Abstract
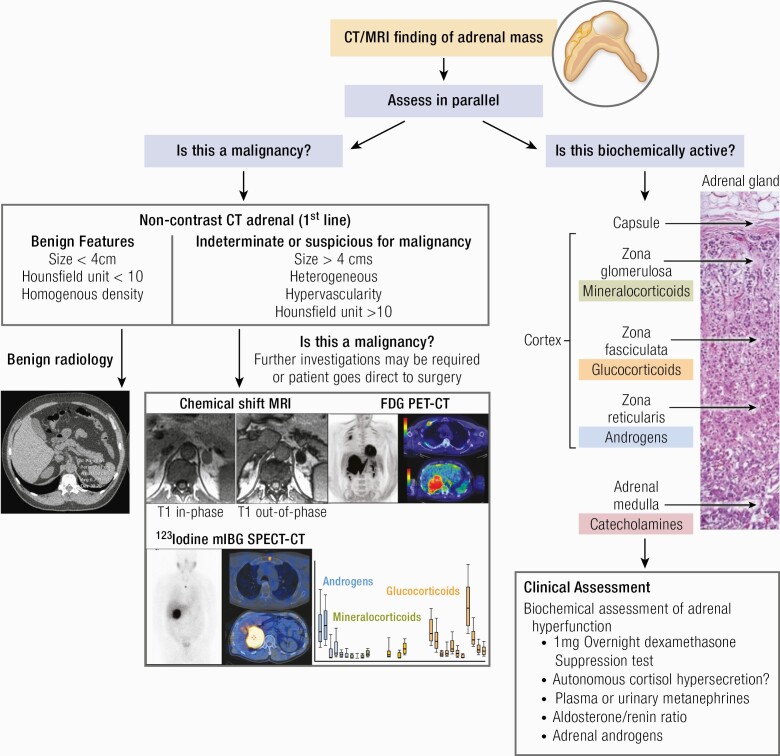
An adrenal incidentaloma is now established as a common endocrine diagnosis that requires a multidisciplinary approach for effective management. The majority of patients can be reassured and discharged, but a personalized approach based upon image analysis, endocrine workup, and clinical symptoms and signs are required in every case. Adrenocortical carcinoma remains a real concern but is restricted to <2% of all cases. Functional adrenal incidentaloma lesions are commoner (but still probably <10% of total) and the greatest challenge remains the diagnosis and optimum management of autonomous cortisol secretion. Modern-day surgery has improved outcomes and novel radiological and urinary biomarkers will improve early detection and patient stratification in future years to come.
Keywords: adrenal adenoma, adrenal incidentaloma, adrenal computed tomography, autonomous cortisol secretion, adrenal cortical carcinoma
Graphical Abstract
Graphical Abstract.
Essential Points.
Adrenal incidentaloma (AI) is a common endocrine diagnosis affecting ~2% of the general population, but over 7% of those over 70 years. It is rare in subjects below 40 years of age
~2% of patients with AI have adrenocortical cancer
Up to 10% of patients with AI have autonomous secretion of adrenal hormones
The initial investigation of choice is an unenhanced computed tomography scan of both adrenal glands
Pheochromocytoma and autonomous cortisol secretion should be excluded in every case and aldosteronism in patients with underlying hypertension and/or hypokalemia
Most patients with AI can be discharged once malignancy and hormone hypersecretion have been excluded
A causative link between cortisol hypersecretion and age-related comorbidities should be firmly established before recommending surgical excision
The use of diagnostic imaging has increased dramatically over the last 3 decades, driven by several factors, including technological advancement in imaging modalities, growing awareness of preventive care, the rising number of diagnostic imaging centers, and increasing prevalence of chronic disease driven in large part by an aging population. According to estimates from the Organisation for Economic Co-operation and Development, in 2016, the United States performed 245 computed tomography (CT) scans per 1000 population compared with a mean of 151 per 1000 population across 11 other high-income countries (1). For magnetic resonance imaging (MRI) the figures were 118 per 1000 population in the US and 82 per 1000 in other countries (1). Therefore, approximately 80 million CT scans are performed each year in the US (2), and in the UK over 5 million CT scans were performed in 2018 (3). Improvements in imaging modalities and their increasing use have led to the increased discovery of unexpected pathological findings. One of the most common unexpected findings revealed by CT, MRI, or ultrasonography is an incidental adrenal mass or incidentaloma. An adrenal incidentaloma (AI) is defined as a clinically unapparent adrenal mass greater than 1 cm in diameter detected during imaging performed for reasons other than for suspected adrenal disease (4). The term “incidentaloma” was coined in 1982 by Geelhoed and Druy (5), who recognized that with the advent of improved resolution of radiological techniques clinicians were faced with the unfamiliar dilemma of early diagnosis of an asymptomatic adrenal mass. This strict definition, recognized by the European Society of Endocrinology and European Network for the Study of Adrenal Tumors (ESE/ENSAT), excludes adrenal lesions discovered during the screening of patients with hereditary syndromes or extra-adrenal tumors (4). Current guidelines do not recommend that incidentally discovered adrenal lesions with a diameter <1 cm undergo further investigation unless clinically indicated (4,6-8).
Prevalence and epidemiology of AI
The prevalence of AIs varies depending on the source of data (autopsy, surgery, or radiology series) and patient selection (from general or specialized units). In the autopsy series with large patient numbers (series with greater than 1000 patients) (9-16), the reported prevalence of AI ranges from 1.05% (9) to 8.7% (10) (Table 1 (9-31)). In a large retrospective Japanese study, Kobayashi et al. investigated all cases of primary adrenocortical tumors recorded in the Pathological Autopsy Case Annuals of Japan during the 12-year period from 1973 to 1984 (17) (n = 321 847 cases) and reported a significantly lower overall prevalence of 0.03% of adrenocortical adenomas compared with historical series; however, the prevalence increased with age, with a peak in the fifth and sixth decades. Of the total number of identified adenomas in this autopsy series (n = 101), only 25 were identified in patients <50 years, while the remaining 75% were identified in patients older than 50 years. The variability in reported prevalence among the postmortem series reflects a combination of patient selection, inclusion criteria and the diagnostic challenge of distinguishing nodular hyperplasia and small adrenal nodules or adenomas. There is some overlap in the literature between the terms adenoma and nodule. Some authors have tried to define and divide these further. Russell et al. used the terms “adenoma” and “nodule” interchangeably to describe grossly visible collections of adrenal cortical cells, without any strict measurement criteria, in an autopsy series of 35 000 cases (15). They reported an overall prevalence of adrenal cortical adenomas (of all sizes) of 1.73%, increasing to 3.03% in patients older than 20 years (15). In a further autopsy series of 498 cases, Reinhard et al. (30) reported a higher prevalence of 5% for adrenal adenomas.
Table 1.
Summary of world literature of prevalence of adrenal incidentaloma based on autopsy series.
| Study/year (ref.) | Total no. of patients | Adenoma frequency (%) |
|---|---|---|
| Rinehart et al. 1941 (18) | 100 | 3 |
| Dempsey 1942 (19) | 50 | 8 |
| Russi et al. 1945 (11) | 9000 | 1.45 |
| Commons and Callaway 1948 (12) | 7437 | 2.86 |
| Schroeder 1953 (13) | 4000 | 1.38 |
| Dawson 1956 (20) | 45 | 8.9 |
| Holmes et al. 1956 (21) | 53 | 1.9 |
| Shamma et al. 1958 (22) | 220 | 1.8 |
| Spain and Weinsaft 1964 (23) | 200 | 15.5 |
| Dévényi 1967 (14) | 5120 | 3.55 |
| Kokko et al. 1967 (9) | 2000 | 1.05 |
| Hedeland et al. 1968 (10) | 739 | 8.7 |
| Dobbie 1969 (24) | 50 | 32 |
| Yamada and Fukunaga 1969 (25) | 948 | 5.4 |
| Granger and Genest 1970 (26) | 2425 | 2.52 |
| Russell et al 1972 (15) | 35000 | 1.73 |
| Abecassis et al. 1985 (27) | 988 | 1.9 |
| Winkelmann et al. 1987 (28) | 117 | 3.4 |
| Meagher et al. 1988 (29) | 2951 | 5 |
| Kawano et al. 1989 (16) | 153000 | 0.24 |
| Kobayashi et al. 1991 (17) | 321847 | 0.03 |
| Reinhard et al. 1996 (30) | 498 | 5 |
| Sington et al. 1999 (31) | 29 | 6.9 |
| Median values for all studies | 948 | 3 |
Source data is highly variable in terms of autopsy, surgery or radiological in origin, patient selection and AI definition.
The prevalence of any disease increases with the observer’s ability to detect the abnormalities associated with the disease (32). The first CT scan series regarding AIs, published between 1982 and 1986, reported a prevalence of 0.6% to 1.3% (33-35), which likely represents an underestimation due to the low-resolution technology available at the time and failure to detect smaller lesions. Over the last 2 decades, there has been a dramatic increase in the detection of AIs; series with contemporary high-resolution CT techniques report a prevalence close to that observed at autopsy (Table 2 (36-44)). In 2006, Bovio et al. (41) reported a frequency of AIs of 4.4% in a prospective study of 520 patients. This was significantly higher than the previous imaging series. While this increase may reflect improved modern scanning technology, the study included only patients older than 55 years of age, thereby only capturing patients at an age at which there is a greater prevalence of adrenal masses. Similarly, Song et al. reported a prevalence of 5% for AI in a retrospective study of CT reports (42). However, the study protocol included a dedicated radiological review of adrenal imaging in a significant percentage of cases, thereby possibly resulting in the diagnosis of more AI than would have been encountered in routine radiological clinical practice (44,45).
Table 2.
Prevalence of incidentally discovered adrenal masses by computed tomography (CT).
| Study (ref) | Year | No. of CT scans | No. of adrenal masses | Frequency (%) |
|---|---|---|---|---|
| Glazer et al. (33) | 1982 | 2200 | 14 | 0.6 |
| Prinz et al. (34) | 1982 | 1423 | 4 | 0.3 |
| Abecassis et al. (27) | 1985 | 1459 | 19 | 1.3 |
| Belldegrun et al. (35) | 1986 | 12000 | 88 | 0.7 |
| Herrera et al. (39) | 1991 | 61054 | 259 | 3.4 |
| Caplan et al. (40) | 1994 | 1779 | 33 | 1.9 |
| Bovio et al. (41) | 2006 | 520 | 23 | 4.4 |
| Song et al. (42) | 2008 | 65,231 | 3307 | 5.1 |
| Hammarstedt et al. (43) | 2010 | 34044 | 534 | 4.5 |
| Davenport et al. (44) | 2011 | 3705 | 37 | 1.0 |
| Davenport et al. (36) | 2014 | 4028 | 75 | 1.9 |
| Maher et al. (37) | 2018 | 38848 | 804 | 2.1 |
| Taya et al. (38) | 2019 | 42575 | 969 | 2.3 |
| Median values for all studies | N/A | 4028 | 75 | 1.9 |
Source data is highly variable in terms of autopsy, surgery or radiological in origin, patient selection and AI definition.
Effect of age, sex, and ethnicity on AI prevalence.
Among autopsy and radiology series, the prevalence of AIs increases with age, showing a peak incidence in the fifth to seventh decades (Table 3 (39,40,42,46-84)). AIs are rarely seen in patients less than 30 years of age (66) and therefore if present should be investigated promptly due to the risk of adrenocortical carcinoma (ACC) or functional lesions. Previous imaging studies have reported that AIs are more common in females (66,71,73); however, this has not been observed in autopsy studies (11,85).
Table 3.
Characteristics of adrenal incidentalomas: age, sex balance, tumor size and lateralization.
| Study (ref) | Year | No. of patients | Mean Age (years) | Female/Male | Tumor size (median, mm) | Unilateral | Right | Left | Bilateral |
|---|---|---|---|---|---|---|---|---|---|
| Virkkala et al. (46) | 1989 | 20 | 59 | 1.4 | 23 | 14 | N/A | N/A | 5 |
| Herrera et al. (39) | 1991 | 342 | 62 | 1.5 | 25 | N/A | |||
| Aso and Homma (47) | 1992 | 210 | 53 | 0.7 | 49 | N/A | |||
| Reincke et al. (48) | 1992 | 68 | 59 | 1.6 | 32 | N/A | |||
| Caplan et al. (40) | 1994 | 26 | 66 | 1.9 | NR | N/A | |||
| Osella et al. (49) | 1994 | 45 | 58 | 1.4 | 30 | N/A | |||
| Seppel and Schlaghecke (50) | 1994 | 52 | 56 | 1.7 | 30 | N/A | |||
| Ambrosi et al. (51) | 1995 | 32 | 55 | 2.5 | 27 | 27 | 22 | 5 | 5 |
| Bencsik et al. (52) | 1995 | 63 | 27—85 | 1.1 | 14—25 | N/A | |||
| Flecchia et al. (53) | 1995 | 32 | 57 | 1.3 | 37 | N/A | |||
| Bardet et al. (54) | 1996 | 35 | N/A | N/A | 26 | 35 | N/A | N/A | 0 |
| Linos et al. (55) | 1996 | 57 | 49 | 1.3 | 59 | N/A | |||
| Bastounis et al. (56) | 1997 | 86 | 61 | 1.5 | 41 | 81 | 45 | 36 | 5 |
| Bondanelli et al. (57) | 1997 | 38 | 58 | 1.4 | 26 | 28 | 16 | 12 | 10 |
| Kasperlik-Zeluska et al. (58) | 1997 | 208 | 52 | 2.5 | 8—210 | 172 | 106 | 66 | 36 |
| Terzolo et al. (59) | 1995 | 45 | 55 | 1.4 | 31 | N/A | |||
| Proye et al. (60) | 1998 | 103 | N/A | N/A | N/A | N/A | |||
| Murai et al. (61) | 1999 | 59 | N/A | N/A | N/A | N/A | |||
| Tütüncü and Gedik (62) | 1999 | 33 | 51 | 1.2 | 51 | N/A | |||
| Favia et al. (63) | 2000 | 158 | 58 | 1.2 | 44 | 158 | 74 | 84 | 0 |
| Mantero and Arnaldi (64) | 2000 | 208 | N/A | N/A | N/A | N/A | |||
| Rossi et al. (65) | 2000 | 50 | 54 | 1.7 | 33 | 47 | 28 | 19 | 3 |
| Mantero et al. (66) | 2000 | 1004 | 58 | 1.4 | 30 | 903 | 596 | 307 | 101 |
| Tanabe et al. (67) | 2001 | 38 | N/A | N/A | N/A | N/A | |||
| Barzon et al. (68) | 2002 | 284 | 56 | 1.5 | 36 | N/A | |||
| Bülow and Ahrén (84) | 2002 | 381 | 64 | 1.3 | 30 | 359 | N/A | N/A | 22 |
| Tsvetov et al. (69) | 2007 | 100 | 62 | 0.9 | 24 | 77 | 34 | 43 | 23 |
| Bhargav et al. (70) | 2008 | 53 | 41 | 1.1 | 78 | 51 | 30 | 21 | 2 |
| Kasperlik-Załuska et al. (71) | 2008 | 1444 | 10—87 | 2.7 | 10—230 | 1175 | 709 | 466 | 269 |
| Song et al. (42) | 2008 | 3307 | 64 | N/A | 20 | N/A | |||
| Vassilatou et al. (72) | 2009 | 77 | 57 | 2.5 | 25 | 59 | 22 | 37 | 17 |
| Comlekci et al. (73) | 2010 | 376 | 55 | 2.3 | 25 | 313 | N/A | N/A | 54 |
| Anagnostis et al. (74) | 2010 | 64 | 62 | 1.9 | N/A | N/A | |||
| Giordano et al. (75) | 2010 | 118 | 62 | 1.5 | 22 | 102 | 57 | 45 | 16 |
| Yener et al. (76) | 2010 | 317 | 55 | 2.7 | 24 | 362 | 190 | 172 | 45 |
| Muth et al. (77) | 2011 | 226 | 67 | 1 | 24.1 | N/A | |||
| Cho et al. (78) | 2013 | 282 | 57 | 0.7 | 23 | 261 | 103 | 158 | 21 |
| Di Dalmazi et al. (79) | 2014 | 129 | 61 | 1.5 | 21 (max) | 92 | N/A | N/A | 22 |
| Hong et al. (80) | 2017 | 1149 | 54 | 0.8 | 18 | N/A | |||
| Ahn et al. (81) | 2018 | 1005 | 44 | 0.7 | 17 | 902 | 308 | 594 | 103 |
| Akkuş et al. (82) | 2018 | 229 | 52 | 1.7 | 48 | 202 | N/A | N/A | 27 |
| Goh et al. (83) | 2018 | 228 | 61 | 1.5 | 18 | 196 | 70 | 126 | 32 |
| Median value for all studies | 64 | 57.5 | — | 30 | — | — | — | — |
Abbreviation: N/A, data not available.
A recent large prospective Korean study, the COAR (the Co-work Of Adrenal Research) (81), investigated the characteristics of 1005 Korean patients with AIs and compared them with those of the largest previous retrospective study conducted in a Study Group on Adrenal Tumors of the Italian Society of Endocrinology cohort (66). The results showed some discordance between the patient cohorts. AIs in Korean patients were more frequent in men (57%) and the population was younger (median 55 years) than the Italian patient cohort. Also, fewer AIs underwent surgical resection in the Korean study. These differences likely reflect the different time period of the studies: the patients of the Italian study were recruited from 1980 to 1995, while those of the COAR were recruited from 2011 to 2014. The fact that fewer patients in the COAR study underwent adrenalectomy may be due to smaller adenoma size at discovery, an increase in the detailed characterization of AIs using improved imaging techniques (discussed in “Imaging Evaluation of an AI”), and endocrinological assessment (discussed in “Endocrine Work-up of AI”) leading to more reassurance regarding their benign nature. There has also been an increase in our knowledge concerning the natural history of untreated adrenal lesions and the recent development of international evidence-based management guidelines reflect this (4,6).
Size and lateralization of AI.
A large number of clinical studies have investigated the characteristics of AIs (Table 3 (39, 40,42,46-84)). The mean diameter of AI discovered by CT scan is 30 mm, ranging from 8 to 230 mm (Table 3 (39,40,42,46-84)) (the 8-mm lesions reflect the results of older studies before adopting 1 cm as the threshold for the definition of an AI). Many studies are limited by their retrospective nature, specialized center bias, patient selection bias, recall bias, and small sample size. However, it should be noted that all studies consistently report a higher incidence of ACC if the adrenal mass is greater than 4 cm in size (39,49,63,66,71).
The development of new CT protocols has improved the detection and characterization of adrenal masses (87). A similar distribution of lesions in the right and left adrenal gland has been reported in many CT series, in keeping with autopsy studies (Table 3). However, some studies suggest a higher prevalence of left-sided adrenal tumors detected on imaging (81,88,89), for example, the COAR study cohort described above (81). This observation may reflect a detection bias as left-sided adrenal tumors may be more readily apparent to the radiologist. Similarly, a recent large cross-sectional study of abdominal CT and MRI imaging in 1376 patients (90) reported a higher detection of left-sided adenomas than right-sided adenomas in each size category except when the tumor size was ≥30 mm. The authors concluded that this detection bias may result in under-recognition of small (<30 mm) right-sided lesions and bilateral disease (90).
Anatomy and Physiology of the Adrenal Gland
Anatomy of the adrenal gland
A brief overview of adrenal embryology, anatomy, physiology, and pathology is required to appreciate the clinical significance of AIs as it relates to the investigation and treatment of these lesions.
Historical perspective
The anatomy of the adrenal gland was first described by Bartholomeo Eustacius in 1563 and its functional importance subsequently elucidated by the pioneering work of Thomas Addison in 1855 (91). Shortly after Addison’s work, Brown-Séquard performed a series of bilateral adrenalectomies in several species of small animals and demonstrated that the adrenal glands are essential for life (92). Improvement in microscopy techniques in the nineteenth century helped describe the anatomy of the adrenals (Kölliker 1852), and the distinction between “cortical and medullary substances” (93).
Embryology and development
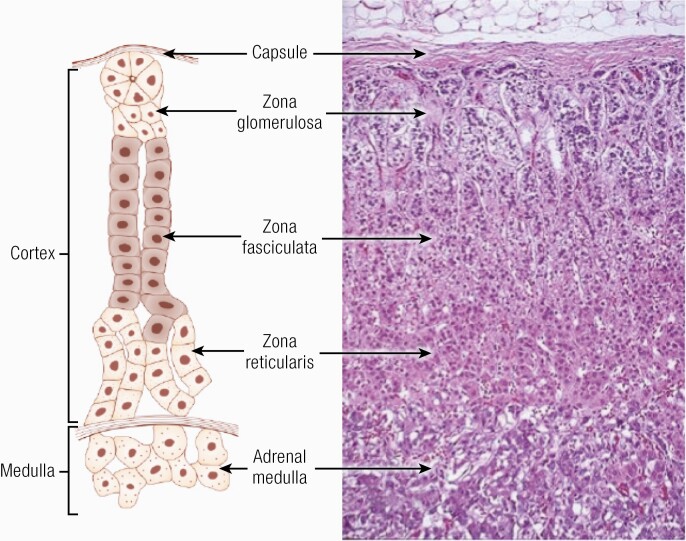
The adrenal gland is derived from 2 embryologically distinct origins with the adrenal cortex arising from the coelomic mesoderm of the urogenital ridge and the medulla from the neuroectoderm (neural crest cells) (92). The fetal adrenal gland is evident from 6 to 8 weeks of gestation and rapidly increases in size so that by midgestation it is larger than its adjacent kidney. In later stages of embryonic development, the cortex engulfs and eventually encapsulates the entire medulla. The adrenal cortex differentiates fully into its 3 constitutive zones (zona glomerulosa, zona fasciculata, and zona reticularis) by 3 years of age (94, 95) (Fig. 1).
Figure 1.
Schematic diagram of the structure of the human adrenal cortex (92). Adapted from PM Stewart, Chapter 14 The Adrenal Cortex. In Williams Textbook of Endocrinology, 10th ed. , Copyright © 2003 Elsevier Reproduced from Williams RH, Larsen PR. Williams Textbook of Endocrinology. 10th ed./ P. Reed Larsen….[et al.] ed. United States: Philadelphia : Saunders, ©2003. Copyright © 2003 Elsevier.
The development of the adrenal cortex is dependent on the blood supply, paracrine adrenal factors, hormonal factors, and adrenocortical innervation (96). The nuclear receptor steroidogenic factor-1 (SF1 also known as NR5A1) is a pivotal factor for the initiation and fetal maturation of the adrenal cortex (97), with its absence resulting in adrenal aplasia (98). An interplay between the transcription factors SF1 and an SF1 target gene, DAX 1, determines the extent to which steroidogenic enzymes are induced, and adrenocortical cells become differentiated (97). While adrenocortical growth and differentiation are independent of adrenocorticotropin (ACTH) during the first trimester of pregnancy, ACTH begins to play an essential role in the morphological and functional development of the adrenal gland after 15 weeks of gestation.
Structure, vasculature, and innervation of the adrenal gland
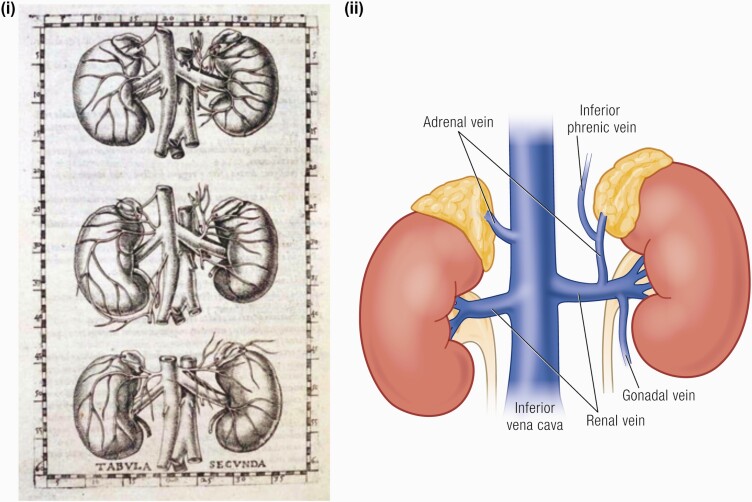
The adult adrenal gland is a pyramidal structure weighing approximately 4 grams, and is approximately 2 cm wide, 5 cm long, and 1 cm thick. It lies immediately above the kidney on its posteromedial surface (96). Although the left and right adrenal glands are symmetrical, the left gland is in a more caudal position, lying anteromedially to the left renal upper pole, laterally to the aorta and left diaphragmatic crus, and superior to the left renal vein (Fig. 2).
Figure 2.
Anatomy of the adrenal gland. (i) Eustachio’s original drawing from Tabulae anatomicae published by Johannes Maria Lancisi in 1714 (99). (ii) The left adrenal–renal venous complex. The right adrenal vein (AV) drains directly into the IVC (100).
Beneath the adrenal capsule, the zona glomerulosa, constitutes approximately 15% of the mass of the cortex (depending upon salt intake), (Fig. 1 (92)). The zona fasciculata constitutes 75% of the cortex comprising lipid-laden cells that are larger than those in the zona glomerulosa, organized into bundles, leading to the origin of its name “fascicles.” The innermost layer of the adrenal cortex is the zona reticularis comprising irregular cells arranged as cords with little lipid content (92).
Though small, the adrenal glands have an extensive vasculature. This may account for the predilection of cancer metastases to the adrenal gland (101) and also for its susceptibility to nontraumatic adrenal hemorrhage (102). Three arteries supply each adrenal gland: the superior suprarenal artery from the inferior phrenic artery, the middle suprarenal artery directly from the abdominal aorta, and the inferior suprarenal artery from the renal artery. Blood is channeled into the subcapsular arteriolar plexus and subsequently distributed to the sinusoids, which in turn supply the adrenal cortex and medulla (96, 103) (Fig. 2). There are numerous variations of the venous drainage of the adrenal gland based on the adrenal and renal vein configurations and combinations, which have been extensively reviewed by Cesmebasi et al. (100). These variations are important both for the surgical management of adrenal lesions but also for diagnostic adrenal vein sampling (100).
Physiology of the adrenal gland
Functional zonation of the adrenal cortex.
Aldosterone is the primary mineralocorticoid produced by the zona glomerulosa cells under the control of angiotensin II and extracellular potassium. The daily production rate of aldosterone varies between 80 and 200 μg/day (104), depending on daily salt intake. Aldosterone functions as the ligand for the mineralocorticoid receptor in target tissues that include the colon, salivary gland, and the renal distal convoluted tubule and collecting ducts, where it causes increased reabsorption of sodium and increased excretion of both potassium (by principal cells) and hydrogen ions (by intercalated cells of the collecting duct). Aldosterone secretion is confined to the outer zona glomerulosa due to the restricted expression of CYP11B2.
Glucocorticoids are secreted in relatively high amounts (cortisol 10-20 mg/day) from the zona fasciculata cells under the control of ACTH secreted from the anterior pituitary (92). In humans, cortisol is the main glucocorticoid produced by the adrenal cortex under normal conditions and its actions include mobilization of fats, proteins, and carbohydrates. Once produced and released into the bloodstream, glucocorticoids facilitate the release of energy stores for utilization during stress. Integral to the feedback control of the activated hypothalamic–pituitary–adrenal (HPA) axis, glucocorticoids inhibit the production and secretion of both corticotropin-releasing hormone (CRH) and ACTH from the HPA axis. As a class, adrenal androgens (dehydroepiandrosterone [DHEA], DHEA sulfate [DHEAS], and androstenedione) are the most abundant steroids secreted from the adult adrenal gland (>20 mg/day). DHEA is sulfated only in the zona reticularis to form DHEAS.
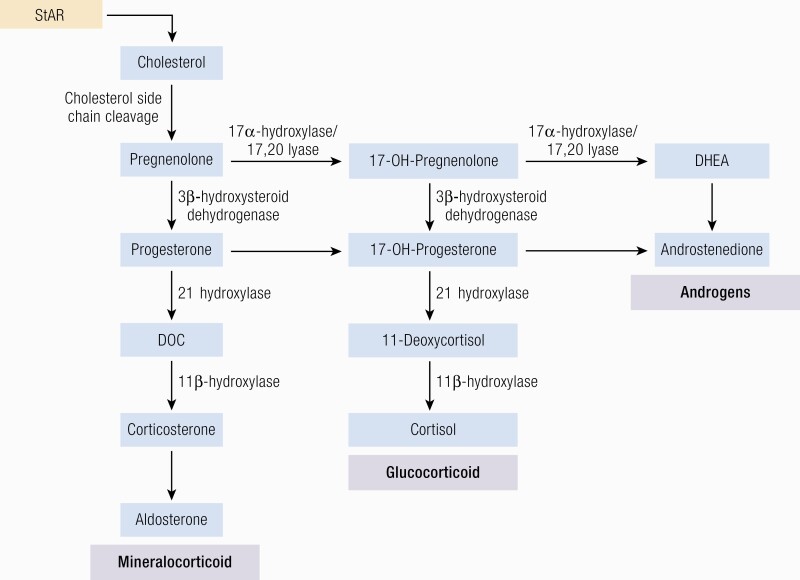
Steroidogenesis.
