and could inform and support Expanded Programme on Immunization (EPI) stakeholders and partners in devising strategies to minimize the number of dropped-out children (children between the age of 0–23 months who start the EPI recommended vaccination schedule but fail to complete it) [23] during the COVID-19 lockdown, and cover all missed children with accelerated efforts as soon as restrictions are eased. Our primary research question is to examine the impact of COVID-19 lockdown on routine immunization in Sindh province, Pakistan, using data from the provincial Electronic Immunization Registry (EIR). We aim to measure the reduction in daily immunization rates in Sindh province, report antigen-wise coverage, and drop-out rates for 0–23 month children, identify baseline characteristics associated with drop-outs, and observe the spatial distribution of immunization activity.
2. Methods
2.1. Population
Sindh province, in the south of Pakistan, is home to at least 47.9 million people. With a population density of 339.9 people/km2 [24], the province is spread across seven divisions comprising 29 districts further subdivided into 1123 union councils (or UC; the smallest sub-district geographic administrative unit [25]). The median population of districts is 1,608,849 (range 725,922–4,744,538) while that of UCs is 37,554 (range 2926–265,842). The annual target population (0–23 month old children) for EPI is 3.5 million in 2020 [25], and the immunizations are administered predominantly through public services (1518 immunization centers supplemented by outreach), supported by approximately 225 private clinics [25], [26]. Outreach is defined as “immunization sessions held in a location other than a health facility, from which health workers can go out and return the same day [27]”. Outreach vaccinations only occur through public immunization centers. Approximately 60% of all immunizations in the province occur at fixed centers, whereas the rest are delivered through outreach sessions [28].
2.2. Data source
We used immunization records from the Government of Sindh’s Zindagi Mehfooz (Safe Life) Electronic Immunization Registry (ZM EIR). The ZM EIR [29] is an Android-based application for immunization management that enables vaccinators to enroll and follow children using smartphones. The ZM EIR is rolled-out across 29 districts of Sindh and is used by all 2755 vaccinators (comprising of 12.8% (352/2755) females) working at 1518 public and 151 private immunization clinics across those districts. As of July 2020, >3.1 million children and >1.1 million women have been enrolled, and >24 million immunization events (administration of a vaccine dose) have been recorded in the ZM EIR. In 2019, ZM EIR enrolled 83% of the EPI estimated annual live birth cohort for the 27 districts. The EIR was launched in the remaining two districts, District Khairpur and District Dadu, as of March 01, 2020, and July 03, 2020, respectively. The analysis was deemed to be exempt by the Institutional Review Board (IRB) at Interactive Research and Development under 45 CFR 46.101(b). The IRB is registered with the US Department of Health and Human Services (DHHS) Office for Human Research Protections (OHRP) with registration number IRB 00005148.
2.3. Vaccination schedule
Pakistan’s routine EPI immunization schedule includes six visits and covers ten VPDs including Tuberculosis (BCG; Bacille Calmette Guérin), Polio (OPV/IPV; Oral and Inactivated polio vaccine), Diphtheria, Tetanus, Pertussis, Haemophilus influenza, Hepatitis B (penta; pentavalent vaccine), Pneumococcal diseases (PCV 10), rotavirus diarrhea, and Measles. As of January 2020, Typhoid Conjugate Vaccine (TCV) was also added to the routine immunization schedule.
2.4. COVID-19 lockdown
The Sindh provincial government announced a 15-day lockdown starting at midnight on March 23, 2020, which was initially extended to April 14, then to April 30, 2020, and finally to May 09, 2020. It was a complete ban on movement, and exemptions were given only to essential service providers, including health, law enforcement, utility, and telecommunications [30]. For the public, they allowed limited exemptions for grocery shopping or urgent medical care. For immunizations, EPI-Sindh issued a notification on March 23, 2020, suspending all outreach activities with immediate effect; however, District and Town (administrative sub-division of a district) supervisors (responsible for overseeing vaccine supply chain and administration, and monitoring the vaccinators at district and town level respectively) were ordered to continue routine vaccination activities at immunization centers. Due to the rising infection rates, a smart lockdown (shutting down potential COVID-19 hotspot areas only) was later imposed from June 19, 2020.
2.5. Outcome
Primary outcome of the analysis was the receipt of EPI recommended vaccinations (BCG, polio, penta, PCV10, rotavirus, and measles) during the COVID-19 lockdown period. The number of antigens and the vaccine administration site i.e. fixed vs. outreach were compared for baseline period and COVID-19 lockdown period. The completion of 3 doses of pentavalent vaccine was used as the outcome in the regression analysis. Three doses of Pentavalent vaccine (penta-3) is one of the standard measures for indicating the reach of routine immunization systems in countries that have taken pentavalent to scale [31]. All the outcomes were measured in children 0–23 months of age.
2.6. Procedure
We used immunization records from the ZM EIR from September 23, 2019, to July 11, 2020. We extracted immunization history (antigen and dates of administrations) and other routinely collected data (gender, place, and date of birth, maternal education, cell phone access, Computerized National Identity Card (CNIC) provision) including geographical location (district, urban areas, slum areas) and modality of immunization service delivery (fixed or outreach activity) for all children who received immunizations or were due for immunization during the baseline and COVID-19 lockdown periods. We also extracted facility and vaccinator attendance and immunization activity data. A 6-month baseline period (September 23, 2019, to March 22, 2020) was selected and compared to COVID-19 lockdown period (March 23–May 09, 2020). We used a 6-month period prior to the COVID-19 lockdown as our baseline to average out the impact of confounding exogenous variables (seasonality, periodic enhanced outreach immunization activities in the province, and other interventions to boost immunization coverage). The comparison analysis included data from 27 districts as baseline data was not available for District Khairpur and Dadu. However, the regression analysis utilized data from COVID-19 lockdown period covering 28 districts to utilize the maximum data available for the analysis. Based on EPI-Sindh’s classification of slum areas in seven districts of Karachi and Hyderabad, we defined slum UCs as having >75% population living in slum areas. Slum is a contiguous settlement where the inhabitants are characterized as having inadequate housing and basic services. Slums are often not recognized and addressed by the public authorities as an integral or equal part of a city [32]. The Super High Risk Union Councils (SHRUCs) (8 out 1123 in Sindh) are defined by the EPI based on poliovirus circulation, the occurrence of polio cases, and accessibility. Enrollments were defined as children getting registered into EIR for the first time (83% enrollments happen at BCG and penta-1) while follow-up visits were for remaining immunization visits. The due dates for follow-up immunizations were calculated as per the EPI recommended schedule for all children enrolled in the EIR.
