Abstract
Background
Among US Hispanics/Latinos, the largest ethnic minority population in the United States, hypertension incidence has not been thoroughly reported. The goal of this study was to describe the incidence of hypertension among US Hispanic/Latino men and women of diverse Hispanic/Latino background.
Methods and Results
We studied 6171 participants of the Hispanic Community Health Study/Study of Latinos, a diverse group of self‐identified Hispanics/Latinos from 4 US urban communities, aged 18 to 74 years, and free from hypertension in 2008 to 2011 and re‐examined in 2014 to 2017. Hypertension was defined as self‐reported use of anti‐hypertension medication, or measured systolic blood pressure ≥130 mm Hg, or diastolic blood pressure ≥80 mm Hg. Results were weighted given the complex survey design to reflect the target population. Among men, the 6‐year age‐adjusted probability of developing hypertension was 21.7% (95% CI, 19.5–24.1) and differed by Hispanic/Latino background. Specifically, the probability was significantly higher among men of Cuban (27.1%; 95% CI, 20.2–35.2) and Dominican (28.1%; 95% CI, 19.5–38.8) backgrounds compared with Mexican Americans (17.6%; 95% CI: 14.5–21.2). Among women, the 6‐year age‐adjusted probability of developing hypertension was 19.7% (95% CI, 18.1–21.5) and also differed by Hispanic/Latino background. Specifically, the probability was significantly higher among women of Cuban (22.6%; 95% CI, 18.3–27.5), Dominican (23.3%; 95% CI, 18.0–29.5), and Puerto Rican (28.2%; 95% CI, 22.7–34.4) backgrounds compared with Mexican Americans (16.0%; 95% CI, 13.9–18.4).
Conclusions
Hypertension incidence varies by Hispanic/Latino background, with highest incidence among those of Caribbean background.
Keywords: blood pressure, Hispanics/Latinos, hypertension
Subject Categories: Hypertension, High Blood Pressure, Epidemiology, Race and Ethnicity
Nonstandard Abbreviations and Acronyms
- ACC/AHA
American College of Cardiology/American Heart Association
- AHEI
alternative healthy eating index
- BMI
body mass index
- BP
blood pressure
- CVD
cardiovascular disease
- DBP
diastolic blood pressure
- HCHS/SOL
Hispanic Community Health Survey/Study of Latinos
- IR
incidence rate
- IRR
incidence rate ratio
- JNC7
Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure
- SBP
systolic blood pressure
Clinical Perspective
What Is New?
Over 6 years, roughly 1 in 5 US Hispanics/Latinos of the Hispanic Community Health Study/Study of Latinos developed hypertension according to the American College of Cardiology/American Heart Association guidelines, with rates of incident hypertension substantially higher among Hispanics/Latinos of Caribbean background.
Rates of hypertension treatment and control were low across all US Hispanic/Latino background groups.
What Are the Clinical Implications?
Efforts to prevent the development of hypertension and improve rates of hypertension treatment and control among US Hispanics/Latinos require broad‐based public health strategies.
Hypertension is a major contributor to cardiovascular disease (CVD),1 the leading cause of death in the United States. It is associated with shorter overall life expectancy and a shorter duration of living free from CVD.2 In 2017, lower blood pressure (BP) thresholds were introduced to define hypertension.3 In accordance with these guidelines, it is estimated that 46% of US adults now have hypertension, with 36% indicated for hypertension treatment.4
However, among US Hispanics/Latinos, the largest ethnic minority population and also the third‐fastest growing segment of the US population,5 the epidemiology of hypertension has not been adequately described.6 Instead findings have focused on Mexican Americans. For example, the National Health and Nutrition Examination Survey4 and the San Antonio Heart Study7, 8 both show that prevalence or incidence of hypertension among Mexican Americans is comparable or lower than that of non‐Hispanic/Latino whites. However, the broader US Hispanic/Latino population is heterogeneous with respect to background, genetic makeup,9, 10 social composition,11 as well as health‐related behaviors.12, 13 In fact, there is increasing evidence of health differences by Hispanic/Latino background group with a higher prevalence of CVD risk factors, including hypertension, among US Hispanics/Latinos of non‐Mexican versus Mexican background. For instance, cross‐sectional results from the HCHS/SOL (Hispanic Community Health Study/Study of Latinos); showed that the prevalence of hypertension varies considerably across Hispanic/Latino backgrounds with higher prevalence rates among US Hispanics/Latinos from Puerto Rican, Dominican, and Cuban backgrounds and lower rates among US Hispanics/Latinos from Mexican, Central American, and South American backgrounds.14 Yet to date, rates of incident hypertension among diverse US Hispanics/Latinos have not been thoroughly described.
The goals of this study are 2‐fold. First, we aim to estimate incidence rates of hypertension across diverse Hispanic/Latino backgrounds. Second, we aim to estimate the proportion of the HCHS/SOL cohort recommended for hypertension treatment, and who are treated and controlled, according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline for the prevention, detection, evaluation, and management of high BP in adults.3 To do so, we will leverage longitudinal data from the HCHS/SOL study.
Methods
The data, analytic methods, and study materials can be been made available to other researchers who apply to the HCHS/SOL Publications Committee for purposes of reproducing the results or replicating the procedure.
Study Population
The HCHS/SOL is an ongoing prospective population based cohort study of 16 415 community dwelling, self‐identified Hispanics/Latinos.15, 16 Participants aged 18 to 74 years were recruited in areas surrounding 4 field sites selected because of high populations of Hispanic backgrounds: Bronx, NY; Chicago, IL; Miami‐Dade, FL; and San Diego, CA. A 2‐stage area probability sample of households was selected; stratification and over‐sampling at each stage were used to obtain a diverse and representative sample.15 The baseline visit occurred between 2008 and 2011 and consisted of a standardized examination. A second standardized examination occurred roughly 6 years later between 2014 and 2017. In brief, during the visits, participants underwent laboratory tests and procedures and answered a series of surveys pertaining to their medical history and health behaviors. Informed consent and IRB approval were obtained.
Measurement of Medication and Blood Pressure
During both examinations, participants were asked to self‐report all current medications, including medications for BP, which were recorded by study staff. Following a 5‐minute rest period, BP was measured on the right arm using a cuff which was sized to the upper right arm circumference. Using an OMRON HEM‐907 XL (Omron Healthcare, Inc., Lake Forest, IL)17 automated sphygmomanometer, a trained technician took 3 BP measurements spaced 1 minute apart from seated participants. These 3 measurements were then averaged.
Definition of Hypertension
We considered 2 definitions of hypertension: hypertension according to the updated ACC/AHA guidelines (our primary definition) and for a supplementary analysis (described below), hypertension as defined by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7),18 which was contemporaneous with the first HCHS/SOL examination (2008–2011) and for most of the second HCHS/SOL examination (2014–2017). Hypertension as per the ACC/AHA guidelines (our primary measure) was defined by meeting any of the following conditions: self‐reported use of hypertension medication, average measured systolic BP (SBP) ≥130 mm Hg, or average diastolic BP (DBP) ≥80 mm Hg.3 Hypertension as per the JNC7 guideline (used in supplementary analysis) was defined by meeting any of the following conditions: self‐reported use of hypertension medication, average measured SBP ≥140 mm Hg, or average DBP ≥90 mm Hg.18 Going forward, all analyses refer to our primary measure (ACC/AHA defined hypertension), unless otherwise stated.