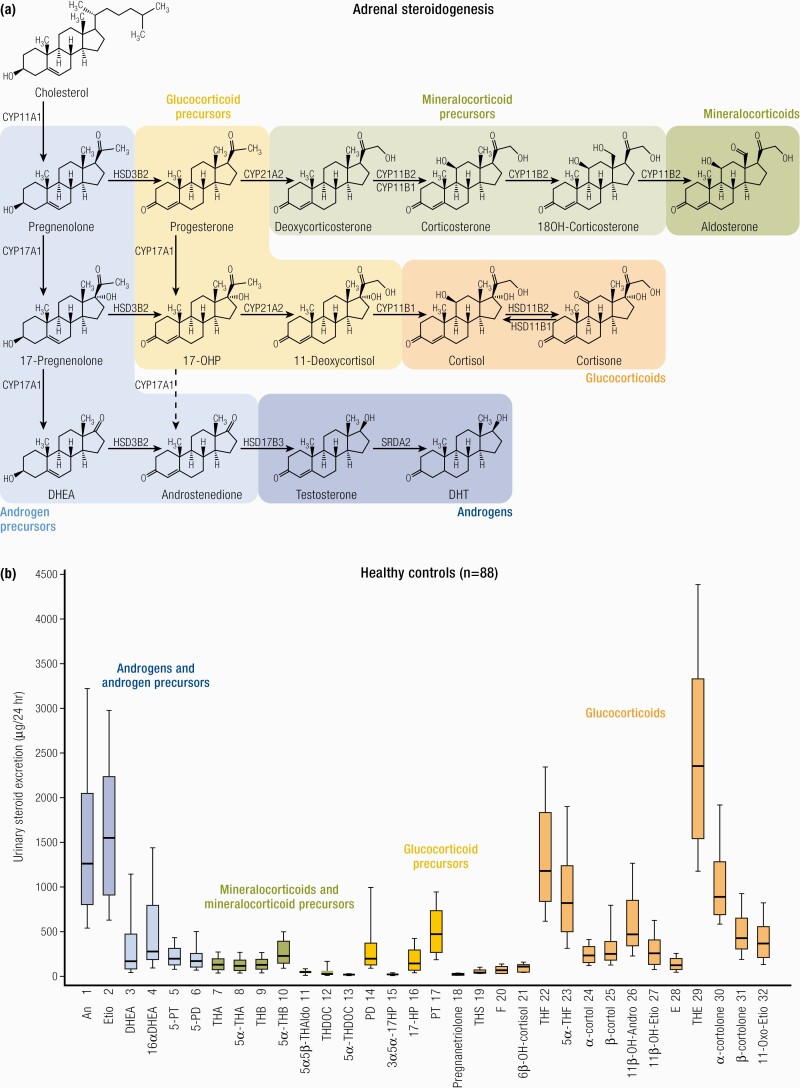
Three main subclasses of steroid hormones are produced by the adrenal cortex: glucocorticoids (cortisol, corticosterone), mineralocorticoids (aldosterone, deoxycorticosterone [DOC]), and adrenal androgen and their precursors [mainly DHEA, DHEAS, and androstenedione]. Steroid hormones regulate a wide variety of developmental and physiological processes from fetal life to adulthood. Steroid hormones are all synthesized from cholesterol and hence have closely related structures based on the classic cyclopentanophenanthrene 4-ring structure. The physiology of human steroidogenesis has been extensively described previously by Miller et al. (105) and the biochemical pathways involved in adrenal steroidogenesis are shown in Fig. 3, to highlight their increasing importance in clinical practice as a diagnostic tool (discussed in “The Future: Investigation and Management”). As depicted, steroidogenesis involves the collaborative action of a series of enzymes including cytochrome P450 enzymes following the transport of intracellular cholesterol into the adrenal cortex under stimulation from ACTH (92,106).
Figure 3.
Adrenal steroidogenesis. After the steroidogenic acute regulatory (StAR) protein-mediated uptake of cholesterol into mitochondria within adrenocortical cells, aldosterone, cortisol, and adrenal androgens are synthesized through the coordinated action of a series of steroidogenic enzymes in a zone-specific fashion. A'dione, androstenedione; DHEA, dehydroepiandrosterone; DOC, deoxycorticosterone.
PM Stewart, Chapter 14 The Adrenal Cortex. In Williams Textbook of Endocrinology, 10th ed. , Copyright © 2003 Elsevier Reproduced from van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. Eur J Endocrinol 2014; 170:R109-119.
Importantly, the functional zonation of the adrenal cortex is dependent upon the zonal expression of 2 key enzymes: the final step in cortisol biosynthesis involves the conversion of 11-deoxycortisol to cortisol by the enzyme 11β-hydroxylase (CYP11B1), largely in the zona fasciculata. By contrast in the zona glomerulosa (although 11 β -hydroxylase may also convert deoxycorticosterone to corticosterone) it is the enzyme CYP11B2 or aldosterone synthase that is uniquely required for the conversion of corticosterone to aldosterone through the intermediate 18-OH corticosterone.
Physiology of the adrenal medulla.
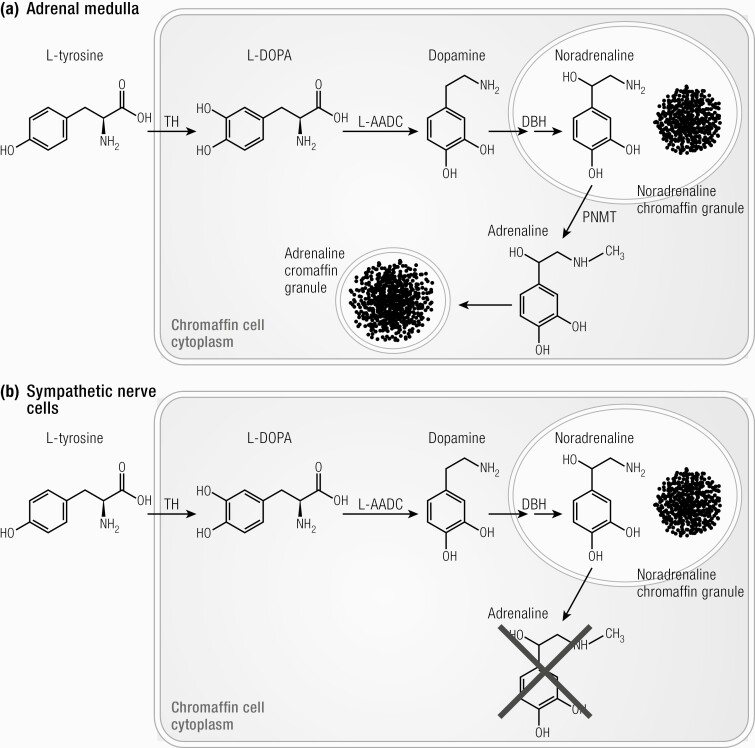
Understanding the biosynthesis pathways, metabolism, and breakdown of catecholamines is crucial to understanding the biochemical assessment of pheochromocytomas and paragangliomas (107, 108). Briefly, the biosynthesis of catecholamines starts with the conversion of amino acid L-tyrosine to L-3,4-dihydroxyphenylalanine (L-DOPA) by the enzyme tyrosine hydroxylase (TH). L-DOPA is converted to dopamine which is translocated to catecholamine storage vesicles of chromaffin cells of the adrenal medulla, sympathetic nerves, and paraganglia (Fig. 4 (108)). The enzyme dopamine- β hydroxylase is responsible for the conversion of dopamine into norepinephrine (noradrenaline). In adrenal medullary chromaffin cells, norepinephrine (noradrenaline) is further converted to epinephrine (adrenaline) by phenylethanolamine N-methyltransferase (Fig. 4 (108)). As this enzyme is only present in these cells, epinephrine (adrenaline) is almost exclusively produced within the adrenal medulla (108).
Figure 4.
Biosynthesis of catecholamines in (A) chromaffin cells of adrenal medulla and (B) sympathetic nerve cells. TH, tyrosine hydroxylase; L-AADC, aromatic L-amino-acid decarboxylase; DBH, dopamine- β -hydroxylase; PNMT, phenylethanolamine-N-methyltransferase (108). Reproduced from van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. Eur J Endocrinol 2014; 170:R109-119.
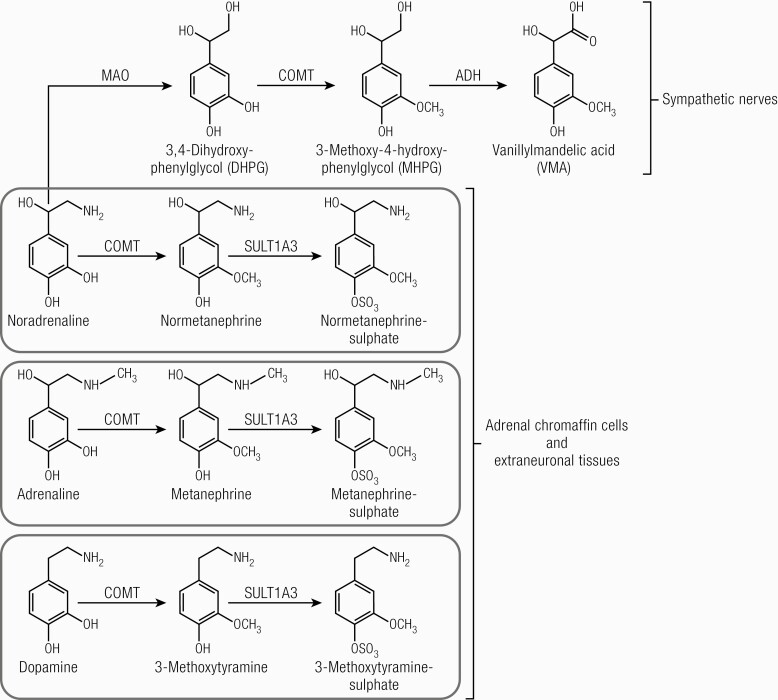
Catecholamines are metabolized through several pathways, resulting in numerous metabolites (Fig. 5)). The majority of circulating norepinephrine (noradrenaline) is derived from noradrenergic neurons of the central and sympathetic nervous system (108). Deamination of neuronal norepinephrine (noradrenaline) to 3,4-dihydroxyphenylglycol occurs by monoamine oxidase. Norepinephrine (noradrenaline) is also partially metabolized in extraneuronal tissues and adrenal chromaffin cells, where it is converted to normetanephrine by catechol-O-methyltransferase (COMT) (108). Epinephrine (adrenaline) is mainly metabolized within adrenal chromaffin cells by COMT, resulting in the O-methylated metabolite metanephrine. Metabolism of dopamine follows other pathways, resulting in the production of the O-methylated metabolite methoxytyramine. Plasma free metanephrines are conjugated to sulfates by gut wall enzymes (108).
Figure 5.
Metabolism of catecholamines. ADH, alcohol dehydrogenase; MAO, monoamine oxidase; COMT, catechol-O-methyltransferase; SULT1A3, sulfotransferase 1 A3. Adrenaline, epinephrine; noradrenaline, norepinephrine. (108). Reproduced from van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: Biochemical diagnosis of phaeochromocytoma and paraganglioma. Eur J Endocrinol 2014; 170:R109-119.
In patients with pheochromocytomas/paragangliomas, more than 90% of catecholamine catabolism occurs continuously within the tumor itself, mostly through the action of COMT (107). Elevated circulating levels of O-methylated metabolites, therefore, point to the presence of pheochromocytoma or paraganglioma with greater sensitivity and specificity than elevated levels of the parent amines. Elevation in amines may result from increased sympathetic nervous system activity or originate from other sources (107).
Histology of adrenal tumors
This has been extensively reviewed by Erickson et al. (109). In brief, there are several methods for immunophenotyping adrenal tissue and tumors. Both adrenocortical tumors and pheochromocytomas stain positive for synaptophysin but adrenocortical tumors are negative for chromogranin (109). S100 protein usually highlights sustentacular cells in pheochromocytomas and is negative in adrenocortical tumors. Adrenocortical tumors are also usually (but not always) positive (and pheochromocytomas negative) for Cytokeratin CAM 5.2, α-inhibin and calretinin. Steroidogenic factor 1 is increasingly recognized as a key marker of adrenocortical cell lesions (109).
Both adrenocortical cancers and melanomas stain positive for Melan A, but adrenocortical tumors are negative for S100 (a positive marker for melanoma). Additional markers may be required to exclude other primary lesions, for example, thyroid transcription factor 1 and cytokeratin.
Differentiation of adrenocortical adenoma and carcinoma.
Although there are several clinical, endocrinological and radiological features that help risk stratify an adrenal lesion with regard to the likelihood of ACC (see “Etiology and clinical presentation of AI”), the final diagnosis is a histological one and requires the input of an experienced adrenal pathologist (110). The most widely used histological scoring system is the Weiss score (Table 4) based on 9 histological parameters (scored as 0 if absent and 1 if present) (110,111).
Table 4.
Summary of Weiss score criteria.
| Criteria | Scoring points | |
|---|---|---|
| 0 | 1 | |
| Nuclear grade (Fuhrmann nuclear grade system) | I/II | III/IV |
| Mitoses | <6/10 HPF | ≥6/10 HPF |
| Atypical mitoses | − | + |
| Clear cell component | <25% | ≥25% |
| Diffuse architecture | <1/3 | ≥1/3 |
| Confluent necrosis | − | + |
| Venous invasion | − | + |
| Sinusoidal invasion | − | + |
| Capsular infiltration | − | + |
Adapted from references (111-113).
Abbreviation: HPF, high power fields.
A threshold above a Weiss score of 3 (also on the modified score) was associated with an increased risk of malignant behavior (112). In the initial study by Weiss, the features with the strongest association to outcome were the mitotic rate >5/50 high powered field, atypical mitoses, and venous invasion (111) and in the second study by Weiss in 1989 the strongest association with patient outcome was the mitotic rate (112).
Another key predictor of malignant behavior is the Ki67 proliferative index (114). The cutoff at which a Ki67 labeling index confirms the diagnosis of ACC and predicts aggressive disease is debated and ranges from >2.5% to >7% (113,115-117). However, because of the enormous intratumoral heterogeneity of ACC, the site in which the Ki67 labeling index is obtained markedly influences the results. In particular, the question of whether the Ki67 labeling index should be calculated as the average of the entire tumor specimen or the summation of hot spots in the specimens has not been resolved (113). This limitation should be kept in mind when applying the Ki67 labeling index to categorizing and adrenal lesion and as a prognostic marker for ACC (113). The Helsinki score used in some centers incorporates the Ki67 labeling index and has been proposed to be a better predictor of outcome (118).
Pheochromocytoma of the Adrenal Gland Scaled Score and Grading of Adrenal Pheochromocytoma and Paraganglioma tool.
In 2002 Thompson described a tool, Pheochromocytoma of the Adrenal gland Scaled Score (PASS), based on the presence or absence of 12 specific histological features to allow better distinction between benign and malignant tumors (119). The histological features include vascular/capsular/periadrenal adipose tissue invasion, large nests or diffuse growth, focal or confluent necrosis, high cellularity, tumor cell spindling, cellular monotony, increased mitotic figures (>3/10 high power fields), atypical mitotic figures, nuclear pleomorphism, and hyperchromasia with weighted scores between 1 and 2. Tumors with a PASS score >4 were defined as having malignant potential, whereas those with a lower score were considered benign. Subsequent validation by a panel of experienced pathologists concluded that due to significant inter- and intraobserver variation PASS was not recommended for clinical prognostication (120).
Subsequently, Kimura et al. (121) developed a less involved scoring system for prediction of metastases, Grading of Adrenal Pheochromocytoma and Paraganglioma (GAPP) consisting of a smaller number of pathological parameters with weighted scoring (1 or 2 points) including histological pattern; cellularity; comedo necrosis; capsular/vascular invasion; Ki67 proliferative index; and catecholamine phenotype. A GAPP score of 0 to 2 is considered low risk, 3 to 6 intermediate risk, and 7 to 10 high risk. GAPP scoring was independently validated by Koh et al. and is considered a useful risk stratification tool for the prediction of metastatic potential (122).
Etiology and Clinical Presentation of AI
Many AIs, while picked up incidentally, may have clinical symptoms or associated signs on closer questioning and clinical examination. The etiology of an AI is variable and includes tumors from the adrenal cortex, the adrenal medulla, and metastatic deposits.
Etiology: tumors of the adrenal cortex
Adrenocortical adenoma.
An ACA is a benign neoplasm of adrenocortical cells. The majority of these lesions are nonsecretory; however, some may produce glucocorticoids independent of ACTH and mineralocorticoids independent of stimulation from the renin–angiotensin system. Rarely, they may also produce androgens or estrogens which may result in virilization or feminization. The 3′,5′-cyclic adenosine 5′-monohosphate–protein kinase A (cAMP–PKA) pathway is important for the regulation of adrenocortical cell development. ACTH binds to the ACTH receptor (a G-protein coupled receptor encoded for by the MCR2 gene) in the adrenocortical cell, thereby activating adenylyl cyclase, cAMP synthesis and activation of PKA. Abnormally increased cAMP–PKA signaling is thought to be the key mechanism in the development of most benign adrenocortical tumors (123).
Cortisol-producing adenoma.
Autonomous cortisol secretion (ACS) (of variable clinical significance and severity) is frequently found in patients with an ACA. The majority of these cases are due to non-ACTH-dependent ACS from the adenoma. However, aberrant expression and activation of G-protein coupled receptors have been implicated as a possible mechanism explaining cortisol hypersecretion (and in primary hyperaldosteronism) (124, 125).
ACC, adrenal lymphoma, and adrenal metastases.
Adrenocortical carcinoma.
Primary ACC is rare, with an estimated population incidence of 1 to 2 per million per year (126,127). Between 40% and 60% of ACCs are functional and may present with symptoms of hormonal hypersecretion (126,127,128,129), most commonly with Cushing’s syndrome (estimated 45%). Approximately 25% of ACCs will cosecrete glucocorticoids and androgens. Solely androgen-secreting ACCs are less common (approximately 10%), usually presenting with virilization without features of glucocorticoid excess. Feminization and hyperaldosteronism are rare occurring in <10% of cases (127,130). Importantly, if there is evidence of hypersecretion from 2 adrenal zones this is highly suggestive of an ACC as benign lesions do not secrete in this pattern.
Approximately 30% of ACCs present with symptoms of local mass effect, such as abdominal or flank pain. As ACCs are retroperitoneal they may present late and have often reached a large size (131).
The impact of the functional status and clinical features of ACCs on survival is unclear (132,133). However, cortisol hypersecretion leading to clinically evident Cushing’s syndrome is recognized as a significant cause of morbidity and mortality (134,135) due to increased risk of infection, metabolic, bone, and vascular complications (136).
Malignancy is also suspected based on imaging characteristics of the adrenal mass and size. The size of the adrenal mass is predictive (but not 100%) of malignancy. In an Italian study of 887 patients with AIs, 90% of ACCs had a diameter of greater than 4 cm at presentation, with a 4-cm cut-off having a 93% sensitivity for detecting ACC (64). Size at presentation may also impact prognosis from ACC, with a smaller size of tumor at diagnosis associated with a significantly higher 5-year survival (137). Imaging characteristics of adrenal lesions will be discussed in detail in “Imaging evaluation of an AI.”
Mutations in β -catenin (CTNNB1) leading to constitutive activation of the Wnt signaling pathway is a frequent finding in benign and malignant adrenocortical tumors (138). The Wnt signaling pathway is thought to be important in the embryonic development of the adrenal gland (139). Constitutive activation of this pathway is also implicated in cancer development in several other organs (140). In 1 study of 100 adrenal adenomas that had been surgically excised, 36% were found to contain CTNNB1 mutations (141). Somatic activating mutations of GNAS, which encodes the α-subunit of the stimulatory G protein (GSα), occur in 5% to 17% of adrenal adenomas which are cortisol secreting (142,143). An example of this is constitutive activation of adenylyl cyclase as a result of somatic GNAS mutations in McCune–Albright syndrome (144).
Inactivating mutations in PRKAR1A have been described in cortisol-producing adrenal tumors. PRKAR1A gene encodes for a regulatory subunit of PKA, and inactivating mutations lead to constitutive activation of the cAMP–PKA pathway. Although mutations in this gene were first described in Carney complex (145), somatic mutations of PRKAR1A have been described in some sporadic adrenocortical tumors (146).
Somatic activating mutations of protein kinase A catalytic subunit (PRKACA) has been implicated in up to 50% of patients with adenomas with clinical Cushing’s syndrome, but not in adenomas producing less cortisol (138,142,147). Mutations in PRKACA may be associated with smaller adenomas but higher levels of cortisol production than adenomas where this mutation is not present (143,148). The lower frequency of these mutations in adenomas which produce less cortisol may be an explanation for the lack of progression in these patients to a clinically apparent Cushing’s syndrome.
Mutations in cyclic nucleotide phosphodiesterase have also been noted in cortisol-producing ACAs. These are enzymes that breakdown cyclic nucleotides and as a consequence regulate cAMP levels and cAMP–PKA pathway activity. Mutations in PDE11A and PDE8B genes are the most commonly reported (149,150).
Aldosterone-producing adenoma.
Mutations in KCNJ5 (potassium channel) have been documented in patients with aldosterone-producing adenomas in approximately 40% of patients (151) from European cohorts, though much higher rates are reported in patients from Japan and Asia (152,153). These mutations lead to increased sodium conductance and cellular depolarization leading to calcium influx, increased intracellular calcium signaling, and increased CYP11B2 mRNA expression with increased aldosterone production and glomerulosa cell proliferation (123). Adenomas with KCNJ5 mutations tend to be larger than those which do not carry the mutation and appear to be more common in women than men (154).
Other somatic mutations in several of the genes involved in the regulation of aldosterone production have also been identified (155). In aldosterone-producing adenomas that did not have KCNJ5 mutations, abnormalities in ATP1A1 (encoding a Na+/K+ ATPase α subunit) were found in 5.2% and of ATP2B3 (encoding a Ca2+ ATPase) in 1.6%, with these mutations associated with increased plasma aldosterone concentrations and lower potassium concentrations than cases without the mutation (156). Additionally, mutations in the CACNA1D gene have been identified and recently gain of function mutations in the CLCN2 chloride channel gene (157) has also been described. This gene encodes a voltage-gated calcium channel and 11% of aldosterone-producing adenomas without mutations in KCNJ5 have been reported to carry mutations in this gene (158). Mutations in KCNJ5, CACNA1H, ATP1A1, ATP2B3, and CACNA1D account for approximately 50% of aldosterone-producing adrenal adenomas (159) in patients from Europe; this is likely to be higher in Asian patients.
Adrenocortical carcinoma.
ACC is rare and aggressive and can occur at any age. However, peak incidence tends to be before the age of 5 and between the ages of 40 and 60 years of age (126,127). Most cases of ACC are sporadic but some are known to occur with other tumor syndromes (160). The most well known of these are Li–Fraumeni syndrome (TP53 gene), Multiple Endocrine Neoplasia type I (MEN1 gene) and Beckwith–Weidemann syndrome (abnormalities in 11p15I gene). The genetic mutations in these syndromes are well characterized. ACCs have also been noted in familial adenomatous polyposis (FAP gene), neurofibromatosis type 1 (NF1 gene), and Carney complex (PRKAR1A gene) (161).
In contrast, the genetic basis for sporadic ACCs is less clear. Loss of heterozygosity of chromosome 17p13, which codes for the tumor suppressor gene TP53, is a common finding in sporadic ACCs (162). However, only one-third of these ACCs have a mutation of TP53 (163). As previously described, mutations in CTNNB1 are also present in ACCs and may be associated with poor outcome (164). ZNRF3 is thought to be a tumor suppressor gene related to the β -catenin pathway, encoding a cell surface E3 ubiquitin ligase. Mutations in this gene were identified in 21% of 123 ACCs following genomic characterization (165).
Loss of heterozygosity at the 11p15 locus can lead to insulin-like growth factor-2 overexpression which is associated with malignant ACCs (166,167). Pan-genomic characterization of ACCs has identified several other driver genes including CDKN2A, RB1, DAXX, TERT, MED12, PRKAR1A, RPL22, TERF2, CCNE1, and NF-1 (165,168).
Bilateral adrenocortical tumors.
Although the majority of AIs are unilateral, bilateral AIs may be found in 10% to 15% of cases (169). Two large studies (169,170) found that the most common causes of bilateral AI were metastasis, primary bilateral macronodular adrenal hyperplasia (PBMAH), and bilateral cortical adenomas. Other causes of bilateral AI include bilateral pheochromocytomas, congenital adrenal hyperplasia (CAH), Cushing’s disease, or ectopic ACTH secretion with secondary bilateral adrenal hyperplasia.
Bilateral adrenal hyperplasia is characterized by a nodule diameter of less than 1 cm (micronodular) and greater than 1 cm (macronodular). Primary pigmented nodular adrenocortical disease is characterized by multiple pigmented micronodules and does not usually present as an AI, and therefore will not be discussed further in this review.
PBMAH presents on imaging with characteristic multiple bilateral macronodules. Whole-genome sequencing, along with single nucleotide polymorphism array analyses, identified recurrent mutations in an armadillo repeat containing 5 (ARMC5) gene, located in chromosome 16p, in 50% of BMAH patients who underwent surgery (171). Patients with ARMC5 mutations tend to display adrenal hyperplasia associated with multiple nodules (172-175). Discovering ARMC5 mutations was the first evidence of BMAH as a genetic disease. ARMC5 is a putative tumor suppressor, with 2 hits in each adrenal nodule: a first germline alteration, found in leukocyte DNA and common to all nodules, and a second somatic hit (171). The penetrance of ARMC5 mutations is variable (172). ARMC5 overexpression induces apoptosis in vitro and its inactivation decreases steroidogenesis (171). The pathophysiology of BMAH is discussed further in “Bilateral AI and ACS.”
Etiology: tumors of the adrenal medulla
Tumors that originate from the chromaffin cells of the adrenal medulla, which secrete catecholamines, are termed pheochromocytomas. They may be benign or malignant. They can occur at any age, although are most common in the fourth to the fifth decade (176). The annual incidence of pheochromocytoma is estimated at 0.8 per 100 000 person-years (177). It is estimated 40% of catecholamine-secreting tumors are part of a hereditary syndrome and many endocrinologists are now offering genetic analysis to all affected cases. Von Hippel Lindau (VHL), multiple endocrine neoplasia (MEN) type 2, and NF1 are the most well known of these and all have an autosomal dominant inheritance.
Other mutations have been associated with sporadic pheochromocytoma clustering to 2 common pathways: hypoxic signaling and kinase signaling genes. Affected genes in cluster 1 (hypoxic pathway) include subunits of succinate dehydrogenase (SDHD, SDHC, SDHB, SDHA, SDHAF2), HIF-1alpha, EGLN1/2, and KIF1B in addition to VHL. Cluster 2 genes code for activating proteins in kinase signaling and include NF1, RET, MAX, and TNEM127. Cluster 2 gene mutations are more likely to result in adrenal pheochromocytomas, whereas those in Cluster 1 mostly result in extra-adrenal noradrenergic paragangliomas (except for mutations in VHL). Mutations in VHL, RET, NF1, SDHB, and SDHD account for 90% of all pheochromocytomas and paragangliomas (123).
Hereditary pheochromocytomas tend to be diagnosed at a younger age, because of routine biochemical screening or genetic testing and are also more likely to be bilateral. In contrast, sporadic pheochromocytomas may be discovered incidentally on adrenal imaging (178,179). SDHB (10.3%) and SDHD (8.9%) mutations are the most frequent germline mutations in pheochromocytoma and paragangliomas (180).
The relative production of plasma metanephrine compared with plasma normetanephrine and methoxytyramine may help distinguish the genetic etiology of pheochromocytoma. In 1 large study of patients with pheochromocytoma and/or paraganglioma, patients with NF1 and MEN2 mutations could be discriminated from those with VHL and SDH mutations in 99% of cases by the relative concentrations of normetanephrine and metanephrine, as all patients with NF1 and MEN2 presented with tumors characterized by increased plasma concentrations of metanephrine, in contrast to patients with VHL and SDH mutations, usually presenting with increases in normetanephrine or methoxytyramine. Additionally, measurements of plasma methoxytyramine discriminated patients with SDH mutations from those with VHL mutations in a further 78% of cases (181).