2.7. Statistical analysis
For summary measures, we used frequencies (%) for categorical data, and means, and standard deviation (SD) for continuous data. The percentage of missing entries for variables is reported. Student's t-test and the Pearson’s chi-square test were used to evaluate differences between groups. We analyzed the decline in the number of immunization visits and antigens administered across Sindh province, comparing geographic variation by district, urbanization, slum, and super high-risk UC status. Factors influencing the probability of a child being immunized with penta-3 during the COVID-19 lockdown were explored through logistic regression analysis using generalized linear modeling (GLM). The a-priori specified covariates were selected based on evidence and knowledge including gender, place of birth, enrollment area (urban/rural status), enrolment vaccination site (fixed/outreach), maternal education, age at enrollment, age at immunization visits to denote timeliness of immunizations, and provision of contact number [33], [34], [35], [36], [37]. We used a backward stepwise approach for final multivariable model selection with adjustment for gender as a lockterm. We specified p-value of 0.05 for entry and 0.1 for removal as the criterion for multivariable model selection to identify a parsimonious model with the lowest Akaike’s information criterion (AIC) score. All tests were 2-sided, and the measure of statistical significance was set at 0.05. We calculated coverage using monthly vaccination targets as per EPI estimated annual birth cohort, which is calculated as 3.5% of the total population. We performed statistical analyses with Stata, release 14 (StataCorp, College Station, TX). Digital maps were used to review the percentage change in immunization coverage by the district using QGIS (version 2.16).
2.8. Role of the funding source
The data analyzed in this manuscript was collected through the EIR system supported by Gavi, the Vaccine Alliance, and WHO. There was no funding source for the specific analyses conducted as part of the study. The corresponding author had full access to all the data and the final responsibility to submit for publication.
3. Result
From September 23, 2019, to May 09, 2020, a total of 2,787,450 children were immunized, out of whom 31.2% (869,685/2,787,450) were first visits (enrollments). During the baseline (September 23, 2019, to March 22, 2020) there were 2,463,595 immunization visits, out of which 31.9% (786,325/2,463,595) were enrollments while 323,855 immunization visits occurred during the lockdown (March 23 - May 09, 2020), out of which 25.7% (83,360/323,855) were enrollments. Moreover, during the lockdown, 561,826 children were due for follow-up immunizations, out of whom 30.7% (172,228/561,826) were vaccinated. In contrast, the follow-up success rate during the baseline was 70.5% (1,142,915/1,620,896).
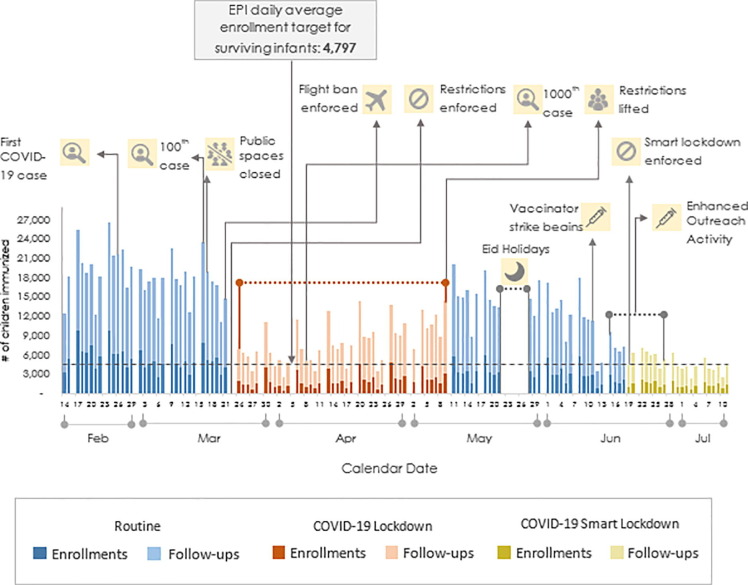
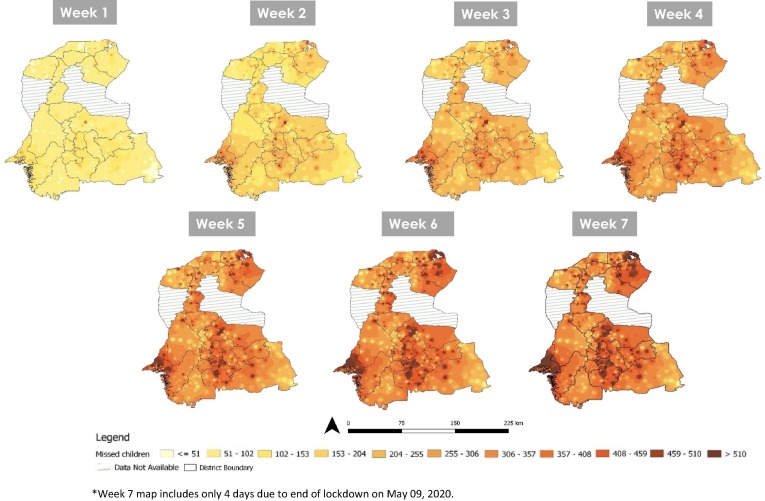
A 51.0% decrease in average daily immunizations was noted during the lockdown compared to baseline, and the reduction was heterogeneous across districts and union councils (Figure S-1 in supplementary information). A more detailed breakdown by districts is provided in Figure S-2 and Table S-1 in the Supplementary information. On average, 8438 children (aged 0–23 months)/day missed routine immunizations in the Sindh, out of whom 37.8% (3193/8438) were for enrollments i.e. these children had potentially not had any prior contact with the immunization system. Further analysis after the lockdown was lifted on May 10, 2020, showed a steady recovery in coverage rates. From May 10 to July 11, 2020, there was an absolute improvement of 9% in average daily immunization visits (42% decrease during post-lockdown vs. 51% during lockdown periods) (Fig. 1 ). The cohort of children who missed follow-up immunizations was accumulating disproportionately through the province (Fig. 2 ). District West Karachi had the highest number of missed children (6.8%; 26,620/389,598), and overall 29.4% (114,442/389,598) of the missed children were concentrated in 5 districts of Sindh (West Karachi, Hyderabad, Badin, Sanghar and Naushero Feroz).
Fig. 1.
Daily immunization visits and enrollments of 0-23 months old children in ZM EIR during pre-COVID-19 lockdown period (February 14-March 22, 2020), COVID-19 lockdown period (March 23-May 09, 2020), post COVID-19 lockdown period (May 10-June 18, 2020) and COVID-19 Smart lockdown period (June 19-July 11, 2020) in Sindh province.
Fig. 2.
Weekly cumulative distribution of 0-23 months old children (geocoded at enrollment visit) who missed immunization follow-up visits across Sindh Province during COVID-19 lockdown (March 23-May 09, 2020) (n = 389,598).
There was a significant decline in the daily average number of vaccine doses administered for all the antigens (Table 1 ). The attrition trend showed a lower drop in percentage for antigens given later in the EPI schedule. For maternal Tetanus Toxoid (TT) vaccinations, there was a 28.8% (807/2,798) decrease in daily average TT vaccinations administered during the lockdown compared to baseline (1,991 vs. 2,798 vaccinations). There was limited outreach activity in five out of 27 districts during the first four weeks of lockdown (March 23, 2020-April 23, 2020) showing a decline of 79.3% (range 73.0%−83.5%), while the fixed sites showed a decrease of 32.1% (range 20.9%–40.6%), with an overall reduction of 52.5% (range: 47.4%–56.6%). At fixed sites, the largest decline was seen with the BCG vaccine dose (40.6%), while the measles-1 dose showed the least reduction (20.9%). Overall, the 52.5% drop in the daily average number of immunization doses administered was predominantly because of the lack of immunizations given at outreach sites during the lockdown.