Recommendation for Hypertension Treatment, Hypertension Treatment, and Control
Recommendation for Hypertension Treatment
As per the 2017 ACC/AHA hypertension guideline,3 age, presence of diabetes mellitus, chronic kidney disease (CKD), prior CVD, or ≥10% 10‐year risk of a first hard CVD event (all defined in the covariates section below) were used to define recommendation for hypertension treatment. Recommendation for hypertension treatment was defined as: SBP ≥130 mm Hg for individuals aged ≥65 years, with diabetes mellitus, CKD, a history of CVD, a ≥10% 10‐year risk of a first hard CVD event, or as a DBP ≥80 mm Hg for individuals with diabetes mellitus, CKD, a history of CVD, or a ≥10% 10‐year risk of a first hard CVD event.3 For the general population, recommendation for hypertension treatment was defined by SBP ≥140 mm Hg or DBP ≥90 mm Hg.3 Hypertension treatment was defined as being treated for hypertension (based on self‐reported medication use), among individuals recommended for treatment of hypertension.3 Hypertension control was defined as SBP <130 mm Hg and DBP <80 mm Hg, among individuals recommended for treatment of hypertension.3
Measurement of Other Variables
Variables Measured at the First Examination
Participants were asked to state their country of birth and select a category that best described their Hispanic/Latino background, based on the following response options: Central American, Cuban, Dominican, Mexican, Puerto‐Rican, South American, >1 group, or other. All study participants also reported their age, sex, educational attainment (<high school, high school degree or more), annual household income from all sources (grouped as <$30 000 or ≥$30 000), and health insurance status. Additionally, participants reported their nativity and were classified as US born (excluding the island of Puerto Rico) or non‐US born (including the island of Puerto Rico). Participants who were identified as non‐US born further reported the duration that they had lived in the United States. Nativity/years in the United States was classified as: non‐US born with <10 years in the United States, non‐US born with ≥10 years in the United States, or US born.19 Body mass index (BMI) in kg/m2 was derived from measured weight and height wearing light clothing.16 Elevated SBP (at baseline) was defined as having an average SBP between 120 and 129 mm Hg without meeting the definition for hypertension (defined above). Participants were also queried about their smoking status (never, current, or former smokers) and physical activity was self‐reported using the modified version of the World Health Organization Global Physical Activity Questionnaire and grouped into meeting or not meeting 2008 recommendations.20 Described elsewhere,21 the Alternative Healthy Eating Index‐2010 (AHEI‐2010, range from 0 to 110) was used to assess overall diet.
Variables Measured at the Second Examination
To identify individuals recommended for treatment of hypertension (described above), the following variables were measured at the second examination: age, diabetes mellitus, CKD, prior CVD, and 10‐year risk of first CVD event. Diabetes mellitus/impaired glucose classification was measured from self‐reported medication use, an oral glucose tolerance test, or fasting blood samples and defined as: fasting plasma glucose ≥126 mg/dL, an oral glucose tolerance test 2‐hour post‐load glucose level ≥200 mg/dL, glycated hemoglobin ≥6.5%, or self‐reported use of hypoglycemic agents.22 CKD was defined as having an estimated glomerular filtration rate <60 mL/min per 1.73 m2.23 Age at examination 2 was self‐reported along with history of CVD (defined as prior heart attack, stroke, or heart procedure such as: angioplasty, stent, or bypass). Among individuals without a history of CVD, 10‐year predicted risk of CVD was calculated using the pooled cohort risk equations.24
Analytical Sample
For our primary analyses, of the 16 415 HCHS/SOL participants recruited from 2008 to 2011, we excluded individuals: with hypertension (n=5300) or missing hypertension information (n=66) at examination 1, and those who did not show up (n=4792) or were missing hypertension information (n=86) at examination 2. Our final analytic sample included 6171 participants. For our supplementary analysis using JNC7 to define hypertension our analytic sample size was larger and included n=7730 participants free from JNC7 defined hypertension at examination 1 and with complete information. Individuals who participated in both visits versus only the first visit, were older (43.1 versus 37.3 years old, P<0.01), more likely to be female (56.2% versus 44.6%, P<0.01), had higher mean BMI (29.5 versus 29.1 kg/m2, P=0.04), higher SBP (120.3 versus 119.3 mm Hg, P=0.02) but did not differ based on DBP (72.4 versus 71.8 mm Hg, P=0.60) during the first examination.
Statistical Analysis
All analyses accounted for the complex survey design including cluster sampling and the use of stratification in sample selection. The sampling weights were calculated based on the baseline sampling weights and accounted for the non‐responses for examination 2. The sampling weights are trimmed, calibrated to the age, sex, and Hispanic/Latino background distributions from the 2010 US Census for the 4 study field centers based on participants’ age at the first examination, and normalized.
Among the population free from hypertension, we first described baseline demographic, socioeconomic, clinical, and behavioral characteristics. We calculated mean follow‐up time beginning at the date of each participant's first study visit (baseline examination) and ending at the date of the second study visit (follow‐up examination). Using Poisson regression through generalized linear regression models, we estimated incidence rates (IRs) of hypertension, per 1000 person‐years (PY), as well as incidence rate ratios (IRRs) overall and according to baseline demographic, socioeconomic, clinical, and behavioral factors of interest. Except for the estimates reported across age groups, all IRs and IRRs were age adjusted to the overall HCHS/SOL baseline age distribution. We also estimated IRRs fully adjusted for: age, Hispanic/Latino background, education, income, nativity/years in the United States, health insurance, BMI, elevated SBP, smoking, physical activity, and AHEI 2010.
Additionally, for each Hispanic/Latino background group, we reported the 6‐year age‐adjusted predicted probability of developing hypertension. Next, we estimated the percentage of individuals recommended for treatment of hypertension (in the whole population and restricted to individuals with hypertension). Among individuals recommended for treatment of hypertension, we estimated the proportion treated and the proportion controlled. Finally, as a supplementary analysis, we also presented age standardized cumulative incidences along with age‐adjusted IRs, and IRRs according to the JNC7 definition of hypertension. All results were stratified by sex. Analyses were conducted in SUDAAN (Version 11.0.1, Research Triangle Institute, NC) to account for the complex survey design and the sampling weights.