Clinical presentation of AI
By definition, an AI is discovered when imaging is performed for another indication without any obvious clinical features of adrenal disease. However, on closer history and examination following the discovery of the adrenal lesion, there may be features suggestive of adrenal disease. In cases where an adrenal mass is large (causing local pressure effect) or the tumor demonstrates clinically significant hormone hypersecretion, specific clinical features may be uncovered. However, it is important to note that even functional tumors may not result in significant clinical symptoms. Imaging characteristics cannot reliably distinguish between functional and nonfunctional tumors. As such, all patients with an AI should be systematically assessed for functional activity by endocrine biochemical testing, regardless of the presence or absence of symptoms (4).
Adrenal lymphoma.
Adrenal gland involvement is well recognized and seen in up to 25% of patients with non-Hodgkin lymphoma usually as part of disseminated disease (182). Conversely primary adrenal lymphoma is much rarer accounting for <1% of all cases of non-Hodgkin lymphoma (183). Primary adrenal lymphoma usually manifests as a large well-defined mass with homogeneous enhancement and may invade into surrounding structures and biopsy may be required to differentiate from other more common tumors (184).
Adrenal metastases.
A metastatic tumor is a common finding in the adrenal gland at postmortem and the predilection of the adrenal gland for metastatic deposits is thought to be due to its extensive sinusoidal blood supply (185). In one series of 464 patients with metastatic adrenal gland lesions, 90% were carcinomas, with the others being hematological, sarcomas, or melanomas. Of the carcinomas, the most common primary site in 35% of cases was lung, followed by gastrointestinal, kidney, and breast. Interestingly, bilateral adrenal involvement was noted in almost half the patients in this case series (186). Adrenal metastases occur late in the course of disseminated cancers, and the primary site is usually already known.
Rarely metastatic adrenal tumors may lead to adrenal insufficiency, particularly in the context of large bilateral adrenal lesions (187). Therefore, in these circumstances, patients may present with symptoms and signs of adrenal insufficiency (fatigue, anorexia nausea, vomiting, postural hypotension, hyponatremia, and hyperkalemia). However, some of these clinical features are often difficult to distinguish from those of progressive metastatic malignancy.
Functional AI.
Ten to 15% of AIs secrete hormones in excess (170). The clinical features ascribed to functional AI will be discussed in “Endocrine work-up of AI.”
Endocrine Work-up of AI
Clarification of the endocrine status of patients with AI is a cornerstone of management alongside the exclusion of malignancy. Clinical signs and symptoms of hormone excess and associated comorbidities together with a biochemical evaluation underpins personalized management. As a general principle, every patient with AI should be screened for adrenal catecholamine (although recent data has suggested this may not need to be the case in low Hounsfield unit lesions (188)) and glucocorticoid excess. Mineralocorticoid excess should be excluded in patients with hypertension and/or hypokalemia. Hirsutism or virilization or suspicion of an ACC should prompt measurement of androgens and gynecomastia estrogens.
Screening for pheochromocytoma
Pheochromocytoma may present incidentally, but on closer questioning, approximately 50% of cases have classical paroxysmal symptoms of sweating, headache, and tachycardia (189). Additionally, the diagnosis may be suspected if there is a family history of a heritable disorder commonly associated with pheochromocytoma as discussed in “Etiology and clinical presentation of AI.” Hypertension is a common sign of pheochromocytoma, but 5% to 15% of patients may have normal blood pressure at presentation, particularly in those with incidentaloma or having familial screening where the tumor may be smaller and less functionally active at presentation (190). Paradoxically, tumors that secrete only epinephrine may cause hypotension (191). Headache occurs in up to 90% of symptomatic patients (190) with sweating in 60% to 70%. Other symptoms include tremors, weakness, palpitations, anxiety, constipation, visual blurring, hyperglycemia, polyuria, and polydipsia (192).
Catecholamine-induced cardiomyopathy related to pheochromocytoma may present with signs of heart failure such as pulmonary edema (193). Rarely patients may also present with “pheochromocytoma crisis,” with hypertension or hypotension, multiorgan failure, psychiatric disorder, and hyperthermia (194).
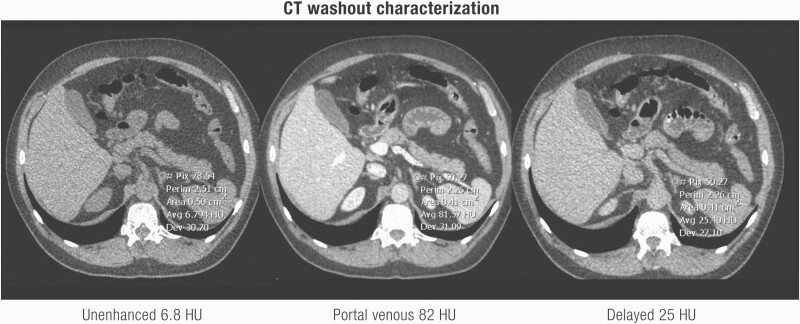
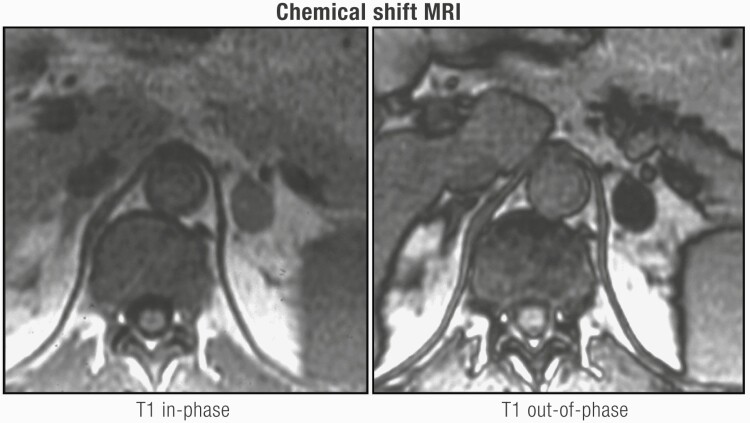
Patients with familial pheochromocytoma may be asymptomatic in 50% of cases, with only a third presenting with hypertension, possibly representing earlier diagnosis and smaller lesions as a result of regular screening in these patients (195,196). While evaluation for catecholamine excess is recommended by ESE/ENSAT guidelines in all AI patients (4), it may be possible to omit this in lipid-rich cortical adenomas. As discussed in detail in “Imaging evaluation of an AI,” an unenhanced/noncontrast CT is recommended as the first-line investigation to confirm if an AI is homogeneous and to calculate the attenuation value measured in Hounsfield units (HU). A HU ≤ 10 is consistent with a benign adrenal adenoma or other benign lesions (eg, myelolipomas, lipomas). Mean HU scores for pheochromocytoma are 30 to 35 (197) with only 0.5% of pheochromocytoma having an unenhanced CT attenuation of ≤10 HU (97,197,198). Buitenwerf et al. (197) reviewed the CT images of 222 histologically proven pheochromocytomas, yielding only a single tumor with an unenhanced attenuation of <10 HU. Canu et al. (188) identified 2 (0.5%) of 376 histologically proven pheochromocytomas with unenhanced CT attenuation value of exactly 10 HU, 99.5% (n = 374) had a HU > 10. Despite the inherent drawbacks of the retrospective study design which include variable radiological techniques and selection of the region of interest, unenhanced attenuation is a valuable tool to distinguish lipid poor adenomas from pheochromocytomas. Set against this are the inherent risks of a missed diagnosis and prolonged exposure to catecholamines and cardiovascular morbidity/mortality (199,200). Additional pointers for considering biochemical testing in a patient with an unenhanced CT attenuation of ≤10 HU for pheochromocytoma are elderly patients (4), heterogeneity, or evidence of tumor necrosis.
Biochemical testing for pheochromocytoma has an excellent negative predictive value of 0.99. As described above in “Anatomy and physiology of the adrenal gland,” measurement of the O-methylated metabolites of catecholamines is now the main focus for specific measurement in an era of advanced analytics employing liquid chromatography tandem mass spectrometry (LC-MS/MS) (201). Plasma free or 24-hour urine fractionated metanephrines are recommended as the screening test of choice for pheochromocytoma with a sensitivity of 90% to 95% (202, 203). Specificity rates of 85% to 89% decrease to 77% in elderly people and can be improved by using age-adjusted reference ranges (204-206). Similarly, false positives can occur with concomitant medications such as sympathomimetic drugs or interfering substances including caffeine; avoiding these for 24 hours before testing is recommended (108,207,208). For plasma free metanephrines, blood is drawn after resting in the supine position at least 30 minutes (209) into prechilled heparinized tubes (108, 210). For 24-hour urine estimation, the use of acidified containers (to achieve urine pH <4) and storage in a cold place is recommended; measurement of creatinine is often used to ensure adequate collection (108,202,211).
Screening for autonomous cortisol secretion
The clinical features of Cushing’s syndrome are well defined; while individual susceptibility varies, generally, these are dictated by the degree and duration of cortisol hypersecretion. In many cases of AI with documented autonomous cortisol hypersecretion (ACS), cortisol secretion rates may not be significantly elevated. As a result, the patient may be asymptomatic, have no clinical features and have few comorbidities that may be ascribed to cortisol hypersecretion.
With nonspecific and wide-ranging signs and symptoms, diagnosing cortisol excess in patients with AI, particularly at levels that may be only marginally above “normal,” is challenging. For patients with overt Cushing’s syndrome, the Endocrine Society recommends the use of 2 of 3 highly sensitive screening tests: 24-hour urine free cortisol (UFC) excretion, late-night salivary cortisol (LNSC) levels and 9 am plasma cortisol following an overnight dexamethasone suppression test (1-mg dexamethasone suppression test [DST]; or low-dose DST) (212). Different assays (radioimmunoassay (RIA), enzyme-linked immunosorbent assay, automated chemiluminescence, high-performance liquid chromatography or mass spectrometry), patient comorbidities causing physiological hypercortisolism, and pseudo-Cushing’s syndrome are all confounding factors in the assessment of cortisol excess in patients with AI (212-214).
ACS is defined as an alteration of the HPA axis characterized by ACTH independent cortisol excess often without clinical signs and symptoms of overt Cushing’s syndrome. Nomenclature around this term has caused confusion with multiple names being given to this phenomenon including “subclinical Cushing’s syndrome,” “subclinical hypercortisolism,” and “preclinical Cushing’s syndrome” have all been used. However, we suggest the universal adoption of the term “autonomous cortisol secretion” as proposed by ESE/ENSAT (4). Despite the absence of florid signs and symptoms, ACS in patients AI has been associated with hypertension (215), insulin resistance (216), type 2 diabetes mellitus (217), obesity (218), metabolic syndrome (219), and increased mortality (75). ACS has emerged as the commonest functional abnormality in patients with AI with prevalence rates of up to 20% (64,65,72).
As highlighted through a summary of published guidelines, there is no gold standard test for diagnosing ACS. As can be seen in Table 5 there is a wide variety of first screening, secondary screening and confirmation tests depending on the guideline. The sensitivity and specificity of these tests in patients with ACS have also been widely reported and are summarized in Table 6. Overall, the consensus from these recommendations supports the use of the 1-mg DST as having the highest sensitivity for screening for ACS, Table 6. A post-dexamethasone cortisol level ≤1.8 µg/dL (≤50 nmol/L) is considered “normal” and excludes cortisol excess in most patients. Levels between 1.9 and 5.0 μg/dL (50-140 nmol/L) may indicate “possible autonomous cortisol secretion,” and cortisol levels above 5.0 μg/dL (140 nmol/L) are suggested to confirm ACS (79,220). Sensitivity increases as the stringency of the “cut-off” is lowered; from 80% at a cut off of 140 nmol/L to 95% at 50 nmol/L, but this is offset by lower specificity, such that at a cut off of 50 nmol/L 20% of the “normal” population will fail to suppress cortisol. Even at a cut-off concentration of 140 nmol/L specificity is only 95%; the investigator must consider that a false positive result is far more likely than a true positive (45). Furthermore, many of the age-related comorbidities ascribed to ACS (notably obesity, diabetes, anxiety/depression—see later) are in themselves causes of physiological hypercortisolism, and therefore confirming a diagnosis and ascribing clinical features to ACS that might prompt surgical intervention remains a major challenge.
Table 5.
Summary of published guidelines for the diagnosis of subclinical Cushing’s syndrome (SCS)/autonomous cortisol secretion (ACS) in patients with AI.
| Guideline (year) (ref.) | NIH (2003) (221) | Endocrine Society (2008) (212) | AACE/AAES (2009) (86) | FSE (2008) (7) | IACE (2011) (222) | ESE/ENSAT (2016) (4) | Korea (2017) (223) | JES (2018) (224) |
|---|---|---|---|---|---|---|---|---|
| Terminology | SCS | SCS | ACS | Asymptomatic hypercortisolism | SCS | |||
| Country | USA | USA | USA | France | Italy | Europe | Korea | Japan |
| First screening test (cut-off) | ||||||||
| 1-mg DST cut-off point | Yes >5 μg/dL: possible SCS | Yes >1.8 μg/dL | Yes >5 μg/dL | Yes >1.8 µg/dL | Yes <1.8 μg/dL: exclude >5.0 μg/dL: consider 1.8–5.0 μg/dL: indeterminate | Yes <1.8 μg/dL: exclude >5.0 μg/dL: ACS 1.8–5.0 μg/dL: possible ACS | Yes <1.8 μg/dL: normal >5.0 μg/dL: asymptomatic hypercortisolism 1.8–5.0 μg/dL: additional testing | Yes >5.0 μg/dL ≥3 μg/dL with (any of A-D) or E ≥1.8 μg/dL with (A and B) or E |
| Late night salivary cortisol | NM | Yes (> 145 ng/dL) | NR | NR | NR | NR | NM | NR |
| Second screening test | ||||||||
| 24-hour UFC | NM | NR | NR | Yes | Yes | Yes (if 1mg DST > 5ug/dL) | Not recommended | |
| Late-night serum cortisol | NM | NM | NM | Yes | Yes | NM | NM | Serum 21.00-24.00 ≥5 μg/dL |
| ACTH | Yes | |||||||
| Late-night salivary cortisol | NM | NM | NR | NM | NR | Yes (if 1mg DST > 5ug/dL) | NM | |
| 4-mg DST | NM | NM | NM | NM | NR | Yes (if 1mg DST > 5ug/dL) | NR | |
| Confirmatory test | ||||||||
| 4-mg DST | NM | NR | Yes | NM | NR | NM | NR | |
| 8-mg DST | NM | NR | NM | NR | NM | NR | ||
| Localization (adrenal in origin) | ||||||||
| ACTH | NM | Yes | Yes | Yes | Yes | Yes | <10 pg/mL | |
| DHEA-S | NM | Yes | Yes | NR | NR | NM | NM | |
| 4-mg DST | NM | NM | NM | NM | NM | |||
| 8-mg DST | NM | NM | NM | NM | NM | |||
| Adrenal scintigraphy | NR | NM | NM | Yes | NR | NM | NM |
Abbreviations: NIH, National Institutes of Health; ES, Endocrine Society; AACE/AAES, American Association of Clinical Endocrinologists/American Association of Endocrine Surgeons; FSE, French Society of Endocrinology; IACE, Italian Association of Clinical Endocrinologists; DST, dexamethasone suppression test; ACTH, adrenocorticotrophic hormone; DHEAS, DHEA sulfate; NM, not mentioned; NR, not recommended; JES, Japan Endocrine Society; UFC, urine free cortisol.
JES abbreviations: A, low plasma levels of ACTH in the early morning; B, no diurnal changes in serum cortisol levels; C, unilateral uptake on adrenal scintigraphy; D, low serum levels of DHEA-S; E, transient adrenal insufficiency or atrophy of the attached normal adrenal cortex after removal of the adrenal tumor.
Adapted from reference (224).
Table 6.
Summary of published data on diagnostic screening tests for investigating autonomous cortisol secretion and Cushing’s syndrome in patients with adrenal incidentaloma.
| CS | ACS or mild CS or occult CS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Test | Cut-off | Sensitivity (%) | Specificity (%) | False positive (%) | False negative (%) | Ref. | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Ref. |
| 1-mg DST | 1.8 µg/dL (50 nmol/L) | 95-100 | 60-80.2 | 8 | 0 | (225,226) | 75-100 | 62–72 | 59 | 100 | (64,68,227-231) |
| 2.0 µg/dL | 91.3 | 56.3 | (68,230,231) | ||||||||
| 2.2 µg/dL | 100 | 67 | (230,231) | ||||||||
| 3 µg/dL (86 nmol/L) | 100 | 91.8 | (226) | 52.4-86.4 | 52.4-96.3 | (230,231) | |||||
| 5 µg/dL (138 nmol/L) | 86.5 | 92-97.4 | 3 | 12-15 | (225) | 44–83.3 | 83-100 | 57 | 95 | (64,68,227,228,230,231) | |
| LNSC | 2.7 nmol/L (RIA) | 97 | 77 | (232) | |||||||
| 2.8 nmol/L (LC-MS/MS) | 31.3 | 83.3 | (233) | ||||||||
| 100 ng/dL (2.76 nmol/L) LC-MS/MS | 93 | 91 | (234) | 93 | 91 | (234) | |||||
| 0.350 μg/dL | 93.8 | 79.5 | (227) | ||||||||
| 3.6 nmol/L (RIA) | 92 | 100 | (232) | ||||||||
| 5.1 nmol/L | 100 | 100 | (226) | 22.7 | 87.7 | (235) | |||||
| 14.46 nmol/L | 86 (73–93) | 92 (86–95) | (228) | ||||||||
| 24-h UFC | 80 µg (170 nmol) or ULN | 91-96 | 89.6-92.5 | 8 | 2 | (225, 226) | 31.8-76 | 80-100 | 49 (100) | 96 (93.3) | (227,228) |
| DHEA-S ratio | 1.2 | 100 | 91.1 | (236) | |||||||
| ACTH | 41-86.4 | 38-96 | 47 | 96 | (64,230) | ||||||
| Midnight serum cortisol | 1.8 µg/dL (50 nmol/L) | 99-100 | 20.2 | (225) | 22.7 | 87.7 | (64) | ||||
| 5 µg/dL (135 nmol/L) | 95-100 | 73.9 | (225) | 77 | 68 | ||||||
| 7.5 µg/dL | 90-96 | 87.7 | (225) | ||||||||
| Plasma steroid metabolomic | Sensitivity 97 AUC 0.991 | (237) | |||||||||
| Combination of tests | |||||||||||
| 24-hour UFC + LNSC | >70 µg UFC + LNSC > 5.4 µg/dL (149 nmol/L) | 30.8 | 100 | ||||||||
| 1-mg DST and 24-hour UFC and ACTH <10 pg/mL | >70 µg UFC + LNSC >3 µg/dL (86 nmol/L) | 55.6-65.2 | 68.8-82.9 | (230) | |||||||
| 1-mg DST + Dexamethasone level > 3.3 nmol/L | Serum cortisol 1.8 µg/dL (50 nmol/L) | 100 | 84 | (238) | |||||||
| 1-mg DST + Dexamethasone level > 3.3 nmol/L | Salivary cortisol 0.55 nmol/L | 71 | 90 | (238) | |||||||
| 1-mg DST + dexamethasone level >3.3 nmol/L | Salivary cortisone 2.7 nmol/L | 91 | 82 | (238) | |||||||
| 1 mg DST + LNSC (LC-MS/MS) | Serum cortisol 1.8 µg/dL (50 nmol/L), LNSC 1.4 nmol/L | 88.9 | 85.2 | (233) | |||||||
Abbreviations: CS, Cushing’s syndrome; ACS, autonomous cortisol secretion; LRneg, negative likelihood ratio; LRpos, positive likelihood ratio; CI, confidence interval; 1-mg dexamethasone suppression test (DST); LNSC, late night salivary cortisol; PPV, positive predictive value [TP/(TP + FP)]; negative NPV, negative predictive value [TN/(TN + FN)]; DHEAS ratio calculated by dividing the measured DHEAS by the lower limit of the reference range (age and sex matched); ULN, upper limit of normal.
*Consider pseudo-CS state: alcoholism, psychiatric disorders, stress, diabetes, obesity, vigorous exercise, pain, hypothalamic amenorrhea, pregnancy.
UFC in isolation has a low sensitivity (31.8-76.0%) in diagnosing ACS but this can be improved by LC-MS/MS methodology (sensitivity 98%, specificity 91%, and negative/positive likelihood ratios of 0.02/10.83, respectively). A combination of the 1-mg DST with UFC decreases the false positive rate further (239). LNSC is emerging as perhaps the most accurate test in diagnosing overt Cushing’s syndrome (240), but for ACS the published studies have given mixed results. In some cases, sensitivity reached 93.8%, but with relatively poor specificity at 79.5% (227) (Table 6).
An Italian study diagnosed ACS based on 2 out of the following 3 tests: serum cortisol >3 µg/dL (83 nmol/L) after 1 mg of ONDST, UFC >70 µg/24 hours (193 nmol/24 hours) or ACTH <10 pg/mL (2.2 pmol/L) (228). While this was put forward as a way of improving accuracy, it also increases the likelihood of a false positive result and is not our usual practice. Intuitively a low/suppressed ACTH would seem a sensible adjunct in the diagnosis of ACS (Tables 5 and 6).
Clinical consequences of ACS—cardiometabolic and bone.
Based on the established clinical features of overt Cushing’s syndrome, there is now an extensive literature on the potential clinical impact of more modest increases in cortisol secretion as seen in ACS.
This has been reviewed extensively in focused articles on “subclinical Cushing’s” (now termed ACS) (241-245). In brief, cardiovascular morbidity includes increased left ventricular hypertrophy and arterial stiffness (246), hypertension, coronary heart disease, stroke, and fatal or nonfatal myocardial infarction. ACS is associated with mild to moderate hypertension in 41% to 92% of cases (47). A recent systematic review showed that ACS patients had a higher prevalence of cardiovascular events (16.7-26.8%) compared with patients with nonfunctional AI (6.7-10.4%) (79,244,245,247). Increased cardiovascular disease has been linked to the post-1-mg DST cortisol level as an independent cardiovascular risk factor (245). A study with up to 15 years of follow-up in patients with ACS has documented increased cardiovascular morbidity (43% vs 8.8%, P < .005) and mortality (22.6% vs 2.5%, P < .02) in ACS patients compared with nonfunctioning AI. Pulmonary infection and cardiovascular complications were the major causes of death (220,247).
It is well established that glucose intolerance and diabetes mellitus are prevalent features of overt Cushing’s syndrome (228,248). Impaired glucose tolerance or diabetes has been reported to occur in 10% to 69% of patients with ACS (249) and improved glycemic control (and in some cases reversal of diabetes) following surgery is reported in some studies but not others (Table 7).
Table 7.
Summary of published studies evaluating the effect of adrenalectomy on clinical and biochemical features of autonomous cortisol secretion.
| Proportion of patients with improvement postop | ||||||
|---|---|---|---|---|---|---|
| Study, year (ref.) | Design | Diagnostic criteria DST cortisol nmol/L ACTH pg/mL | Operated patients (n) | Arterial HTN | Weight | Impaired glucose metabolism |
| Perysinakis 2013 (250) | Retrospective no control | DST >50 and 1 of the following: ACTH <2.2 24-h UFC >276 blunted diurnal CCR | 29 | 12/17 | 6/14 | 5/12 |
| Iacobone 2012 (251) | Retrospective | DST >138 ACTH <2.2 high 24-h UFC | 20 | 8/15 | 6/15 | 5/10 |
| Maehana 2012 (252) | Retrospective nonfunctioning No control | DST >50 and 1 of the following: low ACTH, loss of CCR, scintigraphy, low DHEAS | 13 | 5/7 | n/a | 2/2 |
| Guerrieri 2010 (253) | Retrospective | 2 of the following: DST >50, high 24-h UFC ACTH <2.2. | 19 | 12/12 | n/a | n/a |
| Chiodini 2010 (254) | Retrospective | 2 of: the following DST >83, high 24-h UFC, ACTH <2.2. | 25 | n/a | n/a | n/a |
| Toniato 2009 (255) | Prospective randomized | DST >69 and 2 of the following: low ACTH, high 24-h UFC, loss of CCR, low DHEAS | 23 | 12/18 | 3/6 | 5/8 |
| Tsuiki 2008 (243) | Retrospective | DST (8mg) >28 and one of the following: ACTH<2.2, blunted ACTH after CRH, loss of CCR, low DHEAS, scintigraphy | 10 | 5/6 | 0/3 | 2/9 |
| Salcuni 2016 (256) | Retrospective 23 controls refused surgery | DST >138 or 2 of the following DST >83 low ACTH high 24h-UFC | 32 | No change | — | No change |
Adapted from Iacobone et al. (257).
Abbreviations: n/a, not assessed/ available; DST, dexamethasone suppression test; ACTH, adrenocorticotropic hormone; UFC, urinary free cortisol; CCR, cortisol circadian rhythm (ratio of plasma cortisol at 24.00 hours to 08.00 hours >50%); DHEAS, dehydroepiandrosterone sulfate; CRH, corticotropin-releasing hormone.
Similarly, the deleterious effects of chronic glucocorticoid excess on bone mineral density leading to osteoporosis are well established (258). However, in patients with ACS, a mixed picture is reported with either decreased, normal, or even increased bone formation reported alongside normal bone resorption (229,242,259-262). This variance is likely to be explained by differences in bone turnover markers studied, underlying vitamin D, parathyroid hormone concentrations, age, sex (notably the percentage of postmenopausal women), and the sample size. Cortisol affects trabecular bone to a greater degree than cortical bone, which is similar to the postmenopausal state. Both trabecular (65,261-263) and cortical (259,262,264-266) bone loss have been described in patients with ACS. For bone fracture, a meta-analysis reported a prevalence of vertebral fracture in patients with ACS of 63.6% (95% CI 55.98-71.26%) (254) and this risk is independent of age, sex, gonadal status, or bone mineral density (264).
Reversal of ACS.
Several studies have reported the outcome of surgical intervention but most involve small numbers and are retrospective, uncontrolled, and lack randomization (230,243,250-253,255) (Table 7). ClinicalTrials.gov lists several prospective trials that are underway but are yet to report.
Metabolic improvement after adrenalectomy, including weight loss, blood pressure lowering, glucose tolerance, lower lipids, and beneficial effects on bone have been reported (230,267). A recent systematic review addressed cardiovascular benefit in ACS patients (247) with adrenalectomy improving cardiovascular outcome and mortality (4,247).
In the absence of a robust evidence base for the surgical treatment of ACS and reversal of symptoms and signs, establishing a causative link of ACS to cardiometabolic traits that increase naturally with age and low bone mineral density remains a challenge. It is reasonable to assume that patients, albeit with mild forms of adrenal Cushing’s syndrome, should benefit from surgery, noting that even in patients with established Cushing’s syndrome, the reversal of the clinical phenotype can take many months or years. The degree of hypercortisolism within the ACS definition, the severity of clinical features detailed earlier, balanced against risks of surgery in an aged population must be considered as an individualized approach. The real risk is an unnecessary procedure for an elderly patient with coincidental age-related comorbidities that have no causative relationship to a false positive ACS diagnosis. Over and above evidence-based guidelines for the non-AI background population, we strongly recommend aggressive treatment of comorbidities (hypertension, hyperlipidemia, glucose intolerance, weight, and reduced bone mass) in patients with AI. This will likely have a far greater impact on preventing and reversing cardiometabolic morbidity and mortality than lowering borderline cortisol secretion rates. Large randomized prospective trials of treatment of ACS are required to answer many of the above questions.
The natural history of “untreated” ACS.
A recent New Zealand study, prospectively evaluated 101 patients with benign adrenal adenomas over a 3-year follow up period. Nine patients had evidence of ACS at diagnosis (defined as an elevated 24-hour UFC and a 1mg-DST), while the remaining 92 patients were diagnosed with a nonfunctioning AI. At 3 years, 5 of the 9 patients with ACS at diagnosis (44%) showed normalization of cortisol parameters, while 5 of the 92 patients with a nonfunctional AI developed ACS (5%) (268). Barzon et al. reported the cumulative incidence of ACS after 1and 5 years as 3.8% and 6.6%, respectively (68). An Italian group reported an increased risk of ACS development if the adenoma size was >2.4 cm (sensitivity 73.3% and specificity 60.5%, P = .014) (244).
A recent systematic review and meta-analysis reported the follow-up of 4121 patients with nonfunctioning adrenal tumors (NFATs) and/or mild autonomous cortisol excess (MACE) (269). Clinically overt hormone excess (Cushing’s syndrome) was unlikely to develop (<0.1%) in patients with NFATs or MACE. Only 4.3% of patients with NFATs developed MACE, and pre-existing MACE was unlikely to resolve (<0.1%). Hypertension, obesity, dyslipidemia, and type 2 diabetes were more likely to develop and worsen in MACE than NFATs and new cardiovascular events were more prevalent in MACE (15.5%) than NFATs (6.4%) during follow-up. However, reported mortality (11.2%) was similar between NFATs and MACE.