Table 1.
Average daily number of vaccine doses administered to 0–23 months old children by fixed and outreach vaccination services in ZM EIR during baseline (September 23, 2019 - March 22, 2020) and COVID-19 lockdown (March 23-May 09, 2020) periods in Sindh, Pakistan (n = 8,321,931).
| Baseline period (n = 7,380,161) |
COVID-19 lockdown(n = 941,770) |
Difference in COVID-19 lockdown vs. baseline |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Fixed | Outreach | Total | Fixed | Outreach | Total | Fixed | Outreach | Total | |
| % | % | % | |||||||
| BCG | 2360 | 1396 | 3756 | 1402 | 230 | 1632 | −40.6 | −83.5 | −56.6 |
| OPV-0 | 1885 | 841 | 2726 | 1170 | 149 | 1319 | −37.9 | −82.3 | −51.6 |
| Penta-1 | 2107 | 1561 | 3668 | 1312 | 287 | 1600 | −37.7 | −81.6 | −56.4 |
| OPV-1 | 2107 | 1569 | 3676 | 1323 | 288 | 1611 | −37.2 | −81.6 | −56.2 |
| PCV-1 | 2104 | 1558 | 3663 | 1310 | 286 | 1596 | −37.8 | −81.6 | −56.4 |
| Rota-1 | 2067 | 1529 | 3596 | 1302 | 278 | 1580 | −37.0 | −81.8 | −56.1 |
| Penta-2 | 1762 | 1369 | 3131 | 1227 | 306 | 1533 | −30.3 | −77.7 | −51.0 |
| OPV-2 | 1762 | 1370 | 3132 | 1236 | 308 | 1543 | −29.9 | −77.5 | −50.7 |
| PCV-2 | 1761 | 1367 | 3128 | 1226 | 303 | 1529 | −30.4 | −77.8 | −51.1 |
| Rota-2 | 1703 | 1317 | 3019 | 1200 | 290 | 1489 | −29.5 | −78.0 | −50.7 |
| Penta-3 | 1564 | 1310 | 2874 | 1167 | 283 | 1450 | −25.3 | −78.4 | −49.5 |
| OPV-3 | 1566 | 1311 | 2878 | 1176 | 285 | 1461 | −24.9 | −78.3 | −49.2 |
| IPV | 1655 | 1419 | 3074 | 1193 | 295 | 1488 | −27.9 | −79.2 | −51.6 |
| PCV-3 | 1563 | 1309 | 2872 | 1163 | 281 | 1444 | −25.6 | −78.5 | −49.7 |
| Measles-1 | 1233 | 1211 | 2444 | 976 | 310 | 1286 | −20.9 | −74.4 | −47.4 |
| Measles-2 | 909 | 986 | 1896 | 716 | 266 | 982 | −21.2 | −73.0 | −48.2 |
| Total | 28,108 | 21,423 | 49,531 | 19,099 | 4445 | 23,544 | –32.1 | −79.3 | −52.5 |
* Outreach Activities were only conducted in West District, Karachi, Ghotki District, Sujawal District, Shaheed Benazir Abad District Mirpurkhas District from March 23-April 23, 2020.
Several characteristics of children immunized during lockdown were different compared to the baseline period (Table 2 ). During the baseline, the number of children enrolled is higher than the EPI estimated target of enrollments, whereas during lockdown enrollments were reduced (109.7% vs. 43.3%). Although the sex distribution between baseline and lockdown is statistically significant, the actual difference from baseline is small (0.7%, p-value ≤ 0.0001; 95% CI: 0.34–1.06). Children immunized during lockdown, as compared to baseline, had a higher proportion of facility-based births, more caregivers had provided contact numbers (33.2% vs. 27.4%, p-value ≤ 0.01; 95% CI: 5.47–6.13), and the mean age at BCG vaccination was lower (4.3 vs. 6.3 weeks, p-value ≤ 0.01; 95% CI: 1.93–2.07). Additionally, more children with higher maternal education, (in the category 9 years and above) were enrolled during lockdown as compared to baseline (p-value ≤ 0.01; 95% CI: 1.01–1.45). Daily average vaccinator attendance was 7.4% (p-value < 0.0001; 95% CI: 5.29–9.51) lower during the lockdown compared to baseline (78.8% (79,252/100,600 person days) vs. 86.2% (312,386/362,551 person days) respectively). The reduction in mean proportion of vaccinators who attended work during the lockdown compared with baseline was higher for female vaccinators (13.7%; 95% CI: 12.9–14.5) vs male vaccinators (6.3%; 95% CI: 6.0–6.6). According to the daily average, 6.8% (98/1437) of all centers were closed during the lockdown, whereas 31.6% (423/1339) of the open centers had no client flow.
Table 2.
Characteristics of children enrolled in ZM EIR during baseline period (September 23, 2019-March 22, 2020) and COVID-19 lockdown period (March 23-May 09, 2020) in Sindh, Pakistan.