Results
Baseline demographic and socioeconomic characteristics of the overall US Hispanics/Latinos free from hypertension in the HCHS/SOL target population in 2008 to 2011 (displayed in Table 1) were similar between men and women with 7.8% (95% CI, 6.4–9.4) in Central American, 15.3% (95% CI, 12.7–18.3) in Cuban, 9.1% (95% CI, 7.6–10.7) in Dominican, 44.2% (95% CI, 40.7–47.7) in Mexican, 13.4% (95% CI, 11.8–15.2) in Puerto Rican, and 5.4% (95% CI, 4.5–6.5) in South American background groups. The overall study population was mostly young with 53.6% (95% CI, 51.6–55.5) aged 18 to 34 years, 31.9% (95% CI, 30.2–33.7) aged 35 to 49 years, 12.3% (95% CI, 11.4–13.3) aged 50 to 64 years, and 2.2% (95% CI, 1.7–2.8) aged 65 to 74 years. Overall, 29.0% (95% CI, 27.1–31.0) had less than a high school education, with 59.9% (95% CI, 57.7–62.0) having an income <$30 000 per year, 27.7% (95% CI, 25.7–29.7) born in the United States, and 46.3% (95% CI, 43.9–48.5) with health insurance. Compared with men, at baseline, women were more likely to have the following: lower income, health insurance, obesity, and lower (less favorable) AHEI 2010 scores. Women were less likely to: be US born, have elevated SBP, smoke, or meet physical activity guidelines compared with men (P values all <0.05).
Table 1.
Baseline Characteristics of Individuals Free From Hypertension in the HCHS/SOL Target Population by Sex, 2008 to 2011
| Overall (Unweighted N=6171) | Men (Unweighted n=2137) | Women (Unweighted n=4034) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Unweighted | Weighted | Unweighted | Weighted | Unweighted | Weighted | ||||
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | |
| Hispanic/Latino backgrounda | |||||||||
| Mexican | 3031 | 44.2 | 40.7–47.7 | 1001 | 41.8 | 37.8–46.0 | 2030 | 46.1 | 42.3–49.9 |
| Central American | 659 | 7.8 | 6.4–9.4 | 209 | 7.6 | 5.9–9.9 | 450 | 7.9 | 6.5–9.5 |
| Cuban | 636 | 15.3 | 12.7–18.3 | 262 | 16.7 | 13.6–20.3 | 374 | 14.2 | 11.6–17.3 |
| Dominican | 452 | 9.1 | 7.6–10.7 | 122 | 7.5 | 5.7–9.8 | 330 | 10.3 | 8.7–12.3 |
| Puer– Rican | 726 | 13.4 | 11.8–15.2 | 288 | 15.3 | 13.0–17.8 | 438 | 11.8 | 10.1–13.8 |
| South American | 483 | 5.4 | 4.5–6.5 | 177 | 5.5 | 4.3–6.9 | 306 | 5.4 | 4.4–6.5 |
| Mixed/other | 173 | 4.9 | 4.0–6.0 | 73 | 5.6 | 4.1–7.5 | 100 | 4.3 | 3.3–5.6 |
| Women | 4034 | 54.3 | 52.5–56.1 | ||||||
| Age group | |||||||||
| 18–34 y | 1825 | 53.6 | 51.6–55.5 | 691 | 54.5 | 51.3–57.6 | 1134 | 52.8 | 50.6–55.0 |
| 35–49 y | 2490 | 31.9 | 30.2–33.7 | 806 | 31.4 | 28.6–34.4 | 1684 | 32.3 | 30.5–34.3 |
| 50–64 y | 1703 | 12.3 | 11.4–13.3 | 580 | 11.8 | 10.5–13.3 | 1123 | 12.7 | 11.7–13.9 |
| 65–74 y | 153 | 2.2 | 1.7–2.8 | 60 | 2.3 | 1.5–3.5 | 93 | 2.1 | 1.5–2.8 |
| Less than HS education | 2093 | 29.0 | 27.1–31.0 | 728 | 29.7 | 27.0–32.5 | 1365 | 28.4 | 26.1–30.8 |
| Income <$30 000a | 3880 | 59.8 | 57.7–62.0 | 1228 | 54.6 | 51.4–57.8 | 2652 | 64.2 | 61.9–66.5 |
| Nativity/years in the United Statesa | |||||||||
| Non‐US born <10 y in United States | 1591 | 30.7 | 28.4–33.1 | 503 | 28.5 | 25.5–31.8 | 1088 | 32.5 | 29.8–35.3 |
| Non‐US born, ≥10 y in United States | 3391 | 41.6 | 39.7–43.6 | 1172 | 41.4 | 38.6–44.2 | 2219 | 41.8 | 39.6–44.1 |
| US born | 1169 | 27.7 | 25.7–29.7 | 455 | 30.1 | 27.2–33.1 | 714 | 25.7 | 23.4–28.1 |
| Health insureda | 2768 | 46.2 | 43.9–48.5 | 902 | 44.2 | 41.0–47.4 | 1866 | 47.9 | 45.3–50.4 |
| Body mass indexa | |||||||||
| Normal | 1590 | 30.5 | 28.7–32.4 | 553 | 30.4 | 27.6–33.3 | 1037 | 30.6 | 28.4–32.9 |
| Overweight | 2402 | 37.0 | 35.3–38.8 | 930 | 40.2 | 37.4–43.1 | 1472 | 34.4 | 32.3–36.5 |
| Obese | 2170 | 32.5 | 30.6–34.4 | 563 | 29.4 | 26.6–32.4 | 1517 | 35.0 | 32.7–37.4 |
| Elevated SBPa (120–129 mm Hg) | 1330 | 20.1 | 18.7–21.6 | 698 | 30.8 | 28.2–33.5 | 632 | 11.0 | 9.9–12.3 |
| Smokinga | |||||||||
| Never | 3984 | 66.4 | 64.6–68.1 | 1097 | 57.3 | 54.3–60.3 | 2887 | 73.9 | 71.7–75.9 |
| Current | 1136 | 20.2 | 18.6–21.8 | 530 | 25.4 | 22.8–28.3 | 606 | 15.8 | 14.2–17.6 |
| Former | 1033 | 13.5 | 12.4–14.6 | 498 | 17.2 | 15.3–19.4 | 535 | 10.3 | 9.1–11.7 |
| Meets 2008 PA guidelinesa | 4059 | 71.1 | 69.3–72.8 | 1651 | 80.7 | 78.4–82.9 | 2408 | 63.0 | 60.7–65.2 |
| AHEI 2010, meana | 47.0 | 46.6–47.4 | 48.4 | 47.9–48.9 | 45.8 | 45.4–46.3 | |||
Except for age‐specific estimates, all estimates are age standardized to the overall baseline age distribution. AHEI indicates alternative healthy eating index; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HS, high school; PA, physical activity; PY, person‐years; and SBP, systolic blood pressure.
Indicates that estimates are differ significant (P<0.05) according to sex using Chi‐squares for proportions and t tests for means.