Guidelines suggest that where functional secretion has been excluded at diagnosis, repeat endocrine testing is not required unless clinical features significantly change (4). Annual clinical assessment for up to 5 years is recommended in patients with ACS (4) together with an ongoing individualized risk assessment for potential benefit from surgical intervention based upon strengthening evidence linking cortisol excess to clinical symptoms and signs.
Screening for primary aldosteronism
The discovery of hyperaldosteronism in the context of an AI is relatively uncommon, compared with the detection of cortisol hypersecretion or pheochromocytoma (45,270). Normokalemic primary aldosteronism (PA) has been reported in up to 5.5% of AI (271). A few publications have reported normotensive PA in AI; however, most of these patients demonstrated occasional hypokalemia (8,272-274). Hypertension and hypokalemia are the major classical clinical findings of PA and the presence of either in the context of AI should prompt appropriate screening investigations. PA is associated with low plasma renin activity (or concentration) because aldosterone-induced hypervolemia results in suppression of renin release (275). Although hypokalemia in the context of hypertension in a patient with AI is suspicious of PA, the finding of hypokalemia is not a reliable marker. A recent multicenter analysis estimated that only 9% to 37% of patients with primary hyperaldosteronism were hypokalemic (276,277).
PA is associated with an increased risk of stroke (odds ratio [OR] 2.58, 95% CI 1.93-3.45), coronary artery disease (1.77, 1.10-2.83), atrial fibrillation (3.52, 2.06-5.99), heart failure (2.05, 1.11-3.78), and mortality (hazard ratio [HR] 1.34, 95% CI 1.06-1.71) compared with matched populations with essential hypertension (278,279). Therefore, the diagnosis of PA is important and requires either surgical excision or targeted antihypertensive therapy with mineralocorticoid receptor antagonists. Diabetes mellitus/metabolic syndrome (278,279), renal damage (280), impaired bone mineral density (81), and osteoporosis (264,281,282) have also been reported to be more prevalent in AI patients with PA.
Clinical guidelines recommend screening for PA in every (AI) patient with hypertension or hypokalemia (283,284). However, normotensive patients with suppressible aldosterone/renin ratios may frequently develop hypertension and PA (285). Brown and colleagues (285) reported that populations with suppressed plasma renin activity (≤0.5 ng/mL/h) and high aldosterone levels were at increased risk of hypertension (HR 1.18; 95% CI 1.03-1.36) (285). These studies draw attention to the concept of a preclinical stage of PA. Further studies are required before the routine screening of all AI patients is recommended.
The 3-step approach for screening, confirmatory, and subtype classification of PA has been thoroughly covered in an excellent Endocrine Society Clinical Practice Guideline and will not be repeated here (284). Only to say that initial assessment using plasma aldosterone concentrations and plasma renin activity or the direct renin concentration and derivation of the aldosterone/renin ratios yields a sensitivity of 68% to 94% and negative predictive value approaching 100%.
AI-secreting sex steroids
AIs that secrete either estrogen or testosterone in isolation are rare. Although benign cortisol-secreting adenomas may very rarely produce androgens (286), elevated sex steroids are highly suspicious for ACC and urgent diagnostic evaluation is required (287-289).
In women, androgen-secreting tumors may present with features of virilization, such as excessive facial hair growth, skin changes such as acne, deepening of the voice, clitoromegaly, and male pattern baldness. Estrogen-secreting tumors in women may cause irregular uterine bleeding and breast tenderness. In men, estrogen-secreting tumors may cause feminization with decreased libido, testicular atrophy, and gynecomastia as key clinical features.
Imaging Evaluation of an AI
Multiple different groups have developed guidelines for the work-up of AIs (4). A key consideration for the diagnostic workup of an AI is whether there is a possibility of malignancy. Patients with an AI >1 cm in the short axis should undergo an imaging procedure to determine if the lesion is benign or malignant at the time of initial diagnosis. Some lesions with overtly benign features such as the presence of bulk macroscopic fat (myelolipoma) or simple cysts may not require any further imaging assessment.
Multiple imaging parameters are employed for the differential diagnosis of AI. There is a correlation between tumor size and risk of adrenocortical cancer: 2% risk in AIs <4 cm, 6% in AIs 4.1 to 6 cm, and 25% in AIs >6 cm (290). A large Italian study of patients with AI (n = 887) reported that 90% of ACCs had a diameter of >4 cm at presentation, a 4-cm cut-off had a 93% sensitivity for detecting ACCs (64, 137). Other imaging features used for characterization include unenhanced CT with the assessment of tumor density, contrast-enhanced timed washout CT studies, MRI chemical shift analysis, and, more recently, 18-fluorodeoxyglucose (FDG) positron emission tomography (FDG-PET) in combination with CT (PET-CT) (291).
Unenhanced CT
For all AIs, a noncontrast (unenhanced) CT is recommended as the first-line investigation. HU assessment on an unenhanced CT is a method for quantifying X-ray absorption of tissues compared with water, which conventionally has a HU of 0 (Fig. 6). Care is required when placing a region of interest to measure HU, this should cover at least two-thirds of the circumference of the nodule while avoiding areas of heterogeneity such as necrosis or calcification (292,293). A recent meta-analysis (291) on the use of imaging for differentiating benign from malignant adrenal lesions identified only 2 studies with 102 true incidentalomas, based on strict meta-analysis inclusion criteria. In patients without known extra-adrenal malignancy, an HU of ≤10 on a noncontrast CT is consistent with a lipid-rich benign adenoma (294). Importantly, the assessment of HU is for homogeneous lesions and care must be taken in heterogeneous lesions given the variability of HU and the potential to miss more solid components that may be malignant.
Figure 6.
Characterization of AI by CT. Axial images obtained pre and post-IV contrast at the portal-venous (60-70 seconds) and delayed (10-15 minutes) phases post injection. Calculation of adrenal lesion attenuation value showing benign pattern washout in a lipid-rich left adrenal adenoma.
Contrast-enhanced washout CT
Approximately 30% of benign adrenal adenomas do not contain large amounts of fat and have an attenuation value of >10 HU (ie, lipid-poor adenomas), these lesions cannot be reliably characterized on unenhanced CT due to an overlapping density with malignant lesions and pheochromocytomas (295,296). For lesions with an attenuation value of >10 HU, further assessment is required and there is no clear consensus regarding which is the best second-line imaging for these patients. Our institutional practice is to perform a dedicated adrenal washout protocol CT as the next test because this is more accurate for characterizing lipid-poor adenomas than MRI (297), although as a recent meta-analysis has shown there is a need for further studies to optimize this technique as there is significant variability in scanning protocols and timings described and sensitivities and specificities (291).
Washout studies consist of CT imaging performed before and at 2 time points after administration of intravenous contrast (typically, imaging is performed at 60-90 seconds and 10 or 15 minutes postcontrast) with no clear evidence about the best time interval for the later time point (298). Adenomas typically enhance rapidly and show prompt washout of intravenous contrast, in contrast to malignant adrenal lesions which usually enhance rapidly but demonstrate a slower washout of contrast medium. Absolute washout values of >60% (early enhanced HU – delayed HU)/(early enhanced HU – unenhanced HU) × 100% suggest a benign adenoma (295,299). Relative washout can be calculated when unenhanced CT is not available (early enhanced HU – delayed HU)/enhanced HU × 100%. Values of > 40% suggest a benign adenoma (296,299,300) (Fig. 6). However, only 1 previous study has evaluated the test performance of CT contrast-enhanced washout in the evaluation of truly incidentally discovered adrenal masses (301), that is in patients not undergoing surveillance imaging for previous nonadrenal malignancy. This study reported high sensitivity (96%) and specificity (95%) for differentiating benign from malignant adrenal lesions (301); however, it considered only 50 cases, therefore larger prospective studies are required to validate the performance of contrast CT washout in patients with AI. Caution is also required because whilst pheochromocytomas usually show slow contrast washout, occasionally they can mimic benign lipid-poor adenomas by showing rapid washout (302). Therefore, following multidisciplinary team (MDT) discussion if there is still a suspicion regarding a lesion with indeterminate HU further scanning should be requested to ensure no further growth.
Dual-energy CT
Dual- or multi-energy CT is becoming more widely available and can provide additional specific data about attenuation properties of different materials at different energies (303). A frequent clinical dilemma is the detection of an AI on a single-phase contrast-enhanced CT typically performed 60 to 90 seconds postcontrast administration when the HU value of benign adenomas and nonadenoma lesions overlap significantly (304). Dual-energy CT offers the potential to extract a virtual noncontrast CT dataset from routinely acquired variable energy single-phase contrast-enhanced CT (305). A recent systematic review and meta-analysis reported that virtual non-contrast CT images generated from dual-energy CT demonstrate comparable sensitivity with standard noncontrast CT for diagnosis of lipid-rich adenomas, but data were only available from a small number of heterogeneous studies at high risk of bias (306). This technique requires prospective evaluation in a larger patient cohort before routine clinical use.
Magnetic resonance imaging
More recent guidelines suggest that MRI evaluation of adrenal lesions should be used primarily as a problem-solving tool. MRI with chemical shift imaging should only be the first choice where CT is less desirable, for example during pregnancy, in children, or for patients with allergies to iodinated contrast (this is not an issue in noncontrast scans) (307). The use of chemical shift MRI to detect intracellular fat within lipid-rich adrenal adenomas and differentiate these from other lesions was first described in 1992 (310) (Fig. 7). There are both qualitative (visual analysis) and quantitative methods of imaging evaluation which involve assessing change in signal intensity of adrenal lesions between in-phase and out-of-phase sequences (309). A recent systematic review and meta-analysis reported that visual analysis and quantitative analysis of adrenal signal intensity index and adrenal-to-spleen ratio all have high accuracy for lipid-rich adenoma detection (95-98%), and diagnostic performance is not significantly improved by adrenal signal intensity index or the adrenal-to-spleen ratio (310). Consequently, if AIs are detected on MRI and findings are unambiguous for a benign lipid-rich adenoma further imaging may not be warranted.
Figure 7.
Chemical shift MRI. Paired axial T1-weighted MRI images showing loss of signal within a left adrenal nodule on out-of-phase imaging consistent with lipid-content within a lipid-rich adrenal adenoma.
Positron emission tomography-computed tomography
FDG PET-CT has high diagnostic accuracy for characterization of adrenal masses with a pooled sensitivity of 91% and specificity of 91% in a recent meta-analysis of 29 studies involving 2421 patients (311). This technique is more expensive and less available than CT and MRI but may help to discriminate metastatic disease from benign masses in patients with known malignancy (4,312) (Fig. 8). One limitation is that benign adrenal lesions particularly functional adenomas and nonmetastatic pheochromocytomas can be FDG positive (313,314). As with MRI, there are both qualitative (visual analysis) and quantitative criteria used for the diagnosis of malignant adrenal lesions. Visual assessment of FDG activity within adrenal lesions compared to background (physiological) uptake in the liver or blood pool has similar pooled sensitivity and specificity (91-92%) to quantitative analysis using adrenal to liver standardized uptake value (SUV) ratio (89-91%) or maximum SUV (SUVmax) (85-91%) (309). False-negative findings are recognized in the setting of small malignant lesions, metastases from non-FDG avid tumors such as some subtypes of renal carcinoma and well-differentiated neuroendocrine malignancies and in necrotic lesions (315). In patients with a suspected solitary adrenal metastasis being considered for adrenalectomy, FDG PET-CT should be considered to exclude extra-adrenal metastatic disease not detected on CT or MRI (4).
Figure 8.
18F-fluorodeoxyglucose PET-CT. Coronal PET maximum intensity projection and axial fused PET-CT images in a patient with a locally advanced right adrenocortical carcinoma and an unsuspected tracer-avid right-sided rib metastasis.
Follow-up imaging
European guidelines suggest no further imaging for patients with adrenal lesions with benign characteristics <4 cm in diameter (4). This is further supported by a recent systematic review and meta-analysis of nonfunctioning adrenal lesions where a mean tumor growth of 2 mm occurred over a median of 52.8 months, and clinically significant tumor enlargement (≥10 mm) occurred in only 2.5% of patients, and none developed adrenal cancer (269).
Data from a large Italian cohort study reported a 4 cm size cut-off had the highest sensitivity (93%) but low specificity (24%) for prediction of malignancy (66). For this reason, larger lesions with clear benign features warrant interval reassessment with imaging after 6 to 12 months to exclude significant growth (>20% increase in size with at least 5 mm absolute increase in diameter) which would prompt surgical resection. Less marked interim lesion growth warrants reassessment with a further scan after 6 to 12 months.
Ideally, every patient with an AI should be managed by an expert MDT, incorporating an endocrinologist, radiologist, pathologist, and a surgeon, with significant expertise in adrenal tumors. However, this is a challenging aspiration given the increasing prevalence of AI. Therefore the ESE/ENSAT guideline (4) identifies certain patients who are most likely to benefit from MDT discussion. This includes conditions where one of the following criteria is met; imaging is not consistent with a benign lesion; there is evidence of hormone excess (including ACS); there is evidence of significant tumor growth during follow-up imaging; and where adrenal surgery is considered.
Special Circumstances
Bilateral adrenal incidentalomas
Bilateral adrenal masses may represent co-occurrence of different entities; therefore both lesions should be separately assessed as per recommendations for a unilateral lesion (4). Interestingly, in patients with bilateral disease, it is possible for 1 mass to be a nonfunctioning cortical adenoma while the other mass may be hormone secreting (316). Additionally, there is a possibility that both masses (particularly in the context of hemorrhage and metastases) may lead to adrenal hypofunction and therefore this should be considered in the evaluation of the patient with bilateral AIs.
Bilateral AI and ACS.
ACS is more frequently encountered in patients with bilateral AI than in those with unilateral lesions (317-319). A prospective study of 298 patients (224 with unilateral AI and 74 with bilateral AI) reported evidence of ACS in 35.1% of patients with bilateral AI, but only 17.9% of patients with unilateral AI (P = .003) (319). This supports previous retrospective studies (320-322) and a more recent surgical series including 112 unilateral AI and 23 bilateral AI, where mild cortisol excess was present in 21.7% bilateral AI versus 6.2% of unilateral AI (321). Vassiliadi et al. (320) demonstrated an exaggerated response of cortisol and ACTH in patients with bilateral AI during the combined tests of a DST followed by CRH stimulation when compared with unilateral AI and to a control group suggesting that regulation of the hypothalamic–pituitary axis was disturbed in patients with bilateral AI; however the diagnosis of BMAH was not excluded in this group (319).
PBMAH is suspected when there are bilateral AI and evidence of ACS (323). Cortisol secretion is in part regulated by the expression of multiple aberrant G protein-coupled receptors in the zona fasciculata cells including receptors for vasopressin, serotonin, luteinizing hormone/human chorionic gonadotropin, β -adrenergic agonists, gastric inhibitory polypeptide, glucagon, and angiotensin (324). These G protein-coupled receptors lead to activation of cAMP–PKA signaling pathway, similar to the pathway activated by ACTH receptor consequently leading to the transcription of steroidogenic factors.
On unenhanced CT, both adrenal glands are enlarged usually with multiple nodules but diffuse enlargement without nodules is also seen (325). On contrast-enhanced imaging, nodules can have marked enhancement, and HU >10 has also been described. Despite PBMAH being a benign disease limited studies using FDG uptake demonstrated an uptake similar to that seen in malignant tumors (326).
Bilateral AI and CAH.
CAH can rarely present as bilateral adrenal lesions in adult life, although the majority of patients present with symptoms of adrenal insufficiency in childhood. The most common form of CAH, affecting over 90% of individuals, involves the gene for 21-hydroxylase and if suspected 17-hydroxyprogesterone (17-OHP) testing and mutation analysis for the gene CYP21B should be undertaken. The measurement of 17-OHP in the setting of bilateral adrenal hyperplasia should be interpreted with caution. In some cases, increased levels of 17-OHP may represent increased secretion of steroid precursors (327) from the lesion(s) especially in malignant tumors or in bilateral macronodular adrenal hyperplasia. In these cases, low or suppressed ACTH levels may argue against CAH.
Bilateral AI and pheochromocytoma.
Pheochromocytomas occur bilaterally in 10% cases and although some cases are sporadic, they are often seen as part of a genetic syndrome, discussed in detail in “Etiology: Tumors of the Adrenal Medulla.” It should be noted that patients who have a unilateral pheochromocytoma may also have an incidental adrenal adenoma and as such every adrenal lesion should be assessed individually.
Bilateral AI and metastases.
The most common primary cancers to metastasize to the adrenal gland include lung, breast, renal, melanoma, and the gastrointestinal tract, although multiple other primary sites have been reported. The adrenal glands have been reported to be the fourth most common site of metastases in malignancy. In up to 75% of patients with an AI and extra-adrenal cancer, the adrenal mass is a metastasis and bilateral adrenal metastases are seen in a significant number of patients. However, 25% of patients with extra-adrenal cancer will have a primary adrenal lesion (101).
From an endocrine perspective, bilateral adrenal metastases may rarely cause adrenal insufficiency and patients should be clinically assessed and undergo further investigations if suspected. A unilateral adrenal metastasis would not cause adrenal insufficiency and patients do not usually require evaluation.
Management of bilateral AI.
Surgical management of unilateral AI is discussed in “Surgical Management of Adrenal Incidentaloma.” The management of bilateral AI is challenging because the size of the tumors is not a criterion for surgery. As there is no clear consensus on the criteria defining abnormal cortisol secretion, the indication for adrenalectomy in the case of bilateral adrenal lesions remains controversial. Bilateral adrenalectomy may be considered if urinary cortisol levels are higher than 3 to 4 times the upper limit of normal with both adrenals having a relatively symmetrical size (324). The European Society of Endocrinology suggests that in selected patients, unilateral adrenalectomy of the dominant lesion may be considered based on the age of the patient, degree of cortisol excess, general condition, comorbidities, and patient preference (4). A recently published observational study analyzed the long-term clinical and biochemical outcomes of unilateral adrenalectomy versus bilateral adrenalectomy in patients with PBMAH and ACS and compared it to the outcome of cortisol-producing adenomas treated with unilateral adrenalectomy (328). The data, albeit retrospective and observational, showed that unilateral adrenalectomy of patients with PMAH lead to initial clinical remission in 84% of patients but at follow-up (median, 50 months), only 32% of patients were biochemically controlled (defined as a cortisol after dexamethasone <1.8 μg/dL) compared with all patients with bilateral adrenalectomy and unilateral adrenalectomy for a cortisol-producing adenoma. Additionally, 3 deaths occurred in the group of patients who were not biochemically controlled after unilateral adrenalectomy.
Bilateral adrenalectomy is recommended for bilateral pheochromocytomas; however, the risk of adrenal insufficiency and the side effects of life long glucocorticoid replacement have led to certain centers performing adrenal cortex sparing resections particularly in the setting of genetic syndromes such as VHL and MEN2A where the risk of malignant tumors is low (325).
Adrenal gland biopsy
The number of adrenal biopsies has significantly reduced in recent years due to improvements in noninvasive imaging techniques, which can increasingly accurately diagnose benign adrenal lesions. There are a number of reasons not to perform a biopsy on an adrenal lesion which includes the risk of seeding of adrenal cancer after biopsy (329), the adverse hemodynamic effects of performing a biopsy on an undiagnosed pheochromocytoma or paraganglioma, and most importantly of all it is frequently not possible to distinguish between an adrenal adenoma and an adrenal cortical carcinoma on the sample which is obtained and therefore it often does not help the clinical decision-making process.
In a recent systematic review and meta-analysis, Bancos et al. concluded that an adrenal biopsy is most useful in confirming the diagnosis of metastasis from extra-adrenal cancer (330). It should only be undertaken following detailed discussion at an adrenal tumor multidisciplinary meeting and if the lesion is not conclusively benign on imaging and, most importantly, the outcome will affect the therapeutic management of the patient (eg, if the patient has an extra-adrenal primary and a lesion in the adrenal would affect the staging and further management of the patient). Pheochromocytoma should be excluded before an adrenal biopsy, to prevent precipitating a potential hypertensive crisis. The biopsy itself is not without risk. The most frequent complications are pneumothorax (due to the proximity of the adrenal gland to the diaphragm) and hemorrhage. Patients should, therefore, be able to hold their breath and have normal coagulation (331).
Surgical Management of Adrenal Incidentaloma
Indications for unilateral adrenalectomy
The principle threat of a unilateral adrenal lesion, with indeterminate imaging characteristics, is an ACC. For ACC without metastases, surgery is the most important single therapeutic measure. Guidelines recommend that surgery for patients with ACC should be limited to referral centers and performed by surgeons with expertise in adrenal surgery (open and laparoscopic) and with a volume of more than 15 adrenalectomies per year (benign and malignant) (332).
Patients with a functional unilateral adenoma, with clinically significant hormone excess, are offered unilateral adrenalectomy. Patients with a unilateral adrenal adenoma and ACS, are considered for surgery on an individual basis and after MDT discussion (4). Surgery is taken into consideration along with the patient’s age, degree of cortisol excess, general health, comorbidities, and patient preference. In all patients, considered for surgery, ACTH-independent cortisol excess should be confirmed (4).
There is no absolute size for the recommendation of surgery in nonfunctioning adenomas. Due to the paucity of follow-up data on the natural history of large suspected benign AIs, and the realization that the larger the mass, the higher the incidence of malignancy (333), surgery may be considered in larger lesions (>4 cm) even if imaging characteristics suggest a benign lesion. Any indeterminate nodule on imaging greater than 4 cm should be offered surgery (4).
Occasionally myelolipomas and adrenal cysts are removed if they get to a significant size and cause compressive symptoms. Adrenal metastases are resected if appropriate in the context of the underlying pathology. In general, patients are deemed suitable if the underlying extra-adrenal malignancy is controlled, the metastasis is isolated to the adrenal gland and the patient has an adequate performance status to justify aggressive treatment.
Perioperative care of patients for adrenalectomy
Adrenal surgery involves a multidisciplinary team approach in order to achieve the best outcomes. Any patient who has unilateral adrenalectomy for Cushing’s syndrome or evidence of ACS is at risk of contralateral adrenal gland suppression, due to the chronically elevated pre-operative cortisol levels with consequent ACTH suppression and adrenal atrophy. Peri- and postoperative stress dose glucocorticoids are required, which are weaned down to oral maintenance therapy prior to discharge. After unilateral adrenalectomy, patients require regular follow-up and synacthen testing to assess when the contralateral adrenal function recovers and steroid replacement can be stopped. All patients require education regarding hydrocortisone treatment prior to discharge and an understanding of adrenal insufficiency sick rules.
Before adrenal surgery for pheochromocytoma patients are treated with α -blockers, intravascular volume expansion, and in some patients β -blockers (particularly if concerns regarding tachyarrhythmia are present) (180). After the tumor is devascularized, especially after dividing the adrenal vein intraoperatively, patients may develop profound hypotension, which requires fluid optimization and inotropic support, which may need to be continued in the initial postoperative period (334).
Patients with AI and primary hyperaldosteronism are often prescribed a mineralocorticoid receptor antagonist, such as spironolactone or eplerenone. Following adrenalectomy for PA, this should be discontinued to prevent hyperkalemia. Other antihypertensives are stopped or reduced depending on the patient’s postoperative blood pressure. Older patients and those with longstanding hypertension are more likely to have irreversible vascular damage and have persistent hypertension requiring antihypertensive medication, despite successful surgery (335).
Surgical techniques
Adrenal surgery has significantly changed over the past 100 years. There have been multiple open approaches to the adrenal gland, including transperitoneal, posterior, and flank. In 1992 the first laparoscopic transperitoneal adrenalectomy was performed and more recently the laparoscopic posterior (retroperitoneoscopic) adrenalectomy technique has been developed.
Laparoscopic adrenalectomy is now considered the gold standard of surgical treatment for the majority of small and medium-sized adrenal lesions. Multiple studies have demonstrated a shorter hospital stay, reduced pain, minimal morbidity, and improved recovery (336). The adrenal is a relatively inaccessible organ and difficult to access through an open incision, therefore lending itself to minimally invasive surgery. The posterior retroperitoneoscopic adrenalectomy has been developed more recently and uses high insufflation pressures in the retroperitoneal cavity. It provides direct access to the adrenal gland, avoids the intra-abdominal cavity and allows bilateral procedures to take place without repositioning the patient. Disadvantages of the posterior retroperitoneoscopic approach include a smaller working space, which makes removal of larger tumors more challenging and increased difficulty in patients with a high body mass index (BMI). This technique has been reported to lead to reduced post-operative analgesia and length of hospital stay (337,338).
More recently robotic-assisted laparoscopic adrenalectomy has been developed via the transperitoneal technique and has been shown to be safe and effective. Robotic surgery offers a greater range of motion, improved magnification, and stereoscopic vision than traditional laparoscopic surgery. The main advantages have been reported in patients with a high BMI and larger tumors. However, there is an increased cost, longer operative time, and a significant learning curve (339).
The role of laparoscopic surgery for the treatment of ACCs remains controversial. Complete resection (R0) of the entire tumor along with any adjacent involved structures or lymph nodes is the only chance of cure. Laparoscopic surgery is only advised if the tumor can be removed completely with an intact adrenal capsule and there is no evidence of tumor invasion. Based on the available data and clinical experience, the European guidelines suggest that laparoscopic adrenalectomy may be justified for adrenal tumors ≤6 cm with radiological signs of malignancy and without evidence of local invasion (4). Open resection is recommended in larger tumors due to the higher risk of tumor capsule rupture and in those with any evidence of local invasion and or when adjacent organ resection is required. The decision to convert to an open procedure should be made early, before any rupture of the tumor capsule (340). In many cases, an individualized decision process by a multidisciplinary team is required to find the best surgical approach for a given patient.
Solitary adrenal metastases often are confined within the adrenal gland and laparoscopic adrenalectomy is a safe technique, which achieves negative margins and reduces patient morbidity (340). If there is any evidence of local invasion into surrounding tissue intraoperatively the procedure should be converted to an open operation.
Follow-up in patients without surgery
The American Association of Clinical Endocrinologists recommends repeated imaging for up to 5 years for benign tumors (86). However, the more recent European guidelines do not recommend further imaging for benign, nonfunctioning lesions of less than 4 cm (4). Patients with adrenal lesions over 4cm or indeterminate lesions, who have not undergone surgery are recommended to have repeat imaging, either a noncontrast CT or MRI in 6 to 12 months, the optimal timing is at the discretion of the MDT and depends on the index of suspicion (4). Surgical resection is recommended if there is a 20% increase in size, in addition to at least a 5 mm increase in diameter over this period. Both adrenocortical cancers and metastases usually demonstrate rapid growth over months, in contrast to a benign adenoma. Further imaging should be undertaken, again at 6 to 12 months, if there is an increase in size, but not at the threshold for surgical intervention (4). For younger patients, MRI surveillance, rather than CT, is preferred due to lower radiation exposure. In elderly patients follow up with imaging, even with nodules over 4 cm might be favored over surgery, in the presence of multiple comorbidities. Patients are treated on an individual basis but it is acknowledged that many clinicians and patients would not feel comfortable following up a tumor over 4 cm on imaging, even if radiologically benign, in a young patient and surgery is often the preferred option.
Repeat hormonal testing is not advised in patients without evidence of hormone oversecretion on their initial assessment (4). It should only be considered if patients develop new clinical signs of adrenal hormone hypersecretion or worsening of comorbidities, including diabetes, hypertension, or osteoporosis (4).
The risk of patients with ACS progressing to overt Cushing’s syndrome is negligible; however, ACS is associated with numerous comorbidities (269). If patients with ACS do not undergo surgery initially, they should be annually reassessed for cortisol hypersecretion and potential worsening of comorbidities. If there is clinical or biochemical progression then patients can be re-evaluated for surgery (341).
The Future: Investigation and Management
Given the sensitivity and specificity limitations of standard endocrine testing (discussed in “Endocrine Work-up of AI”) and radiological investigations (discussed in “Imaging Evaluation of an AI”) in determining whether an adrenal lesion is benign or malignant, further advances are required to help risk-stratify patients with adrenal lesions.
The role of urine steroid metabolomics
Standard serum steroid measurements are variable because of the diurnal variation in adrenal steroid secretion. Twenty-four-hour urine steroid excretion analysis represents a more accurate estimate of total corticosteroid production and of adrenal precursor steroids and metabolites (342, 343) and therefore has significant potential in the assessment of adrenal diseases. This has been extensively reviewed by Storbeck et al. (344).