| Baseline (n = 786,325) |
COVID-19 lockdown (n = 83,360) |
% Difference | 95% CI | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| a | b | c | d | d-b | ||||
| n | % | n | % | |||||
| Proportion of the target children enrolled (Children enrolled in ZM/Target of Surviving Infants) | 786,325/717,039 | 109.7 | 83,360/192,480 | 43.3* | ||||
| Female | 378,915 | 48.2 | 39,632 | 47.5 | −0.7 | −1.06 | −0.34 | 0.0001 |
| Place of birth† | ||||||||
| Home | 55,643 | 40.2 | 4608 | 34.5 | −5.7 | −6.04 | −5.36 | <0.0001 |
| Maternity Home | 8118 | 5.9 | 889 | 6.7 | 0.8 | 0.62 | 0.98 | <0.0001 |
| Hospital | 74,664 | 53.9 | 7865 | 58.9 | 5.0 | 4.64 | 5.35 | <0.0001 |
| Enrollment Area | ||||||||
| Rural | 341,353 | 43.4 | 35,251 | 42.3 | −1.1 | −1.45 | −0.75 | <0.0001 |
| Urban | 444,972 | 56.6 | 48,109 | 57.7 | 1.1 | 0.74 | 1.45 | <0.0001 |
| Enrollment Event | ||||||||
| Fixed Site | 505,830 | 64.3 | 73,470 | 88.1 | 23.8 | 23.5 | 24.0 | <0.0001 |
| Outreach | 280,495 | 35.7 | 9890 | 11.9 | –23.8 | −24.0 | –23.5 | <0.0001 |
| Mother’s Education (in years)† | ||||||||
| 0 | 64,764 | 46.8 | 5855 | 43.7 | −3.1 | −3.45 | −2.74 | <0.0001 |
| 1–8 | 63,805 | 46.1 | 6122 | 45.6 | −0.5 | −0.86 | −0.14 | 0.0059 |
| 9–10 | 5283 | 3.8 | 688 | 5.1 | 1.3 | 1.14 | 1.45 | <0.0001 |
| 11–12 | 2492 | 1.8 | 397 | 3.0 | 1.2 | 1.08 | 1.32 | <0.0001 |
| >12 | 1939 | 1.4 | 351 | 2.6 | 1.2 | 1.01 | 1.31 | <0.0001 |
| Proportion of Caregivers who provided cell phone numbers | 215,280 | 27.4 | 27,689 | 33.2 | 5.8 | 5.47 | 6.13 | <0.0001 |
| Enrollment Age (in months) | ||||||||
| 0–1 | 357,070 | 45.4 | 46,856 | 56.2 | 10.8 | 10.4 | 11.1 | <0.0001 |
| 2–3 | 192,711 | 24.5 | 18,219 | 21.9 | −2.6 | −2.90 | −2.30 | <0.0001 |
| 4–6 | 97,948 | 12.5 | 7592 | 9.1 | −3.4 | −3.61 | −3.19 | <0.0001 |
| 7–12 | 79,874 | 10.2 | 6027 | 7.2 | −3.0 | −3.19 | −2.81 | <0.0001 |
| 13–18 | 41,412 | 5.3 | 3372 | 4.1 | −1.2 | −1.34 | −1.06 | <0.0001 |
| 19–24 | 14,013 | 1.8 | 1020 | 1.2 | −0.6 | −0.68 | −0.52 | <0.0001 |
| above 24 | 3297 | 0.4 | 274 | 0.3 | −0.1 | −0.14 | −0.06 | <0.0001 |
| Mean | SD | Mean | SD | Mean Difference (c-a | ||||
| Age (in weeks) at Vaccination | ||||||||
| BCG/OPV-0 | 6.3 | 10.6 | 4.3 | 7.6 | -2.20 | −2.07 | −1.93 | <0.0001 |
| Penta-1/OPV-1/PCV-1 | 12.5 | 10.9 | 10.3 | 8.1 | -2.20 | −2.28 | −2.12 | <0.0001 |
| Penta-2/OPV-2/PCV-2 | 17.8 | 10.9 | 16.3 | 9.6 | -1.50 | −1.58 | −1.42 | <0.0001 |
| Penta-3/OPV-3/PCV-3 | 23.8 | 12.8 | 24.2 | 13.3 | 0.40 | 0.31 | 0.49 | <0.0001 |
| Measles-1 | 49.6 | 15.1 | 47.4 | 13.8 | -2.20 | −2.31 | −2.09 | <0.0001 |
| Measles-2 | 75.7 | 15.8 | 75.4 | 15.1 | -0.30 | −0.41 | −0.19 | <0.0001 |
Since EPI estimated enrollment target was 109.7% and erroneous, for statistical comparison, following two scenarios were analysed: a) Adjusted target of baseline (by 9.7%) to meet observed number of enrollments: Baseline 100% (786,325/786,325) vs. Lockdown 43.3% (83,360/192,480); difference 56.7%, p-value = 0.0000; 95% CI (-57.0—-56.4). b) Adjusting targets of both baseline and COVID-19 by 9.7%: Baseline 100% (786,325/786,325) vs. Lockdown 39.5% (83,360/211,150); difference 60.5%, p-value = 0.0000; 95% CI (-60.8—-60.2).
82.5% observations for place of birth and mother’s education are missing in the baseline period vs. 83.9% observations missing in COVID-19 lockdown period.
The lockdown affected routine immunization in rural areas more than in urban areas (Table 3 ). Slum UCs had a slightly larger decrease in immunization coverage than non-slum UCs (53.8% vs 51.3%). The decline in immunization visits was worst in SHRUCs (68.1%) followed by rural (54.9%) UCs and slums (53.8%), with one falling by 89.0% (Table S-2). Enrollments, as compared to follow-ups, were more adversely affected across the province, indicating vaccinations earlier in the EPI schedule were affected more than the later ones. Enrollments in SHRUCs had the worst decline (80.1%) overall.
Table 3.
Percentage decline in daily average immunization visits in ZM EIR during lockdown (March 23-May 09, 2020) compared to baseline (September 23, 2019-March 22, 2020) periods in Union Councils by enrollment Area in Sindh, Pakistan (n = 2,787,450).
| Baseline (n = 2,463,595) |
COVID-19 lockdown (n = 323,855) |
Percentage reduction |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Average Number of visits |
Average Number of visits |
||||||||
| n | n | n | n | n | n | % | % | % | |
| Urban | Rural | Total | Urban | Rural | Total | Urban | Rural | Total | |
| Enrollment | 2986 | 2291 | 5277 | 1203 | 881 | 2084 | −59.7 | −61.5 | −60.5 |
| Follow-up | 5662 | 5595 | 11,257 | 3337 | 2676 | 6012 | −41.1 | −52.2 | −46.6 |
| Total | 8,649 | 7886 | 16,534 | 4540 | 3557 | 8096 | −47.5 | −54.9 | −51.0 |
| Slum | Non-slum | Total | Slum | Non-slum | Total | Slum | Non-slum | Total | |
| Enrollment | 817 | 1064 | 1881 | 289 | 441 | 730 | −64.6 | −58.6 | −61.2 |
| Follow-up | 1655 | 2535 | 4190 | 852 | 1313 | 2166 | −48.5 | −48.2 | −48.3 |
| Total | 2472 | 3599 | 6071 | 1141 | 1754 | 2896 | −53.8 | −51.3 | −52.3 |
| SHRUC | Non-SHRUC | Total | SHRUC | Non-SHRUC | Total | SHRUC | Non-SHRUC | Total | |
| Enrollment | 157 | 5119 | 5277 | 31 | 2053 | 2084 | −80.1 | −59.9 | −60.5 |
| Follow-up | 248 | 11,010 | 11,258 | 98 | 5914 | 6012 | −60.5 | −46.3 | −46.6 |
| Total | 405 | 16,129 | 16,534 | 129 | 7967 | 8096 | −68.1 | −50.6 | −51.0 |
*n = 2,787,450 for Urban/Rural and SHRUCs/Non-SHRUCs; n = 1,020,390 for slums/non-slums.
*Slum analysis is limited to EPI identified slums in 7 districts of Hyderabad and Karachi.
We included 20,712 children with complete data for all variables in the regression analysis. Hospital births had a 1.09 times and maternal education 1.19 to 1.50 times (based on education level) higher probability of penta-3 completion during lockdown (Table 4 ). The probability of getting penta-3 immunization decreased by 6% for each previous vaccination received through outreach, and by 5% for each week’s delay in enrollment. The gender did not show any significant effect on the penta-3 immunization coverage.