The mean follow‐up time between each examination was 6.2 years (95% CI, 6.1–6.2) with an overall age adjusted IR of 34 per 1000 PY (95% CI, 31–36). Among men, the overall age adjusted IR of hypertension was 36 per 1000 PY (95% CI, 32–40), though it differed by Hispanic/Latino background group, P=0.04 (Table 2). For example, hypertension IRs were 58% higher (IRR, 1.58; 95% CI, 1.19–2.10) among men of Cuban background (IR, 45 per 1000 PY; 95% CI, 37–56) and 61% higher (IRR, 1.61; 95% CI, 1.03–2.52) among men of Dominican background (IR, 46 per 1000 PY; 95% CI, 31–70) compared with Mexican American men (IR, 29 per 1000 PR; 95% CI, 24–35). Additionally, among men, IRs were higher with older age, greater education, higher BMI, and elevated BP, and lower with a higher (more favorable) AHEI score. From fully adjusted models, hypertension IRRs remained higher among men of Cuban (IRR, 1.66; 95% CI, 1.08–2.53) and Dominican (IRR, 1.69; 95% CI, 1.07–2.68) background compared with Mexican American men.
Table 2.
Incidence of Hypertension Among US Hispanic/Latino Men in the HCHS/SOL Target Population by Baseline Characteristics
| Incidence Rate (Per 1000 PY) | Incidence Rate Ratio | Fully Adjusteda Incidence Rate Ratio | ||||
|---|---|---|---|---|---|---|
| IR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Overall | 35 | 32–39 | ··· | ··· | ||
| Hispanic/Latino background | ||||||
| Mexican (ref) | 29 | 24–35 | 1.00 | ··· | 1.00 | ··· |
| Central American | 32 | 22–46 | 1.10 | 0.72–1.70 | 1.20 | 0.78–1.85 |
| Cuban | 45b | 37–56 | 1.58 | 1.19–2.10 | 1.66b | 1.08–2.53 |
| Dominican | 46 | 31–70 | 1.61 | 1.03–2.52 | 1.69b | 1.07–2.68 |
| Puer– Rican | 35 | 27–45 | 1.22 | 0.90–1.66 | 1.29 | 0.85–1.94 |
| South American | 30 | 20–45 | 1.04 | 0.66–1.63 | 1.12 | 0.69–1.81 |
| Mixed/other | 42 | 25–70 | 1.47 | 0.85–2.53 | 1.48 | 0.86–2.57 |
| Age group | ||||||
| 18–34 y (ref) | 21 | 26–26 | 1.00 | ··· | 1.00 | ··· |
| 35–49 y | 45b | 39–52 | 2.19 | 1.65–2.92 | 1.99b | 1.44–2.75 |
| 50–64 y | 67b | 59–76 | 3.25 | 2.47–4.27 | 2.82b | 1.98–4.00 |
| 65–74 y | 85b | 56–128 | 4.13 | 2.56–6.68 | 3.59b | 2.12–6.08 |
| Education | ||||||
| HS or more (ref) | 37 | 33–43 | 1.00 | ··· | 1.00 | ··· |
| Less than HS | 30b | 25–35 | 0.80b | 0.64–0.99 | 0.77b | 0.61–0.96 |
| Income | ||||||
| ≥$30 000 (ref) | 33 | 27–40 | 1.00 | ··· | 1.00 | ··· |
| <$30 000 | 37 | 32–42 | 1.12 | 0.88–1.42 | 1.08 | 0.85–1.36 |
| Nativity/y in the United States | ||||||
| Non‐US born <10 y in United States (ref) | 33 | 27–41 | 1.00 | ··· | 1.00 | ··· |
| Non‐US born, ≥10 y in United States | 36 | 31–41 | 1.07 | 0.84–1.36 | 1.21 | 0.96–1.54 |
| US born | 34 | 27–43 | 1.03 | 0.75–1.40 | 1.09 | 0.78–1.53 |
| Health insurance | ||||||
| Yes (ref) | 34 | 28–40 | 1.00 | ··· | 1.00 | ··· |
| No | 37 | 28–40 | 1.09 | 0.88–1.35 | 1.06 | 0.85–1.31 |
| Body mass index | ||||||
| Normal (ref) | 25 | 20–31 | 1.00 | ··· | 1.00 | ··· |
| Overweight | 34b | 29–40 | 1.37 | 1.05–1.78 | 1.43b | 1.09–1.88 |
| Obese | 47b | 39–56 | 1.90 | 1.44–2.52 | 1.95b | 1.47–2.58 |
| Systolic BP | ||||||
| <120 mm Hg (ref) | 28 | 24–32 | 1.00 | ··· | 1.00 | ··· |
| 120–129 mm Hg | 51b | 44–59 | 1.85b | 1.52–2.26 | 1.87b | 1.53–2.27 |
| Smoking | ||||||
| Never (ref) | 33 | 28–39 | 1.00 | ··· | 1.00 | ··· |
| Current | 38 | 31–46 | 1.34 | 0.89–1.45 | 1.24 | 0.98–1.58 |
| Former | 35 | 28–43 | 1.05 | 0.82–1.35 | 1.11 | 0.88–1.41 |
| Meets 2008 PA guidelines | ||||||
| Yes (ref) | 32 | 26–40 | 1.00 | ··· | 1.00 | ··· |
| No | 36 | 32–41 | 0.90 | 0.70–1.15 | 0.89 | 0.70–1.13 |
| AHEI 2010‡ | 36 | 32–40 | 0.88b | 0.80–0.97 | 0.97 | 0.85–1.11 |
Except for age specific estimates, all IRs and IRRs are age adjusted. AHEI indicates alternative healthy eating index; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HS, high school; IR, incidence rate; IRR, incidence rate ratio; PA, physical activity; PY, person‐years; and SBP, systolic blood pressure.
Fully adjusted for all covariates in the table.
Estimate is significantly different from the reference category, P<0.05.
IR estimated at a mean value of AHEI 2010 (47 units); IRR estimates reflect 1 SD (7.6 units).
Among women, the overall age adjusted IR of hypertension was 32 per 1000 PY (95% CI, 30–35), though it differed by Hispanic/Latino background group, P<0.01 (Table 3). For example, hypertension IRs were 46% higher (IRR, 1.46; 95% CI, 1.16–1.83) among women of Cuban background (IR, 38 per 1000 PY; 95% CI, 32–46), 48% higher (IRR, 1.48; 95% CI, 1.08–2.04) among women of Dominican background (IR, 39 per 1000 PY; 95% CI, 29–51), and 71% higher (IRR, 1.71; 95% CI, 1.34–2.19) among women of Puerto Rican background (IR, 45 per 1000 PY; 95% CI, 37–55) compared with Mexican American women (IR, 26 per 1000 PR; 95% CI, 23–30). Additionally, among women, IRs were higher with older age, less education, lower income, health insurance, higher BMI, elevated BP, current smoking, and lower with a higher (more favorable) AHEI score. From fully adjusted models, hypertension IRRs attenuated such that IRRs were no longer higher among women of Cuban (IRR, 1.32; 95% CI, 0.98–1.77), Dominican (IRR, 1.38; 95% CI, 0.99–1.93), or Puerto Rican (IRR, 1.16; 95% CI, 0.87–1.56) background compared with Mexican American women.