Adrenal steroid production and metabolism are affected by sex, age, and BMI (342,345,346). Glucocorticoid metabolites are higher in men than in women and in obese than in lean persons (345,346). Assessing ratios of steroids that are substrates and products, respectively, of a distinct steroidogenic enzyme activity allows for representative assessment of elements of the steroidogenic pathway, which has been particularly informative in the diagnosis of inborn steroidogenic disorders, including CAH.
Mass spectrometry.
There are a number of different methods of mass spectrometry including gas chromatography-mass spectrometry (GC-MS) and LC-MS/MS (191,220,327), each of which has its pros and cons, which have been reviewed in detail by Krone et al. (347). In mass spectrometry, steroids are identified by unique retention times and or multiple reaction monitoring (206) with the area under the peak in the chromatogram is proportional to its concentration and quantifiable via comparison to standard reference materials of known concentration.
Urinary steroid profiling using GC-MS permits the analysis of multiple corticosteroids and their metabolites from a single urine sample (347) (Fig. 9). As most urinary steroids are conjugated, samples need to be deconjugated followed by a derivatization step before analysis which is both time consuming and labor intensive. LC-MS/MS is considerably faster and less labor intensive and allows a much higher throughput than GC-MS; however, LC-MS/MS has a poorer resolving capacity (206). As a result, LC-MS/MS is more suited to a smaller panel of corticosteroids and their metabolites and as a result does not have the same broad scope of analysis that GC-MS allows (206). Given the preanalytical and analytical advantages of LC-MS/MS over GC-MS, it is better suited to clinical practice once adequate optimization has been performed. However, GC-MS has several advantages, particularly in the research environment, over LC-MS/MS, including a better chromatographic resolution which permits the ready characterization of structures; use of GC-MS in scan mode allows for nontargeted steroid profiling and the discovery of novel compounds, metabolomes, and pathways of synthesis and metabolism. Importantly, scanned data can be stored indefinitely for future research (347).
Figure 9.
(A) Schematic representation of steroidogenesis depicting the major products of adrenocortical steroid synthesis, the mineralocorticoid aldosterone (dark green), and its precursors (light green), glucocorticoid precursors (yellow), the active glucocorticoid cortisol (orange) and its metabolite cortisone, and the adrenal androgens and their precursors (light blue). Synthesis of active androgens (dark blue) mainly takes place in the gonads. (B0. The 24-hour urinary steroid metabolite excretion in healthy controls (n=88). Box plots represent median and interquartile ranges; the whiskers represent 5th and 95th percentile, respectively. Color coding of steroid metabolites mirrors that used for depicting the major adrenal corticosteroid classes in (A). CYP, cytochrome P450; HSD, hydroxysteroid dehydrogenase; DHT, 5 α -dihydrotestosterone (342). From Arlt W, Biehl M, Taylor AE, Hahner S, Libe R, Hughes BA, Schneider P, Smith DJ, Stiekema H, Krone N, Porfiri E, Opocher G, Bertherat J, Mantero F, Allolio B, Terzolo M, Nightingale P, Shackleton CH, Bertagna X, Fassnacht M, Stewart PM. Urine steroid metabolomics as a biomarker tool for detecting malignancy in adrenal tumors. J Clin Endocrinol Metab 2011; 96:3775-3784 (Under Open Access License).
Use of urinary steroid metabolome in research and clinical practice.
Increasingly, the results from panels of multiple steroids are being analyzed using novel statistical technical techniques including machine learning (which allows for the discovery of diagnostic and disease-specific patterns) revealing a personalized “urinary steroid metabolome.” This approach has been used for some time for diagnosing inborn errors of steroidogenesis such as CAH but has recently been developed for the evaluation of functionality and malignant potential of patients with adrenal nodules (281).
Use of urinary corticosteroid metabolism markers in differentiating between benign and malignant adrenal lesions.
This area has been extensively reviewed recently by Bancos et al. (342,348-350). Studies have shown that ACCs have a distinct pattern of urinary corticosteroids, characterized by an excess of precursor steroid metabolites (Fig. 10 (342)). In particular, the cosecretion of a distinct combination of glucocorticoid and androgen metabolites is emerging as a sensitive diagnostic tool for ACC (342,348,349).
Figure 10.
Steroid metabolite excretion in ACA (n = 102) and ACC (n = 45) according to steroid classes. (A) Metabolites of adrenal androgen precursors and active androgens; (B) metabolites of mineralocorticoids and their precursors; (C) metabolites of glucocorticoid precursors; (D) cortisol and cortisone metabolites. Box plots represent median and interquartile ranges; the whiskers represent 5th and 95th percentile, respectively.*P < .05; **P < .01; ***P < .001 comparing ACA with ACC. (342) From Arlt W, Biehl M, Taylor AE, Hahner S, Libe R, Hughes BA, Schneider P, Smith DJ, Stiekema H, Krone N, Porfiri E, Opocher G, Bertherat J, Mantero F, Allolio B, Terzolo M, Nightingale P, Shackleton CH, Bertagna X, Fassnacht M, Stewart PM. Urine steroid metabolomics as a biomarker tool for detecting malignancy in adrenal tumors. J Clin Endocrinol Metab 2011; 96:3775-3784 (Under Open Access License).
The study by Arlt et al. (342) assessed the 24-hour urinary steroid metabolome using GC-MS in 102 patients with benign adrenal adenomas and 45 patients with ACC. They used generalized matrix learning vector quantization to identify the most discriminate steroids which differentiated between a benign adenoma and a malignant ACC. They reported that 27% of patients with ACC had no hormonal excess on routine biochemical testing. Urinary steroid profiling revealed distinct differences between adrenocortical adenomas and ACC patients (Fig. 10). ACC patients had a significantly higher excretion of androgen precursor metabolites, metabolites of active androgens, deoxycorticosterone, and glucocorticoid precursor metabolites were significantly higher in ACC, as was free cortisol.
ACC patients exhibited significantly increased excretion of metabolites derived from the precursors of androgen, mineralocorticoid, and glucocorticoid synthesis. Even when analyzing the ACC patients without evidence of hormone excess on routine biochemistry, urinary excretion of androgen, and glucocorticoid precursor metabolites remained significantly increased. By contrast, steroid precursor metabolite excretion in nonmalignant AI did not differ from healthy controls. The majority of ACC patients (69%) showed androgen precursor excess, either combined with increased excretion of glucocorticoid precursors (36%) or both glucocorticoid and mineralocorticoid precursors (33%). There was no effect of age, sex, tumor size, or presence of metastasis on the characteristics of the urine steroid metabolomes in ACC and ACA patients. Using machine learning, the authors were able to identify that tetrahydro-11-deoxycortisol (THS), pregnenetriol (5-PT), and pregnenediol (5-PD) were the most discriminatory between ACC and ACA. They then included the next 6 most discriminatory to develop a panel that could be used for future validation on an LC/MS-MS platform (342).
Kotłowska et al. (343) have also reported the use of GC-MS analysis of 19 major urinary corticosteroids and their metabolites in 30 controls and 28 patients with “nonsecretory” incidentalomas. In this study, the diagnosis of an adrenal cancer was excluded by “examining the diameter of the tumor, its clinical image and properties revealed during additional test” and all adenomas were less than 4 cm as all lesions greater than this were surgically removed. Interestingly, 25% of patients with “nonsecretory” AIs had distinct patterns of urinary steroids compared to the controls and other patients with AIs. There is, therefore, the possibility that some of these patients could have had an autonomously secreting lesion or a small ACC.
In 2015, Kerkhofs et al. (348) reported data relating to 27 ACCs and 125 ACA patients. They performed GC-MS analysis of 22 steroid metabolites and identified 15 individual steroid markers with a sensitivity of 90% or above in detecting ACC, with the 11-deoxycortisol metabolite (THS) again representing the most informative marker. Other informative markers identified by that study included pregnanediol, pregnanetriol, etiocholanolone, the major androgen metabolite androsterone, and the major glucocorticoid metabolites tetrahydrocortisol and tetrahydrocortisone. In a recent study by Velikanova et al. (349), assessing 32 steroid metabolites by GC-MS in 24-hour urine samples from 31 patients with ACC and 96 patients with ACA, the authors confirmed the findings reported by Arlt et al. (342). Similar to Kerkhofs et al. (348) they did not employ unbiased computational data analysis of the steroid excretion data. All studies identified THS as the most informative steroid marker indicative of ACC. THS is the metabolite of 11-deoxycortisol, which is converted to cortisol by the adrenal-specific steroidogenic enzyme cytochrome P450 family 11 subfamily B member 1 (CYP11B1). Measurement of 11-deoxycortisol is not routinely used clinically, though recently serum results were reported in a cohort of benign adrenal tumors (249).
A recent study has also shown the utility of urinary steroid metabolomics in the follow up of patients with ACC as a marker of recurrence (351).
Future directions and challenges with steroid metabolomics.
Arlt et al. have used GC-MS analysis to reveal previously unrecognized significant glucocorticoid excess in patients with primary hyperaldosteronism, labeled “Connshing” syndrome (281). They performed mass spectrometry-based analysis (GC-MS) of a 24-hour urine steroid metabolome in patients with primary aldosteronism in comparison to healthy controls, patients with endocrine inactive adrenal adenoma, patients with ACS, and with clinically overt adrenal cortisol excess. Patients with primary hyperaldosteronism had significantly increased cortisol and total glucocorticoid metabolite excretion. Several surrogate parameters of metabolic risk (including BMI, waist–hip ratio, fasting insulin, HOMA-IR, and high-density lipoprotein cholesterol) correlated significantly with glucocorticoid but not mineralocorticoid output.
Unilateral adrenalectomy resolved both mineralocorticoid and glucocorticoid excess, indeed, postoperative evidence of adrenal insufficiency as evidenced by a suboptimal cortisol response to synacthen testing was found in 29% of patients despite a normal preoperative dexamethasone suppression test.
These data are of significant interest given the other comorbidities reported in patients with primary hyperaldosteronism such as increased rates of insulin resistance/type 2 diabetes and osteoporosis, which were difficult to attribute to aldosterone effect per se (281). More research is needed in this area as it raises several important questions, not least the impact of this glucocorticoid excess in patients who are not surgically cured of their primary hyperaldosteronism but receive mineralocorticoid receptor antagonist therapy which has no antiglucocorticoid effect. Further prospective data are required to validate these retrospective studies.
There are several important future directions of research in this area including the potential to use a spot urine sample rather than a 24-hour collection and transferring this technology to an LC/MS-MS based high throughput platform which will be easily performed in routine biochemistry laboratories. In recent years, LC-MS/MS has also been used on serum samples to differentiate between benign and malignant adrenal disease (352,353).
Ultimately, the use of a noninvasive steroid metabolomic assessment may be able to risk-stratify patients rapidly and accurately, thus leading to prompt and appropriate therapy for patients with ACC and a reduction in the need for follow-up of patients with benign adrenal disease and unnecessary surgery for patients with radiologically indeterminate lesions. The combination of the above will hopefully lead to improved survival for patients with ACC as they are recognized and treated promptly and a decrease in healthcare costs (due to a reduction in surgical procedures) and exposure to ionizing radiation by reducing CT imaging in patients with benign disease (45).
Other diagnostic innovations
There are a number of other exciting developments in the field of adrenal tumors in terms of improved histopathological techniques that include In situ metabolomics utilizing high‑mass resolution matrix‑assisted laser desorption/ionization mass spectrometry imaging, which has been extensively reviewed by Papathomas et al. (206) and is beyond the scope of this review. Other advances include the use of molecular biology techniques to predict prognosis in patients with ACC (165,354-356) which may give the promise of delivering a more personalized approach to prognostication, treatment, and follow-up.
Functional imaging of the adrenal cortex.
Scintigraphy techniques have been used for imaging of the adrenal glands for several decades. iodine-131 labelled 6-beta-iodomethyl-19-norcholesterol (NP-59), a cholesterol analog that incorporates into low-density lipoproteins and accumulates in the adrenal cortex via a receptor-mediated process, has been used for imaging of the adrenal cortex as a marker of adrenal cholesterol metabolism since the 1970s (357). The emergence of integrated single-photon emission computed tomography-computed tomography (SPECT-CT) systems has led to a resurgence of interest in the use of NP-59 scintigraphy (358). Recent data have reported a positive predictive value of 92% for differentiation of aldosterone-producing adenoma from bilateral adrenal hyperplasia in primary aldosteronism, potentially reducing the need for invasive adrenal venous sampling (359). Limitations of NP-59 scintigraphy including the requirement for prolonged dexamethasone suppression, the need for sequential imaging over several days, and relatively high radiation dose, have stimulated the development of other functional imaging techniques in the diagnosis of primary aldosteronism (360).
Etomidate derivatives with high affinity and specificity for enzymes within the cytochrome P450 11B family (CYP11B) which are expressed exclusively within adrenocortical cells have been developed (361). CYP11B1 (11-beta-hydroxylase) and CYP11B2 (aldosterone synthetase) enzymes are key regulators of adrenal cortisol and aldosterone synthesis (362). Carbon-11 (11C) metomidate (MTO) PET-CT is a sensitive and specific technique for diagnosing adrenocortical tumors (363) and has high accuracy for lateralizing aldosterone secretion by Conn’s adenomas (364,365). The 20-minute half-life of 11C restricts the use of this tracer to centers with an on-site cyclotron and consequently, this technique is not widely available (Fig. 11). This limitation has led to the development of longer half-life radiotracers which are required before more widespread availability can be achieved. Recently, an 18F-labeled analog of MTO (18F-FAMTO) has been developed with high selectivity for CYP11B enzymes (366). 123I-labeled iodometomidate (IMTO) has also been evaluated as a potentially more widely available radiotracer (367). 123I-IMTO SPECT-CT permits highly specific characterization of adrenocortical tissue with lower radiation exposure and investigation than NP-59 scintigraphy (368) and also has reported value for the staging of ACC (369). Labeling of metomidate with iodine-131 offers the potential for targeted radionuclide therapy in advanced adrenocortical cancer but this requires validation in a prospective clinical trial (370).
Figure 11.
Carbon-11 metomidate PET-CT: Coronal PET maximum intensity projection and axial fused PET-CT images in a patient with a left adrenocortical carcinoma and an unsuspected tracer-avid right sided liver metastasis. Prominent physiological tracer uptake is present in the gastric wall and left renal collecting system. Images courtesy of Professor Anders Sundin, Consultant Radiologist, Uppsala University Hospital, Sweden.
Functional imaging of the adrenal medulla.
Iodine-labelled metaiodobenzylguanidine (MIBG), a guanethidine analog, has been used for functional imaging of tumors arising from the adrenal medulla for over 30 years (371). 123I-MIBG has significant limitations, including a 2-day imaging protocol and the need for thyroid blockade with potassium iodide prior to tracer injection (Fig. 12). 124I-MIBG has been evaluated as a potential PET imaging tracer but this undergoes complex decay with emission of high energy gamma radiation leading to poorer image quality and unfavorable dosimetry (372). Other PET tracers including dopamine analogs such as 18F-fluorodopamine and 18F-fluorodihydroxyphenylalanine (DOPA) which image norepinephrine (noradrenaline) and amino acid transporter expression, along with 11C-hydroxyephedrine, a catecholamine analog, have been used to evaluate tumors arising from the neural crest (373) (Fig. 13). These tracers are limited to highly specialized centers and the published data is limited to relatively small cohorts. Recently an 18F-labeled analog of MIBG has been developed, meta-fluorobenzylguanidine (18F-MFBG); preliminary data report high accuracy and favorable dosimetry in a single-day protocol overcoming some of the limitations of other tracers and showing promise for the future (374).
Figure 12.
Iodine-123 metaiodobenzylguanidine SPECT-CT. Anterior half-body planar view and axial fused SPECT-CT images in a patient with a large MIBG-avid right adrenal pheochromocytoma with an unsuspected tracer-avid bone metastasis within the manubrium.
Figure 13.
Carbon-11 hydroxyephedrine PET-CT. Coronal PET maximum intensity projection and axial fused PET-CT images in a patient with a left adrenal pheochromocytoma and an unsuspected tracer-avid subcentimeter right paratracheal node which was biopsied and confirmed to represent a nodal metastasis. Images courtesy of Professor Anders Sundin, Consultant Radiologist, Uppsala University Hospital, Sweden.
Textural analysis/radiomics
Radiomics is a relatively new area of research activity which involves the extraction of “invisible” quantitative features from medical imaging based on intensity, shape, volume, and textural features (375). Textural analysis permits the evaluation of spatial inter-relationships within lesions to quantify lesion heterogeneity (376). The potential to obtain additional data from standard-of-care imaging could improve diagnostic accuracy and help guide optimal patient management (377) (Fig. 14).
Figure 14.
CT textural analysis. Axial CT image showing left adrenal lesion segmentation (blue contours, top left) and adrenal lesion textural features displayed using fine (top right), medium (bottom left) and coarse (bottom right) filters using TexRADTM software. First-order textural parameters extracted from the lesion are tabulated below. SSF, spacial scaling factor; SD, standard deviation; MPP, mean of positive pixels.
Preliminary data on the use of CT textural analysis for the characterization of indeterminate adrenal lesions has shown promising results. In a feasibility study of 164 patients with indeterminate adrenal lesions at CT (98 pheochromocytoma; 66 lipid-poor adrenal adenomas), intralesion textural features (mean gray-level intensity and mean positive pixels) extracted from unenhanced images allowed differentiation between adenoma and pheochromocytoma with an accuracy of 81% (378). In a recent larger patient cohort (n = 225) the same Chinese group has reported an accuracy of 77% for distinguishing metastases from benign adrenal lesions using this CT textural feature analysis technique (379). Other groups have shown similar results in small retrospective series evaluating the accuracy of MRI and PET-CT textural features for distinguishing benign and malignant adrenal lesions (380,381).
Machine learning and imaging
There is a great interest in the use of artificial intelligence and machine learning techniques in medical imaging (382). The combination of textural analysis with machine learning classification may improve diagnostic accuracy and reproducibility. Early data evaluating the efficacy of textural analysis-derived parameters extracted from MRI of adrenal lesions in 60 patients using a machine learning approach showed a diagnostic accuracy of 80% compared to expert radiologist accuracy of 73% (383). A feasibility study assessing machine learning-based quantitative textural analysis of unenhanced CT in 108 patients with indeterminate adrenal lesions had a 94% accuracy for differentiating pheochromocytoma from lipid-poor adenoma (384). At present, there is insufficient evidence to support clinical translation, but these techniques have the potential to improve diagnostic accuracy and more informed decision making in the future. These initial findings warrant validation in a well-designed prospective multicenter clinical trial.
Conclusion
An AI is now established as a common endocrine diagnosis that requires a multidisciplinary approach for effective management. The majority of patients can be reassured and discharged, but a personalized approach based upon image analysis, endocrine workup, and clinical symptoms and signs is required in every case. ACC remains a real concern but is restricted to <2% of all cases. Functional AI lesions are commoner (but still probably <10% of total) and the greatest challenge remains the diagnosis and optimum management of ACS. Modern-day surgery has improved outcomes and novel radiological and urinary biomarkers will improve early detection and patient stratification in future years to come.
Acknowledgments
Financial Support: National Institute for Health Research (Senior Fellowship) Paul M. Stewart.
Glossary
Abbreviations
- 17-OHP
17-hydroxyprogesterone
- ACA
adrenocortical adenoma
- ACC
adrenocortical carcinoma
- ACS
autonomous cortisol secretion
- ACTH
adrenocorticotropin
- AI
adrenal incidentaloma
- BMI
body mass index
- CAH
congenital adrenal hyperplasia
- cAMP
3′,5′-cyclic adenosine 5′-monohosphate
- COMT
catechol-O-methyltransferase
- CT
computed tomography
- DHEA
dehydroepiandrosterone
- DHEAS
DHEA sulfate
- FDG
18-fluorodeoxyglucose
- GC-MS
gas chromatography-mass spectrometry
- HPA
hypothalamic–pituitary–adrenal
- HU
Hounsfield units
- LC-MS/MS
liquid chromatography tandem mass spectrometry
- MACE
mild autonomous cortisol excess
- MEN
multiple endocrine neoplasia
- MRI
magnetic resonance imaging
- MTO
metomidate
- NF1
neurofibromatosis type 1
- NFAT
nonfunctioning adrenal tumor
- PA
primary aldosteronism
- PET
positron emission tomography
- PKA
protein kinase A
- PBMAH
primary bilateral macronodular adrenal hyperplasia
- SPECT-CT
single-photon emission computed tomography-computed tomography
- SUV
standardized uptake value
- TH
tyrosine hydroxylase
- THS
tetrahydro-11-deoxycortisol
- UFC
urine free cortisol
- VHL
Von Hippel Lindau
Additional Information
Disclosure Summary: All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed. I certify that neither I nor my co-authors have a conflict of interest as described above that is relevant to the subject matter or materials included in this Work.
Data Availability
All data generated or analyzed during this study are included in this published article or in the data repositories listed in References.