Table 4.
Predictors of age-appropriate Penta-3 immunization completion in children due for immunization during COVID19 lockdown (March 23-May 09, 2020) in Sindh, Pakistan (n = 20,712).
| Unadjusted analysis |
Adjusted analysis |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | RR | p-value | 95% Confidence Interval | RR | p-value | 95% Confidence Interval | ||
| Sex | ||||||||
| Female | 0.99 | 0.807 | 0.95 | 1.04 | 0.99 | 0.472 | 0.95 | 1.03 |
| Place of Birth | ||||||||
| Hospital | 1.37 | 0.000 | 1.31 | 1.43 | 1.09 | 0.000 | 1.04 | 1.15 |
| Maternity Home | 1.17 | 0.001 | 1.06 | 1.28 | 1.06 | 0.222 | 0.97 | 1.17 |
| Enrollment Area | ||||||||
| Urban | 1.35 | 0.000 | 1.30 | 1.41 | 1.03 | 0.254 | 0.98 | 1.08 |
| Enrollment Age Weeks | 0.89 | 0.000 | 0.88 | 0.90 | 0.95 | 0.000 | 0.92 | 0.97 |
| Mother’s Education (in years) | ||||||||
| 1–5 | 1.31 | 0.000 | 1.25 | 1.37 | 1.19 | 0.000 | 1.13 | 1.25 |
| 6–10 | 1.81 | 0.000 | 1.67 | 1.97 | 1.38 | 0.000 | 1.27 | 1.50 |
| 11–12 | 2.14 | 0.000 | 1.95 | 2.35 | 1.50 | 0.000 | 1.35 | 1.65 |
| >12 | 2.14 | 0.000 | 1.92 | 2.37 | 1.38 | 0.000 | 1.23 | 1.55 |
| Penta-2 vaccination at Outreach | 0.67 | 0.000 | 0.64 | 0.70 | 0.94 | 0.091 | 0.87 | 1.01 |
| Outreach vaccination history | 0.86 | 0.000 | 0.84 | 0.87 | 0.94 | 0.000 | 0.91 | 0.97 |
| Age at Penta-2 vaccination (in weeks) | 0.81 | 0.000 | 0.79 | 0.82 | 0.81 | 0.000 | 0.79 | 0.83 |
| Age at BCG vaccination (in weeks) | 0.86 | 0.000 | 0.85 | 0.88 | 1.05 | 0.000 | 1.02 | 1.08 |
| Provision of Phone Number | 1.43 | 0.000 | 1.24 | 1.64 | – | – | – | – |
*Provision of phone number was excluded in stepwise multivariable model selection.
4. Discussion
This study provides a comprehensive and evidence-based analysis of the impact of COVID-19 restrictions on immunization coverage in a large population. The overall immunization visits in Sindh province have declined by 51.0% during the COVID-19 lockdown compared to the preceding six months. On average, over 8438 children per day are missing out on life-saving immunizations in Sindh, leaving them susceptible to measles, polio and other VPDs. This decrease in coverage can partly be explained by a reduction in provision of immunization services (supply) and a diminishing demand for the services by caregivers.
On the supply side, the provision of services was affected by a strict restriction on the movement of vaccinators to do outreach [38], resulting in a 79.3% decrease in the vaccinations administered through outreach compared to the baseline. With 2 out of 5 children (39.6%) being immunized through outreach services in Sindh, these children are the least likely to attend immunization clinics [28]. Immunization services were also impacted due to health workers’ concerns about the possibility of infection through engaging with clients in the absence of clear guidelines and protective equipment [39]. Personal protective equipment (PPE) such as masks, eye-shields, or hand sanitizers was not available for workers in the early weeks of COVID-19 lockdown. Without a viable and bilateral channel of communication between vaccinators and health authorities, it becomes challenging for health workers to communicate their concerns and needs, and for health authorities to disseminate new guidelines and protocols to all vaccinators that could potentially alleviate the supply side challenges. Considering that vaccinators have to quickly adapt to new ways of working with PPE, and ensure social distancing, a rapid channel of communication with EPI is needed to enable them to adopt these new measures. There is a need for user-centric and innovative technologies such as virtual engagement and learning platforms to disseminate training materials and videos to vaccinators, and provide on-demand access to essential information related to standard operating procedures in the COVID-19 context. Such platforms can also serve as a channel for peer-to-peer messaging and communication with EPI.
There were also concerns around vaccine stock-outs because of disruptions in global manufacturing and supply chains, border closures, and restrictions on local mobility [40], [41]. While some parts of the country faced a stock-out of penta vaccine (and an imminent shortage of measles [42], [43]), our findings show Sindh province was not affected, and all the antigens were administered during the study period (as shown in Table 1). With fewer children coming to health facilities, we expected a sharper decrease in BCG and measles, the vaccines with larger multi-dose vials, with the assumption that health workers may refrain from opening them when only a few children are referred for vaccination. However, our findings did not show such decline, and on the contrary, we see a higher level of enrollment and follow-ups on Mondays, the day of the week that BCG and measles vaccination is most commonly provided in low-volume facilities (data not shown). Based on national immunization coverage estimates, the coverage of Measles vaccine is relatively low as compared to the earlier vaccines in schedule [5]. Although a lower number of caregivers show up for the measles vaccine, they generally have higher education and awareness compared to those who drop out. [44]. We therefore postulate that exogenous shocks like COVID-19 had a lesser impact on measles vaccination rates, as caregivers with higher education and awareness are less likely to be dissuaded from vaccinations due to COVID-19.
On the demand side, there are several factors contributing to the observed decrease in the recorded immunizations. Parental reluctance to get children vaccinated out of the fear of exposing their children to infection during a vaccination session is one of the key challenges that is observed in Pakistan and many other countries [45]. The myths and misinformation regarding vaccinations and rumors around COVID-19 are compounding the existing problem of vaccine hesitancy [46]. Moreover, factors including restriction on movement enforced by the authorities [30] and unavailability of public transportation [47] or an increase in commuting costs could have also played a considerable role in the drop in coverage. This would disproportionately impact the caregivers with the lowest income, widening the equity gap in immunization coverage. Provision of commuting cash subsidies to the parents of children in the lowest socio-economic groups and utilizing digitally enabled ride-sharing and transportation services are among the innovative solutions that can be implemented through EIRs.
Consistent with many other studies, our findings show that the demand for immunizations is higher among parents with higher education and awareness, and this has not changed during the lockdown period [48], [49], [50]. Adding geo-spatial location of delivery of services, the findings suggest that the most vulnerable children are those from poor socio-economic backgrounds, living in slums and SHRUCs. These children have shown to have a higher likelihood of missing vaccines and not finishing their full course of immunization [51]. EIRs can boost demand through leveraging innovative and creative interventions such as two-way Short Messaging Service (SMS) communication and online chatbots [52] to nudge parents and help re-establish community trust by dispelling misconceptions. These channels of communication are also important for conveying caregivers apparently trivial yet crucial information on the importance of completing their child's immunization schedule amidst COVID-19, informing the caregivers regarding the operationalization of fixed sites with adequate availability of PPE, as well as encouraging caregivers to visit a particular EPI facility to redistribute and better manage client load in the facilities. Alternate methods of immunization delivery, such as mobile immunization vans which provide vaccination services in hard-to-reach areas that often remain untapped by the routine outreach sessions, can be used instead of fixed immunization sites in places where services have stopped, in particular in slums and SHRUCs where an accumulation of missed children is observed in this study.