Table 3.
Incidence of Hypertension Among US Hispanic/Latino Women in the HCHS/SOL Target Population by Baseline Characteristics
| Incidence Rate (Per 1000 PY) | Incidence Rate Ratio | Fully Adjusteda Incidence Rate Ratio | ||||
|---|---|---|---|---|---|---|
| IR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Overall | 32 | 30–35 | ··· | ··· | ||
| Hispanic/Latino background | ||||||
| Mexican (ref) | 26 | 23–30 | 1.00 | ··· | 1.00 | ··· |
| Central American | 31 | 32–46 | 1.20 | 0.91–1.57 | 1.13 | 0.85–1.51 |
| Cuban | 38b | 32–46 | 1.46b | 1.16–1.83 | 1.32 | 0.98–1.77 |
| Dominican | 39b | 29–51 | 1.48b | 1.08–2.04 | 1.38 | 0.99–1.93 |
| Puer– Rican | 45b | 37–55 | 1.71b | 1.34–2.19 | 1.16 | 0.87–1.56 |
| South American | 26 | 19–36 | 1.01 | 0.71–1.43 | 1.08 | 0.75–1.55 |
| Mixed/other | 47 | 28–77 | 1.79b | 1.07–2.99 | 1.53 | 0.92–2.53 |
| Age group | ||||||
| 18–34 y (ref) | 18 | 15–23 | 1.00 | ··· | 1.00 | ··· |
| 35–49 y | 38b | 33–43 | 2.07b | 1.60–2.67 | 1.85b | 1.42–2.42 |
| 50–64 y | 63b | 57–70 | 3.47b | 2.76–4.36 | 2.49b | 1.90–3.25 |
| 65–74 y | 120b | 100–144 | 6.58b | 4.93–8.77 | 4.03b | 2.76–5.89 |
| Education | ||||||
| HS or more (ref) | 30 | 27–33 | 1.00 | ··· | 1.00 | ··· |
| Less than HS | 38b | 33–44 | 1.27b | 1.09–1.50 | 1.25b | 1.05–1.48 |
| Income | ||||||
| ≥$30 000 (ref) | 28 | 23–33 | 1.00 | ··· | 1.00 | ··· |
| <$30 000 | 35b | 32–39 | 1.28b | 1.04–1.57 | 1.19 | 0.97–1.45 |
| Nativity/years in the United States | ||||||
| Non‐US born <10 y in United States (ref) | 30 | 26–35 | 1.00 | ··· | 1.00 | ··· |
| Non‐US born, ≥10 y in United States | 32 | 28–36 | 1.05 | 0.87–1.28 | 0.99 | 0.80–1.22 |
| US born | 37 | 30–46 | 1.23 | 0.94–1.60 | 1.02 | 0.74–1.40 |
| Health insurance | ||||||
| Yes (ref) | 38 | 24–31 | 1.00 | ··· | 1.00 | ··· |
| No | 28b | 33–42 | 0.73b | 0.62–0.88 | 0.76b | 0.62–0.92 |
| Body mass index | ||||||
| Normal (ref) | 21 | 17–26 | 1.00 | ··· | 1.00 | ··· |
| Overweight | 31b | 27–36 | 1.50b | 1.14–1.97 | 1.39b | 1.06–1.81 |
| Obese | 42b | 37–48 | 2.02b | 1.57–2.60 | 1.81b | 1.42–2.31 |
| Systolic BP | ||||||
| <120 mm Hg (ref) | 27 | 24–30 | 1.00 | ··· | 1.00 | ··· |
| 120–129 mm Hg | 63b | 54–72 | 2.32b | 1.95–2.76 | 2.19b | 1.83–2.62 |
| Smoking | ||||||
| Never (ref) | 30 | 27–34 | 1.00 | ··· | 1.00 | ··· |
| Current | 41b | 34–49 | 1.35b | 1.10–1.65 | 1.29b | 1.03–1.61 |
| Former | 34 | 27–44 | 1.13 | 0.87–1.48 | 1.11 | 0.88–1.41 |
| Meets 2008 PA guidelines | ||||||
| Yes (ref) | 32 | 29–36 | 1.00 | ··· | 1.00 | ··· |
| No | 34 | 29–36 | 1.05 | 0.89–1.25 | 1.05 | 0.89–1.23 |
| AHEI 2010c | 33 | 30–36 | 0.83b | 0.77–0.90 | 0.94 | 0.83–1.06 |
Except for age specific estimates, all IRs and IRRs are age adjusted. AHEI indicates alternative healthy eating index; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HS, high school; IR, incidence rate; IRR, incidence rate ratio; PA, physical activity; PY, person‐years; and SBP, systolic blood pressure.
Fully adjusted for all covariates in the table.
Estimate is significantly different from the reference category, P<0.05.
IR estimated at a mean value of AHEI 2010 (47 units); IRR estimates reflect 1 SD (7.6 units).
Among individuals free from hypertension at baseline, ≈1 in 5 developed hypertension 6 years later (20.6%; 95% CI, 19.2–22.1), see Figure which depicts the 6‐year age‐adjusted probability of developing hypertension by sex and Hispanic/Latino background group. Also, among all individuals free from hypertension at baseline, the prevalence of hypertension treatment recommendation was 14.4% for men (95% CI, 12.8–16.1) and 11.9% for women (95% CI, 10.7–13.3), Table 4. When restricted to individuals with incident hypertension, the prevalence of hypertension treatment recommendation was 56.7% for men (95% CI, 49.6–63.5) and 51.5% for women (95% CI, 44.9–58.1). Among individuals recommended for hypertension treatment, the prevalence of hypertension treatment was 30.9% among men (95% CI, 23.6–39.2) and 37.4% among women (95% CI, 30.3–45.0). Also, among individuals recommended for hypertension treatment, the prevalence of hypertension control was 18.4% among men (95% CI, 12.8–25.9) and 22.7% among women (95% CI, 17.1–29.5). The prevalence of hypertension treatment recommendation, treatment, and control by Hispanic/Latino background group are also presented in Table 4.
Figure 1. Age‐adjusted predicted probability of developing of hypertension over 6 years among US Hispanic/Latino men and women, Hispanic Community Health Study/Study of Latinos, 2008 to 2017.
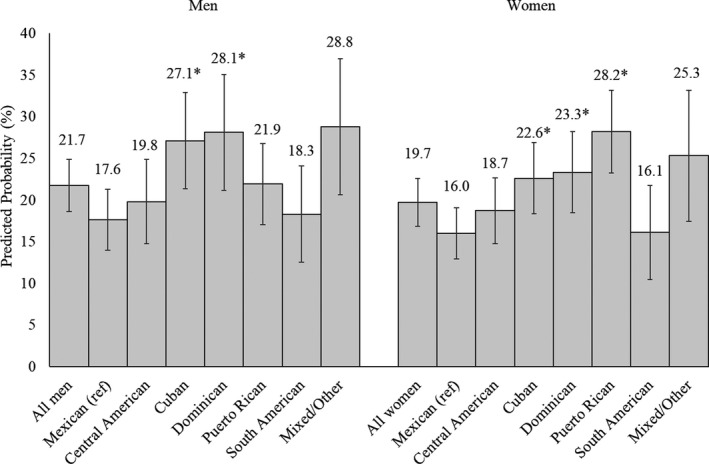
Predicted probability of developing hypertension differs among US Hispanic/Latino women (P<0.05); men (P=0.11). *Predicted probability of developing hypertension is significantly greater than Mexican Americans, P<0.05.