References
- 1. Papanicolas I, Woskie LR, Jha AK. Health care spending in the united states and other high-income countries. JAMA. 2018;319(10):1024-1039. [DOI] [PubMed] [Google Scholar]
- 2. Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307(22):2400-2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Operational Information for Commissioning NE . Diagnostic Imaging Dataset Statistical Release: Provisional monthly statistics, November 2017 to November 2018. 2019.. https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2019/12/Annual-Statistical-Release-2018-19-PDF-1.9MB.pdf. [Google Scholar]
- 4. Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016;175(2):G1-G34. [DOI] [PubMed] [Google Scholar]
- 5. Geelhoed GW, Druy EM. Management of the adrenal “incidentaloma”. Surgery. 1982;92(5):866-874. [PubMed] [Google Scholar]
- 6. Zeiger MA, Thompson GB, Duh QY, et al. ; American Association of Clinical Endocrinologists; American Association of Endocrine Surgeons . The American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr Pract. 2009;15(Suppl 1):1-20. [DOI] [PubMed] [Google Scholar]
- 7. Tabarin A, Bardet S, Bertherat J, et al. ; French Society of Endocrinology Consensus . Exploration and management of adrenal incidentalomas. French Society of Endocrinology Consensus. Ann Endocrinol (Paris). 2008;69(6):487-500. [DOI] [PubMed] [Google Scholar]
- 8. Muth A, Hammarstedt L, Hellstrom M, et al. Swedish guidelines for the management of adrenal incidentalomas. Lakartidningen 2017;114. [PubMed] [Google Scholar]
- 9. Kokko JP, Brown TC, Berman MM. Adrenal adenoma and hypertension. Lancet. 1967;1(7488):468-470. [DOI] [PubMed] [Google Scholar]
- 10. Hedeland H, Ostberg G, Hökfelt B. On the prevalence of adrenocortical adenomas in an autopsy material in relation to hypertension and diabetes. Acta Med Scand. 1968;184(3):211-214. [DOI] [PubMed] [Google Scholar]
- 11. Russi S, Blumenthal HT, Gray SH. Small adenomas of the adrenal cortex in hypertension and diabetes. Arch Intern Med (Chic). 1945;76(5):284-291. [DOI] [PubMed] [Google Scholar]
- 12. Commons RR, Callaway CP. Adenomas of the adrenal cortex. Arch Intern Med (Chic). 1948;81(1):37-41. [DOI] [PubMed] [Google Scholar]
- 13. Schroeder HA, Davies DF. Studies on “essential” hypertension. V. An endocrine hypertensive syndrome. Ann Intern Med. 1954;40(3):516-539. [DOI] [PubMed] [Google Scholar]
- 14. Dévényi I. Possibility of normokalaemic primary aldosteronism as reflected in the frequency of adrenal cortical adenomas. J Clin Pathol. 1967;20(1):49-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Russell RP, Masi AT, Richter ED. Adrenal cortical adenomas and hypertension. A clinical pathologic analysis of 690 cases with matched controls and a review of the literature. Medicine (Baltimore). 1972;51(3):211-225. [PubMed] [Google Scholar]
- 16. Kawano M, Kodama T, Ito Y, Obara T, Fujimoto Y. Adrenal incidentaloma–report of 14 operated cases and analysis of 4-year autopsy series of Japan. Nihon Geka Gakkai Zasshi. 1989;90(12):2031-2036. [PubMed] [Google Scholar]
- 17. Kobayashi S, Iwase H, Matsuo K, Fukuoka H, Ito Y, Masaoka A. Primary adrenocortical tumors in autopsy records--a survey of “Cumulative Reports in Japan” from 1973 to 1984. Jpn J Surg 1991;21:494-498. [DOI] [PubMed] [Google Scholar]
- 18. Rinehart JF, Williams OO, Cappeller WS. Adenomatous hyperplasia of the adrenal cortex associated with essential hypertension. Arch Pathol 1941;32:169-177. [Google Scholar]
- 19. Dempsey WS. The adrenal cortex in essential hypertension. Arch Pathol 1942;34:1031-1034. [Google Scholar]
- 20. Dawson IM. Changes in the adrenal cortex in essential and renal hypertension. J Pathol Bacteriol 1956;122:393-409. [DOI] [PubMed] [Google Scholar]
- 21. Holmes RO, Moon HD, Rinehart JF. A morphologic study of adrenal glands with correlations of body size and heart size. Am J Pathol. 1951;27(4):724-726. [PubMed] [Google Scholar]
- 22. Shamma AH, Goddard JW, Sommers SC. A study of the adrenal status in hypertension. J Chronic Dis. 1958;8(5):587-595. [DOI] [PubMed] [Google Scholar]
- 23. Spain DM, Weinsaft P. Solitary adrenal cortical adenoma in elderly female; frequency. Arch Pathol. 1964;78:231-233. [PubMed] [Google Scholar]
- 24. Dobbie JW. Adrenocortical nodular hyperplasia: the ageing adrenal. J Pathol. 1969;99(1):1-18. [DOI] [PubMed] [Google Scholar]
- 25. Yamada EY, Fukunaga FH. Adrenal adenoma and hypertension. A study in the Japanese in Hawaii. Jpn Heart J. 1969;10(1):11-19. [DOI] [PubMed] [Google Scholar]
- 26. Granger P, Genest J. Autopsy study of adrenals in unselected normotensive and hypertensive patients. Can Med Assoc J. 1970;103(1):34-36. [PMC free article] [PubMed] [Google Scholar]
- 27. Abecassis M, McLoughlin MJ, Langer B, Kudlow JE. Serendipitous adrenal masses: prevalence, significance, and management. Am J Surg. 1985;149(6):783-788. [DOI] [PubMed] [Google Scholar]
- 28. Winkelmann M, Schoppe WD, Volk N, Bürrig KF, Jungblut RM, Schneider W. Correlation of abdominal CT imaging with autopsy findings in patients with malignant tumors. J Cancer Res Clin Oncol. 1987;113(3):279-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Meagher AP, Hugh TB, Casey JH, Chisholm DJ, Farrell JC, Yeates M. Primary adrenal tumours–a ten-year experience. Aust N Z J Surg. 1988;58(6):457-462. [DOI] [PubMed] [Google Scholar]
- 30. Reinhard C, Saeger W, Schubert B. Adrenocortical nodules in post-mortem series. Development, functional significance, and differentiation from adenomas. Gen Diagn Pathol. 1996;141(3-4):203-208. [PubMed] [Google Scholar]
- 31. Sington JD, Syn WK, Suvarna SK, et al. Lack of association between thyroid and adrenal nodules: a histological study. J Endocrinol Invest. 1999;22(4):262-265. [DOI] [PubMed] [Google Scholar]
- 32. Black WC, Welch HG. Advances in diagnostic imaging and overestimations of disease prevalence and the benefits of therapy. N Engl J Med. 1993;328(17):1237-1243. [DOI] [PubMed] [Google Scholar]
- 33. Glazer HS, Weyman PJ, Sagel SS, Levitt RG, McClennan BL. Nonfunctioning adrenal masses: incidental discovery on computed tomography. AJR Am J Roentgenol. 1982;139(1):81-85. [DOI] [PubMed] [Google Scholar]
- 34. Prinz RA, Brooks MH, Churchill R, et al. Incidental asymptomatic adrenal masses detected by computed tomographic scanning. Is operation required? JAMA. 1982;248(6):701-704. [PubMed] [Google Scholar]
- 35. Belldegrun A, Hussain S, Seltzer SE, Loughlin KR, Gittes RF, Richie JP. Incidentally discovered mass of the adrenal gland. Surg Gynecol Obstet. 1986;163(3):203-208. [PubMed] [Google Scholar]
- 36. Davenport E, Lang Ping Nam P, Wilson M, Reid A, Aspinall S. Adrenal incidentalomas: management in British district general hospitals. Postgrad Med J. 2014;90(1065):365-369. [DOI] [PubMed] [Google Scholar]
- 37. Maher DI, Williams E, Grodski S, Serpell JW, Lee JC. Adrenal incidentaloma follow-up is influenced by patient, radiologic, and medical provider factors: a review of 804 cases. Surgery. 2018;164(6):1360-1365. [DOI] [PubMed] [Google Scholar]
- 38. Taya M, Paroder V, Bellin E, Haramati LB. The relationship between adrenal incidentalomas and mortality risk. Eur Radiol. 2019;29(11):6245-6255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Herrera MF, Grant CS, van Heerden JA, Sheedy PF, Ilstrup DM. Incidentally discovered adrenal tumors: an institutional perspective. Surgery. 1991;110(6):1014-1021. [PubMed] [Google Scholar]
- 40. Caplan RH, Strutt PJ, Wickus GG. Subclinical hormone secretion by incidentally discovered adrenal masses. Arch Surg. 1994;129(3):291-296. [DOI] [PubMed] [Google Scholar]
- 41. Bovio S, Cataldi A, Reimondo G, et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest. 2006;29(4):298-302. [DOI] [PubMed] [Google Scholar]
- 42. Song JH, Chaudhry FS, Mayo-Smith WW. The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol. 2008;190(5):1163-1168. [DOI] [PubMed] [Google Scholar]
- 43. Hammarstedt L, Muth A, Wängberg B, et al. ; Adrenal Study Group of Western Sweden . Adrenal lesion frequency: a prospective, cross-sectional CT study in a defined region, including systematic re-evaluation. Acta Radiol. 2010;51(10):1149-1156. [DOI] [PubMed] [Google Scholar]
- 44. Davenport C, Liew A, Doherty B, et al. The prevalence of adrenal incidentaloma in routine clinical practice. Endocrine. 2011;40(1):80-83. [DOI] [PubMed] [Google Scholar]
- 45. Cawood TJ, Hunt PJ, O’Shea D, Cole D, Soule S. Recommended evaluation of adrenal incidentalomas is costly, has high false-positive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink? Eur J Endocrinol. 2009;161(4):513-527. [DOI] [PubMed] [Google Scholar]
- 46. Virkkala A, Välimäki M, Pelkonen R, et al. Endocrine abnormalities in patients with adrenal tumours incidentally discovered on computed tomography. Acta Endocrinol (Copenh). 1989;121(1):67-72. [DOI] [PubMed] [Google Scholar]
- 47. Aso Y, Homma Y. A survey on incidental adrenal tumors in Japan. J Urol. 1992;147(6):1478-1481. [DOI] [PubMed] [Google Scholar]
- 48. Reincke M, Nieke J, Krestin GP, Saeger W, Allolio B, Winkelmann W. Preclinical Cushing’s syndrome in adrenal “incidentalomas”: comparison with adrenal Cushing’s syndrome. J Clin Endocrinol Metab. 1992;75(3):826-832. [DOI] [PubMed] [Google Scholar]
- 49. Osella G, Terzolo M, Borretta G, et al. Endocrine evaluation of incidentally discovered adrenal masses (incidentalomas). J Clin Endocrinol Metab. 1994;79(6):1532-1539. [DOI] [PubMed] [Google Scholar]
- 50. Seppel T, Schlaghecke R. Augmented 17 alpha-hydroxyprogesterone response to ACTH stimulation as evidence of decreased 21-hydroxylase activity in patients with incidentally discovered adrenal tumours (‘incidentalomas’). Clin Endocrinol (Oxf). 1994;41(4):445-451. [DOI] [PubMed] [Google Scholar]
- 51. Ambrosi B, Peverelli S, Passini E, et al. Abnormalities of endocrine function in patients with clinically “silent” adrenal masses. Eur J Endocrinol. 1995;132(4):422-428. [DOI] [PubMed] [Google Scholar]
- 52. Bencsik Z, Szabolcs I, Góth M, et al. Incidentally detected adrenal tumours (incidentalomas): histological heterogeneity and differentiated therapeutic approach. J Intern Med. 1995;237(6):585-589. [DOI] [PubMed] [Google Scholar]
- 53. Flecchia D, Mazza E, Carlini M, et al. Reduced serum levels of dehydroepiandrosterone sulphate in adrenal incidentalomas: a marker of adrenocortical tumour. Clin Endocrinol (Oxf). 1995;42(2):129-134. [DOI] [PubMed] [Google Scholar]
- 54. Bardet S, Rohmer V, Murat A, et al. 131I-6 beta-iodomethylnorcholesterol scintigraphy: an assessment of its role in the investigation of adrenocortical incidentalomas. Clin Endocrinol (Oxf). 1996;44(5):587-596. [DOI] [PubMed] [Google Scholar]
- 55. Linos DA, Stylopoulos N, Raptis SA. Adrenaloma: a call for more aggressive management. World J Surg. 1996;20(7):788-792; discussion 792. [DOI] [PubMed] [Google Scholar]
- 56. Bastounis EA, Karayiannakis AJ, Anapliotou ML, Nakopoulou L, Makri GG, Papalambros EL. Incidentalomas of the adrenal gland: diagnostic and therapeutic implications. Am Surg. 1997;63(4):356-360. [PubMed] [Google Scholar]
- 57. Bondanelli M, Campo M, Trasforini G, et al. Evaluation of hormonal function in a series of incidentally discovered adrenal masses. Metabolism. 1997;46(1):107-113. [DOI] [PubMed] [Google Scholar]
- 58. Kasperlik-Zeluska AA, Rosłonowska E, Słowinska-Srzednicka J, et al. Incidentally discovered adrenal mass (incidentaloma): investigation and management of 208 patients. Clin Endocrinol (Oxf). 1997;46(1):29-37. [DOI] [PubMed] [Google Scholar]
- 59. Terzolo M, Osella G, Alì A, et al. Adrenal incidentaloma, a five year experience. Minerva Endocrinol. 1995;20(1):69-78. [PubMed] [Google Scholar]
- 60. Proye C, Jafari Manjili M, Combemale F, et al. Experience gained from operation of 103 adrenal incidentalomas. Langenbecks Arch Surg. 1998;383(5):330-333. [DOI] [PubMed] [Google Scholar]
- 61. Murai M, Baba S, Nakashima J, Tachibana M. Management of incidentally discovered adrenal masses. World J Urol. 1999;17(1):9-14. [DOI] [PubMed] [Google Scholar]
- 62. Tütüncü NB, Gedik O. Adrenal incidentaloma: report of 33 cases. J Surg Oncol. 1999;70(4):247-250. [DOI] [PubMed] [Google Scholar]
- 63. Favia G, Lumachi F, Basso S, D’Amico DF. Management of incidentally discovered adrenal masses and risk of malignancy. Surgery. 2000;128(6):918-924. [DOI] [PubMed] [Google Scholar]
- 64. Mantero F, Arnaldi G. Management approaches to adrenal incidentalomas. A view from Ancona, Italy. Endocrinol Metab Clin North Am. 2000;29(1):107-125, ix. [DOI] [PubMed] [Google Scholar]
- 65. Rossi R, Tauchmanova L, Luciano A, et al. Subclinical Cushing’s syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J Clin Endocrinol Metab. 2000;85(4):1440-1448. [DOI] [PubMed] [Google Scholar]
- 66. Mantero F, Terzolo M, Arnaldi G, et al. A survey on adrenal incidentaloma in Italy. Study Group on Adrenal Tumors of the Italian Society of Endocrinology. J Clin Endocrinol Metab. 2000;85(2):637-644. [DOI] [PubMed] [Google Scholar]
- 67. Tanabe A, Naruse M, Nishikawa T, et al. Autonomy of cortisol secretion in clinically silent adrenal incidentaloma. Horm Metab Res. 2001;33(7):444-450. [DOI] [PubMed] [Google Scholar]
- 68. Barzon L, Fallo F, Sonino N, Boscaro M. Development of overt Cushing’s syndrome in patients with adrenal incidentaloma. Eur J Endocrinol. 2002;146(1):61-66. [DOI] [PubMed] [Google Scholar]
- 69. Tsvetov G, Shimon I, Benbassat C. Adrenal incidentaloma: clinical characteristics and comparison between patients with and without extraadrenal malignancy. J Endocrinol Invest. 2007;30(8):647-652. [DOI] [PubMed] [Google Scholar]
- 70. Bhargav PR, Mishra A, Agarwal G, Agarwal A, Verma AK, Mishra SK. Adrenal incidentalomas: experience in a developing country. World J Surg. 2008;32(8):1802-1808. [DOI] [PubMed] [Google Scholar]
- 71. Kasperlik-Załuska AA, Otto M, Cichocki A, et al. Incidentally discovered adrenal tumors: a lesson from observation of 1,444 patients. Horm Metab Res. 2008;40(5):338-341. [DOI] [PubMed] [Google Scholar]
- 72. Vassilatou E, Vryonidou A, Michalopoulou S, et al. Hormonal activity of adrenal incidentalomas: results from a long-term follow-up study. Clin Endocrinol (Oxf). 2009;70(5):674-679. [DOI] [PubMed] [Google Scholar]
- 73. Comlekci A, Yener S, Ertilav S, et al. Adrenal incidentaloma, clinical, metabolic, follow-up aspects: single centre experience. Endocrine. 2010;37(1):40-46. [DOI] [PubMed] [Google Scholar]
- 74. Anagnostis P, Efstathiadou Z, Polyzos SA, et al. Long term follow-up of patients with adrenal incidentalomas–a single center experience and review of the literature. Exp Clin Endocrinol Diabetes. 2010;118(9):610-616. [DOI] [PubMed] [Google Scholar]
- 75. Giordano R, Marinazzo E, Berardelli R, et al. Long-term morphological, hormonal, and clinical follow-up in a single unit on 118 patients with adrenal incidentalomas. Eur J Endocrinol. 2010;162(4):779-785. [DOI] [PubMed] [Google Scholar]
- 76. Yener S, Ertilav S, Secil M, et al. Prospective evaluation of tumor size and hormonal status in adrenal incidentalomas. J Endocrinol Invest. 2010;33(1):32-36. [DOI] [PubMed] [Google Scholar]
- 77. Muth A, Hammarstedt L, Hellström M, Sigurjónsdóttir HÁ, Almqvist E, Wängberg B; Adrenal Study Group of Western Sweden . Cohort study of patients with adrenal lesions discovered incidentally. Br J Surg. 2011;98(10):1383-1391. [DOI] [PubMed] [Google Scholar]
- 78. Cho YY, Suh S, Joung JY, et al. Clinical characteristics and follow-up of Korean patients with adrenal incidentalomas. Korean J Intern Med. 2013;28(5):557-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Di Dalmazi G, Vicennati V, Garelli S, et al. Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. Lancet Diabetes Endocrinol. 2014;2(5):396-405. [DOI] [PubMed] [Google Scholar]
- 80. Hong AR, Kim JH, Park KS, et al. Optimal follow-up strategies for adrenal incidentalomas: reappraisal of the 2016 ESE-ENSAT guidelines in real clinical practice. Eur J Endocrinol 2017;177(6):475-483. [DOI] [PubMed] [Google Scholar]
- 81. Ahn SH, Kim JH, Baek SH, et al. Characteristics of adrenal incidentalomas in a large, prospective computed tomography-based multicenter study: the COAR study in Korea. Yonsei Med J. 2018;59(4):501-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Akkuş G, Evran M, Sert M, Ok F, Tetiker T. Multidisciplinary approach for patients with functional and non-functional adrenal masses and review of the literature. Health Sci Rep. 2018;1(3):e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Goh Z, Phillips I, Hunt PJ, Soule S, Cawood TJ. Characteristics of adrenal incidentalomas in a New Zealand centre. Intern Med J. 2018;48(2):173-178. [DOI] [PubMed] [Google Scholar]
- 84. Bülow B, Ahrén B; Swedish Research Council Study Group of Endocrine Abdominal Tumours . Adrenal incidentaloma–experience of a standardized diagnostic programme in the Swedish prospective study. J Intern Med. 2002;252(3):239-246. [DOI] [PubMed] [Google Scholar]
- 85. Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B. Incidentally discovered adrenal masses. Endocr Rev. 1995;16(4):460-484. [DOI] [PubMed] [Google Scholar]
- 86. Zeiger MA, Thompson GB, Duh QY, et al. ; American Association of Clinical Endocrinologists; American Association of Endocrine Surgeons . American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: executive summary of recommendations. Endocr Pract. 2009;15(5):450-453. [DOI] [PubMed] [Google Scholar]
- 87. Foti G, Malleo G, Faccioli N, Guerriero A, Furlani L, Carbognin G. Characterization of adrenal lesions using MDCT wash-out parameters: diagnostic accuracy of several combinations of intermediate and delayed phases. Radiol Med. 2018;123(11):833-840. [DOI] [PubMed] [Google Scholar]
- 88. Kim J, Bae KH, Choi YK, et al. Clinical characteristics for 348 patients with adrenal incidentaloma. Endocrinol Metab (Seoul). 2013;28(1):20-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Sangwaiya MJ, Boland GW, Cronin CG, Blake MA, Halpern EF, Hahn PF. Incidental adrenal lesions: accuracy of characterization with contrast-enhanced washout multidetector CT – 10-minute delayed imaging protocol revisited in a large patient cohort. Radiology. 2010;256(2):504-510. [DOI] [PubMed] [Google Scholar]
- 90. Hao M, Lopez D, Luque-Fernandez MA, et al. The lateralizing asymmetry of adrenal adenomas. J Endocr Soc. 2018;2(4):374-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Addison T. On the constitutional and local effects of disease of the supra-renal capsules 1855.
- 92. Stewart PM The adrenal cortex. In: Williams Textbook of Endocrinology. 10th ed. Larsen PR, Kronenberg HM, Melmed S, Polonsky KS, eds. Philadelphia, PA: Saunders; 2003):491-551. [Google Scholar]
- 93. Kölliker A Manual of Human Histology. Vol. 1. London: The Sydenham Society; 1853. [Google Scholar]
- 94. Mesiano S, Jaffe RB. Developmental and functional biology of the primate fetal adrenal cortex. Endocr Rev. 1997;18(3):378-403. [DOI] [PubMed] [Google Scholar]
- 95. Jaffe RB, Mesiano S, Smith R, Coulter CL, Spencer SJ, Chakravorty A. The regulation and role of fetal adrenal development in human pregnancy. Endocr Res. 1998;24(3-4):919-926. [DOI] [PubMed] [Google Scholar]
- 96. Willenberg HS, Bornstein SR. Adrenal cortex; development, anatomy, physiology. In: Feingold KR, Anawalt B, Boyce A, et al. , eds. Endotext [Internet]. South Dartmouth, MA: MDText.com, Inc.; 2000. Available from:https://www.ncbi.nlm.nih.gov/books/NBK278945/2000. [Google Scholar]
- 97. Xing Y, Lerario AM, Rainey W, Hammer GD. Development of adrenal cortex zonation. Endocrinol Metab Clin North Am. 2015;44(2):243-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. El-Khairi R, Martinez-Aguayo A, Ferraz-de-Souza B, Lin L, Achermann JC. Role of DAX-1 (NR0B1) and steroidogenic factor-1 (NR5A1) in human adrenal function. Endocr Dev. 2011;20:38-46. [DOI] [PubMed] [Google Scholar]
- 99. Lenard AThe history of research on the adrenals, 1563-1900. J Hist Med. 1951;6:496-505. [DOI] [PubMed] [Google Scholar]
- 100. Cesmebasi A, Du Plessis M, Iannatuono M, Shah S, Tubbs RS, Loukas M. A review of the anatomy and clinical significance of adrenal veins. Clin Anat. 2014;27(8):1253-1263. [DOI] [PubMed] [Google Scholar]
- 101. Cingam SR, Karanchi H Cancer, Adrenal Metastasis. Treasure Island, FL: StatPearls; 2019. [Google Scholar]
- 102. Marti JL, Millet J, Sosa JA, Roman SA, Carling T, Udelsman R. Spontaneous adrenal hemorrhage with associated masses: etiology and management in 6 cases and a review of 133 reported cases. World J Surg. 2012;36(1):75-82. [DOI] [PubMed] [Google Scholar]
- 103. Dobbie JW, Symington T. The human adrenal gland with special reference to the vasculature. J Endocrinol. 1966;34(4):479-489. [DOI] [PubMed] [Google Scholar]
- 104. Thomas JP, Oake RJ. An accurate method for measurement of aldosterone production. Biochem J. 1969;115(1):109-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Miller WL, Auchus RJ. The molecular biology, biochemistry, and physiology of human steroidogenesis and its disorders. Endocr Rev. 2011;32(1):81-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Stocco DM, Clark BJ. Regulation of the acute production of steroids in steroidogenic cells. Endocr Rev. 1996;17(3):221-244. [DOI] [PubMed] [Google Scholar]
- 107. Tischler AS, Pacak K, Eisenhofer G. The adrenal medulla and extra-adrenal paraganglia: then and now. Endocr Pathol. 2014;25(1):49-58. [DOI] [PubMed] [Google Scholar]
- 108. van Berkel A, Lenders JW, Timmers HJ. Diagnosis of endocrine disease: biochemical diagnosis of phaeochromocytoma and paraganglioma. Eur J Endocrinol. 2014;170(3):R109-R119. [DOI] [PubMed] [Google Scholar]
- 109. Erickson LA. Challenges in surgical pathology of adrenocortical tumours. Histopathology. 2018;72(1): 82-96. [DOI] [PubMed] [Google Scholar]
- 110. Papotti M, Duregon E, Volante M, McNicol AM. Pathology of the adrenal cortex: a reappraisal of the past 25 years focusing on adrenal cortical tumors. Endocr Pathol. 2014;25(1):35-48. [DOI] [PubMed] [Google Scholar]
- 111. Weiss LM. Comparative histologic study of 43 metastasizing and nonmetastasizing adrenocortical tumors. Am J Surg Pathol. 1984;8(3):163-169. [DOI] [PubMed] [Google Scholar]
- 112. Weiss LM, Medeiros LJ, Vickery AL Jr. Pathologic features of prognostic significance in adrenocortical carcinoma. Am J Surg Pathol. 1989;13(3):202-206. [DOI] [PubMed] [Google Scholar]
- 113. Nakamura Y, Yamazaki Y, Felizola SJ, et al. Adrenocortical carcinoma: review of the pathologic features, production of adrenal steroids, and molecular pathogenesis. Endocrinol Metab Clin North Am. 2015;44(2):399-410. [DOI] [PubMed] [Google Scholar]
- 114. Iino K, Sasano H, Yabuki N, et al. DNA topoisomerase II alpha and Ki-67 in human adrenocortical neoplasms: a possible marker of differentiation between adenomas and carcinomas. Mod Pathol. 1997;10(9):901-907. [PubMed] [Google Scholar]
- 115. McNicol AM. Lesions of the adrenal cortex. Arch Pathol Lab Med. 2008;132(8):1263-1271. [DOI] [PubMed] [Google Scholar]
- 116. Morimoto R, Satoh F, Murakami O, et al. Immunohistochemistry of a proliferation marker Ki67/MIB1 in adrenocortical carcinomas: Ki67/MIB1 labeling index is a predictor for recurrence of adrenocortical carcinomas. Endocr J. 2008;55(1):49-55. [DOI] [PubMed] [Google Scholar]
- 117. Schmitt A, Saremaslani P, Schmid S, et al. IGFII and MIB1 immunohistochemistry is helpful for the differentiation of benign from malignant adrenocortical tumours. Histopathology. 2006;49(3):298-307. [DOI] [PubMed] [Google Scholar]
- 118. Duregon E, Cappellesso R, Maffeis V, et al. Validation of the prognostic role of the “Helsinki Score” in 225 cases of adrenocortical carcinoma. Hum Pathol. 2017;62:1-7. [DOI] [PubMed] [Google Scholar]
- 119. Thompson LD. Pheochromocytoma of the Adrenal gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol. 2002;26(5):551-566. [DOI] [PubMed] [Google Scholar]
- 120. Wu D, Tischler AS, Lloyd RV, et al. Observer variation in the application of the Pheochromocytoma of the Adrenal Gland Scaled Score. Am J Surg Pathol. 2009;33(4):599-608. [DOI] [PubMed] [Google Scholar]
- 121. Kimura N, Takayanagi R, Takizawa N, et al. Pathological grading for predicting metastasis in phaeochromocytoma and paraganglioma. Endocr Relat Cancer. 2014;21(3):405-14. [DOI] [PubMed] [Google Scholar]
- 122. Koh JM, Ahn SH, Kim H, et al. Validation of pathological grading systems for predicting metastatic potential in pheochromocytoma and paraganglioma. PLoS One. 2017;12(11):e0187398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Kamilaris CDC, Stratakis CA. An update on adrenal endocrinology: significant discoveries in the last 10 years and where the field is heading in the next decade. Hormones (Athens). 2018;17(4):479-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Reznik Y, Lefebvre H, Rohmer V, et al. ; REHOS study group . Aberrant adrenal sensitivity to multiple ligands in unilateral incidentaloma with subclinical autonomous cortisol hypersecretion: a prospective clinical study. Clin Endocrinol (Oxf). 2004;61(3):311-319. [DOI] [PubMed] [Google Scholar]
- 125. Lampron A, Bourdeau I, Oble S, et al. Regulation of aldosterone secretion by several aberrant receptors including for glucose-dependent insulinotropic peptide in a patient with an aldosteronoma. J Clin Endocrinol Metab. 2009;94(3):750-756. [DOI] [PubMed] [Google Scholar]
- 126. Allolio B, Fassnacht M. Clinical review: adrenocortical carcinoma: clinical update. J Clin Endocrinol Metab. 2006;91(6):2027-2037. [DOI] [PubMed] [Google Scholar]
- 127. Ng L, Libertino JM. Adrenocortical carcinoma: diagnosis, evaluation and treatment. J Urol. 2003;169(1):5-11. [DOI] [PubMed] [Google Scholar]
- 128. Crucitti F, Bellantone R, Ferrante A, Boscherini M, Crucitti P. The Italian Registry for Adrenal Cortical Carcinoma: analysis of a multiinstitutional series of 129 patients. The ACC Italian Registry Study Group. Surgery. 1996;119(2):161-170. [DOI] [PubMed] [Google Scholar]
- 129. Icard P, Goudet P, Charpenay C, et al. Adrenocortical carcinomas: surgical trends and results of a 253-patient series from the French Association of Endocrine Surgeons study group. World J Surg. 2001;25(7):891-897. [DOI] [PubMed] [Google Scholar]
- 130. Wajchenberg BL, Albergaria Pereira MA, Medonca BB, et al. Adrenocortical carcinoma: clinical and laboratory observations. Cancer. 2000;88(4):711-736. [PubMed] [Google Scholar]
- 131. Schteingart DE, Giordano TJ, Benitez RS, et al. Overexpression of CXC chemokines by an adrenocortical carcinoma: a novel clinical syndrome. J Clin Endocrinol Metab. 2001;86(8):3968-3974. [DOI] [PubMed] [Google Scholar]
- 132. Hough AJ, Hollifield JW, Page DL, Hartmann WH. Prognostic factors in adrenal cortical tumors. A mathematical analysis of clinical and morphologic data. Am J Clin Pathol. 1979;72(3):390-399. [DOI] [PubMed] [Google Scholar]
- 133. Abiven G, Coste J, Groussin L, et al. Clinical and biological features in the prognosis of adrenocortical cancer: poor outcome of cortisol-secreting tumors in a series of 202 consecutive patients. J Clin Endocrinol Metab. 2006;91(7):2650-2655. [DOI] [PubMed] [Google Scholar]
- 134. Lindholm J, Juul S, Jørgensen JO, et al. Incidence and late prognosis of Cushing’s syndrome: a population-based study. J Clin Endocrinol Metab. 2001;86(1):117-123. [DOI] [PubMed] [Google Scholar]
- 135. Clayton RN, Jones PW, Reulen RC, et al. Mortality in patients with Cushing’s disease more than 10 years after remission: a multicentre, multinational, retrospective cohort study. Lancet Diabetes Endocrinol. 2016;4(7):569-576. [DOI] [PubMed] [Google Scholar]