Our study shows a delay in the vaccination of children because of the lockdown. Previous studies have shown, without accounting for herd protection, that delays in vaccination can cause up to 6% more deaths from vaccine-preventable diseases such as Pneumonia in Pakistan [53]. We note that the value of vaccines and essential immunization in preventing deaths and children’s suffering largely override the risks of COVID-19 infection. Additionally, a recent modeling analysis from Africa has shown that for each excess COVID-19 death attributable to acquiring infection through an immunization clinic, over 84 (95% UI: 14–267) deaths can be prevented through sustained immunization [54]. Considering the low measles immunization coverage rates and circulation of poliovirus in Pakistan, the country may stand to the upper limits of the benefit ratio. The number of additional children missing their essential immunization is a major risk for bringing herd immunity below the threshold and presents a significant risk of outbreaks of measles, diphtheria, and polio in the province. This has been observed in countries where measles vaccination rates were already high [55]. For Pakistan and Sindh in particular, the threat of such an outbreak is considerably higher given that the target population for EPI in Sindh is an under-estimate and does not include thousands of children who remain unaccounted for and unvaccinated [56]. This became evident through the use of EIR in the province; enrollments in ZM EIR prior to lockdown were on average 9% above the target. ZM EIR was not rolled-out across one entire district till June 2020 and many private sector facilities do not account for zero-dose children or those who are marginalized and undocumented with no access to health services. With this pool of unvaccinated children existing in the province, there is a real possibility of heading towards a measles outbreak with over 5000 suspected cases reported in the first quarter of 2020 alone, compared to 9000 cases reported for the entire last year (2019) [57]. While there are assertions that the social distancing measures may lead to a temporary drop in transmissions of infectious diseases [58], including measles, there is a viable threat of a rapid resurgence of diseases once the restrictions are gradually relaxed. Such contentions do not hold for poliovirus that can be transmitted through the fecal-oral route.
While countries are repeatedly being asked to tailor immunization strategies to best suit their situation [15], there is little to no evidence on which intervention will work under these unprecedented circumstances. This problem is compounded more so in LMICs as, unfortunately, most countries cannot assess the impact of the interventions on RI, given that many of these countries still use a paper-based reporting that has its limitations. We see a real potential for LMICs such as Pakistan, Tanzania, Zambia to leverage EIRs and study the impact of new interventions on RI to ascertain what works. We have shown how the ZM EIR enables tracking every child who missed one or more essential immunization doses to ensure that the health system can reach and immunize every child. Furthermore, many of the interventions we have proposed for the demand-side (cash subsidies, SMS reminders, chatbots) and supply-side side (monitoring stock-outs, defaulter list generation, conducting outreach sessions through mobile vans, performance management of vaccinators) can all be linked to a centralized EIR.
Real-time data from EIRs can also facilitate governments in giving timely responses to changing trends through policy and guidelines. For instance, our results show that immunizations are declining more in rural than in urban areas. Health crisis could have prompted people from rural and peri-urban areas to undertake strict measures of physical distancing knowing that they have a less robust healthcare infrastructure than their urban counterparts [59]. Observations during the lockdown indicate that rural communities in Sindh Province were more receptive to social distancing [60]. However, it is crucial to monitor any variation in trend over time as urban health facilities become increasingly strained because of the influx of COVID-19 patients.
The first detailed guidelines for maintaining RI services in Sindh were issued by the EPI office after three weeks into the lockdown. Looking beyond immediate interventions, as the focus gradually shifts from containing the COVID-19 outbreak to normalizing existing health services, EPI and partners should be proactive in preparing a long term strategy to mitigate the losses in immunization coverage. The current time should be utilized to calibrate the correct policy response for the post-lockdown period for immediate implementation as soon as restrictions are lifted. The above recommended tools can help the EPI Department navigate some of the post-lockdown strategies for resuming immunization activities. Some of the strategies put into action by EPI include the following; immediate resumption of vaccination services both at fixed and outreach sites with clear standard operating procedures (SOPs) including social distancing, use of PPE and necessary hygiene measures. Additionally, defaulter lists are being generated through the EIR for catch-up of children who have missed vaccinations during the lockdown. EPI is also actively engaged in implementing enhanced outreach activities and mop-up activities that are targeted in hotspots with the highest incidence of missed children. The enhanced outreach activities are closely being monitored through the real-time EIR data which is also being leveraged to monitor vaccinator attendance and conduct evidence-based performance management. In addition to vaccinator’s performance management, there is an increased focus on reorienting and updating communication skills of vaccinators to help teach them Infection Prevention Control (IPC) skills and enable them to counsel caregivers for safe immunizations for their children during the pandemic. As EPI remains focused on sustaining immunization services through the above mentioned strategies, the coming months will reveal the effectiveness of these interventions in bridging the gap in immunization coverage brought about by the pandemic.
One of the limitations of the analysis is using the 6-month period preceding the lockdown as the baseline period rather than the same calendar dates (March 23–May 9) from 2019. The latter did not provide an appropriate baseline period as the compliance of the use of EIR by government vaccinators was lower during March-May 2019, compared to the same time in the current year (March-May 2020). Therefore, using the three-month period from 2019 as a baseline would have underestimated the impact of COVID-19. Both the attendance and performance of vaccinators started improving from May 2019 given the increased sense of accountability after the Health Minister started reviewing the EIR data during regular vaccinator performance reviews. An additional limitation of the analysis is that ZM EIR included enrollment of only 83% of the estimated annual birth cohort as per EPI Sindh targets, from 27 districts of Sindh Province in 2019. The EIR was rolled-out in the remaining 2 districts on March 01, 2020, and July 03, 2020, therefore their targets have not been taken into account. Under-registration in EIRs has been identified as a significant challenge for data utilization [61]. Another limitation is the lack of exact slum area mapping. The UC level slum analyses relied upon EPI estimated population living in slums. Therefore, the actual immunization decline in slum areas may be higher than reported. Additionally, despite ZM EIR currently functioning across the province, children vaccinated through private immunization schemes and some private/public EPI collaborations are not registered in the EIR and not included in our evaluation. Nevertheless, the large, diverse, and accurate individual-level immunization data available in the ZM EIR allows us to provide key insights that are relevant for other demographically similar LMICs as they navigate through their respective COVID-19 lockdowns.