Table 4.
Prevalence of US Hispanics/Latinos Recommended for Hypertension Treatment, Treated, and Controlled in the HCHS/SOL Target Population by Sex
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Recommended for Treatment | Treated | Controlled | Recommended for Treatment | Treated | Controlled | |||
| (Among All Men) | (Among All Men With Hypertensiona) | (Among All Men Recommended for Hypertension Treatmentb) | (Among All Women) | (Among All Women With Hypertensiona) | (Among All Women Recommended For Hypertension Treatmentb) | |||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Overall | 14.4 (12.8–16.1) | 56.7 (49.6–63.5) | 26.6 (19.9–34.5) | 18.4 (12.8–25.9) | 11.9 (10.7–13.3) | 51.5 (44.9–58.1) | 36.4 (29.6–43.8) | 22.7 (17.1–29.5) |
| Hispanic/Latino background | ||||||||
| Mexican (reference) | 12.5 (10.2–15.3) | 63.3 (51.7–73.4) | 27.7 (18.3–39.5) | 20.3 (12.1–31.9) | 10.8 (9.2–12.6) | 56.8 (47.0–66.2) | 49.8 (36.2–63.4) | 33.5 (22.0–47.4) |
| Central American | 13.3 (9.6–18.0) | 47.1 (31.4–63.5) | 15.4 (8.2–27.2) | 11.8 (5.5–23.3) | 9.6 (7.5–12.2) | 41.3 (31.2–52.2)c | 30.0 (18.1–45.4)c | 19.1 (12.9–27.3) |
| Cuban | 17.4 (12.9–23.2) | 55.4 (32.7–76.1) | 16.6 (10.5–25.2) | 10.6 (5.4–19.8) | 12.1 (9.2–15.8) | 47.2 (28.4–66.8) | 25.5 (17.2–36.1)c | 19.0 (11.3–30.2) |
| Dominican | 14.4 (10.2–20.1) | 38.1 (22.1–57.2)c | 43.4 (13.4–79.2) | 36.3 (9.5–75.5) | 10.8 (8.2–14.1) | 34.2 (25.0–44.9)c | 22.8 (14.2–34.4)c | 12.5 (5.7–25.3)c |
| Puerto Rican | 14.2 (10.5–18.9) | 55.5 (39.3–70.7) | 24.3 (11.1–45.2) | 20.4 (8.2–42.3) | 18.2 (13.5–24.2)c | 63.7 (46.8–77.8) | 28.7 (18.7–41.5)c | 7.9 (3.3–17.7)c |
| South American | 9.3 (5.8–14.4) | 39.6 (23.7–58.1)c | 7.8 (3.6–16.0)c | 7.5 (3.3–15.8)c | 7.5 (5.5–10.0)c | 32.0 (24.3–40.9)c | 77.4 (63.9–86.9)c | 72.9 (60.5–82.6)c |
| Mixed/other | 23.5 (13.7–37.2) | 74.3 (48.0–90.1) | 27.3 (7.9–62.3) | 10.9 (2.6–35.8) | 16.3 (8.7–28.4) | 58.8 (33.1–80.4) | 25.1 (10.4–49.3)c | 20.1 (8.4–41.0) |
All estimates are age standardized to the overall baseline age distribution (shown in Table 1). HCHS/SOL indicates Hispanic Community Health Study/Study of Latinos.
Among individuals with hypertension (unweighted n=575 for men and n=970 for women).
Among individuals recommended for treatment of hypertension (unweighted n=456 for men and n=669 for women).
Estimate is significantly different from Mexican Americans, the reference category, P<0.05.
The incidence of hypertension according to JNC7 defined guidelines are displayed in Table S1 and show similar results, with higher incidence of hypertension among US Hispanics/Latinos of Caribbean background.
Discussion
In a large cohort of diverse US Hispanics/Latinos free from hypertension in 2008 to 2011, the 6‐year probability of developing hypertension was 21% overall or 22% among men and 20% among women. Hypertension IRs were highest among US Hispanics/Latinos from Caribbean backgrounds (Cuban, Dominican, and Puerto Rican). Among US Hispanics/Latinos without hypertension in 2008 to 2011, 14% of men and 12% of women were recommended for treatment of hypertension 6 years later. Among individuals recommended for treatment of hypertension, the prevalence of treatment was 27% among men and 36% among women; the prevalence of control was 18% among men 23% among women. Thus, our findings demonstrate substantial variation in hypertension incidence by Hispanic/Latino background group and emphasize that rates of hypertension treatment and control among US Hispanics/Latinos are low.
Though most studies classify Hispanics/Latinos as a homogeneous group, US Hispanics/Latinos are diverse with respect to background of origin, race, immigration history, socioeconomic status, and culture.6 This diversity likely manifests in variation in CVD and its risk factors across Hispanic/Latino background groups.14 In fact, results from the Multi‐Ethnic Study of Atherosclerosis first showed a higher prevalence of hypertension among Dominican versus Mexican or Puerto Rican backgrounds.25 Data from the National Health Interview Survey showed a higher prevalence of hypertension among black versus white Hispanics/Latinos.26 Cross‐sectional results from HCHS/SOL, the largest study of Hispanics/Latinos of diverse backgrounds also showed variation in the prevalence of CVD risk factors14, 17—including hypertension, with the highest rates among HCHS/SOL participants of Caribbean backgrounds.17 Our findings, which serve as a longitudinal extension of prior HCHS/SOL cross‐sectional results, are consistent and show higher rates of incident hypertension among US Hispanics/Latino of Cuban, Dominican, and Puerto Rican (women only) compared with Mexican backgrounds.