- 136. Vanbrabant T, Fassnacht M, Assie G, Dekkers OM. Influence of hormonal functional status on survival in adrenocortical carcinoma: systematic review and meta-analysis. Eur J Endocrinol. 2018;179(6):429-436. [DOI] [PubMed] [Google Scholar]
- 137. Henley DJ, van Heerden JA, Grant CS, Carney JA, Carpenter PC. Adrenal cortical carcinoma–a continuing challenge. Surgery. 1983;94(6):926-931. [PubMed] [Google Scholar]
- 138. Bonnet-Serrano F, Bertherat J. Genetics of tumors of the adrenal cortex. Endocr Relat Cancer. 2018;25(3):R131-R152. [DOI] [PubMed] [Google Scholar]
- 139. Kim AC, Reuter AL, Zubair M, et al. Targeted disruption of beta-catenin in Sf1-expressing cells impairs development and maintenance of the adrenal cortex. Development. 2008;135(15):2593-2602. [DOI] [PubMed] [Google Scholar]
- 140. Polakis P. Wnt signaling and cancer. Genes Dev. 2000;14(15):1837-1851. [PubMed] [Google Scholar]
- 141. Bonnet S, Gaujoux S, Launay P, et al. Wnt/β-catenin pathway activation in adrenocortical adenomas is frequently due to somatic CTNNB1-activating mutations, which are associated with larger and nonsecreting tumors: a study in cortisol-secreting and -nonsecreting tumors. J Clin Endocrinol Metab. 2011;96(2):E419-E426. [DOI] [PubMed] [Google Scholar]
- 142. Sato Y, Maekawa S, Ishii R, et al. Recurrent somatic mutations underlie corticotropin-independent Cushing’s syndrome. Science. 2014;344(6186):917-920. [DOI] [PubMed] [Google Scholar]
- 143. Ronchi CL, Di Dalmazi G, Faillot S, et al. ; European Network for the Study of Adrenocortical Tumors (ENSAT) . Genetic landscape of sporadic unilateral adrenocortical adenomas without PRKACA p.Leu206Arg mutation. J Clin Endocrinol Metab. 2016;101(9):3526-3538. [DOI] [PubMed] [Google Scholar]
- 144. Bertherat J, Horvath A, Groussin L, et al. Mutations in regulatory subunit type 1A of cyclic adenosine 5’-monophosphate-dependent protein kinase (PRKAR1A): phenotype analysis in 353 patients and 80 different genotypes. J Clin Endocrinol Metab. 2009;94(6):2085-2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Kirschner LS, Carney JA, Pack SD, et al. Mutations of the gene encoding the protein kinase A type I-alpha regulatory subunit in patients with the Carney complex. Nat Genet. 2000;26(1):89-92. [DOI] [PubMed] [Google Scholar]
- 146. Bertherat J, Groussin L, Sandrini F, et al. Molecular and functional analysis of PRKAR1A and its locus (17q22-24) in sporadic adrenocortical tumors: 17q losses, somatic mutations, and protein kinase A expression and activity. Cancer Res. 2003;63(17):5308-5319. [PubMed] [Google Scholar]
- 147. Beuschlein F, Fassnacht M, Assié G, et al. Constitutive activation of PKA catalytic subunit in adrenal Cushing’s syndrome. N Engl J Med. 2013;470(11):1019-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Di Dalmazi G, Kisker C, Calebiro D, et al. Novel somatic mutations in the catalytic subunit of the protein kinase A as a cause of adrenal Cushing’s syndrome: a European multicentric study. J Clin Endocrinol Metab. 2014;99(10):E2093-E2100. [DOI] [PubMed] [Google Scholar]
- 149. Horvath A, Boikos S, Giatzakis C, et al. A genome-wide scan identifies mutations in the gene encoding phosphodiesterase 11A4 (PDE11A) in individuals with adrenocortical hyperplasia. Nat Genet. 2006;38(7):794-800. [DOI] [PubMed] [Google Scholar]
- 150. Rothenbuhler A, Horvath A, Libé R, et al. Identification of novel genetic variants in phosphodiesterase 8B (PDE8B), a cAMP-specific phosphodiesterase highly expressed in the adrenal cortex, in a cohort of patients with adrenal tumours. Clin Endocrinol (Oxf). 2012;77(2):195-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Boulkroun S, Beuschlein F, Rossi GP, et al. Prevalence, clinical, and molecular correlates of KCNJ5 mutations in primary aldosteronism. Hypertension. 2012;59(3):592-598. [DOI] [PubMed] [Google Scholar]
- 152. Zheng FF, Zhu LM, Nie AF, et al. Clinical characteristics of somatic mutations in Chinese patients with aldosterone-producing adenoma. Hypertension. 2015;65(3):622-628. [DOI] [PubMed] [Google Scholar]
- 153. Felizola SJ, Katsu K, Ise K, et al. Pre-B lymphocyte protein 3 (VPREB3) expression in the adrenal cortex: precedent for non-immunological roles in normal and neoplastic human tissues. Endocr Pathol. 2015;26(2):119-128. [DOI] [PubMed] [Google Scholar]
- 154. Åkerström T, Crona J, Delgado Verdugo A, et al. Comprehensive re-sequencing of adrenal aldosterone producing lesions reveal three somatic mutations near the KCNJ5 potassium channel selectivity filter. PLoS One. 2012;7(7):e41926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Zennaro MC, Boulkroun S, Fernandes-Rosa F. Genetic causes of functional adrenocortical adenomas. Endocr Rev. 2017;38(6):516-537. [DOI] [PubMed] [Google Scholar]
- 156. Beuschlein F, Boulkroun S, Osswald A, et al. Somatic mutations in ATP1A1 and ATP2B3 lead to aldosterone-producing adenomas and secondary hypertension. Nat Genet. 2013;45:440-444. [DOI] [PubMed] [Google Scholar]
- 157. Fernandes-Rosa FL, Daniil G, Orozco IJ, et al. A gain-of-function mutation in the CLCN2 chloride channel gene causes primary aldosteronism. Nat Genet. 2018;50(3):355-361. [DOI] [PubMed] [Google Scholar]
- 158. Scholl UI, Goh G, Stölting G, et al. Somatic and germline CACNA1D calcium channel mutations in aldosterone-producing adenomas and primary aldosteronism. Nat Genet. 2013;45(9):1050-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Fernandes-Rosa FL, Williams TA, Riester A, et al. Genetic spectrum and clinical correlates of somatic mutations in aldosterone-producing adenoma. Hypertension. 2014;64(2):354-361. [DOI] [PubMed] [Google Scholar]
- 160. Koch CA, Pacak K, Chrousos GP. The molecular pathogenesis of hereditary and sporadic adrenocortical and adrenomedullary tumors. J Clin Endocrinol Metab. 2002;87(12):5367-5384. [DOI] [PubMed] [Google Scholar]
- 161. Else T, Kim AC, Sabolch A, et al. Adrenocortical carcinoma. Endocr Rev. 2014;35(2):282-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Gicquel C, Bertagna X, Gaston V, et al. Molecular markers and long-term recurrences in a large cohort of patients with sporadic adrenocortical tumors. Cancer Res. 2001;61(18):6762-6767. [PubMed] [Google Scholar]
- 163. Libè R, Groussin L, Tissier F, et al. Somatic TP53 mutations are relatively rare among adrenocortical cancers with the frequent 17p13 loss of heterozygosity. Clin Cancer Res. 2007;13(3):844-850. [DOI] [PubMed] [Google Scholar]
- 164. Gaujoux S, Grabar S, Fassnacht M, et al. β-Catenin activation is associated with specific clinical and pathologic characteristics and a poor outcome in adrenocortical carcinoma. Clin Cancer Res. 2011;17(2):328-336. [DOI] [PubMed] [Google Scholar]
- 165. Assié G, Letouzé E, Fassnacht M, et al. Integrated genomic characterization of adrenocortical carcinoma. Nat Genet. 2014;46(6):607-612. [DOI] [PubMed] [Google Scholar]
- 166. Gicquel C, Bertagna X, Schneid H, et al. Rearrangements at the 11p15 locus and overexpression of insulin-like growth factor-II gene in sporadic adrenocortical tumors. J Clin Endocrinol Metab. 1994;78(6):1444-1453. [DOI] [PubMed] [Google Scholar]
- 167. Gicquel C, Raffin-Sanson ML, Gaston V, et al. Structural and functional abnormalities at 11p15 are associated with the malignant phenotype in sporadic adrenocortical tumors: study on a series of 82 tumors. J Clin Endocrinol Metab. 1997;82(8):2559-2565. [DOI] [PubMed] [Google Scholar]
- 168. Zheng S, Cherniack AD, Dewal N, et al. ; Cancer Genome Atlas Research Network . Comprehensive pan-genomic characterization of adrenocortical carcinoma. Cancer Cell. 2016;30(2):363. [DOI] [PubMed] [Google Scholar]
- 169. Angeli A, Osella G, Ali A, Terzolo M. Adrenal incidentaloma: an overview of clinical and epidemiological data from the National Italian Study Group. Horm Res. 1997;47:279-283. [DOI] [PubMed] [Google Scholar]
- 170. Barzon L, Scaroni C, Sonino N, et al. Incidentally discovered adrenal tumors: endocrine and scintigraphic correlates. J Clin Endocrinol Metab. 1998;83(1):55-62. [DOI] [PubMed] [Google Scholar]
- 171. Assié G, Libé R, Espiard S, et al. ARMC5 mutations in macronodular adrenal hyperplasia with Cushing’s syndrome. N Engl J Med. 2013;369(22):2105-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Alencar GA, Lerario AM, Nishi MY, et al. ARMC5 mutations are a frequent cause of primary macronodular adrenal hyperplasia. J Clin Endocrinol Metab. 2014;99(8):E1501-E1509. [DOI] [PubMed] [Google Scholar]
- 173. Gagliardi L, Schreiber AW, Hahn CN, et al. ARMC5 mutations are common in familial bilateral macronodular adrenal hyperplasia. J Clin Endocrinol Metab. 2014;99(9):E1784-E1792. [DOI] [PubMed] [Google Scholar]
- 174. Espiard S, Drougat L, Libé R, et al. ARMC5 mutations in a large cohort of primary macronodular adrenal hyperplasia: clinical and functional consequences. J Clin Endocrinol Metab. 2015;100(6):E926-E935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Faucz FR, Zilbermint M, Lodish MB, et al. Macronodular adrenal hyperplasia due to mutations in an armadillo repeat containing 5 (ARMC5) gene: a clinical and genetic investigation. J Clin Endocrinol Metab. 2014;99(6):E1113-E1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Guerrero MA, Schreinemakers JM, Vriens MR, et al. Clinical spectrum of pheochromocytoma. J Am Coll Surg. 2009;209(6):727-732. [DOI] [PubMed] [Google Scholar]
- 177. Beard CM, Sheps SG, Kurland LT, Carney JA, Lie JT. Occurrence of pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin Proc. 1983;58(12):802-804. [PubMed] [Google Scholar]
- 178. Pawlu C, Bausch B, Reisch N, Neumann HP, Genetic testing for pheochromocytoma associated syndromes. Ann Endocrinol (Paris). 2005;66(3):178-185. [DOI] [PubMed] [Google Scholar]
- 179. Neumann HP, Bausch B, McWhinney SR, et al. ; Freiburg-Warsaw-Columbus Pheochromocytoma Study Group . Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med. 2002;346(19):1459-1466. [DOI] [PubMed] [Google Scholar]
- 180. Lenders JW, Duh QY, Eisenhofer G, et al. ; Endocrine Society . Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915-1942. [DOI] [PubMed] [Google Scholar]
- 181. Eisenhofer G, Lenders JW, Timmers H, et al. Measurements of plasma methoxytyramine, normetanephrine, and metanephrine as discriminators of different hereditary forms of pheochromocytoma. Clin Chem. 2011;57(3):411-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Rosenberg SA, Diamond HD, Jaslowitz B, Craver LF. Lymphosarcoma: a review of 1269 cases. Medicine (Baltimore). 1961;40:31-84. [DOI] [PubMed] [Google Scholar]
- 183. Singh D, Kumar L, Sharma A, Vijayaraghavan M, Thulkar S, Tandon N. Adrenal involvement in non-Hodgkin’s lymphoma: four cases and review of literature. Leuk Lymphoma. 2004;45(4):789-794. [DOI] [PubMed] [Google Scholar]
- 184. Zhou L, Peng W, Wang C, Liu X, Shen Y, Zhou K. Primary adrenal lymphoma: radiological; pathological, clinical correlation. Eur J Radiol. 2012;81(3):401-405. [DOI] [PubMed] [Google Scholar]
- 185. Kung AW, Pun KK, Lam K, Wang C, Leung CY. Addisonian crisis as presenting feature in malignancies. Cancer. 1990;65(1):177-179. [DOI] [PubMed] [Google Scholar]
- 186. Lam KY, Lo CY. Metastatic tumours of the adrenal glands: a 30-year experience in a teaching hospital. Clin Endocrinol (Oxf). 2002;56(1):95-101. [DOI] [PubMed] [Google Scholar]
- 187. Lutz A, Stojkovic M, Schmidt M, Arlt W, Allolio B, Reincke M. Adrenocortical function in patients with macrometastases of the adrenal gland. Eur J Endocrinol. 2000;143(1):91-97. [DOI] [PubMed] [Google Scholar]
- 188. Canu L, Van Hemert JAW, Kerstens MN, et al. CT characteristics of pheochromocytoma: relevance for the evaluation of adrenal incidentaloma. J Clin Endocrinol Metab. 2019;104(2):312-318. [DOI] [PubMed] [Google Scholar]
- 189. Pacak K, Linehan WM, Eisenhofer G, Walther MM, Goldstein DS. Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med. 2001;134(4):315-329. [DOI] [PubMed] [Google Scholar]
- 190. Manger WM, Gifford RW. Pheochromocytoma. J Clin Hypertens (Greenwich). 2002;4(1):62-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Baxter MA, Hunter P, Thompson GR, London DR. Phaeochromocytomas as a cause of hypotension. Clin Endocrinol (Oxf). 1992;37(3):304-306. [DOI] [PubMed] [Google Scholar]
- 192. Bravo EL, Gifford RW Jr. Pheochromocytoma. Endocrinol Metab Clin North Am. 1993;22(2):329-341. [PubMed] [Google Scholar]
- 193. Kassim TA, Clarke DD, Mai VQ, Clyde PW, Mohamed Shakir KM. Catecholamine-induced cardiomyopathy. Endocr Pract. 2008;14(9):1137-1149. [DOI] [PubMed] [Google Scholar]
- 194. Kakoki K, Miyata Y, Shida Y, et al. Pheochromocytoma multisystem crisis treated with emergency surgery: a case report and literature review. BMC Res Notes. 2015;8:758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Pomares FJ, Cañas R, Rodriguez JM, Hernandez AM, Parrilla P, Tebar FJ. Differences between sporadic and multiple endocrine neoplasia type 2A phaeochromocytoma. Clin Endocrinol (Oxf). 1998;48(2):195-200. [DOI] [PubMed] [Google Scholar]
- 196. Walther MM, Reiter R, Keiser HR, et al. Clinical and genetic characterization of pheochromocytoma in von Hippel-Lindau families: comparison with sporadic pheochromocytoma gives insight into natural history of pheochromocytoma. J Urol. 1999;162(3 Pt 1):659-664. [DOI] [PubMed] [Google Scholar]
- 197. Buitenwerf E, Korteweg T, Visser A, et al. Unenhanced CT imaging is highly sensitive to exclude pheochromocytoma: a multicenter study. Eur J Endocrinol. 2018;178(5):431-437. [DOI] [PubMed] [Google Scholar]
- 198. Blake MA, Krishnamoorthy SK, Boland GW, et al. Low-density pheochromocytoma on CT: a mimicker of adrenal adenoma. AJR Am J Roentgenol. 2003;181(6):1663-1668. [DOI] [PubMed] [Google Scholar]
- 199. Stolk RF, Bakx C, Mulder J, Timmers HJ, Lenders JW. Is the excess cardiovascular morbidity in pheochromocytoma related to blood pressure or to catecholamines? J Clin Endocrinol Metab. 2013;98(3):1100-1106. [DOI] [PubMed] [Google Scholar]
- 200. Zelinka T, Petrák O, Turková H, et al. High incidence of cardiovascular complications in pheochromocytoma. Horm Metab Res. 2012;44(5):379-384. [DOI] [PubMed] [Google Scholar]
- 201. Eisenhofer G, Pacak K, Huynh TT, et al. Catecholamine metabolomic and secretory phenotypes in phaeochromocytoma. Endocr Relat Cancer. 2011;18(1):97-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Därr R, Kuhn M, Bode C, et al. Accuracy of recommended sampling and assay methods for the determination of plasma-free and urinary fractionated metanephrines in the diagnosis of pheochromocytoma and paraganglioma: a systematic review. Endocrine. 2017;56(3):495-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Lenders JW, Pacak K, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: which test is best? JAMA. 2002;287(11):1427-1434. [DOI] [PubMed] [Google Scholar]
- 204. Eisenhofer G, Lattke P, Herberg M, et al. Reference intervals for plasma free metanephrines with an age adjustment for normetanephrine for optimized laboratory testing of phaeochromocytoma. Ann Clin Biochem. 2013;50(Pt 1):62-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Eisenhofer G, Prejbisz A, Peitzsch M, et al. Biochemical diagnosis of chromaffin cell tumors in patients at high and low risk of disease: plasma versus urinary free or deconjugated O-methylated catecholamine metabolites. Clin Chem. 2018;64(11):1646-1656. [DOI] [PubMed] [Google Scholar]
- 206. Papathomas TG, Sun N, Chortis V, et al. Novel methods in adrenal research: a metabolomics approach. Histochem Cell Biol. 2019;151(3):201-216. [DOI] [PubMed] [Google Scholar]
- 207. Eisenhofer G, Goldstein DS, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: how to distinguish true- from false-positive test results. J Clin Endocrinol Metab. 2003;88(6):2656-2666. [DOI] [PubMed] [Google Scholar]
- 208. de Jong WH, Eisenhofer G, Post WJ, Muskiet FA, de Vries EG, Kema IP. Dietary influences on plasma and urinary metanephrines: implications for diagnosis of catecholamine-producing tumors. J Clin Endocrinol Metab. 2009;94(8):2841-2849. [DOI] [PubMed] [Google Scholar]
- 209. Casey R, Griffin TP, Wall D, Dennedy MC, Bell M, O’Shea PM. Screening for phaeochromocytoma and paraganglioma: impact of using supine reference intervals for plasma metanephrines with samples collected from fasted/seated patients. Ann Clin Biochem. 2017;54(1):170-173. [DOI] [PubMed] [Google Scholar]
- 210. Därr R, Pamporaki C, Peitzsch M, et al. Biochemical diagnosis of phaeochromocytoma using plasma-free normetanephrine, metanephrine and methoxytyramine: importance of supine sampling under fasting conditions. Clin Endocrinol (Oxf). 2014;80(4):478-486. [DOI] [PubMed] [Google Scholar]
- 211. Plouin PF, Amar L, Dekkers OM, et al. ; Guideline Working Group . European Society of Endocrinology Clinical Practice Guideline for long-term follow-up of patients operated on for a phaeochromocytoma or a paraganglioma. Eur J Endocrinol. 2016;174(5):G1-G10. [DOI] [PubMed] [Google Scholar]
- 212. Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008;93(5):1526-1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. El-Farhan N, Rees DA, Evans C. Measuring cortisol in serum, urine and saliva - are our assays good enough? Ann Clin Biochem. 2017;54(3):308-322. [DOI] [PubMed] [Google Scholar]
- 214. Boscaro M, Arnaldi G. Approach to the patient with possible Cushing’s syndrome. J Clin Endocrinol Metab. 2009;94(9):3121-3131. [DOI] [PubMed] [Google Scholar]
- 215. Terzolo M, Bovio S, Reimondo G, et al. Subclinical Cushing’s syndrome in adrenal incidentalomas. Endocrinol Metab Clin North Am. 2005;34(2):423-39, x. [DOI] [PubMed] [Google Scholar]
- 216. Reincke M, Fassnacht M, Väth S, Mora P, Allolio B. Adrenal incidentalomas: a manifestation of the metabolic syndrome? Endocr Res. 1996;22(4):757-761. [DOI] [PubMed] [Google Scholar]
- 217. Fernández-Real JM, Engel WR, Simó R, Salinas I, Webb SM. Study of glucose tolerance in consecutive patients harbouring incidental adrenal tumours. Study Group of Incidental Adrenal Adenoma. Clin Endocrinol (Oxf). 1998;49(1):53-61. [DOI] [PubMed] [Google Scholar]
- 218. Terzolo M, Bovio S, Pia A, et al. Midnight serum cortisol as a marker of increased cardiovascular risk in patients with a clinically inapparent adrenal adenoma. Eur J Endocrinol. 2005;153(2):307-315. [DOI] [PubMed] [Google Scholar]
- 219. Tauchmanovà L, Rossi R, Biondi B, et al. Patients with subclinical Cushing’s syndrome due to adrenal adenoma have increased cardiovascular risk. J Clin Endocrinol Metab. 2002;87(11):4872-4878. [DOI] [PubMed] [Google Scholar]
- 220. Debono M, Bradburn M, Bull M, Harrison B, Ross RJ, Newell-Price J. Cortisol as a marker for increased mortality in patients with incidental adrenocortical adenomas. J Clin Endocrinol Metab. 2014;99(12):4462-4470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Grumbach MM, Biller BM, Braunstein GD, et al. Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med. 2003;138(5):424-429. [DOI] [PubMed] [Google Scholar]
- 222. Terzolo M, Stigliano A, Chiodini I, et al. ; Italian Association of Clinical Endocrinologists . AME position statement on adrenal incidentaloma. Eur J Endocrinol. 2011;164(6):851-870. [DOI] [PubMed] [Google Scholar]
- 223. Lee JM, Kim MK, Ko SH, et al. ; Korean Endocrine Society, Committee for Clinical Practice Guidelines . Clinical guidelines for the management of adrenal incidentaloma. Endocrinol Metab (Seoul). 2017;32(2):200-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Yanase T, Oki Y, Katabami T, et al. New diagnostic criteria of adrenal subclinical Cushing’s syndrome: opinion from the Japan Endocrine Society. Endocr J. 2018;65(4):383-393. [DOI] [PubMed] [Google Scholar]
- 225. Pecori Giraldi F, Ambrogio AG, De Martin M, Fatti LM, Scacchi M, Cavagnini F. Specificity of first-line tests for the diagnosis of Cushing’s syndrome: assessment in a large series. J Clin Endocrinol Metab. 2007;92(11):4123-4129. [DOI] [PubMed] [Google Scholar]
- 226. Viardot A, Huber P, Puder JJ, Zulewski H, Keller U, Müller B. Reproducibility of nighttime salivary cortisol and its use in the diagnosis of hypercortisolism compared with urinary free cortisol and overnight dexamethasone suppression test. J Clin Endocrinol Metab. 2005;90(10):5730-5736. [DOI] [PubMed] [Google Scholar]
- 227. Ferreira L, Oliveira JC, Palma I. Screening tests for hypercortisolism in patients with adrenal incidentaloma. J Endocrinol Metab. 2018;8(4):62-68. [Google Scholar]
- 228. Ceccato F, Antonelli G, Frigo AC, et al. First-line screening tests for Cushing’s syndrome in patients with adrenal incidentaloma: the role of urinary free cortisol measured by LC-MS/MS. J Endocrinol Invest. 2017;40(7):753-760. [DOI] [PubMed] [Google Scholar]
- 229. Chiodini I, Torlontano M, Carnevale V, et al. Bone loss rate in adrenal incidentalomas: a longitudinal study. J Clin Endocrinol Metab. 2001;86(11):5337-5341. [DOI] [PubMed] [Google Scholar]
- 230. Chiodini I, Morelli V, Salcuni AS, et al. Beneficial metabolic effects of prompt surgical treatment in patients with an adrenal incidentaloma causing biochemical hypercortisolism. J Clin Endocrinol Metab. 2010;95(6):2736-2745. [DOI] [PubMed] [Google Scholar]
- 231. Valli N, Catargi B, Ronci N, et al. Biochemical screening for subclinical cortisol-secreting adenomas amongst adrenal incidentalomas. Eur J Endocrinol. 2001;144(4):401-408. [DOI] [PubMed] [Google Scholar]
- 232. Raff H, Raff JL, Findling JW. Late-night salivary cortisol as a screening test for Cushing’s syndrome. J Clin Endocrinol Metab. 1998;83(8):2681-2686. [DOI] [PubMed] [Google Scholar]
- 233. Palmieri S, Morelli V, Polledri E, et al. The role of salivary cortisol measured by liquid chromatography-tandem mass spectrometry in the diagnosis of subclinical hypercortisolism. Eur J Endocrinol. 2013;168(3):289-296. [DOI] [PubMed] [Google Scholar]
- 234. Zerikly RK, Amiri L, Faiman C, et al. Diagnostic characteristics of late-night salivary cortisol using liquid chromatography-tandem mass spectrometry. J Clin Endocrinol Metab. 2010;95(10):4555-4559. [DOI] [PubMed] [Google Scholar]
- 235. Masserini B, Morelli V, Bergamaschi S, et al. The limited role of midnight salivary cortisol levels in the diagnosis of subclinical hypercortisolism in patients with adrenal incidentaloma. Eur J Endocrinol. 2009;160(1):87-92. [DOI] [PubMed] [Google Scholar]
- 236. Dennedy MC, Annamalai AK, Prankerd-Smith O, et al. Low DHEAS: a sensitive and specific test for the detection of subclinical hypercortisolism in adrenal incidentalomas. J Clin Endocrinol Metab. 2017;102(3):786-792. [DOI] [PubMed] [Google Scholar]
- 237. Masjkur J, Gruber M, Peitzsch M, et al. Plasma steroid profiles in subclinical compared with overt adrenal Cushing syndrome. J Clin Endocrinol Metab. 2019;104(10):4331-4340. [DOI] [PubMed] [Google Scholar]
- 238. Ueland GÅ, Methlie P, Kellmann R, et al. Simultaneous assay of cortisol and dexamethasone improved diagnostic accuracy of the dexamethasone suppression test. Eur J Endocrinol. 2017;176(6):705-713. [DOI] [PubMed] [Google Scholar]
- 239. Ceccato F, Barbot M, Albiger N, et al. Daily salivary cortisol and cortisone rhythm in patients with adrenal incidentaloma. Endocrine. 2018;59(3):510-519. [DOI] [PubMed] [Google Scholar]
- 240. Elamin MB, Murad MH, Mullan R, et al. Accuracy of diagnostic tests for Cushing’s syndrome: a systematic review and metaanalyses. J Clin Endocrinol Metab. 2008;93(5):1553-1562. [DOI] [PubMed] [Google Scholar]
- 241. Di Dalmazi G, Vicennati V, Rinaldi E, et al. Progressively increased patterns of subclinical cortisol hypersecretion in adrenal incidentalomas differently predict major metabolic and cardiovascular outcomes: a large cross-sectional study. Eur J Endocrinol. 2012;166(4):669-677. [DOI] [PubMed] [Google Scholar]
- 242. Chiodini I, Tauchmanovà L, Torlontano M, et al. Bone involvement in eugonadal male patients with adrenal incidentaloma and subclinical hypercortisolism. J Clin Endocrinol Metab. 2002;87(12):5491-5494. [DOI] [PubMed] [Google Scholar]
- 243. Tsuiki M, Tanabe A, Takagi S, Naruse M, Takano K. Cardiovascular risks and their long-term clinical outcome in patients with subclinical Cushing’s syndrome. Endocr J. 2008;55(4):737-745. [DOI] [PubMed] [Google Scholar]
- 244. Morelli V, Reimondo G, Giordano R, et al. Long-term follow-up in adrenal incidentalomas: an Italian multicenter study. J Clin Endocrinol Metab. 2014;99(3):827-834. [DOI] [PubMed] [Google Scholar]
- 245. Morelli V, Palmieri S, Lania A, et al. Cardiovascular events in patients with mild autonomous cortisol secretion: analysis with artificial neural networks. Eur J Endocrinol. 2017;177(1):73-83. [DOI] [PubMed] [Google Scholar]
- 246. Sbardella E, Minnetti M, D’Aluisio D, et al. Cardiovascular features of possible autonomous cortisol secretion in patients with adrenal incidentalomas. Eur J Endocrinol. 2018;178(5):501-511. [DOI] [PubMed] [Google Scholar]
- 247. Park J, De Luca A, Dutton H, Malcolm JC, Doyle MA. Cardiovascular outcomes in autonomous cortisol secretion and nonfunctioning adrenal adenoma: a systematic review. J Endocr Soc. 2019;3(5):996-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Giordano R, Guaraldi F, Berardelli R, et al. Glucose metabolism in patients with subclinical Cushing’s syndrome. Endocrine. 2012;41(3):415-423. [DOI] [PubMed] [Google Scholar]
- 249. Di Dalmazi G, Fanelli F, Mezzullo M, et al. Steroid profiling by LC-MS/MS in nonsecreting and subclinical cortisol-secreting adrenocortical adenomas. J Clin Endocrinol Metab. 2015;100(9):3529-3538. [DOI] [PubMed] [Google Scholar]
- 250. Perysinakis I, Marakaki C, Avlonitis S, et al. Laparoscopic adrenalectomy in patients with subclinical Cushing syndrome. Surg Endosc. 2013;27(6):2145-2148. [DOI] [PubMed] [Google Scholar]
- 251. Iacobone M, Citton M, Viel G, et al. Adrenalectomy may improve cardiovascular and metabolic impairment and ameliorate quality of life in patients with adrenal incidentalomas and subclinical Cushing’s syndrome. Surgery. 2012;152(6):991-997. [DOI] [PubMed] [Google Scholar]
- 252. Maehana T, Tanaka T, Itoh N, Masumori N, Tsukamoto T. Clinical outcomes of surgical treatment and longitudinal non-surgical observation of patients with subclinical Cushing’s syndrome and nonfunctioning adrenocortical adenoma. Indian J Urol. 2012;28(2):179-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Guerrieri M, Campagnacci R, Patrizi A, Romiti C, Arnaldi G, Boscaro M. Primary adrenal hypercortisolism: minimally invasive surgical treatment or medical therapy? A retrospective study with long-term follow-up evaluation. Surg Endosc. 2010;24(10):2542-2546. [DOI] [PubMed] [Google Scholar]
- 254. Chiodini I, Vainicher CE, Morelli V, et al. Mechanisms in endocrinology: endogenous subclinical hypercortisolism and bone: a clinical review. Eur J Endocrinol. 2016;175(6):R265-R282. [DOI] [PubMed] [Google Scholar]
- 255. Toniato A, Merante-Boschin I, Opocher G, Pelizzo MR, Schiavi F, Ballotta E. Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann Surg. 2009;249(3):388-391. [DOI] [PubMed] [Google Scholar]
- 256. Salcuni AS, Morelli V, Eller Vainicher C, et al. Adrenalectomy reduces the risk of vertebral fractures in patients with monolateral adrenal incidentalomas and subclinical hypercortisolism. Eur J Endocrinol. 2016;174(3):261-269. [DOI] [PubMed] [Google Scholar]
- 257. Iacobone M, Citton M, Scarpa M, Viel G, Boscaro M, Nitti D. Systematic review of surgical treatment of subclinical Cushing’s syndrome. Br J Surg. 2015;102(4):318-330. [DOI] [PubMed] [Google Scholar]
- 258. Hardy RS, Zhou H, Seibel MJ, Cooper MS. Glucocorticoids and bone: consequences of endogenous and exogenous excess and replacement therapy. Endocr Rev. 2018;39(5):519-548. [DOI] [PubMed] [Google Scholar]