Sustained immunizations during COVID-19 are essential to prevent secondary outbreaks of VPDs. There is a need to ensure both service availability and demand, during and immediately after lockdowns, for parents to bring their children to EPI centers. To prepare for the post-lockdown efforts, immunization programs should leverage data for better allocation of scarce resources, and use tailored approaches targeted at known high-risk areas and geographies with the highest numbers of missed children.
Author contributions
SC designed the study. SC, DAS, MM, AM, VKD, MTS, SA, MAA have contributed to the implementation of the project. MM and AM extracted the data. SC and MM did all statistical analyses and interpreted the data. HS and AJK advised on the data analysis. MS supported spatial analyses. SC and DAS wrote the paper while HS contributed to the discussion. AJK, HS, RS, and AK reviewed drafts and provided input. All authors approved the final version of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank frontline health workers who vaccinate children and maintain ZM EIR, and their supervisors and support staff. We also thank the donors and partners of ZM EIR, including EPI-Pakistan, EPI-Sindh, UN Foundation, WHO, Gavi, the Vaccine Alliance, Interactive Health Solutions, Acasus, and many others. Finally, we would like to thank Dr. Muhammad Akram Sultan, Project Director, EPI-Sindh, and Dr. Mohammed Osama Mere, EPI Team Lead, WHO-Pakistan, for their valuable support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2020.08.019.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Locke PRT. PM: COVID-19 'Worst Public Health Crisis in a Generation. In Medscape News UK. UK; 2020.
- 2.WHO. Coronavirus disease (COVID-19) Pandemic; 2019 [cited 2020 Jul 15]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 3.WHO. COVID-19 significantly impacts health services for noncommunicable diseases; 2020 [cited 2020 Jul 15]. Available from: https://www.who.int/news-room/detail/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases.
- 4.GAVI, COVID-19 Situation Report #8. May 5; 2020.
- 5.Pakistan Demographic and Health Survey 2017-18. NIPS and ICF; Islamabad, Pakistan, and Rockville, Maryland, USA: 2019. National Institute of Population Studies (NIPS) [Pakistan] and ICF. [Google Scholar]
- 6.WHO. Emergencies preparedness, response. Measles – Global situation; 2019 [cited 2020 Jul 15]. Available from: https://www.who.int/csr/don/26-november-2019-measles-global_situation/en/.
- 7.GPEI. Pakistan: affected by wild poliovirus type 1 and circulating vaccine-derived poliovirus type 2; 2020 [cited 2020 Jul 15]. Available from: http://polioeradication.org/where-we-work/pakistan/.
- 8.National Information Technology Board, Government of Pakistan. COVID-19 Dashboard; 2020. Available from: http://covid.gov.pk/stats/pakistan.
- 9.WHO. Protecting lifesaving immunization services during COVID-19: New guidance from WHO; 2020. Available from: https://www.who.int/immunization/news_guidance_immunization_services_during_COVID-19/en/.
- 10.Hirabayashi DK. Unicef; 2020. The impact of COVID-19 on routine vaccinations. [Google Scholar]
- 11.Life-saving vaccinations must not ‘fall victim’ to COVID-19 pandemic – UNICEF chief. In UN News; 2020.
- 12.GPEI. “The first call“: Polio eradication staff support COVID-19 response; 2020. Available from: https://reliefweb.int/report/pakistan/first-call-polio-eradication-staff-support-covid-19-response.
- 13.EOC Sindh. Postponement of fIPV Campaign, Karachi, March 2020; March 17, 2020.
- 14.GPEI, Polio Eradication Programme Continuity Planning measures to ensure continuity of operations in the context of the COVID-19 pandemic; 2020.
- 15.WHO, Guiding principles for immunization activities during the COVID-19 pandemic: interim guidance, 26 March 2020. Geneva: World Health Organization; 2020.
- 16.Colavita F., Biava M., Castilletti C., et al. Measles Cases during Ebola Outbreak, West Africa, 2013–2106. Emerg Infect Dis. 2017;23(6):1035–1037. doi: 10.3201/eid2306.161682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolkan H., Bash-Taqi D.A., Samai M., et al. Ebola and Indirect Effects on Health Service Function in Sierra Leone. PLoS Curr. 2014;6 doi: 10.1371/currents.outbreaks.0307d588df619f9c9447f8ead5b72b2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parpia A., Ndeffo-Mbah M.L., Wenzel N.S., et al. Effects of Response to 2014–2015 Ebola Outbreak on Deaths from Malaria, HIV/AIDS, and Tuberculosis, West Africa. Emerg Infect Dis. 2016;22(3):433–441. doi: 10.3201/eid2203.150977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau J.T., Yang X., Pang E., Tsui H.Y., Wong E., Wing Y.K. SARS-related perceptions in Hong Kong. Emerg Infect Dis. 2005;11(3):417–424. doi: 10.3201/eid1103.040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts L.D. Infectious Diseases. As Ebola fades, a new threat. Science. 2015;347(6227):1189. doi: 10.1126/science.347.6227.1189. [DOI] [PubMed] [Google Scholar]
- 21.Truelove S.A., Moss W.J., Lessler J. Mitigating measles outbreaks in West Africa post-Ebola. Exp Rev Anti-infective Therapy. 2015;13(11):1299–1301. doi: 10.1586/14787210.2015.1085305. [DOI] [PubMed] [Google Scholar]
- 22.WHO. Guidance on routine immunization services during COVID-19 pandemic in the WHO European Region; 2020. Available from: http://www.euro.who.int/en/health-topics/communicable-diseases/hepatitis/publications/2020/guidance-on-routine-immunization-services-during-covid-19-pandemic-in-the-who-european-region-2020.
- 23.WHO. Analysis and Use of Health Facility Data. Guidance for immunization program managers; 2018. Available from: https://www.who.int/healthinfo/FacilityAnalysisGuide_Immunization.pdf?ua=1.
- 24.Bureau of Statistics, Government of Sindh. Sindh At Glance; 2020 [cited 2020 Jul 15]. Available from: http://sindhbos.gov.pk/sindh-at-glance/.
- 25.EPI Sindh. Mid Term Review for National Immunization Support Project (NISP). Technical Workshop. February 3-5, 2020; Pakistan. Presentation slides [cited 2020 April 22].
- 26.Mangrio N.K., Alam M.M., Shaikh B.T. Is Expanded Programme on Immunization doing enough? Viewpoint of health workers and managers in Sindh, Pakistan. J Pak Med Assoc. 2008;58(2):64–67. [PubMed] [Google Scholar]
- 27.WHO. Immunization in Practice - Modules 1-11. 2001. WHO/EPI/TRAM/98.01-11 REV.1. Available from: http://helid.digicollection.org/en/d/Js2979e/.
- 28.IRD/EPI-Sindh. Zindagi Mehfooz Electronic Immunization Registry Analysis. Unpublished 2020.