Reasons underlying the higher rates of hypertension among Hispanics/Latinos of Dominican and Cuban versus Mexican backgrounds warrant additional investigation. It has been noted that a longer duration of US residence is associated with hypertension.19, 27, 28 For example, studies show that Mexican Americans born in the United States have a lower prevalence of hypertension than their Mexican born counterparts.19, 29 However, our findings showed that recent immigration (within 10 years) was not protective against the development of hypertension 6‐years later. As acculturation experience and its relationship to hypertension may differ based on country of origin,6, 28 research related to acculturation may be more informative when conducted within one specific Hispanic/Latino background, rather than in aggregate. It has also been suggested that a higher proportion of African admixture may manifest in higher rates of hypertension25—particularly among Hispanics/Latinos shown to have a greater proportion of African admixture, such as those of Dominican background.9 However, disentangling the role of African admixture from skin color based discrimination,30 or Hispanic/Latino background,9 in the development of hypertension would be challenging. Further, prior work has seldom shown hypertension to be primarily genetically mediated. For example, results from the Family Blood Pressure Program showed that racial differences in blood pressure between whites and blacks may be better explained by education than by genetics.31 While our results accounted for common behavioral contributors to hypertension which may differ across Hispanic/Latino background groups such as: BMI, physical activity, and diet, future studies may focus more closely on other contributing factors. In a recent paper, sodium, potassium, and the ratio of sodium to potassium, all of which are associated with blood pressure,32 and also hypertension control,33 were shown to differ among US Hispanics/Latinos of the HCHS/SOL.34 Whether differences in sodium intake, and salt sensitivity35, 36, 37 across Hispanic/Latino background groups played a role in the noted differences in hypertension incidence is yet to determined.
Trends in incident hypertension also differed by sex. For example, lower educational attainment was associated with lower risk of hypertension among men, but higher risk of hypertension among women. These results are consistent with literature showing strong associations of low socioeconomic factors with poorer health status, among women in particular.38, 39, 40 Additionally, among US Hispanic/Latino women, Puerto Ricans had the highest rate of incident hypertension—71% higher than Mexican Americans. Yet after adjustment for socioeconomic, clinical, and behavioral characteristics, Puerto Rican women fared no different than women of Mexican background. Further, the risk of hypertension among women of Cuban and Dominican versus Mexican background were attenuated in fully adjusted models—a finding which was not reproduced in men. Taken together these data suggest that factors driving hypertension among US Hispanics/Latinos may differ based on sex. Further investigation is necessary to determine which sex‐specific factors drive such differences.
The 2017 ACC/AHA hypertension guideline recommends treatment for hypertension at a higher BP threshold (in the general population) than what is used to define hypertension.3 Therefore, there is a discrepancy between the proportion classified as having hypertension versus those requiring treatment. Among US Hispanics/Latinos who developed hypertension, slightly greater than half were recommended for treatment. Of concern are the particularly low rates of hypertension treatment and control among US Hispanics/Latinos (<40% treated and 23% controlled). While these data may suggest low rates of hypertension awareness among recent cases, they nevertheless emphasize the need for a concerted public health effort to increase the proportion of US Hispanics/Latinos controlled. A lack of health insurance has been routinely linked to poor outcomes41 including uncontrolled hypertension.42 In the current sample, less than half of participants had health insurance at baseline—potentially having important implications related to hypertension management. Further assessment of the impact of insurance status on management of hypertension among US Hispanics/Latinos, particularly after the passage of the Affordable Care Act, may be warranted.
Study Limitations
This work is not without limitations. First, we acknowledge that there was considerable loss to follow‐up in this study resulting in a smaller sample size. However, given the descriptive nature of our findings, it is unlikely that loss to follow‐up influenced study results. Further, due in part to sample size constraints, we were unable to present results for all US Hispanics/Latinos by background country of origin. As a result, US Hispanics/Latinos of South American and Central American backgrounds (not including Mexico) were aggregated, limiting our ability to make more specific conclusions based on country of origin for these groups.
Additionally, the 2017 ACC/AHA guideline for the diagnosis of hypertension requires a measurement of high BP on 2 separate occasions.3 In the current study, incident hypertension was defined by BP measurements ascertained once (at the follow‐up examination). Likewise, hypertension treatment may be subject to some measurement error given that it was assessed via self‐report. Further, we were unable to assess hypertension awareness, as the 2017 ACC/AHA guideline was released in November 2017, 1 month before the completion of the HCHS/SOL follow‐up examination. This is notable given historically low rates of hypertension awareness among US Hispanics/Latinos,43 ranging from 57% among Central American men to 78% among Cuban men and from 72% among South American women to 79% among Cuban and Dominican women.17 Additionally, our measures of hypertension treatment recommendation, hypertension treatment, and BP control were estimated among individuals with new onset hypertension (within 6 years) and therefore do not reflect individuals with prevalent hypertension. For example, rates of hypertension treatment may be more common among older individuals or more established cases of hypertension.44 Further, the proportion with controlled hypertension may be particularly low among those with new onset hypertension as control may be a function of time since diagnosis. Though we note among Mexican Americans sampled in National Health and Nutrition Examination Survey, rates of hypertension treatment, and control have also been historically lower than among non‐Hispanic whites.43 Taken together, these findings suggest, at the least, that an examination of whether a more culturalized approach to primary care may be effective at improving outcomes in this population is warranted.
Despite limitations, this study makes an important contribution to the sparse6 literature related to the development of hypertension among US Hispanics/Latinos. To our knowledge, it is the first study of its kind to report on rates of incidence hypertension among Hispanics/Latinos of diverse backgrounds using the 2017 ACC/AHA guidelines. It includes standardized measurements of BP which were clinically ascertained. Additionally, given the large sample, we were able to describe and compare rates of hypertension not only across Hispanic/Latino background groups, but also by sex. Therefore, this study provides an important first look into the development of hypertension among US Hispanics/Latinos adults and highlights disparities across different Hispanic/Latino background groups.
Conclusions
In summary, among participants of a large population based study of US Hispanics/Latinos of diverse backgrounds, we found substantial variation in rates of incident hypertension. US Hispanics/Latinos from Caribbean backgrounds had the highest rates of hypertension. Disparities could not be fully explained by traditional hypertension risk factors (especially true among men), warranting further investigation. Additionally, rates of hypertension treatment and control among US Hispanics/Latinos were found to be suboptimal. Efforts to improve these indices require broad based public health strategies.
Sources of Funding
The Hispanic Community Health Study/Study of Latinos was performed as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute to the University of North Carolina (N01‐HC65233), University of Miami (N01‐HC65234), Albert Einstein College of Medicine (N01‐HC65235), Northwestern University (N01‐HC65236), and San Diego State University (N01‐HC65237). Dr Elfassy was supported by the University of Miami Clinical and Translational Science Institute, from National Institutes of Health/National Center for Advancing Translational Sciences (KL2TR002737), she is currently supported by National Institutes of Health/National Institute on Minority Health and Health Disparities (K01MD014158).
Disclosures
None.
Supporting information
Table S1
(J Am Heart Assoc. 2020;9:e015031 DOI: 10.1161/JAHA.119.015031.)
For Sources of Funding and Disclosures, see page 12.