- 259. Torlontano M, Chiodini I, Pileri M, et al. Altered bone mass and turnover in female patients with adrenal incidentaloma: the effect of subclinical hypercortisolism. J Clin Endocrinol Metab. 1999;84(7):2381-2385. [DOI] [PubMed] [Google Scholar]
- 260. Sartorio A, Conti A, Ferrero S, et al. Evaluation of markers of bone and collagen turnover in patients with active and preclinical Cushing’s syndrome and in patients with adrenal incidentaloma. Eur J Endocrinol. 1998;138(2):146-152. [DOI] [PubMed] [Google Scholar]
- 261. Francucci CM, Pantanetti P, Garrapa GG, Massi F, Arnaldi G, Mantero F. Bone metabolism and mass in women with Cushing’s syndrome and adrenal incidentaloma. Clin Endocrinol (Oxf). 2002;57(5):587-593. [DOI] [PubMed] [Google Scholar]
- 262. Hadjidakis D, Tsagarakis S, Roboti C, et al. Does subclinical hypercortisolism adversely affect the bone mineral density of patients with adrenal incidentalomas? Clin Endocrinol (Oxf). 2003;58(1):72-77. [DOI] [PubMed] [Google Scholar]
- 263. Osella G, Reimondo G, Peretti P, et al. The patients with incidentally discovered adrenal adenoma (incidentaloma) are not at increased risk of osteoporosis. J Clin Endocrinol Metab. 2001;86(2):604-607. [DOI] [PubMed] [Google Scholar]
- 264. Chiodini I, Morelli V, Masserini B, et al. Bone mineral density, prevalence of vertebral fractures, and bone quality in patients with adrenal incidentalomas with and without subclinical hypercortisolism: an Italian multicenter study. J Clin Endocrinol Metab. 2009;94(9):3207-3214. [DOI] [PubMed] [Google Scholar]
- 265. Tauchmanovà L, Pivonello R, De Martino MC, et al. Effects of sex steroids on bone in women with subclinical or overt endogenous hypercortisolism. Eur J Endocrinol. 2007;157(3):359-366. [DOI] [PubMed] [Google Scholar]
- 266. Tauchmanovà L, Rossi R, Nuzzo V, et al. Bone loss determined by quantitative ultrasonometry correlates inversely with disease activity in patients with endogenous glucocorticoid excess due to adrenal mass. Eur J Endocrinol. 2001;145(3):241-247. [DOI] [PubMed] [Google Scholar]
- 267. Perogamvros I, Vassiliadi DA, Karapanou O, Botoula E, Tzanela M, Tsagarakis S. Biochemical and clinical benefits of unilateral adrenalectomy in patients with subclinical hypercortisolism and bilateral adrenal incidentalomas. Eur J Endocrinol. 2015;173(6):719-725. [DOI] [PubMed] [Google Scholar]
- 268. Goh Z, Phillips I, Hunt PJ, Soule S, Cawood TJ. Three-year follow up of adrenal incidentalomas in a New Zealand centre. Intern Med J. 2020;50(3):350-356. [DOI] [PubMed] [Google Scholar]
- 269. Elhassan YS, Alahdab F, Prete A, et al. Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: a systematic review and meta-analysis. Ann Intern Med. 2019;171(2):107-116. [DOI] [PubMed] [Google Scholar]
- 270. Stavropoulos K, Imprialos KP, Katsiki N, et al. Primary aldosteronism in patients with adrenal incidentaloma: is screening appropriate for everyone? J Clin Hypertens (Greenwich). 2018;20(5):942-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Bernini G, Moretti A, Argenio G, Salvetti A. Primary aldosteronism in normokalemic patients with adrenal incidentalomas. Eur J Endocrinol. 2002;146(4):523-529. [DOI] [PubMed] [Google Scholar]
- 272. Markou A, Pappa T, Kaltsas G, et al. Evidence of primary aldosteronism in a predominantly female cohort of normotensive individuals: a very high odds ratio for progression into arterial hypertension. J Clin Endocrinol Metab. 2013;98(4):1409-1416. [DOI] [PubMed] [Google Scholar]
- 273. Médeau V, Moreau F, Trinquart L, et al. Clinical and biochemical characteristics of normotensive patients with primary aldosteronism: a comparison with hypertensive cases. Clin Endocrinol (Oxf). 2008;69(1):20-28. [DOI] [PubMed] [Google Scholar]
- 274. Moradi S, Shafiepour M, Amirbaigloo A. A woman with normotensive primary hyperaldosteronism. Acta Med Iran. 2016;54(2):156-158. [PubMed] [Google Scholar]
- 275. Young WF. Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol (Oxf). 2007;66(5):607-618. [DOI] [PubMed] [Google Scholar]
- 276. Mulatero P, Stowasser M, Loh KC, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89(3):1045-1050. [DOI] [PubMed] [Google Scholar]
- 277. Rossi GP, Bernini G, Caliumi C, et al. ; PAPY Study Investigators . A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48(11):2293-2300. [DOI] [PubMed] [Google Scholar]
- 278. Monticone S, D’Ascenzo F, Moretti C, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6(1):41-50. [DOI] [PubMed] [Google Scholar]
- 279. Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(1):51-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Rossi GP, Bernini G, Desideri G, et al. ; PAPY Study Participants . Renal damage in primary aldosteronism: results of the PAPY study. Hypertension. 2006;48(2):232-238. [DOI] [PubMed] [Google Scholar]
- 281. Arlt W, Lang K, Sitch AJ, et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight. 2017;2(8):e93136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Salcuni AS, Carnevale V, Battista C, et al. Primary aldosteronism as a cause of secondary osteoporosis. Eur J Endocrinol. 2017;177(5):431-437. [DOI] [PubMed] [Google Scholar]
- 283. Espiard S, Benomar K, Loyer C, Vahé C, Vantyghem MC. European recommendations for the management of adrenal incidentalomas: a debate on patients follow-up. Ann Endocrinol (Paris). 2018;79(1):45-48. [DOI] [PubMed] [Google Scholar]
- 284. Funder JW, Carey RM, Mantero F, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(5):1889-1916. [DOI] [PubMed] [Google Scholar]
- 285. Brown JM, Robinson-Cohen C, Luque-Fernandez MA, et al. The spectrum of subclinical primary aldosteronism and incident hypertension: a cohort study. Ann Intern Med. 2017;167(9):630-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286. Kamenicky P, Houdoin L, Ferlicot S, et al. Benign cortisol-secreting adrenocortical adenomas produce small amounts of androgens. Clin Endocrinol (Oxf). 2007;66(6):778-788. [DOI] [PubMed] [Google Scholar]
- 287. Fassnacht M, Libé R, Kroiss M, Allolio B. Adrenocortical carcinoma: a clinician’s update. Nat Rev Endocrinol. 2011;7(6):323-335. [DOI] [PubMed] [Google Scholar]
- 288. Moreno S, Guillermo M, Decoulx M, Dewailly D, Bresson R, Proye Ch. Feminizing adreno-cortical carcinomas in male adults. A dire prognosis. Three cases in a series of 801 adrenalectomies and review of the literature. Ann Endocrinol (Paris). 2006;67(1):32-38. [DOI] [PubMed] [Google Scholar]
- 289. Moreno S, Montoya G, Armstrong J, et al. Profile and outcome of pure androgen-secreting adrenal tumors in women: experience of 21 cases. Surgery. 2004;136(6):1192-1198. [DOI] [PubMed] [Google Scholar]
- 290. NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens State Sci Statements. 2002;19(2):1-25. [PubMed] [Google Scholar]
- 291. Dinnes J, Bancos I, Ferrante di Ruffano L, et al. Management of endocrine disease: imaging for the diagnosis of malignancy in incidentally discovered adrenal masses: a systematic review and meta-analysis. Eur J Endocrinol. 2016;175(2):R51-R64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292. Taffel M, Haji-Momenian S, Nikolaidis P, Miller FH. Adrenal imaging: a comprehensive review. Radiol Clin North Am. 2012;50(2):219-243, v. [DOI] [PubMed] [Google Scholar]
- 293. Blake MA, Holalkere NS, Boland GW. Imaging techniques for adrenal lesion characterization. Radiol Clin North Am. 2008;46(1):65-78, vi. [DOI] [PubMed] [Google Scholar]
- 294. Boland GW, Lee MJ, Gazelle GS, Halpern EF, McNicholas MM, Mueller PR. Characterization of adrenal masses using unenhanced CT: an analysis of the CT literature. AJR Am J Roentgenol. 1998;171(1):201-204. [DOI] [PubMed] [Google Scholar]
- 295. Peña CS, Boland GW, Hahn PF, Lee MJ, Mueller PR. Characterization of indeterminate (lipid-poor) adrenal masses: use of washout characteristics at contrast-enhanced CT. Radiology. 2000;217(3):798-802. [DOI] [PubMed] [Google Scholar]
- 296. Szolar DH, Korobkin M, Reittner P, et al. Adrenocortical carcinomas and adrenal pheochromocytomas: mass and enhancement loss evaluation at delayed contrast-enhanced CT. Radiology. 2005;234(2):479-485. [DOI] [PubMed] [Google Scholar]
- 297. Seo JM, Park BK, Park SY, Kim CK. Characterization of lipid-poor adrenal adenoma: chemical-shift MRI and washout CT. AJR Am J Roentgenol. 2014;202(5):1043-1050. [DOI] [PubMed] [Google Scholar]
- 298. Sahdev A. Recommendations for the management of adrenal incidentalomas: what is pertinent for radiologists? Br J Radiol. 2017;90(1072):20160627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299. Marty M, Gaye D, Perez P, et al. Diagnostic accuracy of computed tomography to identify adenomas among adrenal incidentalomas in an endocrinological population. Eur J Endocrinol. 2018;178(5):439-446. [DOI] [PubMed] [Google Scholar]
- 300. Korobkin M, Brodeur FJ, Francis IR, Quint LE, Dunnick NR, Londy F. CT time-attenuation washout curves of adrenal adenomas and nonadenomas. AJR Am J Roentgenol. 1998;170(3):747-752. [DOI] [PubMed] [Google Scholar]
- 301. Angelelli G, Mancini ME, Moschetta M, Pedote P, Pignataro P, Scardapane A. MDCT in the differentiation of adrenal masses: comparison between different scan delays for the evaluation of intralesional washout. ScientificWorldJournal. 2013;2013:957680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Park BK, Kim CK, Kwon GY, Kim JH. Re-evaluation of pheochromocytomas on delayed contrast-enhanced CT: washout enhancement and other imaging features. Eur Radiol. 2007;17(11):2804-2809. [DOI] [PubMed] [Google Scholar]
- 303. Hartman R, Kawashima A, Takahashi N, et al. Applications of dual-energy CT in urologic imaging: an update. Radiol Clin North Am. 2012;50(2):191-205, v. [DOI] [PubMed] [Google Scholar]
- 304. Patel J, Davenport MS, Cohan RH, Caoili EM. Can established CT attenuation and washout criteria for adrenal adenoma accurately exclude pheochromocytoma? AJR Am J Roentgenol. 2013;201(1):122-127. [DOI] [PubMed] [Google Scholar]
- 305. Marin D, Boll DT, Mileto A, Nelson RC. State of the art: dual-energy CT of the abdomen. Radiology. 2014;271(2):327-342. [DOI] [PubMed] [Google Scholar]
- 306. Connolly MJ, McInnes MDF, El-Khodary M, McGrath TA, Schieda N. Diagnostic accuracy of virtual non-contrast enhanced dual-energy CT for diagnosis of adrenal adenoma: a systematic review and meta-analysis. Eur Radiol. 2017;27(10):4324-4335. [DOI] [PubMed] [Google Scholar]
- 307. Caoili EM, Korobkin M, Francis IR, et al. Adrenal masses: characterization with combined unenhanced and delayed enhanced CT. Radiology. 2002;222(3):629-633. [DOI] [PubMed] [Google Scholar]
- 308. Mitchell DG, Crovello M, Matteucci T, Petersen RO, Miettinen MM. Benign adrenocortical masses: diagnosis with chemical shift MR imaging. Radiology. 1992;185(2):345-351. [DOI] [PubMed] [Google Scholar]
- 309. Schieda N, Siegelman ES. Update on CT and MRI of adrenal nodules. AJR Am J Roentgenol. 2017;208(6):1206-1217. [DOI] [PubMed] [Google Scholar]
- 310. Platzek I, Sieron D, Plodeck V, Borkowetz A, Laniado M, Hoffmann RT. Chemical shift imaging for evaluation of adrenal masses: a systematic review and meta-analysis. Eur Radiol. 2019;29(2):806-817. [DOI] [PubMed] [Google Scholar]
- 311. Kim SJ, Lee SW, Pak K, Kim IJ, Kim K. Diagnostic accuracy of 18F-FDG PET or PET/CT for the characterization of adrenal masses: a systematic review and meta-analysis. Br J Radiol. 2018;91(1086):20170520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Mayo-Smith WW, Song JH, Boland GL, et al. Management of incidental adrenal masses: a white paper of the ACR incidental findings committee. J Am Coll Radiol. 2017;14(8):1038-1044. [DOI] [PubMed] [Google Scholar]
- 313. Maurea S, Mainolfi C, Bazzicalupo L, et al. Imaging of adrenal tumors using FDG PET: comparison of benign and malignant lesions. AJR Am J Roentgenol. 1999;173(1):25-29. [DOI] [PubMed] [Google Scholar]
- 314. Yun M, Kim W, Alnafisi N, Lacorte L, Jang S, Alavi A. 18F-FDG PET in characterizing adrenal lesions detected on CT or MRI. J Nucl Med. 2001;42(12):1795-1799. [PubMed] [Google Scholar]
- 315. Metser U, Miller E, Lerman H, Lievshitz G, Avital S, Even-Sapir E. 18F-FDG PET/CT in the evaluation of adrenal masses. J Nucl Med. 2006;47(1):32-37. [PubMed] [Google Scholar]
- 316. Young WF Jr. Management approaches to adrenal incidentalomas. A view from Rochester, Minnesota. Endocrinol Metab Clin North Am. 2000;29(1):159-85, x. [DOI] [PubMed] [Google Scholar]
- 317. Olsen H, Nordenström E, Bergenfelz A, Nyman U, Valdemarsson S, Palmqvist E. Subclinical hypercortisolism and CT appearance in adrenal incidentalomas: a multicenter study from Southern Sweden. Endocrine. 2012;42(1):164-173. [DOI] [PubMed] [Google Scholar]
- 318. Morelli V, Palmieri S, Salcuni AS, et al. Bilateral and unilateral adrenal incidentalomas: biochemical and clinical characteristics. Eur J Endocrinol. 2013;168(2):235-241. [DOI] [PubMed] [Google Scholar]
- 319. Vassilatou E, Vryonidou A, Ioannidis D, Paschou SA, Panagou M, Tzavara I. Bilateral adrenal incidentalomas differ from unilateral adrenal incidentalomas in subclinical cortisol hypersecretion but not in potential clinical implications. Eur J Endocrinol. 2014;171(1):37-45. [DOI] [PubMed] [Google Scholar]
- 320. Vassiliadi DA, Ntali G, Stratigou T, Adali M, Tsagarakis S. Aberrant cortisol responses to physiological stimuli in patients presenting with bilateral adrenal incidentalomas. Endocrine. 2011;40(3):437-444. [DOI] [PubMed] [Google Scholar]
- 321. Pasternak JD, Seib CD, Seiser N, et al. Differences between bilateral adrenal incidentalomas and unilateral lesions. JAMA Surg. 2015;150(10):974-978. [DOI] [PubMed] [Google Scholar]
- 322. Androulakis II, Kaltsas GA, Markou A, et al. The functional status of incidentally discovered bilateral adrenal lesions. Clin Endocrinol (Oxf). 2011;75(1):44-49. [DOI] [PubMed] [Google Scholar]
- 323. De Venanzi A, Alencar GA, Bourdeau I, Fragoso MC, Lacroix A. Primary bilateral macronodular adrenal hyperplasia. Curr Opin Endocrinol Diabetes Obes. 2014;21(3):177-184. [DOI] [PubMed] [Google Scholar]
- 324. El Ghorayeb N, Bourdeau I, Lacroix A. Multiple aberrant hormone receptors in Cushing’s syndrome. Eur J Endocrinol. 2015;173(4):M45-M60. [DOI] [PubMed] [Google Scholar]
- 325. Bourdeau I, El Ghorayeb N, Gagnon N, Lacroix A. Management of endocrine disease: differential diagnosis, investigation and therapy of bilateral adrenal incidentalomas. Eur J Endocrinol. 2018;179(2):R57-R67. [DOI] [PubMed] [Google Scholar]
- 326. Pencharz D, Nathan M, Wagner TL. Evidence-based management of incidental focal uptake of fluorodeoxyglucose on PET-CT. Br J Radiol. 2018;91(1084):20170774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327. Del Monte P, Bernasconi D, Bertolazzi L, et al. Increased 17 alpha-hydroxyprogesterone response to ACTH in silent adrenal adenoma: cause or effect? Clin Endocrinol (Oxf). 1995;42(3):273-277. [DOI] [PubMed] [Google Scholar]
- 328. Osswald A, Quinkler M, Di Dalmazi G, et al. Long-term outcome of primary bilateral macronodular adrenocortical hyperplasia after unilateral adrenalectomy. J Clin Endocrinol Metab. 2019;104(7):2985-2993. [DOI] [PubMed] [Google Scholar]
- 329. Ierardi AM, Petrillo M, Patella F, et al. Interventional radiology of the adrenal glands: current status. Gland Surg. 2018;7(2):147-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330. Bancos I, Tamhane S, Shah M, et al. Diagnosis of endocrine disease: The diagnostic performance of adrenal biopsy: a systematic review and meta-analysis. Eur J Endocrinol. 2016;175(2):R65-R80. [DOI] [PubMed] [Google Scholar]
- 331. Sharma KV, Venkatesan AM, Swerdlow D, et al. Image-guided adrenal and renal biopsy. Tech Vasc Interv Radiol. 2010;13(2):100-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332. Gaujoux S, Mihai R; joint working group of ESES and ENSAT . European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal Tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br J Surg. 2017;104(4):358-376. [DOI] [PubMed] [Google Scholar]
- 333. Sturgeon C, Shen WT, Clark OH, Duh QY, Kebebew E. Risk assessment in 457 adrenal cortical carcinomas: how much does tumor size predict the likelihood of malignancy? J Am Coll Surg. 2006;202(3):423-430. [DOI] [PubMed] [Google Scholar]
- 334. David Connor SB. Perioperative care of phaeochromocytoma. BJA Education. 2016; 16:153-158. [Google Scholar]
- 335. Wang W, Hu W, Zhang X, Wang B, Bin C, Huang H. Predictors of successful outcome after adrenalectomy for primary aldosteronism. Int Surg. 2012;97(2):104-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Mellon MJ, Sethi A, Sundaram CP. Laparoscopic adrenalectomy: Surgical techniques. Indian J Urol. 2008;24(4):583-589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337. Walz MK, Alesina PF, Wenger FA, et al. Posterior retroperitoneoscopic adrenalectomy–results of 560 procedures in 520 patients. Surgery. 2006;140(6):943-948; discussion 948. [DOI] [PubMed] [Google Scholar]
- 338. Berber E, Tellioglu G, Harvey A, Mitchell J, Milas M, Siperstein A. Comparison of laparoscopic transabdominal lateral versus posterior retroperitoneal adrenalectomy. Surgery. 2009;146(4):621-625; discussion 625. [DOI] [PubMed] [Google Scholar]
- 339. Ball MW, Allaf ME. Robotic adrenalectomy: the jury is still out. Gland Surg. 2015;4(4):277-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340. Zografos GN, Vasiliadis G, Farfaras AN, Aggeli C, Digalakis M. Laparoscopic surgery for malignant adrenal tumors. Jsls. 2009;13(2):196-202. [PMC free article] [PubMed] [Google Scholar]
- 341. Araujo-Castro M, Sampedro Núñez MA, Marazuela M. Autonomous cortisol secretion in adrenal incidentalomas. Endocrine. 2019;64(1):1-13. [DOI] [PubMed] [Google Scholar]
- 342. Arlt W, Biehl M, Taylor AE, et al. Urine steroid metabolomics as a biomarker tool for detecting malignancy in adrenal tumors. J Clin Endocrinol Metab. 2011;96(12):3775-3784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343. Kotłowska A, Maliński E, Sworczak K, Kumirska J, Stepnowski P. The urinary steroid profile in patients diagnosed with adrenal incidentaloma. Clin Biochem. 2009;42(6):448-454. [DOI] [PubMed] [Google Scholar]
- 344. Storbeck KH, Schiffer L, Baranowski ES, et al. Steroid metabolome analysis in disorders of adrenal steroid biosynthesis and metabolism. Endocr Rev. 2019;40(6):1605-1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345. Crowley RK, Hughes B, Gray J, et al. Longitudinal changes in glucocorticoid metabolism are associated with later development of adverse metabolic phenotype. Eur J Endocrinol. 2014;171(4):433-442. [DOI] [PubMed] [Google Scholar]
- 346. Tomlinson JW, Finney J, Hughes BA, Hughes SV, Stewart PM. Reduced glucocorticoid production rate, decreased 5alpha-reductase activity, and adipose tissue insulin sensitization after weight loss. Diabetes. 2008;57(6):1536-1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Krone N, Hughes BA, Lavery GG, Stewart PM, Arlt W, Shackleton CH. Gas chromatography/mass spectrometry (GC/MS) remains a pre-eminent discovery tool in clinical steroid investigations even in the era of fast liquid chromatography tandem mass spectrometry (LC/MS/MS). J Steroid Biochem Mol Biol. 2010;121(3-5):496-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348. Kerkhofs TM, Kerstens MN, Kema IP, Willems TP, Haak HR. Diagnostic value of urinary steroid profiling in the evaluation of adrenal tumors. Horm Cancer. 2015;6(4):168-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349. Velikanova LI, Shafigullina ZR, Lisitsin AA, et al. Different types of urinary steroid profiling obtained by high-performance liquid chromatography and gas chromatography-mass spectrometry in patients with adrenocortical carcinoma. Horm Cancer. 2016;7(5-6):327-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350. Bancos I, Arlt W. Diagnosis of a malignant adrenal mass: the role of urinary steroid metabolite profiling. Curr Opin Endocrinol Diabetes Obes. 2017;24(3):200-207. [DOI] [PubMed] [Google Scholar]
- 351. Chortis V, Bancos I, Nijman T, et al. Urine steroid metabolomics as a novel tool for detection of recurrent adrenocortical carcinoma. J Clin Endocrinol Metab. 2020;105(3):e307-e318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352. Schweitzer S, Kunz M, Kurlbaum M, et al. Plasma steroid metabolome profiling for the diagnosis of adrenocortical carcinoma. Eur J Endocrinol. 2019;180(2):117-125. [DOI] [PubMed] [Google Scholar]
- 353. Taylor DR, Ghataore L, Couchman L, et al. A 13-steroid serum panel based on LC-MS/MS: use in detection of adrenocortical carcinoma. Clin Chem. 2017;63(12):1836-1846. [DOI] [PubMed] [Google Scholar]
- 354. Lippert J, Appenzeller S, Liang R, et al. Targeted molecular analysis in adrenocortical carcinomas: a strategy toward improved personalized prognostication. J Clin Endocrinol Metab. 2018;103(12):4511-4523. [DOI] [PubMed] [Google Scholar]
- 355. Jouinot A, Assie G, Libe R, et al. DNA methylation is an independent prognostic marker of survival in adrenocortical cancer. J Clin Endocrinol Metab. 2017;102(3):923-932. [DOI] [PubMed] [Google Scholar]
- 356. Zheng S, Cherniack AD, Dewal N, et al. ; Cancer Genome Atlas Research Network . Comprehensive pan-genomic characterization of adrenocortical carcinoma. Cancer Cell. 2016;29(5):723-736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357. Sarkar SD, Cohen EL, Beierwaltes WH, Ice RD, Cooper R, Gold EN. A new and superior adrenal imaging agent, 131I-6beta-iodomethyl-19-nor-cholesterol (NP-59): evaluation in humans. J Clin Endocrinol Metab. 1977;45(2):353-362. [DOI] [PubMed] [Google Scholar]
- 358. Yen RF, Wu VC, Liu KL, et al. ; TAIPAI Study Group . 131I-6beta-iodomethyl-19-norcholesterol SPECT/CT for primary aldosteronism patients with inconclusive adrenal venous sampling and CT results. J Nucl Med. 2009;50(10):1631-1637. [DOI] [PubMed] [Google Scholar]
- 359. Wu MH, Liu FH, Lin KJ, Sun JH, Chen ST. Diagnostic value of adrenal iodine-131 6-beta-iodomethyl-19-norcholesterol scintigraphy for primary aldosteronism: a retrospective study at a medical center in North Taiwan. Nucl Med Commun. 2019;40(6):568-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360. Powlson AS, Gurnell M, Brown MJ. Nuclear imaging in the diagnosis of primary aldosteronism. Curr Opin Endocrinol Diabetes Obes. 2015;22(3):150-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361. Hahner S, Sundin A. Metomidate-based imaging of adrenal masses. Horm Cancer. 2011;2(6):348-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Weber MM, Lang J, Abedinpour F, Zeilberger K, Adelmann B, Engelhardt D. Different inhibitory effect of etomidate and ketoconazole on the human adrenal steroid biosynthesis. Clin Investig. 1993;71(11):933-938. [DOI] [PubMed] [Google Scholar]
- 363. Hennings J, Sundin A, Hägg A, Hellman P. 11C-metomidate positron emission tomography after dexamethasone suppression for detection of small adrenocortical adenomas in primary aldosteronism. Langenbecks Arch Surg. 2010;395(7):963-967. [DOI] [PubMed] [Google Scholar]
- 364. Burton TJ, Mackenzie IS, Balan K, et al. Evaluation of the sensitivity and specificity of (11)C-metomidate positron emission tomography (PET)-CT for lateralizing aldosterone secretion by Conn’s adenomas. J Clin Endocrinol Metab. 2012;97(1):100-109. [DOI] [PubMed] [Google Scholar]
- 365. O’Shea PM, O’Donoghue D, Bashari W, et al. 11 C-Metomidate PET/CT is a useful adjunct for lateralization of primary aldosteronism in routine clinical practice. Clin Endocrinol (Oxf). 2019;90(5):670-679. [DOI] [PubMed] [Google Scholar]
- 366. Bongarzone S, Basagni F, Sementa T, et al. Development of [18F]FAMTO: A novel fluorine-18 labelled positron emission tomography (PET) radiotracer for imaging CYP11B1 and CYP11B2 enzymes in adrenal glands. Nucl Med Biol. 2019;68-69:14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367. Hahner S, Stuermer A, Kreissl M, et al. [123I]Iodometomidate for molecular imaging of adrenocortical cytochrome P450 family 11B enzymes. J Clin Endocrinol Metab. 2008;93(6):2358-2365. [DOI] [PubMed] [Google Scholar]
- 368. Hahner S, Kreissl MC, Fassnacht M, et al. Functional characterization of adrenal lesions using [123I]IMTO-SPECT/CT. J Clin Endocrinol Metab. 2013;98(4):1508-1518. [DOI] [PubMed] [Google Scholar]
- 369. Kreissl MC, Schirbel A, Fassnacht M, et al. [¹²³I]Iodometomidate imaging in adrenocortical carcinoma. J Clin Endocrinol Metab. 2013;98(7): 2755-2764. [DOI] [PubMed] [Google Scholar]
- 370. Hahner S, Kreissl MC, Fassnacht M, et al. [131I]iodometomidate for targeted radionuclide therapy of advanced adrenocortical carcinoma. J Clin Endocrinol Metab. 2012;97(3):914-922. [DOI] [PubMed] [Google Scholar]
- 371. Avram AM, Fig LM, Gross MD. Adrenal gland scintigraphy. Semin Nucl Med. 2006;36(3):212-227. [DOI] [PubMed] [Google Scholar]
- 372. Pentlow KS, Graham MC, Lambrecht RM, et al. Quantitative imaging of iodine-124 with PET. J Nucl Med. 1996;37(9):1557-1562. [PubMed] [Google Scholar]
- 373. Wong KK, Waterfield RT, Marzola MC, et al. Contemporary nuclear medicine imaging of neuroendocrine tumours. Clin Radiol. 2012;67(11):1035-1050. [DOI] [PubMed] [Google Scholar]
- 374. Pandit-Taskar N, Zanzonico P, Staton KD, et al. Biodistribution and dosimetry of 18F-meta-fluorobenzylguanidine: a first-in-human PET/CT imaging study of patients with neuroendocrine malignancies. J Nucl Med. 2018;59(1):147-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375. Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278(2):563-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Lambin P, Rios-Velazquez E, Leijenaar R, et al. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012;48(4):441-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377. Summers RM. Texture analysis in radiology: does the emperor have no clothes? Abdom Radiol (NY). 2017;42(2):342-345. [DOI] [PubMed] [Google Scholar]
- 378. Zhang GM, Shi B, Sun H, Jin ZY, Xue HD. Differentiating pheochromocytoma from lipid-poor adrenocortical adenoma by CT texture analysis: feasibility study. Abdom Radiol (NY). 2017;42(9):2305-2313. [DOI] [PubMed] [Google Scholar]
- 379. Shi B, Zhang GM, Xu M, Jin ZY, Sun H. Distinguishing metastases from benign adrenal masses: what can CT texture analysis do? Acta Radiol. 2019;60(11):1553-1561. [DOI] [PubMed] [Google Scholar]
- 380. Ho LM, Samei E, Mazurowski MA, et al. Can texture analysis be used to distinguish benign from malignant adrenal nodules on unenhanced CT, contrast-enhanced CT, or in-phase and opposed-phase MRI? AJR Am J Roentgenol. 2019;212(3):554-561. [DOI] [PubMed] [Google Scholar]
- 381. Nakajo M, Jinguji M, Nakajo M, et al. Texture analysis of FDG PET/CT for differentiating between FDG-avid benign and metastatic adrenal tumors: efficacy of combining SUV and texture parameters. Abdom Radiol (NY). 2017;42(12):2882-2889. [DOI] [PubMed] [Google Scholar]
- 382. Choy G, Khalilzadeh O, Michalski M, et al. Current applications and future impact of machine learning in radiology. Radiology. 2018;288(2):318-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383. Romeo V, Maurea S, Cuocolo R, et al. Characterization of adrenal lesions on unenhanced MRI using texture analysis: a machine-learning approach. J Magn Reson Imaging. 2018;48(1):198-204. [DOI] [PubMed] [Google Scholar]
- 384. Yi X, Guan X, Chen C, et al. Adrenal incidentaloma: machine learning-based quantitative texture analysis of unenhanced CT can effectively differentiate sPHEO from lipid-poor adrenal adenoma. J Cancer. 2018;9(19):3577-3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article or in the data repositories listed in References.