- 29.Chandir S, Siddiqi DA, Dharma VK, et al. Zindagi Mehfooz (Safe Life) Digital Immunization Registry: Leveraging Low-Cost Technology to Improve Immunization Coverage and Timeliness in Pakistan iproc. 2018;4(2) doi: 10.2196/11770. [DOI] [Google Scholar]
- 30.Lockdown imposed in Sindh for next 15 days; movement restricted to need-only basis. Dawn News; 2020 [cited 2020 May 1]. Available from: https://www.dawn.com/news/1542901.
- 31.WHO. The Global Vaccines Action Plan 2011–2020. Review and Lessons Learnt. WHO; 2019. Available from: https://www.who.int/immunization/global_vaccine_action_plan/en/.
- 32.Profiling of urban/peri-urban slums of Karachi and Hyderabad. Unicef; Pakistan: 2017. [Google Scholar]
- 33.Schoeps A., Ouédraogo N., Kagoné M., et al. Socio-demographic determinants of timely adherence to BCG, Penta3, measles, and complete vaccination schedule in Burkina Faso. Vaccine. 2013;32(1):96–102. doi: 10.1016/j.vaccine.2013.10.063. [DOI] [PubMed] [Google Scholar]
- 34.Acharya P., Kismul H., Mapatano M.A., et al. Individual- and community-level determinants of child immunization in the Democratic Republic of Congo: A multilevel analysis. PLoS ONE. 2018;13(8) doi: 10.1371/journal.pone.0202742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mbengue M.A.S., Mboup A., Ly I.D., et al. Vaccination coverage and immunization timeliness among children aged 12–23 months in Senegal: a Kaplan-Meier and Cox regression analysis approach. Pan Afr Med J. 2017;27(Suppl 3):8. doi: 10.11604/pamj.supp.2017.27.3.11534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gibson D., Ochieng B., Kagucia E.W., et al. Individual level determinants for not receiving immunization, receiving immunization with delay, and being severely underimmunized among rural western Kenyan children. Vaccine. 2015;33(48):6778–6785. doi: 10.1016/j.vaccine.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 37.Haque S.M., Bari W. Positive Role of Maternal Education on Measles Vaccination Coverage in Bangladesh. Int J Psychol Behav Sci. 2013;3:11–17. [Google Scholar]
- 38.Government of Sindh, Office of the District Health Officer. District Kamber Shahdad Kot. Office Order. No. DHO/KSK 3591/95; March 23, 2020.
- 39.CDC, Operational Considerations for Immunization Services during COVID-19 in Non-US Settings Focusing on Low-Middle Income Countries; 2020.
- 40.Unicef. Impact of COVID-19 on vaccine supplies. Unicef; 2020. Available from: https://www.unicef.org/supply/stories/impact-covid-19-vaccine-supplies
- 41.WHO and Unicef. (2020). Immunization in the context of COVID-19 pandemic: frequently asked questions (FAQ), 16 April 2020. WHO. Available from: https://apps.who.int/iris/handle/10665/331818.
- 42.Directorate General Health Services Sindh, H., Directorate General Health Services Sindh, Hyderabad. Impact of COVID-19 on EPI Vaccine Supplies. DGHSS (Gen Br: COVID-19 Vaccine-17770/802). March 26, 2020, in DGHSS (Gen Br: COVID-19 Vaccine-17770/802, H. Directorate General Health Services Sindh, Editor.
- 43.Office of the Project Director. EPI Sindh. Guidelines for the Immunization services in the COVID-19. No. PDEPISK (2666/2737); April 14, 2020.
- 44.Noh J.W., Kim Y.M., Akram N., et al. Factors affecting complete and timely childhood immunization coverage in Sindh, Pakistan; A secondary analysis of cross-sectional survey data. PLoS ONE. 2018;13(10) doi: 10.1371/journal.pone.0206766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hoffman J. Vaccine Rates Drop Dangerously as Parents Avoid Doctor’s Visits. In Newyork Times; 2020.
- 46.COVID-19 putting routine childhood immunization in danger: UN health agency. In UN News; 2020.
- 47.Sindh govt refuses to lift ban on public transport, ride-hailing services. Dawn News; 2020 [cited 2020 Jul 15]. Available from: https://www.dawn.com/news/1557383.
- 48.Maina L., Karanja S., Kombich J. Immunization coverage and its determinants among children aged 12–23 months in a peri-urban area of Kenya. Pan African Med J. 2013;14:3. doi: 10.11604/pamj.2013.14.3.2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Subhani S, Yaseen R, Khan M, et al. Impact of Mother’s Education on Child Immunization: A Comparative Study of India and Pakistan. Journal of Finance and Economics. 2015;3:51–54. doi: 10.12691/JFE-3-3-1. [DOI] [Google Scholar]
- 50.Parashar S. Moving beyond the mother-child dyad: Women's education, child immunization, and the importance of context in rural India. Soc Sci Med. 1982;2005(61):989–1000. doi: 10.1016/j.socscimed.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 51.Crocker-Buque T., Mindra G., Duncan R., et al. Immunization, urbanization and slums - A systematic review of factors and interventions. BMC Public Health. 2017;17(1):556. doi: 10.1186/s12889-017-4473-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Buechner MM. UNICEF’s U-Report Playing Key Role In Global COVID-19 Response. In Forbes 2020.
- 53.Carter E.D., Tam Y., Walker N. Impact of vaccination delay on deaths averted by pneumococcal conjugate vaccine: Modeled effects in 8 country scenarios. Vaccine. 2019;37(36):5242–5249. doi: 10.1016/j.vaccine.2019.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abbas K., Procter S.R., van Zandvoort K., et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit-risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. 2020 doi: 10.1016/S2214-109X(20)30308-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Santoli JM, LM, DeSilva MB, et al, Effects of the COVID-19 Pandemic on Routine Pediatric Vaccine Ordering and Administration — United States; 2020. [DOI] [PubMed]
- 56.Inequities and trends in birth registration. Unicef; New York: 2013. Every Child’s Birth Right. [Google Scholar]
- 57.Khawar H. Children at risk of missing out on essential routine immunisation amid Covid-19. Dawn News; 2020. Available from: https://www.dawn.com/news/1546379/children-at-risk-of-missing-out-on-essential-routine-immunisation-amid-covid-19.
- 58.Hungerford D., Cunliffe N. Coronavirus disease (COVID-19) – impact on vaccine preventable diseases. Eurosurveillance: European communicable disease bulletin. 2020;25:2000756. doi: 10.2807/1560-7917.ES.2020.25.18.2000756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ranscombe P. Rural areas at risk during COVID-19 pandemic. Lancet Infect Dis. 2020;20(5):545. doi: 10.1016/S1473-3099(20)30301-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Qureshi Z. COVID-19: Rural Sindh more receptive to social distancing than urban areas, in Gulf News 2020: Pakistan.
- 61.Dolan S.B., Carnahan E., Shearer J.C., et al. Redefining vaccination coverage and timeliness measures using electronic immunization registry data in low- and middle-income countries. Vaccine. 2019;37(13):1859–1867. doi: 10.1016/j.vaccine.2019.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.