References
- 1. Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart disease and stroke statistics‐2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 2. Franco OH, Peeters A, Bonneux L, de Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–286. [DOI] [PubMed] [Google Scholar]
- 3. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 4. Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, Whelton PK. Potential U.S. population impact of the 2017 American College of Cardiology/American Heart Association high blood pressure guideline. Circulation. 2018;71:109–118. [Google Scholar]
- 5. Colby SL, Ortman JM. Projesctions of the Size and Composition of the US Population: 2014 to 2060. Current Population Reports, P25–1143, US Census Bureau, Washington, DC, 2014. Available at: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf. Accessed May 21, 2020. [Google Scholar]
- 6. Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, Palaniappan L, Pina IL, Ramirez S, Rodriguez B, et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014;130:593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haffner SM. Hypertension in the San Antonio Heart Study and the Mexico City Diabetes Study: clinical and metabolic correlates. Public Health Rep. 1996;111(suppl 2):11–14. [PMC free article] [PubMed] [Google Scholar]
- 8. Haffner SM, Mitchell BD, Valdez RA, Hazuda HP, Morales PA, Stern MP. Eight‐year incidence of hypertension in Mexican‐Americans and non‐Hispanic whites. The San Antonio Heart Study. Am J Hypertens. 1992;5:147–153. [DOI] [PubMed] [Google Scholar]
- 9. Conomos MP, Laurie CA, Stilp AM, Gogarten SM, McHugh CP, Nelson SC, Sofer T, Fernandez‐Rhodes L, Justice AE, Graff M, et al. Genetic diversity and association studies in US Hispanic/Latino populations: applications in the Hispanic Community Health Study/Study of Latinos. Am J Hum Genet. 2016;98:165–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sofer T, Baier LJ, Browning SR, Thornton TA, Talavera G, Wassertheil‐Smoller S, Daviglus M, Hanson R, Kobes S, Cooper RS, et al. Admixture mapping in the Hispanic Community Health Study/Study of Latinos reveals regions of genetic associations with blood pressure traits. PLoS One. 2017;12:e0188400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13:477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Siega‐Riz AM, Sotres‐Alvarez D, Ayala GX, Ginsberg M, Himes JH, Liu K, Loria CM, Mossavar‐Rahmani Y, Rock CL, Rodriguez B, et al. Food‐group and nutrient‐density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am J Clin Nutr. 2014;99:1487–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Arredondo EM, Sotres‐Alvarez D, Stoutenberg M, Davis SM, Crespo NC, Carnethon MR, Castaneda SF, Isasi CR, Espinoza RA, Daviglus M, et al. Physical activity levels in U.S. Latino/Hispanic adults: results from the Hispanic Community Health Study/Study of Latinos. Am J Prev Med. 2016;50:500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Daviglus ML, Pirzada A, Talavera GA. Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prog Cardiovasc Dis. 2014;57:230–236. [DOI] [PubMed] [Google Scholar]
- 15. Lavange LM, Kalsbeek WD, Sorlie PD, Aviles‐Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sorlie PD, Allison MA, Avilés‐Santa ML, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sorlie PD, Allison MA, Aviles‐Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green WC, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 19. Moran A, Diez Roux AV, Jackson SA, Kramer H, Manolio TA, Shrager S, Shea S. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–363. [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization . Global Physical Activity Surveillance. World Health Organization. Chronic Diseases and Health Promotion Web site. Published 2015. Available at: http://www.who.int/chp/steps/GPAQ/en/. Accessed December 24, 2015.
- 21. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough MJ, Wang M, Stampfer MJ, Willett W. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 suppl 1):S1–S266. [PubMed] [Google Scholar]
- 24. Goff DC Jr, Lloyd‐Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, Greenland P, Lackland D, Levy D, O'Donnell CJ, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi‐Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:962–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Balfour PC, Ruiz JM, Talavera GA, Allison MA, Rodriguez CJ. Cardiovascular disease in Hispanics/Latinos in the United States. J Lat Psychol. 2016;4:98–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Commodore‐Mensah Y, Ukonu N, Obisesan O, Aboagye JK, Agyemang C, Reilly CM, Dunbar SB, Okosun IS. Length of residence in the United States is associated with a higher prevalence of cardiometabolic risk factors in immigrants: a contemporary analysis of the National Health Interview Survey. J Am Heart Assoc. 2016;5:e004059 DOI: 10.1161/JAHA.116.004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yi S, Elfassy T, Gupta L, Myers C, Kerker B. Nativity, language spoken at home, length of time in the United States, and race/ethnicity: associations with self‐reported hypertension. Am J Hypertens. 2014;27:237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican‐Americans. J Immigr Minor Health. 2011;13:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and hypertension: a review of the empirical evidence and implications for clinical practice. Am J Hypertens. 2011;24:518–529. [DOI] [PubMed] [Google Scholar]
- 31. Non AL, Gravlee CC, Mulligan CJ. Education, genetic ancestry, and blood pressure in African Americans and Whites. Am J Public Health. 2012;102:1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Adrogue H, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007;356:1966–1978. [DOI] [PubMed] [Google Scholar]
- 33. Elfassy T, Chamany S, Bartley K, Yi SS, Angell SY. Lower 24‐h urinary sodium excretion is associated with hypertension control: the 2010 Heart Follow‐Up Study. J Hum Hypertens. 2019. DOI: 10.1038/s41371-019-0285-9 . [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Elfassy T, Sotres‐Alvarez D, Van Horn L, Angell A, Schneiderman N, Rundek T, Raij L, Wassertheil‐Smoller S, Mossavar‐Rahmani Y, Daviglus M, et al. Daily intake of sodium and potassium among diverse US Hispanics/Latinos, the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2019;32:868–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Svetkey LP, McKeown SP, Wilson AF. Heritability of salt sensitivity in black Americans. Hypertension. 1996;28:854–858. [DOI] [PubMed] [Google Scholar]
- 36. Richardson SI, Freedman BI, Ellison DH, Rodriguez CJ. Salt sensitivity: a review with a focus on non‐Hispanic blacks and Hispanics. J Am Soc Hypertens. 2013;7:170–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Elijovich F, Weinberger MH, Anderson CA, Appel LA, Bursztyn M, Cook NR, Cart RA, Newton‐Cheh CH, Sacks FM, Laffer CL, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68:e7–e46. [DOI] [PubMed] [Google Scholar]
- 38. Jenkins KR, Ofstedal MB. The association between socioeconomic status and cardiovascular risk factors among middle‐aged and older men and women. Women Health. 2014;54:15–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ogden CLLM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United‐States, 2005–2008. NCHS Data Brief. 2010;50:1–8. [PubMed] [Google Scholar]
- 40. Back JH, Lee Y. Gender differences in the association between socioeconomic status (SES) and depressive symptoms in older adults. Arch Gerontol Geriatr. 2011;52:e140–e144. [DOI] [PubMed] [Google Scholar]
- 41. Sorlie PD, Johnson NJ, Backlund E, Bradham DD. Mortality in the uninsured compared with that in persons with public and private health insurance. Arch Intern Med. 1994;154:2409–2416. [PubMed] [Google Scholar]
- 42. Norris KC. Health insurance and blood pressure control. J Am Heart Assoc. 2016;5:e005130 DOI: 10.1161/JAHA.116.005130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Foti K, Wang D, Appel LJ, Selvin E. Hypertension awareness, treatment and control in US adults: trends in the hypertension control cascade by population subgroup (NHANES 1999–2016). Am J Epidemiol. 2019;188:2165–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


